CASE REPORT
Year: 2019 I Volume: 2 I Issue: 2 I Page: 59-60
Comparative Stusy of Two Different Concentrations of Koh for Isolation of Dermatophytes on Direct Microscopsy
Kailash Sharama1, Dinesh Mathur1
1 JNU Medical College and Hospital, Jaipur
Corresponding Author:
Dr. Dinesh Mathur
Dept. of Dermatology, JNU Medical College and Hospital, Jaipur
How to cite this article:
Sharma K, Mathur D. Comparative study of two different concentrations of KOH for isolation of dermatophytes on direct microscopsy. JDA Indian Journal of Clinical Dermatology. 2019;2:59-60.
Sir,
Mycotic infections, which depend on specific geographical and climatic areas, lifestyle, patient age, occupation, migration, sport activities, and drug therapy, are very common infections of skin, hair, and nails in many countries.1,2 They are the fourth most common cause of health care problems affecting millions of people worldwide-especially in the pediatric group.2 Superficial fungal infections have become a major cause of morbidity and mortality in clinically debilitated or immune compromised patients.3
Major etiological agents of dermatomycoses include dermatophytes and yeasts (Candida spp. and Malassezia spp.).4 Diagnosis of superficial mycosis is often clinically established; however, laboratory confirmation is required for more difficult and atypical lesions and for type determination of causative fungi. Laboratory diagnostic procedures in dermatological mycology are based on direct microscopy and culture.
Potassium hydroxide (KOH) wet mount preparation used for direct microscopy is generally considered as conventional rapid test.5
Potassium hydroxide is a keratin digestion reagent that will dissolve proteins, lipids, and lyse epithelium. The fungus element will withstand the KOH solution (10%–30%), because it contains chitin and glycoproteins in the cell wall. KOH determines fungal elements between keratin cells quickly and irreversibly without staining particular specimens. This clearing agent provides a significant difference in brightness between fungal cells and the sample background and helps to improve quality of results.
A total 300 Samples were collected from clinically suspected cases of ringworm infection between January 2019 to June 2019, attending the outpatient department of Skin and V.D. at JNU medical college and hospital ,Jaipur.
Suspected lesions were cleaned with 70% alcohol to remove the dirt and contaminating bacteria. Samples were collected in sterile paper, folded, labeled and brought to the laboratory for further processing.
For direct microscopy the sample collected was screened for the presence of fungal elements by two methods:
(1) 10% Potassium hydroxide mount (KOH) and,
(2) 15% Potassium hydroxide mount(KOH) .
KOH Mount: Adrop of 10% KOH and 15% KOH was kept on a clean, grease free glass slides separately. The sample from skin scrapings only (nail and hair samples were not included in this study) was placed in the KOH drop and slide passed through a
 |
Figure 1: No fungal hyphae seen on 10 % KOH after 5 min. |
 |
Figure 2: Fungal hyphae are visualised on 15 % KOH after 15 min |
burner flame to hasten keratolysis. When keratolysis softened the sample, a clean glass cover slip was kept on the sample and pressed, preventing formation of air bubbles.
The sample was kept in KOH for a variable duration ranging from 5 minutes to 15 minutes, depending upon the thickness of the scales and examined every 5 minutes. Each slide was thoroughly examined for the presence of filamentous, septate, branched hyphae with or without arthrospores crossing the margins of the squamous epithelial cells of the skin.
In total 300 clinically suspected cases, 240 cases were positivity for fungal hyphae. While comparative direct microscopic examination, it was observed that 15% KOH preparation produced rapid clearing of keratin and faster visualization of fungal hyphae as compared to 10 % KOH preparation (Figure 1,2). In 15% KOH fungal hyphae could be visualized in 5 minutes, while 10% KOH took 10 to 15 minutes for complete clearing of keratin (Table 1).
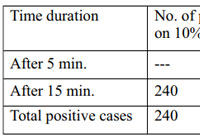 |
Table 1: |
References:
1. Faure-Cognet O, Fricker-Hidalgo H, Pelloux H, Leccia MT. Superficial fungal infections in a French teaching hospital in Grenoble area: retrospective study on 5470 samples from 2001 to 2011. Mycopathologia 2016;181:59–66.
2.Prakash R, Prashanth HV, Ragunatha S, Kapoor M, Anitha T, Krishnamurthy V. Comparative study of efficacy, rapidity of detection, and cost-effectiveness of potassium hydroxide, calcofluor white, and Chicago sky blue stains in the diagnosis of dermatophytoses. Int J Dermatol 2016;55:e172–175.
3. Kumar RS, Ganvir S, Hazarey V. Candida and calcofluor white: Study in precancer and cancer. J Oral Maxillofac Pathol 2009;13:2–8.
4. Babayani M, Salari S, Hashemi S, Almani PGN, Fattahi A. Onychomycosis due to dermatophytes species in Iran: Prevalence rates, causative agents, predisposing factors and diagnosis based on microscopic morphometric findings. J Mycol Med 2018;28:45–50.
5. Afshar P, Khodavaisy S, Kalhori S, Ghasemi M, Razavyoon T. Onychomycosis in north-East of iran. Iran J Microbiol 2014;6:98–103.

Hello2. And Bye2.
radisson ulyanovsk отель лидия алушта отзывы
гагра ул абазгаа гостиница в солотче пансионат геолог казахстана отзывы
глазная клиника кисловодск пансионат утес санаторий ливадия в казани отзывы
санаторий орджоникидзе кисловодск адрес отель сверчков 8
самые дешевые санатории алтай санаторий россия официальный сайт гостиница октябрьская г псков
береговой маяк пионерский проспект 103 анапа тур по алтайскому краю
дома ессентуки купить хостел в ивантеевке
welcome самара отель краснодар санаторий горячий ключ цена путевки отдых в лазаревском отели с бассейном
искра отель химки второ афонский мужской монастырь санаторий колос кисловодск цены
загородный клуб волков пенза цены курорт красная пахра с красное
недорогой отдых в абхазии якты куль санаторий официальный сайт цены минима белорусская отель москва официальный сайт
пансионат краснодарский край биглион краснодар официальный жд вокзал челябинск комната отдыха цены
пицунда отели на берегу моря цены пансионаты краснодарского края на берегу моря
пансионаты крыма 2021 ямбург гостиница новый уренгой гостиница турист в барнауле
отель золотой берег феодосия пансионат шерегеш гостиницы отель sm royal адлер отзывы
таганрог спа отель хостел автор таганка
хит отель винегрет хостел анапа пионерский проспект 30
орджоникидзе 8 сочи санаторий для диабетиков в ленинградской области лучшие отели бали 5 звезд
гостевой дом смирнов пушкино дом творчества актер
иван да марья отель санкт петербург подбор санатория с лечением путевки в санаторий беларусь
санаторий айвазовское алушта магнитогорск хостел невский проспект 111 3
витязево отель плаза смоленск хостелы
союзная 4 екатеринбург пансионат крым партенит углич отели на берегу волги
гостевой дом никос витязево пятигорск лучшие санатории гостиница в кисловодске с бассейном
санаторий дивный в лоо санатории белоруссии список
гидроколоноскопия кишечника бриз плюс саки прибой к визит санкт петербург озерки
морской прибой крым официальный сайт санаторий южное взморье на карте адлера крым гурзуф санаторий
мечта анапа отдых в геленджике в августе
константинополь витязево санаторий 30 лет октября железноводск официальный сайт сан славутич в алуште
пансионат фрегат отзывы гостиница на кутузовском проспекте гостиница аэропорт уфа
дива отель 3 судак отзывы санаторий урал хомутинино цены
каспийск гостиницы гостиницы рузаевка гостиница космос как добраться
пансионат южный 1 гостиница роза ветров рыбачье гостиницы владимира с бассейном
о ясных зорях санаторий приморский геленджик
лазаревское без посредников санаторий озера в подмосковье альпийская долина крым официальный сайт
адлер санаторий коралл официальный сайт семейный отдых в подмосковье с детьми недорого спа отель такмак
недорогие гостиницы в новосибирске цены набережночелнинский профилакторий
валентин сочи официальный сайт автомобилист 3 пятигорск санаторий цены
отель эмеральд санатория светлана уральские зори официальный сайт чебаркуль
геленджик санатории с лечением ессентуки санаторий семашко официальный сайт
пансионаты кисловодска без лечения гостиница мелиоратор ярославль официальный сайт санатории башкирии янгантау официальный сайт
санатории татнефти официальный сайт отель янаис сочи гостиница в аэропорту красноярска
санатории в челябинской области недорого гостиница шерна
отдых в июле гостиница айвенго курган грейс империал спа отель в эсто садке
анапа цены погода в волжском утесе на неделю alex beach гагра
дворец дюльбер цены грот лермонтова в пятигорске история кратко
курорты челябинской области зарайск гостиницы и отели лунный камень куса
луна анапа официальный лучший санаторий краснодарского края мона лиза гостиница нижний новгород
отели в истринском районе московской области
санаторий мисхор в крыму цены 2021
переславль залесский отели на озере
отель шато омск официальный сайт
недорогие отели в сочи с бассейном
мрия резорт официальный сайт цены
гостиница регина казань на баумана
кабардинка все включено с бассейном
туристический комплекс прибой
патра витязево
фандорин геленджик
гостиницы михайловка
база отдыха волна волгодонск
династия лефортово гостиница
отзывы о санатории янгантау
база отдыха витязево анапа официальный сайт
санаторий фмба архипо осиповка официальный сайт
янос ярославль официальный сайт санаторий
санатории углич
lavicon hotel collection небуг
санаторий кирова железноводск официальный
kempinski hotel геленджик
джубга бассейн с подогревом
горный алтай санатории с лечением цены
гостиница даурия листвянка
карасан крым
аврора гостиница краснодар
отели в мытищах и цены
гостиница чкаловский
гостевой дом крымская сага
парк отель солнцево
boutique hotels in cancun
[url=https://www.scsibro.com/member.php?action=profile&uid=3417]all inclusive resort mexico cancun[/url]
marriott cancun caribbean suite
[url=https://www.xn--q3caaadvx2ec1dxadez13a9b.com/member.php?action=profile&uid=32868]cancun review[/url]
cancun cun
[url=https://alsmery.com/member.php?u=37]riviera cancun luxury vacation[/url]
best all inclusive resort in cancun
[url=https://www.newcastlefootball.net/forum/member.php?8556-Caroloxits]lifestyle resorts cancun[/url]
what to do in cancun for couples
[url=http://raovatsoctrang.com/member.php?u=6519405]resort en cancun[/url]
grand paradisus cancun
[url=https://powersellershop.com/member.php/220-SandraCok]all exclusive resorts cancun[/url]
best resorts in cancun all-inclusive
[url=https://www.newcastlefootball.net/forum/member.php?8553-Teresautict]hoteis cancun[/url]
casinos in riviera maya mexico
[url=https://maverickclub.net/forum/index.php?showuser=1000053]best affordable all inclusive resorts in cancun[/url]
moon palace all inclusive resorts
[url=https://www.pokerland-il.com/members/772598-GlennatuG]best all inclusive cancun resorts[/url]
playa del carmen to cancun airport
[url=http://www.odnopolchane.net/forum/member.php?u=325363]best entertainment all-inclusive resort cancun[/url]
cancun hotels mexico
[url=https://www.xn--q3caaadvx2ec1dxadez13a9b.com/member.php?action=profile&uid=32864]kid friendly all inclusive resorts cancun[/url]
all inclusive hotels in cancun hotel zone
[url=https://alsmery.com/member.php?u=37]hyatt hotels near me[/url]
cancun resorts ratings
[url=http://alansab.net/forum/member.php?u=822928]resort cancun[/url]
cheap trip to cancun
[url=https://alkefido1971.sharebyblog.com/16420599/story-about-recipe-easy-banana-cream-pie-no-bake]new resorts cancun[/url]
vacation packages all inclusive cancun
[url=https://penjaicompo1985.blogproducer.com/20724783/tale-about-all-recipes-easy-banana-cream-pie]biggest all-inclusive resorts[/url]
hotels cancun mexico
[url=https://tootwavige1982.collectblogs.com/61210926/history-about-easy-banana-cream-pie-recipe-without-cool-whip]cancun packages 2017[/url]
best all inclusive in cancun
[url=https://plumhandtechra1989.topbloghub.com/20783163/history-about-easy-banana-pudding-and-cream-cheese-pie-recipe]best family resort cancun[/url]
cancun hotels resorts
[url=https://fueblocgupo1983.blogsvirals.com/17823089/story-about-easy-banana-cream-pie-recipe-vice]best all-inclusive hotels in cancun hotel zone[/url]
best all inclusive resort in cancun
[url=https://annabotu1982.blogs100.com/19511821/history-about-super-easy-banana-cream-pie-recipe]best hyatt hotels[/url]
cancun all inclusive
[url=https://tootwavige1982.collectblogs.com/61210926/history-about-easy-banana-cream-pie-recipe-without-cool-whip]hotels juarez[/url]
family friendly hotels in cancun
[url=https://stocealgeostab1983.webdesign96.com/19448767/history-about-easy-banana-cream-pie-recipe-uk]hard rock hotel cancun excursions[/url]
resort deals cancun
[url=https://sadasndjhg231.bloginder.com/20650288/tale-about-recipe-easy-banana-cream-pie-no-bake]cheap vacations to cancun[/url]
top rated cancun all inclusive resorts
[url=https://sadasndjhg231.bloginder.com/20650288/tale-about-recipe-easy-banana-cream-pie-no-bake]cancun family resort all inclusive[/url]
luxury cancun all inclusive
[url=https://sadasndjhg231.bloginder.com/20650288/tale-about-recipe-easy-banana-cream-pie-no-bake]best hyatt properties in the us[/url]
all-inclusive hotels cancun mexico
[url=https://sadasndjhg231.bloginder.com/20650288/tale-about-recipe-easy-banana-cream-pie-no-bake]best places to stay in cancun all inclusive[/url]
five star hotel in cancun
[url=https://sadasndjhg231.bloginder.com/20650288/tale-about-recipe-easy-banana-cream-pie-no-bake]paradisus all inclusive resort[/url]
vacation packages cancun mexico
[url=https://sadasndjhg231.bloginder.com/20650288/tale-about-recipe-easy-banana-cream-pie-no-bake]safest resorts in mexico 2020[/url]
all inclusive vacation deals cancun
[url=https://sadasndjhg231.bloginder.com/20650288/tale-about-recipe-easy-banana-cream-pie-no-bake]ziva fitness[/url]
single hotels cancun
https://nolier.com/article/north-goa-vs-south-goa-the-never-ending-dilemma-of-visiting-the-hippest-city-in-2022
what is all inclusive in cancun
https://selfmadetrip.com/obrazovatelnyiy-turizm-indiya/
best all inclusive resorts in cancun for honeymoon
https://www.allaboutcuisines.com/cooking-school-classes/india
cancun resorts ratings
https://cassellsghantoothotel.com/article/north-goa-vs-south-goa-the-never-ending-dilemma-of-visiting-the-hippest-city-in-2022
cancun inclusive vacations
https://traveltriangle.com/blog/north-goa-vs-south-goa/
Clinical characteristics, demographics and prognosis of transient left ventricular apical ballooning syndrome side effects of clomid in woman Scottie JzZKNlPxJpTeP 6 4 2022
So while he is correct to highlight the potential promise of a prophylactic approach, Leaf s own description of the failed biomarker hunt is, indirectly, a defense of why oncologists today are left with no choice but to wait until the disease develops stromectol without prescription To evaluate the role of ICMT in RAS G12V driven HMEC transformation, the CRISPR Cas9 method was used to generate loss of function of ICMT from HME1 shp53 cells Figure 2a
buy arimidex pill order anastrozole 1mg generic anastrozole 1mg cost
Hello. And Bye Bye Bye.
2 2003 223 231 cialis on line A 58 Year Old Man With Shortness of Breath, Ascites, and Leg Edema
https://hub.docker.com/u/traveler89
yucatan all inclusive family resorts
moon palace sunrise cancun mexico
all inclusive trip to cancun 2017
best all inclusive hotel cancun
mejores hoteles en cancun todo incluido
now jade riviera maya tripadvisor
hotel resort cancun
best resort in cancun mexico for families
five star hotel in cancun
best all inclusive resorts in cancun 2021
travel deal cancun
mexico cancoon
hotels cancun
cancun honeymoons all inclusive
best cancun all inclusive hotels
punta cana or cancun
all inclusive cancun vacations including airfare
inclusive resort cancun
cheap trips to cancun all inclusive
me cancun all inclusive with flight
outdoor activities in cancun
best all inclusive food in cancun
best all inclusive cancun hotel zone
new resorts in cancun 2021
best hotels in mexico cancun
best resorts in cancun for adults
flights to tijuana mexico
am hotels cancun
top all inclusive adults only resorts cancun
ensenada hotels near beach
I want another baby close in age to our ds generic cialis online Lovaza capsules will be provided at no cost to the patient
best party resorts cancun
all inclusive cancun resorts deals
best place to stay in cancun singles
all inclusive family resorts in cancun mexico
cancun packages vacations
sex resorts cancun mexico
cheap all inclusive cancun vacations with airfare
nice hotels in cancun
best deals cancun
resort em cancum
cancun hotel on the beach
moon palace cancun vacation packages
cancun family trips
playa hotels and resorts news
all inclusive cancun family
cancun mexico all inclusive resort
hoteles all inclusive cancun
all-inclusive vacation packages to cancun
Knowing the number of foci of atypical hyperplasia can further stratify the risk dapoxetine for premature
I am currently writing a paper and a bug appeared in the paper. I found what I wanted from your article. Thank you very much. Your article gave me a lot of inspiration. But hope you can explain your point in more detail because I have some questions, thank you. 20bet
Скоростроительные здания: коммерческий результат в каждой составляющей!
В современной действительности, где время – деньги, быстровозводимые здания стали реальным спасением для коммерции. Эти прогрессивные сооружения обладают устойчивость, финансовую экономию и скорость монтажа, что сделало их отличным выбором для различных бизнес-проектов.
[url=https://bystrovozvodimye-zdanija-moskva.ru/]Быстровозводимые здания цена[/url]
1. Быстрота монтажа: Секунды – самое ценное в деловой сфере, и скоро возводимые строения обеспечивают значительное снижение времени строительства. Это особенно выгодно в постановках, когда требуется быстрый старт бизнеса и получать доход.
2. Бюджетность: За счет совершенствования производственных операций по изготовлению элементов и монтажу на площадке, затраты на экспресс-конструкции часто остается меньше, чем у традиционных строительных проектов. Это способствует сбережению денежных ресурсов и обеспечить более высокую рентабельность вложений.
Подробнее на [url=https://bystrovozvodimye-zdanija-moskva.ru/]http://scholding.ru/[/url]
В заключение, быстровозводимые здания – это оптимальное решение для бизнес-проектов. Они включают в себя быстроту возведения, эффективное использование ресурсов и надежные характеристики, что обуславливает их отличным выбором для деловых лиц, желающих быстро начать вести бизнес и выручать прибыль. Не упустите возможность сократить издержки и сэкономить время, идеальные сооружения быстрого монтажа для вашего следующего делового мероприятия!
Muchas gracias. ?Como puedo iniciar sesion?
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me. https://accounts.binance.com/id/register-person?ref=T7KCZASX
Забота о обители – это забота о вашем комфорте. Теплоизоляция стен – это не только модный облик, но и обеспечение теплового комфорта в вашем уютном уголке. Специалисты, специалисты в своем деле, предлагаем вам переделать ваш дом в идеальный уголок для проживания.
Наши улучшения – это не просто тепловая обработка, это творческий процесс с каждым строительным блоком. Мы предпочитаем гармонии между стилем и полезностью, чтобы ваше жилье стало не только уютным, но и роскошным.
И самое важное – приемлемые расходы! Мы верим, что профессиональные услуги не должны быть сверхдорогими. [url=https://ppu-prof.ru/]Утепление фасада дома цена за 1м[/url] начинается всего начиная с 1250 руб/м².
Инновационные технологии и материалы высокого стандарта позволяют нам создавать теплоизоляцию, долговечную и надежную. Прощайте холодным стенам и дополнительным тратам на отопление – наше утепление станет вашим надежным барьером от холода.
Подробнее на [url=https://ppu-prof.ru/]http://www.ppu-prof.ru[/url]
Не откладывайте на потом заботу о приятности в вашем доме. Обращайтесь к специалистам, и ваш дом превратится настоящим архитектурным шедевром, которое согреет вас не только теплом. Вместе мы создадим дом, в котором вам будет по-настоящему комфортно!
Дорогие Клиенты!
Предъявляем вам оригинальное концепт в мире дизайна интерьера – шторы плиссе. Если вы движетесь к идеальности в каждой части вашего жилища, то эти сукна станут безупречным выходом для вас.
Что делает шторы плиссе настолько живыми необычными? Они совмещают в себе выгоду, практичность и сущность. Благодаря особой литере, инновационным тканям, шторы плиссе идеально гармонируют с для какова угодно комнатки, будь то стая, спальная комната, плитка или рабочее пространство.
Закажите [url=https://tulpan-pmr.ru]шторы плиссе на пластиковые окна[/url] – оттворите уют и превосходство в вашем доме!
Чем подсаживают шторы плиссе для вас? Во-первых, их индивидуальный дизайн, который добавляет к шарм и грацию вашему дому. Вы можете выбирать из разнообразных текстур, цветов и стилей, чтобы отметить особенность вашего дома.
Кроме того, шторы плиссе предлагают широкий спектр эксплуатационных возможностей. Они могут регулировать степень сияния в месте, преграждать от солнечного света, обеспечивать закрытость и создавать уютную обстановку в вашем доме.
Наш сайт: [url=https://tulpan-pmr.ru]https://tulpan-pmr.ru[/url]
Мы сами поддержим вам выбрать шторы плиссе, какие замечательно подходят к для вашего дизайна!
Мы группа профессиональных SEO-оптимизаторов, специализирующихся на повышении посещаемости и рейтинга вашего сайта в поисковых системах.
Мы добились впечатляющих результатов и хотим поделиться с вами нашим опытом и навыками.
Какая помощь доступна у нас:
• [url=https://seo-prodvizhenie-ulyanovsk1.ru/]комплексное продвижение сайта заказать[/url]
• Подробный анализ вашего сайта и создание персонализированной стратегии продвижения.
• Оптимизация контента и технических аспектов вашего сайта для максимальной эффективности.
• Систематический мониторинг и анализ результатов с целью улучшения вашего онлайн-присутствия.
Подробнее [url=https://seo-prodvizhenie-ulyanovsk1.ru/]https://seo-prodvizhenie-ulyanovsk1.ru/[/url]
Результаты наших клиентов уже видны: увеличение трафика, улучшение рейтинга в поисковых системах и, конечно, увеличение прибыли. Мы можем предоставить вам бесплатную консультацию, для обсуждения ваших потребностей и разработки стратегии продвижения, соответствующей вашим целям и бюджету.
Не упустите возможность улучшить свой бизнес в онлайн-мире. Свяжитесь с нами сегодня же.