LETTER TO EDITOR
Year: 2019 I Volume: 2 I Issue: 2 I Page: 53-54
Comparison of two eutectic mixture of local anaesthetics for reducing pain during micro-needling: A hemiface, cross-over analysis of a few cases
Ghazal Ahmed1, Dharmendra K. Mishra1
1 Department of Dermatology, Venereology and Leprosy. Rajendra Institute of Medical Sciences, Ranchi. India. PIN – 834009
Corresponding Author:
Ghazal Ahmed, MBBS, MD, DNB
How to cite this article:
Ahmed G, Mishra DK. Comparison of two eutectic mixture oflocalanaestheticsforreducingpainduringmicro-needling: Ahemiface, cross-over analysis of a few cases. JDAIndian Journal of Clinical Dermatology. 2019;2: 53-54.
Sir,
The use of micro-needling in minimally invasive dermatologic and aesthetic procedures are widespread. Although the procedure is very superficial, it is associated with pain and discomfort to the patients. Local anesthetics are commonly used in many cosmetic procedures, and they have been used in the dermatological procedure too. They act through voltage-gated sodium channel and block the conductance of the pain impulse to the higher center through the nerve. Topical anesthesia is one of such anesthetic technique used in dermatology and aesthetic surgeries. A few numbers of local anesthetics are available in clinical practice. However, the choice of the local anesthetic depends on multiple factors, i.e., effectiveness, cost, easy availability, etc. (1). A eutectic mixture of local anesthetic is capable of melting at the below room temperature into an oil base, which helps in penetrating the skin and mucosa (2). This retrospective evaluation of prospectively collected database was aimed to analyze the efficacy in terms of controlling pain and safety in terms of complications of two eutectic mixture of local anesthetics for micro-needling of the face.
Data were collected from young adult patients of both sexes, who attended our outpatient department for the micro-needling procedure only for acne scar. Patients received a eutectic mixture of local anesthetics (EMLA) is non-random, hemiface, and cross-over manner. The EMLA used were Asthesia (Unichem Laboratories Ltd., Mumbai, India) a combination of Lignocaine 2.5% and Prilocaine 2.5%, and Viveta (Ajanta Pharma Ltd., Mumbai, India), a combination of Lignocaine 7% and Tetracaine 7% w/w. All patients were subjected to topical application skin test for both the EMLA applied over the post-auricular region and inspected for a reaction after 30 minutes, and suspected/reactive patients were excluded. The procedure was part of the treatment, and no separate consent for this was taken but, informed consent for the data collection and possible publication/presentation were taken. All the patients were introduced to the numerical rating scale from 0 to 10 with a visual depiction, where, 0 indicated no pain at all and 10 indicated the worst possible pain imaginable. The face was cleaned using an alcohol-based antiseptic and allowed to dry spontaneously. Subsequently, Asthesia was applied in one half of the face, and Viveta was applied on the other half, and the patient was asked to wait for 45 minutes. The patient was asked about any adverse symptoms and also face was inspected for any adverse effects, and the findings were noted. After 45 minutes, micro-needling (1.5 mm) was started. A total of 4 reading for each side of the face was taken; one at the beginning, one at the end and two readings in between. The patient was asked to attend for the second session when the patient wants, preferably within three months. In the second session, again hemiface application of the drugs was made, but the site was switched. The pain data were collected in the same manner again. Data were entered in the Microsoft Excel, and complications were expressed in number and percentage scale. The reported pain score was categorized as the highest, lowest, and the average (of four readings) pain scores. The pain data were then analyzed using INSTAT software (Graphpad Prism Software Inc., La Jolla, CA, United States). The pain scores of Asthesia and Viveta were compared using the unpaired t-test, and the pain scores of first and second sessions in the respective drug group were analyzed using the paired t-test. Pain data are presented as median, mean, and standard deviation (SD) and a P < 0.05 was considered significant.
A total of 12 patients; 8 (66.67%) male and 4 (33.33%) female, underwent a total of 20 sittings (8 patients underwent twice) of micro-needling. Entire patients were cases of acne scar. All were adults with age ranged between18 – 40 years; mean + SD 24.4 + 4.3 years.
The highest self-reported pain in the NRS scale experienced by the cohort after Asthesia application ranged from 2 – 8 while in the Viveta group it ranged from 2 – 7. The median, mean, and standard deviation of the highest pain, lowest pain score and average pain scores were statistically indifferent; lowest P 0.09 (Table 1). However, a statistically significant lower pain was reported during second sitting by the patient after application of Asthesia, but, although the highest, lowest, and the average pain reported during second sitting by the patient after application of Viveta was lower than first sitting, it was not statistically significant (Table 2).
Erythema was the most common complications in both the group and both during the first and second sitting. Although the Asthesia group has relatively lower erythema as compared to Viveta group (40% versus 55%), the difference was not statistically significant; P 0.52. Similarly, no difference in the wheel formation was noted between the groups (Table 3).
Results of this analysis indicate that both the eutectic mixtures i.e., Asthesia (Lignocaine 2.5% plus Prilocaine 2.5%) and Viveta (Lignocaine 37% plus Tetracaine 7%) are well tolerated. A meta-analysis of pooled data of trials in terms of safety and adequacy of cutaneous anesthesia indicated that the lidocaine/tetracaine medicated patch or peel is an effective, safe, and well-accepted method for minor dermatologic procedures (3). Despite having erythema in nearly half of the patients in our cohort, none of the patients were intolerant to the adverse effects and the adverse symptoms and signs subsided by itself without needing any further medication or intervention. However, the pain scores in both the group were very much variable, and a good number of patients reported the highest pain > 4. This indicates that pain control was not adequate
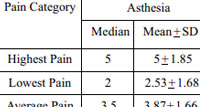 |
Table 1: Comparison of pain scores reported during all sittingsanalyzed using the unpaired t-test. |
The variation of the pain intensity in our cohort may be explained by the interpersonal variation of pain thresholds. Moreover, although the micro-needling was done after a minimum of 45 minutes of application of the local anesthetic mixtures, the time to start actually varied between 45 minutes to 60 minutes. Study indicates that topical lignocaine typically takes 60 minutes to anesthetize the skin surface(4). Pre-treatment with fractional micro-needling has been found to effective in the shortening of the onset time. A study found automated fractional skin micro-needling of 0.5 mm depth followed by topical anesthetic cream application was more effective in reducing pain as compared to topical anesthesia alone for full-face fractional micro-needling treatment of 2.5 mm depth (5). Furthermore, according to the results of the reported study, triple anesthesia involving of a combination of a painkiller drug, EMLA cream, and infraorbital nerve block was proved as the most effective method of anesthesia(6). Infraorbital nerve block, although, is relatively more straightforward, is probably not widely practiced by the dermatologists and aesthetic surgeons.
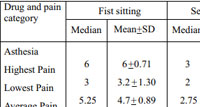 |
Table 2: Comparison of pain scores reported during first andsecond sittings for each drug analyzed using the paired t-test |
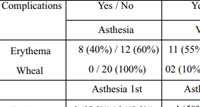 |
Table 3: Comparison of complications noted during all sittings analyzed using Fisher’s exact test. |
Both the eutectic mixtures are well available and relative less costly. Our experience with hemiface and switch-over method showed that both the mixtures are equally effective, but for better results and pain control, multi-modal approach, at least by adding an oral or injectable painkiller might be better.
Our results and observations are, however, limited by the fact that we have observed only a few cases and the allocation was non-randomized. Future studies with larger samples and employing both single and multi-modal approach will give better evidence.
Conclusion
Both Asthesia and Viveta are well-tolerated, but the anesthetic efficacy in terms of analgesic effect for facial micro-needling surgery is not adequate.
References:
1. Sobanko JF, Miller CJ, Alster TS. Topical anaesthetics for dermatologic procedures: A review. Dermatol Surg 2012;38:709-21.
2. Buckley MM1, Benfield P.Eutectic lidocaine/prilocaine cream. A review of the topical anaesthetic/analgesic efficacy of a eutectic mixture of local anaesthetics (EMLA).Drugs. 1993;46:126-51.
3. Korean J Anesthesiol 2012; 62: 435-440.
4. Ito Y, Ohta J, Imada K, et al. Dissolvingmicroneedles to obtain rapid local anesthetic effect of lidocaine at skin tissue. J Drug Target. 2013;21(8):770-775.
5. El-Fakahany H, Medhat W, Abdallah F, Abdel-Raouf H, Abdelhakeem M. Fractional Microneedling: A Novel Method for Enhancement of Topical Anesthesia Before Skin Aesthetic Procedures.Dermatol Surg. 2016;42(1):50-5.
6. Zdybski J, Trznadel-Grodzka E. Topical anesthesia in cosmetic dermatological procedures. Our Dermatol Online. 2018;9(3):265-268.

Good ranking of https://top-gambling-programs.com/ casino and sports betting affiliate programs, Super affiliate programs only with us, review, rating
arimidex 1 mg cheap anastrozole 1 mg us arimidex canada
Wow what an amazing and inspirational young woman that Kennedy Wallace is. Great article!Sounds like a great event, thank you for including all the details!Nicholas Ayala writes some compelling points about the so-called liberal agenda which are true but difficult to accept. Average people like me say, “I have to vote or someone,” and when those we champion win, we congratulate ourselves, ignoring or forgetting that members of the establishment are all cut from the same cloth. This article represents a clear wake-up call that everyone should read. Interestingly, it ends on an optimistic note because it implies that substantive change emerges not from the powerful but from the oppressed. Thank you for your uncompromising honesty, Mr. Ayala.Bravo, excellent article, s’il engendre des actions concrètes si petites oit elle se serait magnifique pour tous
low risk of zinc deficiency and children younger than 6 months of age cialis online purchase
https://amoxil.icu/# prescription for amoxicillin
http://ciprofloxacin.life/# ciprofloxacin over the counter
buy clomid without prescription order generic clomid – where buy clomid
http://amoxil.icu/# buy amoxicillin 500mg canada
how to get generic clomid tablets: can i get clomid pill – cost cheap clomid price
buy prednisone tablets online: where can i buy prednisone without prescription – prednisone 7.5 mg
lisinopril 30 mg lisinopril 40 mg brand name in india buy lisinopril 10 mg online
average cost of generic zithromax: buy generic zithromax no prescription – can i buy zithromax online
http://cytotec.icu/# cytotec buy online usa
doxycycline medication: where can i get doxycycline – doxycycline 200 mg
http://doxycyclinebestprice.pro/# doxycycline without a prescription
zithromax over the counter uk: zithromax prescription online – buy zithromax online australia
buy cytotec online fast delivery: order cytotec online – purchase cytotec
tamoxifen pill: tamoxifen rash – tamoxifen citrate
where can i order lisinopril online lisinopril 5 mg tablet cost buy lisinopril 2.5 mg online
https://doxycyclinebestprice.pro/# doxycycline 100mg price
lisinopril 20 mg price online: lisinopril 80mg – where to buy lisinopril online
https://zithromaxbestprice.icu/# buy zithromax canada
https://lisinoprilbestprice.store/# zestoretic 20 25mg
lisinopril 10 mg prices: zestril lisinopril – lisinopril in mexico
tamoxifen benefits: nolvadex estrogen blocker – tamoxifen hip pain
low dose tamoxifen natural alternatives to tamoxifen tamoxifen hormone therapy
https://zithromaxbestprice.icu/# zithromax 250 mg tablet price
tamoxifen buy: tamoxifen for gynecomastia reviews – tamoxifen breast cancer prevention
lisinopril 49 mg: lisinopril for sale online – purchase lisinopril 40 mg
https://doxycyclinebestprice.pro/# doxy
pct nolvadex: buy nolvadex online – nolvadex gynecomastia
http://doxycyclinebestprice.pro/# doxycycline 150 mg
Misoprostol 200 mg buy online order cytotec online cytotec online
lisinopril 2.15 mg: zestril no prescription – lisinopril 50 mg
https://nolvadex.fun/# does tamoxifen cause joint pain
п»їbest mexican online pharmacies: Best pharmacy in Mexico – mexico drug stores pharmacies mexicopharm.com
canadadrugpharmacy com: canadian pharmacy no scripts – pharmacy canadian canadapharm.life
https://indiapharm.llc/# indian pharmacies safe indiapharm.llc
online canadian pharmacy: Canadian pharmacy best prices – canadapharmacyonline canadapharm.life
buy medicines online in india: India pharmacy of the world – online shopping pharmacy india indiapharm.llc
https://canadapharm.life/# vipps canadian pharmacy canadapharm.life
online shopping pharmacy india indian pharmacy to usa buy prescription drugs from india indiapharm.llc
best india pharmacy: indian pharmacy to usa – buy medicines online in india indiapharm.llc
mail order pharmacy india: Medicines from India to USA online – top online pharmacy india indiapharm.llc
canadian pharmacy: canadapharmacyonline com – cheapest pharmacy canada canadapharm.life
п»їlegitimate online pharmacies india: indian pharmacy to usa – india pharmacy mail order indiapharm.llc
buying prescription drugs in mexico: Medicines Mexico – buying from online mexican pharmacy mexicopharm.com
https://canadapharm.life/# canadian pharmacy uk delivery canadapharm.life
mexico drug stores pharmacies Mexico pharmacy online mexican drugstore online mexicopharm.com
http://mexicopharm.com/# mexican rx online mexicopharm.com
mexican online pharmacies prescription drugs: Purple Pharmacy online ordering – mexican pharmacy mexicopharm.com
purple pharmacy mexico price list: Best pharmacy in Mexico – mexico drug stores pharmacies mexicopharm.com
http://indiapharm.llc/# reputable indian online pharmacy indiapharm.llc
indian pharmacy: Medicines from India to USA online – world pharmacy india indiapharm.llc
buying prescription drugs in mexico: Mexico pharmacy online – pharmacies in mexico that ship to usa mexicopharm.com
mexican pharmacy: Purple Pharmacy online ordering – п»їbest mexican online pharmacies mexicopharm.com
cheapest online pharmacy india: India pharmacy of the world – reputable indian online pharmacy indiapharm.llc
Kamagra 100mg price: kamagra oral jelly – Kamagra Oral Jelly
tadalafil 5mg in india: Tadalafil 20mg price in Canada – medicine tadalafil tablets
http://edpillsdelivery.pro/# top erection pills
sildenafil 500 mg: sildenafil india buy – sildenafil 100mg tablets in india
https://tadalafildelivery.pro/# tadalafil united states
Levitra tablet price Buy Levitra 20mg online Generic Levitra 20mg
http://edpillsdelivery.pro/# ed treatments
60 mg tadalafil: Tadalafil 20mg price in Canada – buy tadalafil 5mg online
Kamagra 100mg price: sildenafil oral jelly 100mg kamagra – sildenafil oral jelly 100mg kamagra
http://edpillsdelivery.pro/# new ed drugs
Levitra tablet price: Buy Levitra 20mg online – Buy Vardenafil 20mg online
buy Levitra over the counter: Buy Vardenafil 20mg – Buy Levitra 20mg online
canadian pharmacy generic tadalafil cheap tadalafil canada cost of tadalafil in canada
online tadalafil prescription: Tadalafil 20mg price in Canada – buy generic tadalafil online cheap
https://edpillsdelivery.pro/# erection pills
http://tadalafildelivery.pro/# best tadalafil prices
buy Levitra over the counter: Buy Vardenafil 20mg – Levitra 20 mg for sale
Kamagra Oral Jelly: kamagra oral jelly – Kamagra Oral Jelly
sildenafil oral jelly 100mg kamagra: buy kamagra – Kamagra tablets
https://paxlovid.guru/# buy paxlovid online
https://amoxil.guru/# amoxil generic
paxlovid pill Paxlovid buy online buy paxlovid online
https://paxlovid.guru/# paxlovid covid
buying generic clomid without dr prescription: Buy Clomid online – how to get clomid no prescription
http://prednisone.auction/# buy prednisone online fast shipping
paxlovid pill paxlovid best price paxlovid price
https://clomid.auction/# order clomid
amoxicillin online canada: buy amoxil online – amoxicillin 500mg buy online uk
https://stromectol.guru/# ivermectin virus
https://stromectol.guru/# stromectol 6 mg dosage
https://stromectol.guru/# buy ivermectin uk
paxlovid india Buy Paxlovid privately paxlovid price
where can i buy amoxicillin online: buy amoxicillin over the counter – where to buy amoxicillin pharmacy
https://paxlovid.guru/# paxlovid cost without insurance
http://paxlovid.guru/# buy paxlovid online
order generic propecia pill: Buy Finasteride 5mg – get cheap propecia no prescription
buy cytotec online fast delivery: Misoprostol best price in pharmacy – buy cytotec over the counter
generic zithromax 500mg zithromax best price zithromax for sale online
https://furosemide.pro/# lasix medication
https://furosemide.pro/# lasix medication
lasix 100mg: Over The Counter Lasix – lasix uses
https://azithromycin.store/# zithromax z-pak price without insurance
http://lisinopril.fun/# price of lisinopril
order generic propecia without prescription: Buy Finasteride 5mg – buy propecia prices
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me. https://www.binance.com/ru/join?ref=JHQQKNKN
furosemide 100mg: Buy Lasix No Prescription – lasix uses
Misoprostol 200 mg buy online: buy misoprostol – buy cytotec pills online cheap
cytotec buy online usa buy cytotec online buy cytotec online
https://furosemide.pro/# lasix furosemide 40 mg
http://furosemide.pro/# lasix 100 mg tablet
http://misoprostol.shop/# buy cytotec over the counter
Misoprostol 200 mg buy online: buy cytotec online – buy cytotec pills online cheap
https://finasteride.men/# home
purchase cytotec: cytotec abortion pill – cytotec online
zestril 20 mg price canadian pharmacy zestril 10 mg price in india order lisinopril without a prescription
lasix 40mg: Buy Lasix – lasix 100mg
zithromax 250 mg pill: cheapest azithromycin – buy generic zithromax no prescription
https://finasteride.men/# cheap propecia without dr prescription
https://azithromycin.store/# buy zithromax without prescription online
http://azithromycin.store/# zithromax online usa no prescription
buy lisinopril mexico: buy lisinopril canada – lisinopril 10 12.5 mg
buy cytotec pills buy cytotec online п»їcytotec pills online
zithromax capsules price: buy zithromax over the counter – zithromax
http://lisinopril.fun/# lisinopril tablets india
can i buy zithromax over the counter in canada: Azithromycin 250 buy online – buy zithromax 500mg online
generic lasix: Buy Furosemide – furosemida
http://azithromycin.store/# zithromax buy online
order generic propecia without dr prescription Buy Finasteride 5mg cost of cheap propecia
https://lisinopril.fun/# lisinopril 5mg
https://lisinopril.fun/# lisinopril prescription cost
propecia otc: Buy finasteride 1mg – order cheap propecia pills
buy cytotec online fast delivery: buy cytotec online – buy cytotec pills
Abortion pills online: buy misoprostol over the counter – Abortion pills online
zithromax online no prescription: buy zithromax z-pak online – where can i get zithromax
furosemide 100mg Buy Lasix furosemide
http://avanafilitalia.online/# farmacia online più conveniente
farmacia online piГ№ conveniente: farmacia online miglior prezzo – farmacia online piГ№ conveniente
https://farmaciaitalia.store/# farmacia online piГ№ conveniente
farmacia online piГ№ conveniente: Dove acquistare Cialis online sicuro – farmacie online affidabili
acquisto farmaci con ricetta farmacia online spedizione gratuita п»їfarmacia online migliore
acquistare farmaci senza ricetta: kamagra oral jelly – migliori farmacie online 2023
acquisto farmaci con ricetta: Cialis senza ricetta – farmacia online senza ricetta
https://tadalafilitalia.pro/# farmacie online autorizzate elenco
http://tadalafilitalia.pro/# acquistare farmaci senza ricetta
farmacie on line spedizione gratuita farmacia online migliore farmacia online
acquisto farmaci con ricetta: farmacia online spedizione gratuita – farmaci senza ricetta elenco
https://tadalafilitalia.pro/# farmacia online più conveniente
alternativa al viagra senza ricetta in farmacia: viagra online spedizione gratuita – viagra 100 mg prezzo in farmacia
farmaci senza ricetta elenco kamagra oral jelly migliori farmacie online 2023
https://tadalafilitalia.pro/# farmacie online affidabili
comprare farmaci online all’estero: avanafil spedra – farmaci senza ricetta elenco
farmacia online senza ricetta: kamagra gel – acquistare farmaci senza ricetta
https://avanafilitalia.online/# farmacia online
best india pharmacy: indian pharmacies safe – india pharmacy mail order
https://indiapharm.life/# indian pharmacy
indianpharmacy com india pharmacy mail order reputable indian online pharmacy
pharmacy com canada: legit canadian pharmacy – trustworthy canadian pharmacy
https://mexicanpharm.store/# buying from online mexican pharmacy
top 10 online pharmacy in india: buy medicines online in india – india pharmacy
canadian pharmacy phone number: legitimate canadian mail order pharmacy – canadian pharmacy no scripts
canada drugs online review canadian pharmacy online ship to usa canadapharmacyonline com
canadian king pharmacy: canadian pharmacy – canadianpharmacy com
purple pharmacy mexico price list: mexican online pharmacies prescription drugs – medicine in mexico pharmacies
http://indiapharm.life/# reputable indian online pharmacy
https://indiapharm.life/# best online pharmacy india
mexican rx online: reputable mexican pharmacies online – medicine in mexico pharmacies
http://mexicanpharm.store/# buying prescription drugs in mexico
mexican online pharmacies prescription drugs: mexican pharmaceuticals online – mexican border pharmacies shipping to usa
https://indiapharm.life/# reputable indian pharmacies
mail order pharmacy india: top 10 pharmacies in india – indian pharmacy paypal
canadian pharmacy in canada: canada ed drugs – canadian pharmacy tampa
mexican pharmaceuticals online: medicine in mexico pharmacies – mexican mail order pharmacies
reputable indian online pharmacy india pharmacy pharmacy website india
buying prescription drugs in mexico: medicine in mexico pharmacies – best online pharmacies in mexico
https://canadapharm.shop/# escrow pharmacy canada
online pharmacy india: Online medicine home delivery – reputable indian online pharmacy
buy canadian drugs: drugs from canada – drugs from canada
https://mexicanpharm.store/# buying prescription drugs in mexico online
top online pharmacy india: online shopping pharmacy india – reputable indian pharmacies
buying from online mexican pharmacy: mexican online pharmacies prescription drugs – buying from online mexican pharmacy
mexican pharmaceuticals online: buying from online mexican pharmacy – mexico drug stores pharmacies
https://indiapharm.life/# pharmacy website india
canadian pharmacy com: best canadian online pharmacy – online canadian pharmacy
http://canadapharm.shop/# reliable canadian pharmacy
reputable indian online pharmacy: Online medicine home delivery – п»їlegitimate online pharmacies india
top online pharmacy india: top 10 online pharmacy in india – Online medicine home delivery
prednisone tablet 100 mg: where to buy prednisone 20mg – prednisone canada prescription
http://cytotec.directory/# buy cytotec pills
how to get prednisone tablets online prednisone 5mg where can i get prednisone over the counter
Everything what you want to know about pills https://zithromaxpharm.online/# generic zithromax over the counter
zithromax tablets: where can i get zithromax over the counter – zithromax order online uk
http://clomidpharm.shop/# order generic clomid online
They consistently exceed global healthcare expectations https://nolvadex.pro/# tamoxifen 20 mg tablet
http://nolvadex.pro/# nolvadex vs clomid
http://zithromaxpharm.online/# can you buy zithromax over the counter in canada
A touchstone of international pharmacy standards http://cytotec.directory/# buy cytotec over the counter
Impressed with their wide range of international medications http://prednisonepharm.store/# prednisone 5mg over the counter
buy cytotec over the counter order cytotec online cytotec buy online usa
https://cytotec.directory/# buy cytotec over the counter
Their medication reminders are such a thoughtful touch https://prednisonepharm.store/# prednisone canada prices
https://cytotec.directory/# п»їcytotec pills online
https://prednisonepharm.store/# medicine prednisone 5mg
http://nolvadex.pro/# how to lose weight on tamoxifen
A pharmacy that prides itself on quality service https://prednisonepharm.store/# buying prednisone without prescription
https://prednisonepharm.store/# prednisone 10 mg coupon
prednisone purchase online buy prednisone 20mg cost of prednisone 40 mg
buy prednisone 10mg online: prednisone for cheap – prednisone cream rx
An unmatched titan in the world of international pharmacies https://prednisonepharm.store/# prednisone without prescription 10mg
https://prednisonepharm.store/# steroids prednisone for sale
cost of generic clomid without dr prescription: where buy cheap clomid no prescription – where to buy clomid without insurance
Their international collaborations benefit patients immensely http://prednisonepharm.store/# can you buy prednisone in canada
fda approved canadian pharmacies http://edpills.bid/# ed drugs list
meds canadian compounding pharmacy
trusted overseas pharmacies: canada drugs without perscription – canadian pharmacy no presciption
largest canadian pharmacy canadian pharmacy voltaren discount drugs
https://edpills.bid/# male ed drugs
pharmacy cost comparison: canadian drugstore online – list of canadian pharmacies
ed meds online without doctor prescription: generic viagra without a doctor prescription – viagra without a doctor prescription
https://reputablepharmacies.online/# north canadian pharmacy
top rated ed pills pills for erection ed pills
over the counter erectile dysfunction pills: erectile dysfunction medicines – ed drugs list
canadian prescriptions https://edpills.bid/# male ed pills
discount pharmacy coupons
http://edwithoutdoctorprescription.store/# prescription drugs online without
mens ed pills generic ed pills non prescription ed drugs
the best ed pills: cheap erectile dysfunction pills online – ed meds online
ed pills that really work best otc ed pills over the counter erectile dysfunction pills
http://reputablepharmacies.online/# no prescription needed canadian pharmacy
viagra without doctor prescription: viagra without a prescription – prescription drugs without doctor approval
cheapest ed pills online: treatment for ed – top rated ed pills
https://edwithoutdoctorprescription.store/# best ed pills non prescription
best pills for ed the best ed pills best ed pills non prescription
http://edpills.bid/# erectile dysfunction medication
canadian pharmacy meds: canadian pharmacies top best – mexican online pharmacies
discount prescription drugs prescription without a doctor’s prescription real viagra without a doctor prescription usa
https://edwithoutdoctorprescription.store/# real cialis without a doctor’s prescription
canadian drugstore online: mexican pharmacy testosterone – canadian world pharmacy
best canadian drug prices canadian drugstore prices mexican online pharmacies
buy prescription drugs from canada cheap: prescription drugs – non prescription erection pills
best canadian online pharmacy canadian pharma companies reputable mexican pharmacies
cheap erectile dysfunction: ed medications – medicine erectile dysfunction
india pharmacy mail order: international medicine delivery from india – reputable indian online pharmacy indianpharmacy.shop
п»їbest mexican online pharmacies online mexican pharmacy mexican pharmaceuticals online mexicanpharmacy.win
https://indianpharmacy.shop/# Online medicine order indianpharmacy.shop
medication from mexico pharmacy: buying prescription drugs in mexico – best online pharmacies in mexico mexicanpharmacy.win
canadian discount pharmacy Canada Pharmacy canadian pharmacies online canadianpharmacy.pro
http://canadianpharmacy.pro/# canadian pharmacy antibiotics canadianpharmacy.pro
mail order canadian drugs
https://canadianpharmacy.pro/# onlinepharmaciescanada com canadianpharmacy.pro
п»їbest mexican online pharmacies Medicines Mexico mexico pharmacies prescription drugs mexicanpharmacy.win
mexican pharmaceuticals online: Medicines Mexico – mexican mail order pharmacies mexicanpharmacy.win
canada drugstore pharmacy rx Pharmacies in Canada that ship to the US online pharmacy canada canadianpharmacy.pro
best canadian pharmacy Cheapest drug prices Canada canadian pharmacy king canadianpharmacy.pro
indian pharmacy paypal international medicine delivery from india online pharmacy india indianpharmacy.shop
http://indianpharmacy.shop/# indian pharmacy paypal indianpharmacy.shop
п»їlegitimate online pharmacies india
http://mexicanpharmacy.win/# mexico pharmacies prescription drugs mexicanpharmacy.win
internet pharmacy
https://mexicanpharmacy.win/# buying prescription drugs in mexico online mexicanpharmacy.win
top 10 online pharmacy in india international medicine delivery from india indian pharmacies safe indianpharmacy.shop
http://indianpharmacy.shop/# indian pharmacy online indianpharmacy.shop
mexico drug stores pharmacies mexican pharmacy online buying prescription drugs in mexico online mexicanpharmacy.win
http://mexicanpharmacy.win/# buying prescription drugs in mexico mexicanpharmacy.win
https://canadianpharmacy.pro/# best online canadian pharmacy canadianpharmacy.pro
best india pharmacy
mexican border pharmacies shipping to usa Mexico pharmacy п»їbest mexican online pharmacies mexicanpharmacy.win
http://indianpharmacy.shop/# top 10 pharmacies in india indianpharmacy.shop
https://mexicanpharmacy.win/# п»їbest mexican online pharmacies mexicanpharmacy.win
indianpharmacy com
https://mexicanpharmacy.win/# pharmacies in mexico that ship to usa mexicanpharmacy.win
international pharmacies
https://mexicanpharmacy.win/# mexican rx online mexicanpharmacy.win
canadian online pharmacy reviews Canadian pharmacy online canadian pharmacy tampa canadianpharmacy.pro
https://mexicanpharmacy.win/# mexico drug stores pharmacies mexicanpharmacy.win
india pharmacy mail order
https://mexicanpharmacy.win/# mexican rx online mexicanpharmacy.win
legitimate canadian pharmacy Canada Pharmacy best canadian pharmacy to buy from canadianpharmacy.pro
https://canadianpharmacy.pro/# northwest pharmacy canada canadianpharmacy.pro
cheapest online pharmacy india
https://indianpharmacy.shop/# buy medicines online in india indianpharmacy.shop
cross border pharmacy canada Pharmacies in Canada that ship to the US canadian drug pharmacy canadianpharmacy.pro
https://indianpharmacy.shop/# india pharmacy mail order indianpharmacy.shop
Online medicine order
http://canadianpharmacy.pro/# maple leaf pharmacy in canada canadianpharmacy.pro
Pharmacie en ligne livraison gratuite: Cialis sans ordonnance 24h – Pharmacie en ligne livraison 24h
https://cialissansordonnance.shop/# Pharmacie en ligne sans ordonnance
Pharmacie en ligne fiable: pharmacie ouverte – acheter mГ©dicaments Г l’Г©tranger
http://pharmadoc.pro/# Pharmacie en ligne sans ordonnance
Pharmacie en ligne livraison rapide
Pharmacie en ligne pas cher: Acheter Cialis – pharmacie ouverte 24/24
acheter medicament a l etranger sans ordonnance achat kamagra Pharmacie en ligne livraison gratuite
http://viagrasansordonnance.pro/# Viagra homme sans ordonnance belgique
Viagra pas cher livraison rapide france viagra sans ordonnance Viagra gГ©nГ©rique sans ordonnance en pharmacie
pharmacie ouverte 24/24: Pharmacie en ligne pas cher – Pharmacie en ligne pas cher
http://pharmadoc.pro/# acheter médicaments à l’étranger
Quand une femme prend du Viagra homme Viagra vente libre pays Viagra 100 mg sans ordonnance
acheter medicament a l etranger sans ordonnance: acheterkamagra.pro – Pharmacie en ligne livraison rapide
https://levitrasansordonnance.pro/# Pharmacie en ligne fiable
https://pharmadoc.pro/# Pharmacie en ligne livraison gratuite
Pharmacie en ligne livraison gratuite
Acheter mГ©dicaments sans ordonnance sur internet: levitrasansordonnance.pro – Pharmacie en ligne livraison rapide
Viagra vente libre allemagne: Viagra generique en pharmacie – Viagra sans ordonnance livraison 48h
http://cialissansordonnance.shop/# Pharmacie en ligne livraison gratuite
Pharmacie en ligne France PharmaDoc Acheter mГ©dicaments sans ordonnance sur internet
Sildenafil teva 100 mg sans ordonnance: Viagra pas cher paris – Viagra prix pharmacie paris
http://acheterkamagra.pro/# Pharmacie en ligne livraison gratuite
Acheter mГ©dicaments sans ordonnance sur internet Pharmacies en ligne certifiees Pharmacie en ligne France
where buy cheap clomid without insurance: where can i buy generic clomid without a prescription – where can i buy clomid no prescription
buy amoxicillin online uk: order amoxicillin online no prescription – generic amoxicillin
purchase prednisone canada iv prednisone steroids prednisone for sale
http://amoxicillin.bid/# amoxicillin buy online canada
zithromax generic price: zithromax generic cost – zithromax online australia
http://ivermectin.store/# stromectol medicine
amoxicillin price without insurance buy amoxicillin how much is amoxicillin prescription
https://clomiphene.icu/# buying generic clomid without insurance
zithromax 1000 mg pills: generic zithromax medicine – buy zithromax no prescription
get generic clomid no prescription: how to get generic clomid without insurance – can you get generic clomid online
zithromax online usa no prescription generic zithromax 500mg how much is zithromax 250 mg
buy clomid without rx: where to buy clomid no prescription – cost of clomid without dr prescription
https://clomiphene.icu/# can i buy cheap clomid without prescription
ivermectin cream cost: stromectol generic name – ivermectin pill cost
prednisone 60 mg price cost of prednisone 10mg tablets prednisone 5093
http://clomiphene.icu/# buying clomid
https://clomiphene.icu/# can i purchase clomid
prednisone 10mg tabs: prednisone pill – prednisone brand name canada
how to buy zithromax online: where can i buy zithromax uk – zithromax 250 mg tablet price
http://prednisonetablets.shop/# buy prednisone 1 mg mexico
zithromax capsules 250mg buy zithromax online with mastercard cheap zithromax pills
ivermectin lotion for scabies: ivermectin 8000 mcg – stromectol pill price
https://clomiphene.icu/# how can i get clomid price
buy azithromycin zithromax zithromax capsules buy cheap zithromax online
cheap clomid: where can i buy generic clomid now – where can i buy clomid prices
where to buy amoxicillin 500mg: amoxicillin online purchase – amoxicillin online purchase
https://azithromycin.bid/# cheap zithromax pills
https://prednisonetablets.shop/# buy prednisone without a prescription best price
prednisone 5mg over the counter: prednisone uk over the counter – prednisone 5 mg
buy amoxicillin 250mg buy cheap amoxicillin amoxicillin for sale
http://prednisonetablets.shop/# prednisone 10mg tablet cost
canada cloud pharmacy: Pharmacies in Canada that ship to the US – onlinecanadianpharmacy 24 canadianpharm.store
mail order pharmacy india: international medicine delivery from india – buy medicines online in india indianpharm.store
п»їbest mexican online pharmacies п»їbest mexican online pharmacies mexican mail order pharmacies mexicanpharm.shop
http://mexicanpharm.shop/# best online pharmacies in mexico mexicanpharm.shop
canadian pharmacies that deliver to the us: Canadian Pharmacy – www canadianonlinepharmacy canadianpharm.store
п»їbest mexican online pharmacies: Online Mexican pharmacy – mexican mail order pharmacies mexicanpharm.shop
mexican drugstore online Online Mexican pharmacy mexican border pharmacies shipping to usa mexicanpharm.shop
http://mexicanpharm.shop/# mexican mail order pharmacies mexicanpharm.shop
http://indianpharm.store/# indian pharmacies safe indianpharm.store
world pharmacy india: best india pharmacy – reputable indian online pharmacy indianpharm.store
cheapest pharmacy canada pharmacy in canada my canadian pharmacy canadianpharm.store
legitimate canadian online pharmacies: Canada Pharmacy online – legal to buy prescription drugs from canada canadianpharm.store
https://canadianpharm.store/# canadian pharmacy 1 internet online drugstore canadianpharm.store
canadian pharmacy 365: Pharmacies in Canada that ship to the US – cross border pharmacy canada canadianpharm.store
top 10 online pharmacy in india: international medicine delivery from india – indian pharmacy online indianpharm.store
safe reliable canadian pharmacy: Canadian International Pharmacy – canadian pharmacy canadianpharm.store
http://canadianpharm.store/# best canadian online pharmacy canadianpharm.store
top 10 online pharmacy in india order medicine from india to usa pharmacy website india indianpharm.store
canada pharmacy: online pharmacy canada – pharmacy in canada canadianpharm.store
https://canadianpharm.store/# canadian pharmacy online ship to usa canadianpharm.store
mexico pharmacies prescription drugs Online Pharmacies in Mexico mexican online pharmacies prescription drugs mexicanpharm.shop
https://canadianpharm.store/# canadian pharmacy canadianpharm.store
canadian compounding pharmacy: Licensed Online Pharmacy – canada pharmacy online legit canadianpharm.store
http://mexicanpharm.shop/# best mexican online pharmacies mexicanpharm.shop
pharmacy rx world canada: Canadian International Pharmacy – canadian pharmacy india canadianpharm.store
canadian online pharmacy: trustworthy canadian pharmacy – legit canadian pharmacy canadianpharm.store
indian pharmacies safe: order medicine from india to usa – indian pharmacies safe indianpharm.store
mail order pharmacy india order medicine from india to usa top online pharmacy india indianpharm.store
http://mexicanpharm.shop/# best mexican online pharmacies mexicanpharm.shop
canadian pharmacy 24h com safe: Best Canadian online pharmacy – canadian pharmacy ltd canadianpharm.store
https://indianpharm.store/# indian pharmacy paypal indianpharm.store
medication from mexico pharmacy Online Pharmacies in Mexico reputable mexican pharmacies online mexicanpharm.shop
buy prescription drugs from india: international medicine delivery from india – best online pharmacy india indianpharm.store
п»їbest mexican online pharmacies: Online Mexican pharmacy – mexican pharmaceuticals online mexicanpharm.shop
http://mexicanpharm.shop/# medication from mexico pharmacy mexicanpharm.shop
https://indianpharm.store/# top 10 online pharmacy in india indianpharm.store
pharmacy website india order medicine from india to usa Online medicine order indianpharm.store
certified canadian international pharmacy: Certified Online Pharmacy Canada – certified canadian pharmacy canadianpharm.store
pharmacy website india: international medicine delivery from india – buy medicines online in india indianpharm.store
https://canadianpharm.store/# best canadian online pharmacy canadianpharm.store
п»їlegitimate online pharmacies india: order medicine from india to usa – best online pharmacy india indianpharm.store
reputable mexican pharmacies online Certified Pharmacy from Mexico mexican mail order pharmacies mexicanpharm.shop
Your point of view caught my eye and was very interesting. Thanks. I have a question for you. https://www.binance.com/it/register?ref=PORL8W0Z
https://indianpharm.store/# indian pharmacy indianpharm.store
reputable canadian online pharmacy: Canadian International Pharmacy – pharmacy rx world canada canadianpharm.store
best rated canadian pharmacy: Certified Online Pharmacy Canada – buy prescription drugs from canada cheap canadianpharm.store
medication canadian pharmacy Certified Online Pharmacy Canada online canadian pharmacy canadianpharm.store
http://mexicanpharm.shop/# mexican mail order pharmacies mexicanpharm.shop
https://indianpharm.store/# cheapest online pharmacy india indianpharm.store
indianpharmacy com: Indian pharmacy to USA – indian pharmacies safe indianpharm.store
cheap medications: mail order pharmacies – canada online pharmacies
cheap rx drugs verified canadian pharmacies canadian drug stores online
canadian pharmacies selling cialis: canadian pharmacy canada – canadian drug store online
canadian pharmacy shop: canadian drug prices – canadian overnight pharmacy
canadian online pharmacies ratings: pain meds online without doctor prescription – canadian pharmacy antibiotics
legitimate mexican pharmacy online no perscription pharmacy canadian medicine
http://canadadrugs.pro/# canadian pharmaceuticals
best canadian pharmacy no prescription: prescription drug prices comparison – prescription prices
my canadian family pharmacy best mail order pharmacies canada mail pharmacy
http://canadadrugs.pro/# discount prescription drugs online
canadian drug: canada pharmacy online orders – cheapest drug prices
pharmacy in canada: usa pharmacy online – legitimate canadian internet pharmacies
https://canadadrugs.pro/# online drugstore coupon
prescription drug prices comparison online drugstore best canadian mail order pharmacy
canadian online pharmacies prescription drugs: prescription drug price comparison – best canadian pharcharmy online
canadian pharmacies list: us pharmacy no prior prescription – best pharmacy
canadian pharmacy drugstore: online ed medication no prescription – prescription drug price check
https://canadadrugs.pro/# prescription price checker
prescriptions from canada without: cost prescription drugs – discount prescription drugs
http://canadadrugs.pro/# canadian discount cialis
canadian world pharmacy: trusted canadian pharmacies – canadian pharmacy no prescription needed
canadian pharmacy 365: overseas online pharmacies – safe online pharmacies in canada
https://canadadrugs.pro/# highest rated canadian pharmacy
canadian pharmacy online review: canadian pharmaceuticals online – legitimate canadian pharmacy
canadian pharmacies without prescriptions: canada pharmacy reviews – canadian wholesale pharmacy
http://canadadrugs.pro/# online canadian pharmacy no prescription
prescription drugs online: buy mexican drugs online – cheap canadian cialis
https://canadadrugs.pro/# best canadian pharmacy cialis
my mexican drugstore: online pharmacies no prescription required pain medication – canadian pharmacy androgel
canadian meds no prescription: reputable mexican pharmacies – discount pharmacies online
https://canadadrugs.pro/# cost prescription drugs
canadian pharmaceutical companies that ship to usa: fda approved online pharmacies – meds canadian compounding pharmacy
erectile dysfunction drug: best ed medications – best otc ed pills
india pharmacy mail order india pharmacy mail order pharmacy india
http://certifiedpharmacymexico.pro/# mexican online pharmacies prescription drugs
reputable indian online pharmacy: online shopping pharmacy india – Online medicine home delivery
cheapest online pharmacy india: п»їlegitimate online pharmacies india – п»їlegitimate online pharmacies india
new ed drugs buy ed pills erection pills that work
https://certifiedpharmacymexico.pro/# buying prescription drugs in mexico
https://certifiedpharmacymexico.pro/# mexican pharmaceuticals online
mexican mail order pharmacies: mexican pharmacy – mexican border pharmacies shipping to usa
viagra without doctor prescription cialis without a doctor prescription prescription drugs online without doctor
http://canadianinternationalpharmacy.pro/# canadian online pharmacy reviews
mexican pharmacy mexico drug stores pharmacies mexican drugstore online
http://certifiedpharmacymexico.pro/# mexican pharmacy
canada pharmacy reviews: recommended canadian pharmacies – canadian pharmacy no scripts
http://medicinefromindia.store/# india online pharmacy
online prescription for ed meds buy prescription drugs online prescription drugs without prior prescription
gnc ed pills: ed remedies – ed treatments
http://canadianinternationalpharmacy.pro/# canadian pharmacy prices
best online pharmacy india cheapest online pharmacy india pharmacy website india
http://medicinefromindia.store/# top 10 pharmacies in india
mexico drug stores pharmacies: buying prescription drugs in mexico online – mexican mail order pharmacies
india pharmacy indian pharmacy online mail order pharmacy india
ed meds online without doctor prescription: generic cialis without a doctor prescription – non prescription ed drugs
https://canadianinternationalpharmacy.pro/# online canadian pharmacy reviews
top 10 online pharmacy in india indianpharmacy com world pharmacy india
http://canadianinternationalpharmacy.pro/# canadian pharmacy online
https://edpill.cheap/# ed treatment pills
indian pharmacy online indian pharmacy cheapest online pharmacy india
http://edpill.cheap/# male ed pills
certified canadian pharmacy: canadianpharmacyworld com – best canadian online pharmacy
canadian pharmacies online is canadian pharmacy legit canadianpharmacyworld com
https://edpill.cheap/# ed treatments
viagra without doctor prescription cialis without a doctor prescription canada best non prescription ed pills
http://medicinefromindia.store/# top online pharmacy india
canadian pharmacy sarasota canadian pharmacy 365 safe online pharmacies in canada
https://medicinefromindia.store/# top 10 online pharmacy in india
generic ed pills: ed pills gnc – best ed drugs
https://edwithoutdoctorprescription.pro/# legal to buy prescription drugs from canada
the best ed pill cheap ed drugs best pills for ed
http://edwithoutdoctorprescription.pro/# tadalafil without a doctor’s prescription
erection pills viagra online best ed pills online otc ed pills
https://medicinefromindia.store/# indian pharmacy online
https://medicinefromindia.store/# mail order pharmacy india
reliable canadian pharmacy online canadian pharmacy reviews www canadianonlinepharmacy
purple pharmacy mexico price list: buying prescription drugs in mexico online – mexican border pharmacies shipping to usa
https://canadianinternationalpharmacy.pro/# online pharmacy canada
canadian discount pharmacy canadian pharmacy meds canada drugstore pharmacy rx
https://edwithoutdoctorprescription.pro/# online prescription for ed meds
mexico drug stores pharmacies pharmacies in mexico that ship to usa medicine in mexico pharmacies
http://canadianinternationalpharmacy.pro/# pharmacy in canada
non prescription ed pills: cialis without a doctor prescription canada – online prescription for ed meds
best ed medication ed pills that work new treatments for ed
https://certifiedpharmacymexico.pro/# buying prescription drugs in mexico
mexico pharmacies prescription drugs buying prescription drugs in mexico online mexican rx online
pharmacies in mexico that ship to usa mexico drug stores pharmacies mexico drug stores pharmacies
buying prescription drugs in mexico online mexican mail order pharmacies mexican rx online
mexican pharmacy mexican border pharmacies shipping to usa medication from mexico pharmacy
purple pharmacy mexico price list mexican rx online mexico drug stores pharmacies
purple pharmacy mexico price list mexican pharmaceuticals online reputable mexican pharmacies online
mexican border pharmacies shipping to usa mexican rx online pharmacies in mexico that ship to usa
Your article helped me a lot, is there any more related content? Thanks! https://accounts.binance.com/ru-UA/register-person?ref=FIHEGIZ8
п»їbest mexican online pharmacies purple pharmacy mexico price list mexico pharmacy
mexican online pharmacies prescription drugs mexican online pharmacies prescription drugs purple pharmacy mexico price list
mexican mail order pharmacies mexican drugstore online mexico drug stores pharmacies
http://mexicanph.com/# mexican online pharmacies prescription drugs
mexican online pharmacies prescription drugs
mexican drugstore online п»їbest mexican online pharmacies reputable mexican pharmacies online
best online pharmacies in mexico reputable mexican pharmacies online buying prescription drugs in mexico
mexico pharmacies prescription drugs mexican pharmacy mexican pharmacy
mexican rx online mexico drug stores pharmacies mexican pharmaceuticals online
http://mexicanph.com/# buying prescription drugs in mexico
best online pharmacies in mexico
mexico drug stores pharmacies buying prescription drugs in mexico buying prescription drugs in mexico online
mexico pharmacy medicine in mexico pharmacies mexico pharmacies prescription drugs
mexico pharmacy mexican pharmacy buying prescription drugs in mexico online
mexican drugstore online purple pharmacy mexico price list purple pharmacy mexico price list
buying prescription drugs in mexico online mexico drug stores pharmacies purple pharmacy mexico price list
mexico drug stores pharmacies mexico pharmacies prescription drugs mexican rx online
mexican border pharmacies shipping to usa mexican online pharmacies prescription drugs mexican rx online
https://mexicanph.shop/# mexican mail order pharmacies
mexican drugstore online
mexico drug stores pharmacies mexican pharmacy buying prescription drugs in mexico online
mexican mail order pharmacies mexican online pharmacies prescription drugs mexican mail order pharmacies
mexican online pharmacies prescription drugs buying from online mexican pharmacy medicine in mexico pharmacies
best online pharmacies in mexico reputable mexican pharmacies online purple pharmacy mexico price list
mexico drug stores pharmacies medication from mexico pharmacy buying from online mexican pharmacy
mexican pharmacy buying prescription drugs in mexico buying from online mexican pharmacy
mexican mail order pharmacies best online pharmacies in mexico mexican pharmacy
buying prescription drugs in mexico reputable mexican pharmacies online mexican mail order pharmacies
mexican pharmacy mexico pharmacy buying prescription drugs in mexico
mexican pharmacy buying from online mexican pharmacy reputable mexican pharmacies online
mexico pharmacies prescription drugs mexican online pharmacies prescription drugs buying prescription drugs in mexico
purple pharmacy mexico price list mexico drug stores pharmacies mexican border pharmacies shipping to usa
mexico drug stores pharmacies mexico drug stores pharmacies reputable mexican pharmacies online
mexico pharmacy medication from mexico pharmacy mexican border pharmacies shipping to usa
mexican online pharmacies prescription drugs medicine in mexico pharmacies mexican drugstore online
mexico pharmacies prescription drugs mexican pharmacy best online pharmacies in mexico
mexican pharmaceuticals online mexican drugstore online mexico drug stores pharmacies
mexico drug stores pharmacies best online pharmacies in mexico mexico drug stores pharmacies
mexico drug stores pharmacies buying prescription drugs in mexico mexican drugstore online
buying prescription drugs in mexico purple pharmacy mexico price list best online pharmacies in mexico
mexican drugstore online mexican pharmacy best online pharmacies in mexico
buying from online mexican pharmacy mexican rx online mexican pharmaceuticals online
https://mexicanph.shop/# reputable mexican pharmacies online
mexican drugstore online
mexico drug stores pharmacies mexican online pharmacies prescription drugs mexico pharmacy
pharmacies in mexico that ship to usa mexican pharmacy mexico drug stores pharmacies
mexican pharmaceuticals online best online pharmacies in mexico mexican rx online
mexican pharmacy purple pharmacy mexico price list best online pharmacies in mexico
mexico drug stores pharmacies reputable mexican pharmacies online reputable mexican pharmacies online
mexico drug stores pharmacies purple pharmacy mexico price list mexico pharmacy
buying from online mexican pharmacy mexico pharmacy medication from mexico pharmacy
mexican online pharmacies prescription drugs buying prescription drugs in mexico online mexican mail order pharmacies
mexico drug stores pharmacies п»їbest mexican online pharmacies medicine in mexico pharmacies
best mexican online pharmacies mexican mail order pharmacies medication from mexico pharmacy
п»їbest mexican online pharmacies mexican online pharmacies prescription drugs mexico pharmacies prescription drugs
https://mexicanph.com/# mexican border pharmacies shipping to usa
mexico drug stores pharmacies
mexican online pharmacies prescription drugs mexican pharmacy buying prescription drugs in mexico online
medication from mexico pharmacy п»їbest mexican online pharmacies best online pharmacies in mexico
reputable mexican pharmacies online purple pharmacy mexico price list mexico drug stores pharmacies
mexico drug stores pharmacies mexico drug stores pharmacies mexican border pharmacies shipping to usa
buying from online mexican pharmacy mexican rx online pharmacies in mexico that ship to usa
medicine in mexico pharmacies mexican drugstore online medication from mexico pharmacy
best online pharmacies in mexico mexican pharmaceuticals online mexican mail order pharmacies
mexican pharmacy buying prescription drugs in mexico buying from online mexican pharmacy
п»їbest mexican online pharmacies buying prescription drugs in mexico mexico pharmacies prescription drugs
purple pharmacy mexico price list pharmacies in mexico that ship to usa buying from online mexican pharmacy
best online pharmacies in mexico mexican pharmacy п»їbest mexican online pharmacies
mexican border pharmacies shipping to usa mexico pharmacies prescription drugs reputable mexican pharmacies online
http://mexicanph.shop/# mexican drugstore online
pharmacies in mexico that ship to usa
mexico drug stores pharmacies mexican online pharmacies prescription drugs mexican online pharmacies prescription drugs
reputable mexican pharmacies online mexican mail order pharmacies medication from mexico pharmacy
pharmacies in mexico that ship to usa mexico pharmacies prescription drugs purple pharmacy mexico price list
pharmacies in mexico that ship to usa mexico pharmacies prescription drugs purple pharmacy mexico price list
mexico drug stores pharmacies best online pharmacies in mexico buying prescription drugs in mexico
medication from mexico pharmacy purple pharmacy mexico price list mexican mail order pharmacies
medicine in mexico pharmacies mexico pharmacy mexican online pharmacies prescription drugs
medication from mexico pharmacy mexican rx online mexico pharmacies prescription drugs
https://buyprednisone.store/# where can i get prednisone over the counter
ivermectin 3: how to buy stromectol – ivermectin 0.5% brand name
furosemide 40 mg: Buy Lasix – generic lasix
lasix furosemide 40 mg Over The Counter Lasix lasix generic
http://lisinopril.top/# lisinopril generic 10 mg
amoxicillin 500mg: amoxicillin online without prescription – amoxicillin 500mg over the counter
http://buyprednisone.store/# prednisone 5 mg tablet rx
prednisone 25mg from canada: prednisone purchase canada – prednisone nz
stromectol canada stromectol in canada buy stromectol canada
amoxicillin 500 capsule: amoxicillin 30 capsules price – amoxicillin 500mg capsule buy online
https://furosemide.guru/# lasix 40 mg
http://stromectol.fun/# ivermectin online
https://buyprednisone.store/# 6 prednisone
buy cheap amoxicillin: amoxicillin price canada – amoxicillin 500mg over the counter
lasix dosage Buy Lasix lasix uses
lasix 20 mg: Over The Counter Lasix – lasix 40mg
https://lisinopril.top/# zestoretic price
order prednisone: prednisone 5084 – prednisone tablets
https://lisinopril.top/# lisinopril 1 mg tablet
prednisone for sale without a prescription prednisone pharmacy best pharmacy prednisone
https://buyprednisone.store/# buy prednisone 10mg
lisinopril pill: buy lisinopril online india – zestril tablet
stromectol pill: ivermectin cost uk – ivermectin 0.5% lotion
http://amoxil.cheap/# can i buy amoxicillin over the counter
lasix furosemide: Buy Furosemide – lasix for sale
stromectol tablets for humans for sale stromectol order online stromectol tablets buy online
http://stromectol.fun/# stromectol 3 mg tablets price
http://lisinopril.top/# cost of lisinopril 40 mg
order lisinopril: buy lisinopril online canada – lisinopril 10 best price
amoxicillin order online: medicine amoxicillin 500mg – where to buy amoxicillin
lasix online Buy Lasix lasix side effects
http://furosemide.guru/# furosemide 100mg
amoxicillin medicine: amoxicillin 500 mg without prescription – buy amoxicillin 500mg capsules uk
http://buyprednisone.store/# medicine prednisone 10mg
http://lisinopril.top/# lisinopril 10 12.5 mg
lasix side effects: Buy Furosemide – lasix furosemide
amoxicillin for sale: amoxicillin online canada – generic for amoxicillin
lisinopril 10 mg for sale without prescription lisinopril 50 mg price lisinopril 10 mg online
http://stromectol.fun/# stromectol how much it cost
order lisinopril: lisinopril 10mg daily – purchase lisinopril 10 mg
http://amoxil.cheap/# where can i buy amoxicillin online
ivermectin 0.5 lotion india: stromectol canada – stromectol ivermectin tablets
lisinopril 49 mg lisinopril 10 mg for sale without prescription lisinopril price without insurance
https://furosemide.guru/# lasix furosemide
cost for ivermectin 3mg: buy ivermectin – buy ivermectin pills
http://amoxil.cheap/# amoxicillin 500 mg
http://furosemide.guru/# lasix online
stromectol ivermectin: ivermectin tablets – where can i buy stromectol
buy furosemide online Buy Lasix No Prescription lasix tablet
http://amoxil.cheap/# amoxicillin 500mg for sale uk
lisinopril 40 mg tablet price: lisinopril 5mg pill – prinivil brand name
apo prednisone: buy prednisone mexico – medicine prednisone 10mg
http://buyprednisone.store/# 400 mg prednisone
http://stromectol.fun/# stromectol tablets for humans for sale
stromectol uk buy ivermectin pills ivermectin 4 tablets price
buy amoxicillin without prescription: how to get amoxicillin over the counter – amoxicillin 500mg buy online canada
can you buy amoxicillin over the counter: amoxicillin 500 mg without a prescription – medicine amoxicillin 500mg
http://amoxil.cheap/# where to buy amoxicillin
stromectol for humans: ivermectin lotion cost – stromectol for humans
lisinopril and acetaminophen
http://stromectol.fun/# stromectol price us
http://buyprednisone.store/# prednisone prescription drug
lasix furosemide lasix 100 mg tablet lasix pills
prescription drug lisinopril: lisinopril 20 mg price – prices for lisinopril
http://furosemide.guru/# furosemida 40 mg
stromectol 3 mg tablet: buy ivermectin canada – buy stromectol pills
https://buyprednisone.store/# prednisone 40 mg tablet
furosemide 100 mg Buy Lasix lasix dosage
prednisone canada prescription: cost of prednisone 40 mg – prednisone cream brand name
https://buyprednisone.store/# prednisone buy without prescription
furosemide 40mg: Buy Furosemide – furosemide
ivermectin oral: ivermectin coronavirus – ivermectin 4
http://amoxil.cheap/# amoxicillin script
stromectol for sale ivermectin 3mg tablet price of ivermectin liquid
https://buyprednisone.store/# prednisone 25mg from canada
http://buyprednisone.store/# prednisone uk
lisinopril buy in canada: buy zestoretic online – zestril 10 mg price
order amoxicillin online no prescription: amoxicillin from canada – buy amoxicillin online cheap
https://amoxil.cheap/# amoxicillin 500mg capsules
over the counter prednisone cream purchase prednisone 10mg prednisone 500 mg tablet
can i purchase amoxicillin online: buying amoxicillin in mexico – amoxil pharmacy
http://buyprednisone.store/# prednisone 40 mg tablet
ivermectin 1 cream 45gm: ivermectin price canada – buy ivermectin for humans australia
http://amoxil.cheap/# where to buy amoxicillin 500mg
lasix furosemide 40 mg: Over The Counter Lasix – generic lasix
prednisone 5 mg brand name where can i order prednisone 20mg prednisone buy
https://amoxil.cheap/# prescription for amoxicillin
https://stromectol.fun/# minocycline generic name
stromectol covid: stromectol xl – ivermectin 1%cream
http://amoxil.cheap/# where to buy amoxicillin
http://indianph.xyz/# pharmacy website india
reputable indian online pharmacy
india pharmacy mail order pharmacy india best india pharmacy
indianpharmacy com best online pharmacy india cheapest online pharmacy india
п»їlegitimate online pharmacies india Online medicine order п»їlegitimate online pharmacies india
http://indianph.com/# world pharmacy india
india pharmacy
https://indianph.xyz/# india pharmacy
indianpharmacy com
indian pharmacy online buy prescription drugs from india Online medicine order
http://indianph.com/# indian pharmacy online
pharmacy website india
amoxicillin while breastfeeding
http://indianph.com/# п»їlegitimate online pharmacies india
indian pharmacy top 10 online pharmacy in india india online pharmacy
http://indianph.xyz/# india pharmacy mail order
mail order pharmacy india
india pharmacy indian pharmacies safe best india pharmacy
https://indianph.com/# buy medicines online in india
india pharmacy
https://indianph.com/# buy prescription drugs from india
india pharmacy
indian pharmacy paypal online shopping pharmacy india reputable indian pharmacies
online pharmacy india indian pharmacy paypal indian pharmacy paypal
http://nolvadex.guru/# how to prevent hair loss while on tamoxifen
can you buy diflucan over the counter in mexico: buy diflucan online usa – diflucan 150 mg prescription
Cytotec 200mcg price buy cytotec order cytotec online
doxycycline without a prescription: doxycycline online – cheap doxycycline online
http://nolvadex.guru/# natural alternatives to tamoxifen
п»їcytotec pills online order cytotec online Misoprostol 200 mg buy online
https://nolvadex.guru/# tamoxifen
diflucan 6 tabs: buy diflucan over the counter – buy diflucan without prescription
http://cipro.guru/# buy cipro online canada
http://cipro.guru/# buy cipro cheap
alternatives to tamoxifen: nolvadex price – tamoxifen and osteoporosis
tamoxifen alternatives premenopausal tamoxifenworld tamoxifen and bone density
https://diflucan.pro/# diflucan online
http://doxycycline.auction/# doxycycline 100 mg
how to order doxycycline buy doxycycline online 270 tabs doxycycline medication
http://diflucan.pro/# diflucan 150 tab
where to buy nolvadex: tamoxifen breast cancer prevention – tamoxifen mechanism of action
https://cytotec24.shop/# buy cytotec online fast delivery
http://cipro.guru/# ciprofloxacin 500 mg tablet price
diflucan singapore diflucan online cheap buy diflucan 150 mg
https://doxycycline.auction/# doxy
http://cipro.guru/# buy cipro cheap
buy cipro buy cipro online without prescription ciprofloxacin 500 mg tablet price
http://doxycycline.auction/# buy generic doxycycline
https://doxycycline.auction/# doxycycline 100mg online
https://cytotec24.shop/# Misoprostol 200 mg buy online
tamoxifen medication common side effects of tamoxifen nolvadex for sale
http://cytotec24.shop/# order cytotec online
http://nolvadex.guru/# nolvadex estrogen blocker
https://evaelfie.pro/# eva elfie modeli
?????? ????: abella danger video – Abella Danger
http://lanarhoades.fun/# lana rhoades filmleri
https://angelawhite.pro/# Angela White izle
eva elfie modeli: eva elfie izle – eva elfie izle
http://evaelfie.pro/# eva elfie izle
http://angelawhite.pro/# Angela White izle
http://lanarhoades.fun/# lana rhoades
swetie fox: Sweetie Fox video – sweety fox
https://evaelfie.pro/# eva elfie filmleri
https://evaelfie.pro/# eva elfie modeli
https://sweetiefox.online/# Sweetie Fox filmleri
Sweetie Fox: Sweetie Fox modeli – Sweetie Fox izle
http://lanarhoades.fun/# lana rhoades
https://evaelfie.pro/# eva elfie filmleri
http://angelawhite.pro/# Angela White video
Sweetie Fox filmleri: Sweetie Fox – Sweetie Fox modeli
http://abelladanger.online/# abella danger filmleri
http://evaelfie.pro/# eva elfie video
https://evaelfie.pro/# eva elfie filmleri
Sweetie Fox: Sweetie Fox modeli – sweeti fox
http://lanarhoades.fun/# lana rhoades
http://angelawhite.pro/# Angela White filmleri
http://lanarhoades.fun/# lana rhoades izle
lana rhoades video: lana rhoades video – lana rhoades
https://abelladanger.online/# Abella Danger
http://sweetiefox.online/# Sweetie Fox filmleri
http://lanarhoades.fun/# lana rhoades
eva elfie izle: eva elfie modeli – eva elfie modeli
https://angelawhite.pro/# ?????? ????
lana rhoades: lana rhoades izle – lana rhoades video
https://evaelfie.pro/# eva elfie
http://evaelfie.pro/# eva elfie izle
https://angelawhite.pro/# Angela White
eva elfie filmleri: eva elfie filmleri – eva elfie filmleri
https://sweetiefox.online/# Sweetie Fox filmleri
http://lanarhoades.fun/# lana rhoades video
http://abelladanger.online/# abella danger izle
https://lanarhoades.fun/# lana rhoades modeli
http://angelawhite.pro/# Angela White filmleri
lana rhoades video: lana rhoades – lana rhoades modeli
https://sweetiefox.online/# Sweetie Fox filmleri
http://abelladanger.online/# Abella Danger
eva elfie modeli: eva elfie modeli – eva elfie
https://evaelfie.pro/# eva elfie izle
http://angelawhite.pro/# Angela White izle
Angela White izle: abella danger filmleri – abella danger video
sweetie fox cosplay: fox sweetie – sweetie fox full video
http://sweetiefox.pro/# sweetie fox video
lana rhoades pics: lana rhoades unleashed – lana rhoades videos
women dates local no fee: http://miamalkova.life/# mia malkova latest
https://lanarhoades.pro/# lana rhoades videos
sweetie fox full: ph sweetie fox – sweetie fox full video
mia malkova photos: mia malkova movie – mia malkova full video
https://lanarhoades.pro/# lana rhoades videos
eva elfie new videos: eva elfie – eva elfie hd
best date online: https://lanarhoades.pro/# lana rhoades hot
mia malkova photos: mia malkova full video – mia malkova latest
http://evaelfie.site/# eva elfie videos
lana rhoades videos: lana rhoades hot – lana rhoades full video
sweetie fox: fox sweetie – sweetie fox full
http://evaelfie.site/# eva elfie videos
farmers only dating website: http://lanarhoades.pro/# lana rhoades boyfriend
mia malkova latest: mia malkova latest – mia malkova photos
mia malkova girl: mia malkova full video – mia malkova hd
https://miamalkova.life/# mia malkova latest
mia malkova only fans: mia malkova videos – mia malkova videos
free dating site chatting: http://lanarhoades.pro/# lana rhoades unleashed
http://sweetiefox.pro/# sweetie fox full video
mia malkova girl: mia malkova movie – mia malkova
eva elfie new video: eva elfie full videos – eva elfie
https://sweetiefox.pro/# sweetie fox full video
eva elfie: eva elfie full videos – eva elfie
strydom mail: https://evaelfie.site/# eva elfie hd
http://evaelfie.site/# eva elfie hd
lana rhoades videos: lana rhoades pics – lana rhoades solo
eva elfie full videos: eva elfie hd – eva elfie videos
lana rhoades solo: lana rhoades full video – lana rhoades hot
http://lanarhoades.pro/# lana rhoades
free on chatting: https://lanarhoades.pro/# lana rhoades videos
lana rhoades full video: lana rhoades unleashed – lana rhoades full video
https://lanarhoades.pro/# lana rhoades unleashed
ph sweetie fox: sweetie fox cosplay – sweetie fox video
https://aviatoroyunu.pro/# aviator oyna
jogar aviator: jogar aviator – aviator mz
https://aviatorghana.pro/# play aviator
http://pinupcassino.pro/# aviator pin up casino
aviator sportybet ghana: play aviator – play aviator
aviator login: play aviator – aviator betting game
aviator bet: aviator malawi – aviator bet
https://pinupcassino.pro/# pin up bet
https://pinupcassino.pro/# pin up
aviator: aviator game – aviator game
aviator: como jogar aviator em mocambique – aviator mocambique
como jogar aviator: jogar aviator – aviator mz
http://aviatormocambique.site/# aviator online
http://aviatorjogar.online/# aviator jogar
aviator: aviator game online – play aviator
http://aviatorjogar.online/# aviator game
https://pinupcassino.pro/# pin-up casino entrar
aviator bet: aviator – aviator
aviator game bet: aviator game – aviator
jogo de aposta: site de apostas – aviator jogo de aposta
jogos que dao dinheiro: aviator jogo de aposta – jogo de aposta
aviator sinyal hilesi: aviator oyna slot – pin up aviator
http://aviatorjogar.online/# aviator jogo
aviator game: aviator game – aviator game
aviator: aviator sportybet ghana – play aviator
aviator bet: aviator betting game – aviator game online
aviator oyna: aviator bahis – aviator oyna slot
https://aviatorjogar.online/# aviator betano
zithromax over the counter canada – https://azithromycin.pro/sinus-infection-zithromax.html generic zithromax 500mg india
como jogar aviator em moçambique: aviator – como jogar aviator
zithromax cost canada – https://azithromycin.pro/does-zithromax-cause-diarrhea.html where to get zithromax over the counter
melhor jogo de aposta: jogo de aposta online – depósito mínimo 1 real
how to buy zithromax online – https://azithromycin.pro/zithromax-500-mg-coupon.html buy zithromax online fast shipping
aviator betting game: aviator betting game – aviator login
play aviator: aviator bet – aviator game bet
purple pharmacy mexico price list: Mexico pharmacy online – purple pharmacy mexico price list mexicanpharm.shop
reliable canadian online pharmacy Best Canadian online pharmacy canadian drug prices canadianpharm.store
top 10 pharmacies in india: Pharmacies in India that ship to USA – best india pharmacy indianpharm.store
http://canadianpharmlk.com/# canadian medications canadianpharm.store
canadian world pharmacy: Pharmacies in Canada that ship to the US – recommended canadian pharmacies canadianpharm.store
best online pharmacies in mexico Medicines Mexico mexican online pharmacies prescription drugs mexicanpharm.shop
http://canadianpharmlk.shop/# reliable canadian pharmacy reviews canadianpharm.store
http://indianpharm24.com/# top online pharmacy india indianpharm.store
legit canadian pharmacy online: Canada pharmacy online – canadian pharmacy uk delivery canadianpharm.store
http://indianpharm24.shop/# indian pharmacy indianpharm.store
http://mexicanpharm24.com/# mexican rx online mexicanpharm.shop
http://mexicanpharm24.com/# mexican rx online mexicanpharm.shop
medication from mexico pharmacy: Medicines Mexico – mexican rx online mexicanpharm.shop
https://mexicanpharm24.com/# mexican drugstore online mexicanpharm.shop
canadian pharmacy: Pharmacies in Canada that ship to the US – canadian neighbor pharmacy canadianpharm.store
http://mexicanpharm24.shop/# reputable mexican pharmacies online mexicanpharm.shop
http://mexicanpharm24.shop/# buying prescription drugs in mexico online mexicanpharm.shop
https://canadianpharmlk.shop/# pet meds without vet prescription canada canadianpharm.store
online shopping pharmacy india Best Indian pharmacy world pharmacy india indianpharm.store
online shopping pharmacy india: Pharmacies in India that ship to USA – п»їlegitimate online pharmacies india indianpharm.store
https://canadianpharmlk.com/# canadian pharmacy service canadianpharm.store
http://canadianpharmlk.com/# canada ed drugs canadianpharm.store
https://indianpharm24.shop/# top online pharmacy india indianpharm.store
https://canadianpharmlk.com/# canadian online pharmacy reviews canadianpharm.store
mexican mail order pharmacies: mexican pharmacy – buying prescription drugs in mexico mexicanpharm.shop
https://indianpharm24.com/# indian pharmacy paypal indianpharm.store
https://mexicanpharm24.com/# mexican pharmaceuticals online mexicanpharm.shop
mexican drugstore online mexican rx online medication from mexico pharmacy mexicanpharm.shop
canada drug pharmacy: Canada pharmacy online – canada drugs online review canadianpharm.store
http://mexicanpharm24.shop/# mexico drug stores pharmacies mexicanpharm.shop
http://indianpharm24.com/# online shopping pharmacy india indianpharm.store
http://canadianpharmlk.com/# canadian pharmacy review canadianpharm.store
https://indianpharm24.shop/# reputable indian pharmacies indianpharm.store
https://canadianpharmlk.shop/# online canadian pharmacy canadianpharm.store
top 10 pharmacies in india: Generic Medicine India to USA – Online medicine home delivery indianpharm.store
amoxicillin tablet 500mg: amoxicillin for tooth infection – how to buy amoxicillin online
buy amoxicillin online without prescription: amoxicillin/clavulanate potassium – order amoxicillin online
https://clomidst.pro/# where to buy clomid tablets
prednisone 20 mg in india: ibuprofen and prednisone – prednisone 40mg
buy cheap amoxicillin: amoxicillin for sale – amoxicillin 50 mg tablets
http://prednisonest.pro/# prednisone 20mg tab price
can i buy generic clomid now: cost clomid price – order clomid pills
amoxicillin 500mg capsules price cost of amoxicillin buy amoxicillin 500mg usa
amoxicillin over counter: amoxicillin 500mg price – buy amoxicillin from canada
buy 10 mg prednisone: prednisone and ibuprofen – over the counter prednisone pills
prednisone pills cost: prednisone 10 mg – prednisone brand name
https://prednisonest.pro/# prednisone cost in india
can i get clomid without insurance: clomid twins – where can i buy cheap clomid price
where to get clomid prices: can i order generic clomid pills – can i purchase clomid without insurance
amoxicillin pills 500 mg: where to buy amoxicillin over the counter – amoxicillin azithromycin
http://clomidst.pro/# buying generic clomid without insurance
clomid generics: order clomid prices – where can i get cheap clomid without insurance
where buy cheap clomid without prescription how can i get clomid prices can you buy generic clomid for sale
cost cheap clomid price: how to buy cheap clomid without prescription – can i get generic clomid online
where to buy cheap clomid without insurance: can you buy generic clomid for sale – how to get generic clomid without insurance
http://clomidst.pro/# can i purchase cheap clomid
amoxicillin order online: amoxil pharmacy – can i purchase amoxicillin online
prednisone 10mg price in india: prednisone taper schedule – can i order prednisone
amoxicillin 500mg pill: amoxicillin where to get – buy amoxicillin online cheap
https://clomidst.pro/# get generic clomid
cost of amoxicillin 30 capsules: amoxicillin 500mg capsules – buy amoxicillin
prednisone daily: prednisone where can i buy – prednisone ordering online
https://onlinepharmacy.cheap/# buying prescription drugs from canada
buying drugs without prescription: buying prescription drugs online without a prescription – canadian pharmacy no prescription
http://onlinepharmacy.cheap/# online pharmacy discount code
get ed prescription online: online ed medicine – erectile dysfunction medicine online
cheapest ed medication: edmeds – online erectile dysfunction medication
promo code for canadian pharmacy meds: Best online pharmacy – canadian online pharmacy no prescription
http://edpills.guru/# ed med online
https://onlinepharmacy.cheap/# cheapest pharmacy prescription drugs
meds online without prescription: canada prescription drugs online – buy prescription online
order prescription from canada: buy meds online without prescription – buy drugs online without prescription
canadian pharmacies not requiring prescription discount pharmacy promo code for canadian pharmacy meds
canadian pharmacy coupon: canada online pharmacy – canadian pharmacies not requiring prescription
https://pharmnoprescription.pro/# canadian pharmacy no prescription needed
edmeds: what is the cheapest ed medication – ed medicine online
canadian pharmacy discount coupon: canadian pharmacy online – canadian pharmacy world coupon
how to get ed meds online: ed pills online – cheap ed medication
http://onlinepharmacy.cheap/# canadian pharmacy world coupon code
canada pharmacy coupon: canadian online pharmacy – cheapest pharmacy for prescription drugs
online pharmacy prescription: canadian online pharmacy – canadian pharmacy world coupon code
cheap prescription drugs online: online prescription canada – mexican pharmacies no prescription
canadian prescription drugstore review: buying prescription drugs online from canada – canadian pharmacy online no prescription
http://pharmnoprescription.pro/# best online pharmacy without prescriptions
mail order pharmacy no prescription Cheapest online pharmacy canadian pharmacy world coupon
http://edpills.guru/# where to get ed pills
promo code for canadian pharmacy meds: canada pharmacy online – canadian pharmacy coupon code
will flexeril show on a drug test
meds online without prescription: no prescription needed – prescription from canada
https://onlinepharmacy.cheap/# non prescription medicine pharmacy
online no prescription pharmacy: online drugs without prescription – mail order prescriptions from canada
india pharmacy: reputable indian online pharmacy – indianpharmacy com
http://indianpharm.shop/# best online pharmacy india
canadian medications: canadian pharmacy scam – canadian pharmacy world reviews
http://canadianpharm.guru/# canadian pharmacy reviews
pharmacy rx world canada legitimate canadian pharmacy canadian neighbor pharmacy
http://canadianpharm.guru/# best canadian online pharmacy
buy medicines online in india: indian pharmacy paypal – buy prescription drugs from india
mexican pharmaceuticals online: mexican pharmaceuticals online – mexican mail order pharmacies
cheap canadian pharmacy online: canadian pharmacy antibiotics – adderall canadian pharmacy
http://canadianpharm.guru/# canadian online pharmacy
pharmacies in mexico that ship to usa: mexican pharmacy – buying from online mexican pharmacy
prescription canada: buy meds online no prescription – buy medications online without prescription
online drugstore no prescription: prescription from canada – canadian pharmacy online no prescription
http://pharmacynoprescription.pro/# online meds no prescription
https://pharmacynoprescription.pro/# buy medication online without prescription
purple pharmacy mexico price list: buying prescription drugs in mexico online – mexican mail order pharmacies
pharmacy no prescription required: mexico prescription drugs online – no prescription online pharmacy
https://canadianpharm.guru/# canada pharmacy online
canadian compounding pharmacy: cheap canadian pharmacy – canada pharmacy online
best no prescription online pharmacies: buy meds online no prescription – buying prescription drugs in india
safe canadian pharmacy: reputable canadian online pharmacy – canadian pharmacy 365
best canadian online pharmacy: best online canadian pharmacy – canadian online drugs
https://pharmacynoprescription.pro/# canadian pharmacy prescription
top online pharmacy india: reputable indian pharmacies – india online pharmacy
https://indianpharm.shop/# indian pharmacy online
buy pills without prescription: buy prescription drugs online without doctor – best online pharmacy no prescription
canadian prescription drugstore reviews canadian prescription no prescription drugs
Online medicine order: india pharmacy – india pharmacy
https://indianpharm.shop/# pharmacy website india
buy medicines online in india: india pharmacy mail order – online pharmacy india
pharmacies in mexico that ship to usa: pharmacies in mexico that ship to usa – purple pharmacy mexico price list
buy medications without a prescription: online pharmacy no prescriptions – online pharmacy canada no prescription
http://mexicanpharm.online/# pharmacies in mexico that ship to usa
buying from online mexican pharmacy: mexico drug stores pharmacies – mexico drug stores pharmacies
reliable canadian pharmacy: online canadian pharmacy – buy canadian drugs
best india pharmacy: reputable indian online pharmacy – п»їlegitimate online pharmacies india
https://indianpharm.shop/# world pharmacy india
reputable indian online pharmacy: pharmacy website india – legitimate online pharmacies india
https://indianpharm.shop/# mail order pharmacy india
mail order prescriptions from canada best online prescription online pharmacy not requiring prescription
canada drug pharmacy: reputable canadian online pharmacy – cheap canadian pharmacy online
ordering prescription drugs from canada: online pharmacies no prescription usa – meds online without prescription
https://pharmacynoprescription.pro/# buy drugs online without prescription
order prescription from canada: non prescription online pharmacy india – buy medication online no prescription
medication from mexico pharmacy: purple pharmacy mexico price list – mexican mail order pharmacies
https://indianpharm.shop/# buy medicines online in india
indian pharmacies safe: reputable indian pharmacies – best online pharmacy india
buy medication online with prescription: cheap prescription drugs online – best no prescription online pharmacy
Online medicine order: best india pharmacy – india pharmacy
safe canadian pharmacy: canadian family pharmacy – canadapharmacyonline legit
https://mexicanpharm.online/# medication from mexico pharmacy
https://canadianpharm.guru/# canadian pharmacy online ship to usa
canadian drugs pharmacy canadian valley pharmacy best canadian pharmacy to order from
canadianpharmacy com: canadian pharmacy ltd – reliable canadian pharmacy
mexico drug stores pharmacies: mexican border pharmacies shipping to usa – mexican border pharmacies shipping to usa
mail order pharmacy india: legitimate online pharmacies india – top online pharmacy india
https://pharmacynoprescription.pro/# no prescription medicine
best india pharmacy: world pharmacy india – cheapest online pharmacy india
legitimate canadian pharmacies: canada rx pharmacy – canadian online pharmacy
cheap canadian pharmacy: reputable canadian online pharmacies – safe online pharmacies in canada
http://canadianpharm.guru/# canadian pharmacy
cheap drugs no prescription: canada drugs no prescription – prescription meds from canada
http://mexicanpharm.online/# mexico pharmacies prescription drugs
celebrex side effects mayo clinic
no prescription needed: canada online prescription – buying drugs online no prescription
prescription drugs canada order prescription drugs online without doctor buy medications online without prescription
best online pharmacy india: reputable indian online pharmacy – top 10 pharmacies in india
https://mexicanpharm.online/# mexico pharmacies prescription drugs
canada pharmacy online: canadian pharmacy ratings – canadian pharmacy 365
best mexican online pharmacies: mexico drug stores pharmacies – medication from mexico pharmacy
https://aviatoroyna.bid/# aviator oyunu 50 tl
pin up casino: pin up giris – pin-up online
http://gatesofolympus.auction/# gates of olympus demo türkçe
http://pinupgiris.fun/# pin up casino
pin up: pin-up casino indir – pin up aviator
pin up: pin-up giris – aviator pin up
http://aviatoroyna.bid/# aviator hilesi ücretsiz
http://gatesofolympus.auction/# gates of olympus hilesi
aviator sinyal hilesi ucretsiz: aviator oyunu giris – aviator sinyal hilesi apk
http://sweetbonanza.bid/# sweet bonanza hilesi
http://slotsiteleri.guru/# oyun siteleri slot
aviator sinyal hilesi: aviator oyunu 20 tl – aviator oyna
https://slotsiteleri.guru/# slot bahis siteleri
casino slot siteleri: yeni slot siteleri – slot casino siteleri
http://sweetbonanza.bid/# sweet bonanza
guvenilir slot siteleri: slot oyun siteleri – en iyi slot siteleri
https://aviatoroyna.bid/# aviator hilesi
http://aviatoroyna.bid/# aviator oyunu 50 tl
guvenilir slot siteleri: slot casino siteleri – en iyi slot siteleri
http://gatesofolympus.auction/# gates of olympus nasil para kazanilir
pin up aviator: pin up casino giris – pin up aviator
https://sweetbonanza.bid/# güncel sweet bonanza
pragmatic play gates of olympus: gates of olympus oyna demo – gates of olympus nas?l para kazanilir
aviator oyna: aviator sinyal hilesi – aviator mostbet
https://aviatoroyna.bid/# aviator sinyal hilesi ücretsiz
https://gatesofolympus.auction/# gates of olympus guncel
http://slotsiteleri.guru/# slot siteleri güvenilir
sweet bonanza yorumlar: sweet bonanza – slot oyunlari
https://gatesofolympus.auction/# gates of olympus oyna ücretsiz
sweet bonanza free spin demo: sweet bonanza indir – sweet bonanza bahis
gates of olympus giris: gates of olympus demo free spin – gates of olympus guncel
https://sweetbonanza.bid/# sweet bonanza
guvenilir slot siteleri 2024: deneme veren slot siteleri – canl? slot siteleri
http://pinupgiris.fun/# pin up casino indir
legal canadian pharmacy online Licensed Canadian Pharmacy canadian pharmacy no rx needed
canadian drugs pharmacy: Prescription Drugs from Canada – best canadian pharmacy online
http://indianpharmacy.icu/# online shopping pharmacy india
buy medicines online in india indian pharmacy indian pharmacy
mexican pharmacy: Online Pharmacies in Mexico – mexican pharmaceuticals online
canadian pharmacy mall: pills now even cheaper – pharmacy com canada
online canadian pharmacy reviews Certified Canadian Pharmacy canadian pharmacy world
top online pharmacy india: Healthcare and medicines from India – world pharmacy india
indian pharmacy online Healthcare and medicines from India cheapest online pharmacy india
purple pharmacy mexico price list: mexico pharmacy – mexico drug stores pharmacies
buying prescription drugs in mexico: mexico pharmacy – buying prescription drugs in mexico online
https://indianpharmacy.icu/# Online medicine home delivery
buying from online mexican pharmacy: mexican drugstore online – mexican pharmaceuticals online
mexico pharmacies prescription drugs: best online pharmacies in mexico – mexican pharmaceuticals online
best canadian pharmacy: pills now even cheaper – canadian online drugstore
mexican mail order pharmacies Mexican Pharmacy Online medicine in mexico pharmacies
best online pharmacies in mexico: mexico pharmacy – mexican border pharmacies shipping to usa
pharmacies in mexico that ship to usa: cheapest mexico drugs – buying prescription drugs in mexico online
top 10 online pharmacy in india Cheapest online pharmacy reputable indian pharmacies
online pharmacy india: Healthcare and medicines from India – legitimate online pharmacies india
indian pharmacies safe Cheapest online pharmacy buy medicines online in india
https://mexicanpharmacy.shop/# medicine in mexico pharmacies
drugs from canada: Prescription Drugs from Canada – canadian medications
indianpharmacy com: Cheapest online pharmacy – top online pharmacy india
legit canadian pharmacy: Large Selection of Medications – canadian pharmacy online reviews
mexican online pharmacies prescription drugs: Mexican Pharmacy Online – mexico drug stores pharmacies
top 10 online pharmacy in india indian pharmacy indianpharmacy com
the canadian pharmacy: Prescription Drugs from Canada – trusted canadian pharmacy
buying prescription drugs in mexico online reputable mexican pharmacies online mexican rx online
purple pharmacy mexico price list: buying prescription drugs in mexico – mexican pharmaceuticals online
http://indianpharmacy.icu/# п»їlegitimate online pharmacies india
canadian pharmacy world Certified Canadian Pharmacy global pharmacy canada
top 10 online pharmacy in india: Healthcare and medicines from India – world pharmacy india
purple pharmacy mexico price list: cheapest mexico drugs – п»їbest mexican online pharmacies
indian pharmacy paypal: Cheapest online pharmacy – buy prescription drugs from india
mexican online pharmacies prescription drugs: mexico pharmacy – mexico drug stores pharmacies
prednisone 50 mg canada prednisone pills for sale buy prednisone 20mg without a prescription best price
http://prednisoneall.shop/# prednisone 50 mg for sale
https://amoxilall.shop/# buy amoxicillin 500mg uk
http://zithromaxall.com/# zithromax buy online
buy cheap zithromax online can i buy zithromax over the counter in canada zithromax online australia
get cheap clomid without dr prescription: can i buy clomid no prescription – buying clomid without prescription
how can i get cheap clomid without a prescription: buy clomid without prescription – clomid for sale
http://prednisoneall.com/# purchase prednisone from india
amoxicillin price canada amoxicillin order online amoxicillin over the counter in canada
http://prednisoneall.com/# buy prednisone without a prescription
https://amoxilall.com/# amoxicillin 500mg price canada
https://clomidall.com/# cost of clomid pills
how to get zithromax over the counter can you buy zithromax over the counter buy zithromax 1000 mg online
http://zithromaxall.com/# zithromax 250 mg pill
how to buy generic clomid without prescription can i order cheap clomid pill cost cheap clomid now
https://clomidall.shop/# can you buy clomid for sale
https://amoxilall.shop/# canadian pharmacy amoxicillin
5 mg prednisone daily: prednisone for sale – prednisone 2.5 mg price
prednisone 5mg price: prednisone 10mg tablet price – 20 mg prednisone tablet
https://zithromaxall.shop/# zithromax online
buy generic zithromax online generic zithromax online paypal can you buy zithromax online
https://zithromaxall.com/# zithromax 1000 mg online
https://clomidall.shop/# where can i get clomid now
zithromax online paypal buy azithromycin zithromax zithromax tablets
https://amoxilall.shop/# amoxicillin 500mg over the counter
http://zithromaxall.shop/# zithromax 500 mg
acarbose india
can you buy zithromax over the counter in canada zithromax 250 mg tablet price zithromax buy online
https://prednisoneall.com/# price for 15 prednisone
can i buy prednisone from canada without a script: prednisone 20mg buy online – purchase prednisone
amoxicillin discount: amoxicillin 250 mg – amoxicillin discount coupon
https://prednisoneall.com/# prednisone without prescription 10mg
http://zithromaxall.com/# zithromax 500 without prescription
zithromax drug zithromax 500 price zithromax 500 without prescription
http://zithromaxall.com/# buy zithromax no prescription
amoxicillin 500mg buy online canada generic amoxicillin 500mg amoxicillin 875 mg tablet
best price for viagra 100mg: buy viagra online – Viagra Tablet price
Kamagra 100mg Kamagra Oral Jelly п»їkamagra
http://kamagraiq.com/# Kamagra 100mg
Tadalafil Tablet: cialis generic – cheapest cialis
Kamagra 100mg price: Kamagra Oral Jelly Price – sildenafil oral jelly 100mg kamagra
buy Viagra over the counter Viagra online price Generic Viagra online
https://tadalafiliq.shop/# Cialis 20mg price
https://sildenafiliq.xyz/# cheapest viagra
buy Kamagra: Sildenafil Oral Jelly – Kamagra 100mg
Cialis 20mg price Buy Cialis online Generic Cialis price
Generic Tadalafil 20mg price: tadalafil iq – Cheap Cialis
http://tadalafiliq.shop/# Tadalafil price
Kamagra 100mg: Kamagra Oral Jelly Price – Kamagra 100mg price
Cialis over the counter: cialis best price – Tadalafil Tablet
Buy Tadalafil 20mg cheapest cialis Cialis 20mg price in USA
Buy Tadalafil 10mg: Buy Tadalafil 10mg – cialis generic
http://sildenafiliq.com/# Viagra without a doctor prescription Canada
sildenafil oral jelly 100mg kamagra Kamagra gel Kamagra 100mg
http://tadalafiliq.shop/# Buy Cialis online
https://sildenafiliq.com/# Cheap generic Viagra
п»їBuy generic 100mg Viagra online generic ed pills viagra without prescription
https://sildenafiliq.xyz/# Generic Viagra for sale
Cialis 20mg price: Buy Cialis online – Cialis without a doctor prescription
Buy Tadalafil 10mg: cheapest cialis – Generic Cialis without a doctor prescription
Viagra online price: cheapest viagra – Cheap generic Viagra online
Buy Cialis online cheapest cialis Cialis over the counter
http://kamagraiq.shop/# п»їkamagra
http://tadalafiliq.com/# Generic Tadalafil 20mg price
Cialis 20mg price in USA: cialis best price – Cialis without a doctor prescription
http://tadalafiliq.shop/# Tadalafil Tablet
Viagra online price Generic Viagra online sildenafil over the counter
buy cialis pill: Buy Cialis online – Generic Cialis price
https://tadalafiliq.com/# Cialis 20mg price in USA
Cheap Cialis: Generic Tadalafil 20mg price – Buy Tadalafil 20mg
https://sildenafiliq.com/# sildenafil online
Kamagra Oral Jelly Sildenafil Oral Jelly cheap kamagra
Kamagra 100mg price: Kamagra 100mg price – Kamagra 100mg price
Cialis 20mg price in USA: Buy Cialis online – Cialis 20mg price
http://sildenafiliq.com/# generic sildenafil
sildenafil oral jelly 100mg kamagra Kamagra Oral Jelly Price Kamagra 100mg price
https://tadalafiliq.shop/# Tadalafil price
http://sildenafiliq.xyz/# best price for viagra 100mg
https://mexicanpharmgrx.shop/# mexican pharmaceuticals online
buy prescription drugs from india india pharmacy mail order top 10 pharmacies in india
mexico drug stores pharmacies: Mexico drugstore – buying from online mexican pharmacy
http://mexicanpharmgrx.shop/# mexico drug stores pharmacies
canadianpharmacymeds CIPA approved pharmacies canadian pharmacy sarasota
reputable indian pharmacies: indian pharmacy delivery – buy medicines online in india
http://mexicanpharmgrx.shop/# mexican mail order pharmacies
canada drugs online reviews: Cheapest drug prices Canada – online pharmacy canada
canada pharmacy online Canada pharmacy online canadian online pharmacy reviews
https://mexicanpharmgrx.shop/# mexico pharmacy
mexican pharmaceuticals online: Mexico drugstore – purple pharmacy mexico price list
http://mexicanpharmgrx.com/# mexican mail order pharmacies
reputable canadian online pharmacy List of Canadian pharmacies reputable canadian online pharmacies
http://mexicanpharmgrx.shop/# mexican online pharmacies prescription drugs
canadian neighbor pharmacy: canadian pharmacy – canadianpharmacymeds com
canadian pharmacy in canada Cheapest drug prices Canada best canadian pharmacy to buy from
india pharmacy mail order: Healthcare and medicines from India – mail order pharmacy india
http://indianpharmgrx.com/# pharmacy website india
mexican border pharmacies shipping to usa: buying from online mexican pharmacy – mexican drugstore online
top 10 pharmacies in india indian pharmacy delivery indian pharmacy online
http://mexicanpharmgrx.shop/# mexican pharmacy
https://mexicanpharmgrx.com/# mexico drug stores pharmacies
indian pharmacy Online medicine order india pharmacy mail order
indian pharmacy online: indian pharmacy – top online pharmacy india
http://mexicanpharmgrx.shop/# best mexican online pharmacies
canadian pharmacy cheap List of Canadian pharmacies canadian pharmacy antibiotics
my canadian pharmacy: online canadian pharmacy – canada rx pharmacy world
https://indianpharmgrx.shop/# india pharmacy
mexican pharmacy: mexican pharmacy – mexico drug stores pharmacies
buying from online mexican pharmacy: buying prescription drugs in mexico online – mexican rx online
pharmacies in mexico that ship to usa buying from online mexican pharmacy purple pharmacy mexico price list
http://canadianpharmgrx.com/# canadian pharmacies that deliver to the us
mexican rx online Pills from Mexican Pharmacy п»їbest mexican online pharmacies
canada drugs online: International Pharmacy delivery – canadian drug
http://indianpharmgrx.com/# indian pharmacy paypal
diflucan prescription: diflucan otc – diflucan pill over the counter
doxycycline online buy doxycycline cheap cheap doxycycline online
Misoprostol 200 mg buy online: buy cytotec over the counter – order cytotec online
doxycycline medication: price of doxycycline – doxycycline 150 mg
ciprofloxacin 500mg buy online: buy cipro online – cipro 500mg best prices
http://ciprofloxacin.guru/# where to buy cipro online
cipro: antibiotics cipro – ciprofloxacin 500 mg tablet price
tamoxifen chemo tamoxifen bone pain tamoxifen for sale
buy cytotec over the counter: Abortion pills online – purchase cytotec
doxycycline 50mg: doxycycline tablets – doxycycline hyclate 100 mg cap
buy cytotec in usa buy cytotec pills online cheap buy cytotec
buy generic diflucan: diflucan online cheap without a prescription – diflucan 100mg
purchase cipro: cipro ciprofloxacin – ciprofloxacin 500 mg tablet price
diflucan 100 mg diflucan 150 mg buy online can i buy diflucan over the counter in australia
Cytotec 200mcg price: order cytotec online – buy cytotec over the counter
п»їcipro generic: buy ciprofloxacin – buy cipro online canada
how to buy doxycycline online: doxycycline 50 mg – doxycycline 100 mg
http://misoprostol.top/# buy cytotec
doxycycline pills price of doxycycline doxycycline without prescription
tamoxifen rash pictures: tamoxifen dose – nolvadex generic
Cytotec 200mcg price: п»їcytotec pills online – cytotec buy online usa
buy cytotec over the counter buy cytotec online fast delivery Abortion pills online
can you purchase diflucan over the counter: diflucan tabs – can you buy diflucan over the counter in canada
buy cytotec online fast delivery: buy cytotec online – cytotec online
buy cytotec in usa cytotec pills buy online cytotec pills buy online
buy cheap doxycycline: where to purchase doxycycline – buy generic doxycycline
ciprofloxacin generic price: cipro – cipro online no prescription in the usa
http://misoprostol.top/# buy cytotec over the counter
cytotec pills buy online buy cytotec online п»їcytotec pills online
cytotec buy online usa: order cytotec online – cytotec pills online
cytotec abortion pill order cytotec online buy cytotec
diflucan canadian pharmacy: buy diflucan online uk – buy diflucan without a prescription
order cytotec online: buy cytotec online – buy cytotec in usa
where can i get doxycycline doxycycline 150 mg doxycycline without a prescription
ciprofloxacin 500 mg tablet price: buy cipro cheap – cipro online no prescription in the usa
stromectol south africa: ivermectin goodrx – stromectol 3mg
prednisone 10mg tabs prednisone 20mg tablets where to buy prednisone 5 mg tablet cost
zithromax tablets: where to get zithromax over the counter – generic zithromax medicine
buy clomid without prescription: how to get cheap clomid without a prescription – cost of clomid
can you get clomid pills can you get cheap clomid without insurance where can i buy generic clomid now
prednisone without prescription.net: buy prednisone no prescription – prednisone buy canada
stromectol tab 3mg: ivermectin 3mg tablets – stromectol xl
https://clomida.pro/# where to get generic clomid without prescription
http://stromectola.top/# ivermectin 0.08%
amoxil pharmacy: buy amoxicillin online uk – amoxicillin 500
can you buy amoxicillin over the counter canada where can i buy amoxicillin over the counter order amoxicillin 500mg
can you buy prednisone over the counter in canada: prednisone price south africa – prednisone tablets 2.5 mg
https://azithromycina.pro/# zithromax for sale 500 mg
how can i get generic clomid without prescription: buy clomid tablets – order cheap clomid pills
buying prednisone without prescription prednisone 20mg prednisone 2.5 mg tab
how can i get clomid online: generic clomid without prescription – cost of clomid without prescription
http://stromectola.top/# ivermectin over the counter
zithromax 500mg over the counter: zithromax 600 mg tablets – zithromax 500 without prescription
how to get zithromax: zithromax online australia – zithromax 1000 mg online
amoxicillin 250 mg buy amoxicillin 250mg buy amoxicillin without prescription
http://stromectola.top/# ivermectin 5 mg
how to buy amoxicillin online: buy cheap amoxicillin online – purchase amoxicillin 500 mg
http://azithromycina.pro/# zithromax 500mg over the counter
canadian prescription drugstore review: discount prescription drugs canada – best online pharmacy no prescription
canadian prescription pharmacy buying prescription drugs from canada foreign pharmacy no prescription
https://onlinepharmacyworld.shop/# cheapest pharmacy for prescription drugs
http://edpill.top/# online ed prescription
http://onlinepharmacyworld.shop/# canadian pharmacy discount code
buying prescription medications online: buy drugs online without a prescription – best online pharmacy without prescriptions
no prescription pharmacy online best online pharmacy without prescriptions no prescription drugs online
https://edpill.top/# where to get ed pills
https://edpill.top/# buy ed medication
http://medicationnoprescription.pro/# online pharmacy no prescriptions
non prescription medicine pharmacy: non prescription medicine pharmacy – no prescription required pharmacy
http://edpill.top/# ed online meds
us pharmacy no prescription canada pharmacy coupon pharmacy coupons
https://edpill.top/# cheap erectile dysfunction pills
cheapest erectile dysfunction pills: generic ed meds online – erectile dysfunction medications online
legit non prescription pharmacies online pharmacy without prescription best no prescription pharmacy
https://onlinepharmacyworld.shop/# canadian pharmacy world coupons
http://edpill.top/# online erectile dysfunction
canadian drugs no prescription: mexican pharmacy no prescription – online pharmacy without prescriptions
https://edpill.top/# order ed meds online
cheapest pharmacy to fill prescriptions with insurance canadian pharmacy discount coupon no prescription needed pharmacy
affordable ed medication: buy erectile dysfunction pills – cheapest online ed treatment
https://casinvietnam.com/# casino tr?c tuy?n vi?t nam
casino online uy tín: casino tr?c tuy?n vi?t nam – casino tr?c tuy?n vi?t nam
https://casinvietnam.shop/# casino online uy tin
dánh bài tr?c tuy?n: game c? b?c online uy tín – choi casino tr?c tuy?n trên di?n tho?i
web c? b?c online uy tin web c? b?c online uy tin choi casino tr?c tuy?n tren di?n tho?i
http://casinvietnam.shop/# choi casino tr?c tuy?n tren di?n tho?i
casino online uy tin choi casino tr?c tuy?n tren di?n tho?i casino tr?c tuy?n vi?t nam
http://casinvietnam.com/# web c? b?c online uy tin
casino tr?c tuy?n uy tín: game c? b?c online uy tín – choi casino tr?c tuy?n trên di?n tho?i
casino tr?c tuy?n vi?t nam: casino tr?c tuy?n – web c? b?c online uy tín
casino tr?c tuy?n vi?t nam: casino tr?c tuy?n uy tín – dánh bài tr?c tuy?n
casino tr?c tuy?n vi?t nam: game c? b?c online uy tín – casino online uy tín
https://casinvietnam.shop/# choi casino tr?c tuy?n tren di?n tho?i
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
web c? b?c online uy tín: casino tr?c tuy?n – choi casino tr?c tuy?n trên di?n tho?i
casino tr?c tuy?n uy tín: casino tr?c tuy?n uy tín – casino tr?c tuy?n
https://casinvietnam.shop/# casino online uy tin
web c? b?c online uy tín: dánh bài tr?c tuy?n – casino online uy tín
http://casinvietnam.com/# casino tr?c tuy?n vi?t nam
https://casinvietnam.com/# web c? b?c online uy tin
web c? b?c online uy tín: casino online uy tín – casino tr?c tuy?n uy tín
game c? b?c online uy tín: dánh bài tr?c tuy?n – casino tr?c tuy?n uy tín
http://casinvietnam.shop/# web c? b?c online uy tin
choi casino tr?c tuy?n trên di?n tho?i: dánh bài tr?c tuy?n – casino tr?c tuy?n vi?t nam
https://canadaph24.pro/# best canadian online pharmacy
http://mexicoph24.life/# purple pharmacy mexico price list
https://canadaph24.pro/# best canadian pharmacy to buy from
http://indiaph24.store/# Online medicine order
http://mexicoph24.life/# mexican online pharmacies prescription drugs
https://indiaph24.store/# world pharmacy india
http://indiaph24.store/# online shopping pharmacy india
https://indiaph24.store/# best online pharmacy india
https://indiaph24.store/# reputable indian online pharmacy
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
http://canadaph24.pro/# canada cloud pharmacy
http://canadaph24.pro/# canadian pharmacy drugs online
https://canadaph24.pro/# buying drugs from canada
http://mexicoph24.life/# mexican mail order pharmacies
http://indiaph24.store/# legitimate online pharmacies india
https://indiaph24.store/# indianpharmacy com
https://canadaph24.pro/# pharmacy canadian
https://indiaph24.store/# indianpharmacy com
http://indiaph24.store/# mail order pharmacy india
https://indiaph24.store/# online pharmacy india
http://mexicoph24.life/# mexican drugstore online
https://mexicoph24.life/# mexican drugstore online
https://mexicoph24.life/# buying from online mexican pharmacy
http://canadaph24.pro/# best canadian pharmacy to buy from
http://mexicoph24.life/# pharmacies in mexico that ship to usa
https://canadaph24.pro/# canadian discount pharmacy
http://indiaph24.store/# indian pharmacy online
https://indiaph24.store/# world pharmacy india
http://indiaph24.store/# best india pharmacy
http://indiaph24.store/# indian pharmacy online
http://canadaph24.pro/# thecanadianpharmacy
https://canadaph24.pro/# reliable canadian pharmacy reviews
https://mexicoph24.life/# purple pharmacy mexico price list
https://mexicoph24.life/# best mexican online pharmacies
https://canadaph24.pro/# canadian pharmacy world
http://mexicoph24.life/# mexican mail order pharmacies
https://indiaph24.store/# india pharmacy
https://mexicoph24.life/# mexico pharmacy
http://mexicoph24.life/# buying prescription drugs in mexico
http://mexicoph24.life/# mexico pharmacy
https://indiaph24.store/# online pharmacy india
https://indiaph24.store/# india pharmacy mail order
https://mexicoph24.life/# mexico pharmacies prescription drugs
http://indiaph24.store/# reputable indian pharmacies
https://mexicoph24.life/# mexican rx online
india pharmacy mail order http://indiaph24.store/# best online pharmacy india
reputable indian online pharmacy
http://indiaph24.store/# top 10 pharmacies in india
india pharmacy mail order https://indiaph24.store/# indianpharmacy com
best online pharmacy india
http://mexicoph24.life/# reputable mexican pharmacies online
mexican pharmaceuticals online: mexico drug stores pharmacies – mexican pharmacy
mexico drug stores pharmacies cheapest mexico drugs reputable mexican pharmacies online
cheap canadian pharmacy online canadian pharmacies canadian pharmacy price checker
http://canadaph24.pro/# canadian drugs
http://mexicoph24.life/# mexican mail order pharmacies
purple pharmacy mexico price list: mexican pharmacy – mexico pharmacies prescription drugs
http://nolvadex.life/# tamoxifen vs raloxifene
tamoxifen depression: nolvadex pills – tamoxifen hormone therapy
https://ciprofloxacin.tech/# cipro ciprofloxacin
Cytotec 200mcg price: order cytotec online – cytotec pills buy online
https://finasteride.store/# cost of propecia price
buy generic ciprofloxacin buy generic ciprofloxacin ciprofloxacin generic price
buy generic ciprofloxacin cipro for sale buy cipro online without prescription
http://ciprofloxacin.tech/# cipro 500mg best prices
buy cipro online canada: cipro online no prescription in the usa – ciprofloxacin generic price
buy cytotec over the counter Abortion pills online buy cytotec pills
nolvadex side effects: tamoxifen alternatives – tamoxifen medication
https://lisinopril.network/# prinivil drug
http://finasteride.store/# generic propecia pills
ciprofloxacin generic cipro online no prescription in the usa buy cipro
aromatase inhibitors tamoxifen: tamoxifen side effects forum – nolvadex only pct
where can i buy cipro online cipro for sale cipro 500mg best prices
http://finasteride.store/# cost cheap propecia no prescription
http://ciprofloxacin.tech/# cipro pharmacy
discount zestril: zestril 10 mg price in india – lisinopril 40 mg no prescription
https://ciprofloxacin.tech/# ciprofloxacin mail online
https://ciprofloxacin.tech/# п»їcipro generic
Misoprostol 200 mg buy online cytotec pills buy online buy cytotec over the counter
nolvadex estrogen blocker: should i take tamoxifen – tamoxifen reviews
https://finasteride.store/# cost propecia without rx
lisinopril 80mg price of lisinopril in india zestril 20 mg tablet
http://lisinopril.network/# lisinopril 30mg coupon
buy ciprofloxacin antibiotics cipro buy cipro cheap
tamoxifen and osteoporosis: common side effects of tamoxifen – generic tamoxifen
http://lisinopril.network/# zestril 10
http://ciprofloxacin.tech/# ciprofloxacin generic
ciprofloxacin over the counter: cipro – buy ciprofloxacin over the counter
order cytotec online buy cytotec in usa Misoprostol 200 mg buy online
https://ciprofloxacin.tech/# antibiotics cipro
natural alternatives to tamoxifen tamoxifen moa what happens when you stop taking tamoxifen
https://finasteride.store/# buying cheap propecia without insurance
lisinopril brand name in india: zestoretic online – can i buy lisinopril in mexico
http://ciprofloxacin.tech/# buy ciprofloxacin
alternative to tamoxifen tamoxifen and depression what happens when you stop taking tamoxifen
Cytotec 200mcg price: cytotec buy online usa – buy cytotec over the counter
https://nolvadex.life/# alternative to tamoxifen
tamoxifen menopause: how to lose weight on tamoxifen – tamoxifen hip pain
lisinopril 5 mg tablet price in india lisinopril 40 mg for sale lisinopril cost us
https://cytotec.club/# buy cytotec pills online cheap
cytotec abortion pill purchase cytotec buy cytotec over the counter
cipro 500mg best prices: cipro generic – ciprofloxacin
https://ciprofloxacin.tech/# buy ciprofloxacin
https://ciprofloxacin.tech/# buy cipro online canada
https://cytotec.club/# buy cytotec pills online cheap
cost of prinivil lisinopril 2.5 mg prinivil 20mg tabs
lisinopril 20mg online: http://lisinoprilpharm.com/%5Dlisinopril – lisinopril 12.5 mg
how to order lisinopril online lisinopril 40 coupon cheapest lisinopril 10 mg
http://lisinopril.network/# 2 lisinopril
purchase cytotec: Misoprostol 200 mg buy online – cytotec buy online usa
https://ciprofloxacin.tech/# ciprofloxacin 500mg buy online
cytotec buy online usa buy misoprostol over the counter purchase cytotec
cytotec online: buy cytotec online – buy cytotec over the counter
https://cytotec.club/# buy cytotec online fast delivery
Misoprostol 200 mg buy online: Cytotec 200mcg price – order cytotec online
https://cytotec.club/# buy cytotec in usa
buy cytotec pills online cheap cytotec abortion pill order cytotec online
http://finasteride.store/# buy propecia without dr prescription
ciprofloxacin order online: cipro for sale – ciprofloxacin generic price
http://ciprofloxacin.tech/# ciprofloxacin
http://nolvadex.life/# tamoxifen
tamoxifen bone density: tamoxifen and ovarian cancer – tamoxifen moa
buy cipro cipro online no prescription in the usa п»їcipro generic
https://nolvadex.life/# tamoxifen
ciprofloxacin mail online buy cipro online without prescription buy cipro online canada
tamoxifen: tamoxifen buy – tamoxifen blood clots
http://nolvadex.life/# hysterectomy after breast cancer tamoxifen
raloxifene vs tamoxifen nolvadex during cycle tamoxifen citrate
does tamoxifen cause weight loss natural alternatives to tamoxifen nolvadex 10mg
cheap kamagra: buy kamagra online – Kamagra 100mg
https://viagras.online/# over the counter sildenafil
Buy Cenforce 100mg Online: Purchase Cenforce Online – Cenforce 100mg tablets for sale
https://levitrav.store/# Levitra 20 mg for sale
Generic Cialis without a doctor prescription: Generic Cialis without a doctor prescription – cheapest cialis
https://viagras.online/# Sildenafil 100mg price
buy cialis online overnight delivery
best price for viagra 100mg Buy generic 100mg Viagra online viagra without prescription
sildenafil online Buy Viagra online best price for viagra 100mg
https://levitrav.store/# Vardenafil online prescription
cheapest cenforce: Cenforce 150 mg online – cenforce.pro
Buy Tadalafil 5mg: buy cialis pill – Buy Tadalafil 10mg
Viagra without a doctor prescription Canada: Buy Viagra online cheap – Buy generic 100mg Viagra online
https://kamagra.win/# Kamagra 100mg
Levitra 20 mg for sale Vardenafil online prescription Levitra generic best price
http://kamagra.win/# cheap kamagra
Cheap Levitra online: buy Levitra over the counter – Vardenafil online prescription
cheapest cialis: Generic Cialis without a doctor prescription – Cialis over the counter
Buy Cenforce 100mg Online cheapest cenforce cenforce.pro
Kamagra 100mg: kamagra – kamagra
Buy Viagra online cheap Buy Viagra online cheap Viagra without a doctor prescription Canada
https://viagras.online/# order viagra
http://kamagra.win/# super kamagra
https://cenforce.pro/# buy cenforce
https://kamagra.win/# buy Kamagra
best price for viagra 100mg: Buy Viagra online cheap – Viagra tablet online
super kamagra kamagra.win Kamagra 100mg
super kamagra kamagra pills sildenafil oral jelly 100mg kamagra
buy cenforce: Cenforce 150 mg online – Cenforce 150 mg online
Buy generic 100mg Viagra online: viagras.online – sildenafil online
http://viagras.online/# viagra without prescription
http://cialist.pro/# п»їcialis generic
cenforce for sale Purchase Cenforce Online cenforce for sale
cialis generic: Cialis 20mg price in USA – Buy Tadalafil 10mg
Buy Cenforce 100mg Online cenforce for sale Cenforce 150 mg online
Kamagra 100mg: kamagra – Kamagra 100mg price
best price for viagra 100mg: Cheapest Sildenafil online – order viagra
https://cenforce.pro/# cheapest cenforce
sildenafil over the counter Generic Viagra for sale order viagra
http://cialist.pro/# Tadalafil Tablet
Cenforce 150 mg online Buy Cenforce 100mg Online order cenforce
Cheap generic Viagra online: Buy generic 100mg Viagra online – Cheap generic Viagra online
http://cialist.pro/# Cialis 20mg price in USA
Kamagra 100mg: buy kamagra online – Kamagra tablets
https://cialist.pro/# Cialis 20mg price
http://kamagra.win/# Kamagra 100mg price
cheapest pharmacy prescription drugs: pharm world store – cheapest pharmacy for prescriptions without insurance
best online pharmacy india: buy prescription drugs from india – buy prescription drugs from india
indian pharmacy: buy medicines online in india – indian pharmacy online
http://pharmindia.online/# world pharmacy india
Online medicine home delivery india pharmacy mail order Online medicine order
canada pharmacy not requiring prescription online pharmacy prescription online canadian pharmacy coupon
https://pharmnoprescription.icu/# buy medication online with prescription
non prescription medicine pharmacy: cheapest pharmacy – us pharmacy no prescription
mail order prescription drugs from canada: canadian pharmacy no prescription needed – overseas pharmacy no prescription
mexico online pharmacy prescription drugs no prescription drugs online prescription canada
online pharmacy without prescription: pharm world – canadian online pharmacy no prescription
http://pharmworld.store/# non prescription medicine pharmacy
online pharmacy discount code pharm world canadian pharmacy world coupon code
mexican online pharmacies prescription drugs: mexican online pharmacies prescription drugs – reputable mexican pharmacies online
https://pharmcanada.shop/# best mail order pharmacy canada
uk pharmacy no prescription: online pharmacy – canadian pharmacy coupon
best online pharmacies in mexico mexican drugstore online п»їbest mexican online pharmacies
mexican online pharmacies prescription drugs: mexican online pharmacies prescription drugs – п»їbest mexican online pharmacies
reputable canadian online pharmacy canadian pharmacy prices canadian drugs
pharmacies in mexico that ship to usa: reputable mexican pharmacies online – pharmacies in mexico that ship to usa
http://pharmmexico.online/# mexican rx online
pharmacies in mexico that ship to usa: mexican drugstore online – best online pharmacies in mexico
https://pharmindia.online/# best online pharmacy india
http://pharmmexico.online/# mexican mail order pharmacies
online pharmacy no prescriptions: buying prescription medications online – how to get prescription drugs from canada
world pharmacy india: п»їlegitimate online pharmacies india – online shopping pharmacy india
medicine in mexico pharmacies medication from mexico pharmacy mexican rx online
rx pharmacy no prescription online pharmacy online canadian pharmacy coupon
india online pharmacy: buy medicines online in india – india pharmacy
https://pharmnoprescription.icu/# best online pharmacy without prescription
http://pharmindia.online/# best india pharmacy
pharmacies in canada that ship to the us: buy canadian drugs – canadian neighbor pharmacy
canadian pharmacy coupon code: pharm world – pharmacy online 365 discount code
canadian pharmacy coupon code pharm world store canadian pharmacy without prescription
Online medicine home delivery india pharmacy indianpharmacy com
top 10 online pharmacy in india: top 10 online pharmacy in india – reputable indian pharmacies
https://pharmmexico.online/# mexican border pharmacies shipping to usa
https://pharmcanada.shop/# canadian 24 hour pharmacy
medication online without prescription: medications online without prescription – pills no prescription
non prescription online pharmacy india: medications online without prescription – best website to buy prescription drugs
prescription from canada non prescription online pharmacy no prescription pharmacy online
canadian drug stores: online pharmacy canada – canadian pharmacy no rx needed
http://pharmnoprescription.icu/# can i buy prescription drugs in canada
best canadian online pharmacy canadian pharmacy online canadian pharmacy meds
zithromax 250mg: buy cheap zithromax online – generic zithromax medicine
generic amoxicillin: amoxicillin 500 mg online – amoxicillin 500mg over the counter
http://amoxila.pro/# buy amoxicillin online with paypal
neurontin 100mg tablet: 600 mg neurontin tablets – neurontin 800 mg price
neurontin cost uk: neurontin tablets no script – neurontin 214
neurontin 3 over the counter neurontin neurontin for sale
neurontin 600mg: neurontin 800 mg tablets best price – neurontin 300 mg cap
amoxicillin online pharmacy generic amoxicillin amoxicillin 800 mg price
https://prednisoned.online/# buying prednisone from canada
prednisone 60 mg tablet: prednisone without prescription 10mg – where to buy prednisone without prescription
https://zithromaxa.store/# zithromax cost
amoxicillin medicine over the counter buy amoxicillin 500mg usa amoxicillin 500 mg without prescription
2000 mg neurontin: neurontin tablets 100mg – neurontin 100mg discount
neurontin generic brand: buy neurontin 100 mg – neurontin prescription cost
zithromax online no prescription: zithromax antibiotic – how to get zithromax
ampicillin amoxicillin: buy amoxicillin from canada – amoxicillin 875 125 mg tab
buy zithromax 1000 mg online: zithromax online usa – zithromax capsules price
prednisone 500 mg tablet: prednisone over the counter uk – prednisone 50 mg for sale
neurontin 600 mg pill: neurontin mexico – gabapentin 300
zithromax prescription online: zithromax cost canada – zithromax 250 mg pill
https://gabapentinneurontin.pro/# gabapentin medication
cost of amoxicillin prescription: rexall pharmacy amoxicillin 500mg – amoxicillin 500mg without prescription
daniel, lee tadalafil
https://doxycyclinea.online/# doxycycline hyclate 100 mg cap
order doxycycline online doxycycline without a prescription 200 mg doxycycline
doxycycline prices: buy doxycycline online 270 tabs – cheap doxycycline online
zithromax 250mg zithromax order online uk zithromax canadian pharmacy
buy doxycycline monohydrate: doxycycline tablets – buy doxycycline without prescription uk
how to get zithromax: zithromax for sale cheap – zithromax for sale usa
amoxicillin in india: 875 mg amoxicillin cost – where to buy amoxicillin over the counter
http://gabapentinneurontin.pro/# neurontin 600 mg pill
india buy prednisone online: prednisone brand name india – prednisone buying
https://amoxila.pro/# rexall pharmacy amoxicillin 500mg
zithromax 250 mg australia where can i get zithromax zithromax cost canada
doxycycline 200 mg: odering doxycycline – order doxycycline online
free coupon for cialis
bph treatment cialis
where to get doxycycline: doxycycline 100mg tablets – doxycycline prices
https://zithromaxa.store/# zithromax online pharmacy canada
doxycycline pills: buy doxycycline hyclate 100mg without a rx – doxycycline 500mg
generic prednisone for sale prednisone 20mg price in india generic over the counter prednisone
http://prednisoned.online/# prednisone cost 10mg
where to buy zithromax in canada zithromax online usa no prescription zithromax price south africa
zithromax antibiotic: where can i get zithromax over the counter – zithromax buy online
http://amoxila.pro/# amoxicillin online no prescription
buy doxycycline hyclate 100mg without a rx: doxycycline 100mg price – buy doxycycline 100mg
zithromax price south africa: zithromax tablets for sale – buy generic zithromax no prescription
prednisone 10mg prednisone 200 mg tablets buy prednisone online india
generic doxycycline: buy doxycycline monohydrate – doxycycline tablets
http://zithromaxa.store/# how much is zithromax 250 mg
buy doxycycline for dogs: doxycycline prices – doxycycline 100 mg
zithromax 500mg: zithromax price south africa – how much is zithromax 250 mg
https://amoxila.pro/# where can i get amoxicillin
buy amoxicillin 500mg online: amoxicillin script – buy amoxicillin 500mg
amoxicillin 30 capsules price amoxicillin 500 mg for sale how much is amoxicillin prescription
doxycycline generic order doxycycline 100mg without prescription doxycycline tetracycline
http://zithromaxa.store/# generic zithromax medicine
canada neurontin 100mg lowest price: prescription medication neurontin – neurontin online usa
can you buy amoxicillin over the counter: amoxicillin in india – buy cheap amoxicillin
amoxicillin 250 mg: cost of amoxicillin 875 mg – purchase amoxicillin online without prescription
http://doxycyclinea.online/# doxycycline generic
where to buy prednisone 20mg can you buy prednisone over the counter in mexico prednisone 250 mg
doxycycline vibramycin doxy 200 cheap doxycycline online
http://amoxila.pro/# can you buy amoxicillin over the counter canada
50 mg prednisone tablet: 5mg prednisone – prednisone rx coupon
amoxicillin 500 mg brand name: amoxicillin 50 mg tablets – amoxicillin 500mg prescription
otc prednisone cream: prednisone for cheap – average cost of prednisone
purchase doxycycline online: buy doxycycline for dogs – buy cheap doxycycline
http://gabapentinneurontin.pro/# neurontin price uk
purchase amoxicillin 500 mg amoxicillin 500mg buy amoxicillin 250mg
neurontin capsules 300mg: neurontin 100 mg – 2000 mg neurontin
where to get doxycycline buy doxycycline online without prescription generic doxycycline
https://doxycyclinea.online/# cheap doxycycline online
neurontin 600: neurontin cost generic – neurontin tablets 300mg
can you buy zithromax online: can you buy zithromax over the counter in australia – zithromax antibiotic
https://zithromaxa.store/# zithromax 250mg
order neurontin online: neurontin 800 mg – cost of neurontin 100mg
order zithromax without prescription zithromax 500 mg lowest price pharmacy online zithromax drug
neurontin 300 mg capsule medication neurontin neurontin coupon
http://prednisoned.online/# buy prednisone online without a script
amoxicillin in india: amoxicillin 500mg tablets price in india – amoxicillin medicine
order amoxicillin uk: amoxicillin 250 mg price in india – buy amoxicillin 250mg
http://amoxila.pro/# amoxicillin 875 125 mg tab
zithromax over the counter uk zithromax without prescription zithromax prescription in canada
neurontin capsule 400 mg neurontin tablets neurontin medicine
https://doxycyclinea.online/# doxycycline without prescription
buy prednisone no prescription: where can you buy prednisone – prednisone 20mg tablets where to buy
how to buy amoxicillin online: buy cheap amoxicillin online – amoxicillin 500mg
buy doxycycline: doxycycline without prescription – doxycycline generic
amoxicillin 500mg: amoxicillin 500mg over the counter – generic amoxil 500 mg
zithromax coupon: zithromax 1000 mg pills – zithromax 500mg
https://amoxila.pro/# amoxicillin canada price
doxycycline 100mg dogs generic doxycycline doxycycline monohydrate
order doxycycline online order doxycycline online how to buy doxycycline online
https://doxycyclinea.online/# doxycycline pills
prednisone oral: buy prednisone online paypal – 20 mg prednisone
buy zithromax 1000 mg online: zithromax over the counter canada – buy zithromax canada
prednisone 50 mg coupon: canine prednisone 5mg no prescription – prednisone online sale
https://doxycyclinea.online/# doxycycline
neurontin 100mg discount neurontin capsules 300mg neurontin 100mg tablet
cheap prednisone 20 mg canine prednisone 5mg no prescription prednisone without rx
http://doxycyclinea.online/# buy doxycycline without prescription uk
pharmacy xenical india
neurontin 100mg price: neurontin tablets 300mg – drug neurontin 200 mg
buy amoxicillin online mexico: amoxicillin 500mg without prescription – amoxicillin 500 mg capsule
6 prednisone: prednisone online paypal – 50mg prednisone tablet
canada pharmacy prednisone: over the counter prednisone pills – prednisone online sale
prednisone for sale online order prednisone online no prescription where can i buy prednisone without prescription
http://gabapentinneurontin.pro/# gabapentin 600 mg
neurontin prices generic: neurontin rx – neurontin pills for sale
where can i buy amoxicillin without prec where can you get amoxicillin 875 mg amoxicillin cost
https://prednisoned.online/# buy prednisone online fast shipping
prednisone 10mg: order prednisone on line – prednisone 50mg cost
doxycycline hyc 100mg: where to get doxycycline – buy doxycycline hyclate 100mg without a rx
order doxycycline 100mg without prescription: doxylin – doxy
amoxicillin capsule 500mg price amoxicillin medicine over the counter amoxicillin 500mg price in canada
http://doxycyclinea.online/# doxycycline order online
where to buy prednisone 20mg prednisone for sale in canada how can i get prednisone online without a prescription
http://zithromaxa.store/# zithromax 250 mg
prednisone over the counter: prednisone cream rx – 60 mg prednisone daily
prednisone for dogs prednisone 10mg tablet cost buy prednisone online australia
prednisone medicine: prednisone canada prescription – prednisone 4 mg daily
neurontin price: price of neurontin – cost of neurontin
doxycycline order online doxycycline without prescription buy doxycycline without prescription uk
buying prescription drugs in mexico online: mexican border pharmacies shipping to usa – buying prescription drugs in mexico
http://mexicanpharmacy1st.com/# mexican pharmaceuticals online
mexican pharmaceuticals online: mexican border pharmacies shipping to usa – mexican border pharmacies shipping to usa
best mexican online pharmacies: mexican drugstore online – medicine in mexico pharmacies
https://mexicanpharmacy1st.shop/# mexican mail order pharmacies
mexican pharmaceuticals online mexico pharmacy best online pharmacies in mexico
http://mexicanpharmacy1st.com/# mexican pharmacy
medication from mexico pharmacy reputable mexican pharmacies online best online pharmacies in mexico
purple pharmacy mexico price list: mexican pharmaceuticals online – medication from mexico pharmacy
mexico drug stores pharmacies: buying prescription drugs in mexico online – medicine in mexico pharmacies
mexican mail order pharmacies: best online pharmacies in mexico – mexico pharmacy
https://mexicanpharmacy1st.com/# mexico drug stores pharmacies
mexican rx online: mexico pharmacies prescription drugs – buying from online mexican pharmacy
п»їbest mexican online pharmacies mexican border pharmacies shipping to usa pharmacies in mexico that ship to usa
purple pharmacy mexico price list: mexico drug stores pharmacies – mexican pharmaceuticals online
reputable mexican pharmacies online: mexican drugstore online – mexican pharmaceuticals online
buying prescription drugs in mexico: medication from mexico pharmacy – mexican pharmacy
https://mexicanpharmacy1st.shop/# medication from mexico pharmacy
https://mexicanpharmacy1st.shop/# mexican drugstore online
mexico pharmacy mexico drug stores pharmacies mexican border pharmacies shipping to usa
https://mexicanpharmacy1st.com/# mexican pharmacy
https://mexicanpharmacy1st.shop/# buying prescription drugs in mexico
mexico pharmacies prescription drugs mexican online pharmacies prescription drugs mexican drugstore online
buying prescription drugs in mexico: mexican drugstore online – medication from mexico pharmacy
mexican border pharmacies shipping to usa: п»їbest mexican online pharmacies – mexico drug stores pharmacies
http://mexicanpharmacy1st.com/# mexican mail order pharmacies
mexico pharmacy mexican rx online mexico drug stores pharmacies
http://mexicanpharmacy1st.com/# mexico pharmacy
pharmacies in mexico that ship to usa buying prescription drugs in mexico mexico drug stores pharmacies
mexican pharmaceuticals online: mexican online pharmacies prescription drugs – mexican pharmacy
purple pharmacy mexico price list: reputable mexican pharmacies online – medication from mexico pharmacy
http://mexicanpharmacy1st.com/# medicine in mexico pharmacies
purple pharmacy mexico price list reputable mexican pharmacies online mexican border pharmacies shipping to usa
mexico pharmacies prescription drugs: mexican mail order pharmacies – medicine in mexico pharmacies
purple pharmacy mexico price list mexico drug stores pharmacies mexican online pharmacies prescription drugs
medication from mexico pharmacy: mexico pharmacies prescription drugs – best online pharmacies in mexico
http://mexicanpharmacy1st.com/# medicine in mexico pharmacies
mexico drug stores pharmacies: medication from mexico pharmacy – buying prescription drugs in mexico
http://mexicanpharmacy1st.com/# buying prescription drugs in mexico
https://mexicanpharmacy1st.com/# mexican rx online
https://mexicanpharmacy1st.com/# mexican drugstore online
mexican rx online: mexican rx online – mexican mail order pharmacies
medication from mexico pharmacy medicine in mexico pharmacies mexican mail order pharmacies
medicine in mexico pharmacies: mexican mail order pharmacies – mexican pharmaceuticals online
buying prescription drugs in mexico online: buying prescription drugs in mexico online – medication from mexico pharmacy
mexico drug stores pharmacies: medicine in mexico pharmacies – mexico drug stores pharmacies
https://mexicanpharmacy1st.com/# buying from online mexican pharmacy
mexico pharmacies prescription drugs: buying prescription drugs in mexico – mexican border pharmacies shipping to usa
pharmacies in mexico that ship to usa pharmacies in mexico that ship to usa mexican rx online
https://mexicanpharmacy1st.com/# buying prescription drugs in mexico
mexican drugstore online: best online pharmacies in mexico – mexico drug stores pharmacies
https://mexicanpharmacy1st.com/# mexican mail order pharmacies
mexican pharmaceuticals online: buying from online mexican pharmacy – mexican rx online
mexican mail order pharmacies medicine in mexico pharmacies mexican border pharmacies shipping to usa
buying prescription drugs in mexico purple pharmacy mexico price list п»їbest mexican online pharmacies
http://mexicanpharmacy1st.com/# mexican rx online
medication from mexico pharmacy: mexico drug stores pharmacies – mexican rx online
https://mexicanpharmacy1st.online/# medicine in mexico pharmacies
http://clomiphene.shop/# how to buy clomid no prescription
https://gabapentin.club/# neurontin tablets uk
where to buy clomid: can you get clomid price – get cheap clomid no prescription
п»їcytotec pills online order cytotec online order cytotec online
neurontin 800 mg cost: neurontin 800 mg tablet – drug neurontin 20 mg
neurontin 100mg cost: order neurontin over the counter – neurontin generic cost
buying propecia pill buying generic propecia online order cheap propecia prices
http://gabapentin.club/# ordering neurontin online
Misoprostol 200 mg buy online: buy cytotec online – purchase cytotec
https://clomiphene.shop/# can i order clomid online
cost of generic clomid price can you buy generic clomid without insurance where can i buy cheap clomid without a prescription
lisinopril medication otc: lisinopril cost uk – drug lisinopril 5 mg
https://lisinopril.club/# lisinopril 10 12.55mg
medicine neurontin 300 mg: neurontin medication – neurontin price comparison
order cheap clomid without prescription can i order generic clomid can i get clomid without rx
https://cytotec.xyz/# cytotec abortion pill
cytotec abortion pill: cytotec abortion pill – buy cytotec pills
buy misoprostol over the counter buy cytotec pills buy misoprostol over the counter
https://cytotec.xyz/# cytotec pills buy online
buy cheap clomid price: where to get clomid now – can you get clomid without a prescription
cost of cheap propecia pill generic propecia price cost of cheap propecia price
https://gabapentin.club/# buy gabapentin
buy cytotec online fast delivery: buy cytotec online – buy cytotec online fast delivery
get cheap propecia without dr prescription: buy cheap propecia pill – buying propecia for sale
buy cytotec pills buy cytotec online buy cytotec over the counter
http://lisinopril.club/# lisinopril 20mg 37.5mg
http://gabapentin.club/# generic gabapentin
https://lisinopril.club/# lisinopril 1 mg
cytotec pills buy online: buy cytotec in usa – cytotec buy online usa
brand neurontin 100 mg canada: neurontin 300 mg cap – neurontin mexico
http://cytotec.xyz/# cytotec buy online usa
cost cheap propecia without insurance buy propecia online buying propecia without a prescription
cost of neurontin: prescription drug neurontin – medicine neurontin
generic clomid tablets how to get generic clomid without dr prescription cost generic clomid for sale
https://cytotec.xyz/# buy cytotec online fast delivery
buy cytotec over the counter: buy cytotec over the counter – cytotec pills buy online
http://cytotec.xyz/# buy misoprostol over the counter
buy cytotec online buy misoprostol over the counter cytotec buy online usa
cheap propecia pills: cost of generic propecia tablets – buying generic propecia tablets
http://clomiphene.shop/# can i order generic clomid for sale
neurontin 300 mg price in india: neurontin capsules 600mg – buy neurontin
buy cheap propecia tablets cost of cheap propecia without a prescription cost of propecia pill
buying generic propecia for sale buy propecia price order generic propecia without rx
https://propeciaf.online/# cheap propecia tablets
buy cheap propecia pills: cost propecia without rx – buying generic propecia
http://lisinopril.club/# lisinopril online canadian pharmacy
lisinopril metoprolol: lisinopril 2.5 mg tablet – lisinopril 10 mg on line prescription
buying generic clomid without dr prescription buying cheap clomid without insurance where can i get clomid without prescription
buy cytotec over the counter buy cytotec over the counter purchase cytotec
neurontin 100mg capsule price: buy generic neurontin – neurontin sale
cheap propecia pill: propecia order – get propecia
lisinopril 10 mg online lisinopril brand name zestoretic 20 12.5
neurontin cap: drug neurontin – drug neurontin 20 mg
best online pharmacies in mexico mexico pharmacy best online pharmacies in mexico
https://36and6health.shop/# drugstore com online pharmacy prescription drugs
https://cheapestindia.shop/# top online pharmacy india
https://36and6health.com/# canadian pharmacy world coupon code
online pharmacy with prescription: buying prescription drugs in india – buying prescription drugs online from canada
https://cheapestcanada.com/# canada drugs online review
http://cheapestmexico.com/# medicine in mexico pharmacies
п»їbest mexican online pharmacies: purple pharmacy mexico price list – purple pharmacy mexico price list
https://cheapestmexico.com/# mexican mail order pharmacies
indian pharmacies safe п»їlegitimate online pharmacies india cheapest online pharmacy india
prescription online canada cheapest & fast pharmacy canadian pharmacy prescription
https://36and6health.com/# pharmacy discount coupons
http://cheapestmexico.com/# mexico drug stores pharmacies
https://cheapestmexico.com/# best mexican online pharmacies
https://cheapestindia.com/# Online medicine order
https://cheapestcanada.shop/# canada ed drugs
https://cheapestindia.shop/# indian pharmacies safe
buy prescription drugs from canada cheap: certified canadian pharmacy – reputable canadian pharmacy
mexico pharmacy mexican pharmaceuticals online best online pharmacies in mexico
http://cheapestindia.com/# pharmacy website india
buy medicines online in india india online pharmacy online pharmacy india
my canadian pharmacy: cheapest canada – canadian pharmacy com
http://36and6health.com/# best no prescription pharmacy
http://36and6health.com/# cheapest pharmacy to get prescriptions filled
https://cheapestcanada.shop/# canadapharmacyonline
https://36and6health.com/# prescription drugs online
http://cheapestandfast.com/# mexico prescription drugs online
https://36and6health.shop/# canadian pharmacy no prescription needed
https://cheapestindia.shop/# Online medicine home delivery
https://cheapestcanada.shop/# canadian pharmacies compare
http://36and6health.com/# non prescription medicine pharmacy
world pharmacy india best india pharmacy india online pharmacy
legal online pharmacy coupon code: cheapest pharmacy – canadian pharmacy no prescription needed
http://cheapestcanada.com/# northwest canadian pharmacy
https://36and6health.shop/# cheapest pharmacy for prescriptions without insurance
farmacia online madrid: farmacia online españa envÃo internacional – farmacias online seguras en españa
comprare farmaci online con ricetta: Farmacie on line spedizione gratuita – acquisto farmaci con ricetta
farmacie online autorizzate elenco Farmacia online miglior prezzo acquistare farmaci senza ricetta
https://euapothekeohnerezept.com/# medikamente rezeptfrei
Pharmacie sans ordonnance: trouver un mГ©dicament en pharmacie – pharmacie en ligne france pas cher
pharmacie en ligne france fiable Achat mГ©dicament en ligne fiable pharmacie en ligne
apotheke online: internet apotheke – europa apotheke
online apotheke: beste online-apotheke ohne rezept – online apotheke preisvergleich
farmacia online barata: farmacia online envÃo gratis – farmacias direct
apotheke online: ohne rezept apotheke – apotheke online
pharmacie en ligne france livraison belgique: pharmacies en ligne certifiГ©es – trouver un mГ©dicament en pharmacie
apotheke online online apotheke rezept beste online-apotheke ohne rezept
farmacia online barcelona: farmacia online barcelona – farmacias online seguras
https://euapothekeohnerezept.shop/# eu apotheke ohne rezept
п»їshop apotheke gutschein online apotheke gГјnstig gГјnstigste online apotheke
pharmacie en ligne livraison europe: Achat mГ©dicament en ligne fiable – Pharmacie Internationale en ligne
Pharmacie sans ordonnance: vente de m̩dicament en ligne Рpharmacie en ligne sans ordonnance
pharmacie en ligne france livraison internationale: pharmacie en ligne france pas cher – pharmacie en ligne sans ordonnance
farmacia online barata: farmacias online baratas – farmacia online 24 horas
farmacias direct farmacia online barata farmacia online madrid
internet apotheke: gГјnstige online apotheke – apotheke online
farmacias online baratas farmacias online seguras en espaГ±a farmacia online madrid
farmacias online seguras en espa̱a: farmacia online 24 horas Рfarmacia barata
ohne rezept apotheke: п»їshop apotheke gutschein – ohne rezept apotheke
farmacias online seguras: farmacia online barcelona – farmacia online barata y fiable
comprare farmaci online con ricetta Farmacia online miglior prezzo migliori farmacie online 2024
farmacia online barcelona: farmacia online envГo gratis – farmacia en casa online descuento
farmacia online piГ№ conveniente п»їFarmacia online migliore farmaci senza ricetta elenco
farmacia online senza ricetta: Farmacie online sicure – farmacia online più conveniente
top farmacia online: Farmacie online sicure – farmacia online piГ№ conveniente
farmacias online seguras: farmacia barata – farmacias direct
farmacie online sicure: Farmacia online migliore – acquistare farmaci senza ricetta
http://euapothekeohnerezept.com/# europa apotheke
acquisto farmaci con ricetta farmacia online farmacie online autorizzate elenco
medikament ohne rezept notfall: internet apotheke – gГјnstigste online apotheke
acquisto farmaci con ricetta: comprare farmaci online all’estero – farmacia online
pharmacie en ligne livraison europe pharmacie en ligne pas cher pharmacie en ligne pas cher
farmacias online seguras: farmacia online madrid – farmacia online envÃo gratis
pharmacie en ligne fiable: pharmacie en ligne sans ordonnance – pharmacie en ligne avec ordonnance
farmacie online affidabili: Farmacie on line spedizione gratuita – Farmacia online migliore
pharmacie en ligne france livraison belgique: pharmacie en ligne livraison europe – trouver un mГ©dicament en pharmacie
pharmacie en ligne france livraison internationale pharmacie en ligne france fiable trouver un mГ©dicament en pharmacie
https://eufarmaciaonline.shop/# farmacia online madrid
farmacia online barcelona farmacia online madrid farmacia online barcelona
Farmacia online miglior prezzo: farmacia online piГ№ conveniente – Farmacia online miglior prezzo
internet apotheke: günstigste online apotheke – europa apotheke
farmacia online espaГ±a envГo internacional: farmacia online 24 horas – farmacia online madrid
medikament ohne rezept notfall: europa apotheke – ohne rezept apotheke
п»їFarmacia online migliore: farmacia online piГ№ conveniente – Farmacie online sicure
pharmacie en ligne pharmacie en ligne avec ordonnance pharmacie en ligne
pharmacie en ligne avec ordonnance Pharmacie Internationale en ligne pharmacies en ligne certifiГ©es
farmacias online seguras en espaГ±a: farmacias online seguras – farmacia barata
pharmacie en ligne sans ordonnance: Pharmacie sans ordonnance – pharmacie en ligne sans ordonnance
https://eumedicamentenligne.shop/# pharmacie en ligne france fiable
medikamente rezeptfrei: gГјnstigste online apotheke – apotheke online
farmacia online españa envÃo internacional: farmacias online seguras – farmacia online barata
online apotheke rezept medikamente rezeptfrei medikamente rezeptfrei
farmacie online autorizzate elenco: comprare farmaci online con ricetta – acquisto farmaci con ricetta
vente de mГ©dicament en ligne pharmacie en ligne sans ordonnance acheter mГ©dicament en ligne sans ordonnance
farmacias direct: farmacias direct – п»їfarmacia online espaГ±a
farmacie online affidabili: п»їFarmacia online migliore – farmacia online piГ№ conveniente
farmacias online seguras: farmacias direct – farmacia online barata y fiable
http://eumedicamentenligne.com/# pharmacie en ligne france livraison internationale
ohne rezept apotheke ohne rezept apotheke apotheke online
apotheke online: internet apotheke – online apotheke rezept
beste online-apotheke ohne rezept: internet apotheke – п»їshop apotheke gutschein
farmacias online seguras: farmacia en casa online descuento – farmacias online seguras
pharmacie en ligne france livraison internationale: pharmacie en ligne france – pharmacie en ligne avec ordonnance
farmacias online seguras farmacia online envГo gratis farmacia online madrid
online apotheke versandkostenfrei: beste online-apotheke ohne rezept – medikamente rezeptfrei
online apotheke rezept: europa apotheke – eu apotheke ohne rezept
http://eufarmaciaonline.com/# farmacias online baratas
http://phenligne.com/# pharmacie en ligne france livraison belgique
Achat mГ©dicament en ligne fiable: pharmacie en ligne sans ordonnance – Pharmacie en ligne livraison Europe
pharmacie en ligne france livraison internationale: pharmacie en ligne sans ordonnance – pharmacie en ligne pas cher
п»їpharmacie en ligne france Pharmacie en ligne livraison Europe acheter mГ©dicament en ligne sans ordonnance
pharmacies en ligne certifiГ©es: kamagra en ligne – trouver un mГ©dicament en pharmacie
pharmacie en ligne livraison europe: Levitra 20mg prix en pharmacie – vente de mГ©dicament en ligne
http://kamagraenligne.com/# pharmacie en ligne france
pharmacie en ligne fiable: Medicaments en ligne livres en 24h – pharmacie en ligne avec ordonnance
acheter mГ©dicament en ligne sans ordonnance: Levitra sans ordonnance 24h – pharmacie en ligne fiable
Viagra vente libre pays: Viagra generique en pharmacie – Quand une femme prend du Viagra homme
SildГ©nafil Teva 100 mg acheter: Prix du Viagra en pharmacie en France – Quand une femme prend du Viagra homme
Achat mГ©dicament en ligne fiable: pharmacie en ligne sans ordonnance – trouver un mГ©dicament en pharmacie
Pharmacie Internationale en ligne Acheter Cialis 20 mg pas cher pharmacies en ligne certifiГ©es
pharmacie en ligne livraison europe: Pharmacie sans ordonnance – pharmacie en ligne avec ordonnance
п»їpharmacie en ligne france: Medicaments en ligne livres en 24h – п»їpharmacie en ligne france
pharmacie en ligne pas cher: pharmacie en ligne – Pharmacie Internationale en ligne
vente de mГ©dicament en ligne: cialis generique – acheter mГ©dicament en ligne sans ordonnance
Hello!
This post was created with XRumer 23 StrongAI.
Good luck 🙂
Hello.
This post was created with XRumer 23 StrongAI.
Good luck 🙂
pharmacie en ligne france livraison belgique: kamagra pas cher – pharmacie en ligne france livraison belgique
Viagra sans ordonnance pharmacie France: Viagra prix pharmacie paris – Viagra gГ©nГ©rique pas cher livraison rapide
https://kamagraenligne.com/# pharmacie en ligne france
Viagra homme prix en pharmacie sans ordonnance: Viagra sans ordonnance 24h Amazon – Viagra pas cher livraison rapide france
pharmacie en ligne: levitra en ligne – Pharmacie en ligne livraison Europe
pharmacie en ligne fiable: Achat mГ©dicament en ligne fiable – pharmacies en ligne certifiГ©es
pharmacie en ligne france fiable: pharmacies en ligne certifiГ©es – pharmacies en ligne certifiГ©es
Sildenafil teva 100 mg sans ordonnance: Viagra generique en pharmacie – Le gГ©nГ©rique de Viagra
Pharmacie sans ordonnance: levitra generique prix en pharmacie – pharmacie en ligne sans ordonnance
Viagra 100 mg sans ordonnance: Viagra sans ordonnance 24h – Viagra 100 mg sans ordonnance
Viagra 100 mg sans ordonnance: Acheter du Viagra sans ordonnance – Viagra homme sans prescription
acheter mГ©dicament en ligne sans ordonnance: kamagra pas cher – pharmacie en ligne avec ordonnance
pharmacie en ligne avec ordonnance: Medicaments en ligne livres en 24h – Pharmacie sans ordonnance
pharmacie en ligne france livraison internationale: levitra generique sites surs – pharmacie en ligne fiable
pharmacie en ligne avec ordonnance: Medicaments en ligne livres en 24h – acheter mГ©dicament en ligne sans ordonnance
п»їpharmacie en ligne france: pharmacie en ligne pas cher – acheter mГ©dicament en ligne sans ordonnance
acheter mГ©dicament en ligne sans ordonnance: kamagra oral jelly – п»їpharmacie en ligne france
Meilleur Viagra sans ordonnance 24h: Viagra generique en pharmacie – Viagra sans ordonnance 24h suisse
Prix du Viagra 100mg en France: viagra en ligne – Viagra homme prix en pharmacie sans ordonnance
pharmacie en ligne livraison europe: pharmacie en ligne sans ordonnance – pharmacie en ligne sans ordonnance
Pharmacie Internationale en ligne: pharmacie en ligne sans ordonnance – Pharmacie Internationale en ligne
Pharmacie sans ordonnance: levitra generique prix en pharmacie – Pharmacie sans ordonnance
Achat mГ©dicament en ligne fiable: Pharmacies en ligne certifiees – Achat mГ©dicament en ligne fiable
п»їpharmacie en ligne france: cialis generique – acheter mГ©dicament en ligne sans ordonnance
pharmacie en ligne sans ordonnance: Levitra pharmacie en ligne – pharmacie en ligne sans ordonnance
п»їpharmacie en ligne france: Levitra 20mg prix en pharmacie – trouver un mГ©dicament en pharmacie
acheter mГ©dicament en ligne sans ordonnance: Medicaments en ligne livres en 24h – pharmacie en ligne france livraison internationale
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Achat mГ©dicament en ligne fiable: cialis generique – vente de mГ©dicament en ligne
trouver un mГ©dicament en pharmacie: Pharmacies en ligne certifiees – vente de mГ©dicament en ligne
Viagra homme prix en pharmacie: Acheter du Viagra sans ordonnance – Prix du Viagra 100mg en France
Pharmacie en ligne livraison Europe: kamagra en ligne – pharmacie en ligne avec ordonnance
pharmacie en ligne avec ordonnance: cialis sans ordonnance – pharmacie en ligne france pas cher
pharmacie en ligne avec ordonnance: cialis prix – Achat mГ©dicament en ligne fiable
п»їpharmacie en ligne france: vente de mГ©dicament en ligne – pharmacie en ligne france livraison belgique
pharmacie en ligne fiable: levitra en ligne – pharmacie en ligne france pas cher
pharmacie en ligne france pas cher: Medicaments en ligne livres en 24h – vente de mГ©dicament en ligne
Viagra vente libre allemagne: Meilleur Viagra sans ordonnance 24h – Viagra prix pharmacie paris
п»їpharmacie en ligne france: pharmacie en ligne sans ordonnance – pharmacie en ligne
vente de mГ©dicament en ligne: levitra generique prix en pharmacie – pharmacie en ligne avec ordonnance
Viagra gГ©nГ©rique pas cher livraison rapide: viagra en ligne – Meilleur Viagra sans ordonnance 24h
Pharmacie en ligne livraison Europe: kamagra gel – pharmacie en ligne france livraison belgique
pharmacies en ligne certifiГ©es: levitra en ligne – pharmacie en ligne
pharmacie en ligne france livraison belgique: kamagra livraison 24h – pharmacie en ligne france fiable
pharmacie en ligne livraison europe: vente de mГ©dicament en ligne – Pharmacie sans ordonnance
pharmacie en ligne france livraison belgique: Levitra acheter – pharmacie en ligne france livraison internationale
pharmacie en ligne france livraison belgique: levitra generique – pharmacie en ligne france livraison belgique
pharmacie en ligne france livraison internationale: Cialis sans ordonnance 24h – pharmacie en ligne france fiable
п»їpharmacie en ligne france: Levitra sans ordonnance 24h – acheter mГ©dicament en ligne sans ordonnance
п»їpharmacie en ligne france: cialis prix – pharmacie en ligne france fiable
pharmacie en ligne france livraison internationale: pharmacie en ligne sans ordonnance – pharmacie en ligne france livraison belgique
trouver un mГ©dicament en pharmacie: achat kamagra – pharmacie en ligne fiable
pharmacie en ligne fiable: pharmacie en ligne avec ordonnance – п»їpharmacie en ligne france
pharmacie en ligne avec ordonnance: cialis generique – vente de mГ©dicament en ligne
pharmacie en ligne france fiable: Cialis sans ordonnance 24h – pharmacie en ligne
trouver un mГ©dicament en pharmacie: cialis prix – pharmacie en ligne
Achat mГ©dicament en ligne fiable: Levitra pharmacie en ligne – pharmacie en ligne avec ordonnance
pharmacies en ligne certifiГ©es: pharmacie en ligne pas cher – pharmacie en ligne
pharmacie en ligne pas cher: achat kamagra – Pharmacie en ligne livraison Europe
vente de mГ©dicament en ligne: kamagra livraison 24h – pharmacies en ligne certifiГ©es
pharmacie en ligne france fiable: Medicaments en ligne livres en 24h – pharmacie en ligne sans ordonnance
pharmacie en ligne fiable: Medicaments en ligne livres en 24h – acheter mГ©dicament en ligne sans ordonnance
https://cenligne.com/# pharmacie en ligne sans ordonnance
Viagra gГ©nГ©rique sans ordonnance en pharmacie: Acheter du Viagra sans ordonnance – SildГ©nafil Teva 100 mg acheter
pharmacie en ligne fiable: kamagra pas cher – vente de mГ©dicament en ligne
pharmacie en ligne france pas cher: acheter mГ©dicament en ligne sans ordonnance – pharmacie en ligne pas cher
Pharmacie en ligne livraison Europe: cialis prix – acheter mГ©dicament en ligne sans ordonnance
Viagra 100mg prix: viagra en ligne – Viagra femme sans ordonnance 24h
https://kamagraenligne.com/# Pharmacie Internationale en ligne
pharmacie en ligne france pas cher: Levitra acheter – п»їpharmacie en ligne france
Quand une femme prend du Viagra homme: SildГ©nafil 100 mg sans ordonnance – SildГ©nafil 100 mg sans ordonnance
Viagra homme prix en pharmacie sans ordonnance: Viagra sans ordonnance 24h – Viagra homme sans ordonnance belgique
pharmacie en ligne france fiable: Levitra sans ordonnance 24h – pharmacie en ligne france pas cher
vente de mГ©dicament en ligne: Pharmacies en ligne certifiees – pharmacie en ligne livraison europe
pharmacie en ligne sans ordonnance: cialis generique – pharmacie en ligne fiable
pharmacie en ligne france livraison internationale: kamagra 100mg prix – pharmacie en ligne fiable
pharmacie en ligne france livraison internationale: cialis sans ordonnance – pharmacie en ligne france fiable
Viagra Pfizer sans ordonnance: Viagra generique en pharmacie – SildГ©nafil 100 mg sans ordonnance
pharmacie en ligne: Levitra pharmacie en ligne – Pharmacie Internationale en ligne
vente de mГ©dicament en ligne: Levitra sans ordonnance 24h – pharmacie en ligne fiable
pharmacies en ligne certifiГ©es: kamagra en ligne – pharmacie en ligne livraison europe
trouver un mГ©dicament en pharmacie: kamagra livraison 24h – Pharmacie en ligne livraison Europe
Pharmacie en ligne livraison Europe: Levitra sans ordonnance 24h – pharmacie en ligne pas cher
https://autolux-azerbaijan.com/# Pin up 306 casino
Pin Up Kazino ?Onlayn: Pin Up Kazino ?Onlayn – Pin Up Azerbaycan
Pin Up Azerbaycan ?Onlayn Kazino: Pin-Up Casino – pin-up kazino
?Onlayn Kazino: Pin Up – pin-up 141 casino
pin-up kazino: Pin-up Giris – pin-up 141 casino
https://autolux-azerbaijan.com/# Pin-Up Casino
Pin up 306 casino: Pin Up Kazino ?Onlayn – Pin Up Kazino ?Onlayn
https://autolux-azerbaijan.com/# Pin up 306 casino
Pin-Up Casino: Pin-up Giris – ?Onlayn Kazino
Pin-up Giris: pin-up 141 casino – Pin up 306 casino
https://autolux-azerbaijan.com/# Pin Up Azerbaycan ?Onlayn Kazino
Pin-Up Casino: pin-up 141 casino – ?Onlayn Kazino
?Onlayn Kazino: ?Onlayn Kazino – Pin-up Giris
https://autolux-azerbaijan.com/# Pin Up Azerbaycan ?Onlayn Kazino
https://autolux-azerbaijan.com/# pin-up 141 casino
pin-up 141 casino: pin-up kazino – Pin-up Giris