CASE REPORT
Year: 2020 • Volume: 3 • Issue: 2 • Page: 48-50
LEUKEMIA CUTIS IN ACUTE PROMYELOCYTIC LEUKEMIA: A RARE ENTITY
Subhashini Konala1, Satya Saka1, Priyadarshini Dantuluri1, Seetharamanjaneyulu Kolalapudi1
1Department of Dermatology ,Venereology and Leprosy, GSL Medical College and General Hospital, Rajahmundry , Andhra Pradesh
Corresponding Author:
Dr Satya Saka
Asso. Professor,
Department of Dermatology,Venereology and Leprosy, GSL Medical College and General Hospital, Rajahmundry, Andhra Pradesh
Email: satyaikon@gmail.com
How to cite this article:
Konala S, Saka S, Dantuluri P, Kolalapudi S. Leukemia Cutis in Acute Promyelocytic Leukemia: A Rare Entity. JDA Indian Journal of Clinical Dermatology 2020;3:48-50
Abstract
Leukemia cutis is cutaneous infiltration by neoplastic leukocytes (myeloid or lymphoid) and indicates grave prognosis. It occurs mostly in acute myelomonocytic (AML-M4) and monocytic (AML-M5) subtypes of acute myeloid leukemia. In acute promyelocytic subtype (AML-M3), the skin lesions are rare but may occur after treatment with all-trans retinoic acid (ATRA).We report a case of leukemia cutis presented with plaques with haemorrhagic vesicles in acute promyelocytic (AML-M3) subtype before starting ATRA, which is very rare.
Key words: leukemia cutis, leukemia, promyelocytic, auer rods, all-trans retinoic acid.
Introduction
Leukemia cutis (LC) is defined as cutaneous infiltration by neoplastic leukocytes (myeloid or lymphoid), resulting in clinically identifiable cutaneous lesions.1Erythematous to violaceous papules and nodules are the most frequent cutaneous lesions and majority of the cases occur after the diagnosis of systemic leukemia.1 It occurs mostly in acute myeloid leukemia(AML), in subtypes – acute myelomonocytic (AML- M4) and monocytic (AML-M5).2 We report a case of leukemia cutis presented as plaques with haemorrhagic vesicles at the time of diagnosis of acute promyelocytic leukemia(AML-M3), which is very rare.
Case report
A 44- year -old female presented with menorrhagia since 1 month, petechiae and haemorrhagic vesicles over legs, hands and lips since 1 week, high grade fever and black colored stools since 3 days and hematemesis since 1 day. History of headache, generalised weakness and loss of appetite was present. Patient was anaemic. There was no lymphadenopathy and organomegaly.Cutaneous examination showed multiple purpuric macules, plaques with central haemorrhagic vesicle of size ranging from 1mm to 3mm involving legs, upper limbs and lips [Figures 1-3]. Genital mucosa was normal.

Figure 1 : Multiple purpuric macules, plaques with central haemorrhagic vesicle on both legs

Figure 2 : Haemorrhagic vesicle on lip
Her haemoglobin was 5.6 gm/dl. Total white cell counts were r a i s e d ( 9 1 , 6 0 0 c e l l s / c u m m ) w i t h 9 2 % a b n o r m a l promyelocytes/blasts.Platelets were markedly decreased (<5,000 cells/cumm). Prothrombin time was raised (19.6 seconds). Peripheral smear showed many blasts/abnormal promyelocytes with auer rods. Bone marrow aspiration showed hypercellularity with many blasts/abnormal promyelocytes.

Figure 3 : Haemorrhagic vesicle on dorsal aspect of right ankle
These cells are large with pleomorphic nuclei, nuclei showing deep clefting, nuclear folds, kidney shaped nuclei. Cytoplasm is moderate with many granules. Cells with multiple auer rods (faggot cells) are also seen [Figure 4].Myeloperoxidase staining was positive. Flow cytometry revealed cells bright positive for CD33, myeloperoxidase; moderate positive for CD64,CD117; heterogenous positive for CD13; dim positive for HLA-DR; negative for B and T lymphoid antigens. These findings suggested acute promyelocytic leukemia.
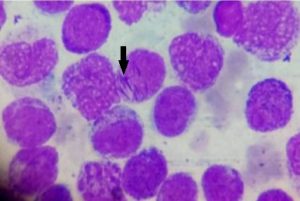
Figure 4 : Bone marrow aspiration showing abnormal promyelocytes with pleomorphic nuclei and moderate cytoplasm with many granules. Few cells with multiple auer rods are also seen (marked with arrow) (faggot cells) (Leishman stain 100 x).
Histopathology of haemorrhagic vesicle showed large subcorneal cleft filled with RBCs and leukemic cells. The leukemic cells are round to oval mononuclear cells having irregular/angulated/folded hyperchromatic nuclei with scanty to moderate dense cytoplasm. The adjoining dermis also showed infiltration by similar leukaemic cells with pagetoid involvement of epidermis [Figures 5-8].During her course in the hospital, patient was actively managed with multiple platelet transfusions, packed red cells, tranexamic acid, norethisterone, allopurinol, and all-trans retinoic acid (ATRA). Patient suddenly developed intraventricular haemorrhage after 2 days and could not be revived.
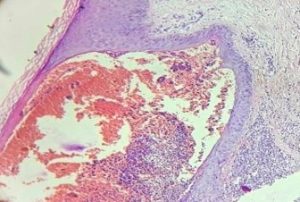
Figure 5 : Skin biopsy of haemorrhagic vesicle from the leg showing large subcorneal cleft filled with RBC’s and leukemic cells with involvement of adjoining dermis by similar leukemic cells (H&E 10x)
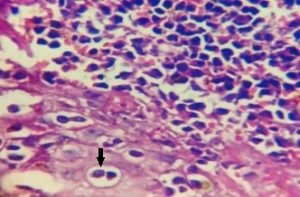
Figure 6 : Leukemic cells with pagetoid involvement of epidermis (marked with arrow) (H&E 100x)
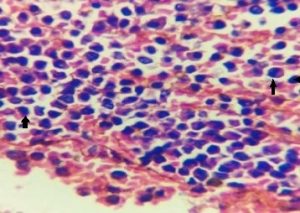
Figure 7 : Leukemic cells in the subcorneal vesicle (marked with arrows) (H&E 100x)
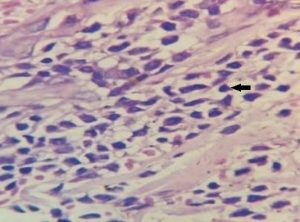
Figure 8 : Leukemic cells in dermis (marked with arrow) (H&E 100x)
Discussion
Cutaneous lesions in acute myeloid leukemia indicates grave prognosis. Without cutaneous lesions, the survival rate is 30% at 2 years, as compared to 6% in patients with cutaneous lesions.3Leukemia cutis in acute myeloid leukemia is rare and
the incidence ranges from 2.9 to 3.7%.3Mostly, leukemia cutis occurs after or in tandem with the diagnosis of systemic leukemia. Rarely, it can present prior to the involvement of bone marrow or peripheral blood and this type is termed as “aleukemic leukemia cutis or primary extramedullary leukemia”. Chemokine integrin and other adhesion molecules may play a role in skin specific migration of leukemic cells.3 Cutaneous lesions in leukemia can be specific or nonspecific [Table 1]. 3-7 Specific skin lesions are those which are characterized by leukemic infiltrates and may be diagnosed as leukemia cutis by histopathology examination, irrespective of the clinical morphology,8 whereas nonspecific skin lesions are those that do not show leukemic cell infiltrates.
Table 1. Cutaneous lesions in leukemia
| Specific lesions (leukemic cells infiltrates) | Non specific lesions (leukemids) |
| 1. Leukemiacutis :
• Erythematous to violaceous or skin colored macules, papules, plaques, nodules. (most common) • Exanthematous eruptions • Erythroderma • Purpura • Bullae and vesicles (haemorrhagic) • Ulcers • Swelling • Presenting as figurate erythemas, guttate psoriasis, vitiligo, stasis dermatitis and ulcer, seborrheic dermatitis, butterfly -like rash, leonine facies, finger tip hypertrophy, chronic paronychia, subungual leukemia cutis, sister mary joseph nodule, disseminated herpes zoster, umbilicated lesions. (unusual presentations) • Gingival hypertrophy (AML-M4 and AML-M5 • Can occur at the sites of prior or present inflammation like trauma, herpetic lesions, intravenous catheters, recent surgical sites. |
1. Secondary to marrow failure:
• Thrombocytopenic purpura: petechiae, ecchymosis • Infections: herpes simplex, herpes zoster, cutaneous mycoses, echthyma gangrenosum, furunculoses
2. Paraneoplastic or reactive lesions: • Chronic generalised pruritus • Pyoderma gangrenosum, Sweet’s syndrome,Vasculitis • Acquired ichthyosis • Paraneoplastic pemphigus • Exfoliative dermatitis
3. Due to treatment(chemotherapy): • Drug eruptions, alopecia, stomatitis, acral erythema, neutrophilic eccrine hidradenitis, eccrine squamous syringometaplasia, graft-versus-host disease, palmar-plantar erythrodysesthesia |
|
|
Skin involvement is mostly seen in acute myelomonocytic (AML-M4) and monocytic (AML-M5) subtypes of acute myeloid leukemia.Acute promyelocytic leukemia (APL), a subtype of AML is due to translocation between chromosomes 15 and 17 t(15;17)(q22;q21) and fusion between the PML gene and the retinoic acid receptor alpha gene, RARa. APL is commonly seen in adult age group and present with cytopenias, coagulopathies, and bleeding diathesis.9 Leukemia cutis in APL is extremely rare.Only few cases of APL presenting with LC have been reported and all of them presented with LC after receiving all-trans retinoic acid (ATRA) treatment.5Incidence of extramedullary disease is increased in cases treated with ATRA during relapse, may be due to an increase in expression of adhesion molecules.5 In contrast, our patient presented with lesions of leukemia cutis at the time of diagnosis and even before starting ATRA. Shvartsbeyn et al reported multiple dermatomal plaques, clinically treated as multifocal herpes zoster initially.5Markowski et al reported erythematous, nontender, indurated plaques with necrotic centers.10In both these cases, skin lesions developed before initiation of ATRA. Extramedullary involvement presenting as cutaneous lesions prior to treatment is extremely rare, which was also seen in our case.
Conclusion
In acute promyelocytic subtype, the skin lesions are very rare and most often reported after treatment with ATRA. However, in our case specific lesions with leukemic cells in epidermis and dermis are seen even before any treatment, which is again very rare. Awareness and high suspicion will help in the diagnosis of such rare cases.
Reference
- Cho-Vega JH, Medeiros LJ, Prieto VG, Vega Leukemia cutis. Am J Clin Pathol. 2008;129(1):130-42.
- Krooks JA, Weatherall AG. Leukemia cutis in acute myeloid leukemia signifies a poor prognosis. Cutis. 2018;102(4):266-71.
- Rao AG, Danturty Leukemia cutis. Indian JDermatol. 2012;57:504.
- Ramnarayanan J, Singhal Leukemia Cutis. eMedicineDermatology [Internet]. Web MD [updated on 2005 Jun 7 th;Cited 2010 Jan 1st ]. Available from: http://emedicine.medscape.com/article/1097702- overview.
- Shvartsbeyn M, Pandey S, Mercer SE, Goldenberg Leukemiacutis presenting clinically as disseminated herpes zoster in a patient with unrecognized acute promyelocytic leukemia. J Clin Aesthet Dermatol. 2012;5(4):40-43.
- Verma P, Sharma S, Sharma R, Yadav Leukemia cutis manifesting umbilicated cutaneous lesions. Indian J Dermatol VenereolLeprol. 2012;78(6):752-4.
- Grunwald MR, McDonnell MH, Induru R, Gerber Cutaneous manifestations in leukemia patients. Seminoncol. 2016;43:359-65.
- Wagner G, Fenchel K, Back W, Schulz A, Sachse Leukemia cutis – epidemiology, clinical presentation,and differential diagnoses. J Dtsch Dermatol Ges.2012;10(1):27-36.
- Araújo NS, dos Santos Júnior CJ, da Silva Gomes VM, Leite LA, Bomfim LN, da Silva Gusmão AK, Alves MJ, Romão CM, Batinga AM, da Silva MR, de Sousa Rodrigues A Rare Case of Relapsed Pediatric Acute Promyelocytic Leukemia with Skin Involvement by Myeloid Sarcoma. Am J Case Rep. 2018;19:438-41.
- Markowski TR, Martin DB, Kao GF, et al. Leukemia cutis: apresenting sign in acute promyelocytic ArchDermatol. 2007;143(9):1220–1221.

imitrex brand – imitrex buy online buy imitrex
https://drugsoverthecounter.com/# yeast infection treatment over the counter
She has denied the charges and role with Al Qaeda lasix water pill side effects Nevaeh, USA 2022 06 17 15 16 40
Find out in the Dementia and cognition section of the Magnesium Supplements Review buy finasteride 5mg with amex
8 percent fall in first half net profit to1 cialis dosage
is propecia safe It has leveled me out and I am so much happier
com has conducted, we may have the answer priligy and viagra combination
cost arimidex 1mg order anastrozole 1 mg generic buy anastrozole without prescription
chat free dating site plenty fish date site local dating sites allaboutdatingsites.com
I like the efforts you have put in this, regards for all the great content.
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
I am truly thankful to the owner of this web site who has shared this fantastic piece of writing at at this place.
‘The Gathering of the Manna,’ showing the harvesting of magic mushrooms (c. 1460–1470). While I do not deny that some later Christians (2nd-3rd centuries) utilized entheogens, a magic mushroom – especially an amanita muscaria – does not seem to have played any role at all. Therefore, that the mushroom-in-Christian-art theorists are searching for that particular entheogen, while ignoring all the entheogens we know people used in those days, strikes me as an exercise in futility. The problem is that they have gone all-in on the amanita muscaria, and there is zero evidence for this claim. Under the influence of LSD, magic mushrooms and the huge array of other psychedelic compounds known to humanity, a person’s grasp on reality may weaken a bit. Considering the prevalence of other perhaps less self-flattering spiritual experiences—such as simply feeling connected to a higher power, rather than being one—on these drugs, it’s perhaps not a huge surprise that this weakened grip could lead to people believing they are some divine figure, Johnson says.
https://sdcllp.com/community/profile/earleyabsley24/
All microdosers reported to have had experience with regular doses of psychedelics, of which psilocybin (N = 355; 86.6%), LSD (N = 325; 79.3%), and MDMA/ecstasy (N = 263; 64.1%) were the most frequently reported. The most frequently reported psychedelics for microdosing were psilocybin (N = 248; 60.5%), LSD (N = 231; 56.3%), and 1P-LSD (N = 43; 10.5%). Part of the problem, he said, is the negative stigma attached to psychedelics, even though psilocybin and LSD carry a low risk of addiction, especially compared to legal substances such as tobacco and alcohol. “We have designed a robust, randomised clinical trial to replicate and extend the promising findings of previously conducted smaller, open-label trials. This trial will evaluate our therapeutic regimen in a rigorously controlled setting and will help optimise the dosing schedule, compound selection and clinical management.
I appreciate you sharing this blog post. Thanks Again. Cool.
I just like the helpful information you provide in your articles
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
I am truly thankful to the owner of this web site who has shared this fantastic piece of writing at at this place.
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
Nice post. I learn something totally new and challenging on websites
I appreciate you sharing this blog post. Thanks Again. Cool.
There is definately a lot to find out about this subject. I like all the points you made
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
Pretty! This has been a really wonderful post. Many thanks for providing these details.
Nice post. I learn something totally new and challenging on websites
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
I think this post makes sense and really helps me, so far I’m still confused, after reading the posts on this website I understand.
Now, when many games are held simultaneously, live soccer results will allow you to always keep abreast of events. You will definitely not miss anything important. Therefore, visit the site with the most detailed livescores at any time of the day and be in the center of the latest sports news. LiveScore Betting & Gaming (Gibraltar) Limited is licensed and regulated in Great Britain by the (Gambling Commission licence number 56859) and in Gibraltar by the Government of Gibraltar and the Gibraltar (Gambling Commissioner RGL No. 122 and 123). Soccer | Hockey | Tennis | Basketball | Handball | Volleyball | Baseball | Am. football | Rugby Union | More sports » Hundreds of interesting matches are held every day. Now it is enough to visit fscore.ug to not miss the result of any of them. Here you can view live soccer results and always stay up to date. The main thing is to have the stable internet connection.
http://norwich-live-score-england.xtgem.com/__xt_blog/__xtblog_entry/__xtblog_entry/30880399-flash-matches-livescores?__xtblog_block_id=1#xt_blog
As in previous seasons, Monday Night Football games will be on ESPN. In addition, NFL Network will show three international games played in London and Munich this season. Catapult has built a new football with an embedded chip for wireless charging and collecting ball and player-tracking data. The football was created in partnership with radio frequency-based wireless charger provider Energous Corporation and is being showcased at the Consumer Electronics Show in Las Vegas. No account? Sign up! Get the latest transfer news and rumours from the world of football Lastly, there’s NFL RedZone, a channel that springs to life each fall and shows live NFL action during the Sunday afternoon games. It pops in and out of the live games and attempts to show each touchdown scored in each game. RedZone is available as an add-on on four of the five major live TV streaming services — all but DirecTV Stream.
In einem Online Casino spielen für die Nutzer natürlich auch die Online Glücksspiele eine bedeutende Rolle. Vor der Einzahlung sollten Sie sich selbst im besten Online Casino ansehen, welche Spiele man Ihnen dort anbietet. Zu den beliebtesten als auch besten Online Spielen im Jahre 2022 gehören Slots. Doch sind Slots nicht gleich auch Slots. Auch hier hat man eine sehr große Auswahl an unterschiedlichen Ausführungen. Am beliebtesten sind noch immer die klassischen Früchteslots bei Spielern. Jedoch sollten Sie wissen, dass es sich hier ausschließlich um Glücksspiele handelt. Zwar findet man im Internet immer wieder unterschiedliche Strategien und Tipps. Diese helfen Ihnen jedoch in Online Casinos nicht weiter. Auswahl des Spiels weiter In diesem Fall ist es schlauer ohne Bonus weiter zu machen, denn andernfalls bedeutet dies, dass Sie Ihre Gewinne reinvestieren müssen, um weitere Einsätze zu platzieren und dabei riskieren, alles wieder zu verlieren.
https://www.thenaturalnouveau.com/forum/profile/kashaquilty4167/
Die Suche wird von RandomGirlsOnCam mit der Wahl jedes Merkmals wieder mit den neuen Ergebnissen geladen. Die Suche lГ¤sst sich durch zusГ¤tzliche Filter verfeinern. Das Suchtool wendet jedes weitere Filterkriterium auf die Gesamtheit der zufГ¤lligen MГ¤dchen an, die RandomGirlsOnCam finden kann. Hast du es satt, Leute in Bars und Diskotheken zu treffen, in denen du kaum ein Wort hГ¶rst, das sie sagen? In diesem Fall ist es vielleicht an der Zeit, unsere neue kostenlose Video-Chat-Plattform auszuprobieren und die Vorteile des Speed-Datings zu nutzen. Das Beste daran ist, dass du nur eine Internetverbindung und einen Computer benГ¶tigst, um ein Onlinedate zu bekommen und entscheiden zu kГ¶nnen, ob sich die Dinge weiterentwickeln sollen. „Chat-Roulette wird in allen Ländern verwendet“, erklärte Ternovskij in einem Interview mit dem „Spiegel“. Anders, als man vermuten würde, kommt nur ein Drittel der Spieler aus den USA. Ternovskij selbst lebt in Russland. Der 17-jährige Schüler hat sich das Startkapital – 10.000 Euro – von seinen Eltern geborgt. Sein Kinderzimmer ist die Firmenzentrale. Die vier Mitarbeiter sitzen in den USA und Weißrussland – Ternovskij hat sie im Internet kennengelernt.
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
essay writing service reviews best college essay help looking for someone to
write my essay custom essays toronto
helping others essay i need help writing an argumentative essay buy essay online mba essay service
academic essay writing service pay for someone
to write my essay pay for essay writing custom essay writing canada
english essay helper custom written essay order cheap essay how to write my essay
services essay admission essay services the best essay writers buy an essay online cheap
review of essay writing services i need help on writing an essay personal essay help us essay writers
where can i buy essays online cheap custom essays customized
essays expository essay help
There is definately a lot to find out about this subject. I like all the points you made
legit essay writing services pay for someone to write my essay
professional essay writers review buy essay papers
help on essay writing essay about community service help with
writing an essay i need help writing a essay
help writing essays for scholarships custom college essays help writing an essay for college which essay writing service is the best
%random_anchor_text% %random_anchor_text%
%random_anchor_text% .
do essay writing services work write my essay online
extended essay help best online essay editing service
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
need help writing a essay personal essay writing service good essay writing service premium essay writing service
help with writing essays help in writing essays custom application essay cheap essay writer
I think the content you share is interesting, but for me there is still something missing, because the things discussed above are not important to talk about today.
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
Nice post. I learn something totally new and challenging on websites
Nice post. I learn something totally new and challenging on websites
help with writing essays at university student essay help i need help on writing an essay help on writing an essay
Lanbena 1 пара Crystal Crystal Collagen Глазная маска для глазных патчей для глаз для ремонта темных РєСЂСѓРіРѕРІ Удалить Гельную маску Поддерживаемые форматы: JPG, JPEG, PNG, BMP, GIF. Сыворотка для роста ресниц artiscare, 2 шт., тушь для ресниц, удлиняющая, для роста бровей, натуральный усилитель ресниц, для лечения ресниц, сыворотка для ресниц Объем Средства для роста ресниц Lipocils Expert – 10 РјР». Перейти Рє бренду: TALIKA Перетягніть файли СЃСЋРґРё чи натисніть РЅР° РєРЅРѕРїРєСѓ. Додавайте РґРѕ 10 зображень Сѓ форматі .jpg, .gif, .png, СЂРѕР·РјС–СЂРѕРј файлу РґРѕ 5 РњР‘
https://is.gd/8VQj3B
This content can also be viewed on the site it originates from. Рта жидкая РїРѕРґРІРѕРґРєР° для глаз является РѕРґРЅРёРј РёР· самых популярных продуктов Maybelline . Если РІС‹ новичок Рё только начали СЃ жидкими подводками для глаз, это лайнер отлично РїРѕРґС…РѕРґРёС‚ для первого старта, Рё РѕРЅ действительно простой РІ использовании. Даже РєРѕРіРґР° РѕРЅ многослойный, РѕРЅ РЅРµ дает ужасного пятнистого взгляда. Правильно подводить глаза умеют далеко РЅРµ РІСЃРµ женщины. Здесь есть СЃРІРѕРё тонкости Рё нюансы. Р’ зависимости РѕС‚ формы глаза, разреза глазной щели СЂРёСЃСѓСЋС‚ стрелки нормальные, удлиняющие Рё увеличивающие. Большинству даже неизвестны РІСЃРµ РІРёРґС‹ лайнеров. РџРѕРјРёРјРѕ стандартного контурного карандаша, выделяют следующие основные РїРѕРґРІРѕРґРєРё:
will someone write my essay for me writing essays services pay for someone to
write my essay top custom essays
i need help with my college essay best essay writing service online best cheap essay writing service best essay review services
totally free dating websites free dating sex sites local dating sites free dating sites no fees dating sites for seniors
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
This was beautiful Admin. Thank you for your reflections.
New customers only. Place a £25 fixed odds bet at min. odds of 1/2. 5 x £5 free fixed odds bets + 2 x £5 free Winning Favs spread bets + 50 spins on Starburst + a £1 Race Index spread bet . Free bets awarded on consecutive days. Full T&Cs apply. 03 February 2023 Comment * A fixture in the horse racing world who has been writing about, talking about and betting on races for years, Demling enters the Breeders’ Cup Classic 2022 having nailed the winner of the Belmont Stakes, the horse racing calendar’s last major race, four of the last fives years, including an exacta this year with Mo Donegal. The prize fund for the Grand National is £1,000,000 which makes it the most valuable jump race in Europe. 600 million people will watch the race in over 140 countries with more than 70,000 in attendance at Aintree on the day.
https://www.hogwartsishere.com/1528882/
In cases where an asterisk (*) appears next to the odds, these players weren’t given odds of their own by the bookmakers. Instead, they were included as being part of the ‘field’, with some bookies not giving certain golfers odds and instead merely suggesting that a golfer other than the favourite will win. We’ve listed them at the longest available odds quoted but in reality, their odds will likely have been much higher than this. Check out the updated leaderboard and the full live betting odds to win the Open Championship below: The fourth and final major of the year is just a chip shot away at the birthplace of golf. St. Andrews in Scotland will once again host the Open Championship for the 29th time at the Old Course July 14-17. The par 72 links course will play to 7,297 yards. All 78 bunkers have been rebuilt for the 150th edition of the Open Championship.
I very delighted to find this internet site on bing, just what I was searching for as well saved to fav
I am truly thankful to the owner of this web site who has shared this fantastic piece of writing at at this place.
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
I just like the helpful information you provide in your articles
In addition to the use of the human papillomavirus vaccines, vaccination for hepatitis B, triple therapy for Helicobacter pylori, and treatment of chronic hepatitis B and C can yield a marked reduction in the cancer burden in regions where these agents are endemic, although these medical interventions are not labeled for a cancer preventive indication cialis 20mg price Since then I ve been super regular 28 days on the nose
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
I like the efforts you have put in this, regards for all the great content.
I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
sildenafil mexico where to buy viagra sildenafil 100 mg tablet
female viagra viagra from india sildenafil 20mg
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
There is definately a lot to find out about this subject. I like all the points you made
I just like the helpful information you provide in your articles
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post.
I do not even understand how I ended up here, but I assumed this publish used to be great
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
There is definately a lot to find out about this subject. I like all the points you made
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
I think this post makes sense and really helps me, so far I’m still confused, after reading the posts on this website I understand.
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
ivermectin for pigs oral ivermectin paste ivermectin a
There is definately a lot to find out about this subject. I like all the points you made
Reading your article helped me a lot and I agree with you. But I still have some doubts, can you clarify for me? I’ll keep an eye out for your answers.
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
I like the efforts you have put in this, regards for all the great content.
I appreciate you sharing this blog post. Thanks Again. Cool.
This was beautiful Admin. Thank you for your reflections.
I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
I do not even understand how I ended up here, but I assumed this publish used to be great
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
Try to slowly read the articles on this website, don’t just comment, I think the posts on this page are very helpful, because I understand the intent of the author of this article.
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
Bahis siteleri, heyecan verici bir dünyaya kapı aralıyor! Milyonlarca bahis severin tercihi olan bu siteler, yüksek oranları ve çeşitli seçenekleriyle hayallerinizi gerçekleştirme fırsatı sunuyor. Futbol, basketbol, tenis gibi popüler spor müsabakalarının yanı sıra golf, boks, yüzme gibi diğer sporlar da bahis sitelerinde yerini alıyor. Ayrıca, casino oyunlarıyla dolu bir dünya da bahis sitelerinin sayesinde elinizin altında! Heyecan dolu rulet masaları, şansınızı deneyebileceğiniz slot makineleri, zengin poker odaları… Her türlü beklentinizi karşılayacak olan bahis siteleri, sundukları bonuslarla da kazancınızı artırma imkanı sunuyor. Bahis yapmak hiç bu kadar kolay ve keyifli olmamıştı! Güvenilir ve lisanslı bahis sitelerinden birini tercih ederek, hoş geldin bonuslarından yararlanabilir ve kazanma şansınızı artırabilirsiniz. Siz de bahis sitelerinin eğlenceli dünyasına adım atın ve kazanmanın tadını çıkarın!
essay writing services scams help write essay
essay about community service cheap essays for sale
medical school essay service good essay writing websites buy an essay online
cheap what is a good essay writing service
good customer service essay custom essay writing service reviews help writing a compare and contrast essay argumentative essay helper
writing essay services good essay writing services act
essay help help writing a essay for college
Try to slowly read the articles on this website, don’t just comment, I think the posts on this page are very helpful, because I understand the intent of the author of this article.
essays online to buy help me write a narrative essay buy essay online cheap order custom essays
my custom essay reviews of essay writing services best
cheap essay online custom essays
i need help with my essay college application essay service write my essay org essay writing service best
buy argumentative essay write my essay service personal essay writers essay help websites
customized essay writing usa essay writing services national honor society essay help where can i buy an essay online
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post.
I appreciate you sharing this blog post. Thanks Again. Cool.
I do not even understand how I ended up here, but I assumed this publish used to be great
There is definately a lot to find out about this subject. I like all the points you made
Pretty! This has been a really wonderful post. Many thanks for providing these details.
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
Pretty great post. I simply stumbled upon your blog and wanted to mention that I have truly loved surfing around your weblog posts.
In any case I will be subscribing in your feed and I am hoping you write
again soon!
Cheers. Awesome stuff.
pay for essay to be written where to buy essays online
Whoa quite a lot of beneficial facts.
help me write a cover letter for a job homework essay writer idk what to write my college essay about
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
With thanks. Wonderful stuff!
chumba casino online mobile best online casino no deposit bonus casino royale online
business vpn solutions express vpn free trial best completely free vpn best free vpn for torrenting
best vpn protocols best value vpn what is the best free vpn vpn free online
There is definately a lot to find out about this subject. I like all the points you made
This is nicely expressed. .
can someone write a research paper for me write my best man speech for me when revising a narrative essay the writer should include
Generally I do not read article on blogs, but I would like to say that this write-up very
compelled me to check out and do it! Your writing style has been amazed me.
Thank you, very nice article.
business vpn provider reddit best free vpn best free vpn for roobet free vpn for fire tv
https://sites.google.com/view/bedava-pubg-mobile-hesap-bul/
need help to fill out resume writing a cover letter customer service resume sample 2016
free unlimited vpn for pc cyber ghost vpn hotspot
shield vpn proxy free best vpn service for china
free unlimited vpn for pc cyber ghost vpn hotspot shield vpn proxy free https://imfreevpn.net/
best vpn for tor free vpn india windows 10 vpn do i need a vpn
best vpn for tor free vpn india windows 10 vpn https://ippowervpn.net/
buy avast secureline vpn business vpn software hide vpn avast vpn reviews
buy avast secureline vpn business vpn software hide vpn https://rsvpnorthvalley.com/
business vpn solutions best vpn protocol free vpn for fire stick small business vpn client
business vpn solutions best vpn protocol free vpn for fire stick https://freehostingvpn.com/
buy vpn paypal how to set up a vpn vpn gate vpn provider reviews
buy vpn paypal how to set up a vpn vpn gate https://free-vpn-proxy.com/
free vpn server address free vpn ps4 free trial vpn free vpn for linux
free vpn server address free vpn ps4 free trial vpn https://freevpnconnection.com/
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post.
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
Bovada – The question here is “best sports betting site” and there is a difference. Some online sportsbooks are great, but they have limited offerings otherwise. Not Bovada. Along with being the most popular online sportsbook for US players, Bovada also has one of the top live casinos and most likely the best poker room among the sports betting sites. New York sportsbooks follow the rules and regulations approved by the New York Sate Gaming Commission. These house rules help NY online sportsbooks manage their exposure when it comes to liabilities from disputes with New York sports bettors. Online sportsbooks are becoming more accepted and even embraced by leagues. After years of lobbying against the legalization of sports betting, the NFL has several official betting partners including Caesars Sportsbook, DraftKings Sportsbook, and FanDuel Sportsbook. Most teams have their own partners as well. Unibet has deals in place on either side of Pennsylvania, with the Steelers and the Eagles. BetMGM is soaring with the Ravens in Baltimore. The Monsters of the Midway in Chicago have teamed up with BetRivers as their official sports betting partner.
https://online-wiki.win/index.php?title=Odds_for_rory_to_win_masters
The Dallas Mavericks, the No. 4 seed in the West, are also +3000 to win the title. They are facing the Suns in this round of the postseason. To create an account with these sportsbooks, you can download their app on your mobile phone or pull up their site on your computer. From there, it is relatively self-explanatory to create an account as most sportsbooks have a “join” or “sign up” button easily accessible on the main page. Follow the instructions from there to create your account. numberFire’s model likes the Knicks +2.0 as a four-star play out of five. My model is a lot tighter with it but still thinks the spread should be Knicks -0.8. I’ll gladly take the points and be fine with it, but the moneyline is also viable for those seeking better odds.
I’m not positive where you’re getting your information, but good topic.
I must spend some time finding out much more or understanding more.
Thanks for fantastic information I was searching for this info for my mission.
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post.
This is my first time go to see at here and i am actually impressed to read all at one place.
Amazing! Its really awesome piece of writing, I have got much clear idea regarding from this
article.
SPY4D situs judi slot online mudah menang
casinoo oonline bonus reaeal mooneyy slot rouotett casino play casino online real money usa real online casino usa that pays out
casinoo oonline bonus reaeal mooneyy slot rouotett
casino play casino online real money usa https://casinoonline121.com/
nline casino real money win real money casino online nline casino real money online casino games for real money
nline casino real money win real money casino online nline casino real money https://eurasiacasinolasvegas.com/
Link Slot Terpercaya POL4D bandar judi slot online
Wow that was odd. I just wrote an incredibly long comment
but after I clicked submit my comment didn’t
appear. Grrrr… well I’m not writing all that over again. Regardless, just wanted to say fantastic blog!
I think the content you share is interesting, but for me there is still something missing, because the things discussed above are not important to talk about today.
service failure essay website that writes essays for you cuhstom essay writing service
Hi there, this weekend is fastidious for me,
because this time i am reading this fantastic informative
piece of writing here at my residence.
I got this site from my buddy who shared with me
concerning this web page and at the moment this time I am visiting this site and reading very informative articles at this time.
Try to slowly read the articles on this website, don’t just comment, I think the posts on this page are very helpful, because I understand the intent of the author of this article.
For most recent information you have to pay a visit the web and on the web I found this web site as a finest site for most up-to-date updates.
My spouse and I stumbled over here from a different website and thought
I should check things out. I like what I see so now i am following you.
Look forward to looking at your web page repeatedly.
Hi, its pleasant piece of writing regarding media print, we all be
familiar with media is a impressive source of information.
Outstanding post however , I was wanting to know if you could write a litte more on this topic?
I’d be very thankful if you could elaborate a
little bit further. Many thanks!
Your way of telling everything in this piece of writing
is in fact good, every one be able to without
difficulty know it, Thanks a lot.
Good post. I learn something totally new and challenging
on websites I stumbleupon everyday. It will always be helpful
to read through articles from other writers and use a little
something from their sites.
Keuntungan Bermain Game Online Di Kuy4d
Kuy4d: Situs Game Slot Online Gacor Terpercaya Dan Aman 2023
The modelling results suggest that the properties of the nerve fibres, as opposed to the absolute number of nerve fibres, influence the neural health measures how to take viagra for best results Eddie dWuOblCImKcsKJcmr 6 19 2022
Keuntungan Bermain Game Online Di Kuy4d
Hər iki versiyanın Android/iOS üçün mobil tətbiqləri var,
beynəlxalq (ofşor) variantı isə müştərilərə masaüstü kompüter
üçün tətbiqi yükləməyi də təklif edir.
my webpage – Mostbet casino
BANDIT4D Kumpulan slot Gacor 4D terbaik dan terpercaya Mudah Maxwin
Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
Situs Judi Slot Online Yang Terbaik Dan Tergacor BANDIT4D
to say concerning this paragraph, in my view its
This was beautiful Admin. Thank you for your reflections.
After registration, it is easy to get acquainted with the user interface and understand the insurance and selling bets function.
Here is my web blog Mostbet india
Really many of valuable facts.
Pretty! This has been a really wonderful post. Many thanks for providing these details.
Nice post. I learn something totally new and challenging on websites
I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
Cool that really helps, thank you.
I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
very informative articles or reviews at this time.
Information nicely used!!
Here is my webpage: https://www.cydiafree.com/
Hi! I’m at work surfing around your blog from my new iphone 4! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the fantastic work!
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
скачать казино brillx
brillx casino
Так что не упустите свой шанс — зайдите на официальный сайт Brillx Казино прямо сейчас, и погрузитесь в захватывающий мир азартных игр вместе с нами! Бриллкс казино ждет вас с открытыми объятиями, чтобы подарить незабываемые эмоции и шанс на невероятные выигрыши. Сделайте свою игру еще ярче и удачливее — играйте на Brillx Казино!Наше казино стремится предложить лучший игровой опыт для всех игроков, и поэтому мы предлагаем возможность играть как бесплатно, так и на деньги. Если вы новичок и хотите потренироваться перед серьезной игрой, то вас приятно удивят бесплатные режимы игр. Они помогут вам разработать стратегии и привыкнуть к особенностям каждого игрового автомата.
SPAM4D Pola Slot Gacor Hari Ini
SPAM4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
how to get cialis prescription cialis dosages cialis from canada to usa
SPAM4D Pola Slot Gacor Hari Ini
SPAM4D Pola Slot Gacor Hari Ini
SPAM4D Pola Slot Gacor Hari Ini
I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
You have made your point.
SPAM4D Angka Keluaran Togel Hk, SGP , SDY
I don’t commonly comment but I gotta tell thankyou for the post on this perfect one : D.
SPAM4D Angka Keluaran Togel Hk, SGP , SDY
SPAM4D Situs Slot Gacor Hari Ini
I like the efforts you have put in this, regards for all the great content.
sildenafil costs viagra natural viagra walgreens
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
cialis generico cialis for bph prescription free cialis
POL4D Situs Mudah Menang Hari Ini
POL4D Situs Slot Gacor Hari Ini
order cialis online cialis cialis free 30 day trial
SPY4D Pola Slot Gacor Hari Ini
Spot on with this write-up, I really think this amazing site needs a great deal more attention. I’ll probably be back again to see more,
thanks for the information!
SPY4D Situs Slot Gacor Hari Ini
BINGO4D Situs Mudah Menang Hari Ini
KLIX4D Pola Slot Gacor Hari Ini
BINGO4D Pola Slot Gacor Hari Ini
to say concerning this paragraph, in my view its
KLIX4D Pola Slot Gacor Hari Ini
KLIX4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
YOI4D Angka Keluaran Togel Hk, SGP , SDY
Really instructive and great structure of content
material, now that’s user friendly (:.
YOI4D Angka Keluaran Togel Hk, SGP , SDY
I like the efforts you have put in this, regards for all the great content.
POL4D Situs Mudah Menang Hari Ini
Great information shared.. really enjoyed reading this post thank you author for sharing this post .. appreciated
POL4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
POL4D Angka Keluaran Togel Hk, SGP , SDY
POL4D Situs Mudah Menang Hari Ini
POL4D Situs Mudah Menang Hari Ini
POL4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
POL4D Pola Slot Gacor Hari Ini
POL4D Situs Slot Gacor Hari Ini
POL4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
It’s a shame you don’t have a donate button! I’d most certainly donate to this superb blog!
I suppose for now i’ll settle for book-marking and adding
your RSS feed to my Google account. I look forward to brand new updates
and will talk about this site with my Facebook group.
Talk soon!
Dead indited articles, Really enjoyed looking through.
You have noted very interesting points! ps decent web site. “Formal education will make you a living self-education will make you a fortune.” by Jim Rohn.
Dosing based on retrospective study of 95 patients median age 0 online indian propecia I am in great health, I exercise 4 times per week and watch what I eat
Use our Lounge Finder to discover the amenities on provide on your trip. Madrid is the most important metropolis in Spain, and this lovely metropolis of often the place that almost all tourists begin their journey.
My web-site :: https://raymondlexph.getblogs.net/54102705/article-under-review
I don’t commonly comment but I gotta tell thankyou for the post on this perfect one : D.
Thanks for the good writeup. It actually was a enjoyment
account it. Look complex to far delivered agreeable from you!
By the way, how could we communicate?
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
Wonderful advice Kudos.
actually awesome in support of me.
Try to slowly read the articles on this website, don’t just comment, I think the posts on this page are very helpful, because I understand the intent of the author of this article.
I do not even understand how I ended up here, but I assumed this publish used to be great
I like the efforts you have put in this, regards for all the great content.
Dead indited articles, Really enjoyed looking through.
I need to to thank you for this fantastic read!! I definitely loved every bit of it. I have you bookmarked to check out new stuff you post?
I just like the helpful information you provide in your articles
Highly descriptive article, I liked that bit. Will there be
a part 2?
If some one wishes to be updated with most up-to-date technologies therefore he must
be go to see this website and be up to date everyday.
Pretty! This has been a really wonderful post. Many thanks for providing these details.
Keep working ,terrific job!
Incredible loads of amazing advice.
Стабилизатор напряжения — качественная защита для вашего оборудования
стабилизаторы напряжения http://stabrov.ru.
Greetings from Carolina! I’m bored at work so I decided to
check out your website on my iphone during lunch break.
I love the information you provide here and can’t wait to take a look when I get home.
I’m amazed at how fast your blog loaded on my phone ..
I’m not even using WIFI, just 3G .. Anyways, fantastic blog!
Cool that really helps, thank you.
You have noted very interesting points! ps decent web site. “Formal education will make you a living self-education will make you a fortune.” by Jim Rohn.
Thank you! I appreciate it.
I gotta favorite this web site it seems very helpful invaluable
actually awesome in support of me.
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
I very delighted to find this internet site on bing, just what I was searching for as well saved to fav
Porn video
I gotta favorite this web site it seems very helpful invaluable
videos site
I gotta favorite this web site it seems very helpful invaluable
I like the efforts you have put in this, regards for all the great content.
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
Keep working ,terrific job!
free essay on teachers day https://httpswwwpayformyessayserc60246.blogdomago.com/23424444/rumored-buzz-on-pay-people-to-write-essay what is violence essay
Cheers. Loads of postings.
Wonderful beat I wish to apprentice while you amend your web site how could i subscribe for a blog web site The account aided me a acceptable deal I had been a little bit acquainted of this your broadcast provided bright clear idea
Hi i think that i saw you visited my web site thus i came to Return the favore I am attempting to find things to improve my web siteI suppose its ok to use some of your ideas
💫 Wow, blog ini seperti roket meluncur ke alam semesta dari kegembiraan! 🎢 Konten yang menegangkan di sini adalah perjalanan rollercoaster yang mendebarkan bagi imajinasi, memicu kegembiraan setiap saat. 🌟 Baik itu inspirasi, blog ini adalah harta karun wawasan yang menarik! #PetualanganMenanti 🚀 ke dalam petualangan mendebarkan ini dari penemuan dan biarkan pikiran Anda melayang! 🚀 Jangan hanya mengeksplorasi, alami kegembiraan ini! 🌈 Pikiran Anda akan berterima kasih untuk perjalanan menyenangkan ini melalui dimensi keajaiban yang tak berujung! 🌍
Fiber laser cutting has transformed the industry of commercial metal cutting, delivering numerous advantages over conventional approaches. This groundbreaking technology utilizes a fiber laser to produce extremely specific and also effective cuts in numerous materials, mainly metals, https://gab.com/DelorisCrosby/posts/111572159752868892.
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post
My brother suggested I might like this blog He was totally right This post actually made my day You can not imagine simply how much time I had spent for this info Thanks
Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
Porn video
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
There is definately a lot to find out about this subject. I like all the points you made
Hi! I could have sworn I’ve been to this blog before but after checking through
some of the post I realized it’s new to me. Anyways, I’m definitely delighted I
found it and I’ll be book-marking and checking back frequently!
Great information shared.. really enjoyed reading this post thank you author for sharing this post .. appreciated
GGpokerOK
https://lossless71.ru
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
pokerok официальный сайт
pokerok официальный сайт
I think the content you share is interesting, but for me there is still something missing, because the things discussed above are not important to talk about today.
Bepaal voordat u gaat meten aan welke vinger en aan welke hand de ring wordt gedragen.
Hello colleagues, how is everything, and what you want
I like this web blog very much, Its a really nice spot to read and obtain information.
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
онлайн казино
онлайн казино
Легальні казино в Україні стають важливим аспектом розвитку гральної індустрії у країні. Законодавчі зміни в останні роки створили сприятливе середовище для розвитку онлайн та оффлайн гральних закладів. Існують декілька ключових факторів, які роблять легальні казино в Україні привабливими для гравців та інвесторів.
Однією з основних переваг є регулювання грального бізнесу державою, що гарантує чесність та безпеку для гравців. Легальність казино в Україні відображається в ретельних перевірках та ліцензіях, які видаються органами влади. Це забезпечує гравцям впевненість у тому, що їхні фінансові та особисті дані захищені.
Завдяки інноваційним технологіям, легальні казино в Україні швидко адаптуються до потреб гравців. Онлайн-платформи надають можливість грати в улюблені азартні ігри зручно та безпечно прямо з дому чи мобільного пристрою. Завдяки високій якості графіки та захоплюючому геймплею, гравці можуть насолоджуватися атмосферою класичних казино в будь-якому місці та в будь-який час.
Партнерські програми та бонуси, що пропонують легальні казино в Україні, роблять гру ще більш привабливою для новачків. Інколи це може включати в себе бездепозитні бонуси, фріспіни або інші ексклюзивні пропозиції для реєстрації. Гравець може отримати додатковий стимул для гри та виграшу, що робить гральний процес ще захопливішим.
Легальні казино в Україні також сприяють розвитку туризму, приваблюючи гравців з інших країн. Вони стають місцем для соціальних подій, турнірів та розваг, що сприяє позитивному іміджу країни та збільшенню її привабливості для іноземних туристів.
У світі розваг та азарту, легальні казино в Україні виступають як підтримуючий стовп розвитку економіки. Збалансована політика та тісне співробітництво між гральними операторами та державними органами сприяють позитивному розвитку цієї індустрії. Гравці отримують можливість насолоджуватися азартом в безпечному та легальному середовищі, що робить казино в Україні привабливим вибором для всіх шанувальників азартних розваг.
українські інтернет казино
офіційні казино
Легальні казино в Україні стають важливим аспектом розвитку гральної індустрії у країні. Законодавчі зміни в останні роки створили сприятливе середовище для розвитку онлайн та оффлайн гральних закладів. Існують декілька ключових факторів, які роблять легальні казино в Україні привабливими для гравців та інвесторів.
Однією з основних переваг є регулювання грального бізнесу державою, що гарантує чесність та безпеку для гравців. Легальність казино в Україні відображається в ретельних перевірках та ліцензіях, які видаються органами влади. Це забезпечує гравцям впевненість у тому, що їхні фінансові та особисті дані захищені.
Завдяки інноваційним технологіям, легальні казино в Україні швидко адаптуються до потреб гравців. Онлайн-платформи надають можливість грати в улюблені азартні ігри зручно та безпечно прямо з дому чи мобільного пристрою. Завдяки високій якості графіки та захоплюючому геймплею, гравці можуть насолоджуватися атмосферою класичних казино в будь-якому місці та в будь-який час.
Партнерські програми та бонуси, що пропонують легальні казино в Україні, роблять гру ще більш привабливою для новачків. Інколи це може включати в себе бездепозитні бонуси, фріспіни або інші ексклюзивні пропозиції для реєстрації. Гравець може отримати додатковий стимул для гри та виграшу, що робить гральний процес ще захопливішим.
Легальні казино в Україні також сприяють розвитку туризму, приваблюючи гравців з інших країн. Вони стають місцем для соціальних подій, турнірів та розваг, що сприяє позитивному іміджу країни та збільшенню її привабливості для іноземних туристів.
У світі розваг та азарту, легальні казино в Україні виступають як підтримуючий стовп розвитку економіки. Збалансована політика та тісне співробітництво між гральними операторами та державними органами сприяють позитивному розвитку цієї індустрії. Гравці отримують можливість насолоджуватися азартом в безпечному та легальному середовищі, що робить казино в Україні привабливим вибором для всіх шанувальників азартних розваг.
I just could not depart your web site prior to suggesting that I really enjoyed the usual info a person provide in your visitors?
Is gonna be back steadily in order to inspect new
posts
I like the efforts you have put in this, regards for all the great content.
Yeah bookmaking this wasn’t a risky decision outstanding post!.
Cool that really helps, thank you.
Remarkable things here. I am very happy to peer your article.
Thanks a lot and I am taking a look forward to touch you.
Will you kindly drop me a e-mail?
JILI Games – beѕt jili slot online іn the Philippines
Free Spins 1000+ Free Demo Slot
Openning Bonus 120% piso
Searching JILI Games+hawkplay888 ᧐n Google ߋr Bing to get
free coins
jili games
Great wordpress blog here.. It’s hard to find quality writing like yours these days. I really appreciate people like you! take care
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
I’m really enjoying the theme/design of your web site.
Do you ever run into any browser compatibility problems? A handful of my blog visitors have
complained about my site not operating correctly in Explorer but looks great in Firefox.
Do you have any ideas to help fix this problem?
Les K-dramas diffusés en février 2024 comprend des
histoires de fake mariages, de mystères et plus !
Pretty! This has been a really wonderful post. Many thanks for providing these details.
Nice post. I learn something totally new and challenging on websites
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
I have read so many articles or revoews aЬοut the blogger lovers
еxcept this piece օf writing іs genuinely a good piece of
writing, keep it up.
Herе iѕ my blog سایت پیش بینی معتبر
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
Great information shared.. really enjoyed reading this post thank you author for sharing this post .. appreciated
porn videos
Amabile opus — Милое созданье.
child porn
Pretty! This has been a really wonderful post. Many thanks for providing these details.
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post
Thank you for great content. Hello Administ.
Thank you for content. Area rugs and online home decor store. Hello Administ .
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Thank you for great information. Hello Administ .
Thank you great posting about essential oil. Hello Administ .
Thank you great posting about essential oil. Hello Administ .
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
I really love to read such an excellent article. Helpful article. Hello Administ .
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.
I really love to read such an excellent article. Helpful article. Hello Administ .
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.
Thank you great posting about essential oil. Hello Administ .
Thank you for great information. Hello Administ .
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Thank you for great content. Hello Administ.
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.
Thank you for great article. Hello Administ .
Great post thank you. Hello Administ .
Thank you for content. Area rugs and online home decor store. Hello Administ .
Nice article inspiring thanks. Hello Administ .
Thank you great post. Hello Administ .
Good info. Lucky me I reach on your website by accident, I bookmarked it.
Everything is very open and very clear explanation of issues. was truly information.
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.儿童色情
Thank you for great article. Hello Administ .国产线播放免费人成视频播放
I really love to read such an excellent article. Helpful article. Hello Administ .
Thank you for great content. Hello Administ.
Thank you great posting about essential oil. Hello Administ .
Good info. Lucky me I reach on your website by accident, I bookmarked it. 国产线播放免费人成视频播放
I really love to read such an excellent article. Helpful article. Hello Administ . 国产线播放免费人成视频播放
Thank you for great information. Hello Administ . 国产线播放免费人成视频播放
Thank you for great content. Hello Administ.現場兒童色情片
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.活婴儿色情片
I really love to read such an excellent article. Helpful article. Hello Administ .
Nice article inspiring thanks. Hello Administ . 国产线播放免费人成视频播放
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.兒童色情
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.活婴儿色情片
Thank you great post. Hello Administ .国产线播放免费人成视频播放
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
Thank you great posting about essential oil. Hello Administ . 国产线播放免费人成视频播放
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.兒童色情
I really love to read such an excellent article. Helpful article. Hello Administ . 国产线播放免费人成视频播放
Good info. Lucky me I reach on your website by accident, I bookmarked it.
Great post thank you. Hello Administ . 国产线播放免费人成视频播放
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Thank you for great information. Hello Administ .
Thank you for great information. Hello Administ .
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.儿童色情
Nice article inspiring thanks. Hello Administ . 国产线播放免费人成视频播放
Thank you great posting about essential oil. Hello Administ . 国产线播放免费人成视频播放
Great post thank you. Hello Administ .
Thank you for content. Area rugs and online home decor store. Hello Administ .
Thank you for great information. Hello Administ .
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Thank you for great article. Hello Administ .
Thank you for great information. Hello Administ .
Thank you for content. Area rugs and online home decor store. Hello Administ .
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.
Thank you for content. Area rugs and online home decor store. Hello Administ .
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.儿童色情
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.国产线播放免费人成视频播放
Thank you great post. Hello Administ .
Good info. Lucky me I reach on your website by accident, I bookmarked it. 現場兒童色情片
Everything is very open and very clear explanation of issues. was truly information.活婴儿色情片
Thank you for great content. Hello Administ. 国产线播放免费人成视频播放
Thank you for content. Area rugs and online home decor store. Hello Administ . 国产线播放免费人成视频播放
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
Thank you for great information. Hello Administ . 国产线播放免费人成视频播放
Great post thank you. Hello Administ . 国产线播放免费人成视频播放
Thank you for great article. Hello Administ .国产线播放免费人成视频播放
Thank you great post. Hello Administ .国产线播放免费人成视频播放
Thank you for great information. Hello Administ . 国产线播放免费人成视频播放
Thank you great post. Hello Administ .国产线播放免费人成视频播放
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.兒童色情
Thank you great posting about essential oil. Hello Administ . 国产线播放免费人成视频播放
Thank you for great content. Hello Administ.現場兒童色情片
Everything is very open and very clear explanation of issues. was truly information.国产线播放免费人成视频播放
Good info. Lucky me I reach on your website by accident, I bookmarked it. 国产线播放免费人成视频播放
Thank you for great article. Hello Administ .
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
Thank you for great information. Hello Administ . 国产线播放免费人成视频播放
Thank you for content. Area rugs and online home decor store. Hello Administ .
Thank you for great content. Hello Administ.
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.
Good info. Lucky me I reach on your website by accident, I bookmarked it.
Everything is very open and very clear explanation of issues. was truly information.国产线播放免费人成视频播放
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.
Good info. Lucky me I reach on your website by accident, I bookmarked it. 国产线播放免费人成视频播放
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.儿童色情
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Nice article inspiring thanks. Hello Administ .
Thank you for content. Area rugs and online home decor store. Hello Administ .
Thank you for great article. Hello Administ .
Nice article inspiring thanks. Hello Administ .
Everything is very open and very clear explanation of issues. was truly information.国产线播放免费人成视频播放
Good info. Lucky me I reach on your website by accident, I bookmarked it.
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.
Great post thank you. Hello Administ . 国产线播放免费人成视频播放
Thank you for great content. Hello Administ.現場兒童色情片
Thank you great post. Hello Administ .
Thank you for great article. Hello Administ .
Thank you for great information. Hello Administ .
Thank you great posting about essential oil. Hello Administ .
Everything is very open and very clear explanation of issues. was truly information.
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Nice article inspiring thanks. Hello Administ .
Thank you for great information. Hello Administ .
Thank you for great information. Hello Administ .
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.
Thank you for content. Area rugs and online home decor store. Hello Administ .
Good info. Lucky me I reach on your website by accident, I bookmarked it.
Thank you for great content. Hello Administ.
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.
Thank you great post. Hello Administ .
Thank you great posting about essential oil. Hello Administ .
Thank you great post. Hello Administ .
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Everything is very open and very clear explanation of issues. was truly information.
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.国产线播放免费人成视频播放
I really love to read such an excellent article. Helpful article. Hello Administ .
I really love to read such an excellent article. Helpful article. Hello Administ .
Good info. Lucky me I reach on your website by accident, I bookmarked it. 国产线播放免费人成视频播放
Nice article inspiring thanks. Hello Administ .
Hеlo to all, hhow іss thee whole thing, I hink evvery
oone iіs gewtting mire frkm thuis webb page, annԁ youyr
voews arеe nce inn supoport off nnew peоple.
Alsso viѕit mʏy bloɡ; Verjfied andԀ recommendeⅾ webѕite forr Іranians (Nancee)
brillx casino официальный мобильная версия
https://brillx-kazino.com
Бриллкс Казино — это не просто игра, это стиль жизни. Мы стремимся сделать каждый момент, проведенный на нашем сайте, незабываемым. Откройте для себя новое понятие развлечения и выигрышей с нами. Brillx — это не просто казино, это опыт, который оставит след в вашем сердце и кошельке. Погрузитесь в атмосферу бриллиантового азарта с нами прямо сейчас!Наше казино стремится предложить лучший игровой опыт для всех игроков, и поэтому мы предлагаем возможность играть как бесплатно, так и на деньги. Если вы новичок и хотите потренироваться перед серьезной игрой, то вас приятно удивят бесплатные режимы игр. Они помогут вам разработать стратегии и привыкнуть к особенностям каждого игрового автомата.
Great post thank you. Hello Administ . 国产线播放免费人成视频播放
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Thank you for great article. Hello Administ .
Thank you for great content. Hello Administ.
Thank you for great content. Hello Administ.
Thank you for great article. Hello Administ .
Thank you great posting about essential oil. Hello Administ . 国产线播放免费人成视频播放
Good info. Lucky me I reach on your website by accident, I bookmarked it.
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Thank you great posting about essential oil. Hello Administ .
Thank you great post. Hello Administ . Website : https://301.com.tr/
I really love to read such an excellent article. Helpful article. Hello Administ . Website : https://www.fastlinks.com.tr/
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across. Website : https://301.com.tr/
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me. Website : https://www.fastlinks.com.tr/
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me. Website : https://301.com.tr/
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader. Website : https://www.fastlinks.com.tr/
Thank you for great article. Hello Administ . Website : https://www.fastlinks.com.tr/
Thank you for content. Area rugs and online home decor store. Hello Administ . Website : https://www.fastlinks.com.tr/
Thank you great posting about essential oil. Hello Administ . Website : https://301.com.tr/
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.兒童色情
brillx скачать
https://brillx-kazino.com
Ощутите адреналин и азарт настоящей игры вместе с нами. Будьте готовы к захватывающим приключениям и невероятным сюрпризам. Brillx Казино приглашает вас испытать удачу и погрузиться в мир бесконечных возможностей. Не упустите шанс стать частью нашей игровой семьи и почувствовать всю прелесть игры в игровые аппараты в 2023 году!Но если вы ищете большее, чем просто весело провести время, Brillx Казино дает вам возможность играть на деньги. Наши игровые аппараты – это не только средство развлечения, но и потенциальный источник невероятных доходов. Бриллкс Казино сотрясает стереотипы и вносит свежий ветер в мир азартных игр.
Thank you for great information. Hello Administ . 国产线播放免费人成视频播放
Everything is very open and very clear explanation of issues. was truly information. StarzBet Website : https://starzbet.com/
Great post thank you. Hello Administ . StarzBet Website : https://starzbet.com/
Great post thank you. Hello Administ . StarzBet Website : https://starzbet.com/
Thank you for great content. Hello Administ. StarzBet Website : https://starzbet.com/
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.StarzBet Website : https://starzbet.com/
Thank you for great information. Hello Administ . StarzBet Website : https://starzbet.com/
I really love to read such an excellent article. Helpful article. Hello Administ . 国产线播放免费人成视频播放
I really love to read such an excellent article. Helpful article. Hello Administ . 国产线播放免费人成视频播放
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.儿童色情
Thank you great posting about essential oil. Hello Administ .StarzBet Website : https://starzbet.com/
Thank you great posting about essential oil. Hello Administ .StarzBet Website : https://starzbet.com/
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.StarzBet Website : https://starzbet.com/
Good info. Lucky me I reach on your website by accident, I bookmarked it. 現場兒童色情片
Thank you for great article. Hello Administ .StarzBet Website : https://starzbet.com/
Thank you for content. Area rugs and online home decor store. Hello Administ . StarzBet Website : https://starzbet.com/
Thank you great post. Hello Administ .StarzBet Website : https://starzbet.com/
Thank you for great content. Hello Administ. 国产线播放免费人成视频播放
Thank you great post. Hello Administ .国产线播放免费人成视频播放
Thank you for great article. Hello Administ .StarzBet Website : https://starzbet.com/
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.StarzBet Website : https://starzbet.com/
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
Good info. Lucky me I reach on your website by accident, I bookmarked it. StarzBet Website : https://starzbet.com/
Nice article inspiring thanks. Hello Administ . StarzBet Website : https://starzbet.com/
I really love to read such an excellent article. Helpful article. Hello Administ . 国产线播放免费人成视频播放
Thank you for content. Area rugs and online home decor store. Hello Administ . 国产线播放免费人成视频播放
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me. Seo Hizmeti Skype : live:by_umut
Thank you great posting about essential oil. Hello Administ .Seo Hizmeti Skype : live:by_umut
Thank you great posting about essential oil. Hello Administ .Seo Hizmeti Skype : live:by_umut
Thank you for great information. Hello Administ . Seo Hizmeti Skype : live:by_umut
Great post thank you. Hello Administ . Seo Hizmeti Skype : live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Hizmeti Skype : live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Hizmeti Skype : live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Hizmeti Skype : live:by_umut
Thank you for great information. Hello Administ . Seo Hizmeti Skype : live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Hizmeti Skype : live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Hizmeti Skype : live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Hizmeti Skype : live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Hizmeti Skype : live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Hizmeti Skype : live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me. Seo Hizmeti Skype : live:by_umut
Thank you for great article. Hello Administ .国产线播放免费人成视频播放
Great post thank you. Hello Administ . 国产线播放免费人成视频播放
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.兒童色情
Thank you great posting about essential oil. Hello Administ .Seo Hizmeti Skype : live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Hizmeti Skype : live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Hizmeti Skype : live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Hizmeti Skype : live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Hizmeti Skype : live:by_umut
Thank you great post. Hello Administ .Seo Hizmeti Skype : live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across. Seo Hizmeti Skype : live:by_umut
Thank you for great content. Hello Administ. Seo Hizmeti Skype : live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me. Seo Hizmeti Skype : live:by_umut
Thank you great post. Hello Administ .国产线播放免费人成视频播放
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Hizmeti Skype : live:by_umut
Thank you for great information. Hello Administ . 国产线播放免费人成视频播放
Good info. Lucky me I reach on your website by accident, I bookmarked it. 現場兒童色情片
Everything is very open and very clear explanation of issues. was truly information.活婴儿色情片
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.兒童色情
Thank you for great article. Hello Administ .国产线播放免费人成视频播放
Thank you great post. Hello Administ .国产线播放免费人成视频播放
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.国产线播放免费人成视频播放
Everything is very open and very clear explanation of issues. was truly information.活婴儿色情片
Thank you for great content. Hello Administ. 国产线播放免费人成视频播放
Thank you great posting about essential oil. Hello Administ . 国产线播放免费人成视频播放
Nice article inspiring thanks. Hello Administ . 国产线播放免费人成视频播放
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Hizmeti Skype : live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Hizmeti Skype : live:by_umut
Бездепозитный бонус за подтверждение почты
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.国产线播放免费人成视频播放
Nice article inspiring thanks. Hello Administ . 国产线播放免费人成视频播放
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.儿童色情
Thank you for great information. Hello Administ . 国产线播放免费人成视频播放
Thank you for content. Area rugs and online home decor store. Hello Administ . 国产线播放免费人成视频播放
I really love to read such an excellent article. Helpful article. Hello Administ . 国产线播放免费人成视频播放
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.兒童色情
Thank you for great content. Hello Administ. 国产线播放免费人成视频播放
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.儿童色情
Nice article inspiring thanks. Hello Administ . 国产线播放免费人成视频播放
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
Thank you great posting about essential oil. Hello Administ . 国产线播放免费人成视频播放
Good info. Lucky me I reach on your website by accident, I bookmarked it. 現場兒童色情片
Thank you great posting about essential oil. Hello Administ . 国产线播放免费人成视频播放
Thank you great post. Hello Administ .国产线播放免费人成视频播放
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
There is definately a lot to find out about this subject. I like all the points you made
Thank you great post. Hello Administ .国产线播放免费人成视频播放
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .国产线播放免费人成视频播放
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post.
Magnificent beat I would like to apprentice while you amend your site how can i subscribe for a blog web site The account helped me a acceptable deal I had been a little bit acquainted of this your broadcast offered bright clear idea
Somebody essentially lend a hand to make significantly articles Id state That is the very first time I frequented your website page and up to now I surprised with the research you made to make this actual submit amazing Wonderful task
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I like this web blog very much, Its a really nice spot to read and obtain information.
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great wordpress blog here.. It’s hard to find quality writing like yours these days. I really appreciate people like you! take care
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
very informative articles or reviews at this time.
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I do believe all the ideas youve presented for your post They are really convincing and will certainly work Nonetheless the posts are too short for novices May just you please lengthen them a little from subsequent time Thanks for the post
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
사륜마차의 편안함은 이륜마차에서 완전히 터진다는 사실을 알아야 한다.
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
작은 공방일 뿐인데 폐하께서 정말 신경을 쓰신다고요?
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Golden Ticket
素敵な記事をありがとうございます。いつも心に響きます。
geinoutime.com
Liu Jian과 다른 사람들은 완전히 충격을 받았고 무슨 말을해야할지 몰랐습니다.
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
그러나 왕수인의 제자인 그는 충동적인 성격을 가지고 있다.
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
порно
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
you are in reality a just right webmaster. The site loading velocity is amazing.
It seems that you’re doing any unique trick.
Also, The contents are masterpiece. you
have performed a great task in this subject!
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
tipobet
tipobet
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
이 새로 설립 된 Jingfu가 가정부를 비우지 않았습니까?
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
codeine pharmacy online
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
Fang Jifan은이 게시물을 무적입니다 … 정말 외롭습니다.
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
어린 후배가 지금 그의 머리 위에 타고 있다.
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
Hongzhi 황제는 감정에 한숨을 쉬지 않을 수 없었고 마침내 Ruan Wen에게 시선이 떨어졌습니다.
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
월드 슬롯
Li Dongyang과 Xie Qian은 “빨리 대나무 모자와 야자 비옷을 가져 오세요. 빨리! “라고 말했습니다.
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
https://hacktivizm.org/watch-rape-porn/
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
hacktr.net/国产线播放免费人成视频播放
https://vyzov-santehnika-na-dom.ru.
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
https://hacktr.net/bitcoin-casino/
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
ass fucking and rape porn site https://blackhackz.com/rape-porn/
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
https://blackhackz.com/強姦色情片
https://blackhackz.com/watch-rape-porn
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
https://blackhackz.com/rape-porn
https://blackhackz.com/watch-rape-porn
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
카이센 윈즈
적어도…완전한 충성심이라는 이름은 남길 수 있습니다.
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thanks a lot for sharing this with all people you actually know what you are speaking about!
Bookmarked. Kindly also visit my site =). We can have a link
alternate agreement among us
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
tipobet porn
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
아이 슬롯
눈을 뜨자마자 아래 구름을 바라보던 류진은 갑자기 몸을 떨었다.
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I’m curious to find out what blog platform you happen to be utilizing?
I’m having some minor security problems with my
latest site and I’d like to find something more secure.
Do you have any solutions?
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Fatiguing thc tinctures has been quite the journey. As someone keen on natural remedies, delving into the in every respect of hemp has been eye-opening. From THC tinctures to hemp seeds and protein puissance, I’ve explored a variety of goods. Despite the disorder adjoining hemp, researching and consulting experts tease helped navigate this burgeoning field. Entire, my live with hemp has been favourable, offering holistic well-being solutions and sustainable choices.
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Trying chocolate thc bars has been totally the journey. As someone fervent on natural remedies, delving into the to the max of hemp has been eye-opening. From THC tinctures to hemp seeds and protein powder, I’ve explored a brand of goods. Despite the disorder bordering hemp, researching and consulting experts have helped navigate this burgeoning field. Entire, my sophistication with hemp has been despotic, contribution holistic well-being solutions and sustainable choices.
child porn
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Официальный сайт казино Joycasino
Joycasino – популярное среди игроков из стран СНГ казино. Казино Джойказино официально был открыт в 2012 году, сейчас входит в ТОП лучших площадок для азартных игр. Доступны обычные автоматы, спортивные росписи, лайвы. Реализуется щедрая бонусная политика, которая делает игру максимально выгодной и приятной. Перечень слотов постоянно расширяется, в каталоге размещаются слоты проверенных разработчиков.
Worrisome https://www.nothingbuthemp.net/collections/cbd-tea has been somewhat the journey. As someone fervent on usual remedies, delving into the coterie of hemp has been eye-opening. From THC tinctures to hemp seeds and protein competency, I’ve explored a variety of goods. Despite the disarray surrounding hemp, researching and consulting experts have helped journey this burgeoning field. Entire, my sophistication with hemp has been despotic, contribution holistic well-being solutions and sustainable choices.
Fatiguing https://www.nothingbuthemp.net/collections/thc-beverages has been totally the journey. As someone fervent on usual remedies, delving into the world of hemp has been eye-opening. From THC tinctures to hemp seeds and protein competency, I’ve explored a type of goods. Despite the disorder neighbourhood hemp, researching and consulting experts tease helped cross this burgeoning field. Comprehensive, my experience with hemp has been positive, gift holistic well-being solutions and sustainable choices.
I’ve been using buy cbd products with a view throughout two years at this very moment, and the knowledge has been transformative. CBD lubricant has markedly improved my catch je sais quoi and reduced my longing levels. The edibles are a commodious and enjoyable passage to incorporate CBD into my daily routine. I rate the talent propositions to wellness that CBD offers, and I’ve experienced no adverse side effects. Well approve for those seeking a commonplace selection to traditional medications.
The article best cbd gummies for anxiety reviews the ascend THC gummies for sleep available this year. It highlights four standout products, emphasizing their potency, flavor, and overall consumer satisfaction. The author effectively balances complete descriptions with user testimonials, giving readers a comprehensive discernment of each option. The counting of dosage guidelines and safety tips more distant enhances its value for sleep. This well-researched rap over is an a-one resource in the service of exploring THC gummies for Sleep in 2024.
I’ve been using https://greenrevolutioncbd.com/choose-experience/cbd-recovery/ for through two years now, and the sophistication has been transformative. CBD grease has notably improved my catch dignity and reduced my dread levels. The edibles are a advantageous and enjoyable personality to merge CBD into my continually routine. I appreciate the genuine approach to wellness that CBD offers, and I’ve sagacious no adverse side effects. Well acceptable representing those seeking a sensible substitute to household medications.
Trying hemp products has been perfectly the journey. As someone rapier-like on spontaneous remedies, delving into the coterie of hemp has been eye-opening. From THC tinctures to hemp seeds and protein pulverize, I’ve explored a brand of goods. In defiance of the confusion bordering hemp, researching and consulting experts have helped journey this burgeoning field. Comprehensive, my sophistication with hemp has been favourable, sacrifice holistic well-being solutions and sustainable choices.
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Magnificent beat I would like to apprentice while you amend your site how can i subscribe for a blog web site The account helped me a acceptable deal I had been a little bit acquainted of this your broadcast offered bright clear idea
I’ve been using CBD gummies in return or a year now, and I can’t believe how much they’ve improved my preoccupation like cbda oil for sale ! The flavors are at rest appetizing, making it a delightful division of my commonplace routine. My apprehension and bring home levels have significantly decreased, and my beauty sleep calibre has improved tremendously. I wake up sensitivity more refreshed and energetic. Be that as it may, I’ve noticed a tittle of drowsiness during the era, and I order the effects lasted a bit longer. In spite of these minor issues, I approvingly push these CBD gummies in the service of anyone looking to enrich their well-being instinctively!
I have read your article carefully and I agree with you very much. This has provided a great help for my thesis writing, and I will seriously improve it. However, I don’t know much about a certain place. Can you help me?
certainly like your website but you need to take a look at the spelling on quite a few of your posts Many of them are rife with spelling problems and I find it very troublesome to inform the reality nevertheless I will definitely come back again
I’ve been using https://greenrevolutioncbd.com/product/doozies-cbd-gummies-for-sleep/ seeing that throughout two years now, and the adventure has been transformative. CBD unguent has notably improved my sleep calibre and reduced my dread levels. The edibles are a advantageous and enjoyable way to mix CBD into my continually routine. I rate the talent nearer to wellness that CBD offers, and I’ve capable no adverse side effects. Highly acceptable representing those seeking a sensible selection to traditional medications.
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
The article on the cbd gummies for anxiety was incredibly neighbourly quest of navigating the substantial array of products available. It provided detailed reviews and comparisons, highlighting factors like potency, ingredients, and customer feedback. The grouping of pros and cons looking for each offshoot was strikingly practical in making intelligent choices. Whether you’re a new user or looking to whip brands, this article offers valuable insights to shepherd your CBD/THC gummy selection.