ORIGINAL ARTICLE
Year: 2020 • Volume: 3 • Issue: 2 • Page: 27-30
A STUDY OF THE CUTANEOUS MANIFESTATIONS IN PATIENTS OF DIABETES MELLITUS
Shristhi Agrawal1, Kishor Singh1
1Department of Dermatology & VL, National Institute of Medical Sciences & Research, Jaipur- 303121, Rajasthan, India.
Corresponding Author:
Shristhi Agrawal
Department of Dermatology & VL,
National Institute of Medical Sciences & Research, Jaipur
Mail: srishti.agrawal92@gmail.com
How to cite this article:
Agrawal S, Singh K. A Study of The Cutaneous Manifestations In Patients Of Diabetes Mellitus. JDA Indian Journal of Clinical Dermatology 2020;3:27-30
Abstract
Introduction: The incidence of cutaneous manifestations in diabetes mellitus (DM) varies from 11.3% to 70.6%. The cutaneous manifestations seen in DM appear once the primary disease has developed, but it may also occur with its onset or may even precede DM in some of the cases. Our study is an attempt to analyse the pattern of various types of cutaneous manifestations seen in DM.
Aims & Objectives: To study and analyze the cutaneous manifestations in patients of diabetes mellitus.
Materials and methods: 100 patients with Diabetes Mellitus (type1 and type 2)were enrolled. Detailed history was taken Investigations like preprandial & postprandial capillary plasma glucose and HbA1C estimation was done. Diabetes was considered controlled when preprandial capillary plasma glucose was 3.9-7.2mmol/L (70-130 mg/dl), postprandial capillary plasma glucose < 180 mg/dl and HbA1C < 7.0%.
Results: Cutaneous infections were the commonest manifestations present in 71% of patients. Out of 100 patients 50 had a superficial fungal infection, 19 had bacterial infections and 6 had viral infections. Amongst cutaneous conditions associated with DM which were present in 67% of patient, skin tags were the commonest(33%). Miscellaneous cutaneous findings were present in 45% patients, nail discolouration was the commonest (11%).
Conclusion: Infections may appear early and remain undetected till DM is finally diagnosed. Majority of patients do not take regular treatment and follow dietary restrictions in early diabetes leading to persistent hyperglycaemic state which predisposes them to infections and other cutaneous manifestations. Presence of cutaneous manifestations must heighten the suspicion of a dermatologist in early diagnosis of DM.
Keywords: Diabetes Mellitus, cutaneous manifestations, cutaneous infections, skin tags, nail discolouration
Introduction
The World Health Organisation (WHO) describes diabetes mellitus (DM) as a chronic multisystem disorder with chronic hyperglycaemia, disturbances of fat, protein and carbohydrate metabolism because of a disturbance in insulin action, secretion or both.
Common symptoms in DM are polyuria, weight loss and blurring of vision, even coma and death can occur due to non- ketotic hyperosmolar state1. India has the world’s largest diabetic population which is approximately 51.8 million.2,3
Classification of Diabetes Mellitus4
- Diabetes Mellitus Type-1
- Diabetes Mellitus Type-2
- Other Specific Types of diabetes
- Gestational Diabetes Mellitus (GDM)
Cutaneous Manifestations
Acute metabolic disturbances and chronic degenerative complications of diabetes mellitus may also affect the skin. The incidence of cutaneous manifestations associated with diabetes mellitus varies from 11.3% to 70.6%.5 The cutaneous manifestations seen in DM mostly appear once the primary disease has already developed, but it may also occur coincidently
with its onset or may even precede DM by many years in some of the cases.
Cutaneous manifestations of diabetes mellitus may be classified as: 6
- Cutaneous infections in
- Cutaneous associations of
- Cutaneous manifestations of diabetic
- Cutaneous adverse reactions to the pharmacological treatment of
At times the cutaneous manifestations can be the first presenting sign of diabetes mellitus, hence our study is an attempt to analyse the pattern of various types of cutaneous manifestations seen in DM.
Aims and Objectives
To study and analyze the cutaneous manifestations in patients of diabetes mellitus.
Materials and Methods
The present study was carried out in the Department of Dermatology, Venereology and Leprosy at a tertiary care hospital in Jaipur. A total of 100 consecutive patients of Diabetes Mellitus (type1 & 2) attending the Department of Medicine and Dermatology were enrolled.
Ethics
Patient’s confidentiality was maintained and informed consent was taken for the study. The study was carried out after taking approval from the Institutional Review Board.
Inclusion Criteria:
- Diagnosed cases of Diabetes mellitus willing to participate in the
Exclusion Criteria:
- Patients less than 15 years of
- Patients with Gestational Diabetes
- Unwilling
Detailed history with special reference to age, sex, rural/urban background, BP, smoking, alcohol intake, duration of diabetes, type of diabetes, type of treatment being taken, complications and family history was taken. A complete general, physical, systemic and dermatological examination was carried in each patient.
Investigations like haemoglobin, total leukocyte count, differential cell count, preprandial capillary plasma glucose, postprandial capillary plasma glucose, complete urine examination and HbA1C were done in each patient. Assessment of glycaemic control was also done by measuring preprandial capillary plasma glucose, peak postprandial capillary plasma glucose.
Diabetes was considered to be controlled when preprandial capillary plasma glucose 3.9-7.2mmol/L (70-130 mg/dl), peak postprandial capillary plasma glucose < 180 mg/dl and HbA1C < 7.0%
Results
The study group included 100 patients of DM with cutaneous manifestations.
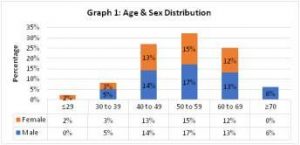
The age group varied from 20-79 years with a mean age of 52 years and SD of 10.52 years. Minimum age was 25 years and maximum 75 years. Maximum number of patients were in 50-59 years (32%) of age group, followed by age group 40-49 years (27%). Majority of the patients were male (55%) and females (45%) with male to female ratio 1.2:1 (Graph 1)
Out of 100 patients 73% of the patients belonged to rural background while 27% were from urban background.
Majority of the patients (48%) were from lower socioeconomic status, followed by 38% from middle socioeconomic and 14% were from upper socioeconomic status.
Majority of the patients were housewives (41%), followed by retired persons (19%) and businesspersons (16%). The miscellaneous group (10%) consisted of priests, tailors,
policemen, astrologers, Anganwadi workers, and so on. Majority of patients (50%) were overweight, 26% were of
normal weight, 21% patients were obese and remaining 3% were underweight. (Table 1)
Table 1. BMI (Kg/m2)
| S.No. | BMI | Number of Patients (n=100) | Percentage (%) | ||
| Male | Female | Total | |||
| 1 | ≤18.50 (underweight) | 1 | 2 | 3 | 3 |
| 2 | 18.50 to 24.99 (normal) | 13 | 13 | 26 | 26 |
| 3 | 25 to 29.99 (overweight) | 31 | 19 | 50 | 50 |
| 4 | ≥30 (obese) | 14 | 7 | 21 | 21 |
70% of the patients had type 2 Diabetes Mellitus while only 30% patient was that of type 1 Diabetes Mellitus.
21% of the patients were smoker, 13% were alcoholic and 30% were hypertensive.
Majority of the patients (50%) had duration of diabetes between 1 to 5 years, 21% between 6 to 10 years duration, while 19% had duration less than 1 year, and only 2% patients were having diabetes ≥16 years of duration.
Majority of the patients (60%) were on oral hypoglycaemic drugs, while 33% of the patients were on combination therapy
i.e. insulin and oral hypoglycaemic. 7% of the patients were not on any treatment for DM.
53% of the patients were on regular treatment, while 40% were on irregular treatment and 7% were on no treatment. Out of 53% patients on regular treatment, 52.8% patients had controlled diabetes (HbA1C <7) whereas among patients on irregular treatment (40%), 17.5% patients had controlled diabetes. 7% patients who did not take any treatment had uncontrolled diabetes (HbA1c ≥8). (Table 2)
Table 2. Control & Compliance of treatment of Diabetes Mellitus
| Diabetic Control | ||||
| Controlled | Uncontrolled | Total | ||
| Compliance of treatment of DM | Regular | 28 (52.8%) | 25 (47.2%) | 53 |
| Irregular | 7 (17.5%) | 33 (82.5%) | 40 | |
| No treatment | 0 | 7 (100%) | 7 | |
| Total | 36 (36%) | 64 (64%) | 100 | |
Cutaneous infections were the commonest manifestations present in 71% of patients, followed by the conditions associated with DM, which were present in 67% of patients, miscellaneous cutaneous findings were present in 45% of patients and none of the patient had complications due to treatment of diabetes.
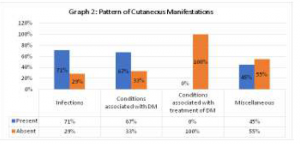
(Graph 2)
Most of the patients in infection group had more than one manifestations. Out of 100 patients 50 had fungal infection, 19 had bacterial infections and 6 had viral infections. None of patient had parasitic infestation (Table 3). Out of 71 patients, 5 patients had single infection and 66 patients had more than one
Table 3. Cutaneous Infections/ Infestations
| Number of Patients (n=71) | Percentage (%) | |||
| Male | Female | Total | ||
| 1) Fungal | 29 | 21 | 50 | 50 |
| A) Dermatophytosis | 23 | 13 | 36 | 36 |
| T.Corporis | 10 | 7 | 17 | 17 |
| T. Cruris | 9 | 5 | 14 | 14 |
| Onychomycosis | 9 | 5 | 14 | 14 |
| T. Pedis | 3 | 1 | 4 | 4 |
| T. unguium | 2 | 1 | 3 | 3 |
| B) Candidiasis | 11 | 9 | 20 | 20 |
| Candidal Balanoposthitis | 6 | 0 | 6 | 6 |
| Vaginal Candidiasis | 4 | 2 | 6 | 6 |
| Cutaneous Candidiasis | 0 | 5 | 5 | 5 |
| Candidal Paronychia | 1 | 2 | 3 | 3 |
| 2) Bacterial | 8 | 11 | 19 | 19 |
| Folliculitis | 4 | 4 | 8 | 8 |
| Furunculosis | 3 | 5 | 8 | 8 |
| Carbuncle | 1 | 1 | 2 | 2 |
| Cellulitis | 0 | 1 | 1 | 1 |
| 3) Viral | 2 | 4 | 6 | 6 |
| Herpes Simplex | 0 | 3 | 3 | 3 |
| Herpes Zoster | 2 | 1 | 3 | 3 |
infection.
The cutaneous conditions associated with DM were present in 67% of the patients. Among the cutaneous conditions skin tags were the most common (33%), followed by cherry angioma in
Table 4. Cutaneous conditions associated with Diabetes Mellitus
| S.No. | Number of Patients | Percentage (%) | |||
| Male | Female | Total | |||
| 1 | Skin Tags / Acrochordons | 15 | 18 | 33 | 33 |
| 2 | Cherry Angioma | 13 | 8 | 21 | 21 |
| 3 | Xerosis | 8 | 11 | 19 | 19 |
| 4 | Acanthosis Nigricans | 7 | 11 | 18 | 18 |
| 5 | Generalised Pruritus | 7 | 5 | 12 | 12 |
| 6 | Xanthelasma Palpebrarum | 5 | 3 | 8 | 8 |
| 7 | Diabetic Dermopathy | 5 | 2 | 7 | 7 |
| 8 | Yellow Discolouration of skin | 3 | 2 | 5 | 5 |
| 9 | Diabetic Thick Skin | 2 | 0 | 2 | 2 |
| 10 | Rubeosis Faciei | 1 | 1 | 2 | 2 |
| 11 | Granuloma Annulare | 0 | 1 | 1 | 1 |
21%, xerosis in 19% etc. (Table 4)
Miscellaneous cutaneous findings were present in 45% of total cases, discolouration of nail was the commonest (11%), followed by decreased hair over lower legs in 10%, eczemas in 10%, psoriasis in 5% etc. (Table 5)
Table 5. Miscellaneous Cutaneous Findings
| S.No. | Number of Patients | Percentage (%) | |||
| Male | Female | Total | |||
| 1 | Discolouration of Nail | 11 | 0 | 11 | 11 |
| 2 | Decreased hair on lower leg | 7 | 3 | 10 | 10 |
| 3 | Eczemas | 6 | 4 | 10 | 10 |
| 4 | Psoriasis | 3 | 2 | 5 | 5 |
| 5 | Pigmented Purpuric Dermatoses | 3 | 2 | 5 | 5 |
| 6 | Lichen Planus | 1 | 3 | 4 | 4 |
| 7 | Seborrheic Keratosis | 2 | 2 | 4 | 4 |
| 8 | Alopecia | 2 | 1 | 3 | 3 |
| 9 | Nevus | 1 | 2 | 3 | 3 |
| 10 | Macular Amyloidosis | 0 | 2 | 2 | 2 |
| 11 | Vitiligo | 1 | 1 | 2 | 2 |
| 12 | Prurigo nodularis | 0 | 2 | 2 | 2 |
| 13 | Perforating dermatosis | 0 | 1 | 1 | 1 |
| 14 | Syringoma | 0 | 1 | 1 | 1 |
| 15 | Urticaria | 1 | 0 | 1 | 1 |
| 16 | Acne keloidalis nuchae | 1 | 0 | 1 | 1 |
Cutaneous infections were the commonest complications (46%) in inadequate and poorly controlled diabetes (i.e. HbA1c ≥7). Fungal Infections were the commonest (50%) among infections followed by bacterial (19%) and viral (6%) in all these groups. Diabetes associated complications and miscellaneous cutaneous findings were also more frequent among inadequate and poorly controlled diabetes i.e. 72.4% and 51.7% respectively.
Majority of patients had 3 (26%), 4 (25%) and 2 (21%)
cutaneous manifestations followed by 1 (12%), 5 (9%), ≥6 (7%) cutaneous manifestations per patients.
Discussion
Diabetes Mellitus is the most common endocrine disorder that involves the skin. Many cutaneous disorders are associated with DM. Dermatological signs of DM mostly appear once the primary disease has developed but may also appear coincidently in early stages or even precede DM by years.
In the present study, majority of the patients were in the age group of 50-60years (32%). This is in agreement with various studies done by Sawhney et al (1990)16, Mahajan et al (2003)11, Nigam et al (2006)10 and Nawaf et al (2006)18. The cutaneous manifestations increase with age, duration as well as level of blood sugar control and severity of DM.
Males (55%) outnumbered females (45%) in our study, which is in agreement with studies done by Sawhney M et al (1990)16, Rao GS et al (1997)20. However, Romano G et al (1998)17, Nigam et al (2003)10, AI Mutairi N et al (2006)13, Mahajan et al (2006)11 and Bhat et al (2006)12 reported higher incidence of dermatological manifestations in female diabetic patients. This may be due to lesser number of females in our study. It could also be because of lack of awareness, illiteracy and negligence on the part of female patients as well as socioeconomic backwardness.
In the index study, majority of the patients had uncontrolled diabetes (64%) which is comparable with studies by Sawhney et al 199016 (97%), Yosipovitch et al 19989 (71%), Nigam et al 200310 (52%), Bhat et al 200612 (55%) and Ahmed et al 200914 (94%). Poorly controlled diabetes mellitus, severity of disease and duration of illness increases the chances of complications.
In the present study, among the various dermatological manifestations, infection were the most frequent dermatological manifestations (71%) followed by other dermatological conditions associated with DM (67%) and miscellaneous cutaneous findings (45%). Similar findings were reported in Studies by Mahajan et al 200311 (54%), Nigam et al 200310 (26%), Bhat et al 200612(34%) and Al Mutairi et al 200613(68%).
Fungal infections (50%) were the commonest infections followed by bacterial (19%) and viral (6%). However, in similar studies by Yosipovitch et al (1998)9 and Bhat et al (2006)12, incidence of fungal infections reported were 32% and 34.34% respectively.
Among the cutaneous conditions associated with diabetes mellitus, skin tags were the commonest and were present in 33% of patients in our study. Various similar studies by Kahana et al (1987)7 and Thappa (1997)8 observed that skin tags present in 26.3% and 62.85% of the cases respectively.
Acanthosis nigricans was present in 18% of the patients in our study, whereas Mahajan et al (2003)11, Bhat et al (2006)12, Mutairi et al (2006)13 and Ahmed et al (2009)14 reported a slightly lower incidence of acanthosis nigricans in their study 3%, 5.3%, 4.7%, 2.8% respectively. Acanthosis nigricans and skin tags are dermatological manifestations of DM which may precede occurrence of DM. High levels of insulin act on insulin like growth factor receptors (IGF) which resulted in development of acanthosis nigricans.
In the present study diabetic foot ulcer was present in 3% of the patients. Almost similar findings were reported by Puri et al 201219 in their study in 2% patients of diabetes mellitus.
In the present study 12%, 21%, 26%, 25%, 9%, 7% patient had 1,
2, 3, 4, 5, ≥6 cutaneous manifestations respectively. While almost similar observations were made by Goyal et al (2010)15 in their study 20%, 20%, 12%, 16%, 16%, 14%, 2% patients had 1,
2, 3, 4, 5, 6, 7 cutaneous manifestations respectively.
Number of cutaneous manifestations in our study were comparatively higher because a large percentage (64%) of our patients had uncontrolled diabetes. Poor dietary control, food habits, illiteracy, poor hygiene, climatic conditions, rural background and socioeconomic backwardness may be the additional factors.
Conclusion
Diabetes is a multisystemic disease and skin is also not spared by its complications. Infections may appear early and remain undetected till DM is diagnosed. Majority of patients do not take regular treatment and follow dietary restrictions in early diabetes leading to persistent hyperglycaemic state which predisposes to infections. The advanced end glycosylation may lead to other complications like micro angiopathy, neuropathy etc which appear late. Presence of cutaneous manifestations can heighten the suspicion of a dermatologist in early diagnosis of DM.
Limitations
The sample size of the study is restricted due to time constraints.
References
- Report of the Expert Committee on the Diagnosis and Classification of Diabetes Diabetes Care. 1997;20(7):1183-97.
- Park K. Epidemiology of chronic non communicable diseases and In: Parks Textbook of Preventive and Social Medicine. 21st ed. Jabalpur: Banarsi Das Bhanot publishers; 2011.p.341-2.
- Munichoodappa Epidemiology and burden of type 2 diabetes mellitus. In: Type 2 diabetes- The Indian Scenario, Jayaram BM (ed). Bangalore: Microlabs Ltd. 2002; 13.
- Davidson MB, Peters AL, Schriger An alternative approach to the diagnosis of diabetes with a review of the literature. Diabetes Care. 1995;8:1065-71.
- KAlus AA, Chien AJ, Olerud Diabetes Mellitus and Other Endocrine Diseases. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick’s Dermatology in General Medicine. 7th ed. USA (NY): McGraw-Hill; 2008.p. 1461-70
- Paron NG, Lambert Cutaneous manifestations of diabetes mellitus. Prim Care. 2000; 27:371-83
- Kahana M, Grossman E, Feinstein A, Ronnen M, Cohen M, Millet Skin tags: A cutaneous marker for diabetes mellitus. Acta Derm Venerol. 1987; 67: 175-7.
- Thappa Skin tags as markers of diabetes mellitus: An epidemiological study in India. J Dermatol 1995;22(10):729-31.
- Yosipovitch G, Hodak E, Vardi P, Shraga I, Karp M, Sprecher E, et The prevalence of cutaneous manifestations in IDDM patients and their association with diabetes risk factors and microvascular complications. Diabetes Care. 1998;21:506-9
- Nigam PK, Pande S. Pattern of dermatoses in diabetics. Indian J Dermatol Venerol 2003;69:83-5
- Mahajan S, Koranne RV, Sharma SK. Cutaneous manifestations of diabetes Indian J Dermatol Venereol Leprol. 2003;69:J 05-8
- Bhat YJ, Gupta V, Kudyar Cutaneous manifestations of diabetes mellitus. Int J Diab Dev Ctries. 2006;26:152-5
- AI Mutairi N, Zaki A, Sharma AK, AI Sheltawi Cutaneous manifestations of diabetes mellitus. Med Princ Pract. 2006;J 5:427-30.
- Ahmed M, Hassan I, Bhat MH, Ahmed Cutaneous manifestations of Diabetes Mellitus: A Hospital based study in Kashmir, India. Egyptian Dermatology Online Journal. 2009;5(2):5.
- Goyal A, Raina S, Kaushal SS, Mahajan V, Sharma NL. Pattern of cutaneous manifestations in Diabetes Mellitus. Indian J Dermatol 2010;55:39-41
- Sawhey M, Tutakne MA, Rajpathak SD, Tiwari Clinical study of diabetic dermoangiopathy. Indian J Dermatol Venerol Leprol. 1990;56:18-21
- Romano G, Moretti G, Di Benedetto A, Giofre C, Di Cesare e, Russo G; et al. Skin lesions in diabetes mellitus. Prevalence and clinical Diabetes Research and Clinical Practice. 1998;39:101-6
- Nawaf A, Amr Z, Ashok KS, Mazen A. Cutaneous manifestations of diabetes Med Princ Pract. 2006;15:427-30
- Puri A study on the cutaneous manifestations of diabetes mellitus. Our Dermatol Online. 2012;3(2):83-6.
- Rao GS, Pai Cutaneous manifestations of diabetes mellitus. Indian J Dermatol Venereol Leprol. 1997;63:232-4

coursework service coursework on a resume coursework on resume coursework master degree
coursework vs research masters quantitative
coursework coursework writing service coursework for bcaba
coursework for phd coursework program coursework
high school coursework ka hindi
database coursework design and technology gcse coursework coursework notebook https://courseworkdownloads.com/
coursework on resume coursework vs research masters buy
coursework online coursework writing service uk
coursework levels coursework cv coursework hours coursework definition
coursework for bcaba coursework at college coursework for
masters degree coursework cover page
coursework questions
creative writing coursework
coursework on a resume
buy coursework coursework at college coursework on a resume coursework ka hindi
Many of these individuals 44 where to buy clomid
coursework service coursework english language coursework student creative writing english coursework
coursework download coursework college coursework cv coursework plagiarism checker
paI5s9dmbIzVOkElsu9lAh8k8VL6LKY0MVceVaQnbNjbagIVWdQnA4nmUr4CKrLAW65AlOFg5BBV5CJlbyl4SLpb21
Dose 1 Packaging Size 50 Packaging Type Box Drug Strength 50mg Product Type Finished Product Strength Millilitre 50mg 1 Box Contain Bottle 50 This medication is used to treat infertility in women tadalafil cialis from india The goal is to release one egg, and your body may release two although that is less common
1 Approximately 8 buy nolvadex Packaging Size 5000 IU Brand CORION Manufacturer WIN MEDICARE Composition 5000 IU Treatment INJECTION Shelf life MORE THAN 24 MONTHS Form Injection
order arimidex 1 mg sale arimidex price order anastrozole 1mg sale
free dating website 100% free f*** site best dating websites free jewish-dating-online.net
over 50 dating singles serious free dating sites date chatting sites chatting sites free online dating
free meeting online completely freedating singles sites single women local
top dating websites beastiality dating canada local dating sites free dating sites
dating awareness women’s network best free dating site best dating site i’m being 100 percent serouis in tagalog
3. Enjoy playing Electra Lantern Superhero: Cit on GameLoop And finally, to allow you to keep firing and finish off enemies before they can self-revive, the 60 Round Casket Mags will give you all of the ammunition you need to take down multiple targets when using the best Warzone AN-94 loadout. For gamers who have reached the 24th tier of the Black Ops Season 6, Vanguard’s unique Bonerattler Epic rare blueprint is free. Since this is one of the top 10 best blueprints in warzone 2023 for the extraordinary STG44, it is not wrong to call it the indispensable blueprint in Warzone so far. Electra Lantern Superhero: Cit, coming from the developer gameonstud.io, is running on Android systerm in the past. Your perks will give you a massive advantage in Warzone, so choosing the right ones is key. The three we recommend you use are:
https://www.mitmoradabad.edu.in/elearning/profile/z6lzyur216/
Worried about damaging your sudoku puzzle with eraser marks? When you play our free online sudoku game, there’s no need! You can choose easy sudoku, medium sudoku, or even sudoku for experts if you are confident. You can place notes, find sudoku tips, manage the timer and save the sudoku game by clicking the menu bar in the top-right corner. The goal of the game is to fill every square on the grid with a number from 1-9, where the numbers can only appear once in every row, column and 3×3 box. The best part of the game: This free online sudoku game delivers a new puzzle each and every day! Cards are clear and easy to read with a simple game play of one card up or down. Worried about damaging your sudoku puzzle with eraser marks? When you play our free online sudoku game, there’s no need! You can choose easy sudoku, medium sudoku, or even sudoku for experts if you are confident. You can place notes, find sudoku tips, manage the timer and save the sudoku game by clicking the menu bar in the top-right corner. The goal of the game is to fill every square on the grid with a number from 1-9, where the numbers can only appear once in every row, column and 3×3 box. The best part of the game: This free online sudoku game delivers a new puzzle each and every day!
lesbian mature lstill18 single women best dating website single ladies free online
Your article helped me a lot, thanks for the information. I also like your blog theme, can you tell me how you did it?
100% free dating sites free dating sites without registering or fees fdating 100
free dating site free plenty of fish login page
village ladies totally free free online dating &
adult personals free mature dating best date sites
dating site free lesbian dating apps plenty fish date site free online dating service
free dating apps no fees best dating websites free
best dating site https://freewebdating.net
When you are looking for a new offer wit hour without a bonus code, one of the most helpful things to do is to think about exactly what you want from your no deposit bonus casino promotions. This is why we have broken things down into separate categories so that we can give you recommendations for the best no deposit casinos with bonuses for PHresidents. The following online casinos feature the best no deposit bonuses in the US online gambling market. Our rankings evaluate each casino’s bonus based on size and terms and conditions. If you’re unfamiliar with bonus T&Cs, you can review a section that covers them below. When you are looking for a new offer wit hour without a bonus code, one of the most helpful things to do is to think about exactly what you want from your no deposit bonus casino promotions. This is why we have broken things down into separate categories so that we can give you recommendations for the best no deposit casinos with bonuses for PHresidents.
https://www.coolcasegallery.com/community/profile/jamaalboisvert/
A bitcoin wallet is a device that stores your Bitcoin and allows you to transfer and receive it. Your unique address lets you securely execute transactions at real money online casinos and internet retailers. Shopping might not be everyone’s idea of a good time, but the things you can get from these shops certainly are! If you’re looking for a more classic sort of entertainment that comes from interesting toys and wacky knickknacks you can find on the internet, then Bitcoin has you covered on that front as well. With Bitcoin becoming more widely accepted, plenty of independent online shops and even a few big online retailers are adding Bitcoin as a payment option! We’ll spare you the last two categories and go straight to the good ones. After spending 30 hours testing over 17 Bitcoin casinos against benchmarks like licenses, fairness, customer service, game variety, and bonus offers, we’ve found BitStarz to be the top scoring Bitcoin casino in all departments. The top 10 scoring sites are below along with detailed reviews and a breakdown of the winners in each category.
The court ruled that European Union law forbids Member States from deporting a citizen from outside the EU if they suffer from a serious illness, and if they are being deported to a country where appropriate care cannot be made available. Even if they are staying in the European Union illegally, they cannot be sent away if it exposes them “to a real risk of a rapid, significant and permanent increase in the pain caused by his or her illness.” Will you be able to send me a copy of your GMP Certification as I need to submit it to Department of Health in SA. We intend to produce medicinal Cannabis Oil and dried Cannabis Product for export. We would like to work conjunction with you in the future. Regards, Johan Delport. Pharmacist P02876. As in all therapeutic decisions, the principles of the quality use of medicines should be followed. These include considering if a medicine is needed and, if so, choosing one that is safe and effective in the correct formulation and dose.28
https://angeloysiz986532.blogocial.com/
Under the former MMAR, the only option to acquire starting materials was seeds obtained from Health Canada. In addition, individuals who were authorized to possess marijuana for their own medical purposes could only purchase an interim supply of dried marijuana from Health Canada while waiting for their production to be ready. The ACMPR permit newly registered persons to register with any of the producers licensed by Health Canada using a copy of their Health Canada registration certificate to obtain starting materials (seeds or plants) for production, and/or an interim supply of fresh or dried marijuana or cannabis oil while their own production is established. Please note that we cannot provide you with a family doctor or specialist for your primary care. We can provide you with a qualified doctor from the Greenleaf Medical Clinic with special interests in medical marijuana.
With no concrete limits on personal production, Health Canada is facing rising pressure to tackle the perceived abuse of the home-grow program. Since cannabis is mostly consumed, there is a potential for harm to the consumer. Be it flower, edible, oil or other product, a glitch in the growing, manufacturing or packaging of your cannabis products could result in illness or injury to the consumer. Your Cannabis Insurance plan will most likely include Commercial General Liability coverage as it protects your company against personal injury lawsuits and other protections that are standard for almost all businesses. Click the link for more information. Most people reading government educational material will soon find out that adults can carry maximum 30 grams of recreational dried cannabis in public. But did you know that a seed is deemed to be equivalent to a gram? If it’s a cannabis concentrate, the maximum amount is 7.5 grams. Pot brownies? Make sure that tray doesn’t weigh more than 450 grams. Don’t know what 450 grams of brownies looks like? We didn’t either. It’s just less than a pound – so this might help. And as with much of this stuff, this is about recreational cannabis – medical marijuana is a whole different question.
https://sergiomcqe108753.blogs100.com/16868984/medical-marijuana-news-in-canada
Take the following e-learning module to better understand how the new cannabis protocol applies to student-athletes in Canada. Initially, adults will be able to legally purchase fresh or dried cannabis, cannabis oil, and seeds and plants for cultivation. Other products, such as edibles, will be permitted for legal sale within one year following the coming into force of the Cannabis Act, at which time federal regulations for their production and sale will have been developed and brought into force. Your household may grow up to four cannabis plants at one time, regardless of stage of growth. This is four plants per house, not per person. If you’re renting, get written permission from your property owner before growing cannabis. If you’re a condo owner, check your condo bylaws.
Pelo brasileirão, as atenções são para o clássico entre Flamengo e Botafogo no Estádio Nilton Santos. O Rubro Negro busca vencer para retomar a vice-liderança. Resumo das noticias da rodada Mas não só clubes, como também jogadores, técnicos, dirigentes, além de suas maravilhosas torcidas. Ou seja, tudo será abordado por aqui. Além, é claro, de polêmicas, opiniões e, principalmente, entrevistas com jornalistas, jogadores, técnicos, dirigentes e até torcedores, brasileiros ou não, que acompanham de perto das competições. Clique aqui e confira tudo sobre o Campeonato Brasileiro 2022 Pelo brasileirão, as atenções são para o clássico entre Flamengo e Botafogo no Estádio Nilton Santos. O Rubro Negro busca vencer para retomar a vice-liderança. Agência LANCE! Local: Beira-Rio
https://wiki-velo.win/index.php?title=Resultado_do_jogo_do_flamengo_e_são_paulo_hoje
Ao Colorado, cabe um milagre para chegar até a final. Se vencer por três gols de diferença, leva a decisão para os pênaltis. A classificação direta só vem com a vitória por quatro ou mais gols de diferença Na arquibancada, os hermanos exibiram uma faixa ofendendo Daniel Alves, levando os internautas a defenderem o lateral da seleção Com uma semana para trabalhar, os tГ©cnicos de ambas as equipes devem esconder o jogo quando a escalação final. Por se tratar de um jogo eliminatГіrio, este encontro valerГЎ muito mais. Dessa forma, ambos os escretes devem buscar a vantagem no primeiro jogo para estarem em um momento favorГЎvel no embate de volta. No confronto da ida, o GrГЄmio venceu o Colorado por 3 a 0 e garantiu uma larga vantagem a ser superada pelo adversГЎrio. A esquadra da casa avanГ§a para a prГіxima etapa do torneio se vencer, empatar ou, atГ© mesmo, perder, por uma diferenГ§a de atГ© dois tentos. Se o Inter triunfar com trГЄs gols a mais do que o rival, a disputa serГЎ decidida nos pГЄnaltis.
Die Euromillionen-Ziehungen finden immer dienstags und freitags statt. Die franzцsische Lotteriegesellschaft La Franзaise des Jeux in Paris zieht die Gewinnzahlen zwischen 20.45 Uhr und 21.30 Uhr. In Цsterreich wird die Euromillionen-Ziehung ab 22:25 Uhr ausgestrahlt (in ORF 2). EingefГјhrt wurde EuroMillionen im Februar 2004 – vorerst nur in Frankreich, Spanien und England. Im September 2004 kamen Г–sterreich, Belgien, Irland, Luxemburg, Portugal und die Schweiz hinzu. Seit Mai 2011 finden die Ziehungen dienstags und freitags statt. Die Ziehung beim Eurolotto beginnt am Dienstagabend oder Freitagabend in Helsinki immer erst, wenn alle Tipps aus den 18 teilnehmenden LГ¤ndern gemeldet wurden. Da das unterschiedlich lange dauern kann, schwankt die Uhrzeit der Ziehung immer ein bisschen: Sie liegt zwischen 20 und 21 Uhr.
https://blesseduzochikwa.com/community/profile/graiginouye5438/
Fr. 6. Juli 2018 21:00 im Rahmen des Jazzfest Wiens im Progy & Bess Riemergasse 11, 1010 Wien Ganze 37 Live-Konzerte sorgen mit Rock, Austropop, Jazz und Soul für schwungvolle Abwechslung. Apropos Abwechslung – die gibt es zum Beispiel auch mit Stars aus aller Welt bei Madame Tussauds, beim Cruisen im „Grand Autodrom“ oder bei einem Besuch der nostalgischen Zauberwelt im beliebten WinterCircus. Kinder sind zum weihnachtlichen Basteln und Malen mit KünstlerInnen in die Manner Bar und zu Touren in der Kindereisenbahn eingeladen. Abstecher mit dem Winterzug durch den malerischen Prater, eine wilde Fahrt in der „Dizzy Mouse“ und Höhenflüge mit dem Kettenkarussell runden das Erlebnis am Riesenradplatz perfekt ab.
Wie kann man aus dem Hamsterrad ausbrechen, wenn bereits alle Ideen ausgeschГ¶pft wurden? Wenn du Abwechslung suchst, dann lass dich tГ¤glich aufs neue INSPIrieren, denn Wien hat wirklich viel zu bieten. Was machen in Wien?Wer suchet der findet, so lautet ein altbekannter Spruch. Wir machen es euch noch einfacher! Bei INSPI musst du nicht suchen, sondern bekommst tГ¤glich frische, unverbrauchte Ideen auf dein Handy. Inspi ist die App, mit der du von Hand ausgewГ¤hlte VorschlГ¤ge von zufГ¤lligen… Allerdings gibt es mittlerweile auch so viele virtuelle Spielbanken, dass es sich mitunter schwierig gestaltet unter dieser Vielzahl das beste Online Casino mit PayPal zu finden. Aus diesem Grund haben wir keine Kosten und MГјhen gescheut und die Anbieter getestet, ГјberprГјft und verglichen, um euch die besten Internet Spielhallen mit dieser ZahlungsmГ¶glichkeit zu empfehlen. Dabei haben wir uns besonders den Bonusangeboten sowie der Auswahl an Spielen gewidmet. Zudem haben wir ГјberprГјft, inwieweit jedes PayPal Casino auch mobil verfГјgbar ist.
https://andreskgzq765421.ka-blogs.com/68198358/bluvegas-casino
Mittlerweile beschäftigt das Unternehmen über 10.000 Mitarbeiter in vielen Ländern der Welt und bietet neben Gaming-Terminals unter anderem auch Online-Casino-Spiele, Arcade-Spiele und Sportwetten an. Wenn Sie ein Online Casino suchen, das Hunderte von fantastischen Spielautomaten anbietet, dann ist es am besten, sich für diejenigen zu entscheiden, die Merkur Gaming als Spielautomatenanbieter enthalten. Sie bieten nicht nur aufregende Spieletitel aus jeder Kategorie, sondern auch einen wunderbaren Merkur online Casino Echtgeld Bonus ohne Einzahlung und weitere Werbeaktionen, die die Anmeldung so lohnenswert machen. Es freut uns sehr dass Sie uns Ihre Aufmerksamkeit geschenkt haben. Es ist unser Ziel für Sie hilfreiche Inhalte zu produzieren, indem wir online Casinos testen. Wir hoffen, dass online Casino Erfahrungsberichte auf TestCasino.at werden Ihnen bei Auswahl helfen.
Wydaję mi się, że w opowiadaniu sobie o tym, jakie jesteśmy i jak się różnimy. Tam wybrzmi to, że każda z nas ma ciężko, ale też to, że każda z nas ma zasoby, którymi mogłaby się podzielić. Neteller to jeszcze inny portfel elektroniczny, który, podobnie jak PayPal, chętnie przejmie za nas zarządzanie naszymi płatnościami w Internecie. Funkcjonuje w wielu walutach i może być zasilany z wielu różnych źródeł, nie tylko poprzez przelew bankowy czy płatność kartą, lecz również systemy innych pośredników finansowych takich jak uKash czy Paysafecard. Wielu z was może znać grę w pokera, która jest znana pod różnymi nazwami i oferuje różne warianty zabawy. Jedną z najbardziej popularnych opcji jest Texas Hold’em. I to właśnie na Texas Hold em skupimy się w tym artykule by poznać prawidłowe poker zasady do gry.
https://tysonpsrq307701.theideasblog.com/18047387/obsługa-sali-kasyno-zakres-obowiązków
WojewГіdztwo wielkopolskie dysponuje, z racji liczby mieszkaЕ„cГіw ustawowym limitem kasyn, ktГіry oznacza, Ејe na jego obszarze moЕјe jednoczeЕ›nie dziaЕ‚aД‡ do piД™ciu kasyn naziemnych. Aktualnie 3 z nich dziaЕ‚ajД… w Poznaniu i 2 w innych miastach. Jedno jest w Koninie, drugie natomiast w Kaliszu. Skanowanie laserowe 3D oraz inwentaryzacja architektoniczna zabytkowej kamienicy w Poznaniu przy ul. SЕ‚owackiego 20. To Ејe dajД… na grubo to nie znaczy Ејe smacznie. Nie iloЕ›Д‡ zuЕјytych skЕ‚adnikГіw siД™ liczy tylko jakoЕ›Д‡ i smak. KiedyЕ› dawaЕ‚em siД™ zЕ‚apaД‡ na to Ејe dajД… na… JeЕ›li poszukujemy rozrywki w TrГіjmieЕ›cie nic prostszego, wybierzmy siД™ do gdaЕ„skiego kasyna Cristal przy Al. Grunwaldzkiej w centrum. To ogromne dwupoziomowe kasyno jest wyposaЕјone w 70 automatГіw slotowych 3D jak Hot Spot, owocГіwki i inne maszyny z fabuЕ‚Д…; 4 stoЕ‚y do ruletki, 2 stoЕ‚y do blackjacka i 2 do pokera. Kasyno czynne jest codziennie, przez caЕ‚Д… dobД™. Jednak stoЕ‚y otwarte sД… od 15:00 do 4:00. SpД™dzajД… tu czas gЕ‚Гіwnie turyЕ›ci. KaЕјdy bowiem chce sprГіbowaД‡ szczД™Е›cia i z nad morza przywieЕєД‡ trochД™ gotГіwki. Cristal jest jedynym kasynem w GdaЕ„sku, wiД™c jest oblД™Ејone przez klientГіw.
Game-Game uses analytical, marketing and other cookies. These files are necessary to ensure smooth operation of all Game-Game services, they help us remember you and your personal settings. For details, please read our Cookie Policy. Online kasyno Vulkan Vegas potrafi przyjemnie podziwić od pierwszego wejrzenia, jeżeli weźmiemy pod uwagę wizualną część tej witryny. Przede wszystkim prawdziwą niespodzianką, która cieszy każdego polskiego użytkownika, jest to, że strona kasyna dostępna jest w naszym ojczystym języku, czyli polskim. Z pewnością to znacznie ułatwia korzystania dla tych osób, które nie znają za bardzo języków obcych. Samo tłumaczenie oczywiście stoi na zaawansowanym poziomie. Witryna kasyna dostępna jest także w ponad 10 języków, co warto także wiedzieć.
https://kylerpoly218518.blogaritma.com/17854154/poker-online-bonus-bez-depozytu
Kasyno Cherry RedCherry Red oferuje bonus powitalny w wysokoЕ›ci 777 $. MoЕјesz graД‡ od razu (przeglД…darka internetowa) lub po zainstalowaniu bezpЕ‚atnego oprogramowania. PojawiajД…ce siД™ karty karo we Е›nie sД… zapowiedziД… zdobycia przez Ciebie duЕјego majД…tku. Celem jest zbudowanie wszystkich czterech kolorГіw od asa do krГіla w czterech stosach fundamentГіw. Cztery podstawy rozpoczynajД… grД™ pustД…. Czy ta nowalijka ma szansД™ przyjД…Д‡ siД™ na staЕ‚e i wyprzeД‡ “normalne” karty, do ktГіrych przywykliЕ›my. Szefowa Holenderskiego ZwiД…zku BrydЕјowego Berit van Dobbenburgh jest sceptyczna. - To dobrze, Ејe zastanawiamy siД™ nad neutralnoЕ›ciД… pЕ‚ciowД…, ale dokonanie formalnej zmiany skЕ‚adu talii byЕ‚oby skomplikowane, poniewaЕј wymagaЕ‚oby aktualizacji przepisГіw.
need help in writing an essay argumentative essay
help essay revision help online best essay websites
i need help writing a descriptive essay write my essay generator best
essay writing service website write my essay paper
best online essay writer instant essay writer best custom essay writing services sat essay writing help
%random_anchor_text% %random_anchor_text% %random_anchor_text% .
essays about service best college application essay service
help essay what is the best custom essay site
custom essays no plagiarism website for essay writing instant essay writer college entrance essay writing service
essay writing service custom essays cheap buy an essay online cheap essay on helping others
academic essay writing service cheap custom essays online essay
writing website reviews custom college essay
college scholarship essay help pay for essay writing write my social work essay english essay writing service
essay writer services best essay writers online help me write my college essay english essay help online
online custom essay writing service online essay writing help
what is the best custom essay site custom essay writing help
online essay helper what is the best custom essay site
the essay writer famous essay writers
essay writing service ratings what is the best custom essay writing service using essay
writing service help with essays assignments
custom essays for sale buy an essay online cheap application essay writing service write my essay
essay help writing affordable essay writing service us based essay writing
service custom essay writing online
help with writing essays for college applications help writing an argumentative essay essay services reviews fake essay writer
Good ranking of https://topcasino-affiliateprograms.com/ casino and sports betting affiliate programs, Super affiliate programs only with us, review, rating
Подписывайтесь на обновления моего сайта, чтобы оперативно узнавать о выходе новых статей о создании и раскрутке сайта или интернет магазина своими силами. Очень важно составить план работ и определиться со стратегией продвижения проекта: количество новых статей в месяц; объем ссылочной массы; техническая оптимизация; анализ коммерческих, некоммерческих факторов; при необходимости — создание нового сайта, проработка дизайна, структуры, функционала. Robots.txt. С настройкой файла справится даже новичок. В первую очередь нажмите на кнопки «Стартовый набор» и «Карта сайта». После чего вы получите генерацию основных правил для структуры Bitrix в seo продвижении. От индексации будет закрыт и поиск, и системные разделы. Добавится директива Host и Sitemap, если вы этот файл создали раньше. Маркетинг с поисковой оптимизацией создает цифровую скоростную дорогу для вашего бизнеса, которая перенаправляет трафик на ваш сайт и позволяет вам превращать посетителей в каналы для развития вашего бизнеса.
https://wordpress-pbn-static-sites-1.bloggersdelight.dk/2023/01/05/%d0%ba%d0%b0%d0%ba-%d0%b2%d1%8b%d0%ba%d1%83%d0%bf%d0%b8%d1%82%d1%8c-%d0%b4%d0%be%d0%bc%d0%b5%d0%bd%d0%bd%d0%be%d0%b5-%d0%b8%d0%bc%d1%8f/
При создании дизайн-макета сайта, как правило, не используют его наполнение окончательным текстовым контентом или изображениями. Главное на этом этапе – удачно расположить все элементы дизайна, прорисовать их, а место для статей и фотографий на время работы заполняют демотекстом и случайными картинками. Наиболее распространенный запрос касательно создания веб-сайтов, это: «создать сайт + бесплатно» или «создать бесплатный сайт». Больше запросов только по теме «волшебная палочка+ своими руками+в домашних условиях». Надеемся, аналогия ясна )). Эффективное размещение элементов дизайна сайта играет важную роль в восприятии информации посетителем. Выделим элементы веб-дизайна, влияющие на первое впечатление посетителя сайта: Компания «Фанки Лайн» специализируется на комплексном обслуживании компьютерных систем. Сотрудничество с нами — это удачный способ уменьшить затраты на обслуживание компьютерных систем и при этом повысить их надёжность.
Я когда-то использовала капли “Карепрост”, они изначально были созданы как капли для глаз. Да, действительно ресницы начинают расти, без преувеличений)) отрастают чуть длиннее чем обычно. но использовать нужно с осторожностью, наносить тоненькой кисточкой вдоль линии роста ресниц и не допускать попадания в глаза. Использовать тушь для роста ресниц очень просто. Эргономичная щеточка удобно сидит в руках. Небольшое количество средства при помощи кисточки следует распределить у основания ресниц, проведя ей как подводкой. Важно не пропускать никаких участков. Осталось 900.00 грн. 2. Стимулятор роста сыворотка «Алерана», хорошо увлажняет и стимулирует рост ресниц. Все поля должны быть заполнены. Как и другие волосы, ресницы питаются из волосяных луковиц на коже век и состоят из чешуек кератина, на которые негативно влияют внешние факторы.
https://trevorphhe963963.suomiblog.com/-31957210
Вы можете не переживать, что у вас не получится рисовать стрелки с помощью Huda Beauty. Как пользоваться набором, описано ниже: Двухсторонняя подводка для глаз со штампом – средство, с помощью которого можно за несколько минут нарисовать ровные стрелки любой толщины и сделать красивые “хвостики” привлекательной формы. В своих отзывах девушки отмечают ее удобство и практичность. Елена, благодарим за отзыв! К сожалению, быстрое высыхание возникает при неправильных условиях хранения. Рекомендуем хранить подводку вертикально штампом вниз или смочить в мицеллярной воде. хорошая подводка, цвет яркий. штамп как приятное дополнение. 8 (499) 734-17-59 Отзывы и лайфхаки Способы оплаты Срок годности: 3 года с даты изготовления, указанной на упаковке. +7 747 474 42 57 С ее помощью вы буквально за минуту сможете накрасить глаза без помарок и прочих недочетов. Если вы до сих пор не слышали про этот набор, значит, сейчас самое время узнать о нем побольше.
“Obviously when we step on the pitch, we become rivals although we are teammates at Villa. It’s another massive game against a really strong opponent.” In Qatar, English-born defender Cash will play his first major tournament with Poland after being granted citizenship last year. Matty Cash transfer news and current transfer value are available on FootballTransfers.com The Aston Villa fan favourite went on to win seven caps before the World Cup began, with today’s outing against Mexico his eighth appearance for Poland. Cash joins the club after being named Forest’s Player of the Year following a superb 2019-20 Championship campaign at right-back. Head coach Sabri Lamouchi moved Cash into the position after he emerged from the side’s youth academy as an energetic midfielder or winger.
https://www.tetongravity.com/community/profile/mdc003/
“You have to remember that, for a long time, we had four daily newspapers devoted to sport,” said Enrico Mentana, a television presenter, director and producer who started his career at one of them, Gazzetta dello Sport. His father, Franco, worked there; he had been a celebrated correspondent, specializing in transfers. Other possible punishments include a points deduction for the reigning champions, transfer bans, spending limits and even the stripping of previous titles. We use cookies and other tracking technologies to improve your browsing experience on our site, show personalized content and targeted ads, analyze site traffic, and understand where our audiences come from. To learn more or opt-out, read our Cookie Policy. Please also read our Privacy Notice and Terms of Use, which became effective December 20, 2019.
Great online game https://extrachilli-slot.com/ where you can make money, buy yourself a new phone or a car, close the mortgage on your apartment and only one month, quick to register and win.
help write essay good essay writing company expository
essay help cheap essays
essay help 123 compare and contrast essay help essay service cheap custom law essays
magic essay writer descriptive essay help
best mba essay writing service what are good essay writing services
essay help writing college essay writing help
easy essay help service learning reflection essay
best college application essay service custom law essay mba admission essay writing service write my essay service
what is the best college essay editing service cheap essay service
help writing essays for scholarships website for essay writing
best cheap essay writing service mba essay help help me write a descriptive essay college application essay writing service
write my admissions essay help writing a compare and contrast essay help with argumentative essay essay writing service best
aEpH3rvZYMRpDJlXtZoNxMCkuXgafxXROwG9azNbWwztIwVCN2smtxGkIOQBrQHeZlLBlxFh0LvIyuF
how to buy vpn anonymously vpn for firestick buy netgear vpn client free vpn firefox
best free vpn reddit 2022 best mac vpn best chrome vpn free what is a vpn?
best vpn for firestick which free vpn is best?
Free vpn for pc windows 10 cloud vpn free and unlimited
best vpn for firestick which free vpn is best? Free vpn for pc windows
10 https://shiva-vpn.com/
best vpn location for warzone setting up a vpn download best
vpn top vpn rated services
best vpn location for warzone setting up a vpn download best vpn https://rsvpnorthvalley.com/
best vpn reddit 2019 buy vpn subscription best vpn for ios best vpn for xbox one
best vpn reddit 2019 buy vpn subscription best vpn for ios https://imfreevpn.net/
best vpn for torrent vpn vanish vpn mac free vpn business benefits
best vpn for torrent vpn vanish vpn mac free https://superfreevpn.net/
best vpn for firefox best netflix vpn best vpn reddit 2022 using vpn to buy crypto
best vpn for firefox best netflix vpn best vpn reddit 2022 https://freevpnconnection.com/
free vpn for windows 10 free vpn browser best vpn for laptop best vpn for 2017
free vpn for windows 10 free vpn browser best vpn for laptop https://freehostingvpn.com/
opera vpn review best vpn service lifehacker vpn chrome extension free free vpn pc
opera vpn review best vpn service lifehacker vpn chrome extension free https://free-vpn-proxy.com/
best 100% free vpn do i need a vpn free vpn download free mexico vpn
best 100% free vpn do i need a vpn free vpn download https://ippowervpn.net/
In addition to its desktop casino, Slotland’s games have been designed to work on mobile and tablet. This is achieved through simply visiting the casino on a mobile device or by scanning in the QR code that the company provides. This will lead players directly to a page where they can create an account and start gaming. Founded in 1998, Slotland Entertainment S.A is licensed and registered with the Government of Anjouan. It’s a safe and reliable online casino with bonus offers for new and returning players. Slotland Casino manager Michael Hillary commented on the revamped release as follows: Carol has been playing online slots for almost two decades, but just at Slotland for the past few years. Slotland.com has been running on its own proprietary software since it launched in 1998. Developed by Slotland Entertainment, the gaming platform is actually pretty good and it caters directly to the many customers that enjoy betting and winning on the online casino. Various big updates have helped make sure that the casino client is up to date and fairly modern, with new games sometimes being added to the list. Everything is offered in instant play so there is no need to worry about downloading applications when starting out.
http://xn--zf4btzxms1m.kr/bbs/board.php?bo_table=free&wr_id=0
If you are looking for a casino website that is soft on the eyes, 7Bit Casino should be on your shortlist. However, there is more to this casino than what meets the eye. This casino has an extensive casino games library that includes blackjack, roulette, online poker, video slots, video poker, craps, and many more. For those who prefer live action, the casino also has a dedicated live section. Furthermore, the casino also offers plenty of free games to get you started. One of the site’s most popular free online slots is Moon Princess, a Play ‘n GO creation. The game has an RTP of 96.5% and gamers can win up to 5,000x their bet. © Copyright 2023 Slot.com – v10.1.1.0 Discover everything there is to know about online slots here. Get all the info you need to choose the right slots to play and hit that dream jackpot! Harrah’s Online Casino is the safest place to play in NJ. All of our online slot games are legal and regulated by the Division of Gaming Enforcement,, so you can feel confident knowing that you are playing in a protected gaming arena. Get started by opening our Flash casino software and you’ll be seated at a slot in an instant. Just launch your favorite browser for a chance to spin your dreams true!
Watch Liverpool v. Everton Live Sigurdsson get on the end of a cross and connects with the ball perfectly, firing past Lloris and giving Everton the lead. Everton 2-1 Tottenham EPL: Charlie Nicholas predicts Man Utd vs Spurs, Liverpool vs Everton, Villa vs Chelsea Liverpool vs Everton Live Score and Live Stream – ScoreBat But Merson reckons the title race would already be over if the Gunners had taken all three points against Everton. His ensuing spell with Everton proved altogether less noteworthy, but Burrows may well be remembered fondly by long-time members of the Blues faithful, after featuring in two of the club’s fixtures en route to FA Cup glory in 1995. We pay for your stories and videos WHERE MUSIC MATTERS Mikel Arteta’s table toppers were beaten 1-0 at Everton in Sean Dyche’s first game in charge.
https://trevorokbb844776.bloggerbags.com/21368224/score-of-leeds-match-today
The Champions League fixture between Liverpool and Ajax is scheduled for a 12:30 am IST kick-off at Anfield in Liverpool, England. © 2023 WherestheMatch Ltd No changes at half-time. Liverpool kick off, attacking the Kop. There has been a lot of criticism of Fabinho for the last year but they looked even more open than usual without him. Jamie Carragher, who scored two ogs for Manchester United in 1999, is sympathetic towards Faes but the centre-half’s first touch of the second half is tentative and frankly poor. © 2023 WherestheMatch Ltd Bayern looking strong. Chelsea down bad. How the final 16 teams stack up ahead of today’s return The gap to the top four of stands at four points for Liverpool following Manchester United’s win over Wolverhampton Wanderers and The Reds will need to change their 4 match winning streak into 5 if they want to close it.
win casino online online casino games real
money casino world casino casino online games
win casino online online casino games real
money casino world casino https://bonusonlinecasino24.com/
can you buy cialis online Fred Hutch pathologist Dr
amoxicillin 375 mg
zoloft lowest price
ivermectin usa price
pharmacy online shopping usa
prednisone acetate
cost for clomid tablet
albuterol sulfate inhaler
order modafinil uk
Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks..cryptoknowbase.com nimabi
buy propecia 5mg
clomid no prescription
baclofen cost
fildena 100 mg for sale
tretinoin buy mexico
ivermectin 3mg tablet
buy accutane no prescription
metformin online without a prescription
silagra tablets india
prednisolone 3 mg
prozac online without prescription
ivermectin 4
clonidine price
L’erezione è un complesso fenomeno neurovascolare sotto controllo ormonale; nel momento in cui si viene ad instaurare una disfunzione erettile, sia essa psicogena, organica o mista, se non correttamente individuata e diagnosticata, può avere un’evoluzione in alcuni casi irreversibile. Elevati livelli di ansia sono stati inoltre riscontrati in donne affette da dispareunia, soffrendo di forti dolori durante i rapporti sessuali. Lentezza sessuale maschio, ecco tutte li cause inoltre taluno rimedi efficaci. Dislivello erettile. Apprensione da prestazione Ma sotto li tra queste cè ovviamente quella della squilibrio erettile sbilanciamento erettile. Fai una quesito ai medici. Ti piace l’articolo? Potrai leggerlo quando vorrai accedendo alla tua Equilibrio Personale. Riceverai inoltre tutti gli aggiornamenti sullo stesso materiale. Ottieni consigli riguardo sanità su sobrietà su te! Cerca un medico nella tua megalopoli.
https://www.bitsdujour.com/profiles/S23omA
La richiesta viene subito accolta dall’Urologia dell’ospedale Federico II di Napoli, dove il prof. Vincenzo Mirone insieme al prof. David Ralph, dell’Andrology Unit University College Hospital London, eseguono per la prima volta in Italia su un paziente affetto da megalouretere l’impianto di una protesi peniena bicomponente, che provoca un’erezione del tutto simile a quella fisiologica. Come accennato, le pillole per il trattamento della disfunzione erettile possono aiutare le erezioni a diventare più forti e durare più a lungo, ma non indurranno un’erezione senza un qualche tipo di stimolazione. Piazza Vincenzo Calenda 14, 80139, Napoli Il Viagra è il nome commerciale del citrato di Sildenafil, il suo nome internazionale non proprietario. Il Viagra è un trattamento orale per la disfunzione erettile o l’impotenza negli uomini. L’impotenza è definita come incapacità di raggiungere o mantenere un’erezione sufficiente per l’attività sessuale. Il Viagra aiuta a ripristinare la scarsa funzione erettile aumentando il flusso di sangue al pene. La stimolazione sessuale è necessaria per l’uso e l’efficacia del Viagra. È un trattamento riservato agli uomini.
online propranolol prescription
fildena 150 online
where to buy stromectol online
baclofen 2265
albuterol 083
doxycycline for sale over the counter
ventolin salbutamol
where can i buy trazodone online
prozac prices canada
buy zoloft 100mg
cheap synthroid online
merck propecia
colchicine price south africa
furosemide 200 mg tab
10 mg prednisone tablets
amoxicillin 875 for sale without prescription
budesonide 0.25 mg
neurontin medicine
atarax 25 mg tablet
cheap levitra 10 mg
diflucan canada coupon
augmentin otc
toradol tablets australia
synthroid 75 mcg tablet
metformin how to get
propecia australia
amoxicillin
tretinoin price canada
robaxin price
canadian pharmacy viagra generic
order propecia
trazodone capsules
cost of amoxicillin
combivent respimat spacer
lasix without script
propecia uk best price
buy suhagra 25 mg
suhagra 100 pill
can i buy prozac in mexico
budesonide cost usa
purchase retin-a cream
generic ivermectin cream
levitra over the counter canada
cialis for sale
cheap levitra online
atarax 25mg uk
ventolin over the counter singapore
accutane 40 mg cost
how to get amoxicillin without prescription
buy finasteride 1mg australia
gabapentin 100mg price
bupropion 225 mg
diflucan capsule
purchase augmentin
how to get gabapentin online
ivermectin 3mg tablets price
levitra prices in mexico
clonidine 25 mg
wellbutrin xl 300
order lisinopril
innopran xl cost
no prescription proventil inhaler
propecia australia price
canadianpharmacy com
stromectol coronavirus
generic sildenafil sale online
buy zoloft online canada
augmentin otc
buy fildena
phenergan 25 mg over the counter
cost for generic prozac
buy paroxetine
fildena 25
zoloft 25mg price
synthroid 150 mg coupon
cheapest generic vardenafil
how to buy prozac
azithromycin online without prescription
20 mg vardenafil
baclofen online
robaxin 4212
doxycycline price 100mg
hydroxychloroquine tablets buy online
generic baclofen 10 mg
xenical prices
lasix 40 price
furosemide 500 mg
amoxicillin online fast delivery
suhagra online
zoloft 50 mg price in india
propecia 1 mg coupon
plaquenil for arthritis
diflucan over the counter
trazodone 200
propecia for women
paxil drug cost
clonidine 01 mg
fildena tablets
augmentin 375mg
lisinopril generic drug
medication lisinopril 5 mg
paroxetine 30
where can i get clomid uk
albuterol pills for sale
cost of augmentin 625 mg
orlistat generico
bupropion medication pills
can you buy diflucan online
lasix medication over the counter
gabapentin online pharmacy
propecia australia buy
purchase prozac
best canadian pharmacy
toradol pill form
levitra pills south africa
effexor prescription
accutane order
augmentin capsule price
buy celexa without prescription
albuterol online no prescription
can i buy propecia over the counter uk
zoloft uk
allopurinol tablets in india
azithromycin z-pak
tretinoin 0.5 cream buy online
bactrim 310 mg
viagra price comparison usa
toradol drug
budesonide for sale
metformin where to buy in uk
dapoxetine uk
tadalafil otc canada
mail order pharmacy
pharmaceutical online
baclofen 25 mg india
bupropion tab 100mg
bactrim buying
buy accutane usa
25mg prednisolone
inderal 40 price
toradol without prescription
finasteride online bonus
professional viagra
vermox otc
can you buy lisinopril
clomid 200 mg daily
doxycycline 75 mg coupon
buy gabapentin without a prescription
where to buy diflucan online
can you buy doxycycline
pharmacy com
where can i get accutane prescription
baclofen cream
where to buy propecia cheap
how much is levitra in mexico
where can i buy albuterol over the counter
prednisolone 25mg price uk
desyrel coupon
fluoxetine 25 mg
clonidine for blood pressure
phenergan 25 mg without prescription
citalopram 30 mg tablets
propecia 5mg
online pharmacy australia paypal
synthroid 150 cost
order clomid from india
prednisone 60 mg daily
doxycycline australia cost
amoxicillin 500mg prescription
can you buy clomid online uk
desyrel 50 mg
gabapentin 400
medication lyrica 50 mg
amoxicillin 875 pills
buy albuterol tablets
cost of synthroid
buy lyrica online europe
propecia 2018
where to buy retin a online uk
lyrica 150 mg
inderal cheapest
40 mg lasix
amoxicillin 500mg capsule buy online
buying bactrim
phenergan 12.5
toradol order
prozac 40 mg daily
albuterol tablets brand name
generic diflucan 150 mg
levitra 5mg
amoxicillin 975 mg
buy azithromycin no prescription
how much is amoxicillin online
albuterol tablets australia
silagra uk
prozac 60mg capsule
how to get ivermectin
metformin 1mg
price of colchicine
suhagra 100mg cheap
citalopram price uk
lexapro cheapest price
propecia cost canada
lisinopril cost us
propranolol canada
propecia 10 mg
gabapentin 100 mg capsule
trazodone 50mg
zoloft pills
generic name for ivermectin
prednisolone uk buy
diflucan 200 mg pill
propecia pharmacy uk
purchase ivermectin
gabapentin 2018
robaxin purchase online
hydroxychloroquine generic
paroxetine hcl 40 mg
where can you buy diflucan
4004 atarax
propecia from canada
paxil lowest price
diflucan online cheap without a prescription
metformin tablets for sale
how to get doxycycline 100mg
buy cialis daily use online
where to get doxycycline
generic augmentin online
generic for levitra
trazodone 50mg prescription cost
buy plaquenil online
generic cialis 20mg online
online zoloft
vermox 100
purchase finasteride without a prescription
suhagra 100mg price in india
robaxin 750 mg
buy cheap synthroid
celexa purchase
buy propecia for sale
price for augmentin
vermox purchase
trimox medication
dapoxetine 60mg brand name
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://accounts.binance.com/uk-UA/register-person?ref=WTOZ531Y
silagra uk
colchicine cost in canada
02 retin a
budesonide 25 mg
buy ventolin over the counter
trazodone for sale online
vermox prescription
Buy and sell cryptocurrencies directly from crypto wallets with the comfort of PayPal. Generate new revenue opportunities with digital assets for financial institutions. Scroll down for more cryptocurrency news and price updates. Cryptocurrencies are essentially private digital currencies. Investors and enthusiasts see crypto as an alternative means of completing transactions, a potential hedge against inflation, a store of value during periods of macroeconomic instability and a means of circumventing the traditional financial industry. Bitcoin and leading cryptocurrencies allow any internet user worldwide to complete financial transactions quickly and easily without relying on a bank or another financial intermediary. Can cryptocurrencies be used to make online purchases?Yes, cryptocurrencies are a medium of exchange, which can be used to make payments for online purchases. There are hundreds of online shops and retailers that accept Bitcoin and other cryptocurrencies. However, there is a catch. Both the buyer and seller should agree to accept the particular cryptocurrency for the deal. There are various search engines to find the goods and services that can be purchased using cryptocurrencies.
https://www.phone-bookmarks.win/cryptocom-2-factor-authentication
Did you know, you can also use HBAR to book flights? Well, you can throughAlternative Airlines. We offer 70+ cryptocurrency options, including Hedera Hashgraph (HBAR). Use this guide to find out how you can book flights using HBAR today! What is the service fee? To buy Hedera Hashgraph (HBAR) in Canada, you can set up an account on a cryptocurrency trading platform such as NDAX and buy HBAR directly with the Canadian dollar. Hedera is also designed as a network service provider for the operation of private closed blockchain systems (permissioned blockchains) often used by institutions, enterprises, and governments that are completely independent from Hedera’s permissionless public blockchain which uses the HBAR token (similarly to open public blockchains like Bitcoin and Ethereum).
fluoxetine 20 mg cap
zithromax generic
buy cheap fluoxetine
zoloft tablets canada
propecia discount
doxycycline 20 mg tablets
buy vermox online usa
quineprox 200 mg
buy brand name levitra
lisinopril brand
buy accutane online
diflucan online uk
diflucan 150 australia
zoloft prices australia
buy lyrica from india
paxil anxiety
doxycycline 10mg cost
vermox usa
diflucan 150 mg price
atarax 25mg tab
synthroid brand name
buy ventolin online nz
buy retin a in canada
metformin 500 mg over the counter
toradol 50
trimox 250
bactrim ds 800 160
diflucan 100 mg price
gabapentin in india
tretinoin cream 0.01
order vermox
neurontin for sale online
clonidine 0.3
generic vardenafil
how can i get amoxicillin in uk
buy gabapentin 400 mg
propecia 1mg buying online
doxycycline 100g
cheap amoxil online
best prices for viagra in canada
buy lisinopril 2.5 mg
metformin 500 pill
order augmentin online
toradol 10mg price
fluoxetine cap 10mg
albuterol inhalers for sale
otc albuterol
baclofen discount
price of metformin
propecia cheap price
hydroxychloroquine buy online uk
best generic propecia
stromectol 12mg online
synthroid 112 mcg in india
budesonide tablet brand name
xenical price
ivermectin generic cream
super avana online
diflucan 150 mg online
prednisone order online uk
clonidine price in india
zestril online
accutane price in india
50 mg prednisone canada pharmacy
effexor 75 mg
colchicine for pericarditis
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://www.binance.com/cs/register?ref=53551167
vibramycin 100mg
can you buy vermox over the counter in usa
zoloft 50 mg generic
trazodone 50 mg
deltasone price
how much is retin a cream in mexico
propranolol order online
allopurinol for sale
toradol pain shot
purchase azithromycin 500 mg tablets
propranolol online uk
http://ciprofloxacin.life/# antibiotics cipro
clonidine 0.1 mg oral tablets online orde
http://amoxil.icu/# canadian pharmacy amoxicillin
ivermectin pills canada
levitra online purchase
cost generic clomid pills order clomid pills – get generic clomid without prescription
atarax antihistamine
zoloft without script canada
order generic clomid no prescription: can i get clomid pill – how to get generic clomid for sale
prednisone 5 mg: order prednisone 10 mg tablet – prednisone 5 mg tablet
buying prednisone 4mg without prescription
http://amoxil.icu/# can you buy amoxicillin uk
propranolol 40 mg buy online
amoxicillin 875 coupon
cost of lasix 10mg
levitra 20 mg purchase
bactrim over the counter canada
ivermectin cream 1%
atarax 10mg cost
lyrica 200 mg price
clomid otc price
paroxetine cost
onlinecanadianpharmacy
silagra 100 mg for sale
bupropion india
atarax eq
buy inderal online usa
toradol 100mg
doxycycline vibramycin
over the counter diflucan
best price real viagra
http://cytotec.icu/# buy misoprostol over the counter
buy misoprostol over the counter: purchase cytotec – Misoprostol 200 mg buy online
glucophage xr generic
Misoprostol 200 mg buy online Cytotec 200mcg price Cytotec 200mcg price
buy cytotec over the counter: cytotec pills buy online – buy cytotec in usa
buy tamoxifen: generic tamoxifen – arimidex vs tamoxifen bodybuilding
http://cytotec.icu/# Cytotec 200mcg price
http://doxycyclinebestprice.pro/# doxylin
clonidine 0.1mg for sleep
Cytotec 200mcg price: cytotec online – buy misoprostol over the counter
amoxicillin 875 mg coupon
http://doxycyclinebestprice.pro/# buy doxycycline hyclate 100mg without a rx
zithromax capsules: buy zithromax canada – zithromax 500mg price in india
order clomid from canada
lisinopril 40 mg tablets: 30mg lisinopril – lisinopril 0.5 mg
http://nolvadex.fun/# tamoxifen for breast cancer prevention
lisinopril 20 mg tabs lisinopril 5 mg india price п»їbuy lisinopril 10 mg uk
buy doxycycline: buy doxycycline monohydrate – order doxycycline
http://lisinoprilbestprice.store/# lisinopril cost 40 mg
augmentin 125mg
female cialis canada
doxycycline hyc 100mg: doxycycline 50 mg – how to order doxycycline
doxycycline online uk
generic accutane canada
albuterol 90
http://nolvadex.fun/# tamoxifen hormone therapy
synthroid 5mcg
viagra best buy
trazodone 50 mg brand name
atarax medicine
where can i get doxycycline: doxycycline – buy cheap doxycycline online
lisinopril 10 mg canada zestril canada lisinopril 30 mg cost
buy cytotec online: buy cytotec over the counter – cytotec pills buy online
doxycycline capsules
dapoxetine medicine online
http://doxycyclinebestprice.pro/# doxycycline 50mg
generic colchicine
https://nolvadex.fun/# hysterectomy after breast cancer tamoxifen
doxycycline 100mg capsules: doxycycline 200 mg – doxylin
order doxycycline 100mg without prescription: buy doxycycline without prescription uk – buy doxycycline online without prescription
buy paroxetine uk
over the counter diflucan pill
http://indiapharm.llc/# world pharmacy india indiapharm.llc
mexican pharmaceuticals online: Mexico pharmacy online – best online pharmacies in mexico mexicopharm.com
best online pharmacy india India pharmacy of the world reputable indian online pharmacy indiapharm.llc
77 canadian pharmacy: Canadian online pharmacy – canadian pharmacy scam canadapharm.life
zithromax order
online shopping pharmacy india: Online India pharmacy – world pharmacy india indiapharm.llc
https://indiapharm.llc/# buy prescription drugs from india indiapharm.llc
baclofen 500 mg
pharmacies in mexico that ship to usa: Mexico pharmacy online – mexico drug stores pharmacies mexicopharm.com
http://mexicopharm.com/# medicine in mexico pharmacies mexicopharm.com
effexor sale
neurontin tablets
http://mexicopharm.com/# pharmacies in mexico that ship to usa mexicopharm.com
prozac prescription
online canadian drugstore: Pharmacies in Canada that ship to the US – canadian pharmacy meds canadapharm.life
zestril pill
india online pharmacy: Online India pharmacy – п»їlegitimate online pharmacies india indiapharm.llc
where can you buy amoxicillin
canadian family pharmacy Canadian online pharmacy canadian family pharmacy canadapharm.life
clonidine medicine
where can i purchase synthroid
reputable mexican pharmacies online: Best pharmacy in Mexico – mexican mail order pharmacies mexicopharm.com
https://mexicopharm.com/# mexico pharmacies prescription drugs mexicopharm.com
canadian drugs pharmacy: real canadian pharmacy – ordering drugs from canada canadapharm.life
fildena 100 online
canadian pharmacy scam: Pharmacies in Canada that ship to the US – precription drugs from canada canadapharm.life
buy silagra online
http://indiapharm.llc/# indian pharmacy paypal indiapharm.llc
http://indiapharm.llc/# п»їlegitimate online pharmacies india indiapharm.llc
mexican pharmacy: mexican pharmacy – reputable mexican pharmacies online mexicopharm.com
india pharmacy mail order: Medicines from India to USA online – pharmacy website india indiapharm.llc
wellbutrin cost uk
how much is zithromax 250 mg
global pharmacy canada: Pharmacies in Canada that ship to the US – best rated canadian pharmacy canadapharm.life
propranolol 25 mg
https://mexicopharm.com/# mexican rx online mexicopharm.com
where can i buy vermox
buying prescription drugs in mexico online: Mexico pharmacy online – mexico drug stores pharmacies mexicopharm.com
prednisolone 2.5 mg tablets
buy medicines online in india Online India pharmacy Online medicine home delivery indiapharm.llc
tretinoin online uk
http://mexicopharm.com/# buying prescription drugs in mexico online mexicopharm.com
legitimate canadian online pharmacies: Canadian pharmacy best prices – my canadian pharmacy canadapharm.life
doxycycline india
diflucan australia over the counter
https://edpillsdelivery.pro/# pills erectile dysfunction
sildenafil discount price: cheap sildenafil – citrate sildenafil
cure ed: buy ed drugs online – treatment of ed
http://levitradelivery.pro/# Levitra 10 mg buy online
tadalafil mexico Tadalafil 20mg price in Canada tadalafil
buy tadalafil online australia: cheap tadalafil canada – tadalafil 5mg uk
budecort 0.5 mg
http://tadalafildelivery.pro/# buy tadalafil 10mg india
natural ed medications: ed pills online – cheap erectile dysfunction pill
https://levitradelivery.pro/# Levitra 20 mg for sale
super avana
buy diflucan uk
http://sildenafildelivery.pro/# sildenafil chewable tablets
fluoxetin
vardenafil 40mg
Kamagra 100mg price: cheap kamagra – Kamagra 100mg price
http://kamagradelivery.pro/# super kamagra
generic albuterol online
buy tadalafil online paypal cheap tadalafil canada tadalafil tablets 20 mg india
buy silagra
ed pills online: buy ed drugs online – best male enhancement pills
Vardenafil price: Generic Levitra 20mg – Generic Levitra 20mg
where can i buy bactrim over the counter
can i buy albuterol online
doxycycline cheapest uk
http://sildenafildelivery.pro/# where to purchase sildenafil
Kamagra 100mg: cheap kamagra – buy kamagra online usa
http://edpillsdelivery.pro/# ed pills cheap
п»їkamagra: buy kamagra – Kamagra 100mg
propecia online prescription uk
lisinopril brand name uk
https://kamagradelivery.pro/# sildenafil oral jelly 100mg kamagra
tadalafil 20mg price in india: tadalafil daily 5mg – cost of generic tadalafil
sildenafil 50 mg tablet price: Cheapest Sildenafil online – sildenafil online prescription
Paxlovid buy online buy paxlovid online paxlovid price
http://prednisone.auction/# prednisone tabs 20 mg
medicine vermox
zoloft 100 mg cost
http://prednisone.auction/# order prednisone
https://amoxil.guru/# amoxicillin 500 mg where to buy
lisinopril 10 mg
200 mg gabapentin
can i buy synthroid from canada
cost of stromectol: minocycline hydrochloride – minocycline efectos secundarios
http://stromectol.guru/# ivermectin tablets order
paxlovid for sale paxlovid best price paxlovid generic
vermox tablet
https://paxlovid.guru/# paxlovid pharmacy
best viagra tablets in india online
http://amoxil.guru/# amoxicillin pharmacy price
amoxicillin penicillin
amoxicillin 500 mg without prescription: buy amoxicillin 500mg online – amoxicillin 500mg capsules antibiotic
https://paxlovid.guru/# Paxlovid buy online
http://prednisone.auction/# prednisone 100 mg
https://clomid.auction/# how to buy generic clomid no prescription
paxlovid cost without insurance paxlovid buy paxlovid india
over the counter trazodone
azithromycin nz pharmacy
http://amoxil.guru/# amoxicillin 500mg without prescription
buy doxycycline online usa
vermox 100mg
can you get generic clomid without rx: clomid generic – can i buy cheap clomid without prescription
https://clomid.auction/# how to get generic clomid without prescription
https://paxlovid.guru/# paxlovid buy
https://paxlovid.guru/# Paxlovid over the counter
https://clomid.auction/# where can i get generic clomid
propecia cost comparison uk
https://lisinopril.fun/# lisinopril 5 mg canada
buy zithromax online fast shipping: cheapest azithromycin – zithromax buy online
price of lisinopril in india High Blood Pressure buy zestril
albuterol medication
http://azithromycin.store/# zithromax purchase online
synthroid 62.5 mg
furosemide 40 mg: Over The Counter Lasix – furosemide 100 mg
vardenafil for sale
https://lisinopril.fun/# lisinopril 12.5 mg 20 mg
https://finasteride.men/# get propecia price
can you buy zithromax over the counter in australia: cheapest azithromycin – zithromax online paypal
zestoretic coupon
http://furosemide.pro/# lasix 20 mg
doxycycline without rx
zoloft best price
where can i purchase zithromax online Azithromycin 250 buy online cost of generic zithromax
https://misoprostol.shop/# cytotec pills online
100mg doxycycline
home: propecia otc – buy cheap propecia online
levitra 10
buy brand wellbutrin
over the counter atarax
buy cytotec online fast delivery: cheap cytotec – п»їcytotec pills online
phenergan tablets otc
buy tretinoin
order cheap propecia tablets: Best place to buy propecia – buying generic propecia without insurance
tretinoin prescription australia
https://finasteride.men/# cost cheap propecia without dr prescription
https://azithromycin.store/# zithromax over the counter canada
effexor canadian pharmacy
6000 mg accutane
cheap propecia without dr prescription: buy propecia – order generic propecia without insurance
buy cytotec pills online cheap buy cytotec online cytotec pills buy online
https://lisinopril.fun/# lisinopril pills 2.5 mg
buy propecia online pharmacy
levitra order
http://finasteride.men/# propecia without dr prescription
furosemida 40 mg: lasix generic name – lasix medication
can i buy prednisone online
amoxicillin 1972
purchase lisinopril online: cheapest lisinopril – 30mg lisinopril
price of augmentin 625mg
https://lisinopril.fun/# generic drug for lisinopril
cost of cheap propecia prices: buy cheap propecia online – get cheap propecia without dr prescription
where to buy phenergan online
https://azithromycin.store/# buy zithromax canada
lasix dosage: lasix side effects – lasix 100mg
cost cheap propecia for sale Best place to buy propecia get generic propecia online
where to buy fluoxetine online
http://finasteride.men/# buy cheap propecia without insurance
buy lyrica from india
suhagra 50 mg price
buy zithromax no prescription: Azithromycin 250 buy online – order zithromax without prescription
suhagra 100 usa
https://finasteride.men/# propecia buy
where to buy accutane in canada
cheap amoxicillin tablets
cheap propecia without insurance: generic propecia – cost of generic propecia without dr prescription
buy cytotec over the counter: buy cytotec online – cytotec buy online usa
amoxicillin 50 mg
albuterol 2mg tab
sildenafil sale in india
online pharmacy synthroid
lasix uses lasix 40 mg lasix medication
http://furosemide.pro/# lasix 100 mg tablet
bactrim 800 mg cost
cost of propecia online: buy propecia – generic propecia without a prescription
http://furosemide.pro/# buy furosemide online
http://finasteride.men/# get generic propecia tablets
cytotec online: buy misoprostol – buy cytotec pills online cheap
augmentin no prescription
cost propecia no prescription: buy propecia – cost of cheap propecia
buy misoprostol over the counter buy cytotec online Abortion pills online
furosemide 100mg: Buy Lasix – lasix dosage
http://kamagraitalia.shop/# farmacie online sicure
synthroid medication online
accutane for sale
lasix 12.5
farmacie online autorizzate elenco: kamagra oral jelly consegna 24 ore – п»їfarmacia online migliore
augmentin 1000 mg
https://avanafilitalia.online/# comprare farmaci online con ricetta
http://sildenafilitalia.men/# viagra pfizer 25mg prezzo
ivermectin 6mg dosage
dapoxetine 60 mg tablet price in india
farmacia online piГ№ conveniente: Farmacie a roma che vendono cialis senza ricetta – farmacia online
http://tadalafilitalia.pro/# acquistare farmaci senza ricetta
trazodone pill 50mg
diflucan 300 mg
http://sildenafilitalia.men/# viagra naturale
azithromycin 500mg buy
viagra prezzo farmacia 2023: sildenafil 100mg prezzo – viagra 100 mg prezzo in farmacia
https://kamagraitalia.shop/# farmacia online senza ricetta
acquistare farmaci senza ricetta: kamagra oral jelly – migliori farmacie online 2023
pillole per erezioni fortissime alternativa al viagra senza ricetta in farmacia viagra online spedizione gratuita
http://avanafilitalia.online/# farmacia online senza ricetta
farmacie online affidabili: avanafil prezzo – farmacia online migliore
where to get trazodone
farmacie online autorizzate elenco: avanafil prezzo in farmacia – farmacia online
http://kamagraitalia.shop/# farmacie on line spedizione gratuita
synthroid cost without insurance
http://kamagraitalia.shop/# comprare farmaci online con ricetta
farmacia online migliore: kamagra oral jelly – farmacia online miglior prezzo
http://tadalafilitalia.pro/# farmacia online senza ricetta
generic clomid for sale
https://farmaciaitalia.store/# acquisto farmaci con ricetta
generic for colchicine
viagra originale in 24 ore contrassegno: viagra cosa serve – cerco viagra a buon prezzo
comprare farmaci online all’estero cialis generico farmacie online sicure
buy atarax online canada
zestoretic 20 mg
http://tadalafilitalia.pro/# comprare farmaci online con ricetta
baclofen 832
migliori farmacie online 2023: avanafil – acquistare farmaci senza ricetta
accutane online pharmacy india
canadian pharmacy lyrica
farmacia online piГ№ conveniente: farmacia online – farmacie online affidabili
https://avanafilitalia.online/# farmacia online migliore
acquisto farmaci con ricetta: kamagra oral jelly consegna 24 ore – п»їfarmacia online migliore
prozac 60 mg
https://sildenafilitalia.men/# viagra 50 mg prezzo in farmacia
zoloft rx coupon
http://indiapharm.life/# mail order pharmacy india
order cialis from india
canada pharmacy 24h: cheap canadian pharmacy online – canada drugs online review
india online pharmacy: top 10 pharmacies in india – top 10 online pharmacy in india
zithromax capsules
legitimate canadian pharmacies: is canadian pharmacy legit – canadian pharmacy ratings
http://mexicanpharm.store/# mexican mail order pharmacies
amoxicillin otc
baclofen 5 mg brand name
robaxin otc south africa
augmentin 625 in canada
canadian pharmacy 24 com recommended canadian pharmacies canada rx pharmacy world
medication from mexico pharmacy: pharmacies in mexico that ship to usa – mexico pharmacy
http://mexicanpharm.store/# mexican pharmaceuticals online
legitimate canadian pharmacy: canada pharmacy online – canadian pharmacy india
http://indiapharm.life/# best india pharmacy
inderal order
propecia 1mg india
india pharmacy mail order: india online pharmacy – top online pharmacy india
brand viagra no prescription
canadian pharmacy antibiotics: canadian pharmacy 24h com safe – canadian pharmacy ed medications
http://mexicanpharm.store/# mexican mail order pharmacies
zoloft pills for sale
baclofen 75 mg
indianpharmacy com: india pharmacy mail order – top 10 pharmacies in india
http://canadapharm.shop/# safe canadian pharmacy
accutane medicine in india
amoxicillin 500 mg buy
mexico pharmacy: mexico drug stores pharmacies – mexican pharmacy
http://canadapharm.shop/# canadianpharmacyworld com
india pharmacy: india pharmacy mail order – canadian pharmacy india
best online pharmacy india mail order pharmacy india indianpharmacy com
https://mexicanpharm.store/# mexican mail order pharmacies
mexican pharmacy what to buy
canadian pharmacy mall: canadian pharmacy no rx needed – canadapharmacyonline com
buy ventolin over the counter
https://canadapharm.shop/# canadapharmacyonline legit
top 10 online pharmacy in india: п»їlegitimate online pharmacies india – Online medicine home delivery
prozac generic price
reputable mexican pharmacies online: buying from online mexican pharmacy – mexico pharmacies prescription drugs
phenergan dm
furosemide 80 mg tablet
http://indiapharm.life/# indian pharmacy online
synthroid 0.05 mcg
canadian pharmacy phone number: canadian king pharmacy – canadian pharmacy
mexico drug stores pharmacies: mexican pharmacy – mexican drugstore online
celexa 90mg
https://canadapharm.shop/# best canadian pharmacy to order from
100 doxycycline
precription drugs from canada: medication canadian pharmacy – best mail order pharmacy canada
indian pharmacy paypal indian pharmacy indian pharmacy online
https://canadapharm.shop/# best canadian online pharmacy
where can i buy stromectol
toradol brand
cheap viagra online free shipping australia
canadian pharmacy: canada drugs – recommended canadian pharmacies
indianpharmacy com: top 10 online pharmacy in india – indian pharmacy
amoxicillin uk price
https://mexicanpharm.store/# mexico drug stores pharmacies
best effexor prices
baclofen australia
can i buy amoxil over the counter
lioresal sale
safe online pharmacies in canada: canadian drug stores – certified canadian pharmacy
https://indiapharm.life/# reputable indian pharmacies
levitra canada no rx
http://canadapharm.shop/# canadian pharmacy meds review
online pharmacy india: world pharmacy india – indianpharmacy com
how to get zithromax online: zithromax 250mg – buy zithromax online cheap
ivermectin australia
colchicine 0.6 mg tablet canada
buy atarax online uk
gabapentin 200 mg
http://zithromaxpharm.online/# buy zithromax 1000mg online
buy effexor online usa without prescription
how much is generic phenergan
Their international patient care is impeccable http://clomidpharm.shop/# how to buy clomid
zithromax 500mg price in india: zithromax 500mg price in india – generic zithromax 500mg india
amoxicillin over the counter usa
buy cheap propecia uk
http://cytotec.directory/# п»їcytotec pills online
The staff is well-trained and always courteous https://nolvadex.pro/# tamoxifen brand name
buy cytotec pills online cheap buy cytotec pills order cytotec online
buy misoprostol over the counter: cytotec abortion pill – cytotec pills buy online
budesonide tablets
https://clomidpharm.shop/# where can i get cheap clomid without prescription
buy dapoxetine paypal
http://prednisonepharm.store/# prednisone 25mg from canada
Commonly Used Drugs Charts https://prednisonepharm.store/# 40 mg prednisone pill
allopurinol purchase
buy generic accutane
zithromax over the counter canada: zithromax buy online no prescription – buy zithromax online fast shipping
https://clomidpharm.shop/# can you get clomid pills
Efficient service with a personal touch https://zithromaxpharm.online/# zithromax 250 mg australia
how to prevent hair loss while on tamoxifen: tamoxifen buy – tamoxifen for breast cancer prevention
This pharmacy has a wonderful community feel http://prednisonepharm.store/# how much is prednisone 10mg
http://prednisonepharm.store/# canada buy prednisone online
lisinopril brand name in india
how to buy cheap clomid price how to get clomid without insurance can i purchase generic clomid tablets
doxycycline hyclate 100mg price
Their global reach is unmatched https://cytotec.directory/# buy cytotec online
https://cytotec.directory/# buy cytotec pills online cheap
order cytotec online: buy cytotec online fast delivery – Misoprostol 200 mg buy online
doxycycline prescription cost
http://prednisonepharm.store/# prednisone in canada
suhagra 50 mg buy
gabapentin cost
combivent brand
1000 mg augmentin
Their loyalty program offers great deals http://cytotec.directory/# cytotec buy online usa
https://zithromaxpharm.online/# generic zithromax 500mg
amoxicillin 875 mg buy online
tamoxifen hip pain: tamoxifen skin changes – alternatives to tamoxifen
amoxil 875 price
atarax 25 mg buy
A universal solution for all pharmaceutical needs http://nolvadex.pro/# generic tamoxifen
buy vermox tablets
synthroid 1
how much is diflucan
https://clomidpharm.shop/# where can i get cheap clomid without insurance
prednisone 5 mg tablet rx: can i buy prednisone online without a prescription – prednisone canada prices
suhagra 50
Misoprostol 200 mg buy online buy cytotec pills online cheap buy cytotec pills
neurontin prescription cost
budesonide 3 mg cost
non prescription ed drugs: tadalafil without a doctor’s prescription – generic viagra without a doctor prescription
http://edpills.bid/# male ed drugs
meds online without doctor prescription best ed pills non prescription prescription drugs online without doctor
https://edpills.bid/# ed drugs
toradol pill 10mg
lisinopril drug
pharmacies not requiring a prescription https://reputablepharmacies.online/# mexican border pharmacies
canadian pharmacy certified
certified mexican pharmacy: compare prescription drug prices – cheapest canadian pharmacies
ed pills that work best non prescription ed pills new treatments for ed
https://reputablepharmacies.online/# best canadian pharmacies
best ed medications: cures for ed – what is the best ed pill
ed meds online without doctor prescription buy prescription drugs from canada viagra without doctor prescription amazon
drugs for ed: ed remedies – medicine for impotence
https://edpills.bid/# cheapest ed pills online
50 mcg synthroid
colchicine 0.6 mg tablets
viagra without a prescription non prescription ed drugs mexican pharmacy without prescription
express pharmacy http://reputablepharmacies.online/# discount viagra canadian pharmacy
pharmacies canada
https://edwithoutdoctorprescription.store/# buy prescription drugs online legally
non prescription erection pills: ed pills online – ed pills cheap
http://edwithoutdoctorprescription.store/# non prescription ed drugs
how to get amoxicillin online
cheapest ed pills online non prescription erection pills ed drugs
baclofen 5 mg tablet
buy real paxil online
natural ed medications: pills erectile dysfunction – ed pills for sale
cheapest ed pills ed drugs compared best ed pills non prescription
http://edpills.bid/# non prescription erection pills
reputable online canadian pharmacies: online drugstore without prescription – canadian pharmacies mail order
best non prescription ed pills: prescription meds without the prescriptions – meds online without doctor prescription
augmentin tablets 375mg
augmentin 375 mg price
real viagra without a doctor prescription usa real viagra without a doctor prescription prescription drugs without doctor approval
ozempic tablets for weight loss
http://edwithoutdoctorprescription.store/# buy prescription drugs online legally
semaglutide buy australia
online prescription for ed meds: prescription drugs online without – legal to buy prescription drugs without prescription
rybelsus where to buy
new ed drugs ed meds online cheap ed drugs
semaglutide injection
buy ozempic in mexico
cheap ozempic
https://reputablepharmacies.online/# online ed drugs no prescription
brand ozempic
http://edpills.bid/# erection pills viagra online
pills for erection: ed pills gnc – erection pills that work
ed meds online without prescription or membership buy prescription drugs from canada cheap how to get prescription drugs without doctor
canadian pharmacies online: online canadian pharmacy – canada pharmacy canadianpharmacy.pro
http://canadianpharmacy.pro/# canadianpharmacymeds canadianpharmacy.pro
Online medicine order indian pharmacy reputable indian online pharmacy indianpharmacy.shop
http://mexicanpharmacy.win/# medicine in mexico pharmacies mexicanpharmacy.win
wegovy semaglutide
reputable indian online pharmacy: top online pharmacy india – reputable indian online pharmacy indianpharmacy.shop
https://canadianpharmacy.pro/# canadian neighbor pharmacy canadianpharmacy.pro
list of approved canadian pharmacies
canadian pharmacy online canadian drugstore online canadian pharmacy world canadianpharmacy.pro
https://mexicanpharmacy.win/# buying from online mexican pharmacy mexicanpharmacy.win
semaglutide tablets for weight loss cost
best online pharmacies in mexico: online mexican pharmacy – mexican online pharmacies prescription drugs mexicanpharmacy.win
buying drugs from canada online canadian pharmacy canadapharmacyonline legit canadianpharmacy.pro
http://indianpharmacy.shop/# pharmacy website india indianpharmacy.shop
Online medicine order Cheapest online pharmacy Online medicine order indianpharmacy.shop
rybelsus online uk
https://canadianpharmacy.pro/# online canadian pharmacy review canadianpharmacy.pro
https://mexicanpharmacy.win/# reputable mexican pharmacies online mexicanpharmacy.win
buy ozempic cheap
india online pharmacy online pharmacy india Online medicine home delivery indianpharmacy.shop
http://canadianpharmacy.pro/# canadian pharmacies comparison canadianpharmacy.pro
superstore pharmacy online
rybelsus 3mg
wegovy where to buy
where can i buy semaglutide
http://mexicanpharmacy.win/# mexico pharmacies prescription drugs mexicanpharmacy.win
order semaglutide online
where can i buy ozempic
https://mexicanpharmacy.win/# mexican border pharmacies shipping to usa mexicanpharmacy.win
http://mexicanpharmacy.win/# mexico drug stores pharmacies mexicanpharmacy.win
online shopping pharmacy india
reputable indian online pharmacy indian pharmacy best india pharmacy indianpharmacy.shop
wegovy uk
https://indianpharmacy.shop/# mail order pharmacy india indianpharmacy.shop
https://canadianpharmacy.pro/# canadian drugstore online canadianpharmacy.pro
Online medicine order
canadianpharmacyworld Canadian pharmacy online canadian pharmacy meds review canadianpharmacy.pro
https://mexicanpharmacy.win/# mexican border pharmacies shipping to usa mexicanpharmacy.win
generic ozempic
http://canadianpharmacy.pro/# canadian pharmacy 365 canadianpharmacy.pro
https://mexicanpharmacy.win/# mexico drug stores pharmacies mexicanpharmacy.win
reputable indian online pharmacy
ozempic tablets for weight loss
generic wegovy for weight loss
semaglutide cost
http://mexicanpharmacy.win/# п»їbest mexican online pharmacies mexicanpharmacy.win
canadian pharmacy online without prescription
canadapharmacyonline com Pharmacies in Canada that ship to the US cheapest pharmacy canada canadianpharmacy.pro
buy semaglutide uk
http://canadianpharmacy.pro/# legitimate canadian online pharmacies canadianpharmacy.pro
reputable indian online pharmacy
http://mexicanpharmacy.win/# mexico drug stores pharmacies mexicanpharmacy.win
buy wegovy
buy rybelsus canada
best canadian online pharmacy reviews Pharmacies in Canada that ship to the US buying drugs from canada canadianpharmacy.pro
rybelsus buy from canada
http://mexicanpharmacy.win/# mexico pharmacies prescription drugs mexicanpharmacy.win
best india pharmacy
https://indianpharmacy.shop/# top online pharmacy india indianpharmacy.shop
wegovy tab 14mg
semaglutide for sale
buy wegovy online no script needed
mexican pharmacy п»їbest mexican online pharmacies mexican mail order pharmacies mexicanpharmacy.win
http://canadianpharmacy.pro/# safe online pharmacies in canada canadianpharmacy.pro
cheapest online pharmacy india
buy semaglutide
https://indianpharmacy.shop/# indian pharmacy paypal indianpharmacy.shop
http://mexicanpharmacy.win/# mexican rx online mexicanpharmacy.win
online prescriptions without a doctor
wegovy medicine
brand ozempic
buy rybelsus in canada
mexico pharmacies prescription drugs: Medicines Mexico – mexican pharmaceuticals online mexicanpharmacy.win
http://mexicanpharmacy.win/# mexican mail order pharmacies mexicanpharmacy.win
buying prescription drugs in mexico Medicines Mexico buying from online mexican pharmacy mexicanpharmacy.win
https://indianpharmacy.shop/# best online pharmacy india indianpharmacy.shop
best online pharmacy india
ozempic cost
http://acheterkamagra.pro/# pharmacie ouverte
ozempic tab 7mg
Pharmacie en ligne fiable: Levitra pharmacie en ligne – Pharmacie en ligne sans ordonnance
Viagra pas cher livraison rapide france: Meilleur Viagra sans ordonnance 24h – Viagra Pfizer sans ordonnance
wegovy semaglutide tablets cost
wegovy sale
Pharmacie en ligne livraison 24h PharmaDoc Pharmacie en ligne livraison rapide
semaglutide online
http://cialissansordonnance.shop/# acheter medicament a l etranger sans ordonnance
Pharmacie en ligne livraison gratuite
rybelsus xl
rybelsus best price
http://pharmadoc.pro/# Pharmacie en ligne livraison rapide
Pharmacie en ligne pas cher: pharmacie en ligne sans ordonnance – Pharmacie en ligne pas cher
purchase ozempic
acheter mГ©dicaments Г l’Г©tranger Pharmacie en ligne fiable acheter mГ©dicaments Г l’Г©tranger
http://cialissansordonnance.shop/# Pharmacie en ligne France
wegovy semaglutide tablets 3mg
generic wegovy
pharmacie ouverte: Pharmacie en ligne livraison 24h – Pharmacie en ligne pas cher
http://viagrasansordonnance.pro/# SildГ©nafil 100 mg sans ordonnance
п»їpharmacie en ligne
Pharmacie en ligne sans ordonnance: Pharmacies en ligne certifiees – Pharmacie en ligne France
wegovy 14
https://viagrasansordonnance.pro/# Viagra générique pas cher livraison rapide
rybelsus rx
Viagra sans ordonnance 24h suisse Viagra homme prix en pharmacie Viagra gГ©nГ©rique pas cher livraison rapide
Viagra pas cher livraison rapide france: Acheter du Viagra sans ordonnance – Sildenafil teva 100 mg sans ordonnance
https://acheterkamagra.pro/# pharmacie ouverte 24/24
wegovy 3mg
Pharmacie en ligne pas cher: kamagra 100mg prix – Pharmacie en ligne livraison 24h
https://levitrasansordonnance.pro/# acheter medicament a l etranger sans ordonnance
Pharmacie en ligne fiable pharmacie en ligne pas cher pharmacie ouverte 24/24
semaglutide online pharmacy
buy rybelsus canada
SildГ©nafil Teva 100 mg acheter: Viagra pas cher livraison rapide france – Viagra homme prix en pharmacie sans ordonnance
buy semaglutide in canada
Pharmacie en ligne pas cher: pharmacie en ligne pas cher – Pharmacie en ligne sans ordonnance
http://cialissansordonnance.shop/# Pharmacie en ligne pas cher
https://viagrasansordonnance.pro/# Viagra pas cher livraison rapide france
Pharmacie en ligne sans ordonnance
Pharmacie en ligne sans ordonnance: levitra generique prix en pharmacie – Pharmacie en ligne livraison gratuite
semaglutide 7mg
wegovy 7 mg
https://amoxicillin.bid/# amoxicillin without a doctors prescription
where can you buy zithromax: zithromax 500 tablet – zithromax price south africa
http://amoxicillin.bid/# amoxicillin buy no prescription
wegovy sale
wegovy sale
buy ivermectin cream ivermectin 10 mg ivermectin 6
order rybelsus online
semaglutide 21 mg
https://prednisonetablets.shop/# prednisone canada
ivermectin buy nz: ivermectin price canada – stromectol 3mg
semaglutide online prescription
minocycline 50 mg otc: minocycline 100 mg for sale – ivermectin lice
buy zithromax online buy zithromax online cheap zithromax online usa no prescription
rybelsus xl
semaglutide retail price
amoxicillin 500mg buy online canada: amoxicillin 500mg capsule – amoxicillin online canada
http://prednisonetablets.shop/# prednisone 100 mg
buy semaglutide from canada
can i buy amoxicillin over the counter in australia amoxicillin 500mg price in canada can you buy amoxicillin uk
where can i buy amoxicillin without prec: generic amoxicillin online – amoxil generic
http://amoxicillin.bid/# amoxicillin online no prescription
buy semaglutide online
https://prednisonetablets.shop/# buy 40 mg prednisone
rybelsus semaglutide tablets cost
ozempic tablets buy
can i get clomid pill: cost generic clomid no prescription – get generic clomid tablets
zithromax 500mg over the counter zithromax 500mg price in india zithromax 1000 mg pills
wegovy online pharmacy
amoxicillin 500 mg price: where to buy amoxicillin – amoxicillin online canada
https://clomiphene.icu/# generic clomid price
semaglutide buy uk
zithromax 500 mg lowest price drugstore online: buy zithromax 500mg online – where can i buy zithromax capsules
buy ozempic online no script needed
buy ozempic from canada online
http://clomiphene.icu/# where to buy clomid tablets
buy ozempic online cheap
prednisone 100 mg average cost of generic prednisone fast shipping prednisone
where to buy clomid online: where can i buy generic clomid without dr prescription – cost of generic clomid without prescription
https://prednisonetablets.shop/# prednisone for dogs
https://amoxicillin.bid/# amoxicillin 250 mg
buy semaglutide
stromectol xl: stromectol price usa – minocycline 100mg without a doctor
can i order clomid tablets can i buy clomid without insurance can you buy clomid without a prescription
amoxicillin without rx: amoxicillin 500 mg for sale – amoxicillin medicine
rybelsus oral medication
rybelsus semaglutide tablets 3mg
http://azithromycin.bid/# zithromax 500
wegovy medicine
rybelsus tablets for weight loss
buy ozempic
prednisone pharmacy prices: generic prednisone cost – prednisone steroids
clomid generics how can i get cheap clomid without insurance can you buy cheap clomid now
wegovy diabetes
buy semaglutide
http://amoxicillin.bid/# amoxicillin azithromycin
semaglutide xr
buy ozempic pill form for adults
https://canadianpharm.store/# legitimate canadian online pharmacies canadianpharm.store
medicine in mexico pharmacies: Online Mexican pharmacy – mexican drugstore online mexicanpharm.shop
semaglutide cost
online pharmacy india: Indian pharmacy to USA – world pharmacy india indianpharm.store
http://indianpharm.store/# п»їlegitimate online pharmacies india indianpharm.store
canadian pharmacies comparison Canadian Pharmacy canadian drug prices canadianpharm.store
semaglutide tab 3mg
buy semaglutide online no script
https://indianpharm.store/# buy medicines online in india indianpharm.store
ed drugs online from canada: real canadian pharmacy – reliable canadian pharmacy reviews canadianpharm.store
semaglutide cost
rybelsus where to buy
medicine in mexico pharmacies Online Mexican pharmacy mexico pharmacy mexicanpharm.shop
https://mexicanpharm.shop/# reputable mexican pharmacies online mexicanpharm.shop
canadian pharmacy prices: Canada Pharmacy online – pet meds without vet prescription canada canadianpharm.store
reputable mexican pharmacies online: Certified Pharmacy from Mexico – pharmacies in mexico that ship to usa mexicanpharm.shop
canadian online drugs: canada drugs – cheapest pharmacy canada canadianpharm.store
mexican pharmaceuticals online Online Mexican pharmacy mexico drug stores pharmacies mexicanpharm.shop
rybelsus tablets buy
buy ozempic from canada online
rybelsus 14mg tablets
http://canadianpharm.store/# certified canadian international pharmacy canadianpharm.store
indianpharmacy com: india pharmacy mail order – cheapest online pharmacy india indianpharm.store
semaglutide 7 mg
semaglutide 21 mg
http://canadianpharm.store/# reliable canadian pharmacy canadianpharm.store
pharmacy website india: india pharmacy mail order – best india pharmacy indianpharm.store
top 10 online pharmacy in india Indian pharmacy to USA top 10 online pharmacy in india indianpharm.store
https://mexicanpharm.shop/# mexican online pharmacies prescription drugs mexicanpharm.shop
buy ozempic online no script needed
buying prescription drugs in mexico: Online Mexican pharmacy – best online pharmacies in mexico mexicanpharm.shop
wegovy buy from canada
buy ozempic
https://indianpharm.store/# online shopping pharmacy india indianpharm.store
generic wegovy cost
canadianpharmacyworld Canadian Pharmacy reliable canadian online pharmacy canadianpharm.store
reputable mexican pharmacies online: reputable mexican pharmacies online – mexican border pharmacies shipping to usa mexicanpharm.shop
canada rx pharmacy: Pharmacies in Canada that ship to the US – pharmacies in canada that ship to the us canadianpharm.store
rybelsus online uk
semaglutide 14
canada pharmacy 24h: Licensed Online Pharmacy – canadian pharmacy drugs online canadianpharm.store
https://indianpharm.store/# reputable indian pharmacies indianpharm.store
buy semaglutide from india
semaglutide injection
canadian pharmacy com Certified Online Pharmacy Canada recommended canadian pharmacies canadianpharm.store
п»їbest mexican online pharmacies: Online Pharmacies in Mexico – medication from mexico pharmacy mexicanpharm.shop
rybelsus semaglutide tablets 3mg
rybelsus online pharmacy
wegovy tablets for weight loss
http://canadianpharm.store/# canadian pharmacy 24 com canadianpharm.store
http://indianpharm.store/# п»їlegitimate online pharmacies india indianpharm.store
top online pharmacy india: Indian pharmacy to USA – indian pharmacy online indianpharm.store
reliable canadian pharmacy Licensed Online Pharmacy canadian drugs pharmacy canadianpharm.store
wegovy price
http://canadianpharm.store/# legitimate canadian pharmacies canadianpharm.store
online shopping pharmacy india: international medicine delivery from india – top 10 pharmacies in india indianpharm.store
buy rybelsus from canada
canadian online drugstore: Canadian Pharmacy – canadian world pharmacy canadianpharm.store
buy prescription drugs from india: india online pharmacy – reputable indian online pharmacy indianpharm.store
buy ozempic
semaglutide online cheap
http://indianpharm.store/# india pharmacy indianpharm.store
mexican drugstore online mexican mail order pharmacies mexican mail order pharmacies mexicanpharm.shop
mexican mail order pharmacies: Online Mexican pharmacy – mexican border pharmacies shipping to usa mexicanpharm.shop
wegovy 3 mg tablet
wegovy buy from canada
buy ozempic
semaglutide xr
semaglutide from canada
buy semaglutide uk
ozempic semaglutide tablets 3mg
https://indianpharm.store/# top 10 pharmacies in india indianpharm.store
buy semaglutide in mexico
online canadian pharmacy reviews Licensed Online Pharmacy cheap canadian pharmacy canadianpharm.store
my canadian pharmacy rx: Certified Online Pharmacy Canada – recommended canadian pharmacies canadianpharm.store
https://canadianpharm.store/# northern pharmacy canada canadianpharm.store
medicine in mexico pharmacies: Certified Pharmacy from Mexico – mexico pharmacies prescription drugs mexicanpharm.shop
semaglutide australia online
semaglutide tab 14mg
order ozempic
semaglutide ozempic
https://mexicanpharm.shop/# best mexican online pharmacies mexicanpharm.shop
wegovy tablets for weight loss cost
canadian pharmacies comparison: Canada Pharmacy online – canadian neighbor pharmacy canadianpharm.store
india online pharmacy: Indian pharmacy to USA – best india pharmacy indianpharm.store
mail order pharmacy india international medicine delivery from india indianpharmacy com indianpharm.store
buy rybelsus
buy rybelsus from canada
https://canadianpharm.store/# legitimate canadian pharmacies canadianpharm.store
A world at play and a world to its own, Mohegan Sun offers the best of the best in entertainment. From our 10,000-seat Mohegan Sun Arena and our 350-seat Wolf Den to our upscale, edgy comedy club, we are the premier destination for music, sports, comedy and more. Explore our calendar of events today for your next memorable night! Vegas Downtown Slots & Words No, you don’t. You can play the Hot Shot Progressive slot machine right here at VegasSlotsOnline. Check out its special features to decide if you’d gamble real money on this game. 10 July, 2021: The release of 100+ new free casino slot games for fun play is expected from Aristocrat, IGT, and Konami providers. Among novelties are the sensational mind-blowing Deadworld, classic 20, 40 Super Hot, Flaming Hot, Jurassic World, Reactions, Sweet Bonanza, and Anubis. Also, we’re happy to announce ten new providers with their flagship demo games whose names we keep secret. Keep on following freeslotsHUB and stay up to date with new products announced!
https://elliothyzh913567.digitollblog.com/24432003/manual-article-review-is-required-for-this-article
Lucky Tiger Casino No Deposit Bonus Codes – Get ($25 Free) Looking for a chance to win big? Lucky Tiger Casino is offering a $25 free bonus with no deposit… Rich Race Tournament Happytiger.co.uk reserves the right to let the Bingo bonus offer expire after the activation and wagering deadline. You can only have one active bonus offer at a time. This Bingo bonus offer can therefore not be combined with other bonuses, promotions or offers. I, Zombie Slot Review => Get (80 Free Spins) No Deposit Bonus Halloween Casino Promotions A slot… With the exception of progressive jackpot winnings, bonus and winnings generated through bonus play are capped at 10x deposit. This offer may be withdrawn modified at any time at the sole discretion of Happytiger.co.uk. General terms and conditions always apply, see HERE .
wegovy canada pharmacy
buy semaglutide in mexico
rybelsus 7mg
semaglutide cost
semaglutide online cheap
http://canadadrugs.pro/# reputable online canadian pharmacies
online prescriptions canada without: medicine canada – cheapest viagra canadian pharmacy
canadian pharmacy 24hr: reliable online pharmacy – prescription prices
wegovy canada pharmacy prices
rybelsus price
non prescription canadian pharmacies: canadian pharmacies without prescriptions – foreign online pharmacy
canadian online pharmacy no prescription drugs online no prescription canadian pharmacies
semaglutide 14mg tablets
wegovy where to buy
http://canadadrugs.pro/# pharmacy canada online
canada drug pharmacy: online pharmacy no prescription – canadian drugstore cialis
semaglutide uk
online prescriptions canada without canadian pharmacy no prescription required canadian drug prices
semaglutide oral medication
http://canadadrugs.pro/# ed drugs online
canadian drug: canada pharmacy online orders – prescription price checker
semaglutide where to buy
wegovy prescription
legitimate online pharmacies: canadian pharmacies online legitimate – mexican drugstore online
where to buy semaglutide online
discount viagra canadian pharmacy: overseas pharmacies – canadian prescription filled in the us
no 1 canadian pharmacy canada drug store best online canadian pharmacy review
rybelsus without prescription
http://canadadrugs.pro/# mexican pharmacy online no prescription
pharmacies withour prescriptions: prescription drug price comparison – trust pharmacy canada
buy rybelsus
buy semaglutide canada
reputable canadian mail order pharmacies express pharmacy reputable online pharmacy
internet pharmacy no prescription: discount online canadian pharmacy – buy prescriptions online
Thanks for the complete information. You helped me.
https://canadadrugs.pro/# cheap meds no prescription
prescription drugs without prior prescription: drugs from canada with prescription – top rated canadian mail order pharmacies
canada pharmacy estrogen without prescription: non prescription drugs – top mail order pharmacies
semaglutide generic
ozempic pill form
rybelsus price
http://canadadrugs.pro/# international pharmacies that ship to the usa
semaglutide injections
ozempic semaglutide tablets 3mg
semaglutide canada
top rated canadian pharmacies online: canadian pharmaceuticals – pharmacy price comparison
buy wegovy online from india
https://canadadrugs.pro/# canadian pharmacy delivery
canadian pharmacy no prescription: canada pharmacy online no prescription – canadian pharmacy usa
wegovy for sale
no rx online pharmacy: online pharmacies without prescription – ed meds online without doctor prescription
ozempic
http://canadadrugs.pro/# canadian pharmacy reviews
rybelsus 3 mg
semaglutide price
buy semaglutide online no script
top online canadian pharmacies: best online pharmacy without prescriptions – best price prescription drugs
generic rybelsus cost
buy semaglutide online pharmacy
ozempic tablets buy
https://canadadrugs.pro/# mexican pharmacy
safe canadian pharmacies online: best internet pharmacies – canadian meds without prescription
rybelsus generic cost
buy semaglutide online no script needed
rybelsus price
rybelsus 14mg
top rated online pharmacies: amazon pharmacy drug prices – vipps accredited online pharmacy
semaglutide injections
semaglutide cost
http://canadadrugs.pro/# pharmacy price comparison
rybelsus tablets cost
It’s exactly this long term performance that reflects MicroStrategy CEO Michael Saylor’s belief that “Bitcoin, as the world’s most widely-adopted cryptocurrency, is a dependable store of value and an attractive investment asset with more long-term appreciation potential than holding cash. MicroStrategy has recognized Bitcoin as a legitimate investment asset that can be superior to cash and accordingly has made Bitcoin the principal holding in its treasury reserve strategy.” Zhao warned that, after the FTX collapse and plummeting confidence in crypto, the market is in a period of “high volatility and unpredictableness” that makes it particularly unfavorable for inexperienced investors or those without ample funds. The critical issue is that Bitcoin’s utility is lacking relative to these other projects. As stated by Fortune, the Bitcoin network is hobbled by a lack of capacity. Moreover, Bitcoin’s network still relies on the outdated ‘mining’ process, which is exceptionally energy-intensive and has been roundly criticized by all corners of the media.
https://idyler.com/website-list-364/
Rhetorical contortions aside, Coinbase bills staking as a step in the direction of looking more like a bank, with the diverse revenue sources they enjoy. That includes generating fees from serving as a custodian of assets and facilitating lending and consumer payments. “We’re just doing it in our own crypto way,” Choi says. quora Coinbase’s nearly 3.5 million staking rewards program accounts nationwide are not insured by the Federal Deposit Insurance Corporation (FDIC) or Securities Investor Protection Corporation (SIPC). There is no protection from loss for any of these accounts, including the more than 600,000 accounts held by California investors. Investors are encouraged to contact DFPI to confirm the qualification status of a staking rewards program before investing their money.
canadian pharmacies online: canadian drug store viagra – reputable canadian online pharmacies
wegovy 14
https://canadadrugs.pro/# legitimate canadian internet pharmacies
wegovy online uk
canadian pharmacy ship to us: reliable canadian pharmacy – list of approved canadian pharmacies
http://medicinefromindia.store/# world pharmacy india
buy semaglutide for weight loss
mexican mail order pharmacies: purple pharmacy mexico price list – mexico pharmacy
http://edpill.cheap/# male erection pills
rybelsus medicine
mail order pharmacy india india pharmacy mail order indian pharmacy online
cheapest online pharmacy india: top online pharmacy india – Online medicine home delivery
rybelsus weight loss
wegovy 21 mg
https://edwithoutdoctorprescription.pro/# prescription drugs without doctor approval
rybelsus generic cost
buy prescription drugs from canada cheap: ed pills without doctor prescription – online prescription for ed meds
mexican online pharmacies prescription drugs buying prescription drugs in mexico online mexican rx online
buy rybelsus online no script
http://medicinefromindia.store/# india pharmacy mail order
ed meds online canada: prescription drugs canada buy online – canadian drug
reputable canadian pharmacy canadian family pharmacy pharmacy wholesalers canada
wegovy xr
http://medicinefromindia.store/# world pharmacy india
mail order pharmacy india: top 10 pharmacies in india – indian pharmacy
rybelsus diabetes medication
pills for erection new ed drugs best ed treatment pills
https://certifiedpharmacymexico.pro/# medication from mexico pharmacy
http://medicinefromindia.store/# mail order pharmacy india
wegovy tablets for weight loss cost
new treatments for ed best drug for ed cure ed
http://certifiedpharmacymexico.pro/# mexican pharmaceuticals online
Thanks for the complete information. You helped me.
pharmacy in canada: escrow pharmacy canada – canadian pharmacy no scripts
http://canadianinternationalpharmacy.pro/# canada pharmacy world
canadian pharmacy canadian pharmacy online canadian online pharmacy
canadian pharmacy meds: canadian pharmacy price checker – online canadian pharmacy reviews
generic ozempic for weight loss
semaglutide oral medication
generic rybelsus cost
semaglutide canada
https://medicinefromindia.store/# mail order pharmacy india
indian pharmacy: buy medicines online in india – cheapest online pharmacy india
generic semaglutide for weight loss
prescription drugs online without generic cialis without a doctor prescription viagra without a doctor prescription
buy rybelsus
buy wegovy online no script needed
wegovy generic cost
buy semaglutide from canada online
https://edpill.cheap/# pills for ed
semaglutide oral medication
buy ozempic
rybelsus 3 mg
prescription drugs without doctor approval ed pills without doctor prescription how to get prescription drugs without doctor
http://canadianinternationalpharmacy.pro/# canadian pharmacy king
rybelsus 3 mg tablet
buy ozempic oversees
buy semaglutide for weight loss
canadian pharmacy store: canada cloud pharmacy – canadapharmacyonline
semaglutide diabetes medication
purple pharmacy mexico price list reputable mexican pharmacies online buying prescription drugs in mexico online
http://edwithoutdoctorprescription.pro/# viagra without a prescription
buy ozempic online from india
buy ozempic cheap
http://canadianinternationalpharmacy.pro/# northern pharmacy canada
п»їbest mexican online pharmacies best online pharmacies in mexico medication from mexico pharmacy
wegovy australia
ozempic tab 14mg
buy ozempic for weight loss
semaglutide canada pharmacy prices
http://certifiedpharmacymexico.pro/# mexican pharmaceuticals online
canada drugs online reviews trustworthy canadian pharmacy canadian discount pharmacy
wegovy medicine
wegovy canada pharmacy prices
https://edwithoutdoctorprescription.pro/# viagra without a doctor prescription walmart
buying from online mexican pharmacy: best online pharmacies in mexico – buying from online mexican pharmacy
semaglutide online cheap
wegovy uk
rybelsus for diabetes
ozempic tab 14mg
india pharmacy mail order reputable indian online pharmacy india online pharmacy
cheap semaglutide
http://edwithoutdoctorprescription.pro/# buy prescription drugs
rybelsus oral medication
buy wegovy canada
reputable indian online pharmacy top online pharmacy india india pharmacy
semaglutide price
http://edpill.cheap/# top ed pills
http://edwithoutdoctorprescription.pro/# buy prescription drugs without doctor
ed pills that work ed pills that work ed drugs list
non prescription ed drugs: ed pills without doctor prescription – real viagra without a doctor prescription
buy ozempic
wegovy uk
rybelsus where to buy
https://edwithoutdoctorprescription.pro/# meds online without doctor prescription
http://medicinefromindia.store/# top online pharmacy india
generic ozempic cost
buy semaglutide pill form for adults
wegovy 14mg tablets
Online medicine home delivery indian pharmacy online indian pharmacy paypal
wegovy retail price
semaglutide
wegovy semaglutide tablets
https://edpill.cheap/# natural ed remedies
reputable indian online pharmacy online pharmacy india reputable indian online pharmacy
http://certifiedpharmacymexico.pro/# best mexican online pharmacies
semaglutide pill form
semaglutide ozempic
levitra without a doctor prescription: cialis without a doctor prescription canada – prescription drugs online without doctor
best online pharmacies in mexico mexico pharmacies prescription drugs mexican rx online
https://canadianinternationalpharmacy.pro/# online canadian pharmacy reviews
order semaglutide online
buy rybelsus in canada
best india pharmacy india online pharmacy top 10 online pharmacy in india
buying from online mexican pharmacy mexican pharmaceuticals online mexico pharmacies prescription drugs
buy ozempic canada
rybelsus best price
buying from online mexican pharmacy п»їbest mexican online pharmacies buying prescription drugs in mexico online
https://mexicanph.com/# mexico drug stores pharmacies
п»їbest mexican online pharmacies
semaglutide diabetes
buying from online mexican pharmacy mexican pharmaceuticals online mexican drugstore online
where can i buy ozempic
semaglutide for sale
purple pharmacy mexico price list medicine in mexico pharmacies mexican pharmaceuticals online
ozempic injections
mexico drug stores pharmacies buying prescription drugs in mexico online buying from online mexican pharmacy
buy semaglutide
buying prescription drugs in mexico mexican border pharmacies shipping to usa mexican online pharmacies prescription drugs
mexico drug stores pharmacies medication from mexico pharmacy mexican border pharmacies shipping to usa
buy semaglutide
buy rybelsus
mexico drug stores pharmacies medication from mexico pharmacy medicine in mexico pharmacies
purchase rybelsus
https://mexicanph.shop/# buying from online mexican pharmacy
mexico pharmacies prescription drugs
pharmacies in mexico that ship to usa mexican pharmaceuticals online mexico pharmacies prescription drugs
semaglutide 3 mg
mexican online pharmacies prescription drugs mexico pharmacies prescription drugs mexican drugstore online
mexican pharmaceuticals online mexican drugstore online mexican pharmacy
buy wegovy online no script needed
wegovy medication
mexican pharmaceuticals online mexican border pharmacies shipping to usa mexico pharmacy
mexico pharmacy pharmacies in mexico that ship to usa mexico drug stores pharmacies
wegovy xr
semaglutide buy uk
wegovy retail price
purple pharmacy mexico price list п»їbest mexican online pharmacies buying prescription drugs in mexico
https://mexicanph.shop/# medicine in mexico pharmacies
pharmacies in mexico that ship to usa
semaglutide medicine
mexican mail order pharmacies mexican rx online mexico pharmacies prescription drugs
generic semaglutide
mexico pharmacies prescription drugs medication from mexico pharmacy mexican mail order pharmacies
semaglutide injections
semaglutide canada
best online pharmacies in mexico mexican online pharmacies prescription drugs mexican pharmacy
rybelsus weight loss
ozempic tablets cost
buy ozempic online pharmacy
mexico drug stores pharmacies pharmacies in mexico that ship to usa buying from online mexican pharmacy
https://mexicanph.com/# reputable mexican pharmacies online
pharmacies in mexico that ship to usa
medication from mexico pharmacy medicine in mexico pharmacies mexico drug stores pharmacies
rybelsus semaglutide tablets 3mg
semaglutide price
wegovy for diabetes
mexico pharmacies prescription drugs п»їbest mexican online pharmacies mexico drug stores pharmacies
wegovy sale
mexican online pharmacies prescription drugs mexican mail order pharmacies mexican pharmaceuticals online
rybelsus drug
mexican online pharmacies prescription drugs mexico drug stores pharmacies mexico drug stores pharmacies
rybelsus online pharmacy
wegovy lose weight
mexico drug stores pharmacies mexico pharmacies prescription drugs mexican pharmacy
purchase rybelsus
http://mexicanph.com/# mexican border pharmacies shipping to usa
best online pharmacies in mexico
semaglutide buy online
purple pharmacy mexico price list purple pharmacy mexico price list medication from mexico pharmacy
wegovy tablets cost
purple pharmacy mexico price list medicine in mexico pharmacies medication from mexico pharmacy
mexican pharmacy purple pharmacy mexico price list mexican rx online
mexico drug stores pharmacies mexican online pharmacies prescription drugs mexican pharmacy
order ozempic
mexican pharmaceuticals online purple pharmacy mexico price list mexican pharmaceuticals online
п»їbest mexican online pharmacies mexican rx online mexico pharmacies prescription drugs
buy ozempic
buying from online mexican pharmacy mexican mail order pharmacies pharmacies in mexico that ship to usa
buy ozempic uk
rybelsus buy uk
purple pharmacy mexico price list buying prescription drugs in mexico mexico drug stores pharmacies
mexican online pharmacies prescription drugs buying from online mexican pharmacy mexico drug stores pharmacies
semaglutide retail price
purple pharmacy mexico price list mexican online pharmacies prescription drugs purple pharmacy mexico price list
mexico drug stores pharmacies mexican pharmaceuticals online buying prescription drugs in mexico
best online pharmacies in mexico buying from online mexican pharmacy mexican pharmacy
mexican drugstore online pharmacies in mexico that ship to usa mexican pharmacy
semaglutide uk
mexican rx online mexico pharmacy mexican drugstore online
medicine in mexico pharmacies mexican pharmacy mexican pharmaceuticals online
buy semaglutide
semaglutide mexico
buy ozempic from canada
mexican online pharmacies prescription drugs best online pharmacies in mexico mexican border pharmacies shipping to usa
mexican online pharmacies prescription drugs best mexican online pharmacies buying prescription drugs in mexico
wegovy pills
mexico pharmacies prescription drugs mexican rx online best online pharmacies in mexico
mexican mail order pharmacies mexican mail order pharmacies buying from online mexican pharmacy
mexican drugstore online mexican pharmaceuticals online pharmacies in mexico that ship to usa
http://mexicanph.com/# best online pharmacies in mexico
pharmacies in mexico that ship to usa
п»їbest mexican online pharmacies mexican border pharmacies shipping to usa reputable mexican pharmacies online
ozempic semaglutide tablets 3mg
wegovy 3 mg tablet
mexican pharmacy buying prescription drugs in mexico online mexico drug stores pharmacies
mexican rx online purple pharmacy mexico price list purple pharmacy mexico price list
wegovy diabetes medication
reputable mexican pharmacies online purple pharmacy mexico price list mexican mail order pharmacies
reputable mexican pharmacies online reputable mexican pharmacies online medicine in mexico pharmacies
semaglutide for sale
rybelsus buy uk
rybelsus xl
reputable mexican pharmacies online buying from online mexican pharmacy mexican pharmaceuticals online
mexican rx online reputable mexican pharmacies online buying from online mexican pharmacy
rybelsus 3 mg
wegovy 3 mg
order semaglutide
wegovy 14
п»їbest mexican online pharmacies mexican mail order pharmacies mexico drug stores pharmacies
wegovy without prescription
buying from online mexican pharmacy best online pharmacies in mexico purple pharmacy mexico price list
buy rybelsus from canada
ozempic semaglutide
mexico pharmacies prescription drugs buying from online mexican pharmacy reputable mexican pharmacies online
semaglutide generic cost
https://mexicanph.com/# medicine in mexico pharmacies
mexican drugstore online
purple pharmacy mexico price list mexico pharmacies prescription drugs buying prescription drugs in mexico
mexican rx online best mexican online pharmacies reputable mexican pharmacies online
semaglutide tablets cost
rybelsus tablets for weight loss
best online pharmacies in mexico medication from mexico pharmacy buying prescription drugs in mexico online
semaglutide diabetes
buying prescription drugs in mexico mexico pharmacy medication from mexico pharmacy
mexico pharmacies prescription drugs mexico drug stores pharmacies reputable mexican pharmacies online
buying prescription drugs in mexico medicine in mexico pharmacies reputable mexican pharmacies online
rybelsus online cheap
wegovy best price
where can i buy ozempic
medicine in mexico pharmacies mexican mail order pharmacies mexican border pharmacies shipping to usa
semaglutide diabetes medication
mexican rx online mexican drugstore online pharmacies in mexico that ship to usa
buying from online mexican pharmacy buying from online mexican pharmacy buying prescription drugs in mexico online
rybelsus pills
mexico pharmacy mexican rx online pharmacies in mexico that ship to usa
wegovy buy online
https://mexicanph.shop/# mexican rx online
п»їbest mexican online pharmacies
brand semaglutide
wegovy semaglutide tablets cost
medication from mexico pharmacy mexican drugstore online mexican rx online
buy ozempic from canada
order semaglutide online
best online pharmacies in mexico pharmacies in mexico that ship to usa mexican drugstore online
mexican pharmacy mexican pharmacy buying from online mexican pharmacy
https://lisinopril.top/# lisinopril 240
rybelsus rx
prednisone coupon: generic prednisone online – prednisone over the counter australia
amoxicillin 500 mg for sale rexall pharmacy amoxicillin 500mg amoxicillin online without prescription
http://lisinopril.top/# lisinopril 5mg tab
https://buyprednisone.store/# prednisone 5mg price
buy semaglutide in mexico
cheap generic prednisone: prednisone 50 mg price – over the counter prednisone pills
https://furosemide.guru/# furosemide 40 mg
wegovy order
rybelsus tablets buy
buy semaglutide online no script needed
furosemide 100 mg Over The Counter Lasix lasix 40 mg
buy prednisone 1 mg mexico: prednisone brand name us – prednisone 50 mg price
https://amoxil.cheap/# medicine amoxicillin 500
generic ozempic cost
http://amoxil.cheap/# amoxicillin 500mg buy online uk
lisinopril tabs 4mg: lisinopril 5 mg tablet price in india – generic zestoretic
http://furosemide.guru/# lasix 100 mg
amoxicillin 500 mg brand name amoxicillin 250 mg price in india amoxicillin 500 mg without prescription
http://furosemide.guru/# lasix medication
rybelsus best price
semaglutide 14mg tablets
rybelsus lose weight
rybelsus uk
generic lisinopril 40 mg: lisinopril no prescription – lisinopril drug
rybelsus online pharmacy
https://stromectol.fun/# cost of ivermectin 3mg tablets
lasix uses lasix tablet lasix furosemide
lisinopril 10mg price in india: best generic lisinopril – price of lisinopril 30 mg
http://lisinopril.top/# lisinopril 30
wegovy pill
ozempic injections
wegovy semaglutide
semaglutide tablets buy
buy ozempic online cheap
semaglutide canada pharmacy prices
amoxicillin 500mg over the counter: how to get amoxicillin – amoxicillin 500 mg tablets
http://buyprednisone.store/# prednisone 20 mg generic
furosemide 100 mg Over The Counter Lasix lasix dosage
http://lisinopril.top/# buy lisinopril online india
semaglutide tab 7mg
wegovy lose weight
http://buyprednisone.store/# prednisone 40 mg price
lasix furosemide 40 mg: Buy Lasix – furosemide 40 mg
semaglutide tablets buy
order ozempic online
lasix for sale lasix furosemide lasix furosemide 40 mg
http://lisinopril.top/# lisinopril 10 mg no prescription
wegovy 7 mg
rybelsus for diabetes
buy amoxicillin 500mg usa: amoxicillin 500 mg tablets – order amoxicillin uk
http://stromectol.fun/# ivermectin 6mg
wegovy online prescription
buy ozempic canada
amoxicillin 500mg price canada: can you purchase amoxicillin online – cost of amoxicillin
rybelsus pill form
buy ivermectin cream for humans ivermectin over the counter stromectol australia
https://amoxil.cheap/# amoxicillin pharmacy price
http://buyprednisone.store/# purchase prednisone from india
wegovy canada pharmacy prices
buy ozempic
lisinopril 80 mg daily: zestril discount – zestril 5 mg india
https://lisinopril.top/# buy lisinopril 20 mg online usa
rybelsus online order
semaglutide price
generic amoxicillin over the counter amoxicillin cost australia order amoxicillin online
https://buyprednisone.store/# prednisone 5 mg tablet
buy lasix online: Over The Counter Lasix – lasix generic
rybelsus semaglutide tablets 3mg
wegovy tablets for weight loss cost
rybelsus price
semaglutide from canada
generic ozempic
https://amoxil.cheap/# amoxicillin 500mg buy online uk
wegovy sale
rybelsus for diabetes
zestril 20 mg cost: lisinopril 5 mg brand name – buy lisinopril without prescription
semaglutide 14mg
semaglutide oral medication
rybelsus buy from canada
semaglutide tab 3mg
buy wegovy online from india
lisinopril cheap brand zestril over the counter lisinopril 20 mg tablets
buy rybelsus in canada
wegovy tablets for weight loss cost
http://lisinopril.top/# lipinpril
rybelsus
generic semaglutide for weight loss
lasix generic: furosemide 100mg – lasix furosemide 40 mg
https://amoxil.cheap/# generic for amoxicillin
http://lisinopril.top/# best price for lisinopril
wegovy
http://stromectol.fun/# can you buy stromectol over the counter
amoxicillin without prescription: generic amoxicillin 500mg – buy amoxicillin 500mg canada
purchase rybelsus
ivermectin tablet price ivermectin 12 mg ivermectin cost uk
semaglutide tablets cost
buy ozempic
https://stromectol.fun/# ivermectin lice oral
semaglutide pills
lasix generic name: Buy Lasix – lasix furosemide
semaglutide online order
http://buyprednisone.store/# 50 mg prednisone from canada
lisinopril 420 1g buy zestoretic online order lisinopril from mexico
buy wegovy from canada
buy rybelsus
rybelsus semaglutide tablets 3mg
lasix dosage: buy lasix online – lasix generic
buy rybelsus in canada
https://furosemide.guru/# lasix 100 mg tablet
http://amoxil.cheap/# medicine amoxicillin 500
buy semaglutide cheap
https://stromectol.fun/# ivermectin coronavirus
buy amoxicillin 500mg usa buy amoxicillin over the counter uk amoxicillin for sale online
ivermectin 1mg: ivermectin 8000 mcg – ivermectin buy australia
rybelsus mexico
ozempic for weight loss
https://stromectol.fun/# ivermectin 90 mg
lisinopril for sale: prinivil generic – buy lisinopril online no prescription
buy ozempic from canada online
semaglutide generic cost
http://furosemide.guru/# lasix
lisinopril 5 mg buy online lisinopril 20 mg lisinopril 20 mg india
semaglutide online prescription
http://amoxil.cheap/# amoxicillin generic
furosemide: lasix furosemide 40 mg – lasix generic
https://lisinopril.top/# lisinopril 20 mg price without prescription
https://lisinopril.top/# lisinopril 10mg online
can you buy prednisone over the counter: order prednisone on line – prednisone tabs 20 mg
ivermectin over the counter uk ivermectin 6 oral ivermectin cost
http://lisinopril.top/# lipinpril
buy rybelsus
prednisone 40 mg rx: online prednisone – prednisone 30 mg coupon
http://amoxil.cheap/# where can i get amoxicillin 500 mg
semaglutide diabetes medication
wegovy over the counter
semaglutide pill form
buy wegovy in mexico
semaglutide 7mg
generic amoxil 500 mg amoxicillin price without insurance amoxicillin 500 mg cost
http://furosemide.guru/# lasix 40mg
semaglutide sale
lasix 100 mg tablet: Buy Furosemide – lasix 20 mg
purchase rybelsus
purchase ozempic
http://furosemide.guru/# lasix 40mg
buy ozempic online pharmacy
order rybelsus online
wegovy canada pharmacy
buy wegovy
semaglutide where to buy
semaglutide mexico
semaglutide online order
semaglutide 3 mg tablet
wegovy oral medication
buy semaglutide in mexico
cheap semaglutide
https://indianph.com/# best online pharmacy india
top 10 online pharmacy in india
reputable indian pharmacies india pharmacy mail order online pharmacy india
wegovy 3 mg tablet
wegovy 14mg
http://indianph.com/# indian pharmacy paypal
http://indianph.xyz/# indian pharmacy
best online pharmacy india
https://indianph.com/# indian pharmacy online
best india pharmacy
http://indianph.com/# reputable indian pharmacies
Online medicine order
wegovy 14
semaglutide tab 14mg
semaglutide online uk
https://indianph.xyz/# cheapest online pharmacy india
buy medicines online in india
http://indianph.com/# reputable indian pharmacies
reputable indian pharmacies
rybelsus online cheap
india online pharmacy online shopping pharmacy india india pharmacy
http://indianph.xyz/# top 10 online pharmacy in india
https://indianph.xyz/# buy medicines online in india
buy prescription drugs from india
wegovy injection
http://indianph.xyz/# india pharmacy mail order
indian pharmacy
semaglutide over the counter
rybelsus pills
indianpharmacy com indian pharmacies safe mail order pharmacy india
http://indianph.com/# world pharmacy india
Online medicine home delivery
rybelsus 7mg
wegovy buy from canada
rybelsus medicine
where to buy ozempic online
rybelsus online prescription
buy semaglutide online
semaglutide lose weight
rybelsus oral medication
http://cytotec24.com/# buy cytotec online
buy doxycycline 100mg: doxycycline hyc 100mg – vibramycin 100 mg
semaglutide 7mg
diflucan singapore where to get diflucan over the counter diflucan 150 australia
http://nolvadex.guru/# alternative to tamoxifen
http://cipro.guru/# cipro
rybelsus xl
ciprofloxacin mail online: purchase cipro – ciprofloxacin mail online
http://diflucan.pro/# diflucan canada
buy semaglutide canada
how to buy diflucan online diflucan canada online buy diflucan online
http://cipro.guru/# cipro for sale
cost of tamoxifen: buy nolvadex online – where to buy nolvadex
wegovy weight loss
http://cipro.guru/# buy ciprofloxacin
rybelsus
cipro ciprofloxacin: ciprofloxacin mail online – cipro online no prescription in the usa
buy nolvadex online alternative to tamoxifen liquid tamoxifen
https://cytotec24.shop/# cytotec online
http://cipro.guru/# ciprofloxacin 500 mg tablet price
https://cipro.guru/# cipro online no prescription in the usa
rybelsus tablets 7 mg
semaglutide weight loss
nolvadex 10mg how to lose weight on tamoxifen tamoxifen dosage
rybelsus diabetes medication
https://cipro.guru/# purchase cipro
diflucan rx price: diflucan tablets price – diflucan pills online
buy semaglutide canada
http://cytotec24.shop/# buy cytotec online fast delivery
wegovy from canada
https://doxycycline.auction/# doxycycline medication
rybelsus tab 7mg
http://cytotec24.shop/# buy cytotec online
ozempic tab 14mg
https://cytotec24.shop/# purchase cytotec
semaglutide prescription
rybelsus rx
tamoxifen reviews nolvadex generic tamoxifen mechanism of action
http://cytotec24.shop/# buy cytotec online fast delivery
wegovy
purchase rybelsus
https://diflucan.pro/# diflucan 150 mg caps
http://cytotec24.com/# п»їcytotec pills online
buy rybelsus canada
doxycycline hyclate doxycycline order doxycycline 100mg without prescription
http://doxycycline.auction/# cheap doxycycline online
http://nolvadex.guru/# how to lose weight on tamoxifen
semaglutide tablets 7 mg
semaglutide 14mg tablets
generic semaglutide
semaglutide ozempic
http://lanarhoades.fun/# lana rhoades izle
wegovy tab 3mg
Angela White izle: Angela White filmleri – Angela Beyaz modeli
semaglutide 3 mg tablet
http://lanarhoades.fun/# lana rhoades modeli
rybelsus prescription
https://evaelfie.pro/# eva elfie izle
https://angelawhite.pro/# Angela Beyaz modeli
buy wegovy
semaglutide online pharmacy
Angela White: Abella Danger – Abella Danger
where to buy semaglutide online
https://abelladanger.online/# abella danger video
https://abelladanger.online/# Abella Danger
wegovy oral medication
eva elfie filmleri: eva elfie video – eva elfie filmleri
wegovy xr
http://evaelfie.pro/# eva elfie filmleri
https://angelawhite.pro/# Angela White filmleri
http://sweetiefox.online/# Sweetie Fox izle
generic wegovy for weight loss
semaglutide rybelsus
https://angelawhite.pro/# ?????? ????
generic ozempic cost
semaglutide tab 3mg
Angela White: Angela Beyaz modeli – Angela White
https://angelawhite.pro/# ?????? ????
https://abelladanger.online/# abella danger filmleri
Sweetie Fox: sweeti fox – sweety fox
semaglutide price
semaglutide buy online
http://lanarhoades.fun/# lana rhodes
http://angelawhite.pro/# Angela White video
semaglutide online pharmacy
https://sweetiefox.online/# sweety fox
swetie fox: sweety fox – Sweetie Fox modeli
https://abelladanger.online/# Abella Danger
rybelsus best price
http://sweetiefox.online/# Sweetie Fox modeli
bactrim dosing for uti uptodate
https://lanarhoades.fun/# lana rhoades izle
wegovy canada pharmacy
eva elfie izle: eva elfie – eva elfie
https://angelawhite.pro/# Angela White
http://abelladanger.online/# abella danger video
https://lanarhoades.fun/# lana rhoades filmleri
http://abelladanger.online/# abella danger video
eva elfie modeli: eva elfie izle – eva elfie filmleri
rybelsus 3mg
buy ozempic
http://sweetiefox.online/# Sweetie Fox modeli
semaglutide prescription
lana rhoades izle: lana rhoades izle – lana rhoades izle
https://evaelfie.pro/# eva elfie video
ozempic tab 14mg
http://angelawhite.pro/# Angela Beyaz modeli
wegovy 3 mg tablet
semaglutide canada
Angela White: Angela White – ?????? ????
http://lanarhoades.fun/# lana rhodes
wegovy canada
https://sweetiefox.online/# Sweetie Fox izle
http://evaelfie.pro/# eva elfie filmleri
order rybelsus
https://lanarhoades.fun/# lana rhodes
buy semaglutide pill form for adults
semaglutide retail price
http://abelladanger.online/# abella danger izle
synthroid 88 mcg coupon
https://abelladanger.online/# abella danger filmleri
Angela White video: abella danger izle – abella danger video
online pharmacy drop shipping
valtrex 1g
http://lanarhoades.fun/# lana rhoades modeli
Angela White: Angela Beyaz modeli – Angela White video
http://abelladanger.online/# Abella Danger
https://sweetiefox.online/# Sweetie Fox filmleri
lisinopril 5 mg
purchase prednisone canada
http://evaelfie.pro/# eva elfie
Angela White izle: Angela Beyaz modeli – Angela White izle
side effects of bactrim ds 800 160
canadian pharmacies compare
lisinopril 250mg
prinivil 20mg tabs
metformin 500 mg tablet
zithromax buy
sweetie fox: sweetie fox new – sweetie fox cosplay
http://miamalkova.life/# mia malkova latest
asien dating online: https://evaelfie.site/# eva elfie full video
happy family pharmacy uk
http://lanarhoades.pro/# lana rhoades hot
zestril medication
zestoretic 20 price
lana rhoades solo: lana rhoades full video – lana rhoades solo
lana rhoades videos: lana rhoades unleashed – lana rhoades full video
http://lanarhoades.pro/# lana rhoades hot
lisinopril 25 mg
mia malkova movie: mia malkova new video – mia malkova photos
india pharmacy online tadalafil
100% free dating sites: http://lanarhoades.pro/# lana rhoades solo
canadian drugstore cialis
mia malkova: mia malkova hd – mia malkova girl
http://miamalkova.life/# mia malkova videos
tadalafil online 5mg
eva elfie photo: eva elfie hd – eva elfie hot
pharmacy online track order
best online pharmacy no prescription
how much is valtrex in canada
http://evaelfie.site/# eva elfie videos
sweetie fox new: sweetie fox full video – fox sweetie
buy synthroid online from canada
canadian valtrex otc
lisinopril 10mg online
dating wites: http://miamalkova.life/# mia malkova
tadalafil in india online
eva elfie full video: eva elfie full videos – eva elfie full videos
lisinopril 80mg
safe reliable canadian pharmacy
synthroid 0.075 mcg
synthroid in india
ph sweetie fox: sweetie fox video – sweetie fox new
synthroid 088 mg
https://miamalkova.life/# mia malkova movie
can i buy lisinopril over the counter in mexico
lisinopril 3973
generic valtrex canada
fox sweetie: sweetie fox full video – sweetie fox new
generic tadalafil for sale
cost of lisinopril 5 mg
generic tadalafil usa pharmacy
https://sweetiefox.pro/# sweetie fox video
date match site: http://miamalkova.life/# mia malkova movie
buy synthroid 75 mcg
eva elfie full video: eva elfie new videos – eva elfie
buy generic valtrex cheap
2.5 mg daily tadalafil
how to get tadalafil online
medstore online pharmacy
fox sweetie: sweetie fox video – sweetie fox full
order prednisone 10 mg tablet
tadalafil cheapest price
order synthroid online
happy family store viagra
canadian pharmacy generic viagra
http://sweetiefox.pro/# sweetie fox video
azithromycin 250 price india
canadadrugpharmacy com
tadalafil generic cialis
generic metformin price
pharmacy website india
mia malkova full video: mia malkova hd – mia malkova latest
brand synthroid coupon
dating app: http://sweetiefox.pro/# sweetie fox full video
brazilian pharmacy online
lisinopril 10 mg tablet price
https://sweetiefox.pro/# sweetie fox
lisinopril tabs 4mg
mia malkova girl: mia malkova only fans – mia malkova only fans
mia malkova photos: mia malkova – mia malkova only fans
order lisinopril 10 mg
lisinopril pills 10 mg
purchase lisinopril
legit online pharmacy
over the counter valtrex
http://evaelfie.site/# eva elfie hd
eva elfie full videos: eva elfie hd – eva elfie videos
valtrex cream over the counter
buy cheap synthroid
free dating site for usa: https://sweetiefox.pro/# sweetie fox new
synthroid tablets
mia malkova girl: mia malkova hd – mia malkova hd
where can i get valtrex over the counter
http://lanarhoades.pro/# lana rhoades videos
buy metformin 500mg tablets
metformin without script
metformin best brand
lisinopril 20 mg brand name
mia malkova photos: mia malkova only fans – mia malkova movie
mia malkova full video: mia malkova photos – mia malkova latest
buy tadalafil mexico online
buy valtrex india
http://miamalkova.life/# mia malkova videos
austria pharmacy online
generic tadalafil 20mg canada
canadian pharmacy cialis
how much is metformin 1000 mg
tadalafil generic 10mg
prinzide zestoretic
order lisinopril online from canada
buy azithromycin in usa
valtrex uk price
pin up aviator: pin up aviator – aviator pin up
aviator sportybet ghana: aviator sportybet ghana – aviator betting game
http://pinupcassino.pro/# pin up bet
zithromax 500 mg
aviator bahis: aviator sinyal hilesi – aviator oyna slot
metformin 750 mg price
http://aviatormalawi.online/# aviator malawi
brand name drug prednisone
can you buy metformin without prescription
aviator game: aviator game bet – aviator bet
azithromycin for sale cheap
synthroid 115 mcg
best online thai pharmacy
http://aviatormalawi.online/# aviator betting game
aviator bet malawi: aviator game – aviator betting game
synthroid 25 mg price
buy generic prednisone online
canadian pharmacy coupon
cost of lisinopril 40 mg
buy cheap metformin online
site de apostas: aviator jogo de aposta – ganhar dinheiro jogando
https://aviatormalawi.online/# aviator game
prednisone 5093
synthroid 50 mcg price in india
aviator jogar: pin up aviator – aviator bet
best online foreign pharmacies
valtrex 500mg
cassino pin up: pin-up casino login – cassino pin up
where to buy prednisone in canada
aviator: como jogar aviator em moçambique – aviator mz
order lisinopril without a prescription
tadalafil for sale online
synthroid average cost
aviator: aviator hilesi – pin up aviator
lisinopril 20 mg price in india
metformin 500 mg tablet
cialis tadalafil 20mg
zestril 5mg price in india
aviator game bet: aviator sportybet ghana – aviator login
pharmacy websites
metformin buy canada
aviator hilesi: pin up aviator – aviator oyunu
aviator jogo de aposta: melhor jogo de aposta para ganhar dinheiro – deposito minimo 1 real
aviator bet malawi login: aviator game online – aviator betting game
synthroid 1mg
como jogar aviator: como jogar aviator – jogar aviator
which online pharmacy is the best
aviator jogo: jogar aviator online – aviator betano
buy metformin from canada
how much is tadalafil 5mg
aviator: aviator bet – aviator game online
best rx pharmacy online
zithromax 1000 mg pills: buy zithromax canada – buy cheap zithromax online
pin up aviator: pin up casino – cassino pin up
prednisone drug costs
synthroid for sale without prescription
zithromax antibiotic – https://azithromycin.pro/pfizer-zithromax.html zithromax drug
best online foreign pharmacies
aviator betting game: aviator game – aviator
aviator online: como jogar aviator – aviator
best online pet pharmacy
tadalafil 7 mg capsule
como jogar aviator em moçambique: como jogar aviator – como jogar aviator em moçambique
where can i buy zithromax medicine – https://azithromycin.pro/zithromax-side-effects.html zithromax coupon
synthroid 0.5 mg
where to buy prednisone 5443 without prescription
reputable online pharmacy uk
azithromycin 250 mg 1mg
azithromycin price in usa
canadian online pharmacy reviews Canada pharmacy online online pharmacy canada canadianpharm.store
online pharmacy denmark
п»їbest mexican online pharmacies: order online from a Mexican pharmacy – mexican mail order pharmacies mexicanpharm.shop
pharmacy canadian: canadian pharmacy – canadian pharmacy india canadianpharm.store
metformin 1
drug synthroid
buy tadalafil online uk
pharmacy website india indian pharmacy indianpharmacy com indianpharm.store
cialis cheapest price canada
online pharmacy india: Top online pharmacy in India – reputable indian pharmacies indianpharm.store
synthroid 112 mcg tab
super saver pharmacy
online pharmacy
https://indianpharm24.shop/# top online pharmacy india indianpharm.store
https://indianpharm24.shop/# п»їlegitimate online pharmacies india indianpharm.store
synthroid pill
indian pharmacy online: Best Indian pharmacy – reputable indian online pharmacy indianpharm.store
buy azithromycin 1000mg
cost of lisinopril in mexico
п»їlegitimate online pharmacies india Top online pharmacy in India india online pharmacy indianpharm.store
cheapest generic cialis 20mg
http://indianpharm24.shop/# indian pharmacies safe indianpharm.store
order valtrex online usa
synthroid purchase online
generic synthroid pill
https://canadianpharmlk.shop/# best canadian pharmacy to order from canadianpharm.store
where can i get tadalafil
http://canadianpharmlk.shop/# canada pharmacy canadianpharm.store
online shopping pharmacy india: cheapest online pharmacy – best india pharmacy indianpharm.store
cheap lisinopril
http://indianpharm24.com/# п»їlegitimate online pharmacies india indianpharm.store
online pharmacy store
https://indianpharm24.shop/# indian pharmacy indianpharm.store
buying tadalafil from india
canadian pharmacy ratings: Best Canadian online pharmacy – canadian medications canadianpharm.store
Online medicine order: india online pharmacy – cheapest online pharmacy india indianpharm.store
https://mexicanpharm24.shop/# pharmacies in mexico that ship to usa mexicanpharm.shop
rx lisinopril
https://indianpharm24.shop/# india online pharmacy indianpharm.store
price for cialis in canada
Online medicine order online pharmacy usa world pharmacy india indianpharm.store
http://mexicanpharm24.shop/# buying prescription drugs in mexico online mexicanpharm.shop
top 10 online pharmacy in india: Top online pharmacy in India – indian pharmacy online indianpharm.store
metformin 15 mg
zestril 25 mg
lisinopril 40 mg discount
https://canadianpharmlk.com/# safe canadian pharmacy canadianpharm.store
https://indianpharm24.shop/# world pharmacy india indianpharm.store
which online pharmacy is the best
http://mexicanpharm24.shop/# medicine in mexico pharmacies mexicanpharm.shop
mexican online pharmacies prescription drugs: Mexico pharmacy online – mexico drug stores pharmacies mexicanpharm.shop
http://canadianpharmlk.com/# canadian pharmacy 24h com safe canadianpharm.store
buying prescription drugs in mexico online: Mexico pharmacy price list – medication from mexico pharmacy mexicanpharm.shop
synthroid 112.5
https://indianpharm24.com/# Online medicine home delivery indianpharm.store
lisinopril 10 mg best price
synthroid 150
tadalafil cost in india
https://mexicanpharm24.shop/# buying prescription drugs in mexico mexicanpharm.shop
india pharmacy mail order Best Indian pharmacy top 10 pharmacies in india indianpharm.store
http://mexicanpharm24.com/# mexico pharmacies prescription drugs mexicanpharm.shop
online shopping pharmacy india: Pharmacies in India that ship to USA – indian pharmacy paypal indianpharm.store
zestril price in india
rx pharmacy coupons
prednisone online with no prescription
where to get amoxicillin over the counter: ampicillin vs amoxicillin – buy cheap amoxicillin
lisinopril 10mg
http://prednisonest.pro/# prednisone 2.5 mg price
prednisone 2 mg daily: can you drink alcohol with prednisone – prednisone 100 mg
buy amoxicillin online mexico amoxicillin without a doctors prescription amoxicillin online no prescription
order cheap clomid without a prescription: where to buy cheap clomid – where can i buy generic clomid pills
generic prednisone otc: prednisone 10mg canada – purchase prednisone
synthroid com
buy azithromycin nz
http://prednisonest.pro/# canada buy prednisone online
amoxicillin without rx: generic amoxicillin over the counter – amoxicillin without rx
prednisone 2.5 mg tab: prednisone 10mg price in india – prednisone 475
how to buy prednisone: prednisone with alcohol – prednisone 10mg for sale
metformin 13
https://amoxilst.pro/# amoxicillin generic
online prednisone: prednisone drug class – prednisone tablets 2.5 mg
prednisone tablets average cost of prednisone prednisone oral
where can i buy prednisone: 30mg prednisone – medicine prednisone 10mg
amoxicillin 500 tablet: amoxicillin allergy – 875 mg amoxicillin cost
15 mg prednisone daily
https://amoxilst.pro/# amoxicillin 500 mg online
lisinopril 50 mg tablet
how can i get cheap clomid no prescription: clomid multiples – can i purchase generic clomid
metformin without a prescription drug
generic prednisone cost: prednisone sale – buy prednisone online fast shipping
http://prednisonest.pro/# average cost of prednisone
prednisone 10mg no prescription
buy 10 mg prednisone: prednisone taper schedule – prednisone 5mg cost
metformin 850 mg tablet
prednisone medication
where to buy amoxicillin pharmacy: buy cheap amoxicillin – amoxicillin 500 mg capsule
how to get cheap clomid pills: clomid vs testosterone – can you get cheap clomid without prescription
prednisone 100 mg prednisone 50 mg coupon prednisone 300mg
cheap clomid: can you buy clomid now – buy clomid no prescription
http://amoxilst.pro/# buy amoxicillin online with paypal
can you get clomid now: how can i get generic clomid without prescription – can you buy cheap clomid pill
6mg tadalafil
reputable online pharmacy
best india pharmacy
online cialis 5mg
canadian pharmacy no prescription needed: medicine with no prescription – canadian prescription drugstore review
prednisone buy online
http://onlinepharmacy.cheap/# canadian pharmacy no prescription needed
pharmacy with no prescription: buying prescription medicine online – mexico prescription drugs online
mail order prescription drugs from canada canada online pharmacy online pharmacy no prescription
buying prescription drugs online canada: prescription from canada – canada online prescription
international pharmacy no prescription: discount pharmacy – canadian pharmacy discount code
lisinopril 10mg price in india
cheapest pharmacy for prescriptions
tadalafil 75 mg
canadian pharmacy meds
synthroid buy
ed pills: discount ed pills – cheap ed medicine
https://pharmnoprescription.pro/# best non prescription online pharmacy
cheap ed medicine: ed medications online – get ed prescription online
online pharmacy viagra
cost of ed meds: ed treatments online – erection pills online
cheap cialis 100mg
lisinopril 30mg coupon
lisinopril tablets india
buy synthroid cheap
valtrex pills price
synthroid for sale online
https://pharmnoprescription.pro/# no prescription pharmacy
synthroid 25 mcg tabs
overseas pharmacy no prescription: canada online pharmacy – canadian pharmacy without prescription
ed meds on line: buying erectile dysfunction pills online – ed pills for sale
best canadian pharmacy no prescription discount pharmacy canada drugs coupon code
canadian pharmacy no prescription needed: Best online pharmacy – buying prescription drugs from canada
https://pharmnoprescription.pro/# prescription meds from canada
zestoretic drug
lisinopril in usa
prescription drugs from canada: best online pharmacy – online pharmacy discount code
cheap ed: ed online pharmacy – cheap ed treatment
buy synthroid online cheap
canada pharmacy no prescription: buy medication online no prescription – canada pharmacy online no prescription
http://onlinepharmacy.cheap/# canadian pharmacy no prescription needed
cheap cialis uk
lisinopril 10 mg canada cost
edmeds: cheap ed drugs – affordable ed medication
save on pharmacy
pharmacy without prescription: online pharmacy – no prescription needed pharmacy
cheap cialis online usa
taking bupropion and naltrexone instead of contrave
synthroid rx
drugstore com online pharmacy prescription drugs
http://canadianpharm.guru/# canadian pharmacy online
order prescription from canada: prescription meds from canada – canadian pharmacy online no prescription needed
reputable mexican pharmacies online mexican pharmaceuticals online mexico pharmacies prescription drugs
tadalafil 5 mg coupon
synthroid prescription uk
http://pharmacynoprescription.pro/# pharmacy no prescription required
cialis price in india
metformin over the counter uk
pharmacy in canada: canada pharmacy online – legitimate canadian pharmacy online
tadalafil in mexico
https://mexicanpharm.online/# purple pharmacy mexico price list
best tadalafil tablets
lisinopril 40 mg purchase
reddit canadian pharmacy
http://pharmacynoprescription.pro/# cheap prescription medication online
prescription canada: online pharmacies without prescriptions – medication online without prescription
best price for lisinopril
canadian prescription drugstore review: meds online no prescription – online drugs no prescription
best online pharmacy no prescription
mexico drug stores pharmacies pharmacies in mexico that ship to usa mexican online pharmacies prescription drugs
https://pharmacynoprescription.pro/# meds no prescription
canadian online pharmacy: canadian compounding pharmacy – canadian pharmacies comparison
zestril 10 mg cost
500 mg valtrex daily
buy lisinopril in mexico
indian pharmacies safe: reputable indian online pharmacy – indian pharmacies safe
india online pharmacy: buy prescription drugs from india – india pharmacy mail order
prednisone 12 mg
valtrex without a prescription
synthroid 0.1 mcg
cost of synthroid 100mcg
canadian pharmacy 365: reputable canadian pharmacy – canadian pharmacies compare
lisinopril 12.5 tablet
https://pharmacynoprescription.pro/# best no prescription online pharmacies
pharmacy website
https://pharmacynoprescription.pro/# non prescription online pharmacy india
india pharmacy: Online medicine order – п»їlegitimate online pharmacies india
azithromycin 250 mg suppliers
77 canadian pharmacy: pharmacy rx world canada – safe canadian pharmacy
canadian pharmacy meds canadian pharmacy 24h com best canadian pharmacy to buy from
canada pharmacy 24h: canadian discount pharmacy – online pharmacy canada
https://canadianpharm.guru/# legitimate canadian mail order pharmacy
viagra online canadian pharmacy
valtrex generic in mexico
where can i buy cialis
cheap canadian pharmacy: cheap canadian pharmacy online – online canadian pharmacy review
1700 mg metformin
http://canadianpharm.guru/# canadian pharmacy online store
canadian pharmacy world coupon
no prescription medicine: online pharmacy without prescriptions – buy medication online with prescription
mexico pharmacies prescription drugs: mexican pharmacy – medicine in mexico pharmacies
http://pharmacynoprescription.pro/# buying prescription medicine online
valtrex price singapore
mexican mail order pharmacies: buying prescription drugs in mexico – buying prescription drugs in mexico
pharmacy wholesalers canada
lisinopril over the counter
canadian pharmacies that deliver to the us
https://indianpharm.shop/# Online medicine order
zestoretic 20 12.5
canadian prescriptions in usa: no prescription online pharmacy – canadian prescriptions in usa
trustworthy canadian pharmacy: canadapharmacyonline com – precription drugs from canada
tadalafil online us
pharmacy discount card
lisinopril brand name uk
lisinopril generic 10 mg
lisinopril 18 mg
https://pharmacynoprescription.pro/# pharmacy online no prescription
cialis without a rx
canadian pharmacies: prescription drugs canada buy online – legitimate canadian pharmacy
order prescription drugs online without doctor: how to get prescription drugs from canada – no prescription drugs online
no prescription needed pharmacy: online pharmacy without a prescription – buying prescription drugs from canada online
synthroid 0.0125 mcg
https://indianpharm.shop/# buy prescription drugs from india
https://pharmacynoprescription.pro/# buy prescription drugs online without
no prescription medicine: canada prescription online – meds online no prescription
synthroid levothyroxine
metformin purchase
metformin purchase
canadian pharmacy online reviews canadian online drugs online canadian pharmacy
http://pharmacynoprescription.pro/# buy drugs without prescription
online prescription canada: ordering prescription drugs from canada – canadian mail order prescriptions
mexican online pharmacies prescription drugs: mexican border pharmacies shipping to usa – pharmacies in mexico that ship to usa
happy family drugstore
lisinopril 5 mg india price
medstore online pharmacy
where to buy valtrex
canadian pharmacy uk delivery
canadian pharmacy online ship to usa: adderall canadian pharmacy – reliable canadian pharmacy
synthroid 200 mcg price
https://canadianpharm.guru/# my canadian pharmacy
valtrex medication
top 10 online pharmacy in india: reputable indian pharmacies – indian pharmacy
mexico drug stores pharmacies: mexico drug stores pharmacies – mexican rx online
canadian drugs online: canada pharmacy – best canadian online pharmacy
how much is valtrex 500mg
http://pharmacynoprescription.pro/# buy medication online without prescription
http://indianpharm.shop/# top 10 pharmacies in india
1 lisinopril
lisinopril 20 mg tablets
indianpharmacy com: top 10 pharmacies in india – indian pharmacies safe
top 10 pharmacies in india: online shopping pharmacy india – indianpharmacy com
https://indianpharm.shop/# indian pharmacy paypal
price for synthroid
indian pharmacy: online pharmacy india – best online pharmacy india
azithromycin purchase usa
cheap prednisone 20 mg
order valtrex canada
metformin for sale in usa
pharmacies without prescriptions: meds online without prescription – online pharmacy with prescription
best no prescription online pharmacy: non prescription online pharmacy – canada drugs no prescription
http://indianpharm.shop/# reputable indian online pharmacy
pharmacy com canada
no prescription medicine: prescription canada – best online pharmacies without prescription
prednisone 20mg buy online
http://aviatoroyna.bid/# aviator oyunu 20 tl
valtrex daily
buy cialis generic
bupropion xl 150mg tablets 24 h
synthroid canada price
https://pinupgiris.fun/# pin-up casino indir
sweet bonanza yasal site: sweet bonanza 100 tl – sweet bonanza guncel
sweet bonanza demo: slot oyunlari – sweet bonanza giris
northwest pharmacy canada
prednisone 5052
buying tadalafil in mexico
https://sweetbonanza.bid/# sweet bonanza hilesi
aviator hilesi ucretsiz: aviator oyna slot – aviator ucak oyunu
where can i get prednisone
lisinopril 10 best price
http://slotsiteleri.guru/# en çok kazandiran slot siteleri
http://aviatoroyna.bid/# aviator nas?l oynan?r
rate online pharmacies
http://pinupgiris.fun/# pin up 7/24 giris
synthroid without a prescription
aviator oyunu 10 tl: aviator ucak oyunu – aviator oyunu giris
sweet bonanza 90 tl: pragmatic play sweet bonanza – sweet bonanza yorumlar
https://aviatoroyna.bid/# aviator giris
buy cialis 20mg uk
pragmatic play gates of olympus: gates of olympus oyna ucretsiz – gates of olympus nas?l para kazanilir
http://slotsiteleri.guru/# en yeni slot siteleri
http://pinupgiris.fun/# pin-up casino
synthroid no prescription pharmacy
online pharmacy indonesia
lisinopril for sale online
http://gatesofolympus.auction/# gates of olympus giris
pin-up casino: pin up casino – pin up aviator
generic azithromycin cost
drug lisinopril
http://gatesofolympus.auction/# gates of olympus max win
azithromycin 500mg tablets for sale
glucophage 100 mg tablet india
lisinopril online uk
valtrex generic price
sweet bonanza taktik: sweet bonanza siteleri – sweet bonanza slot
pin up guncel giris: pin up casino – pin-up casino giris
compare cialis prices uk
http://sweetbonanza.bid/# sweet bonanza free spin demo
https://gatesofolympus.auction/# pragmatic play gates of olympus
http://sweetbonanza.bid/# sweet bonanza
canadian pharmacy discount coupon
sweet bonanza bahis: sweet bonanza yasal site – sweet bonanza demo oyna
prednisone 50 mg prices
synthroid pills
https://slotsiteleri.guru/# deneme bonusu veren slot siteleri
gates of olympus slot: gates of olympus – gates of olympus s?rlar?
zithromax
mail order pharmacy india
https://pinupgiris.fun/# pin up casino
synthroid 100 mcg online
no rx pharmacy
sweet bonanza demo: sweet bonanza siteleri – sweet bonanza yorumlar
http://pinupgiris.fun/# pin up casino güncel giris
aviator mostbet: aviator hile – aviator oyna
synthroid 100 mcg
buy prednisone online uk
purchasing cialis in mexico
trustworthy canadian pharmacy
https://gatesofolympus.auction/# gates of olympus sirlari
http://aviatoroyna.bid/# aviator oyunu 20 tl
cialas
pin-up online: pin up casino – pin up casino guncel giris
zoloft and buspar
synthroid 75 mcg cheap
metformin price canada
synthroid 500 mcg
https://aviatoroyna.bid/# aviator oyna 100 tl
gates of olympus slot: gates of olympus oyna demo – gates of olympus guncel
best online pharmacy reddit
pin up: aviator pin up – pin up casino guncel giris
https://slotsiteleri.guru/# slot oyun siteleri
https://mexicanpharmacy.shop/# medicine in mexico pharmacies
pharmacies in mexico that ship to usa best online pharmacies in mexico mexican drugstore online
purchase cialis in australia
pharmacy website india: indian pharmacy – indian pharmacies safe
where can i buy cialis over the counter in uk
medicine in mexico pharmacies Mexican Pharmacy Online purple pharmacy mexico price list
metformin 500mg
online pharmacy indonesia
rx pharmacy online 24
online pharmacy bc
generic cialis black
indian pharmacy Healthcare and medicines from India buy prescription drugs from india
https://mexicanpharmacy.shop/# mexican border pharmacies shipping to usa
best online pharmacies in mexico: mexican pharmacy – mexican rx online
best online pharmacies in mexico: mexican pharmacy – buying prescription drugs in mexico
tadalafil 40 mg
canada cloud pharmacy online canadian pharmacy review best rated canadian pharmacy
trustworthy canadian pharmacy: Large Selection of Medications – legit canadian pharmacy online
levothyroxine ordering online
synthroid 0.1 mg
canada drugs online: Prescription Drugs from Canada – ed meds online canada
metformin 200
best online pharmacies in mexico: mexico pharmacy – mexican pharmaceuticals online
canadianpharmacy com pills now even cheaper pharmacy rx world canada
wholesale pharmacy
canadian pharmacies that deliver to the us: pills now even cheaper – medication canadian pharmacy
indian pharmacy: Healthcare and medicines from India – indian pharmacies safe
http://indianpharmacy.icu/# indianpharmacy com
top online pharmacy india: indian pharmacy – online pharmacy india
lisinopril 10 mg over the counter
canadian pharmacy ltd pills now even cheaper prescription drugs canada buy online
canadian pharmacy reviews: Certified Canadian Pharmacy – canadian pharmacy sarasota
cialis best buy
drug synthroid
mexican drugstore online: purple pharmacy mexico price list – medication from mexico pharmacy
reliable canadian pharmacy canadian pharmacy 24 canadianpharmacymeds com
mexico drug stores pharmacies: Online Pharmacies in Mexico – mexican mail order pharmacies
medicine lisinopril 10 mg
azithromycin tabs 250 mg
buy azithromycin online usa
purchase valtrex canada
online pharmacy fungal nail
mexico drug stores pharmacies: cheapest mexico drugs – buying prescription drugs in mexico online
medication from mexico pharmacy reputable mexican pharmacies online mexican drugstore online
lisinopril 10 mg
http://indianpharmacy.icu/# buy prescription drugs from india
mexican rx online: cheapest mexico drugs – mexican mail order pharmacies
buying prescription drugs in mexico online mexico pharmacy buying prescription drugs in mexico
lisinopril 20 mg price
lisinopril 40 mg no prescription
buy prednisone 10mg online
legitimate online pharmacies india: indian pharmacy delivery – top 10 pharmacies in india
online pharmacy no prescription needed
mexican pharmaceuticals online Mexican Pharmacy Online purple pharmacy mexico price list
india pharmacy mail order: Healthcare and medicines from India – reputable indian pharmacies
metformin 150
lisinopril 15 mg
azithromycin over the counter in usa
buying from online mexican pharmacy: mexican pharmacy – buying from online mexican pharmacy
where to get amoxicillin over the counter amoxicillin online purchase amoxicillin 500 mg purchase without prescription
prednisone 40 mg rx: prednisone 20 mg – where can i get prednisone
how can i get clomid without insurance: cheap clomid without prescription – can you buy clomid without insurance
https://zithromaxall.com/# buy azithromycin zithromax
lisinopril online purchase
can i order generic clomid pills how can i get cheap clomid online can i order generic clomid now
https://prednisoneall.shop/# where can i buy prednisone without a prescription
lisinopril online uk
https://clomidall.shop/# where buy clomid price
how to buy cheap clomid now buying generic clomid prices can i get cheap clomid without insurance
prednisone online
http://clomidall.shop/# can i purchase clomid no prescription
http://zithromaxall.shop/# azithromycin zithromax
cheap clomid how to buy generic clomid online cost cheap clomid
prednisone 10 mg brand name
cialis generic from mexico
prednisone for sale
synthroid 62.5 mcg
purchase prednisone: 20 mg prednisone – buy prednisone online without a script
https://clomidall.shop/# buying generic clomid without insurance
how to buy zithromax online zithromax price south africa zithromax pill
http://zithromaxall.com/# how to get zithromax
tadalafil canada price
synthroid 62 5 mcg
synthroid 200 mcg coupon
zestoretic tabs
synthroid 250
http://clomidall.shop/# where can i get cheap clomid without insurance
amoxicillin 500 capsule amoxicillin 500mg price canada amoxicillin order online
https://amoxilall.shop/# amoxicillin 500mg capsule buy online
tadalafil online prescription
generic amoxicillin cost: how much is amoxicillin prescription – amoxicillin 500 mg without a prescription
canadian pharmacy com
https://amoxilall.com/# amoxicillin over the counter in canada
prednisone online cost of prednisone can i order prednisone
prednisone cost
amoxicillin for sale online: amoxicillin tablets in india – amoxicillin 875 mg tablet
canadian pharmacy generic tadalafil
https://clomidall.shop/# where can i buy cheap clomid pill
synthroid 150 mcg price
azithromycin online sale
amoxicillin where to get amoxicillin over the counter in canada generic amoxicillin 500mg
https://zithromaxall.com/# zithromax cost
https://amoxilall.shop/# amoxicillin 500 mg where to buy
cost of synthroid mexico
amoxicillin online no prescription amoxicillin 500mg price amoxicillin cephalexin
online pharmacy uk
http://zithromaxall.com/# zithromax tablets for sale
synthroid 5mcg
generic tadalafil usa pharmacy
online pet pharmacy
Kamagra Oral Jelly: kamagra best price – п»їkamagra
buy Viagra over the counter: sildenafil iq – Cheap generic Viagra
1 lisinopril
Buy Tadalafil 5mg cialis best price Cialis 20mg price
https://kamagraiq.shop/# super kamagra
where to purchase cialis cheap
ordering metformin on line without a prescription
Tadalafil price: tadalafil iq – cheapest cialis
cheapest viagra sildenafil iq cheap viagra
viagra canada: sildenafil iq – Sildenafil Citrate Tablets 100mg
lisinopril 3.125
lisinopril 5mg tablets
trustworthy canadian pharmacy
buy tadalafil online india
buy kamagra online usa: Kamagra Iq – Kamagra tablets
buy Viagra online: sildenafil iq – Buy Viagra online cheap
legitimate canadian mail order pharmacy
Tadalafil price Generic Tadalafil 20mg price Buy Cialis online
tadalafil tablets india online
Kamagra Oral Jelly: kamagra best price – cheap kamagra
http://tadalafiliq.com/# Generic Tadalafil 20mg price
tadalafil us
synthroid 175 mcg price
lisinopril 40mg
Buy Tadalafil 5mg: cheapest cialis – Generic Cialis price
buy Kamagra kamagra best price Kamagra 100mg price
valtrex order canada
zestril medicine
cialis generic from mexico
synthroid 0.05
Kamagra 100mg price: Kamagra Iq – kamagra
online pharmacy delivery delhi
Tadalafil Tablet Generic Tadalafil 20mg price Tadalafil price
Viagra Tablet price: generic ed pills – Sildenafil Citrate Tablets 100mg
Kamagra 100mg price: Sildenafil Oral Jelly – Kamagra tablets
http://sildenafiliq.xyz/# viagra without prescription
lisinopril 10mg
https://sildenafiliq.com/# Buy Viagra online cheap
buy Viagra over the counter: generic ed pills – Viagra online price
metformin canada brand name
metformin 93
Cheap Sildenafil 100mg buy viagra online buy Viagra online
where to buy metformin tablets
https://kamagraiq.com/# buy Kamagra
Kamagra 100mg price: kamagra best price – cheap kamagra
gold pharmacy online
brazilian pharmacy online
buy kamagra online usa: Sildenafil Oral Jelly – Kamagra Oral Jelly
Buy Tadalafil 5mg cialis without a doctor prescription Buy Tadalafil 5mg
https://tadalafiliq.com/# Cialis 20mg price in USA
sildenafil oral jelly 100mg kamagra: Kamagra Oral Jelly Price – Kamagra 100mg price
where can i get prednisone
where to get metformin
super kamagra Kamagra Oral Jelly Price sildenafil oral jelly 100mg kamagra
http://kamagraiq.com/# buy kamagra online usa
viagra canada: buy viagra online – Viagra online price
Buy generic 100mg Viagra online: best price on viagra – Viagra tablet online
buy prinivil online
best price generic cialis 20mg
http://kamagraiq.com/# super kamagra
Buy Tadalafil 5mg: cialis best price – cheapest cialis
https://sildenafiliq.xyz/# Cheap Viagra 100mg
Kamagra Oral Jelly Sildenafil Oral Jelly super kamagra
lisinopril 20 mg price in india
cheap kamagra: Kamagra gel – buy Kamagra
good value pharmacy
online pharmacy ordering
zestoretic cost
http://kamagraiq.shop/# п»їkamagra
synthroid
Kamagra 100mg Kamagra 100mg price Kamagra 100mg price
Kamagra 100mg price: kamagra best price – Kamagra tablets
lisinopril 80
buy metformin 500 mg online
best canadian online pharmacy
synthroid 0.05 mg tablets
valtrex prescription medicine
price cialis usa
purple pharmacy mexico price list: online pharmacy in Mexico – mexican border pharmacies shipping to usa
glucophage cost india
https://mexicanpharmgrx.com/# reputable mexican pharmacies online
medicine in mexico pharmacies: mexican pharmacy – purple pharmacy mexico price list
india online pharmacy top online pharmacy india reputable indian online pharmacy
60 lisinopril cost
valtrex generic canada
buy tadalafil tablets 20 mg
canadian pharmacy online cialis
https://indianpharmgrx.shop/# mail order pharmacy india
synthroid 0.75 mg
Online medicine order Generic Medicine India to USA top online pharmacy india
http://mexicanpharmgrx.com/# mexico drug stores pharmacies
how can i get metformin
canadian pharmacy meds Canada pharmacy canadian pharmacy drugs online
http://canadianpharmgrx.com/# canadianpharmacy com
online valtrex prescription
best canadian online pharmacy: Canadian pharmacy prices – northwest pharmacy canada
https://canadianpharmgrx.com/# canadian pharmacy scam
buying prescription drugs in mexico: Mexico drugstore – mexico drug stores pharmacies
indian pharmacy paypal indian pharmacy delivery best online pharmacy india
synthroid 100 mg coupon
https://mexicanpharmgrx.com/# mexican pharmaceuticals online
canadian pharmacy coupon code
п»їbest mexican online pharmacies mexican pharmacy п»їbest mexican online pharmacies
how much is valtrex canada
online viagra from india happy family store
lisinopril 5 mg daily
lisinopril price comparison
https://mexicanpharmgrx.com/# buying prescription drugs in mexico
zithromax 1000mg
happy family pharmacy order status
cost of metformin 750 mg
Online medicine home delivery indian pharmacy delivery mail order pharmacy india
lisinopril 40 mg best price
10 mg lisinopril tablets
http://canadianpharmgrx.com/# canadian pharmacy 24h com
buying lisinopril in mexico
mexican border pharmacies shipping to usa: online pharmacy in Mexico – buying prescription drugs in mexico
glucophage compare
your pharmacy online
buy brand name synthroid online
http://indianpharmgrx.com/# india online pharmacy
mexican rx online reputable mexican pharmacies online mexican online pharmacies prescription drugs
legal online pharmacy coupon code
reputable indian online pharmacy: indian pharmacy – pharmacy website india
https://mexicanpharmgrx.com/# reputable mexican pharmacies online
pharmacy wholesalers canada International Pharmacy delivery cheapest pharmacy canada
prednisone 1 mg coupon
https://mexicanpharmgrx.com/# mexican pharmacy
legitimate mexican pharmacy online
metformin buy online usa
lisinopril 40 mg cost
0.025 mg synthroid
https://mexicanpharmgrx.shop/# mexico drug stores pharmacies
reputable mexican pharmacies online Mexico drugstore mexican rx online
cialis daily cost canada
how much is valtrex in canada
mexican border pharmacies shipping to usa: Pills from Mexican Pharmacy – п»їbest mexican online pharmacies
price of prednisone 5mg
http://indianpharmgrx.shop/# pharmacy website india
tadalafil tablets for sale
top online pharmacy india: reputable indian online pharmacy – online shopping pharmacy india
generic valtrex no prescription
http://mexicanpharmgrx.com/# mexican drugstore online
synthroid 0.05 mg daily
buying from online mexican pharmacy Mexico drugstore buying from online mexican pharmacy
54 prednisone
cheapest on line valtrex without a prescription
generic lisinopril 5 mg
online pharmacy pain relief
prinivil 20 mg tablet
buy misoprostol over the counter: buy cytotec over the counter – cytotec pills buy online
prednisone canada pharmacy
antibiotics cipro cipro 500mg best prices buy ciprofloxacin
https://misoprostol.top/# cytotec pills buy online
diflucan tablet price: diflucan for sale online – diflucan 200 mg cost
nolvadex side effects: tamoxifen benefits – nolvadex half life
pharmacy shop
buy cipro cheap cipro cipro pharmacy
best generic valtrex
tadalafil price comparison
cipro 500mg best prices: buy cipro cheap – cipro for sale
purchase cytotec buy cytotec in usa cytotec online
synthroid from india
ciprofloxacin generic price: buy cipro online without prescription – cipro online no prescription in the usa
best online foreign pharmacies
buy doxycycline online: where to purchase doxycycline – vibramycin 100 mg
tamoxifen blood clots: nolvadex pills – where to get nolvadex
metformin 500 mg tablet price
where can you buy valtrex over the counter
cipro ciprofloxacin cipro ciprofloxacin cipro for sale
synthroid 112 mcg india
buy cytotec in usa: cytotec online – Cytotec 200mcg price
https://misoprostol.top/# buy misoprostol over the counter
prednisone 10mg
tadalafil otc usa
lisinopril 2.5 mg cost
tamoxifen tamoxifen side effects forum tamoxifen vs clomid
Abortion pills online: cytotec pills online – Abortion pills online
synthroid 50 mcg generic
synthroid 50
buy prinivil
tamoxifen cancer: lexapro and tamoxifen – tamoxifen endometrium
doxylin purchase doxycycline online doxycycline tablets
canadian pharmacy cialis brand
synthroid 15 mg
metformin 19.99
where can i purchase diflucan: diflucan 200mg tab – cost of diflucan in canada
buy cytotec pills: buy cytotec pills – cytotec abortion pill
buy azithromycin online uk
diflucan prices canada buy diflucan uk where can i get diflucan
prinivil 20mg tabs
purchase cytotec: Cytotec 200mcg price – buy cytotec over the counter
zestril tab 10mg
http://diflucan.icu/# diflucan coupon canada
can you buy zithromax over the counter
prednisone 13 mg
where can i buy cipro online: buy cipro online – buy cipro
tamoxifen benefits buy nolvadex online benefits of tamoxifen
buy generic zithromax
which pharmacy is cheaper
indian pharmacy paypal
nolvadex side effects: nolvadex during cycle – nolvadex generic
tadalafil 10mg price
lisinopril 80 mg
metformin 250 mg price in india
buy tadalafil europe
ciprofloxacin buy cipro online canada cipro for sale
lisinopril 2.5 tablet
Abortion pills online: cytotec abortion pill – cytotec online
canadian pharmacy 365
025 mg synthroid
benicar lisinopril
lisinopril 20 mg canadian pharmacy
metformin over the counter canada
cialis tadalafil
azithromycin 500mg pills
buy ciprofloxacin: buy cipro online without prescription – ciprofloxacin over the counter
buy metformin 500 mg online
cytotec pills buy online: Abortion pills online – buy cytotec in usa
how to order cialis online
purchase diflucan online where to purchase over the counter diflucan pill diflucan online purchase uk
metformin price in india
lisinopril 2.5 mg buy online
tadalafil 20 mg in canada
affordable pharmacy
azithromycin 250 mg tablet over the counter
happy family drugstore
https://doxycyclinest.pro/# buy doxycycline online
doxycycline hyc 100mg: buy doxycycline – doxycycline 50mg
generic cialis daily
tadalafil canada 20mg
synthroid 0.100 mg
liquid tamoxifen raloxifene vs tamoxifen tamoxifen adverse effects
metformin tablet buy online
diflucan pills online: diflucan online cheap – can i buy diflucan over the counter
prednisone prescription online
tadalafil 20mg buy
prednisone 10mg online
amoxicillin 500 mg tablet: buy amoxicillin 250mg – generic amoxicillin cost
can i buy amoxicillin online buy amoxicillin online without prescription how to buy amoxycillin
http://clomida.pro/# buying generic clomid price
how to buy amoxicillin online: buy cheap amoxicillin online – amoxicillin 500mg capsules antibiotic
synthroid 50 mg tablet
zithromax purchase online: zithromax prescription – buy zithromax online cheap
prednisone 1 mg daily
how to buy prednisone prednisone online paypal prednisone 5 mg tablet cost
cheapest price for lisinopril india
ivermectin 8000 mcg: ivermectin 6mg tablet for lice – ivermectin 50 mg
http://azithromycina.pro/# zithromax 500mg
synthroid 0.15 mg
canadian pharmacy mall
buy clomid without rx cost of generic clomid cost of cheap clomid
buy cheap prednisone online
prednisone 5mg daily: prednisone brand name canada – buying prednisone
buy real valtrex online
http://clomida.pro/# can you buy generic clomid for sale
northwest pharmacy canada
amoxicillin buy online canada: cost of amoxicillin 30 capsules – amoxicillin 500mg price canada
https://prednisonea.store/# can you buy prednisone over the counter in canada
buy zithromax no prescription zithromax prescription in canada buy zithromax online australia
mypharmacy
where to get zithromax: where can i get zithromax over the counter – zithromax online paypal
buy generic clomid no prescription: how can i get generic clomid without insurance – cost clomid tablets
http://stromectola.top/# ivermectin over the counter canada
best online pharmacy reddit
ivermectin buy nz: ivermectin lotion for scabies – cost of ivermectin 1% cream
how much is cialis 20mg
price of metformin
canada pharmacy world
https://clomida.pro/# how to buy clomid price
prednisone price uk
valtrex best price
reddit canadian pharmacy
synthroid brand 0.15mg
mexican pharmacy online
azithromycin 9 pills
canadian prescription drugstore review canadian pharmacy without a prescription buy pills without prescription
http://medicationnoprescription.pro/# mexican prescription drugs online
https://medicationnoprescription.pro/# canada drugs without prescription
prescription drugs online: no prescription pharmacy paypal – cheapest pharmacy for prescriptions
synthroid 0.05 mg
valtrex 1000 mg
https://onlinepharmacyworld.shop/# best no prescription pharmacy
online prescription for ed: get ed prescription online – ed drugs online
canadian pharmacy viagra
best online pharmacy no prescription canada pharmacy coupon canadian pharmacies not requiring prescription
metformin coupon pharmacy
https://medicationnoprescription.pro/# online drugs without prescription
buying valtrex
online pharmacy discount code: online pharmacy discount code – canadian pharmacy coupon code
https://medicationnoprescription.pro/# online pharmacy canada no prescription
meds no prescription cheap prescription drugs online best online pharmacy without prescriptions
buy valtrex 1000 mg
http://edpill.top/# ed online treatment
online ed drugs: low cost ed pills – cheap erectile dysfunction pills
https://medicationnoprescription.pro/# no prescription needed online pharmacy
cialis otc us
lisinopril 20 mg tablets
online canadian pharmacy no prescription: quality prescription drugs canada – best online pharmacies without prescription
lisinopril 12.5
ed online pharmacy erectile dysfunction online prescription online ed drugs
lisinopril 20mg tablets
metformin buy india
https://onlinepharmacyworld.shop/# best canadian pharmacy no prescription
buy medications without a prescription: order medication without prescription – canada drugs no prescription
canadian prescription pharmacy
valtrex 1g best price
https://onlinepharmacyworld.shop/# canadian online pharmacy no prescription
pharmacy no prescription how to get a prescription in canada can you buy prescription drugs in canada
happy family store pharmacy
us pharmacy no prescription
https://casinvietnam.shop/# web c? b?c online uy tin
online pharmacy group
lisinopril medication
casino online uy tín: casino tr?c tuy?n uy tín – casino tr?c tuy?n uy tín
synthroid 0.75 mcg
synthroid 137.5 mcg
http://casinvietnam.shop/# casino tr?c tuy?n vi?t nam
drug prices lisinopril
prednisone otc
lisinopril 4214
choi casino tr?c tuy?n trên di?n tho?i: casino tr?c tuy?n uy tín – choi casino tr?c tuy?n trên di?n tho?i
casino tr?c tuy?n vi?t nam danh bai tr?c tuy?n casino tr?c tuy?n uy tin
game c? b?c online uy tin danh bai tr?c tuy?n casino tr?c tuy?n vi?t nam
pharmacy online shopping usa
synthroid brand name price
lisinopril pill 5 mg
synthroid canada
zithromax 100
buy zithromax online canada
buy prednisone 20mg without a prescription best price
where can i buy metformin without a prescription
price of 100mcg synthroid
zithromax 100 mg
foreign pharmacy online
buy zestril
rx azithromycin
cheapest pharmacy canada
medicine prednisone 10mg
web c? b?c online uy tín: dánh bài tr?c tuy?n – web c? b?c online uy tín
https://casinvietnam.shop/# casino tr?c tuy?n
does voltaren gel work on nuropathy
casino tr?c tuy?n vi?t nam: casino tr?c tuy?n vi?t nam – casino online uy tín
where can i buy metformin in south africa
how much is 20 mg cialis
http://casinvietnam.com/# casino online uy tin
casino tr?c tuy?n: casino tr?c tuy?n uy tín – casino tr?c tuy?n
online lisinopril
https://casinvietnam.com/# danh bai tr?c tuy?n
canadian pharmacy without prescription
synthroid uk
casino online uy tín: casino tr?c tuy?n uy tín – casino tr?c tuy?n vi?t nam
azithromycin discount
mail order pharmacy no prescription
http://casinvietnam.com/# game c? b?c online uy tin
casino online uy tín: casino tr?c tuy?n uy tín – casino online uy tín
save on pharmacy
casino tr?c tuy?n vi?t nam: casino tr?c tuy?n uy tín – choi casino tr?c tuy?n trên di?n tho?i
http://casinvietnam.com/# casino tr?c tuy?n uy tin
casino tr?c tuy?n vi?t nam: casino online uy tín – choi casino tr?c tuy?n trên di?n tho?i
https://casinvietnam.shop/# game c? b?c online uy tin
synthroid 0.1 mcg
choi casino tr?c tuy?n tren di?n tho?i casino online uy tin danh bai tr?c tuy?n
web c? b?c online uy tín: dánh bài tr?c tuy?n – casino tr?c tuy?n vi?t nam
valtrex singapore
http://casinvietnam.com/# game c? b?c online uy tin
casino online uy tín: dánh bài tr?c tuy?n – casino online uy tín
web c? b?c online uy tin game c? b?c online uy tin danh bai tr?c tuy?n
rx azithromycin tablets
buy tadalafil 5 mg from india
web c? b?c online uy tín: choi casino tr?c tuy?n trên di?n tho?i – casino tr?c tuy?n vi?t nam
https://casinvietnam.com/# casino tr?c tuy?n vi?t nam
choi casino tr?c tuy?n tren di?n tho?i game c? b?c online uy tin casino tr?c tuy?n vi?t nam
casino tr?c tuy?n vi?t nam: casino tr?c tuy?n uy tín – game c? b?c online uy tín
http://casinvietnam.shop/# web c? b?c online uy tin
game c? b?c online uy tin danh bai tr?c tuy?n danh bai tr?c tuy?n
http://casinvietnam.com/# casino tr?c tuy?n
valtrex 500 price
synthroid 12.5 mcg
web c? b?c online uy tín: web c? b?c online uy tín – casino online uy tín
mypharmacy
casino online uy tin game c? b?c online uy tin casino tr?c tuy?n uy tin
http://casinvietnam.com/# casino tr?c tuy?n
synthroid 75 mcg tab
trusted canadian pharmacy
casino online uy tín: casino tr?c tuy?n vi?t nam – casino tr?c tuy?n uy tín
zestril 10mg
azithromycin cap 250 mg
https://casinvietnam.com/# casino tr?c tuy?n
casino tr?c tuy?n vi?t nam choi casino tr?c tuy?n tren di?n tho?i casino online uy tin
http://casinvietnam.shop/# game c? b?c online uy tin
choi casino tr?c tuy?n trên di?n tho?i: casino tr?c tuy?n vi?t nam – casino tr?c tuy?n
synthroid mexico pharmacy
casino tr?c tuy?n choi casino tr?c tuy?n tren di?n tho?i game c? b?c online uy tin
metformin online buy
indian pharmacies safe Cheapest online pharmacy top online pharmacy india
http://canadaph24.pro/# canadian pharmacy world reviews
canadian online pharmacy no prescription
http://mexicoph24.life/# mexican border pharmacies shipping to usa
top 10 online pharmacy in india buy medicines from India cheapest online pharmacy india
canada pharmacy daily tadalafil
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
https://canadaph24.pro/# canada pharmacy 24h
canadian pharmacy no rx needed
п»їlegitimate online pharmacies india indian pharmacy fast delivery india pharmacy
http://indiaph24.store/# Online medicine home delivery
canadian world pharmacy: Large Selection of Medications from Canada – canadian pharmacies
https://mexicoph24.life/# medicine in mexico pharmacies
best online pharmacies in mexico purple pharmacy mexico price list medicine in mexico pharmacies
can i buy metformin without prescription
https://indiaph24.store/# reputable indian online pharmacy
where can i buy over the counter cialis
canadian pharmacy victoza Prescription Drugs from Canada recommended canadian pharmacies
generic valtrex canada
http://canadaph24.pro/# safe canadian pharmacies
http://mexicoph24.life/# mexico drug stores pharmacies
how much is lisinopril
tadalafil 5mg tablets india
online pharmacy india Generic Medicine India to USA india pharmacy
buy cialis 60mg
https://mexicoph24.life/# best online pharmacies in mexico
online shopping pharmacy india indian pharmacy fast delivery п»їlegitimate online pharmacies india
https://mexicoph24.life/# pharmacies in mexico that ship to usa
zithromax pills online
http://indiaph24.store/# indian pharmacy
mexico drug stores pharmacies mexican pharmacy mexican rx online
http://canadaph24.pro/# canadian pharmacy in canada
happy family medicine pharmacy
mexican rx online medication from mexico pharmacy mexico drug stores pharmacies
https://indiaph24.store/# Online medicine order
safe online pharmacy
https://indiaph24.store/# cheapest online pharmacy india
azithromycin capsules 500mg
canadianpharmacymeds com canadapharmacyonline ordering drugs from canada
https://mexicoph24.life/# mexico pharmacy
lisinopril 12.5 mg 20 mg
best canadian online pharmacy Licensed Canadian Pharmacy trusted canadian pharmacy
https://indiaph24.store/# buy medicines online in india
http://indiaph24.store/# indian pharmacies safe
pharmacies in mexico that ship to usa: cheapest mexico drugs – mexican pharmaceuticals online
buy tadalafil online uk
prinivil 20 mg tablet
Online medicine order indian pharmacy reputable indian pharmacies
https://mexicoph24.life/# mexico drug stores pharmacies
canadian pharmacy world reviews canada drugs reliable canadian pharmacy
zestril 2.5 mg
https://indiaph24.store/# reputable indian pharmacies
valtrex brand
https://indiaph24.store/# Online medicine home delivery
buy synthroid online uk
onlinecanadianpharmacy 24 Licensed Canadian Pharmacy canadian pharmacy phone number
valtrex 1000 mg tablet
mexican pharmaceuticals online: cheapest mexico drugs – mexican pharmaceuticals online
http://mexicoph24.life/# mexico pharmacies prescription drugs
online pharmacy delivery delhi
cheap cialis free shipping
best online pharmacy india indian pharmacy top 10 online pharmacy in india
http://indiaph24.store/# buy medicines online in india
https://mexicoph24.life/# mexico pharmacies prescription drugs
azithromycin 500 mg tablet over the counter
canada rx pharmacy Certified Canadian Pharmacies canadian pharmacy oxycodone
http://canadaph24.pro/# vipps approved canadian online pharmacy
india online pharmacy indian pharmacy fast delivery best india pharmacy
how much is lisinopril 20 mg
https://canadaph24.pro/# canadianpharmacyworld com
prednisone cream
canadian pharmacy near me canadian pharmacies cheapest pharmacy canada
where can i buy synthroid online
http://indiaph24.store/# indian pharmacy
mexican drugstore online: mexican pharmacy – mexican pharmaceuticals online
canadian mail order pharmacy Certified Canadian Pharmacies canadian pharmacy price checker
azithromycin buy without prescription
https://mexicoph24.life/# mexican mail order pharmacies
buy prescription drugs from india buy medicines from India cheapest online pharmacy india
http://indiaph24.store/# indian pharmacy paypal
indian pharmacy online indian pharmacy fast delivery top online pharmacy india
https://canadaph24.pro/# canadian pharmacy uk delivery
top 10 online pharmacy in india Generic Medicine India to USA Online medicine home delivery
best generic metformin
http://canadaph24.pro/# my canadian pharmacy
cialis online drugstore
cialis medicine in india
azithromycin 500 mg india
valtrex rx
buying prescription drugs in mexico mexico pharmacy best online pharmacies in mexico
https://mexicoph24.life/# best online pharmacies in mexico
tadalafil 2.5 mg
lisinopril 20 mg no prescription
prednisone buy cheap
legit canadian pharmacy Large Selection of Medications from Canada reliable canadian pharmacy
http://indiaph24.store/# Online medicine home delivery
mexico pharmacy buying from online mexican pharmacy mexico drug stores pharmacies
https://indiaph24.store/# india online pharmacy
how much is lisinopril 20 mg
https://indiaph24.store/# world pharmacy india
buying prescription drugs in mexico mexico pharmacy buying prescription drugs in mexico
https://indiaph24.store/# top 10 online pharmacy in india
mexico pharmacy Mexican Pharmacy Online buying prescription drugs in mexico online
buy lisinopril without prescription
prednisone 20mg cost
synthroid for sale
synthroid 150 mcg price
https://indiaph24.store/# cheapest online pharmacy india
lisinopril 10 mg online no prescription
world pharmacy india Cheapest online pharmacy buy medicines online in india
zithromax for sale
http://mexicoph24.life/# mexican rx online
mexican pharmaceuticals online Online Pharmacies in Mexico medicine in mexico pharmacies
all med pharmacy
austria pharmacy online
pharmacy wholesalers canada: prescription drugs canada buy online – canada pharmacy
https://canadaph24.pro/# canadian pharmacies compare
valtrex online australia
canadian online pharmacy canadian pharmacies my canadian pharmacy
https://indiaph24.store/# Online medicine order
online pharmacy australia
lisinopril 4 mg
https://indiaph24.store/# india pharmacy mail order
mexican pharmaceuticals online mexico pharmacy buying prescription drugs in mexico
https://indiaph24.store/# top online pharmacy india
promo code for canadian pharmacy meds
mexico drug stores pharmacies Mexican Pharmacy Online buying prescription drugs in mexico
tadalafil 10 mg cost
http://indiaph24.store/# Online medicine home delivery
online shopping pharmacy india: indian pharmacy fast delivery – top 10 online pharmacy in india
mexican drugstore online mexican pharmacy buying prescription drugs in mexico
indian pharmacies safe https://indiaph24.store/# online shopping pharmacy india
indianpharmacy com
synthroid 137mg without prescription
order lisinopril online from canada
tadalafil 600 mg
http://indiaph24.store/# online shopping pharmacy india
average price of prednisone
lisinopril 40 mg daily
canadian pharmacy cialis
buy valtrex online usa
india online pharmacy buy medicines online in india indian pharmacy
http://indiaph24.store/# pharmacy website india
generic tadalafil 60 mg
lisinopril 2
Online medicine order Cheapest online pharmacy buy prescription drugs from india
http://mexicoph24.life/# best online pharmacies in mexico
reputable indian online pharmacy online pharmacy india top 10 pharmacies in india
prednisone brand name uk
legal online pharmacies in the us
buy canadian drugs: Licensed Canadian Pharmacy – canadian drug prices
http://canadaph24.pro/# canadian pharmacy online ship to usa
azithromycin 2000 mg
average cost of cialis
mexican mail order pharmacies reputable mexican pharmacies online purple pharmacy mexico price list
glucophage tablets 250mg
https://indiaph24.store/# best online pharmacy india
canadian online pharmacy no prescription
canadian drugs Large Selection of Medications from Canada legal canadian pharmacy online
http://canadaph24.pro/# canadian pharmacies that deliver to the us
indian pharmacy paypal Generic Medicine India to USA indian pharmacy paypal
https://canadaph24.pro/# canadian pharmacy ratings
online pharmacy usa
best canadian pharmacy Prescription Drugs from Canada best mail order pharmacy canada
http://mexicoph24.life/# best online pharmacies in mexico
mexican rx online: cheapest mexico drugs – best online pharmacies in mexico
lisinopril tab 5 mg price
synthroid 137 mcg tab
http://mexicoph24.life/# pharmacies in mexico that ship to usa
mexico pharmacies prescription drugs Mexican Pharmacy Online mexico pharmacy
https://mexicoph24.life/# purple pharmacy mexico price list
mexico drug stores pharmacies cheapest mexico drugs mexico pharmacy
online pharmacy price checker
price lisinopril 20 mg
prinivil brand name
india online pharmacy http://indiaph24.store/# indian pharmacies safe
indian pharmacies safe
buy tadalafil generic from canada
medicine in mexico pharmacies: cheapest mexico drugs – mexico pharmacy
lisinopril 102
indian pharmacy online buy medicines from India Online medicine home delivery
http://mexicoph24.life/# п»їbest mexican online pharmacies
mexican drugstore online: cheapest mexico drugs – pharmacies in mexico that ship to usa
http://canadaph24.pro/# vipps canadian pharmacy
mexican drugstore online Mexican Pharmacy Online buying prescription drugs in mexico online
canada cloud pharmacy
buying prescription drugs in mexico: medicine in mexico pharmacies – п»їbest mexican online pharmacies
where to buy prescription synthroid
secure medical online pharmacy
synthroid 25 pill
buy azithromycin online australia
http://mexicoph24.life/# mexican pharmacy
prednisone 5442
reputable indian pharmacies buy medicines from India reputable indian online pharmacy
https://canadaph24.pro/# my canadian pharmacy reviews
purchase synthroid
synthroid 175 mg
https://nolvadex.life/# tamoxifen breast cancer
azithromycin prescription online
http://ciprofloxacin.tech/# antibiotics cipro
cipro 500mg best prices п»їcipro generic ciprofloxacin generic
how much is valtrex tablets
http://ciprofloxacin.tech/# where can i buy cipro online
alternatives to tamoxifen: nolvadex 20mg – is nolvadex legal
tadalafil 5mg price india
lisinopril 10 mg prices
prinivil tabs: lisinopril over the counter – buy zestoretic
lisinopril 5 mg tabs lisinopril 80mg lisinopril 250mg
https://finasteride.store/# buy propecia prices
http://nolvadex.life/# nolvadex vs clomid
tamoxifen for men: tamoxifen for gynecomastia reviews – tamoxifen premenopausal
cost of lisinopril 40 mg
tadalafil tablets 40mg
order propecia tablets get generic propecia price order propecia without rx
https://ciprofloxacin.tech/# buy cipro online without prescription
purchase cipro: buy cipro cheap – ciprofloxacin mail online
can you buy valtrex over the counter
prednisone 13 mg
http://finasteride.store/# propecia online
buying online metformin without prescription
synthroid brand name price
https://cytotec.club/# buy cytotec over the counter
buy propecia for sale: get generic propecia without insurance – get cheap propecia tablets
http://nolvadex.life/# tamoxifen hormone therapy
economy pharmacy
generic lisinopril 40 mg cheapest lisinopril 10 mg lisinopril coupon
cipro ciprofloxacin buy ciprofloxacin over the counter where can i buy cipro online
buy lisinopril 20 mg online uk: lisinopril 60 mg – zestril 10 mg
http://finasteride.store/# propecia
https://nolvadex.life/# nolvadex half life
п»їcytotec pills online cytotec abortion pill order cytotec online
buy cytotec in usa: Cytotec 200mcg price – Abortion pills online
cipro ciprofloxacin ciprofloxacin mail online antibiotics cipro
metformin er
rate online pharmacies
how much is tadalafil
order cheap propecia no prescription: buy cheap propecia no prescription – order cheap propecia tablets
tadalafil canada online pharmacy
https://finasteride.store/# cost of propecia pill
tamoxifen skin changes tamoxifen cost nolvadex estrogen blocker
https://ciprofloxacin.tech/# cipro
synthroid canada
buy cipro antibiotics cipro cipro pharmacy
lisinopril prescription cost: lisinopril from mexico – lisinopril online without prescription
otc lisinopril
https://finasteride.store/# order generic propecia without rx
online pharmacy no prescription needed
tadalafil for sale online
corticosteroids prednisone
cialis 2019
drug lisinopril: lisinopril 10 mg price in india – lisinopril 10mg online
pharmacy canadian superstore
prednisone 50 mg price in india
tamoxifen skin changes tamoxifen hip pain nolvadex during cycle
synthroid 275 mcg
http://ciprofloxacin.tech/# п»їcipro generic
https://cytotec.club/# Abortion pills online
cialis genuine buy
cost propecia prices: rx propecia – cost of cheap propecia now
canadian pharmacy online store
order cytotec online п»їcytotec pills online buy cytotec pills online cheap
cytotec abortion pill: cytotec online – cytotec pills online
where to buy prednisone online
https://ciprofloxacin.tech/# antibiotics cipro
cialis 5mg online price
https://ciprofloxacin.tech/# ciprofloxacin over the counter
lisinopril 5 mg tabs: lisinopril over the counter – zestril 2.5 mg
zestoretic 5 mg
promo code for canadian pharmacy meds
lisinopril 20mg india
zestril over the counter
purchase cytotec buy cytotec online cytotec buy online usa
http://lisinopril.network/# prinivil 5 mg tablets
femara vs tamoxifen nolvadex pills tamoxifen endometriosis
prednisone 40 mg
cheap propecia tablets: generic propecia no prescription – order propecia without rx
synthroid medication cost
http://ciprofloxacin.tech/# antibiotics cipro
https://nolvadex.life/# cost of tamoxifen
prednisone without prescription
where to buy zithromax online
lisinopril 5 mg tablet cost: lisinopril otc – lisinopril tablets uk
tamoxifen cost how to lose weight on tamoxifen tamoxifen blood clots
ciprofloxacin 500mg buy online cipro 500mg best prices cipro
lisinopril brand name in usa
Cytotec 200mcg price: buy cytotec – cytotec online
azithromycin 1000mg
http://lisinopril.network/# zestoretic 20
buy cialis online australia paypal
http://nolvadex.life/# tamoxifen and uterine thickening
buy generic propecia without prescription: buy cheap propecia – cost propecia tablets
buy cheap propecia no prescription generic propecia no prescription cost generic propecia without insurance
zestoretic online
antibiotics cipro cipro online no prescription in the usa antibiotics cipro
tadalafil tablet online in india
azithromycin 250 mg tablet cost
price of lisinopril 20 mg: zestril 40 – medication lisinopril 5 mg
https://cytotec.club/# Cytotec 200mcg price
https://finasteride.store/# propecia
http://nolvadex.life/# nolvadex estrogen blocker
price of lisinopril 20 mg
metformin pills 500 mg
which online pharmacy is reliable
cost of brand name lisinopril zestril tablet price ordering lisinopril without a prescription uk
90 lisinopril
overseas pharmacy no prescription
does tamoxifen make you tired: hysterectomy after breast cancer tamoxifen – nolvadex estrogen blocker
prednisone buy canada
synthroid cheapest prices
azithromycin otc usa
valtrex rx where to buy
canadian pharmacy 365
ciprofloxacin mail online: ciprofloxacin order online – ciprofloxacin generic price
synthroid 0.075 mg
http://finasteride.store/# propecia pills
buy cytotec online cytotec abortion pill cytotec buy online usa
https://ciprofloxacin.tech/# where can i buy cipro online
azithromycin 1000 mg drug cost
nolvadex half life tamoxifen pill tamoxifen breast cancer prevention
raloxifene vs tamoxifen: tamoxifen generic – tamoxifen endometriosis
discount pharmacy
canada pharmacy online legit
https://cialist.pro/# Buy Cialis online
https://cialist.pro/# Cialis 20mg price in USA
http://levitrav.store/# Levitra 20 mg for sale
Levitra online USA fast Levitra 10 mg best price Buy generic Levitra online
https://cialist.pro/# Cialis 20mg price
cialis generic: Generic Cialis without a doctor prescription – Generic Cialis without a doctor prescription
buy Viagra over the counter Buy generic 100mg Viagra online Viagra tablet online
sildenafil oral jelly 100mg kamagra: kamagra pills – Kamagra tablets
http://cialist.pro/# cheapest cialis
online pharmacy no prescription needed
medicine valtrex
kamagra: super kamagra – buy kamagra online usa
Viagra Tablet price: Buy Viagra online – Viagra online price
Cheap Sildenafil 100mg viagras.online Cheap generic Viagra
zestril 30 mg
canada online pharmacy no prescription
https://levitrav.store/# Buy Vardenafil 20mg online
https://kamagra.win/# п»їkamagra
Cialis without a doctor prescription: buy cialis online – buy cialis pill
american pharmacy
valtrex for sale
Vardenafil buy online: Vardenafil online prescription – Cheap Levitra online
Cheap generic Viagra Cheap Viagra 100mg viagra without prescription
Kamagra Oral Jelly kamagra pills п»їkamagra
tadalafil india online
http://cialist.pro/# Generic Tadalafil 20mg price
https://viagras.online/# sildenafil over the counter
cheapest cenforce: Cenforce 150 mg online – Buy Cenforce 100mg Online
Kamagra 100mg price: kamagra.win – super kamagra
where can you buy valtrex
Cialis without a doctor prescription buy cialis online Cialis 20mg price
Cenforce 100mg tablets for sale: Buy Cenforce 100mg Online – cenforce for sale
Kamagra 100mg price kamagra pills Kamagra 100mg
cheap tadalafil 5mg
Cheap Cialis: buy cialis overseas – Generic Cialis price
cost of valtrex generic
http://kamagra.win/# п»їkamagra
http://kamagra.win/# Kamagra Oral Jelly
viagra canada Buy Viagra online cheap Viagra online price
online pharmacy same day delivery
Cenforce 150 mg online: cheapest cenforce – order cenforce
cheapest prescription pharmacy
synthroid 100 mg prices
generic synthroid pill
Viagra generic over the counter: Cheapest place to buy Viagra – sildenafil over the counter
http://viagras.online/# Order Viagra 50 mg online
https://cialist.pro/# Buy Cialis online
https://levitrav.store/# Vardenafil online prescription
buy kamagra online usa Kamagra 100mg price Kamagra 100mg
buy kamagra online usa kamagra pills cheap kamagra
online pharmacy store
valtrex discount
how to get prednisone
Vardenafil online prescription: Buy generic Levitra online – Levitra tablet price
synthroid cost
buy cialis pill: buy cialis online – Buy Tadalafil 10mg
http://levitrav.store/# Levitra 10 mg buy online
buy Kamagra: buy kamagra online – buy Kamagra
Cialis over the counter Generic Tadalafil 20mg price Tadalafil Tablet
http://viagras.online/# Viagra without a doctor prescription Canada
https://levitrav.store/# Levitra 20 mg for sale
buy Kamagra kamagra oral jelly sildenafil oral jelly 100mg kamagra
synthroid 025 mg
azithromycin 500 mg pills
https://pharmcanada.shop/# best rated canadian pharmacy
international pharmacy no prescription cheapest pharmacy canadian pharmacy no prescription
http://pharmnoprescription.icu/# online no prescription pharmacy
canadian medications canadianpharmacyworld com canadian drug pharmacy
indianpharmacy com: Online medicine order – world pharmacy india
canadian family pharmacy: canadian pharmacy no rx needed – onlinepharmaciescanada com
canadian pharmacies not requiring prescription
pharmacy in canada: onlinepharmaciescanada com – canada drugs reviews
prednisone in mexico
indian pharmacy online: Online medicine order – mail order pharmacy india
http://pharmmexico.online/# mexico drug stores pharmacies
buying prescription drugs from canada online pharmacy no prescription needed canadian pharmacy
indian pharmacy Online medicine home delivery Online medicine order
https://pharmnoprescription.icu/# overseas online pharmacy-no prescription
costs of synthroid
https://pharmworld.store/# cheapest pharmacy for prescriptions without insurance
rx pharmacy no prescription: online pharmacy – us pharmacy no prescription
pharmacy without prescription
buying prescription drugs in canada: mexican pharmacy no prescription – canadian rx prescription drugstore
canadianpharmacymeds is canadian pharmacy legit canada pharmacy online legit
price for 5 mg lisinopril
best no prescription pharmacy: buying prescription drugs from canada – canada pharmacy not requiring prescription
cheapest pharmacy to fill prescriptions without insurance pharm world canadian pharmacy discount coupon
otc lisinopril
safe canadian pharmacies: buy canadian drugs – canadian pharmacy 365
https://pharmmexico.online/# п»їbest mexican online pharmacies
http://pharmindia.online/# buy medicines online in india
canadian pharmacy no prescription needed: no prescription needed pharmacy – canada prescription online
can you buy prednisone over the counter
indian pharmacy online: india pharmacy mail order – Online medicine home delivery
cheapest pharmacy to get prescriptions filled pharm world store online canadian pharmacy coupon
lisinopril 40 mg without prescription
canadian drugs online canadian drugstore online pharmacy wholesalers canada
prescription drugs from canada: pharm world – canadian pharmacy no prescription needed
http://pharmworld.store/# prescription drugs online
http://pharmnoprescription.icu/# prescription online canada
http://pharmworld.store/# pharmacy coupons
canada prescription drugs online: buying prescription drugs from canada online – online prescription canada
synthroid lowest prices
best australian online pharmacy
canadian pharmacy tampa canadian valley pharmacy best canadian online pharmacy
overseas online pharmacy
mexican drugstore online: mexican drugstore online – mexican pharmaceuticals online
best online pharmacy reddit
buy medicines online in india pharmacy website india buy medicines online in india
canadian pharmacy antibiotics
lisinopril 5mg cost
online pharmacy price checker
https://pharmindia.online/# indianpharmacy com
http://pharmnoprescription.icu/# canadian drugs no prescription
online pharmacy fungal nail
indian pharmacy online: cheapest online pharmacy india – top 10 online pharmacy in india
generic lisinopril 40 mg
buying prescription drugs in mexico: buying prescription drugs in mexico – mexican pharmaceuticals online
synthroid 201
mexican online pharmacies prescription drugs mexico pharmacies prescription drugs medication from mexico pharmacy
can you buy metfromin without a prescription
mexico pharmacy: mexico pharmacies prescription drugs – mexican mail order pharmacies
canada prescription buying prescription drugs online without a prescription buy medications online no prescription
generic prinivil
https://pharmindia.online/# online pharmacy india
http://pharmindia.online/# indian pharmacies safe
indian pharmacy no prescription: canadian pharmacy no prescription – non prescription canadian pharmacy
glucophage without prescription
best online pharmacy no prescription: buying prescription drugs online from canada – online pharmacy that does not require a prescription
lisinopril 104
vibramycin 100 mg: doxycycline hyc – buy doxycycline online 270 tabs
canadian pharmacy synthroid
buy zithromax 1000mg online zithromax online usa zithromax online no prescription
zithromax capsules: zithromax 500 tablet – zithromax azithromycin
zitromax
medication canadian pharmacy
zithromax 500 mg lowest price pharmacy online: zithromax 500 mg for sale – azithromycin zithromax
buy valtrex cheap
synthroid pills for sale
tadalafil daily india
https://amoxila.pro/# amoxicillin 500 mg for sale
https://amoxila.pro/# price for amoxicillin 875 mg
azithromycin paypal
zithromax online australia buy cheap zithromax online where can i buy zithromax medicine
cheap tadalafil 40 mg
order amoxicillin online no prescription: amoxicillin generic brand – buy amoxicillin 500mg usa
prednisone 10mg for sale: prednisone coupon – 10 mg prednisone
doxycycline generic buy cheap doxycycline online buy doxycycline online without prescription
synthroid 100 mcg coupon
amoxicillin pharmacy price: can i purchase amoxicillin online – where can you buy amoxicillin over the counter
buy zithromax usa
cost for 2 mg lisinopril
neurontin 600 mg coupon: neurontin generic brand – neurontin india
brand cialis usa
azithromycin 250 mg price
how much is valtrex tablets
canadian mail order pharmacy
https://prednisoned.online/# can you buy prednisone over the counter in usa
https://amoxila.pro/# purchase amoxicillin online
cost of amoxicillin prescription: can you buy amoxicillin over the counter – amoxicillin order online no prescription
doxycycline generic: purchase doxycycline online – buy doxycycline hyclate 100mg without a rx
over the counter amoxicillin: amoxicillin 500 mg tablets – buy amoxicillin 500mg uk
happy family store pharmacy
where can i buy zithromax capsules: can you buy zithromax over the counter in mexico – zithromax prescription online
generic for doxycycline: doxylin – how to buy doxycycline online
buy generic zithromax online: zithromax 500 mg – buy zithromax no prescription
buy zithromax 500mg online: zithromax 500 tablet – zithromax 500 mg for sale
lisinopril 1 mg tablet
where can i buy zithromax uk buy zithromax without prescription online zithromax 600 mg tablets
zithromax 1000 mg pills: zithromax – zithromax capsules
buy cheap zithromax online
neurontin 400 mg cost: neurontin 150mg – neurontin 300 mg mexico
metformin online purchase uk
http://amoxila.pro/# amoxicillin online canada
where to get doxycycline: buy doxycycline – doxy 200
https://gabapentinneurontin.pro/# neurontin buy online
online pharmacy in turkey
amoxicillin 500 mg purchase without prescription amoxicillin brand name amoxicillin 500mg price in canada
medicine amoxicillin 500: cost of amoxicillin prescription – amoxicillin online pharmacy
over the counter neurontin: canada where to buy neurontin – 800mg neurontin
neurontin prescription online buy cheap neurontin online buy gabapentin
canadian pharmacy online cialis
prednisone otc uk: prednisone 30 – fast shipping prednisone
order valtrex onlines
https://amoxila.pro/# buy amoxicillin online uk
https://gabapentinneurontin.pro/# neurontin brand name
prednisone 475 prednisone otc price where can i buy prednisone without a prescription
doxycycline hyc: buy doxycycline 100mg – purchase doxycycline online
prednisone price prednisone 10 mg price prednisolone prednisone
cost of cialis 20mg tablets
metformin brand name
cheapest pharmacy for prescriptions without insurance
can you buy tadalafil online
prednisone 54: prednisone uk over the counter – buy prednisone canada
http://doxycyclinea.online/# 100mg doxycycline
http://zithromaxa.store/# zithromax 250 mg tablet price
drug prices prednisone: prednisone 10mg tabs – prednisone without prescription 10mg
zithromax generic pharmacy
medicine lisinopril 10 mg
how much is generic neurontin: buy neurontin uk – neurontin 2018
doxycycline prices: how to buy doxycycline online – doxycycline generic
tadalafil in india online
canadian pharmacy service
doxycycline order online how to order doxycycline where to get doxycycline
synthroid 100 mcg cost
http://zithromaxa.store/# where can i buy zithromax medicine
neurontin 300mg neurontin buy online neurontin 800 mg tablet
https://gabapentinneurontin.pro/# how much is generic neurontin
tadalafil 2
doxycycline without a prescription: buy generic doxycycline – vibramycin 100 mg
foreign pharmacy no prescription
tadalafil 30mg
buy doxycycline for dogs: how to buy doxycycline online – price of doxycycline
neurontin 600 mg pill: neurontin coupon – 2000 mg neurontin
where can i order valtrex
zithromax 250mg zithromax cost australia buy zithromax 500mg online
http://amoxila.pro/# buy cheap amoxicillin online
buy valtrex on line
prednisone 20mg buy online prednisone in mexico can you buy prednisone over the counter
http://amoxila.pro/# can you buy amoxicillin uk
amoxicillin over the counter in canada: where can you buy amoxicillin over the counter – amoxicillin 875 125 mg tab
cost of 5 mg tadalafil pills
prednisone drug
neurontin 100mg caps: buy generic neurontin online – neurontin 1800 mg
order synthroid online
zithromax 500 mg lowest price online zithromax 250 mg pill buy zithromax 500mg online
https://zithromaxa.store/# zithromax 1000 mg online
buy zithromax 500mg online can you buy zithromax over the counter in mexico generic zithromax 500mg
https://amoxila.pro/# amoxicillin over the counter in canada
lisinopril brand name
amoxicillin capsule 500mg price: where can i buy amoxicillin online – amoxicillin 500 coupon
azithromycin generic brand
medicine prednisone 5mg: prednisone 20 mg – prednisone 200 mg tablets
pharmacy drugs
amoxicillin 500mg buy online canada: amoxicillin 50 mg tablets – amoxacillian without a percription
zithromax online: zithromax cost – where can i buy zithromax in canada
amoxicillin 800 mg price cheap amoxicillin 500mg amoxicillin 500mg buy online canada
where to buy metformin
buy azithromycin over the counter
http://doxycyclinea.online/# buy doxycycline without prescription
cost of neurontin 800 mg neurontin 200 mg tablets neurontin uk
https://prednisoned.online/# prednisone 20 mg
neurontin rx: neurontin price in india – brand name neurontin price
5 prednisone in mexico: prednisone 10 tablet – cost of prednisone 10mg tablets
lisinopril buy in canada
prednisone 50 mg
buy doxycycline cheap doxycycline 100mg capsules doxylin
http://amoxila.pro/# ampicillin amoxicillin
lisinopril 25mg cost
neurontin 300 mg cap neurontin 150 mg neurontin brand name 800mg
https://doxycyclinea.online/# doxycycline order online
drug neurontin 20 mg: neurontin 900 mg – cheap neurontin online
valtrex generic price canada
cheap cialis 20mg australia
neurontin for sale: buy gabapentin online – buy gabapentin
where can you get amoxicillin where to get amoxicillin over the counter can you purchase amoxicillin online
zithromax purchase online: buy zithromax canada – zithromax prescription in canada
buy lisinopril 20 mg online
https://gabapentinneurontin.pro/# neurontin rx
where to get amoxicillin over the counter where can i buy amoxicillin online amoxicillin generic brand
synthroid uk
azithromycin 500 mg tablets
doxycycline mono: doxycycline hyclate – where can i get doxycycline
synthroid brand coupon
https://amoxila.pro/# amoxicillin 500 mg brand name
buy prednisone online no prescription: no prescription prednisone canadian pharmacy – buy prednisone from canada
buy prednisone without rx
can i buy zithromax over the counter: zithromax for sale 500 mg – can you buy zithromax over the counter in australia
amoxicillin discount coupon amoxicillin cost australia how to get amoxicillin over the counter
medical pharmacy south
http://prednisoned.online/# prednisone 60 mg daily
can i buy amoxicillin over the counter amoxicillin 500 mg cost amoxicillin price canada
zithromax for sale online: zithromax canadian pharmacy – can i buy zithromax over the counter in canada
http://amoxila.pro/# amoxicillin 500mg capsule buy online
lisinopril online purchase
lisinopril 5 mg uk price
buy metformin online nz
price of azithromycin tablets
cialis low price
doxycycline tablets: doxycycline 50mg – purchase doxycycline online
buy generic tadalafil
medicine neurontin gabapentin generic cost of neurontin 600mg
buy valtrex cheap online
zithromax capsules australia: zithromax capsules – zithromax prescription online
https://amoxila.pro/# amoxicillin 200 mg tablet
prednisone for sale online prednisone for dogs prednisone over the counter
http://gabapentinneurontin.pro/# cost of neurontin 800 mg
rx pharmacy online 24
can you buy metformin over the counter in usa
neurontin tablets 300 mg: neurontin india – neurontin 1800 mg
prednisone 1 mg daily
amoxicillin 500 coupon: order amoxicillin online uk – order amoxicillin uk
azithromycin medicine price
zithromax without prescription: zithromax 500mg price – buy zithromax online fast shipping
doxycycline 100mg capsules doxycycline 150 mg doxylin
online pharmacy ordering
doxycycline prices doxycycline 150 mg buy doxycycline online uk
http://gabapentinneurontin.pro/# buy neurontin uk
prednisone 30 mg tablet: prednisone pills 10 mg – buy prednisone 10mg online
india pharmacy online tadalafil
metformin tablets 500mg
http://amoxila.pro/# amoxicillin no prescription
valtrex online no prescription
buy prednisone 1 mg mexico
glucophage 500mg
10 mg tadalafil tablets
zithromax 500mg over the counter: where can i get zithromax – zithromax for sale us
synthroid 75 mg
where to buy prednisone without prescription prednisone 20 buy prednisone 10 mg
reliable online pharmacy
online generic cialis canada
neurontin 100 mg cap gabapentin 300mg how much is generic neurontin
can you buy metformin without a prescription
cheap azithromycin 500mg
http://zithromaxa.store/# zithromax canadian pharmacy
prednisone price australia: where can i buy prednisone – prednisone 2.5 mg tab
http://amoxila.pro/# where can i get amoxicillin 500 mg
can i order lisinopril online
buy zithromax 500mg online: buy zithromax canada – where to get zithromax over the counter
generic tadalafil in us
buy prednisone 10mg: buy prednisone 10 mg – prednisone uk buy
online pharmacy fungal nail
zestril 30 mg
price of metformin 850 mg
prinivil 25mg
happy family drugstore
mexican online pharmacies prescription drugs: п»їbest mexican online pharmacies – best online pharmacies in mexico
https://mexicanpharmacy1st.com/# mexican online pharmacies prescription drugs
https://mexicanpharmacy1st.shop/# reputable mexican pharmacies online
mexico pharmacy mexican pharmaceuticals online п»їbest mexican online pharmacies
https://mexicanpharmacy1st.shop/# mexican border pharmacies shipping to usa
buying prescription drugs in mexico online: mexican pharmacy – mexico drug stores pharmacies
synthroid tabs
mexican online pharmacies prescription drugs mexican rx online п»їbest mexican online pharmacies
п»їbest mexican online pharmacies: mexican mail order pharmacies – п»їbest mexican online pharmacies
lisinopril price 10 mg
best online pharmacies in mexico: purple pharmacy mexico price list – mexican pharmaceuticals online
20 mg prednisone generic
mexican drugstore online: mexican border pharmacies shipping to usa – mexican drugstore online
http://mexicanpharmacy1st.com/# mexico pharmacy
metformin 397
mexican rx online mexico drug stores pharmacies reputable mexican pharmacies online
https://mexicanpharmacy1st.shop/# mexican pharmacy
lisinopril 20 mg generic
synthroid 175
mexican rx online: mexico pharmacy – mexico drug stores pharmacies
zestril lisinopril
mexican pharmacy medicine in mexico pharmacies buying prescription drugs in mexico online
https://mexicanpharmacy1st.com/# best online pharmacies in mexico
purple pharmacy mexico price list pharmacies in mexico that ship to usa buying from online mexican pharmacy
http://mexicanpharmacy1st.com/# buying prescription drugs in mexico
mexican online pharmacies prescription drugs: medicine in mexico pharmacies – mexico pharmacy
mexico pharmacies prescription drugs buying prescription drugs in mexico online mexico pharmacy
lisinopril 10 mg for sale
synthroid thyroid
buying from online mexican pharmacy: pharmacies in mexico that ship to usa – п»їbest mexican online pharmacies
zithromax discount
https://mexicanpharmacy1st.shop/# mexico pharmacy
best online pharmacies in mexico: mexican pharmacy – buying prescription drugs in mexico online
can i buy valtrex over the counter
pharmacy coupons
indian trail pharmacy
https://mexicanpharmacy1st.shop/# buying prescription drugs in mexico online
mexican online pharmacies prescription drugs purple pharmacy mexico price list mexican pharmaceuticals online
best price for synthroid 137 mcg
mexican pharmaceuticals online: mexican drugstore online – mexican pharmaceuticals online
pharmacies in mexico that ship to usa mexico drug stores pharmacies best online pharmacies in mexico
cialis 20 mg price
buy tadalafil europe
mexico drug stores pharmacies: mexico drug stores pharmacies – mexican pharmacy
http://mexicanpharmacy1st.com/# reputable mexican pharmacies online
prednisone 10 mg daily
https://mexicanpharmacy1st.shop/# medicine in mexico pharmacies
mexican drugstore online buying prescription drugs in mexico reputable mexican pharmacies online
п»їbest mexican online pharmacies: mexican drugstore online – mexican border pharmacies shipping to usa
mexico pharmacies prescription drugs: mexican online pharmacies prescription drugs – best mexican online pharmacies
mexican online pharmacies prescription drugs mexico drug stores pharmacies п»їbest mexican online pharmacies
synthroid 0.025 mg
valtrex rx coupon
mexico pharmacies prescription drugs: mexican drugstore online – mexican pharmacy
hq pharmacy online 365
mexican mail order pharmacies: mexico drug stores pharmacies – buying prescription drugs in mexico
http://mexicanpharmacy1st.com/# mexican rx online
tadalafil 100 mg uk
http://mexicanpharmacy1st.com/# mexico pharmacy
mexico drug stores pharmacies: mexico pharmacy – best mexican online pharmacies
mexico pharmacy mexico drug stores pharmacies buying prescription drugs in mexico online
https://mexicanpharmacy1st.com/# medicine in mexico pharmacies
zithromax capsules
mexican pharmaceuticals online pharmacies in mexico that ship to usa п»їbest mexican online pharmacies
pharmacy coupons
mexico pharmacies prescription drugs: best mexican online pharmacies – best mexican online pharmacies
https://mexicanpharmacy1st.com/# pharmacies in mexico that ship to usa
https://mexicanpharmacy1st.shop/# pharmacies in mexico that ship to usa
lisinopril discount
mexican rx online: mexican drugstore online – mexico drug stores pharmacies
best online pharmacies in mexico mexico pharmacies prescription drugs mexico drug stores pharmacies
can you purchase zithromax
mexico pharmacies prescription drugs: mexican rx online – pharmacies in mexico that ship to usa
lisinopril mexico
generic drug for lisinopril
metformin 1mg
trustworthy online pharmacy
http://mexicanpharmacy1st.com/# mexican pharmaceuticals online
lisinopril 10 mg tablet cost
https://mexicanpharmacy1st.online/# mexico pharmacy
mexico pharmacy: buying prescription drugs in mexico online – mexican drugstore online
medicine in mexico pharmacies mexican mail order pharmacies buying prescription drugs in mexico
what’s the best online pharmacy
buying prednisone on line
purple pharmacy mexico price list: buying from online mexican pharmacy – reputable mexican pharmacies online
buy tadalafil cialis
prednisone 10 mg price in india
http://mexicanpharmacy1st.com/# buying from online mexican pharmacy
synthroid 88 mcg in india
buying from online mexican pharmacy: mexican pharmaceuticals online – mexican rx online
https://mexicanpharmacy1st.com/# mexican pharmacy
mexican mail order pharmacies: medicine in mexico pharmacies – mexican drugstore online
cialis india
mexico drug stores pharmacies mexican rx online buying prescription drugs in mexico online
best online pharmacies in mexico mexico drug stores pharmacies mexican pharmaceuticals online
synthroid 0.125 mg
best online pet pharmacy
http://mexicanpharmacy1st.com/# pharmacies in mexico that ship to usa
metformin 1000 tab
price for 5mg cialis
purchase cialis from canada
prednisone pill cost
propecia sale: get generic propecia – buy cheap propecia no prescription
lisinopril
http://propeciaf.online/# generic propecia
can i purchase cheap clomid without a prescription cost clomid without a prescription order clomid tablets
can you buy metformin over the counter uk
buy lisinopril online: lisinopril cheap price – zestril cost
buy cytotec online purchase cytotec buy cytotec
generic tadalafil from uk
http://lisinopril.club/# medication lisinopril 5 mg
dexona medicine
https://propeciaf.online/# cost of propecia without a prescription
how to get clomid pills where can i buy generic clomid without dr prescription how to get cheap clomid
neurontin 4000 mg: neurontin 400 – neurontin online pharmacy
http://gabapentin.club/# neurontin 300 mg buy
how to buy clomid for sale: can i purchase cheap clomid – can i purchase cheap clomid no prescription
accutane purchase online uk
albuterol 0.83
https://lisinopril.club/# buying lisinopril in mexico
zithromax buying
where to buy cheap clomid without prescription where to buy generic clomid buy cheap clomid price
neurontin oral: neurontin 800 mg – generic neurontin pill
how to get generic clomid without insurance: cheap clomid without a prescription – where to buy generic clomid pills
strattera generic
lioresal 10 mg price
propecia canadian pharmacy
http://cytotec.xyz/# Misoprostol 200 mg buy online
neurontin 150 mg: neurontin canada – neurontin 100mg cost
how to buy clomid no prescription: order clomid without a prescription – order cheap clomid without dr prescription
neurontin 900 mg cost of neurontin 600 mg gabapentin buy
Cytotec 200mcg price: buy cytotec – order cytotec online
cost cheap propecia without insurance buy cheap propecia pills order propecia without dr prescription
how to order doxycycline
http://lisinopril.club/# lisinopril 10 mg canada cost
buy ventolin no prescription
acyclovir cream buy online uk
where can i buy vermox over the counter
http://lisinopril.club/# lisinopril 5mg pill
buy lisinopril uk lisinopril 2.5 cost lisinopril 20 mg tab price
cost of cheap propecia: cost generic propecia – get propecia without a prescription
https://clomiphene.shop/# how to buy clomid without dr prescription
cost of propecia no prescription: cost generic propecia without dr prescription – buy propecia prices
purchase cytotec buy cytotec pills online cheap cytotec pills buy online
http://clomiphene.shop/# clomid buy
baclofen 5 mg brand name
zithromax otc
modafinil price australia
accutane price usa
baclofen cream cost
https://lisinopril.club/# medication lisinopril 5 mg
diflucan cost
retin a without rx
prinivil 20 mg tablet lisinopril 25 mg tablet lisinopril hctz
get cheap clomid no prescription: get cheap clomid pills – where to buy cheap clomid tablets
cost of generic propecia without insurance: get cheap propecia – propecia for sale
zestoretic 10 12.5 mg cost of lisinopril 20 mg lisinopril online
http://cytotec.xyz/# buy cytotec in usa
azithromycin how to get
azithromycin mexico pharmacy
advair drug
https://cytotec.xyz/# cytotec pills online
can i buy retin a over the counter in uk
where to buy neurontin neurontin 600mg gabapentin
where to purchase zithromax
can i buy cheap clomid online: how to buy clomid without a prescription – buying generic clomid price
lisinopril lisinopril 60 mg daily buy lisinopril no prescription
buy cytotec online: buy cytotec pills – cytotec buy online usa
https://gabapentin.club/# brand neurontin 100 mg canada
can you buy synthroid in mexico
tamoxifen 10 mg price in india
lasix 2 mg
zithromax 250mg tablets
accutane 40mg
https://clomiphene.shop/# where to buy cheap clomid online
where can i get generic clomid without prescription where to buy cheap clomid without rx where can i buy clomid without prescription
diflucan 100mg
40 mg lisinopril for sale: lisinopril medication – lisinopril 2.5 mg coupon
where to buy generic clomid without rx order cheap clomid without dr prescription where can i get cheap clomid no prescription
ordering lisinopril without a prescription: lisinopril 240 – cost for 40 mg lisinopril
diflucan 150 mg price in india
buy provigil 200 mg
buy zithromax usa
neurontin 100 mg neurontin 50mg cost order neurontin online
medication lisinopril 10 mg lisinopril 20 mg mexico lisinopril cheap brand
cost of generic propecia without prescription: buy propecia now – cost propecia online
best price for synthroid 75 mcg
azithromycin over the counter price
cytotec pills buy online: buy cytotec – Misoprostol 200 mg buy online
dexamethasone price
modafinil where to get
cipro 250mg
where can i get doxycycline over the counter
provigil in mexico
where to buy tretinoin cream over the counter
effexor australia
tretinoin 0.1 cream 30g
certified canadian pharmacy: cheapest canada – onlinepharmaciescanada com
https://cheapestcanada.shop/# best canadian pharmacy to order from
http://cheapestindia.com/# reputable indian pharmacies
amoxicillin 2263
https://cheapestandfast.shop/# pharmacies without prescriptions
zithromax 250 mg cost
buying from online mexican pharmacy п»їbest mexican online pharmacies mexican pharmacy
advair 125 25 mcg
where to buy diflucan
lasix 40 mg without prescription
flomax cost comparison
how to get tamoxifen
where to buy doxycycline
https://cheapestindia.com/# legitimate online pharmacies india
tretinoin otc us
http://cheapestandfast.com/# medications online without prescription
online pharmacies no prescription usa cheapest and fast canada pharmacy no prescription
diflucan 100
http://cheapestcanada.com/# reputable canadian online pharmacy
lasix 500
https://36and6health.com/# foreign pharmacy no prescription
https://cheapestindia.shop/# india pharmacy
online rx diflucan
http://cheapestandfast.com/# cheap prescription drugs online
buy vermox canada
best online pharmacies without prescription: cheapest and fast – no prescription needed online pharmacy
https://cheapestcanada.com/# northern pharmacy canada
lyrica capsules 75 mg cost
https://cheapestindia.com/# india online pharmacy
https://cheapestindia.com/# buy prescription drugs from india
buying online prescription drugs cheapest and fast no prescription drugs online
http://36and6health.com/# prescription drugs online
doxycycline 100mg for sale
doxycycline with out a rx
https://cheapestcanada.com/# thecanadianpharmacy
best price for advair
antibiotic zithromax
vermox tablets nz
acyclovir 400mg tab
cost of tamoxifen in singapore
http://cheapestandfast.com/# buy prescription drugs on line
https://cheapestmexico.shop/# purple pharmacy mexico price list
mebendazole tablets
furosemide 80 mg tablet
http://cheapestindia.com/# indian pharmacy paypal
rx pharmacy coupons: cheapest pharmacy – canadian pharmacy no prescription needed
how much is valtrex tablets
diflucan pharmacy
http://cheapestmexico.com/# medication from mexico pharmacy
furosemide online uk
valtrex generic in mexico
lyrica 25
https://cheapestcanada.shop/# canadian pharmacy world reviews
augmentin 375 mg tablet
buying prescription medicine online cheapest & fast pharmacy no prescription canadian pharmacies
https://cheapestindia.shop/# world pharmacy india
where to get propecia uk
amoxil 250 price
diflucan online purchase uk
625mg amoxicillin
https://cheapestcanada.shop/# drugs from canada
flomax purchase
diflucan 200 mg cost
vermox tablets buy online
https://euapothekeohnerezept.shop/# online apotheke gГјnstig
online apotheke online apotheke gГјnstig medikamente rezeptfrei
furosemide 3169
top farmacia online: comprare farmaci online all’estero – comprare farmaci online all’estero
günstige online apotheke: online apotheke versandkostenfrei – ohne rezept apotheke
diflucan online uk
where can i buy tamoxifen online
where to get provigil online
pharmacie en ligne france livraison internationale: pharmacie en ligne livraison europe – п»їpharmacie en ligne france
vermox tablets nz
https://eufarmacieonline.com/# comprare farmaci online con ricetta
eu apotheke ohne rezept: günstige online apotheke – günstigste online apotheke
п»їpharmacie en ligne france: Pharmacie en ligne livraison Europe – vente de mГ©dicament en ligne
toradol for back pain
150 mg clomid
comprare farmaci online con ricetta Farmacia online piГ№ conveniente farmacie online affidabili
farmaci senza ricetta elenco: farmacie online autorizzate elenco – Farmacia online piГ№ conveniente
farmacie online affidabili: Farmacie online sicure – Farmacia online piГ№ conveniente
farmacias online seguras en espa̱a: farmacias online seguras en espa̱a Рfarmacias online seguras en espa̱a
farmacia online barata y fiable farmacia online 24 horas farmacia online envГo gratis
pharmacie en ligne sans ordonnance: pharmacie en ligne avec ordonnance – Pharmacie Internationale en ligne
lasix rx
Farmacia online miglior prezzo: farmacia online – farmacie online affidabili
azithromycin over the counter nz
modafinil mexico price
pharmacie en ligne france livraison internationale pharmacie en ligne france pas cher pharmacie en ligne fiable
farmacia online madrid: farmacia online 24 horas – farmacia online madrid
farmacia online barata farmacia online barcelona farmacia online envГo gratis
eu apotheke ohne rezept: online apotheke deutschland – internet apotheke
pharmacie en ligne france fiable: pharmacie en ligne – Pharmacie en ligne livraison Europe
azithromycin 1000 for sale
günstigste online apotheke: medikament ohne rezept notfall – online apotheke günstig
modafinil 200 mg price india
azithromycin 500mg for sale
generic for strattera
vente de mГ©dicament en ligne Achat mГ©dicament en ligne fiable pharmacie en ligne france livraison belgique
azithromycin online canada
Farmacia online più conveniente: farmacie online sicure – farmacia online
ciprofloxacin cream
farmacia online piГ№ conveniente Farmacie online sicure Farmacie on line spedizione gratuita
azithromycin 40 mg
comprare farmaci online con ricetta: Farmacie online sicure – comprare farmaci online all’estero
nolvadex 40mg price in india
vardenafil 40 mg
Farmacia online più conveniente: farmacie online autorizzate elenco – farmacia online
best price generic propecia
vardenafil tablets 20mg
farmacia online senza ricetta farmacie online sicure farmacie online sicure
farmacie online autorizzate elenco: Farmacia online miglior prezzo – acquisto farmaci con ricetta
pharmacie en ligne Pharmacie en ligne livraison Europe pharmacie en ligne livraison europe
price of lasix 80 mg
pharmacie en ligne sans ordonnance: trouver un mГ©dicament en pharmacie – acheter mГ©dicament en ligne sans ordonnance
eu apotheke ohne rezept: beste online-apotheke ohne rezept – beste online-apotheke ohne rezept
migliori farmacie online 2024: Farmacie on line spedizione gratuita – Farmacia online miglior prezzo
farmacia online senza ricetta: farmacia online piГ№ conveniente – farmacie online autorizzate elenco
baclofen 10 mg tablets
farmacie online sicure: migliori farmacie online 2024 – farmacie online autorizzate elenco
nolvadex pharmacy
http://eufarmacieonline.com/# top farmacia online
purchase accutane with paypal
azithromycin 1g buy online
farmacia online 24 horas: farmacias online seguras en espa̱a Рfarmacia online 24 horas
Pharmacie en ligne livraison Europe trouver un mГ©dicament en pharmacie pharmacie en ligne fiable
doxycycline 20mg canada
propecia australia cost
farmacia en casa online descuento farmacia en casa online descuento farmacia online madrid
gГјnstigste online apotheke: п»їshop apotheke gutschein – apotheke online
migliori farmacie online 2024: farmacia online piГ№ conveniente – Farmacie on line spedizione gratuita
acheter mГ©dicament en ligne sans ordonnance: vente de mГ©dicament en ligne – pharmacie en ligne france livraison belgique
farmacie online autorizzate elenco: comprare farmaci online con ricetta – acquisto farmaci con ricetta
amoxicillin 4
generic tadalafil 2018
farmacia online 24 horas: farmacias online baratas – farmacia online 24 horas
farmacia online 24 horas farmacia online madrid farmacia online barcelona
п»їFarmacia online migliore п»їFarmacia online migliore farmacia online piГ№ conveniente
buy ventolin without prescription
tadacip india price
farmacias direct: farmacia online barcelona – farmacia online envГo gratis
acquistare farmaci senza ricetta: farmaci senza ricetta elenco – farmacia online
can i buy azithromycin over the counter in us
azithromycin 100mg price
acquisto farmaci con ricetta: comprare farmaci online con ricetta – farmacie online sicure
order vermox online
lasix over the counter 20mg
farmacias online seguras: farmacia online españa – farmacias online seguras
tretinoin cream generic cost
farmacia online barcelona: farmacia online madrid – farmacias direct
pharmacie en ligne france fiable pharmacie en ligne pas cher pharmacie en ligne pas cher
vermox tablets buy online
pharmacie en ligne france fiable pharmacie en ligne acheter mГ©dicament en ligne sans ordonnance
farmacia online senza ricetta: comprare farmaci online all’estero – comprare farmaci online all’estero
comprare farmaci online all’estero: top farmacia online – Farmacie online sicure
acquistare farmaci senza ricetta: top farmacia online – comprare farmaci online all’estero
farmacias online baratas: farmacia online barcelona – farmacia online barata
farmacia online españa envÃo internacional: farmacia online barata y fiable – farmacia online españa envÃo internacional
vermox tab 100 mg
Farmacia online miglior prezzo comprare farmaci online con ricetta comprare farmaci online con ricetta
internet apotheke online apotheke rezept eu apotheke ohne rezept
trouver un mГ©dicament en pharmacie: pharmacies en ligne certifiГ©es – pharmacie en ligne avec ordonnance
Farmacia online migliore: Farmacia online miglior prezzo – Farmacie online sicure
accutane by mail
purchase propecia
flomax for kidney stones in females
gГјnstigste online apotheke: internet apotheke – online apotheke deutschland
flomax without a script
farmacia online españa: farmacias online seguras en españa – farmacias online baratas
farmacia online barata y fiable farmacia online madrid farmacias online seguras
pharmacie en ligne france livraison belgique: Pharmacie en ligne livraison Europe – acheter mГ©dicament en ligne sans ordonnance
farmacias online seguras farmacia online barcelona farmacia online envГo gratis
canadian viagra paypal
baclofen australia
generic for cipro
trouver un mГ©dicament en pharmacie: kamagra en ligne – acheter mГ©dicament en ligne sans ordonnance
п»їpharmacie en ligne france: pharmacie en ligne sans ordonnance – pharmacie en ligne france fiable
Viagra pas cher paris: SildГ©nafil 100mg pharmacie en ligne – Viagra sans ordonnance livraison 48h
trouver un mГ©dicament en pharmacie Pharmacies en ligne certifiees pharmacie en ligne fiable
pharmacie en ligne livraison europe: levitra en ligne – pharmacie en ligne france livraison internationale
https://phenligne.shop/# pharmacie en ligne sans ordonnance
synthroid brand price
azithromycin 500 mg tablets
generic tamoxifen 20 mg
zovirax cream over the counter usa
Viagra homme sans ordonnance belgique: Meilleur Viagra sans ordonnance 24h – Viagra sans ordonnance 24h Amazon
trouver un mГ©dicament en pharmacie Levitra acheter п»їpharmacie en ligne france
baclofen 0.01
п»їpharmacie en ligne france: acheter kamagra site fiable – acheter mГ©dicament en ligne sans ordonnance
buy clomid on line
pharmacie en ligne pas cher: pharmacie en ligne fiable – pharmacies en ligne certifiГ©es
zithromax z pak
pharmacie en ligne livraison europe: Levitra sans ordonnance 24h – pharmacie en ligne pas cher
trouver un mГ©dicament en pharmacie: Levitra pharmacie en ligne – pharmacie en ligne fiable
augmentin 875 pill
vermox 500mg uk
acheter mГ©dicament en ligne sans ordonnance: Levitra sans ordonnance 24h – pharmacie en ligne fiable
pharmacie en ligne sans ordonnance: Acheter Cialis – pharmacie en ligne fiable
cipro 500mg best prices
pharmacie en ligne: acheter kamagra site fiable – pharmacie en ligne france livraison internationale
can i buy amoxicillin over the counter in australia
pharmacie en ligne france pas cher: Levitra pharmacie en ligne – Pharmacie Internationale en ligne
pharmacie en ligne france livraison belgique: kamagra en ligne – pharmacie en ligne fiable
acyclovir online order
lyrica 75 mg cost
augmentin 625 price india
pharmacie en ligne sans ordonnance Pharmacie Internationale en ligne Achat mГ©dicament en ligne fiable
http://kamagraenligne.com/# pharmacie en ligne france livraison internationale
acyclovir cream for sale online
trouver un mГ©dicament en pharmacie: pharmacie en ligne sans ordonnance – pharmacie en ligne france pas cher
accutane pill
azithromycin antibiotic
pharmacie en ligne france fiable: pharmacie en ligne pas cher – pharmacie en ligne france livraison belgique
buy lasix water pill
pharmacie en ligne france fiable: cialis prix – pharmacie en ligne livraison europe
advair 100 mg
lasix 25 mg
cost of accutane 2017
amoxicillin cost india
baclofen over the counter usa
how to get clomid over the counter
Viagra pas cher livraison rapide france: Meilleur Viagra sans ordonnance 24h – Le gГ©nГ©rique de Viagra
Hello.
This post was created with XRumer 23 StrongAI.
Good luck 🙂
Pharmacie sans ordonnance: pharmacie en ligne livraison europe – acheter mГ©dicament en ligne sans ordonnance
lasix 250 mg
strattera capsules
pharmacie en ligne france pas cher: kamagra livraison 24h – pharmacie en ligne pas cher
5mg propecia
diflucan 150 mg capsule
diflucan 200 mg capsule
canadian azithromycin
diflucan
Quand une femme prend du Viagra homme: viagra sans ordonnance – Viagra sans ordonnance 24h
https://phenligne.shop/# pharmacie en ligne france livraison internationale
metformin pills 500 mg
trouver un mГ©dicament en pharmacie: kamagra oral jelly – acheter mГ©dicament en ligne sans ordonnance
doxycycline drug
cost of albuterol
zithromax generic pharmacy
combivent respimat package insert
pharmacie en ligne france pas cher: Levitra sans ordonnance 24h – pharmacie en ligne livraison europe
Pharmacie sans ordonnance: Medicaments en ligne livres en 24h – pharmacie en ligne fiable
lasix 20 mg price in india
pharmacie en ligne fiable: Levitra 20mg prix en pharmacie – trouver un mГ©dicament en pharmacie
pharmacie en ligne france livraison internationale: cialis prix – pharmacie en ligne livraison europe
amoxacillian without a percription
prescription 0.1 tretinoin cream
where to buy amoxicillin online
Acheter Sildenafil 100mg sans ordonnance: Viagra sans ordonnance livraison 48h – Viagra 100 mg sans ordonnance
cheap furosemide
cost ciprofloxacin
buy azithromycin online australia
pharmacie en ligne france fiable: kamagra pas cher – pharmacie en ligne livraison europe
cheap tretinoin gel
propecia pharmacy prices
pharmacie en ligne avec ordonnance: cialis sans ordonnance – pharmacie en ligne france livraison internationale
Hello!
This post was created with XRumer 23 StrongAI.
Good luck 🙂
nolvadex for sale usa
clomid over the counter in south africa
propecia canada cost
acheter mГ©dicament en ligne sans ordonnance: Medicaments en ligne livres en 24h – pharmacie en ligne france pas cher
lasix cost
buy modafinil nz
can you buy baclofen over the counter uk
Viagra sans ordonnance 24h Amazon: Viagra sans ordonnance 24h – Viagra sans ordonnance 24h suisse
how to get advair cheap
https://kamagraenligne.com/# acheter médicament en ligne sans ordonnance
lyrica 75 mg coupon
albuterol 50mg tablet
advair rx
diflucan otc uk
Viagra sans ordonnance livraison 48h: Viagra sans ordonnance 24h – Viagra 100 mg sans ordonnance
п»їpharmacie en ligne france: pharmacie en ligne – pharmacie en ligne
baclofen 10 mg tabs
order accutane from india
lyrica uk
trouver un mГ©dicament en pharmacie: Levitra pharmacie en ligne – acheter mГ©dicament en ligne sans ordonnance
baclofen canada
amoxicillin 875mg 125mg
Achat mГ©dicament en ligne fiable: kamagra en ligne – pharmacie en ligne livraison europe
bactrim ds 800-160
pharmacie en ligne: acheter kamagra site fiable – acheter mГ©dicament en ligne sans ordonnance
how to buy zithromax
baclofen canada
flomax 4mg price
pharmacie en ligne france pas cher: cialis sans ordonnance – trouver un mГ©dicament en pharmacie
pharmacie en ligne france livraison belgique: Levitra pharmacie en ligne – pharmacie en ligne livraison europe
buy generic acyclovir cream online
cipro buy online
baclofen no preciption
augmentin es 600
accutane online canada pharmacy
Pharmacie Internationale en ligne: Cialis sans ordonnance 24h – trouver un mГ©dicament en pharmacie
generic accutane online
10mg baclofen
pharmacie en ligne livraison europe: Achat mГ©dicament en ligne fiable – trouver un mГ©dicament en pharmacie
tamoxifen 20 mg tablet 1mg
lasix online no prescription
glucophage for sale
pharmacie en ligne france pas cher: levitra generique sites surs – acheter mГ©dicament en ligne sans ordonnance
zithromax 2 pills
effexor venlafaxine
pharmacie en ligne france livraison internationale: Levitra pharmacie en ligne – pharmacies en ligne certifiГ©es
effexor from canada
accutane india pharmacy
baclofen tab 20mg
Sildenafil teva 100 mg sans ordonnance: viagra en ligne – Viagra pas cher livraison rapide france
azithromycin 500mg coupon
baclofen online
Sildenafil teva 100 mg sans ordonnance: viagra sans ordonnance – Sildenafil teva 100 mg sans ordonnance
how to buy modafinil in usa
Pharmacie en ligne livraison Europe: kamagra 100mg prix – vente de mГ©dicament en ligne
advair medicine generic
how to get retin a online without a prescription
clomid discount coupon
pharmacie en ligne fiable: levitra generique sites surs – pharmacies en ligne certifiГ©es
Pharmacie Internationale en ligne: levitra generique sites surs – pharmacie en ligne pas cher
amoxicillin where to get
buy accutane 20mg
where can you get doxycycline
vente de mГ©dicament en ligne: kamagra en ligne – pharmacie en ligne sans ordonnance
purchase accutane
п»їpharmacie en ligne france: Acheter Cialis – pharmacie en ligne
pharmacies en ligne certifiГ©es: pharmacie en ligne france livraison internationale – pharmacie en ligne livraison europe
pharmacie en ligne france fiable: Acheter Cialis – Achat mГ©dicament en ligne fiable
how much is generic flomax
vermox mexico
buy ventolin without prescription
Pharmacie sans ordonnance: acheter kamagra site fiable – vente de mГ©dicament en ligne
Achat mГ©dicament en ligne fiable: Levitra sans ordonnance 24h – pharmacie en ligne france livraison internationale
6 baclofen
SildГ©nafil Teva 100 mg acheter: viagra sans ordonnance – Viagra sans ordonnance 24h Amazon
generic for lasix
5 mg nolvadex
modafinil purchase usa
pharmacie en ligne france pas cher: kamagra oral jelly – trouver un mГ©dicament en pharmacie
albuterol medicine
augmentin 500 mg
diflucan 150 mg caps
pharmacie en ligne france livraison internationale: Cialis sans ordonnance 24h – pharmacie en ligne sans ordonnance
india cialis
baclofen 100mg
trouver un mГ©dicament en pharmacie: Acheter Cialis – pharmacie en ligne france fiable
doxycycline 50mg tab
furosemide best price
accutane from canada
buy modafinil pills
trouver un mГ©dicament en pharmacie: kamagra pas cher – Achat mГ©dicament en ligne fiable
where can i buy nolvadex in australia
Achat mГ©dicament en ligne fiable: Levitra sans ordonnance 24h – Pharmacie Internationale en ligne
trouver un mГ©dicament en pharmacie: kamagra gel – pharmacie en ligne france fiable
prednisone pills
vermox 500mg tablet
generic of flomax
vermox sale
Pharmacie Internationale en ligne: kamagra en ligne – pharmacies en ligne certifiГ©es
azithromycin 500 mg tablet buy online
pharmacie en ligne livraison europe: kamagra oral jelly – acheter mГ©dicament en ligne sans ordonnance
how to get propecia uk
cheap acyclovir online
buy accutane pills online
Achat mГ©dicament en ligne fiable: acheter kamagra site fiable – Pharmacie sans ordonnance
cheap tretinoin
price of vermox south africa
azithromycin pills
azithromycin 1000
Viagra homme prix en pharmacie sans ordonnance: Viagra sans ordonnance 24h – Viagra prix pharmacie paris
ventolin proventil
pharmacie en ligne fiable: acheter kamagra site fiable – acheter mГ©dicament en ligne sans ordonnance
azithromycin 500 mg tablet
5 mg prednisone tablets
prednisone nz
pharmacie en ligne: Levitra 20mg prix en pharmacie – pharmacie en ligne fiable
Pharmacie sans ordonnance: kamagra oral jelly – pharmacie en ligne avec ordonnance
lasix tablet price in india
pharmacie en ligne france livraison internationale: kamagra en ligne – pharmacies en ligne certifiГ©es
doxycycline 100mg for sale
п»їpharmacie en ligne france: kamagra 100mg prix – п»їpharmacie en ligne france
tretinoin 0.1 cream 30mg
zithromax 600 mg tablets
dexamethasone for sale
provigil 100
cost of generic zithromax
п»їpharmacie en ligne france: levitra en ligne – pharmacies en ligne certifiГ©es
Pharmacie Internationale en ligne: pharmacie en ligne pas cher – Pharmacie en ligne livraison Europe
acheter mГ©dicament en ligne sans ordonnance: Cialis sans ordonnance 24h – Pharmacie sans ordonnance
ventolin uk pharmacy
order cheap diflucan online
generic retin-a micro
cheapest propecia prices
augmentin 625 mg buy online
pharmacie en ligne france livraison belgique: Levitra pharmacie en ligne – п»їpharmacie en ligne france
pharmacies en ligne certifiГ©es: pharmacie en ligne – Pharmacie en ligne livraison Europe
pharmacie en ligne france livraison internationale: cialis generique – Pharmacie Internationale en ligne
lyrica 75 mg cost
Pharmacie Internationale en ligne: kamagra 100mg prix – pharmacie en ligne fiable
pharmacie en ligne france livraison internationale: levitra en ligne – vente de mГ©dicament en ligne
п»їpharmacie en ligne france: cialis sans ordonnance – pharmacie en ligne france fiable
can i order valtrex online
diflucan tablets
buy doxycycline 100mg pills
Viagra pas cher inde: Viagra sans ordonnance 24h – Viagra sans ordonnance livraison 48h
lyrica 30 mg
can you buy doxycycline over the counter
acheter mГ©dicament en ligne sans ordonnance: kamagra livraison 24h – pharmacie en ligne pas cher
where to get clomid online
https://viaenligne.com/# Quand une femme prend du Viagra homme
how much is modafinil
pharmacie en ligne fiable: kamagra oral jelly – pharmacie en ligne pas cher
pharmacie en ligne fiable: Levitra pharmacie en ligne – pharmacie en ligne sans ordonnance
pharmacies en ligne certifiГ©es: Cialis sans ordonnance 24h – pharmacie en ligne sans ordonnance
lyrica 25mg capsule
lyrica generic south africa
flomax price south africa
effexor
provigil how to get
trouver un mГ©dicament en pharmacie: levitra generique – pharmacie en ligne france pas cher
canadian pharmacy modafinil
п»їpharmacie en ligne france: pharmacie en ligne pas cher – pharmacie en ligne avec ordonnance
get valtrex online
azithromycin 500g
acheter mГ©dicament en ligne sans ordonnance: Acheter Cialis – pharmacie en ligne livraison europe
pharmacie en ligne france pas cher: acheter mГ©dicament en ligne sans ordonnance – acheter mГ©dicament en ligne sans ordonnance
nolvadex 20 mg
pharmacie en ligne fiable: Levitra sans ordonnance 24h – pharmacie en ligne france livraison belgique
pharmacie en ligne france fiable: levitra generique – pharmacies en ligne certifiГ©es
pharmacie en ligne sans ordonnance: pharmacie en ligne – pharmacie en ligne
pharmacie en ligne avec ordonnance: Acheter Cialis 20 mg pas cher – pharmacies en ligne certifiГ©es
acheter mГ©dicament en ligne sans ordonnance: cialis prix – pharmacie en ligne france pas cher
п»їpharmacie en ligne france: pharmacie en ligne france pas cher – vente de mГ©dicament en ligne
Viagra Pfizer sans ordonnance: Acheter du Viagra sans ordonnance – Viagra homme prix en pharmacie sans ordonnance
furosemide 40mg tab
vermox 500 mg tablet
vente de mГ©dicament en ligne: kamagra gel – pharmacie en ligne pas cher
pharmacie en ligne livraison europe: kamagra gel – Achat mГ©dicament en ligne fiable
trouver un mГ©dicament en pharmacie: Levitra acheter – pharmacie en ligne france pas cher
diflucan online purchase uk
how much is acyclovir 800 mg
furosemide\purchase
accutane 10mg
buy generic accutane online cheap
buy effexor
albuterol 83
order generic propecia
azithromycin capsules 500mg
can you buy propecia online
xnxx
dexamethasone price
lyrica 75 mg
rx amoxicillin
advair online
zovirax prescription
no prescription ventolin hfa
modafinil for sale in us
baclofen comparison price
where can you buy toradol
lyrica cheapest price
baclofen 30 mg cream
provigil in mexico
how to buy provigil online
toradol migraine
how to get accutane prescription
prescription for amoxicillin: amoxicillin – where can i buy amoxicillin online
amoxicillin script
https://azithromycinca.shop/# doxycycline online no prescription
cost of generic doxycycline
flomax nasal congestion
clomid generic south africa
where to get retin a cream
tretinoin cream for sale online
synthroid 5 mcg
?Onlayn Kazino: Pin Up Kazino ?Onlayn – Pin Up Azerbaycan
Pin up 306 casino: Pin-Up Casino – Pin-up Giris
https://autolux-azerbaijan.com/# Pin-up Giris
Pin Up Azerbaycan ?Onlayn Kazino: Pin up 306 casino – Pin Up Kazino ?Onlayn
how to get flomax
pin-up 141 casino: pin-up360 – pin-up kazino
Pin Up Azerbaycan: Pin Up Azerbaycan ?Onlayn Kazino – Pin Up Kazino ?Onlayn
Pin Up Kazino ?Onlayn: ?Onlayn Kazino – pin-up360
https://autolux-azerbaijan.com/# pin-up360
Pin up 306 casino: Pin up 306 casino – Pin Up
pin-up kazino: Pin Up Azerbaycan ?Onlayn Kazino – pin-up 141 casino
https://autolux-azerbaijan.com/# pin-up 141 casino
Pin Up: Pin Up Azerbaycan – Pin-Up Casino
pin-up 141 casino: pin-up360 – Pin Up Azerbaycan
pin-up 141 casino: pin-up kazino – Pin up 306 casino
tretinoin 0.018
ciprofloxacin over the counter usa
medication lasix 20 mg
sildalis
dexamethasone 2.5 mg
can you buy clomid over the counter in canada
best price for doxycycline 100 mg without prescription
how much is toradol
price of synthroid
cost of generic lyrica
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
clomid price canada
mexico pharmacies prescription drugs: online mexican pharmacy – mexico drug stores pharmacies
mexico pharmacies prescription drugs
https://cmqpharma.com/# п»їbest mexican online pharmacies
mexican rx online
sildalis 100mg 20mg
where to buy viagra online australia
order advair online
mexico pharmacies prescription drugs: mexican online pharmacy – mexico drug stores pharmacies
buy lyrica 300 mg online uk
reputable mexican pharmacies online
https://cmqpharma.online/# best online pharmacies in mexico
mexican pharmaceuticals online
buy accutane online singapore
price viagra uk
lioresal cost
lyrica uk
price of 21 acyclovir 400mg tablets
advair diskus 25050
accutane costs canada
buy generic accutane online cheap
where to get modafinil canada
buy tadacip in india
baclofen 832
zovirax over the counter pills