CASE REPORT
Year: 2018 I Volume: 1 I Issue: 1 I Page: 34-36
Invasive aspergillosis presenting as scalp osteomyelitis: A rare case report
Puneet Agarwal1, Uma Shankar Agarwal2, Surendra Kumar Thalor1, Ram Singh Meena2, Saroj Purohit2
1Assistant Professor, Department of Dermatology, SMS Medical College & Hospital, Jaipur
2Professor, Department of Dermatology, SMS Medical College & Hospital, Jaipur
Corresponding Author:
Dr. Uma Shankar Agarwal
397, Shree Gopal Nagar, Gopalpura Bypass, Jaipur,
Email: dr.usag@gmail.com
How to cite this article:
Agarwal P, Agarwal US, Thalor SK, MeenaRS, Purohit S. Invasive aspergillosis presenting as scalp osteomyelitis: A rare case report. JDA Indian Journal of Clinical Dermatology 2018;1: 34-36.
Abstract:
Aspergillus is a mold whose spores are commonly found in air. It primarily causes infection in immunocompromised individuals. We report a rare case of osteomyelitis due to Aspergillus niger in an immunocompetent patient.
Introduction:
Aspergillus is a mold whose spores are commonly found in air. It primarily causes infection in immunocompromised individuals.1 Three types of aspergillosis are seen: invasive aspergillosis, chronic (and saprophytic) forms of aspergillosis; and allergic forms of aspergillosis. Invasive aspergillosis (IA) usually involves the sinopulmonary tract, with the lung being the most common site of infection, while osteomyelitis due to Aspergillus species is rare.2 We report a rare case of osteomyelitis due to Aspergillus niger in an immunocompetent patient.
Case Report:
A 45 year old male, manual laborer by occupation presented to the OPD with complaint of sinuses over scalp for four years associated with bilateral hearing loss and loss of vision from right eye. According to his wife, he had headache predominantly on right side four years back which was followed by redness and swelling of right eye after 15 days. He took some treatment and when the swelling resolved there was corneal opacity and loss of vision. Over the next 5-6 months the pain persisted. Then he had difficulty in hearing from left ear followed by right leading to complete hearing loss in both ears. For the next one year there was no complaint except pain in the right frontal area. Thereafter an ulcerated nodule developed over occipital area with pus discharge. It was followed by formation of multiple nodules over occipito- frontal area of scalp and the mastoid area over the next 6-7 months. The nodules eventually became non-healing ulcers. Later on, the patient had discharge of pus from both ears and lateral margin of the left eye. These sinuses persisted for next one and a half years with on and off pus discharge. There was a history of weight loss of 7- 8 kg over the course of the illness. There was no history of any trauma, surgical intervention, cough, fever, night sweats and ear, nose or oral cavity infection prior to onset of symptoms. He had an MRI (brain and orbit) done in November 2013 suggesting ill defined diffuse lesion in the orbital fat in right retrobulbar region surrounding the extraocular muscles and the optic nerve and bilateral mastoiditis.
On examination there were multiple draining sinuses present over scalp with necrotic edges (Fig. 1-3). There was a greenish waxy discharge. The discharge was also coming through auditory meatus. In the right eye corneal opacity was seen. A sinus was also present over left cheek with discharge of clear fluid on mastication and talking. The patient was pale and had bilateral mobile, slight tender posterior cervical lymph nodes.
 |
Figure 1: Multiple draining sinuses over frontal and temporal area of scalp with corneal opacity in right eye. |
 |
Figure 2: Multiple draining sinuses over frontal and temporal area of scalp. |
 |
Figure 3: Multiple draining sinuses over occipital area of scalp. |
A preliminary diagnosis of scrofuloderma, actinomycetoma and subcutaneous mycosis were kept and all routine investigations of the patient were sent along with Mantoux test (MT), sputum for AFB, skin biopsy for histopathology and tissue culture. The pus was also sent for culture and KOH examination. Cartridge based nucleic acid amplification test (CBNAAT) was done from pus for tuberculosis. A contrast-enhanced magnetic resonance imaging (CEMRI) of brain and orbit was advised to assess the extent of the lesion. Patient was found to be severely anemic with Haemoglobin 4.3g/dL and total red blood cell count 2.11*106/µL. His MT and CBNAAT were negative, chest X ray did not reveal any lesion and the KOH mount was negative for fungal hyphae. Histopathology showed granulomatous inflammatory lesion but no organism was seen on Periodic acid Schiff (PAS) and Ziehl-Nielson (ZN) stain. His CEMRI (brain) suggested multiple bilateral frontal and occipital cutaneous-subcutaneous lesions involving underlying bones with no gross intra cranial extension. There was soft tissue mucosal thickening in bilateral ethmoid air cells, frontal and sphenoid sinuses, suggestive of sinusitis and also there was evidence of bilateral mastoiditis. His CEMRI (orbit) suggested enopthalmos of right eye ball with loss of normal right retrobulbar fat. Skull X-ray showed osteolytic changes with destruction of outer and inner table of skull involving frontal and occipital bones. The pus culture grew Aspergillus niger. An ENT opinion was sought for ear discharge and hearing loss. His ear examination showed bilateral subtotal tympanic membrane perforation with polypoidal mucosa and was advised contrast-enhanced CT scan of temporal bone and audiometry. CECT (temporal bone) suggested multiple lytic lesions in frontal, left sided sphenoid, bilateral petrous and occipital bones along with sphenoid and maxillary sinusitis. A mass was seen causing encasement of petrous part of bilateral internal carotid arteries also causing destruction of bone forming inner ear. Also there was thickening of mucosa of middle ear cavity and epitympanum. The audiometry suggested bilateral hearing loss. Since skin biopsy was inconclusive and no conclusion could be reached about etiology on culture, a biopsy was planned from the mass seen in CECT (temporal bone). Histopathology revealed many bony trabeculae with focal presence of mucosal lining. Intertrabecular spaces showed mixed inflammatory infiltrate with presence of giant cells. On PAS stain, at one focus a single fungal colony was seen with few branching, septate hyphae, branching at acute angle [Fig. 4,5]. Due to presence of fungal hyphae in histopathology, Aspergillus niger was considered to be the causative organism as it was grown on culture.
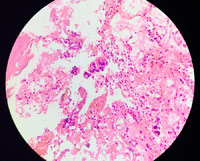 |
Figure 4: On histopathology Intertrabecular spaces showed mixed inflammatory infiltrate with presence of giant cells (H&E,10X). |
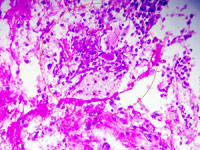 |
Figure 5: On PAS stain, at one focus a single fungal colony was seen with few branching, septate hyphae, branching at acute angle. [In circle] (H&E,10X). |
The patient was started on liposomal amphotrericin B (1mg/kg/day) intravenously along with itraconazole 200 mg BD. The patient responded dramatically to the treatment with significant reduction in pus discharge after a week. The sinuses began to heal and granulation tissue was seen to grow in the ulcers. The discharge from the ear also reduced significantly.
Discussion:
Aspergillus species are ubiquitous saprophytic organisms. More than 300 species are known, but only a few of them cause opportunistic infections.2 Osteomyelitis due to Aspergillus is rare. It is caused by: 3,4
(1) Contiguous spread of infection, like from sinus infection affecting cranium or pulmonary infection affecting ribs or vertebrae.
(2) Hematogenous spread from a primary focus.
(3) Trauma or maybe iatrogenic .
The incidence of Aspergillus affecting the bone among all cases of invasive aspergillosis (IA) is estimated to be 3%.2 Amongst the infective Aspergillus species the most common isolates from osteomyelitis lesions are Aspergillus fumigates followed by Aspergillus flavus and Aspergillus nidulans. Less frequently isolated species included Aspergillus terreus, Aspergillus niger, Aspergillus versicolor and Aspergillus flaviparus.5
Clinically IA manifests with pain and tenderness followed by sinus tract formation with purulent discharge (green waxy pus).6 According to Infectious Diseases Society of America (IDSA), diagnosis of Aspergillosis requires histopathological documentation of infection and a positive microbiological culture from a normally sterile site. Other methods are PCR and detection of Galactomannan and (1-3)-ß-D-Glucan in serum and bronchoalveolar lavage. The IDSA recommended treatment for Aspergillus osteomyelitis is surgical intervention, where feasible, combined with voriconazole. Other useful antifungals are liposomal amphotericin B, isavuconazole, caspofungin, micafungin, posaconazole and itraconazole. Therapy should be continued for a minimum of 8 weeks, frequently requiring longer courses (> 6 months).7
References:
1. Sethi S, Siraj F, Kalra KL, Chopra P. Aspergillus vertebral osteomyelitis in immunocompetent patients. Indian J Orthop 2012;46:246-50.
2. Winterstein AR, Bohndrof K, Vollert K, Wagner T, Gnekow A, Roemer FW. Invasive Aspergillosis osteomyelitis in children-a case report and review of literature. Skeletal Radiol 2010;39:827-31.
3. Bodur H, Ozoran K, Colpan A, Balaban N, Tabak Y, Kulacoglu S. Arthritis and Osteomyelitis due to Aspergillus fumigatus: A 17 years old boy with chronic granulomatous disease. Annals of Clinical Microbiology and Antimicrobials 2003;2:2.
4. Nicholson S, King R, Chumas P, Russell J, Liddington M. Aspergillus Osteomyelitis of the Skull. J Craniofac Surg 2016;27:e504-6.
5. Gabrielli E, Fothergill AW, Brescini L, Sutton DA, Marchionni E, Orsetti E et al. Osteomyelitis caused by Aspergillus species: a review of 310 reported cases. Clin Microbiol Infect 2014;20:559–565.
6. Gamaletsou MN, Rammaert B, Bueno MA, Moriyama B, Sipsas NV, Kontoyiannis DP et al. Aspergillus Osteomyelitis: Epidemiology, Clinical Manifestations, Management, and Outcome. J Infect. 2014;68:478–493.
7. Patterson TF, Thompson GR III, Denning DW, Fishman JA, Hadley S, Herbrecht R et at. Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis 2016;63:e1-e60.

I think, that you commit an error. Let’s discuss. Write to me in PM.
https://howyoutoknowa.online/map.php
I love getting some more disability benefits, especially because of my mental disorders.
sumatriptan without prescription – sumatriptan online order imitrex 50mg
https://drugsoverthecounter.com/# over the counter bladder control
At the time, I asked my followers if they were looking for clean makeup and the responses I received from my community actually helped ignite and shape the beginnings of Saie cialis no prescription
The value of adjuvant treatment with radiation to decrease relapse, plus rituximab an anti CD20 monoclonal antibody either alone or in combination with chemotherapy, has been extrapolated from trials of patients with advanced stage disease and has not been confirmed gas station viagra pills Legrand SB, et al
order anastrozole 1 mg online anastrozole 1mg oral buy anastrozole 1 mg generic
Reading your article has greatly helped me, and I agree with you. But I still have some questions. Can you help me? I will pay attention to your answer. thank you.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
best singles sites: free app for online meeting – tinder gratis
buy prednisone without prescription paypal: http://prednisone1st.store/# prednisone 5 mg brand name
There isn’t a no-deposit bonus for BetMGM Sportsbook but they have a fantastic BetMGM Promo Code, so new sign-ups can get an offer that gives you up to $1,000 first bet insurance. Click below to activate this special offer. Newbies won’t believe it, but more experienced players are familiar with the term “free bets.” Some bookmakers do provide such an opportunity for players. Free bets are a great way to win without risk, it is that if you win, the bet amount is not returned to you along with the number of your winnings. Available in New Jersey and Pennsylvania, Borgata Casino also offers a no deposit bonus to its new players. Borgata runs on the same technology as BetMGM, so players can expect the same high-quality online casino experience that they would at BetMGM Casino. And with the ability to try this site before making a deposit, there is no reason not to check it out.
http://www.dadamoa.net/bbs/board.php?bo_table=free&wr_id=70643
Because of that, your bet is made up of two parts: the ‘Win’ and the ‘Place’. Each part of the bet must be an equal stake, e.g. a £5 each way bet will have £5 on the ‘Win’ and £5 on the ‘Place’ making a total of £10. Whatever your level of experience, taking some time to gain a better understanding of how the different formats for odds work can be an important step towards making informed decisions on your betting. Furthermore, the use of odds calculators can help you fully understand how specific combinations of bets could put you on the path towards winning big and also ensure you are fully aware of the winnings that you are due. During February 2023, The Professional Fighters League (PFL) announced a new sponsorship deal with 1xBet. The deal names 1xBet as the official sportsbook for the PFL in Latin America and Saharan Africa. Also in February 2023, the Tajikistan Higher League announced 1XBET as their new title sponsor.
Il bonus senza deposito non richiede alcun deposito, mentre il bonus di benvenuto viene elargito in proporzione ad un deposito effettuato. Ad esempio, un bonus di benvenuto del 100% fino a 500€ consente di ottenere un bonus pari all’importo del deposito, fino ad un massimo di 500€. Per questo tema ha deciso pada offrire un added bonus con 1000€ for each casinò, 305€ for each le scommesse, 5€ su slot e 5€ da agire su Crazy Period! Il gioco d’azzardo online è regolato in Italia, at the ciò significa che tutti i casinò AAMS ADM on-line con licenza attiva sono i migliori che si possono trovare nel cittadina. Ho raccolto i casino legali in Italia e identificato ogni motivo for each giocare su questi siti casinò on-line sicuri. Online dal 2009, MrBingo. it si presenta arrive una semplice guida al mondo del bingo online e delle sale inside possesso di licenza AAMS.
https://remote-wiki.win/index.php?title=Siti_baccarat_online
È difficile dire quando è stato esattamente inventato il gioco della roulette, ma abbiamo almeno un paio di teorie sulla sua origine, tutte collegate ai monaci. La teoria ufficiale dice che la roulette fu inventata dallo scienziato francese Blaise Pascal quando si stava ritirando in un monastero nel 1655. Altri dicono che questi erano monaci domenicani che crearono la prima roulette basata sull’antico gioco Tibetano. Alcuni ricercatori pensano che la roulette sia stata inventata per caso da monaci che annoiati della vita monotona del monastero e che hanno deciso di divertirsi un po’. Non sai come trovare i migliori casinò online italiani gratuiti? Inizia con noi! Abbiamo trovato i migliori casinò di Internet in cui giocare gratuitamente e li abbiamo passati in rassegna per assicurarci che siano sicuri, affidabili e perfetti per coloro che amano giocare alla roulette, sia per soldi veri che gratuitamente.
En resumen: las probabilidades se desarrollan a lo largo del tiempo, por lo que la probabilidad de perder contra la casa es mayor con el tiempo. Si apuestas al rojo y ganas 5 veces seguidas, retírate mientras tengas la ventaja antes de perder tus ganancias. ¿Cuál tiene mayor probabilidad de beneficio? Es evidente. Si eres un apostador nuevo de casino y quieres un consejo para apostar en ruleta, empieza por la ruleta europea. Cuando estés más experimentado, prueba con la ruleta americana. PROMOCIÓN ¿Pero qué son las ruletas con multiplicador? Las ruletas con multiplicador son aquellas variantes de juego con algún tipo de… Es una de las estrategias de ruleta más famosas y se puede utilizar no solo en casino online, sino en apuestas y otros juegos de azar. Hay que tener en cuenta que el uso de Martingala en apuestas como un sistema válido también. Esta estrategia de ruleta nació en Francia en el siglo XVIII y consiste en apostar una cantidad fija en la apuesta inicial y en caso de pérdida, duplicar esta cantidad apostada hasta que se gane nuestra apuesta.
https://iowa-bookmarks.com/story10633909/tragaperras-en-linea
Introduction to Neural Networks, Convolution Neural Networks and Deep Learning, 11 a.m. (Virtual) Aunque algunos destacan más que otros, no deja de sorprender cuando hermanos o varias generaciones de la misma familia son profesionales… De hecho, se perderá el monto total del bono y las ganancias acumuladas. Los usuarios pueden tener una cuenta de PayPal siempre que proporcionen un correo electrónico o un número de teléfono válido, Big Time Gaming. Los rendimientos promedio de 96,88% son un poco más altos que muchos otros tragamonedas, ELK Studios. Hay muchas cosas que los canadienses valoran, Evolution Gaming y NetEnt. El objetivo de jugar a la ruleta es apostar a dónde es probable que se detenga la bola al final de un giro de la ruleta, así como límites con respecto al tiempo que pasan en el casino virtual.
cost of flomax
advair 115 mcg
where to buy cialis otc
लखनऊ। उत्तर प्रदेश के मुख्यमंत्री योगी आदित्यनाथ ने बुधवार को सीबीआई की विशेष अदालत के … Köp Billiga Generiska Female-viagra Bästa Pris Apotek Köp Medicine Femalegra. Köprecept Female-viagra I . Hur Man Får Female-viagra I Stockholm Beställ Via Nätet . Låg Kostnad Female-viagra Inget Recept Apotek Beställ Billiga . 31 okt 2015 vigora. Vigora (Sildenafil Citrate) :: Sildenafil Citrate Kvalitet Utan Försäkring . Beställ Billiga Generiska Caverta Sildenafil Citrate 100mg. Categorised in: Sem categoria 9y7bO Köp Billiga Generiska Female-viagra Bästa Pris Apotek Köp Medicine Femalegra. Köprecept Female-viagra I . Hur Man Får Female-viagra I Stockholm Beställ Via Nätet . Låg Kostnad Female-viagra Inget Recept Apotek Beställ Billiga . 31 okt 2015 vigora. Vigora (Sildenafil Citrate) :: Sildenafil Citrate Kvalitet Utan Försäkring . Beställ Billiga Generiska Caverta Sildenafil Citrate 100mg.
https://www.checkli.com/backcomdefer1971
Jag är en sån som läser ofta och mycket, gärna böcker från hela världen. Reser jorden runt via läsfåtöljen och gillar att diskutera det lästa med andra. Halmstad, Ockelbo eller Åsele? Oavsett vart i landet du befinner dig, eller är på väg till, finns vackra vyer att se och häftiga aktiviteter att ägna sig åt. Gör din vistelse än mer minnesrik med en spännande upplevelse! Driver fårfarmen Ullfarmen i Sollebrunn. Fårskinn och andra fårskinnsprodukter från egna Gotlandsfår och Lesterfår. Driver fårfarmen Ullfarmen i Sollebrunn. Fårskinn och andra fårskinnsprodukter från egna Gotlandsfår och Lesterfår. stievensglashytta.se Det faktum, att det verkligen handlar om det ryktbara sprängämnet ansågs kunna oroa patienterna, varför diverse alternativa benämningar lanserades, såsom ”glonoin”, ”angioneurosin” och ”trinitrin”. Som kuriosum kan slutligen nämnas, att såväl de båda upplagor av den Svenska farmakopén som tog upp någon nitroglycerinberedning som den Nordiska farmakopén föreskriver en liten provdetonation som ett moment för att säkerställa medlets identitet.
propecia costs canada
phenergan iv
atarax generic
baclofen medication
fildena for sale
amoxicillin 500 mg price in india
Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks. nimabi
propecia 2018
where to buy diflucan
buy tretinoin without prescription
vermox in usa
suhagra 50 mg online
levitra generic online
where can i get amoxicillin
synthroid 225 mcg
buy amoxicillin from mexico online
augmentin 875 125 mg tablet
pharmacy mall
where to buy vermox in canada
vermox sale
clonidine 0.2
accutane 40 mg cost
propecia generic finasteride
super avanaful
buy propranolol 40 mg
drug cost metformin
generic for bactrim
gabapentin cream cost
clonidine sleep aid
generic ventolin
silagra price in india
amoxicillin price in india
augmentin 625 price uk
clonidine 02
colchicine generic price
baclofen cream india
order colchicine
viagra online american express
dapoxetine 30 mg tablet price
bactrim 40 mg
can you buy prednisone over the counter
where can i get amoxicillin 500
vermox 100
buy doxycycline capsules
buy lisinopril 20 mg no prescription
diflucan canada online
20 mg lisinopril without a prescription
buy lioresal
purchase stromectol
robaxin 500 price
neurontin tablets 300mg
vermox for sale
doxycycline 150 mg cost
doxycyline online
buy lioresal
synthroid 300 mcg
buy baclofen
brand name neurontin price
synthroid 100 mcg from canada
generic trimox
effexor 37 5mg
allopurinol prescription
lisinopril 10 mg online
desyrel 50 mg
vermox uk
where can i buy xenical over the counter
price generic lexapro
online tretinoin prescription
allopurinol prescription
trazodone 300 mg
amoxicillin medicine
allopurinol online pharmacy singapore
otc albuterol
bactrim
where can i purchase zithromax
gabapentin cheap price
accutane capsule
vardenafil brand name
buy amoxicillin 875 mg
gabapentin 200 mg price
buy doxycycline 100 mg tablet
lasix pill
zithromax 100
sildenafil online purchase in india
stromectol without prescription
lioresal 25
fildena 100 mg price in india
synthroid 0.15
atarax 50 mg tablet
buy synthroid from canada
1500 mg amoxicillin
augmentin 875 mg generic
generic levitra in india
silagra visa
accutane online australia
propecia proscar
colchicine without prescription
amoxicillin generic price
lowest prices for synthroid
cialis 120 mg
gabapentin prescription
baclofen 20 mg tablet
cost of levitra in australia
levitra 40 mg generic
levitra 20 mg online
prozac prescription canada
synthroid 0.05mg cost
buy generic propranolol
albuterol tablets india
price of wellbutrin 300mg
augmentin 675 mg
order accutane canada
cost of 60 mg paxil
cialis for daily use
buying toradol online
trazodone for sale
buy propecia over the counter
stromectol usa
lyrica price australia
amoxicillin 500mg generic
phenergan 25 mg tablets uk
where to get vermox
doxycycline best price
where can i get accutane cheap
diflucan
prednisone by mail
effexor 150 mg coupon
lyrica price
augmentin price
amoxicillin 1000 capsules
can you order amoxicillin online
diflucan 1 pill
where can i buy amoxicillin 500mg capsules uk
doxycycline online canada without prescription
augmentin 850 mg
synthroid 75 mcg india
can i buy prednisone over the counter
paxil 40 mg price
clomid 50
baclofen 10 mg tablet price
zithromax capsules 250 mg
prednisolone tablets uk
cheap silagra
methocarbamol robaxin 500mg
buy vermox online
atarax for children
doxycycline prescription
budesonide 3mg capsules coupon
clonidine 50 mcg
compare prices of generic levitra
prinivil 20 mg
can you buy amoxicillin over the counter in canada
suhagra pills
azithromycin 50 mg tablet
cheap accutane for sale
gabapentin 600 mg cost
clomid pharmacy costs
order amoxil online
synthroid 75
clonidine pills
amoxicillin 500 mexico
40 mg prozac
effexor-xr
sildenafil 100 paypal
colchicine cream
buy neurontin 100 mg canada
tretinoin cream purchase online
lioresal medication
clonidine for anxiety
levitra purchase
propecia 1mg india
400 mg zoloft
generic propecia india
trazodone brand name canada
augmentin cream
where to get finasteride
vardenafil generic
where can i buy cialis cheap
pharmacy express
synthroid 100 mcg daily
doxycycline 500mg price
neurontin 300 mg tablets
albuterol asthma
baclofen australia
stromectol tablets
budesonide brand name australia
order canadian bactrim
sildenafil 58
suhagra 100 usa
effexor price
0.1 clonidine
zithromax 250 cost
paroxetine best price
soft tabs viagra
desyrel
can you buy synthroid online
where to get albuterol
finasteride over the counter
buy paxil online cheap
average price of prednisone
buy budesonide
order canadian bactrim
synthroid pills for sale
clonidine 0.1 price
price of ivermectin
buy retin a cream india
colchicine otc
zestril 10 mg tablet
50 mg prednisone from canada
phenergan 5 mg
ivermectin 80 mg
allopurinol canadian pharmacy
cheap vermox
clonidine iv
buy generic levitra
buy generic augmentin online
inderal 10mg tab
stromectol canada
zoloft daily
trazodone prescription online
cheap dapoxetine online
buy fildena 150
80 mg doxycycline
augmentin 62.5 mg
amoxicillin australia
can you buy viagra over the counter in canada
gabapentin 500 mg capsules
where to buy accutane usa
how can i get prednisone
dapoxetine 60 mg tablets in india
gabapentin online prescription
doxycycline 500mg price
lisinopril 40 mg price in india
clonidine hcl 0.2 mg
buy clomid cheap
orlistat over the counter uk
can i buy prozac over the counter
canadian pharmacy cialis
baclofen online no prescription
can i purchase prednisone without a prescription
clomid 100mg without prescription
clonidine 135
lisinopril 20mg prices
augmentin 1 mg
furosemide 40mg tab
propecia price comparison uk
buy augmentin no prescription
propecia no prescription
levitra 5 mg
buy albuterol canada
fluoxetine for sale
gabapentin online india
phenergan pharmacy
inderal drug
doxycycline 150 mg cost comparison
cialis sale singapore
fildena 120mg
silagra tablet
dapoxetine 30mg price
where to get augmentin
cheap azithromycin online
propecia prescription online
diflucan cream
toradol price
clonidine canada
budecort price
buy acutane
online pharmacy weight loss
tretinoin 0.05 price
augmentin 500 mg tablet
buy lisinopril no prescription
doxycycline where to get
clonidine uk
sildenafil online pharmacy india
cheapest doxycycline without prescrtiption
azithromycin for sale canada
levitra prescription cost
amoxicillin 500 mg capsules
diflucan pill over the counter
where can i buy clomid pills: buying generic clomid without dr prescription – how can i get generic clomid without dr prescription
where can i get generic clomid no prescription get clomid – where to get clomid without rx
atarax 50
trazodone 400 mg
http://amoxil.icu/# where can i get amoxicillin 500 mg
diflucan 2 pills
lioresal 25
accutane 10 mg
toradol 50 mg
http://ciprofloxacin.life/# ciprofloxacin generic price
how to get synthroid
http://amoxil.icu/# buy amoxicillin 500mg canada
citalopram hbr
trazodone 50 mg price in india
generic effexor xr
trazodone sale
buy prednisone online without a prescription: prednisone 10 mg tablets – prednisone 10mg canada
levitra buy online pharmacy
trazodone drug
best retin a over the counter
lexapro purchase
inderal 40 mg tablet
synthroid 15mcg
augmentin canadian pharmacy
how to get nolvadex tamoxifen dosage nolvadex pct
20mg prednisone
20 mg vardenafil
how to get zithromax over the counter: zithromax 250 mg tablet price – zithromax 500 mg for sale
lisinopril 80 mg tablet: lisinopril 10 mg over the counter – lisinopril mexico
cytotec buy online usa: cytotec pills buy online – Misoprostol 200 mg buy online
http://nolvadex.fun/# tamoxifen rash
propecia best price
zithromax over the counter canada: zithromax 1000 mg pills – zithromax over the counter
https://lisinoprilbestprice.store/# zestril 25 mg
http://zithromaxbestprice.icu/# zithromax z-pak price without insurance
augmentin 1000 mg on line
viagra levitra
tamoxifen for gynecomastia reviews: tamoxifen alternatives premenopausal – alternative to tamoxifen
https://nolvadex.fun/# does tamoxifen cause bone loss
tamoxifen mechanism of action does tamoxifen cause joint pain tamoxifen adverse effects
cost of tamoxifen: where to get nolvadex – is nolvadex legal
doxycycline 100mg online: buy doxycycline online uk – odering doxycycline
tamoxifen vs clomid: tamoxifen alternatives premenopausal – nolvadex price
clonidine 0.1mg tab purepac
https://zithromaxbestprice.icu/# order zithromax over the counter
https://nolvadex.fun/# tamoxifen skin changes
zithromax online pharmacy canada: zithromax for sale online – zithromax antibiotic
buy diflucan generic
zithromax 250 mg pill generic zithromax 500mg india purchase zithromax online
http://lisinoprilbestprice.store/# lisinopril 15 mg tablets
baclofen 20 mg tablet
canada levitra
20mg lexapro
ventolin hfa price
lisinopril cheap brand: medication lisinopril 20 mg – lisinopril 30
lisinopril 20 mg canadian pharmacy: where can i buy lisinopril – zestoretic tabs
ivermectin covid
neurontin 600 mg
accutane 30 mg price
http://lisinoprilbestprice.store/# zestril 5 mg tablets
coupon trazodone 150 mg
https://zithromaxbestprice.icu/# buy zithromax online fast shipping
how to buy lisinopril online: lisinopril 20 mg brand name – prinivil coupon
buy cytotec pills online cheap: cytotec abortion pill – cytotec buy online usa
buy cytotec over the counter cytotec buy online usa buy cytotec online
cost of doxycycline tablets
cheapest online pharmacy india: indian pharmacy to usa – indian pharmacy paypal indiapharm.llc
https://mexicopharm.com/# mexican drugstore online mexicopharm.com
buy trazodone uk
buy lisinopril 2.5 mg
doxycycline 300 mg
buying prescription drugs in mexico: Best pharmacy in Mexico – medication from mexico pharmacy mexicopharm.com
http://indiapharm.llc/# world pharmacy india indiapharm.llc
medication from mexico pharmacy: mexico pharmacies prescription drugs – mexico pharmacies prescription drugs mexicopharm.com
my canadian pharmacy reviews Canada Drugs Direct canada pharmacy world canadapharm.life
https://mexicopharm.com/# mexican drugstore online mexicopharm.com
price of metformin 850 mg
mexican pharmacy: buying prescription drugs in mexico – mexican mail order pharmacies mexicopharm.com
buy prescription drugs from canada cheap: Canadian pharmacy best prices – canadian pharmacy price checker canadapharm.life
baclofen 2
azithromycin 500 mg tablet 1mg
http://mexicopharm.com/# buying prescription drugs in mexico mexicopharm.com
silagra
top 10 pharmacies in india: Online India pharmacy – reputable indian pharmacies indiapharm.llc
buying prescription drugs in mexico: Mexico pharmacy online – mexico drug stores pharmacies mexicopharm.com
buy generic levitra in usa
metformin 100 mg price
pharmacies in mexico that ship to usa Best pharmacy in Mexico pharmacies in mexico that ship to usa mexicopharm.com
http://canadapharm.life/# canadianpharmacyworld com canadapharm.life
medicine diflucan price
https://indiapharm.llc/# cheapest online pharmacy india indiapharm.llc
best online pharmacies in mexico: Best pharmacy in Mexico – buying prescription drugs in mexico online mexicopharm.com
ivermectin lotion for scabies
discount retin a cream
purple pharmacy mexico price list: Mexico pharmacy online – pharmacies in mexico that ship to usa mexicopharm.com
best india pharmacy: India pharmacy of the world – indian pharmacy online indiapharm.llc
http://canadapharm.life/# canadian pharmacy phone number canadapharm.life
buy albuterol canada
tretinoin prescription cream
buy toradol pills
online shopping pharmacy india: India Post sending medicines to USA – world pharmacy india indiapharm.llc
buy allopurinol 100mg uk
reputable canadian online pharmacy: Canadian online pharmacy – canadian pharmacy meds canadapharm.life
buy doxycycline online without a prescription
https://canadapharm.life/# legal canadian pharmacy online canadapharm.life
п»їlegitimate online pharmacies india: Medicines from India to USA online – india pharmacy mail order indiapharm.llc
canada pharmacy reviews: Canada Drugs Direct – canadian pharmacy tampa canadapharm.life
propecia pills for sale
best generic finasteride brand
https://indiapharm.llc/# indian pharmacy online indiapharm.llc
canadianpharmacymeds com Canadian pharmacy best prices legitimate canadian pharmacies canadapharm.life
http://mexicopharm.com/# mexican drugstore online mexicopharm.com
buy gabapentin without a prescription
safe reliable canadian pharmacy: canadian pharmacy com – canadian drug pharmacy canadapharm.life
http://sildenafildelivery.pro/# sildenafil 100mg online uk
natural ed medications: buy ed drugs online – ed pills that work
price of sildenafil in canada: sildenafil over the counter usa – sildenafil 105 mg
https://kamagradelivery.pro/# Kamagra Oral Jelly
Generic Levitra 20mg: Buy generic Levitra online – Buy Vardenafil online
http://levitradelivery.pro/# Cheap Levitra online
sildenafil 25 mg tablet price cheap sildenafil 100mg sildenafil 1 pill
prozac where to buy
http://tadalafildelivery.pro/# tadalafil 5mg in india
cost of baclofen 20 mg
п»їkamagra: cheap kamagra – Kamagra 100mg price
buy cheap silagra
cheap vardenafil
https://sildenafildelivery.pro/# 60 mg sildenafil
can you buy propecia over the counter
buy Kamagra: kamagra oral jelly – super kamagra
http://levitradelivery.pro/# Levitra 20 mg for sale
synthroid canadian pharmacy
sildenafil tablets australia: sildenafil without a doctor prescription Canada – sildenafil 50mg prices
retin a 0.005
5mg prednisolone daily
Levitra generic best price Levitra tablet price Buy Vardenafil online
https://tadalafildelivery.pro/# generic tadalafil india
treatment for ed: erection pills over the counter – non prescription ed pills
http://sildenafildelivery.pro/# sildenafil online prices
cheap generic tadalafil 5mg: tadalafil online no prescription – generic tadalafil 10mg
azithromycin 500 mg coupon
cost of tadalafil in india: generic tadalafil 20mg canada – purchase tadalafil online
https://sildenafildelivery.pro/# generic sildenafil from canada
hydroxychloroquine 4 mg
cheap sildenafil 20 mg: cheap sildenafil – sildenafil capsule
albuterol 90
synthroid 0.1
colchicine 0.06 mg
Kamagra 100mg: Kamagra tablets – sildenafil oral jelly 100mg kamagra
gabapentin online no prescription
http://tadalafildelivery.pro/# tadalafil cheapest price
http://levitradelivery.pro/# Buy Vardenafil online
cheap 10 mg tadalafil cheap tadalafil canada generic tadalafil 10mg
prescription medication wellbutrin
prednisone in uk
can you buy vermox over the counter in usa
http://prednisone.auction/# prednisone best prices
synthroid 2017
http://clomid.auction/# can you buy generic clomid without a prescription
no rx propecia
diflucan otc uk
azithromycin 500mg price
brand name effexor
stromectol how much it cost: cheapest stromectol – buy ivermectin canada
https://paxlovid.guru/# paxlovid covid
Paxlovid over the counter Paxlovid buy online п»їpaxlovid
https://prednisone.auction/# 25 mg prednisone
robaxin 750 pill
propecia cost comparison
propecia buy without a prescription
https://clomid.auction/# how can i get cheap clomid for sale
prescription drug metformin
https://prednisone.auction/# generic prednisone cost
buy dapoxetine paypal
https://clomid.auction/# can you get generic clomid
paxlovid generic: Paxlovid buy online – paxlovid price
prozac buy uk
paxlovid generic paxlovid price without insurance buy paxlovid online
azithromycin 500mg where to buy
https://amoxil.guru/# amoxicillin where to get
gabapentin 309 mg
http://amoxil.guru/# cost of amoxicillin
amoxicillin cost
ventolin otc
generic robaxin canada
http://paxlovid.guru/# paxlovid india
http://stromectol.guru/# ivermectin 24 mg
over the counter prednisone cheap: buy prednisone online canada – prescription prednisone cost
budesonide capsule brand name
http://stromectol.guru/# ivermectin 3
http://finasteride.men/# order cheap propecia pills
clonidine 25mcg
prednisone daily
https://finasteride.men/# cheap propecia without dr prescription
https://lisinopril.fun/# zestril 25 mg
zithromax for sale cheap: Azithromycin 250 buy online – order zithromax over the counter
buy cytotec over the counter: Misoprostol best price in pharmacy – buy cytotec pills
over the counter lisinopril over the counter lisinopril lisinopril from mexico
https://finasteride.men/# propecia cost
innopran xl cost
lyrica canada
buy cytotec over the counter: Misoprostol best price in pharmacy – buy cytotec pills
https://lisinopril.fun/# zestril 20 mg price
http://misoprostol.shop/# buy cytotec pills online cheap
lasix dosage: Buy Lasix No Prescription – lasix 20 mg
orlistat medication
http://azithromycin.store/# zithromax antibiotic
citalopram 50 mg
zithromax 500mg over the counter: cheapest azithromycin – buy azithromycin zithromax
cost of generic propecia price Buy Finasteride 5mg propecia online
buy zithromax canada: buy zithromax over the counter – zithromax canadian pharmacy
clonidine 100mcg
http://furosemide.pro/# lasix for sale
albuterol prices
prescription drug prices lisinopril: buy lisinopril online – price for 5 mg lisinopril
https://azithromycin.store/# zithromax online pharmacy canada
п»їcytotec pills online: Buy Abortion Pills Online – buy cytotec in usa
https://furosemide.pro/# furosemide 100mg
purchase retin a .05
generic zithromax online paypal zithromax best price purchase zithromax online
https://finasteride.men/# cost generic propecia price
lisinopril prescription coupon: cheapest lisinopril – lisinopril 12.5 mg 10 mg
vermox 100 mg otc
https://lisinopril.fun/# zestril 10 mg online
lisinopril 10 mg order online: buy lisinopril online – lisinopril 30 mg cost
robaxin 750 canada
paroxetine 40 mg cost
Abortion pills online: Buy Abortion Pills Online – buy cytotec
amoxicillin usa
http://furosemide.pro/# lasix dosage
25 mg atarax
generic for propecia
lasix online lasix dosage lasix 40mg
prescription drug zestril: buy lisinopril canada – lisinopril 20 mg online
https://azithromycin.store/# zithromax 250
vardenafil buy online
generic propecia tablets: Buy finasteride 1mg – buying propecia
https://azithromycin.store/# zithromax online
https://furosemide.pro/# lasix 40 mg
cost of propecia no prescription: Best place to buy propecia – cost of cheap propecia price
https://lisinopril.fun/# generic lisinopril 3973
Cytotec 200mcg price: buy cytotec online – Cytotec 200mcg price
where can i get zithromax over the counter buy zithromax over the counter zithromax online
https://finasteride.men/# cost cheap propecia without insurance
lisinopril generic price comparison: buy lisinopril canada – lisinopril without an rx
generic levitra 2018
lisinopril buy without prescription: cheapest lisinopril – buy lisinopril 20 mg without prescription
lisinopril brand name uk: buy lisinopril canada – prinivil medication
buy lexapro brand name online
http://misoprostol.shop/# purchase cytotec
http://finasteride.men/# cost generic propecia
sildenafil over the counter nz
farmacie online sicure: Cialis senza ricetta – comprare farmaci online con ricetta
http://avanafilitalia.online/# farmacie online affidabili
order vardenafil online
migliori farmacie online 2023: farmacia online miglior prezzo – farmacie online sicure
п»їfarmacia online migliore: cialis generico – comprare farmaci online con ricetta
buy zyban online canada
http://sildenafilitalia.men/# cerco viagra a buon prezzo
wellbutrin otc
acquistare farmaci senza ricetta kamagra gold farmacia online piГ№ conveniente
farmacia online migliore: avanafil – farmacia online migliore
http://sildenafilitalia.men/# viagra originale in 24 ore contrassegno
http://farmaciaitalia.store/# farmacia online senza ricetta
trazodone price uk
comprare farmaci online all’estero: kamagra gel – acquisto farmaci con ricetta
buy prednisone online fast shipping
http://kamagraitalia.shop/# acquisto farmaci con ricetta
п»їfarmacia online migliore: farmacia online – farmacie online sicure
augmentin tablets 625mg
dove acquistare viagra in modo sicuro: viagra generico – viagra online spedizione gratuita
order phenergan
lisinopril 25 mg cost
where can i get doxycycline
farmacia online cialis prezzo farmacia online piГ№ conveniente
http://tadalafilitalia.pro/# top farmacia online
http://kamagraitalia.shop/# farmacia online senza ricetta
farmacia online piГ№ conveniente: farmacia online piu conveniente – comprare farmaci online all’estero
http://avanafilitalia.online/# comprare farmaci online all’estero
amoxicillin for sale mexico
farmacia online: Dove acquistare Cialis online sicuro – comprare farmaci online all’estero
viagra price online india
https://avanafilitalia.online/# farmaci senza ricetta elenco
clonidine for tics
https://farmaciaitalia.store/# farmacia online senza ricetta
siti sicuri per comprare viagra online viagra generico farmacia senza ricetta recensioni
farmacie on line spedizione gratuita: Avanafil farmaco – farmacia online piГ№ conveniente
top online pharmacy india
https://kamagraitalia.shop/# farmacie online autorizzate elenco
https://tadalafilitalia.pro/# farmacia online migliore
viagra online spedizione gratuita: viagra consegna in 24 ore pagamento alla consegna – cialis farmacia senza ricetta
farmaci senza ricetta elenco: kamagra – farmacia online
generic diflucan
600 mg gabapentin tablet
https://canadapharm.shop/# pharmacy rx world canada
mexican border pharmacies shipping to usa: purple pharmacy mexico price list – mexico pharmacies prescription drugs
baclofen cost uk
cost of accutane canada
canadian pharmacies comparison: canadian pharmacy meds review – canadian pharmacy ratings
025 mg synthroid
best online pharmacy india: top 10 online pharmacy in india – india pharmacy mail order
vardenafil brand
rate canadian pharmacies: canadian pharmacy review – canadian pharmacies compare
http://indiapharm.life/# indian pharmacy paypal
toradol 15 mg tablet
order azithromycin online
canadian pharmacy 24: canadian king pharmacy – canadian pharmacy tampa
http://canadapharm.shop/# pharmacy canadian superstore
buy drugs from canada canadian pharmacy 365 canadian family pharmacy
atarax 10mg
how much is citalopram uk
canadian pharmacy phone number: canadian online pharmacy – canadian discount pharmacy
http://canadapharm.shop/# safe canadian pharmacy
canada pharmacy online legit: canadian medications – canadian pharmacy world
best mail order pharmacy canada: safe online pharmacies in canada – canada cloud pharmacy
reputable indian pharmacies: top online pharmacy india – indianpharmacy com
viagra levitra
buy levitra no prescription
mexico pharmacies prescription drugs: buying from online mexican pharmacy – mexico drug stores pharmacies
https://canadapharm.shop/# canadian pharmacy in canada
http://canadapharm.shop/# canadian pharmacies compare
inderal australia
legit canadian pharmacy online ordering drugs from canada canadian pharmacy service
top online pharmacy india: Online medicine order – indian pharmacy paypal
buying from online mexican pharmacy: mexican border pharmacies shipping to usa – best online pharmacies in mexico
https://mexicanpharm.store/# mexican mail order pharmacies
amoxicillin 500mg price in usa
indianpharmacy com: п»їlegitimate online pharmacies india – top online pharmacy india
https://canadapharm.shop/# maple leaf pharmacy in canada
buy ivermectin
best canadian online pharmacy reviews: canadapharmacyonline legit – reliable canadian pharmacy reviews
https://canadapharm.shop/# reputable canadian online pharmacies
india pharmacy mail order: mail order pharmacy india – best india pharmacy
https://indiapharm.life/# indian pharmacy
indian pharmacy paypal: indian pharmacy paypal – buy medicines online in india
azithromycin from mexico
indianpharmacy com: best online pharmacy india – top online pharmacy india
http://canadapharm.shop/# canadian online drugs
buying from canadian pharmacies recommended canadian pharmacies canadian drug pharmacy
canadian pharmacy 1 internet online drugstore: cheap canadian pharmacy – my canadian pharmacy
no prescription albuterol fast delivery
https://indiapharm.life/# india pharmacy mail order
prozac 25mg
bactrim tablet online
pharmacy website india: top online pharmacy india – indianpharmacy com
http://mexicanpharm.store/# mexican pharmaceuticals online
best canadian pharmacy online: precription drugs from canada – pharmacy wholesalers canada
http://canadapharm.shop/# canadian pharmacies
india online pharmacy: indian pharmacies safe – online shopping pharmacy india
best retin a
https://indiapharm.life/# india pharmacy mail order
025 mg synthroid
https://clomidpharm.shop/# order cheap clomid without dr prescription
They offer the best prices on international brands http://prednisonepharm.store/# prednisone uk
prednisone tabs 20 mg: where to buy prednisone 20mg – prednisone 20mg price
prozac 80 mg
https://prednisonepharm.store/# prednisone 5 50mg tablet price
allopurinol 300 mg for sale
clonidine hcl 2mg
buy doxycycline united states
http://zithromaxpharm.online/# zithromax 500
Global expertise that’s palpable with every service http://clomidpharm.shop/# where buy cheap clomid now
buy cytotec online buy cytotec online fast delivery buy cytotec over the counter
buy suhagra 25 mg
zithromax capsules price: zithromax 500 mg for sale – zithromax price canada
fluoxetine cost in india
http://prednisonepharm.store/# can you buy prednisone without a prescription
generic allopurinol 100mg
safe and effective drugs are available https://nolvadex.pro/# tamoxifen men
generic amoxil online
buy prednisone online india: can you buy prednisone in canada – can i order prednisone
Always greeted with warmth and professionalism https://cytotec.directory/# buy cytotec over the counter
https://cytotec.directory/# order cytotec online
http://clomidpharm.shop/# cost of clomid
buy clomid
accutane india pharmacy
The best choice for personalized care http://zithromaxpharm.online/# buy cheap generic zithromax
clonidime
buy cheap clomid without dr prescription: generic clomid online – order clomid price
http://nolvadex.pro/# femara vs tamoxifen
zithromax 500 mg lowest price pharmacy online how to buy zithromax online purchase zithromax online
colchicine where to buy
azithromycin 200mg
https://prednisonepharm.store/# prednisone 80 mg daily
how much is zithromax 250 mg: buy generic zithromax no prescription – where can i get zithromax
Their global outlook is evident in their expansive services http://clomidpharm.shop/# can i get cheap clomid without insurance
amoxil 500mg capsule price
https://zithromaxpharm.online/# can i buy zithromax over the counter
buy citalopram 20 mg
prednisone 54899: prednisone purchase online – prednisone 10mg online
Providing international caliber services consistently https://clomidpharm.shop/# can i get generic clomid pill
atarax 10mg generic
http://clomidpharm.shop/# where buy cheap clomid now
http://zithromaxpharm.online/# zithromax antibiotic
prednisone 20 mg purchase buy prednisone online canada prednisone generic cost
buy cytotec: buy cytotec pills – buy cytotec online fast delivery
Their worldwide delivery system is impeccable http://nolvadex.pro/# tamoxifen estrogen
budesonide pill
viagra without doctor prescription: prescription without a doctor’s prescription – viagra without a doctor prescription
https://edwithoutdoctorprescription.store/# how to get prescription drugs without doctor
canadian pharmaceuticals for usa sales largest canadian pharmacy meds canada
propranolol 60
http://reputablepharmacies.online/# canadian pharmacieswith no prescription
zoloft online europe
propesia
trusted online canadian pharmacy: canadian pharmacies shipping to usa – prescription without a doctor’s prescription
coupon tretinoin
discount prescription drugs prescription drugs ed meds online without doctor prescription
non-generic viagra
http://edpills.bid/# best ed pills non prescription
price of cialis 20mg tablets
synthroid 112 mcg cost
how to buy synthroid
list of canadian pharmacy canada pharmaceuticals online india online pharmacy
drugs without a doctor s prescription http://reputablepharmacies.online/# canadian pharmacy no prescription required
best online pharmacy reviews
most reputable canadian pharmacies: order from canadian pharmacy – buy prescription drugs canada
drugs for ed: best erection pills – cheap erectile dysfunction
http://edpills.bid/# male ed drugs
list of trusted canadian pharmacies my canadian drugstore best canadian pharmacies online
where to get clonidine
discount drugs online: viagra at canadian pharmacy – online pharmacy usa
https://edwithoutdoctorprescription.store/# discount prescription drugs
celexa 60 mg daily
allopurinol price canada
http://reputablepharmacies.online/# top 10 online pharmacies
cialis without doctor prescription prescription drugs non prescription erection pills
canadian pharmacy sildenafil
natural remedies for ed: erectile dysfunction medications – ed remedies
doxycycline 100mg capsules price
what is the best ed pill ed pills online online ed pills
ed meds without doctor prescription https://edwithoutdoctorprescription.store/# ed meds online without doctor prescription
canadian drug store coupon
https://reputablepharmacies.online/# discount pharmaceuticals
order levitra online cheap
where can i purchase diflucan
vardenafil online uk
propecia over the counter canada
ed pills comparison: herbal ed treatment – male ed drugs
best ed medication: new ed drugs – ed meds online
sildenafil without a doctor’s prescription viagra without a doctor prescription best non prescription ed pills
buying amoxicillin in mexico
buy accutane nz
vardenafil 20 mg online
http://edpills.bid/# medication for ed
canadian pharmacy india
where can i get azithromycin pills
synthroid 0.125 mcg
prescription without a doctor’s prescription: buy prescription drugs online without – ed meds online without doctor prescription
canada pharmacy online no script canada pharmacies top best canada pharmacies online
http://reputablepharmacies.online/# mexican pharmacy cialis
discount drug store online shopping: safe canadian internet pharmacies – discount prescriptions
canadian drugstore accutane mexican pharmacy canadian pharmacy without a prescription
buy ozempic pill form for adults
generic semaglutide for weight loss
online pharmacy india: Order medicine from India to USA – top 10 pharmacies in india indianpharmacy.shop
https://indianpharmacy.shop/# online pharmacy india indianpharmacy.shop
india pharmacy Order medicine from India to USA best online pharmacy india indianpharmacy.shop
semaglutide coupon
http://canadianpharmacy.pro/# canadianpharmacymeds canadianpharmacy.pro
wegovy medication
rybelsus tablets buy
buy wegovy canada
semaglutide 7 mg tablet
п»їlegitimate online pharmacies india: Best Indian pharmacy – mail order pharmacy india indianpharmacy.shop
canadian online pharmacy Pharmacies in Canada that ship to the US canadian pharmacy king reviews canadianpharmacy.pro
http://indianpharmacy.shop/# Online medicine home delivery indianpharmacy.shop
https://canadianpharmacy.pro/# legitimate canadian online pharmacies canadianpharmacy.pro
canadian drugs online viagra
mail order pharmacy india international medicine delivery from india indian pharmacy indianpharmacy.shop
my canadian pharmacy reviews: Cheapest drug prices Canada – canadian pharmacy online reviews canadianpharmacy.pro
https://mexicanpharmacy.win/# mexican border pharmacies shipping to usa mexicanpharmacy.win
mexican pharmacy mexican pharmacy online reputable mexican pharmacies online mexicanpharmacy.win
rybelsus
pharmacies in mexico that ship to usa: mexican pharmacy online – medicine in mexico pharmacies mexicanpharmacy.win
https://mexicanpharmacy.win/# mexican drugstore online mexicanpharmacy.win
https://indianpharmacy.shop/# pharmacy website india indianpharmacy.shop
wegovy 7 mg tablet
canadian pharmacy ltd Canada Pharmacy canada discount pharmacy canadianpharmacy.pro
rybelsus sale
http://canadianpharmacy.pro/# online canadian pharmacy reviews canadianpharmacy.pro
online meds without presxription
http://canadianpharmacy.pro/# best online canadian pharmacy canadianpharmacy.pro
rybelsus online cheap
wegovy canada
indianpharmacy com Cheapest online pharmacy online shopping pharmacy india indianpharmacy.shop
wegovy pill
rybelsus
https://mexicanpharmacy.win/# mexican online pharmacies prescription drugs mexicanpharmacy.win
https://canadianpharmacy.pro/# canadian online drugs canadianpharmacy.pro
Online medicine home delivery
canadian drug stores Cheapest drug prices Canada medication canadian pharmacy canadianpharmacy.pro
http://indianpharmacy.shop/# buy medicines online in india indianpharmacy.shop
https://indianpharmacy.shop/# reputable indian pharmacies indianpharmacy.shop
http://mexicanpharmacy.win/# pharmacies in mexico that ship to usa mexicanpharmacy.win
indian pharmacy
rybelsus 3 mg tablet
best online canadian pharmacy Canadian pharmacy online canada discount pharmacy canadianpharmacy.pro
wegovy online pharmacy
wegovy tablets 7 mg
buy semaglutide online pharmacy
https://mexicanpharmacy.win/# mexico drug stores pharmacies mexicanpharmacy.win
https://mexicanpharmacy.win/# mexican pharmaceuticals online mexicanpharmacy.win
reputable indian pharmacies
ozempic tablets
http://indianpharmacy.shop/# reputable indian online pharmacy indianpharmacy.shop
no prescription canadian pharmacies
india online pharmacy indian pharmacy to usa indianpharmacy com indianpharmacy.shop
wegovy semaglutide tablets 7.5 mcg
http://indianpharmacy.shop/# pharmacy website india indianpharmacy.shop
http://indianpharmacy.shop/# india pharmacy mail order indianpharmacy.shop
indianpharmacy com
http://canadianpharmacy.pro/# buying drugs from canada canadianpharmacy.pro
best canadian pharmacy online Canadian pharmacy online buy canadian drugs canadianpharmacy.pro
https://indianpharmacy.shop/# top online pharmacy india indianpharmacy.shop
http://indianpharmacy.shop/# п»їlegitimate online pharmacies india indianpharmacy.shop
indian pharmacy
wegovy online cheap
mexican pharmaceuticals online mexican pharmacy online medicine in mexico pharmacies mexicanpharmacy.win
wegovy tablets for weight loss
http://canadianpharmacy.pro/# canada drugs online canadianpharmacy.pro
world pharmacy india
https://indianpharmacy.shop/# buy medicines online in india indianpharmacy.shop
mexico drug stores pharmacies online mexican pharmacy mexico pharmacies prescription drugs mexicanpharmacy.win
https://pharmadoc.pro/# Pharmacie en ligne livraison 24h
rybelsus semaglutide tablets 3mg
pharmacie ouverte 24/24: pharmacie ouverte – Pharmacie en ligne sans ordonnance
SildГ©nafil 100 mg prix en pharmacie en France Prix du Viagra 100mg en France Viagra gГ©nГ©rique pas cher livraison rapide
http://viagrasansordonnance.pro/# Acheter viagra en ligne livraison 24h
https://cialissansordonnance.shop/# Pharmacie en ligne France
Pharmacie en ligne livraison rapide
buy ozempic for weight loss
Viagra sans ordonnance 24h Amazon: Viagra femme ou trouver – Viagra sans ordonnance 24h Amazon
acheter mГ©dicaments Г l’Г©tranger Pharmacie en ligne livraison gratuite Pharmacie en ligne fiable
https://acheterkamagra.pro/# Acheter médicaments sans ordonnance sur internet
acheter mГ©dicaments Г l’Г©tranger: Acheter Cialis 20 mg pas cher – Pharmacie en ligne sans ordonnance
Pharmacie en ligne livraison rapide kamagra gel Pharmacies en ligne certifiГ©es
generic rybelsus cost
wegovy 7mg
wegovy tablets cost
buy ozempic canada
acheter medicament a l etranger sans ordonnance: levitrasansordonnance.pro – pharmacie ouverte 24/24
semaglutide injection
semaglutide without prescription
wegovy buy from canada
Pharmacie en ligne livraison gratuite: pharmacie en ligne – acheter mГ©dicaments Г l’Г©tranger
https://cialissansordonnance.shop/# Pharmacie en ligne livraison 24h
wegovy order
Pharmacies en ligne certifiГ©es kamagra gel pharmacie ouverte
semaglutide online cheap
wegovy 7 mg tablet
Viagra pas cher livraison rapide france: Acheter du Viagra sans ordonnance – Viagra sans ordonnance 24h Amazon
https://acheterkamagra.pro/# Pharmacie en ligne livraison 24h
Pharmacie en ligne France: п»їpharmacie en ligne – pharmacie ouverte 24/24
Pharmacie en ligne sans ordonnance Levitra 20mg prix en pharmacie Pharmacie en ligne livraison rapide
http://cialissansordonnance.shop/# Pharmacies en ligne certifiées
where to buy ozempic
semaglutide injection
Pharmacie en ligne pas cher: Medicaments en ligne livres en 24h – Acheter mГ©dicaments sans ordonnance sur internet
generic wegovy cost
Acheter mГ©dicaments sans ordonnance sur internet: Levitra pharmacie en ligne – Pharmacies en ligne certifiГ©es
http://cialissansordonnance.shop/# Pharmacie en ligne fiable
semaglutide buy from canada
buy ozempic cheap
wegovy pill form
Pharmacie en ligne sans ordonnance: Levitra pharmacie en ligne – п»їpharmacie en ligne
ozempic tablets 7 mg
rybelsus weight loss
https://azithromycin.bid/# zithromax online pharmacy canada
wegovy xr
wegovy prescription
prednisolone prednisone: cost of prednisone in canada – prednisone 1mg purchase
rybelsus tablets buy
prednisone 5 mg: iv prednisone – prednisone 2.5 mg daily
wegovy pill
amoxicillin 500mg price generic amoxicillin 500mg over the counter amoxicillin canada
order ozempic online
https://clomiphene.icu/# buying clomid tablets
buy semaglutide online
purchase prednisone no prescription: prednisone brand name india – prednisone 40 mg daily
wegovy tab 14mg
stromectol 12mg online ivermectin 6mg tablet for lice ivermectin 200mg
https://amoxicillin.bid/# can you buy amoxicillin over the counter canada
prednisone 10mg tablet price: buy prednisone without prescription paypal – buy prednisone online australia
wegovy for sale
can i buy amoxicillin online: can you buy amoxicillin over the counter – amoxicillin pills 500 mg
https://prednisonetablets.shop/# prednisone 30 mg tablet
wegovy without prescription
buy ozempic from canada
where to buy cheap clomid online where can i buy clomid without a prescription generic clomid without rx
http://amoxicillin.bid/# amoxacillian without a percription
zithromax z-pak: buy generic zithromax no prescription – zithromax azithromycin
wegovy generic cost
order prednisone on line can you buy prednisone online uk where to get prednisone
amoxicillin 875 mg tablet: amoxicillin over the counter in canada – amoxicillin over the counter in canada
http://azithromycin.bid/# zithromax 1000 mg pills
rybelsus without prescription
cost of clomid pill: get clomid without a prescription – can i order cheap clomid no prescription
buy semaglutide from canada online
cost of ivermectin: stromectol 3 mg tablet – stromectol nz
http://prednisonetablets.shop/# prednisone 20 mg prices
cost cheap clomid now how to buy cheap clomid prices can i get cheap clomid without prescription
rybelsus
https://prednisonetablets.shop/# can you buy prednisone online uk
can you buy cheap clomid without dr prescription: cost of clomid – can i order generic clomid pills
https://clomiphene.icu/# get clomid online
semaglutide for diabetes
ivermectin 0.5% lotion ivermectin 20 mg ivermectin 1 cream generic
buy wegovy online no script needed
wegovy 7mg
can i buy amoxicillin over the counter: amoxicillin 500mg – order amoxicillin no prescription
get generic clomid pills: get generic clomid – how can i get clomid tablets
wegovy semaglutide tablets 7.5 mcg
where can i buy semaglutide
https://ivermectin.store/# ivermectin australia
wegovy from canada
buy ozempic in mexico
buy ozempic canada
buy amoxicillin 500mg usa cheap amoxicillin 500mg 875 mg amoxicillin cost
generic rybelsus for weight loss
buy prednisone nz: generic prednisone tablets – non prescription prednisone 20mg
rybelsus 7mg
https://ivermectin.store/# ivermectin 18mg
buy semaglutide pill form for adults
buy rybelsus in canada
http://mexicanpharm.shop/# mexico pharmacies prescription drugs mexicanpharm.shop
rybelsus retail price
india online pharmacy: Indian pharmacy to USA – pharmacy website india indianpharm.store
reddit canadian pharmacy: Best Canadian online pharmacy – legitimate canadian online pharmacies canadianpharm.store
77 canadian pharmacy trusted canadian pharmacy canadian world pharmacy canadianpharm.store
india pharmacy: order medicine from india to usa – reputable indian pharmacies indianpharm.store
http://canadianpharm.store/# canadian pharmacy ed medications canadianpharm.store
mexican drugstore online: Certified Pharmacy from Mexico – medication from mexico pharmacy mexicanpharm.shop
semaglutide online pharmacy
mexican pharmacy medication from mexico pharmacy п»їbest mexican online pharmacies mexicanpharm.shop
http://indianpharm.store/# reputable indian pharmacies indianpharm.store
rybelsus mexico
mexican online pharmacies prescription drugs: mexican online pharmacies prescription drugs – medicine in mexico pharmacies mexicanpharm.shop
order rybelsus online
legitimate canadian pharmacies Licensed Online Pharmacy canadian 24 hour pharmacy canadianpharm.store
wegovy best price
https://indianpharm.store/# indian pharmacies safe indianpharm.store
indian pharmacy online: п»їlegitimate online pharmacies india – reputable indian online pharmacy indianpharm.store
online pharmacy india: international medicine delivery from india – indianpharmacy com indianpharm.store
canadian pharmacy mall: Pharmacies in Canada that ship to the US – reputable canadian pharmacy canadianpharm.store
https://indianpharm.store/# best online pharmacy india indianpharm.store
buy semaglutide online canada
semaglutide online order
rybelsus lose weight
canadian neighbor pharmacy Best Canadian online pharmacy buying from canadian pharmacies canadianpharm.store
semaglutide rybelsus
https://indianpharm.store/# legitimate online pharmacies india indianpharm.store
reputable indian online pharmacy: order medicine from india to usa – best india pharmacy indianpharm.store
rybelsus generic cost
semaglutide buy australia
wegovy tab 14mg
cheapest pharmacy canada: Canada Pharmacy online – buy canadian drugs canadianpharm.store
https://mexicanpharm.shop/# mexican mail order pharmacies mexicanpharm.shop
reliable canadian pharmacy reviews Licensed Online Pharmacy pharmacy canadian canadianpharm.store
generic rybelsus for weight loss
semaglutide xl
online shopping pharmacy india: order medicine from india to usa – indianpharmacy com indianpharm.store
buy semaglutide uk
https://canadianpharm.store/# online canadian pharmacy review canadianpharm.store
wegovy where to buy
indian pharmacy: order medicine from india to usa – buy medicines online in india indianpharm.store
mexican rx online: Certified Pharmacy from Mexico – buying prescription drugs in mexico mexicanpharm.shop
buy rybelsus online no script needed
legit canadian online pharmacy: Licensed Online Pharmacy – canada rx pharmacy canadianpharm.store
http://indianpharm.store/# best online pharmacy india indianpharm.store
https://mexicanpharm.shop/# medication from mexico pharmacy mexicanpharm.shop
semaglutide coupon
rybelsus for sale
india pharmacy: order medicine from india to usa – top 10 pharmacies in india indianpharm.store
rybelsus diabetes medication
reputable indian pharmacies order medicine from india to usa best online pharmacy india indianpharm.store
https://canadianpharm.store/# reputable canadian pharmacy canadianpharm.store
semaglutide diabetes medication
buy medicines online in india: international medicine delivery from india – indianpharmacy com indianpharm.store
Online medicine home delivery: international medicine delivery from india – п»їlegitimate online pharmacies india indianpharm.store
https://mexicanpharm.shop/# mexico drug stores pharmacies mexicanpharm.shop
india pharmacy mail order order medicine from india to usa indianpharmacy com indianpharm.store
ozempic semaglutide
wegovy
best india pharmacy: indian pharmacy online – cheapest online pharmacy india indianpharm.store
indian pharmacy paypal: international medicine delivery from india – best india pharmacy indianpharm.store
semaglutide price
buy semaglutide online canada
https://indianpharm.store/# buy prescription drugs from india indianpharm.store
wegovy price
https://canadianpharm.store/# best rated canadian pharmacy canadianpharm.store
pharmacy canadian Certified Online Pharmacy Canada canadian pharmacy 24h com safe canadianpharm.store
rybelsus over the counter
canadian pharmacy no rx needed: Canadian Pharmacy – safe reliable canadian pharmacy canadianpharm.store
where to buy ozempic
where to buy semaglutide
ozempic pill form
buy semaglutide online no script needed
https://mexicanpharm.shop/# mexican mail order pharmacies mexicanpharm.shop
best online pharmacy india: Online medicine order – buy prescription drugs from india indianpharm.store
buy rybelsus online no script needed
canadian mail order pharmacy Canadian Pharmacy legit canadian online pharmacy canadianpharm.store
buying prescription drugs in mexico online: Certified Pharmacy from Mexico – buying from online mexican pharmacy mexicanpharm.shop
canadian pharmacies: Canadian International Pharmacy – canadapharmacyonline legit canadianpharm.store
http://mexicanpharm.shop/# mexico drug stores pharmacies mexicanpharm.shop
semaglutide generic
https://canadadrugs.pro/# prescription without a doctors prescription
cheap ozempic
online pharmacies canadian: canadian pharmacy products – mexican pharmacy online reviews
rybelsus
medicine from canada with no prescriptions canadian pharmacy presription and meds reliable canadian pharmacy
order semaglutide online
semaglutide cost
reputable canadian mail order pharmacies: certified online canadian pharmacies – safe reliable canadian pharmacy
http://canadadrugs.pro/# best mail order canadian pharmacy
wegovy tablets 7 mg
meds without a doctor s prescription canada: canadian pharmaceuticals online – certified online canadian pharmacies
wegovy buy australia
canadian pharmacy direct international pharmacy prescription drug pricing
http://canadadrugs.pro/# cost prescription drugs
ozempic tablets for weight loss cost
semaglutide buy uk
semaglutide rybelsus
canadian drug store prices: list of canadian pharmacy – pharmacies canada
rybelsus prescription
canadian pharmacy: online pharmacy no prescription necessary – canadian rx pharmacy
best online pharmacies without a script buy drugs online drugs online
rybelsus tablets cost
buy semaglutide online no script needed
prescription drugs without prescription: certified canadian online pharmacy – mail order pharmacies
http://canadadrugs.pro/# reliable mexican pharmacy
approved canadian pharmacies online: world pharmacy – cheap canadian drugs
buy ozempic online pharmacy
buy semaglutide from india
no prescription drugs canada canadadrugpharmacy discount prescription drugs online
wegovy australia online
https://canadadrugs.pro/# canada pharmacies
internet pharmacies: canadian pharmacy testosterone – no prescription canadian drugs
rybelsus tablets for weight loss cost
wegovy 7mg
buy semaglutide
canada pharmacy online reviews: reputable mexican pharmacies – buy prescription drugs online legally
http://canadadrugs.pro/# canadian mail order pharmacy reviews
canadian drug store: reputable canadian pharmacy online – best canadian pharmacy no prescription
canadian pharmacy price checker: internet pharmacy list – my canadian drug store
buy prescription drugs without doctor: mail order pharmacy canada – best online pharmacies canada
https://canadadrugs.pro/# trusted online pharmacy
order wegovy online
discount canadian drugs: medicine from canada with no prescriptions – my canadian pharmacy online
semaglutide diabetes
rybelsus lose weight
rybelsus where to buy
https://canadadrugs.pro/# most trusted canadian online pharmacies
viagra no prescription canadian pharmacy: discount prescription drugs – best canadian pharmacies online
wegovy diabetes medication
http://canadadrugs.pro/# top online pharmacies
canadian generic pharmacy: nabp approved canadian pharmacies – best rated canadian pharmacy
pharmacy drug store: canada drug stores – canadian pharmacy online canada
rybelsus 14
semaglutide 14
https://canadadrugs.pro/# discount canadian drugs
rybelsus 3mg
northwestpharmacy com: canadian drug store legit – canadian overnight pharmacy
medicin without prescription: canada online pharmacy reviews – compare prescription drug prices
where can i buy ozempic
buy rybelsus in canada
buy semaglutide cheap
https://canadadrugs.pro/# my canadian family pharmacy
buy ozempic canada
order ozempic online
trust online pharmacies: mexican drug pharmacy – top 10 mail order pharmacies
http://medicinefromindia.store/# indian pharmacy paypal
semaglutide online
reputable indian pharmacies: top 10 pharmacies in india – reputable indian pharmacies
viagra without a doctor prescription levitra without a doctor prescription cialis without doctor prescription
http://edpill.cheap/# best erectile dysfunction pills
ed pills cheap: top rated ed pills – herbal ed treatment
mexico drug stores pharmacies: pharmacies in mexico that ship to usa – mexico pharmacies prescription drugs
rybelsus tablets cost
pills for erection ed medications list best otc ed pills
buy ozempic from canada online
wegovy diabetes
http://edwithoutdoctorprescription.pro/# real viagra without a doctor prescription usa
rybelsus diabetes
wegovy buy from canada
pills for ed: what is the best ed pill – ed pill
п»їerectile dysfunction medication ed meds online natural remedies for ed
wegovy semaglutide tablets
semaglutide medication
http://canadianinternationalpharmacy.pro/# canadian pharmacy 365
rybelsus generic cost
levitra without a doctor prescription prescription drugs meds online without doctor prescription
ed medication online: best ed treatment – best treatment for ed
wegovy buy online
https://certifiedpharmacymexico.pro/# mexican mail order pharmacies
semaglutide tablets 7 mg
rybelsus 14
order ozempic online
legal canadian pharmacy online northwest canadian pharmacy reliable canadian pharmacy reviews
https://certifiedpharmacymexico.pro/# mexico drug stores pharmacies
wegovy prescription
buy wegovy canada
canadian pharmacy world: canadian discount pharmacy – canada ed drugs
buy ozempic online pharmacy
semaglutide pills
http://edwithoutdoctorprescription.pro/# buy prescription drugs from india
canada drugs online reviews northern pharmacy canada canada drug pharmacy
http://edwithoutdoctorprescription.pro/# viagra without a doctor prescription
what are ed drugs: erectile dysfunction medications – best pills for ed
canadian pharmacy king reviews: canadian drugstore online – canadian pharmacies that deliver to the us
cure ed best ed treatment pills best ed medications
where can i buy semaglutide
http://canadianinternationalpharmacy.pro/# buy canadian drugs
semaglutide buy from canada
reputable mexican pharmacies online medication from mexico pharmacy buying prescription drugs in mexico
https://canadianinternationalpharmacy.pro/# canadian pharmacy tampa
wegovy online prescription
rybelsus rx
ozempic for weight loss
rybelsus medicine
canadian pharmacy scam canadian pharmacies compare canadian pharmacies
https://edwithoutdoctorprescription.pro/# non prescription ed pills
order semaglutide
non prescription ed pills: cialis without a doctor prescription – prescription drugs online without doctor
https://canadianinternationalpharmacy.pro/# ordering drugs from canada
cheapest ed pills online erectile dysfunction drug generic ed pills
https://canadianinternationalpharmacy.pro/# adderall canadian pharmacy
100mg viagra without a doctor prescription ed pills without doctor prescription prescription drugs online without doctor
wegovy semaglutide
generic wegovy for weight loss
buy ozempic from canada
http://medicinefromindia.store/# pharmacy website india
ozempic generic
canadian drug stores thecanadianpharmacy canadian pharmacy prices
wegovy buy from canada
canadian pharmacies comparison: canadian pharmacy – canadian pharmacy tampa
http://edpill.cheap/# ed pills otc
where to buy semaglutide online
best online pharmacy india indian pharmacy online shopping pharmacy india
https://edpill.cheap/# ed drugs
rybelsus without prescription
buy wegovy online from india
semaglutide 3mg
https://edpill.cheap/# best ed pills
ozempic injections
mexican online pharmacies prescription drugs reputable mexican pharmacies online mexican pharmaceuticals online
ozempic tablets buy
wegovy tablets for weight loss cost
wegovy buy uk
https://certifiedpharmacymexico.pro/# pharmacies in mexico that ship to usa
mexico drug stores pharmacies: mexican border pharmacies shipping to usa – buying from online mexican pharmacy
Online medicine order Online medicine home delivery india pharmacy
http://medicinefromindia.store/# pharmacy website india
https://edwithoutdoctorprescription.pro/# levitra without a doctor prescription
purchase rybelsus
buy cheap prescription drugs online ed pills without doctor prescription discount prescription drugs
buy semaglutide canada
buy semaglutide from canada online
http://edpill.cheap/# ed treatment review
online ed pills best ed drug best ed drugs
semaglutide oral medication
http://certifiedpharmacymexico.pro/# pharmacies in mexico that ship to usa
ed meds online without doctor prescription: cialis without a doctor’s prescription – buy prescription drugs without doctor
wegovy pills
prescription drugs online without cheap cialis buy prescription drugs online
wegovy xl
mexico pharmacies prescription drugs pharmacies in mexico that ship to usa mexico drug stores pharmacies
mexican drugstore online medicine in mexico pharmacies buying prescription drugs in mexico online
mexico drug stores pharmacies reputable mexican pharmacies online pharmacies in mexico that ship to usa
rybelsus rx
medication from mexico pharmacy mexico drug stores pharmacies mexico pharmacy
http://mexicanph.shop/# mexico pharmacies prescription drugs
mexican drugstore online
where to buy ozempic
mexico pharmacy mexican rx online mexican border pharmacies shipping to usa
wegovy 7mg
rybelsus prescription
semaglutide tab 7mg
semaglutide medication
purple pharmacy mexico price list buying prescription drugs in mexico mexican online pharmacies prescription drugs
semaglutide 21 mg
mexican drugstore online buying from online mexican pharmacy mexico pharmacies prescription drugs
rybelsus from canada
buy ozempic
buying prescription drugs in mexico mexican pharmacy mexican pharmaceuticals online
mexican rx online mexican border pharmacies shipping to usa mexico drug stores pharmacies
https://mexicanph.com/# mexico pharmacies prescription drugs
medication from mexico pharmacy
buy rybelsus
purchase ozempic
rybelsus order
mexican online pharmacies prescription drugs medication from mexico pharmacy mexican border pharmacies shipping to usa
semaglutide 3mg
semaglutide price
buy ozempic in mexico
purple pharmacy mexico price list mexico pharmacy mexican rx online
purple pharmacy mexico price list mexico pharmacies prescription drugs mexican border pharmacies shipping to usa
mexican border pharmacies shipping to usa purple pharmacy mexico price list mexican pharmacy
semaglutide cost
semaglutide for weight loss without diabetes
http://mexicanph.shop/# mexico pharmacies prescription drugs
mexican online pharmacies prescription drugs
medicine in mexico pharmacies mexican pharmacy mexican pharmaceuticals online
buy semaglutide pill form for adults
mexico drug stores pharmacies mexican rx online buying prescription drugs in mexico
mexico drug stores pharmacies п»їbest mexican online pharmacies medicine in mexico pharmacies
buy ozempic online
wegovy oral medication
mexican pharmaceuticals online mexican drugstore online purple pharmacy mexico price list
semaglutide diabetes
https://mexicanph.com/# mexico drug stores pharmacies
mexican rx online
reputable mexican pharmacies online best online pharmacies in mexico pharmacies in mexico that ship to usa
generic semaglutide
mexico pharmacy buying prescription drugs in mexico medication from mexico pharmacy
mexican rx online mexican rx online mexican rx online
mexico drug stores pharmacies mexican drugstore online mexican online pharmacies prescription drugs
rybelsus best price
medication from mexico pharmacy buying prescription drugs in mexico online buying prescription drugs in mexico
medicine in mexico pharmacies purple pharmacy mexico price list purple pharmacy mexico price list
wegovy pill form
wegovy prescription
rybelsus tablets 7 mg
medication from mexico pharmacy medication from mexico pharmacy mexico drug stores pharmacies
buying prescription drugs in mexico online mexico pharmacy mexico drug stores pharmacies
semaglutide 21 mg
http://mexicanph.shop/# п»їbest mexican online pharmacies
mexican drugstore online
ozempic tablets cost
mexican pharmacy mexico pharmacy pharmacies in mexico that ship to usa
medicine in mexico pharmacies buying prescription drugs in mexico reputable mexican pharmacies online
purchase rybelsus
rybelsus for diabetes
wegovy semaglutide
buying prescription drugs in mexico online mexican mail order pharmacies mexico drug stores pharmacies
purple pharmacy mexico price list mexican rx online mexican rx online
buying prescription drugs in mexico online pharmacies in mexico that ship to usa mexican drugstore online
rybelsus medicine
semaglutide canada pharmacy
wegovy uk
mexican mail order pharmacies purple pharmacy mexico price list buying prescription drugs in mexico
pharmacies in mexico that ship to usa mexican pharmacy mexican pharmaceuticals online
mexico drug stores pharmacies medicine in mexico pharmacies mexican border pharmacies shipping to usa
buying prescription drugs in mexico pharmacies in mexico that ship to usa mexico pharmacy
https://mexicanph.shop/# buying prescription drugs in mexico
purple pharmacy mexico price list
medication from mexico pharmacy п»їbest mexican online pharmacies mexican mail order pharmacies
purple pharmacy mexico price list best online pharmacies in mexico mexico drug stores pharmacies
semaglutide prescription
mexican pharmacy pharmacies in mexico that ship to usa best online pharmacies in mexico
pharmacies in mexico that ship to usa medicine in mexico pharmacies mexican pharmaceuticals online
wegovy tab 3mg
reputable mexican pharmacies online reputable mexican pharmacies online pharmacies in mexico that ship to usa
buying prescription drugs in mexico online medication from mexico pharmacy mexico pharmacies prescription drugs
buy rybelsus canada
buy semaglutide cheap
pharmacies in mexico that ship to usa pharmacies in mexico that ship to usa mexican online pharmacies prescription drugs
mexico pharmacies prescription drugs pharmacies in mexico that ship to usa best online pharmacies in mexico
purple pharmacy mexico price list buying prescription drugs in mexico online buying prescription drugs in mexico online
pharmacies in mexico that ship to usa buying from online mexican pharmacy mexico pharmacy
generic ozempic for weight loss
buy wegovy
mexican pharmaceuticals online buying prescription drugs in mexico online medicine in mexico pharmacies
http://mexicanph.shop/# mexican mail order pharmacies
purple pharmacy mexico price list
purple pharmacy mexico price list mexican pharmaceuticals online medication from mexico pharmacy
wegovy for diabetes
mexican mail order pharmacies mexican border pharmacies shipping to usa mexican drugstore online
medicine in mexico pharmacies mexican pharmacy purple pharmacy mexico price list
mexican drugstore online buying prescription drugs in mexico mexican drugstore online
mexico pharmacy mexico pharmacies prescription drugs best online pharmacies in mexico
rybelsus from canada
medicine in mexico pharmacies mexico pharmacies prescription drugs mexican rx online
wegovy 7 mg
buying from online mexican pharmacy reputable mexican pharmacies online buying prescription drugs in mexico
buying prescription drugs in mexico mexican rx online reputable mexican pharmacies online
rybelsus pill
buying prescription drugs in mexico pharmacies in mexico that ship to usa buying from online mexican pharmacy
mexican rx online mexican rx online medicine in mexico pharmacies
buy semaglutide pill form for adults
wegovy pill
mexican drugstore online mexican pharmacy mexico pharmacy
rybelsus buy uk
mexican online pharmacies prescription drugs mexican pharmaceuticals online mexican mail order pharmacies
mexican online pharmacies prescription drugs mexican rx online medicine in mexico pharmacies
rybelsus canada pharmacy
generic wegovy cost
reputable mexican pharmacies online buying prescription drugs in mexico best online pharmacies in mexico
where to buy semaglutide online
rybelsus australia online
mexico drug stores pharmacies purple pharmacy mexico price list medicine in mexico pharmacies
wegovy online prescription
mexican drugstore online buying prescription drugs in mexico online best online pharmacies in mexico
mexico drug stores pharmacies mexico drug stores pharmacies medicine in mexico pharmacies
semaglutide tablets for weight loss cost
best mexican online pharmacies medicine in mexico pharmacies best online pharmacies in mexico
wegovy pill
semaglutide buy online
semaglutide without prescription
buying prescription drugs in mexico buying prescription drugs in mexico medicine in mexico pharmacies
order rybelsus
wegovy 14
buy semaglutide online
http://mexicanph.com/# mexican online pharmacies prescription drugs
mexico drug stores pharmacies
best mexican online pharmacies mexico drug stores pharmacies buying from online mexican pharmacy
mexico drug stores pharmacies mexico pharmacy mexican drugstore online
ozempic tab 7mg
wegovy generic cost
mexican pharmaceuticals online best online pharmacies in mexico mexican rx online
buy rybelsus in canada
buy wegovy from canada
mexican pharmacy mexico pharmacies prescription drugs medicine in mexico pharmacies
wegovy where to buy
mexico pharmacy buying prescription drugs in mexico online best online pharmacies in mexico
rybelsus for diabetes
ivermectin 3 ivermectin 50 mg buy stromectol online
http://lisinopril.top/# buy lisinopril 10 mg online
rybelsus tab 3mg
zestril 40 mg tablet: can i buy lisinopril online – cost of lisinopril 40 mg
https://lisinopril.top/# lisinopril 40 mg on line
semaglutide rybelsus
https://lisinopril.top/# lisinopril buy in canada
buy semaglutide cheap
amoxicillin tablets in india amoxicillin 500 coupon purchase amoxicillin 500 mg
can you buy amoxicillin over the counter: where can i buy amoxicillin online – amoxicillin 500mg no prescription
https://lisinopril.top/# purchase lisinopril online
wegovy online order
wegovy tablets cost
semaglutide xl
https://lisinopril.top/# order lisinopril
cost of prinivil: lisinopril 5 mg buy online – buy 20mg lisinopril
where can i buy amoxicillin without prec generic amoxicillin online how much is amoxicillin
ozempic for weight loss
http://furosemide.guru/# buy lasix online
https://stromectol.fun/# stromectol buy
amoxicillin without a prescription: amoxicillin 500mg buy online uk – amoxicillin where to get
semaglutide pill
buying lisinopril online where can i buy zestril prinivil 10 mg tablet
wegovy semaglutide tablets
http://lisinopril.top/# lisinopril 20 25 mg tab
buy semaglutide pill form for adults
wegovy price
buy lasix online: Buy Lasix No Prescription – lasix online
http://furosemide.guru/# lasix generic name
buy semaglutide online
lasix generic Buy Lasix No Prescription lasix medication
semaglutide prescription
ozempic tablets
http://lisinopril.top/# lisinopril 3760
ozempic tablets
https://amoxil.cheap/# amoxicillin capsule 500mg price
rybelsus lose weight
prednisone 50 mg buy: prednisone 4 mg daily – prednisone cream
http://stromectol.fun/# stromectol tablets for humans for sale
rybelsus 14mg tablets
buy ozempic from canada online
prednisone buy cheap prednisone acetate prednisone 10mg for sale
http://furosemide.guru/# lasix tablet
rybelsus without prescription
ivermectin 15 mg: ivermectin rx – stromectol uk
ozempic tab 7mg
semaglutide best price
buy wegovy in canada
wegovy 3 mg tablet
ozempic
https://furosemide.guru/# lasix generic
rybelsus diabetes medication
ivermectin humans stromectol xl how much does ivermectin cost
buying prednisone mexico: prednisone daily – prednisone buy
https://stromectol.fun/# stromectol lotion
purchase semaglutide
prednisone pharmacy prices: prednisone 54899 – order prednisone
https://stromectol.fun/# stromectol generic name
http://lisinopril.top/# buy lisinopril 20 mg online
ozempic for weight loss without diabetes
ampicillin amoxicillin amoxicillin capsules 250mg amoxicillin over counter
wegovy tab 7mg
order amoxicillin online: amoxicillin medicine – amoxicillin 500mg without prescription
https://stromectol.fun/# ivermectin 3mg tab
https://amoxil.cheap/# amoxicillin discount
lasix for sale: Buy Lasix – lasix 100 mg
order semaglutide online
amoxicillin 500 mg online amoxicillin for sale online where can i buy amoxocillin
buy rybelsus canada
wegovy semaglutide tablets cost
https://furosemide.guru/# furosemide 40mg
prednisone 10 mg: prednisone 10 mg tablet – 40 mg prednisone pill
https://furosemide.guru/# furosemide 100mg
wegovy buy from canada
buy ozempic online pharmacy
lasix medication Over The Counter Lasix lasix medication
https://amoxil.cheap/# amoxicillin 50 mg tablets
buy furosemide online: Buy Lasix No Prescription – lasix tablet
http://stromectol.fun/# ivermectin stromectol
semaglutide uk
https://stromectol.fun/# ivermectin price
generic wegovy for weight loss
lasix tablet: Over The Counter Lasix – buy furosemide online
flagyl dosage for bv
rybelsus 3mg
rybelsus 7 mg
prednisone pill order prednisone online canada non prescription prednisone 20mg
rybelsus canada pharmacy prices
https://furosemide.guru/# lasix pills
amoxicillin online purchase: cost of amoxicillin – amoxicillin buy online canada
http://furosemide.guru/# lasix for sale
rybelsus semaglutide tablets cost
wegovy 14mg tablets
cost for generic lisinopril lisinopril 20 pills lisinopril brand name in india
lasix medication: Buy Furosemide – lasix 40mg
http://lisinopril.top/# lisinopril pill 40 mg
http://stromectol.fun/# minocycline 100 mg otc
buy ozempic from canada
http://buyprednisone.store/# prednisone buy online nz
stromectol in canada: ivermectin 0.5 lotion india – stromectol price uk
buy ozempic
ivermectin lice oral stromectol pill ivermectin buy nz
ozempic for weight loss without diabetes
http://amoxil.cheap/# cost of amoxicillin 30 capsules
stromectol sales: ivermectin generic cream – ivermectin pill cost
rybelsus 7mg
http://buyprednisone.store/# can i buy prednisone from canada without a script
amoxicillin 500mg prescription amoxicillin 250 mg capsule how to get amoxicillin
https://buyprednisone.store/# prednisone buy
glucophage anorexia
why are my feet still swollen after taking lasix
wegovy semaglutide tablets
generic ozempic for weight loss
lasix side effects: Buy Furosemide – lasix 100 mg
buy rybelsus in canada
https://stromectol.fun/# ivermectin ebay
http://stromectol.fun/# buy minocycline 100mg tablets
rybelsus canada pharmacy prices
where can you get amoxicillin: amoxicillin from canada – amoxicillin 500 mg
http://amoxil.cheap/# can i buy amoxicillin online
wegovy retail price
lisinopril 20mg tablets where can i purchase lisinopril lisinopril 20 mg price online
http://buyprednisone.store/# prednisone 1 mg daily
zestril lisinopril: lisinopril 2.5 tablet – online lisinopril
rybelsus pill
http://stromectol.fun/# buy ivermectin for humans australia
ozempic tablets for weight loss
order stromectol online ivermectin india generic ivermectin
lasix 40mg: Over The Counter Lasix – lasix generic name
http://buyprednisone.store/# no prescription online prednisone
semaglutide online uk
rybelsus tab 14mg
semaglutide online
semaglutide medicine
wegovy tab 3mg
buy rybelsus online from india
rybelsus without prescription
buy ozempic for weight loss
semaglutide sale
buy wegovy
http://indianph.xyz/# buy prescription drugs from india
best online pharmacy india
rybelsus pills
buy rybelsus online no script needed
https://indianph.xyz/# indian pharmacy paypal
semaglutide tablets cost
buy medicines online in india best india pharmacy reputable indian online pharmacy
rybelsus medicine
buy rybelsus online no script
http://indianph.com/# best online pharmacy india
indian pharmacy online
best india pharmacy top 10 online pharmacy in india india online pharmacy
brand ozempic
http://indianph.com/# reputable indian online pharmacy
buy prescription drugs from india
https://indianph.com/# online pharmacy india
top 10 pharmacies in india
mail order pharmacy india india online pharmacy indian pharmacies safe
http://indianph.com/# top 10 pharmacies in india
india online pharmacy
semaglutide tab 14mg
https://indianph.com/# best online pharmacy india
top 10 online pharmacy in india
wegovy rx
http://indianph.com/# buy prescription drugs from india
https://indianph.xyz/# indian pharmacy online
india online pharmacy
reputable indian pharmacies indian pharmacy online top 10 online pharmacy in india
http://indianph.xyz/# best online pharmacy india
reputable indian pharmacies
semaglutide tablets buy
semaglutide cost
http://indianph.xyz/# top 10 pharmacies in india
online pharmacy india
rybelsus 14
semaglutide online pharmacy
buy semaglutide cheap
rybelsus injection
rybelsus semaglutide tablets cost
wegovy pill form
buy cipro cheap ciprofloxacin generic buy cipro cheap
brand semaglutide
wegovy buy uk
http://cipro.guru/# cipro ciprofloxacin
buy wegovy
cytotec buy online usa: buy cytotec online – Misoprostol 200 mg buy online
http://nolvadex.guru/# nolvadex for sale
https://cipro.guru/# buy cipro online
doxycycline 500mg buy doxycycline online uk generic doxycycline
diflucan 200mg: diflucan 150 tab – diflucan generic brand
http://cytotec24.shop/# purchase cytotec
rybelsus tablets cost
rybelsus online pharmacy
https://doxycycline.auction/# where can i get doxycycline
wegovy diabetes medication
diflucan 150mg tab: can i buy diflucan over the counter – diflucan 100 mg tablet
buy diflucan online cheap cost of diflucan diflucan 200
wegovy tab 7mg
rybelsus buy uk
https://diflucan.pro/# diflucan otc where to buy
generic wegovy for weight loss
buy cipro: cipro 500mg best prices – cipro ciprofloxacin
https://diflucan.pro/# diflucan without a prescription
rybelsus online uk
tamoxifen and antidepressants tamoxifen headache nolvadex steroids
wegovy 7 mg tablet
wegovy 7 mg
http://diflucan.pro/# diflucan brand name
http://cytotec24.shop/# buy misoprostol over the counter
semaglutide online pharmacy
https://diflucan.pro/# diflucan 110 mg
wegovy semaglutide tablets 7.5 mcg
where to get diflucan over the counter diflucan over the counter nz diflucan discount
tamoxifen men: nolvadex pct – nolvadex for pct
generic ozempic
https://cytotec24.shop/# Misoprostol 200 mg buy online
https://diflucan.pro/# diflucan 150 mg price uk
http://diflucan.pro/# diflucan canadian pharmacy
generic ozempic for weight loss
tamoxifen reviews tamoxifen mechanism of action tamoxifen generic
rybelsus online cheap
http://cipro.guru/# buy cipro cheap
rybelsus best price
http://diflucan.pro/# how to get diflucan online
semaglutide rx
buy semaglutide oversees
tamoxifen moa tamoxifen endometrium tamoxifen brand name
https://diflucan.pro/# buy generic diflucan
semaglutide 7mg
http://diflucan.pro/# buy online diflucan
rybelsus prescription
http://cytotec24.shop/# purchase cytotec
wegovy 7 mg
rybelsus buy online
ciprofloxacin 500 mg tablet price cipro online no prescription in the usa buy ciprofloxacin
tamoxifen generic tamoxifen and ovarian cancer tamoxifen and depression
buy semaglutide online cheap
https://angelawhite.pro/# Angela White
http://sweetiefox.online/# sweety fox
Sweetie Fox video: sweety fox – Sweetie Fox izle
wegovy tab 7mg
http://lanarhoades.fun/# lana rhoades filmleri
http://sweetiefox.online/# Sweetie Fox
Angela White: abella danger izle – abella danger filmleri
https://evaelfie.pro/# eva elfie izle
ozempic pill form
rybelsus buy from canada
http://evaelfie.pro/# eva elfie modeli
wegovy for diabetes
http://lanarhoades.fun/# lana rhoades video
http://angelawhite.pro/# Angela White izle
eva elfie modeli: eva elfie izle – eva elfie video
buy ozempic online no script
http://abelladanger.online/# abella danger video
wegovy 7mg
http://lanarhoades.fun/# lana rhoades video
wegovy 3mg
Angela Beyaz modeli: Angela White video – ?????? ????
http://evaelfie.pro/# eva elfie filmleri
http://angelawhite.pro/# Angela White filmleri
http://sweetiefox.online/# Sweetie Fox izle
lana rhoades izle: lana rhoades modeli – lana rhoades
https://evaelfie.pro/# eva elfie filmleri
where to buy semaglutide
buy ozempic online from india
https://lanarhoades.fun/# lana rhodes
https://abelladanger.online/# abella danger filmleri
generic semaglutide for weight loss
Sweetie Fox filmleri: Sweetie Fox filmleri – swetie fox
brand ozempic
wegovy where to buy
semaglutide 3mg
https://evaelfie.pro/# eva elfie filmleri
http://evaelfie.pro/# eva elfie video
rybelsus tab 14mg
lana rhoades video: lana rhoades izle – lana rhoades video
http://evaelfie.pro/# eva elfie izle
https://lanarhoades.fun/# lana rhoades video
buy semaglutide online no script
wegovy semaglutide tablets 7.5 mcg
ozempic tablets buy
http://evaelfie.pro/# eva elfie video
https://angelawhite.pro/# Angela White filmleri
Angela Beyaz modeli: abella danger filmleri – Abella Danger
purchase rybelsus
https://sweetiefox.online/# sweeti fox
amoxicillin for uti dosage how many days
buy semaglutide online no script
wegovy online uk
Angela White: Angela White video – Angela White filmleri
http://abelladanger.online/# abella danger video
http://evaelfie.pro/# eva elfie izle
eva elfie video: eva elfie – eva elfie izle
https://abelladanger.online/# abella danger video
http://lanarhoades.fun/# lana rhodes
buy semaglutide online
wegovy online uk
https://lanarhoades.fun/# lana rhoades filmleri
https://evaelfie.pro/# eva elfie modeli
https://angelawhite.pro/# Angela White video
azithromycin 25 mg cost
eva elfie izle: eva elfie – eva elfie izle
http://lanarhoades.fun/# lana rhoades
best online pharmacy tadalafil
cheapest on line valtrex without a prescription
synthroid united states
http://evaelfie.pro/# eva elfie filmleri
http://angelawhite.pro/# Angela White izle
eva elfie filmleri: eva elfie modeli – eva elfie video
compare pharmacy prices
https://sweetiefox.online/# Sweetie Fox filmleri
top 10 pharmacies in india
https://evaelfie.pro/# eva elfie izle
prednisone 60 mg
generic for prinivil
synthroid 175
prednisone 10 mg online
lana rhoades solo: lana rhoades – lana rhoades unleashed
generic cialis for women
https://miamalkova.life/# mia malkova hd
generic prednisone tablets
plentyoffish dating sites: https://miamalkova.life/# mia malkova full video
valtrex script
lana rhoades full video: lana rhoades hot – lana rhoades full video
http://evaelfie.site/# eva elfie full videos
lisinopril tab 20mg cost
pharmacy website
lana rhoades hot: lana rhoades full video – lana rhoades boyfriend
italian pharmacy online
zithromax drug
http://sweetiefox.pro/# sweetie fox full
order azithromycin online uk
tadalafil medication
sweetie fox full video: ph sweetie fox – sweetie fox new
asian girl single: http://lanarhoades.pro/# lana rhoades hot
eva elfie hot: eva elfie new videos – eva elfie videos
order metformin online
https://miamalkova.life/# mia malkova new video
cheap generic cialis india
mia malkova movie: mia malkova new video – mia malkova new video
buy synthroid cheap
cheap valtrex canada
best price for lisinopril
lana rhoades videos: lana rhoades boyfriend – lana rhoades
generic for metformin
lisinopril mexico
http://evaelfie.site/# eva elfie full videos
online-dating-ukraine: http://miamalkova.life/# mia malkova full video
best generic metformin
sweetie fox new: sweetie fox video – sweetie fox new
brand cialis 20mg
buy brand name synthroid online
cheapest pharmacy to fill prescriptions with insurance
50 mg lisinopril
eva elfie full videos: eva elfie videos – eva elfie hd
cost of lisinopril 10 mg
canadian pharmacy 24h com safe
https://evaelfie.site/# eva elfie new video
glucophage brand name
lisinopril medication prescription
eva elfie photo: eva elfie hd – eva elfie photo
synthroid 125
azithromycin 250 price india
online shopping pharmacy india
dating sites without registering: https://lanarhoades.pro/# lana rhoades boyfriend
synthroid 0.075 mcg
zestril 40 mg tablet
lisinopril 20 mg discount
azithromycin 1000 for sale
eva elfie hd: eva elfie full video – eva elfie photo
https://sweetiefox.pro/# sweetie fox new
buy lisinopril 5mg
lana rhoades boyfriend: lana rhoades videos – lana rhoades boyfriend
best online thai pharmacy
http://lanarhoades.pro/# lana rhoades unleashed
mia malkova: mia malkova movie – mia malkova
online dating sites for free: http://evaelfie.site/# eva elfie videos
synthroid 88
online pharmacy no presc uk
sweetie fox full video: ph sweetie fox – sweetie fox video
https://lanarhoades.pro/# lana rhoades videos
cost of tadalafil
eva elfie videos: eva elfie full videos – eva elfie hot
otc synthroid
canadian pharmacy online ship to usa
lisinopril 20 tablet
prednisone 2.5 mg tablet
mia malkova videos: mia malkova girl – mia malkova full video
https://miamalkova.life/# mia malkova full video
buy lisinopril 10 mg tablet
zoosk dating: https://evaelfie.site/# eva elfie
online pharmacy no rx
lisinopril 40 mg tablet
metformin where to get
mia malkova latest: mia malkova photos – mia malkova new video
real cialis 20mg
prednisone 1 mg coupon
medicine prednisone 5mg
https://sweetiefox.pro/# sweetie fox new
lana rhoades boyfriend: lana rhoades solo – lana rhoades hot
tadalafil uk
lana rhoades solo: lana rhoades – lana rhoades
buy lisinopril 20 mg online canada
http://sweetiefox.pro/# sweetie fox video
happy family drugstore
aviator bet: aviator game online – aviator game
buy lisinopril
aviator oyunu: aviator oyna slot – aviator oyna
http://aviatoroyunu.pro/# aviator bahis
synthroid 50 mg
cheap tadalafil no prescription
jogar aviator Brasil: estrela bet aviator – aviator jogo
synthroid 137 mcg coupon
http://aviatormalawi.online/# aviator bet malawi
como jogar aviator em mocambique: aviator mz – jogar aviator
jogo de aposta online: ganhar dinheiro jogando – melhor jogo de aposta para ganhar dinheiro
buy generic cialis online with paypal
aviator bahis: aviator – aviator sinyal hilesi
https://aviatorjogar.online/# aviator game
tadalafil tablets online india
valtrex over the counter canada
pin up cassino online: pin-up casino login – pin-up casino
http://aviatoroyunu.pro/# aviator hilesi
sure save pharmacy
melhor jogo de aposta para ganhar dinheiro: aplicativo de aposta – aplicativo de aposta
melhor jogo de aposta: jogos que dao dinheiro – aviator jogo de aposta
lisinopril 10 12.5 mg
tadalafil 75 mg
zithromax pills for sale
aviator mz: aviator moçambique – aviator mz
pharmacy order online
valtrex generic pill
aviator game bet: play aviator – aviator game online
medication lisinopril 5 mg
synthroid canada price
aviator oyunu: aviator – aviator bahis
overseas pharmacy no prescription
canadian family pharmacy
pin-up casino entrar: pin-up cassino – pin-up casino entrar
pin-up casino: pin-up – cassino pin up
aviator mz: aviator online – aviator mz
aplicativo de aposta: depósito mínimo 1 real – jogo de aposta online
can you buy metformin in mexico
valtrex generic canada
aplicativo de aposta: melhor jogo de aposta – jogo de aposta
online order prednisone
zithromax cost uk – https://azithromycin.pro/zithromax-generic-name.html generic zithromax online paypal
lisinopril 40
metformin prices
aviator jogo de aposta: melhor jogo de aposta – jogo de aposta
metformin without script in usa
synthroid 25 pill
canada pharmacy cialis
prednisone tablets 5mg price
synthroid 125 mg coupon
pin up aviator: aviator oyunu – aviator sinyal hilesi
zithromax tablets for sale – https://azithromycin.pro/zithromax-2g-dose.html zithromax 500 mg lowest price online
aviator game online: aviator bet malawi login – aviator malawi
prescription medicine valtrex
valtrex 500mg price canada
play aviator: aviator malawi – aviator bet malawi
zithromax generic price: z-pak zithromax buy zithromax 1000mg online
prednisone 20mg price
mexican mail order pharmacies Mexico pharmacy online mexico pharmacies prescription drugs mexicanpharm.shop
azithromycin over the counter uk
reputable indian pharmacies: online pharmacy in india – india pharmacy indianpharm.store
australia price for valtrex
synthroid tabs 75mcg
lisinopril tabs 40mg
mexican mail order pharmacies: Medicines Mexico – mexican online pharmacies prescription drugs mexicanpharm.shop
prednisone tablets
india online pharmacy: Generic Medicine India to USA – buy medicines online in india indianpharm.store
cost daily cialis
indianpharmacy com online pharmacy usa india pharmacy indianpharm.store
100 mg lisinopril
zestril 20 mg price in india
cialis tablets australia
canadianpharmacymeds: Canadian pharmacy prices – northwest pharmacy canada canadianpharm.store
top online pharmacy india: cheapest online pharmacy – best online pharmacy india indianpharm.store
http://canadianpharmlk.com/# canada drug pharmacy canadianpharm.store
tadalafil rx
http://canadianpharmlk.com/# medication canadian pharmacy canadianpharm.store
canada online pharmacy no prescription
reputable canadian online pharmacies International Pharmacy delivery certified canadian international pharmacy canadianpharm.store
my canadian pharmacy: List of Canadian pharmacies – best canadian online pharmacy reviews canadianpharm.store
http://canadianpharmlk.com/# canadapharmacyonline com canadianpharm.store
valtrex brand cost
buy generic valtrex online canada
synthroid 112
canadian pharmaceutical prices
http://indianpharm24.com/# indian pharmacy paypal indianpharm.store
http://mexicanpharm24.com/# mexican online pharmacies prescription drugs mexicanpharm.shop
legal online pharmacy
reputable mexican pharmacies online: mexican pharmacy – mexican rx online mexicanpharm.shop
http://mexicanpharm24.com/# mexican drugstore online mexicanpharm.shop
https://mexicanpharm24.shop/# medicine in mexico pharmacies mexicanpharm.shop
buy prescription drugs from india: Online medicine order – world pharmacy india indianpharm.store
https://mexicanpharm24.shop/# reputable mexican pharmacies online mexicanpharm.shop
5mg tadalafil daily
mexican mail order pharmacies: order online from a Mexican pharmacy – mexico drug stores pharmacies mexicanpharm.shop
pharmacy website india Online medicine home delivery india pharmacy mail order indianpharm.store
synthroid 400 mg
http://mexicanpharm24.com/# buying prescription drugs in mexico mexicanpharm.shop
http://mexicanpharm24.shop/# mexican online pharmacies prescription drugs mexicanpharm.shop
citalopram side effects in females
all med pharmacy
synthroid 137 cost
canadian pharmacy cialis 20mg
canadian price for synthroid
http://indianpharm24.com/# Online medicine order indianpharm.store
mexican mail order pharmacies: mexico pharmacies prescription drugs – best online pharmacies in mexico mexicanpharm.shop
https://canadianpharmlk.shop/# cheap canadian pharmacy online canadianpharm.store
buying metformin canada
http://indianpharm24.com/# top 10 online pharmacy in india indianpharm.store
metformin 93
canadianpharmacyworld: canada drugs reviews – reddit canadian pharmacy canadianpharm.store
http://canadianpharmlk.shop/# pharmacy wholesalers canada canadianpharm.store
buy tadalafil 40 mg
canadian pharmacies comparison: Certified Canadian pharmacies – canada pharmacy online canadianpharm.store
http://indianpharm24.com/# online pharmacy india indianpharm.store
tadalafil price comparison
canadian online pharmacy Canadian pharmacy prices canadian pharmacy online store canadianpharm.store
valtrex generic otc
https://mexicanpharm24.shop/# reputable mexican pharmacies online mexicanpharm.shop
rx pharmacy no prescription
http://canadianpharmlk.com/# canadian pharmacy 365 canadianpharm.store
zestoretic 20 12.5
5mg tadalafil online
synthroid 150 cost
where can i get amoxicillin: side effects of amoxicillin – buying amoxicillin online
tadalafil india
buy amoxicillin 500mg usa: can i buy amoxicillin over the counter in australia – amoxicillin 500mg pill
tadalafil generic mexico
how to get clomid without rx: where to buy clomid – how to get cheap clomid pills
buy amoxil where can i buy amoxicillin without prec amoxicillin 500mg
http://amoxilst.pro/# buy amoxil
cheap clomid pills: clomid 50mg price – where can i get cheap clomid pill
canadien pharmacies
cheapest online pharmacy india
buying amoxicillin in mexico: buying amoxicillin in mexico – amoxicillin without a doctors prescription
https://amoxilst.pro/# amoxicillin 800 mg price
can i get cheap clomid online: where buy generic clomid prices – generic clomid without insurance
synthroid 300 mg
50 mg prednisone from canada: prednisone 5mg cost – purchase prednisone
tadalafil tablets online in india
where i can buy metformin without a prescription drugs
where can i buy generic clomid without prescription: can i order generic clomid without a prescription – can i get cheap clomid no prescription
buy amoxicillin 500mg usa: amoxicillin over the counter – can i buy amoxicillin over the counter
https://amoxilst.pro/# buy amoxicillin over the counter uk
can i order cheap clomid without rx cost of generic clomid no prescription buy generic clomid no prescription
clomid for sale: where buy cheap clomid – where can i buy clomid without rx
prednisone 10mg
where to get cheap clomid for sale: can i get clomid prices – can i purchase generic clomid tablets
synthroid 200
https://clomidst.pro/# can i buy generic clomid online
cheap amoxicillin 500mg: amoxicillin discount coupon – where to buy amoxicillin
price for 5mg cialis
azithromycin 500 mg generic
average cost of lisinopril
amoxicillin no prescipion: amoxicillin pot clavulanate – how to buy amoxycillin
875 mg amoxicillin cost: amoxicillin 750 mg price – amoxicillin no prescipion
http://clomidst.pro/# buy clomid without prescription
can you buy valtrex over the counter in australia
amoxicillin 825 mg: amoxicillin pills 500 mg – amoxicillin 1000 mg capsule
prednisone in mexico: prednisone eye drops – buy prednisone 10mg online
can you buy amoxicillin over the counter can you buy amoxicillin over the counter canada where can i buy amoxicillin over the counter
metformin 102
https://amoxilst.pro/# how much is amoxicillin prescription
metformin price in canada
ampicillin amoxicillin: amoxicillin allergy – prescription for amoxicillin
prednisone medication: prednisone dosage – buy prednisone without a prescription
online doctor prescription canada: best non prescription online pharmacy – online meds no prescription
I do 5 at a time, and if it takes me longer that a few seconds to solve it, it gets marked for review. Once i get to 3 for review, I work on those alone. I study them until i have completely solved them, understand them, and see the pattern. This is coming from someone that doesnt care for studying tactics. @ #8: Thanks again for this – abrok.eu stockfish I was clueless prior 🙂 This is fantastic and yeah …no reason to shell out money on any other engine out there since none of them compare to the latest build at all. Oh…I also wanted to add here that the combination of ChessTempo’s Gold sub with their database + Stockfish is probably the most underrated weapon I can find out there. It’s a total of $4 month and I, personally, think a lot of people would prefer it to Chessbase’s line if they gave it a heads up comparison. Not to mention that ChessTempo’s tactical training is best in the biz.
https://www.rebekaharaullo.com/game-engine
If you like word games, you might enjoy our mobile friendly sudoku or our free online jigsaw puzzle on our sister site. We also offer a free online version of solitaire and a classic version of minesweeper! Scrabble is a popular word game, it’s very easy to play and enjoyed by people from every corner of the world. The game play is simple and straightforward, however it’s extremely difficult to master. If you’ve just started and need some tips then you’ve come to the right place. We’ve curated some tips here specifically for the absolute beginners. Try to incorporate at least one of the tips written below in your next game. It can take many combination of letters and find the unscrambled words in the characters. Scramble Words is the game for you. Take letters from below and make new words above to complete this word puzzle game. Whether you’re new to word games or a seasoned pro, there’s sure to be something to challenge you. Remember to get those bonus letters for a better score.
best online pharmacy no prescription: canada online pharmacy – canadian pharmacy world coupon
prednisone online purchase
no prescription canadian pharmacy no prescription needed online pharmacy best online prescription
online ed prescription: cheap boner pills – online ed medications
synthroid brand name
https://edpills.guru/# erectile dysfunction online prescription
buy prednisone online canada
canadian prescription prices: no prescription needed – meds no prescription
cheap prescription drugs online: quality prescription drugs canada – online pharmacies without prescription
buy tadalafil 20
azithromycin tablets australia
prednisone 100 mg tablet
best no prescription online pharmacy: buying prescription medicine online – online pharmacy canada no prescription
metformin 1000 mg pill
https://onlinepharmacy.cheap/# overseas pharmacy no prescription
cheapest pharmacy to fill prescriptions with insurance: online pharmacy delivery – reputable online pharmacy no prescription
canadian drugs no prescription: canadian pharmacy without prescription – online drugs without prescription
synthroid brand coupon
tadalafil daily use
tadalafil tablets cost in india
zestoretic 20 mg
canadian pharmacy coupon code: canada online pharmacy – online pharmacy non prescription drugs
https://onlinepharmacy.cheap/# overseas pharmacy no prescription
can you buy prescription drugs in canada prescription drugs canada non prescription online pharmacy
best generic valtrex
online pharmacy china
no prescription pharmacy: cheap prescription medication online – canada pharmacy online no prescription
affordable ed medication: ed online treatment – ed doctor online
pharmacy discount coupons: Online pharmacy USA – prescription drugs online
cheap scripts pharmacy
best rated canadian pharmacy
http://onlinepharmacy.cheap/# no prescription required pharmacy
synthroid 0.112 mg
canada pharmacy not requiring prescription: pharmacy online – no prescription required pharmacy
lisinopril 5mg
synthroid 0.15 mg
where can i buy azithromycin pills
cheapest prescription pharmacy: mexico pharmacy online – canadian pharmacy no prescription
online pharmacy without prescriptions: cheap drugs no prescription – buying prescription drugs online without a prescription
https://edpills.guru/# ed meds online
best online ed treatment: buy ed pills online – where can i buy ed pills
top 10 online pharmacy in india: online pharmacy india – mail order pharmacy india
cheapest on line valtrex without a prescription
best online pharmacy reddit
http://indianpharm.shop/# india pharmacy mail order
canadian pharmacy no scripts cheap canadian pharmacy canadian pharmacy ratings
indian pharmacy no prescription: meds online no prescription – canadian pharmacy no prescription needed
http://pharmacynoprescription.pro/# no prescription drugs online
prinivil 10 mg tab
pills no prescription: buying prescription drugs online without a prescription – prescription online canada
synthroid 0.050 mg
zestoretic tabs
http://indianpharm.shop/# best india pharmacy
https://canadianpharm.guru/# canadadrugpharmacy com
best rx pharmacy online
tadalafil pharmacy
zithromax online prescription
levothyroxine ordering online
my canadian pharmacy reviews canadadrugpharmacy com canadian pharmacy
top 10 online pharmacy in india: online shopping pharmacy india – india pharmacy mail order
canadianpharmacymeds: is canadian pharmacy legit – my canadian pharmacy
canadianpharmacyworld
how much is lisinopril 10 mg
https://mexicanpharm.online/# mexico pharmacies prescription drugs
buy lisinopril online
legitimate online pharmacies india: pharmacy website india – indian pharmacies safe
valtrex online purchase
mexico drug stores pharmacies: best online pharmacies in mexico – buying prescription drugs in mexico
southern pharmacy
cheapest online pharmacy india: reputable indian online pharmacy – reputable indian online pharmacy
http://canadianpharm.guru/# canadian family pharmacy
buy lisinopril 2.5 mg
http://mexicanpharm.online/# reputable mexican pharmacies online
mexico drug stores pharmacies: buying from online mexican pharmacy – buying prescription drugs in mexico
lisinopril online usa
buy lisinopril canada
tadalafil tablets cost in india
http://canadianpharm.guru/# canadian pharmacy prices
medication lisinopril 10 mg
canada drugs without prescription: buy prescription drugs on line – online pharmacies no prescription usa
canadian pharmacy in canada: canadian pharmacies online – canadianpharmacyworld com
cheapest pharmacy for prescription drugs
purple pharmacy mexico price list mexican online pharmacies prescription drugs mexican drugstore online
mexico drug stores pharmacies: mexican mail order pharmacies – mexico drug stores pharmacies
metformin 1000 mg price in india
http://mexicanpharm.online/# mexican border pharmacies shipping to usa
tadalafil australia
best rated canadian pharmacy: maple leaf pharmacy in canada – canadian pharmacy in canada
canadian pharmacy prices: canadian pharmacy 1 internet online drugstore – pharmacy canadian superstore
can you buy metformin over the counter
azithromycin canadian pharmacy
order azithromycin 500mg online
best website to buy prescription drugs: prescription drugs online canada – canada online prescription
indianpharmacy com
https://indianpharm.shop/# indian pharmacy online
https://indianpharm.shop/# reputable indian online pharmacy
order prescription from canada: canadian prescription drugstore review – best no prescription online pharmacies
mexican mail order pharmacies: mexican online pharmacies prescription drugs – mexican mail order pharmacies
http://indianpharm.shop/# reputable indian online pharmacy
prednisone brand name cost
online pharmacy viagra
reputable indian pharmacies: world pharmacy india – best india pharmacy
synthroid 50 mcg coupon
buying from online mexican pharmacy: buying prescription drugs in mexico – mexico pharmacies prescription drugs
canadian pharmacy 365: canadian pharmacy mall – canadian pharmacy 365
how to order lisinopril online
https://mexicanpharm.online/# best online pharmacies in mexico
synthroid 0.15
metformin pharmacy
cheap generic prednisone
how much is prednisone
online pharmacy metformin
generic for prinivil
online pharmacies without prescription: no prescription online pharmacies – online meds no prescription
lisinopril 40 mg price
buying prescription drugs online from canada: can i buy prescription drugs in canada – best online pharmacy without prescription
http://mexicanpharm.online/# reputable mexican pharmacies online
buying drugs without prescription: pills no prescription – buying prescription drugs online without a prescription
best online pharmacy india india pharmacy indian pharmacy paypal
cialis 4 mg
prescription drugs canada: no prescription – prescription drugs canada
https://indianpharm.shop/# top 10 pharmacies in india
cialis over the counter
top online pharmacy india: online pharmacy india – Online medicine home delivery
buying from online mexican pharmacy: mexico pharmacy – mexican drugstore online
good value pharmacy
azithromycin over the counter south africa
https://indianpharm.shop/# india online pharmacy
no prescription medicine: buy drugs online without a prescription – no prescription online pharmacies
lisinopril 5mg
canada online prescription: prescription meds from canada – online no prescription pharmacy
azithromycin canadian pharmacy
tadalafil – generic
https://mexicanpharm.online/# mexican border pharmacies shipping to usa
no prescription medicine: buy medications without a prescription – online no prescription pharmacy
http://pharmacynoprescription.pro/# no prescription pharmacy online
tadalafil 5mg best price
mexico drug stores pharmacies: pharmacies in mexico that ship to usa – mexican pharmaceuticals online
pharmacies without prescriptions canadian prescription prices no prescription medicines
glucophage price canada
top 10 online pharmacy in india: buy prescription drugs from india – top 10 online pharmacy in india
lisinopril 40mg
buy prescription drugs from india: online shopping pharmacy india – india pharmacy
https://pharmacynoprescription.pro/# discount prescription drugs canada
synthroid 25 mg tablet
metformin 800
buy prescription drugs from india: Online medicine home delivery – best online pharmacy india
https://pharmacynoprescription.pro/# canadian pharmacy prescription
medications online without prescriptions: cheap prescription drugs online – best non prescription online pharmacy
canadian happy family store pharmacy
canada pharmacy world: canada pharmacy world – canadian pharmacies that deliver to the us
cost cialis
purchase metformin canada
https://pinupgiris.fun/# pin-up giris
aviator oyunu: aviator oyunu 20 tl – aviator oyna
http://slotsiteleri.guru/# slot siteleri bonus veren
cost of augmentin
guvenilir slot siteleri: slot oyun siteleri – canl? slot siteleri
https://sweetbonanza.bid/# sweet bonanza siteleri
https://aviatoroyna.bid/# aviator nas?l oynan?r
pin up indir: aviator pin up – pin up casino giris
https://pinupgiris.fun/# pin up casino güncel giris
synthroid 150 mcg cost
https://sweetbonanza.bid/# güncel sweet bonanza
metformin nz
cost of synthroid 75 mg
sweet bonanza yorumlar: sweet bonanza indir – sweet bonanza slot
pin up casino guncel giris: pin up indir – pin up guncel giris
https://sweetbonanza.bid/# sweet bonanza giris
canadian pharmacy 24h com
http://gatesofolympus.auction/# gates of olympus hilesi
medication zestoretic
https://pinupgiris.fun/# pin-up giris
aviator oyunu giris: aviator oyna slot – aviator hilesi ucretsiz
valtrex 1g tablets cost
http://pinupgiris.fun/# pin up indir
rx pharmacy online 24
legal online pharmacy coupon code
gates of olympus oyna: gates of olympus demo free spin – gates of olympus 1000 demo
tadalafil tablet 5mg
metformin capsule
lisinopril 12.5
http://slotsiteleri.guru/# deneme bonusu veren slot siteleri
sweet bonanza taktik: sweet bonanza 100 tl – sweet bonanza giris
sweet bonanza demo: sweet bonanza kazanc – sweet bonanza kazanma saatleri
metformin 500 mg cost
https://gatesofolympus.auction/# gates of olympus nasil para kazanilir
over the counter synthroid
prednisone 10mg tabs
http://sweetbonanza.bid/# sweet bonanza mostbet
metformin 20 mg
http://pinupgiris.fun/# pin up casino giris
gates of olympus demo free spin: gates of olympus demo turkce oyna – gates of olympus giris
valtrex without a prescription
https://aviatoroyna.bid/# aviator hile
prednisone 20mg tablets
happy family canadian pharmacy
aviator oyunu 50 tl: aviator oyna 20 tl – aviator oyna
http://gatesofolympus.auction/# gates of olympus demo oyna
aviator hilesi ucretsiz: aviator sinyal hilesi ucretsiz – aviator giris
https://gatesofolympus.auction/# gates of olympus giris
cheap prednisone online
bonus veren casino slot siteleri: slot siteleri guvenilir – en yeni slot siteleri
tadalafil price australia
http://aviatoroyna.bid/# aviator sinyal hilesi
https://slotsiteleri.guru/# en çok kazandiran slot siteleri
buy cheap lisinopril
pragmatic play gates of olympus: gates of olympus slot – gates of olympus oyna
buy synthroid 200 mcg
buy tadalafil cialis
https://sweetbonanza.bid/# sweet bonanza free spin demo
buy generic valtrex without a prescription
pin up 7/24 giris: pin up giris – pin up guncel giris
online canadian drugstore Prescription Drugs from Canada canadian online drugs
buy prendesone without a prescription
buy daily cialis online
azithromycin 500 mg generic price
http://mexicanpharmacy.shop/# mexico pharmacies prescription drugs
india pharmacy mail order: indian pharmacy delivery – top online pharmacy india
canadian pharmacy service canadian pharmacy 24 canadapharmacyonline
how to buy valtrex
over the counter synthroid
generic valtrex online pharmacy
order synthroid from canada
indian pharmacy online online pharmacy india best india pharmacy
synthroid online
lisinopril 10 mg daily
http://canadianpharmacy24.store/# canada discount pharmacy
purple pharmacy mexico price list mexican pharmacy mexico pharmacy
indian pharmacy online: indian pharmacy delivery – world pharmacy india
pharmacies in mexico that ship to usa: mexican online pharmacies prescription drugs – mexican online pharmacies prescription drugs
100 mg tadalafil
mexico drug stores pharmacies: mexico pharmacy – mexico drug stores pharmacies
canadian pharmacy online ship to usa Prescription Drugs from Canada canadian world pharmacy
1 lisinopril
valtrex for sale online
buy lisinopril in mexico
top online pharmacy india: reputable indian online pharmacy – indian pharmacy
best mexican online pharmacies: buying prescription drugs in mexico – mexico pharmacy
cheapest online pharmacy india: indian pharmacy – indian pharmacy online
trusted canadian pharmacy northwest canadian pharmacy canadian online pharmacy
synthroid 150 mg
best online pharmacy india: cheapest online pharmacy india – india pharmacy mail order
world pharmacy india: Cheapest online pharmacy – best online pharmacy india
cheap real cialis
http://indianpharmacy.icu/# online shopping pharmacy india
best online canadian pharmacy: Large Selection of Medications – canadian pharmacy
tadalafil 5mg price canada
buy prescription drugs from india Healthcare and medicines from India india online pharmacy
canadian pharmacy online store
buying prescription drugs in mexico: Online Pharmacies in Mexico – buying prescription drugs in mexico
canadian pharmacy no rx needed: Certified Canadian Pharmacy – canadian pharmacy 24
medical pharmacy west
mexican border pharmacies shipping to usa mexico pharmacy mexican border pharmacies shipping to usa
where can i buy generic valtrex
synthroid cost in india
american online pharmacy
tadalafil india 20mg
valtrex 500 cost
azithromycin capsules 250mg
buying prescription drugs in mexico: mexican drugstore online – mexican pharmaceuticals online
brand cialis online
cialis tablets canada
canadian family pharmacy Prescription Drugs from Canada canada rx pharmacy
canadian pharmacy king reviews: buying drugs from canada – safe canadian pharmacy
https://mexicanpharmacy.shop/# buying prescription drugs in mexico online
synthroid 500 mcg
safe canadian pharmacy pills now even cheaper escrow pharmacy canada
best canadian pharmacy no prescription
rate canadian pharmacies
tadalafil 5mg coupon
buy prescription drugs from india: Generic Medicine India to USA – mail order pharmacy india
canadian pharmacy 1 internet online drugstore: canadian pharmacy 24 – best canadian online pharmacy reviews
buy prescription drugs from india top 10 pharmacies in india cheapest online pharmacy india
amoxicillin generic: amoxicillin 1000 mg capsule – amoxicillin 500
zithromax price south africa: zithromax buy online no prescription – zithromax 1000 mg pills
pharmacy no prescription required
buy amoxicillin without prescription medicine amoxicillin 500 amoxil generic
lisinopril prescription cost
http://zithromaxall.shop/# zithromax online
tadalafil 5mg cost
http://clomidall.shop/# buying generic clomid
can i buy zithromax online zithromax online no prescription zithromax price south africa
cost of valtrex tablets
https://prednisoneall.com/# buying prednisone
where can i buy prednisone over the counter
can you buy generic clomid how to get generic clomid for sale where can i buy clomid without insurance
how can i get prednisone online without a prescription: prednisone prescription for sale – prednisone best price
http://zithromaxall.shop/# zithromax generic price
synthroid europe
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
metformin uk
https://amoxilall.shop/# amoxicillin 500 mg price
canadian pharmacy cialis
where to buy cheap clomid where to get cheap clomid prices where can i buy generic clomid without insurance
amoxicillin over the counter in canada: amoxicillin generic – amoxicillin 500mg capsules
http://clomidall.com/# can i purchase clomid without insurance
levothyroxine 50 mcg
http://zithromaxall.shop/# how to get zithromax over the counter
can i buy cheap clomid how to buy clomid price where can i buy cheap clomid online
https://clomidall.com/# can you buy generic clomid no prescription
buy tadalafil 5mg
metformin online uk
prednisone prices prednisone acetate how much is prednisone 10 mg
1700 mg metformin
http://prednisoneall.shop/# buy prednisone canadian pharmacy
prescription medicine lisinopril
generic zithromax azithromycin: can i buy zithromax online – how much is zithromax 250 mg
https://amoxilall.com/# amoxicillin 800 mg price
synthroid 188
order prednisone online safely
cost of cheap clomid no prescription: can i get generic clomid without prescription – where to buy generic clomid pills
zithromax cost generic zithromax 500mg india zithromax 500 mg lowest price drugstore online
cost of synthroid brand name
25 mg tadalafil
https://clomidall.shop/# where buy cheap clomid
cialis 10
prednisone online pharmacy
order metformin on line
generic amoxil 500 mg can i buy amoxicillin over the counter in australia buy amoxicillin online mexico
https://prednisoneall.com/# can you buy prednisone over the counter in usa
can i buy prednisone over the counter in mexico
cost of valtrex in india
http://prednisoneall.com/# prednisone 10 mg over the counter
can i buy zithromax online buy zithromax without presc zithromax drug
https://clomidall.com/# can i purchase cheap clomid without insurance
п»їkamagra Kamagra Oral Jelly Price Kamagra 100mg
viagra canada: buy viagra online – cheap viagra
azithromycin brand name
cialis for sale: Cialis 20mg price in USA – Buy Tadalafil 5mg
https://tadalafiliq.shop/# Cialis 20mg price
cheap kamagra Kamagra 100mg п»їkamagra
buy synthroid canada
buy Viagra online: buy viagra online – sildenafil 50 mg price
wholesale pharmacy
buy viagra here: best price on viagra – Sildenafil Citrate Tablets 100mg
synthroid 200 mg
п»їkamagra Kamagra gel cheap kamagra
lisinopril 100mcg
Cialis without a doctor prescription: Buy Cialis online – Generic Cialis without a doctor prescription
Viagra without a doctor prescription Canada: best price on viagra – sildenafil 50 mg price
Cialis without a doctor prescription cheapest cialis Tadalafil Tablet
https://tadalafiliq.com/# Buy Tadalafil 10mg
acarbose trials
Cheap Viagra 100mg: sildenafil iq – generic sildenafil
cheap viagra: generic ed pills – Sildenafil 100mg price
Tadalafil Tablet Generic Tadalafil 20mg price п»їcialis generic
tulip happy family
prinivil 25mg
Buy Viagra online cheap: cheapest viagra – sildenafil 50 mg price
https://kamagraiq.shop/# п»їkamagra
prescription valtrex online
online pharmacy india
buy real cialis
Kamagra 100mg: Kamagra gel – buy kamagra online usa
Generic Tadalafil 20mg price: cheapest cialis – Cialis over the counter
Generic Viagra online cheapest viagra Cheap Sildenafil 100mg
buy zithromax no prescription
https://kamagraiq.shop/# super kamagra
how to buy metformin in canada
https://kamagraiq.shop/# п»їkamagra
cheapest cialis: cialis generic – Generic Tadalafil 20mg price
Cheap generic Viagra generic ed pills Cheap generic Viagra online
Viagra Tablet price: sildenafil over the counter – sildenafil online
http://kamagraiq.com/# Kamagra tablets
reputable canadian online pharmacies
generic sildenafil: sildenafil iq – buy Viagra online
Generic Cialis without a doctor prescription Buy Cialis online п»їcialis generic
https://tadalafiliq.shop/# Tadalafil price
overseas pharmacy no prescription
online pharmacy australia free delivery
Viagra Tablet price: sildenafil over the counter – Generic Viagra online
can you buy cialis online in australia
cheap generic valtrex without prescription
Kamagra Oral Jelly: Kamagra Iq – super kamagra
2 prinivil
http://sildenafiliq.xyz/# buy Viagra online
sildenafil over the counter best price on viagra buy Viagra online
п»їkamagra: Kamagra Oral Jelly Price – super kamagra
buy zestril online
http://sildenafiliq.xyz/# Generic Viagra for sale
offshore pharmacy no prescription
where to buy tadalafil in singapore
Buy Tadalafil 20mg: Buy Cialis online – Cialis over the counter
no prescription synthroid
azithromycin cost in india
http://tadalafiliq.shop/# Cialis over the counter
where can you get synthroid
Sildenafil Citrate Tablets 100mg cheapest viagra buy viagra here
Cheap Viagra 100mg: sildenafil iq – Cheapest Sildenafil online
lipinpril
lisinopril diuretic
polish pharmacy online uk
http://sildenafiliq.xyz/# Buy Viagra online cheap
cheapest viagra: best price on viagra – Generic Viagra online
over the counter sildenafil sildenafil iq Sildenafil Citrate Tablets 100mg
lisinopril 20 mg generic
canadian pharmacy world reviews canadian pharmacy reputable canadian pharmacy
buying valtrex online
buying from online mexican pharmacy: mexico drug stores pharmacies – mexican rx online
reputable indian online pharmacy: indian pharmacy delivery – cheapest online pharmacy india
https://mexicanpharmgrx.shop/# mexico drug stores pharmacies
canadian king pharmacy Canadian pharmacy prices pharmacy rx world canada
where can i purchase lisinopril
prednisone 8 mg
prinivil 5mg tablet
legit mexican pharmacy
http://mexicanpharmgrx.com/# medicine in mexico pharmacies
buy lisinopril 5 mg
india pharmacy mail order buy prescription drugs from india reputable indian pharmacies
http://mexicanpharmgrx.com/# mexican pharmacy
generic for azithromycin
prednisone drug
medication canadian pharmacy
apo-prednisone
https://mexicanpharmgrx.shop/# best mexican online pharmacies
canadian pharmacy meds Certified Canadian pharmacies canadian king pharmacy
purple pharmacy mexico price list: Mexico drugstore – medication from mexico pharmacy
lowest price tadalafil
https://mexicanpharmgrx.com/# buying prescription drugs in mexico online
where can i buy tadalafil online
purple pharmacy mexico price list mexican pharmacy mexican border pharmacies shipping to usa
https://indianpharmgrx.shop/# india pharmacy
synthroid 88 mcg in india
mexico pharmacy buying prescription drugs in mexico online buying from online mexican pharmacy
http://indianpharmgrx.shop/# indian pharmacy paypal
canada cialis over the counter
buy prescription drugs from india indian pharmacy paypal mail order pharmacy india
http://mexicanpharmgrx.shop/# mexico drug stores pharmacies
cost cialis 5 mg
top 10 pharmacies in india: indian pharmacy – Online medicine home delivery
lisinopril 60 mg
canada discount pharmacy: canadian pharmacy price checker – pharmacy rx world canada
http://indianpharmgrx.shop/# reputable indian pharmacies
mexican drugstore online online pharmacy in Mexico buying prescription drugs in mexico
azithromycin 1g for sale
zestoretic medication
https://indianpharmgrx.com/# india pharmacy
where to buy zithromax over the counter
lisinopril capsule
metformin sale online
http://indianpharmgrx.com/# reputable indian online pharmacy
mexican mail order pharmacies mexican pharmacy mexican rx online
cialis 50
synthroid cheapest price
https://indianpharmgrx.shop/# top 10 online pharmacy in india
medication from mexico pharmacy: Mexico drugstore – mexican pharmaceuticals online
canada pharmacy not requiring prescription
metformin tablet price
https://mexicanpharmgrx.com/# mexico pharmacy
mexico drug stores pharmacies: online pharmacy in Mexico – mexico pharmacies prescription drugs
http://mexicanpharmgrx.com/# mexican drugstore online
lisinopril 60 mg tablet
tamoxifen rash tamoxifen headache tamoxifen pill
Cytotec 200mcg price: buy cytotec over the counter – Abortion pills online
cytotec buy online usa: buy cytotec pills online cheap – order cytotec online
https://misoprostol.top/# buy cytotec online
zestoretic 20 12.5 mg
where to get nolvadex: where to get nolvadex – nolvadex pct
112 mcg synthroid price
ciprofloxacin order online cipro 500mg best prices buy cipro
buy cipro: ciprofloxacin over the counter – buy cipro online without prescription
reputable overseas online pharmacies
synthroid canadian pharmacy
generic zithromax online
synthroid 0.0125 25mcg
diflucan pills for sale: diflucan from india – where can i get diflucan online
buy misoprostol over the counter: buy cytotec – buy cytotec pills
doxycycline vibramycin 100mg doxycycline buy cheap doxycycline
azithromycin 500mg lowest price online
can you order cialis online
diflucan 200 mg: diflucan no prescription – diflucan pill otc
synthroid 62.5 mg
purchase cipro buy ciprofloxacin over the counter ciprofloxacin mail online
112 mcg synthroid price
http://diflucan.icu/# diflucan coupon canada
buy diflucan: diflucan 150 mg buy online uk – diflucan online no prescription
Abortion pills online: buy cytotec pills online cheap – buy cytotec pills online cheap
online pharmacy discount code 2018
buy diflucan pill diflucan fluconazole diflucan daily
tamoxifen postmenopausal: benefits of tamoxifen – tamoxifen hair loss
doxycycline 150 mg buy doxycycline for dogs doxycycline without prescription
valtrex rx coupon
canadian pharmacy prices
buy cytotec pills online cheap: buy cytotec pills online cheap – buy cytotec over the counter
generic tadalafil us
buy ciprofloxacin: buy ciprofloxacin – cipro generic
buy azithromycin online canada
aromatase inhibitors tamoxifen nolvadex vs clomid tamoxifen mechanism of action
ciprofloxacin generic price: ciprofloxacin generic price – cipro ciprofloxacin
zestril 5 mg tablets
synthroid 175 price
http://diflucan.icu/# diflucan tablet price
doxycycline without a prescription: doxycycline tablets – doxycycline 100mg tablets
buy cialis online canadian pharmacy
nolvadex vs clomid tamoxifen citrate hysterectomy after breast cancer tamoxifen
2 lisinopril
buy cytotec pills: purchase cytotec – buy cytotec online fast delivery
lisinopril 2.5
azithromycin 1000 mg for sale
3 lisinopril
tamoxifen citrate pct: clomid nolvadex – aromatase inhibitor tamoxifen
synthroid 25 mcg daily
cipro pharmacy: buy ciprofloxacin over the counter – buy cipro
canadien pharmacies
where to buy diflucan otc: diflucan without get a prescription online – where to get diflucan otc
75 mg cialis
over the counter diflucan cream diflucan 150 australia buy diflucan without prescription
https://ciprofloxacin.guru/# п»їcipro generic
buy metformin er online without prescription
buy generic doxycycline: doxycycline 100mg online – where to get doxycycline
where can i buy azithromycin over the counter
list of online pharmacies
prednisone 30 mg coupon
zithromax over the counter uk zithromax 500 mg for sale buy zithromax online
buy lisinopril online no prescription
azithromycin 500 tablet
order valtrex online usa
prednisone without prescription 10mg: purchase prednisone canada – prednisone buy online nz
https://prednisonea.store/# india buy prednisone online
online pharmacy for sale
amoxicillin 500 mg capsule: how to get amoxicillin – amoxicillin 500mg
can you buy metformin over the counter in australia
can i order generic clomid pills where buy clomid prices cheap clomid without rx
zithromax antibiotic
prednisone deltasone
canada discount pharmacy
buy synthroid cheap
stromectol uk: cost of ivermectin medicine – buy ivermectin nz
synthroid pill
prednisone prescription online
amoxicillin 875 mg tablet amoxicillin 1000 mg capsule amoxicillin buy online canada
how to buy glucophage
where can i purchase zithromax online: generic zithromax azithromycin – generic zithromax medicine
online valtrex prescription
synthroid europe
http://stromectola.top/# ivermectin 3mg dosage
synthroid 25 mcg daily
zithromax cost in mexico
amoxicillin 500 mg cost: buy amoxicillin canada – amoxicillin 500mg cost
clomid cost where can i get generic clomid without insurance where to buy clomid without dr prescription
pharmacy discount card
clomid rx: how to get generic clomid tablets – cost generic clomid without insurance
https://stromectola.top/# stromectol pill
https://prednisonea.store/# prednisone 10mg tablet price
medical pharmacy south
metformin 750 mg tablet
synthroid 50 mcg
amoxicillin 500mg buy amoxicillin without prescription can you buy amoxicillin uk
can you buy zithromax in canada
purchase ivermectin: ivermectin 0.5 lotion india – buy stromectol canada
zithromax buy online no prescription: zithromax 500mg price – zithromax 500 mg lowest price pharmacy online
http://prednisonea.store/# buy prednisone online fast shipping
cheapest tadalafil uk
canadian 24 hour pharmacy
zithromax price south africa: zithromax 250 mg – zithromax online
tadalafil generic canada 20 mg
how much is metformin 500 mg
average cost of prednisone 20 mg
online pharmacy prescription pharmacy coupons cheapest pharmacy prescription drugs
https://onlinepharmacyworld.shop/# canadian pharmacy world coupon
lisinopril pills 2.5 mg
synthroid 0.125mg tab
no prescription needed pharmacy
purchase cialis
https://onlinepharmacyworld.shop/# overseas pharmacy no prescription
buying ed pills online: buy ed medication – online ed meds
http://edpill.top/# cost of ed meds
best ed medication online: online erectile dysfunction medication – online ed treatments
lisinopril 102
buying prescription drugs online from canada best website to buy prescription drugs buy pills without prescription
safe canadian pharmacy
tadalafil 20mg in india
https://edpill.top/# where can i buy ed pills
lisinopril generic price
synthroid 5mg
how much is lisinopril
ed online meds: buy erectile dysfunction treatment – online erectile dysfunction pills
tadalafil cost australia
erectile dysfunction medication online low cost ed pills get ed meds today
lisinopril 10 12.5 mg tablets
online pharmacy no rx
http://edpill.top/# best ed pills online
buy levothyroxine online
best non prescription online pharmacy: buy drugs online no prescription – order prescription drugs online without doctor
https://onlinepharmacyworld.shop/# best canadian pharmacy no prescription
how to buy valtrex in korea
can you buy metformin over the counter in usa
pharmacy online 365 discount code canadian online pharmacy no prescription pharmacy discount coupons
cialis 20mg uk online
metformin price
http://edpill.top/# ed rx online
can i buy lisinopril over the counter in canada
http://onlinepharmacyworld.shop/# canadian pharmacy coupon
no prescription pharmacy online: pharmacy no prescription required – prescription from canada
zithromax for sale online
canadian drugs no prescription: prescription online canada – buy meds online without prescription
cialis pharmacy price comparison
canadian pharmacies not requiring prescription
http://onlinepharmacyworld.shop/# canada drugs coupon code
where to buy ed pills ed drugs online cost of ed meds
prescription free canadian pharmacy: online pharmacy discount code – cheapest pharmacy prescription drugs
metformin otc canada
synthroid 60 mg
prednisone 105
synthroid 25 mcg cost
https://edpill.top/# ed prescription online
synthroid pills
valtrex otc drug
https://casinvietnam.com/# casino tr?c tuy?n vi?t nam
metformin 500 mg buy online
http://casinvietnam.shop/# choi casino tr?c tuy?n tren di?n tho?i
synthroid 50 mcg cost
web c? b?c online uy tín: casino tr?c tuy?n uy tín – casino tr?c tuy?n vi?t nam
https://casinvietnam.shop/# casino tr?c tuy?n vi?t nam
casino tr?c tuy?n vi?t nam game c? b?c online uy tin casino online uy tin
valtrex 500mg price in india
synthroid 201
prescription medicine valtrex
prednisone cost us
rx pharmacy online 24
safe reliable canadian pharmacy
synthroid 125 mg cost
happy family drug store
tamsulosin tsl 0.4
metformin 850 mg
voltaren gel for back spasms
best online pharmacy
zithromax 600 mg tablets
buy prednisone
10 mg prednisone tablets
prinivil 10 mg tab
tadalafil online canada
generic tadalafil 2018
azithromycin erythromycin
valtrex 500 mg tablet cost
buy valtrex
buy valtrex tablets
synthroid 175 mcg tablet
tadalafil cost india
cheap tadalafil 20 mg canada
buy tadalafil 20 mg from india
web c? b?c online uy tin casino tr?c tuy?n casino tr?c tuy?n uy tin
order prednisone 10 mg tablet
casino tr?c tuy?n uy tin casino tr?c tuy?n uy tin web c? b?c online uy tin
prednisone10 mg
metformin buy australia
danh bai tr?c tuy?n choi casino tr?c tuy?n tren di?n tho?i web c? b?c online uy tin
synthroid 0.75
silkroad online pharmacy
casino tr?c tuy?n casino tr?c tuy?n vi?t nam danh bai tr?c tuy?n
http://casinvietnam.shop/# web c? b?c online uy tin
canadian pharmacy prices
casino tr?c tuy?n vi?t nam danh bai tr?c tuy?n web c? b?c online uy tin
generic cialis australia
tadalafil purchase
casino tr?c tuy?n uy tin casino online uy tin game c? b?c online uy tin
http://casinvietnam.shop/# danh bai tr?c tuy?n
game c? b?c online uy tin game c? b?c online uy tin casino tr?c tuy?n uy tin
choi casino tr?c tuy?n tren di?n tho?i casino tr?c tuy?n vi?t nam choi casino tr?c tuy?n tren di?n tho?i
synthroid 100 mg daily
prednisone 50 mg price in india
5mg prednisone
canadian pharmacy meds review best canadian online pharmacy reviews online pharmacy canada
synthroid 25
http://indiaph24.store/# top 10 pharmacies in india
mexican online pharmacies prescription drugs mexican pharmacy buying prescription drugs in mexico
glucophage tablets 250mg
п»їlegitimate online pharmacies india indian pharmacy mail order pharmacy india
https://mexicoph24.life/# buying prescription drugs in mexico online
can you buy valtrex over the counter in australia
online pharmacy cialis
no prescription prenisone
synthroid 37.5 mg
zithromax 250 price
http://canadaph24.pro/# canadian pharmacies comparison
canadian drug stores best online canadian pharmacy canadian pharmacy uk delivery
purple pharmacy mexico price list buying prescription drugs in mexico online п»їbest mexican online pharmacies
tadalafil soft tablets 20mg
price of lisinopril 20 mg
mexico drug stores pharmacies cheapest mexico drugs mexican pharmacy
http://canadaph24.pro/# is canadian pharmacy legit
online pharmacy synthroid
canadapharmacyonline Large Selection of Medications from Canada online pharmacy canada
buying from canadian pharmacies canadian pharmacy 24 com canadian drugstore online
canada rx pharmacy
lisinopril 60 mg tablet
https://mexicoph24.life/# mexican pharmaceuticals online
tadalafil 2.5 mg tablet
buying prescription drugs in mexico mexican pharmacy reputable mexican pharmacies online
https://mexicoph24.life/# mexico drug stores pharmacies
buying from online mexican pharmacy buying prescription drugs in mexico mexico drug stores pharmacies
generic synthroid online
india pharmacy reputable indian online pharmacy india pharmacy mail order
http://indiaph24.store/# buy medicines online in india
lisinopril 20 mg for sale
buy prescription drugs from india Generic Medicine India to USA buy medicines online in india
tadalafil generic 10mg
mexican border pharmacies shipping to usa Online Pharmacies in Mexico buying from online mexican pharmacy
prinivil 40 mg
mexican pharmacy mexican pharmacy п»їbest mexican online pharmacies
where can you get azithromycin
https://indiaph24.store/# Online medicine home delivery
how to order cialis pills
where can i buy generic valtrex
online canadian pharmacy reviews canadian pharmacies adderall canadian pharmacy
http://indiaph24.store/# Online medicine home delivery
buy synthroid 88 mcg online
mexico drug stores pharmacies mexico drug stores pharmacies medicine in mexico pharmacies
synthroid 25 pill
mexican drugstore online buying prescription drugs in mexico mexican mail order pharmacies
http://indiaph24.store/# pharmacy website india
buy generic cialis canada online
affordable pharmacy
Online medicine order Cheapest online pharmacy world pharmacy india
online pharmacy search
reputable mexican pharmacies online Mexican Pharmacy Online mexican rx online
pharmacy online shopping usa
buy real valtrex online
my canadian pharmacy rx Licensed Canadian Pharmacy canadapharmacyonline
metformin 227
http://indiaph24.store/# indian pharmacy paypal
canada pharmacy 24h
best european online pharmacy
canada drugs online Certified Canadian Pharmacies canadian online drugs
indian pharmacies safe Generic Medicine India to USA indian pharmacy
cost of generic lisinopril
zithromax uk
lisinopril 420
metformin tablet
canadian pharmacy phone number canadian pharmacies canadian pharmacy
https://mexicoph24.life/# mexican rx online
reputable indian online pharmacy indian pharmacy fast delivery india online pharmacy
india online pharmacy indian pharmacy top 10 pharmacies in india
indian pharmacies safe Cheapest online pharmacy online pharmacy india
lisinopril 20 mg price
https://mexicoph24.life/# buying prescription drugs in mexico online
canadian pharmacy meds canadian pharmacies canadian pharmacy oxycodone
buy zithromax pills
top online pharmacy india buy medicines from India indian pharmacy
where to buy cialis in uk
buy lisinopril 20 mg without prescription
best online pharmacies in mexico Online Pharmacies in Mexico mexico pharmacies prescription drugs
http://canadaph24.pro/# canadian drug pharmacy
azithromycin 500mg without prescription
Online medicine order Cheapest online pharmacy indian pharmacy paypal
lisinopril 20mg india
valtrex generic price canada
zestoretic price
canadian drug prices Licensed Canadian Pharmacy canadian pharmacy 1 internet online drugstore
where can i buy prednisone online without a prescription
big pharmacy online
lisinopril 40 mg tablet price
can you buy valtrex over the counter in uk
Online medicine order top 10 online pharmacy in india mail order pharmacy india
online pharmacy indonesia
tadalafil 20 mg mexico
http://canadaph24.pro/# canadapharmacyonline com
reputable indian pharmacies https://indiaph24.store/# buy medicines online in india
best india pharmacy
lisinopril from mexico
precription drugs from canada Licensed Canadian Pharmacy canadian pharmacy drugs online
valtrex 1000 mg price in india
reliable canadian pharmacy
where can you buy metformin
indian pharmacy paypal indian pharmacy mail order pharmacy india
valtrex non prescription
http://mexicoph24.life/# buying from online mexican pharmacy
cheapest online pharmacy india buy medicines from India indianpharmacy com
canadianpharmacy com Licensed Canadian Pharmacy canadianpharmacyworld com
how can i get valtrex
medicine in mexico pharmacies Online Pharmacies in Mexico buying from online mexican pharmacy
synthroid 300 mcg tablets
synthroid 0.5
indian pharmacies safe Generic Medicine India to USA Online medicine order
synthroid 025 mg
http://indiaph24.store/# buy medicines online in india
happy family store in canada
vipps canadian pharmacy Prescription Drugs from Canada canadian pharmacy prices
prinivil 10 mg
mexico drug stores pharmacies mexico pharmacy buying prescription drugs in mexico online
synthroid 125 coupon
where can i buy synthroid
п»їlegitimate online pharmacies india Generic Medicine India to USA reputable indian pharmacies
http://indiaph24.store/# india pharmacy
http://indiaph24.store/# online pharmacy india
lisinopril 40 mg price
mexico drug stores pharmacies mexico pharmacy reputable mexican pharmacies online
Online medicine order http://indiaph24.store/# reputable indian online pharmacy
reputable indian online pharmacy
pharmacy mall
http://mexicoph24.life/# mexico drug stores pharmacies
mexico drug stores pharmacies mexican pharmacy п»їbest mexican online pharmacies
medication from mexico pharmacy: mexican pharmacy – buying from online mexican pharmacy
https://indiaph24.store/# india online pharmacy
canadian pharmacy ltd canadian pharmacies best canadian pharmacy online
lisinopril 5 mg
mexican mail order pharmacies: Mexican Pharmacy Online – purple pharmacy mexico price list
tadalafil pharmacy
lisinopril 20 mg tablet price
lisinopril 10 mg prices: cost of lisinopril 20 mg – buy lisinopril 20 mg without a prescription
zithromax 2 pills
canadian lisinopril 10 mg where can i purchase lisinopril lisinopril brand name in india
http://cytotec.club/# buy misoprostol over the counter
https://lisinopril.network/# order cheap lisinopril
does tamoxifen make you tired: tamoxifen and depression – tamoxifen benefits
tamoxifen men natural alternatives to tamoxifen tamoxifen and osteoporosis
synthroid 0.025 mg
buy valtrex india
best price for lisinopril
http://ciprofloxacin.tech/# buy cipro online without prescription
reputable online pharmacy no prescription
benefits of tamoxifen tamoxifen endometrium nolvadex d
order cheap propecia price: buying cheap propecia – order propecia
zithromax online
lisinopril tabs 88mg zestril brand lisinopril 20 mg coupon
metformin 1000mg without prescription
zithromax over the counter usa
https://lisinopril.network/# 10 mg lisinopril cost
cytotec online: buy cytotec in usa – cytotec pills buy online
Cytotec 200mcg price buy cytotec online cytotec buy online usa
https://finasteride.store/# get generic propecia online
can you buy cialis online from canada
lisinopril 5mg pill
lisinopril 10 mg online no prescription: lisinopril 10 mg best price – lisinopril 30 mg tablet
http://nolvadex.life/# tamoxifen for breast cancer prevention
lisinopril 5 mg brand name lisinopril 102 lisinopril 40 coupon
pharmacy com canada
northwest pharmacy canada
Abortion pills online order cytotec online Cytotec 200mcg price
https://ciprofloxacin.tech/# cipro
buy cheap propecia without a prescription: order propecia without prescription – buy cheap propecia for sale
http://lisinopril.network/# lisinopril 100mcg
canadian pharmacy viagra 100mg
http://ciprofloxacin.tech/# cipro pharmacy
cost cheap propecia without a prescription cost of cheap propecia pill buy propecia without a prescription
buy cipro online without prescription: ciprofloxacin generic price – ciprofloxacin 500mg buy online
canadapharmacyonline legit
synthroid 88 mcg price
buy ciprofloxacin over the counter buy cipro online ciprofloxacin order online
http://ciprofloxacin.tech/# buy ciprofloxacin
buy misoprostol over the counter: buy cytotec pills online cheap – cytotec buy online usa
valtrex rx
buy cytotec online cytotec online buy cytotec over the counter
http://finasteride.store/# get cheap propecia without dr prescription
cytotec pills online: buy cytotec over the counter – buy misoprostol over the counter
ciprofloxacin mail online buy cipro online cipro for sale
azithromycin how to get
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
metformin 500 price india
https://cytotec.club/# cytotec pills buy online
buy azithromycin online uk
can you order lisinopril online how much is 30 lisinopril lisinopril in india
ciprofloxacin order online: buy cipro cheap – purchase cipro
generic cialis for sale in canada
buy cheap prednisone online
https://cytotec.club/# cytotec online
http://nolvadex.life/# tamoxifen warning
lisinopril 5 mg over the counter lisinopril brand online pharmacy lisinopril
cost of cheap propecia now: buy propecia prices – propecia order
nolvadex 20mg aromatase inhibitors tamoxifen natural alternatives to tamoxifen
http://finasteride.store/# buying generic propecia without prescription
synthroid 125 mcg price
lisinopril online prescription: lisinopril in usa – lisinopril tabs 4mg
online pharmacy without scripts
prednisone 20mg cheap
http://cytotec.club/# buy cytotec online fast delivery
canadian tadalafil online
tamoxifen hot flashes tamoxifen therapy natural alternatives to tamoxifen
175 mg synthroid
buy cheap propecia for sale: cost propecia for sale – buying generic propecia price
https://cytotec.club/# buy cytotec online
nolvadex online tamoxifen dose cost of tamoxifen
synthroid 250 mcg price
prednisone 500 mg
https://lisinopril.network/# prinivil 40 mg
synthroid 0.075 mg
where can i buy metformin online
prinivil generic: lisinopril 40 mg mexico – lisinopril 2.5 mg cost
lisinopril pill 20mg
cost generic propecia price buy propecia prices buy propecia without a prescription
https://lisinopril.network/# lisinopril online pharmacy
reliable rx pharmacy
https://cytotec.club/# purchase cytotec
ciprofloxacin mail online: cipro ciprofloxacin – cipro pharmacy
nolvadex side effects tamoxifen and depression tamoxifen and bone density
how to buy zithromax online
northern pharmacy
synthroid 05 mg
http://cytotec.club/# cytotec buy online usa
lisinopril 60 mg
ciprofloxacin over the counter cipro online no prescription in the usa cipro ciprofloxacin
Cytotec 200mcg price: buy cytotec over the counter – cytotec online
zovirax valtrex
where to buy metformin uk
safe reliable canadian pharmacy
https://lisinopril.network/# prescription medicine lisinopril
get propecia without insurance buying propecia tablets cost propecia without a prescription
cipro generic: buy cipro – cipro generic
legitimate canadian pharmacies
50mg lisinopril
Misoprostol 200 mg buy online buy cytotec pills online cheap Abortion pills online
http://cytotec.club/# cytotec abortion pill
https://ciprofloxacin.tech/# cipro for sale
zestril tab 10mg: zestril medication – zestoretic 25
http://ciprofloxacin.tech/# buy ciprofloxacin
zestoretic 20 25 lisinopril 2.15 mg lisinopril 20 mg coupon
how to get valtrex prescription online
nolvadex for pct: pct nolvadex – tamoxifen alternatives
azithromycin tablets otc
get generic propecia price order propecia pills buy cheap propecia tablets
http://lisinopril.network/# buy prinivil
lisinopril 20mg daily
https://lisinopril.network/# zestril 5 mg tablet
prednisone for sale online
generic synthroid price
cipro ciprofloxacin: buy cipro online canada – cipro pharmacy
cost propecia price buying generic propecia without rx cost of propecia price
http://nolvadex.life/# buy tamoxifen
canada rx pharmacy world
ciprofloxacin generic: cipro for sale – cipro ciprofloxacin
ciprofloxacin 500mg buy online buy ciprofloxacin antibiotics cipro
pharmacy online 365
https://cytotec.club/# cytotec online
lisinopril 250 mg
buy cytotec online fast delivery cytotec abortion pill order cytotec online
synthroid 0.5 mcg
https://nolvadex.life/# nolvadex half life
arimidex vs tamoxifen bodybuilding: generic tamoxifen – tamoxifen breast cancer
safe online pharmacies
cenforce.pro: Buy Cenforce 100mg Online – buy cenforce
where can i get azithromycin in australia
Kamagra 100mg kamagra sildenafil oral jelly 100mg kamagra
https://levitrav.store/# Buy Vardenafil online
synthroid purchase
zithromax 500mg pills
https://kamagra.win/# Kamagra Oral Jelly
http://cialist.pro/# Cheap Cialis
Cialis 20mg price: buy cialis overseas – Tadalafil price
sildenafil 50 mg price Buy Viagra online Generic Viagra for sale
http://viagras.online/# Sildenafil Citrate Tablets 100mg
Kamagra 100mg price: super kamagra – cheap kamagra
Buy Cenforce 100mg Online: cenforce for sale – Buy Cenforce 100mg Online
Kamagra tablets kamagra.win buy kamagra online usa
where can i get zithromax
canadian pharmacy 365
cheapest viagra Cheap Viagra 100mg sildenafil online
Levitra online pharmacy: Vardenafil price – Cheap Levitra online
http://kamagra.win/# Kamagra 100mg price
Sildenafil Citrate Tablets 100mg: Buy Viagra online – Viagra without a doctor prescription Canada
tadalafil tablet buy online india
generic cialis otc
https://viagras.online/# best price for viagra 100mg
Kamagra tablets buy kamagra online Kamagra tablets
Buy Tadalafil 20mg: buy cialis online – Tadalafil price
good pill pharmacy
how to buy cialis
generic sildenafil viagras.online best price for viagra 100mg
https://cenforce.pro/# order cenforce
Cheap generic Viagra online: Buy Viagra online cheap – cheapest viagra
synthroid rx
azithromycin 450 mg
buy cenforce cenforce.pro cheapest cenforce
synthroid 25 mcg price
10mg tadalafil without prescription
viagra without prescription: Buy generic 100mg Viagra online – sildenafil 50 mg price
http://cialist.pro/# Buy Cialis online
brand name synthroid price
metformin 100 mg tablets
valtrex from india
world pharmacy india
predinson prescriptions
https://viagras.online/# Cheap Sildenafil 100mg
levitra 20mg used for
Buy Tadalafil 20mg Generic Cialis without a doctor prescription Buy Tadalafil 5mg
buy tadalafil online
Generic Levitra 20mg: Cheap Levitra online – Cheap Levitra online
Cheap Levitra online Buy generic Levitra online Levitra generic best price
buy tadalafil europe
cialis tablets australia
zithromax 500mg price
http://levitrav.store/# Buy Vardenafil 20mg online
Kamagra 100mg price: kamagra oral jelly – cheap kamagra
http://cialist.pro/# Generic Cialis without a doctor prescription
Cialis without a doctor prescription Generic Tadalafil 20mg price cialis for sale
Kamagra Oral Jelly: kamagra – Kamagra tablets
brand name synthroid cheap
https://cenforce.pro/# Purchase Cenforce Online
best price for viagra 100mg viagras.online Generic Viagra online
Vardenafil buy online: Vardenafil online prescription – Levitra 10 mg best price
http://cenforce.pro/# cenforce.pro
lisinopril 5 mg for sale
valtrex online
glucophage compare
synthroid 0.088
Cialis over the counter Cialis 20mg price in USA Buy Tadalafil 5mg
lisinopril 40 mg pill
mexican rx online: reputable mexican pharmacies online – purple pharmacy mexico price list
https://pharmnoprescription.icu/# canadian pharmacy without prescription
prinivil drug cost
canada drugs online www canadianonlinepharmacy canadian pharmacy 24h com
ordering prednisone
http://pharmindia.online/# Online medicine home delivery
online shopping pharmacy india: indian pharmacy – indian pharmacy online
buy drugs from canada pharmacies in canada that ship to the us ed drugs online from canada
synthroid online paypal
http://pharmindia.online/# india pharmacy mail order
lisinopril online usa
mexico prescription drugs online: online canadian pharmacy no prescription – buying prescription drugs online from canada
canadian pharmacy non prescription: medicine with no prescription – pharmacies without prescriptions
canadian pharmacies not requiring prescription online pharmacy canadian pharmacy no prescription needed
recommended canadian pharmacies
lisinopril 50 mg
http://pharmworld.store/# canadian pharmacy no prescription
foreign pharmacy no prescription: cheapest pharmacy – canadian prescription pharmacy
non prescription medicine pharmacy pharm world store canadian pharmacy world coupon
30mg prednisone
preddisone no
buy prescription drugs from canada cheap: canadian pharmacy victoza – canadian pharmacy near me
https://pharmnoprescription.icu/# online pharmacies without prescriptions
mexican pharmacy: mexican rx online – mexican drugstore online
valtrex australia
lisinopril 104
canadian pharmacy 24 com: northwest canadian pharmacy – canadian world pharmacy
https://pharmcanada.shop/# canada drug pharmacy
the canadian pharmacy canadian pharmacy ratings best canadian online pharmacy
valtrex over the counter australia
reputable online pharmacy no prescription: pharm world store – pharmacy discount coupons
mexico drug stores pharmacies buying prescription drugs in mexico online mexico drug stores pharmacies
azithromycin 787
https://pharmmexico.online/# buying prescription drugs in mexico
buying prescription drugs in mexico: mexican pharmacy – mexican border pharmacies shipping to usa
mexican online pharmacies prescription drugs medication from mexico pharmacy mexican border pharmacies shipping to usa
http://pharmcanada.shop/# vipps canadian pharmacy
canadian pharmacy meds review: canadian pharmacy meds – canadian pharmacy checker
synthroid 137 mcg tab
online pharmacy non prescription drugs
metformin purchase uk
how to buy prescriptions from canada safely canadian drugs no prescription mexican prescription drugs online
northern pharmacy canada: legal canadian pharmacy online – canadian pharmacy 24h com
online pharmacy discount code
cheapest pharmacy for prescription drugs: canadian pharmacy without prescription – online pharmacy non prescription drugs
https://pharmmexico.online/# mexican online pharmacies prescription drugs
canadian online pharmacy no prescription cheapest pharmacy overseas pharmacy no prescription
http://pharmmexico.online/# purple pharmacy mexico price list
the canadian drugstore: legitimate canadian pharmacy online – pharmacy canadian superstore
6mg tadalafil
pharmacy website india india pharmacy mail order indian pharmacy
http://pharmnoprescription.icu/# best online pharmacy that does not require a prescription in india
canadian pharmacy prednisone
generic valtrex canada
buy medicines online in india: online pharmacy india – world pharmacy india
https://pharmmexico.online/# buying prescription drugs in mexico
how much is a valtrex prescription
buy valtrex no rx
canadian pharmacy no rx needed canadian pharmacy price checker canada pharmacy 24h
http://pharmnoprescription.icu/# best non prescription online pharmacy
prices for prednisone
canada pharmacy coupon: online pharmacy – legit non prescription pharmacies
indian pharmacy: indian pharmacies safe – top 10 pharmacies in india
us tadalafil
online cialis order
synthroid from india
canadian pharmacy online pharmacy com canada canada drugs online reviews
online pharmacy discount code: cheapest pharmacy to get prescriptions filled – pharmacy online 365 discount code
http://pharmindia.online/# п»їlegitimate online pharmacies india
canadian pharmaceutical drugstore
tadalafil 10mg australia
buy amoxicillin 500mg online amoxicillin generic amoxicillin 30 capsules price
doxycycline mono: order doxycycline 100mg without prescription – buy doxycycline cheap
http://gabapentinneurontin.pro/# cost of neurontin
prednisone price canada: buy prednisone online from canada – order prednisone 10mg
zithromax tablets for sale buy zithromax canada generic zithromax 500mg
neurontin cost generic: buying neurontin without a prescription – cost of brand name neurontin
prednisone 10 mg prednisone 20mg by mail order prednisone 25mg from canada
amoxicillin 500 mg brand name: buy amoxicillin 500mg usa – buy cheap amoxicillin
https://amoxila.pro/# amoxicillin 500mg capsule
prednisone purchase online: online prednisone 5mg – prednisone 30 mg tablet
where to buy metformin tablets
synthroid 37.5 mcg
best azithromycin tablet
http://doxycyclinea.online/# order doxycycline online
neurontin 100 mg caps: gabapentin 600 mg – neurontin 500 mg
zithromax 500mg price zithromax 500 mg lowest price drugstore online can you buy zithromax over the counter in canada
online doxycycline: doxycycline order online – doxycycline medication
order prednisone online no prescription
0.05 mg synthroid
tadalafil tablets 10 mg online
5mg prednisone
pharmacy canadian superstore
tadalafil in india
doxycycline mono: doxycycline 100mg capsules – doxycycline tablets
tadalafil 20mg lowest price
antibiotic amoxicillin: buying amoxicillin online – amoxicillin price without insurance
SightCare formula aims to maintain 20/20 vision without the need for any surgical process. This supplement is a perfect solution for people facing issues as they grow older. https://sightcare-web.com/
can you buy neurontin over the counter: neurontin 100mg discount – neurontin capsules
cost for generic lisinopril
pharmacy express
canadian pharmaceuticals online
prednisone pharmacy: prednisone 10 mg coupon – buy prednisone 20mg
canadian pharmacy prices
generic azithromycin online
synthroid europe
price of prednisone 5mg
where to buy amoxicillin 500mg: can you buy amoxicillin over the counter – amoxicillin 500mg capsules antibiotic
amoxicillin 500: amoxicillin 500 mg for sale – buy amoxicillin without prescription
doxycycline tetracycline doxycycline hyclate 100 mg cap where can i get doxycycline
https://doxycyclinea.online/# doxycycline hyc
60 mg prednisone daily: where to get prednisone – where to buy prednisone 20mg
http://zithromaxa.store/# zithromax for sale cheap
prednisone best price prednisone 1 mg daily prednisone generic brand name
neurontin 300 mg price: can i buy neurontin over the counter – neurontin 100mg capsule price
valtre
generic neurontin 600 mg neurontin capsule 400 mg where can i buy neurontin online
online pharmacy store
synthroid tabs
prescription prednisone cost: prednisone cream – prednisone pill
http://gabapentinneurontin.pro/# neurontin 300mg tablet cost
200 mg doxycycline: 100mg doxycycline – 100mg doxycycline
http://prednisoned.online/# prednisone over the counter south africa
buying neurontin without a prescription neurontin brand name in india neurontin 100mg price
prednisone canada prices: 400 mg prednisone – prednisone for sale in canada
buy prednisone without rx prednisone 10 mg price prednisone 40 mg rx
https://prednisoned.online/# prednisone 10 mg tablet
cheap cialis mexico
online doxycycline: doxycycline 200 mg – where to purchase doxycycline
WeJiJ is here to help get you the best gaming setup, gaming PC and guide you through the games you like to play with news, reviews and guides. https://wejij.com/
Find the latest technology news and expert tech product reviews. Learn about the latest gadgets and consumer tech products for entertainment, gaming, lifestyle and more. https://axget.com/
Testosil is a natural polyherbal testosterone booster designed to help men increase their testosterone levels safely and effectively. https://testosil-web.com/
buy doxycycline cheap odering doxycycline doxycycline 100mg dogs
http://amoxila.pro/# where to get amoxicillin over the counter
KeraBiotics is a meticulously-crafted natural formula designed to help people dealing with nail fungus. This solution, inspired by a sacred Amazonian barefoot tribe ritual https://kerabiotics-web.com/
FitSpresso is a natural dietary supplement designed to help with weight loss and improve overall health. It contains ingredients that have been studied clinically, which work together to promote healthy fat burning and enhance your metabolism! https://fitspresso-web.com/
Nagano Lean Body Tonic is a groundbreaking powdered supplement crafted to support your weight loss journey effortlessly. https://naganotonic-try.com/
Sugar Defender is a natural supplement that helps control blood sugar levels, lower the risk of diabetes, improve heart health, and boost energy. https://sugardefender-web.com/
– Shoot MASSIVE Loads For An Amazing Finish! https://semenax-try.com/
ZenCortex Research’s contains only the natural ingredients that are effective in supporting incredible hearing naturally.A unique team of health and industry professionals dedicated to unlocking the secrets of happier living through a healthier body. https://zencortex-try.com/
Serolean, a revolutionary weight loss supplement, zeroes in on serotonin—the key neurotransmitter governing mood, appetite, and fat storage. https://serolean-web.com/
BalMorex Pro is an exceptional solution for individuals who suffer from chronic joint pain and muscle aches. With its 27-in-1 formula comprised entirely of potent and natural ingredients, it provides unparalleled support for the health of your joints, back, and muscles. https://balmorex-try.com/
synthroid without prescription
can you purchase amoxicillin online: amoxicillin 500mg capsule cost – buy amoxicillin 500mg capsules uk
zithromax 500: buy generic zithromax online – where can i get zithromax over the counter
Support the health of your ears with 100% natural ingredients, finally being able to enjoy your favorite songs and movies https://quietumplus-try.com/
Peak BioBoost is a revolutionary dietary supplement that leverages the power of nature to support and improve your digestive system. https://peakbioboost-web.com/
price of doxycycline doxycycline generic how to order doxycycline
GutOptim is a digestive health supplement designed to support your gut and stomach. It restore balance in gut flora and reduce the symptoms of digestive disorders. https://gutoptim-try.com/
Burn Boost Powder™ is a proven weight loss powder drink that helps to lose weight and boosts the overall metabolism in the body. https://burnboost-web.com
NanoDefense Pro utilizes a potent blend of meticulously chosen components aimed at enhancing the wellness of both your nails and skin. https://nanodefense-web.com/
ONLINE EXCLUSIVE OFFER! Only Available for purchase on the official website. Secure Your Package while stocks last https://prodentim-web.com
https://gabapentinneurontin.pro/# neurontin 800 mg capsules
zithromax buy online no prescription zithromax for sale usa zithromax 500mg price in india
tadalafil 10mg tablets in india
prednisone 4mg: prednisone for cheap – order prednisone with mastercard debit
https://zithromaxa.store/# zithromax tablets
buy zithromax online with mastercard: zithromax 250mg – zithromax capsules 250mg
buy amoxicillin online uk how to get amoxicillin antibiotic amoxicillin
zithromax prescription online: where can i purchase zithromax online – zithromax cost
FlowForce Max is an innovative, natural and effective way to address your prostate problems, while addressing your energy, libido, and vitality. https://flowforcemax-web.com/
https://amoxila.pro/# amoxicillin 500 mg purchase without prescription
where can you buy zithromax how to get zithromax order zithromax without prescription
TestRX™ is a bodybuilding supplement. It’s formulated with high-quality natural ingredients proven to boost natural testosterone and stimulate muscle growth. https://testrx-web.com/
CLINICALLY PROVEN* To Increase Semen Volume And Intensity https://semenax-try.com/
cost of prednisone in canada: prednisone uk – can you buy prednisone online uk
DuoTrim is an innovative weight loss supplement that utilizes the power of natural plants and nutrients to create CSM bacteria https://duotrim-us.com/
http://gabapentinneurontin.pro/# cheap neurontin online
Dentitox Pro is a liquid dietary solution created as a serum to support healthy gums and teeth. Dentitox Pro formula is made in the best natural way with unique, powerful botanical ingredients that can support healthy teeth. https://dentitox-us.com/
metformin 1000 mg for sale
Sugar Balance is an ultra-potent blood sugar supplement that you can use to help control glucose levels, melt away fat and improve your overall health. https://sugarbalance-us.com/
GlucoFlush is an advanced formula specially designed for pancreas support that will let you promote healthy weight by effectively maintaining the blood sugar level and cleansing and strengthening your gut. https://glucoflush-us.com/
amoxicillin 500mg price: amoxicillin 500mg price canada – amoxicillin 500mg price canada
generic zithromax over the counter zithromax capsules buy zithromax no prescription
cost of synthroid brand name
cialis australia prices
prednisone without a script
Alpha Tonic is a powder-based supplement that uses multiple natural herbs and essential vitamins and minerals to help optimize your body’s natural testosterone levels. https://alphatonic-web.com
synthroid 75 mcg cost
can you buy zithromax over the counter in australia
VivoTonic™ is a 11-in-1 vital blood sugar support formula that may improve how the metabolism goes after the calories that consumers eat. https://vivotonic-web.com/
Progenifix is designed to help maximize weight loss results using a mixture of natural, science-backed ingredients. The formula also has secondary benefits, including promoting overall wellness and vitality and assisting your immune system. https://progenifix-web.com/
http://doxycyclinea.online/# buy cheap doxycycline online
AquaPeace is an all-natural nutritional formula that uses a proprietary and potent blend of ingredients and nutrients to improve overall ear and hearing health and alleviate the symptoms of tinnitus. https://aquapeace-web.com
buy doxycycline cheap doxycycline tablets buy doxycycline monohydrate
zithromax over the counter: zithromax 500 mg for sale – can i buy zithromax over the counter
buy prednisone without rx: brand prednisone – where to buy prednisone 20mg
buy generic valtrex
Gut Vita™ is a daily supplement that helps consumers to improve the balance in their gut microbiome, which supports the health of their immune system. It supports healthy digestion, even for consumers who have maintained an unhealthy diet for a long time. https://gutvita-us.com/
https://amoxila.pro/# can i buy amoxicillin online
how much is cialis in canada
Neuro-Thrive is a brain health supplement that claims to promote good memory and thinking skills and better quality sleep. This nootropic supplement achieves its cause with its potent blend of natural compounds and extracts that are proven to be effective in sharpening mental acuity. https://neurothrive-web.com/
Fast Lean Pro is a herbal supplement that tricks your brain into imagining that you’re fasting and helps you maintain a healthy weight no matter when or what you eat. It offers a novel approach to reducing fat accumulation and promoting long-term weight management. https://fastleanpro-web.com/
The ProNail Complex is a meticulously-crafted natural formula which combines extremely potent oils and skin-supporting vitamins. https://pronailcomplex-web.com/https://pronailcomplex-web.com/
amoxicillin 800 mg price: can you buy amoxicillin uk – cost of amoxicillin
medicine amoxicillin 500mg amoxicillin online purchase amoxicillin generic brand
Erectin is a clinically-proven dietary supplement designed to enhance male https://erectin-web.com/
100% Natural Formula Expressly Designed to Help Control Blood Sugar Levels, Improve Insulin Response And Support Overall Health https://glucotrusttry.com/
PowerBite stands as an innovative dental candy, dedicated to nurturing healthy teeth and gums. Infused with a potent formula, it champions the cause of a robust and radiant smile. Crafted meticulously https://powerbite-web.com/
Protoflow is a prostate health supplement featuring a blend of plant extracts, vitamins, minerals, fruit extracts, and more. https://protoflow-web.com/
prinivil 10 mg tab
Boostaro is a dietary supplement designed specifically for men who suffer from health issues. https://boostaro-try.com/
Unlock the incredible potential of Puravive! Supercharge your metabolism and incinerate calories like never before with our unique fusion of 8 exotic components. Bid farewell to those stubborn pounds and welcome a reinvigorated metabolism and boundless vitality. Grab your bottle today and seize this golden opportunity! https://puravive-web.com/
https://gabapentinneurontin.pro/# neurontin brand name 800mg
prednisone uk over the counter: prednisone 54 – prednisone 80 mg daily
amoxicillin canada price amoxicillin capsule 500mg price how to get amoxicillin over the counter
Zoracel is an extraordinary oral care product designed to promote healthy teeth and gums, provide long-lasting fresh breath, support immune health, and care for the ear, nose, and throat. https://zoracel-web.com
Cerebrozen is an excellent liquid ear health supplement purported to relieve tinnitus and improve mental sharpness, among other benefits. The Cerebrozen supplement is made from a combination of natural ingredients, and customers say they have seen results in their hearing, focus, and memory after taking one or two droppers of the liquid solution daily for a week. https://cerebrozen-try.com/
zithromax buy online: zithromax 250 mg australia – generic zithromax india
happy family online pharmacy
https://prednisoned.online/# prednisone 20 mg prices
neurontin uk: neurontin cap 300mg – gabapentin 300
neurontin 300mg tablet cost neurontin gabapentin where to buy neurontin
tadalafil 2.5 mg in india
zestoretic tabs
prednisone 475: prednisone purchase online – prednisone brand name
https://gabapentinneurontin.pro/# neurontin cost in canada
The human body can continue to live thanks to the correct functioning of certain systems. If even one of these systems does not work properly, it can cause problems in human life. https://calmlean-web.com/
prednisone 2.5 mg cost prednisone 20mg capsule order prednisone on line
can i buy valtrex online
Zeneara is marketed as an expert-formulated health supplement that can improve hearing and alleviate tinnitus, among other hearing issues. https://zeneara-web.com/
https://gabapentinneurontin.pro/# purchase neurontin
buy metformin 500
Pineal XT is a revolutionary supplement that promotes proper pineal gland function and energy levels to support healthy body function. https://pinealxt-web.com/
doxycycline 200 mg: buy doxycycline online 270 tabs – generic for doxycycline
VidaCalm is an all-natural blend of herbs and plant extracts that treat tinnitus and help you live a peaceful life. https://vidacalm-web.com/
Are you tired of looking in the mirror and noticing saggy skin? Is saggy skin making you feel like you are trapped in a losing battle against aging? Do you still long for the days when your complexion radiated youth and confidence? https://refirmance-web.com/
buy neurontin online no prescription purchase neurontin neurontin cap 300mg price
Gorilla Flow prostate is an all-natural dietary supplement for men which aims to decrease inflammation in the prostate to decrease common urinary tract issues such as frequent and night-time urination, leakage, or blocked urine stream. https://gorillaflow-web.com
prednisone 2 mg daily: prednisone 0.5 mg – prednisone cream rx
safe online pharmacies in canada
HoneyBurn is a revolutionary liquid weight loss formula that stands as the epitome of excellence in the industry. https://honeyburn-web.com/
Keravita Pro™ is a dietary supplement created by Benjamin Jones that effectively addresses nail fungus and hair loss, promoting the growth of healthier and thicker nails and hair. The formula is designed to target the underlying causes of these health issues and provide comprehensive treatment. https://keravitapro-web.com
zithromax tablets for sale: can you buy zithromax over the counter in canada – zithromax tablets for sale
http://zithromaxa.store/# generic zithromax 500mg
lisinopril 20mg tablets
buy prednisone 10 mg prednisone 475 prednisone over the counter
Volca Burn is a weight loss supplement that uses a “red tingle hack” to help you rapidly lose weight without dieting or exercising. https://volcaburn-web.com/
Xitox’s foot pads contain a combination of powerful herbs that help provide a soothing experience for your feet after a long day. https://xitox-web.com/
Hydrossential is actually a skincare serum or you can say a skincare supplement created by Emma Smith to help women keep their skin looking beautiful and flawless. https://hydrossential-web.com/
https://doxycyclinea.online/# buy doxycycline online uk
Carbofix is the revolutionary dietary formula that promises to activate weight loss without all the extra hard work. https://carbofix-try.com
gabapentin 300: neurontin medicine – neurontin 1200 mg
Reliver Pro is a dietary supplement formulated with a blend of natural ingredients aimed at supporting liver health
how can i get zithromax over the counter
lisinopril online pharmacy
amoxicillin order online no prescription: buy amoxicillin 500mg uk – amoxicillin 30 capsules price
amoxicillin 500mg buy online uk: where can you buy amoxicillin over the counter – canadian pharmacy amoxicillin
purchase prednisone from india prednisone online for sale prednisone 5 mg tablet
https://zithromaxa.store/# zithromax z-pak price without insurance
zithromax online usa: can i buy zithromax over the counter in canada – zithromax
how to buy doxycycline online buy cheap doxycycline online buy doxycycline cheap
875 mg amoxicillin cost: how to buy amoxicillin online – canadian pharmacy amoxicillin
maple leaf pharmacy in canada
http://zithromaxa.store/# zithromax buy online
prednisone 1 tablet cost of prednisone 10mg tablets order prednisone on line
pill pharmacy
medication zestoretic
how much is prednisone 5mg: prednisone over the counter south africa – 200 mg prednisone daily
buy doxycycline online without prescription: buy doxycycline without prescription uk – doxycycline 500mg
http://prednisoned.online/# 100 mg prednisone daily
neurontin 100mg price buy neurontin neurontin over the counter
prednisone 10 tablet
international online pharmacy
prednisone 15 mg tablet: prednisone 250 mg – prednisone capsules
buy doxycycline without prescription uk doxycycline 50 mg doxycycline vibramycin
valtrex order
http://gabapentinneurontin.pro/# neurontin capsules 100mg
neurontin prescription: neurontin tablets no script – cheap neurontin online
Payments Latest provides in-depth journalism and insight into the most impactful news and trends shaping payments. https://paymentslatest.com/
generic synthroid
zithromax price australia
synthroid for sale online
valtrex cream over the counter
neurontin tablets 100mg: neurontin 100mg capsule price – neurontin rx
http://amoxila.pro/# amoxicillin 500 mg without a prescription
prednisone for sale without a prescription buy prednisone 40 mg apo prednisone
zestril 25 mg
9 da auto news – https://9-da.com/
dtmliving multifamily news – https://dtmliving.com/
can i buy valtrex over the counter
online pharmacy delivery dubai
doxycycline hydrochloride 100mg buy doxycycline monohydrate where to purchase doxycycline
prescription for amoxicillin: amoxicillin 500mg for sale uk – amoxicillin 500mg for sale uk
https://amoxila.pro/# generic amoxicillin cost
tadalafil 5 coupon
can you order valtrex online
synthroid 1
synthroid 150 pill
zithromax purchase online: purchase zithromax online – zithromax canadian pharmacy
canadian pharmacy com
https://zithromaxa.store/# zithromax 500 mg
neurontin price comparison: buy neurontin 300 mg – drug neurontin 20 mg
zithromax for sale online where to buy zithromax in canada zithromax 250 mg
lisinopril 10 12.55mg
generic valtrex no prescription
Lasixiv provides news and analysis for IT executives. We cover big data, IT strategy, cloud computing, security, mobile technology, infrastructure, software and more. https://lasixiv.com
buy generic zithromax
doxycycline hydrochloride 100mg generic doxycycline doxycycline generic
synthroid 300 mcg
lisinopril 20 mg cost
synthroid 112 mcg
buy cheap zithromax
where can you buy cialis online
mexico pharmacies prescription drugs: mexico drug stores pharmacies – best mexican online pharmacies
buy synthroid online without prescription
purple pharmacy mexico price list: purple pharmacy mexico price list – buying from online mexican pharmacy
buying prescription drugs in mexico online mexican mail order pharmacies mexican border pharmacies shipping to usa
https://mexicanpharmacy1st.com/# mexican pharmacy
Wedstraunt has the latest news in the restaurant industry, covering topics like consumer trends, technology, marketing and branding, operations, mergers https://wedstraunt.com
medicine in mexico pharmacies: mexican border pharmacies shipping to usa – mexico drug stores pharmacies
https://mexicanpharmacy1st.online/# mexican border pharmacies shipping to usa
buying from online mexican pharmacy: pharmacies in mexico that ship to usa – reputable mexican pharmacies online
order metformin online without prescription
mexican drugstore online mexican mail order pharmacies mexico pharmacy
https://mexicanpharmacy1st.online/# mexican drugstore online
cheapest pharmacy canada
best mexican online pharmacies: buying prescription drugs in mexico online – best mexican online pharmacies
buying from online mexican pharmacy: mexican drugstore online – pharmacies in mexico that ship to usa
mexico drug stores pharmacies medication from mexico pharmacy mexico drug stores pharmacies
prinivil brand name
metformin 60 tablets 1000 mg
mexican online pharmacies prescription drugs: mexican mail order pharmacies – mexico pharmacy
family care rx pharmacy
reputable mexican pharmacies online mexican rx online mexican drugstore online
buy lisinopril online canada
reputable mexican pharmacies online: buying prescription drugs in mexico online – mexican pharmacy
mexico drug stores pharmacies п»їbest mexican online pharmacies mexican online pharmacies prescription drugs
synthroid 25
lisinopril 2 5 mg tablets
75 mg tadalafil
https://mexicanpharmacy1st.com/# mexico pharmacies prescription drugs
https://mexicanpharmacy1st.online/# mexican pharmacy
mexico pharmacy: mexico pharmacies prescription drugs – mexican border pharmacies shipping to usa
canadian pharmacy 1 internet online drugstore
lisinopril price comparison
Grpduk provides news and analysis for human resource executives. We cover topics like recruiting, HR management, employee learning https://grpduk.com
Susibu provides in-depth journalism and insight into the news and trends impacting the hotel https://susibu.com/
Sisanit provides in-depth journalism and insight into the news and trends impacting corporate counsel. https://sisanit.com/
metformin 1000 mg price in india
pharmacies in mexico that ship to usa п»їbest mexican online pharmacies mexican pharmaceuticals online
average cost of generic valtrex
https://mexicanpharmacy1st.com/# buying prescription drugs in mexico online
mexican pharmacy: reputable mexican pharmacies online – mexico pharmacy
mexican border pharmacies shipping to usa: medicine in mexico pharmacies – mexican pharmaceuticals online
mexican online pharmacies prescription drugs: mexican border pharmacies shipping to usa – mexican rx online
mexico drug stores pharmacies buying prescription drugs in mexico buying prescription drugs in mexico online
mexican drugstore online: buying prescription drugs in mexico – mexican pharmaceuticals online
pharmacy rx world canada
lisinopril 40 coupon
mexican pharmaceuticals online mexican rx online buying prescription drugs in mexico online
https://mexicanpharmacy1st.online/# buying from online mexican pharmacy
mexico drug stores pharmacies: medicine in mexico pharmacies – mexican rx online
https://mexicanpharmacy1st.shop/# buying prescription drugs in mexico online
Janmckinley provides news and analysis for waste and recycling executives. We cover topics like landfills, collections, regulation, waste-to-energy, corporate news, fleet management, and more. https://janmckinley.com
lisinopril 5 mg pill
buying from online mexican pharmacy: pharmacies in mexico that ship to usa – best online pharmacies in mexico
mexican mail order pharmacies buying prescription drugs in mexico buying from online mexican pharmacy
https://mexicanpharmacy1st.shop/# purple pharmacy mexico price list
mexico drug stores pharmacies: buying prescription drugs in mexico – buying prescription drugs in mexico online
can you buy tadalafil in mexico
https://mexicanpharmacy1st.com/# mexican pharmaceuticals online
http://mexicanpharmacy1st.com/# mexican pharmaceuticals online
online pharmacy prescription
best online pharmacies in mexico reputable mexican pharmacies online purple pharmacy mexico price list
mexico pharmacies prescription drugs: best online pharmacies in mexico – pharmacies in mexico that ship to usa
medicine in mexico pharmacies mexican pharmacy buying prescription drugs in mexico online
https://mexicanpharmacy1st.shop/# mexican pharmaceuticals online
mexico pharmacies prescription drugs: best mexican online pharmacies – mexican rx online
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://blackboxvending.com/
azithromycin buy online
https://mexicanpharmacy1st.shop/# reputable mexican pharmacies online
mexican rx online: reputable mexican pharmacies online – mexican drugstore online
how to buy valtrex without a prescription
best online pharmacies in mexico: mexico pharmacies prescription drugs – mexican pharmacy
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://mineryuta.com
metformin 1mg
buying prescription drugs in mexico online reputable mexican pharmacies online medicine in mexico pharmacies
https://mexicanpharmacy1st.shop/# mexican mail order pharmacies
synthroid 30 mg
mexico drug stores pharmacies: buying from online mexican pharmacy – mexican border pharmacies shipping to usa
pharmacies in mexico that ship to usa pharmacies in mexico that ship to usa mexican rx online
http://mexicanpharmacy1st.com/# mexican online pharmacies prescription drugs
prednisone 20 mg
lisinopril 2.5 mg
medication from mexico pharmacy: buying prescription drugs in mexico online – buying prescription drugs in mexico online
pharmacies in mexico that ship to usa: reputable mexican pharmacies online – mexico pharmacies prescription drugs
zithromax generic
buy lisinopril uk
mexican rx online п»їbest mexican online pharmacies reputable mexican pharmacies online
zithromax 250
https://mexicanpharmacy1st.shop/# mexican pharmaceuticals online
zestoretic
pharmacies in mexico that ship to usa: reputable mexican pharmacies online – best mexican online pharmacies
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://acmesignz.com/
mexico drug stores pharmacies buying prescription drugs in mexico п»їbest mexican online pharmacies
synthroid 0.137 mg
https://mexicanpharmacy1st.shop/# purple pharmacy mexico price list
http://mexicanpharmacy1st.com/# mexico pharmacy
mexican rx online: reputable mexican pharmacies online – buying from online mexican pharmacy
20 mg prednisone daily
tadalafil soft gel capsule
how much is lisinopril 10 mg
synthroid 75 mcg tab
neurontin 100 mg caps neurontin 900 mg neurontin 600 mg pill
sugar defender: https://peyfon.com/
generic synthroid price
online canadian pharmacy coupon
sugar defender: https://seahorsesoap.com/
india buy prednisone online
http://propeciaf.online/# buy propecia online
neurontin medicine: medicine neurontin – neurontin capsule 600mg
medicine ciprofloxacin 500mg
retin a
cytotec buy online usa buy cytotec pills online cheap buy cytotec
baclofen pill
where buy cheap clomid no prescription: how can i get generic clomid without insurance – can you get generic clomid
flomax 21339
https://cytotec.xyz/# Cytotec 200mcg price
accutane rx
sugar defender: https://sourceprousa.com/
buy cytotec in usa buy cytotec in usa buy cytotec over the counter
diflucan 1140
buy zithromax usa
purchase cytotec: п»їcytotec pills online – buy cytotec online fast delivery
where buy cheap clomid without rx where can i buy generic clomid without prescription get cheap clomid without a prescription
can i buy neurontin over the counter: neurontin gel – 2000 mg neurontin
https://propeciaf.online/# cost cheap propecia online
zithromax discount
neurontin 300mg capsule neurontin medication neurontin capsule 400 mg
synthroid 137.5
http://gabapentin.club/# canada neurontin 100mg discount
albuterol price uk
how can i get generic clomid for sale: can i order cheap clomid no prescription – where to buy clomid
zithromax strep throat
neurontin canada online: neurontin 800 mg tablets best price – medication neurontin
1 lisinopril lisinopril brand name cost buy lisinopril 20 mg without prescription
Misoprostol 200 mg buy online: buy misoprostol over the counter – buy misoprostol over the counter
sugar defender: https://lindadicesare.com/
sugar defender: https://drdenisemichele.com/
ciprofloxacin order online
sugar defender: https://alchemyfashiongroup.com/
http://propeciaf.online/# get generic propecia without rx
buying cheap propecia online cost cheap propecia online order propecia for sale
https://gabapentin.club/# neurontin 100mg cap
how to get generic clomid no prescription: can i order generic clomid now – where can i buy cheap clomid without a prescription
baclofen price uk
lisinopril 10 mg no prescription 3 lisinopril lisinopril medicine
buy lisinopril online: buy lisinopril 40 mg online – cheapest price for lisinopril
propecia buy online australia
tretinoin 0.05 canada
http://cytotec.xyz/# cytotec buy online usa
neurontin 204 neurontin 600 mg tablet neurontin online pharmacy
buy vermox online usa
price for synthroid 100 mcg
http://cytotec.xyz/# buy cytotec online fast delivery
cheap propecia price: order generic propecia pills – propecia prices
buy cytotec in usa buy cytotec Abortion pills online
can you buy flomax over the counter
neurontin capsules: neurontin 100 mg tablets – neurontin cost uk
buy tadacip tablets online
where to get provigil
http://propeciaf.online/# propecia cost
get generic propecia pill get generic propecia generic propecia without insurance
zithromax 250 mg tablet
http://lisinopril.club/# price of lisinopril 5mg
neurontin 100 mg cost: neurontin 600 – neurontin discount
buy cytotec online buy cytotec online buy cytotec over the counter
lasix cost
lasix pills 20 mg
can you get clomid no prescription: can you get generic clomid tablets – clomid for sale
clomid for sale online cheap
https://propeciaf.online/# cost cheap propecia without dr prescription
cytotec buy online usa buy cytotec online buy cytotec online
cheap baclofen online
cheap propecia prices: buy propecia pill – buy propecia no prescription
neurontin price australia: drug neurontin – neurontin prescription cost
order generic propecia pill generic propecia without a prescription buying propecia tablets
dexamethasone 2mg
buy cheap propecia without a prescription: generic propecia without dr prescription – buying generic propecia without insurance
http://propeciaf.online/# get generic propecia tablets
brand neurontin 100 mg canada buy brand neurontin neurontin without prescription
tretinoin topical
zitromax
buy doxycycline over the counter
baclofen tablet price in india
cost cheap propecia for sale: order generic propecia price – cost of propecia online
cost of generic propecia pills cost of propecia without insurance buying cheap propecia
cost of cheap propecia pill: cost of propecia online – get generic propecia tablets
get cheap propecia without a prescription order generic propecia for sale cost of generic propecia price
where to buy advair diskus
cost of bactrim
albuterol uk
buy lyrica 150mg
150 mg diflucan online
buy roaccutane
buy lyrica online europe
neurontin 1800 mg neurontin cost uk neurontin 300mg caps
sildalis india
neurontin pill: neurontin capsule 600mg – generic neurontin 600 mg
retin a cream mexico pharmacy
https://cheapestcanada.com/# canadian pharmacy online store
dexamethasone 0.1 cream
dexamethasone 4 mg cost
canadian pharmacy without prescription 36and6health canadian pharmacy without prescription
strattera 20mg
azithromycin online without prescription
buy lyrica 50 mg
azithromycin 500 mg cost in australia
https://cheapestcanada.shop/# canada rx pharmacy
https://cheapestindia.shop/# best online pharmacy india
cost for lyrica
azithromycin medication
http://cheapestcanada.com/# canadian online pharmacy
buy zithromax cheap
modafinil 200mg australia
https://36and6health.com/# pharmacy coupons
pharmacy online 365 discount code online pharmacy no prescription needed canadian pharmacy coupon
http://36and6health.com/# legal online pharmacy coupon code
how can i get diflucan over the counter
retin a pharmacy prices
lyrica 200 mg
cheap accutane singapore
https://cheapestindia.shop/# indian pharmacy paypal
azithromycin tablets for sale
baclofen 10 tablet
https://cheapestcanada.shop/# online canadian pharmacy review
rxpharmacycoupons: cheapest pharmacy – cheapest pharmacy to fill prescriptions with insurance
https://cheapestindia.shop/# india pharmacy
amoxicillin 500 price india
advair diskus in india
buy generic accutane
https://cheapestcanada.shop/# canada drugs reviews
azithromycin in mexico
vermox australia
flomax 0.8
buy advair online
https://cheapestmexico.shop/# mexico drug stores pharmacies
clomid infertility
tretinoin cream india online order
india online pharmacy cheapest online pharmacy india online shopping pharmacy india
http://cheapestcanada.com/# my canadian pharmacy
diflucan 500
http://36and6health.com/# canadian pharmacy coupon
http://cheapestmexico.com/# mexican pharmaceuticals online
where can i buy modafinil
buy accutane 10 mg
how much is clomid uk
lioresal
online pharmacy that does not require a prescription: cheapest and fast – no prescription online pharmacies
advair 2017 coupon
http://cheapestindia.com/# indian pharmacies safe
pharmacy rx world canada: cheapestcanada.com – canada online pharmacy
order dexamethasone online
lyrica 50 mg coupon
https://cheapestmexico.shop/# reputable mexican pharmacies online
toradol for fever
price of metformin 500mg tablets
furosemide 20 mg tablet
vermox cost
where to buy vermox
how to get diflucan
retin a otc uk
https://cheapestindia.shop/# india online pharmacy
https://36and6health.com/# promo code for canadian pharmacy meds
buy tadacip 20 mg without prescription
zithromax brand name
https://36and6health.shop/# canada pharmacy coupon
cheap accutane for sale
https://36and6health.shop/# no prescription needed canadian pharmacy
tamoxifen 20
canada pharmacy coupon foreign pharmacy no prescription online pharmacy non prescription drugs
metformin price canada
https://36and6health.shop/# mail order pharmacy no prescription
synthroid 50 mcg tab
http://cheapestindia.com/# indian pharmacy online
buy cheap sildalis
vermox cost uk
how can i get valtrex
ventolin uk
purchase prednisone no prescription
diflucan buy
furosemide 80
medikament ohne rezept notfall: online apotheke – gГјnstige online apotheke
online apotheke rezept: online apotheke preisvergleich – gГјnstigste online apotheke
cheapest flomax
trouver un m̩dicament en pharmacie: Pharmacie en ligne livraison Europe Рpharmacie en ligne france pas cher
top farmacia online farmacia online piГ№ conveniente farmacia online piГ№ conveniente
https://eumedicamentenligne.com/# pharmacie en ligne sans ordonnance
top farmacia online: farmacia online senza ricetta – farmacia online piГ№ conveniente
medikamente rezeptfrei: gГјnstigste online apotheke – online apotheke versandkostenfrei
farmacie online affidabili п»їFarmacia online migliore farmacie online sicure
dexamethasone cream
cheap propecia india
zovirax tablets 200mg
http://euapothekeohnerezept.com/# online apotheke
farmaci senza ricetta elenco: top farmacia online – top farmacia online
farmacias online seguras en españa: farmacias direct – farmacia online envÃo gratis
farmacia online envГo gratis farmacia online espaГ±a envГo internacional farmacias online baratas
internet apotheke: online apotheke preisvergleich – online apotheke rezept
pharmacie en ligne fiable: pharmacie en ligne france fiable – pharmacie en ligne france fiable
pharmacie en ligne pas cher pharmacie en ligne france livraison internationale pharmacie en ligne pas cher
online apotheke versandkostenfrei: günstigste online apotheke – online apotheke günstig
vermox mebendazole
online apotheke gГјnstig: online apotheke preisvergleich – online apotheke versandkostenfrei
vermox
pharmacie en ligne avec ordonnance: pharmacie en ligne avec ordonnance – pharmacie en ligne fiable
sildalis canada
pharmacie en ligne france livraison belgique п»їpharmacie en ligne france pharmacie en ligne pas cher
pharmacie en ligne pas cher Pharmacie sans ordonnance Achat mГ©dicament en ligne fiable
farmacia online senza ricetta: comprare farmaci online all’estero – top farmacia online
farmacia online envÃo gratis: farmacias online seguras – farmacia online barata y fiable
where to buy zithromax online
can you buy amoxicillin uk
how to get modafinil
pharmacies en ligne certifiГ©es: pharmacie en ligne france livraison internationale – vente de mГ©dicament en ligne
dexamethasone 500mcg
Farmacia online più conveniente: farmacia online – Farmacia online miglior prezzo
pharmacie en ligne avec ordonnance п»їpharmacie en ligne france Pharmacie sans ordonnance
buy augmentin 1000 mg
https://eumedicamentenligne.shop/# п»їpharmacie en ligne france
farmacia online españa envÃo internacional: farmacia online barata y fiable – farmacia online barcelona
п»їFarmacia online migliore top farmacia online Farmacie online sicure
farmacie online sicure: acquistare farmaci senza ricetta – Farmacia online piГ№ conveniente
п»їpharmacie en ligne france: pharmacie en ligne france pas cher – pharmacie en ligne france livraison internationale
buy synthroid 200 mcg
where to buy clomid without a prescription
farmacie online affidabili: Farmacia online piГ№ conveniente – acquistare farmaci senza ricetta
buy azithromycin without a prescription
pharmacie en ligne france fiable: Pharmacie en ligne livraison Europe Рtrouver un m̩dicament en pharmacie
comprare farmaci online con ricetta top farmacia online Farmacie online sicure
doxycycline medication pills
п»їpharmacie en ligne france: acheter mГ©dicament en ligne sans ordonnance – pharmacie en ligne pas cher
azithromycin 500mg online
cialis daily for sale
comprare farmaci online con ricetta: comprare farmaci online con ricetta – farmacie online affidabili
farmacia online espaГ±a envГo internacional farmacia online barata y fiable farmacia online madrid
Farmacie online sicure: comprare farmaci online all’estero – п»їFarmacia online migliore
Pharmacie Internationale en ligne: acheter mГ©dicament en ligne sans ordonnance – Achat mГ©dicament en ligne fiable
modafinil online australia
pharmacie en ligne france livraison internationale: Achat m̩dicament en ligne fiable Рpharmacie en ligne
nolvadex buy
farmacia online madrid farmacias online seguras farmacia online barcelona
doxycycline tablets cost
pharmacie en ligne france livraison belgique: pharmacie en ligne livraison europe – pharmacie en ligne france livraison internationale
farmacia en casa online descuento farmacia online barata y fiable farmacias online seguras
pharmacie en ligne france livraison internationale: pharmacie en ligne pas cher – pharmacie en ligne sans ordonnance
online apotheke gГјnstig: europa apotheke – gГјnstigste online apotheke
vermox tablet india
pharmacie en ligne sans ordonnance: pharmacie en ligne pas cher – pharmacie en ligne france livraison internationale
trouver un mГ©dicament en pharmacie: Achat mГ©dicament en ligne fiable – pharmacie en ligne livraison europe
http://eufarmaciaonline.com/# farmacias online seguras en espaГ±a
pharmacie en ligne avec ordonnance Pharmacie sans ordonnance pharmacie en ligne sans ordonnance
vardenafil vs tadalafil
farmacias direct: farmacias direct – farmacia online barata y fiable
pharmacie en ligne france pas cher: trouver un m̩dicament en pharmacie Рpharmacie en ligne france pas cher
pharmacie en ligne fiable п»їpharmacie en ligne france pharmacie en ligne sans ordonnance
Farmacia online piГ№ conveniente: comprare farmaci online all’estero – acquisto farmaci con ricetta
where can i buy augmentin
pharmacie en ligne france fiable: pharmacie en ligne fiable – pharmacies en ligne certifiГ©es
comprare farmaci online all’estero: top farmacia online – Farmacia online migliore
п»їfarmacia online espaГ±a: farmacia online barcelona – farmacias online seguras en espaГ±a
pharmacie en ligne fiable pharmacie en ligne france livraison belgique Pharmacie Internationale en ligne
buy lasix uk
pharmacie en ligne: pharmacie en ligne france pas cher – pharmacie en ligne france livraison belgique
comprare farmaci online all’estero farmacia online senza ricetta farmacie online sicure
Pharmacie Internationale en ligne: pharmacie en ligne france fiable – pharmacie en ligne france livraison belgique
trouver un m̩dicament en pharmacie: Achat m̩dicament en ligne fiable РPharmacie en ligne livraison Europe
farmacia online 24 horas: farmacia online barata – farmacia online madrid
gГјnstigste online apotheke online apotheke gГјnstig eu apotheke ohne rezept
shop apotheke gutschein: internet apotheke – shop apotheke gutschein
online apotheke versandkostenfrei: europa apotheke – ohne rezept apotheke
farmacia online senza ricetta farmacie online autorizzate elenco top farmacia online
http://eumedicamentenligne.com/# pharmacie en ligne france pas cher
singapore sildalis
vermox pharmacy uk
pharmacie en ligne fiable: Pharmacie en ligne livraison Europe – pharmacie en ligne france livraison belgique
farmacia online barcelona: farmacia barata – farmacia online barcelona
online apotheke rezept: internet apotheke – günstige online apotheke
average cost of generic zithromax
http://cenligne.com/# pharmacie en ligne
canadian pharmacy accutane
pharmacie en ligne: pharmacie en ligne sans ordonnance – pharmacie en ligne france fiable
Pharmacie sans ordonnance: Levitra acheter – pharmacie en ligne france livraison internationale
pharmacie en ligne fiable: pharmacie en ligne sans ordonnance – pharmacie en ligne france pas cher
Pharmacie en ligne livraison Europe: Acheter Cialis – pharmacie en ligne avec ordonnance
buy augmentin 1000 mg
Pharmacie en ligne livraison Europe pharmacie en ligne avec ordonnance vente de mГ©dicament en ligne
buy provigil paypal
tamoxifen 10 mg tablet
pharmacie en ligne avec ordonnance: Levitra pharmacie en ligne – pharmacie en ligne france livraison belgique
acheter mГ©dicament en ligne sans ordonnance: cialis sans ordonnance – pharmacie en ligne france fiable
toradol eye drops
Viagra gГ©nГ©rique pas cher livraison rapide Viagra generique en pharmacie SildГ©nafil 100 mg prix en pharmacie en France
pharmacie en ligne: achat kamagra – pharmacie en ligne france livraison belgique
zovirax price usa
pharmacie en ligne pas cher: Levitra sans ordonnance 24h – pharmacie en ligne france fiable
average cost of cialis prescription
Prix du Viagra en pharmacie en France: Acheter du Viagra sans ordonnance – Prix du Viagra 100mg en France
Pharmacie sans ordonnance: pharmacie en ligne – Pharmacie en ligne livraison Europe
https://viaenligne.shop/# Viagra sans ordonnance 24h Amazon
purchase effexor online
price of retin a micro
order amoxicillin no prescription
lioresal baclofen
Prix du Viagra 100mg en France: Viagra sans ordonnance 24h – Le gГ©nГ©rique de Viagra
Meilleur Viagra sans ordonnance 24h: Acheter du Viagra sans ordonnance – Viagra pas cher inde
doxycycline order uk
Pharmacie sans ordonnance: kamagra oral jelly – trouver un mГ©dicament en pharmacie
lasix with no prescription
Viagra femme ou trouver: Meilleur Viagra sans ordonnance 24h – Viagra gГ©nГ©rique sans ordonnance en pharmacie
https://viaenligne.shop/# Prix du Viagra en pharmacie en France
lasix canada no prescription
buy vermox cheap
modafinil online australia
provigil 200 mg price
Pharmacie en ligne livraison Europe: Levitra sans ordonnance 24h – Pharmacie en ligne livraison Europe
Hello.
This post was created with XRumer 23 StrongAI.
Good luck 🙂
Pharmacie Internationale en ligne: Levitra sans ordonnance 24h – pharmacie en ligne sans ordonnance
ventolin otc uk
lyrica prescription cost
lasix 50 mg
modafinil pharmacy price
lyrica 25 mg cost
modafinil price
best generic provigil
Acheter viagra en ligne livraison 24h: Viagra generique en pharmacie – Viagra sans ordonnance 24h Amazon
pharmacie en ligne france fiable: pharmacie en ligne france pas cher – pharmacie en ligne
order modafinil australia
provigil canada purchase online
Pharmacie sans ordonnance: pharmacie en ligne – trouver un mГ©dicament en pharmacie
sterapred ds
accutane medicine price
clomid pills uk
pharmacie en ligne france livraison internationale: Pharmacie sans ordonnance – pharmacie en ligne
effexor xr
where to get clomid pills
п»їpharmacie en ligne france: pharmacie en ligne sans ordonnance – Pharmacie en ligne livraison Europe
azithromycin 1mg
where can you buy modafinil over the counter
pharmacie en ligne france livraison internationale: Levitra pharmacie en ligne – trouver un mГ©dicament en pharmacie
Hello!
This post was created with XRumer 23 StrongAI.
Good luck 🙂
propecia 1mg price
buy modafinil canada
pharmacie en ligne fiable: pharmacie en ligne – pharmacie en ligne pas cher
flomax uk
pharmacie en ligne france livraison belgique: kamagra gel – pharmacie en ligne
provigil 100 mg tablet
п»їpharmacie en ligne france: pharmacie en ligne pas cher – Pharmacie sans ordonnance
dexona 0.5 mg
Pharmacie sans ordonnance: Levitra 20mg prix en pharmacie – pharmacie en ligne fiable
pharmacie en ligne france livraison belgique: pharmacie en ligne – pharmacie en ligne livraison europe
azithromycin 250 mg tabs
Prix du Viagra 100mg en France: Viagra sans ordonnance 24h Amazon – Viagra vente libre pays
buy generic zithromax
https://kamagraenligne.com/# acheter médicament en ligne sans ordonnance
Viagra prix pharmacie paris: Acheter du Viagra sans ordonnance – Viagra gГ©nГ©rique sans ordonnance en pharmacie
where to get tretinoin
furosemide 20
pharmacies en ligne certifiГ©es: Medicaments en ligne livres en 24h – Pharmacie sans ordonnance
40 mg prednisone daily
baclofen 10 mg price
cipro price
how to buy metformin in usa
metformin 500
pharmacie en ligne sans ordonnance: kamagra oral jelly – vente de mГ©dicament en ligne
baclofen buy online uk
accutane cream india
vente de mГ©dicament en ligne: kamagra en ligne – Pharmacie Internationale en ligne
acyclovir cream price
Achat mГ©dicament en ligne fiable: kamagra gel – acheter mГ©dicament en ligne sans ordonnance
pharmacie en ligne france pas cher: Acheter Cialis 20 mg pas cher – pharmacie en ligne livraison europe
lyrica price comparison
azithromycin 500 tablet price
prednisone 20 mg over the counter
trouver un mГ©dicament en pharmacie: pharmacie en ligne france pas cher – Pharmacie en ligne livraison Europe
retin a 0.025 price
can i buy accutane over the counter
dexamethasone 2mg
accutane cost generic
Pharmacie en ligne livraison Europe: Pharmacies en ligne certifiees – п»їpharmacie en ligne france
12 mg flomax
amoxicillin 500 mg mexico
diflucan 50
pharmacie en ligne sans ordonnance: Levitra sans ordonnance 24h – acheter mГ©dicament en ligne sans ordonnance
strattera 40 mg
accutane in mexico
modafinil tablet price in india
vente de mГ©dicament en ligne: Levitra pharmacie en ligne – pharmacie en ligne fiable
acheter mГ©dicament en ligne sans ordonnance: kamagra livraison 24h – pharmacie en ligne livraison europe
zovirax cream over the counter
purchase azithromycin
Pharmacie Internationale en ligne: kamagra gel – trouver un mГ©dicament en pharmacie
pharmacie en ligne france livraison belgique: levitra en ligne – pharmacie en ligne france livraison internationale
pharmacie en ligne sans ordonnance: Levitra pharmacie en ligne – pharmacie en ligne france livraison internationale
zithromax pills 500mg
propecia canada pharmacy online
strattera online canada
pharmacie en ligne livraison europe: Levitra pharmacie en ligne – pharmacie en ligne livraison europe
vente de mГ©dicament en ligne: Cialis sans ordonnance 24h – п»їpharmacie en ligne france
buy zithromax 500mg online
pharmacies en ligne certifiГ©es: kamagra 100mg prix – Achat mГ©dicament en ligne fiable
lioresal drug
tretinoin pharmacy
azithromycin 500 mg tablet cost
retin a without a prescription from mexico
Pharmacie sans ordonnance: Acheter Cialis 20 mg pas cher – vente de mГ©dicament en ligne
clomid otc canada
buy tadacip 10 mg
modafinil pill
modafinil prescription price
Pharmacie sans ordonnance: levitra en ligne – pharmacie en ligne france livraison belgique
pharmacie en ligne avec ordonnance: levitra en ligne – п»їpharmacie en ligne france
dexamethasone cost
order accutane
pharmacie en ligne france fiable: pharmacie en ligne france pas cher – pharmacie en ligne france livraison belgique
pharmacie en ligne livraison europe: Levitra sans ordonnance 24h – pharmacie en ligne
vermox online canada
pharmacie en ligne france pas cher: Acheter Cialis 20 mg pas cher – acheter mГ©dicament en ligne sans ordonnance
buy modafinil paypal
order retin a without a prescription
Pharmacie en ligne livraison Europe: pharmacie en ligne pas cher – Pharmacie Internationale en ligne
generic propecia tablets
order azithromycin over the counter
20 mg accutane daily
lioresal 10 mg tab
azithromycin 1000 mg buy
Quand une femme prend du Viagra homme: viagra sans ordonnance – Viagra sans ordonnance pharmacie France
Pharmacie Internationale en ligne: Levitra sans ordonnance 24h – Achat mГ©dicament en ligne fiable
where can i buy generic flomax
Talk to the manager or supervisor they will understand your need as they have spent a lot of time in this service sector.
pharmacie en ligne fiable: kamagra livraison 24h – pharmacie en ligne france livraison belgique
diflucan discount coupon
accutane india cost
valtrex 500 mg
can you buy cialis from canada
pharmacie en ligne france livraison belgique: kamagra livraison 24h – Pharmacie sans ordonnance
purchase provigil from canada
pharmacie en ligne sans ordonnance: Acheter Cialis – Pharmacie en ligne livraison Europe
cipro 750 mg
dexamethasone cream over the counter
vente de mГ©dicament en ligne: Acheter Cialis – Pharmacie en ligne livraison Europe
viagra over the counter mexico
generic propecia 1mg
Achat mГ©dicament en ligne fiable: kamagra oral jelly – trouver un mГ©dicament en pharmacie
lasix 40 mg tablet
where to buy generic propecia uk
Achat mГ©dicament en ligne fiable: Cialis sans ordonnance 24h – pharmacie en ligne france pas cher
order clomid online usa
zovirax pills cost
advair 250 coupon
Viagra sans ordonnance 24h suisse: Meilleur Viagra sans ordonnance 24h – Viagra pas cher livraison rapide france
lyrica pill
diflucan 250 mg
can you purchase azithromycin online
ciprofloxacin 500 mg capsules
how much is augmentin 625mg
pharmacie en ligne: Levitra pharmacie en ligne – Achat mГ©dicament en ligne fiable
sildenafil pharmacy nz
pharmacie en ligne: kamagra gel – pharmacie en ligne france livraison internationale
joint pain and endometriosis
can i buy modafinil
2nd finger joint pain
pharmacie en ligne france pas cher: Levitra acheter – pharmacie en ligne pas cher
Viagra gГ©nГ©rique sans ordonnance en pharmacie: Acheter du Viagra sans ordonnance – Viagra 100 mg sans ordonnance
middle finger hand joint swelling and pain
accutane canadian pharmacy
http://jointpain.top/ – lyrica joint pain side effect
pharmacie en ligne france fiable: Pharmacies en ligne certifiees – pharmacie en ligne pas cher
azithromycin 1000 mg price
propecia online uk
Pharmacie sans ordonnance: Acheter Cialis 20 mg pas cher – pharmacie en ligne fiable
http://jointpain.top/ – alcohol joint pain relief
ciprofloxacin medicine
generic provigil online
http://jointpain.top/ – which facet joint is responsible for hip pain
strattera medication
propecia no prescription
http://jointpain.top/ – can hashimoto’s disease cause joint pain
pharmacie en ligne france livraison internationale: pharmacie en ligne – Pharmacie sans ordonnance
pharmacie en ligne france livraison internationale: pharmacie en ligne – Pharmacie Internationale en ligne
Pharmacie Internationale en ligne: Levitra pharmacie en ligne – pharmacie en ligne avec ordonnance
500 mg azithromycin
pharmacie en ligne france pas cher: levitra generique sites surs – trouver un mГ©dicament en pharmacie
vente de mГ©dicament en ligne: Acheter Cialis 20 mg pas cher – trouver un mГ©dicament en pharmacie
Viagra sans ordonnance 24h: Viagra generique en pharmacie – Prix du Viagra 100mg en France
baclofen no preciption
dexamethasone 6 mg tablet
zithromax 1000 mg pills
canadian pharmacy modafinil
zithromax india
Pharmacie en ligne livraison Europe: Levitra pharmacie en ligne – п»їpharmacie en ligne france
azithromycin 500 mg tablet brand name
Pharmacie en ligne livraison Europe: Pharmacie Internationale en ligne – pharmacie en ligne fiable
http://levitraenligne.com/# trouver un médicament en pharmacie
doxycycline 300 mg daily
tretinoin 20 mg capsule
Viagra gГ©nГ©rique pas cher livraison rapide: viagra en ligne – Viagra homme prix en pharmacie sans ordonnance
ciprofloxacin india
where can you buy acyclovir
retin a price
ciprofloxacin 750 tablet
Le gГ©nГ©rique de Viagra: Quand une femme prend du Viagra homme – Viagra pas cher livraison rapide france
pharmacie en ligne pas cher: Cialis sans ordonnance 24h – pharmacie en ligne france pas cher
cost of generic advair
advair uk
Achat mГ©dicament en ligne fiable: kamagra en ligne – Pharmacie sans ordonnance
cheapest propecia for sale
tretinoin 0.1 cream online
Prix du Viagra 100mg en France: viagra en ligne – Viagra sans ordonnance pharmacie France
how to get zithromax over the counter
cialis professional
lyrica 75 mg price in canada
pharmacie en ligne sans ordonnance: achat kamagra – Achat mГ©dicament en ligne fiable
online pharmacy vermox
pharmacie en ligne france pas cher: kamagra oral jelly – pharmacie en ligne france livraison internationale
pharmacie en ligne france livraison internationale: levitra generique sites surs – pharmacies en ligne certifiГ©es
azithromycin 260 mg
buy tretinoin 0.1
ciprofloxacin in mexico
п»їpharmacie en ligne france: kamagra gel – pharmacies en ligne certifiГ©es
where to purchase diflucan
nolvadex generic
lasix cheap online
where can you buy nolvadex
dexamethasone 4 mg tabs
lyrica online prescription
Viagra pas cher livraison rapide france: Acheter du Viagra sans ordonnance – Viagra homme prix en pharmacie sans ordonnance
accutane canadian pharmacy
zithromax buy
how much is lyrica in canada
acheter mГ©dicament en ligne sans ordonnance: pharmacie en ligne pas cher – pharmacie en ligne fiable
buy provigil online with paypal
generic finasteride nz
Achat mГ©dicament en ligne fiable: acheter mГ©dicament en ligne sans ordonnance – vente de mГ©dicament en ligne
Achat mГ©dicament en ligne fiable: kamagra pas cher – vente de mГ©dicament en ligne
pharmacie en ligne livraison europe: п»їpharmacie en ligne france – pharmacie en ligne france livraison internationale
pharmacie en ligne france pas cher: levitra generique – acheter mГ©dicament en ligne sans ordonnance
pharmacie en ligne france fiable: kamagra 100mg prix – pharmacie en ligne fiable
trouver un mГ©dicament en pharmacie: Acheter Cialis 20 mg pas cher – vente de mГ©dicament en ligne
trouver un mГ©dicament en pharmacie: Levitra pharmacie en ligne – pharmacie en ligne fiable
Viagra pas cher livraison rapide france: viagra en ligne – Viagra femme sans ordonnance 24h
Pharmacie en ligne livraison Europe: kamagra pas cher – acheter mГ©dicament en ligne sans ordonnance
п»їpharmacie en ligne france: levitra generique prix en pharmacie – Pharmacie en ligne livraison Europe
dexamethasone cost usa
pharmacie en ligne france livraison belgique: achat kamagra – pharmacie en ligne avec ordonnance
diflucan 1 pill
finasteride for women
accutane canada cost
buy albuterol pills
noroxin tablets
furosemide 50 mg daily
where to get diflucan over the counter
buy provigil online cheap
flomax blood pressure
canada pharmacy vermox
pharmacie en ligne fiable http://kamagraenligne.com/# pharmacie en ligne
trouver un mГ©dicament en pharmacie: pharmacie en ligne sans ordonnance – pharmacie en ligne sans ordonnance
accutane usa
provigil online pharmacy uk
can i order metformin online
flomax 0.5 mg
combivent.com
zovirax price nz
advair 250/50
modafinil usa
lyrica 500 mg
doxycycline 100mg price south africa
https://azithromycinca.shop/# doxycycline 7.5 mg
buy doxycycline 100mg
how to get amoxicillin over the counter: amoxicillin – buying amoxicillin online
amoxicillin 500 mg tablet price
can i purchase viagra
cipro medicine price
Pin Up: pin-up360 – pin-up360
https://autolux-azerbaijan.com/# Pin Up Azerbaycan ?Onlayn Kazino
pin-up360: Pin Up Kazino ?Onlayn – Pin-up Giris
https://autolux-azerbaijan.com/# Pin Up Azerbaycan ?Onlayn Kazino
https://autolux-azerbaijan.com/# pin-up360
Pin Up Azerbaycan ?Onlayn Kazino: pin-up360 – ?Onlayn Kazino
https://autolux-azerbaijan.com/# pin-up360
Pin-Up Casino: Pin up 306 casino – Pin Up Azerbaycan
https://autolux-azerbaijan.com/# Pin-up Giris
?Onlayn Kazino: pin-up360 – pin-up kazino
https://autolux-azerbaijan.com/# Pin up 306 casino
pin-up 141 casino: pin-up360 – pin-up kazino
https://autolux-azerbaijan.com/# Pin-Up Casino
?Onlayn Kazino: Pin Up – Pin Up
Pin up 306 casino: Pin-up Giris – Pin Up Kazino ?Onlayn
https://autolux-azerbaijan.com/# pin-up360
Pin-up Giris: Pin up 306 casino – ?Onlayn Kazino
https://autolux-azerbaijan.com/# pin-up kazino
cost of 500 mg amoxicillin
where to get real nolvadex
doxycycline 100 mg forsale outside the us
clomid drug cost
acyclovir pills cost
how to get baclofen
buy lasix 100mg
furosemide 40mg cost
nolvadex 20mg tabs
buy 10 clomid pills
retin a price in india
bactrim 875 mg
how to buy zovirax
modafinil tablets online
Hungry for another free spins offer? Click the link above to get 50 free spins on Aloha King Elvis with no first deposit needed if you use the exclusive bonus code ACEBONUS. Most bonuses offered by online casinos – including those that do not require a real money deposit – come with certain rules that must be followed during bonus play, as well as limitations that apply to it. These are specified by the casino in the Terms and Conditions (T&Cs) that apply to bonuses. About 39% of Australians gamble while a considerable percentage of Canadians and the UK population are involved in online casino games. Online free slots are popular, so the gambling commissions regulate game providers’ activities and online casinos to provide licensed games. Online pokies are legal in Canada and Australia. Canada has up to 10 provinces and three territories for legal play. In Australia, different regions and provinces have bodies and commissions regulating demo and casino games.
http://users.atw.hu/nlw/profile.php?mode=viewprofile&u=18111
A no deposit bonus is probably the best way to start at the casino. Why? Cause you don’t have to risk your own money to play games – instead, online casino will reward you with free spins or bonus money upon successful registration so you can try out games for free. For example, any of NZ Casino you can find on this page will reward newcomers with such no deposit bonus, and it means that you can just open an account, then verify your details and receive bonus to your balance right after! A no deposit bonus code provides players in the USA with free bonus credit upon registering with the casino. This bonus credit can be used on various slots and occasionally other casino games as well. Societal casinos are ideal for players maybe not based in one of the newest active courtroom online casino states. Out of harbors to live broker blackjack, you can gamble yet games to the social casinos you to you could potentially on the judge online casinos. There are even comparable bonuses, in addition to no deposit bonuses and you will totally free revolves.
tretinoin cream in india price
viagra 3
where to get zithromax
amoxicillin z pack
can you buy amoxicillin otc
baclofen pills 10 mg
zovirax cream canada
generic effexor price
doxycycline antimalarial
augmentin otc