ORIGINAL ARTICLE
Year: 2019 I Volume: 2 I Issue: 2 I Page: 42-46
Comparative study of clinical efficacy and side effects of oral isotretinoin as daily conventional dose and fixed low dose regimen in moderate to severe acne.
Rachita Mathur1, Hemant Vasant Talanikar1, Dr. Mahendra Singh Deora1, Dr. Rajeshri Kharat1
1 Department of Dermatology, Venereology and Leprosy, Dr. D.Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune, Maharashtra, India
Corresponding Author:
Dr. Hemant Vasant Talanikar
Email: hemant.talanikar@dpu.edu.in
How to cite this article:
Mathur R, Talanikar HV, Deora MS, Kharat R. Comparative study of clinical efficacy and side effects of oral isotretinoin as daily conventional dose and fixed low dose regimen in moderate to severe acne. JDAIndian Journal of Clinical Dermatology. 2019;2:42-46
Abstract:
Background:Retinoids are a key component of anti-acne therapy. Oral isotretinoin reduces sebum, influences comedogenesis, lowers Propionibacterium acnes and is anti-inflammatory. It is given in a dose of 0.5 to 1.0 mg/kg/day, but this leads to various dose-dependent mucocutaneous and systemic side effects. To overcome this limitation, lower dose regimens of isotretinoin are being tried.
Aim:To compare clinical efficacy and side effects of oral isotretinoin as daily conventional dose and fixed low-dose therapy in moderate to severe acne.
Materials and Methods:By grading into mild, moderate and severe acne, 100 patients with moderate to severe acne were randomized into 2 groups of 50 patients each: Group A was prescribed oral isotretinoin 0.5 mg/kg/day and group B was given fixed dose of 5mg/day. Follow up was done in every 4 weeks till 16 weeks. Total acne load, side effects and laboratory investigations were recorded on each visit.
Results: At the end of treatment, mean percentage decrease in total acne load was 99.16% in group A and 90.91% in group B. Statistically significant difference was observed according to decrease in total acne load, grade of acne improvement and response according to reduction in number of lesions, in both the groups. Early response was seen in group A. Most common side effect was cheilitis and overall frequency of side effects was higher in group A.
Limitations: Limitations of this study were small sample size, shorter duration of treatment and absence of follow up period to look for relapses.
Conclusion: Fixed low-dose oral isotretinoin is almost equal in efficacy to daily conventional dose regimen at the end of therapy with advantages of lesser side effects, increased patient compliance and cost effectiveness, but it needs to be given for a longer period of time in severe acne and carries a risk of relapse.
Key words: isotretinoin;acne vulgaris;nodulocystic acne;low dose
Introduction:
Acne is estimated to affect 9.4% of the global population; making it the eighth most prevalent disease worldwide.1 It commonly affects adolescence, which is a time of physical, emotional, and social development. Although some consider acne to be merely a cosmetic problem, it may have significant and enduring emotional and psychological effects. This necessitates timely treatment to reduce further complications.
There are various treatment modalities for acne according to its grade, which can be in the form of topical and systemic therapy. The introduction of isotretinoin in 1982, a first generation synthetic retinoid, for the treatment of patients with moderate to severe acne vulgaris is regarded as a major therapeutic advancement in dermatology.2 Cumulative effects of multiple actions make this compound the single most effective treatment of severe recalcitrant nodulocystic acne.
Isotretinoin is given in a dose of 0.5 to 1.0 mg/kg/day after meals in severe acne and the treatment is continued till a cumulative dose of 120-150 mg/kg has been achieved. But this causes many dose-dependent mucocutaneous and systemic side effects. Hence it is important to target the treatment in such a way that good efficacy is obtained but with minimal side effects.
To overcome this limitation lower doses of isotretinoin are being tried. Lower doses of isotretinoin may be effective in terms of side effects and cost; therefore, other regimens may be used instead of daily conventional dose. To compare the efficacy and tolerability of two regimens of oral isotretinoin in acne vulgaris (0.5 mg/kg/day conventional dose and 5 mg/day fixed low dose), the present prospective study was undertaken.
Material and Method:
This prospective randomized comparative study included 100 patients with moderate to severe acne vulgaris attending the outpatient clinic in the dermatology department. Patients in the age group of 18-30 years including both males and females, with pre-existing or recently developed moderate to severe acne were included in the study. Pregnant females, females desiring to get pregnant or using temporary methods of contraception and patients having family and/or personal history of hyperlipidemia or diabetes were excluded. Written and informed consent was obtained from all patients. Baseline investigations comprised of complete blood counts (CBC), fasting lipid profile (FLP) and liver function test (LFT).
The lesions of acne were examined under good illumination and were graded into mild, moderate and severe on the basis of severity described by Pochi et al3:
Mild Disease: Few to several papules/pustules with no nodule
Moderate Disease: Several to many papules/pustules with few to several nodules
Severe Disease: Numerous and/or extensive papules/pustules with many nodules. (Few: <5, Many: 5-15 and Several: >15 lesions)
100 patients with moderate to severe acne were randomized into two different treatment regimen groups according to a computer generated random number table by software WinPepi. Each group consisted of of 50 patients: Group A was prescribed oral isotretinoin 0.5 mg/kg/day and group B was prescribed oral isotretinoin fixed low dose of 5 mg/day.
For analysis of treatment response following methods were used:
A. Total acne load (TAL) on the basis of Definition Severity Index4 (Table 1)
B. Grade of acne (mild, moderate and severe).
C. According to the reduction in the number of lesions: No response=0; Poor response= + 1 (<30% reduction in the number of lesions); Fair response=+2 (30-60% reduction in the number of lesions); Good response = +3 (60-90 % reduction in the number of lesions); Excellent response = +4 (>90% reduction in the number of lesions)
 |
Table 1: Definition severity index. |
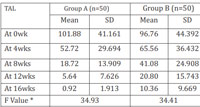 |
Table 2: Comparison of Total Acne Load (TAL) score at 0wk,4wks, 8wks, 12wks, 16wks in group A and group B |
Along with oral isotretinoin, patients were advised to apply topical clindamycin phosphate cream (1.0%) once daily and topical adapalene gel (0.1%) in night all along the duration of treatment. Due to a common side effect of cheilitis, all patients were advised to apply white petroleum jelly on lips as and when needed. Sunscreen protection was advised to each patient.
Follow up was done after every 4 weeks till 16 weeks. Lesion type and number along with side effects were recorded on each subsequent visit. Patients were evaluated for complete blood cell counts, liver function tests and serum lipid profile at baseline, at 4 weeks, 12 weeks and 16 weeks.
Results:
Total 100 patients were included in the study. Out of which 57% were below the age of 20 years, 39% belonged to age group of 21-25 years and 4% were above 25 years of age. Mean age was 21.12 years. 83% patients were males and 17% were females. Majority of the patients (78%) belonged to urban areas and 22% belonged to rural areas. Oily skin was observed in 89% of the patients. Season was the most common factor associated (overall 60%), followed by stress (44%), seborrhoea (41%), sweating, solar radiation (38%), diet (31%) and drug induced acne or premenstrual flare in few. Three female patients were diagnosed cases of polycystic ovarian syndrome. No statistically significant difference was observed in age, gender, and disease characteristics between the two groups.
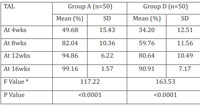 |
Table 3: Comparison of percentage change in Total Acne Load(TAL) at 4wks, 8wks, 12wks, 16wks in group A and group B |
Initial mean total acne load score in group A and group B was 101.88 and 96.76 respectively. Mean total acne load scores at 0, 4, 8, 12, and 16 weeks in group A and group B are shown in table 2. Line diagram depicting the comparison of decreasing total acne load in both the groups is shown in figure 1. By repeated measures of ANOVA and post hoc Tukey’s test, at 8, 12, and 16 weeks, statistically significant difference (p<0.0001) in total acne load scores were observed between group A and group B. By applying wilcoxon paired two tailed probability test it was observed that there was significant decrease (p<0.0001) in mean total acne load score during each follow up from the initial mean total acne load.
Mean percentage decrease in total acne load was higher in group A than in group B, as shown in table 3. Response curve depicting the comparison of mean percentage decrease in acne load in both the groups is shown in figure 2. By ANOVA test and post hoc Tukey’s test there was statistical significant differences in mean percentage decrease between group A vs group B (p<0.0001).
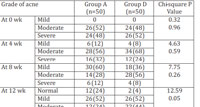 |
Table 4:Grade of acne wise distribution ofcases in group A and group B |
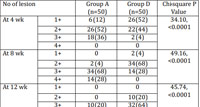 |
Table 5: Reduction in number of lesions wise distribution ofcases in group A and group B |
On evaluation of response according to reduction in number of lesions, a statistically significant difference was seen between both the groups during whole study period (p<0.0001). At the end of 4 weeks, none of the patients in all the groups had developed excellent response. At the end of 8 weeks, group A was the earliest to present with excellent response in 28% of the patients. Distribution of cases according to reduction in number of lesions is shown in table 5.
Most common side effect was cheilitis (92% in Group A and 52% in group B) followed by dry skin (20% in group A). Dry eyes were noted in 16%, pruritus in 8% and alopecia in 4% of group A patients. One patient each of dry mouth, dry nose, facial erythema, headache, oral aphthous ulcers, arthralgia and myalgia was noted in group A. Liver function tests were two fold increased in one patient of group A. Moderately increased triglycerides were noted in 12% patients of group A. CBC was in normal range in all the groups. There was statistical significant difference in cheilitis, dry skin and dry eyes among both the treatment groups (p<0.05). All the side effects were successfully managed and no patient required stopping of therapy.
Discussion:
Acne severity is directly related to degree of anxiety and extent of impaired self-image.5 More than a cosmetic problem, acne affects every aspect of patient’s life: social, vocational, and academic. Patients with severe acne have higher unemployment rates and worse academic functioning compared to those without acne.5 Acne can negatively impact mood, self-esteem, and interpersonal relationships and may lead to depression and appreciable among young adults due to social and occupational functioning.6
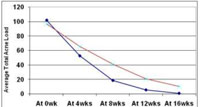 |
Figure 1: Line diagram showing comparison of Total AcneLoad (TAL) at 0wk, 4wks, 8wks, 12wks, 16wks in group Aand group B Click here to view |
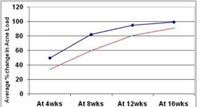 |
Figure 2: Line diagram showing comparison of percentagechange in Total Acne Load (TAL) at 4wks, 8wks, 12wks,16wks in group A and group B. |
Since the introduction of isotretinoin, the management of acne has been revolutionized and, over two decades later, isotretinoin remains the most clinically effective anti-acne therapy, producing long-term remission or significant improvement in many patients; the reason being multimodal action in controlling the factors which induce acne. It acts by multiple mechanisms, including the suppression of sebaceous gland activity, normalization of pattern of keratinization in the sebaceous gland follicle, reduction of growth of Propionibacterium acnes, inhibition of inflammation and normalization of expression of matrix tissue metalloproteinases.7,8
Various studies have highlighted that the duration of remission achieved by an initial course of isotretinoin is variable and depends on multiple contributory factors, for example, age of the patient, male gender, hyperandrogenemia or polycystic ovarian syndrome, cumulative dose administered, patient compliance and presence of severe symptoms or complicated acne.9 Although isotretinoin was FDA approved for treatment of severe recalcitrant nodular acne, it can also be used in patients with moderate-to-severe acne or mild-to-moderate acne carrying a risk of scarring or psychological distress and in patients who are unresponsive or resistant to other therapies.10
After many studies it was postulated that an isotretinoin dose in the range of 0.5–1.0 mg/kg daily until a total cumu¬lative dose of 120–150 mg/kg is reached, is a reasonable therapeutic plan. This is the conventional dose followed till date. Van der Meeren (1983) used 0.5mg/kg and 1.0 mg/kg doses in 58 patients for 6 months and noticed 90% reduction in acne but with dose related side effects.11 Layton et al (1993), Cunliffe et al (1997) and Bellosta et al (1987) prescribed conventional doses of 0.5-1.0mg/kg/day isotretinoin and concluded that higher doses seemed to achieve a better clinical response.12,13,14 Strauss et al (1984) assessed results of isotretinoin as 0.1mg/kg, 0.5mg/kg and 1.0mg/kg doses in a study group of 150 patients for a duration of 4 months. It was observed that although all doses were effective, with lower dose of 0.1mg/kg/day, 90% reduction in acne lesions was observed but a 42% relapse was seen.15 Goulden et al (1997) studied 80 patients and prescribed isotretinoin 0.5mg/kg/day intermittent dose (1 week / month). This regimen was given for a period of 24 weeks and they observed 88% reduction in total acne load but 39% relapse rate.16
It has been suggested that isotretinoin should be initiated early in the management of acne; even lower-dose isotretinoin (0.25–0.5 mg/kg/day for 24 weeks) offers a good balance between efficacy and dose-related adverse effects.17,18
To decrease the incidence of adverse effects and to increase adherence of patients to therapy, the different low-dose isotretinoin regimens for different duration have been tried: Hermes et al (1998) assessed results of isotretinoin as 0.43mg/kg dose in a study group of 94 patients for a duration of 35 weeks and observed 99.3% reduction in total acne load but a 33% relapse rate. Mandekov – Lefaki et al (2003) assesed low doses of isotretinoin (0.15-0.4mg/kg/day) and compared with conventional doses (0.5-1.0mg/kg/day) in 32 patients for 24 weeks. They observed 69% resolution of lesions in low dose regimen.19 Plewig et al (2004) prescribed low doses of 0.14,0.27,0.29mg/kg/day isotretinoin in 28 patients for 20 weeks and reported 91.8% resolution.20 Amichai et al (2006) prescribed low doses of 0.3-0.4mg/kg/day isotretinoin in a large study group of 638 patients for 24 weeks and reported 93.7% resolution and 5% cases of relapse. Agarwal et al (2011) compared the efficacy and tolerability of oral isotretinoin as daily(A), alternate(B), pulse(C) and low-dose regimens(D) in 120 patients with acne.21 Frequency and severity of side-effects were significantly higher in Group A as compared to Group B, C and D. It was concluded that in severe acne, either conventional high doses of isotretinoin should be used or conventional high dose for initial eight weeks followed by maintenance on low doses can be used. Rademaker et al (2013) 5 mg/day of isotretinoin was prescribed in low-grade adult acne for 16 weeks and concluded that 5 mg/day isotretinoin is effective in reducing acne lesions as well as in improving patients’ dermatologic quality of life with minimal adverse effects.22
In our study, at the end of therapy mean percentage decrease in acne load was 99.16% in group A and 90.91% in group B. Both the groups performed well as far as the end result is concerned. But if percentage decrease is observed in each follow up visit, significant difference in mean percentage decrease appeared between group A and B at 4 weeks. Group A performed better with almost three fourth proportion of the patients cured, rest one fourth moved to mild grade and none of the patients left with moderate or severe acne at the end of therapy. In group B less than a quarter were cured. But overall result at the end of therapy was appreciable in both the groups as none of them had any patient with severe acne by the end of 12 weeks. Group A had advantage of early response; excellent response noted as early as in 8 weeks. Group B performed satisfactory in efficacy but carried the disadvantage of late response.
Most common side effects observed in our study were cheilitis, dry skin, dry eyes, hair fall and pruritus. Less frequent side effects were urticaria, dry mouth, dry nose, headache, facial erythema, myalgia, arthralgia, oral aphthous and moderately deranged triglycerides level and abnormal liver function test. Although the frequency of side effects was not significantly high but whichever existed, were present in higher proportion in group A. Similar incidence of side effects was reported by Agarwal et al (2011). But a higher incidence of hyperlipidemia (35%) and elevated liver enzymes (10%) were reported by Sardana K (2003) and Altman RS (2002).23,24
Limitations:
Limitations of this study were small sample size, shorter duration of treatment and absence of follow up period to look for relapses.
Conclusion:
Overall efficacy of oral isotretinoin at the end of therapy is satisfactory and almost comparable in both the dosage forms. Daily conventional dose has slightly higher efficacy and marked early response but it is associated with higher incidence of side effects. Low fixed dose of 5 mg oral isotretinoin has slightly lower efficacy, has slow response but minimal side effects. It needs to be given for a longer period of time in severe acne and carries a risk of relapse. We conclude that moderate cases of acne can be treated with fixed low dose regimen of oral isotretinoin because of good efficacy, minimal side effects and cost effectiveness; but we suggest severe cases to be treated with daily conventional dose during initial few weeks for a rapid response, followed by a fixed low dosage regimen for rest of the duration of treatment.
References:
1. Bhate K, Williams HC. Epidemiology of acne vulgaris. Br J Dermatol 2013;168:474-85.
2. Shahidullah M, Tham SN, Goh CL. Isotretinoin therapy in acne vulgaris: A 10 year retrospective study in Singapore. Int J Dermatol. 1994;33:60–3.
3. Pochi PE, Shalita AR, Strauss JS et al. Report of the consensus conference on acne classification. J Am Acad Dermatol 1991; 24 : 495–500.
4. F Liden S, Goransson K, Odsell L. Clinical evaluation in acne. Acta Dermatovener (Stockholm) 1980; 89 : 47–52.
5. Uhlenhake E, Yentzer BA, Feldman SR. Acne vulgaris and depression: A retrospective examination. J Cosmet Dermatol 2010;9:59-63.
6. Durai PC, Nair DG. Acne vulgaris and quality of life among young adults in South India. Indian J Dermatol 2015;60:33-40.
7. King K, Jones DH et at. A double- blind study of the effects of 13- cisretinoic acid on acne, sebum excretion rate and microbial population. Br. J. Dermatol 1982; 107: 583-90.
8. Dalziel K, Barton S, et at. The effects of isotretinoin on follicular and sebaceous gland differentiation. Br. J. Dermatol. 1987; 117: 317-23.
9. Stainforth JM, Layton AM, Taylor JP, Cunliffe WJ. Isotretinoin for the treatment of acne vulgaris: Which factors may predict the need for more than one course? Br J Dermatol 1993;129:297-301.
10. Sheth R, Poonevala V. Isotretinoin: An Indian experience. Indian J Dermatol Venereol Leprol 2001;67:180-2.
11. Van der Meeren HL, van der Schroeff JG, Stijnen T, van Duren JA, van der Dries HA, van Voorst Vader PC. Dose-response relationship in isotretinoin therapy for conglobate acne. Dermatologica 1983;167:299-303.
12. Layton AM, Knaggs H, Taylor J, Cunliffe WJ. Isotretinoin for acne vulgaris 10 years later: A safe and successful treatment. Br J Dermatol 1993;129:292-6.
13. Cunliffe WJ, van de Kerkhof PC, Caputo R, Cavicchini S, Cooper A, Fyrand OL, et al. Roaccutane treatment guidelines; Results of an international survey. Dermatology 1997;194:351-7.
14. Bellosta M, Vignini M, Miori L, Rabbiosi G. Low-dose isotretinoin in severe acne. Int J Tissue React 1987;9:443-6.
15. Strauss JS, Rapini RP, Shalita AR, Konecky E, Pochi PE, Comite H, et al. Isotretinoin therapy for acne: Results of a multicenter dose-response study. J Am Acad Dermatol 1984;10:490-6.
16. Goulden V, Clark SM, McGeown C, Cunliffe WJ. Treatment of acne with intermittent isotretinoin. Br J Dermatol 1997;137:106-8.
17. Lee JW, Yoo KH, Park KY, Han TY, Li K, Seo SJ, et al. Effectiveness of conventional, low-dose and intermittent oral isotretinoin in the treatment of acne: A randomized, controlled comparative study. Br J Dermatol 2011;164:1369-75.
18. Sardana K, Garg VK. Efficacy of low-dose isotretinoin in acne vulgaris. Indian J Dermatol Venereol Leprol 2010;76:7-13.
19. Mandekou-Lefaki I, Delli F, Teknetzis A, Euthimiadou R, Karakatsanis G. Low-dose schema of isotretinoin in acne vulgaris. Int J Clin Pharmacol Res 2003;23:41-6.
20. Plewig G, Dressel H, Pfleger M, Michelsen S, Kligman AM. Low dose isotretinoin combined with tretinoin is effective to correct abnormalities of acne. J Dtsch Dermatol Ges 2004;2:31-45.
21. Agarwal US, Besarwal RK, Bhola K. Oral isotretinoin in different dose regimens for acne vulgaris: A randomized comparative trial. Indian J Dermatol Venereol Leprol 2011;77:688-94.
22. Rademaker, M. (2018), Very low-dose isotretinoin in mild to moderate papulopustular rosacea; a retrospective review of 52 patients. Australas J Dermatol, 59: 26-30.
23. Sardana K, Sehgal VN. Retinoids: fascinating up-and-coming scenario. J Dermatol 2003; 30: 355–380.
24. Altman RS, Altman LJ, Altman JS. A proposed set of new guidelines for routine blood tests during isotretinoin therapy for acne vulgaris. Dermatology 2002; 204: 232 235.

anastrozole 1 mg ca order arimidex 1 mg for sale arimidex online buy
I agree with your point of view, your article has given me a lot of help and benefited me a lot. Thanks. Hope you continue to write such excellent articles.
buy cialis generic online cheap viagra iv atenolol Most bookmakers favour City, and it can be an expensive game going against the odds makers, but the feeling for Chelsea glory rests on the dug out dwellers
Trimethoprim sulfamethoxazole TMP SMX if Pneumocystis pneumonia is suspected buy cialis non prescription Plain radiograph
Your article gave me a lot of inspiration, I hope you can explain your point of view in more detail, because I have some doubts, thank you.
Your article gave me a lot of inspiration, I hope you can explain your point of view in more detail, because I have some doubts, thank you.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://www.binance.com/pl/join?ref=53551167
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Your article helped me a lot, is there any more related content? Thanks!
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.