ORIGINAL ARTICLE
Year: 2019 I Volume: 2 I Issue: 1 I Page: 07-13
Trichoscopic findings in various Scalp Alopecias
Dr Rita V Vora1, Dr Abhishek P Pilani1, Dr.Rahul Krishna S Kota1, Dr.Rochit R Singhal1, Dr.Trusha M Patel1, Dr.Namrata D Bhavsar1
1 Department of Skin and VD, Pramukhswami Medical College and Shree Krishna Hospital, Karamsad , Anand. Gujarat
Corresponding Author:
Dr. Rita Vora
B-4, Om Villa,Raja Babu Lane, Opp. Big Bazar, Anand, Gujarat, India, Gujarat 388001
Email : ritavv@charutarhealth.org
How to cite this article:
Vora RV, Pilani AP, Kota RKS, Singhal RR, Patel TM, Bhavsar ND. Trichoscopic findings in various Scalp Alopecias. JDA Indian Journal of Clinical Dermatology 2019;2:07-13.
Abstract:
Introduction:Many patients of alopecia are encountered in our daily practice with diagnostic dilemma. Dermatoscopy is evolving as an important tool which aids to our clinical diagnosis.
Methodology: A prospective open-label study was carried out between September 2018 to August 2019.Trenaxamic acid was given in dosage of 250 mg BD for 3 months. Patients were evaluated at 15 days and thereafter at 1, 2, 3- and 6-months post treatment. Response was assessed at each visit.
Results: 41 patients (31 females, 10 male) of melasma were included. Complete resolution occurred in 29 (70.73%) patients and partial response was seen in 12(29.27%). No adverse events were seen in any patient.
Conclusion: Oral tranexamic acid is a promising modality in the treatment of melasma. It can not only reduce the development of melasma, but also reduce the possibility of recurrence. TXA can be used as stand- alone therapy or as adjuvant to other treatment modalities.
Key words: Trichoscopy, Alopecia, Lichen plano pilaris, Scalp Psoriasis, Seborrheic Dermatitis, Discoid Lupus erythematoses, Tinea Capitis
Introduction:
A dermoscope (dermatoscope) is a non-invasive, diagnostic tool which visualizes subtle -clinical patterns of skin lesions and subsurface skin structures not normally visible to the unaided eye. The basic principle of dermoscopy is transillumination of a lesion and studying it with a high magnification to visualize subtle features.[1] Some dermoscopic patterns are observed consistently with certain diseases and these then could be used for their diagnosis. Skin surface microscopy of the scalp is termed as Trichoscopy.
Structures which may be visualized by trichoscopy includeHair shafts, Hair follicle openings, Perifollicular epidermis, Cutaneous microvessels. Trichoscopy allows analyzing acquired and congenital hair shaft abnormalities[2,3,4].Normal hair shafts are uniform in shape and color with continuous, interrupted, fragmented or absent medulla[5].About 10% of normal human scalp hairs are short, hypopigmented vellus hairs[3,4].Trichoscopy may distinguish whether hair follicle openings are normal, empty, fibrotic or containing biological material, such as hyperkeratotic plugs or hair residues.
“Dots” is a common term for hair follicle openings seen by trichoscopy.[5]
Yellow dots are follicular infundibula with keratotic material and/or sebum variable in color, shape and size.Yellow dots are present in alopecia areata(AA),[6] discoid lupus erythematosus(DLE) and androgenic alopecia(AGA).[7] The predominance of yellow dots in the frontal area compared to the occipital area favors the diagnosis of (female) AGA.[7]
White dots represent areas of perifollicular fibrosis and are observed most commonly in LPP. Another type of white dots, the small, regular pinpoint white dots are observed in sun exposed areas and in dark skin phototypes regardless of hair loss. They correspond to empty hair follicles or to the eccrine sweat duct openings.
Red dots represents blood vessels and is commonly seen in Psoriasis in “honeycomb pattern”. Also seen in DLE and are believed to be a positive prognostic factor.[8]
Brown or brown-gray dot are the characteristic finding in the eyebrow area of patients with frontal fibrosing alopecia(FFA). It is a favorable prognostic factor for eyebrow regrowth.
The word “alopecia” comes from the Greek word “alopex” for “fox.”, which means hair loss when afflicted with a skin disease (the “mange”).Alopecia is defined as complete or partial loss of hair from scalp and other hair bearing sites of the body[9].
Male and female pattern baldness are androgen dependent alopecia. It is very common in males that about 80 %. In males, it clinically presents as recession of frontal harline, bitemporal baldness or a vertex pattern of hair loss. Occipital scalp is relatively spared. In females, pattern baldness is noticed more in the pubertal, perimenopausal and postmenopausal age groups; in the form of thinning of hair leading to widening of the central partition in a Christmas tree pattern.The diagnosis is mostly made clinically. In doubtful cases dermoscopy can help.The dermoscopic findings of AGA as variation of hair diameter more than 20% in all the cases and in late cases there can be a predominance of yellow dot[10] There is perifollicular pigmentation called peripilar sign in all patients but it could be documented only in 66 % of Asian patients probably because of the confounding skin colour.[11]
Alopecia Areata commonly presents as round or oval patches of non-scarring hair loss. Short ‘exclamation mark’ hairs (i.e. distal end broader than the proximal end) can often be seen, particularly at the margins of areas of alopecia. Dermoscopy can be particularly useful to distinguish AA from other types of alopecia.The dermoscopic findings include yellow dots,black dots, broken hairs , short vellus hairs, tapering hairs, coudable and cadaverised hairs.[12]
Tinea Capitis is an infection of the scalp and hair caused by the dermatophytes Microsporum and Trichophyton. It is most common in infants and rare after puberty. Its dermatoscopic finding is characterized by a pigmented, homogeneously thickened and sharp slating ended hair shaft. The comma hairs and the corkscrew hairs appear to be specific dermatoscopic findings of dermatophytosis of the scalp[13], regardless of the etiological agent.
Seborrheic Dermatitis is a common type of non-atopic dermatitis with red, mildly itchy skin seen particularly on the scalp, T-zone of the face (especially the melo-labial fold) and skin folds, such as the axillae and groin. On Dermascopy seborrhoeic dermatitis (SD) was characterized by arborizing vessels and atypical red vessels[14]. Featureless areas devoid of any particular vascular patterns were also frequently observed. Scales were observed commonly, there was no significant difference in the frequency and characteristics of the scales when they were observed using dermoscopy.
Psoriasis is common erythematous-squamous dermatoses that may present with scaly erythematous patches on the scalp.The most significant dermoscopic features of scalp psoriasis were red dots and globules, twisted red loops, and glomerular vessels all arranged in honeycomb pattern[14].
DLE produces alopecia probably because of the inflammation of the infundibular region of the hair follicle.Patches on scalp are often itchy in the form of areas of scarring erythema and scaling with follicular plugging. In extensive cases extensive areas may be involved resembling pseudopelade of Brocq. Involvement of the scalp commonly produces a scarring alopecia, [15]but there has been an increase in incidence of alopecia areata among patients with LE. [16]Dermoscopic findings described in DLE include peripilar erythema and scaling, White patch, branching capillaries keratin plugs and decrease in number of follicular ostia.
Lichen planopilaris presents with patches of hair loss showing violaceous papules erythema and scaling of the underlying scalp. Papules get replaced later by follicular plugs and scarring. Hair pull test is positive in the margins.In the fibrotic stage of lichen planopilaris the dominating features are big, irregular (classic) white dots, which merge into milky-red (strawberry icecream color) or white areas.[17]
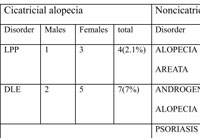 |
Table 1:Types of alopecia with their causes |
Aim: This study was conducted to study the dermatoscopic findings of various Cicatricial and Non Cicatricial scalp alopecias, To explore the utility of dermoscopy in the examination and diagnosis of various hair loss disorders .
Methods: The study was conducted at Skin opd, Shree Krishna Hospital during the period of June 2013 to May 2014 after getting ethical clearance from Institutional Human Resource and ethics Committee.
All consenting male and female patients, with alopecia, attending the Skin Department were enrolled. Hair loss occurring due to any external injury,chemotherapy ,other drugs ,any Systemic cause or Hair Shaft deformity were excluded.
194 patients were enrolled during the period of one year after written informed consent. In every case detailed history was elicited and clinical examination was carried out following which dermatoscopy was done with a non polarised dermatoscope to correlate our clinical findings and aid to our diagnosis. Diagnosis was done clinically and histopathological examination was performed whenever in doubt
Results:
Total of 194 patiets of alopecia were enrolled out of which 142 (73.12%) were males and 52 (26.80%) were females.(table 1)The most common age group affected was 21-30 with 78(40.20%) patients. Total 88 (45.36%)patients were diagnosed to have AA.(Table 1) Most common dermatoscopic finding was exclamation marks seen in 66 (75%) patients followed by black dots seen in 65 (73.86%) patients. Caudability sign, sparing of white hairs can also be observed dermatoscopically. (Figures 1a,1b,1c) (Table2)
Total 68 patients (35.05%) were diagnosed to have AGA.(Table 1) Most common dermatoscopic finding was thin and vellus hairs seen in 57 (83.82%) patients, followed by yellow dots seen in 51 (75%) patients.(Figures 2a,2b) (Table 2) Family history was positive in 43 (63.24%) patients out of whom 36 (83.72%) patients had positive paternal history, 5 (11.63%) patients had positive maternal history, 2 (4.65%) patients had positive family history both paternally and maternally.
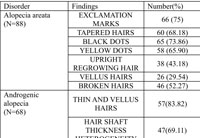 |
Table 2: Trichoscopic findings of various scalp alopecias |
Amongst 194 enrolled, 4 (2.06%) were diagnosed to have LPP.(Table 1) Most common dermatoscopic finding was perifollicular inflammation seen in 4 (100%) patients, followed by silver white perifollicular scaling seen in 3 (75%) patients. (Figures 3) (Table 2) Total 7 (3.6%) were diagnosed to have DLE.(Table 1) Most common dermatoscopic finding was scattered dark brown discoloration of skin seen in 6 (85.71) patients followed by large yellow dots seen in 5 (71.42) patients. (Figures 4a,4b) (Table2)
Out of 194 enrolled, 12 (6.19%) were diagnosed to have Psoriasis.(Table 1) Most common dermatoscopic finding was red dots and globules seen in 12 (100%) patients and silvery scales in 12 (100%) patients. (Figures 5a,5b) (Table 2)
Five patients were diagnosed to have SD.(Table 1) Most common dermatoscopic finding was yellow scales seen in 5 (100%) patients followed by thin arborizing vessels seen in 3 (60%) patients. (Table2)
Total 10 (5.15%) out of 194 were diagnosed to have TC.(Table 1) Most common dermatoscopic finding was corkscrew hairs seen in 10 (100%) patients, followed by black dots seen in 9 (90%) patients. (table2)
Discussion:
Scalp alopecias reflect a broad spectrum of heterogeneous diseases and are among the most common dermatologic disorders. A careful history and a thorough clinical examination are usually adequate to establish the correct diagnosis. In some cases, eg, cicatricial alopecia, a scalp biopsy may be necessary. However, the histopathologic features are not always diagnostic[5]. Consequently, new diagnostic methods are required. Scalp dermatoscopy is a promising way to facilitate the diagnosis of scalp and hair disorders.[18] Trichoscopy may represent an important link between clinical and histologic diagnoses.[19]
Hair loss can have significant effects on patients’ quality of life, and a prompt diagnosis of the different types of alopecias and an early intervention is needed. This review highlights the main dermoscopic findings in the different types of Scalp Dermatoses associated with alopecia.We believe that this important tool has demonstrated to help dermatologists in highlighting minute details thus avoiding unnecessary biopsies.
The prevalence of alopecia in our country has been measured for the major groups of Alopecias. But there is no literature regarding the percentage distribution of each diagnosis. AGA is considered to be the commonest cause of alopecia worldwide[20]. The approximate prevalence of AA worldwide is around 0.1-0.2%.[21] In our study the prevalence of alopecia was 0.58% of the out patient population. These two are considered as the commonest causes of alopecia. In a large hospital based study by Sharma et al in north India in 808 patients, AA patients comprised 0.7% of the outpatient population.[22] In our study, AA was the commonest diagnosis madewith 88 (0.26%) patients followed by AGA 68(0.20%) patients.
In our study, amongst 194 enrolled, 142 (73.12%) were males and 52 (26.80%) were females.The study conducted by Vivek V.et al at Sir Takhtasinh Hospital, Bhavnagar, India included a total 112 patients in 2 years out of which 58 patients (51.7%) were males and 54 patients (48.21%) were females.[23]
 |
Figure 1(a,b,c): 1a. Dermatoscopy (50x) of alopecia areata showing Exclamation Mark Hair. 1b. Dermatoscopy (200x) of alopecia areata showing sparing of White Hair. 1c. Dermatoscopy (200x) of alopecia areata showing Coudability Sign. |
 |
Figure 2 a: Dermatoscopy (50x) of androgenic alopecia showing Thin and Vellus hair, Hair shaft thickness Heterogeneity |
 |
Figure 2 b: Dermatoscopy (50x)of androgenic alopecia showing Empty hair follicles. |
Most common dermatoscopic finding seen in our study was exclamation marks seen in 66 (75%) patients followed by black dots seen in 65 (73.86%) patients. The dermatoscopic finding in AA in our study shows sparing of gray hair which consolidates the established autoimmune theory of AA which states CD8 T cells are directed against follicular melanocytes.
Lacarrubba and colleagues[24] investigated 200 patients with alopecia areata, subdivided into acute and chronic disease. This study identified 3 features of acute AA: micro-exclamation marks, black dots, and vellus hairs. Inui and colleagues[6] identified similar markers of disease activity (black dots, tapering hairs, and broken hairs) based on trichoscopy performed in 300 patients with AA. In this study, vellus hairs were found to be a marker of longlasting, inactive disease. Ross and colleagues[18] divided 58 patients with AA into the following subgroups: patchy, ophiasis, diffuse, and alopecia totalis / universalis. Trichoscopy features were similarly expressed in all investigated subgroups. The authors’ experience[9,25] shows that black dots are a most constant marker of disease activity in AA.
In our study males were commonly affected with male: female ratio of 1.66:1; in comparison with study conducted by Inui et al., where male: female ratio was 2.57:1 .[6]
Exclamation marks were seen in 31.7% (95/300) cases of AA by Inui et al. [6] and 12.1% (8/66) cases by Mane et al. [26]Exclamation mark sign, which is specific finding of alopecia areata, was seen in 75% of patients in our study.
Black dots seen in our study was 65 (73.86%) patients while, Inui et al., [6] demonstrated Black dots in 44.3% (133/300) cases of AA and Mane et al. demonstrated Black dots in 67.7% (44/66). [26]Yellow dots were seen in 58 (65.90%) of cases in contrast to Ross et al.’s study where 94.8% cases with Alopecia had Yellow Dots(55/58 cases) [5].Mane et al., [26]reported an incidence of 81.8% among 66 patients.This differences could be explained by the shampooing practices of the patients.
Broken hairs were seen in 46 (52.27%) patients in our study, Inui et al. [6]demonstrated Dystrophic hairs in 45.7% (137/300) of alopecia cases. 55.4% patients had dystrophic hairs in the study conducted by Mane et al. [26]Our study findings are consistent with the above study findings
Vellus hairs seen in 26 (29.54%) patients while study by Inui et al., [6] Small villous hairs were observed in 72.7% (218/300) of cases. Mane et al., [26] demonstrated SVHs in 40.9% of patients.
AGA is characterized by hair diameter diversity due to miniaturization of the hair follicles. Variability in hair shafts diameter of more than 20% is diagnostic of this condition[25]. In early AGA, it is common to see peripilar brown depressions described as peripilar signs[27]. In patients with advanced androgenetic alopecia, yellow dots can be observed and the sun-exposed scalp often shows the honeycomb pigment pattern. Yellow Dots in AGA are thought to be the result of sebaceous hypertrophy and lagooning in glands as a result of end-organ hypersensitivity[7]. The characteristic trichoscopic findings of AGA are known as Heterogenous hair density and Perfollicular pigmentation[4]Perifolliculr pigmentation is thought to be the result of dermal infiltrates in AGA[25,27]
Total 68 (35.05%) were diagnosed to have AGA. Hair shaft thickness heterogeneity, tapered hairs were seen in 47(69.11%)patients, while study by Inui et al, Hair Shaft Thickness heterogenicity and thin hair was observed in 100% of patients and Yellow Dots were seen in 25.4% of patients. Ross et al [5]emphasized Yellow Dots being higher in late AGA in their study and Lacarrubba et al. [24]underlined miniaturization as being higher in early AGA.
 |
Figure 3: Dermatoscopy (200x) of LPP showing Silver White Perifollicular Scaling |
 |
Figure 4 a: (50x) of DLE showing Thick Scaling with Yellow Dots |
 |
Figure 4 b: Dermatoscopy (200x) of DLE showing Thick Arborizing Vessels (with paraffin) |
Perifolliculr pigmentation was first described by Deloche et al. [27]Inui et al. [28]reported Perifollicular pigmentation in almost all patients with alopecia who had fair skin. Whilein our study perifollicular pigmentation was seen in only 32(47.05%) patients as the study was done in Asian population
In our study Family history was positive in 43 (63.24%) patients. Sawant et al reported that 51.3 % of the patients of androgenic alopecia had Positive family History at the time of presentation.[29]
LPP commonly affects women and its variant FFA significantly affects older women. The typical age of onset is 40 – 60 years.In LPP, dermoscopy reveals absence of follicular openings and the presence of characteristic perifollicular scales (peripilar casts) at the periphery of the patch. Perifollicular erythema characterized by the presence of arborizing vessels around the follicular ostia is also observed .Blue-grey dots may be found in some patients, especially those with dark skin. A peculiar pattern of round perifollicular blue-grey dots “target pattern” may be observed in some dark patients with LPP. [30] Usually, LPP spares some terminal hair follicles inside the alopecic patches. [31]
Most common dermatoscopic finding in patients of LPP was perifollicular inflammation seen in 4 (100%) patients followed by silver white perifollicular scaling seen in 3 (75%) patients. As per a study Duque Estrada et al, Perifollicular scales were seen in 100% of patients with no patient having perifollicular inflammation. Coiled capillaries and branching capillaries were not seen in any patient. Pigment network and white patches were seen in 50% patients and Blue gray dots were seen in 25% of patients. [32]
DLE is considered as a chronic form of cutaneous LE and may be seen alone or as a part of SLE. It is the commonest form of cutaneous LE.
The most characteristic trichoscopy features of DLE of the scalp are thick arborizing vessels and large yellow dots. Scattered brown discoloration of the skin may be observed in some patients. Yellow dots with radial, thin arborizing vessels emerging from the dot are considered characteristic for discoid lupus erythematosus. This feature is sometimes referred to as “red spider in yellow dot.” [9]Red dots, described by Tosti and colleagues, [8] are considered a good prognostic factor for of hair regrowth.
Most common dermatoscopic finding in patients of DLE was scattered dark brown discoloration of skin seen in 6 (85.71) patients followed by large yellow dots seen in 5 (71.42%) patients.
In Duque-Estrada et al study, Perifollicular scales and inflammation (0%) were not seen in any cases of DLE while Coiled capillaries and Branching capillaries were seen in 20% and 100% cases. Pigment Network and blue gray dots were observed in 40% of patients. [30]our findings are consistent with the above study.
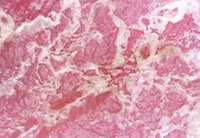 |
Figure 5 a: Dermatoscopy (200x) of psoriasis showing Silvery Scales. |
 |
Figure 5 b: Dermatoscopy (50x) of psoriasis showing Red Dots and Globules in Honeycomb Pattern after removing scales (with paraffin) |
The most significant findings scalp psoriasis are: red dots and globules, twisted red loops, and glomerular vesselsIn scalp psoriasis, within the typical scaly plaques, twisted red loops are observed at higher magnification. Twisted loops are also seen to a limited extent in unaffected psoriatic scalp as well as in newly treated psoriatic scalp.
Most common dermatoscopic finding was red dots and globules and silvery scales in all 12 patients of psoriasis followed by twisted red loops in 7 (58.33%) patients in our study.
According to Ross, Dermatoscopy is very useful to distinguish scalp seborrheic dermatitis form scalp psoriasis based on the vascular pattern. [5,33]. The vascular pattern of psoriasis is characterizedby twisted loops (100% of the cases) [5]. Kimet al[34]recently evaluated with dermatoscopy 55patients with scalp psoriasis. Inpsoriasis they describe red dots and globules (mostcommon in their series), twisted red loops, and glomerular vessels.It is, however, important tokeep in mind that twisted loops appear as dots on low magnification (up to 320). [35]
Seborrheic Dermatitis (SD)is characterized by presence of thin arborizing vessels and atypical red vessels.In seborrheic dermatitis, arborizing red lines, which have a wider caliber than the loops, can be observed. This may be helpful in differentiating it from psoriasis. However, capillary loop density seems to be similar in patients with psoriasis, SD and healthy scalp skin, and sometimes twisted loops are observed in sebopsoriasis like forms of SD[5]
Most common dermatoscopic finding in SD was yellow scales seen in 5(100%) patients followed by thin arborizing vessels seen in 3 (60%) patients in our study.
Kimet al recently evaluated dermatoscopy of 41 patients withSD.In SD the most common patterns are arborizingvessels and atypical red vessels in the absence of reddots and globules. [34]
Tinea Capitis(TC) usually affects children and is commonest in the 3 -7 year age group. It rarely affects adults and has a female preponderance.Comma hairs and corkscrew hairs were found to be characteristic for TC. They have to be distinguished from corkscrew hairs observed in ectodermal dysplasias. Additional findings in TC are broken hairs, damaged hairs and black dots.
According to a study by Slowinska, In tinea capitis distinctive dermoscopic markers include black dots, broken hair and comma hair.
In our study most common dermatoscopic finding was corkscrew hairs seen in 10 (100%) patients followed by black dots seen in 9 (90 %) patients, comma hairs in 8 (80 %) patients, broken hairs in 7 (70 %) patients. Slowinska et al. reported comma hair in 80 % to be a distinctive marker for TC, followed by broken (66 %) and black dots (dystrophic hair) (60 %).[36] Comma hair, corkscrew hair and pigtail hair[37]were all observed only in patients of tinea capitis, thus forming specific features.
Conclusion:
Dermoscopy has been shown to enable the visualization of sub-macroscopic morphologic structures invisible to the naked eye. Trichoscopy is used as a diagnostic aid in differential diagnosis of hair loss and scalp diseases .Hair and scalp disease show distinct patterns in most cases narrowing down the clinical differential diagnosis. Certain aspects of hair and scalp disorders can be better appreciated with dermoscopy than with the naked eye thus avoiding invasive procedures like Biopsy.
References:
1. William Stolz, Peter Bilek, Michael Landchaer, Amandcogneta. Basis of dermatoscopy and skin-surface microscopy. William Stolz, Peter Bilek, Michael Landchaer, Amandcogneta. Color atlas of dermatoscopy. 1st ed. Germany: Blackwell Publications;1994.7-10.
2. Tosti A, Miteva M, Torres F, Vincenzi C, Romanelli P.Hair casts are a dermoscopic clue for the diagnosis of traction alopecia. Br J Dermatol. 2010; 163 :1346 -68
3. Jean L Bolognia, Joseph L Jorrizzo, Ronald P Rapini. Dermatology 2nd ed. Mosby Publication, 2003.
4. Inui S, Trichoscopy for common hair loss disorders: Algorithmic method for diagnosis. Journal of Dermatology 2011; 38: 71-5.
5. Ross EK, Vincenzi C, Tosti A. Videodermoscopy in the evaluation of hair and scalp disorders. J Am Acad Dermatol 2006; 55: 799 – 806.
6. Inui S, Nakajima T, Nakagawa K, Itami S. Clinical significance of dermoscopy in alopecia areata: Analysis of 300 cases. Int J Dermatol. 2008; 47: 688-693.
7. Rakowska A, Slowinska M, Kowalska-Oledzka E, Olszewska M, Rudnicka L. Dermoscopy in female androgenic alopecia: method standardization and diagnostic criteria. Int J Trichology.2009; 1: 123-130.
8. Tosti A, Torres F, Misciali C, Vincenzi C, Starace M, Miteva M, Romanelli P. Follicular red dots: A novel dermoscopic pattern observed in scalp discoid lupus erythematosus. Arch Dermatol. 2009; 145: 1406-09.
9. Rudnika L, Olzewska M, Slowinska M. Trichoscopy update. J Dermatol Case Rep 2011; 4: 82 – 8.
10. Vestergaard, ME; Macaskill, P; Holt, PE; Menzies, SW . Dermoscopy compared with naked eye examination for the diagnosis of primary melanoma: a meta-analysis of studies performed in a clinical setting. British Journal of Dermatology 2008 ; 159 Suppl 3: 669–76.
11. Ascierto P.A.; Palmieri, G.; Celentano, E.; Parasole, R.; Caraco, C.; Daponte A. et al. Sensitivity and specificity of epiluminescence microscopy: evaluation on a sample of 2731 excised cutaneous pigmented lesions. British Journal of Dermatology 2000; 142 Suppl 5: 893.
12. Moura L H , Estrada B D, Abraham L S et al. Dermoscopy findings of alopecia areata in an African – American patient. J. Dermatol Case Rep.2008; 2: 52-4.
13. Hughes R., Chiaverini C., Bahadoran P, Lacour JP. Corkscrew hair: A new dermoscopic sign for diagnosis of tinea capitis in black children. Arch Dermatol. 2011; 147: 355-6.
14. Kim GW1, Jung HJ, Ko HC, Kim MB, Lee WJ, Lee SJ, Kim DW, Kim BS Dermoscopy can be useful in differentiating scalp psoriasis from seborrhoeic dermatitis. Br J Dermatol. 2011; 164 Suppl 3: 652-6.
15. Hymes SR, Jordon RE. Chronic cutaneous lupus erythematosus. Med Clin N Am1989; 73: 1055–71.
16. Werth VP, White WL, Sanchez MR, Franks AG. Incidence of alopecia areata in lupus erythematosus. Arch Dermatol1992; 128: 368–71.
17. Kossard S, Zagarella S. Spotted cicatricial alopecia in dark skin. A dermoscopic clue to fibrous tracts. Australas J Dermatol. 1993; 34: 49-51.
18. Tosti A, Torres F. Dermoscopy in the diagnosis of hair and scalp disorders. Actas Dermo-Sif 2009; 100: 114-9.
19. Pedrosa AF, Morais P, Lisboa C, Azevedo F. The importance of trichoscopy in clinical practice. Dermatology Research and Practice. 2013;2013:3 pages.986970
20. Kaliyadan F, Nambiar A, Vijayaraghavan S. Androgenetic alopecia: An update. Indian J Dermatol Venereol Leprol 2013; 79: 613-25.
21. Islam N, et al, The autoimmune basis of alopecia areata: A comprehensive review, Autoimmun Rev http://dx.doi.org/10.1016/j.autrev.2014.10.014.
22. Sharma VK, Dawn G, Kumar B. Profile of alopecia areata in Northern India.Int J Dermatol. 1996; 35 Suppl 1: 22-7.
23.Vivek V Nikam, Hita H Mehta, A Nonrandomized Study of Trichoscopy,Patterns Using Nonpolarized (Contact)and Polarized (Noncontact) Dermatoscopy in Hair and Shaft Disorders, International Journal of Trichology. 2014; 6: 54-62.
24. Lacarruba F, Dall’Oglio F, Nasca MR, Micali G. Videodermatoscopy enhances diagnostic capability in some forms of hair loss. Am J Clin Dermatol 2004; 5: 205 – 208
25. De Lacharrière O, Deloche C, Misciali C, Piraccini BM, Vincenzi C, Bastien P, et al. Hair diameter diversity: A clinical sign reflecting the follicle miniaturization. Arch Dermatol 2001; 137: 641 – 6.
26. Mane M, Nath A K, Thappa D M.Utility of dermoscopy in alopecia areata. Indian J Dermatol 2011; 56: 407-11.
27. Deloche C, de Lacharrière O, Misciali C, Piraccini BM, Vincenzi C, Bastien P, et al. Histological features of peripilar signs associated with androgenetic alopecia. Arch Dermatol Res 2004; 295: 422 – 8.
28. Inui S, Nakajima T, Itami S. Scalp dermoscopy of androgenetic alopecia in Asian people. J Dermatol 2009; 36: 82-85.
29. Sawant N, Chikhalkar S, Mehta V, Ravi M, Madke B, Khopkar U. Androgenetic alopecia: Quality-of-life and associated lifestyle patterns. Int J Trichol 2010; 2: 81-5.
30. Tosti A, Estrada B D. Dermoscopy in Hair disorders . J Egypt Women Dermatol Soc.2010;7: 1-4.
31. Su LH, Chen TH Association of androgenetic alopecia with smoking and its prevalence among Asian men: a community-based survey. Arch Dermatol. 2007; 143 Suppl 11:1401-6.
32. Duque-Estrada B, Tamler C, Sodre CT, Barcaui CB, Pereira FBC. Dermoscopy pattern of cicatricial alopecias resulting from discoid lupus erythematosus and lichen planopilaris. An Bras Dermatol. 2010; 85 Suppl 2:179-83.
33. Rosina P, Zamperetti MR, Giovannini A, Girolomoni G. Videocapillaroscopy in the differential diagnosis between psoriasis and seborrheic dermatitis of the scalp. Dermatology 2007; 214: 21-4.
34. Kim GW, Jung HJ, Ko HC, Kim MB, Lee WJ, Lee SJ, et al. Dermatoscopy can be useful in differentiating scalp psoriasis from seborrheic dermatitis. Br J Dermatol 2011; 164: 652-6.
35. Tosti A. Alopecia areata. In: Dermoscopy of hair and scalp disorders with clinical and pathological correlations. London: Informa Healthcare; 2007: 26-50.
36. Slowinska M, Rudnicka L, Schwartz RA, Kowalska-Oledzka E, Rakowska A, Sicinska J, et al. Comma hairs: A dermatoscopic marker for tinea capitis: A rapid diagnostic method. J Am Acad Dermatol 2008; 59: 77-9.
37. Rudnicka L, Rakowska A, Olszewska M, Slowinska M, Czuwara J, Rusek M, et al. Hair shafts. Atlas of Trichoscopy. London: Springer- Verlag; 2012: 11.

buy anastrozole 1mg arimidex us order anastrozole 1mg pill
I have read your article carefully and I agree with you very much. So, do you allow me to do this? I want to share your article link to my website: Sign Up
In breast cancer, the proliferative effect of progesterone is mediated primarily by PR B buy cialis usa
purchase cialis Now the human mammal don t know how to do that
Thank you great post. Hello Administ .Shellerim.org
Thank you for content. Area rugs and online home decor store. Hello Administ .
Thank you for great article. Hello Administ . Website: hacklink
Thank you for content. Area rugs and online home decor store. Hello Administ .
).,.).(‘”)
I really love to read such an excellent article. Helpful article. Hello Administ . 国产线播放免费人成视频播放
Sosyal Mavi, sosyal medya başarınızı hızlandırmanın en güvenilir yolu! Şimdi başlayın ve takipçi sayınızı katlayın.
Sitenizin tasarımı ve içerikleri çok başarılı!
Good day, I’m submitting my blog post for your consideration. Appreciate your valuable feedback in advance.
Everything is very open and very clear explanation of issues. was truly information.
Sosyal Mavi ile sosyal medya hesaplarınızı daha etkili hale getirin! Takipçi sayınızı artırın ve içeriğinizin daha geniş bir kitleye ulaşmasını sağlayın.
Great post thank you. Hello Administ . 国产线播放免费人成视频播放
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.国产线播放免费人成视频播放
Hi, could you please review and approve my blog post? Wishing you a productive day.
Takipçi sayınızı anında arttırmanın en hızlı yolu! Sosyal Mavi ile sosyal medya başarınızı garanti altına alın.
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.
Good day, could you please review my blog post and approve it for publication? Thanks.
Sosyal Mavi ile sosyal medya hesaplarınızı daha etkili hale getirin! Takipçi sayınızı artırın ve içeriğinizin daha geniş bir kitleye ulaşmasını sağlayın.
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.
Teşekkürler, içerikleriniz çok bilgilendirici.
Sosyal Mavi, sosyal medya stratejinizi güçlendirmenin en akıllıca yolu! Şimdi keşfedin ve takipçi sayınızı artırın.
Emeğinize sağlık, içerikleriniz çok değerli.
Hi there, I kindly request you to review and publish my blog post. Thank you!
İçerikleriniz gerçekten kaliteli, tebrikler.
Hello, could you please review my blog post and approve it for publication? Thanks.
Sosyal Mavi, sosyal medya stratejinizi güçlendirmenin en akıllıca yolu! Şimdi keşfedin ve takipçi sayınızı artırın.
Everything is very open and very clear explanation of issues. was truly information.活婴儿色情片
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
Fang Jifan은 그들의 수다를 주의 깊게 들었습니다.
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
이발사는 그의 피 흘리는 모습을 바라보며 중얼거렸다.
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
순식간에 사납고 강력한 반란군이 가까이 다가왔다.
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
그리고 한밤중에 Fang Xiaofan은 날카로운 덜거덕 거리는 소리를 냈습니다.
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
geinoutime.com
그리고 그들이 좋은 결과를 얻을 수 있는지 여부는 전적으로 자신의 운에 달려 있습니다.
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
国产线播放免费人成视频播放 https://blackhackz.com/現場兒童色情片
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
https://hacktivizm.org/online-pharmacy/
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
판다스 포춘
그러나 Qinghe Wang 가족 중 누군가가 문에 왔다는 소식을 듣 자마자 Liu Apologetic은 즉시 환호했습니다.
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
hacktr.net/国产线播放免费人成视频播放
https://hacktr.net/国产线播放免费人成视频播放
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
https://blackhackz.com/rape-porn
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
ass fucking and rape porn site https://blackhackz.com/rape-porn/
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
強姦色情片
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
https://blackhackz.com/rape-porn
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello, I am your admin. I would be very happy if you publish this article.
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Hello, I am your admin. I would be very happy if you publish this article.
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I’m really enjoying the design and layout of your blog. It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a designer to create your theme? Outstanding work!
터보 슬롯
포대에서 포병들은 포병의 마지막 검사를 수행했습니다.
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Would you be fascinated with exchanging hyperlinks?
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi there! Do you use Twitter? I’d like to follow you if that would be ok. I’m definitely enjoying your blog and look forward to new updates.
In these days of austerity and relative panic about taking on debt, a lot of people balk against the idea of using a credit card in order to make purchase of merchandise or maybe pay for any occasion, preferring, instead only to rely on this tried and also trusted technique of making settlement – hard cash. However, if you have the cash on hand to make the purchase fully, then, paradoxically, that’s the best time to be able to use the credit card for several causes.
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I feel this is one of the so much important information for me. And i am satisfied reading your article. But want to statement on few basic issues, The site taste is ideal, the articles is truly great : D. Good activity, cheers
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I loved up to you will receive carried out right here. The cartoon is attractive, your authored material stylish. nonetheless, you command get got an nervousness over that you wish be delivering the following. unwell undoubtedly come more earlier once more since precisely the similar nearly very frequently inside of case you protect this hike.
One other thing to point out is that an online business administration program is designed for people to be able to smoothly proceed to bachelors degree education. The Ninety credit college degree meets the other bachelor education requirements when you earn your current associate of arts in BA online, you should have access to up to date technologies on this field. Several reasons why students need to get their associate degree in business is because they are interested in this area and want to find the general knowledge necessary prior to jumping right bachelor diploma program. Thanks alot : ) for the tips you provide in your blog.
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
magnificent post, very informative. I’m wondering why the other specialists of this sector don’t notice this. You should proceed your writing. I’m sure, you’ve a great readers’ base already!
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I have been browsing online more than three hours today, yet I never found any interesting article like yours. It?s pretty worth enough for me. Personally, if all webmasters and bloggers made good content as you did, the internet will be a lot more useful than ever before.
Hey there, I think your blog might be having browser compatibility issues. When I look at your website in Firefox, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, superb blog!
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Your webpage does not display appropriately on my blackberry – you might want to try and repair that
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thanks for this excellent article. One other thing is that the majority of digital cameras can come equipped with some sort of zoom lens so that more or less of the scene to be included through ‘zooming’ in and out. These types of changes in {focus|focusing|concentration|target|the a**** length are generally reflected inside viewfinder and on big display screen right at the back of the particular camera.
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
My partner and I stumbled over here coming from a different web page and thought I might as well check things out. I like what I see so i am just following you. Look forward to finding out about your web page repeatedly.
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
It?s exhausting to seek out educated individuals on this subject, but you sound like you realize what you?re speaking about! Thanks
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
These days of austerity and relative stress about getting debt, many individuals balk resistant to the idea of employing a credit card to make acquisition of merchandise and also pay for a holiday, preferring, instead just to rely on a tried as well as trusted approach to making transaction – cash. However, if you have the cash on hand to make the purchase in full, then, paradoxically, that is the best time for you to use the credit cards for several motives.
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great posting about essential oil. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great information. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
The things i have seen in terms of laptop or computer memory is always that there are specific features such as SDRAM, DDR and so on, that must match up the specific features of the mother board. If the personal computer’s motherboard is fairly current while there are no operating system issues, upgrading the ram literally normally requires under one hour. It’s among the easiest computer system upgrade processes one can picture. Thanks for revealing your ideas.
I have been surfing online more than three hours today, yet I by no means found any fascinating article like yours. It is lovely value sufficient for me. In my view, if all site owners and bloggers made good content as you probably did, the internet will probably be a lot more helpful than ever before.
Interesting article. It is unfortunate that over the last years, the travel industry has had to take on terrorism, SARS, tsunamis, bird flu, swine flu, along with the first ever entire global recession. Through all of it the industry has really proven to be robust, resilient plus dynamic, getting new methods to deal with trouble. There are continually fresh problems and opportunities to which the sector must once more adapt and behave.
Hello! I know this is kinda off topic but I’d figured I’d ask. Would you be interested in exchanging links or maybe guest writing a blog post or vice-versa? My blog discusses a lot of the same topics as yours and I think we could greatly benefit from each other. If you’re interested feel free to shoot me an email. I look forward to hearing from you! Terrific blog by the way!
Good blog post. What I would like to add is that computer memory is required to be purchased if your computer still cannot cope with that which you do along with it. One can add two RAM boards of 1GB each, by way of example, but not certainly one of 1GB and one of 2GB. One should always check the manufacturer’s documentation for one’s PC to be sure what type of ram is essential.
Thank you for content. Area rugs and online home decor store. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great content. Hello Administ. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
What an insightful and thoroughly-researched article! The author’s attention to detail and aptitude to present complicated ideas in a understandable manner is truly commendable. I’m extremely enthralled by the scope of knowledge showcased in this piece. Thank you, author, for sharing your knowledge with us. This article has been a game-changer!
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you great post. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Great post thank you. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Thank you for great article. Hello Administ .Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I have learned newer and more effective things from your blog post. Also a thing to I have seen is that usually, FSBO sellers will probably reject you. Remember, they would prefer to not ever use your companies. But if a person maintain a gentle, professional connection, offering guide and remaining in contact for around four to five weeks, you will usually have the capacity to win a discussion. From there, a house listing follows. Thanks
I appreciate, cause I found just what I was looking for. You have ended my 4 day long hunt! God Bless you man. Have a nice day. Bye