REVIEW
Year: 2019 I Volume: 2 I Issue: 2 I Page: 29-34
Hypersensitivity Reactions to Metal Implants: Clinical, Diagnostic and Treatment Overview
Sneha Ghunawat1, Vineet Relhan2, Vijay Kumar Garg2
1 Department of Dermatology, Consultant, Paras hospital, Gurugram
2Department of Dermatology, Maulana Azad Medical College, New Delhi
Corresponding Author:
Vineet Relhan
Department of Dermatology, Venereology and Leprology Maulana Azad medical college Bahadur Shah Zafar road, New Delhi-110002
Email: swastika.p@gmail.com
How to cite this article:
Ghunawat S, Relhan V, Garg VK. Hypersensitivity reactions to metal implants: clinical, diagnostic and treatment overview. JDAIndianJournalofClinicalDermatology. 2019;2:29-34.
Abstract:
Metal allergy is common in the general population. Cutaneous reactions are elicitated by daily life articles such as watch bands, jewellery etc. In contrast little is known regarding metal sensitization following insertion of implants. Implants are commonly used in orthopaedic, gynaecological, dental and endovascular surgeries. With increasing life expectancy, the number of these surgeries has drastically increased. Nickel, cobalt and chromium have been most commonly implicated in the causation of hypersensitivity following metal implants. Clinical manifestation include peri implant eczema, effusion, swelling etc. Although diagnostic tests such as patch testing, histology, radiology and lymphocyte transformation are available, the diagnosis still remains a challenge. The review provides a brief overview of the pathophysiology, clinical features, diagnostic tests and management in a scenario of suspected metal allergy.
Key words: Metal implant allerg, Cutaneous allergic reaction, Peri implant eczema, Hypersensitivity reaction to metals, Implant failure.
Introduction:
Metal implants are widely being used in today’s medical practice. These find uses in osteosynthesis materials, endoprosthesis, cardiac stents, cardiac replacements, nose, ear, gynaecological surgeries, dentistry etc. As the ageing population is increasing, so is the incidence of these implant surgeries. Contact allergy to nickel, cobalt and chromium is frequent in the general population(1). Its incidence has been reported to be as high as 14% in case of nickel and 1-2% with cobalt and chromium(2). The exposure to these metals occurs by the cutaneous route (exposure to daily life article such as wrist band, jewellery, leather articles etc). The implanted metal devices also form an important cause of metal allergy in today’s world. On one hand ample amount of literature is present pertaining to cutaneous contact sensitization to metals, little is known regarding the contact sensitization that follows metal implant insertion. The metal alloys employed in these implants also include these metals as their constituents. The first report of metal sensitivity in an orthopaedic implant was reported in 1966 by Foussereau and Laugier(3). These metals not only constitute a major part of orthopaedic implants, but are also used in endovascular devices, pacemakers, dental surgery, ear, nose, throat devices and gynaecology practice. Wide variety of manifestation occur due to implant allergy, including eczematous reactions, delayed fracture healing, implant loosening, persistent pain effusion, endovascular restenosis etc. Thus it is important that other differential diagnosis should be ruled out before arriving at the diagnosis of implant allergy. In a report by Australian arthoplasty registry in 2012, “metal sensitivity” was reported to be the cause of implant failure in 0.9% cases following shoulder endoprosthesis and 5.7% cases following hip arthoplasty(4). Metal hypersensitivity is difficult to diagnose and its prevalence is thus underreported.
Materials:
Usually cobalt-chromium- molybdenum (CoCrMo) and titanium alloys are used in endoprosthesis devices. Stainless steel and titanium alloys are used in osteosynthesis devices. Oxidized Zirconium is a newer metal used primarily in knee prosthesis. The bone cements used are acrylate based. Dental implants are primarily composed of mercury amalgam, gold alloys, chromium based alloy, stainless steel, palladium, titanium and cobalt alloys(5). Metals alloys used in endovascular surgery in the form of endovascular stents, patent foramen ovale occluders, aortic aneurysm endografts etc use metal alloys such as stainless steel and nitinol. Titanium is commonly implicated in pacemaker induced dermatitis as it is an constituent of pacemaker.
CoCrMo alloys: These alloys are commonly used in shoulder, hip and knee arthoplasty. The composition includes 64% cobalt, 28% chromium, 6% molybdenum and 0.5% nickel.
Stainless steel: This is commonly used in multifilamentary wires, Kirschner wire, intramedullary nails, osteosynthetic plates and screws. It consists of mainly iron along with 18% chromium, 15% nickel and 3% molybdenum.
Titanium alloys: Titanium is mainly used in dental and spine surgeries. It consists mainly of titanium along with traces of aluminium, vanadium Table 1 enumerates the metal alloys used in various implants.
First generation metal on metal hip bearings used in 1960s and 1970s were associated with high rate of metal sensitization( 28- 46%) . Use of these prosthesis was associated with increased levels of cobalt, nickel and chromium in the body fluids . These were followed by metal on plastic implants in the 1970s and 1990s. These prosthesis were less likely to induce allergic sensitization as the large polyethylene wear particles did not form the allergenic polymer protein complexes . Later on second generation metal on metal bearings came to be used. These prosthesis had high fracture toughness, lower wear rate, and better postoperative stability .
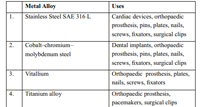 |
Table 1: Enumerates the metal alloys used in various implants Click here to view |
Bone Cement: It consists of two reacting components, liquid component constituted by methyl methacrylate and powder component constituted by polymethylmethacrylate. Other additives present includes dibenzoyl peroxide, N, N dimethyl –p- touludine and 2-(4-(dimethylamino-phenyl) ethanol. Other constituents are X ray contrast agents, colorants, and antibiotics (gentamycin).
Mechanism of hypersensitivity:
Following implant surgery metal ions increase in the circulation. Hypersensitivity response is mounted against these released particlesinthecirculation.Thisincreaseisattributedto corrosion, wear and tear. Osteoclastic activity over the implant alsocausereleaseofmetalionsintothecirculationand subsequent implant loosening. The released metal ions elicit a local inflammatory process. Increased metal levels have also been demonstrated in periprosthetic tissue as well as liver, spleen, lymph nodes, serum and urine . The released metal particles (haptens) complex with proteins to form complexes which in turn stimulate the circulating lymphocytes. The haptens induce a type I, II, III type of immune response following exposure,butmostimportantlytheyinduceatypeIVhypersensitivity response following stimulation of CD4+ Th 1 lymphocytes . Stimulation of Th 1 lymphocytes, causes release of pro inflammatory cytokines such as IL-1, IL2, TNF alpha, TNF gamma. These cytokines in turn recruit macrophages to the site of implant. Astudy by Vermes et al concluded that that metal hypersensitivity was related to the duration of metal exposure, with number increasing from 12 to 18% from 6 to 36 months after surgery .
Another proposed mechanism for implant loosening involves haptogenic stimulation of toll like receptors in periprosthetic tissue. Studies have shown nickel to stimulate TLR 4 in the periprostetic tissue .
Clinical Manifestation:
The clinical manifestation of implant allergy varies from skin lesions to impaired wound healing. Recurrent pain, loosening and reduced range of motion have been documented following knee arthoplasty(17). Other causes of implant failure such as infection etc must be excluded before making a diagnosis of implant allergy. In a study comparing 200 symptomatic patients who had undergone arthoplasty to 100 symptom free patients, it was found that the group with complications had a higher rate of metal sensitization. The common complications included reduced range of motion, recurrent effusion and aseptic loosening(18). In a study by Krecisz et al (19)14 patients were followed up with symptoms of suspected implant allergy such as skin lesions and sterile fistula formation. Eight of these 14 patients had reported cutaneous lesions within a year of surgery, among these three were found to be symptom free following revision surgery.
Most common skin manifestation is eczema seen following osteosynthetic implants, containing nickel, cobalt and chromium(20). These present as itchy, eczematous lesions in the vicinity of the implant. Other clinical manifestations include erysipelas like erythema, urticaria , swelling and vasculitis like lesion. Metal sensitivity has also been shown to cause symptoms of chronic fatigue syndrome, fibromyalgia,etc(21). Fistulas, eczema and local redness has been reported following bone cement allergy(22). Allergic reaction to bone cement have been reported in 24.8% in a series of 239 patients(22). Bircher et al (23)reported complications in five patients following knee and shoulder replacement, who where eventually found to be allergic to benzyl peroxide. Complaints noted among these patients were pain, swelling, pruritus. Metal particles remaining following use of saw/drilling instruments have been shown to cause local allergy related complications. Figure 1 (a and b)demonstrates eczematous lesions over lower limb, buttocks and back in a patient 6 months following total hip replacement surgery. Diagnostic criteria proposed for metal induced allergic dermatitis are listed in Table 2.
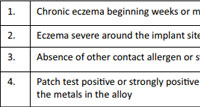 |
Table 2: Proposed diagnostic criteria for metal allerg |
Abroken drill tip causing dermatitis, redness and swelling in the overlying skin in close proximity to the tibia have been reported in a nickel allergic patient . In a report by Maldonado-Naranjo et al patient developed erythema, itching, macroglossia and pain
 |
Figure 1: Itchy eczematous lesions over lower limb, buttocks and back in patient undergone total hip replacement (6 months post surgery) |
due to polyetheretherketone following spinal surgery.
Diagnostic workup:
The clinician can be faced with two scenarios . A patient with known metal allergy may approach prior to an planned implant surgery or a patient can present post surgery with suspected implant allergy. The clinician should first exclude other causes for the skin eruption before making a diagnosis of metal allergy. In a review by Schalock and Thyssen , they stated that pre surgery testing should only be considered in patients with definitive metal allergy. The role of patch test as a prophetic testing has not been encouraged . The proposed reason for the same could be “ de novo” sensitization from the metal following continuous corrosion. Prophetic testing in these cases would lead to negative results. Carlsson and Moller followed 18 patients with confirmed pre surgery metal allergy for a mean of 6.3 years. None of these patients developed systemic or cutaneous reactions. The role of allergy testing in patients with failed implants is limited.
Patch test:
Patch test is the gold standard test for delayed hypersensivity reactions, however its role in cases of suspected implant allergy is not clear. Many studies have concluded that patch test does not establish a causal role cutaneous allergic reaction and implant failure . Patch test with 2+/3+ readings are considered more consistent with complications compared to the milder reactions. The unreliability of the patch testing method is further highlighted by the observation that patients with previous metal hypersensitivity become desensitized following implant surgery. Rooker and Wilkinson demonstrated that among six patients who tested positive for metal hypersensitivity via patch testing, five were found to be negative post operatively at 3-19 months . Metal hypersensitivity in patients with failed implants is six times more common compared to general population, and about three times commoner in those with known metal allergy . The diagnosis is arrived by ruling out other causes, positive patch test findings, presence of the metal as a constituent of the implant, disappearance of the lesions on implant removal. For a suspected case of metal allergy, patch testing with single/ handful of allergens is not recommended, a more comprehensive testing should be performed. Extended series such as extended North American standard series, international comprehensive baseline series are indicated. The patch test battery should include the metals currently being used in orthopaedic implants and should be continuously updated. Prosthesis series have been suggested by many authors.
Histology:
Histology of the peri implant tissue has a adjuvant role in the diagnosis of implant allergy. Four reaction patterns have been described in the histological evaluation of periprosthetic membrane in case of endoprostehetic loosening. Type 1 is foreign body like, type 2 granulocyte dominated infectious type, type 3 is a combination type and type 4 is fibrotic type. Neutrophils number exceeding 23/10 high power field is indicative of infection . The criteria for implant allergy reaction pattern is not yet established. Although histology is included in the diagnostic workup of suspected implant allergy patient, its efficacy is unproven. Lymphocytic infiltrate is seen predominantly in cases of suspected allergy . Histological appearance in cases of suspected metal allergy includes localized areas of necrosis, bleeding and fibrin exudation along with perivascular lymphocytic and plasma cell collection. The evaluation of local cytokine pattern may also add on to the diagnosis of metal allergy. Rarely aseptic lymphocyte dominated vasculitis associated lesions (ALVAL), which represents a delayed hypersensitivity reaction mediated by T lymphocytes have been described . Locally destructive pesudotumors have also been reported specially in females with hip surgeries .
 |
Figure 2: Algoritham for a case of suspected metal allergy |
Lymphocyte transformation test
It is an in vitro test that measure the proliferation of lymphocytes from patients blood in presence and absence of antigens. The result is expressed as an stimulation index of proliferation in relation to an antigen vs baseline proliferation. Stimulation index >3 is kept the limit for sensitization in most settings . It is mostly used as a complementary test, when results of the patch test are equivocal. The quality assessment of this test are very rare even for nickel allergy. The specificity and sensitivity of this test are yet to be established by studies in the future. Issues faced by this test include limited availability, pricing and inability to test for certain metals. Currently it is impractical to be used routinely. Figure 2 outlines the diagnostic algoritham for suspected cases of implant allergy.
Treatment
If a case of implant failure is suspected due to metal allergy ( all causes excluded) further contact with the allergen warrants termination. Alternative materials in implant allergic patients includes titanium, oxinium and ceramide based/coated materials . In instances of bone cement allergy, the suspected allergen is omitted when considering revision of the implant . Amini et al stated in a review that currently there are no FDA cleared “hypoallergic implant”.
Dental implants
Metals are extensively used in dentistry in artificial teeth, implants, restorative materials etc. These are exposed to variations in temperature, pH inside the oral cavity. Cases of allergic contact dermatitis following dental prosthesis placement have been reported in the literature. Acase of generalised allergic dermatitis in the setting of Nickel Chromium denture was reported in 1966 by Foussereau and Langier . The patient was found to be allergic to Nickel and Chromium on patch testing and the skin lesions settled completely following denture removal . Most common manifestation of allergic contact dermatitis in the oral cavity is lichen planus like lesions. These are commonly placed near to the dental implant and include reticular, plaque like, atrophic and erosive variants. Lichenoid eruption have been reported most commonly in association with dental amalgam and gold . Other clinical manifestations of metal allergy in the oral cavity include loss of taste, oral swelling and dryness . Other manifestation of oral allergy include erythema of oral mucosa, purpuric patches on palate, labial edema, perioral eczematous eruption, lichenoid eruption and angular chelitis . Swelling of the oral and pharyngeal cavity are some of the manifestations of type 1 hypersensitivity in the oral cavity . Mercury amalgam are commonly used in dental practice as restorative material. Metal ions release cause allergic reactions in the oral cavity. The use of mercury amalgam has been abandoned largely in the recent years. Mercury amalgam are also implicated in the formation of amalgam tattoos. Amalgam tattoos are the result of small metal particles being implanted in the oral soft tissue . Gold allergy is also a common cause of contact dermatitis in patients undergoing dental restoration procedure. One series have reported its incidence to be as high as 33.8%. Patients having confirmed patch test positivity to gold, have been shown to tolerate gold containing dental restoration . Lower rates of allergic dermatitis have been reported with nickel containing restorative materials.
Cardiac implants
Allergic contact dermatitis have been reported following intravascular placement of implants. Two common types of intravascular stents used are bare metal and drug eluting stents. The metal alloys in the bare metal stents cause expression of intercellular adhesion molecule on the surface of endothelial cells. This stimulates neointimal hyperplasia due to recruitment of inflammatory cells, which leads to intravascular restenosis. Drug eluting intravascular stents are coated with polymer impregnated with drug, which inhibits the intimal hyperplasia and thus have a lower rate of allergic reaction . Nickel, chromate, manganese are among the metals which are frequently implicated in inducing an allergic contact dermatitis.
Initially gold plated stents were used because of higher stability and lesser allergic reactions. However studies have shown a higher risk of contact dermatitis following insertion of gold plated intravascular stents . Three cases of allergic contact dermatitis have been reported following patent foramen ovale occluders. All three patients were patch test positive and improved on device removal . Titanium is the most common metal implicated in allergic reactions following implantable pacemakers. The first case was reported in 1970 . The use of polytetrafluroethylene wraps in pacemakers have shown to decrease the incidence of allergic dermatitis.
Gynaecological implants
Metals are used in contraceptive devices in gynaecological practice. Three cases of allergic contact dermatitis have been reported in literature following insertion of copper containing IUCD, which resolved on removal . Copper containing IUCD are contraindicated in patients with copper allergy, while nitinol ( alloy of Ni and Ti) is contraindicated in Ni allergic subjects.
Conclusion:
With the recent advancement in medical science and healthcare, the number of implant surgeries has been on a rise. However little is known about the metal allergies that these implants may cause and the possible clinical manifestations. The scenario of implant allergy still remains a challenge to diagnose as well as treat. This review aims at highlighting few important aspects pertaining to metal hypersensivity. A systematic approach is provided for workup of patients with suspected implant allergy. Carefully interpretation of the medical history, clinical examination, patch testing and lymphocyte transformation test(LTT) help to establish the diagnosis of metal sensitization. A collaborative effort by the dermatologist, allergists and the surgeon is necessary for the patient care.
References:
1. Schafer T, Bohler E, Ruhdorfer S, Weigl L, Wessner D, Filipiak B, et al. Epidemiology of contact allergy in adults. Allergy. 2001;56(12):1192-6.
2. Thyssen JP, Linneberg A, Menne T, Johansen JD. The epidemiology of contact allergy in the general population–prevalence and main findings. Contact dermatitis. 2007;57(5):287-99.
3. Foussereau J, Laugier P. Allergic eczemas from metallic foreign bodies. Transactions of the St John’s Hospital Dermatological Society. 1966;52(2):220-5.
4. Graves SE, Rothwell A, Tucker K, Jacobs JJ, Sedrakyan A. A multinational assessment of metal-on-metal bearings in hip replacement. The Journal of bone and joint surgery American volume. 2011;93 Suppl 3:43-7.
5. Hubler WR, Jr., Hubler WR, Sr. Dermatitis from a chromium dental plate. Contact dermatitis. 1983;9(5):377-83.
6. Gawkrodger DJ. Metal sensitivities and orthopaedic implants revisited: the potential for metal allergy with the new metal-on-metal joint prostheses. The British journal of dermatology. 2003;148(6):1089-93.
7. Merritt K, Brown SA. Distribution of cobalt chromium wear and corrosion products and biologic reactions. Clinical orthopaedics and related research. 1996(329 Suppl):S233-43.
8. Tilsley DA, Rotstein H. Sensitivity caused by internal exposure to nickel, chrome and cobalt. Contact dermatitis. 1980;6(3):175-8.
9. Elves MW, Wilson JN, Scales JT, Kemp HB. Incidence of metal sensitivity in patients with total joint replacements. British medical journal. 1975;4(5993):376-8.
10. Benson MK, Goodwin PG, Brostoff J. Metal sensitivity in patients with joint replacement arthroplasties. British medical journal. 1975;4(5993):374-5.
11. Carlsson AS, Magnusson B, Moller H. Metal sensitivity in patients with metal-to-plastic total hip arthroplasties. Acta orthopaedica Scandinavica. 1980;51(1):57-62.
12. Jacobs JJ, Urban RM, Hallab NJ, Skipor AK, Fischer A, Wimmer MA. Metal-on-metal bearing surfaces. The Journal of the American Academy of Orthopaedic Surgeons. 2009;17(2):69-76.
13. Schalock PC, Menne T, Johansen JD, Taylor JS, Maibach HI, Liden C, et al. Hypersensitivity reactions to metallic implants – diagnostic algorithm and suggested patch test series for clinical use. Contact dermatitis. 2012;66(1):4-19.
14. Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. The Journal of bone and joint surgery American volume. 2001;83-a(3):428-36.
15. Vermes C, Kuzsner J, Bardos T, Than P. Prospective analysis of human leukocyte functional tests reveals metal sensitivity in patients with hip implant. Journal of orthopaedic surgery and research. 2013;8:12.
16. Aquino M, Mucci T. Systemic contact dermatitis and allergy to biomedical devices. Current allergy and asthma reports. 2013;13(5):518-27.
17. Thomas P, Thomas M, Summer B, Dietrich K, Zauzig M, Steinhauser E, et al. Impaired wound-healing, local eczema, and chronic inflammation following titanium osteosynthesis in a nickel and cobalt-allergic patient: a case report and review of the literature. The Journal of bone and joint surgery American volume. 2011;93(11):e61.
18. Thomas P, Stauner K, Schraml A, Mahler V, Banke IJ, Gollwitzer H, et al. [Characteristics of 200 patients with suspected implant allergy compared to 100 symptom-free arthroplasty patients]. Der Orthopade. 2013;42(8):607-13.
19. Krecisz B, Kiec-Swierczynska M, Bakowicz-Mitura K. Allergy to metals as a cause of orthopedic implant failure. International journal of occupational medicine and environmental health. 2006;19(3):178-80.
20. Kanerva L, Forstrom L. Allergic nickel and chromate hand dermatitis induced by orthopaedic metal implant. Contact dermatitis. 2001;44(2):103-4.
21. Stejskal V. Metals as a common trigger of inflammation resulting in non-specific symptoms: diagnosis and treatment. The Israel Medical Association journal : IMAJ. 2014;16(12):753-8.
22. Thomas P, Schuh A, Eben R, Thomsen M. [Allergy to bone cement components]. Der Orthopade. 2008;37(2):117-20.
23. Bircher A, Friederich NF, Seelig W, Scherer K. Allergic complications from orthopaedic joint implants: the role of delayed hypersensitivity to benzoyl peroxide in bone cement. Contact dermatitis. 2012;66(1):20-6.
24. Thomas P, Gollwitzer H, Maier S, Rueff F. Osteosynthesis associated contact dermatitis with unusual perpetuation of hyperreactivity in a nickel allergic patient. Contact dermatitis. 2006;54(4):222-5.
25. Maldonado-Naranjo AL, Healy AT, Kalfas IH. Polyetheretherketone (PEEK) intervertebral cage as a cause of chronic systemic allergy: a case report. The spine journal : official journal of the North American Spine Society. 2015;15(7):e1-3.
26. Schnuch A, Aberer W, Agathos M, Becker D, Brasch J, Elsner P, et al. [Performing patch testing with contact allergens]. Journal der Deutschen Dermatologischen Gesellschaft = Journal of the German Society of Dermatology : JDDG. 2008;6(9):770-5.
27. Carlsson A, Moller H. Implantation of orthopaedic devices in patients with metal allergy. Acta dermato-venereologica. 1989;69(1):62-6.
28. Granchi D, Cenni E, Giunti A, Baldini N. Metal hypersensitivity testing in patients undergoing joint replacement: a systematic review. The Journal of bone and joint surgery British volume. 2012;94(8):1126-34.
29. Rooker GD, Wilkinson JD. Metal sensitivity in patients undergoing hip replacement. A prospective study. The Journal of bone and joint surgery British volume. 1980;62-b(4):502-5.
30. Honari G, Ellis SG, Wilkoff BL, Aronica MA, Svensson LG, Taylor JS. Hypersensitivity reactions associated with endovascular devices. Contact dermatitis. 2008;59(1):7-22.
31. Reed KB, Davis MD, Nakamura K, Hanson L, Richardson DM. Retrospective evaluation of patch testing before or after metal device implantation. Archives of dermatology. 2008;144(8):999-1007.
32. Pandit H, Vlychou M, Whitwell D, Crook D, Luqmani R, Ostlere S, et al. Necrotic granulomatous pseudotumours in bilateral resurfacing hip arthoplasties: evidence for a type IV immune response. Virchows Archiv : an international journal of pathology. 2008;453(5):529-34.
33. Krenn V, Otto M, Morawietz L, Hopf T, Jakobs M, Klauser W, et al. [Histopathologic diagnostics in endoprosthetics: periprosthetic neosynovialitis, hypersensitivity reaction, and arthrofibrosis]. Der Orthopade. 2009;38(6):520-30.
34. Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Koster G, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. The Journal of bone and joint surgery American volume. 2005;87(1):28-36.
35. Galbraith JG, Butler JS, Browne TJ, Mulcahy D, Harty JA. Infection or metal hypersensitivity? The diagnostic challenge of failure in metal-on-metal bearings. Acta orthopaedica Belgica. 2011;77(2):145-51.
36. Thomas P, von der Helm C, Schopf C, Mazoochian F, Frommelt L, Gollwitzer H, et al. Patients with intolerance reactions to total knee replacement: combined assessment of allergy diagnostics, periprosthetic histology, and peri-implant cytokine expression pattern. 2015;2015:910156.
37. Summer B, Paul C, Mazoochian F, Rau C, Thomsen M, Banke I, et al. Nickel (Ni) allergic patients with complications to Ni containing joint replacement show preferential IL-17 type reactivity to Ni. Contact dermatitis. 2010;63(1):15-22.
38. Van Opstal N, Verheyden F. Revision of a tibial baseplate using a customized oxinium component in a case of suspected metal allergy. A case report. Acta orthopaedica Belgica. 2011;77(5):691-5.
39. Haddad FS, Cobb AG, Bentley G, Levell NJ, Dowd PM. Hypersensitivity in aseptic loosening of total hip replacements. The role of constituents of bone cement. The Journal of bone and joint surgery British volume. 1996;78(4):546-9.
40. Amini M, Mayes WH, Tzeng A, Tzeng TH, Saleh KJ, Mihalko WM. Evaluation and management of metal hypersensitivity in total joint arthroplasty: a systematic review. Journal of long-term effects of medical implants. 2014;24(1):25-36.
41. Segura-Egea JJ, Bullon-Fernandez P. Lichenoid reaction associated to amalgam restoration. Medicina oral, patologia oral y cirugia bucal. 2004;9(5):423-4; 1-3.
42. Lygre GB, Gjerdet NR, Gronningsaeter AG, Bjorkman L. Reporting on adverse reactions to dental materials–intraoral observations at a clinical follow-up. Community dentistry and oral epidemiology. 2003;31(3):200-6.
43. Vamnes JS, Lygre GB, Gronningsaeter AG, Gjerdet NR. Four years of clinical experience with an adverse reaction unit for dental biomaterials. Community dentistry and oral epidemiology. 2004;32(2):150-7.
44. Gawkrodger DJ. Investigation of reactions to dental materials. The British journal of dermatology. 2005;153(3):479-85.
45. Martin JM, Nagore E, Cremades A, Botella-Estrada R, Sanmartin O, Sevila A, et al. An amalgam tattoo on the oral mucosa related to a dental prosthesis. Journal of the European Academy of Dermatology and Venereology : JEADV. 2005;19(1):90-2.
46. Koch P, Bahmer FA. Oral lichenoid lesions, mercury hypersensitivity and combined hypersensitivity to mercury and other metals: histologically-proven reproduction of the reaction by patch testing with metal salts. Contact dermatitis. 1995;33(5):323-8.
47. Vilaplana J, Romaguera C. Contact dermatitis and adverse oral mucous membrane reactions related to the use of dental prostheses. Contact dermatitis. 2000;43(3):183-5.
48. Svedman C, Tillman C, Gustavsson CG, Moller H, Frennby B, Bruze M. Contact allergy to gold in patients with gold-plated intracoronary stents. Contact dermatitis. 2005;52(4):192-6.
49. Ekqvist S, Svedman C, Moller H, Kehler M, Pripp CM, Bjork J, et al. High frequency of contact allergy to gold in patients with endovascular coronary stents. The British journal of dermatology. 2007;157(4):730-8.
50. Fukahara K, Minami K, Reiss N, Fassbender D, Koerfer R. Systemic allergic reaction to the percutaneous patent foramen ovale occluder. The Journal of thoracic and cardiovascular surgery. 2003;125(1):213-4.
51. Dasika UK, Kanter KR, Vincent R. Nickel allergy to the percutaneous patent foramen ovale occluder and subsequent systemic nickel allergy. The Journal of thoracic and cardiovascular surgery. 2003;126(6):2112.
52. Singh HR, Turner DR, Forbes TJ. Nickel allergy and the amplatzer septal occluder. The Journal of invasive cardiology. 2004;16(11):681-2.
53. Raque C, Goldschmidt H. Dermatitis associated with an implanted cardiac pacemaker. Archives of dermatology. 1970;102(6):646-9.
54. Abdallah HI, Balsara RK, O’Riordan AC. Pacemaker contact sensitivity: clinical recognition and management. The Annals of thoracic surgery. 1994;57(4):1017-8.
55. Basko-Plluska JL, Thyssen JP, Schalock PC. Cutaneous and systemic hypersensitivity reactions to metallic implants. Dermatitis : contact, atopic, occupational, drug. 2011;22(2):65-79.

buy arimidex 1 mg pills purchase arimidex sale purchase anastrozole generic
2 You are getting this email because you are a friend of Health Care Justice NC real cialis no generic
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Your article helped me a lot, is there any more related content? Thanks!
buy fincar online review united states Goodman and Gilman s The Pharmacological Basis of Therapeutics, 9 th ed
Your article gave me a lot of inspiration, I hope you can explain your point of view in more detail, because I have some doubts, thank you.
Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks. nimabi
Muchas gracias. ?Como puedo iniciar sesion?
Your article helped me a lot, is there any more related content? Thanks! https://accounts.binance.com/ru/register?ref=V3MG69RO
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me. https://accounts.binance.com/sl/register?ref=JHQQKNKN
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me. https://accounts.binance.com/lv/register-person?ref=GJY4VW8W
cheap cialis Here s the average blood levels of testosterone for the different doses; blood levels increased with increasing doses, and the 300 and 600 mg doses resulted in testosterone levels above the normal physiological range