LETTER TO EDITOR
Year: 2020 • Volume: 3 • Issue: 1 • Page: 12-13
A CASE OF PITYRIASIS LICHENOIDES ET VARIOLIFORMIS ACUTA (PLEVA) LASTING FOR 22 YEARS-A SUBACUTE VARIANT?
Preema Sinha1, Siddharth Bhatt1, Deepti Mutreja1, Sunmeet Sandhu1 1
Department of Dermatology, Armed Forces Medical College, Pune-40
Corresponding Author:
Dr. Preema Sinha
Prof, Department of Dermatology, Armed Forces Medical College, Pune- 411040
E-mail – drpreemasinha@gmail.com
How to cite this article:
Sinha P, Bhatt S, Mutreja D, Sandhu S. A case of Pityriasis lichenoides et varioliformis acuta (PLEVA) lasting for 22 years-a subacute variant? JDA Indian Journal of Clinical Dermatology 2020;3:12-13
Sir,
Pityriasis Lichenoides et Varioliformis acuta (PLEVA) is an acute variant of Pityriasis Lichenoides which encompasses a spectrum of clinical presentations ranging from rapidly progressing severe ulceronecrotic variant with systemic manifestations and a high mortality rate (Febrile ulceronecrotic Mucha Haberman Disease- FUMHD) to a more chronic manifestation consisting of benign-appearing scaly papules of Pityriasis Lichenoides Chronica (PLC).1
It is generally accepted that PLEVA and PLC represent two ends of a continuous spectrum, and therefore it is not uncommon to observe both acute and chronic lesions in the same patient, as well as lesions at intermediate stages between PLEVA and PLC. The maximum duration of PLEVA lasting in any person has been reported as long as 08 years.2 Herein we report a case where it lasted for nearly 22 years.
A 25-year-old female presented to our center with complaints of recurrent crops of red raised lesions over her body, occurring at a frequency of once a week and then resolving spontaneously over a period of 10 to 15 days since the age of three years. There was no history of any pain or itching over the lesions. No history of fever or malaise associated with the occurrence of lesions. There was no history of weight loss, evening rise of temperature or night sweats. The patient denied any similar lesions in family members.
General and systemic examination was essentially normal. Dermatological examination revealed the involvement of face, trunk, and lower limbs in the form of few discrete erythematous papules, few vesiculopustules, with some papules showing a central necrotic eschar or crust, measuring 0.5 cm – 2 cm in diameter [Figures 1 & 2]. Examination of mucosa, palms, and soles was within normal limits.

Figure 1 : Presence of few discrete erythematous papules, few with necrotic centre over the thigh
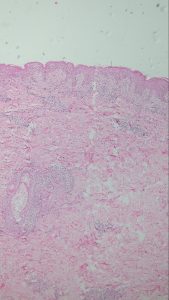
Figure2 : H&E(100x)- scanner view showing predominant interface dermatitis with vacuolar degeneration
and edematous papillary dermis
Relevant hematological and biochemical parameters were within normal limits.
Histopathology showed characteristic features of necrotic keratinocytes with extravasation of RBC’s into the epidermis. Papillary dermis was edematous and the capillaries were congested with RBCs. Superficial and the deep dermis showed endothelial swelling with foci of fibrinoid necrosis within the capillaries[Figure 3]. Perivascular chronic inflammatory infiltrates of lymphocytes was seen. Immunohistochemistry was positive for CD3+,CD7+and CD8+ and CD 30- [Figure 4]. Based on the above clinical, histopathological and immunohistochemistry a diagnosis of PLEVA was made.
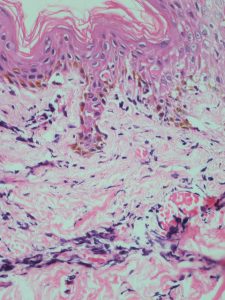
Figure 3 : H & E (200x)Necrotic keratinocytes with extravasation of RBCs into the epidermis with superficial and deep dermis showing endothelial swelling with foci of fibrinoid necrosis within the capillaries. Papillary dermis was edematous and capillaries were congested with RBCs.

Figure 4(a -f) : IHC (200x) showed positivity for CD3+, CD7+, CD8+ and negative for CD 30-
The patient has managed with Cap Doxycycline 100mg twice daily along with 0.1% mometasone cream applied twice daily with which she has shown an excellent response in the form of no new lesions and regression of older lesions.
PLEVA is a disease of young people and children with inflammatory and usually diffuse erythematous papules of rapid onset which evolve to form papules with a central punctum. The papule evolves to become vesicopustular, undergoes hemorrhagic necrosis and becomes ulcerated with overlying crusts. These lesions spontaneously heal to leave behind varioliform or smallpox-like scars and post- inflammatory hyperpigmentation and hypopigmentation. 1,2 Though the distribution of the lesions can be generalized, the trunk, flexors, and extremities are commonly involved.
The etiology of the disease still remains unknown though antibodies against Toxoplasma gondii, cytomegalovirus, parvovirus, adenovirus and Epstein Barr virus have been demonstrated in some studies. 1-3 T-cell dyscrasias and immune complex deposition have also been cited as probable causes in the literature.
The differential diagnosis for PLEVA includes lymphomatoid papulosis, arthropod bite reactions, varicella, Gianotti-Crosti syndrome, erythema multiforme, pityriasis rosea, guttate psoriasis, vasculitis, and secondary syphilis. Differentiation
between PLEVA and lymphamatoid papulosis is important as patients with lymphomatoid papulosis may develop systemic lymphoma. The presence of large CD30+ atypical lymphoid cells is the hallmark of lymphomatoid papulosis and clinically, the papules of lymphomatoid papulosis may develop into nodules, tumors, and large plaques.4
Cinical management of PLEVA is difficult due to exact pathology being unknown. Medications used till date include tetracycline, erythromycin, methotrexate, calciferol, chinoline and acridine derivatives, cyclosporine, intravenous gamma globulin, and retinoids.5 Systemic corticosteroids may have a role in severe cases of PLEVA. Topical corticosteroids and topical tacrolimus are helpful in symptomatic cases, but they do not alter the course of the disease. Despite a lack of randomized controlled trials, oral tetracycline and erythromycin have been prescribed most often in case series.
The existing literature outlines the mean duration of this rare disease to be 1.6 year with an episodic course, the frequency of which varies greatly from individual to individual.2 The longest duration mentioned in literature is 8 years. Our case highlights a case PLEVA with a disease duration of 22 years with a subacute course which till now is the longest reported duration for the disease in literature.
We present this case to stress upon this rare presentation of PLEVA which can exist for years without any systemic manifestations and resolves spontaneously leaving behind post inflammatory hyperpigmentation. To give it a new nomenclature as “Subacute PLEVA” would not be wrong.
Reference
- Khachemoune A, Blyumin Pityriasis lichenoides: pathophysiology, classification, and treatment Am J Clin Dermatol. 2007 ;8:29-36.
- Nair A clinical and histopathological study of pityriasis lichenoides. Indian J Dermatol Venereol Leprol. 2007;73:100.
- Zlatkov NB, Adreev Pityriasis lichenoides and toxoplasmosis. Br J Dermatol 1977;87:114-6.
- Willemze R, Scheffer Clinical and histologic differentiation between lymphomatoid papulosis and pityriasis lichenoides. J Am Acad Dermatol 1985;13:418-28
- Fernandes NF, Rozdeba PJ, Schwartz RA, Kihiczak G, Lambert WC. Pityriasis lichenoides et varioliformis acuta: a disease spectrum. Int J 2010; 49:257-261.

https://drugsoverthecounter.com/# diflucan over the counter
anastrozole cheap order arimidex 1 mg without prescription arimidex brand
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Mauricio, USA 2022 04 30 11 21 02 cialis 5mg online DESIGN, SETTING, AND PARTICIPANTS A total of 16, 608 postmenopausal women aged 50 to 79 years with no prior hysterectomy from 40 US clinical centers were randomly assigned to receive combined conjugated equine estrogens, 0
buy levitra online canada buy Testicular Cancer Awareness Foundation
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.