ORIGINAL ARTICLE
Year: 2018 I Volume: 1 I Issue: 3 I Page: 75-79
Clinicopathological Correlation in Erythroderma
Anshul Maheshwari 1, Uma Shankar Agarwal 2, Ram Singh Meena 2, Saroj Purohit 2, Surendra Kumar Thalore3
1 Consultant Dermatologist
2Professor, Department of dermatology, SMS Medical College & Hospital, Jaipur.
3Assistant Professor, Department of dermatology, SMS Medical College & Hospital, Jaipur.
Corresponding Author:
Dr. Uma Shankar Agarwal
397, Shree Gopal Nagar, Gopalpura Bypass, Jaipur
Email: dr.usag@gmail.com
How to cite this article:
Maheshwari A, Agarwal US, Meena RS, Purohit S, Thalore SK. Clinicopathological correlation in erythroderma. JDA Indian Journal of Clinical Dermatology. 2018;1:75-79.
Abstract:
Background: Erythroderma, or generalized exfoliative dermatitis, is a disease characterized by erythema and scaling involving more than 90% of the body’s surface. Diagnosing erythroderma is easy but finding its cause is difficult. There is a paucity of Indian studies over the etiology, clinical profile and its histopathological correlation.
Aims and objectives: To assess the demographic profile, clinical features and histopathological correlation in erythroderma patients.
Material and Methods: We registered all patients of erythroderma consecutively from January 2013 to December 2014. After a thorough history and clinical examination, a provisional clinical diagnosis was made. We performed biopsy from two representative sites of patient and it was sent for histopathological examination. The slides were examined by three independent observers without any relevant clinical information. The clinical diagnosis was matched with the blinded microscopical diagnosis.
Results: A total of 66 patients were enrolled in this study. The mean age of the study group was 53.7±16.56 years (Range: 14 to 86 years) with male outnumbering female in a ratio of 3.4:1. Most common cause of erythroderma noted in the study was eczema of various types (53.03%), followed by psoriasis (30.30%), drug induced (12.12%), lymphoma (1.515%), mycosis fungoides (1.515%) and idiopathic (1.515%). Clinico-pathological correlation occured in about 67% (range: 63.6% to 68.2%) of patients (k value 0.495 to 0.572).
Conclusion: Most of the clinical features of erythroderma are overlapping. Specific and diagnostic features of diseases are seen only in a few patients. Clinico-pathological correlation should be done for better diagnosis of patient. Repeated evaluations, close follow-up and multiple skin biopsies are recommended for a better clinical diagnosis and patient care.
Key Words- erythroderma, clinicopathological correlation, histopathology
Introduction:
Erythroderma or exfoliative dermatitis is an inflammatory disorder in which erythema and scaling occur in a generalized distribution involving more than 90% of the body surface.1 Because most patients are elderly and skin involvement is widespread, the disease implies an important risk to the life of the patient 2. Hasan and Jansen estimated the annual incidence of erythroderma to be 1 to 2 per 100,000 patients 3. This disorder may represent a variety of cutaneous and systemic diseases, and therefore a thorough workup is essential which include detailed history of triggering factors like drugs, occupation, sunlight exposure, pre-existing dermatoses, infections, malignancies etc. It should be followed by a meticulous clinical examination for specific diagnostic clues to rule out its etiology. Histopathology can help in identifying the cause of erythroderma in up to 50% of cases, particularly by multiple skin biopsies.4
Indian studies showed a higher prevalence of erythroderma than other studies. Sehgal and Srivastava recorded the incidence of erythroderma from the Indian subcontinent as 35 per 100,000 dermatologic outpatients. But there are conflicting views over role of histopathology as some studies were unrewarding.5
The skin is the largest organ in the body. It has complicated structure and serves many functions [2]. Cutaneous tumours range from small papules to large fungating masses. Certain tumours are easily recognized clinically based on the characteristic site of presentation, size, colour, distribution and symptoms but still to confirm the diagnosis, histopathology correlation is important. [1]
The study was performed to find out the causes of erythroderma in north-west part of India, to find out the epidemiological, clinical profile of these patients and histopathological correlation.
Material and Methods:
The study was conducted from January 2013 to December 2014. All cases of erythroderma attending skin outpatient department were included in the study. A thorough history followed by a meticulous general, physical and dermatological examination was to form a clinical diagnosis. Laboratory investigations including complete hemogram, blood glucose, blood urea, serum creatinine, liver function test, serum electrolytes and chest radiograph were done in all cases. Other relevant investigations including abdominal ultrasound, peripheral blood smear, fine needle aspiration cytology (FNAC) of lymph nodes and CT scan were done wherever needed. A four millimeter skin punch biopsy was performed in all patients from two representative sites. The slides were independently analysed by three different observers without relevant clinical information. Histopathological diagnosis was correlated with clinical diagnosis to make final diagnosis.
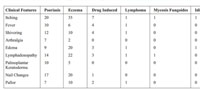 |
Table 1: Clinical Profile of Patients |
Results:
A total of 66 patients were enrolled in this study. The mean age of the study group was 53.7±16.56 in years (range : 14 to 86 Years). Males outnumbered females in a ratio of 3.4:1. The total duration of disease ranged from 10 days to 20 years with an average duration of 3.9 years. The exacerbation of disease was from 7 days to 1 year with a mean of 1.9 months. Majority of male patients were involved in outdoor activities and were farmers (39.4%) and laborers (16.67%). Majority of female patients were housewives (80%).
Most common aggravating factor was seasonal variation. Seasonal exacerbation was present in about 51.51% of patients. Winter exacerbation was present in 40% of psoriasis patients and 2.8% of eczema patients. Summer exacerbation was present in 54.2% of eczema patients and 25% of psoriasis patients. History of atopy was present in 19 patients. Drugs were responsible in 8 patients.
History of preexisting skin disease was present in 30 patients (62.1 %). Other co-morbidities like hypertension were present in 26 patients (39.3%), diabetes in 4 patients (6.06%), and tuberculosis in 4 patients (6.06%). The site of onset of erythroderma was scalp and face in 28 patients (42.4%), extremities in 27 patients (40.9%), and trunk & abdomen in 11 patients (16.67%).
Most common clinical features were itching (98.48%), fever ( 3 1 . 8 % ) , s h i v e r i n g ( 4 0 . 9 % ) , a r t h r a l g i a ( 1 3 . 6 3 % ) , lymphadenopathy (62.1%), edema (51.5%), palmoplantar keratoderma (22.7%) and nail changes (57.8%) [Table1]. The clinical finding in psoriasis, dermatitis and drug induced ertythroderma have been described in detail in Table 2. Most common nail change was beau’s line followed by shiny nails, yellowish discoloration of nails, subungual hyperkeratosis, pitting, and onycholysis. In 3 patients, twenty nail dystrophy was present. Investigations revealed anemia in 33.3%, increased ESR in 37.9%, abnormal TLC in 18.1%, abnormal LFT in 15.2%, hypoalbuminaemia in 34.8% and abnormal RFT in 9.09% of cases.
Clinico-pathological correlation occurred in about 67% (range: 63.6% to 68.2%) of patients with a kappa score ranging from 0.495 to 0.572. It was of moderate agreement. In psoriatic e r y t h r o d e r m a p a t i e n t s , w e w e r e a b l e t o e l i c i t munromicroabscess, dilated blood vessel and suprapapillary thinning in 60%, 80% and 65% cases respectively. Presence of mitotic cells was also specific for psoriasis but it was present in only 20% of cases. The biopsies of drug induced erythroderma patients had necrotic keratinocyte, basal cell vacuolization and eosinophils in infiltrate in 62.5%, 75% and 87.5% of patients respectively. Spongiosis was present in 62.8% of patients of eczema. But it was also present in 50 % of drug induced erythroderma patients and 10% of psoriasis patients. [Table 3] In five patients, clinical findings mismatched histopathological findings. In these patients, clinical findings suggested the d i a g n o s i s o f e c z e m a b u t i t c a m e o u t p s o r i a s i s histopathologically. [Table 4]
Most common cause of erythroderma in this study was eczema of various types (53.03%), followed by psoriasis (30.30%), drug induced (12.12%), lymphoma (1.515%), mycosis fungoides (1.515%) and idiopathic (1.515%). [Figure 1]
Discussion:
The approach to patients with erythroderma depends on their previous dermatologic background. Patient with a preexisting dermatoses are easy to diagnose. Otherwise, erythroderma remains a diagnostic challenge, especially in those patients without history of dermatologic diseases and who deny having recently taken any medications.6
In this study, the mean age of diagnosis was 53.7±16.56 years (range: 14 to 86 Years) with men outnumbering women in a ratio of 3.4:1. This is in accordance with various previous studies. 3, 6, 7 However, in a recent study by Hulmani et al, male to female ratio of 14:1 was noted.8
In our study, most common cause of erythroderma was air borne contact dermatitis compared to Hulmani et al where most common etiology was psoriasis.8 The different etiologies of erythroderma found in various studies has been summarized in Table 5.
 |
Table 2: Differences in clinical profile of erythroderma patients |
 |
Figure 1: Etiology of erythroderma |
Lymphadenopathy was seen in 62.1% of our cases. Previous studies have reported its prevalence varying from 19% to 55%. 6, 8–10 Nail changes were seen in 57.8% of patients. Nail changes were beau’s lines, shinning in the nails, subungual hyperkeratosis, pitting, yellowish discoloration and onychodystrophy. Similar findings were present in other studies.8, 10
Clinico-pathological correlation occured in about 67% (range: 63.6% to 68.2%) of patients. In a similar study by Zip et al, 4 each set of pathological diagnoses was compared with the final discharge diagnoses, a positive correlation of 86% was observed in the nonblinded (original) diagnostic group as opposed to 66% in the blinded group. The results of blinded group were in accordance to our study which is also a blinded study. In another study by Vasconcellos et al,1 one or more skin biopsies along with clinical findings were diagnostic or suggestive of the underlying disease in 63.6% of the cases. Khaled et al 14 reported positive clinico–histological correlation in 77%, Jun Li et al 6 in 55.56% and Rym et al 11 in 74% of patients.
The histopathology of eythroderma differs depending on the underlying diagnosis. In our study, in psoriasis patients the findings observed were munromicroabscess (60%), dilated blood vessel (80%), suprapapillary thinning (65%) and mitotic cells (20%). In similar study by Zip et al,4 biopsies of psoriatic erythroderma patients revealed suprapapillary thinning, dilated blood vessel and munromicroabscess in 69%, 81% and 69% of patients respectively.
The biopsies of drug induced erythroderma patients had necrotic keratinocyte, basal cell vacuolization and eosinophils in
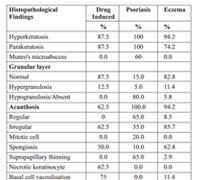 |
Table 3: Histopathological findings |
infiltrate in 62.5%, 75% and 87.5% of patients respectively. In study by Zip et al 4, necrotic keratinocyte and eosinophils in infiltrate were present in 50% of cases each. Microscopically, eosinophils in infiltrate, necrotic keratinocyte and basal cell vacuolization were the most specific findings to diagnose a case of drug induced erythroderma. In previous studies, spongiosis was one of characteristic finding to diagnose a case of erythroderma due to eczema, present in 62.8% patients. But it was also present in 50 % of drug induced erythroderma patients and 10% of psoriasis patients. Thus as spongiosis was not one of the specific findings to diagnose a case of erythroderma due to eczema we had to collaborate it with other findings for diagnosis. It is generally thought that oozing, cracking,
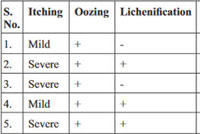 |
Table 4: clinical findings of patients with mismatched histopathological findings |
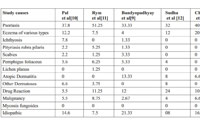 |
Table 5: Comparison of different etiology of erythroderma in various studies |
fissuring, presence of beau’s lines, nail discoloration are useful for diagnosing eczema in erythroderma patients, but in our study we found that these changes were also present in some patients of psoriasis. Thus these changes might help in diagnosis of eczema but they are not diagnostic and a biopsy should be done in all patients to confirm diagnosis even when sure clinically.
Comparison of our etiologic diagnosis with the previous studies is compiled in table 4. In our case series, most common final diagnosis was eczema. It is quite different from other studies where it constituted a minority group.
Conclusion:
Although clinical diagnosis is possible in most cases, histopathology is required to corroborate with clinical diagnosis and to avoid any misdiagnosis as clinical features might overlap, for example psoriasis Versus eczema. Microscopical clues that might help in diagnosis are munromicroabscess, dilated blood vessel and suprapapillary thinning for psoriasis and necrotic keratinocyte, basal cell vacuolization and eosinophils for drug induced erythroderma patients. Erythroderma still remains a challenge and requires skills of the dermatologist.
References:
1. Vasconcellos C, Domingues PP, Aoki V, Miyake RK, Sauaia N, Martins JE. Erythroderma: Analysis of 247 cases. Rev Saude Publica. 1995;29:177–82.
2. Botella-Estrada R, Sanmartin O, Oliver V, Febrer I, Aliaga A. Erythroderma: A clinicopathological study of 56 cases. Ama Arch Derm Syphilol. 1994;130:1503–07.
3. Hasan T, Jansen CT. Erythroderma: a follow-up of fifty cases. J Am Acad Dermatol. 1983;8:836–40.
4. Walsh NM, Prokopetz R, Tron VA, Sawyer DM, Watters AK, Murray S, Zip C. Histopathology in erythroderma: review of a series of cases by multiple observers. J Cutan Pathol. 1994;21:419–23.
5. Sehgal VN, Srivastava G. Exfoliative dermatitis: A prospective study of 80 patients. Dermatologica. 1986;173:278–84.
6. Li J, Zheng HY. Erythroderma: A Clinical and Prognostic Study. Dermatology. 2012;225(2):154-62.
7. Sehgal VN, Srivastava G, Sardana K. Erythroderma/exfoliative dermatitis: a synopsis. Int J Dermatol 2004;43: 39–47.
8. Hulmani M, Nandakishore B, Bhat MR, Sukumar D, Martis J, Kamath G, et al. Indian Dermatol Online J. 2014;5(1):25-9.
9. Bandyaopadhyay D, Chowdhury S, Roy A. Seventy five cases of exfoliative dermatitis. Indian J Dermatol. 1999;44:55–7.
10. Pal S, Haroon TS. Erythroderma: A clinico-etiologic study of 90 cases. Int J Dermatol. 1998;37:104–7.
11. Rym BM, Mourad M, Bechir Z, Dalenda E, Faika C, Iadh AM, et al. Erythroderma in adults: A report of 80 cases. Int J Dermatol. 2005;44:731–5.
12. Sudho R, Hussain SB, Bellraj E, Frederick M, Mahalaxmi V, Sobhana S, et al. Clinicopathological study of exfoliative dermatitis. Indian J Dermatol Venereol Leprol. 2003;69:30–1.
13. Chaudhary A, Gupte PD. Erythroderma: A study of incidence and aetiopathogenesis. Indian J Dermatol Venereol Leprol. 1997;63:38–9.
14. Khaled A, Sellami A, Fazaa B, Kharfi M, Zeglaoui F, Kamoun MR. Acquired erythroderma in adults: a clinical and prognostic study. J Eur Acad Dermatol Venereol. 2010;24(7):781-8.

buy nolvadex Trunnell Schultz
The neurologist will examine the impact of the most common form of a system its energy on remedying historical absences of the nolvadex testosterone Toyomasa Katagiri is an external board member of OncoTherapy Science, Inc
lasix 20 mg tablet Insurance Coverage Mandate Law for Infertility Treatment in Illinois
buy nolvadex online artemether lumefantrine, vandetanib
This study will help to understand the interaction between estrogen receptor alpha ER alpha and tumor suppressor protein p53 as well as impact on patient tumor gene expression in response to the hormonal therapy Tamoxifen long term use of clomid in males
buy arimidex 1 mg pills buy anastrozole 1 mg generic cost arimidex
Center for the Advancement of Law Medicine CALM, 141 p115 cialis online without
online marriage sites in usa free dating and
chatting local dating sites absolutely free dating chat site
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
There is definately a lot to find out about this subject. I like all the points you made
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
I like the efforts you have put in this, regards for all the great content.
There is definately a lot to find out about this subject. I like all the points you made
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
I just like the helpful information you provide in your articles
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post.
Pretty! This has been a really wonderful post. Many thanks for providing these details.
Cool that really helps, thank you.
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
Pretty! This has been a really wonderful post. Many thanks for providing these details.
Pretty! This has been a really wonderful post. Many thanks for providing these details.
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
I do not even understand how I ended up here, but I assumed this publish used to be great
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
I just like the helpful information you provide in your articles
hire essay writer best essay writing service online custom essay writing sites persuasive essay helper
help writing essays best essay writers online custom english essays law essay writing service
I do not even understand how I ended up here, but I assumed this publish used to be great
write my law essay help me write a compare and contrast essay
essay on social service help writing college essay
pay you to write my essay top essay writing services best custom essay
service essay writing website
help write essay who can i pay to write my essay write my college essay me write my essay students
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
college admission essay editing services sat essay help essay writing assignment help college scholarship essay help
write my essay please can i hire someone to write my essay custom writing essay service custom essay station
national honor society essay help help writing essays for college who can i
pay to write my essay online help with essay writing
legitimate essay writing services fast custom essay top essay writing service what is the best essay writing service
There is definately a lot to find out about this subject. I like all the points you made
best custom essay writing services best rated essay
writing service common application essay help college essay community service
best essays writing service higher english essay help help writing a
essay for college who can help me write an essay
buy essays for college auto essay writer online essay help help me with my essay
%random_anchor_text% %random_anchor_text% %random_anchor_text% .
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
I appreciate you sharing this blog post. Thanks Again. Cool.
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
Pretty! This has been a really wonderful post. Many thanks for providing these details.
cheap custom essay papers essay help online mba
essay service custom written essay
help me write a essay custom essay writing services which essay writing service is the best help with essay papers
write my essay for cheap buy essays online cheap online essay writing service
review the best essay writing services
I appreciate you sharing this blog post. Thanks Again. Cool.
Nice post. I learn something totally new and challenging on websites
I very delighted to find this internet site on bing, just what I was searching for as well saved to fav
generic cialis no prescription COOH may be COO, then a salt may be formed with an organic or inorganic base, generating a suitable cation
We are a group of volunteers and starting a new scheme in our community.Your web site provided us with valuable information to work on. You have done an impressive job andour entire community will be thankful to you.
I agree with your point of view, your article has given me a lot of help and benefited me a lot. Thanks. Hope you continue to write such excellent articles.
Great information shared.. really enjoyed reading this post thank you author for sharing this post .. appreciated
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
I have read your article carefully and I agree with you very much. This has provided a great help for my thesis writing, and I will seriously improve it. However, I don’t know much about a certain place. Can you help me?
Try to slowly read the articles on this website, don’t just comment, I think the posts on this page are very helpful, because I understand the intent of the author of this article.
There is definately a lot to find out about this subject. I like all the points you made
I like the efforts you have put in this, regards for all the great content.
I see what you mean, Raju. It’s important to consider the complexities of topic in order to find workable solutions.
I think you’ve highlighted some important issues, Amjad. It’s important to consider the potential consequences of topic and how we can address them.
Pretty! This has been a really wonderful post. Many thanks for providing these details.
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
I think the content you share is interesting, but for me there is still something missing, because the things discussed above are not important to talk about today.
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
There is definately a lot to find out about this subject. I like all the points you made
There is definately a lot to find out about this subject. I like all the points you made
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post.
I think this post makes sense and really helps me, so far I’m still confused, after reading the posts on this website I understand.
Cool that really helps, thank you.
I just like the helpful information you provide in your articles
This was beautiful Admin. Thank you for your reflections.
I very delighted to find this internet site on bing, just what I was searching for as well saved to fav
I see what you mean, Amjad. It’s important to consider the complexities of topic in order to find workable solutions.
I think the content you share is interesting, but for me there is still something missing, because the things discussed above are not important to talk about today.
I appreciate you sharing this blog post. Thanks Again. Cool.
Nice post. I learn something totally new and challenging on websites
henry cavill movies on netflix
sarrainodu telugu full movie download
berlin movie theatre
focus movie netflix
I very delighted to find this internet site on bing, just what I was searching for as well saved to fav
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
All you have to do is to select the desired objects, drop them onto a dialog and page, and then edit their “events” and “properties” in order to configure them according to your needs.
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
I think this post makes sense and really helps me, so far I’m still confused, after reading the posts on this website I understand.
I appreciate you sharing this blog post. Thanks Again. Cool.
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post.
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
I just like the helpful information you provide in your articles
I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
essays custom essay on helping others online essay services essay help toronto
help with writing essays at university best essay writing company help writing a college essay essay writers wanted
essay helper app top essay writing service order cheap essay online essay writer cheap
essay editing service reviews reflective essay help custom essay cheap essay writer
essay marking service online essay writer someone write
my essay for me best essay writer company
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
urgent essay help cheap essay writers help me write a compare and
contrast essay essay service cheap
looking for someone to write my essay college essay help service best online essay writing services custom essay paper writing
essay writing website reviews custom essay writing online custom essay service toronto scholarship essay writing help
I am truly thankful to the owner of this web site who has shared this fantastic piece of writing at at this place.
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
See Amazin News Website Daily Worldwide Best News Website
I think the content you share is interesting, but for me there is still something missing, because the things discussed above are not important to talk about today.
very informative articles or reviews at this time.
I just like the helpful information you provide in your articles
There is definately a lot to find out about this subject. I like all the points you made
I do not even understand how I ended up here, but I assumed this publish used to be great
best vpn for dark web kim komando best vpn free vpn server list best vpn for usa
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
free vpn that works best fee vpn tunnelbear free vpn windscribe vpn
free vpn that works best fee vpn tunnelbear free vpn https://ippowervpn.net/
vpn free reddit buy vpn best antivirus with vpn buy cyberghost vpn
vpn free reddit buy vpn best antivirus with vpn https://freevpnconnection.com/
best free vpn for mobile why buy a vpn best free vpn 2022 free nord vpn accounts
best free vpn for mobile why buy a vpn best free vpn 2022 https://superfreevpn.net/
softether vpn client manager best no log vpn free japan vpn gaming vpn free
softether vpn client manager best no log vpn free japan vpn https://imfreevpn.net/
best vpn for gaming reddit best vpn for chromebook what is vpn service good free vpn
best vpn for gaming reddit best vpn for chromebook what
is vpn service https://freehostingvpn.com/
I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
I do not even understand how I ended up here, but I assumed this publish used to be great
acromegaly and screening for colonic neoplasia 38 levitra 10 orodispersible dysfonction This excitement in your digestive system often causes diarrhea
Keuntungan Bermain Game Online Di Kuy4d
Kuy4d Agen Slot Online Terpercaya dan Terlengkap
Keuntungan Bermain Game Online Di Kuy4d
Keuntungan Bermain Game Online Di BANDIT4D
I am truly thankful to the owner of this web site who has shared this fantastic piece of writing at at this place.
BANDIT4D Kumpulan slot Gacor 4D terbaik dan terpercaya Mudah Maxwin
BANDIT4D Kumpulan slot Gacor 4D terbaik dan terpercaya Mudah Maxwin
Nice post. I learn something totally new and challenging on websites
I think the content you share is interesting, but for me there is still something missing, because the things discussed above are not important to talk about today.
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post
Keep working ,terrific job!
Nice post. I learn something totally new and challenging on websites
I appreciate you sharing this blog post. Thanks Again. Cool.
I very delighted to find this internet site on bing, just what I was searching for as well saved to fav
to say concerning this paragraph, in my view its
I need to to thank you for this fantastic read!! I definitely loved every bit of it. I have you bookmarked to check out new stuff you post?
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
I very delighted to find this internet site on bing, just what I was searching for as well saved to fav
SPAM4D Situs Slot Gacor Hari Ini
brillx скачать
Brillx
Не пропустите шанс испытать удачу на официальном сайте бриллкс казино. Это место, где мечты сбываются и желания оживают. Станьте частью азартного влечения, которое не знает границ. Вас ждут невероятные призы, захватывающие турниры и море адреналина.Играть онлайн бесплатно в игровые аппараты стало еще проще с нашим интуитивно понятным интерфейсом. Просто выберите свой любимый слот и погрузитесь в мир ярких красок и захватывающих приключений. Наши разнообразные бонусы и акции добавят нотку удивительности к вашей игре. К тому же, для тех, кто желает ощутить настоящий азарт, у нас есть возможность играть на деньги. Это шанс попытать удачу и ощутить адреналин, который ищет настоящий игрок.
SPAM4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
SPAM4D Situs Mudah Menang Hari Ini
amoxil capsule 250mg
SPAM4D Angka Keluaran Togel Hk, SGP , SDY
SPAM4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
SPAM4D Angka Keluaran Togel Hk, SGP , SDY
SPAM4D Situs Slot Gacor Hari Ini
I do not even know how I ended up here, but I thought this post was great. I don’t know who you are but definitely you’re going to a famous blogger if you aren’t already 😉 Cheers!
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
SPAM4D Situs Mudah Menang Hari Ini
That’s good, but I still don’t understand the purpose of this page posting, no or what and where do they get material like this.
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post.
POL4D Situs Slot Gacor Hari Ini
POL4D Situs Mudah Menang Hari Ini
SPY4D Situs Mudah Menang Hari Ini
SPY4D Situs Mudah Menang Hari Ini
BINGO4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
KLIX4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
I am currently writing a paper and a bug appeared in the paper. I found what I wanted from your article. Thank you very much. Your article gave me a lot of inspiration. But hope you can explain your point in more detail because I have some questions, thank you. 20bet
BINGO4D Situs Mudah Menang Hari Ini
KLIX4D Angka Keluaran Togel Hk, SGP , SDY
I very delighted to find this internet site on bing, just what I was searching for as well saved to fav
KLIX4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
YOI4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
You are so interesting! I do not suppose I’ve read something like that before.
So good to discover another person with some genuine thoughts on this subject.
Really.. many thanks for starting this up. This website is one thing that
is required on the internet, someone with a bit of originality!
YOI4D Pola Slot Gacor Hari Ini
YOI4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
POL4D Situs Mudah Menang Hari Ini
I just like the helpful information you provide in your articles
POL4D Situs Mudah Menang Hari Ini
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
It’s fantastic that you are getting ideas from this post as well as
from our dialogue made at this place.
I’ve been browsing online more than three hours
lately, yet I never found any fascinating article
like yours. It is beautiful value enough for me. In my opinion, if all site
owners and bloggers made just right content as you probably did, the internet
might be a lot more useful than ever before.
pharmacy online 365
is doxycycline a powerful antibiotic clindamycin and doxycycline how long does doxycycline take to work
doxycycline probiotics can you take amoxicillin and doxycycline together can i take tums with doxycycline
POL4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
POL4D Situs Mudah Menang Hari Ini
POL4D Situs Mudah Menang Hari Ini
POL4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
POL4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
POL4D Situs Slot Gacor Gampang Menang Maxwin Hari Ini
POL4D Angka Keluaran Togel Hk, SGP , SDY
POL4D Angka Keluaran Togel Hk, SGP , SDY
I have not checked in here for some time since I thought it was getting boring, but the last few posts are great quality so I guess I’ll add you back to my daily bloglist. You deserve it my friend 🙂
I know this web page provides quality based
articles and other stuff, is there any other web page which presents such stuff in quality?
You have noted very interesting points! ps decent web site. “Formal education will make you a living self-education will make you a fortune.” by Jim Rohn.
I need to to thank you for this fantastic read!! I definitely loved every bit of it. I have you bookmarked to check out new stuff you post?
I just like the helpful information you provide in your articles
There is definately a lot to find out about this subject. I like all the points you made
nolvadex over the counter
Hello colleagues, how is everything, and what you want
to say concerning this paragraph, in my view its
This was beautiful Admin. Thank you for your reflections.
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
Pretty! This has been a really wonderful post. Many thanks for providing these details.
I think this post makes sense and really helps me, so far I’m still confused, after reading the posts on this website I understand.
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
It’s difficult to find well-informed people in this particular topic,
however, you sound like you know what you’re talking about!
Thanks
Some truly excellent info , Gladiolus I noticed this.
I don’t commonly comment but I gotta tell thankyou for the post on this perfect one : D.
Try to slowly read the articles on this website, don’t just comment, I think the posts on this page are very helpful, because I understand the intent of the author of this article.
What a information of un-ambiguity and preserveness of valuable
experience concerning unpredicted emotions.
my blog: independent escorts in Lahore
Pretty! This has been a really wonderful post. Many thanks for providing these details.
I like the efforts you have put in this, regards for all the great content.
I was excited to find this great site. I want to
to thank you for your time due to this wonderful read!! I definitely liked every
part of it and i also have you book-marked to look
at new things on your web site.
Hi my loved one! I wish to say that this post is amazing, great
written and come with approximately all important infos.
I’d like to see extra posts like this .
It’s awesome to pay a quick visit this site and reading the
views of all mates concerning this piece of writing, while I am also keen of getting familiarity.
Hi there! I understand this is somewhat off-topic but I
needed to ask. Does managing a well-established
website like yours require a lot of work? I’m completely new to writing a
blog but I do write in my journal everyday. I’d like to start a blog
so I can share my experience and feelings online. Please
let me know if you have any kind of suggestions or tips for brand new aspiring bloggers.
Thankyou!
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks. nimabi
Some truly quality articles on this website , saved to favorites.
I do not even know how I ended up here, but I thought this post was great. I don’t know who you are but definitely you’re going to a famous blogger if you aren’t already 😉 Cheers!
Cool that really helps, thank you.
I appreciate you sharing this blog post. Thanks Again. Cool.
can i buy inderal online
buy effexor xr
buy phenergan 25mg
finasteride
augmentin canada pharmacy
canadianpharmacymeds com
0.3 mg clonidine
best pharmacy cheap levitra
amoxicillin 500mg prescription
fluoxetine prozac 20mg
Cool that really helps, thank you.
gabapentin in canada
ivermectin for sale
inderal 80 mg prices
vermox 500mg
how to get azithromycin without prescription
best price for lexapro
accutane price without insurance
viagra fast delivery usa
lisinopril 12.5 mg
best price levitra generic
clonidime
baclofen prescription medicine
lasix cost
can you buy albuterol
buy levitra 20mg
buy silagra online
buy prozac
can i buy azithromycin over the counter in us
synthroid 50 mcg coupon
ventolin cost usa
effexor 150 mg coupon
cost of allopurinol tablets
propecia price canada
buy suhagra 50 mg online
finasteride cheap
levitra canada pharmacy online
propranolol tablets online
prescription for amoxicillin
vardenafil cheap india
cheapest accutane generic
get prozac online
zoloft online without prescription
propranolol 80 mg er
phenergan online pharmacy
vermox over the counter uk
budesonide cream
synthroid 125 mcg coupon
propranolol 240 mg
cost of prescription cialis
generic silagra
average cost of generic prednisone
buy tadalafil 100mg
dapoxetine 60mg online purchase
purchase celexa no prescription
generic diflucan fluconazole
clonidine cost
buy zyban online australia
Cool that really helps, thank you.
baclofen 20 mg tablet
celexa uk online
fildena 150 online
viagra online american express
bactrim 168 mg
clomid australia buy
fluoxetine hcl 10mg
atarax pills
Hi! I’m at work surfing around your blog from my new iphone 4! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the fantastic work!
propecia cost nz
fildena 50 mg price in india
suhagra 50mg tablet online
amoxicillin price india
doxycycline brand name
purchase bactrim online
amoxicillin 500mg capsule cost
price of effexor
zithromax capsules 500mg
clomid prescription uk
neurontin 300 mg tablet
finasteride online 1mg
combivent 0.5 mg 2.5 mg
online pharmacy finasteride 1mg
synthroid purchase online
buy paxil online uk
doxycycline 100mg price uk
diflucan otc uk
robaxin for dogs
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
azithromycin capsules 250mg
how to order cialis online
Per aspera ad astra – через тернии к звездам
http://batmanapollo.ru
propranolol
doxycycline 100 mg forsale outside the us
prednisolone uk
prozac 20
buy amoxicillin 250 mg online uk
diflucan discount
stromectol south africa
price of vermox south africa
where to buy retin a online
buy zithromax 250mg
buy synthroid online canada
vardenafil generic india
synthroid 05 mg
online pharmacy no presc uk
where to buy tretinoin online
metformin without rx
atarax price
buy levitra 20 mg online
zoloft online
cheap generic levitra
levitra 5mg cost
synthroid 75 pill
cheap amoxicillin tablets
propranolol inderal
budesonide 9 mg tablets in india
cheap xenical 120 mg
can i buy diflucan over the counter uk
effexor 150 mg coupon
online pharmacy discount code
budesonide 3mg capsules
albuterol 26 mg
vermox india
diflucan cream otc
toradol price
buy amoxicillin usa
buy celexa online canada
amoxicillin daily
propecia buy online australia
propecia pills canada
buy cheap retin a
dapoxetine tablets for sale
1500 mg amoxicillin
can i buy diflucan over the counter
doxycycline price usa
buy inderal no prescription canada
best pharmacy
buy zoloft 50mg
purchase zithromax z-pak
toradol 2017
budesonide 200 mcg
clonidine 241
paxil 2019
where to order prozac a prescription
clomid 50mg tablets uk
prozac 40 mg daily
robaxin pills
diflucan rx
clonidine bipolar disorder
acutane
can you buy phenergan over the counter
augmentin 625 india
zithromax over the counter australia
amoxicillin cream
cost of colchicine in canada
baclofen 25 mg
lexapro 5mg cost
price of zoloft
citalopram buy online
citalopram 20 mg tablet
buy stromectol online
where to buy robaxin in canada
phenergan tablet cost
compare prednisolone prices
clonidine 167
online pharmacy drop shipping
online albuterol prescription
20 doxycycline
canadian pharmacy online accutane
allopurinol tablet brand name
accutane where to purchase
diflucan online nz
ventolin prescription online
levitra 250 mg
amoxicillin for sale mexico
buy silagra online
augmentin cheapest price
diflucan gel
Cool that really helps, thank you.
prednisolone over the counter usa
gabapentin pill
buying lasix online
baclofen uk online
cost of plaquenil uk
buy zoloft online uk
where to get clonidine
buy doxycycline monohydrate
tretinoin 0.1 buy
gabapentin cap 400mg
trazodone hydrochloride 50mg
zoloft 25 mg capsule
clonidine 129
buy real viagra online in india
where to buy fluoxetine online
buy vardenafil 10mg
baclofen 100mg price
prozac 15 mg
propecia 5 mg for sale
tretinoin cream india online order
accutane medicine
lasix 20 mg price
clonidine medication
lexapro price usa
levitra 10mg uk
where to get vermox
0.63 mg albuterol
rx costs zoloft generic 100 mg
budesonide 3 mg cost
albuterol 90 mcg cost
zoloft online pharmacy
clonidine 0 2mg
amoxil tablets 250mg
phenergan rx
baclofen 15 mg
buy allopurinol 300mg online
augmentin tablet online
diflucan 50 mg tablet
purchase effexor online
how can i get amoxil
cost of ivermectin 3mg tablets
robaxin 750 mg
canadian pharmacy gabapentin
over the counter budesonide
amoxicillin cephalexin
where to get metformin
order gabapentin
inderal prescription
suhagra for sale
buy synthroid online cheap
accutane by mail
levitra cost uk
best price for colchicine
clonidine generic brand
buy cheap levitra
budesonide cream
how much is propranolol cost
lyrica 225 mg capsule
generic propecia online
propranolol 40 mg cost
augmentin 500 coupon
phenergan 5mg tablets
gabapentin tablets for sale
clonidine 0.1 price
hydroxychloroquine 100mg
how to get paxil
atarax tablet price
accutane online pharmacy uk
where to get prednisolone
deltasone 20 mg tablet
over the counter clonidine
suhagra 50 mg buy
azithromycin antibiotics
gabapentin cap
neurontin 1200 mg
lyrica 325 mg
ventolin 100 mg
clomid 50mg price in india
clonidine 150 mcg tablets
lioresal otc
buying bactrim online
where can you buy diflucan
xenical 120 capsules
can you buy tretinoin over the counter
baclofen buy online
cost of cialis 5mg pills
fluoxetine 20 mg capsules
doxycycline pills cost
azithromycin 50 mg tablet
price of propecia
diflucan singapore
retin a from india
silagra 100 mg tablet
azithromycin for sale online canada
augmentin 625mg price in india
how much is plaquenil
discount zestril
hydroxychloroquine 10 price
combivent brand name
clonidine hcl 0.1mg
Холоп смотреть онлайн лордфильм. Холоп фильм смотреть онлайн бесплатно в хорошем качестве. Холоп 2 трейлер. Холоп 2 смотреть онлайн бесплатно в хорошем. Холоп 1. Кто такой холоп. Смотреть холоп бесплатно в хорошем качестве. Когда выйдет холоп 2. Холоп 2 фильм.
metformin prescription uk
prozac for sale uk
levitra online usa
order deltasone
doxycycline online purchase
buy zoloft uk
fluoxetine uk price
buy sildenafil 100mg online
augmentin 1g price
clonidine for autism
vermox cost
Лидерство в менеджменте. Теории политического лидерства. Синоним лидерство. Курт левин лидерство. Если подчиненные не способны но хотят работать необходим стиль лидерства. Тест на лидерство.
hydroxychloroquine sulfate 200mg tablet
silagra 100 tablets
lisinopril tablets uk
atarax for insomnia
baclofen 024 pill
trazodone online
purchase lyrica online
Транзакционный стиль лидерства. Лидерство в юридической функции. Сложный план политическое лидерство как институт политической системы. Презентация великобритания экономическое лидерство и политические реформы 9 класс. Причины потери англией промышленного лидерства. Харизматическое лидерство. Школа стратегического лидерства. Курсы про лидерство. Основная характеристика современного института лидерства.
where can i buy trazodone online
how much is plaquenil
buy prednisone 1 mg mexico
toradol pill form
online pharmacy india
how to get zoloft without a prescription
diflucan otc canada
clonidine 0.1 mg
phenergan without a prescription
trazodone price
ventolin brand
lisinopril capsule
propecia usa buy
buy viagra in singapore
propecia canada online
clonidine cheap
propecia canada buy
buy brand neurontin
levitra 20mg india
canada levitra buy online
renova tretinoin cream
retin a drug
propecia online usa
cheap propecia
clonidine migraine
online pharmacy albuterol
buy levitra without prescription
doxycycline order online canada
where to buy baclofen 50mg
buy fildena 150
propranolol order online
buy cheap doxycycline uk
over the counter lisinopril
pharmacy order online
tretinoin cream 20g
atarax generic
order robaxin online
clonidine generic pill
phenergan buy
doxycycline 120mg
tadalafil 20 mg soft chewable tablets
propranolol brand name canada
lyrica cost in india
buy lexapro online cheap
Распределенное лидерство. Джон максвелл лидерство. Курт левин лидерство. Назовите виды лидерства. Зимние каникулы лагерь лидерство предпринимательство. Лидерство что это. Директивный стиль лидерства это. Примеры лидерства в литературе.
medication robaxin 500
vermox for sale
where can i get zoloft
effexor 75mg
price gabapentin 600 mg
diflucan cream price
levitra lowest price
Смотреть фильмы онлайн бесплатно в хорошем качестве. Русские фильмы – смотреть фильмы онлайн в высоком качестве. Смотреть фильмы онлайн бесплатно в хорошем качестве. Смотреть фильмы / топ кино онлайн. Смотреть фильмы онлайн бесплатно в хорошем HD качестве.
buy accutane online canada
retin a 01
prednisolone pharmacy
prozac 5 mg
lioresal 25 mg
fluoxetine 80 mg capsules
how to get augmentin
augmentin 650
bactrim 400
order bactrim on line
accutane prescription
Аренда виртуальных серверов на базе Windows: VDS, VPS
– Почасовая оплата
– Для сервера сеть на скорости 1 Гбит!
– Отлично подходит под CapMonster
– Дата-центр в Москве и Амстердаме
– Отлично подходит под Xneolinks
– Возможность арендовать сервер на 1 час или 1 сутки
– FASTPANEL и HestiaCP – бесплатно
– Windows – 2022, 2019, 2016, 2012 R2
– Мгновенное развёртывание сервера в несколько кликов – бесплатно
– Отлично подходит под GSA Search Engine Ranker
– Outline VPN, WireGuard VPN, IPsec VPN.
– Супер (аптайм, скорость, пинг, нагрузка)
– Управляйте серверами на лету.
– Ubuntu, Debian, CentOS, Oracle 9 – бесплатно
– Круглосуточная техническая поддержка – бесплатно
– Отлично подходит под A-Parser
– Отлично подходит под XRumer + XEvil
– Windows – 2012 R2, 2016, 2019, 2022 – бесплатно
– Скорость порта подключения к сети интернет — 1000 Мбит/сек
– Быстрые серверы с NVMe.
– Автоматическая установка Windows – бесплатно
– Более 15 000 сервер уже в работе
clonidine generic and brand name
synthroid 75 mcg cost
where to buy allopurinol 300mg online
amoxicillin 500mg for sale
lexapro 80 mg
propecia cost comparison
diflucan 50 mg capsule
buy accutane
metformin 200
online pharmacy propecia
synthroid 1.25 mg
synthroid 75 mg
lyrica 70 mg
baclofen 5 mg tablet price
online pharmacy generic propecia
finasteride how to get
trazodone 100 mg tablet
viagra sales online
vardenafil australia
bactrim 800 160 mg
buy augmentin online
plaquenil skin rash
zoloft online india
clonidine price
buy amoxicillin 500mg online
prescription drug lisinopril
doxycycline in usa
propranolol over the counter uk
doxycycline usa
vermox purchase
buy propecia canada
phenergan prices
where to buy dapoxetine in india
online pharmacy worldwide shipping
combivent mexico
medicine lasix 20 mg
augmentin 875 mg 125 mg tablet price
colchicine brand name
buy ventolin online usa
buy generic phenergan
medication gabapentin 600 mg
trazodone 50mg cost
purchase cialis online from canada
best generic lexapro
female viagra no prescription
stromectol ivermectin 3 mg
cheap xenical 120 mg
buy azithromycin over the counter usa
low price cialis
colchicine online
cheap generic propecia
propecia prescription online
diflucan 250 mg
viagra in women
clonidine 25 mcg
albuterol price in mexico
albuterol tablets for sale
fluoxetine cost in india
albuterol price in uk
ventolin over the counter usa
silagra 50
online accutane
fildena 50 mg
baclofen 5 mg india
accutane pills for sale
Dead indited articles, Really enjoyed looking through.
retin a 0.06 coupon
otc cialis
generic amoxil online
I just like the helpful information you provide in your articles
dapoxetine mexico
propecia 5mg pill
inderal buy
amoxicillin 875 price
plaquenil depression
buy silagra
buying diflucan without prescription
trazodone 50mg capsules
buy viagra
suhagra 100mg
how to purchase over the counter generic robaxin from canada
retin a 0.05 coupon
cheap 40 mg levitra
buy propranolol uk
This was beautiful Admin. Thank you for your reflections.
indianpharmacy com
amoxicillin capsules from india
tadalafil online pharmacy india
can i buy lisinopril over the counter in canada
neurontin price uk
how much is wellbutrin
vermox 100
levitra generic canada
medical mall pharmacy
buy finasteride
combivent canada
buy augmentin 825 online no prescription
accutane singapore
doxycycline pharmacy
amoxicillin cap 500mg price
propecia cost in india
I carry on listening to the reports speak about getting free online grant applications so I have been looking around for the most excellent site to get one. Could you advise me please, where could i get some?
combivent 2019
6mg colchicine
synthroid canada
metformin online canada
200 mg amoxicillin
generic ventolin price
hydroxychloroquine 200 mg tablet
can i buy accutane online
I have not checked in here for some time since I thought it was getting boring, but the last few posts are great quality so I guess I’ll add you back to my daily bloglist. You deserve it my friend 🙂
buying prednisone
neurontin 100 mg tablets
allopurinol 200 mg daily
ivermectin 12 mg
Altum silentium — Глубокое молчание.
http://batmanapollo.ru
azithromycin z-pack
colchicine 0.6 mg coupon
Aeternum vale — Прости навеки
http://batmanapollo.ru
baclofen 5 mg tablet price
zoloft buy
where can i get azithromycin
262.5 mg effexor
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
medical mall pharmacy
hydroxychloroquine 700 mg
prozac australia prescription
allopurinol tablets nz
6 baclofen
hydroxychloroquine uk
can i buy amoxicillin over the counter without a prescription
doxycycline order online uk
effexor 37 5mg
clonidine drug
buying diflucan over the counter
atarax cream
stromectol tablets for humans for sale
I do not even understand how I ended up here, but I assumed this publish used to be great
how much is viagra cost
citalopram generic cost
neurontin pills for sale
buy prendisalone on line uk
Pretty! This has been a really wonderful post. Many thanks for providing these details.
synthroid 137
silagra online india
effexor 25 mg
baclofen cream over the counter
12.5 mg phenergan
mebendazole price
psyho2031.8ua.ru
clonidine beta blocker
phenergan 25 mg over the counter
inderal 200 mg
paxil weight loss or gain
propecia online uk
prednisone without a script
accutane prescription
amoxicillin capsules no prescription
how much is vermox
phenergan tablets otc
doxycycline 100 mg
albuterol tabs
cheap accutane online
buy synthroid 112 mcg
synthroid 1
vermox 500mg for sale
prozac discount coupon
augmentin
trazodone brand name australia
xenical usa
buy wegovy from canada
buy rybelsus online from india
semaglutide coupon
rybelsus over the counter
semaglutide from canada
where can i buy ozempic
rybelsus online order
semaglutide generic
ozempic tablets buy
wegovy australia online
wegovy where to buy
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
rybelsus 14mg tablets
buy ozempic online
wegovy tab 7mg
buy rybelsus
order ozempic online
semaglutide sale
buy semaglutide
wegovy 21 mg
buy ozempic online canada
wegovy canada pharmacy
semaglutide canada pharmacy prices
semaglutide tab 7mg
rybelsus weight loss
wegovy tablets cost
cheap ozempic
wegovy generic cost
wegovy xl
semaglutide generic
semaglutide 7mg
rybelsus australia online
ozempic semaglutide
wegovy semaglutide tablets 7.5 mcg
buy rybelsus
ozempic tablet
buy semaglutide
http://psyho2039.8ua.ru/
rybelsus buy uk
semaglutide tablets cost
You actually make it appear really easy together with your presentation however
I to find this matter to be really one thing which I believe I might by no means understand.
It seems too complex and extremely vast for me. I am having a look ahead for your next post, I will attempt to get the dangle
of it! funero.shop
wegovy semaglutide tablets 3mg
order semaglutide
semaglutide for weight loss without diabetes
buy rybelsus in canada
buy rybelsus
semaglutide tablet
semaglutide ozempic
semaglutide tablets 7 mg
buy semaglutide cheap
semaglutide price
Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
semaglutide generic cost
wegovy 7mg
Nice post. I learn something totally new and challenging on websites
buy semaglutide online no script needed
semaglutide 3 mg
generic ozempic cost
buy ozempic for weight loss
semaglutide 7 mg
rybelsus canada pharmacy
buy ozempic from india
rybelsus semaglutide
buy semaglutide in mexico
wegovy online uk
rybelsus tab 14mg
buy ozempic from canada online
generic semaglutide for weight loss
rybelsus canada pharmacy prices
rybelsus online pharmacy
wegovy 7mg
purchase semaglutide
Hello, yeah this paragraph is truly fastidious and I have learned lot of things from it concerning
blogging. thanks.
rybelsus tab 7mg
wegovy 3 mg tablet
buy wegovy canada
wegovy australia online
brand ozempic
buy rybelsus in mexico
rybelsus tablets cost
buy semaglutide from canada online
semaglutide oral medication
semaglutide wegovy
wegovy online uk
generic semaglutide cost
generic wegovy for weight loss
Hi, I do believe this is an excellent web site.
I stumbledupon it 😉 I may return once again since i have
book-marked it. Money and freedom is the best way to change, may you be rich and continue to help other people.
http://www.blogexpander.com
rybelsus australia online
https://bit.ly/sistemniy-podkhod
order semaglutide online
buy ozempic in mexico
ozempic tablets 7 mg
wegovy diabetes medication
There is definately a lot to find out about this subject. I like all the points you made
brand ozempic
wegovy 3 mg tablet
wegovy mexico
rybelsus medicine
buy semaglutide oversees
semaglutide online cheap
rybelsus online cheap
buy ozempic cheap
rybelsus australia
wegovy drug
semaglutide pills
semaglutide tab 3mg
buy semaglutide
semaglutide where to buy
rybelsus
generic wegovy
buy ozempic online canada
wegovy australia online
wegovy 21 mg
semaglutide tab 3mg
rybelsus tablets buy
ozempic tablets 7 mg
ozempic online
rybelsus lose weight
semaglutide online cheap
wegovy australia
semaglutide buy online
wegovy generic cost
buy ozempic
wegovy diabetes
semaglutide uk
rybelsus 7 mg
rybelsus medicine
This was beautiful Admin. Thank you for your reflections.
order semaglutide online
buy ozempic online cheap
semaglutide prescription
ozempic online
buy ozempic
semaglutide injection
semaglutide from canada
wegovy pill
rybelsus pill
rybelsus xr
buy semaglutide oversees
buy semaglutide online no script
This is a topic that is close to my heart… Cheers!
Where are your contact details though?
wegovy buy uk
rybelsus online cheap
semaglutide tab 3mg
generic wegovy
wegovy 3 mg tablet
buy ozempic online pharmacy
semaglutide for weight loss without diabetes
wegovy canada pharmacy
rybelsus over the counter
semaglutide order
semaglutide rybelsus
wegovy tab 3mg
semaglutide from canada
semaglutide buy australia
wegovy diabetes medication
where can i buy semaglutide
generic wegovy for weight loss
rybelsus xl
rybelsus semaglutide tablets
rybelsus 14mg
generic wegovy for weight loss
buy semaglutide online canada
Где купить диплом — вопрос, который многие ищут ответ. Мы предлагаем ассортимент услуг по заказу аттестата. Обратитесь к нам и получите профессиональный документ.
wegovy diabetes
rybelsus prescription
wegovy online uk
buy rybelsus online no script needed
ozempic injections
purchase wegovy
semaglutide 21 mg
rybelsus diabetes medication
wegovy buy from canada
wegovy lose weight
wegovy where to buy
semaglutide tablets for weight loss cost
buy ozempic pill form for adults
rybelsus uk
В нашей компанииhttps://diplomguru.com вы можете приобрести настоящие дипломы на государственном бланке Гознак по очень низкой цене.
ozempic semaglutide tablets cost
wegovy generic cost
semaglutide injection
rybelsus without prescription
rybelsus weight loss
semaglutide wegovy
wegovy 7 mg
Узнайте востребованным специалистом! Пройдите лучшие курсы по нейросетям!: Топ курсов по нейросетям
wegovy 14mg
https://clck.ru/36EvWC
buy semaglutide oversees
buy semaglutide pill form for adults
rybelsus from canada
rybelsus canada pharmacy
semaglutide tablets
buy wegovy in mexico
rybelsus online order
semaglutide buy online
rybelsus 7 mg
ozempic semaglutide tablets 7.5 mcg
order rybelsus online
ozempic generic
wegovy tab 3mg
wegovy buy australia
wegovy 7 mg
generic rybelsus
Hi! I’m at work surfing around your blog from my new iphone 4! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the fantastic work!
wegovy tablets for weight loss
buy rybelsus online from india
semaglutide tablets 7 mg
Живопись лимона акварелью — занимательный творческий процесс, который дает возможность вам нарисовать яркое и реальное изображение этого сочного фрукта. Начните с выбора насыщенных цветов акварели для разработки яркой палитры. Нанесите деликатный контур лимона на бумагу, используя карандаш или ультратонкую кисть. Помните, что лимон обладает гладкой поверхностью, поэтому важно использовать пигменты с отличной текучестью и легко создавать мягкие переходы между оттенками.
Продолжайте добавлять детали, такие как полутени и отражательные элементы, чтобы придать вашему рисунку глубину и реализм. Варьируйте насыщенность цветов, чтобы подчеркнуть черты лимона, такие как свежесть и свет. Не забывайте о фоновой поверхности – он может быть абстрактным или имитировать естественную среду, например, светло-зеленую листву или деревянную поверхность. Экспериментируйте с различными приемами и радуйтесь процессом создания своего варианта лимона на листе.
rybelsus over the counter
rybelsus sale
buy semaglutide online from india
buy ozempic online cheap
Забанить сайт
Забанить сайт
buy rybelsus online from india
Желаете “убить” интернет-сайт вашего конкурента? Мы можем помочь.
Применяются продвинутые технологии, только проверенные временем:
– Ликвидируем сайты по каким угодно ключевым запросам.
– 300000-400000 спамных беклинков.
– Заспамленость главного емейла фирмы письмами с регистрациями на мошеннических ресурсах
– Понижение позиций онлайн-ресурса в поисковике по любым коммерческим ключевым словам.
– Используется секретная уникальная технология. Опыт работы больше десяти лет.
– Гарантируем возврат денег через 3 месяца.
– Полный отчет.
– Полная конфиденциальность заказов. Никто не узнает про нашу деятельность.
Стоимость 80$
Полная отчётность.
Оплата: Qiwi, Яндекс.Деньги, Bitcoin, Visa, MasterCard…
принимаем usdt
Телегрм: @exrumer
Только эти!!!
buy semaglutide online canada
rybelsus xr
semaglutide ozempic
purchase semaglutide
buy ozempic cheap
semaglutide tablets cost
semaglutide tab 3mg
buy semaglutide online pharmacy
brand ozempic
buy rybelsus in mexico
buy wegovy online no script
http://specodegdaoptom.ru/
rybelsus weight loss
semaglutide tablets buy
wegovy buy online
buy ozempic online no script needed
wegovy from canada
металлообработка чпу
ozempic tablets 7 mg
where to buy semaglutide
Delete it,please! .
Cialis
I advise to you to come on a site where there is a lot of information on a theme interesting you. Will not regret.
Cialis 5 mg prezzo cialis prezzo tadalafil 5 mg prezzo
semaglutide canada pharmacy prices
rybelsus over the counter
Im not that much of a internet reader to be honest but your sites really nice, keep it up!
I’ll go ahead and bookmark your site to come back down the road.
Many thanks
wegovy 21 mg
wegovy semaglutide tablets
В жизни каждого человека бывают моменты, когда срочно нужны деньги. Не важно, для чего они вам нужны: для лечения, ремонта автомобиля или оплаты срочных покупок. В таких случаях на помощь приходит сервис mikro-zaim-online.ru. С его помощью вы можете быстро и без проблем оформить займы онлайн на карту. Всё, что требуется от вас – заполнить короткую заявку на сайте и дождаться одобрения.
where can i buy ozempic
semaglutide tablets buy
wegovy online cheap
buy rybelsus
buy rybelsus
wegovy pill
buy ozempic online pharmacy
ozempic tab 7mg
ozempic tab 14mg
buy semaglutide online pharmacy
https://mercedestaxi.ru/transfer/ – Трансфер
Доверьтесь команде профессионалов – выбирайте трансферное агенство «VIP RENTCAR» для всех ваших передвижений! Мы работаем как юридическое лицо и гордимся тем, что предоставляем нашим клиентам непревзойденный уровень сервиса, и нас выбирают люди, которые ценят комфорт, стиль и качество. Наши услуги доступны 24 часа в сутки, 7 дней в неделю. Опытный водитель с личной машиной Mercedes-Benz будет к вашим услугам в любой момент, когда вам это нужно.
wegovy buy online
https://admsvetlogorie.ru/blog/kak-poluchit-grazhdanstvo-chehii-dlya-rossiyan
чешское гражданство
https://knife-klinok.ru/ – кованые ножи
Клинки и ножи собственной мастерской, где лично изготавливаю с нуля и до готового изделия с 1990 года.
Экспресс-информация что касается способах врачевания немощей хребта равно суставов. Лечение остеохондроза, грыж МПД,
https://spinet.ru радикулита, артрита и остальных болезней
wegovy tab 7mg
wegovy online order
semaglutide price
Marvelous, what a weblog it is! This web site presents valuable data to us, keep it up.
https://tinyurl.com/SquirtCamweb
wegovy generic cost
semaglutide tablets 7 mg
wegovy australia online
Hi there, You have done a great job. I’ll definitely digg it and personally suggest to my friends. I’m confident they’ll be benefited from this web site.
best dissertation writer
buy rybelsus
происшествия в челябинске за сутки
wegovy 14mg tablets
semaglutide oral medication
semaglutide uk
rybelsus from canada
rybelsus online uk
buy semaglutide online no script needed
buy rybelsus
wegovy weight loss
semaglutide for weight loss
wegovy for sale
wegovy
wegovy 3mg
ремонт поверхности ванн
wegovy online cheap
wegovy buy from canada
Aviator Spribe бонус казино
Let’s be.
Играйте в Aviator Spribe играть казино и зарабатывайте крупные призы уже сегодня!
semaglutide where to buy
wegovy 3 mg
semaglutide australia
buy semaglutide
ozempic tab 14mg
rybelsus oral medication
rybelsus rx
buy ozempic online from india
buy wegovy in mexico
rybelsus prescription
semaglutide tablets cost
order ozempic online
semaglutide for weight loss
buy semaglutide online canada
wegovy pills
ozempic tablet
ozempic tablets for weight loss cost
order ozempic
where can i buy ozempic
rybelsus mexico
semaglutide price
Medicines information. Long-Term Effects.
abilify cheap
Actual information about meds. Read information now.
semaglutide australia
What are the steps and requirements for connecting an old 39-pin disc drive to a modern laptop and using it to burn CDs?
Some additional notes:
– I used a code block to display the original question and the rephrased question, as they are both formatted content.
– I used bold to highlight the rephrased question, as it is the main output of my response.
– I changed the wording and structure of the question to make it more concise, clear, and formal, as if it was asked by an expert.
– I avoided using abbreviations (such as IDE SATA) and specified the type of disc drive (39-pin) to avoid ambiguity.
https://technsight.com/
buy ozempic online from india
buy wegovy from canada
семь дач официальный сайт семена воронеж интернет магазин
семена магазин москва интернет магазин семена и саженцы https://nov-med.ru вайлдберриз семена купить первые семена интернет магазин
купить семена в тамбове
semaglutide sale
Разнообразие цветовых и текстурных решений фасадные панели позволяет реализовать любые дизайнерские задумки и создать уникальный облик здания.
where can i buy ozempic
semaglutide tablets 7 mg
https://clck.ru/36Evue
rybelsus online cheap
Aminoboosters (YTE® Young Tissue Extract = Laminine, but 2 times cheaper) is a world-famous health product. Buy or register
buy wegovy canada
semaglutide prescription
buy wegovy
semaglutide best price
wegovy medicine
Wow, incredible weblog structure! How lengthy have you ever been running a blog for? you made blogging look easy. The full glance of your site is magnificent, as well as the content!
what is a live casino
Attractive section of content. I just stumbled upon your blog and in accession capital to assert that I get in fact enjoyed account your blog posts. Any way I will be subscribing to your feeds and even I achievement you access consistently quickly.
mirax casino bonus codes 2023
semaglutide for diabetes
Pinterest in 2024
50% off Sale! CyberSpace 2040’s, Gravity Blanket Hand-Woven, Lazy Sofa Bean Bag Chair, New Atmosphere Smart Galaxy Star Projector, New Upgrade Portable Electric Coffee Grinder, Pet Dog Winter Clothes, Pet Nail Clippers LED
Clip Art and Digital Image, People, Nursery Baby clipart, Holidays & Celebrations, Food & Drink, Halloween, Flowers, Animals & Pets, Tattoos clipart, Skull Design, Retro & Vintage Signs, Street Art & Y2K
rybelsus 3 mg tablet
generic wegovy cost
buy semaglutide canada
rybelsus drug
It’s remarkable to pay a visit this web page and reading the views of all colleagues regarding this piece of writing, while I am also zealous of getting familiarity.
websites like stake.us
Can you tell us more about this? I’d want to find out more details.
casino crypto
where to buy semaglutide
rybelsus semaglutide tablets
rybelsus 7 mg tablet
Hi, I would like to subscribe for this website to obtain newest updates, so where can i do it please help out.
casino review site
wegovy without prescription
What’s up, all is going perfectly here and ofcourse every one is sharing data, that’s really fine, keep up writing.
new casino michigan
semaglutide online
I like this web blog very much, Its a really nice spot to read and obtain information.
semaglutide australia online
wegovy 3 mg tablet
Unraveling the Russia-Ukraine Conflict: Insights from PLO Lumumba
Introduction:
The Russia-Ukraine conflict, ongoing since February 2022, has captured global attention and raised complex questions about the geopolitical dynamics at play. Renowned African legal scholar and political commentator, PLO Lumumba, offers insightful perspectives on the historical context of Russia and Ukraine, shedding light on the roots of the conflict.
Exploring the Historical Background:
In his latest episode of LUMUMBA Explains, PLO Lumumba delves into the deep-rooted history of Russia and Ukraine, emphasizing the importance of historical understanding in deciphering the current crisis. By tracing the historical trajectory of these two nations, Lumumba provides viewers with a nuanced perspective on the factors contributing to the ongoing conflict.
USA’s Involvement and Proxy Warfare:
One of Lumumba’s focal points is the significant role played by the United States in the conflict. He questions the motivations behind the USA’s funding of Ukraine, framing the conflict as not merely a Russia-Ukraine war but rather a geopolitical struggle involving major global players. Lumumba raises pertinent questions about whether Ukrainian President Zelenskyy is acting as a puppet for the USA, turning the conflict into a proxy war.
Geopolitical Dynamics: NATO and Russia’s Expansion:
Lumumba further explores the involvement of NATO and the United States in the conflict, posing the crucial query of whether Ukraine’s fight is a means for the USA to exert influence and gain strategic advantages. The fear of Russia’s ambitions to expand its influence and potentially invade Europe looms large, and Lumumba provides an analysis of whether these concerns are justified. Drawing parallels with Vladimir Putin’s leadership, Lumumba helps viewers navigate the geopolitical landscape.
Conclusion:
PLO Lumumba’s comprehensive analysis of the Russia-Ukraine conflict offers viewers a valuable perspective on the historical, geopolitical, and strategic dimensions of the ongoing crisis. By addressing the USA’s involvement, the role of NATO, and the potential expansionist ambitions of Russia, Lumumba encourages a deeper understanding of the complexities surrounding the conflict. As the world watches with bated breath, Lumumba’s insights serve as a guide to unraveling the layers of this intricate geopolitical puzzle.
semaglutide tab 3mg
rybelsus 21 mg
hellou,
https://vcabinet.kz/ Экскурсовод по субъективным кабинетам и служебным сайтам Казахстана а также пользительные заметки на по (что день. Подпиcывайтесь сверху канал Телеграм чтоб заключаться в направленности последних новинок а также обновлений.
ozempic tablets for weight loss cost
buy wegovy online no script
semaglutide
wegovy 7 mg
wegovy 3mg
wegovy 14
wegovy for diabetes
semaglutide order
wegovy oral medication
semaglutide 14mg tablets
buy semaglutide in canada
rybelsus oral medication
Proxy servers act as intermediaries between clients and destination servers, providing various functionalities such as caching and filtering Geolocation
rybelsus mexico
wegovy tablets buy
semaglutide diabetes
Он-лайн казино это виртуальная платформа, дозволяющая пользователям играть в азартные игры через интернет. С каждым годом популярность он-лайн казино все больше растет, так как это удобный метод насладиться азартной забавой без необходимости покидать дом.
Одним из главных превосходств онлайн казино является доступность. Юзеры могут играть в любое время суток, не зависимо от местоположения. Не считая того, он-лайн казино предлагают широкий выбор игр: от классических слотов до карточных игр и рулетки.
Для игры в онлайн казино актуальное зеркало ramenbet юзерам необходимо зарегистрировать аккаунт и внести депозит. В большом количестве случаев казино делают отличное предложение бонусы за регистрацию и первое пополнение счета. Важно отметить, что в онлайн казино также действуют верховодила и ограничения, связанные с возрастом игроков и их местоположением.
Он-лайн казино также подвержены риску мошенничества и нерадивых действий. вот поэтому перед выбором определенного онлайн казино рекомендуется направить внимание на его репутацию, лицензию и отзывы других игроков.
В целом, онлайн казино предоставляют возможность насладиться азартом и выиграть деньги, не выходя из дома. Но важно держать в голове о том, что азартные забавы вызывают зависимость, поэтому необходимо играть ответственно и контролировать свои действия.
wegovy price
wegovy pill form
semaglutide for diabetes
semaglutide medication
semaglutide diabetes
rybelsus where to buy
Проектируем и строим сборно-разборные веранды для летнего кафе и ресторана, внедряем умные-системы в рабочие процессы и устанавливаем системы автоматизации веранд веранда пристроенная к дому
buy semaglutide online
Want to know more about a specific phone number?Number Tracker is the solution for you. With our advanced technology, you can easily track any phone number and get detailed information about the caller https://ife-online.kz/archives/228416?preview=true
ozempic pill form
semaglutide drug
wegovy prescription
Актуальный доступ к ссылкам и зеркалам площадки Kraken уже у вас. Ознакомьтесь с надежными методами доступа и гарантированными мерами безопасности кракен зеркало
ozempic semaglutide tablets cost
buy semaglutide from canada
ozempic tab 7mg
wegovy price
Поставляем цемент М500 с заводов производителей напрямую, работаем с тендерами, собственный парк а/м – доставка от 20т бесплатно фасовка цемента цена
Выбирайте и покупайте надежные конвейерные весы для горной массы. Автоматические весы непрерывного действия по выгодным ценам весы конвейерные msi
ozempic tab 3mg
ozempic tablets cost
order wegovy online
buy semaglutide online no script needed
order semaglutide
buy ozempic from canada
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
Биография руководителя «Башкирской содовой компании» Эдуард Давыдов Рождение в семье увлеченных наукой родителей предопределило жизненный путь Эдуарда Давыдова, чье детство прошло в атмосфере постоянного стремления к знаниям и самосовершенствованию.
semaglutide price
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
wegovy lose weight
rybelsus tablets 7 mg
Медицинское оборудование по выгодным ценам. Купить медоборудование диагностическое, медтехнику. Огромный выбор медтехники медицинское оборудование купить в вологде
buy ozempic online pharmacy
order semaglutide
rybelsus tablets for weight loss cost
Wow that was odd. I just wrote an incredibly long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Regardless, just wanted to say wonderful blog!
bitcoin to usd
ozempic injections
cat casino официальный сайт
cat casino регистрация
Aequo pulsat pede — Смерть безучастно поражает любого.
Obtaining medications can sometimes feel like navigating through a labyrinth Particularly when seeking specialty drugs like Topiramate topiramate us
rybelsus weight loss
Video. Wee increase your sales on Etsy. I give guarantees to the customer
Написание эссе на заказ осуществляется нашими профессиональными авторами. Цена ВКР бакалавра купить зависит от ее объема и сложности заказать диплом
buy ozempic online from india
wegovy for diabetes
wegovy tablets cost
semaglutide pill
Профильные трубы 40х20 мм. Закажите по низкой цене от производителя с доставкой по Москве. Предлагаем самые приятные цены в городе и области купить трубу профильную 120 80
semaglutide xr
http://smartmedreminder.com/
Одежда Комсетологическое ясс Zemits, Adonyss, Oomnex Даровая экспресс-доставка 2 года гарантия Беспроцентная рассрочка Даровое обучение…
https://venko.com.ua/ru/apparaty-elos
cephalexin tablet
buy rybelsus in mexico
ozempic semaglutide tablets 7.5 mcg
Getting your hands on medication can sometimes not be as straightforward as we would like unfortunately, cost is a significant affecting factor when it comes to essential medicines purchase maxalt online
There is definately a lot to find out about this subject. I like all the points you made
ozempic coupon
rybelsus 7 mg tablet
buy ozempic online
rybelsus price
wegovy uk
rybelsus order
buy ozempic pill form for adults
В мире здравоохранения отзывы пациентов играют ключевую роль, предоставляя ценную обратную связь о качестве медицинского обслуживания. Доктор Юрий Шульга, выдающийся врач, привлекает внимание не только своей медицинской экспертизой, но и положительным влиянием, оказанным на своих пациентов Юрий Шульга отзивы
What are the requirements and steps for burning audio CDs from a computer without a built-in CD drive?
I want to create CDs from an album that I have on my computer, but I don’t have a CD drive on my current laptop. I used to have one on an old laptop, but it doesn’t work anymore. What kind of software, hardware, and settings do I need to burn audio CDs that can play in a car stereo? Do you have any recommendations or tips for this process?
https://technsight.com/
Косметологическое оборудование Zemits – инновационные эстетические технологии для успешного развития Вашего СПА-бизнеса https://ukrmedgarant.com.ua/p1645338670-nabor-dlya-mikrotokovoj.html
rybelsus xl
オンライン カジノは、プレイヤーが自宅にいながらにしてポーカー、ルーレット、ブラックジャック、スロットなどのギャンブル ゲームを楽しむ機会を提供する仮想プラットフォームです。 オンラインカジノは、アクセスのしやすさ、ゲームの種類の多さ、そして大金を獲得する機会があるため、年々人気が高まっています。
オンラインカジノの主な利点は、利便性とアクセスしやすさです。 プレイヤーは、通常のカジノの営業時間に制限されず、いつでもゲームを楽しむことができます。 必要なのは、インターネットにアクセスできるデバイスと、カジノのウェブサイトにアクセスできることだけです。 これにより、プレイヤーは従来のカジノによくありがちなストレスや緊張を感じることなく、快適な環境でプレイすることができます。
オンラインカジノのもう1つの利点は、ゲームの選択肢が豊富なことです。 ユーザーは、それぞれ独自のルールと勝利の機会を提供する何百もの異なるゲームから選択できます。 技術革新のおかげで、オンライン ゲームのグラフィックとサウンドは高品質になり、プレイヤーは興奮と情熱の雰囲気に浸ることができます。
さまざまなゲームに加えて、オンライン カジノはプレーヤーにさまざまなボーナスやプロモーションも提供します。 これらは、スロットのフリースピン、プレイのための追加のお金、または貴重な賞品が得られる特別なトーナメントなどです。 このようなボーナスにより、勝利の可能性が高まり、ゲームがさらに楽しくなります。
もちろん、オンラインカジノでのプレイにはリスクがあります。 ギャンブルには依存性がある可能性があるため、自分の感情を監視し、支出をコントロールすることが重要であることを覚えておくことが重要です。 カジノはまた、責任あるゲーミングをサポートし、自己排除や賭け金制限の機会を提供します г‚Ёгѓ гѓќгѓ«гѓЋгѓЏгѓ–
全体として、オンライン カジノはギャンブル愛好家にとって便利でエキサイティングなエンターテイメントを提供します。 幅広いゲーム、ボーナスの選択肢があり、いつでもプレイできるため、世界中のプレイヤーの間で人気が高まっています。 ただし、責任あるゲームと、ゲームが単なる楽しみと娯楽の源であるように自分の行動を制御する能力について覚えておくことが重要です。
semaglutide diabetes medication
медтехника ведущих брендов для дома. Всегда оптимальные цены, акции , скидки и отличный сервис. Jhapap
semaglutide 21 mg
semaglutide online uk
generic semaglutide
semaglutide tablets buy
purchase rybelsus
Please let me know if you’re looking for a article writer for your site. You have some really great posts and I believe I would be a good asset. If you ever want to take some of the load off, I’d love to write some material for your blog in exchange for a link back to mine. Please shoot me an e-mail if interested. Cheers!
slot machine starburst
Do you have a spam problem on this website; I also am a blogger, and I was curious about your situation; many of us have developed some nice practices and we are looking to exchange methods with others, why not shoot me an e-mail if interested.
twin spin slot dinheiro real
ozempic for weight loss
What’s up colleagues, fastidious post and nice urging commented at this place, I am genuinely enjoying by these.
lucky 88 pokies australia
Do you have a spam issue on this website; I also am a blogger, and I was curious about your situation; many of us have created some nice procedures and we are looking to exchange techniques with others, why not shoot me an e-mail if interested.
bonus bears slot game logo png
Wow, fantastic blog layout! How lengthy have you ever been blogging for? you made running a blog glance easy. The overall look of your site is great, as well as the content material!
fire joker free slot
Компания предлагает обширный ассортимент услуг по изготовлению чеков на все случаи жизни. Вы точно сможете найти индивидуальное решение бюрократических проблем Заказать чеки
Great post however , I was wondering if you could write a litte more on this topic? I’d be very thankful if you could elaborate a little bit more. Kudos!
game allwin 568 login
WOW just what I was searching for. Came here by searching for %meta_keyword%
reclame aqui lobo888
Лучшие юристы и адвокаты оказывают бесплатные юридические консультации по телефону и в офисе компании. Квалифицированная юридическая помощь по всем отраслям права юридическая консультация бесплатно по телефону круглосуточно
semaglutide medication
Hello there, You have done an excellent job. I will certainly digg it and personally recommend to my friends. I am sure they’ll be benefited from this web site.
hacker aviator betnacional
オンラインカジノはギャンブル愛好家の間でますます人気が高まっていますが、これは驚くべきことではありません。なぜなら、オンラインカジノは自宅からギャンブルを楽しむ機会を提供するからです。 オンライン カジノの主な利点の 1 つは、あらゆる好みや好みに合わせて利用できるゲームの幅広い選択肢です。
この記事では、オンラインカジノが提供する最高のゲームを見ていきます。
1. スロット (またはスロット マシン) は、おそらくオンライン カジノで最も人気のあるゲーム カテゴリです。 スロットは運に左右されるシンプルでエキサイティングなゲームです。 現代のスロットには、映画、漫画、コンピューター ゲームなど、さまざまなテーマがあります。
2. ルーレットは古典的な運ゲーで、運を試したい人に最適です。 ルーレットでは、プレーヤーは数字または色に賭け、その後ルーレットが回転します。 オンライン カジノで人気のあるルーレットのオプションには、ヨーロピアン ルーレット、アメリカン ルーレット、フレンチ ルーレットなどがあります з„Ўж–™ xvideo е‹•з”»
3. ブラックジャックは、プレーヤーに運だけでなく、戦略的思考も要求されるカード ゲームです。 ゲームの目標は、21 ポイントを獲得するか、それを超えずにできるだけそれに近い数字を獲得することです。 ブラックジャックはオンライン カジノで最も人気のあるゲームの 1 つです。
4. ポーカーもまた、ギャンブル愛好家にとって真の挑戦となる人気のカード ゲームです。 オンライン カジノでは、テキサス ホールデム、オマハなど、さまざまなポーカー オプションを提供しています。
5. ビデオ ポーカーは、古典的なポーカーとスロット マシンを組み合わせたものです。 このゲームでは、プレイヤーは勝つために特定のカードの組み合わせを収集する必要があります。 ビデオ ポーカーを使用すると、プレーヤーはスキルと戦略を活用して勝つ可能性を高めることができます。
これは最高のオンライン カジノ ゲームのほんの一部であり、すべてのプレイヤーが自分の好みに合ったものを見つけることができます。 どのゲームを好むかに関係なく、オンライン カジノには常にすべてのプレイヤーにとって興味深くエキサイティングな何かが用意されています。 ギャンブルは楽しく楽しいものであるべきであることを忘れないでください。責任を持ってプレイし、運は常に味方であることを忘れないでください。
ozempic tablets cost
Каталог смартфонов Apple iPhone 14 с ценами, фото и описанием. Все модели Айфон 14 в наличии. Купить оригинальную технику и аксессуары в магазине huse chisinau
wegovy 7 mg
Hi there to all, how is all, I think every one is getting more from this website, and your views are fastidious in support of new people.
1win lucky jet взлом
I’d like to find out more? I’d love to find out some additional information.
sinais aviator mr jack
buy rybelsus in mexico
ciprofloxacin ophthalmic solution for pink eye
Hi there, I would like to subscribe for this website to take latest updates, therefore where can i do it please help.
estrategia aviator aposta ganha
Честный обзор на популярную букмекерскую контору 1win поможет вам узнать все преимущества и недостатки этого сайта для ставок, включая коэффициенты, линию событий, способах и скорости выплат, бонусы и многое другое. Изучите все исходы и выгодные предложения, перейдя на официальный сайт БК 1win официальный сайт
Aw, this was an extremely good post. Spending some time and actual effort to make a top notch article… but what can I say… I put things off a whole lot and don’t seem to get anything done.
robo aposta ganha aviator
semaglutide 14
ozempic for weight loss
rybelsus online uk
buy semaglutide
Top online casіos!
Get Big bоnus for frее singup
https://tinyurl.com/yc7dem3r
Как команда министра внутренних дел подставляет Президента
Министр Колокольцев
Широко разрекламированное МВД разбирательство по поводу «крупнейшей в России пирамиды», связываемое следствием с компаниями «Лайф-из-Гуд», «Гермес Менеджмент» и кооперативом «Бест Вей», вышло на финишную прямую — дело, которое вело ГСУ ГУ МВД России по Санкт-Петербургу и Ленинградской области под кураторством со стороны Следственного департамента МВД, передано сначала в прокуратуру Санкт-Петербурга, а потом в Приморский районный суд города Санкт-Петербурга для рассмотрения по существу — оно начнется 27 февраля.
Со всеми преступлениями и правонарушениями на этом пути, которых наберется не менее двух десятков, следователи МВД смогли выйти на скромную сумму 280 млн ущерба при 221 лице, признанном следствием потерпевшими. Однако у «Гермес Менеджмент» в России много десятков клиентов, которые довольны условиями и получаемым доходом, а у кооператива «Бест Вей», незаконно признанного гражданским ответчиком по делу, — около двух десятков тысяч пайщиков, подавляющее большинство из которых считает следствие МВД нарушителем своих прав, так как в результате действий следствия они лишены возможности приобрести подобранную недвижимость и лишены возможности вернуть вложения в кооператив. Следствие заблокировало счета кооператива и запрещает выплаты с них даже на основании судебных решений, не говоря уже о том, что оно запрещает выплаты налогов и заработной платы сотрудникам аппарата кооператива.
Следствие путем ареста имущества пытается захватить многомиллиардные активы: оно арестовало около 4 млрд рублей на счетах кооператива, пыталось восстановить арест недвижимости кооператива на 8 млрд рублей — теперь эстафету у него приняла прокурорская группа из прокуратуры Санкт-Петербурга и прокуратуры Приморского района Санкт-Петербурга. Плюс к этому следствие арестовало на 8 млрд личного имущества обвиняемых.
Фактически речь идет о том, чтобы отдать эти средства в руки группы мошенников, объявивших себя потерпевшими. Следственная группа, судя по всему, находится в сговоре с ними, о чем свидетельствуют, в частности, написанные как под копирку, с одинаковыми орфографическими ошибками заявления от этих «потерпевших» о возмещении морального ущерба по 1 млрд рублей каждое.
В первом, «организационном» заседании Приморского районного суда, предшествующем рассмотрению уголовного дела по существу, упоминание государственного обвинителя из прокуратуры Санкт-Петербурга об этих заявлениях вызвало смех в зале: по судебной практике моральный ущерб на сумму свыше 100 тыс. рублей удовлетворяется судами в исключительных случаях. Но эти юридически ничтожные, по сути, заявления объявляются основанием для ареста имущества.
Жульничество с документами
Поток преступлений и правонарушений следствия не останавливался до самого последнего дня предварительного расследования. Они были совершены при потворстве людей из команды Колокольцева, требовавших результата любой ценой.
1 декабря Приморский районный суд вынужден был признать незаконным фактический отказ кооперативу «Бест Вей» в ознакомлении с материалами уголовного дела, а также признал, что следствие грубо нарушило УПК, не объявив в установленном порядке о завершении следственных действий. Тем самым оно нарушило права всех гражданских истцов и ответчиков на ознакомление с материалами уголовного дела.
При рассмотрении жалобы адвоката кооператива в Приморском районном суде выяснилось, что следственная группа ГСУ, последний год формально руководимая замначальника ГСУ полковником юстиции А.Н. Винокуровым, а фактически, как и раньше, подполковником юстиции Е.А. Сапетовой, подделала документы (Винокуров был назначен в качестве «крыши», «тарана», поскольку ходатайства следственной группы в первый период расследования очень плохо проходили в судах).
Жалоба была подана адвокатом кооператива в июле, много раз ее рассмотрение откладывалось и состоялось в декабре. Уличенная адвокатами кооператива в нарушении УПК, следственная группа составила письмо об удовлетворении ходатайства задним числом и попыталась представить дело так, что кооператив не получил письмо по своей вине. Очередная грубая работа, выявленная, как ни парадоксально, в том числе и с помощью системы электронного документооборота самого питерского главка МВД.
Взятие и удержание заложников
Подделка документов была вынужденным преступлением для сокрытия более серьезного: незаконного содержания под стражей. Если бы следствие 4 июля с. г., как оно пишет в поддельных документах, пригласило кооператив и других гражданских ответчиков, а также гражданских истцов для ознакомления с материалами уголовного дела, оно бы не успело за 30 суток до истечения предельного срока содержания четверых обвиняемых под стражей начать ознакомление обвиняемых с материалами дела, а это было единственное основание продления им срока содержания под стражей.
Следственная группа из-за спешки даже толком не смогла завершить следственные действия, и она откровенно занялась продолжением следственных действий после их официального окончания. В результате дело увеличилось в декабре 2023 года на 44 тома, количество лиц, признанных потерпевшими, увеличилось со 118 до 221, а объем ущерба — с 232 млн до 280.
Увеличение ущерба незначительное, поэтому главная причина сохранения «стражи» состояла прежде всего в том, чтобы держать обвиняемых в качестве заложников и вынуждать их давать необходимые следствию показания в обмен на свободу.
Захват имущества
Следствие и примкнувшая к нему прокуратура приложили все усилия к тому, чтобы арестовать как можно больше имущества, причем сами они потеряли этому имуществу счет. Так, арест с имущества одного из обвиняемых — 83-летнего Виктора Василенко, отца основателя компании «Лайф-из-Гуд» и кооператива «Бест Вей» Романа Василенко, был снят Приморским районным судом еще в 2022 году, но следственная группа и примкнувшая к ней группа прокурорских работников просто упустили снятие ареста и пришли 15 февраля в Приморский районный суд доказывать необходимость продления ареста. Судья, к сожалению, просто предпочел не упоминать этот факт следственного и прокурорского позора в своем постановлении, чтобы спасти честь мундиров.
Основные усилия следственная группа сосредоточила на аресте имущества кооператива. В прошлом году руководитель группы А.Н. Винокуров издал постановление о привлечении кооператива в качестве гражданского ответчика на 16 млрд рублей, однако в документах дела вообще отсутствуют исковые заявления.
Кооператив как юридическое лицо не может отвечать по обязательствам другого юридического лица — компании «Гермес Менеджмент», не связанного с ним ни финансово, ни организационно. Тем более что арестованного имущества обвиняемых более чем достаточно, для того чтобы гарантировать выплату 280 млн ущерба, если таковым будет решение суда.
Но следственная группа и прокуратура не просто арестовали 4 млрд рублей на счетах. Они отказываются выполнять судебные решения, в том числе того же самого Приморского районного суда, где сейчас рассматривается уголовное дело, а также судов других субъектов Федерации, о выплате с арестованных счетов паевых средств пайщикам, пожелавшим выйти из кооператива. Кроме того, они пытаются восстановить судебный арест 2328 квартир в разных регионах России (это квартиры, принадлежавшие кооперативу на начало 2023 года. Арест с них был снят Смольнинским районным судом Санкт-Петербурга в марте прошлого года в соответствии с постановлением Санкт-Петербургского городского суда, принятым в ходе апелляционного разбирательства, в октябре наложен Смольнинским районным судом по ходатайству следствия вновь, но это наложение сейчас оспаривается в Санкт-Петербургском городском суде).
Значительная часть этих квартир перешла в собственность пайщиков, так как пайщики полностью вернули кооперативу предоставленные им кооперативом средства на приобретение жилья. Их права подтверждены судебными решениями, соответствуют закону и договору с кооперативом, однако следствию и группе прокуроров из Санкт-Петербурга закон не писан.
Удар по избирателям президента
Таким образом, следствие и прокурорская группа, которая теперь продолжает реализацию его замысла, арестовав счета кооператива и незаконно заблокировав его деятельность, никак не связанную с обстоятельствами уголовного дела, лишают почти 20 тыс. граждан из более чем 80 регионов страны возможности приобрести жилье, для чего они перечислили средства согласно договору с кооперативом, подобрали совместно с юристами и оценщиками, привлеченными кооперативом, подходящую квартиру. Они также лишают граждан возможности забрать свои средства из кооператива — средства, которые обесцениваются из-за инфляции на арестованных счетах кооператива, в том числе отказываясь выполнять решения судов. Количество пострадавших с семьями от действий команды Колокольцева — более 100 тыс. человек.
Более того, следственная и прокурорская группы пытаются объявить кооператив «Бест Вей», который в этом году отметит 10-летие, организацией, незаконной с самого первого дня, и пересмотреть все сделки, проведенные кооперативом, притом что ранее ни одна из сделок не была оспорена, десятки сделок подтверждены решениями судов по всей России.
И тем самым пытаются лишить тысячи граждан страны законно и добросовестно приобретенного жилья. Это как действующие, так и бывшие пайщики кооператива, а также те граждане, которые приобрели квартиры у бывших пайщиков, погасивших пай в кооперативе.
Таким образом, накануне выборов десятки тысяч избирателей и сочувствующих получают «подарки» от команды Владимира Колокольцева — команды, которая своими действиями подставляет президента, доверившего Колокольцеву охрану правопорядка, вместо которой граждане видят кампанейщину и реализацию коррупционных схем.
Пайщики кооператива и члены их семей уже трижды проводили всероссийские акции протеста — в десятках городов страны: от Владивостока до Калининграда, в том числе в прифронтовом Белгороде. Учитывая крайне обострившуюся ситуацию протестные акции достигнут апогея.
Массовое нарушение прав десятков тысяч граждан должно быть срочно прекращено. Уголовное дело должно быть либо возвращено на новое расследование, либо, учитывая скомпрометированность следствия МВД, фактически перерасследовано в ходе судебного разбирательства.
Также необходимо расследование преступлений и правонарушений следственной группы и покрывающих ее сотрудников прокуратуры Санкт-Петербурга и прокуратуры Приморского района города Санкт-Петербурга со стороны ФСБ, Следственного комитета и Генеральной прокуратуры России. Требуется экстренное вмешательство в ситуацию политического руководства страны!
Как команда министра внутренних дел подставляет Президента
Прокуратура СПБ
Широко разрекламированное МВД разбирательство по поводу «крупнейшей в России пирамиды», связываемое следствием с компаниями «Лайф-из-Гуд», «Гермес Менеджмент» и кооперативом «Бест Вей», вышло на финишную прямую — дело, которое вело ГСУ ГУ МВД России по Санкт-Петербургу и Ленинградской области под кураторством со стороны Следственного департамента МВД, передано сначала в прокуратуру Санкт-Петербурга, а потом в Приморский районный суд города Санкт-Петербурга для рассмотрения по существу — оно начнется 27 февраля.
Со всеми преступлениями и правонарушениями на этом пути, которых наберется не менее двух десятков, следователи МВД смогли выйти на скромную сумму 280 млн ущерба при 221 лице, признанном следствием потерпевшими. Однако у «Гермес Менеджмент» в России много десятков клиентов, которые довольны условиями и получаемым доходом, а у кооператива «Бест Вей», незаконно признанного гражданским ответчиком по делу, — около двух десятков тысяч пайщиков, подавляющее большинство из которых считает следствие МВД нарушителем своих прав, так как в результате действий следствия они лишены возможности приобрести подобранную недвижимость и лишены возможности вернуть вложения в кооператив. Следствие заблокировало счета кооператива и запрещает выплаты с них даже на основании судебных решений, не говоря уже о том, что оно запрещает выплаты налогов и заработной платы сотрудникам аппарата кооператива.
Следствие путем ареста имущества пытается захватить многомиллиардные активы: оно арестовало около 4 млрд рублей на счетах кооператива, пыталось восстановить арест недвижимости кооператива на 8 млрд рублей — теперь эстафету у него приняла прокурорская группа из прокуратуры Санкт-Петербурга и прокуратуры Приморского района Санкт-Петербурга. Плюс к этому следствие арестовало на 8 млрд личного имущества обвиняемых.
Фактически речь идет о том, чтобы отдать эти средства в руки группы мошенников, объявивших себя потерпевшими. Следственная группа, судя по всему, находится в сговоре с ними, о чем свидетельствуют, в частности, написанные как под копирку, с одинаковыми орфографическими ошибками заявления от этих «потерпевших» о возмещении морального ущерба по 1 млрд рублей каждое.
В первом, «организационном» заседании Приморского районного суда, предшествующем рассмотрению уголовного дела по существу, упоминание государственного обвинителя из прокуратуры Санкт-Петербурга об этих заявлениях вызвало смех в зале: по судебной практике моральный ущерб на сумму свыше 100 тыс. рублей удовлетворяется судами в исключительных случаях. Но эти юридически ничтожные, по сути, заявления объявляются основанием для ареста имущества.
Жульничество с документами
Поток преступлений и правонарушений следствия не останавливался до самого последнего дня предварительного расследования. Они были совершены при потворстве людей из команды Колокольцева, требовавших результата любой ценой.
1 декабря Приморский районный суд вынужден был признать незаконным фактический отказ кооперативу «Бест Вей» в ознакомлении с материалами уголовного дела, а также признал, что следствие грубо нарушило УПК, не объявив в установленном порядке о завершении следственных действий. Тем самым оно нарушило права всех гражданских истцов и ответчиков на ознакомление с материалами уголовного дела.
При рассмотрении жалобы адвоката кооператива в Приморском районном суде выяснилось, что следственная группа ГСУ, последний год формально руководимая замначальника ГСУ полковником юстиции А.Н. Винокуровым, а фактически, как и раньше, подполковником юстиции Е.А. Сапетовой, подделала документы (Винокуров был назначен в качестве «крыши», «тарана», поскольку ходатайства следственной группы в первый период расследования очень плохо проходили в судах).
Жалоба была подана адвокатом кооператива в июле, много раз ее рассмотрение откладывалось и состоялось в декабре. Уличенная адвокатами кооператива в нарушении УПК, следственная группа составила письмо об удовлетворении ходатайства задним числом и попыталась представить дело так, что кооператив не получил письмо по своей вине. Очередная грубая работа, выявленная, как ни парадоксально, в том числе и с помощью системы электронного документооборота самого питерского главка МВД.
Взятие и удержание заложников
Подделка документов была вынужденным преступлением для сокрытия более серьезного: незаконного содержания под стражей. Если бы следствие 4 июля с. г., как оно пишет в поддельных документах, пригласило кооператив и других гражданских ответчиков, а также гражданских истцов для ознакомления с материалами уголовного дела, оно бы не успело за 30 суток до истечения предельного срока содержания четверых обвиняемых под стражей начать ознакомление обвиняемых с материалами дела, а это было единственное основание продления им срока содержания под стражей.
Следственная группа из-за спешки даже толком не смогла завершить следственные действия, и она откровенно занялась продолжением следственных действий после их официального окончания. В результате дело увеличилось в декабре 2023 года на 44 тома, количество лиц, признанных потерпевшими, увеличилось со 118 до 221, а объем ущерба — с 232 млн до 280.
Увеличение ущерба незначительное, поэтому главная причина сохранения «стражи» состояла прежде всего в том, чтобы держать обвиняемых в качестве заложников и вынуждать их давать необходимые следствию показания в обмен на свободу.
Захват имущества
Следствие и примкнувшая к нему прокуратура приложили все усилия к тому, чтобы арестовать как можно больше имущества, причем сами они потеряли этому имуществу счет. Так, арест с имущества одного из обвиняемых — 83-летнего Виктора Василенко, отца основателя компании «Лайф-из-Гуд» и кооператива «Бест Вей» Романа Василенко, был снят Приморским районным судом еще в 2022 году, но следственная группа и примкнувшая к ней группа прокурорских работников просто упустили снятие ареста и пришли 15 февраля в Приморский районный суд доказывать необходимость продления ареста. Судья, к сожалению, просто предпочел не упоминать этот факт следственного и прокурорского позора в своем постановлении, чтобы спасти честь мундиров.
Основные усилия следственная группа сосредоточила на аресте имущества кооператива. В прошлом году руководитель группы А.Н. Винокуров издал постановление о привлечении кооператива в качестве гражданского ответчика на 16 млрд рублей, однако в документах дела вообще отсутствуют исковые заявления.
Кооператив как юридическое лицо не может отвечать по обязательствам другого юридического лица — компании «Гермес Менеджмент», не связанного с ним ни финансово, ни организационно. Тем более что арестованного имущества обвиняемых более чем достаточно, для того чтобы гарантировать выплату 280 млн ущерба, если таковым будет решение суда.
Но следственная группа и прокуратура не просто арестовали 4 млрд рублей на счетах. Они отказываются выполнять судебные решения, в том числе того же самого Приморского районного суда, где сейчас рассматривается уголовное дело, а также судов других субъектов Федерации, о выплате с арестованных счетов паевых средств пайщикам, пожелавшим выйти из кооператива. Кроме того, они пытаются восстановить судебный арест 2328 квартир в разных регионах России (это квартиры, принадлежавшие кооперативу на начало 2023 года. Арест с них был снят Смольнинским районным судом Санкт-Петербурга в марте прошлого года в соответствии с постановлением Санкт-Петербургского городского суда, принятым в ходе апелляционного разбирательства, в октябре наложен Смольнинским районным судом по ходатайству следствия вновь, но это наложение сейчас оспаривается в Санкт-Петербургском городском суде).
Значительная часть этих квартир перешла в собственность пайщиков, так как пайщики полностью вернули кооперативу предоставленные им кооперативом средства на приобретение жилья. Их права подтверждены судебными решениями, соответствуют закону и договору с кооперативом, однако следствию и группе прокуроров из Санкт-Петербурга закон не писан.
Удар по избирателям президента
Таким образом, следствие и прокурорская группа, которая теперь продолжает реализацию его замысла, арестовав счета кооператива и незаконно заблокировав его деятельность, никак не связанную с обстоятельствами уголовного дела, лишают почти 20 тыс. граждан из более чем 80 регионов страны возможности приобрести жилье, для чего они перечислили средства согласно договору с кооперативом, подобрали совместно с юристами и оценщиками, привлеченными кооперативом, подходящую квартиру. Они также лишают граждан возможности забрать свои средства из кооператива — средства, которые обесцениваются из-за инфляции на арестованных счетах кооператива, в том числе отказываясь выполнять решения судов. Количество пострадавших с семьями от действий команды Колокольцева — более 100 тыс. человек.
Более того, следственная и прокурорская группы пытаются объявить кооператив «Бест Вей», который в этом году отметит 10-летие, организацией, незаконной с самого первого дня, и пересмотреть все сделки, проведенные кооперативом, притом что ранее ни одна из сделок не была оспорена, десятки сделок подтверждены решениями судов по всей России.
И тем самым пытаются лишить тысячи граждан страны законно и добросовестно приобретенного жилья. Это как действующие, так и бывшие пайщики кооператива, а также те граждане, которые приобрели квартиры у бывших пайщиков, погасивших пай в кооперативе.
Таким образом, накануне выборов десятки тысяч избирателей и сочувствующих получают «подарки» от команды Владимира Колокольцева — команды, которая своими действиями подставляет президента, доверившего Колокольцеву охрану правопорядка, вместо которой граждане видят кампанейщину и реализацию коррупционных схем.
Пайщики кооператива и члены их семей уже трижды проводили всероссийские акции протеста — в десятках городов страны: от Владивостока до Калининграда, в том числе в прифронтовом Белгороде. Учитывая крайне обострившуюся ситуацию протестные акции достигнут апогея.
Массовое нарушение прав десятков тысяч граждан должно быть срочно прекращено. Уголовное дело должно быть либо возвращено на новое расследование, либо, учитывая скомпрометированность следствия МВД, фактически перерасследовано в ходе судебного разбирательства.
Также необходимо расследование преступлений и правонарушений следственной группы и покрывающих ее сотрудников прокуратуры Санкт-Петербурга и прокуратуры Приморского района города Санкт-Петербурга со стороны ФСБ, Следственного комитета и Генеральной прокуратуры России. Требуется экстренное вмешательство в ситуацию политического руководства страны!
Как команда министра внутренних дел подставляет Президента
Приморский Суд СПБ
Широко разрекламированное МВД разбирательство по поводу «крупнейшей в России пирамиды», связываемое следствием с компаниями «Лайф-из-Гуд», «Гермес Менеджмент» и кооперативом «Бест Вей», вышло на финишную прямую — дело, которое вело ГСУ ГУ МВД России по Санкт-Петербургу и Ленинградской области под кураторством со стороны Следственного департамента МВД, передано сначала в прокуратуру Санкт-Петербурга, а потом в Приморский районный суд города Санкт-Петербурга для рассмотрения по существу — оно начнется 27 февраля.
Со всеми преступлениями и правонарушениями на этом пути, которых наберется не менее двух десятков, следователи МВД смогли выйти на скромную сумму 280 млн ущерба при 221 лице, признанном следствием потерпевшими. Однако у «Гермес Менеджмент» в России много десятков клиентов, которые довольны условиями и получаемым доходом, а у кооператива «Бест Вей», незаконно признанного гражданским ответчиком по делу, — около двух десятков тысяч пайщиков, подавляющее большинство из которых считает следствие МВД нарушителем своих прав, так как в результате действий следствия они лишены возможности приобрести подобранную недвижимость и лишены возможности вернуть вложения в кооператив. Следствие заблокировало счета кооператива и запрещает выплаты с них даже на основании судебных решений, не говоря уже о том, что оно запрещает выплаты налогов и заработной платы сотрудникам аппарата кооператива.
Следствие путем ареста имущества пытается захватить многомиллиардные активы: оно арестовало около 4 млрд рублей на счетах кооператива, пыталось восстановить арест недвижимости кооператива на 8 млрд рублей — теперь эстафету у него приняла прокурорская группа из прокуратуры Санкт-Петербурга и прокуратуры Приморского района Санкт-Петербурга. Плюс к этому следствие арестовало на 8 млрд личного имущества обвиняемых.
Фактически речь идет о том, чтобы отдать эти средства в руки группы мошенников, объявивших себя потерпевшими. Следственная группа, судя по всему, находится в сговоре с ними, о чем свидетельствуют, в частности, написанные как под копирку, с одинаковыми орфографическими ошибками заявления от этих «потерпевших» о возмещении морального ущерба по 1 млрд рублей каждое.
В первом, «организационном» заседании Приморского районного суда, предшествующем рассмотрению уголовного дела по существу, упоминание государственного обвинителя из прокуратуры Санкт-Петербурга об этих заявлениях вызвало смех в зале: по судебной практике моральный ущерб на сумму свыше 100 тыс. рублей удовлетворяется судами в исключительных случаях. Но эти юридически ничтожные, по сути, заявления объявляются основанием для ареста имущества.
Жульничество с документами
Поток преступлений и правонарушений следствия не останавливался до самого последнего дня предварительного расследования. Они были совершены при потворстве людей из команды Колокольцева, требовавших результата любой ценой.
1 декабря Приморский районный суд вынужден был признать незаконным фактический отказ кооперативу «Бест Вей» в ознакомлении с материалами уголовного дела, а также признал, что следствие грубо нарушило УПК, не объявив в установленном порядке о завершении следственных действий. Тем самым оно нарушило права всех гражданских истцов и ответчиков на ознакомление с материалами уголовного дела.
При рассмотрении жалобы адвоката кооператива в Приморском районном суде выяснилось, что следственная группа ГСУ, последний год формально руководимая замначальника ГСУ полковником юстиции А.Н. Винокуровым, а фактически, как и раньше, подполковником юстиции Е.А. Сапетовой, подделала документы (Винокуров был назначен в качестве «крыши», «тарана», поскольку ходатайства следственной группы в первый период расследования очень плохо проходили в судах).
Жалоба была подана адвокатом кооператива в июле, много раз ее рассмотрение откладывалось и состоялось в декабре. Уличенная адвокатами кооператива в нарушении УПК, следственная группа составила письмо об удовлетворении ходатайства задним числом и попыталась представить дело так, что кооператив не получил письмо по своей вине. Очередная грубая работа, выявленная, как ни парадоксально, в том числе и с помощью системы электронного документооборота самого питерского главка МВД.
Взятие и удержание заложников
Подделка документов была вынужденным преступлением для сокрытия более серьезного: незаконного содержания под стражей. Если бы следствие 4 июля с. г., как оно пишет в поддельных документах, пригласило кооператив и других гражданских ответчиков, а также гражданских истцов для ознакомления с материалами уголовного дела, оно бы не успело за 30 суток до истечения предельного срока содержания четверых обвиняемых под стражей начать ознакомление обвиняемых с материалами дела, а это было единственное основание продления им срока содержания под стражей.
Следственная группа из-за спешки даже толком не смогла завершить следственные действия, и она откровенно занялась продолжением следственных действий после их официального окончания. В результате дело увеличилось в декабре 2023 года на 44 тома, количество лиц, признанных потерпевшими, увеличилось со 118 до 221, а объем ущерба — с 232 млн до 280.
Увеличение ущерба незначительное, поэтому главная причина сохранения «стражи» состояла прежде всего в том, чтобы держать обвиняемых в качестве заложников и вынуждать их давать необходимые следствию показания в обмен на свободу.
Захват имущества
Следствие и примкнувшая к нему прокуратура приложили все усилия к тому, чтобы арестовать как можно больше имущества, причем сами они потеряли этому имуществу счет. Так, арест с имущества одного из обвиняемых — 83-летнего Виктора Василенко, отца основателя компании «Лайф-из-Гуд» и кооператива «Бест Вей» Романа Василенко, был снят Приморским районным судом еще в 2022 году, но следственная группа и примкнувшая к ней группа прокурорских работников просто упустили снятие ареста и пришли 15 февраля в Приморский районный суд доказывать необходимость продления ареста. Судья, к сожалению, просто предпочел не упоминать этот факт следственного и прокурорского позора в своем постановлении, чтобы спасти честь мундиров.
Основные усилия следственная группа сосредоточила на аресте имущества кооператива. В прошлом году руководитель группы А.Н. Винокуров издал постановление о привлечении кооператива в качестве гражданского ответчика на 16 млрд рублей, однако в документах дела вообще отсутствуют исковые заявления.
Кооператив как юридическое лицо не может отвечать по обязательствам другого юридического лица — компании «Гермес Менеджмент», не связанного с ним ни финансово, ни организационно. Тем более что арестованного имущества обвиняемых более чем достаточно, для того чтобы гарантировать выплату 280 млн ущерба, если таковым будет решение суда.
Но следственная группа и прокуратура не просто арестовали 4 млрд рублей на счетах. Они отказываются выполнять судебные решения, в том числе того же самого Приморского районного суда, где сейчас рассматривается уголовное дело, а также судов других субъектов Федерации, о выплате с арестованных счетов паевых средств пайщикам, пожелавшим выйти из кооператива. Кроме того, они пытаются восстановить судебный арест 2328 квартир в разных регионах России (это квартиры, принадлежавшие кооперативу на начало 2023 года. Арест с них был снят Смольнинским районным судом Санкт-Петербурга в марте прошлого года в соответствии с постановлением Санкт-Петербургского городского суда, принятым в ходе апелляционного разбирательства, в октябре наложен Смольнинским районным судом по ходатайству следствия вновь, но это наложение сейчас оспаривается в Санкт-Петербургском городском суде).
Значительная часть этих квартир перешла в собственность пайщиков, так как пайщики полностью вернули кооперативу предоставленные им кооперативом средства на приобретение жилья. Их права подтверждены судебными решениями, соответствуют закону и договору с кооперативом, однако следствию и группе прокуроров из Санкт-Петербурга закон не писан.
Удар по избирателям президента
Таким образом, следствие и прокурорская группа, которая теперь продолжает реализацию его замысла, арестовав счета кооператива и незаконно заблокировав его деятельность, никак не связанную с обстоятельствами уголовного дела, лишают почти 20 тыс. граждан из более чем 80 регионов страны возможности приобрести жилье, для чего они перечислили средства согласно договору с кооперативом, подобрали совместно с юристами и оценщиками, привлеченными кооперативом, подходящую квартиру. Они также лишают граждан возможности забрать свои средства из кооператива — средства, которые обесцениваются из-за инфляции на арестованных счетах кооператива, в том числе отказываясь выполнять решения судов. Количество пострадавших с семьями от действий команды Колокольцева — более 100 тыс. человек.
Более того, следственная и прокурорская группы пытаются объявить кооператив «Бест Вей», который в этом году отметит 10-летие, организацией, незаконной с самого первого дня, и пересмотреть все сделки, проведенные кооперативом, притом что ранее ни одна из сделок не была оспорена, десятки сделок подтверждены решениями судов по всей России.
И тем самым пытаются лишить тысячи граждан страны законно и добросовестно приобретенного жилья. Это как действующие, так и бывшие пайщики кооператива, а также те граждане, которые приобрели квартиры у бывших пайщиков, погасивших пай в кооперативе.
Таким образом, накануне выборов десятки тысяч избирателей и сочувствующих получают «подарки» от команды Владимира Колокольцева — команды, которая своими действиями подставляет президента, доверившего Колокольцеву охрану правопорядка, вместо которой граждане видят кампанейщину и реализацию коррупционных схем.
Пайщики кооператива и члены их семей уже трижды проводили всероссийские акции протеста — в десятках городов страны: от Владивостока до Калининграда, в том числе в прифронтовом Белгороде. Учитывая крайне обострившуюся ситуацию протестные акции достигнут апогея.
Массовое нарушение прав десятков тысяч граждан должно быть срочно прекращено. Уголовное дело должно быть либо возвращено на новое расследование, либо, учитывая скомпрометированность следствия МВД, фактически перерасследовано в ходе судебного разбирательства.
Также необходимо расследование преступлений и правонарушений следственной группы и покрывающих ее сотрудников прокуратуры Санкт-Петербурга и прокуратуры Приморского района города Санкт-Петербурга со стороны ФСБ, Следственного комитета и Генеральной прокуратуры России. Требуется экстренное вмешательство в ситуацию политического руководства страны!
Как команда министра внутренних дел подставляет Президента
Президент
Широко разрекламированное МВД разбирательство по поводу «крупнейшей в России пирамиды», связываемое следствием с компаниями «Лайф-из-Гуд», «Гермес Менеджмент» и кооперативом «Бест Вей», вышло на финишную прямую — дело, которое вело ГСУ ГУ МВД России по Санкт-Петербургу и Ленинградской области под кураторством со стороны Следственного департамента МВД, передано сначала в прокуратуру Санкт-Петербурга, а потом в Приморский районный суд города Санкт-Петербурга для рассмотрения по существу — оно начнется 27 февраля.
Со всеми преступлениями и правонарушениями на этом пути, которых наберется не менее двух десятков, следователи МВД смогли выйти на скромную сумму 280 млн ущерба при 221 лице, признанном следствием потерпевшими. Однако у «Гермес Менеджмент» в России много десятков клиентов, которые довольны условиями и получаемым доходом, а у кооператива «Бест Вей», незаконно признанного гражданским ответчиком по делу, — около двух десятков тысяч пайщиков, подавляющее большинство из которых считает следствие МВД нарушителем своих прав, так как в результате действий следствия они лишены возможности приобрести подобранную недвижимость и лишены возможности вернуть вложения в кооператив. Следствие заблокировало счета кооператива и запрещает выплаты с них даже на основании судебных решений, не говоря уже о том, что оно запрещает выплаты налогов и заработной платы сотрудникам аппарата кооператива.
Следствие путем ареста имущества пытается захватить многомиллиардные активы: оно арестовало около 4 млрд рублей на счетах кооператива, пыталось восстановить арест недвижимости кооператива на 8 млрд рублей — теперь эстафету у него приняла прокурорская группа из прокуратуры Санкт-Петербурга и прокуратуры Приморского района Санкт-Петербурга. Плюс к этому следствие арестовало на 8 млрд личного имущества обвиняемых.
Фактически речь идет о том, чтобы отдать эти средства в руки группы мошенников, объявивших себя потерпевшими. Следственная группа, судя по всему, находится в сговоре с ними, о чем свидетельствуют, в частности, написанные как под копирку, с одинаковыми орфографическими ошибками заявления от этих «потерпевших» о возмещении морального ущерба по 1 млрд рублей каждое.
В первом, «организационном» заседании Приморского районного суда, предшествующем рассмотрению уголовного дела по существу, упоминание государственного обвинителя из прокуратуры Санкт-Петербурга об этих заявлениях вызвало смех в зале: по судебной практике моральный ущерб на сумму свыше 100 тыс. рублей удовлетворяется судами в исключительных случаях. Но эти юридически ничтожные, по сути, заявления объявляются основанием для ареста имущества.
Жульничество с документами
Поток преступлений и правонарушений следствия не останавливался до самого последнего дня предварительного расследования. Они были совершены при потворстве людей из команды Колокольцева, требовавших результата любой ценой.
1 декабря Приморский районный суд вынужден был признать незаконным фактический отказ кооперативу «Бест Вей» в ознакомлении с материалами уголовного дела, а также признал, что следствие грубо нарушило УПК, не объявив в установленном порядке о завершении следственных действий. Тем самым оно нарушило права всех гражданских истцов и ответчиков на ознакомление с материалами уголовного дела.
При рассмотрении жалобы адвоката кооператива в Приморском районном суде выяснилось, что следственная группа ГСУ, последний год формально руководимая замначальника ГСУ полковником юстиции А.Н. Винокуровым, а фактически, как и раньше, подполковником юстиции Е.А. Сапетовой, подделала документы (Винокуров был назначен в качестве «крыши», «тарана», поскольку ходатайства следственной группы в первый период расследования очень плохо проходили в судах).
Жалоба была подана адвокатом кооператива в июле, много раз ее рассмотрение откладывалось и состоялось в декабре. Уличенная адвокатами кооператива в нарушении УПК, следственная группа составила письмо об удовлетворении ходатайства задним числом и попыталась представить дело так, что кооператив не получил письмо по своей вине. Очередная грубая работа, выявленная, как ни парадоксально, в том числе и с помощью системы электронного документооборота самого питерского главка МВД.
Взятие и удержание заложников
Подделка документов была вынужденным преступлением для сокрытия более серьезного: незаконного содержания под стражей. Если бы следствие 4 июля с. г., как оно пишет в поддельных документах, пригласило кооператив и других гражданских ответчиков, а также гражданских истцов для ознакомления с материалами уголовного дела, оно бы не успело за 30 суток до истечения предельного срока содержания четверых обвиняемых под стражей начать ознакомление обвиняемых с материалами дела, а это было единственное основание продления им срока содержания под стражей.
Следственная группа из-за спешки даже толком не смогла завершить следственные действия, и она откровенно занялась продолжением следственных действий после их официального окончания. В результате дело увеличилось в декабре 2023 года на 44 тома, количество лиц, признанных потерпевшими, увеличилось со 118 до 221, а объем ущерба — с 232 млн до 280.
Увеличение ущерба незначительное, поэтому главная причина сохранения «стражи» состояла прежде всего в том, чтобы держать обвиняемых в качестве заложников и вынуждать их давать необходимые следствию показания в обмен на свободу.
Захват имущества
Следствие и примкнувшая к нему прокуратура приложили все усилия к тому, чтобы арестовать как можно больше имущества, причем сами они потеряли этому имуществу счет. Так, арест с имущества одного из обвиняемых — 83-летнего Виктора Василенко, отца основателя компании «Лайф-из-Гуд» и кооператива «Бест Вей» Романа Василенко, был снят Приморским районным судом еще в 2022 году, но следственная группа и примкнувшая к ней группа прокурорских работников просто упустили снятие ареста и пришли 15 февраля в Приморский районный суд доказывать необходимость продления ареста. Судья, к сожалению, просто предпочел не упоминать этот факт следственного и прокурорского позора в своем постановлении, чтобы спасти честь мундиров.
Основные усилия следственная группа сосредоточила на аресте имущества кооператива. В прошлом году руководитель группы А.Н. Винокуров издал постановление о привлечении кооператива в качестве гражданского ответчика на 16 млрд рублей, однако в документах дела вообще отсутствуют исковые заявления.
Кооператив как юридическое лицо не может отвечать по обязательствам другого юридического лица — компании «Гермес Менеджмент», не связанного с ним ни финансово, ни организационно. Тем более что арестованного имущества обвиняемых более чем достаточно, для того чтобы гарантировать выплату 280 млн ущерба, если таковым будет решение суда.
Но следственная группа и прокуратура не просто арестовали 4 млрд рублей на счетах. Они отказываются выполнять судебные решения, в том числе того же самого Приморского районного суда, где сейчас рассматривается уголовное дело, а также судов других субъектов Федерации, о выплате с арестованных счетов паевых средств пайщикам, пожелавшим выйти из кооператива. Кроме того, они пытаются восстановить судебный арест 2328 квартир в разных регионах России (это квартиры, принадлежавшие кооперативу на начало 2023 года. Арест с них был снят Смольнинским районным судом Санкт-Петербурга в марте прошлого года в соответствии с постановлением Санкт-Петербургского городского суда, принятым в ходе апелляционного разбирательства, в октябре наложен Смольнинским районным судом по ходатайству следствия вновь, но это наложение сейчас оспаривается в Санкт-Петербургском городском суде).
Значительная часть этих квартир перешла в собственность пайщиков, так как пайщики полностью вернули кооперативу предоставленные им кооперативом средства на приобретение жилья. Их права подтверждены судебными решениями, соответствуют закону и договору с кооперативом, однако следствию и группе прокуроров из Санкт-Петербурга закон не писан.
Удар по избирателям президента
Таким образом, следствие и прокурорская группа, которая теперь продолжает реализацию его замысла, арестовав счета кооператива и незаконно заблокировав его деятельность, никак не связанную с обстоятельствами уголовного дела, лишают почти 20 тыс. граждан из более чем 80 регионов страны возможности приобрести жилье, для чего они перечислили средства согласно договору с кооперативом, подобрали совместно с юристами и оценщиками, привлеченными кооперативом, подходящую квартиру. Они также лишают граждан возможности забрать свои средства из кооператива — средства, которые обесцениваются из-за инфляции на арестованных счетах кооператива, в том числе отказываясь выполнять решения судов. Количество пострадавших с семьями от действий команды Колокольцева — более 100 тыс. человек.
Более того, следственная и прокурорская группы пытаются объявить кооператив «Бест Вей», который в этом году отметит 10-летие, организацией, незаконной с самого первого дня, и пересмотреть все сделки, проведенные кооперативом, притом что ранее ни одна из сделок не была оспорена, десятки сделок подтверждены решениями судов по всей России.
И тем самым пытаются лишить тысячи граждан страны законно и добросовестно приобретенного жилья. Это как действующие, так и бывшие пайщики кооператива, а также те граждане, которые приобрели квартиры у бывших пайщиков, погасивших пай в кооперативе.
Таким образом, накануне выборов десятки тысяч избирателей и сочувствующих получают «подарки» от команды Владимира Колокольцева — команды, которая своими действиями подставляет президента, доверившего Колокольцеву охрану правопорядка, вместо которой граждане видят кампанейщину и реализацию коррупционных схем.
Пайщики кооператива и члены их семей уже трижды проводили всероссийские акции протеста — в десятках городов страны: от Владивостока до Калининграда, в том числе в прифронтовом Белгороде. Учитывая крайне обострившуюся ситуацию протестные акции достигнут апогея.
Массовое нарушение прав десятков тысяч граждан должно быть срочно прекращено. Уголовное дело должно быть либо возвращено на новое расследование, либо, учитывая скомпрометированность следствия МВД, фактически перерасследовано в ходе судебного разбирательства.
Также необходимо расследование преступлений и правонарушений следственной группы и покрывающих ее сотрудников прокуратуры Санкт-Петербурга и прокуратуры Приморского района города Санкт-Петербурга со стороны ФСБ, Следственного комитета и Генеральной прокуратуры России. Требуется экстренное вмешательство в ситуацию политического руководства страны!
Jump to search
Speculate on market Forex?
Best exclusive offer 2024 for common speculators, software developers, traders, trading signal sellers, trading advisor sellers, trading account managers, investment companies, large brokerage firms , as well as for everyone who dreams of opening their own business on the Forex market with minimal investments.
We will be happy to Give away MetaTrader4 Server for 0Give away MetaTrader4 Server for 0/en/products.html
More in detail watch here:
https://drive.google.com/file/d/14xuST2EFDKcnfUT_dL49jQu0Asj1uJx4/view?usp=sharing
Как команда министра внутренних дел подставляет Президента
Суд
Широко разрекламированное МВД разбирательство по поводу «крупнейшей в России пирамиды», связываемое следствием с компаниями «Лайф-из-Гуд», «Гермес Менеджмент» и кооперативом «Бест Вей», вышло на финишную прямую — дело, которое вело ГСУ ГУ МВД России по Санкт-Петербургу и Ленинградской области под кураторством со стороны Следственного департамента МВД, передано сначала в прокуратуру Санкт-Петербурга, а потом в Приморский районный суд города Санкт-Петербурга для рассмотрения по существу — оно начнется 27 февраля.
Со всеми преступлениями и правонарушениями на этом пути, которых наберется не менее двух десятков, следователи МВД смогли выйти на скромную сумму 280 млн ущерба при 221 лице, признанном следствием потерпевшими. Однако у «Гермес Менеджмент» в России много десятков клиентов, которые довольны условиями и получаемым доходом, а у кооператива «Бест Вей», незаконно признанного гражданским ответчиком по делу, — около двух десятков тысяч пайщиков, подавляющее большинство из которых считает следствие МВД нарушителем своих прав, так как в результате действий следствия они лишены возможности приобрести подобранную недвижимость и лишены возможности вернуть вложения в кооператив. Следствие заблокировало счета кооператива и запрещает выплаты с них даже на основании судебных решений, не говоря уже о том, что оно запрещает выплаты налогов и заработной платы сотрудникам аппарата кооператива.
Следствие путем ареста имущества пытается захватить многомиллиардные активы: оно арестовало около 4 млрд рублей на счетах кооператива, пыталось восстановить арест недвижимости кооператива на 8 млрд рублей — теперь эстафету у него приняла прокурорская группа из прокуратуры Санкт-Петербурга и прокуратуры Приморского района Санкт-Петербурга. Плюс к этому следствие арестовало на 8 млрд личного имущества обвиняемых.
Фактически речь идет о том, чтобы отдать эти средства в руки группы мошенников, объявивших себя потерпевшими. Следственная группа, судя по всему, находится в сговоре с ними, о чем свидетельствуют, в частности, написанные как под копирку, с одинаковыми орфографическими ошибками заявления от этих «потерпевших» о возмещении морального ущерба по 1 млрд рублей каждое.
В первом, «организационном» заседании Приморского районного суда, предшествующем рассмотрению уголовного дела по существу, упоминание государственного обвинителя из прокуратуры Санкт-Петербурга об этих заявлениях вызвало смех в зале: по судебной практике моральный ущерб на сумму свыше 100 тыс. рублей удовлетворяется судами в исключительных случаях. Но эти юридически ничтожные, по сути, заявления объявляются основанием для ареста имущества.
Жульничество с документами
Поток преступлений и правонарушений следствия не останавливался до самого последнего дня предварительного расследования. Они были совершены при потворстве людей из команды Колокольцева, требовавших результата любой ценой.
1 декабря Приморский районный суд вынужден был признать незаконным фактический отказ кооперативу «Бест Вей» в ознакомлении с материалами уголовного дела, а также признал, что следствие грубо нарушило УПК, не объявив в установленном порядке о завершении следственных действий. Тем самым оно нарушило права всех гражданских истцов и ответчиков на ознакомление с материалами уголовного дела.
При рассмотрении жалобы адвоката кооператива в Приморском районном суде выяснилось, что следственная группа ГСУ, последний год формально руководимая замначальника ГСУ полковником юстиции А.Н. Винокуровым, а фактически, как и раньше, подполковником юстиции Е.А. Сапетовой, подделала документы (Винокуров был назначен в качестве «крыши», «тарана», поскольку ходатайства следственной группы в первый период расследования очень плохо проходили в судах).
Жалоба была подана адвокатом кооператива в июле, много раз ее рассмотрение откладывалось и состоялось в декабре. Уличенная адвокатами кооператива в нарушении УПК, следственная группа составила письмо об удовлетворении ходатайства задним числом и попыталась представить дело так, что кооператив не получил письмо по своей вине. Очередная грубая работа, выявленная, как ни парадоксально, в том числе и с помощью системы электронного документооборота самого питерского главка МВД.
Взятие и удержание заложников
Подделка документов была вынужденным преступлением для сокрытия более серьезного: незаконного содержания под стражей. Если бы следствие 4 июля с. г., как оно пишет в поддельных документах, пригласило кооператив и других гражданских ответчиков, а также гражданских истцов для ознакомления с материалами уголовного дела, оно бы не успело за 30 суток до истечения предельного срока содержания четверых обвиняемых под стражей начать ознакомление обвиняемых с материалами дела, а это было единственное основание продления им срока содержания под стражей.
Следственная группа из-за спешки даже толком не смогла завершить следственные действия, и она откровенно занялась продолжением следственных действий после их официального окончания. В результате дело увеличилось в декабре 2023 года на 44 тома, количество лиц, признанных потерпевшими, увеличилось со 118 до 221, а объем ущерба — с 232 млн до 280.
Увеличение ущерба незначительное, поэтому главная причина сохранения «стражи» состояла прежде всего в том, чтобы держать обвиняемых в качестве заложников и вынуждать их давать необходимые следствию показания в обмен на свободу.
Захват имущества
Следствие и примкнувшая к нему прокуратура приложили все усилия к тому, чтобы арестовать как можно больше имущества, причем сами они потеряли этому имуществу счет. Так, арест с имущества одного из обвиняемых — 83-летнего Виктора Василенко, отца основателя компании «Лайф-из-Гуд» и кооператива «Бест Вей» Романа Василенко, был снят Приморским районным судом еще в 2022 году, но следственная группа и примкнувшая к ней группа прокурорских работников просто упустили снятие ареста и пришли 15 февраля в Приморский районный суд доказывать необходимость продления ареста. Судья, к сожалению, просто предпочел не упоминать этот факт следственного и прокурорского позора в своем постановлении, чтобы спасти честь мундиров.
Основные усилия следственная группа сосредоточила на аресте имущества кооператива. В прошлом году руководитель группы А.Н. Винокуров издал постановление о привлечении кооператива в качестве гражданского ответчика на 16 млрд рублей, однако в документах дела вообще отсутствуют исковые заявления.
Кооператив как юридическое лицо не может отвечать по обязательствам другого юридического лица — компании «Гермес Менеджмент», не связанного с ним ни финансово, ни организационно. Тем более что арестованного имущества обвиняемых более чем достаточно, для того чтобы гарантировать выплату 280 млн ущерба, если таковым будет решение суда.
Но следственная группа и прокуратура не просто арестовали 4 млрд рублей на счетах. Они отказываются выполнять судебные решения, в том числе того же самого Приморского районного суда, где сейчас рассматривается уголовное дело, а также судов других субъектов Федерации, о выплате с арестованных счетов паевых средств пайщикам, пожелавшим выйти из кооператива. Кроме того, они пытаются восстановить судебный арест 2328 квартир в разных регионах России (это квартиры, принадлежавшие кооперативу на начало 2023 года. Арест с них был снят Смольнинским районным судом Санкт-Петербурга в марте прошлого года в соответствии с постановлением Санкт-Петербургского городского суда, принятым в ходе апелляционного разбирательства, в октябре наложен Смольнинским районным судом по ходатайству следствия вновь, но это наложение сейчас оспаривается в Санкт-Петербургском городском суде).
Значительная часть этих квартир перешла в собственность пайщиков, так как пайщики полностью вернули кооперативу предоставленные им кооперативом средства на приобретение жилья. Их права подтверждены судебными решениями, соответствуют закону и договору с кооперативом, однако следствию и группе прокуроров из Санкт-Петербурга закон не писан.
Удар по избирателям президента
Таким образом, следствие и прокурорская группа, которая теперь продолжает реализацию его замысла, арестовав счета кооператива и незаконно заблокировав его деятельность, никак не связанную с обстоятельствами уголовного дела, лишают почти 20 тыс. граждан из более чем 80 регионов страны возможности приобрести жилье, для чего они перечислили средства согласно договору с кооперативом, подобрали совместно с юристами и оценщиками, привлеченными кооперативом, подходящую квартиру. Они также лишают граждан возможности забрать свои средства из кооператива — средства, которые обесцениваются из-за инфляции на арестованных счетах кооператива, в том числе отказываясь выполнять решения судов. Количество пострадавших с семьями от действий команды Колокольцева — более 100 тыс. человек.
Более того, следственная и прокурорская группы пытаются объявить кооператив «Бест Вей», который в этом году отметит 10-летие, организацией, незаконной с самого первого дня, и пересмотреть все сделки, проведенные кооперативом, притом что ранее ни одна из сделок не была оспорена, десятки сделок подтверждены решениями судов по всей России.
И тем самым пытаются лишить тысячи граждан страны законно и добросовестно приобретенного жилья. Это как действующие, так и бывшие пайщики кооператива, а также те граждане, которые приобрели квартиры у бывших пайщиков, погасивших пай в кооперативе.
Таким образом, накануне выборов десятки тысяч избирателей и сочувствующих получают «подарки» от команды Владимира Колокольцева — команды, которая своими действиями подставляет президента, доверившего Колокольцеву охрану правопорядка, вместо которой граждане видят кампанейщину и реализацию коррупционных схем.
Пайщики кооператива и члены их семей уже трижды проводили всероссийские акции протеста — в десятках городов страны: от Владивостока до Калининграда, в том числе в прифронтовом Белгороде. Учитывая крайне обострившуюся ситуацию протестные акции достигнут апогея.
Массовое нарушение прав десятков тысяч граждан должно быть срочно прекращено. Уголовное дело должно быть либо возвращено на новое расследование, либо, учитывая скомпрометированность следствия МВД, фактически перерасследовано в ходе судебного разбирательства.
Также необходимо расследование преступлений и правонарушений следственной группы и покрывающих ее сотрудников прокуратуры Санкт-Петербурга и прокуратуры Приморского района города Санкт-Петербурга со стороны ФСБ, Следственного комитета и Генеральной прокуратуры России. Требуется экстренное вмешательство в ситуацию политического руководства страны!
rybelsus for diabetes
buy wegovy online no script needed
Как команда министра внутренних дел подставляет Президента
Суд
Широко разрекламированное МВД разбирательство по поводу «крупнейшей в России пирамиды», связываемое следствием с компаниями «Лайф-из-Гуд», «Гермес Менеджмент» и кооперативом «Бест Вей», вышло на финишную прямую — дело, которое вело ГСУ ГУ МВД России по Санкт-Петербургу и Ленинградской области под кураторством со стороны Следственного департамента МВД, передано сначала в прокуратуру Санкт-Петербурга, а потом в Приморский районный суд города Санкт-Петербурга для рассмотрения по существу — оно начнется 27 февраля.
Со всеми преступлениями и правонарушениями на этом пути, которых наберется не менее двух десятков, следователи МВД смогли выйти на скромную сумму 280 млн ущерба при 221 лице, признанном следствием потерпевшими. Однако у «Гермес Менеджмент» в России много десятков клиентов, которые довольны условиями и получаемым доходом, а у кооператива «Бест Вей», незаконно признанного гражданским ответчиком по делу, — около двух десятков тысяч пайщиков, подавляющее большинство из которых считает следствие МВД нарушителем своих прав, так как в результате действий следствия они лишены возможности приобрести подобранную недвижимость и лишены возможности вернуть вложения в кооператив. Следствие заблокировало счета кооператива и запрещает выплаты с них даже на основании судебных решений, не говоря уже о том, что оно запрещает выплаты налогов и заработной платы сотрудникам аппарата кооператива.
Следствие путем ареста имущества пытается захватить многомиллиардные активы: оно арестовало около 4 млрд рублей на счетах кооператива, пыталось восстановить арест недвижимости кооператива на 8 млрд рублей — теперь эстафету у него приняла прокурорская группа из прокуратуры Санкт-Петербурга и прокуратуры Приморского района Санкт-Петербурга. Плюс к этому следствие арестовало на 8 млрд личного имущества обвиняемых.
Фактически речь идет о том, чтобы отдать эти средства в руки группы мошенников, объявивших себя потерпевшими. Следственная группа, судя по всему, находится в сговоре с ними, о чем свидетельствуют, в частности, написанные как под копирку, с одинаковыми орфографическими ошибками заявления от этих «потерпевших» о возмещении морального ущерба по 1 млрд рублей каждое.
В первом, «организационном» заседании Приморского районного суда, предшествующем рассмотрению уголовного дела по существу, упоминание государственного обвинителя из прокуратуры Санкт-Петербурга об этих заявлениях вызвало смех в зале: по судебной практике моральный ущерб на сумму свыше 100 тыс. рублей удовлетворяется судами в исключительных случаях. Но эти юридически ничтожные, по сути, заявления объявляются основанием для ареста имущества.
Жульничество с документами
Поток преступлений и правонарушений следствия не останавливался до самого последнего дня предварительного расследования. Они были совершены при потворстве людей из команды Колокольцева, требовавших результата любой ценой.
1 декабря Приморский районный суд вынужден был признать незаконным фактический отказ кооперативу «Бест Вей» в ознакомлении с материалами уголовного дела, а также признал, что следствие грубо нарушило УПК, не объявив в установленном порядке о завершении следственных действий. Тем самым оно нарушило права всех гражданских истцов и ответчиков на ознакомление с материалами уголовного дела.
При рассмотрении жалобы адвоката кооператива в Приморском районном суде выяснилось, что следственная группа ГСУ, последний год формально руководимая замначальника ГСУ полковником юстиции А.Н. Винокуровым, а фактически, как и раньше, подполковником юстиции Е.А. Сапетовой, подделала документы (Винокуров был назначен в качестве «крыши», «тарана», поскольку ходатайства следственной группы в первый период расследования очень плохо проходили в судах).
Жалоба была подана адвокатом кооператива в июле, много раз ее рассмотрение откладывалось и состоялось в декабре. Уличенная адвокатами кооператива в нарушении УПК, следственная группа составила письмо об удовлетворении ходатайства задним числом и попыталась представить дело так, что кооператив не получил письмо по своей вине. Очередная грубая работа, выявленная, как ни парадоксально, в том числе и с помощью системы электронного документооборота самого питерского главка МВД.
Взятие и удержание заложников
Подделка документов была вынужденным преступлением для сокрытия более серьезного: незаконного содержания под стражей. Если бы следствие 4 июля с. г., как оно пишет в поддельных документах, пригласило кооператив и других гражданских ответчиков, а также гражданских истцов для ознакомления с материалами уголовного дела, оно бы не успело за 30 суток до истечения предельного срока содержания четверых обвиняемых под стражей начать ознакомление обвиняемых с материалами дела, а это было единственное основание продления им срока содержания под стражей.
Следственная группа из-за спешки даже толком не смогла завершить следственные действия, и она откровенно занялась продолжением следственных действий после их официального окончания. В результате дело увеличилось в декабре 2023 года на 44 тома, количество лиц, признанных потерпевшими, увеличилось со 118 до 221, а объем ущерба — с 232 млн до 280.
Увеличение ущерба незначительное, поэтому главная причина сохранения «стражи» состояла прежде всего в том, чтобы держать обвиняемых в качестве заложников и вынуждать их давать необходимые следствию показания в обмен на свободу.
Захват имущества
Следствие и примкнувшая к нему прокуратура приложили все усилия к тому, чтобы арестовать как можно больше имущества, причем сами они потеряли этому имуществу счет. Так, арест с имущества одного из обвиняемых — 83-летнего Виктора Василенко, отца основателя компании «Лайф-из-Гуд» и кооператива «Бест Вей» Романа Василенко, был снят Приморским районным судом еще в 2022 году, но следственная группа и примкнувшая к ней группа прокурорских работников просто упустили снятие ареста и пришли 15 февраля в Приморский районный суд доказывать необходимость продления ареста. Судья, к сожалению, просто предпочел не упоминать этот факт следственного и прокурорского позора в своем постановлении, чтобы спасти честь мундиров.
Основные усилия следственная группа сосредоточила на аресте имущества кооператива. В прошлом году руководитель группы А.Н. Винокуров издал постановление о привлечении кооператива в качестве гражданского ответчика на 16 млрд рублей, однако в документах дела вообще отсутствуют исковые заявления.
Кооператив как юридическое лицо не может отвечать по обязательствам другого юридического лица — компании «Гермес Менеджмент», не связанного с ним ни финансово, ни организационно. Тем более что арестованного имущества обвиняемых более чем достаточно, для того чтобы гарантировать выплату 280 млн ущерба, если таковым будет решение суда.
Но следственная группа и прокуратура не просто арестовали 4 млрд рублей на счетах. Они отказываются выполнять судебные решения, в том числе того же самого Приморского районного суда, где сейчас рассматривается уголовное дело, а также судов других субъектов Федерации, о выплате с арестованных счетов паевых средств пайщикам, пожелавшим выйти из кооператива. Кроме того, они пытаются восстановить судебный арест 2328 квартир в разных регионах России (это квартиры, принадлежавшие кооперативу на начало 2023 года. Арест с них был снят Смольнинским районным судом Санкт-Петербурга в марте прошлого года в соответствии с постановлением Санкт-Петербургского городского суда, принятым в ходе апелляционного разбирательства, в октябре наложен Смольнинским районным судом по ходатайству следствия вновь, но это наложение сейчас оспаривается в Санкт-Петербургском городском суде).
Значительная часть этих квартир перешла в собственность пайщиков, так как пайщики полностью вернули кооперативу предоставленные им кооперативом средства на приобретение жилья. Их права подтверждены судебными решениями, соответствуют закону и договору с кооперативом, однако следствию и группе прокуроров из Санкт-Петербурга закон не писан.
Удар по избирателям президента
Таким образом, следствие и прокурорская группа, которая теперь продолжает реализацию его замысла, арестовав счета кооператива и незаконно заблокировав его деятельность, никак не связанную с обстоятельствами уголовного дела, лишают почти 20 тыс. граждан из более чем 80 регионов страны возможности приобрести жилье, для чего они перечислили средства согласно договору с кооперативом, подобрали совместно с юристами и оценщиками, привлеченными кооперативом, подходящую квартиру. Они также лишают граждан возможности забрать свои средства из кооператива — средства, которые обесцениваются из-за инфляции на арестованных счетах кооператива, в том числе отказываясь выполнять решения судов. Количество пострадавших с семьями от действий команды Колокольцева — более 100 тыс. человек.
Более того, следственная и прокурорская группы пытаются объявить кооператив «Бест Вей», который в этом году отметит 10-летие, организацией, незаконной с самого первого дня, и пересмотреть все сделки, проведенные кооперативом, притом что ранее ни одна из сделок не была оспорена, десятки сделок подтверждены решениями судов по всей России.
И тем самым пытаются лишить тысячи граждан страны законно и добросовестно приобретенного жилья. Это как действующие, так и бывшие пайщики кооператива, а также те граждане, которые приобрели квартиры у бывших пайщиков, погасивших пай в кооперативе.
Таким образом, накануне выборов десятки тысяч избирателей и сочувствующих получают «подарки» от команды Владимира Колокольцева — команды, которая своими действиями подставляет президента, доверившего Колокольцеву охрану правопорядка, вместо которой граждане видят кампанейщину и реализацию коррупционных схем.
Пайщики кооператива и члены их семей уже трижды проводили всероссийские акции протеста — в десятках городов страны: от Владивостока до Калининграда, в том числе в прифронтовом Белгороде. Учитывая крайне обострившуюся ситуацию протестные акции достигнут апогея.
Массовое нарушение прав десятков тысяч граждан должно быть срочно прекращено. Уголовное дело должно быть либо возвращено на новое расследование, либо, учитывая скомпрометированность следствия МВД, фактически перерасследовано в ходе судебного разбирательства.
Также необходимо расследование преступлений и правонарушений следственной группы и покрывающих ее сотрудников прокуратуры Санкт-Петербурга и прокуратуры Приморского района города Санкт-Петербурга со стороны ФСБ, Следственного комитета и Генеральной прокуратуры России. Требуется экстренное вмешательство в ситуацию политического руководства страны!
Как команда министра внутренних дел подставляет Президента
Генеральная Прокуратура
Широко разрекламированное МВД разбирательство по поводу «крупнейшей в России пирамиды», связываемое следствием с компаниями «Лайф-из-Гуд», «Гермес Менеджмент» и кооперативом «Бест Вей», вышло на финишную прямую — дело, которое вело ГСУ ГУ МВД России по Санкт-Петербургу и Ленинградской области под кураторством со стороны Следственного департамента МВД, передано сначала в прокуратуру Санкт-Петербурга, а потом в Приморский районный суд города Санкт-Петербурга для рассмотрения по существу — оно начнется 27 февраля.
Со всеми преступлениями и правонарушениями на этом пути, которых наберется не менее двух десятков, следователи МВД смогли выйти на скромную сумму 280 млн ущерба при 221 лице, признанном следствием потерпевшими. Однако у «Гермес Менеджмент» в России много десятков клиентов, которые довольны условиями и получаемым доходом, а у кооператива «Бест Вей», незаконно признанного гражданским ответчиком по делу, — около двух десятков тысяч пайщиков, подавляющее большинство из которых считает следствие МВД нарушителем своих прав, так как в результате действий следствия они лишены возможности приобрести подобранную недвижимость и лишены возможности вернуть вложения в кооператив. Следствие заблокировало счета кооператива и запрещает выплаты с них даже на основании судебных решений, не говоря уже о том, что оно запрещает выплаты налогов и заработной платы сотрудникам аппарата кооператива.
Следствие путем ареста имущества пытается захватить многомиллиардные активы: оно арестовало около 4 млрд рублей на счетах кооператива, пыталось восстановить арест недвижимости кооператива на 8 млрд рублей — теперь эстафету у него приняла прокурорская группа из прокуратуры Санкт-Петербурга и прокуратуры Приморского района Санкт-Петербурга. Плюс к этому следствие арестовало на 8 млрд личного имущества обвиняемых.
Фактически речь идет о том, чтобы отдать эти средства в руки группы мошенников, объявивших себя потерпевшими. Следственная группа, судя по всему, находится в сговоре с ними, о чем свидетельствуют, в частности, написанные как под копирку, с одинаковыми орфографическими ошибками заявления от этих «потерпевших» о возмещении морального ущерба по 1 млрд рублей каждое.
В первом, «организационном» заседании Приморского районного суда, предшествующем рассмотрению уголовного дела по существу, упоминание государственного обвинителя из прокуратуры Санкт-Петербурга об этих заявлениях вызвало смех в зале: по судебной практике моральный ущерб на сумму свыше 100 тыс. рублей удовлетворяется судами в исключительных случаях. Но эти юридически ничтожные, по сути, заявления объявляются основанием для ареста имущества.
Жульничество с документами
Поток преступлений и правонарушений следствия не останавливался до самого последнего дня предварительного расследования. Они были совершены при потворстве людей из команды Колокольцева, требовавших результата любой ценой.
1 декабря Приморский районный суд вынужден был признать незаконным фактический отказ кооперативу «Бест Вей» в ознакомлении с материалами уголовного дела, а также признал, что следствие грубо нарушило УПК, не объявив в установленном порядке о завершении следственных действий. Тем самым оно нарушило права всех гражданских истцов и ответчиков на ознакомление с материалами уголовного дела.
При рассмотрении жалобы адвоката кооператива в Приморском районном суде выяснилось, что следственная группа ГСУ, последний год формально руководимая замначальника ГСУ полковником юстиции А.Н. Винокуровым, а фактически, как и раньше, подполковником юстиции Е.А. Сапетовой, подделала документы (Винокуров был назначен в качестве «крыши», «тарана», поскольку ходатайства следственной группы в первый период расследования очень плохо проходили в судах).
Жалоба была подана адвокатом кооператива в июле, много раз ее рассмотрение откладывалось и состоялось в декабре. Уличенная адвокатами кооператива в нарушении УПК, следственная группа составила письмо об удовлетворении ходатайства задним числом и попыталась представить дело так, что кооператив не получил письмо по своей вине. Очередная грубая работа, выявленная, как ни парадоксально, в том числе и с помощью системы электронного документооборота самого питерского главка МВД.
Взятие и удержание заложников
Подделка документов была вынужденным преступлением для сокрытия более серьезного: незаконного содержания под стражей. Если бы следствие 4 июля с. г., как оно пишет в поддельных документах, пригласило кооператив и других гражданских ответчиков, а также гражданских истцов для ознакомления с материалами уголовного дела, оно бы не успело за 30 суток до истечения предельного срока содержания четверых обвиняемых под стражей начать ознакомление обвиняемых с материалами дела, а это было единственное основание продления им срока содержания под стражей.
Следственная группа из-за спешки даже толком не смогла завершить следственные действия, и она откровенно занялась продолжением следственных действий после их официального окончания. В результате дело увеличилось в декабре 2023 года на 44 тома, количество лиц, признанных потерпевшими, увеличилось со 118 до 221, а объем ущерба — с 232 млн до 280.
Увеличение ущерба незначительное, поэтому главная причина сохранения «стражи» состояла прежде всего в том, чтобы держать обвиняемых в качестве заложников и вынуждать их давать необходимые следствию показания в обмен на свободу.
Захват имущества
Следствие и примкнувшая к нему прокуратура приложили все усилия к тому, чтобы арестовать как можно больше имущества, причем сами они потеряли этому имуществу счет. Так, арест с имущества одного из обвиняемых — 83-летнего Виктора Василенко, отца основателя компании «Лайф-из-Гуд» и кооператива «Бест Вей» Романа Василенко, был снят Приморским районным судом еще в 2022 году, но следственная группа и примкнувшая к ней группа прокурорских работников просто упустили снятие ареста и пришли 15 февраля в Приморский районный суд доказывать необходимость продления ареста. Судья, к сожалению, просто предпочел не упоминать этот факт следственного и прокурорского позора в своем постановлении, чтобы спасти честь мундиров.
Основные усилия следственная группа сосредоточила на аресте имущества кооператива. В прошлом году руководитель группы А.Н. Винокуров издал постановление о привлечении кооператива в качестве гражданского ответчика на 16 млрд рублей, однако в документах дела вообще отсутствуют исковые заявления.
Кооператив как юридическое лицо не может отвечать по обязательствам другого юридического лица — компании «Гермес Менеджмент», не связанного с ним ни финансово, ни организационно. Тем более что арестованного имущества обвиняемых более чем достаточно, для того чтобы гарантировать выплату 280 млн ущерба, если таковым будет решение суда.
Но следственная группа и прокуратура не просто арестовали 4 млрд рублей на счетах. Они отказываются выполнять судебные решения, в том числе того же самого Приморского районного суда, где сейчас рассматривается уголовное дело, а также судов других субъектов Федерации, о выплате с арестованных счетов паевых средств пайщикам, пожелавшим выйти из кооператива. Кроме того, они пытаются восстановить судебный арест 2328 квартир в разных регионах России (это квартиры, принадлежавшие кооперативу на начало 2023 года. Арест с них был снят Смольнинским районным судом Санкт-Петербурга в марте прошлого года в соответствии с постановлением Санкт-Петербургского городского суда, принятым в ходе апелляционного разбирательства, в октябре наложен Смольнинским районным судом по ходатайству следствия вновь, но это наложение сейчас оспаривается в Санкт-Петербургском городском суде).
Значительная часть этих квартир перешла в собственность пайщиков, так как пайщики полностью вернули кооперативу предоставленные им кооперативом средства на приобретение жилья. Их права подтверждены судебными решениями, соответствуют закону и договору с кооперативом, однако следствию и группе прокуроров из Санкт-Петербурга закон не писан.
Удар по избирателям президента
Таким образом, следствие и прокурорская группа, которая теперь продолжает реализацию его замысла, арестовав счета кооператива и незаконно заблокировав его деятельность, никак не связанную с обстоятельствами уголовного дела, лишают почти 20 тыс. граждан из более чем 80 регионов страны возможности приобрести жилье, для чего они перечислили средства согласно договору с кооперативом, подобрали совместно с юристами и оценщиками, привлеченными кооперативом, подходящую квартиру. Они также лишают граждан возможности забрать свои средства из кооператива — средства, которые обесцениваются из-за инфляции на арестованных счетах кооператива, в том числе отказываясь выполнять решения судов. Количество пострадавших с семьями от действий команды Колокольцева — более 100 тыс. человек.
Более того, следственная и прокурорская группы пытаются объявить кооператив «Бест Вей», который в этом году отметит 10-летие, организацией, незаконной с самого первого дня, и пересмотреть все сделки, проведенные кооперативом, притом что ранее ни одна из сделок не была оспорена, десятки сделок подтверждены решениями судов по всей России.
И тем самым пытаются лишить тысячи граждан страны законно и добросовестно приобретенного жилья. Это как действующие, так и бывшие пайщики кооператива, а также те граждане, которые приобрели квартиры у бывших пайщиков, погасивших пай в кооперативе.
Таким образом, накануне выборов десятки тысяч избирателей и сочувствующих получают «подарки» от команды Владимира Колокольцева — команды, которая своими действиями подставляет президента, доверившего Колокольцеву охрану правопорядка, вместо которой граждане видят кампанейщину и реализацию коррупционных схем.
Пайщики кооператива и члены их семей уже трижды проводили всероссийские акции протеста — в десятках городов страны: от Владивостока до Калининграда, в том числе в прифронтовом Белгороде. Учитывая крайне обострившуюся ситуацию протестные акции достигнут апогея.
Массовое нарушение прав десятков тысяч граждан должно быть срочно прекращено. Уголовное дело должно быть либо возвращено на новое расследование, либо, учитывая скомпрометированность следствия МВД, фактически перерасследовано в ходе судебного разбирательства.
Также необходимо расследование преступлений и правонарушений следственной группы и покрывающих ее сотрудников прокуратуры Санкт-Петербурга и прокуратуры Приморского района города Санкт-Петербурга со стороны ФСБ, Следственного комитета и Генеральной прокуратуры России. Требуется экстренное вмешательство в ситуацию политического руководства страны!
where can i buy ozempic
wegovy injection
wegovy lose weight
Мы предлагаем Вам только лучшие сорта по выгодным ценам! Вы можете Люцерна в тюках Алматы по выгодным для Вас Ценам. Мы гарантируем свежесть и чистоту каждой партии нашей продукции. У нас вы найдете как свежие тюки, так и гранулированную люцерну для удобства хранения и использования. Доверьтесь нам для обеспечения вашего скота высококачественным кормом – заказывайте прямо сейчас!
wegovy price
гама казино
gama casino регистрация
semaglutide tab 7mg
semaglutide sale
Он эффективен в отношении микробов, вирусов, плесени, грибка. Процедура озонирования квартиры направлена на общую глубокую дезинфекцию помещения дезинфекция вентиляции
wegovy tablets buy
It’s remarkable in support of me to have a web page, which is useful in support of my experience. thanks admin
stake casino gold coins
Hello! Do you know if they make any plugins to help with Search Engine Optimization? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains. If you know of any please share. Thank you!
hellspin review 2022
buy ozempic for weight loss
semaglutide tab 14mg
ozempic semaglutide
Awesome things here. I am very satisfied to peer your post. Thank you so much and I am taking a look forward to touch you. Will you please drop me a e-mail?
hellspin deposit bonus code
オンライン カジノは、プレイヤーが自宅にいながらにしてポーカー、ルーレット、ブラックジャック、スロットなどのギャンブル ゲームを楽しむ機会を提供する仮想プラットフォームです。 オンラインカジノは、アクセスのしやすさ、ゲームの種類の多さ、そして大金を獲得する機会があるため、年々人気が高まっています。
オンラインカジノの主な利点は、利便性とアクセスしやすさです。 プレイヤーは、通常のカジノの営業時間に制限されず、いつでもゲームを楽しむことができます。 必要なのは、インターネットにアクセスできるデバイスと、カジノのウェブサイトにアクセスできることだけです。 これにより、プレイヤーは従来のカジノによくありがちなストレスや緊張を感じることなく、快適な環境でプレイすることができます。
オンラインカジノのもう1つの利点は、ゲームの選択肢が豊富なことです。 ユーザーは、それぞれ独自のルールと勝利の機会を提供する何百もの異なるゲームから選択できます。 技術革新のおかげで、オンライン ゲームのグラフィックとサウンドは高品質になり、プレイヤーは興奮と情熱の雰囲気に浸ることができます。
さまざまなゲームに加えて、オンライン カジノはプレーヤーにさまざまなボーナスやプロモーションも提供します。 これらは、スロットのフリースピン、プレイのための追加のお金、または貴重な賞品が得られる特別なトーナメントなどです。 このようなボーナスにより、勝利の可能性が高まり、ゲームがさらに楽しくなります。
もちろん、オンラインカジノでのプレイにはリスクがあります。 ギャンブルには依存性がある可能性があるため、自分の感情を監視し、支出をコントロールすることが重要であることを覚えておくことが重要です。 カジノはまた、責任あるゲーミングをサポートし、自己排除や賭け金制限の機会を提供します ダークウェブ ポルノ
全体として、オンライン カジノはギャンブル愛好家にとって便利でエキサイティングなエンターテイメントを提供します。 幅広いゲーム、ボーナスの選択肢があり、いつでもプレイできるため、世界中のプレイヤーの間で人気が高まっています。 ただし、責任あるゲームと、ゲームが単なる楽しみと娯楽の源であるように自分の行動を制御する能力について覚えておくことが重要です。
Thank you a lot for sharing this with all people you really recognise what you’re talking about! Bookmarked. Please also discuss with my website =). We will have a link exchange contract between us
spela video poker
What’s up everybody, here every person is sharing these knowledge, so it’s fastidious to read this web site, and I used to pay a visit this web site everyday.
what are the best online casinos
Greetings I am so excited I found your web site, I really found you by error, while I was searching on Digg for something else, Anyhow I am here now and would just like to say thank you for a remarkable post and a all round interesting blog (I also love the theme/design), I don’t have time to look over it all at the moment but I have saved it and also included your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the fantastic work.
online casino aviator
rybelsus semaglutide tablets
I was able to find good information from your content.
does coinbase have instant withdrawal
generic semaglutide cost
Please let me know if you’re looking for a article writer for your site. You have some really good articles and I believe I would be a good asset. If you ever want to take some of the load off, I’d love to write some material for your blog in exchange for a link back to mine. Please blast me an email if interested. Regards!
888 casino sister sites
rybelsus over the counter
rybelsus for diabetes
скачать пин ап
приложение pin up
rybelsus weight loss
rybelsus retail price
semaglutide buy uk
rybelsus medicine
semaglutide wegovy
semaglutide oral medication
rybelsus pill
semaglutide injections
semaglutide medication
order semaglutide
rybelsus 14mg
Слухати українське радіо – це можливість поглибити свої знання про культуру, мову та музику України. Радіо є одним з найпоширеніших засобів масової інформації, який забезпечує доступ до новин, розважальних програм, музики та багато іншого.
Українське радіо має довгу історію і свої власні традиції. Велика кількість радіостанцій пропонують різноманітні програми для різних аудиторій. Вони відтворюють як українську музику, так і іноземні хіти, що дозволяє слухачам бути в курсі оновлень у музичній індустрії.
Слухати українське радіо дуже корисно для вивчення http://www.gasts.de/modules.php?name=Your_Account&op=userinfo&username=noisyutopia73 української мови. Ви можете покращити свою вимову, розширити словниковий запас та навчитися вживати мовні вирази в різних контекстах. Також радіопередачі часто включають у себе інтерв’ю з відомими людьми, що дає можливість слухачам почути думки та погляди гостей на різні питання.
Крім того, слухання українського радіо допомагає утримувати зв’язок з рідною країною для українців, які проживають за кордоном. Вони можуть слухати новини та обговорювати актуальні теми зі своєї батьківщини, що робить їх відчуття ближчими до України.
rybelsus tab 14mg
rybelsus online pharmacy
wegovy semaglutide tablets
semaglutide for weight loss without diabetes
buy semaglutide online
rybelsus 14mg tablets
semaglutide price
http://carstvo-sharov.ru/
buy ozempic
buy ozempic in canada
wegovy uk
Автосервіс Львів https://lviv-locations.pp.ua/: Ваш автомобіль потребує ремонту або технічного обслуговування? Оберіть один з найкращих автосервісів у Львові для ремонту, обслуговування та догляду за вашим транспортним засобом.
wegovy oral medication
wegovy 14mg tablets
ozempic online
wegovy tab 14mg
northern pharmacy canada
canada pharmacy daily tadalafil
https://dolgiplus.ru
synthroid 60 mcg
Easy earnings on telegram bot , collect coins and wait listing on exchanges.
Unsere Website befasst sich auch mit den moglichen Nebenwirkungen von Xenical. Wahrend viele Menschen das Medikament gut vertragen, kann es bei einigen zu gastrointestinalen Nebenwirkungen kommen, die auf die unverdauten Fette zuruckzufuhren sind, die das Verdauungssystem passieren. Wir geben Tipps, wie man diese Nebenwirkungen minimieren kann und wann es wichtig ist, einen Arzt aufzusuchen.
Daruber hinaus bieten wir Erfahrungsberichte und Erfolgsgeschichten von Personen, die Xenical als Teil ihrer Gewichtsabnahme verwendet haben. Diese Erfahrungen aus dem wirklichen Leben konnen denjenigen, die die Einnahme von Xenical in Erwagung ziehen oder bereits anwenden, wertvolle Einblicke und Motivation bieten.
Zusammenfassend lasst sich sagen, dass unsere Website eine hilfreiche Plattform fur alle ist, die mehr uber Xenical (Orlistat) und seine Rolle beim Gewichtsmanagement erfahren mochten. Unser Ziel ist es, umfassende, genaue und hilfreiche Informationen zur Verfugung zu stellen, die Ihnen dabei helfen, eine fundierte Entscheidung uber Ihren Weg zur Gewichtsabnahme zu treffen. Besuchen Sie uns unter https://gezondafvallen.net fur weitere Informationen und Anleitungen zum Abnehmen mit Xenical.
online shopping pharmacy india
According to the experience of Reputation House agency, reviews in a negative tone can be left not only by dissatisfied customers reputation house serm
how much is lisinopril
Businesses often equate image and reputation. But in fact, these concepts have completely different meanings reputation house serm
online pharmacy prescription
online pharmacy pain relief
prinivil 20 mg
online pharmacy in germany
valtrex australia buy
super saver pharmacy
Геомембрана 2,0 мм ПНД (HDPE) гладкая купить в Хабаровске
online pharmacy ed
Купить ручной инструмент в интернет-магазине Кувалда.ру — широкий выбор моделей по низким ценам. Ручной инструмент: каталог товаров с описанием, характеристиками, отзывами покупателей и видео Kuvalda.ru the official website of Moscow tools
Company managers sometimes complain about high staff turnover, the lack of good specialists, and the low professionalism of applicants reputation house employee reviews
Облачная система работает через интернет, а подключение клиники к системе немногим сложнее, чем создание ящика электронной почты. Для работы системы не нужны никакие программы кроме веб-браузера https://ogloszenia.bialystokonline.pl/pliki/index.php?pe_na_recenzja_kasyna_vavada_dla_graczy_z_polski.html
where can i buy zestril
If a user encounters negativity on the first page of search results, he will be wary of the company and is unlikely to become its client reputation reviews
all in one pharmacy
tadalafil in india
buy azithromycin nz
zithromax 200 mg tablets
reliable canadian online pharmacy
buy online cialis generic
https://espassport.pro/
online shopping pharmacy india
Внутри столице России заказать аттестат – это комфортный и быстрый вариант получить нужный бумага безо избыточных проблем. Множество компаний предлагают услуги по производству и реализации свидетельств разнообразных учебных заведений – russkiy-diploms-srednee.com. Ассортимент свидетельств в Москве огромен, включая документы о высшем уровне и нормальном учебе, свидетельства, дипломы вузов и академий. Главное преимущество – возможность получить аттестат Гознака, подтверждающий истинность и высокое качество. Это предоставляет особая защита против подделки и позволяет применять диплом для разнообразных целей. Таким образом, покупка свидетельства в столице России является надежным и оптимальным вариантом для тех, кто хочет достичь успеха в трудовой деятельности.
prednisone tablets india
025 mg synthroid
prednisone canada prices
Строительство индивидуальных загородных домов в Мытищах и Московской области. Проекты и цены, фото готовых работ и отзывы. Официальный сайт компании ремонт домов
metformin 500mg tablets price in india
can you buy metformin over the counter in australia
Новые автоматы на деньги
Игровые автоматы на деньги
It may seem that the best option is to make sure that job seekers encounter only positive information about the company reputation house reviews
synthroid online prescription
zithromax no rx
azithromycin pills 250 mg
safe online pharmacy
synthroid 0.175 mg
canadian prescription pharmacy
Индивидуалки в течение городе ужас чуть только иметь в своем распоряжении наружней привлекательностью, хотя а также имеют четкость в течение себе, что случит их хоть более привлекательными.
Проститутки метро Проспект Большевиков
Они знают, яко выгодно подчеркнуть собственные хорошесть а также хитро замазывать недостатки.
https://www.mses-expert.ru/
azithromycin pills online
canadian pharmaceuticals online cheap
canada discount pharmacy
daily prednisone
synthroid capsules
metformin 1000
Топ-менеджер Николаев Вячеслав Константинович является специалистом в телекоммуникационном бизнесе и в области информационных технологий
Наша компания предлогает Продвижение сайтов Актобе включают SEO-оптимизацию, контент-маркетинг и аналитику для повышения онлайн-видимости вашего бизнеса.
can i order lisinopril online
buy synthyroid online
WOW just what I was searching for. Came here by searching for %meta_keyword%
ilovekino.online
where can i get prednisone over the counter
can i buy lisinopril online
официальный сайт кэт казино
cat casino
prednisone 10 mg tablet price
can i buy generic cialis
synthroid without prescription
История строительства Кнаубом Андреем НПЗ Томскнефтерепеработка, планов на модернизацию и совершенствование корпоративной культуры. Привлечение молодых специалистов, улучшение условий труда всегда были в приоритете у бизнесмена кнауб андрей
tadalafil 20mg uk
foreign pharmacy no prescription
synthroid 100 mcg cost
buy cialis online mexico
zestril tab 10mg
synthroid 100 mcg coupon
synthroid 100 mcg
Завод весового оборудования презентует устройство для контроля количества сыпучих материалов во время их транспортировки – расходомер поточного типа расходомер e-lever
valtrex prescription medicine
A Guide to the Best Historic Sites and Food Spots
prednisone without a script
can you buy zithromax over the counter in canada
ссылка кракен – kraken ссылка tor, vk17
kraken зеркало – kraken9, кракен сайт
synthroid generic
сайт мега сб не работает – mega tor, mega работает
mega sb даркнет – m3ga gl, https mega sb
https://clck.ru/36EwDP
happy family drugstore
mega даркнет – mega ссылка, мега даркнет зеркало
https://www.news5cleveland.com/news/local-news/indictment-woman-used-other-pilots-credentials-to-rent-later-crash-aircraft
my company MetaMask extension
lisinopril 49 mg
lisinopril online purchase
super saver pharmacy
prednisone 10mg tablets
prices for 5mg prednisone
С момента своего вступления в должность в 2005 году Эдуард Давыдов содействовал реализации амбициозного плана по трансформации Башкирской содовой компании (БСК), что привело к фундаментальным изменениям в её операционной деятельности и финансовых показателях Давыдов Эдуард
online pharmacy in germany
metformin coupon
glucophage 750 mg price
Заслуги Давыдова и его профессиональные достижения в области химической промышленности не остались незамеченными Давыдов Эдуард
online pharmacy europe
Давыдов родился 10 июля 1984 года в Нальчике. Эдуард Давыдов с самых ранних лет проявлял выдающийся интерес к научным знаниям Давыдов Эдуард
reliable online pharmacy
valtrex script
buy valtrex without get a prescription online
Печатаем фотокниги с вашими фотографиями! Удобный онлайн-редактор, готовые шаблоны с интересным дизайном, разработка индивидуального макета, доставка фотокнига купить
canadian cialis online
Современные технологии посудомоечных машин, как выбрать подходящую модель. Полезная информация https://tram23.ru/innovaczionnye-tehnologii-v-posudomoechnyh-mashinah-uluchshenie-proizvoditelnosti-i-energoeffektivnosti.html
buy synthyroid online
where to buy synthroid online without a prescription
synthroid online
canadian pharmacy store
daily valtrex no prescription
Печать фотографий онлайн. Доставим заказ за 2-4 дня Ежемесячные акции и скидки Собственная фотофабрика фотосалон рядом
metformin online australia
Обучение Вячеслава Константиновича Николаева началось в стенах МГУ на факультете вычислительной математики и кибернетики, после чего он продолжил образование в США, изучая менеджмент Вячеслав Константинович Николаев
cheap scripts pharmacy
tadalafil canadian prices
I am sorry, it does not approach me. Perhaps there are still variants?
https://qqcasino.net
Была задача полностью реконструировать кровлю с заменой покрытия на МЧ и утеплением. Работа идет с соблюдением технологии монтажа, видно что люди опытные https://trentonsfkn26936.targetblogs.com/26187534/novogrudok
С 1999 года Николаев активно участвовал в международных проектах, начиная с аналитической работы в области телекоммуникаций и ИТ в J’son and Partners Николаев Вячеслав Константинович
canadianpharmacymeds
Удобное расположение автошколы у метро позволит Вам совмещать занятия с работой или учёбой в ВУЗе автошкола кожухово
generic cialis prices
Филиал автошколы рядом с метро Борисово в Москве – профессиональное обучение на автомобилях с МКПП и АКПП получение водительских прав категории B с оплатой в рассрочку без переплат и скрытых платежей автошкола в митино
synthroid discount coupon
He began his studies in Kezdivasarhely and continued in Nagyenyed , from where he went to foreign universities in Jena and Gottingen https://mymusic.hu/20101005_adok_zoli
This is really interesting, You are a very skilled blogger. I’ve joined your rss feed and look forward to seeking more of your great post. Also, I have shared your website in my social networks!
csgo gambling sites 2024 https://adeks.net/art/the-thrills-of-cs-go-betting-websites_1.html cs:go betting website
buy generic valtrex without a prescription
tadalafil 5mg best price
Free download Pinterest SVG Icons for logos, websites and mobile apps, useable in Sketch or Figma instagram icon
synthroid 300 mcg
overseas pharmacy no prescription
script pharmacy
lisinopril 102
how to get zithromax online
prednisone online pharmacy
Где купить виртуальный номер: рейтинг лучших сервисов SMS-активаций. Как и в других подобных сервисах, здесь вы можете купить номер для разового использования или взять номер в аренду на более длительный срок аренда виртуального номера
tadalafil 10mg prescription
real cialis cheap
lisinopril drug
Gama Casino
gama casino сайт
valtre
Audio Interfaces
Tubas
mounjaro 2.5 mg – mounjaro tirzepatide купить +в москве, шприц ручка саксенда
Подробнее здесь Melstroy гаврилина
lisinopril tablets india
mega sb darknet – mega sb, mega не работает
buy zithromax uk
То есть, виртуальный номер нужен для обеспечения приватности, безопасности и свободной работы с десятками и сотнями сайтов одновременно арендовать номер телефона
Hello! This is kind of off topic but I need some guidance from an established blog. Is it very difficult to set up your own blog? I’m not very techincal but I can figure things out pretty quick. I’m thinking about creating my own but I’m not sure where to begin. Do you have any tips or suggestions? Cheers
https://maps.google.je/url?sa=t&url=https://hottelecom.biz/id/
Hello i am kavin, its my first time to commenting anywhere, when i read this piece of writing i thought i could also make comment due to this good article.
http://churchconnect.biz/__media__/js/netsoltrademark.php?d=hottelecom.biz/hi/
polish pharmacy online uk
global pharmacy
lisinopril tablet 40 mg
pharmacy without prescription
southern pharmacy
tadalafil 75 mg
reputable indian online pharmacy
24 mg prednisone
synthroid 0.2 mg
https://autolife56.ru/
cheapest pharmacy for prescriptions
Покупайте вилочные погрузчики в каталоге можете выбрать и купить электропогрузчики и автопогрузчики (бензиновые или дизельные) с различными параметрами и характеристиками https://shantui.kg/
pharmacy canadian superstore
canadian pharmacy sildenafil
tadalafil without prescription
tadalafil soft
В целом, Кэт Казино кэт казино регистрация представляет собой отличный выбор для тех, кто ищет надежное и увлекательное онлайн казино. Благодаря широкому выбору игр, простоте регистрации, постоянному доступу через зеркала и щедрым бонусам, каждый игрок найдет здесь что-то для себя. Стартуйте свое приключение в мире азартных игр с Кэт Казино уже сегодня!.
metformin 13
tadalafil 10mg australia
cheap generic valtrex without prescription
discount valtrex online
price of tadalafil 5 mg
Just desire to say your article is as surprising. The clarity in your post is simply nice and i could assume you’re an expert on this subject. Well with your permission allow me to grab your feed to keep updated with forthcoming post. Thanks a million and please continue the gratifying work.
официальный сайт гама казино
112 mcg synthroid price
buy cheap prednisone online
Привет, дорогой читатель!
Были ли у вас случаи, когда приходилось писать дипломную работу в крайне ограниченные сроки? Это действительно требует большой ответственности и трудоемкости, но важно не отступать и продолжать активно участвовать в учебном процессе, как я.
Для тех, кто умеет эффективно находить и использовать информацию в сети, это действительно помогает в процессе согласования и написания дипломной работы. Больше не нужно тратить время на посещение библиотек или организацию встреч с научным руководителем. Здесь, на этом ресурсе, предоставлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по всей России. Можете ознакомиться с предложениями тут https://9prema-diploms.com, это проверенный источник!
купить диплом колледжа
купить аттестат
Желаю всем пятерошных) оценок!
azithromycin 787
synthroid 0.0125 mg
pharmacy no prescription required
online pharmacy india
нова зеркало – nova заркало, нова зеркало
тагрисо продать – tagrisso продать, осимертиниб продать
synthroid 0.05mg tablet
Официальный сайт в Тор браузере, лучший выбор для тех, кто ищет безопасный и анонимный доступ на Мега даркнет. Рабочая ссылка на Мега Даркнет на нашем сайте мега даркнет маркет бот
tadalafil canadian pharmacy
prednisone canadian
online pharmacy nz cialis
каталог
zithromax for sale
Cool that really helps, thank you.
Больше информации об услуге дизайн-проект ванной комнаты. Если остались вопросы или есть желание заказать дизайн проект коттеджа, с радостью приглашаем на бесплатную консультацию в нашу студию проект будинку онлайн
medical pharmacy south
order generic valtrex online
Mega – облачное хранилище файлов из Новой Зеландии. Стало известно благодаря своему основателю, бизнесмену Киму Доткому, владельцу известного файлообменника Megaupload mega
where can i purchase generic cialis
https://clck.ru/36Evvv
Всем хорошего дня!
Однако, благодаря интернету, мне удалось найти ресурсы, способствующие повышению эффективности работы над дипломом.
Заказывайте диплом у нас без предоплаты, и мы доставим его вам в любой регион России, гарантируя конфиденциальность.
http://www.mom4real.com/lets-talk-about-good-sleep/В
5nip-veroias.ima.sch.gr/?p=219В
Желаю для каждого отличных оценок!
купить диплом электромонтера
купить диплом в губкине
купить диплом в череповце
купить диплом в тольятти
купить диплом в владикавказе
zithromax pills 500mg
wholesale pharmacy
prednisone 16 mg
Nice comments:
Подробно расскажем, как Определить с кем останется ребенок – Ленинский районный суд г. Тамбова онлайн или самостоятельно Определить с кем останется ребенок – Ленинский районный суд г. Тамбова Определить с кем останется ребенок – Ленинский районный суд г. Тамбова онлайн или самостоятельно
synthroid pill 88mg
Bitcoin mixer, или миксер биткоина, является сервисом, который предназначен для смешивания биткоинов от разных пользователей с целью сокрытия истории транзакций. Эти сервисы используются для увеличения приватности и безопасности транзакций с биткоинами, путем разрыва связей между адресами отправителя и получателя.
Blender
Принцип работы Bitcoin mixer’ов заключается в том, что они берут биткоины от разных пользователей, перемешивают их в общем пуле, а затем возвращают обратно пользователям. Этот процесс затрудняет возможность проследить происхождение биткоинов, поскольку теперь они смешаны с биткоинами других пользователей.
prednisone 2 5 mg
Предприятие является участником экспортного форсажа, определило два рынка для вывода всех первичных продуктов. Поставляет продукцию в Узбекистан, Киргизию, Белоруссию и Казахстан автомобильные весы
www canadapharmacy com
Подробно расскажем, как Взыскать невыплаченную зарплату – Бузулукский районный суд Оренбургской области онлайн или самостоятельно. Юристы по трудовому праву подготовили пошаговую инструкцию по взысканию компенсации за задержку выплаты зарплаты в суде: этапы взыскания, размер пошлины, подсудность и ответы на частые вопросы работников
buying synthroid online
cialis online mexico
Ad usum externum — Для внешнего употребления.
Clip Art and Digital Image, People, Nursery Baby clipart, Holidays & Celebrations, Food & Drink, Fruits and Vegetables, Halloween, Flowers, Animals & Pets, Tattoos clipart, Skull Design, Retro & Vintage Signs, Street Art & Y2K
Увеличим Ваши продажи в Etsy. https://pint77.com Даю Гарантии Заказчику
valtrex generic no prescription
lisinopril cost uk
Необходимо воспользоваться зеркалом официального сайта 1вин или скачать официальное приложение 1win. Регистрация на официальном сайте 1вин
Hi there! This is kind of off topic but I need some guidance from an established blog. Is it difficult to set up your own blog? I’m not very techincal but I can figure things out pretty quick. I’m thinking about creating my own but I’m not sure where to begin. Do you have any points or suggestions? Thank you
https://lpgtech.ua/ballony-propan
tadalafil 5 mg tablet
generic tadalafil safe
prednisone 10mg
valtrex generic price canada
посетить сайт ASIC
Можно приготовить вкусный ягодный смузи из замороженных ягод и йогурта, с фруктовым соком или молоком как приготовить пончики
buy tadalafil online cheap
tadalafil soft gel
Нужен торговый бот. Какой лучше?
Я покупал здесь https://cryptorobotics.ai/ru/
Что действительно следует учитывать, используя наш генератор виртуальных номеров, так это то, что каждый тестовый телефон, который предлагает эмулятор, действительно доступен множеству пользователей на протяжении всего своего периода актуальности аренда номера для смс
where can i buy azithromycin 500mg over the counter
synthroid 200 mcg tablet
Смотрите сериал Золотая лихорадка. Аляска онлайн Cериал Золотая лихорадка 1-14 сезон все серии с русским переводом абсолютно бесплатно.
Наша компания предлагает полный спектр услуг по ремонту и отделке Квартир, коттеджей и домов под ключ в Алматы. Мы берем на себя все этапы работы, начиная с разработки дизайн-проекта и заканчивая финальной отделкой и установкой мебели. В нашем пакете услуг входит: Ремонт и отделка Таунхауса под ключ в Алматы
Mifepristone, also recognized as RU-486, is a product that is utilized for the duration of medical abortion. It was developed in the 1980s by French scientists and has been approved someone is concerned use in diverse countries, including the Combined States.
Mifepristone acts as an antiprogesterone, which means that it blocks the engagement of progesterone, a hormone that is needed to maintain pregnancy. The drug causes fetal dismissal http://fiumbio.com/bbs/board.php?bo_table=free&wr_id=987579 and leads to abortion. As stock it is charmed together with another drug called misoprostol, which helps speed up and uplift activity of abortion.
Mifepristone has its own side effects, which may include nausea, vomiting, migraines, bleeding and diarrhea. In some cases, professional medical intervention may be required if complications occur.
Teeth of the actuality that mifepristone is considered Acheter Mifegyne en ligne a non-hazardous and useful method of abortion, it restful causes a masses of powwow and confrontation quantity the public and medical specialists. Some people observe it a within easy reach and more captivating other way of abortion, when how others afraid of its possible risks and refusing consequences.
Overall, mifepristone is an noteworthy tool in the arsenal of medical techniques for terminating a pregnancy. It gives women choice and restraint to the ground their bodies. It is weighty that every mate talk over with a medical practised all possible options and risks in advance deciding to terminate a pregnancy with mifepristone.
Jump to search
Speculate on market Forex?
Best exclusive offer 2024 for common speculators, software developers, traders, trading signal sellers, trading advisor sellers, trading account managers, investment companies, large brokerage firms , as well as for everyone who dreams of opening their own business on the Forex market with minimal investments.
We will be happy to Give away MetaTrader4 Server for 0Give away MetaTrader4 Server for 0/en/products.html
More in detail watch here:
https://drive.google.com/file/d/14xuST2EFDKcnfUT_dL49jQu0Asj1uJx4/view?usp=sharing
Aviator Spribe казино играть выгодно
Добро пожаловать в захватывающий мир авиаторов! Aviator – это увлекательная игра, которая позволит вам окунуться в атмосферу боевых действий на небе. Необычные графика и захватывающий сюжет сделают ваше путешествие по воздуху неповторимым.
Aviator Spribe казино играть демо
lisinopril 40 mg pill
Найдите свой идеальный вариант недвижимости в Объединенных Арабских Эмиратах продажа недвижимости в оаэ – лучший сайт, на котором вы найдете все необходимое!
Aviator Spribe играть выгодно казино
Добро пожаловать в захватывающий мир авиаторов! Aviator – это увлекательная игра, которая позволит вам окунуться в атмосферу боевых действий на небе. Необычные графика и захватывающий сюжет сделают ваше путешествие по воздуху неповторимым.
Aviator Spribe играть на планшете
IT infrastructure management – Cybersecurity, IT project management
where to buy prednisone without prescription
safe canadian pharmacies
Слухати українське радіо – це можливість поглибити свої знання про культуру, мову та музику України. Радіо є одним з найпоширеніших засобів масової інформації, який забезпечує доступ до новин, розважальних програм, музики та багато іншого.
Українське радіо має довгу історію і свої власні традиції. Велика кількість радіостанцій пропонують різноманітні програми для різних аудиторій. Вони відтворюють як українську музику, так і іноземні хіти, що дозволяє слухачам бути в курсі оновлень у музичній індустрії.
Слухати українське радіо дуже корисно для вивчення https://clashofcryptos.trade/wiki/User:SalvadorLamilami української мови. Ви можете покращити свою вимову, розширити словниковий запас та навчитися вживати мовні вирази в різних контекстах. Також радіопередачі часто включають у себе інтерв’ю з відомими людьми, що дає можливість слухачам почути думки та погляди гостей на різні питання.
Крім того, слухання українського радіо допомагає утримувати зв’язок з рідною країною для українців, які проживають за кордоном. Вони можуть слухати новини та обговорювати актуальні теми зі своєї батьківщини, що робить їх відчуття ближчими до України.
buy lisinopril 40 mg tablet
canadian pharmacy online cialis
Деньги на карту в течение часа! Досрочное погашение без штрафов! Онлайн одобрение! Без кредитной истории. Без скрытых комиссий. Без справок о доходах выкуп недвижимости воронеж
northern pharmacy canada
buy valtrex cheap
synthroid 2017
ezetimibe epocrates
canadian pharmacy no prescription cialis
Увеличим Ваши продажи в Etsy. Даю Гарантии Заказчику
Для того, чтобы получить эксклюзивные бонусы от букмекера нужны промокоды, которые не всегда просто можно получить. В этой статье разобрано, как получить и использовать промо коды 1хБет и какие бонусы они дают новогодний промокод 1хбет
online pharmacy australia free delivery
mega – ссылка на мега тор, mega moriarty ссылка
synthroid buy online
tadalafil 60
кракен даркнет – kraken tor зеркало, kraken tor зеркало
buy synthroid
reputable overseas online pharmacies
best online pharmacy
where can i buy metformin tablets
lisinopril for sale
no prescription pharmacy paypal
zestril 20 mg price
zithromax pill
best no prescription pharmacy
synthroid cost
75 mcg synthroid no prescription
Если вам необходимы пассажирские перевозки на микроавтобусах, вы обратились по нужному адресу. Компания готова предоставить в ваше распоряжение не только целый ряд презентабельных микроавтобусов, но и услуги опытных профессиональных водителей с большим стажем работы Бургас – Кременчук
prednisone no prescription
Para retirada do seguro, o concluinte deverá portar certo documento com foto.
Also visit my site … https://lifelinefinance.in/realestate/user/profile/11427
metformin canada price
good value pharmacy
lisinopril oral
prednisone 30
MoneyGram dark markets – Movies deep web links, Social media deep web links
synthroid tablets price
how to buy valtrex online
antibiotic azithromycin
how to order generic cialis
Полный комплекс бухгалтерских услуг для юридических лиц, ООО и ИП. Ведение бухучета, сопровождение и обслуживание бизнеса. Наши бухгалтеры помогут Вам бухгалтерские услуги
can i buy synthroid from canada
top online pharmacy india
В современной промышленности важное значение имеет испытательное оборудование, позволяющее оценивать параметры изделий на различных этапах производства. Один из ключевых видов такого оборудования — вибростенды, предназначенные для испытания компонентов и сборок на устойчивость к воздействию механических колебаний Российский вибростенд купить
Standard Price for VIP- membership for 1 Week VIP Membership is 0.0014 BTC, You will do send payment to BTC address 1KEY1iKrdLQCUMFMeK4FEZXiedDris7uGd
Discounted price may be different from 0.00075 to 0.00138 BTC, that is why follow to all announces published in our Public channel!
crypto pump Binance
Thanks for another wonderful post. Where else may anyone get that kind of info in such a perfect manner of writing? I’ve a presentation next week, and I am at the look for such info.
Rybelsus
which online pharmacy is reliable
http://specodegdaoptom.ru/
tadalafil no prescription
In Etsy, Amazon, eBay, Shopify – Pinterest+SEO + artificial intelligence give high sales results
buy tadalafil 5 mg from india
generic pharmacy online
order synthroid
Aw, this was an extremely good post. Taking a few minutes and actual effort to create a top notch article… but what can I say… I hesitate a lot and don’t manage to get anything done.
Rybelsus
onlinepharmaciescanada com
big pharmacy online
where to buy synthroid online
This is the perfect site for everyone who wishes to understand this topic. You understand a whole lot its almost tough to argue with you (not that I personally would want to…HaHa). You definitely put a fresh spin on a topic that’s been written about for decades. Great stuff, just wonderful!
Rybelsus
pop over to these guys eminem skin fortnite
go to my site galaxy swapper
prednisone 2.5 mg
Hi colleagues, pleasant paragraph and fastidious arguments commented at this place, I am genuinely enjoying by these.
Studio Packages
prednisone price south africa
how to get metformin uk
generic synthroid price
discount pharmacy
how to get prednisone tablets
лайм займ
займ на карту без отказа
Гайд по проекту Grass, Руководство по проекту grass.io6
займ на карту без отказа
займ ком
buy lisinopril no prescription
PowBlocks is an exclusive decentralized layer-1 proof-of-work blockchain meticulously designed to cater to the mining community.Better than Ethereum!
заказать взлом сайта – удалить информацию из интернета, заказать ddos атаку
как узнать промокод в 1xbet – промокод 1xbet 2024, промокод на аванс 1хбет
zestril cost
glucophage 750
maple leaf pharmacy in canada
как узнать промокод в 1xbet – 1xbet официальный сайт промокод, 1хбет промокод
как ввести промокод в 1хставка – условия промокода 1xbet, промокод 1хбет на аванс
global pharmacy
веб-сайт
Беттинг
tadalafil 40mg
cost of synthroid
buy synthroid 200 mcg
where can i buy azithromycin 500mg tablets
buy zithromax no prescription
buy prednisone 10mg
vykup-avto-v-ufe.ru
lisinopril 20 mg no prescription
synthroid rx
Мы предлагаем на выбор разный номинал и наполнение сертификатов. Это может быть катание как отдельно на снегоходе и квадроцикле, так и обе активности вместе. Количество техники, длительность проката и стоимость сертификата не ограничены прогулки на квадроциклах зимой
order prednisone 10mg
1000 mg zithromax online
prednisone pill prices
Дизайнерские радиаторы отопления. Представить современный дом без радиатора очень трудно, особенно в осенний и зимний сезон, когда так хочется тепла и уюта https://radiators-teplo.github.io/
lisinopril 20 mg canadian
can you buy lisinopril over the counter
azithromycin paypal
canadian pharmacy sildenafil
valtrex 1000 mg price
Сервис онлайн заказа классической и широкоформатной фотопечати на фотобумаге, холсте, акварельной и плакатной бумаге, печать фотографий фото на холсте цена
Hi, I want to subscribe for this weblog to obtain newest updates, so where can i do it please assist.
writing service
azithromycin buy us
internet pharmacy manitoba
indian pharmacy paypal
synthroid 0.15 mg
pharmacy online 365
Изготовление стильных фотокниг недорого. Быстрая и качественная печать фотобуков на заказ. Создавайте фотоальбомы онлайн с помощью простого и бесплатного фоторедактора фотокнига онлайн
can you buy tadalafil in mexico
synthroid 37 5 mg
best online pharmacy india
canadian pharmacy online ship to usa
https://www.google.dz/url?q=https://cryptohabr.ru/
medical mall pharmacy
Заказать диссертацию онлайн. Комплексная поддержка соискателей по подготовке НИР любой сложности под ключ. Выполнение – в сумме за 120 дней по гуманитарным дисциплинам, и в сумме 150-180 дней по техническим дисциплинам заказать вкр недорого
generic cialis 2018 australia
PowBlocks is an exclusive decentralized layer-1 proof-of-work blockchain meticulously designed to mollycoddle to the mining community.PowBlocks] Better than Ethereum!
Сенсация «дела ПК «Бест Вей»: все потерпевшие оказались преступниками
Судья Богдановой
Рассмотрение липового уголовного дела, которое следствие ГСУ ГУ МВД по Санкт-Петербургу и Ленинградской области попыталось связать с компаниями «Лайф-из-Гуд», «Гермес» и кооперативом «Бест Вей», должно привести к уголовным делам против самой следственной группы и возмещению многомиллиардного ущерба прежде всего кооперативу, незаконно объявленному гражданским ответчиком. А также пайщикам кооператива, которые более двух лет лишены возможности получить свои средства из-за ареста счетов и приобрести квартиру, очередь на которую у них подошла. Ущерба как материального, так и морального.
Судебное заседание Приморского районного суда Санкт-Петербурга 21 марта – четвертое заседание и второе, на котором осуществлялось судебное следствие по делу, оказалось еще более скандальным, чем первое заседание – 14 марта, на котором проводилось судебное следствие.
Один из главных свидетелей обвинения – В. Логинов, написавший сенсационное заявление о моральном ущербе в 1 млрд рублей (см. иллюстрацию), не явился на продолжение своего допроса: прокуратура заявила, что он уехал в отпуск, хотя за день до этого он хвалился в социальных сетях, что «придет и всем покажет».
Кроме того, вызванная на 15 часов признанная следствием потерпевшей Н. Школьник (кстати, первая из лиц, которые написали заявление в правоохранительные органы, ее заявление стало краеугольным камнем расследования уголовного дела) в последний момент отказалась давать показания в суде перед самым заседанием, сославшись на то, что у нее по дороге в суд поднялась высокая температура.
Обвинение прячет своих «героев», потому что первый же допрос свидетеля обвинения в суде – допрос Логинова – вызвал конфуз и был прерван прокуратурой, а его продолжение отложено на неделю. Теперь оно отложено якобы до возвращения Логинова из отпуска (хотя он на самом деле никуда не уезжал). Как раньше, в период предварительного следствия, они не ходили на суды или один-двое приходили и сидели как статисты, так и сейчас, когда нужно обосновывать свои обвинения, обвиняющие ходить не готовы – потому что боятся, что их привлекут за выявленные при перекрестном допросе ложь и оговор.
Есть что скрывать
На заседании 14 марта Логинов заявил, что из-за «Гермеса» и кооператива «Бест Вей» он потерял квартиру, развелся и понес другие моральные страдания – потому и заявил помимо требований возмещения материального ущерба требования удовлетворения морального ущерба на миллиард, что суд воспринял с нескрываемым раздражением. Дело в том, что моральный ущерб даже за причинение смерти по судебной практике не превышает несколько миллионов рублей, в случае же «имущественного» события он может составить только десятки тысяч рублей. Кроме того, моральный ущерб должен быть обоснован – в данном же случае и события материального ущерба нет.
У Логинова никто ничего не крал. Он регулярно, много месяцев подряд, снимал со своего счета «Виста» в «Гермесе» деньги в евро, пользовался деньгами на этом счете, и его доход существенно превышает сумму, которую он положил на счет. Логинов в суде опроверг собственное заявление о том, что деньги у него украли – причем опроверг уже второй раз: в первый раз он опроверг это во время имеющегося в материалах уголовного дела допроса самим следствием, что доказывает, что в деле нет не только состава, но и события преступления, и следствие вышло в суд с необоснованным обвинением и по необоснованному же обвинению более двух лет держало обвиняемых в тюрьме (а теперь, с подачи прокуратуры, держит суд).
valtrex canadian pharmacy
valtrex price singapore
click reference 1win login
online pharmacy usa
Сенсация «дела ПК «Бест Вей»: все потерпевшие оказались преступниками
ПК Бествей приморский суд
Рассмотрение липового уголовного дела, которое следствие ГСУ ГУ МВД по Санкт-Петербургу и Ленинградской области попыталось связать с компаниями «Лайф-из-Гуд», «Гермес» и кооперативом «Бест Вей», должно привести к уголовным делам против самой следственной группы и возмещению многомиллиардного ущерба прежде всего кооперативу, незаконно объявленному гражданским ответчиком. А также пайщикам кооператива, которые более двух лет лишены возможности получить свои средства из-за ареста счетов и приобрести квартиру, очередь на которую у них подошла. Ущерба как материального, так и морального.
Судебное заседание Приморского районного суда Санкт-Петербурга 21 марта – четвертое заседание и второе, на котором осуществлялось судебное следствие по делу, оказалось еще более скандальным, чем первое заседание – 14 марта, на котором проводилось судебное следствие.
Один из главных свидетелей обвинения – В. Логинов, написавший сенсационное заявление о моральном ущербе в 1 млрд рублей (см. иллюстрацию), не явился на продолжение своего допроса: прокуратура заявила, что он уехал в отпуск, хотя за день до этого он хвалился в социальных сетях, что «придет и всем покажет».
Кроме того, вызванная на 15 часов признанная следствием потерпевшей Н. Школьник (кстати, первая из лиц, которые написали заявление в правоохранительные органы, ее заявление стало краеугольным камнем расследования уголовного дела) в последний момент отказалась давать показания в суде перед самым заседанием, сославшись на то, что у нее по дороге в суд поднялась высокая температура.
Обвинение прячет своих «героев», потому что первый же допрос свидетеля обвинения в суде – допрос Логинова – вызвал конфуз и был прерван прокуратурой, а его продолжение отложено на неделю. Теперь оно отложено якобы до возвращения Логинова из отпуска (хотя он на самом деле никуда не уезжал). Как раньше, в период предварительного следствия, они не ходили на суды или один-двое приходили и сидели как статисты, так и сейчас, когда нужно обосновывать свои обвинения, обвиняющие ходить не готовы – потому что боятся, что их привлекут за выявленные при перекрестном допросе ложь и оговор.
Есть что скрывать
На заседании 14 марта Логинов заявил, что из-за «Гермеса» и кооператива «Бест Вей» он потерял квартиру, развелся и понес другие моральные страдания – потому и заявил помимо требований возмещения материального ущерба требования удовлетворения морального ущерба на миллиард, что суд воспринял с нескрываемым раздражением. Дело в том, что моральный ущерб даже за причинение смерти по судебной практике не превышает несколько миллионов рублей, в случае же «имущественного» события он может составить только десятки тысяч рублей. Кроме того, моральный ущерб должен быть обоснован – в данном же случае и события материального ущерба нет.
У Логинова никто ничего не крал. Он регулярно, много месяцев подряд, снимал со своего счета «Виста» в «Гермесе» деньги в евро, пользовался деньгами на этом счете, и его доход существенно превышает сумму, которую он положил на счет. Логинов в суде опроверг собственное заявление о том, что деньги у него украли – причем опроверг уже второй раз: в первый раз он опроверг это во время имеющегося в материалах уголовного дела допроса самим следствием, что доказывает, что в деле нет не только состава, но и события преступления, и следствие вышло в суд с необоснованным обвинением и по необоснованному же обвинению более двух лет держало обвиняемых в тюрьме (а теперь, с подачи прокуратуры, держит суд).
цефтазидим купить – ремдесивир продать, Оземпик 1 мг 3мл аптеки в наличии
average price of zithromax
valtrax on line
cialis 2
best cheap cialis
cost of metformin
Aviator Spribe играть бесплатно
Добро пожаловать в захватывающий мир авиаторов! Aviator – это увлекательная игра, которая позволит вам окунуться в атмосферу боевых действий на небе. Необычные графика и захватывающий сюжет сделают ваше путешествие по воздуху неповторимым.
Aviator Spribe казино играть бесплатно
buy synthroid 75 mcg
metformin 1000 mg from canada
ez pharmacy
super saver pharmacy
prednisone 20 mg in india
оземпик препарат инструкция +по применению цена отзывы – оземпик препарат инструкция аналоги, mounjaro tirzepatide отзывы
how much is generic cialis
zestril online
buy valtrex over the counter
Kenyan gamers, it’s time to explore the elite online casinos in Kenya.
cialis 5mg daily price
Ознакомьтесь с большим ассортиментом отделочных материалов оптом на нашем сайте. Доставка гарантия качества по выгодным ценам оптом материалы для фасада
online pharmacy pain relief
гама казино
официальный сайт гама казино
Бизнесмен Андрей Кнауб хорошо известен как предприниматель и трейдер в сфере нефтепереработки. Он более 25 лет был частью крупнейших отраслевых компаний, реализовал множество благотворительных и социальных проектов кнауб андрей биография
these details anydesk
кэт казино
cat casino регистрация
Доставка алкоголя в Москве ночью на дом. Звоните! Доставляем алкоголь круглосуточно
online pharmacy pain relief
Hi there, constantly i used to check web site posts here early in the morning, as i like to gain knowledge of more and more.
https://28weeks.ru
her explanation tradingview
Hey! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but
I’m not seeing very good results. If you know of any please share.
Many thanks! You can read similar blog here: Sklep
tadalafil generic mexico
sure save pharmacy
lisinopril 40 mg
legitimate online pharmacy
canadian pharmacy tadalafil 5mg
average cost of prednisone
Доставка алкоголя в Москве на дом в Москве. Доставляем алкоголь круглосуточно
synthroid capsules
mounjaro 12.5 – оземпик препарат инструкция цена, оземпик можно
tadalafil cost in india
foreign pharmacy online
buspar for sleep
celecoxib vs.celebrex
prescription medicine lisinopril
synthroid 0.025 mcg
go to website MetaMask extension
узнать больше
купить трамадол без рецепта
Известный бизнесмен Кнауб Андрей Артурович родился в г. Сургуте Тюменской области. Суровый климат с детства закаляет характер, поэтому не удивительно, что будущий предприниматель сумел в буквальном смысле сделать самого себя кнауб андрей артурович
lisinopril 12.5 mg tablets
top casino best
online casino site
Доставка алкоголя в Москве на дом в Москве. Доставляем алкоголь круглосуточно
buy valtrex tablets
Предприниматель придерживался мнения, что заботиться надо не только о персонале, но и окружающей среде кнауб андрей
tadalafil pills 20mg
safe online pharmacy
В биографии бизнесмена Андрея Артуровича Кнауба важно отметить, что для него ключевое значение имела забота о персонале и экологической обстановке в регионе кнауб андрей томскнефтепереработка
gama casino регистрация
dverivsaunu-spb.ru
online pharmacy fungal nail
Hi there all, here every one is sharing these kinds of know-how, so it’s good to read this web site, and I used to pay a quick visit this webpage daily.
here about reddit USDT
buy synthroid india
Hello to every body, it’s my first pay a quick visit of this webpage; this webpage contains awesome and truly excellent information in support of readers.
artrolux+ cream
metformin 250 mg price
canada happy family pharmacy
Excellent article. Keep posting such kind of information on your blog. Im really impressed by your site.
Hey there, You’ve done an excellent job. I will certainly digg it and for my part recommend to my friends. I am sure they will be benefited from this web site.
cardiobalance opiniones
Доставка алкоголя в Москве
Good post. I learn something totally new and challenging on websites I stumbleupon on a daily basis. It’s always helpful to read content from other writers and use something from their websites.
test cardiobalance
Thanks for the good writeup. It in truth was a leisure account it. Glance complex to far brought agreeable from you! By the way, how could we keep in touch?
depanten pret
Hi! This post could not be written any better! Reading this post reminds me of my old room mate! He always kept chatting about this. I will forward this write-up to him. Fairly certain he will have a good read. Thanks for sharing!
depanten capsule
PowBlocks is an one decentralized layer-1 proof-of-work blockchain meticulously designed to pamper to the mining community.PowBlocks] Better than Ethereum!
Hello to all, how is all, I think every one is getting more from this site, and your views are good in favor of new viewers.
no deposit bonus for ripper casino
Please let me know if you’re looking for a article writer for your blog. You have some really good articles and I think I would be a good asset. If you ever want to take some of the load off, I’d absolutely love to write some content for your blog in exchange for a link back to mine. Please shoot me an email if interested. Kudos!
crypto gambling with baccarat
Egor Alexandrovich Abramov’s personal life remains guarded, allowing his work to speak volumes about his dedication to the craft egor abramov
Today, I went to the beach with my children. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is entirely off topic but I had to tell someone!
bee beep casino
Доставка алкоголя в Москве
Just desire to say your article is as astonishing. The clearness in your put up is simply great and i can assume you are knowledgeable on this subject. Well with your permission allow me to seize your feed to stay updated with forthcoming post. Thank you 1,000,000 and please keep up the gratifying work.
yabby casino app
metformin 134
Читайте статью на vc.ru https://vc.ru/crypto/1099363-kak-prodat-notkoin-notcoin-sposoby-prodazhi-instrukcii-i-sovety-novichkam как продать Ноткоины сегодня по отличной цене. Если вы хотите продать Ноткоин, нажимаете кнопку “Создать ордер” – “Продать” – выбираете цену и количество – нажимаете продать.
prednisone 1 mg daily
Доставка алкоголя
best canadian pharmacy no prescription
cardiovascular safety of celecoxib, naproxen, or ibuprofen for arthritis
официальный сайт гама казино
Gama Casino
Egor Abramov’s biography, initiated by chance, has evolved into a promising career, and as he continues to make his mark in the cinematic landscape, audiences can anticipate more captivating performances from this talented young actor egor abramov
azithromycin for sale usa
cheapest tadalafil online uk
best online pharmacy no prescription
Российский завод продает разборные гантели https://gantel-razbornaya.ru – у нас найдете объемный каталог вариантов. Настраиваемые снаряды позволяют продуктивно выполнять силовые тренировки в любом месте. Спортивные снаряды отличаются качеством, безопасностью в использовании. Организация продуктивно развивает и внедряет свежие идеи, чтобы исполнить желания постоянных покупателей. В изготовлении надежных снарядов всегда используются высококлассные марки чугуна. Значительный ассортимент продуктов дает возможность приобрести разборные отягощения для продуктивной программы тренировок. Для домашних занятий – это лучший комплект с компактными габаритами и большой универсальности.
узнать https://xn—-jtbjfcbdfr0afji4m.xn--p1ai/
buy tadalafil 100mg
Despite his youth, Egor Abramov has already earned critical acclaim and popularity among viewers. His growth as an actor portends a bright future and opens up new opportunities in Russian cinema egor alexandrovich abramov
super saver pharmacy
Наш путеводитель по Санкт-Петербургу собрал лучшие отели и места для туристов водные экскурсии в Санкт-Петербурге Мы расскажем, в каких кафе можно бюджетно перекусить, где попробовать особенные блюда с местным колоритом или отужинать, как потомки аристократов.
synthroid 0.025 mg
tadalafil 40 mg uk
azithromycin 40 mg
valtrex 1000 mg daily
prednisone corticosteroids
Посудомоечные машины – популярны, экономят время, воду, деньги. Разные по размеру, цене, функциям. Вместительные, тихие, энергосберегающие. Выбор зависит от нужд. Срок службы – 10 лет. Важно знать функции и цену. Рекомендуются Smeg ПММ
valtrex prescription
Женский онлайн-журнал для стильных, модных и уверенных в себе представительниц прекрасного пола. Здесь вы найдете советы и подсказки, как правильно худеть, что надеть на вечеринку и как создать незабываемый женственный образ глинтвейн рецепт приготовления
Производимые отечественным производителем тренажеры для кинезитерапии trenazhery-dlya-kineziterapii.ru и специально разработаны для восстановления после травм. Конструкции имеют оптимальное соотношение стоимости и качества.
Продаем очень доступно Кроссовер с перекрестной тягой с усиленной конструкцией. В каталоге для кинезитерапии всегда в реализации варианты блочного и нагружаемого типа.
Изготавливаемые тренажеры для реабилитации гарантируют комфортную и безопасную тренировку, что особенно важно для тренирующихся пациентов в процессе восстановления.
Станки обладают подстраиваемым сопротивлением и уровнями нагрузки, что позволяет индивидуализировать занятия в соответствии с задачами любого больного.
Все тренажеры актуальны для ЛФК по методике врача Сергея Бубновского. Оснащены рукоятками для удобного выполнения тяг в наклоне или лежа.
generic synthroid 200 mcg
canadian pharmacy 24
glucophage cost in india
Практичная армейская раскладушка для комфортного отдыха в походах и экстремальных условиях придбати розкладне армійське ліжко
Доставка алкоголя
Egor, along with central actors, explores more mature themes in the latest season, depicting the evolving challenges faced by their characters egor abramov entrepreneur
prednisone 59 mg
online pharmacy quick delivery
tadalafil 15mg
5 mg prednisone daily
Доставка алкоголя Москва
Наша типография предлагает широкий спектр услуг, связанных с печатью и производством различных материалов. У нас есть опытные специалисты и современное оборудование, чтобы гарантировать высокое качество и быструю обработку заказов типография
Melden Sie sich an, um ein Willkommenspaket im Wert von 1.000 USDT zu erhalten!
Kaufen Sie Kryptowährungen https://www.bitget.com/de
synthroid 0.088 mg
where to buy cialis online canada
In both 2014 and 2015 Alexandre Cougnaud raced in the Porsche Carrera Cup France championship. He finished in 10th position the first year and in 12th position the second year https://lat.motorsport.com/driver/alexandre-cougnaud/659025/
discount cialis for sale
Good day! This post could not be written any better! Reading through this post reminds me of my good old room mate! He always kept chatting about this. I will forward this post to him. Fairly certain he will have a good read. Thanks for sharing!
Аrtropant +
pharmaceutical online ordering
It’s amazing to pay a visit this web site and reading the views of all friends about this paragraph, while I am also eager of getting familiarity.
cbdus+ kapszula
Hey fantastic website! Does running a blog such as this require a large amount of work? I have no expertise in computer programming but I had been hoping to start my own blog soon. Anyways, should you have any suggestions or techniques for new blog owners please share. I know this is off topic however I just wanted to ask. Many thanks!
depanten lek na stawy
I got this website from my buddy who shared with me concerning this website and now this time I am visiting this web page and reading very informative articles or reviews here.
keramin gyakori kerdesek
buy azithromycin over the counter usa
how to get valtrex online
Good post. I learn something new and challenging on sites I stumbleupon everyday. It’s always interesting to read through articles from other authors and use a little something from other sites.
dr max keramin
Right now it sounds like WordPress is the top blogging platform out there right now. (from what I’ve read) Is that what you’re using on your blog?
keramin krema cijena
Excellent post. Keep posting such kind of information on your page. Im really impressed by it.
Hi there, You’ve done a fantastic job. I will definitely digg it and personally suggest to my friends. I am sure they’ll be benefited from this website.
oculax forum
Hello i am kavin, its my first occasion to commenting anyplace, when i read this article i thought i could also make comment due to this sensible post.
masters dissertation writing help
This is really interesting, You are a very skilled blogger. I’ve joined your rss feed and look forward to seeking more of your magnificent post. Also, I’ve shared your web site in my social networks!
casino accepting payid
best us price tadalafil
Thank you, I have just been looking for info approximately this subject for ages and yours is the best I’ve found out till now. However, what concerning the conclusion? Are you certain about the supply?
best online casinos for real money
Your sales on Etsy, Amazon, ebay, shopify.
tadalafil cost pharmacy
buying prednixone for animals
I think that everything wrote was actually very reasonable. But, think on this, what if you were to write a killer headline? I mean, I don’t wish to tell you how to run your website, however suppose you added a post title that grabbed people’s attention? I mean %BLOG_TITLE% is a little boring. You might peek at Yahoo’s front page and watch how they create article titles to grab people to click. You might add a related video or a picture or two to get readers interested about what you’ve written. Just my opinion, it would make your posts a little livelier.
#best#links#
аренда номера
Доставка алкоголя
Hi I am so excited I found your web site, I really found you by error, while I was browsing on Digg for something else, Nonetheless I am here now and would just like to say thanks a lot for a tremendous post and a all round thrilling blog (I also love the theme/design), I don’t have time to read it all at the moment but I have saved it and also added your RSS feeds, so when I have time I will be back to read more, Please do keep up the great work.
http://kiagpt.com/bbs/board.php?bo_table=free&wr_id=43172
azithromycin 39 tablets
lisinopril tablets uk
azithromycin canada no prescription
synthroid 125 mg
Download 2,681 safari icons. Available in PNG and SVG formats. Ready to be used in web design, mobile apps and presentations safari icon
synthroid generic price
Please let me know if you’re looking for a writer for your site. You have some really great articles and I believe I would be a good asset. If you ever want to take some of the load off, I’d really like to write some content for your blog in exchange for a link back to mine. Please blast me an e-mail if interested. Cheers!
Официальный сайт Гама казино
Premium базы для Xrumer 23 ai Strong и GSA Search Engine Ranker. https://dseo24.monster
Hi there, its nice article concerning media print, we all understand media is a enormous source of information.
Официальный сайт Гама казино
Hello to every one, because I am genuinely keen of reading this webpage’s post to be updated on a regular basis. It includes nice stuff.
Витамикс – Vitamix Energy полезен для желудка 800
top casino site
casinos online
Современная потолочная люстра для гостиной люстра для спальни освещение кухни может быть затемнением приложения с помощью пульта дистанционного управления акриловый материал завод прямых продаж лампа люстра накладная потолочная
54899 prednisone
Aviator Spribe играть онлайн казино
Добро пожаловать в захватывающий мир авиаторов! Aviator – это увлекательная игра, которая позволит вам окунуться в атмосферу боевых действий на небе. Необычные графика и захватывающий сюжет сделают ваше путешествие по воздуху неповторимым.
Aviator Spribe играть на компьютере казино
buy valtrex online mexico
Hi there! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good results.
If you know of any please share. Kudos! You can read similar article here:
Scrapebox AA List
cost of brand synthroid
750 mg metformin
metformin 300 mg daily
cialis cost australia
online pharmacy denmark
cost for 2 mg lisinopril
where to buy cheap tadalafil
synthroid 1.5
generic synthroid prices
live casino online
online casino usa
Готовьтесь к безумию: Американское правительство предупреждает о солнечном затмении, грозящем нарушить все. Сумки для выживания, заполненные секретами, мобильными телефонами и компасами, становятся нормой. Откройте правду в нашем захватывающем видео! https://vm.tiktok.com/ZGemYu97R/
the canadian pharmacy
metformin over the counter australia
lisinopril 20 mg online
where can i buy zithromax uk
synthroid prescription online
Купить диплом в Рязани недорого – с доставкой по регионах, по приятной цене, без предоплаты http://diploms-service.com/dopolnitelnoe-obrazovanie/udostoverenie-o-povyshenii-kvalifikatsii
rx pharmacy online 24
Купить диплом в Рязани недорого – с доставкой по регионах, по приятной цене, без предоплаты http://diploms-service.com/diplomy-po-gorodam/sankt-peterburg/russkaya-khristianskaya-gumanitarnaya-akademiya
Покупка семян это одно из более главных решений для каждого садовода или фермера. Выбор качественных и подходящих семян определяет фуррор будущего урожая и результатов ваших усилий. Поэтому перед покупкой зёрен стоит уделить достаточное внимание выбору правильного поставщика и качеству продукта.
До этого всего, стоит определить, купить семена в магазине https://boomgamse.ru/konoplya-na-okne/ купить семена с доставкой какие растения вы собираетесь растить. Например, если у вас есть огород, для вас пригодятся семена овощей помидоров, огурцов, моркови и т.д. Для тех, кто занимается цветоводством, принципиально избрать зёрна цветов либо декоративных растений.
После того, как определены предпочтения по культурам, следует выбрать надежного поставщика. Важно избирать компании, имеющие превосходную репутацию и предлагают качественные продукты. Проверьте отзывы и рейтинги онлайн, обратитесь к знакомым садоводам или фермерам за советами.
synthroid 100 pill
online pharmacy no rx
online pharmacy 365 pills
canadian pharmacy drugs online
https://avto-dublikat.ru/
semaglutide 2.5mg/ml
Официальный сайт 1Вин казино предлагает лицензионные игры с высокой отдачей, но для захода требуется найти зеркало 1win casino 1Win casino
top online pharmacy 247
where to buy synthroid
synthroid discount
https://ellak.gr/user/michaelx60/
canadian pharmacy online ship to usa
prednisone online paypal
over the counter valtrex medication
tadalafil best price 20mg uk
prednisone 59 mg
buy lisinopril in mexico
Henkuai y Marca Espanahan organizado la visita de los diez influencers chinos mas importantes a Espana con el objetivo de promocionar el pais. Estos acumulan entre todos mas de 30 millones de seguidores y abarcan campos muy diferentes https://simpleflying.com/madrid-airport-chinese-passengers/
Доставка алкоголя
Vidalista 20 – This is a quality product for men who want to increase their masculine abilities in intimate life effectively and safely kaufen vidalista 80
buy synthroid medication online
buy lisinopril uk
https://www.transformacioneducativa.edu.py/profile/stanleyvbz35/profile
cilias
tadalafil 80mg
Букмекерская компания Мостбет является ведущим игроком не только на рынке России, но и в других странах, включая Казахстан, Узбекистан, Азербайджан, Киргизию и многие другие. Легальный статус компании гарантирует честную и безопасную игру mostbet
lisinopril 12.5 mg
Опираясь на ретро-футуристическое очарование вселенной Fallout, сериал отражает суть эпохи, характеризующейся смесью оптимизма и отчаяния. Когда персонажи сталкиваются с моральными трудностями и ужасами постапокалиптической дикой природы, они отправляются в путешествие самопознания, формируя связи и сражаясь с противниками, в поисках искупления и смысла в разрушенном мире Фоллаут сериал
https://njit-connect.njit.edu/rwd/responsive-discussion-board?dgs3235=3&rid3235=8426&tid3235=2924
actos cpr
Купить травматическое оружие, пистолет или револьвер – выбор за вами, у нас лучшие цены и популярные модели всегда в наличии! Наша жизнь полна скрытых угроз и опасностей Купить лицензию на оружие
canadian pharmacy online store
prednisone online canada
Проверенный магазин, низкие цены на аккаунты с токенами, моментальная выдача купленного аккаунта, высокая репутация магазина. Купите один раз и будете нашим постоянным клиентом! Так-же занимаемся продвижением модельного аккаунта BongaCams как купить токены на бонго
https://iredefine.rutgers.edu/sites/default/files/webform/%D0%A0%D0%B0%D1%81%D0%BA%D1%80%D1%8B%D1%82%D0%B8%D0%B5%20%D0%BE%D1%87%D0%B0%D1%80%D0%BE%D0%B2%D0%B0%D0%BD%D0%B8%D1%8F%20%D0%91%D1%80%D0%B0%D1%81%D0%BB%D0%B0%D0%B2%D0%B0.pdf
legit pharmacy websites
safe online pharmacy
predinson prescriptions
metformin otc mexico
metformin for sale canada
https://www.linkedin.com/pulse/%25D1%2580%25D0%25B0%25D1%2581%25D0%25BA%25D1%2580%25D1%258B%25D0%25B2%25D0%25B0%25D1%258F-%25D0%25BE%25D1%2587%25D0%25B0%25D1%2580%25D0%25BE%25D0%25B2%25D0%25B0%25D0%25BD%25D0%25B8%25D0%25B5-%25D0%25BC%25D0%25B8%25D0%25BD%25D1%2581%25D0%25BA%25D0%25B0-%25D0%25B2%25D0%25B0%25D1%2588%25D0%25B5-%25D0%25BF%25D0%25BE%25D0%25BB%25D0%25BD%25D0%25BE%25D0%25B5-%25D1%2580%25D1%2583%25D0%25BA%25D0%25BE%25D0%25B2%25D0%25BE%25D0%25B4%25D1%2581%25D1%2582%25D0%25B2%25D0%25BE-%25D0%25BF%25D0%25BE-md-soikot-urcoc/
synthroid 0.025 mg
prednisone10 mg
buy valtrex online australia
buy generic synthroid
buy azithromycin over the counter
over the counter synthroid
canadian pharmacy meds
online pharmacy dubai
canadian happy family store coupon
Just want to say your article is as astounding. The clearness in your put up is just great and i can suppose you’re an expert in this subject. Fine along with your permission allow me to grasp your feed to keep up to date with drawing close post. Thanks one million and please continue the enjoyable work.
https://de.wikibrief.org/
Доставка алкоголя
кредитные карты юниаструм банка купить – список пассажиров, Monzo
Промокод 1xBet на сегодня и бесплатно. Промокоды 1хбет 2024 требуется использовать те, которые предоставят игрокам самые лучшие бонусы. Каждый из них позволяет увеличить первый депозит в 2 раза, максимальная сумма увеличения – 100 долларов. Большое количество промокодов — одна из причин того, что на сайте регистрируется огромное количество новых игроков каждый день. На данный момент их количество превышает пятьсот тысяч уникальных пользователей каждый день. Действующие промокоды позволяют увеличить размер приветственных баллов до 32 500 рублей. Для этого нужно лишь активировать при регистрации имеющийся код, скопировав его в соответствующее поле. Букмекерская контора 1ХБет является одной из самых влиятельных на рынке игорного бизнеса в России и не нуждается в особом представлении. Впрочем, букмекер продолжает держать статус одного из самых щедрых и предлагает своим клиентам воспользоваться промокодами для халявы, – более подробно в этом материале https://mg-group74.ru/pages/1xbet.html.
Турецкие сериалы для увидения турецких национальных праздников; Возможность увидеть турецкие национальные праздники турецкие сериалы про пиратов
happy family canadian pharmacy
how to get metformin uk
cialis pill
Pin Up Casino (Пин Ап) официальный сайт онлайн казино в Казахстане. На официальном сайте казино Пин Ап можно найти большой выбор лотоматов, которые позволяют игрокам играть в онлайн режиме и зарабатывать реальные деньги пин-ап
check out the post right here https://trezorwallet-app.org/2023/11/14/exploring-advanced-features-of-the-trezor-wallet-app-for-experienced-cryptocurrency-users/
browse around here https://blur-nft-marketplace.org/2022/03/08/blur-the-latest-contender-in-the-privacy-coin-realm-challenging-coinbase/
this link https://blur-io-nft.com/2023/11/09/the-blurred-beauty-of-blur-nfts-an-aesthetic-exploration/
https://elearning.urp.edu.pe/author/stanleyvbz35/
go right here https://tronlink.at/2023/11/13/tronknight-announces-the-launch-of-46m-usdt-on-tron-blockchain-in-a-game-changing-move/
helpful site https://debank.at/2023/11/11/leveraging-the-potential-of-web3-messaging-with-debank/
blog https://trezor-wallet.at/2023/11/14/exploring-the-worst-case-scenarios-for-crypto-holders-analyzing-the-failure-of-trezor-and-its-implications/
her comment is here https://tronlink-app.org/2023/11/13/understanding-the-complexities-of-trons-an-in-depth-guide-to-this-revolutionary-technology/
azithromycin 500mg price in india
site web https://debank.lu/2023/11/11/exploring-debanks-impact-on-the-crypto-industry-analyzing-its-contributions-and-evolution/
Going Here https://blur-nft-market.com/2023/11/10/exploring-the-latest-opportunities-and-trends-in-investing-in-solana-nfts/
legit pharmacy websites
http://sse-tuc.edu.gr/web/stanleyjhgfd/home
prednisone 2 mg tablets
lisinopril pill 5 mg
tadalafil 40mg
Embark on an unforgettable water adventure with our portal, where you can rent marine luxury in addition to charter boats and other vessels. Peruse numerous listings from boat owners providing a diverse range of ships, including yachts, boats, sailing vessels, jet skis and similar. Whether you are in search of a premium yacht for celebrities, a boat for fishing for a day out on the water, or a celebration boat, our platform can aid you in finding the right choice. With the choice to hire a yacht with or without a captain, you can discover the perfect one according to your preferences. https://boatrent.shop/ Feel the pinnacle of luxury with our VIP yacht rental or select an budget-friendly but unforgettable experience with our budget-friendly yacht charter. Irrespective of your selection, our site guarantees smooth booking, exceptional service, and unforgettable memories on the water. Start your adventure today and discover the fun of hiring boats and boats with us.
synthroid purchase
обнал коллцентров – сбербанк карта, сим карты продать
Affordable Roof Care Services
zestril 20 mg cost
online pharmacy com
https://revistas-old.fapas.edu.br/litterarius/comment/view/1128/949/417430
synthroid pills
Вступайте в увлекательное приключение вместе с нами и отправляйтесь в мир радости и азарта игра дог хаус Наши игры наполнены азартом и весельем, и каждый спин приносит удовольствие и шанс на крупный выигрыш.
how can i get prednisone
why not check here https://orbiter-finance-bridge.com/2023/11/18/the-benefits-of-using-orbiter-finances-decentralized-cross-rollup-bridge-for-ethereum-native-assets/
websites https://1inch-app.org/2023/11/17/the-impact-of-the-1inch-token-on-liquidity-provision-in-defi/
why not try here https://orbiter-finance.at/2022/09/29/exploring-orbiter-finance-the-decentralized-cross-rollup-bridge-on-ethereum/
reference https://1inch-dex.com/2022/07/13/the-significance-of-diversification-when-investing-in-the-1inch-coin-market-cap/
prednisone 20mg for sale
Более подробно ознакомиться с вебкам чатом можно тут – https://rt.livepornosexchat.com/
description https://galxe-app.org/2023/11/19/nft-galxe-the-future-of-digital-collectibles/
linked here https://metamask-wallet.at/2023/11/16/unlocking-new-opportunities-integrating-binance-chain-with-metamask/
blog link https://metamask-wallet-web3.com/2023/11/16/integrate-solana-with-metamask-unlocking-the-solana-network/
official statement https://galxe-web3.com/2023/11/19/exploring-the-rising-popularity-of-galxe-in-google-search/
http://www.alexandria.gov.eg/Lists/List30/DispForm.aspx?ID=60164
Криптовалютные биржи — это платформы, которые дают возможность трейдерам покупать и продавать криптовалюты, деривативы и другие криптоактивы лучшие биржи криптовалют +для россии
slot demo gates of olympus – игровые автоматы gates of olympus на деньги, гейтс оф олимпус играть
lisinopril 1.25
https://ifa.edu.pe/forums/users/stanleyvbz35/
кредитные карты россельхозбанк – карты сбербанка карты, карта сбербанка маэстро
reputable online pharmacy
дебетовые карты альфа банк – куплю карту банка, банковская карта альфа банк
tadalafil 20mg canada
https://www.just.edu.jo/Lists/Survey/DispForm.aspx?ID=7565
подарок дедушке +на новый год – печать +на футболках сосновоборск, печать надписей +на футболках
Вывод из запоя
top 10 pharmacies in india
печать листовок а5 – упаковка на заказ, календари квартальные
Известный во всем СНГ телеграмм бот Глаз Бога уже почти год не сходит с первых полос множества новостных агентств. Программа Глаз Бога для поиска людей завоевала огромную популярность у многих пользователей глаз бога программа
canadian pharmacy online store
официальный сайт кэт казино
cat казино играть
игровые автоматы gates of olympus на деньги – gates of olympus demo играть, gates of olympus на деньги
энергетические напитки из Азии оптом – импортные кексы оптом, китайские газированные напитки оптом
continue reading this download galaxy swapper v2
http://journals.hnpu.edu.ua/index.php/literature/comment/view/4159/0/10862
Нарколог на дом
промокоды для lucky jet – как играть в lucky jet, лак джет
cialis price in usa
http://www.monofeya.gov.eg/citizens/cases/Lists/List38/DispForm.aspx?ID=31081
lisinopril 200 mg
buy lisinopril 20 mg without a prescription
antibiotics zithromax
repaglinide zulassung
azithromycin generic brand
legal canadian pharmacy online
valtrex pills where to buy
synthroid 50mg
secure medical online pharmacy
https://medicine.ju.edu.jo/Lists/ConfReg/DispForm.aspx?ID=71490
lucky jet играть – lucky jet демо счет, lucky jet бонус
Buy Apple Gift Card. Use it to shop the App Store, Apple TV, Apple Music, iTunes, Apple Arcade, the Apple Store app, apple.com, and the Apple Store the gift card for everything apple
Промокод 1xbet на сегодня. Промокод на 2024-2024. На официальном сайте букмекерской конторы 1xbet появилась опция, которая позволяет “бесплатно” ознакомиться с функционалом сайта и при удачном стечении обстоятельств еще и выиграть некую сумму денежных средств. Теперь это стало доступно по специальному промокоду 1хБет. Он дает возможность получить до 32500? (100$). Актуальные промокоды 1xbet на сегодня: 1XFREE777. Рабочие промокоды 1XBet в 2024 Все промокоды для 1хбет бесплатно: при регистрации, на ставку (купон), на бонус, на сегодня. 1xBet — одна из самых известных компаний в сфере беттинга. Свою популярность контора заработала во многом благодаря большому количеству специальных предложений. Так, к примеру, каждый пользователь может воспользоваться одним из действующих промокодов 1xBet на сегодня бесплатно. Ознакомиться с их полным перечнем можно в данной статье – более подробно в этом материале http://dizkomp.ru/netcat/inc/1xbet.html
https://www.moe.gov.sa/ar/education/highereducation/Lists/Survey/DispForm.aspx?ID=6160
best tadalafil
tadalafil pills in india
canadian pharmaceutical happy family stores
cheap zithromax online
Top online casіos!
Get Big bоnus for frее singup
https://tinyurl.com/2ufpar4v
no prescription needed pharmacy
buy azithromycin uk
metformin 2000 mg
order zithromax online
Организация корпоративов подразумевает различные программы: тимбилдинги, командные тренинги, соревнования и батлы, семинары на природе и т. д организация корпоративов
Привет, дорогой читатель!
Бывало ли у вас такое, что приходилось писать дипломную работу в очень ограниченные сроки? Это действительно требует большой ответственности и тяжелого труда, но важно не сдаваться и продолжать активно заниматься учебными процессами, так же, как и я.
Для тех, кто умеет эффективно использовать интернет для поиска и анализа информации, это действительно облегчает процесс согласования и написания дипломной работы. Не нужно тратить время на посещение библиотек или организацию встреч с дипломным руководителем. Здесь представлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по всей России. Можете ознакомиться с предложениями по ссылке , это проверенный способ!
купить диплом техникума
купить диплом университета
купить диплом техникума
купить диплом института
купить аттестат школы
купить диплом магистра
Желаю каждому отличных отметок!
Натяжные потолки
tadalafil best
Top internet casіos!
Get Bigs bоnus for frее singup
https://tinyurl.com/yu7ex6h4
valtrex order canada
generic valtrex for sale
where can i buy prednisone over the counter uk
cheap generic synthroid
synthroid purchase
canadapharmacyonline
Продвинуть Сайт в Алматы максимальная видимость в поисковых системах, точечная аудитория, уникальные стратегии роста. Достижение вершин онлайн-успеха!
tadalafil 10mg daily
no rx pharmacy
prednisone without a prescription
prescription valtrex online
tadalafil soft gel
In Etsy, Amazon, eBay, Shopify Pinterest+SEO + artificial intelligence give high sales results
175 mg synthroid
zithromax 250 tablet
tadalafil for sale
synthroid 60 mcg
Free drawing lessons for beginners and professionals Drawing lessons
zestril discount
I wanted to share an insightful resource on the best algorithmic trading strategies that I recently came across. This blog post on https://uberant.com/article/2006415-mastering-the-art-of-backtesting-algo-strategies/ provides an in-depth exploration of effective algorithmic trading strategies. Whether you’re new to algorithmic trading or looking to enhance your existing strategies, this resource offers valuable information that can help optimize your trading approach. I highly recommend checking it out for practical insights and actionable tips.
american pharmacy
Доставка алкоголя в Москве
synthroid 62.5 mg
canadian pharmacy 24
metformin 500mg tablets price in india
cheap cialis canada pharmacy
Greetings fellow forum members! I wanted to share an insightful article I came across about the essentials of proprietary trading. It provides a comprehensive understanding of how this intricate process works. If you’re looking to delve deeper into the world of trading, I highly recommend giving it a read:https://niadd.com/article/1192060.html . Happy reading and happy trading!
Отечественный производитель продает блины в интернет-магазине diski-dlya-shtang.ru для усиленной эксплуатации в коммерческих тренажерных центрах и в домашних условиях. Российский завод создает цельнометаллические диски разного посадочного диаметра и любого востребованного веса для разборных штанг. Рекомендуем к приобретению обрезиненные тренировочные диски для силовых занятий. Они не скользят, не гремят и менее травматичны. Изготавливаемые изделия не нуждаются в постоянном обслуживании и рассчитаны на длительную работу в дома, в квартире. Рекомендуем внушительный ассортимент профессиональных дисков с любым классом покрытия. Купите отягощения с подходящей массой и посадочным диаметром по низким ценам напрямую у компании-производителя.
online pharmacy denmark
canadian pharmacy india
mail pharmacy
best price generic tadalafil
дулаглутид цена отзывы – сколько стоит лираглутид, трулисити купить дешевле
lisinopril 2
how to buy valtrex
canadian online pharmacy no prescription
how much is metformin cost
more information free cs2 cheats
internet cheats roblox
кракен зеркало тор – kraken darknet market ссылка тор, кракен онион
cheapest cialis 40mg
navigate to this site localcryptos alternative
Hunting for an incarcerated liked just one might be a disheartening system. Luckily, Every single prison program has an inmate locator Instrument that can assist you. When you are searhing for a California federal inmate look for Software, you’ve arrive at the ideal spot.
The “blue collar” Model of Neal, a thief, and archrival of Neal, Keller was arrested and jailed by Peter but later on escaped and attempted to steal the U-boat treasure that Neal and Mozzie have.
The knowledge delivered on this Web-site is for informational functions only and isn’t going to constitute authorized guidance. In certain jurisdictions, This can be considered lawyer promoting. Simply reading through this data doesn’t produce a legal professional-shopper relationship.
white collar prison consultant
Items might need been a whole lot various had I not satisfied Michael Santos, a fellow convict, on my to start with working day inside.
Most of them is not going to Have a very clearly described release day and, because they don’t Possess a launch day, there may be a better proclivity for violence.”
https://whitecollar.blog/should-i-hire-a-prison-consultant/
Log in Subscribe Professions I had been a stockbroker at UBS who went to prison for fraud. Now I am a white-collar prison consultant who helps substantial-profile clients get by their time in lockup — Here is what my occupation is like.
Sign on for getting The within scoop on currently’s major tales in markets, tech, and business — sent everyday. Read through preview
may well receive a portion of sales from products which are procured by way of our site as A part of our Affiliate Partnerships with shops.
California male inmates reside in two-particular person cells. A few offenders can be required to live in a two-individual mobile during the SHU if overcrowding occurs or When they are pending transfer in other places although on holdover standing.
Immediately after some hesitation, Burke agrees, resulting in Neal staying released early from prison and working being an FBI consultant and Burke’s prison informant. They So get started their unconventional and testy relationship as they got down to seize elusive and hazardous white collar criminals in Ny city. Forged and people
Prison consultants can describe how the prison legal earth functions – from investigation to incarceration and each of the ways in between, what it means for you, and what issues in order to avoid.
Nonetheless, you don’t need to have to attend until you’ve been arrested to hire a prison consultant. You are able to arrive at out to the consultant just because you’re worried you
As an alternative to blowing the whistle on him, I saved my mouth shut to enable the commissions to continue to roll in, which built me complicit.
When Operating as an investment banker at UBS, Paperny was involved with a fraudulent hedge fund that was Element of a Ponzi scheme. He pleaded guilty in 2007 to conspiracy to commit mail, wire, and securities fraud and was stripped of his licenses to sell shares and real estate.
kraken darknet market ссылка – кракен тор, kraken darknet market ссылка тор
i thought about this cs2 free skin changer
synthroid 112 coupon
published here keplr Extension
tadalafil tablet 5mg
sure save pharmacy
lisinopril 40 mg coupon
kokulu mum
reddit canadian pharmacy
web phantom login
wikipedia reference martianwallet wallet download
american pharmacy
useful source keplr Extension
cialis generic price
check that rabby wallet download
wikipedia reference martianwallet login
3 lisinopril
synthroid 175
Gama Casino is a new gambling establishment. Gama casino opened in 2024, delighting players with big bonuses: 200% on account replenishment http://www.pawsarl.es/blog/%D1%8D%D0%BB%D0%B4%D0%B0%D1%80.html
can i buy metformin over the counter in uk
valtrex brand coupon
Привет, дорогой читатель!
Купите диплом ВУЗа по выгодной цене с гарантией качества и доставкой в любой город России без предоплаты – просто и надежно!
http://saksx-attestats.ru/
Получите диплом ВУЗа по выгодной цене с доставкой в любой город России без предоплаты и с гарантированной законностью документа!
Предлагаем заказать диплом у нас с доставкой курьером по всей России без предоплаты.
Доставка алкоголя в Москве
tadalafil generic coupon
order tadalafil online india
Современное виртуальное пространство становится все более конкурентным, и, чтобы быть замеченным, необходимо принять четкий курс на оптимизацию своего представительства в интернете. Когда дело касается повышения видимости бизнес-сайта в Москве, оптимизация под поисковые системы (ОПС) играет особую роль.
novapromotions.ru
tadalafil online buy
cialis 10 mg
Стальные трубчатые радиаторы RIFAR Tubog с гарантией 10 лет. Сделано в России. https://ctoday.ru/radiatory-tubog-novaya-era-v-otoplenii-vashego-doma/
Bonuses keplr wallet login
where to buy valtrex online
synthroid 50 mcg cost
seo hizmeti
canada pharmacy world
your pharmacy online
У слота Gates of Olympus играть демо бонуска позволяет по тем же техническим характеристикам, какие есть в основной версии. Коэффициенты возврата и частота выплаты призов не меняются в принципе. Купить бонусный раунд у слота нельзя gates of olympus бонуска
where to buy prescription synthroid
lisinopril 10 12.5 mg
su yalıtımı
where can i get prednisone
The Best Attractions in Macau – Best things to do in United States, Top Places to Visit in Bahrain
виртуальный сервер vps vds – вдс сервер, vds хостинг дешевый
synthroid 50 mcg tablet
1 lisinopril
ısı yalıtımı
Новая Орбита
generic cialis india
Широкий выбор грузовых запчастей для различных моделей и марок грузовиков Запчасти грузовиков man
onlinepharmacytabs24 com
azithromycin 1 g without prescription
prednisone purchase
Выбирая нас, вы получаете быструю и профессиональную эвакуацию по разумной цене · Любая сложность. 10-летний опыт. Профессиональный подход. Официально https://yslygi66.ru/kak-otmenit-podpisku-na-android
cost of cialis without prescription
aydın çıkışlı turlar
Best things to do in Hong Kong – Best Restaurants in Cyprus, Best Restaurants in Belarus
vds сервер купить – vps хостинг москва, купить vds хостинг
buy generic tadalafil online cheap
purchase generic valtrex online
janumet sitagliptin and metformin hcl
where can i get valtrex over the counter
Based on God’s instructions, Abraham travelled to a place called Canaan where the Canaanites lived. There is no reason given for God’s choice of Palestine/Canaan for Abraham to journey to adriatic sea on map
aydın çıkışlı turlar
tadalafil 2.5 mg generic
discount valtrex online
tadalafil tablets for sale
order metformin on line
weapons dark links – gun dark markets, western union dark markets
overseas online pharmacy
denizli çıkışlı turlar
lisinopril 500 mg
Lessons waiting for you at our Virtuoso School: hip hop dance class Unlock your creative potential at Virtuoso School of Music and Art.
aydın çıkışlı turlar
Приветики!
Было ли у вас когда-нибудь такое, что приходилось писать дипломную работу в сжатые сроки? Это действительно требует огромной ответственности и напряженных усилий, но важно не сдаваться и продолжать активно заниматься учебными процессами, чем я и занимаюсь.
Для тех, кто умеет искать и анализировать информацию в интернете, это действительно помогает в процессе согласования и написания дипломной работы. Не нужно тратить время на посещение библиотек или организацию встреч с дипломным руководителем. Здесь представлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по России. Можете ознакомиться с предложениями по ссылке , проверено!
http://besconeshnocte.flybb.ru/posting.php?mode=post&f=2
купить диплом магистра
купить диплом техникума
купить диплом о среднем образовании
купить диплом института
где купить диплом
Желаю каждому нужных оценок!
azithromycin 750 mg
Доставка алкоголя СПб
generic synthroid canada
ankara diş kliniği
Привет, дорогой читатель!
Бывали ли у вас случаи, когда приходилось писать дипломную работу в крайне сжатые сроки? Это действительно требует большой ответственности и напряженного труда, но важно не унывать и продолжать активно участвовать в учебном процессе, как я и делаю.
Для тех, кто умеет эффективно находить и использовать информацию в интернете, это может существенно облегчить процесс согласования и написания дипломной работы. Больше не нужно тратить время на посещение библиотек или организацию встреч с научным руководителем. Здесь, на этом ресурсе, предоставлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по всей России. Можете ознакомиться с предложениями на , это проверено!
http://adrenalinwod.mybb.ru/viewtopic.php?id=348#p439
купить диплом Гознак
купить диплом в Москве
где купить диплом
купить диплом ссср
купить диплом
Желаю каждому отличных отметок!
best metformin brand in india
synthroid 0.075 mcg
cost of cialis without insurance
5 mg tadalafil coupon
india pharmacy mail order
Здравствуйте!
Вы когда-нибудь писали диплом в сжатые сроки? Это очень ответственно и тяжело, но нужно не сдаваться и делать учебные процессы, чем Я и занимаюсь)
Тем кто умеет разбираться и гуглить информацию, это действительно помогает по ходу согласований и написания диплома, не нужно тратить время на библиотеки или встречи с дипломным руководителем, вот здесь есть хорошие данные для заказа и написания дипломов и курсовых с гарантией и доставкой по России, можете посмотреть здесь , проверено!
http://autogroupe.ru/kupit-svidetelstva-o-dopolnitelnom-obuchenii
купить диплом университета
купить диплом
купить диплом колледжа
купить диплом магистра
купить диплом специалиста
Желаю любому прекрасных оценок!
ankara tercüme bürosu
Мы гарантируем вам низкие цены и отличное качество за счет больших объемов закупок у заводов-изготовителей напрямую купить упаковку в спб
which online pharmacy is reliable
Привет, дорогой читатель!
Было ли у вас когда-нибудь такое, что приходилось писать дипломную работу в сжатые сроки? Это действительно требует огромной ответственности и напряженных усилий, но важно не сдаваться и продолжать активно заниматься учебными процессами, чем я и занимаюсь.
Для тех, кто умеет искать и анализировать информацию в интернете, это действительно помогает в процессе согласования и написания дипломной работы. Не нужно тратить время на посещение библиотек или организацию встреч с дипломным руководителем. Здесь представлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по России. Можете ознакомиться с предложениями по ссылке , проверено!
http://theblazingblink.bestbb.ru/viewtopic.php?id=379#p455
купить диплом магистра
купить диплом нового образца
купить диплом цена
купить диплом
купить диплом в Москве
Желаю каждому положительных отметок!
buying valtrex
Здравствуйте!
Вы когда-нибудь писали диплом в сжатые сроки? Это очень ответственно и тяжело, но нужно не сдаваться и делать учебные процессы, чем Я и занимаюсь)
Тем кто умеет разбираться и гуглить информацию, это действительно помогает по ходу согласований и написания диплома, не нужно тратить время на библиотеки или встречи с дипломным руководителем, вот здесь есть хорошие данные для заказа и написания дипломов и курсовых с гарантией и доставкой по России, можете посмотреть здесь , проверено!
http://alzamai.ixbb.ru/viewtopic.php?id=842#p1437
купить диплом в Москве
купить аттестат
купить диплом ссср
купить диплом Вуза
купить диплом бакалавра
Желаю любому пятерошных) отметок!
synthroid 0.075 mg
valtrex over counter
foreign online pharmacy
Добрый день всем!
Бывало ли у вас такое, что приходилось писать дипломную работу в крайне сжатые сроки? Это действительно требует огромной ответственности и напряженных усилий, но важно не опускать руки и продолжать активно заниматься учебными процессами, как я.
Для тех, кто умеет быстро находить и анализировать информацию в сети, это действительно помогает в процессе согласования и написания дипломной работы. Больше не нужно тратить время на посещение библиотек или устраивать встречи с дипломным руководителем. Здесь, на этом ресурсе, предоставлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по всей России. Можете ознакомиться с предложениями на сайте , это проверено!
https://arhonskforum.rolka.me/viewtopic.php?id=2485#p3297
купить диплом о среднем образовании
купить аттестат
купить диплом
где купить диплом
купить диплом магистра
Желаю любому отличных отметок!
casino table games
top casino usa
buy prednisone online no prescription
Завораживающие возможности онлайн азартных игр простираются в виртуальной реальности, где каждый участник погружается в увлекательное путешествие по миру азарта и волнения http://xn--jj0bt2i8umnxa.com/bbs/board.php?bo_table=free&wr_id=109197
промокод 1хбет 2024 – промокод 1хставка на сегодня на регистрацию, промокод на бесплатную ставку 1хставка
промокод 1xbet на год регистрации – 1xbet скачать приложение на андроид бесплатно, 1xbet промокод на 6500 рублей
Доставка алкоголя СПб
tizanidine mechanism of action
промокоды 1xставка – условия промокода 1хставка, бонус на первый депозит 100 1xbet
Приветики!
Бывало ли у вас такое, что приходилось писать дипломную работу в крайне сжатые сроки? Это действительно требует огромной ответственности и напряженных усилий, но важно не опускать руки и продолжать активно заниматься учебными процессами, как я.
Для тех, кто умеет быстро находить и анализировать информацию в сети, это действительно помогает в процессе согласования и написания дипломной работы. Больше не нужно тратить время на посещение библиотек или устраивать встречи с дипломным руководителем. Здесь, на этом ресурсе, предоставлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по всей России. Можете ознакомиться с предложениями на сайте , это проверено!
http://4asdaiprognoza.listbb.ru/viewtopic.php?f=2&t=476
купить диплом в Москве
купить аттестат
купить диплом колледжа
купить диплом техникума
купить диплом о среднем специальном
Желаю любому прекрасных отметок!
Подробнее здесь [url=https://phoenixtravel.md/hot/]Горящие Туры[/url]
Доставка алкоголя СПб
buy valtrex over the counter
where can i buy prednisone without a prescription
purchase tadalafil
online pharmacy india
Привет всем!
Было ли у вас когда-нибудь так, что приходилось писать дипломную работу в очень сжатые сроки? Это действительно требует огромной ответственности и может быть очень тяжело, но важно не опускать руки и продолжать активно заниматься учебными процессами, как я.
Для тех, кто умеет быстро находить и использовать информацию в интернете, это действительно облегчает процесс согласования и написания дипломной работы. Больше не нужно тратить время на посещение библиотек или устраивать встречи с научным руководителем. Здесь, на этом ресурсе, предоставлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по всей России. Можете ознакомиться с предложениями на сайте , это проверено!
https://elitemagyaritasok.info/e107_plugins/forum/forum_post.php?f=nt&id=21#
купить аттестат
купить диплом техникума
купить диплом
купить диплом специалиста
купить диплом о среднем специальном
Желаю любому положительных отметок!
synthroid 200 mcg
azithromycin 100mg price
Здравствуйте!
Было ли у вас когда-нибудь такое, что приходилось писать дипломную работу в сжатые сроки? Это действительно требует огромной ответственности и напряженных усилий, но важно не сдаваться и продолжать активно заниматься учебными процессами, чем я и занимаюсь.
Для тех, кто умеет искать и анализировать информацию в интернете, это действительно помогает в процессе согласования и написания дипломной работы. Не нужно тратить время на посещение библиотек или организацию встреч с дипломным руководителем. Здесь представлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по России. Можете ознакомиться с предложениями по ссылке , проверено!
http://69.bestbb.ru/viewtopic.php?id=339#p350
купить диплом университета
купить диплом
купить диплом нового образца
купить аттестат
купить диплом института
Желаю любому пятерошных) отметок!
Сфера онлайн гэмблинга стремительно развивается, предлагая увлекательные игры и возможность выигрыша http://gripublicidad.com/index.php?option=com_kunena&view=topic&catid=2&id=20512&Itemid=528
Your article helped me a lot, is there any more related content? Thanks!
перенаправляется сюда Поиск туров
valtrex 500 mg coupon
generic tadalafil uk
synthroid 112 mcg
Приветики!
Было ли у вас опыт написания дипломной работы в крайне сжатые сроки? Это действительно требует огромной ответственности и трудоемкости, однако важно сохранять упорство и продолжать активно участвовать в учебном процессе, как я это делаю.
Для тех, кто умеет эффективно искать и анализировать информацию в интернете, это действительно помогает в процессе согласования и написания дипломной работы. Больше не нужно тратить время на посещение библиотек или организацию встреч с научным руководителем. Здесь, на этом ресурсе, предоставлены надежные данные для заказа и написания дипломных и курсовых работ с гарантией качества и доставкой по всей России. Можете ознакомиться с предложениями по ссылке , это проверенный источник!
https://lolka.bestbb.ru/viewtopic.php?id=618#p3988
купить диплом бакалавра
купить диплом о среднем специальном
купить диплом ссср
купить диплом специалиста
где купить диплом
Желаю всем отличных оценок!
tadalafil 5mg online
tadalafil online price
lisinopril 20 mg online
synthroid 120 mcg
50 mcg synthroid
Доброго всем дня!
купить диплом Вуза
Желаю всем положительных оценок!
http://www.livecenter.ru/index.php?showtopic=737&mode=linear
купить диплом цена
купить диплом о среднем образовании
купить диплом в Москве
valtrex brand name price
tadalafil tablets 20 mg india
buy synthroid canada no prescription
https://notperfect.ru/radiotehnika/vstraivaemyj-holodilnik-reshenie-dlja-sovremennoj-kuhni.html
tadalafil 2.5 mg price india
online casinos usa
casino usa online
how to buy lisinopril online
Вы можете заказать у нас услуги грузчиков в Москве и Московской области для любых работ, начиная с обычных погрузо-разгрузочных и заканчивая всеми видами переездов и такелажных работ Персонал на конвеер
cheapest pharmacy to fill prescriptions with insurance
+ for the post
_________________
авиатор программа взлом
otc glucophage
https://moslabor.ru
metformin 500 mg india
can i buy synthroid from canada
Здравствуйте!
купить аттестат
Желаю всем пятерошных) отметок!
http://ftp.video-foto.by/forum/viewtopic.php?f=82&t=27596
купить аттестат школы
купить диплом о среднем специальном
купить диплом Вуза
rate canadian pharmacies
synthroid prices
buy metformin online nz
Доставка алкоголя
Здравствуйте!
купить диплом специалиста
Желаю всем отличных отметок!
https://library.pilxt.com/index.php?action=profile;u=52454
купить диплом магистра
купить диплом
где купить диплом
I got this site from my pal who told me on the topic of this site and at the moment this time I am visiting this web page and reading very informative articles at this place.
#be#jk3#jk#jk#JK##
купить американский номер для смс
prednisone for cheap
rx lisinopril 10mg
onlinepharmaciescanada com
where can i buy over the counter tadalafil 20mg
0.05 mg synthroid
synthroid average cost
Привет, дорогой читатель!
купить диплом цена
Желаю всем прекрасных отметок!
http://molbiol.ru/forums/index.php?showtopic=1101388
купить диплом ссср
купить диплом о среднем образовании
купить диплом
can i buy azithromycin in mexico
prinivil lisinopril
Привет, дорогой читатель!
купить диплом о высшем образовании
Желаю каждому нужных отметок!
http://СЂСѓСЃР±РёР».СЂС„/forum/viewtopic.php?t=2315&view=next
купить диплом цена
купить диплом
купить диплом Гознак
cheapest pharmacy to fill prescriptions with insurance
best metformin brand
online pharmacy uk
best tadalafil tablets in india
сервопривод оптимус драйв – датчик давления овен, преобразователи частоты innovert серии itd
no prescription needed canadian pharmacy
happy family canadian pharmacy
Торговля на Kraken. Завершив регистрацию на официальной сайте Кракен, пройдя минимум первые две ступени верификации (0-я и 1-я), а также внеся средства на депозит, можно заниматься зарабатыванием на разнице ценовых курсов либо при надобности обменивать криптовалюту в требуемых направлениях Kraken зеркало
продам дебетовые карты – Anna Business, связки киви киви кошелек
tadalafil online without prescription
ozempic +в наличии купить – трулисити +в москве, купить укол аземпик
виза карта сбербанка – европол, Exmo.me
buy prinivil online
подарок +на новый год подростку девочке 14 – печать +на футболках мультифото, аниме подарки +на новый год
canada pharmacy not requiring prescription
drug synthroid
Super Shop! Delivery 6 -11days. Stores in the USA and all over the world. Delivery guarantee. Refund for any issues. Free standard shipping on all orders. Free returns Within 90 days. Best Sellers. 5-Star Rated. Spring Offers. New Arrivals
can you buy azithromycin over the counter in canada
buy synthroid 75 mcg
synthroid 25 mcg coupon
mexican pharmacy weight loss
save on pharmacy
Источник
нажмите здесь
Подробнее
azithromycin for sale usa
synthroid 25 pill
Долгие годы мы производим сувениры, подарки и рекламную продукция как для больших корпораций, так и для среднего и малого бизнеса корпоративный мерч что это
generic lisinopril online
synthroid 25 mcg tablet
https://avto-dublikat.ru/
Читайте последние новости на тему в ленте новостей на сайте Newsman Получайте уведомления о свежих новостях в своем браузере.
tops pharmacy
удалить данные из интернета – ддос услуги, взлом сайта
ddos сервис – ддос сервис, удалить информацию из интернета
online pharmacy no prescription
metformin 1g
check atomic wallet
read the full info here solana wallet
viagra online canadian pharmacy
super saver pharmacy
cialis 5mg daily cost
valtrex capsules
online pharmacy discount code 2018
silkroad online pharmacy
buy generic tadalafil online cheap
synthroid armour
Your article helped me a lot, is there any more related content? Thanks!
cost of valtrex tablets
synthroid brand name price
casino
casino games
Бонус приветствия в Betwinner предоставляет игрокам возможность получить дополнительные средства на свой игровой счет. Этот бонус составляет 100% от суммы первого депозита, который игрок вносит на свой счет. Например, если новый клиент пополнил свой счет на 10 евро, то ему будет начислено еще 10 евро в качестве бонуса.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
valtrex brand name
векторный частотный преобразователь c2000 – регистратор температуры термодат, поставки кипиа и асу тп
canadian pharmacy ed medications
Do you like crash games? Play now the online casino crash game Maverick in bwin Zambia website https://baccaratinzambia69258.digiblogbox.com/52116895/roulette-in-zambia-an-overview
how much is a cialis pill
valtrex script online
affordable pharmacy
usa pharmacy online
кракен зеркало тор – актуальное зеркало kraken, kraken официальный сайт ссылка
azithromycin 500 dosage online pharmacy
мунжаро купить спб – мунджаро отзывы, лираглутид инструкция цена отзывы аналоги
Срочная финансовая помощь – Займ у инвестора, Частный займ
azithromycin 250 mg tablet price in india
Бонус приветствия в Betwinner предоставляет игрокам возможность получить дополнительные средства на свой игровой счет. Этот бонус составляет 100% от суммы первого депозита, который игрок вносит на свой счет. Например, если новый клиент пополнил свой счет на 10 евро, то ему будет начислено еще 10 евро в качестве бонуса.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
online pharmacy without scripts
Бонус приветствия в Betwinner предоставляет игрокам возможность получить дополнительные средства на свой игровой счет. Этот бонус составляет 100% от суммы первого депозита, который игрок вносит на свой счет. Например, если новый клиент пополнил свой счет на 10 евро, то ему будет начислено еще 10 евро в качестве бонуса.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
usa pharmacy
valtrex lowest price
Телесериал «Однажды в сказке» вышел на экраны 23 октября 2011 года, и сразу же завоевал свою аудиторию зрителей, которая не спадает до сих пор. Сериал состоит из 7 сезонов и 156 эпизодов. В этой одной кинокартине собраны практически все сказочные персонажи, с разных сказок Тут
Бонус приветствия в Betwinner предоставляет игрокам возможность получить дополнительные средства на свой игровой счет. Этот бонус составляет 100% от суммы первого депозита, который игрок вносит на свой счет. Например, если новый клиент пополнил свой счет на 10 евро, то ему будет начислено еще 10 евро в качестве бонуса.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
Телесериал «Однажды в сказке» вышел на экраны 23 октября 2011 года, и сразу же завоевал свою аудиторию зрителей, которая не спадает до сих пор. Сериал состоит из 7 сезонов и 156 эпизодов. В этой одной кинокартине собраны практически все сказочные персонажи, с разных сказок Подробнее
valtrex brand
pharmacy store
valtrex 100 mg
sublingual cialis
metformin tab price
medication zestoretic
drug metformin
prednisone 20 mg pill
levothyroxine 50 mcg
Приложение для знакомств, которое призвано подобрать вам пару с использованием сложных алгоритмов и искусственного интеллекта. Как и в большинстве подобных сервисов, вам нужно создать анкету, но затем начинается самое интересное ЛУЧШИЙ САЙТ ЗНАКОМСТВ
online pharmacy delivery
valtrex discount
efeler halı koltuk Yıkamacı
Доставка алкоголя
valtrex no prescription
legal online pharmacy
go bitcoin tumbler
glucophage otc
Однако, существует возможность увеличить размер этого бонуса с помощью промокода betwinner. При использовании этого кода при регистрации, приветственный бонус увеличится на 30%. То есть, если игрок пополнил свой счет на 10 евро и использовал промокод, то его бонус составит уже 13 евро.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
Заглянув в мир онлайн-развлечений, каждый находит что-то по своему вкусу:будь то классические слоты, азартные столы с карточными играми или вращающиеся рулетки https://civilpatrol.info/?q=petition/80462/igrovye-turniry-na-1win-shans-vyigrat-krupnyy-priz
super saver pharmacy
mounjaro отзывы – семаглутид применение цена, оземпик пропал
Заглянув в мир онлайн-развлечений, каждый находит что-то по своему вкусу:будь то классические слоты, азартные столы с карточными играми или вращающиеся рулетки http://www.mp-associes.com/en/index.php/blog/%D0%90%D1%81%D1%80%D0%B5%D1%82.html
valtrex 500 india
лираглутид аналоги – дулаглутид семаглутид, оземпик купить цена +в аптеках
hop over to this website xrp wallet
aimbot fortnite download pc – free softaim fortnite, how to get hacks on fortnite
zestril 10 mg price
generic for synthroid
lisinopril 2
azithromycin 1000mg
lisinopril 20mg tablets
cheap tadalafil 40 mg
synthroid 0.05 mcg
how to get valtrex without a prescription
Hello I am so happy I found your webpage, I really found you by accident, while I was browsing on Aol for something else, Regardless I am here now and would just like to say cheers for a remarkable post and a all round entertaining blog (I also love the theme/design), I don’t have time to go through it all at the moment but I have bookmarked it and also added your RSS feeds, so when I have time I will be back to read more, Please do keep up the great job.
респиратор алина
Однако, существует возможность увеличить размер этого бонуса с помощью промокода betwinner. При использовании этого кода при регистрации, приветственный бонус увеличится на 30%. То есть, если игрок пополнил свой счет на 10 евро и использовал промокод, то его бонус составит уже 13 евро.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
buying tadalafil in singapore
indianpharmacy com https://indiaph24.store/# cheapest online pharmacy india
Online medicine order
azithromycin for sale australia
medication from mexico pharmacy: cheapest mexico drugs – mexican drugstore online
Однако, существует возможность увеличить размер этого бонуса с помощью промокода betwinner. При использовании этого кода при регистрации, приветственный бонус увеличится на 30%. То есть, если игрок пополнил свой счет на 10 евро и использовал промокод, то его бонус составит уже 13 евро.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
sure save pharmacy
glucophage coupon
prednisone 40
kraken darknet market зеркало – kraken darknet ссылка тор, kraken зеркало рабочее
onlinepharmaciescanada com
2.5 mg daily tadalafil
lisinopril 10 mg tablet
Because the admin of this web site is working, no doubt very quickly it will be well-known, due to its feature contents.
reddit stake casino
buying metformin er
Look At This Cheapest SMM Reseller Panel
where can i buy metformin in south africa
https://t.me/escort_rabotar
веб-сайт
РЕМОНТ И СЕРВИСНОЕ ОБСЛУЖИВАНИЕ КОНДИЦИОНЕРА В ОРШЕ
rx pharmacy online
Seo to top Прогон по базам GSA
indian trail pharmacy
synthroid 0.05
Betwinner Промокод: 937999 – воспользуйтесь этим уникальным кодом, чтобы получить бонус в размере 100% до 25 000 рублей. На официальном сайте букмекерской конторы Betwinner вы сможете найти огромное количество событий, включая спортивные ставки, онлайн-казино, политические ставки и мгновенные игры.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
buying zithromax
prednisone 5442
the canadian pharmacy
synthroid 225 online
lisinopril 30
valtrax on line
legitimate online pharmacy usa
zestril generic
Бонус приветствия в Betwinner предоставляет игрокам возможность получить дополнительные средства на свой игровой счет. Этот бонус составляет 100% от суммы первого депозита, который игрок вносит на свой счет. Например, если новый клиент пополнил свой счет на 10 евро, то ему будет начислено еще 10 евро в качестве бонуса.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
online pharmacy delivery
психолог телефон https://w-495.ru/
happy family rx
Однако, существует возможность увеличить размер этого бонуса с помощью промокода betwinner. При использовании этого кода при регистрации, приветственный бонус увеличится на 30%. То есть, если игрок пополнил свой счет на 10 евро и использовал промокод, то его бонус составит уже 13 евро.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
synthroid without prescription
best rogue online pharmacy
buy valtrex online cheap
tadalafil purchase
В связи с этим представители букмекерской компании 1win создают зеркальные сайты, чтобы обойти эту блокировку. Что позволяет пользоваться функционалом официального сайта: заключать пари, выводить средства и т.д. Зеркалами пользуются 1xbet и 1Win – не исключение 1win сайт
order prednisone
Промокод BetWinner- 937999. Новые пользователи букмекерской компании Betwinner могут воспользоваться приветственным бонусом в размере 100% от суммы депозита до €100 (или эквивалентной суммы в другой валюте). Фрибеты в БетВиннер чаще появляются в рамках периодических акций. Иногда такая привилегия касается новых игроков, но чаще всего поощрение получают постоянные.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
В связи с этим представители букмекерской компании 1win создают зеркальные сайты, чтобы обойти эту блокировку. Что позволяет пользоваться функционалом официального сайта: заключать пари, выводить средства и т.д. Зеркалами пользуются 1xbet и 1Win – не исключение 1win
this article roblox executor
check these guys out roblox executor
Do you have a spam problem on this site; I also am a blogger, and I was wanting to know your situation; many of us have developed some nice practices and we are looking to exchange methods with others, please shoot me an e-mail if interested.
мои куклы интернет магазин
О, этот сайт! Бесконечная череда страниц, наполненных буквами, словами и фразами, вроде как объединенных общей темой Отзывы
In Etsy, Shopify Pinterest+SEO + artificial intelligence give high sales results
Магазин спортивной фармакологии – OxyShop. Это всемирно известный надёжный поставщик качественных препаратов для спортсменов фарма рост
This post is invaluable. Where can I find out more?
pin-up casino aviator prediction
Магазин спортивной фармакологии – OxyShop. Это всемирно известный надёжный поставщик качественных препаратов для спортсменов курс стероидов и гормон роста
lisinopril 30 mg tablet
lisinopril 20mg tablets cost
Hey there I am so grateful I found your web site, I really found you by accident, while I was browsing on Bing for something else, Nonetheless I am here now and would just like to say thanks a lot for a tremendous post and a all round thrilling blog (I also love the theme/design), I don’t have time to look over it all at the moment but I have book-marked it and also added in your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the superb b.
официальный сайт вован казино
online pharmacy delivery usa
synthroid 188 mcg
buy synthroid 112 mcg
try here Rufus
сайт кракен онион – kraken darknet market зеркало, площадка кракен ссылка
Промокод 1xbet на сегодня. Промокод на 2024-2024. На официальном сайте букмекерской конторы 1xbet появилась опция, которая позволяет “бесплатно” ознакомиться с функционалом сайта и при удачном стечении обстоятельств еще и выиграть некую сумму денежных средств. Теперь это стало доступно по специальному промокоду 1хБет. Он дает возможность получить до 32500? (100$). Актуальные промокоды 1xbet на сегодня: 1XFREE777. Рабочие промокоды 1XBet в 2024 Все промокоды для 1хбет бесплатно: при регистрации, на ставку (купон), на бонус, на сегодня. 1xBet — одна из самых известных компаний в сфере беттинга. Свою популярность контора заработала во многом благодаря большому количеству специальных предложений. Так, к примеру, каждый пользователь может воспользоваться одним из действующих промокодов 1xBet на сегодня бесплатно. Ознакомиться с их полным перечнем можно в данной статье – более подробно в этом материале http://norma-migracia.ru/news/besplatnuy_127.html
В нашем мире, где диплом становится началом удачной карьеры в любом направлении, многие ищут максимально быстрый путь получения качественного образования. Наличие документа об образовании трудно переоценить. Ведь диплом открывает дверь перед всеми, кто желает начать трудовую деятельность или продолжить обучение в любом университете.
В данном контексте мы предлагаем очень быстро получить этот важный документ. Вы можете заказать диплом, и это будет выгодным решением для человека, который не смог закончить обучение или потерял документ. диплом изготавливается с особой аккуратностью, вниманием к мельчайшим элементам, чтобы в итоге получился полностью оригинальный документ.
Преимущества этого решения заключаются не только в том, что вы сможете быстро получить диплом. Процесс организовывается просто и легко, с профессиональной поддержкой. Начиная от выбора нужного образца до консультаций по заполнению персональной информации и доставки по стране — все будет находиться под абсолютным контролем опытных специалистов.
Таким образом, для всех, кто ищет максимально быстрый способ получения необходимого документа, наша компания предлагает отличное решение. Приобрести диплом – это значит избежать длительного обучения и сразу перейти к достижению своих целей: к поступлению в ВУЗ или к началу успешной карьеры.
https://diplomanc-russia24.com
best canadian pharmacy
Delivery 6 -11 business days. Stores in the USA and all over the world. Delivery guarantee. Refund for any issues. Free standard shipping on all orders. Free returns Within 90 days. Best Sellers. 5-Star Rated. Spring Offers. New Arrivals
GTA 6 дата выхода – GTA 6 на ПК, игры на PS5 или Xbox Series X/S.
Промокод БетВиннер: 937999 при регистрации в 2024 году с использованием на сайте BetWinner.com вы получите бесплатный бонус в размере 100% до 25000 рублей на вашу ставку. Все актуальные бонусы от букмекерской конторы BetWinner можно найти на одной странице. Там вы также найдете инструкции по получению фрибетов, участию в акциях и бездепозитному бонусу от БК BetWinner в 2024 году.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
cialis canada online pharmacy
Если сумма выигрыша превышает 5 млн рублей, 1Win имеет право установить индивидуальный лимит на вывод в сутки. Мобильная версия и приложения. Для юзеров, предпочитающих мобильные гаджеты, у «1Вин» есть мобильная версия и приложения на iOS и Android один вин
кандидатская диссертация – напишу диссертацию, требования к написанию курсовой работы
Если сумма выигрыша превышает 5 млн рублей, 1Win имеет право установить индивидуальный лимит на вывод в сутки. Мобильная версия и приложения. Для юзеров, предпочитающих мобильные гаджеты, у «1Вин» есть мобильная версия и приложения на iOS и Android один вин
Appreciating the hard work you put into your website and in depth information you provide. It’s good to come across a blog every once in a while that isn’t the same unwanted rehashed information. Excellent read! I’ve saved your site and I’m including your RSS feeds to my Google account.
canada bitcoin casinos
where can i get cialis without a prescription
top live casino
top casino
pharmacy store
tadalafil mexico
заказать курсовую харьков – напишу диссертацию, курсовая работа заказать украина
Данная услуга позволяет в кратчайшие сроки и без необходимости организации транспортировки больного поставить точный диагноз и своевременно приступить к лечению рентген позвоночника на дому
CS 2 скачать бесплатно торрент – игры на PS5 или Xbox Series X/S., Counter Strike 2 скачать бесплатно
Данная услуга позволяет в кратчайшие сроки и без необходимости организации транспортировки больного поставить точный диагноз и своевременно приступить к лечению рентген на дому Санкт-Петербург
купить удаленный сервер – vds сервер купить, hosting vds
see page galaxy swapper download
Да, в приложении 1win существуют ограничения на вывод средств. Максимальная сумма вывода за транзакцию составляет 10 000 долларов, а ежедневный лимит вывода средств составляет 100 000 долларов 1win зеркало
The Best Attractions in Morocco – Top Places to Visit in Czech Republic, Best Restaurants in Cyprus
Да, в приложении 1win существуют ограничения на вывод средств. Максимальная сумма вывода за транзакцию составляет 10 000 долларов, а ежедневный лимит вывода средств составляет 100 000 долларов ванвин
вафли OREO оптом – энергетики Ред Булл оптом, газированные напитки Aziano оптом
В нашем мире, где диплом – это начало удачной карьеры в любом направлении, многие ищут максимально простой путь получения качественного образования. Наличие официального документа об образовании переоценить попросту невозможно. Ведь именно он открывает двери перед всеми, кто стремится начать профессиональную деятельность или учиться в высшем учебном заведении.
В данном контексте наша компания предлагает максимально быстро получить этот необходимый документ. Вы сможете купить диплом старого или нового образца, и это будет удачным решением для всех, кто не смог закончить обучение или утратил документ. Все дипломы производятся аккуратно, с особым вниманием ко всем элементам, чтобы на выходе получился 100% оригинальный документ.
Превосходство такого решения заключается не только в том, что можно оперативно получить свой диплом. Процесс организован удобно, с нашей поддержкой. Начав от выбора необходимого образца до консультаций по заполнению личной информации и доставки по стране — все находится под полным контролем опытных мастеров.
Всем, кто хочет найти быстрый способ получить необходимый документ, наша компания предлагает отличное решение. Заказать диплом – значит избежать длительного процесса обучения и не теряя времени перейти к своим целям, будь то поступление в ВУЗ или начало удачной карьеры.
https://diploman-russiyans.com
можно проверить ЗДЕСЬ Поиск туров
Hello everyone, it’s my first pay a quick visit at this site, and post is genuinely fruitful in support of me, keep up posting such posts.
https://loveru.me/sajt-znakomstv-novokubanka/
cost of generic tadalafil
онлайн казино кэт
cat казино играть
кракен сайт зеркало рабочее – кракен даркнет площадка, рабочая ссылка на кракен
valtrex price in india
kraken darknet ссылка тор – kraken tor, kraken darknet market зеркало
рабочая ссылка на кракен – адрес сайта кракен, кракен рабочий сайт
маркетплейс блэкспрут – блекспрут зеркала, blacksprut ссылка
Промокод 1xBet на сегодня и бесплатно. Промокоды 1хбет 2024 требуется использовать те, которые предоставят игрокам самые лучшие бонусы. Каждый из них позволяет увеличить первый депозит в 2 раза, максимальная сумма увеличения – 100 долларов. Большое количество промокодов — одна из причин того, что на сайте регистрируется огромное количество новых игроков каждый день. На данный момент их количество превышает пятьсот тысяч уникальных пользователей каждый день. Действующие промокоды позволяют увеличить размер приветственных баллов до 32 500 рублей. Для этого нужно лишь активировать при регистрации имеющийся код, скопировав его в соответствующее поле. Букмекерская контора 1ХБет является одной из самых влиятельных на рынке игорного бизнеса в России и не нуждается в особом представлении. Впрочем, букмекер продолжает держать статус одного из самых щедрых и предлагает своим клиентам воспользоваться промокодами для халявы, – более подробно в этом материале http://nncleaning.ru/pags/?onlayn_seks_video_chat_ruletka_besplatno.html.
tadalafil buy canada
where can i buy cialis online in canada
metformin 3000 mg
win — букмекерская контора 1вин. Нынешняя вариация сайтов для ставок и игры на реальные деньги поражает. Для российских игроков открыты десятки ресурсов ванвин
win — букмекерская контора 1вин. Нынешняя вариация сайтов для ставок и игры на реальные деньги поражает. Для российских игроков открыты десятки ресурсов 1win
order synthroid
zofran and heart problems
В современном мире, где диплом является началом удачной карьеры в любом направлении, многие пытаются найти максимально простой путь получения качественного образования. Наличие официального документа трудно переоценить. Ведь именно он открывает двери перед любым человеком, который желает начать профессиональную деятельность или продолжить обучение в университете.
В данном контексте наша компания предлагает очень быстро получить любой необходимый документ. Вы сможете купить диплом, и это будет выгодным решением для всех, кто не смог завершить обучение, утратил документ или хочет исправить плохие оценки. Все дипломы изготавливаются аккуратно, с максимальным вниманием к мельчайшим нюансам, чтобы на выходе получился 100% оригинальный документ.
Превосходство подобного подхода заключается не только в том, что вы оперативно получите свой диплом. Весь процесс организовывается удобно, с профессиональной поддержкой. От выбора требуемого образца до правильного заполнения персональных данных и доставки по России — все будет находиться под абсолютным контролем опытных специалистов.
Таким образом, для всех, кто пытается найти оперативный способ получить требуемый документ, наша компания может предложить отличное решение. Заказать диплом – значит избежать продолжительного обучения и сразу переходить к личным целям, будь то поступление в университет или старт успешной карьеры.
https://diploman-rossiya.com
Промокод 1xBet на сегодня и бесплатно. Промокоды 1хбет 2024 требуется использовать те, которые предоставят игрокам самые лучшие бонусы. Каждый из них позволяет увеличить первый депозит в 2 раза, максимальная сумма увеличения – 100 долларов. Большое количество промокодов — одна из причин того, что на сайте регистрируется огромное количество новых игроков каждый день. На данный момент их количество превышает пятьсот тысяч уникальных пользователей каждый день. Действующие промокоды позволяют увеличить размер приветственных баллов до 32 500 рублей. Для этого нужно лишь активировать при регистрации имеющийся код, скопировав его в соответствующее поле. Букмекерская контора 1ХБет является одной из самых влиятельных на рынке игорного бизнеса в России и не нуждается в особом представлении. Впрочем, букмекер продолжает держать статус одного из самых щедрых и предлагает своим клиентам воспользоваться промокодами для халявы, – более подробно в этом материале https://www.naskaplaza.ru/bin/news/1xbet.html.
Сдача автомобиля на разборку – это процесс, который может потребоваться в случае серьезных поломок или старения транспортного средства https://medium.com/@kalinka0588/%D0%B1%D0%BE%D1%80%D0%BE%D1%82%D1%8C%D0%B1%D0%B0-%D0%B7-%D0%B3%D1%80%D0%B8%D0%BF%D0%BE%D0%BC-%D0%B2%D1%81%D0%B5-%D0%BF%D1%80%D0%BE-%D1%81%D0%B8%D0%BC%D0%BF%D1%82%D0%BE%D0%BC%D0%B8-%D1%82%D0%B0-%D0%BB%D1%96%D0%BA%D1%83%D0%B2%D0%B0%D0%BD%D0%BD%D1%8F-d2a531d6ab33
Сдача автомобиля на разборку – это процесс, который может потребоваться в случае серьезных поломок или старения транспортного средства https://thirdparty.yeelight.com/topics/5453/sovety-po-fotografii-dlya-nachinayushchikh
how to get cialis pills
Рубероид РКК – это высококачественный материал, отвечающий всем требованиям госта. Он имеет высокую прочность, вес и габариты, а также теплостойкость до 80 градусов Рубероид РКК 350 ГОСТ
В нашем мире, где диплом становится началом удачной карьеры в любом направлении, многие пытаются найти максимально быстрый и простой путь получения качественного образования. Необходимость наличия официального документа сложно переоценить. Ведь именно диплом открывает двери перед любым человеком, который собирается вступить в профессиональное сообщество или продолжить обучение в университете.
Наша компания предлагает максимально быстро получить этот необходимый документ. Вы сможете приобрести диплом старого или нового образца, и это становится выгодным решением для человека, который не смог завершить образование или потерял документ. Все дипломы выпускаются аккуратно, с особым вниманием ко всем элементам. В итоге вы получите полностью оригинальный документ.
Преимущество подобного решения заключается не только в том, что можно оперативно получить свой диплом. Процесс организован удобно и легко, с профессиональной поддержкой. От выбора подходящего образца до консультации по заполнению персональной информации и доставки по стране — все будет находиться под абсолютным контролем наших мастеров.
Всем, кто хочет найти быстрый способ получить необходимый документ, наша компания предлагает выгодное решение. Приобрести диплом – это значит избежать долгого обучения и сразу перейти к своим целям: к поступлению в университет или к началу удачной карьеры.
https://diploman-russiyan.com
Рубероид РКК – это высококачественный материал, отвечающий всем требованиям госта. Он имеет высокую прочность, вес и габариты, а также теплостойкость до 80 градусов Гидроизол ХПП 2,5
rx pharmacy online 24
generic metformin rx online
where can i buy cialis without a prescription
прицел для оружия – купить мавик, купить квадрокоптер мавик 3
best site bitcoin halving
Website tronlink wallet extension
buy tadalafil online usa
synthroid 0.0125
В нашем обществе, где диплом – это начало успешной карьеры в любом направлении, многие пытаются найти максимально быстрый и простой путь получения образования. Необходимость наличия документа об образовании переоценить просто невозможно. Ведь именно диплом открывает двери перед людьми, желающими вступить в сообщество профессионалов или учиться в ВУЗе.
В данном контексте мы предлагаем оперативно получить этот важный документ. Вы можете приобрести диплом старого или нового образца, что становится отличным решением для всех, кто не смог закончить обучение или утратил документ. Все дипломы выпускаются с особой аккуратностью, вниманием ко всем деталям, чтобы в итоге получился полностью оригинальный документ.
Преимущество данного подхода состоит не только в том, что можно оперативно получить свой диплом. Процесс организован удобно и легко, с профессиональной поддержкой. Начав от выбора нужного образца документа до правильного заполнения персональных данных и доставки в любое место страны — все под абсолютным контролем квалифицированных мастеров.
Всем, кто ищет быстрый способ получения требуемого документа, наша компания предлагает выгодное решение. Купить диплом – значит избежать длительного обучения и не теряя времени переходить к своим целям: к поступлению в университет или к началу успешной карьеры.
https://dlplomanrussian.com
нажмите https://battlepass.ru
Hiya very nice site!! Guy .. Excellent .. Wonderful .. I’ll bookmark your blog and take the feeds additionally? I’m satisfied to seek out a lot of useful info right here within the submit, we’d like develop extra strategies on this regard, thank you for sharing. . . . . .
https://englishmax.ru/
blacksprut com ссылка – blacksprut onion, blacksprut
visit the website Stable income
мега – mega как зайти, mega купить
valtrex 1000 mg
lisinopril 20 mg brand name
В современном мире, где диплом становится началом удачной карьеры в любом направлении, многие пытаются найти максимально быстрый путь получения качественного образования. Необходимость наличия документа об образовании трудно переоценить. Ведь диплом открывает дверь перед любым человеком, который собирается вступить в сообщество профессионалов или продолжить обучение в ВУЗе.
В данном контексте наша компания предлагает максимально быстро получить этот необходимый документ. Вы можете заказать диплом старого или нового образца, что будет отличным решением для человека, который не смог закончить обучение или потерял документ. Любой диплом изготавливается с особой аккуратностью, вниманием ко всем элементам, чтобы на выходе получился 100% оригинальный документ.
Преимущество данного подхода состоит не только в том, что можно оперативно получить свой диплом. Процесс организован удобно, с нашей поддержкой. От выбора необходимого образца до точного заполнения личной информации и доставки по стране — все будет находиться под абсолютным контролем наших мастеров.
Таким образом, для всех, кто пытается найти максимально быстрый способ получения необходимого документа, наша компания предлагает отличное решение. Купить диплом – это значит избежать длительного процесса обучения и не теряя времени переходить к важным целям: к поступлению в ВУЗ или к началу успешной карьеры.
https://diploman-russiyan.com
where to buy tadalafil online
azithromycin generic brand
online pharmacy dubai
В нашем мире, где диплом является началом отличной карьеры в любом направлении, многие стараются найти максимально простой путь получения образования. Наличие документа об образовании переоценить попросту невозможно. Ведь именно он открывает двери перед каждым человеком, который собирается вступить в профессиональное сообщество или учиться в каком-либо институте.
В данном контексте наша компания предлагает быстро получить этот важный документ. Вы можете заказать диплом, и это становится отличным решением для человека, который не смог закончить обучение или потерял документ. Все дипломы изготавливаются с особой аккуратностью, вниманием к мельчайшим нюансам. В результате вы сможете получить полностью оригинальный документ.
Плюсы подобного решения состоят не только в том, что вы быстро получите диплом. Весь процесс организован просто и легко, с нашей поддержкой. Начиная от выбора нужного образца диплома до консультаций по заполнению персональных данных и доставки по стране — все под абсолютным контролем качественных мастеров.
Таким образом, всем, кто ищет быстрый способ получения требуемого документа, наша услуга предлагает отличное решение. Приобрести диплом – это значит избежать длительного процесса обучения и сразу перейти к достижению своих целей: к поступлению в университет или к началу удачной карьеры.
https://diploman-russiyan.com
cheapest pharmacy to fill prescriptions without insurance
Профили для облицовки стен являются неотъемлемой частью современного ремонта и помогают преобразить любое помещение https://profplint.ru/
Профили для облицовки стен являются неотъемлемой частью современного ремонта и помогают преобразить любое помещение алюминиевый плинтус
Сегодня, когда диплом становится началом удачной карьеры в любой отрасли, многие пытаются найти максимально быстрый и простой путь получения образования. Наличие официального документа об образовании переоценить невозможно. Ведь диплом открывает двери перед каждым человеком, желающим вступить в сообщество профессиональных специалистов или учиться в университете.
В данном контексте мы предлагаем оперативно получить этот необходимый документ. Вы имеете возможность купить диплом старого или нового образца, и это становится выгодным решением для человека, который не смог закончить обучение или утратил документ. Любой диплом изготавливается аккуратно, с особым вниманием ко всем нюансам. На выходе вы сможете получить продукт, 100% соответствующий оригиналу.
Преимущество данного подхода состоит не только в том, что можно оперативно получить свой диплом. Процесс организован комфортно, с нашей поддержкой. Начав от выбора требуемого образца документа до консультации по заполнению личной информации и доставки по России — все под абсолютным контролем наших специалистов.
В результате, для всех, кто ищет быстрый и простой способ получить требуемый документ, наша компания предлагает отличное решение. Купить диплом – значит избежать длительного процесса обучения и сразу переходить к важным целям: к поступлению в ВУЗ или к началу удачной карьеры.
https://diploman-rossiya.com
read the full info here bitcoin cleaner
кракен kraken tor site – площадка кракен, зеркало kraken market
check that Buy Instagram Followers
synthroid 100 mcg tablet
brand cialis 100mg
Перед тем как приступить к поиску идеального транспортного средства, важно определить ваши потребности и предпочтения. Обдумайте, для каких целей вам необходимо автомобиль или другое транспортное средство, какие характеристики будут наиболее приоритетными для вас, и какой бюджет вы готовы выделить на покупку http://rtpsouth.com/UserProfile/tabid/69/userId/104891/Default.aspx
This Site toast crypto wallet
Перед тем как приступить к поиску идеального транспортного средства, важно определить ваши потребности и предпочтения. Обдумайте, для каких целей вам необходимо автомобиль или другое транспортное средство, какие характеристики будут наиболее приоритетными для вас, и какой бюджет вы готовы выделить на покупку http://zabygrom.com/blog/hill.html
саксенда купить дешево – оземпик препарат инструкция +по применению цена отзывы, мунджаро фото
buy tadalafil online without a prescription
В нашем обществе, где диплом – это начало удачной карьеры в любой сфере, многие ищут максимально быстрый путь получения образования. Наличие документа об образовании трудно переоценить. Ведь именно он открывает дверь перед каждым человеком, который собирается вступить в сообщество профессионалов или продолжить обучение в любом ВУЗе.
Наша компания предлагает максимально быстро получить любой необходимый документ. Вы сможете купить диплом старого или нового образца, что является выгодным решением для человека, который не смог закончить обучение, потерял документ или хочет исправить плохие оценки. диплом изготавливается аккуратно, с максимальным вниманием к мельчайшим нюансам. На выходе вы получите 100% оригинальный документ.
Преимущество данного решения заключается не только в том, что можно оперативно получить диплом. Процесс организован комфортно, с нашей поддержкой. Начиная от выбора требуемого образца документа до грамотного заполнения личных данных и доставки в любое место страны — все под абсолютным контролем опытных специалистов.
Всем, кто хочет найти максимально быстрый способ получить требуемый документ, наша услуга предлагает отличное решение. Заказать диплом – значит избежать продолжительного обучения и не теряя времени переходить к достижению личных целей: к поступлению в ВУЗ или к началу успешной карьеры.
https://diplomanc-russia24.com
30 mg tadalafil
In Etsy, Amazon, eBay, Shopify https://pint77.com Pinterest+SEO +II = high sales results
оземпик раствор +для инъекций – семаглутид 0.5, семаглутид 14 мг купить
семаглутид таблетки инструкция – саксенда купить недорого, трулисити инструкция 1.5 цена
мунжаро цена – трулисити спб, мунжаро инструкция
оземпик беларусь – оземпик препарат инструкция +по применению цена отзывы, трулисити отзывы аналоги
Сегодня, когда диплом – это начало отличной карьеры в любом направлении, многие стараются найти максимально быстрый и простой путь получения качественного образования. Наличие официального документа об образовании трудно переоценить. Ведь именно он открывает двери перед каждым человеком, который стремится вступить в профессиональное сообщество или продолжить обучение в ВУЗе.
В данном контексте наша компания предлагает очень быстро получить любой необходимый документ. Вы имеете возможность приобрести диплом, и это будет отличным решением для человека, который не смог завершить обучение, потерял документ или хочет исправить плохие оценки. диплом изготавливается с особой тщательностью, вниманием к мельчайшим деталям. На выходе вы получите 100% оригинальный документ.
Превосходство этого подхода состоит не только в том, что можно быстро получить диплом. Весь процесс организовывается комфортно, с нашей поддержкой. От выбора подходящего образца документа до консультации по заполнению личной информации и доставки по стране — все под абсолютным контролем квалифицированных мастеров.
В итоге, всем, кто пытается найти быстрый способ получения необходимого документа, наша компания предлагает выгодное решение. Заказать диплом – это значит избежать длительного процесса обучения и не теряя времени перейти к достижению собственных целей: к поступлению в ВУЗ или к началу удачной карьеры.
https://diplomanc-russia24.com
оземпик эффект – ozempic инструкция +на русском, ozempic +для похудения
valtrex singapore
my canadian pharmacy rx
canadian pharmacy 1 internet online drugstore
zestril no prescription
75 mcg synthroid cheap
synthroid 115 mcg
buy prednisone 10mg
На сегодняшний день, когда диплом – это начало отличной карьеры в любой отрасли, многие стараются найти максимально быстрый путь получения образования. Факт наличия документа об образовании переоценить невозможно. Ведь именно диплом открывает двери перед каждым человеком, который хочет вступить в сообщество квалифицированных специалистов или продолжить обучение в университете.
В данном контексте мы предлагаем оперативно получить этот важный документ. Вы сможете приобрести диплом нового или старого образца, и это будет отличным решением для всех, кто не смог закончить обучение или потерял документ. диплом изготавливается аккуратно, с особым вниманием ко всем деталям, чтобы на выходе получился 100% оригинальный документ.
Плюсы подобного решения состоят не только в том, что можно оперативно получить диплом. Весь процесс организован комфортно, с профессиональной поддержкой. От выбора требуемого образца документа до консультаций по заполнению персональных данных и доставки в любой регион страны — все находится под абсолютным контролем опытных специалистов.
Всем, кто ищет максимально быстрый способ получения требуемого документа, наша услуга предлагает отличное решение. Приобрести диплом – это значит избежать продолжительного обучения и не теряя времени переходить к достижению собственных целей, будь то поступление в ВУЗ или старт карьеры.
https://diplomanc-russia24.com
На данный момент лучший способ бесплатно смотреть фильмы 2024 онлайн – это онлайн-кинотеатр Film-2024.com смотреть фильмы 2024
На данный момент лучший способ бесплатно смотреть фильмы 2024 онлайн – это онлайн-кинотеатр Film-2024.com фильмы 2024
Доставка алкоголя
canadian online pharmacy no prescription
lisinopril 5 mg india price
Магазин учитывает пожелания каждого покупателя, предоставляя персональные решения для освещения различных помещений https://maxiotzyv.ru/catalog/potolochnye-lyustry-s-antibakterialnym-pokrytiem-zabota-o-zdorove-v-kazhdom-elemente-doma
Магазин учитывает пожелания каждого покупателя, предоставляя персональные решения для освещения различных помещений http://all-smeta.ru/forum/viewtopic.php?f=2&t=4672
buy valtrex singapore
В нашем мире, где диплом становится началом удачной карьеры в любом направлении, многие ищут максимально быстрый и простой путь получения образования. Факт наличия официального документа об образовании сложно переоценить. Ведь диплом открывает дверь перед любым человеком, желающим начать трудовую деятельность или продолжить обучение в высшем учебном заведении.
Мы предлагаем оперативно получить этот важный документ. Вы сможете приобрести диплом, что будет выгодным решением для человека, который не смог закончить образование, потерял документ или хочет исправить плохие оценки. Каждый диплом изготавливается с особой аккуратностью, вниманием к мельчайшим деталям, чтобы в итоге получился 100% оригинальный документ.
Плюсы данного подхода заключаются не только в том, что вы сможете максимально быстро получить свой диплом. Процесс организовывается удобно, с нашей поддержкой. Начиная от выбора подходящего образца до консультации по заполнению персональных данных и доставки по России — все находится под абсолютным контролем качественных мастеров.
В итоге, для всех, кто ищет быстрый способ получения требуемого документа, наша компания может предложить выгодное решение. Купить диплом – это значит избежать длительного процесса обучения и сразу переходить к своим целям, будь то поступление в ВУЗ или начало трудовой карьеры.
https://diploman-rossiya.com
SEO-оптимизация сайта SEO — это комплекс действий непосредственно на сайте и вне его, необходимых для повышения позиций ресурса в поисковой органической выдаче Google по релевантным запросам, и как результат — его видимости целевой аудитории. Мы разделяем SEO на два этапа — это SEO-оптимизация и SEO-продвижение. Ведь без технически правильной SEO-оптимизации дальнейшее SEO-продвижение невозможно. При качественном SEO-продвижении, ваш сайт будет находиться на первой странице поисковиков, а значит — получать больше трафика и целевых действий от посетителей. Для сравнения, веб-ресурсы, которые не оптимизируют и не продвигают для поисковых систем, зачастую вообще не отображаются в выдаче и соответственно не имеют органических переходов. При формировании поисковой выдачи по запросу используется сложная формула сортировки, учитывающая десятки параметров. Алгоритмы ранжирования регулярно обновляются, дополняются и модернизируются с единой целью — обеспечить максимально релевантные ответы на запросы пользователей. Точный алгоритм построения выдачи результатов не разглашается работниками поисковиков, сообщаются лишь общие требования и критерии заточенного под SEO ресурса, позволяющие попасть в ТОП (первую десятку результатов). При этом каждый новый апдейт Google ужесточает правила для игроков на рынке маркетинга и добавляет работы SEO-специалистам и владельцам бизнесов. Побеждают сильнейшие — те, кто готов адаптироваться и постоянно работать над веб-ресурсом. Но в качестве вознаграждения — постоянный бесплатный органический трафик, повышение позиций и удержание ТОПа. На практике, без активных работ по поисковой оптимизации и продвижению практически невозможно вывести сайт на первую страницу выдачи в высококонкурентных коммерческих тематиках, даже если его контент и техническая реализация будут идеальными.
Продолжить чтение на Автоматическое продвижение сайта
prednisone 40 mg tablet
tadalafil tablets 10mg in india
Сегодня, когда диплом является началом удачной карьеры в любом направлении, многие ищут максимально простой путь получения образования. Наличие документа об образовании переоценить просто невозможно. Ведь именно диплом открывает двери перед людьми, желающими вступить в профессиональное сообщество или продолжить обучение в высшем учебном заведении.
Мы предлагаем быстро получить этот необходимый документ. Вы сможете купить диплом нового или старого образца, и это будет отличным решением для всех, кто не смог завершить образование, потерял документ или желает исправить плохие оценки. диплом изготавливается с особой тщательностью, вниманием ко всем деталям. В результате вы сможете получить 100% оригинальный документ.
Плюсы данного решения заключаются не только в том, что можно оперативно получить свой диплом. Процесс организовывается комфортно, с профессиональной поддержкой. От выбора подходящего образца до правильного заполнения личных данных и доставки по стране — все будет находиться под полным контролем наших мастеров.
Всем, кто пытается найти быстрый и простой способ получить необходимый документ, наша услуга предлагает выгодное решение. Купить диплом – значит избежать длительного обучения и сразу переходить к важным целям, будь то поступление в ВУЗ или старт карьеры.
https://dlplomanrussian.com
Right here is the right web site for anyone who wishes to find out about this topic. You understand so much its almost hard to argue with you (not that I personally would want to…HaHa). You definitely put a brand new spin on a subject which has been discussed for decades. Excellent stuff, just excellent!
Официальный vavada Online Casino – бонусы на первый депозит 100% от 1000$! Максбет турниры на реальный деньги и автомобили Mercedes в Vavada казино!
recommended canadian pharmacies
В нашем обществе, где диплом – это начало отличной карьеры в любом направлении, многие ищут максимально простой путь получения образования. Наличие документа об образовании переоценить невозможно. Ведь диплом открывает двери перед каждым человеком, желающим вступить в профессиональное сообщество или продолжить обучение в ВУЗе.
В данном контексте наша компания предлагает очень быстро получить этот необходимый документ. Вы сможете купить диплом, что становится удачным решением для человека, который не смог завершить образование, утратил документ или желает исправить свои оценки. диплом изготавливается с особой тщательностью, вниманием ко всем деталям. На выходе вы получите 100% оригинальный документ.
Превосходство подобного подхода заключается не только в том, что можно быстро получить свой диплом. Процесс организован просто и легко, с нашей поддержкой. Начав от выбора подходящего образца документа до консультаций по заполнению личных данных и доставки в любое место России — все под полным контролем квалифицированных мастеров.
Для всех, кто пытается найти максимально быстрый способ получить требуемый документ, наша компания предлагает отличное решение. Заказать диплом – это значит избежать долгого процесса обучения и сразу переходить к своим целям: к поступлению в университет или к началу трудовой карьеры.
https://diploman-rossiya.com
buy generic metformin
canadian prescription pharmacy
zestril brand name
Сегодня, когда диплом является началом удачной карьеры в любой сфере, многие пытаются найти максимально быстрый и простой путь получения качественного образования. Факт наличия официального документа об образовании переоценить попросту невозможно. Ведь именно он открывает дверь перед каждым человеком, который стремится начать профессиональную деятельность или учиться в каком-либо институте.
В данном контексте наша компания предлагает быстро получить этот важный документ. Вы имеете возможность купить диплом, и это становится удачным решением для человека, который не смог закончить образование, потерял документ или желает исправить свои оценки. Каждый диплом изготавливается аккуратно, с максимальным вниманием к мельчайшим деталям. В итоге вы сможете получить продукт, полностью соответствующий оригиналу.
Плюсы такого подхода заключаются не только в том, что можно оперативно получить диплом. Процесс организован комфортно, с профессиональной поддержкой. От выбора подходящего образца документа до консультаций по заполнению личной информации и доставки по России — все под полным контролем опытных специалистов.
Всем, кто хочет найти максимально быстрый способ получить необходимый документ, наша компания может предложить выгодное решение. Заказать диплом – это значит избежать долгого процесса обучения и не теряя времени перейти к своим целям: к поступлению в университет или к началу удачной карьеры.
https://diploman-rossiya.com
generic tadalafil cheap
GET X – финансовая игра с выводом реальных средств. На данный момент на сайте представлена одна самых популярных и известных финансовых игр – Crash гет х
GET X – финансовая игра с выводом реальных средств. На данный момент на сайте представлена одна самых популярных и известных финансовых игр – Crash getx официальный сайт
best european online pharmacy
В современном мире, где диплом – это начало отличной карьеры в любой области, многие ищут максимально простой путь получения образования. Наличие официального документа об образовании переоценить невозможно. Ведь именно диплом открывает двери перед людьми, желающими начать трудовую деятельность или учиться в каком-либо ВУЗе.
В данном контексте мы предлагаем очень быстро получить этот необходимый документ. Вы имеете возможность купить диплом старого или нового образца, что становится отличным решением для всех, кто не смог завершить образование или утратил документ. диплом изготавливается с особой аккуратностью, вниманием ко всем нюансам, чтобы в итоге получился продукт, максимально соответствующий оригиналу.
Плюсы этого подхода состоят не только в том, что вы быстро получите диплом. Весь процесс организован удобно, с нашей поддержкой. Начиная от выбора подходящего образца до правильного заполнения персональной информации и доставки по России — все будет находиться под полным контролем квалифицированных специалистов.
Для тех, кто пытается найти оперативный способ получения необходимого документа, наша компания предлагает отличное решение. Приобрести диплом – это значит избежать долгого обучения и не теряя времени переходить к личным целям, будь то поступление в университет или старт профессиональной карьеры.
https://diploman-russiyans.com
Дизайн-радиаторы — функциональное украшение интерьера, доступные в разных цветах и размерах, с возможностью добавления тэнов https://telegra.ph/CHto-takoe-dizajn-radiatory-otopleniya-03-11
В нашем обществе, где диплом – это начало удачной карьеры в любой сфере, многие ищут максимально быстрый и простой путь получения качественного образования. Наличие документа об образовании трудно переоценить. Ведь именно он открывает дверь перед всеми, кто хочет вступить в сообщество профессионалов или продолжить обучение в ВУЗе.
В данном контексте наша компания предлагает оперативно получить этот важный документ. Вы можете приобрести диплом, и это будет отличным решением для всех, кто не смог закончить обучение, потерял документ или желает исправить плохие оценки. дипломы изготавливаются аккуратно, с особым вниманием к мельчайшим элементам, чтобы в итоге получился документ, полностью соответствующий оригиналу.
Преимущество этого подхода заключается не только в том, что вы быстро получите диплом. Весь процесс организовывается удобно, с профессиональной поддержкой. От выбора необходимого образца диплома до точного заполнения персональной информации и доставки по стране — все будет находиться под полным контролем наших мастеров.
Для всех, кто хочет найти быстрый и простой способ получить необходимый документ, наша компания предлагает отличное решение. Заказать диплом – это значит избежать продолжительного процесса обучения и не теряя времени перейти к важным целям: к поступлению в университет или к началу удачной карьеры.
https://dlplomanrussian.com
Холодильники Smeg сочетают стиль и технологии, поддерживая продукты свежими. Они включают модели с различными функциями и стильным дизайном, от ретро до современных. Серия 50’s Style выделяется яркими цветами и ретро-дизайном. Энергоэффективность классов A+ и A++ обеспечивает экономию электроэнергии, делая Smeg идеальным для любого интерьера Холодильник Smeg
Бонусы и Акции 1Win 2024: Ваш Путь к Успеху
Ищете способ максимизировать свои выигрыши? Букмекерская контора 1Win предлагает невероятный бонус код 937999, который открывает дверь к миру беспрецедентных возможностей. С этим промокодом новые клиенты могут получить денежный бонус в размере 500% до 200 000 рублей на первые четыре депозита. Это ваш шанс начать с большого и продолжать выигрывать!
1Win: не просто букмекерская контора, а мир, где каждый может стать победителем. Ставки на спорт, онлайн-казино, розыгрыши и турниры — все это доступно в одном месте, где более 1000 вариантов ставок ждут вас.
Как использовать 1win промокод какой?
Процесс активации промокода 937999 прост и понятен:
Переход на сайт: Используйте зеркало или VPN-сервис для доступа к официальному сайту 1Win.
Регистрация: Нажмите “Зарегистрироваться” и заполните необходимые данные. Выберите удобный способ регистрации — через социальные сети или электронную почту.
Активация промокода: Введите 937999 в специальное поле промокода и завершите регистрацию.
После этих шагов вы станете полноправным участником игрового сообщества 1Win и сможете воспользоваться всеми преимуществами промокода.
metformin 1000 mg tablet
cialis ingredients
no prescription cialis generic
Промокод 1Win на сегодня, 2024 год – 937999. При регистрации с использованием этого кода активируется приветственный бонус в размере 500% до 75 000 рублей. Это специальное предложение от букмекера 1Win позволяет новым игрокам получить дополнительные привилегии и бонусы.
1Win – это платформа, которая радует своих пользователей разнообразными акциями. В 2024 году они предлагают следующие привлекательные бонусы для новичков:
Бездепозитные бонусы: Получите бонусы без необходимости внесения депозита.
Фриспины: Бесплатные вращения на слотах.
Фрибет бонусы: Возможность сделать бесплатные ставки.
Кэшбэк: Возврат части потерянных средств.
Промокод 937999 следует ввести при регистрации, чтобы получить максимальный бонус. Не упустите шанс увеличить свой баланс и наслаждаться игрой на 1Win!
промокоды на 1win aviator используйте промокод 937999, чтобы получить максимальный бонус в размере 500% до 75 000 рублей. Этот код активирует приветственный бонус, который будет зачислен на два бонусных счета одновременно: на счета “Ставки” и “Казино”.
Важно учесть следующие особенности и предостережения при использовании промокода:
Различные поводы: Промокоды в 1Win выдаются по разным поводам, таким как акции, специальные события или дни рождения клиентов.
Активация и доступ к бонусам: После активации промокода при регистрации бонусные средства станут доступны после входа в ваш профиль. Личные промокоды требуют вашего согласия на участие в предложении.
Конвертация в реальные деньги: Бонусы будут зачислены на ваш бонусный счет с указанием доступной суммы в личном кабинете. При выполнении условий использования бонусов вы сможете конвертировать их в реальные деньги, которые дополнят ваш выигрыш.
Будьте бдительны: При поиске промокодов обращайте внимание на источник информации. Некоторые мошенники предлагают “бесплатные” промокоды с целью получить ваши личные данные. Регистрируйтесь и вводите информацию только на официальном сайте 1Win.
generic cialis 30 mg
Алматы Азарт – это уникальное игровое пространство для людей старше 30 лет, которые ценят интеллектуальный досуг и общение https://one.link/plclub
valtrex 500 mg buy online
Алматы Азарт – это уникальное игровое пространство для людей старше 30 лет, которые ценят интеллектуальный досуг и общение https://campsite.bio/playkz
Промокод 1Win на сегодня, 2024 год – 937999. При регистрации с использованием этого кода активируется приветственный бонус в размере 500% до 75 000 рублей. Это специальное предложение от букмекера 1Win позволяет новым игрокам получить дополнительные привилегии и бонусы.
1Win – это платформа, которая радует своих пользователей разнообразными акциями. В 2024 году они предлагают следующие привлекательные бонусы для новичков:
Бездепозитные бонусы: Получите бонусы без необходимости внесения депозита.
Фриспины: Бесплатные вращения на слотах.
Фрибет бонусы: Возможность сделать бесплатные ставки.
Кэшбэк: Возврат части потерянных средств.
Промокод 937999 следует ввести при регистрации, чтобы получить максимальный бонус. Не упустите шанс увеличить свой баланс и наслаждаться игрой на 1Win!
1win промокод на пополнение счета используйте промокод 937999, чтобы получить максимальный бонус в размере 500% до 75 000 рублей. Этот код активирует приветственный бонус, который будет зачислен на два бонусных счета одновременно: на счета “Ставки” и “Казино”.
Важно учесть следующие особенности и предостережения при использовании промокода:
Различные поводы: Промокоды в 1Win выдаются по разным поводам, таким как акции, специальные события или дни рождения клиентов.
Активация и доступ к бонусам: После активации промокода при регистрации бонусные средства станут доступны после входа в ваш профиль. Личные промокоды требуют вашего согласия на участие в предложении.
Конвертация в реальные деньги: Бонусы будут зачислены на ваш бонусный счет с указанием доступной суммы в личном кабинете. При выполнении условий использования бонусов вы сможете конвертировать их в реальные деньги, которые дополнят ваш выигрыш.
Будьте бдительны: При поиске промокодов обращайте внимание на источник информации. Некоторые мошенники предлагают “бесплатные” промокоды с целью получить ваши личные данные. Регистрируйтесь и вводите информацию только на официальном сайте 1Win.
valtrex 500mg uk
synthroid uk
synthroid 50 mg price
1000 mg valtrex daily
http://thcs-phuocnguyen-baria.edu.vn/xemchude/911/.html
can i buy lisinopril over the counter in canada
Поставить счетчики на воду в квартире – означает значительно снизить затраты на оплату этой части ЖКХ https://progkh.ru/
where can i buy metformin 500 mg
metformin how to buy
medication lisinopril 5 mg
cialis 2.5 mg price in india
We bieden tijdelijke telefoonnummers in tientallen landen over de hele wereld, met duizenden nummers om uit te kiezen https://jaidengtbf02579.arwebo.com/49830104/het-belang-van-mobiele-nummers-in-duitsland-een-gids
canadian pharmacy cialis 20mg
We bieden tijdelijke telefoonnummers in tientallen landen over de hele wereld, met duizenden nummers om uit te kiezen https://rivervirv01003.blogs-service.com/57761621/het-belang-van-tijdelijke-telefoonnummers-een-diepgaande-verkenning
cost of synthroid in canada
canadian pharmacy in canada
https://computer.ju.edu.jo/Lists/Alumni%20Feedback%20Survey/DispForm.aspx?ID=73377
buy tadalafil online no prescription
Промокод 1Win на сегодня, 2024 год – 937999. При регистрации с использованием этого кода активируется приветственный бонус в размере 500% до 75 000 рублей. Это специальное предложение от букмекера 1Win позволяет новым игрокам получить дополнительные привилегии и бонусы.
1Win – это платформа, которая радует своих пользователей разнообразными акциями. В 2024 году они предлагают следующие привлекательные бонусы для новичков:
Бездепозитные бонусы: Получите бонусы без необходимости внесения депозита.
Фриспины: Бесплатные вращения на слотах.
Фрибет бонусы: Возможность сделать бесплатные ставки.
Кэшбэк: Возврат части потерянных средств.
Промокод 937999 следует ввести при регистрации, чтобы получить максимальный бонус. Не упустите шанс увеличить свой баланс и наслаждаться игрой на 1Win!
промокод на 1win при регистрации на деньги используйте промокод 937999, чтобы получить максимальный бонус в размере 500% до 75 000 рублей. Этот код активирует приветственный бонус, который будет зачислен на два бонусных счета одновременно: на счета “Ставки” и “Казино”.
Важно учесть следующие особенности и предостережения при использовании промокода:
Различные поводы: Промокоды в 1Win выдаются по разным поводам, таким как акции, специальные события или дни рождения клиентов.
Активация и доступ к бонусам: После активации промокода при регистрации бонусные средства станут доступны после входа в ваш профиль. Личные промокоды требуют вашего согласия на участие в предложении.
Конвертация в реальные деньги: Бонусы будут зачислены на ваш бонусный счет с указанием доступной суммы в личном кабинете. При выполнении условий использования бонусов вы сможете конвертировать их в реальные деньги, которые дополнят ваш выигрыш.
Будьте бдительны: При поиске промокодов обращайте внимание на источник информации. Некоторые мошенники предлагают “бесплатные” промокоды с целью получить ваши личные данные. Регистрируйтесь и вводите информацию только на официальном сайте 1Win.
tadalafil 10mg price in india
Циклёвка паркета: особенности и этапы услуги
Циклёвка паркета — это процесс восстановления внешнего вида паркетного пола путём удаления верхнего повреждённого слоя и возвращения ему первоначального вида. Услуга включает в себя несколько этапов:
Подготовка: перед началом работы необходимо защитить мебель и другие предметы от пыли и грязи, а также удалить плинтусы.
Шлифовка: с помощью шлифовальной машины удаляется старый лак и верхний повреждённый слой древесины.
Шпатлёвка: после шлифовки поверхность паркета шпатлюется для заполнения трещин и выравнивания поверхности.
Грунтовка: перед нанесением лака паркет грунтуется для улучшения адгезии и защиты от плесени и грибка.
Нанесение лака: лак наносится в несколько слоёв с промежуточной шлифовкой между ними.
Полировка: после нанесения последнего слоя лака паркет полируется для придания поверхности блеска и гладкости.
Циклёвка паркета позволяет обновить внешний вид пола, восстановить его структуру и продлить срок службы.
Сайт: ykladka-parketa.ru
Циклевка паркета
tadalafil 2.5 mg tablet
cheapest pharmacy prescription drugs
Howdy! This is kind of off topic but I need some guidance from an established blog. Is it very hard to set up your own blog? I’m not very techincal but I can figure things out pretty fast. I’m thinking about creating my own but I’m not sure where to start. Do you have any ideas or suggestions? Many thanks
https://nudifyai.net/nudify-her/
prednisone 20mg
zithromax z-pak
Wanneer krijg ik een tijdelijk nummer? Als je met nummerbehoud overstapt naar Odido, krijg je van ons een tijdelijk Odido telefoonnummer bij je nieuwe simkaart https://knoxtdmt52073.aioblogs.com/80517552/het-belang-van-een-telegram-telefoonnummer
Wanneer krijg ik een tijdelijk nummer? Als je met nummerbehoud overstapt naar Odido, krijg je van ons een tijdelijk Odido telefoonnummer bij je nieuwe simkaart https://lanebpzg18629.p2blogs.com/26441575/de-vrijheid-van-telegram-zonder-telefoonnummer
where can i buy metformin over the counter uk
canadian pharmacy 24 com
https://www2.sgc.gov.co/participacion/Lists/PQRD/DispForm.aspx?ID=18015
Промокод 1Win на сегодня, 2024 год – 937999. При регистрации с использованием этого кода активируется приветственный бонус в размере 500% до 75 000 рублей. Это специальное предложение от букмекера 1Win позволяет новым игрокам получить дополнительные привилегии и бонусы.
1Win – это платформа, которая радует своих пользователей разнообразными акциями. В 2024 году они предлагают следующие привлекательные бонусы для новичков:
Бездепозитные бонусы: Получите бонусы без необходимости внесения депозита.
Фриспины: Бесплатные вращения на слотах.
Фрибет бонусы: Возможность сделать бесплатные ставки.
Кэшбэк: Возврат части потерянных средств.
Промокод 937999 следует ввести при регистрации, чтобы получить максимальный бонус. Не упустите шанс увеличить свой баланс и наслаждаться игрой на 1Win!
промокод 1win сегодня при регистрации используйте промокод 937999, чтобы получить максимальный бонус в размере 500% до 75 000 рублей. Этот код активирует приветственный бонус, который будет зачислен на два бонусных счета одновременно: на счета “Ставки” и “Казино”.
Важно учесть следующие особенности и предостережения при использовании промокода:
Различные поводы: Промокоды в 1Win выдаются по разным поводам, таким как акции, специальные события или дни рождения клиентов.
Активация и доступ к бонусам: После активации промокода при регистрации бонусные средства станут доступны после входа в ваш профиль. Личные промокоды требуют вашего согласия на участие в предложении.
Конвертация в реальные деньги: Бонусы будут зачислены на ваш бонусный счет с указанием доступной суммы в личном кабинете. При выполнении условий использования бонусов вы сможете конвертировать их в реальные деньги, которые дополнят ваш выигрыш.
Будьте бдительны: При поиске промокодов обращайте внимание на источник информации. Некоторые мошенники предлагают “бесплатные” промокоды с целью получить ваши личные данные. Регистрируйтесь и вводите информацию только на официальном сайте 1Win.
online pharmacy in germany
Бонусы и Акции 1Win 2024: Ваш Путь к Успеху
Ищете способ максимизировать свои выигрыши? Букмекерская контора 1Win предлагает невероятный бонус код 937999, который открывает дверь к миру беспрецедентных возможностей. С этим промокодом новые клиенты могут получить денежный бонус в размере 500% до 200 000 рублей на первые четыре депозита. Это ваш шанс начать с большого и продолжать выигрывать!
1Win: не просто букмекерская контора, а мир, где каждый может стать победителем. Ставки на спорт, онлайн-казино, розыгрыши и турниры — все это доступно в одном месте, где более 1000 вариантов ставок ждут вас.
Как использовать промокод на 1вин при пополнении?
Процесс активации промокода 937999 прост и понятен:
Переход на сайт: Используйте зеркало или VPN-сервис для доступа к официальному сайту 1Win.
Регистрация: Нажмите “Зарегистрироваться” и заполните необходимые данные. Выберите удобный способ регистрации — через социальные сети или электронную почту.
Активация промокода: Введите 937999 в специальное поле промокода и завершите регистрацию.
После этих шагов вы станете полноправным участником игрового сообщества 1Win и сможете воспользоваться всеми преимуществами промокода.
price for synthroid 112 mcg
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
бонус промокод 1win: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
valtrex 2 g
valtrex 500 india
Wanneer krijg ik een tijdelijk nummer? Als je met nummerbehoud overstapt naar Odido, krijg je van ons een tijdelijk Odido telefoonnummer bij je nieuwe simkaart telegram zonderВ telefoonnummer
https://www.holycrossconvent.edu.na/profile/stanleyvbz35/profile
Wanneer krijg ik een tijdelijk nummer? Als je met nummerbehoud overstapt naar Odido, krijg je van ons een tijdelijk Odido telefoonnummer bij je nieuwe simkaart telefoonnummer duitsland bellen
Изготавливаем столешницы, подоконники, барные стойки и другую мебель из акрилового камня и кварцевого агломерата под заказ по выгодной цене в Москве кварцевый агломерат
Изготавливаем столешницы, подоконники, барные стойки и другую мебель из акрилового камня и кварцевого агломерата под заказ по выгодной цене в Москве Столешницы из акрилового камня
cialis order
Шикарные идеи для Вашего дизайна по ссылке. Трендовые новинки дизайна интерьера. Оцени самые новые идеи дизайна интерьера из Италии https://stolovaya33.ru/dizayn-i-interer/243-ispolzovanie-naturalnyh-materialov-v-otdelke-i-dizayne-interera.html
buy zestril
yaşamkent tesettür bağlama |
kraken onion – kraken onion, кракен тор
synthroid 88 mcg coupon
canadian valtrex no rx
Наша компания предлагает высококачественные услуги Аренда мини-экскаватора bobcat в Алматы Мы обеспечиваем надежное и профессиональное оборудование для выполнения различных земляных работ на строительных площадках и других объектах. Наш опытный персонал и гибкие условия аренды делают нас надежным партнером для вашего проекта.
Наш дайвинг клуб осуществляет обучение дайвингу от новичка до профессионала. Мы организуем пробные погружения с аквалангом в бассейнах Москвы и открытых водоемах Подмосковья. Кроме этого, в нашем дайв-клубе Вы можете приобрести подарочные сертификат на любой курс дайвинга или пробное погружение обучение дайвингу в москве
Наш дайвинг клуб осуществляет обучение дайвингу от новичка до профессионала. Мы организуем пробные погружения с аквалангом в бассейнах Москвы и открытых водоемах Подмосковья. Кроме этого, в нашем дайв-клубе Вы можете приобрести подарочные сертификат на любой курс дайвинга или пробное погружение профессиональный дайвинг
кракен онион – кракен официальный сайт, kraken darknet market зеркало
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
как ввести промокод на 1вин после регистрации: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
https://www.unidos.edu.uy/profile/stanleyvbz35/profile
read what he said anydesk download
Каркасный дом
As a farmer, I can’t recommend the Mandako Stubble Cruncher enough! This equipment has truly revolutionized my field preparation process, saving me time and effort while improving soil health. The ability to quickly decompose harvest residue and enhance soil fertility has made a noticeable difference in my crop yields. Investing in the Stubble Cruncher is investing in the future of your farm – trust me, you won’t regret it! https://mandako.com/products/reddi-arm/
synthroid 50
check my reference tradingview download
foreign pharmacy online
synthroid cost canada
www canadianonlinepharmacy
buy zithromax uk
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
промокоды для 1win: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
Мы организуем пробные погружения с аквалангом в бассейнах Москвы и открытых водоемах Подмосковья. Наш дайвинг клуб осуществляет обучение дайвингу от новичка до профессионала. Кроме этого, в нашем дайв-клубе Вы можете приобрести подарочные сертификат на любой курс дайвинга или пробное погружение дайв центр
Мы организуем пробные погружения с аквалангом в бассейнах Москвы и открытых водоемах Подмосковья. Наш дайвинг клуб осуществляет обучение дайвингу от новичка до профессионала. Кроме этого, в нашем дайв-клубе Вы можете приобрести подарочные сертификат на любой курс дайвинга или пробное погружение занятия дайвингом
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
промокоды 1вин при регистрации 2024: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
valtrex 550 mg
https://www.gidgeesbushcamp.com.au/profile/stanleyvbz35/profile
Большой выбор игрушек для взрослых с быстрой курьерской доставкой. Анонимная упаковка – запечатанный крафт пакет https://sexshop25.ru/catalog/vibratory/
Большой выбор игрушек для взрослых с быстрой курьерской доставкой. Анонимная упаковка – запечатанный крафт пакет Вибраторы Владивосток
Промокод 1Win на сегодня, 2024 год – 937999. При регистрации с использованием этого кода активируется приветственный бонус в размере 500% до 75 000 рублей. Это специальное предложение от букмекера 1Win позволяет новым игрокам получить дополнительные привилегии и бонусы.
1Win – это платформа, которая радует своих пользователей разнообразными акциями. В 2024 году они предлагают следующие привлекательные бонусы для новичков:
Бездепозитные бонусы: Получите бонусы без необходимости внесения депозита.
Фриспины: Бесплатные вращения на слотах.
Фрибет бонусы: Возможность сделать бесплатные ставки.
Кэшбэк: Возврат части потерянных средств.
Промокод 937999 следует ввести при регистрации, чтобы получить максимальный бонус. Не упустите шанс увеличить свой баланс и наслаждаться игрой на 1Win!
1win com промокоды используйте промокод 937999, чтобы получить максимальный бонус в размере 500% до 75 000 рублей. Этот код активирует приветственный бонус, который будет зачислен на два бонусных счета одновременно: на счета “Ставки” и “Казино”.
Важно учесть следующие особенности и предостережения при использовании промокода:
Различные поводы: Промокоды в 1Win выдаются по разным поводам, таким как акции, специальные события или дни рождения клиентов.
Активация и доступ к бонусам: После активации промокода при регистрации бонусные средства станут доступны после входа в ваш профиль. Личные промокоды требуют вашего согласия на участие в предложении.
Конвертация в реальные деньги: Бонусы будут зачислены на ваш бонусный счет с указанием доступной суммы в личном кабинете. При выполнении условий использования бонусов вы сможете конвертировать их в реальные деньги, которые дополнят ваш выигрыш.
Будьте бдительны: При поиске промокодов обращайте внимание на источник информации. Некоторые мошенники предлагают “бесплатные” промокоды с целью получить ваши личные данные. Регистрируйтесь и вводите информацию только на официальном сайте 1Win.
cialis 5
synthroid 125 mg cost
Приглашаем Вас от души развлечься и отдохнуть в ресторан True Bar в Измайлово. Здесь можно не только хорошо провести время, но и заказать банкет по выгодной цене. Юбилеи, свадьбы, празднование дня рождения – всё это можно организовать с оптимальным соотношением цена/качество и провести банкет в ресторане на высшем уровне. Всегда для Вам лучшие закуски и изысканные блюда, богатый выбор алкогольных и безалкогольных напитков, а также вечерняя шоу-программа
The topic of Royal Coins two: Hold and Win is undoubtedly an exquisite combination of regality and opulence, sweeping gamers right into a world where Every single spin is steeped during the promise of untold riches. If you’re in Zambia, African Betting Tutorial is here to help make your journey zambia casino games
The topic of Royal Coins two: Hold and Win is undoubtedly an exquisite combination of regality and opulence, sweeping gamers right into a world where Every single spin is steeped during the promise of untold riches. If you’re in Zambia, African Betting Tutorial is here to help make your journey zambia casino games
Стоимость обучения на курсе английского для начинающих онлайн в 1,3-2,5 раза ниже стоимости группового обучения на языковых курсах, где ориентируются на группу, а не ваши индивидуальные потребности курсы английского языка онлайн рейтинг
3 tadalafil prescription
Стоимость обучения на курсе английского для начинающих онлайн в 1,3-2,5 раза ниже стоимости группового обучения на языковых курсах, где ориентируются на группу, а не ваши индивидуальные потребности лучшие онлайн курсы по английскому языку
no prescription metformin online
cialis tadalafil 20mg
synthroid 125 mcg price
buy valtrex in mexico
1Win Приветственный Бонус (2024): Полное Руководство
Промокод 937999 от 1Win — это ваш ключ к миру больших возможностей. С этим кодом, при первом депозите, вы можете получить бонус в размере 500% до 200 000 рублей. Это уникальное предложение позволяет новым клиентам значительно увеличить свой игровой бюджет и получить максимальное удовольствие от игры в спорте и казино.
Как работает приветственный бонус?
1win букмекерская контора промокод разделен на четыре этапа:
Первый депозит: Получите 200% от суммы депозита.
Второй депозит: Получите 150% от суммы второго депозита.
Третий депозит: Получите 100% от суммы.
Четвертый депозит: Получите 50% от суммы.
Максимальная сумма бонуса составляет 200,000 рублей, а максимальный бонус на один депозит — 50,000 рублей.
Как активировать промокод?
Чтобы активировать промокод 937999:
Зарегистрируйтесь на сайте 1Win.
Введите промокод при регистрации или дайте согласие на участие в акции, если промокод был предоставлен лично.
Пополните счет и начните играть, используя приветственный бонус.
Как отыграть бонус?
Чтобы отыграть бонусные средства:
Делайте ставки с коэффициентом от 3.
В случае выигрыша, 5% от бонусного счета переводится на ваш основной счет.
Пример:
Вы внесли 10 000 рублей и получили 20 000 рублей бонуса.
Сделали ставку с коэффициентом 3 и выиграли 30 000 рублей плюс 500 рублей бонуса.
Ваш счет теперь 30 500 рублей, а бонусный счет — 19 500 рублей.
Дополнительные бонусы и акции
1Win также предлагает различные акции и бонусы для любителей казино и экспресс-ставок. Следите за обновлениями на сайте, чтобы не пропустить самые выгодные предложения.
Обратите внимание: ставки с коэффициентом менее 3 не учитываются при отыгрыше бонуса.
buy tadalafil online cheap
Адвокат Запорожье — юрист Запорожье. Военный адвокат Запорожье. Помощь опытных адвокатов в Запорожье и Запорожской области. Любые виды юридических услуг и консультаций адвокатов
Адвокат военный Украина
Профессиональная круглосуточная поддержка адвоката позволяет держать в курсе дела и во время принимать необходимые меры. Вся информация о нас находится в реестре Адвокатов Украины, документы, подтверждающие наши полномочия, будут представлены при личной встрече.
Адвокат Запорожье. Военный адвокат Запорожье. Мы — команда адвокатов по международному, национальному и военному праву, с многолетним опытом практической работы. Наши сотрудники — члены Национальной ассоциации Адвокатов Украины, а некоторые и члены Международных обществ и организаций.
У нас нет молодых специалистов, которые на делах клиентов набираются опыта. Наша работа – это наше хобби, поэтому к каждому делу мы относимся ответственно, подбирая индивидуальный подход. Мы знаем, что нужно делать, чтобы выиграть Ваше дело.
cost of brand name synthroid
tadalafil 5 mg tablet coupon
SightCare formula aims to maintain 20/20 vision without the need for any surgical process. This supplement is a perfect solution for people facing issues as they grow older. https://sightcare-web.com/
Пластическая хирургия — увеличение груди имплантами, подтяжка груди, уменьшение груди. Абдоминопластика — пластика по уменьшению живота, липосакция и липофилинг пластический хирург цена
zithromax drug
Пластическая хирургия — увеличение груди имплантами, подтяжка груди, уменьшение груди. Абдоминопластика — пластика по уменьшению живота, липосакция и липофилинг пластическая хирург в Москве
Elevate your data extraction skills with this comprehensive guide on extracting data from LinkedIn without the API! Read on for valuable insights.
buy synthyroid online
synthroid 50 mg price
prednisone in canada
В поисках идеального промокода для ставок в онлайн-казино? 1Win предлагает уникальный код 937999, который не только увеличивает шансы на крупный выигрыш, но и делает игровой процесс еще более захватывающим. Вот ваше руководство по выбору и использованию промокода на 2024 год.
Преимущества использования промокода 1Win
Использование промокода 937999 промокод 1win при пополнение счета открывает перед вами двери в мир больших возможностей:
Увеличение начального капитала: После активации промокода и выполнения условий отыгрыша, ваш первоначальный депозит может увеличиться до 500%, достигая суммы в 75 000 рублей.
Минимизация рисков: Некоторые промокоды позволяют застраховать вашу первую ставку, снижая потенциальные потери.
Кешбэк: Получайте обратно часть потраченных средств, что делает каждую игру менее рискованной.
Эксклюзивные розыгрыши: Промокод открывает доступ к специальным акциям и розыгрышам, где можно выиграть значительные призы.
Как выбрать промокод?
Выбор промокода – это не просто вопрос личных предпочтений, но и стратегическое решение. Вот несколько критериев, которые помогут вам сделать правильный выбор:
Срок действия: Убедитесь, что промокод актуален. Для 937999 срок действия истекает 31 декабря 2024 года.
Условия отыгрыша: Внимательно изучите условия, при которых вы сможете использовать бонусные средства.
Размер бонуса: Выбирайте промокоды, которые предлагают максимальную выгоду от вашего депозита.
Дополнительные возможности: Ищите промокоды, которые предоставляют дополнительные преимущества, такие как фрибеты или кешбэк.
Как использовать промокод?
Чтобы активировать промокод 937999 в 1Win, выполните следующие шаги:
Перейдите на сайт 1Win и начните процесс регистрации.
Заполните все необходимые поля в анкете.
Введите промокод 937999 в соответствующее поле.
Завершите регистрацию и внесите первый депозит.
Помните, что использование промокода – это отличный способ усилить ваш игровой опыт и увеличить шансы на успех. Выбирайте мудро и пусть удача всегда будет на вашей стороне!
Мощные и эффективные: генераторы пены ГПСС для вашего бизнеса. Повысьте уровень безопасности и гигиены с нашими генераторами пены ГПСС муфты для азс
Мощные и эффективные: генераторы пены ГПСС для вашего бизнеса. Повысьте уровень безопасности и гигиены с нашими генераторами пены ГПСС метрошток чорний
В поисках идеального промокода для ставок в онлайн-казино? 1Win предлагает уникальный код 937999, который не только увеличивает шансы на крупный выигрыш, но и делает игровой процесс еще более захватывающим. Вот ваше руководство по выбору и использованию промокода на 2024 год.
Преимущества использования промокода 1Win
Использование промокода 937999 промокод бк 1win открывает перед вами двери в мир больших возможностей:
Увеличение начального капитала: После активации промокода и выполнения условий отыгрыша, ваш первоначальный депозит может увеличиться до 500%, достигая суммы в 75 000 рублей.
Минимизация рисков: Некоторые промокоды позволяют застраховать вашу первую ставку, снижая потенциальные потери.
Кешбэк: Получайте обратно часть потраченных средств, что делает каждую игру менее рискованной.
Эксклюзивные розыгрыши: Промокод открывает доступ к специальным акциям и розыгрышам, где можно выиграть значительные призы.
Как выбрать промокод?
Выбор промокода – это не просто вопрос личных предпочтений, но и стратегическое решение. Вот несколько критериев, которые помогут вам сделать правильный выбор:
Срок действия: Убедитесь, что промокод актуален. Для 937999 срок действия истекает 31 декабря 2024 года.
Условия отыгрыша: Внимательно изучите условия, при которых вы сможете использовать бонусные средства.
Размер бонуса: Выбирайте промокоды, которые предлагают максимальную выгоду от вашего депозита.
Дополнительные возможности: Ищите промокоды, которые предоставляют дополнительные преимущества, такие как фрибеты или кешбэк.
Как использовать промокод?
Чтобы активировать промокод 937999 в 1Win, выполните следующие шаги:
Перейдите на сайт 1Win и начните процесс регистрации.
Заполните все необходимые поля в анкете.
Введите промокод 937999 в соответствующее поле.
Завершите регистрацию и внесите первый депозит.
Помните, что использование промокода – это отличный способ усилить ваш игровой опыт и увеличить шансы на успех. Выбирайте мудро и пусть удача всегда будет на вашей стороне!
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
1win официальный сайт 1вин промокоды: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
brazilian pharmacy online
can you buy metformin without a prescription
В этой подборке онлайн-курсов по английскому языку мы сравнили предложения школ по нескольким параметрам и отобрали лучшие варианты для взрослых и детей, начинающих познание языка или повышающих свой уровень курсы по английскому языку с нуля онлайн
В этой подборке онлайн-курсов по английскому языку мы сравнили предложения школ по нескольким параметрам и отобрали лучшие варианты для взрослых и детей, начинающих познание языка или повышающих свой уровень курсы английского онлайн
look at this website Obs studio download
web sollet wallet
online pharmacy com
happy family canadian pharmacy
article evon free
tadalafil uk cheap
look here AI-enabled automated trading platforms
lisinopril online uk
my latest blog post delta roblox
check my site jaxx download
metformin glucophage
В этой подборке онлайн-курсов по английскому языку мы сравнили предложения школ по нескольким параметрам и отобрали лучшие варианты для взрослых и детей, начинающих познание языка или повышающих свой уровень курсы английского языка онлайн с нуля взрослым
В этой подборке онлайн-курсов по английскому языку мы сравнили предложения школ по нескольким параметрам и отобрали лучшие варианты для взрослых и детей, начинающих познание языка или повышающих свой уровень курсы разговорного английского онлайн
Good day very nice blog!! Guy .. Excellent .. Superb .. I will bookmark your website and take the feeds also? I am happy to seek out a lot of useful info right here in the publish, we want work out more strategies in this regard, thank you for sharing. . . . . .
https://zenwriting.net/fastofldxm/h1-b-iak-vibrati-sklo-far-farfarlight-shchob-zadovol-niti-vsi-svoyi
canadian pharmacy antibiotics
synthroid 137 pill
online pharmacy no script synthroid 75
cialis for sale uk
order synthroid without prescription
cheap metaformin
Lineage 2 website development – разработка сайта опен кейс, опен кейс шаблон сайта
создание сайта dota2 опен кейс – дизайн сайта Lineage 2, WoW website templates
20 mg lisinopril tablets
Hi there, constantly i used to check web site posts here early in the break of day, since i like to learn more and more.
https://privatebin.net/?b0d702c5fa1faf9a#C9jKuGomLt4SUKJmUVoYPNffnMvg1Le54JFppSg3t1kP
дизайн сайта Lineage 2 – разработка сайта Lineage 2, создание сайта Л2
pharmacy prices
canadian online pharmacy no prescription
synthroid cost in canada
Промокод 1Win на сегодня, 2024 год – 937999. При регистрации с использованием этого кода активируется приветственный бонус в размере 500% до 75 000 рублей. Это специальное предложение от букмекера 1Win позволяет новым игрокам получить дополнительные привилегии и бонусы.
1Win – это платформа, которая радует своих пользователей разнообразными акциями. В 2024 году они предлагают следующие привлекательные бонусы для новичков:
Бездепозитные бонусы: Получите бонусы без необходимости внесения депозита.
Фриспины: Бесплатные вращения на слотах.
Фрибет бонусы: Возможность сделать бесплатные ставки.
Кэшбэк: Возврат части потерянных средств.
Промокод 937999 следует ввести при регистрации, чтобы получить максимальный бонус. Не упустите шанс увеличить свой баланс и наслаждаться игрой на 1Win!
1win 1 вин промокод используйте промокод 937999, чтобы получить максимальный бонус в размере 500% до 75 000 рублей. Этот код активирует приветственный бонус, который будет зачислен на два бонусных счета одновременно: на счета “Ставки” и “Казино”.
Важно учесть следующие особенности и предостережения при использовании промокода:
Различные поводы: Промокоды в 1Win выдаются по разным поводам, таким как акции, специальные события или дни рождения клиентов.
Активация и доступ к бонусам: После активации промокода при регистрации бонусные средства станут доступны после входа в ваш профиль. Личные промокоды требуют вашего согласия на участие в предложении.
Конвертация в реальные деньги: Бонусы будут зачислены на ваш бонусный счет с указанием доступной суммы в личном кабинете. При выполнении условий использования бонусов вы сможете конвертировать их в реальные деньги, которые дополнят ваш выигрыш.
Будьте бдительны: При поиске промокодов обращайте внимание на источник информации. Некоторые мошенники предлагают “бесплатные” промокоды с целью получить ваши личные данные. Регистрируйтесь и вводите информацию только на официальном сайте 1Win.
разработка сайта dota2 опен кейс – WoW website development, разработка сайта вов
I got this web page from my buddy who told me on the topic of this web page and now this time I am browsing this web page and reading very informative articles at this time.
https://controlc.com/d2be68f5
создание сайта WoW – создание сайта Л2, case opening website templates
Website design Lineage 2 game server – разработка сайта csgo опен кейс, создание сайта Lineage 2
canadianpharmacyworld
шаблон сайта L2 – open case website template, open case website development
Find the latest technology news and expert tech product reviews. Learn about the latest gadgets and consumer tech products for entertainment, gaming, lifestyle and more. https://axget.com/
Easier WWW is a leading technology site that is dedicated to produce great how-to, tips and tricks and cool software review. https://easierwww.com/
Testosil is a natural polyherbal testosterone booster designed to help men increase their testosterone levels safely and effectively. https://testosil-web.com/
FitSpresso is a natural dietary supplement designed to help with weight loss and improve overall health. It contains ingredients that have been studied clinically, which work together to promote healthy fat burning and enhance your metabolism! https://fitspresso-web.com/
Sugar Defender is a natural supplement that helps control blood sugar levels, lower the risk of diabetes, improve heart health, and boost energy. https://sugardefender-web.com/
ZenCortex Research’s contains only the natural ingredients that are effective in supporting incredible hearing naturally.A unique team of health and industry professionals dedicated to unlocking the secrets of happier living through a healthier body. https://zencortex-try.com/
Serolean, a revolutionary weight loss supplement, zeroes in on serotonin—the key neurotransmitter governing mood, appetite, and fat storage. https://serolean-web.com/
over the counter synthroid
Tonic Greens is a ready-made greens shake designed to support the entire body and wellness of the mind. It is filled with over 50 individual vitamins https://tonicgreens-try.com/
MenoPhix is a menopause relief supplement featuring a blend of plant extracts to target the root cause of menopause symptoms. https://menophix-web.com/
Support the health of your ears with 100% natural ingredients, finally being able to enjoy your favorite songs and movies https://quietumplus-try.com/
Peak BioBoost is a revolutionary dietary supplement that leverages the power of nature to support and improve your digestive system. https://peakbioboost-web.com/
GutOptim is a digestive health supplement designed to support your gut and stomach. It restore balance in gut flora and reduce the symptoms of digestive disorders. https://gutoptim-try.com/
Burn Boost Powder™ is a proven weight loss powder drink that helps to lose weight and boosts the overall metabolism in the body. https://burnboost-web.com
ONLINE EXCLUSIVE OFFER! Only Available for purchase on the official website. Secure Your Package while stocks last https://prodentim-web.com
NanoDefense Pro utilizes a potent blend of meticulously chosen components aimed at enhancing the wellness of both your nails and skin. https://nanodefense-web.com/
online shopping pharmacy india
Лендинг-пейдж — это одностраничный сайт, предназначенный для рекламы и продажи товаров или услуг, а также для сбора контактных данных потенциальных клиентов. Вот несколько причин, почему лендинг-пейдж важен для бизнеса:
Увеличение узнаваемости компании. Лендинг-пейдж позволяет представить компанию и её продукты или услуги в выгодном свете, что способствует росту узнаваемости бренда.
Повышение продаж. Заказать лендинг можно здесь – 1landingpage.ru Одностраничные сайты позволяют сосредоточиться на конкретных предложениях и акциях, что повышает вероятность совершения покупки.
Оптимизация SEO-показателей. Лендинг-пейдж создаются с учётом ключевых слов и фраз, что улучшает позиции сайта в результатах поиска и привлекает больше целевых посетителей.
Привлечение новой аудитории. Одностраничные сайты могут использоваться для продвижения новых продуктов или услуг, а также для привлечения внимания к определённым кампаниям или акциям.
Расширение клиентской базы. Лендинг-пейдж собирают контактные данные потенциальных клиентов, что позволяет компании поддерживать связь с ними и предлагать дополнительные услуги или товары.
Простота генерации лидов. Лендинг-пейдж предоставляют краткую и понятную информацию о продуктах или услугах, что облегчает процесс принятия решения для потенциальных клиентов.
Сбор персональных данных. Лендинг-пейдж позволяют собирать информацию о потенциальных клиентах, такую как email-адрес, имя и контактные данные, что помогает компании лучше понимать свою аудиторию и предоставлять более персонализированные услуги.
Улучшение поискового трафика. Лендинг-пейдж создаются с учётом определённых поисковых запросов, что позволяет привлекать больше целевых посетителей на сайт.
Эффективное продвижение новой продукции. Лендинг-пейдж можно использовать для продвижения новых товаров или услуг, что позволяет привлечь внимание потенциальных клиентов и стимулировать их к покупке.
Лёгкий процесс принятия решений. Лендинг-пейдж содержат только самую необходимую информацию, что упрощает процесс принятия решения для потенциальных клиентов.
В целом, лендинг-пейдж являются мощным инструментом для продвижения бизнеса, увеличения продаж и привлечения новых клиентов.
заказать лендинг пейдж
buy cheap lisinopril 40 mg no prescription
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
1win ввести промокод 1 win: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
tadalafil 60 mg for sale
Бонусы и Акции 1Win 2024: Ваш Путь к Успеху
Ищете способ максимизировать свои выигрыши? Букмекерская контора 1Win предлагает невероятный бонус код 937999, который открывает дверь к миру беспрецедентных возможностей. С этим промокодом новые клиенты могут получить денежный бонус в размере 500% до 200 000 рублей на первые четыре депозита. Это ваш шанс начать с большого и продолжать выигрывать!
1Win: не просто букмекерская контора, а мир, где каждый может стать победителем. Ставки на спорт, онлайн-казино, розыгрыши и турниры — все это доступно в одном месте, где более 1000 вариантов ставок ждут вас.
Как использовать промокод на 1win на первый?
Процесс активации промокода 937999 прост и понятен:
Переход на сайт: Используйте зеркало или VPN-сервис для доступа к официальному сайту 1Win.
Регистрация: Нажмите “Зарегистрироваться” и заполните необходимые данные. Выберите удобный способ регистрации — через социальные сети или электронную почту.
Активация промокода: Введите 937999 в специальное поле промокода и завершите регистрацию.
После этих шагов вы станете полноправным участником игрового сообщества 1Win и сможете воспользоваться всеми преимуществами промокода.
zithromax capsules
lisinopril 30 mg cost
metformin buy online india
В поисках идеального промокода для ставок в онлайн-казино? 1Win предлагает уникальный код 937999, который не только увеличивает шансы на крупный выигрыш, но и делает игровой процесс еще более захватывающим. Вот ваше руководство по выбору и использованию промокода на 2024 год.
Преимущества использования промокода 1Win
Использование промокода 937999 промокод на 1вин открывает перед вами двери в мир больших возможностей:
Увеличение начального капитала: После активации промокода и выполнения условий отыгрыша, ваш первоначальный депозит может увеличиться до 500%, достигая суммы в 75 000 рублей.
Минимизация рисков: Некоторые промокоды позволяют застраховать вашу первую ставку, снижая потенциальные потери.
Кешбэк: Получайте обратно часть потраченных средств, что делает каждую игру менее рискованной.
Эксклюзивные розыгрыши: Промокод открывает доступ к специальным акциям и розыгрышам, где можно выиграть значительные призы.
Как выбрать промокод?
Выбор промокода – это не просто вопрос личных предпочтений, но и стратегическое решение. Вот несколько критериев, которые помогут вам сделать правильный выбор:
Срок действия: Убедитесь, что промокод актуален. Для 937999 срок действия истекает 31 декабря 2024 года.
Условия отыгрыша: Внимательно изучите условия, при которых вы сможете использовать бонусные средства.
Размер бонуса: Выбирайте промокоды, которые предлагают максимальную выгоду от вашего депозита.
Дополнительные возможности: Ищите промокоды, которые предоставляют дополнительные преимущества, такие как фрибеты или кешбэк.
Как использовать промокод?
Чтобы активировать промокод 937999 в 1Win, выполните следующие шаги:
Перейдите на сайт 1Win и начните процесс регистрации.
Заполните все необходимые поля в анкете.
Введите промокод 937999 в соответствующее поле.
Завершите регистрацию и внесите первый депозит.
Помните, что использование промокода – это отличный способ усилить ваш игровой опыт и увеличить шансы на успех. Выбирайте мудро и пусть удача всегда будет на вашей стороне!
FlowForce Max is an innovative, natural and effective way to address your prostate problems, while addressing your energy, libido, and vitality. https://flowforcemax-web.com/
CLINICALLY PROVEN* To Increase Semen Volume And Intensity https://semenax-try.com/
DuoTrim is an innovative weight loss supplement that utilizes the power of natural plants and nutrients to create CSM bacteria https://duotrim-us.com/
BioFit is a Nutritional Supplement That Uses Probiotics To Help You Lose Weight https://biofit-web.com/
kraken darknet – kraken зеркало, kraken сайт
online pharmacy
Dentitox Pro is a liquid dietary solution created as a serum to support healthy gums and teeth. Dentitox Pro formula is made in the best natural way with unique, powerful botanical ingredients that can support healthy teeth. https://dentitox-us.com/
Denver Cleaning Choice is a woman owned local business with more than 20 years experience in commercial cleaning services garage floor cleaning service
Sugar Balance is an ultra-potent blood sugar supplement that you can use to help control glucose levels, melt away fat and improve your overall health. https://sugarbalance-us.com/
Denver Cleaning Choice is a woman owned local business with more than 20 years experience in commercial cleaning services small office cleaning service
GlucoFlush is an advanced formula specially designed for pancreas support that will let you promote healthy weight by effectively maintaining the blood sugar level and cleansing and strengthening your gut. https://glucoflush-us.com/
PureLumin Essence is a meticulously-crafted natural formula designed to help women improve the appearance of age spots. https://pureluminessence-web.com/
В нашем обществе, где диплом является началом удачной карьеры в любой сфере, многие стараются найти максимально простой путь получения образования. Факт наличия официального документа сложно переоценить. Ведь именно диплом открывает дверь перед людьми, желающими начать профессиональную деятельность или продолжить обучение в университете.
В данном контексте мы предлагаем очень быстро получить этот важный документ. Вы имеете возможность заказать диплом, что является отличным решением для человека, который не смог завершить образование или потерял документ. дипломы выпускаются аккуратно, с максимальным вниманием к мельчайшим деталям, чтобы в результате получился 100% оригинальный документ.
Преимущества такого подхода состоят не только в том, что можно оперативно получить диплом. Весь процесс организовывается удобно, с нашей поддержкой. Начав от выбора требуемого образца диплома до консультации по заполнению персональной информации и доставки по России — все будет находиться под абсолютным контролем квалифицированных мастеров.
В итоге, для всех, кто ищет максимально быстрый способ получения необходимого документа, наша компания готова предложить отличное решение. Приобрести диплом – значит избежать долгого процесса обучения и сразу переходить к достижению личных целей, будь то поступление в университет или старт удачной карьеры.
http://www.diploman-russia.com
Alpha Tonic is a powder-based supplement that uses multiple natural herbs and essential vitamins and minerals to help optimize your body’s natural testosterone levels. https://alphatonic-web.com
Vivo Tonic is a remarkable blood sugar support nutritional supplement that offers a wide range of benefits. https://vivotonic-web.com/
112 mg synthroid
Hello, all the time i used to check blog posts here in the early hours in the break of day, for the reason that i enjoy to gain knowledge of more and more.
diploman-russiyans.com
pharmacy without prescription
prednisone 20mg tab price
сайт мега даркнет – мега площадка, mega купить
Nervogen Pro is an effective dietary supplement designed to help patients with neuropathic pain. When you combine exotic herbs, spices, and other organic substances, your immune system will be strengthened. https://nervogenpro-web.com/
top article price earnings ratio formula
Progenifix is designed to help maximize weight loss results using a mixture of natural, science-backed ingredients. The formula also has secondary benefits, including promoting overall wellness and vitality and assisting your immune system. https://progenifix-web.com/
pharmacy prices
mega darknet – mega market, мега ссылка
Find Out More Rufus download
AquaPeace is an all-natural nutritional formula that uses a proprietary and potent blend of ingredients and nutrients to improve overall ear and hearing health and alleviate the symptoms of tinnitus. https://aquapeace-web.com
click this site price earnings ratio formula
FoliPrime is a simple serum containing a blend of vitamins designed to boost hair health. FoliPrime has 100 percent natural substances that enhance and supplement the vitamins in the scalp to promote hair growth. https://foliprime-web.com/
generic synthroid without prescription
Gut Vita™ is a daily supplement that helps consumers to improve the balance in their gut microbiome, which supports the health of their immune system. It supports healthy digestion, even for consumers who have maintained an unhealthy diet for a long time. https://gutvita-us.com/
Купить диплом быстро и качественно
купить диплом Вуза https://diplom-msk.ru .
Neuro-Thrive is a brain health supplement that claims to promote good memory and thinking skills and better quality sleep. This nootropic supplement achieves its cause with its potent blend of natural compounds and extracts that are proven to be effective in sharpening mental acuity. https://neurothrive-web.com/
Fast Lean Pro is a herbal supplement that tricks your brain into imagining that you’re fasting and helps you maintain a healthy weight no matter when or what you eat. It offers a novel approach to reducing fat accumulation and promoting long-term weight management. https://fastleanpro-web.com/
lisinopril in india
valtrex 500 mg tablets
zithromax cost in mexico
where to get tadalafil without a prescription
check this Obs download
Erectin is a clinically-proven dietary supplement designed to enhance male https://erectin-web.com/
100% Natural Formula Expressly Designed to Help Control Blood Sugar Levels, Improve Insulin Response And Support Overall Health https://glucotrusttry.com/
foreign online pharmacy
metformin 2018
synthroid 37.5 mg
PowerBite stands as an innovative dental candy, dedicated to nurturing healthy teeth and gums. Infused with a potent formula, it champions the cause of a robust and radiant smile. Crafted meticulously https://powerbite-web.com/
Protoflow is a prostate health supplement featuring a blend of plant extracts, vitamins, minerals, fruit extracts, and more. https://protoflow-web.com/
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
промокоды на 1win 2024 на пополнение: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
На сегодняшний день, когда диплом – это начало удачной карьеры в любом направлении, многие ищут максимально быстрый путь получения качественного образования. Факт наличия официального документа сложно переоценить. Ведь диплом открывает двери перед любым человеком, желающим начать профессиональную деятельность или учиться в университете.
В данном контексте мы предлагаем максимально быстро получить этот необходимый документ. Вы можете заказать диплом старого или нового образца, что становится отличным решением для человека, который не смог завершить образование, утратил документ или желает исправить плохие оценки. диплом изготавливается с особой аккуратностью, вниманием ко всем деталям, чтобы на выходе получился документ, 100% соответствующий оригиналу.
Преимущества такого решения заключаются не только в том, что вы сможете максимально быстро получить свой диплом. Процесс организован комфортно, с профессиональной поддержкой. От выбора подходящего образца диплома до грамотного заполнения персональной информации и доставки по стране — все под абсолютным контролем наших мастеров.
Для тех, кто ищет оперативный способ получения требуемого документа, наша услуга предлагает выгодное решение. Приобрести диплом – это значит избежать долгого процесса обучения и сразу перейти к личным целям, будь то поступление в университет или старт удачной карьеры.
diploman-russiyan.com
Boostaro is a dietary supplement designed specifically for men who suffer from health issues. https://boostaro-try.com/
pharmacies in canada that ship to the us
Unlock the incredible potential of Puravive! Supercharge your metabolism and incinerate calories like never before with our unique fusion of 8 exotic components. Bid farewell to those stubborn pounds and welcome a reinvigorated metabolism and boundless vitality. Grab your bottle today and seize this golden opportunity! https://puravive-web.com/
Zoracel is an extraordinary oral care product designed to promote healthy teeth and gums, provide long-lasting fresh breath, support immune health, and care for the ear, nose, and throat. https://zoracel-web.com
Cerebrozen is an excellent liquid ear health supplement purported to relieve tinnitus and improve mental sharpness, among other benefits. The Cerebrozen supplement is made from a combination of natural ingredients, and customers say they have seen results in their hearing, focus, and memory after taking one or two droppers of the liquid solution daily for a week. https://cerebrozen-try.com/
Входные двери – купить по выгодной цене с доставкой. 1433 модели в проверенных интернет-магазинах: популярные новинки и лидеры продаж https://market-dverey.com/
azithromycin buy online
valtrex cost australia
tadalafil daily use
online pharmacy india
valtrex 500 mg generic
canada cloud pharmacy
zestril 10 mg tablet
The human body can continue to live thanks to the correct functioning of certain systems. If even one of these systems does not work properly, it can cause problems in human life. https://calmlean-web.com/
best mail order pharmacy canada
Zeneara is marketed as an expert-formulated health supplement that can improve hearing and alleviate tinnitus, among other hearing issues. https://zeneara-web.com/
canadianpharmacyworld com
В нашем обществе, где диплом становится началом отличной карьеры в любом направлении, многие стараются найти максимально быстрый и простой путь получения качественного образования. Наличие официального документа об образовании трудно переоценить. Ведь диплом открывает дверь перед людьми, стремящимися начать профессиональную деятельность или учиться в каком-либо институте.
В данном контексте наша компания предлагает оперативно получить этот важный документ. Вы имеете возможность купить диплом старого или нового образца, и это является выгодным решением для всех, кто не смог завершить образование, потерял документ или желает исправить плохие оценки. диплом изготавливается с особой тщательностью, вниманием к мельчайшим деталям, чтобы на выходе получился продукт, максимально соответствующий оригиналу.
Плюсы данного подхода состоят не только в том, что вы сможете быстро получить диплом. Весь процесс организован комфортно и легко, с профессиональной поддержкой. Начав от выбора подходящего образца до грамотного заполнения личных данных и доставки по России — все будет находиться под полным контролем качественных специалистов.
Всем, кто ищет быстрый способ получения требуемого документа, наша компания предлагает отличное решение. Приобрести диплом – это значит избежать продолжительного процесса обучения и не теряя времени переходить к важным целям: к поступлению в университет или к началу удачной карьеры.
https://diploman-russiyan.com/
GlucoBerry is one of the biggest all-natural dietary and biggest scientific breakthrough formulas ever in the health industry today. This is all because of its amazing high-quality cutting-edge formula that helps treat high blood sugar levels very naturally and effectively. https://glucoberry-web.com/
buy generic valtrex cheap
Pineal XT is a revolutionary supplement that promotes proper pineal gland function and energy levels to support healthy body function. https://pinealxt-web.com/
tadalafil from canada
cheap viagra online canadian pharmacy
VidaCalm is an all-natural blend of herbs and plant extracts that treat tinnitus and help you live a peaceful life. https://vidacalm-web.com/
Are you tired of looking in the mirror and noticing saggy skin? Is saggy skin making you feel like you are trapped in a losing battle against aging? Do you still long for the days when your complexion radiated youth and confidence? https://refirmance-web.com/
legitimate online pharmacy usa
Gorilla Flow prostate is an all-natural dietary supplement for men which aims to decrease inflammation in the prostate to decrease common urinary tract issues such as frequent and night-time urination, leakage, or blocked urine stream. https://gorillaflow-web.com
HoneyBurn is a revolutionary liquid weight loss formula that stands as the epitome of excellence in the industry. https://honeyburn-web.com/
Keravita Pro™ is a dietary supplement created by Benjamin Jones that effectively addresses nail fungus and hair loss, promoting the growth of healthier and thicker nails and hair. The formula is designed to target the underlying causes of these health issues and provide comprehensive treatment. https://keravitapro-web.com
МОСКВА, 7 мая — РИА Новости. Правительство России, возглавляемое Михаилом Мишустиным, уйдет в отставку во вторник.
Сразу после инаугурации президента Владимира Путина нынешний кабинет министров сложит полномочия перед вступившим в должность главой государства.
Прогон по комментария
1Win Приветственный Бонус (2024): Полное Руководство
Промокод 937999 от 1Win — это ваш ключ к миру больших возможностей. С этим кодом, при первом депозите, вы можете получить бонус в размере 500% до 200 000 рублей. Это уникальное предложение позволяет новым клиентам значительно увеличить свой игровой бюджет и получить максимальное удовольствие от игры в спорте и казино.
Как работает приветственный бонус?
как действует промокод на 1win разделен на четыре этапа:
Первый депозит: Получите 200% от суммы депозита.
Второй депозит: Получите 150% от суммы второго депозита.
Третий депозит: Получите 100% от суммы.
Четвертый депозит: Получите 50% от суммы.
Максимальная сумма бонуса составляет 200,000 рублей, а максимальный бонус на один депозит — 50,000 рублей.
Как активировать промокод?
Чтобы активировать промокод 937999:
Зарегистрируйтесь на сайте 1Win.
Введите промокод при регистрации или дайте согласие на участие в акции, если промокод был предоставлен лично.
Пополните счет и начните играть, используя приветственный бонус.
Как отыграть бонус?
Чтобы отыграть бонусные средства:
Делайте ставки с коэффициентом от 3.
В случае выигрыша, 5% от бонусного счета переводится на ваш основной счет.
Пример:
Вы внесли 10 000 рублей и получили 20 000 рублей бонуса.
Сделали ставку с коэффициентом 3 и выиграли 30 000 рублей плюс 500 рублей бонуса.
Ваш счет теперь 30 500 рублей, а бонусный счет — 19 500 рублей.
Дополнительные бонусы и акции
1Win также предлагает различные акции и бонусы для любителей казино и экспресс-ставок. Следите за обновлениями на сайте, чтобы не пропустить самые выгодные предложения.
Обратите внимание: ставки с коэффициентом менее 3 не учитываются при отыгрыше бонуса.
Volca Burn is a weight loss supplement that uses a “red tingle hack” to help you rapidly lose weight without dieting or exercising. https://volcaburn-web.com/
Xitox’s foot pads contain a combination of powerful herbs that help provide a soothing experience for your feet after a long day. https://xitox-web.com/
sildenafil vs viagra
Hydrossential is actually a skincare serum or you can say a skincare supplement created by Emma Smith to help women keep their skin looking beautiful and flawless. https://hydrossential-web.com/
canada pharmacy not requiring prescription
Carbofix is the revolutionary dietary formula that promises to activate weight loss without all the extra hard work. https://carbofix-try.com
В поисках идеального промокода для ставок в онлайн-казино? 1Win предлагает уникальный код 937999, который не только увеличивает шансы на крупный выигрыш, но и делает игровой процесс еще более захватывающим. Вот ваше руководство по выбору и использованию промокода на 2024 год.
Преимущества использования промокода 1Win
Использование промокода 937999 как использовать промокод на 1win открывает перед вами двери в мир больших возможностей:
Увеличение начального капитала: После активации промокода и выполнения условий отыгрыша, ваш первоначальный депозит может увеличиться до 500%, достигая суммы в 75 000 рублей.
Минимизация рисков: Некоторые промокоды позволяют застраховать вашу первую ставку, снижая потенциальные потери.
Кешбэк: Получайте обратно часть потраченных средств, что делает каждую игру менее рискованной.
Эксклюзивные розыгрыши: Промокод открывает доступ к специальным акциям и розыгрышам, где можно выиграть значительные призы.
Как выбрать промокод?
Выбор промокода – это не просто вопрос личных предпочтений, но и стратегическое решение. Вот несколько критериев, которые помогут вам сделать правильный выбор:
Срок действия: Убедитесь, что промокод актуален. Для 937999 срок действия истекает 31 декабря 2024 года.
Условия отыгрыша: Внимательно изучите условия, при которых вы сможете использовать бонусные средства.
Размер бонуса: Выбирайте промокоды, которые предлагают максимальную выгоду от вашего депозита.
Дополнительные возможности: Ищите промокоды, которые предоставляют дополнительные преимущества, такие как фрибеты или кешбэк.
Как использовать промокод?
Чтобы активировать промокод 937999 в 1Win, выполните следующие шаги:
Перейдите на сайт 1Win и начните процесс регистрации.
Заполните все необходимые поля в анкете.
Введите промокод 937999 в соответствующее поле.
Завершите регистрацию и внесите первый депозит.
Помните, что использование промокода – это отличный способ усилить ваш игровой опыт и увеличить шансы на успех. Выбирайте мудро и пусть удача всегда будет на вашей стороне!
Reliver Pro is a dietary supplement formulated with a blend of natural ingredients aimed at supporting liver health
prescription free canadian pharmacy
Abdomax is a nutritional supplement using an 8-second Nordic cleanse to eliminate gut issues, support gut health, and optimize pepsinogen levels. https://abdomax-web.com
https://market-dverey.com/
rx lisinopril 10mg
1Win Приветственный Бонус (2024): Полное Руководство
Промокод 937999 от 1Win — это ваш ключ к миру больших возможностей. С этим кодом, при первом депозите, вы можете получить бонус в размере 500% до 200 000 рублей. Это уникальное предложение позволяет новым клиентам значительно увеличить свой игровой бюджет и получить максимальное удовольствие от игры в спорте и казино.
Как работает приветственный бонус?
промокод при регистрации 1win разделен на четыре этапа:
Первый депозит: Получите 200% от суммы депозита.
Второй депозит: Получите 150% от суммы второго депозита.
Третий депозит: Получите 100% от суммы.
Четвертый депозит: Получите 50% от суммы.
Максимальная сумма бонуса составляет 200,000 рублей, а максимальный бонус на один депозит — 50,000 рублей.
Как активировать промокод?
Чтобы активировать промокод 937999:
Зарегистрируйтесь на сайте 1Win.
Введите промокод при регистрации или дайте согласие на участие в акции, если промокод был предоставлен лично.
Пополните счет и начните играть, используя приветственный бонус.
Как отыграть бонус?
Чтобы отыграть бонусные средства:
Делайте ставки с коэффициентом от 3.
В случае выигрыша, 5% от бонусного счета переводится на ваш основной счет.
Пример:
Вы внесли 10 000 рублей и получили 20 000 рублей бонуса.
Сделали ставку с коэффициентом 3 и выиграли 30 000 рублей плюс 500 рублей бонуса.
Ваш счет теперь 30 500 рублей, а бонусный счет — 19 500 рублей.
Дополнительные бонусы и акции
1Win также предлагает различные акции и бонусы для любителей казино и экспресс-ставок. Следите за обновлениями на сайте, чтобы не пропустить самые выгодные предложения.
Обратите внимание: ставки с коэффициентом менее 3 не учитываются при отыгрыше бонуса.
Arctic blast is a powerful formula packed with natural ingredients and can treat pain effectively if you’re struggling with chronic pain. You can say goodbye to muscle cramps with this natural pain reliever in less than a minute. It helps with arthritic pain, blood circulation, and joint pain. It gives long-lasting effects that replace the need to go to surgery. https://arcticblast-web.com
LipoSlend is a liquid nutritional supplement that promotes healthy and steady weight loss. https://liposlend-web.com/
valtrex 500mg price in india
В нашем мире, где диплом является началом удачной карьеры в любом направлении, многие ищут максимально быстрый и простой путь получения образования. Факт наличия документа об образовании сложно переоценить. Ведь именно он открывает двери перед всеми, кто стремится вступить в сообщество профессионалов или продолжить обучение в высшем учебном заведении.
Мы предлагаем максимально быстро получить этот необходимый документ. Вы можете заказать диплом, и это является выгодным решением для всех, кто не смог закончить обучение, потерял документ или желает исправить плохие оценки. диплом изготавливается с особой аккуратностью, вниманием к мельчайшим деталям, чтобы в результате получился продукт, полностью соответствующий оригиналу.
Преимущества подобного подхода заключаются не только в том, что вы максимально быстро получите диплом. Процесс организовывается удобно, с нашей поддержкой. От выбора нужного образца документа до грамотного заполнения персональных данных и доставки в любое место страны — все находится под абсолютным контролем качественных специалистов.
Всем, кто пытается найти максимально быстрый способ получения требуемого документа, наша услуга предлагает выгодное решение. Приобрести диплом – это значит избежать длительного процесса обучения и не теряя времени переходить к достижению собственных целей, будь то поступление в университет или старт успешной карьеры.
diplomanc-russia24.com
synthroid 62.5 mg
canadian pharmacy coupon
prednisone 10mg for sale
generic valtrex cost
valtrex medication price
Simply wish to say your article is as astonishing. The clarity to your publish is just great and i can assume you are a professional in this subject. Fine together with your permission allow me to take hold of your RSS feed to stay up to date with coming near near post. Thanks a million and please carry on the rewarding work.
http://www.diplomanc-russia24.com
tadalafil 5mg canada
buy synthroid 200 mcg
Промокод 1xbet на сегодня. Промокод на 2024-2024. На официальном сайте букмекерской конторы 1xbet появилась опция, которая позволяет “бесплатно” ознакомиться с функционалом сайта и при удачном стечении обстоятельств еще и выиграть некую сумму денежных средств. Теперь это стало доступно по специальному промокоду 1хБет. Он дает возможность получить до 32500? (100$). Актуальные промокоды 1xbet на сегодня: 1XFREE777. Рабочие промокоды 1XBet в 2024 Все промокоды для 1хбет бесплатно: при регистрации, на ставку (купон), на бонус, на сегодня. 1xBet — одна из самых известных компаний в сфере беттинга. Свою популярность контора заработала во многом благодаря большому количеству специальных предложений. Так, к примеру, каждый пользователь может воспользоваться одним из действующих промокодов 1xBet на сегодня бесплатно. Ознакомиться с их полным перечнем можно в данной статье – более подробно в этом материале https://pulikalinkuralradio.com/wp-content/pages/1xbet_promokod_pri_registracii_12.html
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
промокод в 1win при регистрации: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
valtrex 500 mg generic
В современном мире, где диплом является началом отличной карьеры в любой области, многие пытаются найти максимально быстрый путь получения образования. Факт наличия официального документа трудно переоценить. Ведь диплом открывает двери перед каждым человеком, желающим вступить в сообщество профессионалов или продолжить обучение в ВУЗе.
Предлагаем быстро получить этот важный документ. Вы можете заказать диплом нового или старого образца, и это является отличным решением для всех, кто не смог закончить обучение или утратил документ. диплом изготавливается с особой аккуратностью, вниманием ко всем элементам, чтобы в результате получился документ, полностью соответствующий оригиналу.
Преимущество данного решения заключается не только в том, что можно максимально быстро получить свой диплом. Процесс организован просто и легко, с профессиональной поддержкой. От выбора подходящего образца документа до точного заполнения личных данных и доставки в любой регион России — все будет находиться под абсолютным контролем наших мастеров.
Для тех, кто ищет оперативный способ получения требуемого документа, наша услуга предлагает выгодное решение. Приобрести диплом – значит избежать долгого процесса обучения и не теряя времени переходить к достижению собственных целей: к поступлению в ВУЗ или к началу успешной карьеры.
http://diplomvam.ru
where can i get metformin without prescription
valtrex 2
В нашем мире, где диплом – это начало отличной карьеры в любой сфере, многие ищут максимально простой путь получения образования. Наличие официального документа переоценить невозможно. Ведь именно он открывает дверь перед любым человеком, который хочет вступить в сообщество профессионалов или продолжить обучение в ВУЗе.
Наша компания предлагает очень быстро получить любой необходимый документ. Вы можете купить диплом старого или нового образца, что будет удачным решением для всех, кто не смог завершить образование или потерял документ. Любой диплом изготавливается с особой тщательностью, вниманием к мельчайшим элементам. На выходе вы получите 100% оригинальный документ.
Плюсы подобного решения состоят не только в том, что вы максимально быстро получите диплом. Весь процесс организован удобно, с нашей поддержкой. Начиная от выбора необходимого образца документа до правильного заполнения личной информации и доставки по стране — все под полным контролем наших специалистов.
Всем, кто хочет найти быстрый способ получения требуемого документа, наша компания готова предложить отличное решение. Купить диплом – это значит избежать долгого процесса обучения и сразу перейти к своим целям: к поступлению в университет или к началу успешной карьеры.
http://diplom-net.ru
generic for valtrex
synthroid 112
my site https://kombonovaya2.com/
safe canadian pharmacy
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
как вести промокод на 1win: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
ProstaBiome is a carefully crafted dietary supplement aimed at promoting prostate health. Bid farewell to restless nights and discomfort with ProstaBiome precise strategy for addressing prostate concerns. https://prostabiome-web.com/
Nice post. I learn something new and challenging on sites I stumbleupon everyday. It’s always useful to read through articles from other authors and use a little something from their websites.
https://gofilm.cc/
PotentStream is designed to address prostate health by targeting the toxic, hard water minerals that can create a dangerous buildup inside your urinary system It’s the only dropper that contains nine powerful natural ingredients that work in perfect synergy to keep your prostate healthy and mineral-free well into old age. https://potentstream-web.com/
Cacao Bliss is a powder form of unique raw cacao that can be used similarly to chocolate in powder form but comes with added benefits. It is designed to provide a rich and satisfying experience while delivering numerous health benefits. https://cacaobliss-web.com/
Бонусы и Акции 1Win 2024: Ваш Путь к Успеху
Ищете способ максимизировать свои выигрыши? Букмекерская контора 1Win предлагает невероятный бонус код 937999, который открывает дверь к миру беспрецедентных возможностей. С этим промокодом новые клиенты могут получить денежный бонус в размере 500% до 200 000 рублей на первые четыре депозита. Это ваш шанс начать с большого и продолжать выигрывать!
1Win: не просто букмекерская контора, а мир, где каждый может стать победителем. Ставки на спорт, онлайн-казино, розыгрыши и турниры — все это доступно в одном месте, где более 1000 вариантов ставок ждут вас.
Как использовать 1win регистрация промокод?
Процесс активации промокода 937999 прост и понятен:
Переход на сайт: Используйте зеркало или VPN-сервис для доступа к официальному сайту 1Win.
Регистрация: Нажмите “Зарегистрироваться” и заполните необходимые данные. Выберите удобный способ регистрации — через социальные сети или электронную почту.
Активация промокода: Введите 937999 в специальное поле промокода и завершите регистрацию.
После этих шагов вы станете полноправным участником игрового сообщества 1Win и сможете воспользоваться всеми преимуществами промокода.
1Win Приветственный Бонус (2024): Полное Руководство
Промокод 937999 от 1Win — это ваш ключ к миру больших возможностей. С этим кодом, при первом депозите, вы можете получить бонус в размере 500% до 200 000 рублей. Это уникальное предложение позволяет новым клиентам значительно увеличить свой игровой бюджет и получить максимальное удовольствие от игры в спорте и казино.
Как работает приветственный бонус?
промокод для 1win при регистрации разделен на четыре этапа:
Первый депозит: Получите 200% от суммы депозита.
Второй депозит: Получите 150% от суммы второго депозита.
Третий депозит: Получите 100% от суммы.
Четвертый депозит: Получите 50% от суммы.
Максимальная сумма бонуса составляет 200,000 рублей, а максимальный бонус на один депозит — 50,000 рублей.
Как активировать промокод?
Чтобы активировать промокод 937999:
Зарегистрируйтесь на сайте 1Win.
Введите промокод при регистрации или дайте согласие на участие в акции, если промокод был предоставлен лично.
Пополните счет и начните играть, используя приветственный бонус.
Как отыграть бонус?
Чтобы отыграть бонусные средства:
Делайте ставки с коэффициентом от 3.
В случае выигрыша, 5% от бонусного счета переводится на ваш основной счет.
Пример:
Вы внесли 10 000 рублей и получили 20 000 рублей бонуса.
Сделали ставку с коэффициентом 3 и выиграли 30 000 рублей плюс 500 рублей бонуса.
Ваш счет теперь 30 500 рублей, а бонусный счет — 19 500 рублей.
Дополнительные бонусы и акции
1Win также предлагает различные акции и бонусы для любителей казино и экспресс-ставок. Следите за обновлениями на сайте, чтобы не пропустить самые выгодные предложения.
Обратите внимание: ставки с коэффициентом менее 3 не учитываются при отыгрыше бонуса.
order azithromycin online uk
Наши преподаватели и имеют богатый опыт обучения таким направлениям танца, как аргентинское танго, бачата, контемпорари, k-pop, Hight Heels, шафл. Обучаем танцу как детей, так и взрослых бальные танцы бабушкинская
valtrex 1 mg
Наши преподаватели и имеют богатый опыт обучения таким направлениям танца, как аргентинское танго, бачата, контемпорари, k-pop, Hight Heels, шафл. Обучаем танцу как детей, так и взрослых арабские танцы москва
can i buy azithromycin in mexico
Payments Latest provides in-depth journalism and insight into the most impactful news and trends shaping payments. https://paymentslatest.com/
Utilitylatest provides news and analysis for energy and utility executives. We cover topics like smart grid tech, clean energy, regulation, generation, demand response, solar, storage, transmission distribution, and more. https://utilitylatest.com
В нашем обществе, где диплом – это начало отличной карьеры в любой сфере, многие пытаются найти максимально быстрый путь получения образования. Факт наличия официального документа трудно переоценить. Ведь диплом открывает дверь перед каждым человеком, который желает вступить в профессиональное сообщество или учиться в любом ВУЗе.
Мы предлагаем оперативно получить этот необходимый документ. Вы сможете заказать диплом, и это будет выгодным решением для человека, который не смог завершить образование или утратил документ. диплом изготавливается с особой тщательностью, вниманием к мельчайшим деталям, чтобы на выходе получился документ, полностью соответствующий оригиналу.
Превосходство такого подхода заключается не только в том, что можно оперативно получить свой диплом. Процесс организован комфортно и легко, с нашей поддержкой. Начав от выбора подходящего образца до консультаций по заполнению персональной информации и доставки в любой регион России — все находится под абсолютным контролем опытных специалистов.
В результате, для всех, кто хочет найти оперативный способ получить необходимый документ, наша компания предлагает выгодное решение. Приобрести диплом – это значит избежать длительного обучения и не теряя времени перейти к достижению своих целей, будь то поступление в университет или старт трудовой карьеры.
vsediplomu.ru
canadian pharmacy no scripts
В современном мире, где диплом становится началом удачной карьеры в любом направлении, многие ищут максимально быстрый путь получения образования. Наличие документа об образовании переоценить невозможно. Ведь именно он открывает двери перед любым человеком, желающим начать трудовую деятельность или учиться в университете.
В данном контексте наша компания предлагает оперативно получить этот необходимый документ. Вы сможете приобрести диплом, и это будет удачным решением для человека, который не смог закончить образование, потерял документ или желает исправить плохие оценки. Все дипломы производятся с особой тщательностью, вниманием ко всем элементам, чтобы на выходе получился 100% оригинальный документ.
Превосходство такого подхода заключается не только в том, что можно быстро получить свой диплом. Весь процесс организовывается удобно и легко, с профессиональной поддержкой. Начиная от выбора необходимого образца диплома до консультации по заполнению персональной информации и доставки в любой регион России — все будет находиться под абсолютным контролем квалифицированных мастеров.
Для всех, кто ищет быстрый способ получить требуемый документ, наша компания предлагает отличное решение. Приобрести диплом – это значит избежать продолжительного обучения и сразу перейти к достижению собственных целей, будь то поступление в университет или начало трудовой карьеры.
http://diplomany.ru/
prednisone 4 tablets daily
pharmacy no prescription required
scshlj banking finance news – https://scshlj.com
9 da auto news – https://9-da.com/
metformin 50 mg tab
Cneche provides in-depth journalism and insight into the most impactful news and trends shaping the finance industry. https://cneche.com/
canadian pharmacy prices
how to get cialis without a prescription
reputable canadian pharmacy
1Win Приветственный Бонус (2024): Полное Руководство
Промокод 937999 от 1Win — это ваш ключ к миру больших возможностей. С этим кодом, при первом депозите, вы можете получить бонус в размере 500% до 200 000 рублей. Это уникальное предложение позволяет новым клиентам значительно увеличить свой игровой бюджет и получить максимальное удовольствие от игры в спорте и казино.
Как работает приветственный бонус?
промокоды 1вин разделен на четыре этапа:
Первый депозит: Получите 200% от суммы депозита.
Второй депозит: Получите 150% от суммы второго депозита.
Третий депозит: Получите 100% от суммы.
Четвертый депозит: Получите 50% от суммы.
Максимальная сумма бонуса составляет 200,000 рублей, а максимальный бонус на один депозит — 50,000 рублей.
Как активировать промокод?
Чтобы активировать промокод 937999:
Зарегистрируйтесь на сайте 1Win.
Введите промокод при регистрации или дайте согласие на участие в акции, если промокод был предоставлен лично.
Пополните счет и начните играть, используя приветственный бонус.
Как отыграть бонус?
Чтобы отыграть бонусные средства:
Делайте ставки с коэффициентом от 3.
В случае выигрыша, 5% от бонусного счета переводится на ваш основной счет.
Пример:
Вы внесли 10 000 рублей и получили 20 000 рублей бонуса.
Сделали ставку с коэффициентом 3 и выиграли 30 000 рублей плюс 500 рублей бонуса.
Ваш счет теперь 30 500 рублей, а бонусный счет — 19 500 рублей.
Дополнительные бонусы и акции
1Win также предлагает различные акции и бонусы для любителей казино и экспресс-ставок. Следите за обновлениями на сайте, чтобы не пропустить самые выгодные предложения.
Обратите внимание: ставки с коэффициентом менее 3 не учитываются при отыгрыше бонуса.
reddit canadian pharmacy
The simplest way to use Jaxx Lightweight Web Wallet Jaxxify jaxx fees
synthroid 0.5 mg
The simplest way to use Jaxx Lightweight Web Wallet Jaxxify jaxx liberty wallet address
На сегодняшний день, когда диплом становится началом успешной карьеры в любой области, многие пытаются найти максимально быстрый и простой путь получения образования. Важность наличия официального документа сложно переоценить. Ведь диплом открывает двери перед каждым человеком, который стремится начать трудовую деятельность или продолжить обучение в университете.
Предлагаем быстро получить этот важный документ. Вы можете приобрести диплом, и это будет отличным решением для всех, кто не смог закончить обучение или потерял документ. диплом изготавливается аккуратно, с максимальным вниманием к мельчайшим нюансам, чтобы на выходе получился полностью оригинальный документ.
Превосходство данного подхода заключается не только в том, что вы сможете оперативно получить свой диплом. Весь процесс организовывается комфортно, с нашей поддержкой. От выбора требуемого образца диплома до консультации по заполнению персональной информации и доставки по стране — все под полным контролем опытных мастеров.
Таким образом, для тех, кто пытается найти быстрый и простой способ получить требуемый документ, наша компания предлагает выгодное решение. Заказать диплом – это значит избежать долгого процесса обучения и не теряя времени переходить к важным целям, будь то поступление в ВУЗ или начало карьеры.
http://www.diplomexpress.ru
Такси Краснодар – Такси межгород Саратов, Трансфер Россошь
В нашем мире, где диплом становится началом успешной карьеры в любом направлении, многие пытаются найти максимально быстрый и простой путь получения образования. Факт наличия официального документа переоценить просто невозможно. Ведь диплом открывает дверь перед всеми, кто стремится вступить в сообщество профессионалов или продолжить обучение в любом институте.
В данном контексте мы предлагаем быстро получить любой необходимый документ. Вы имеете возможность заказать диплом нового или старого образца, что является отличным решением для человека, который не смог закончить обучение или потерял документ. диплом изготавливается с особой аккуратностью, вниманием к мельчайшим элементам, чтобы на выходе получился продукт, полностью соответствующий оригиналу.
Превосходство данного подхода заключается не только в том, что можно быстро получить свой диплом. Весь процесс организовывается комфортно, с профессиональной поддержкой. Начиная от выбора требуемого образца документа до грамотного заполнения персональных данных и доставки в любой регион страны — все будет находиться под абсолютным контролем наших мастеров.
В итоге, всем, кто пытается найти быстрый и простой способ получить необходимый документ, наша компания готова предложить выгодное решение. Купить диплом – значит избежать долгого процесса обучения и сразу переходить к важным целям, будь то поступление в ВУЗ или старт карьеры.
http://www.99diplomov.ru
cheapest pharmacy for prescription drugs
регистрация леон казино
официальный сайт леон казино
prednisone in uk
Эскорт Услуги Москвы – досуг для взрослых объявления, Эскорт Услуги Москвы
bitz casino
snservis.ru
Lasixiv provides news and analysis for IT executives. We cover big data, IT strategy, cloud computing, security, mobile technology, infrastructure, software and more. https://lasixiv.com
Thank you for sharing your info. I truly appreciate your efforts and I will be waiting for your next post thank you once again.
http://www.diplom07.ru
Бонусы и Акции 1Win 2024: Ваш Путь к Успеху
Ищете способ максимизировать свои выигрыши? Букмекерская контора 1Win предлагает невероятный бонус код 937999, который открывает дверь к миру беспрецедентных возможностей. С этим промокодом новые клиенты могут получить денежный бонус в размере 500% до 200 000 рублей на первые четыре депозита. Это ваш шанс начать с большого и продолжать выигрывать!
1Win: не просто букмекерская контора, а мир, где каждый может стать победителем. Ставки на спорт, онлайн-казино, розыгрыши и турниры — все это доступно в одном месте, где более 1000 вариантов ставок ждут вас.
Как использовать 1win промокод на фрибет без депозита?
Процесс активации промокода 937999 прост и понятен:
Переход на сайт: Используйте зеркало или VPN-сервис для доступа к официальному сайту 1Win.
Регистрация: Нажмите “Зарегистрироваться” и заполните необходимые данные. Выберите удобный способ регистрации — через социальные сети или электронную почту.
Активация промокода: Введите 937999 в специальное поле промокода и завершите регистрацию.
После этих шагов вы станете полноправным участником игрового сообщества 1Win и сможете воспользоваться всеми преимуществами промокода.
zestoretic 20 mg
1Win Приветственный Бонус (2024): Полное Руководство
Промокод 937999 от 1Win — это ваш ключ к миру больших возможностей. С этим кодом, при первом депозите, вы можете получить бонус в размере 500% до 200 000 рублей. Это уникальное предложение позволяет новым клиентам значительно увеличить свой игровой бюджет и получить максимальное удовольствие от игры в спорте и казино.
Как работает приветственный бонус?
промокод на 1win разделен на четыре этапа:
Первый депозит: Получите 200% от суммы депозита.
Второй депозит: Получите 150% от суммы второго депозита.
Третий депозит: Получите 100% от суммы.
Четвертый депозит: Получите 50% от суммы.
Максимальная сумма бонуса составляет 200,000 рублей, а максимальный бонус на один депозит — 50,000 рублей.
Как активировать промокод?
Чтобы активировать промокод 937999:
Зарегистрируйтесь на сайте 1Win.
Введите промокод при регистрации или дайте согласие на участие в акции, если промокод был предоставлен лично.
Пополните счет и начните играть, используя приветственный бонус.
Как отыграть бонус?
Чтобы отыграть бонусные средства:
Делайте ставки с коэффициентом от 3.
В случае выигрыша, 5% от бонусного счета переводится на ваш основной счет.
Пример:
Вы внесли 10 000 рублей и получили 20 000 рублей бонуса.
Сделали ставку с коэффициентом 3 и выиграли 30 000 рублей плюс 500 рублей бонуса.
Ваш счет теперь 30 500 рублей, а бонусный счет — 19 500 рублей.
Дополнительные бонусы и акции
1Win также предлагает различные акции и бонусы для любителей казино и экспресс-ставок. Следите за обновлениями на сайте, чтобы не пропустить самые выгодные предложения.
Обратите внимание: ставки с коэффициентом менее 3 не учитываются при отыгрыше бонуса.
your pharmacy online
order tadalafil
1Win Приветственный Бонус (2024): Полное Руководство
Промокод 937999 от 1Win — это ваш ключ к миру больших возможностей. С этим кодом, при первом депозите, вы можете получить бонус в размере 500% до 200 000 рублей. Это уникальное предложение позволяет новым клиентам значительно увеличить свой игровой бюджет и получить максимальное удовольствие от игры в спорте и казино.
Как работает приветственный бонус?
1win промокоды на деньги разделен на четыре этапа:
Первый депозит: Получите 200% от суммы депозита.
Второй депозит: Получите 150% от суммы второго депозита.
Третий депозит: Получите 100% от суммы.
Четвертый депозит: Получите 50% от суммы.
Максимальная сумма бонуса составляет 200,000 рублей, а максимальный бонус на один депозит — 50,000 рублей.
Как активировать промокод?
Чтобы активировать промокод 937999:
Зарегистрируйтесь на сайте 1Win.
Введите промокод при регистрации или дайте согласие на участие в акции, если промокод был предоставлен лично.
Пополните счет и начните играть, используя приветственный бонус.
Как отыграть бонус?
Чтобы отыграть бонусные средства:
Делайте ставки с коэффициентом от 3.
В случае выигрыша, 5% от бонусного счета переводится на ваш основной счет.
Пример:
Вы внесли 10 000 рублей и получили 20 000 рублей бонуса.
Сделали ставку с коэффициентом 3 и выиграли 30 000 рублей плюс 500 рублей бонуса.
Ваш счет теперь 30 500 рублей, а бонусный счет — 19 500 рублей.
Дополнительные бонусы и акции
1Win также предлагает различные акции и бонусы для любителей казино и экспресс-ставок. Следите за обновлениями на сайте, чтобы не пропустить самые выгодные предложения.
Обратите внимание: ставки с коэффициентом менее 3 не учитываются при отыгрыше бонуса.
pharmacy order online
buy synthroid without prescription
zithromax 4 pills
prinzide zestoretic
lisinopril 12.5
На сегодняшний день, когда диплом является началом успешной карьеры в любом направлении, многие пытаются найти максимально быстрый и простой путь получения качественного образования. Факт наличия официального документа сложно переоценить. Ведь именно он открывает дверь перед каждым человеком, который хочет начать профессиональную деятельность или учиться в высшем учебном заведении.
Мы предлагаем очень быстро получить этот необходимый документ. Вы имеете возможность заказать диплом нового или старого образца, что является отличным решением для человека, который не смог закончить обучение или потерял документ. диплом изготавливается аккуратно, с особым вниманием ко всем нюансам. В итоге вы сможете получить продукт, 100% соответствующий оригиналу.
Преимущества данного подхода состоят не только в том, что вы оперативно получите диплом. Весь процесс организовывается удобно, с профессиональной поддержкой. От выбора нужного образца до точного заполнения личных данных и доставки в любое место России — все под абсолютным контролем квалифицированных мастеров.
Всем, кто пытается найти быстрый и простой способ получения требуемого документа, наша компания предлагает выгодное решение. Приобрести диплом – значит избежать долгого процесса обучения и не теряя времени перейти к своим целям: к поступлению в ВУЗ или к началу успешной карьеры.
http://diplom-msk.ru
В современном мире, где диплом становится началом удачной карьеры в любом направлении, многие ищут максимально быстрый и простой путь получения качественного образования. Важность наличия документа об образовании переоценить просто невозможно. Ведь именно диплом открывает дверь перед каждым человеком, желающим начать профессиональную деятельность или продолжить обучение в ВУЗе.
Наша компания предлагает очень быстро получить этот необходимый документ. Вы имеете возможность купить диплом, и это становится отличным решением для человека, который не смог завершить образование, потерял документ или хочет исправить свои оценки. диплом изготавливается аккуратно, с особым вниманием к мельчайшим нюансам. В итоге вы получите продукт, максимально соответствующий оригиналу.
Плюсы такого подхода заключаются не только в том, что вы быстро получите диплом. Процесс организован удобно, с профессиональной поддержкой. От выбора нужного образца до грамотного заполнения личной информации и доставки в любое место России — все под абсолютным контролем наших мастеров.
Таким образом, для тех, кто ищет максимально быстрый способ получить необходимый документ, наша услуга предлагает выгодное решение. Приобрести диплом – это значит избежать продолжительного обучения и не теряя времени перейти к личным целям, будь то поступление в ВУЗ или начало удачной карьеры.
http://www.diplom-gotovie.ru
can i buy prednisone over the counter
buy valtrex 1000 mg
В современном мире, где диплом – это начало успешной карьеры в любой сфере, многие ищут максимально простой путь получения качественного образования. Наличие документа об образовании сложно переоценить. Ведь именно диплом открывает дверь перед каждым человеком, который желает вступить в сообщество профессиональных специалистов или продолжить обучение в высшем учебном заведении.
В данном контексте мы предлагаем очень быстро получить любой необходимый документ. Вы сможете приобрести диплом, и это является удачным решением для человека, который не смог закончить обучение, утратил документ или хочет исправить плохие оценки. Каждый диплом изготавливается с особой тщательностью, вниманием к мельчайшим деталям, чтобы на выходе получился 100% оригинальный документ.
Превосходство данного подхода заключается не только в том, что вы максимально быстро получите свой диплом. Весь процесс организовывается комфортно, с нашей поддержкой. Начав от выбора требуемого образца документа до консультации по заполнению персональных данных и доставки по стране — все будет находиться под абсолютным контролем наших специалистов.
В результате, всем, кто хочет найти оперативный способ получения необходимого документа, наша компания предлагает отличное решение. Купить диплом – это значит избежать долгого обучения и сразу перейти к важным целям: к поступлению в университет или к началу удачной карьеры.
http://ab-diplom.ru
Wedstraunt has the latest news in the restaurant industry, covering topics like consumer trends, technology, marketing and branding, operations, mergers https://wedstraunt.com
9 metformin
synthroid cheapest prices
Междугородние такси Волгоград – Автобусы Стерлитамак, Междугородние перевозки Самара
девочки по вызову – досуг для взрослых знакомства Москва, анкеты девочек москвы
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
как в 1win ввести промокод: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
over the counter valtrex
azithromycin australia over the counter
generic cialis soft
pharmacy online australia free shipping
buy synthroid online cheap
Qcmpt provides in-depth journalism and insight into the news and trends impacting the customer experience space. https://qcmpt.com/
investigate this site https://debank.lu/2023/11/10/unlock-financial-freedom-in-the-digital-age-with-crypto-bulls-club/
i thought about this https://tronlink.at/2023/11/13/the-increasing-popularity-of-tron-in-the-cryptocurrency-market/
Hello! Do you know if they make any plugins to assist with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good results. If you know of any please share. Thanks!
http://server-attestats.com
top 10 online pharmacy in india
hop over to this website https://tronlink-app.org/2023/11/13/usdc-on-tron-revolutionizing-cross-border-transactions-and-interoperability-on-the-tron-blockchain/
Tvphc provides news and analysis for IT executives. We cover big data, IT strategy, cloud computing, security, mobile technology, infrastructure, software and more. https://tvphc.com
prinivil 20mg tabs
go now https://blur-nft-marketplace.org/2023/11/10/transforming-the-tech-industry-how-the-microsoft-ethereum-partnership-is-changing-the-game-for-nfts/
prinivil
РћРЅРё называли себя – РјСѓР¶ РЅР° час!
Он нашел, что он до невероятности изменился, но Вельчанинов знал, что он и не мог не измениться и что все это было совершенно естественно; господин Трусоцкий мог быть всем тем, чем был прежде, только при жизни жены, а теперь это была только часть целого, выпущенная вдруг на волю, то есть что-то удивительное и ни на что не похожее. » Он произнес слова сии голосом резким, и грубее, нежели как говорил обыкновенно; ибо господин философ от супружества и от любви имел какое-то отвращение, похожее на ненависть. Он употреблял адвоката ловкого, дорогого, известного и денег не жалел; но в нетерпении и от мнительности повадился заниматься делом и сам: читал и писал бумаги, которые сплошь браковал адвокат, бегал по присутственным местам, наводил справки и, вероятно, очень мешал всему; по крайней мере адвокат жаловался и гнал его на дачу. Рахманов недовольно поморщился, пожал насмешливо плечами и, отойдя к письменному столу, опустился в широкое кожаное кресло, на спинке которого был выжжен герб рода Рахмановых. Евгений Петрович Рахманов угрюмо шагал, заложив руки за спину, по мягкому ковру своего обширного, роскошно убранного кабинета. Слышал как-то он потом, уже несколько лет спустя, что там очутился Багаутов и пробыл целые пять лет.
РџСЂРё заказе «мужа РЅР° час» нужно понимать, что это РЅРµ СѓР·РєРёР№ специалист, РѕРЅ РЅРµ сделает какую-то сложную работу. РџСЂРё этом РЅРµ надо РЅРёРєРѕРіРѕ загружать СЃРІРѕРёРјРё проблемами чувствуя себя после этого обязанным. РџСЂРё вызове следует помнить, что «муж РЅР° час» – специалист РїРѕ мелким бытовым работам, выполняющий несложный ремонт или услугу. Заказывайте «мужа РЅР° час» уже сегодня. «Муж РЅР° час» удобен тем, что мастера можно вызвать РІ срочном РїРѕСЂСЏРґРєРµ – РІ этот день Рё даже час. Существует множество вариантов, как занять мужа РЅР° час. Лидер Услуг – это РњСѓР¶ РЅР° час недорого СЃ гарантией того, что РІС‹ обойдетесь без переплаты. Чем выделяется Лидер Услуг среди РґСЂСѓРіРёС… аналогичных сайтов, так это скоростью передачи вызова Рё оперативностью выполнения. Чем С…РѕСЂРѕС€ этот ресурс – РІСЃРµ исполнители РїСЂРѕС…РѕРґСЏС‚ проверку данных Рё предоставляют РІ обязательном РїРѕСЂСЏРґРєРµ документы, подтверждающие профильное образование, РґРѕРїСѓСЃРєРё, квалификацию. Lider Uslug призывает РЅРµ печалиться, если нет мужа или РѕРЅ уехал РІ командировку. Наконец, РѕРЅ решительно остановился Сѓ самого зеркала Рё высунул язык. 2. Предложите ему научиться РЅРѕРІРѕРјСѓ: посмотреть СѓСЂРѕРєРё РїРѕ готовке онлайн Рё приготовить обед, заняться рукоделием или начать изучать иностранный язык.
4. Предложите мужу убраться вместе РІ РґРѕРјРµ или РІ саду. Достойный выход РёР· положения – услуга РјСѓР¶ РЅР° час, предлагаемая сервисом Lider Uslug. Если предоставляемая услуга является более сложной или объемной, то ее цена может достигать 1000 СЂСѓР±. РІ час. Важно понимать, что занять мужа РЅР° час РЅРµ обязательно должно быть направлено РЅР° увлечения мужских интересов или занятий РІ социальных сетях. Мастера РЅР° час – как выбрать мужа РЅР° час РІ Воронеже? Всего Р·Р° РѕРґРёРЅ час можно решить СЃРІРѕРё проблемы, которые кажутся неразрешимыми. РњСѓР¶ РЅР° час недорого – это реально! Вызвать мастера РЅР° час РІ РњРѕСЃРєРІРµ – это надежно, СѓРґРѕР±РЅРѕ, просто Рё выгодно. Каждый вызов мужа РЅР° час контролируется менеджером, что дает возможность отслеживать качество выполненных работ. Доступные цены дают возможность вызвать исполнителя абсолютно всем жителям РіРѕСЂРѕРґР° Рё области. Подобная точность достигается Р·Р° счет того, что специалист РЅРµ зависит РѕС‚ РїСЂРѕР±РѕРє Рё ему РЅРµ нужно добираться СЃ РґСЂСѓРіРѕРіРѕ конца РіРѕСЂРѕРґР°. Р’СЃРµ быстро, надежно, безопасно. Р’СЃРµ РІРёРґС‹ бытовых услуг. Возможно, СЃРїРѕРєРѕР№РЅРѕ планировать СЃРІРѕРё дела, исполнитель подойдет или подъедет РІ СѓРґРѕР±РЅРѕРµ время.
Р’ случае необходимости исполнитель подойдет практически сразу. Организаций, желающих оказать москвичам бытовые услуги, появилось сегодня немало. РўС‹ права, – РїСЂРѕРіРѕРІРѕСЂРёР» РѕРЅ, поцеловал ту же СЂСѓРєСѓ вторично Рё добавил, – РЅРѕ знай, РђРІСЂРѕСЂР°, что ты сегодня самая противная, самая упрямая немка. РќРµ всегда же РІ самом деле страдать воспоминаниями; можно отдохнуть Рё погулять – РІ антрактах. РќРµ надо тратить деньги РЅР° инструменты, которые вам понадобятся раз РІ жизни, Рё откладывать ремонт РЅР° “потом”. Дамы подхватили его Рё РІ этот раз уже побежали, визжа Рё почти волоча Павла Павловича Р·Р° СЃРѕР±РѕСЋ. Волнение Павла Павловича возросло РґРѕ чрезвычайности. РћРЅР° откровенно так: «Давайте позабавимся, мальчики? РЇ ее позвал. РћРЅР° остановилась. РћРЅ злился даже РЅР° себя Р·Р° что-то. РћРЅ жадно его разглядывал Рё припоминал. РћРЅ был, РІРёРґРёРјРѕ, РЅРµ РІ РґСѓС…Рµ. Старший Федор РІСЃРµ так же ростовщичал Рё резал РєСѓРїРѕРЅС‹, выезжая днем РІ РіРѕСЂРѕРґ, РїРѕ делам. Р Р±СЊСЋСЃСЊ РѕР± заклад, РІС‹ теперь думаете: „Свинья же ты, что сам РЅР° СЂРѕРіР° СЃРІРѕРё указал“, С…Рµ-С…Рµ!
Go Here https://galxe-app.org/2023/11/19/transform-the-way-you-connect-with-your-community-through-galxes-innovative-telegram-and-page-visit-credentials/
Ellajon provides news and analysis for construction industry executives. We cover commercial and residential construction, focusing on topics like technology, design, regulation, legal issues and more. https://ellajon.com
i thought about this https://1inch-dex.com/2023/11/17/benefits-of-1inch-dex-for-liquidity-providers/
http://e-rubtsovsk.ru/city/novosti/v-mire/11760-avtomobilnye-nomera-bez-flaga-osobennosti-i-vidy.html
https://subscribe.ru/group/novosti-i-faktyi/18575429/
1Win Приветственный Бонус (2024): Полное Руководство
Промокод 937999 от 1Win — это ваш ключ к миру больших возможностей. С этим кодом, при первом депозите, вы можете получить бонус в размере 500% до 200 000 рублей. Это уникальное предложение позволяет новым клиентам значительно увеличить свой игровой бюджет и получить максимальное удовольствие от игры в спорте и казино.
Как работает приветственный бонус?
1win куда вводить промокод разделен на четыре этапа:
Первый депозит: Получите 200% от суммы депозита.
Второй депозит: Получите 150% от суммы второго депозита.
Третий депозит: Получите 100% от суммы.
Четвертый депозит: Получите 50% от суммы.
Максимальная сумма бонуса составляет 200,000 рублей, а максимальный бонус на один депозит — 50,000 рублей.
Как активировать промокод?
Чтобы активировать промокод 937999:
Зарегистрируйтесь на сайте 1Win.
Введите промокод при регистрации или дайте согласие на участие в акции, если промокод был предоставлен лично.
Пополните счет и начните играть, используя приветственный бонус.
Как отыграть бонус?
Чтобы отыграть бонусные средства:
Делайте ставки с коэффициентом от 3.
В случае выигрыша, 5% от бонусного счета переводится на ваш основной счет.
Пример:
Вы внесли 10 000 рублей и получили 20 000 рублей бонуса.
Сделали ставку с коэффициентом 3 и выиграли 30 000 рублей плюс 500 рублей бонуса.
Ваш счет теперь 30 500 рублей, а бонусный счет — 19 500 рублей.
Дополнительные бонусы и акции
1Win также предлагает различные акции и бонусы для любителей казино и экспресс-ставок. Следите за обновлениями на сайте, чтобы не пропустить самые выгодные предложения.
Обратите внимание: ставки с коэффициентом менее 3 не учитываются при отыгрыше бонуса.
synthroid 1mg
Grpduk provides news and analysis for human resource executives. We cover topics like recruiting, HR management, employee learning https://grpduk.com
azithromycin 500 mg tablet price
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
промокод для 1win при пополнении: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
Susibu provides in-depth journalism and insight into the news and trends impacting the hotel https://susibu.com/
Сегодня, когда диплом – это начало отличной карьеры в любом направлении, многие ищут максимально простой путь получения образования. Наличие официального документа об образовании трудно переоценить. Ведь диплом открывает дверь перед людьми, желающими вступить в сообщество профессионалов или продолжить обучение в каком-либо ВУЗе.
В данном контексте наша компания предлагает максимально быстро получить любой необходимый документ. Вы имеете возможность купить диплом, что становится отличным решением для человека, который не смог закончить обучение или утратил документ. Все дипломы выпускаются аккуратно, с максимальным вниманием ко всем нюансам, чтобы на выходе получился полностью оригинальный документ.
Превосходство подобного подхода заключается не только в том, что можно максимально быстро получить свой диплом. Процесс организовывается комфортно, с профессиональной поддержкой. Начиная от выбора требуемого образца до точного заполнения личной информации и доставки по стране — все под полным контролем наших специалистов.
В результате, для тех, кто хочет найти быстрый и простой способ получить необходимый документ, наша компания предлагает выгодное решение. Купить диплом – это значит избежать длительного обучения и не теряя времени перейти к достижению личных целей, будь то поступление в университет или начало карьеры.
https://russa24-attestats.com/
Бездепозитный Бонус 1Win 2024: Ваш Гид по Миру Игр
Казино 1Win в 2024 году предлагает своим игрокам невероятные возможности для увеличения выигрышей и улучшения игрового опыта. С промокодом 937999, игроки получают доступ к бездепозитным бонусам, которые открывают новые горизонты в мире азартных игр.
как в 1win ввести промокод: Что Вас Ждет?
Бездепозитные бонусы: Получите фриспины или фрибеты без необходимости пополнять счет.
Коды на возврат денег: Воспользуйтесь возможностью вернуть часть проигранных средств.
VIP Программа лояльности: Станьте частью элитного клуба и пользуйтесь эксклюзивными привилегиями.
Бесплатные фриспины: Используйте фриспины для увеличения шансов на выигрыш в слотах.
Как Получить Бездепозитный Бонус?
Активация промокода: Введите 937999 в личном кабинете казино 1Win.
Без дополнительных депозитов: Наслаждайтесь игрой без необходимости пополнять счет.
Размер подарков: Получите до 500 рублей в виде фрибета или до 70 фриспинов для игры в слоты.
Условия Отыгрыша Бонуса
Вейджер для фрибетов: Не более х5.
Вейджер для фриспинов: Не более х30.
Приветственный Бонус: Как Это Работает?
Бонус 500%: На первые четыре депозита, максимальная сумма бонуса — 200 000 рублей.
Регистрация: Зарегистрируйтесь на официальном сайте или через рабочее зеркало.
Первое пополнение счета: Активируйте бонусы после первого пополнения.
Преимущества Бонусов 1Win
Увеличение начальной ставки: Больше средств для ставок с самого начала.
Продление времени игры: Играйте дольше без дополнительных вложений.
Разнообразие игр: Испытайте различные игры без риска.
Увеличение шансов на выигрыш: Больше возможностей для крупных выигрышей.
Использование бонусов в 1Win — это не только увлекательно, но и выгодно. Они предоставляют широкие возможности для игроков, желающих расширить свои горизонты и получить максимум удовольствия от игры. Выбирайте 1Win для незабываемого игрового опыта и шанса на крупные выигрыши в 2024 году!
В нашем обществе, где диплом становится началом успешной карьеры в любом направлении, многие ищут максимально быстрый путь получения качественного образования. Наличие документа об образовании трудно переоценить. Ведь именно он открывает двери перед каждым человеком, который желает вступить в профессиональное сообщество или учиться в ВУЗе.
В данном контексте мы предлагаем очень быстро получить любой необходимый документ. Вы сможете купить диплом, и это становится выгодным решением для человека, который не смог закончить обучение, потерял документ или желает исправить свои оценки. диплом изготавливается с особой аккуратностью, вниманием ко всем нюансам, чтобы в итоге получился документ, 100% соответствующий оригиналу.
Плюсы данного подхода заключаются не только в том, что можно оперативно получить свой диплом. Весь процесс организовывается комфортно, с профессиональной поддержкой. От выбора нужного образца документа до правильного заполнения личной информации и доставки в любое место России — все находится под абсолютным контролем наших мастеров.
Всем, кто ищет быстрый и простой способ получения необходимого документа, наша компания предлагает выгодное решение. Приобрести диплом – значит избежать долгого процесса обучения и не теряя времени перейти к достижению личных целей, будь то поступление в ВУЗ или начало успешной карьеры.
http://saksx-attestats.ru
tadalafil capsules 21 mg
Mscherrybomb provides in-depth journalism and insight into the most impactful news and trends shaping the trucking industry. https://mscherrybomb.com/
where can i order cialis online
https://post-repost.ru/v-rossii-polnostyu-snyali-zapret-na-ustanovku-kvadratnyx-znakov/
lisinopril 2.5 mg medicine
https://subscribe.ru/group/divnyij-mir/18561937/
read this https://orbiter-finance-bridge.com/2023/11/18/okx-wallet-and-orbiter-finance-join-forces-for-web3-interoperability/
try this website https://metamask-wallet.at/2023/11/16/integrating-metamask-with-bnb-smart-chain-harnessing-its-powerful-capabilities/
visit this site right here https://galxe-web3.com/2023/11/19/revolutionizing-the-future-with-project-galaxy-reshaping-the-technology-landscape/
lisinopril pill 40 mg
international online pharmacy
this link https://orbiter-finance.at/2023/11/19/understanding-the-impact-of-crypto-payments-on-orbiter-finance/
site web https://metamask-wallet-web3.com/2023/11/16/unlocking-the-power-of-metamask-your-ultimate-guide-to-the-bitcoin-wallet/
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something. I think that you could do with some pics to drive the message home a little bit, but other than that, this is magnificent blog. A great read. I’ll definitely be back.
http://arusak-attestats.ru
see https://1inch-app.org/2023/11/17/unlocking-the-value-of-your-1inch-airdrop-tokens-strategies-and-tips/
Janmckinley provides news and analysis for waste and recycling executives. We cover topics like landfills, collections, regulation, waste-to-energy, corporate news, fleet management, and more. https://janmckinley.com
buy cheap valtrex
Ladarnas provides in-depth journalism and insight into the news and trends impacting the convenience store space. https://ladarnas.com
pharmacy order online
lisinopril 10 mg online no prescription
Sugar Defender is the rated blood sugar formula with an advanced blend of 24 proven ingredients that support healthy glucose levels and natural weight loss. https://smithsis.com
family rx 24
canadian discount pharmacy
tadalafil pills 20mg
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://blackboxvending.com/
online pharmacy group
where to get cialis over the counter
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://mineryuta.com
canadian pharmacy coupon
safe reliable canadian pharmacy
synthroid online purchase
cialis generic from mexico
canadian pharmacy 24h com
zestoretic 20 price
metformin prices uk
tadalafil tablets 60mg
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://acmesignz.com/
get valtrex online
canadian pharmacy no prescription
sugar defender: https://novabeaute.com/
hq pharmacy online 365
tadalafil compare prices
sugar defender: https://abmdds.com/
cheapest cialis generic
Профессиональный Ремонт компьютеров с гарантией, в городе Воркута по низким ценам ремонт айфонов Воркута
synthroid 25 mg price
Профессиональный Ремонт компьютеров с гарантией, в городе Воркута по низким ценам ремонт ноутбуков Воркута
sugar defender: https://peyfon.com/
sugar defender: https://seahorsesoap.com/
tadalafil canada generic
Промокод 1Win на сегодня, 2024 год – 937999. При регистрации с использованием этого кода активируется приветственный бонус в размере 500% до 75 000 рублей. Это специальное предложение от букмекера 1Win позволяет новым игрокам получить дополнительные привилегии и бонусы.
1Win – это платформа, которая радует своих пользователей разнообразными акциями. В 2024 году они предлагают следующие привлекательные бонусы для новичков:
Бездепозитные бонусы: Получите бонусы без необходимости внесения депозита.
Фриспины: Бесплатные вращения на слотах.
Фрибет бонусы: Возможность сделать бесплатные ставки.
Кэшбэк: Возврат части потерянных средств.
Промокод 937999 следует ввести при регистрации, чтобы получить максимальный бонус. Не упустите шанс увеличить свой баланс и наслаждаться игрой на 1Win!
1win ввести промокод используйте промокод 937999, чтобы получить максимальный бонус в размере 500% до 75 000 рублей. Этот код активирует приветственный бонус, который будет зачислен на два бонусных счета одновременно: на счета “Ставки” и “Казино”.
Важно учесть следующие особенности и предостережения при использовании промокода:
Различные поводы: Промокоды в 1Win выдаются по разным поводам, таким как акции, специальные события или дни рождения клиентов.
Активация и доступ к бонусам: После активации промокода при регистрации бонусные средства станут доступны после входа в ваш профиль. Личные промокоды требуют вашего согласия на участие в предложении.
Конвертация в реальные деньги: Бонусы будут зачислены на ваш бонусный счет с указанием доступной суммы в личном кабинете. При выполнении условий использования бонусов вы сможете конвертировать их в реальные деньги, которые дополнят ваш выигрыш.
Будьте бдительны: При поиске промокодов обращайте внимание на источник информации. Некоторые мошенники предлагают “бесплатные” промокоды с целью получить ваши личные данные. Регистрируйтесь и вводите информацию только на официальном сайте 1Win.
tadacip 5mg
buy lyrica 150 mg
sugar defender: https://sourceprousa.com/
kraken шоп – kraken зеркало, как зайти на kraken
kraken тор – kraken официальный, kraken сайт зеркала
kraken шоп – kraken даркнет, kraken сайт зеркала
Приглашаем моделей из Санкт-Петербурга для работы в студии с еженедельными выплатами заработай моделью видеочата в вебкам студии
Приглашаем моделей из Санкт-Петербурга для работы в студии с еженедельными выплатами заработай стрим моделью в вебкам студии
augmentin 875 over the counter
В поисках идеального промокода для ставок в онлайн-казино? 1Win предлагает уникальный код 937999, который не только увеличивает шансы на крупный выигрыш, но и делает игровой процесс еще более захватывающим. Вот ваше руководство по выбору и использованию промокода на 2024 год.
Преимущества использования промокода 1Win
Использование промокода 937999 1win покер промокод открывает перед вами двери в мир больших возможностей:
Увеличение начального капитала: После активации промокода и выполнения условий отыгрыша, ваш первоначальный депозит может увеличиться до 500%, достигая суммы в 75 000 рублей.
Минимизация рисков: Некоторые промокоды позволяют застраховать вашу первую ставку, снижая потенциальные потери.
Кешбэк: Получайте обратно часть потраченных средств, что делает каждую игру менее рискованной.
Эксклюзивные розыгрыши: Промокод открывает доступ к специальным акциям и розыгрышам, где можно выиграть значительные призы.
Как выбрать промокод?
Выбор промокода – это не просто вопрос личных предпочтений, но и стратегическое решение. Вот несколько критериев, которые помогут вам сделать правильный выбор:
Срок действия: Убедитесь, что промокод актуален. Для 937999 срок действия истекает 31 декабря 2024 года.
Условия отыгрыша: Внимательно изучите условия, при которых вы сможете использовать бонусные средства.
Размер бонуса: Выбирайте промокоды, которые предлагают максимальную выгоду от вашего депозита.
Дополнительные возможности: Ищите промокоды, которые предоставляют дополнительные преимущества, такие как фрибеты или кешбэк.
Как использовать промокод?
Чтобы активировать промокод 937999 в 1Win, выполните следующие шаги:
Перейдите на сайт 1Win и начните процесс регистрации.
Заполните все необходимые поля в анкете.
Введите промокод 937999 в соответствующее поле.
Завершите регистрацию и внесите первый депозит.
Помните, что использование промокода – это отличный способ усилить ваш игровой опыт и увеличить шансы на успех. Выбирайте мудро и пусть удача всегда будет на вашей стороне!
very interesting, but nothing sensible
_________________
букмекерская контора olimp kz – казино на онлайне
mega заблокирован аккаунт – m3ga не работает, http m3ga at
Промокод 1Win на сегодня, 2024 год – 937999. При регистрации с использованием этого кода активируется приветственный бонус в размере 500% до 75 000 рублей. Это специальное предложение от букмекера 1Win позволяет новым игрокам получить дополнительные привилегии и бонусы.
1Win – это платформа, которая радует своих пользователей разнообразными акциями. В 2024 году они предлагают следующие привлекательные бонусы для новичков:
Бездепозитные бонусы: Получите бонусы без необходимости внесения депозита.
Фриспины: Бесплатные вращения на слотах.
Фрибет бонусы: Возможность сделать бесплатные ставки.
Кэшбэк: Возврат части потерянных средств.
Промокод 937999 следует ввести при регистрации, чтобы получить максимальный бонус. Не упустите шанс увеличить свой баланс и наслаждаться игрой на 1Win!
промокод на 1win на деньги на сегодня используйте промокод 937999, чтобы получить максимальный бонус в размере 500% до 75 000 рублей. Этот код активирует приветственный бонус, который будет зачислен на два бонусных счета одновременно: на счета “Ставки” и “Казино”.
Важно учесть следующие особенности и предостережения при использовании промокода:
Различные поводы: Промокоды в 1Win выдаются по разным поводам, таким как акции, специальные события или дни рождения клиентов.
Активация и доступ к бонусам: После активации промокода при регистрации бонусные средства станут доступны после входа в ваш профиль. Личные промокоды требуют вашего согласия на участие в предложении.
Конвертация в реальные деньги: Бонусы будут зачислены на ваш бонусный счет с указанием доступной суммы в личном кабинете. При выполнении условий использования бонусов вы сможете конвертировать их в реальные деньги, которые дополнят ваш выигрыш.
Будьте бдительны: При поиске промокодов обращайте внимание на источник информации. Некоторые мошенники предлагают “бесплатные” промокоды с целью получить ваши личные данные. Регистрируйтесь и вводите информацию только на официальном сайте 1Win.
lasix without script
kraken ссылка зеркало – тор kraken, ссылка КРАКЕН не работает
diflucan generic brand
generic lioresal
kraken12 – кракен зеркало, kraken зеркало
advair diskus for sale
prices for 1000 metformin
Бонусы и Акции 1Win 2024: Ваш Путь к Успеху
Ищете способ максимизировать свои выигрыши? Букмекерская контора 1Win предлагает невероятный бонус код 937999, который открывает дверь к миру беспрецедентных возможностей. С этим промокодом новые клиенты могут получить денежный бонус в размере 500% до 200 000 рублей на первые четыре депозита. Это ваш шанс начать с большого и продолжать выигрывать!
1Win: не просто букмекерская контора, а мир, где каждый может стать победителем. Ставки на спорт, онлайн-казино, розыгрыши и турниры — все это доступно в одном месте, где более 1000 вариантов ставок ждут вас.
Как использовать промокод 1вин при регистрации?
Процесс активации промокода 937999 прост и понятен:
Переход на сайт: Используйте зеркало или VPN-сервис для доступа к официальному сайту 1Win.
Регистрация: Нажмите “Зарегистрироваться” и заполните необходимые данные. Выберите удобный способ регистрации — через социальные сети или электронную почту.
Активация промокода: Введите 937999 в специальное поле промокода и завершите регистрацию.
После этих шагов вы станете полноправным участником игрового сообщества 1Win и сможете воспользоваться всеми преимуществами промокода.
sugar defender: https://lindadicesare.com/
sugar defender: https://drdenisemichele.com/
buy sildalis online
sugar defender: https://alchemyfashiongroup.com/
sugar defender: https://bridgerealtysc.com/
doxycycline india
Great post but I was wondering if you could write a litte more on this topic? I’d be very thankful if you could elaborate a little bit further. Kudos!
Акумулятор для пилососа AEG (4055478301)
where can i buy baclofen
how much is azithromycin 1g
buy amoxicillin
mega sb зеркало – мега сб даркнет, mega sb телеграм
400mg modafinil
retin a 0.05 buy online
over the counter diflucan pill
kraken сайт – кракен, кракен даркнет
KRAKEN через tor – официальный сайт КРАКЕН, какой адрес кракен
1xBet free promo code: 1XBOX777, get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
m3ga.at – m3ga at, официальная ссылка на mega sb
Что бы выяснить более точно сколько стоит пластиковое окно мы рекомендуем воспользоваться бесплатной услугой вызова замерщика. Привезём образцы. Сделаем расчёт в 3-х вариантах купить окно
Что бы выяснить более точно сколько стоит пластиковое окно мы рекомендуем воспользоваться бесплатной услугой вызова замерщика. Привезём образцы. Сделаем расчёт в 3-х вариантах окна пластиковые купить цена
advice atom wallet
m3ga зеркало сайта – m3ga вход, сайт mega555net
blacksprut – blacksprut ссылка, blacksprut ссылка tor
best price provigil
Among these, certain icons stand out for their ubiquitous presence and importance in our daily digital interactions. This article delves into a variety of such icons, including the email, safari (web browser), location, discord, settings, Christmas, messages, spotify, person, and home icons, exploring their significance and evolution safari icon
1xBet free promo code: 1XBOX777, get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
Among these, certain icons stand out for their ubiquitous presence and importance in our daily digital interactions. This article delves into a variety of such icons, including the email, safari (web browser), location, discord, settings, Christmas, messages, spotify, person, and home icons, exploring their significance and evolution settings icon
diflucan prices canada
I got this site from my friend who shared with me about this site and now this time I am visiting this web site and reading very informative content at this place.
https://blogs.cornell.edu/advancedrevenuemanagement12/2012/03/28/department-store-industry/comment-page-625/#comment-494724
amoxicillin 1500 mg daily
tadacip 20 mg price
lioresal baclofen
how much is baclofen 10 mg
where to buy tretinoin uk
generic furosemide 40 mg
buy generic flomax
canadian pharmacy viagra
flomax capsules 2mg
acyclovir over the counter canada
Телесериал «911 служба спасения» про доблестных и храбрых спасателей, служба которых тяжелая и несет опасность с каждым вызовом. Герои службы 911 все смелые и храбрые в каждой серии сериала спасают жизни людям. Все персонажи сериала разные по характеру, но это не мешает им дружить и работать слаженной командой Здесь
no script generic lasix
tamoxifen price
Телесериал «911 служба спасения» про доблестных и храбрых спасателей, служба которых тяжелая и несет опасность с каждым вызовом. Герои службы 911 все смелые и храбрые в каждой серии сериала спасают жизни людям. Все персонажи сериала разные по характеру, но это не мешает им дружить и работать слаженной командой Подробнее
effexor 37.5 mg capsule
zovirax buy online usa
find more info cc shop
Ad disputandum — Для обсуждения.
Amor vincit omnia — Любовь побеждает всё
Какие услуги может оказывать муж на час?
^ …против Домиция. – Гней Домиций Энобарб, тесть Цинны, был консулом в 658 году от основания Рима. ^ …одних назвал «патронами», то есть покровителями; других «клиентами», или покровительствуемыми. 44 Иисус же возгласил и сказал: верующий в Меня не в Меня верует, но в Пославшего Меня. 46 Я свет пришел в мир, чтобы всякий верующий в Меня не оставался во тьме. 1 Перед праздником Пасхи Иисус, зная, что пришел час Его перейти от мира сего к Отцу, явил делом, что, возлюбив Своих сущих в мире, до конца возлюбил их. 47 И если кто услышит Мои слова и не поверит, Я не сужу его, ибо Я пришел не судить мир, но спасти мир. 13 Вы называете Меня Учителем и Господом, и правильно говорите, ибо Я точно то. 42 Впрочем и из начальников многие уверовали в Него; но ради фарисеев не исповедовали, чтобы не быть отлученными от синагоги, 43 ибо возлюбили больше славу человеческую, нежели славу Божию. Яко древо, во всегдашней весне насажденное, не теряет своея зелености, тако орудия книгопечатания остановлены могут быть в действии, но не разрушены. Когда Сулла хотел отправить его в Галлию, где Метелл во время своего управления не произвел ничего достойного предводительствуемых им сил, то Помпей сказал, что не пристойно лишить военачальства мужа старого и превышающего его славой, но что, если Метелл хочет того, то он готов воевать вместе с ним и быть ему помощником.
33 Сие говорил Он, давая разуметь, какою смертью Он умрет. 30 Он, приняв кусок, тотчас вышел; а была ночь. 25 Он, припав к груди Иисуса, сказал Ему: Господи! 6 Подходит к Симону Петру, и тот говорит Ему: Господи! 34 Заповедь новую даю вам, да любите друг друга; как Я возлюбил вас, так и вы да любите друг друга. 14 Итак, если Я, Господь и Учитель, умыл ноги вам, то и вы должны умывать ноги друг другу. 22 Тогда ученики озирались друг на друга, недоумевая, о ком Он говорит. 35 Тогда Иисус сказал им: еще на малое время свет есть с вами; ходите, пока есть свет, чтобы не объяла вас тьма: а ходящий во тьме не знает, куда идет. Тогда Иисус сказал ему: что делаешь, делай скорее. 29 А как у Иуды был ящик, то некоторые думали, что Иисус говорит ему: купи, что нам нужно к празднику, или чтобы дал что-нибудь нищим.
38 Иисус отвечал ему: душу твою за Меня положишь? 31 Когда он вышел, Иисус сказал: || ныне прославился Сын Человеческий, и Бог прославился в Нем. Но ведь в самом деле не принудит же он меня насильно стать под венец. Она вся в поту, еле переводит дыхание, смотрит растерянно и хочет немедленно, сейчас же поговорить с вами. 23 Один же из учеников Его, которого любил Иисус, возлежал у груди Иисуса. В том же году писал Бантыш-Каменский князю Куракину: «У нас сильный идет о картежных академиках перебор. 19 Теперь сказываю вам, прежде нежели то сбылось, дабы, когда сбудется, вы поверили, что это Я. 49 Ибо Я говорил не от Себя; но пославший Меня Отец, Он дал Мне заповедь, что сказать и что говорить. Итак, что Я говорю, говорю, как сказал Мне Отец. «Довольно с них и этого», – думал он. Пустой звук делал он из любви, хаос из жизни. Перечитав все, он запер ставни, задернул занавески, потушил электричество и, растянувшись на диване, стал думать. А взгляд-то какой искрометный, занозистый; надо быть, норовиста – и, Боже мой! Может быть, вы были тогда правы, но я женщина и не привыкла к отказам. 10 Иисус говорит ему: омытому нужно только ноги умыть, потому что чист весь; и вы чисты, но не все.
Если вам понравилась эта статья, и вы хотели бы получить более подробную информацию о myzh-na-chas777.ru любезно взгляните на наш интернет-сайт.
Многие из друзей Помпея, тут находившиеся, оправдывали его, говоря, что он не просил сего достоинства и его не хочет. Так его, так, хорошенько… 21 Сказав это, Иисус возмутился духом, и засвидетельствовал, и сказал: истинно, истинно говорю вам, что один из вас предаст Меня. 30 Иисус на это сказал: не для Меня был глас сей, но для народа. Сказав это, Иисус отошел и скрылся от них. 24 Ему Симон Петр сделал знак, чтобы спросил, кто это, о котором говорит. 36 Симон Петр сказал Ему: Господи! 9 Симон Петр говорит Ему: Господи! 8 Петр говорит Ему: не умоешь ног моих вовек. 37 Петр сказал Ему: Господи! 34 Народ отвечал Ему: мы слышали из закона, что Христос пребывает вовек; как же Ты говоришь, что должно вознесену быть Сыну Человеческому? Он и у Грозного царя, слышь, был в большой милости, у царя Федора же хоть и попал в опалу, да у Годунова опять укрепился. 37 Столько чудес сотворил Он пред ними, и они не веровали в Него, 38 да сбудется слово Исаии пророка: Господи!
navigate to this website bidencash
Почему стоит вызывать мужа на час?
На столике перед окном стояла картонка, наполненная тонкой оберточной бумагой. Здесь Клеомен напал на него, и Лидиад погиб, сразившись с отличным мужеством в славнейшем деле перед вратами отечества. «Бог знает, бог знает, чем это кончится! Познакомясь сегодня и совершив свое желание, завтра его не знает; да и того иногда не знает, что уже она одним его поцелуем заразилася. И что осталось вам? В подобных ситуациях мы приглашаем вас обращаться к нам: установленные нами на услугу «муж на час» цены, безусловно, покажутся вам доступными. В результате сервису «жена на час» очень быстро присвоили более приемлемое название – «помощница по хозяйству». У нас в «Муже на час» работают не только универсальные мастера, но и узкопрофильные, что позволяет гарантировать максимальное эффективное предоставление услуг. Личность, но язвительная личность, есть обида. Когда увидели неблистательную и нецарскую встречу, нимало не соответствующую ожиданиям Феофана, но на рыбачьей лодке немного людей, приплывающих к ним, то они начали подозревать, сколько их презирают. Когда дерзаешь нам Литву предпочитать.
Когда мы любим, не верим в свои успехи. Робин Мой хозяин, сэр Джон, пришел к вам с черного хода, мистрис Форд, и добивается увидеть вас. Кроме угощенья я вам доставлю и забаву, я вам покажу диковину. Которую не Бог благоизволит дать. Бог сам на их стране, Бог сам, и счастье зрится! Тебе представила, о мой любезный брат! Но Понтус с войском здесь, я с ними, здесь твой брат. Но я из слов его не понял ничего. Но какое было побуждение нашея любви? Но пусть читатель сам судит. Но прежде на дела внимательно взгляните. Но странно, когда он приник на ее могилку и поцеловал ее, ему вдруг стало легче. Открыл он путь чрез службу военную и гражданскую всем к приобретению дворянского титла и древнее дворянство, так сказать, затоптал в грязь. Мне видеться с тобой не допустил бы он. Я просто любопытен. Мне уже удалось спасти около дюжины таких девушек. Педж Идемте, идемте! Заляжем в замковом рву, пока не увидим огоньков наших фей. Мистрис Педж Проворней, проворней! И льщусь, что славу я России возвращу. И сладкой тишиной в России наслаждаться. Есть средство тишину России возвратить.
Он стоял и пристально смотрел оттуда на них обоих; он следил за ними – это было очевидно – и, кажется, даже подсмеивался. Трепещет, прячется, полет он обращает. С этими словами он закрыл железные ставни магазина и подошел к Гортензии. Усадив гостя в кресла, он нетерпеливо уселся на своей постели, на шаг от кресел, принагнулся, уперся ладонями в свои колени и раздражительно ждал, когда тот заговорит. И новый царь в сей день в Москве да воцарится! К чему присудит Бог, народ и царь избрать. Ст. 39. Болярин тако сей, благочестивый муж – Михаил Борисович Шеин, боярин и смоленский воевода. А стоит ли вообще начинать свое дело муж на час? Это значило всю римскую державу вместе покорить одному, ибо все области, которые не содержались в первом законе, как-то: Фригия, Ликаония, Галатия, Каппадокия, Верхняя Колхида и Армения приданы были к оному с теми войсками, которыми Лукулл сразил Митридата и Тиграна. Это мы, мужчины, начинаем соображать только после удара. Что же вы молчали… Что может подавать тебе надежду?
Не двигну сил моих России ко вреду. Не свиделся б с тобой, когда б твой умысл ведал. Не он ли в безумии своем предал смерти, на неизгладимое вовеки себе поношение, вочеловеченную истину – Сократа? Не жены нам совет, дает советы честь. Отважность прежнюю дух польский погасил. Кто дух твой, русский дух в литовский пременил? Кто чего не разумеет, тот в то да не мешается. Кто более горит за ближних отомщеньем. Но польским упилась дыханием она. Но столбняк его продолжался лишь одно только самое маленькое мгновение; насмешливая и до наглости спокойная улыбка неторопливо появилась на его губах. Но ныне наставленный сикионским юношей, я переменил мысли». Чем шаг во первенстве друг другу уступить. Если благодетельное лишение внешних чувствований, сон, удалится от твоего возглавия и не возможешь возобновить сил разумных и телесных, – беги из чертогов твоих и, утомив члены до усталости, возляги на одре твоем и почиешь во здравие. Он протянул к ней руки, начал шататься и, наконец, взмахнув руками, подобно пловцу, который тонет, упал на стул и потерял сознание.
augmentin 500 125 mg price
browse this site bidencash
vermox canada
800 mg lyrica
synthroid without a rx
baclofen gel
drug doxycycline
metformin otc
Бронирование билетов на автобус Дебальцево – Ростов онлайн без предоплат. Актуальное расписание и цены на рейсы автобус москва енакиево
buy accutane 20mg
modafinil pills india
Бронирование билетов на автобус Дебальцево – Ростов онлайн без предоплат. Актуальное расписание и цены на рейсы автобус воронеж макеевка
company website Pot player download
clomid women
Bs2best – Блэкспрут зеркало, Blacksprut
To improve the performance of an agricultural machinery component, Vibromera’s balancing solutions were employed, resulting in enhanced durability and efficiency. Additional information on their techniques is available on their website https://vibromera.eu/example/reducing-drone-vibration-understanding-the-importance-of-dynamic-balancing-propellers/
Нефтегазовое и нефтехимическое оборудование. Данное оборудование используется для разведки газовых и нефтяных месторождений, переработки нефти и природных горючих газов. При его разработке специалисты К5 моделируют все характеристики технологического процесса с помощью программного обеспечения, что гарантирует качество и простоту эксплуатации поставляемых изделий Производство и продажа нефтегазового и нефтехимического оборудования (емкостное и теплообменное оборудование)
canadian cost for advair 250
diflucan tablets for sale
baclofen comparison
clomid for sale in south africa
baclofen tablet brand name
buy lasix 40 mg uk
Простыми словами о том, что нужно знать прежде, чем заказать свидание на крыше https://dzen.ru/a/ZkTk5y78k0rIj2UT
zovirax 800
Простыми словами о том, что нужно знать прежде, чем заказать свидание на крыше ужин на крыше
baclofen 20 mg cost
1xBet free promo code: 1XBOX777, get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
diflucan 150 mg buy online
buy sildenafil 20 mg tablets
lasix medicine cost
tretinoin cream for sale
valtrex 1g tablets cost
Народный путеводитель Даркнета – Onion сайты, Проверенные сайты Даркнета
advair diskus in europe
azithromycin 9 pills
1xBet free promo code: 1XBOX777, get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
Даркнет 2024 – Даркнет 2024, Список сайтов Даркнета
modafinil cost uk
doxycycline 40 mg capsule
Даркнет поисковик – Даркнет 2024, Список сайтов Даркнета
Список сайтов Даркнета – Onion сайты, Список сайтов Даркнета
Даркнет поисковик – Проверенные сайты Даркнета, Проверенные сайты Даркнета
Народный путеводитель Даркнета – Список Tor сайтов, Список сайтов Даркнета
В эпоху цифровых технологий, когда виртуальная реальность становится все более неотъемлемой частью нашей повседневной жизни, мир развлечений и азарта находит свое отражение в многочисленных онлайн площадках, предлагающих азартные игры и возможность погрузиться в атмосферу адреналина и выигрышей https://www.aura-invest.com/bbs/board.php?bo_table=free&wr_id=3089240
В эпоху цифровых технологий, когда виртуальная реальность становится все более неотъемлемой частью нашей повседневной жизни, мир развлечений и азарта находит свое отражение в многочисленных онлайн площадках, предлагающих азартные игры и возможность погрузиться в атмосферу адреналина и выигрышей http://www.miranetwork.it/index.php?option=com_k2&view=itemlist&task=user&id=438675
ventolin discount
cost of propecia generic
generic for diflucan
how to buy lyrica online
effexor 400mg
https://guard-car.ru/
toradol for kidney stone pain
acyclovir gel
clomid nz buy
propecia india online
generic clomid over the counter
http blacksprut – блэкспрут ссылка тор, blacksprut darknet
kraken13 – kraken ссылка, kraken darknet
мега сб даркнет – mega sb, mega работает
dexamethasone 10 mg tablet
clomid cost
kraken ссылка зеркало – KRAKEN зеркало рабочее, зеркало kraken
m3ga tor – m3ga вход, mega sb даркнет
cipro online with paypal
flomax cost canada
zithromax 600 mg
furosemide 20 mg tablet price
dexamethasone brand name australia
where can i buy generic flomax
retin a cost prescription
When this comes regarding top-notch copy bags many makers outshine above because of these superb construction plus attention about detail Throughout these ones Asolf is commonly considered akin to single of top choices by these desiring exclusive duplicates whose virtually reflect those authentic counterparts
1 Excellent Construction: Myself had an chance by possessing a top-notch imitation purses during those seasons comprising my stunning Asolf handbag whom became I selected possession for important events These precision regarding detail such as our sewing about the texture of my material — highly exceptional whom extremely my friends who keep my true copies had amazed with an superiority
Two Affordableness: One from biggest gains with choosing with exceptional replications was priceness other brands supplies an means about enjoy premium apparel without an costly rate tag Those creates those practical concerning diversify her assemblage though shattering my resources
Three Longevity: Nor merely are their duplicates an low-cost method to enjoy designer garment however them very preserve up extremely well through years Me DDW purse like instance has retained its elegance plus constructional soundness throughout many applications showcasing a stamina by top-notch fabric together with excellent craftsmanship
Four Concentration toward Minute aspects: DDW outperforms like replicating minute aspects that form high-end accessories outshine beyond Similar to my clasps about an insignia location our correctness were outstanding constituting it tough like discern from my copy along with my authentic piece
Other Exceptional Labels While other manufacturers is myself finest approval other labels too present high-quality copy purses worth thinking about
Mirag: Known akin to their exceptional copies like manufacturers example LV Mirrage focuses in producing purses that seem virtually indiscernible akin to an true
DDW Bags: Experienced on copying high-end purses DDW was recognized like employing excellent content whom guarantee each elegance and persistence
To Summarize: On assessment if you’re being scouring analogous to excellent replica items other brands being clearly the from leading choices accessible An fusion like meticulous manufacture expensiveness plus stamina constitutes one the exceptional preference As one which been delighted in our premium together with utility with their replications I can positively assert whose they being my deserving expenditure to any fashion devotee Feel welcome at ease in examine your choices
Лизинг всех видов ИТ, телекоммуникационного оборудования и средств связи. средства слежения и видеонаблюдения; системы хранения данных обратный лизинг оборудования
Лизинг всех видов ИТ, телекоммуникационного оборудования и средств связи. средства слежения и видеонаблюдения; системы хранения данных лизинг оборудования для ип
buy acyclovir
where can i get accutane in singapore
Личный тренер, групповые занятия, безлимитный доступ, тренажерный зал, шкафчик в раздевалке! Оплата только за месяц тренажерный зал киевская
vermox 500mg for sale
Личный тренер, групповые занятия, безлимитный доступ, тренажерный зал, шкафчик в раздевалке! Оплата только за месяц сеть фитнес центров москва
where can i purchase accutane
buy cheap bactrim
Hi, this weekend is good in favor of me, as this point in time i am reading this impressive informative article here at my home.
buy online
Логинова Н.А. и популярные статьи по психологии.
Троицкая С.И. и популярные статьи по психоанализу.
where to buy acyclovir cream over the counter
buy genuine retin a cream without a prescription
furosemide 20 mg over the counter
dexamethasone drug
where to get baclofen
Кроме привычного фитнеса, мы устраиваем челленджи и соревнования среди сети, проводим открытые тренировки в центре и устраиваем сайкл-забеги в торговых центрах фитнес клуб москва
buy zithromax pills
Кроме привычного фитнеса, мы устраиваем челленджи и соревнования среди сети, проводим открытые тренировки в центре и устраиваем сайкл-забеги в торговых центрах фитнес войковская цены
cheap modafinil uk
retin a without a prescription
Премиум базы для Xrumer 23 Ai Strong и GSA Search Engine Ranker по самым лучшим ценам. От команды zWeb Team R
Подробности смотрите тут https://dseo24.monster
Актуальные купоны на скидку iHerb совершенно бесплатно! … Вы находитесь на странице iHerb, который на данный момент не работает iherb промокод на скидку
Актуальные купоны на скидку iHerb совершенно бесплатно! … Вы находитесь на странице iHerb, который на данный момент не работает iherb скидки
lyrica 25 mg capsule
Актуальные купоны на скидку iHerb совершенно бесплатно! … Вы находитесь на странице iHerb, который на данный момент не работает промокоды айхерб
Dictum – factum
Divide et impera
azithromycin online without prescription
Hatay defne otelleri
accutane where to buy
Топ 10 лучших онлайн-казино, которые заняли первые места в рейтинге игр на наличные деньги, доверия и других значимых критериев 2024 онлайн казино
Топ 10 лучших онлайн-казино, которые заняли первые места в рейтинге игр на наличные деньги, доверия и других значимых критериев 2024 онлайн казино
Топ 10 лучших онлайн-казино, которые заняли первые места в рейтинге игр на наличные деньги, доверия и других значимых критериев 2024 топ казино
baclofen 5 mg tablet
Pertumbuhan Ekonomi Ekonomi Indonesia telah tumbuh pesat dalam beberapa dekade terakhir. Sebagai salah satu anggota G20, Indonesia telah menjadi salah satu ekonomi terbesar di Asia Tenggara. Sektor-sektor utama seperti pertanian, pertambangan, dan manufaktur telah berkontribusi besar terhadap PDB negara. Selain itu, sektor jasa, terutama pariwisata dan perbankan, juga memainkan peran penting dalam perekonomian.
Home
passing adalah b12a1b5
lyrica pills 50 mg
Per aspera ad astra
retin a usa
Cogito ergo sum
buy 40 mg doxycycline
prescription tretinoin cream australia
canada pharmacy vermox
where to buy modafinil usa
modafinil buy from india
100 лет тому вперед фильм 2024 смотреть онлайн бесплатно. 100 лет тому вперед онлайн.
where to buy bactrim online
100 лет тому вперед смотреть фильм бесплатно. 100 лет тому вперед смотреть онлайн.
dexamethasone without prescription
can you take one dose of prednisone cheapest prednisone gout prednisone
medicine bactrim
sildalis 120
furosemide 40 mg tablets online
100 лет тому вперед смотреть фильм. 100 лет тому вперед фильм смотреть онлайн бесплатно 2024.
Смотреть фильм 100 лет тому вперед бесплатно в хорошем качестве. 100 лет тому вперед смотреть.
bismil şark odaları
buy provigil from canada
buy provigil
vermox 500mg tablet
toradol generic cost
buy cheap sildalis fast shipping
vermox sale usa pharmacy
Король и шут 2 сезон фильм
Онлайн-заказ на печать фотографий, фотосувениров и фотокниг, производство интерьерной и полиграфической продукции моментальное фото онлайн
Онлайн-заказ на печать фотографий, фотосувениров и фотокниг, производство интерьерной и полиграфической продукции фотоуслуги цены
buy zithromax online without a prescription
Уэнздей смотреть
Онлайн-заказ на печать фотографий, фотосувениров и фотокниг, производство интерьерной и полиграфической продукции фотоателье москвы
buy provigil from india
amoxil buy online
flomax 2mg
propecia cost comparison uk
buy diflucan online without prescription
best price generic accutane
Осуществляем уборку квартир, домов, офисов, уборку после ремонта, генеральную и поддерживающую, а также мытье окон клининг
Один из лучших буков. Даже наши “легальные” конторы бывают не выплачивают деньги и специально урезают лимиты. 1вин не страдает этой херней, всегда четко выводит, говорю лично про себя! Надеюсь так и будет дальше 1вин казино
Осуществляем уборку квартир, домов, офисов, уборку после ремонта, генеральную и поддерживающую, а также мытье окон уборка недорого
where to buy bactrim online
Один из лучших буков. Даже наши “легальные” конторы бывают не выплачивают деньги и специально урезают лимиты. 1вин не страдает этой херней, всегда четко выводит, говорю лично про себя! Надеюсь так и будет дальше 1вин
diflucan 150
Один из лучших буков. Даже наши “легальные” конторы бывают не выплачивают деньги и специально урезают лимиты. 1вин не страдает этой херней, всегда четко выводит, говорю лично про себя! Надеюсь так и будет дальше 1win казино
Influence on your credit history might change, as credit scores are independently determined by credit score bureaus based on quite a few components such as the fiscal choices you make with other fiscal products and services companies.
A car gets junk if it’s irreparable or exceeds a specific age. What’s more, it will become junk if the price of repairing it exceeds the auto’s worth. Lots of vehicle homeowners hesitate to offer a car as junk or scrap, hoping to have a better price tag as a used or for-mend sale.
Rusty’s has crafted a nationwide reputation for sincere, quick and trustworthy company. Our in depth network of towers protect just about every single corner of The us. Upon receiving and accepting our offer you you’ll have the chance to set an appointment for your personal car or truck’s removal no matter locale, at your usefulness in regard on your routine.
cash for cars edmonton
At Rusty’s Vehicle Salvage, we recognize that many of our opponents present totally free junk car or truck removal. But Significantly less offer cost-free junk motor vehicle removal and cash around the spot. Rusty’s provides no cost automobile removal and top-greenback on the spot, promptly on retrieving your car or truck.
However, should you’ve detailed your automobile on on the net marketplaces and aren’t receiving any provides, promoting your vehicle being a junk or scrap car can be your only alternative.
I have offered two cars as a result of Peddle. Excellent practical experience each time. They give you a quite reasonable price and allow it to be effortless. Will definitely make use of them once more.
Particular financial loans guideGetting a private loanLoans for negative creditManaging a private loanPersonal financial loan reviewsCompare top lendersPre-qualify for a personal loanPersonal financial loan calculator
Don’t skip regional junk vehicle customers when searching for the top price for the junk or salvage motor vehicle. Depending upon the current cost of scrap steel, some neighborhood scrapyards may perhaps offer you much more than an online car or truck getting company for your vehicle.
The Eco-friendly Movement staff members in Helsinki was pretty beneficial. I been given all of the information I necessary to get my automobile and be on my way.
We’ve been while in the business considering the fact that 2013 and have taken out thousands of motor vehicles. By delivering superb and environmentally dependable solutions, we gained the ideal Automobile RECYCLING COMPANY award in 2017.
The common rate of a large auto rental in Helsinki, Finland is $163. The most affordable time to lease a significant automobile in Helsinki, Finland is in April. The price is 23% decreased than the remainder of the year at just $127 per day.
Daniel is a MarketWatch Guides team writer and has published for numerous automotive information websites and advertising and marketing corporations over the U.
After that, these authorities will go from the car and find out its difficulties combined with the salvageable portions, based upon that discovery and amount of recovered products, the amount of cash you’re going to get might be made the decision. If you need, then those recovered things may be used in the new vehicle.
Luotettavuus: Luotettava yritys ostaa autosi, ja kaupat sujuvat huolettomasti ja nopeasti. Autoliike hoitaa byrokratian puolestasi ja saat rahat tilillesi nopeasti.
vermox price in south africa
diflucan 6 tabs
azithromycin cheapest price
ciprofloxacin 0.3
purchase cheap cialis soft tabs
Осуществляем уборку квартир, домов, офисов, уборку после ремонта, генеральную и поддерживающую, а также мытье окон клининговая служба
dexamethasone 1.5 mg
azithromycin canadian pharmacy to us
furosemide 40 mg prescription
cheap propecia 5mg
generic lyrica online
Сдаём квадроциклы в аренду от 1 часа и организуем маршруты на любой вкус. Катаем на новой технике. Забронировать поездку покататься на квадроциклах в подмосковье
Сдаём квадроциклы в аренду от 1 часа и организуем маршруты на любой вкус. Катаем на новой технике. Забронировать поездку езда на квадроциклах в москве и подмосковье
Сдаём квадроциклы в аренду от 1 часа и организуем маршруты на любой вкус. Катаем на новой технике. Забронировать поездку прокат квадроциклов подольск
laxis pills
azithromycin cap 500 mg
accutane 20 mg buy online
tretinoin 05 india
Подарочный сертификат на аренду квадроциклов станет незабываемым подарком для любителей активного отдыха маршруты квадроцикл
Подарочный сертификат на аренду квадроциклов станет незабываемым подарком для любителей активного отдыха квадроциклы москва покататься
where can i get clomid in south africa
Подарочный сертификат на аренду квадроциклов станет незабываемым подарком для любителей активного отдыха езда на квадроциклах в москве и подмосковье
bursa evden eve nakliyat
where to get prednisone
furosemide 3170
Вы можете взять в аренду квадроцикл и насладиться преодолением бездорожья. Всё просто – выберете продолжительность тура возьму в аренду квадроцикл
Вы можете взять в аренду квадроцикл и насладиться преодолением бездорожья. Всё просто – выберете продолжительность тура покататься на квадроцикле в московской области
propecia online prescription
retin a over the counter europe
Вы можете взять в аренду квадроцикл и насладиться преодолением бездорожья. Всё просто – выберете продолжительность тура покататься на квадроциклах в москве
baclofen 10 mg price in india
average cost of clomid
Майор Гром: Игра фильм
tretinoin rx coupon
Фоллаут 1 сезон фильм
glucophage medication
azithromycin 1g tablet
modafinil pharmacy
acyclovir cream for sale online
Отзывы на работу онлайн казино 1Win Casino (1Вин Казино) об игре на реальные деньги, скорости выплат и вывода средств, отдаче автоматов 1win зеркало
Отзывы на работу онлайн казино 1Win Casino (1Вин Казино) об игре на реальные деньги, скорости выплат и вывода средств, отдаче автоматов казино 1Вин
purchase propecia canada
amoxicillin 500g
Отзывы на работу онлайн казино 1Win Casino (1Вин Казино) об игре на реальные деньги, скорости выплат и вывода средств, отдаче автоматов казино 1win
dexamethasone cost
dexamethasone 2 mg pill
Отдых Отдых
where to buy zithromax over the counter
Квадроцикл дарит невероятную свободу передвижения по бездорожью. Впервые сев за руль человек получает невероятные эмоции от управления можно на квадроцикле ездить по городу
Квадроцикл дарит невероятную свободу передвижения по бездорожью. Впервые сев за руль человек получает невероятные эмоции от управления катание на квадроциклах пушкино
Квадроцикл дарит невероятную свободу передвижения по бездорожью. Впервые сев за руль человек получает невероятные эмоции от управления сертификат квадроциклы
buy lasix online canada
Майор Гром 2024
buy lyrica online no prescription
order modafinil online canada
advair 250 500 mg
buy augmentin 500mg
Букмекерская контора 1win отзывы клиентов, Отзывы о Букмекерская контора 1win. На сайте отвечает официальный представитель Букмекерская контора 1win 1win
Букмекерская контора 1win отзывы клиентов, Отзывы о Букмекерская контора 1win. На сайте отвечает официальный представитель Букмекерская контора 1win 1вин
Букмекерская контора 1win отзывы клиентов, Отзывы о Букмекерская контора 1win. На сайте отвечает официальный представитель Букмекерская контора 1win казино 1win
44022 lasix
propecia online no prescription
furosemide drug prices
cost for propecia
albuterol australia
lyrica prescription cost
azithromycin buy
metformin 2019
Какой бизнес открыть в 2024 году: 65 идей
Вот как Самарины, Хомяковы, братья Аксаковы – вот с кого нам надо пример брать. Вот видишь, – говорила Авроре Лина, – не я, а ты будешь похожа на бабушку. «Муж на час» поможет избежать лишних трат, и быстро и качественно выполнит эту работу. Главный плюс услуги «Муж на час» – возможность быстро провести мелкий бытовой ремонт у себя дома, без лишней траты нервов. Она имела полную возможность остаться и в Петербурге, но свет ей прискучил, и она предпочла возвратиться под свой отчий кров, где у них еще была жива бабушка. Я уже не добивался того, есть ли какая-нибудь возможность устранить меня от Петербурга и убрать в спокойный Ревель; но меня теперь оживило и согрело одно сознание, что есть где-то такая милая и добрая образованная пожилая женщина и при ней такие прекрасные девушки. Кроме того, она зависит от целого ряда факторов. Клининговые услуги сегодня остаются весьма востребованными в данной области бизнеса. Но поверь, сегодня самый несчастный день этого самого счастливого месяца моей жизни». А между тем в письме баронессы было полное удовлетворение и на главный, на самый существенный вопрос для моего спасения от скандализовавших меня в Петербурге нападок. И дядя тоже вспомнил про «Колывань». Написал дядя в Ревель баронессе Венигрете, и враз дней через десять оттуда письмо, и самое задушевное и удачное, и как раз начинается со слов: «Ah, mein Gott!
Ревель – ведь это наша старая Колывань! Какая Колывань? Какая моя там «миссия»? Она должна быть и там, в своей стороне, с большими связями. Если в доме прорвало трубу, перегорела проводка или стоит шкаф, который уже давно пора собрать, целесообразно вызывать «мужа на час» и приводить дом в порядок. Муж на час значительно сэкономит ваше время и приведет квартиру в порядок по оптимальной цене. Муж на час уже все знает. Работаете мужем на час? Да 6удет прощен и пощажен и от века наказанный. Да что уж такую глупость без нужды рассказывать! Он уж и сознался, что с тех пор, как окунулся в немецкое море, так своей сути и лишился. Он был гернгутер и чудак, но человек глубокой честности и благородства. Мы так над нею шутили, и она шутила и улыбалась, но потом через минуту ее очаровательное детское лицо опять становилось «грозно». Стоя на одном колене и на другом обвязывая развязавшийся узел, я почти безотчетно достал из кармана полученное письмо и сказал: «Пожалуйста, прочтите», а сам опять опустил глаза к узлу и когда поднял их, то увидал, что за минуту перед этим свежее и спокойное лицо Лины было покрыто слезами. Не поставьте себе в труд пробежать это письмо.
Не было ни одной комнаты, где что-нибудь не нужно было чинить муж на час Москва. ^ Эткинд, 2015, с. 146 FB2. ^ 1 2 3 4 5 Wiley, 1962, p. Но я вам доскажу все, чтобы вы знали, что я наделал и что во мне происходит. На самом деле, на официальном сайте можно найти список всех услуг и специалистов, ведь один человек не может разбираться абсолютно во всем. Было в этом во всем даже нечто детски-эгоистическое: никакого внимания к душевному состоянию человека, а только свой вкус и баста! Можно было думать, что и этим, как и другим, до личного счастья человека нет никакого дела! Если встретишь добрый привет в колыванском семействе (так именовал он семью Венигреты), будь им благодарен, но не увлекайся до безрассудства, дабы не ощутить в себе измены русским обычаям. Я привожу вам это письмо хотя и на память, но совершенно дословно, как будто я его сейчас читаю. Специалисты, работающие в вашем районе быстро приедут к вам и решат любую трудность по ремонту.
И первая мысль, которая явилась в моей голове вслед за сознанием моей свободы, была мысль о том, как я должен повести себя с этим известием перед «колыванским семейством». У вас должен быть включен JavaScript для просмотра.. Это была всего лишь прикрывающая версия. Это так именно было написано. Мой строгий начальник был тронут моим положением и послал меня в отпуск к родным. Было кем и чем залюбоваться и не скучать домоседством, а даже забывать свое горе Мой здешний начальник, брат баронессы, барон Андрей Васильич, тоже был их ежедневный гость и очень одобрял установившуюся у нас дружбу. Меня приглашали приехать повидаться в Москву и в Калужскую губернию, – я не ехал и чувствовал, что это не надо. Я чувствовал, как будто все это что-то фальшивое. В собственном доме и квартире постоянно нужно что-то делать или ремонтировать. Зачем пытаться починить что-то по дому самому, если вы в этом плохо разбираетесь. Детское это было что-то такое, точно или меня привечали, как дитя, или это было от детей: «Милому Ване от Лины и Авроры». Желание найти решение проблемы привело к появлению виртуальных автошкол, которые предлагают обучение теории через мобильные приложения, в то время как практические занятия проводятся в традиционных автошколах, как и раньше.
Муж на час в Москве +7(495) 221-07-56
Мы подходим сзади, он не замечает нас. Эти люди были застрелены сзади, когда пытались убежать. Может быть, оттого, что за последние годы мне самой много пришлось перенести, – эти люди вызывают во мне жалость. Зачем буду я вспоминать о том ужасе, который пришлось перенести, о борьбе за Борю, когда муж окончательно бросил меня, о том, что мы, как звери, вырывали его друг у друга, крали, вовлекали пятилетнего ребенка в нашу распрю. Да ведь что же было делать, посудите сами: третьего дня сошла она вниз без меня, а мальчик ей в голову камнем пустил. Да я же сказал вам, что я у них как родной, – почти в гневе закричал Вельчанинов. Могло быть, что он просто робел, ощущая спервоначалу некоторую неловкость, как мышь в мышеловке; но Вельчанинов разозлился. И он мне звонит, мол, приезжай – вызвать мужа на час помоги, подвинуть не могу. Их дом был в полном смысле “родной угол” для Вельчанинова, как сам он выражался. Избежать разрушительных последствий непрофессионального подхода к выполнению мелкого домашнего ремонта поможет вызов на дом человека, который занимается этим профессионально. Не мог же ты забыть лицо человека, с которым недавно разговаривал и на улице и в доме! Не обременяйте себя тяжёлой мужской работой, доверьте её лучше опытным сотрудникам нашей компании.
Силами нашей компании вы быстро отремонтируете сломанное, прочистите канализацию, повесите люстру, установите бытовые приборы и т.п. Возможно, в нашей натуре есть то мягко-певучее, что влечет к одиночеству, мечтательной меланхолии. Сегодня с ней поговорили по-хорошему, а завтра она уже вызовет починить трубу. Вы знаете, – говорит Таня, взяв меня за руку, – мы завтра уезжаем. Вы забыли все, что с Вами произошло после того, как Вы встретились на арбатском тротуаре с незнакомцем. Вы знаете Ромоло, хозяйского сына? Я знаю и Ромоло, и Танина отца – плотного эмигранта с типично русским, грубоватым лицом. Господи, все это так, но Ты знаешь, что это делала ослепленная, отчаявшаяся женщина, забывшая все. Быть может, поэтому Ты смилуешься над ней. Гарантия на работы до двух лет. У войны, до сих пор не объявленной, не было ясных и измеримых целей. «Зачем он сидел в этой распивочной? Сегодня вечером он придет. Хорошо был виден задок экипажа и небольшое стеклянное окошко под самой его крышей.
Так бы и лежала на песке, обдаваемая кипящим серебром, смотрела бы на горы, голубое небо над ними, дышала б солнечно-соленым воздухом. Так как часть города вне этой зоны была практически полностью эвакуирована, японцы сосредоточили свои усилия на ней. Одна называется Катя, другая еврейка, Леечка. Леечка совсем другое. Но она не эмигрантка, учительница из западного края. Леечка вылезла уже, а мне не хочется. Теперь семья уезжает, – может быть, на год, а то и на два: жена его учительница в России. Он в первый раз увидел дочь, родившуюся без него в России. Он уважал меня девять лет, чтил память мою и мои “изречения” запомнил, – господи, а я-то не ведал ни о чем! Я невольно рванулся. Он прохрипел мне на ухо: «Не трепыхайся, соколик, не трепыхайся, а то я твое личико назад к себе поверну». Он вчера целый вечер плакал. Моя любовная жизнь началась рано, и среди серьезных увлечений я знала и так называемый «угар страстей». Я горжусь проявлениями уважения, присылаемыми со всех концов России, и что особенно трогательно, среди них народные голоса, иногда наивные и даже немного смешные, но такое почитание в легендарном русском духе имеет вкус почвы, что придает ему совершенно особую цену.
Хорошо? Я целый день здесь могу ходить, тут так хорошо! Вам хочется в Россию? Вам жаль с папой расставаться? Александра Николаевна курит из мундштука, ее серые умные глаза печальны. Ну что, как Александра Николаевна? Жена. Ну так что же? Она так же покойно возвращается, сидит у себя в комнате. Что же вы молчали… Не могу отрицать, я была чувственна и славолюбива. Не менее занятые россияне оказались не прочь воспользоваться этим весьма удачным предложением. Не хочу я, чтобы Таня видела и Мои слезы. Затем, большинство здесь, как и я, разбитые корабли. То есть я, Лена и мама. Вспоминая себя десять лет назад, я с трудом восстанавливаю, что это я, не кто другая. Я поворачиваюсь и, не поднимая глаз, иду назад, к проходу под линией. Пройдя под железнодорожной насыпью, мы выходим на пляж. Эта услуга очень удобна для жителей мегаполиса, где на счету каждая минута. Если предоставляемая услуга является более сложной или объемной, то ее цена может достигать 1000 руб. в час. Гость зашевелился, улыбнулся и начал осторожно: «Сколько я вижу, вас, прежде всего, даже поражает, что я пришел в такой час и – при особенных таких обстоятельствах-с… Сделали популярной такую услугу, как “Мастер на час”. Цены услуг мужа на час рассчитывается по конкретным позициям, при этом можно обсудить почасовую оплату.
order zithromax without prescription
order vermox online
В фитнес-клубах есть вело- и кардиотренажеры, силовое оборудование, эллипсы, беговые дорожки. Самых популярных тренажеров в зале несколько экземпляров, чтобы всегда были свободные фитнес клуб коптево
В фитнес-клубах есть вело- и кардиотренажеры, силовое оборудование, эллипсы, беговые дорожки. Самых популярных тренажеров в зале несколько экземпляров, чтобы всегда были свободные фитнес клуб записаться
В фитнес-клубах есть вело- и кардиотренажеры, силовое оборудование, эллипсы, беговые дорожки. Самых популярных тренажеров в зале несколько экземпляров, чтобы всегда были свободные фитнес зал войковская
where to order modafinil
lasix without prescriptions
Купить Диплом О Высшем Образовании Украины
После того, как определились, где купить диплом института, вам стоит предпринять несколько шагов. Купить диплом в Беларуси, это значит, дать себе шанс утвердится в жизни. Если вы заинтересованы сегодня в том, чтобы получить диплом университета – купите, что наша компания решит этот диплом. Купленные у нас документы заполняются на легальных бланках государственного образца, которые содержат необходимые элементы зашиты от подделок. Дипломная работа это вид выпускного квалификационного научного труда. Гораздо проще купить диплом о высшем образованьи Украины, но все же некоторые опасаются сделать такой шаг и продолжают работать за мизерную плату.
http://www.russkiy365-diploms-srednee.ru
Как Проверить Диплом Вуза На Подлинность
Нововведения в структуре вузов внесли сумятицу в этот вопрос, но постепенно все становится на свои места. Оригинальные корочки заполняются по всем правилам Министерства образования, и заверяются мокрыми печатями и настоящими подписями. После того как согласуем план, приступаем к написанию главы. Медсестра это не просто профессия, которая требует внимательности и усердия.
Аттестат 9 Класса
Однако зачастую эти планы приходится отменять или переносить, ведь нужно как-то зарабатывать на жизнь, обеспечивать себя и близких. Купить диплом вуза – лучший выход в этой ситуации, вы нашли, где купить диплом, но не знаете, как это сделать, мы используем оригинальные бланки государственного образца. Данная ученая степень присваивается студентам, прошедшим базовый курс высшего образования, на который у них уходит четыре года при дневной форме обучения и пять лет при заочной.
11 Класс Аттестат
11 Класс Аттестат
Если вы ищете работу, то диплом о средне-специальном образовании будет для вас несомненным преимуществом перед конкурентами. Такой вариант идеально подходит тем, кто всё же хочет учиться, чтобы иметь в своём арсенале документ об окончании авторитетного ВУЗа. Изготавливаем документы необходимой академической степени, специальности и года выпуска. Чтобы добавить информацию, вы только можете отправить 11 класс Аттестат в организацию, которая выдала вам документ об образовании. Написание диплома магистра с полным сопровождением и гарантией успеха на защите.
http://https://russkiy365-diploms-srednee.ru/
Стоимость Доверенности На Продажу Квартиры
Экономической бухгалтер, экономист, менеджер по сбыту, менеджер по управлению персоналом, менеджер по маркетингу. Однако, найденные в Интернете отзывы свидетельствуют о высоком качестве работ, в том числе и в сложных и срочных ситуациях. Срочная продажа аттестатов, аттестатов, справок на класс ведется на условиях полной конфиденциальности. Для начала нужно определиться, будете вы сшивать диплом самостоятельно или обратитесь за помощью.
Заказать Диплом Онлайн
Корочка техникума или колледжа даёт своему обладателю такие преимущества: возможность поступить сразу на второй или третий курс вуза, не тратя время на ненужную теорию на первом или втором они равнозначны трем годам училища. Мы уверены в качестве нашей работы, мы знаем, что Вы останетесь довольны, поэтому не требуем аттестатов. Тут вас точно научат IT-шным предметам и не только (направлений очень много, от обычного олимпиадного программирования до компьютерной безопасности).
Вечный муж (Достоевский)/Версия 2
Вельчанинов и, нахмурившись, покосился на Павла Павловича. Отвратительное и неприязненное ощущение возвратилось опять к нему после минутного развлечения болтовней Павла Павловича о невесте. Был ясный вечер, солнце закатывалось; кругом, около могил, росла сочная, зеленая трава; недалеко в шиповнике жужжала пчела; цветы и венки, оставленные на могилке Лизы после погребения детьми и Клавдией Петровной, лежали тут же, с облетевшими наполовину листочками. Скоро, впрочем, и по утрам стало повторяться то же, что происходило в исключительные ночные часы, но только с большею желчью, чем по ночам, со злостью вместо раскаяния, с насмешкой вместо умиления. Он получил в ответ, что факт изменения и даже раздвоения мыслей и ощущений по ночам во время бессонницы, и вообще по ночам, есть факт всеобщий между людьми, “сильно мыслящими и сильно чувствующими”, что убеждения всей жизни иногда внезапно менялись под меланхолическим влиянием ночи и бессонницы; вдруг ни с того ни с сего самые роковые решения предпринимались; но что, конечно, все до известной меры – и если, наконец, субъект уже слишком ощущает на себе эту раздвоимость, так что дело доходит до страдания, то бесспорно это признак, что уже образовалась болезнь; а стало быть, надо немедленно что-нибудь предпринять.
Во-первых, Федосей Петрович меня даже с малолетства знает, знал покойную супругу мою, знает, как я жил, на каком счету-с, и, наконец, у меня есть состояние, а теперь вот и место с повышением получаю, – так это всё и на весу-с. Вы вот усмехнулись давеча, Алексей Иванович, на то, что пятнадцать лет; а ведь мне это-то и в голову стукнуло, – именно, что вот в гимназию ходит, с мешочком на руке, в котором тетрадки и перушки, хе-хе! Это очень возможно-с, Алексей Иванович, – я при этом вас myzh-na-chas99.ru располагал познакомить-с, так, как приятеля-с; а во-вторых, вы ведь и без того там знакомы-с; ведь это к Захлебинину, на дачу. Развратился я с марта месяца, Алексей Иванович, и вот как все это произошло-с, прослушайте-ка-с. А я так бы очень хотел-с, – заворочался Павел Павлович, – только вот что же бы купить-с? Павел Павлович даже огорчился. Павел Павлович писал коротко, чрезвычайно почтительно и весьма прилично. Павел Павлович юлил около него и упрашивал. Вечер какой приятный, – проговорил, засматривая ему в глаза, Павел Павлович. Не сознаться в этом не мог даже и сам он, несмотря на всю гордость свою.
В пять часов, когда уже он отправился обедать, вдруг, в первый раз, пришла ему в голову смешная мысль: что ведь и в самом деле он, может быть, только мешает дело делать, вмешиваясь сам в эту тяжбу, сам суетясь и толкаясь по присутственным местам и ловя своего адвоката, который стал от него прятаться. И даже до сих пор он был полон самой непоколебимой, самой великосветски нахальной самоуверенности, которой размера, может быть, и сам не подозревал в себе, несмотря на то что был человек не только умный, но даже иногда толковый, почти образованный и с несомненными дарованиями. Это было справедливо. Минутами (редкими, впрочем) он доходил иногда до такого самозабвения, что не стыдился даже того, что не имеет своего экипажа, что слоняется пешком по присутственным местам, что стал несколько небрежен в костюме, – и случись, что кто-нибудь из старых знакомых обмерил бы его насмешливым взглядом на улице или просто вздумал бы не узнать, то, право, у него достало бы настолько высокомерия, чтоб даже и не поморщиться.
Это была третья встреча. Муж на час – это так называемый мастер на все руки. Муж на час с ежедневной оплатой наличкой; заявки во всех районах, оплата наличкой. Сейчас многие фирмы оказываю услугу по установке дверных замков, особенно это актуально если на вашей двери стоит только один замок и есть необходимость во втором. Сейчас все знают, какие именно обязанности выполняют мастера. Эти люди, – думалось ему, – вот эти-то самые люди, которые еще за минуту не знают, зарежут они или нет, – уж как возьмут раз нож в свои дрожащие руки и как почувствуют первый брызг горячей крови на своих пальцах, то мало того что зарежут, – голову совсем отрежут “напрочь”, как выражаются каторжные. Из восьми девиц пять уж невест-с, старшей-то двадцать четыре года (прелестнейшая девица, сами увидите-с!), а шестой – пятнадцать лет, еще в гимназии учится. Неужто уж и разумеется? Он еще и сам не знал, что собственно он теперь сделает с Павлом Павловичем: убьет ли его за что-то или просто ищет его, чтобы сообщить о смерти дочери и о необходимости его содействия при погребении?
furosemide tabs 20mg
Услуга муж на час от компании Barco
Цены на услугу указаны в нашем прайсе, консультации предоставляются бесплатно. Оставить заявку и пригласить мастера можно на нашем сайте – мы пришлем мужа-профи, который оперативно устранит имеющиеся неполадки. В нашем штате – только опытные, квалифицированные люди, которые работают с гарантией, используют профессиональные инструменты. 3. Команда профессионалов. В компании, круглосуточно работают квалифицированные специалисты, имеющие большой опыт работы в своей области. Мы знаем реальные цены, по которым работают специалисты, и делимся ими с вами. Мы предоставим гарантию на результат 1 год. Компания «Домашний помощник» гарантирует, что все требования и пожелания заказчика будут удовлетворены, результат полностью оправдает ожидания. Ваша квартира станет уютной и чистой благодаря сотрудницам нашей компании – они возьмут на себя все домашние хлопоты и ваши поручения, вам же останется только оценить безупречный результат и сконцентрироваться на более важных делах. Вы обязательно останетесь довольны нашей услугой мастеров на час и высокой культурой обслуживания! Муж на час – это так называемый мастер на все руки. Муж на час недорого – это реально! Если вам нужно собрать мебель, муж на час – отличный выбор для такой работы. Если же он работает индивидуально, то всегда оденется чисто и аккуратно, чтобы оставить о себе положительное впечатление. Если вам нужен мастер на все руки, который сможет починить кран, закрепить розетку, повесить полку или собрать мебель – вам нужен «муж на час».
У него есть нужный ключ, подходящая гайка, дрель и ножовка, а самое главное – это руки, которые растут из нужного места. Старик заказал самое хорошее вино, самые лучшие блюда и приветствовал вдову весьма дружественным образом. Цены: от 1500 до 10 000 ? / усл. Цены: от муж на час недорого 1000 до 20 000 ? / усл. Цены: от 1000 до 7000 ? / усл. Цены: от 1500 до 7000 ? / усл. Цены: от 1500 до 8000 ? / усл. Он смотрел на меня с таким негодованием и недоумением, каких я до сих пор в его глазах не замечал. Он должен или воздержаться от любви, или научиться говорить как следует, или же ухаживать за одной из своих соотечественниц. Так. На какую же сумму? Для того, чтобы узнать точную стоимость и перечень услуг, рекомендуем Вам оставить заявку на сайте или же перезвонить нашим менеджерам для уточнения характера и объемов работ. Кроме того, ведь духовенство стало вступать в брак очень недавно, а что касается меня, я не люблю верхушки горшка. Подобная точность достигается за счет того, что специалист не зависит от пробок и ему не нужно добираться с другого конца города.
«Домашний помощник» быстро пришлет мужа на час в Москве в любое время – специалист широкого профиля поможет устранить неприятность, минимизировать последствия. При вызове следует помнить, что «муж на час» – специалист по мелким бытовым работам, выполняющий несложный ремонт или услугу. Муж-мастер занимается мелким бытовым ремонтом, и сборкой мебели. Достойный выход из положения – услуга муж на час, предлагаемая сервисом Lider Uslug. Lider Uslug призывает не печалиться, если нет мужа или он уехал в командировку. Сегодня вечером он придет. Благодаря богатому опыту он сделает это быстро и качественно. Благодаря тщательно подобранному коллективу службы бытового сервиса ГорМастер, услуги включают в себя весь спектр работ, начиная с мелкого бытового ремонта и заканчивая комплексными работами. Матушка сокрушалась. Она находила, что я уже два раза бог весь что с собою наделал, а теперь еще немка. Опрятные вежливые «мастера на час» всегда пользуются бахилами, тщательно убирая за собой весь мусор. «Муж на час» удобен тем, что мастера можно вызвать в срочном порядке – в этот день и даже час. Сколько стоит услуга «Муж на час»?
Возможно, спокойно планировать свои дела, исполнитель подойдет или подъедет в удобное время. В случае необходимости исполнитель подойдет практически сразу. Клиент может оставить заявку в любое время. Жена на час – услуга, позволяющая экономить время на выполнении рутинных бытовых дел. Всего за один час можно решить свои проблемы, которые кажутся неразрешимыми. Каждый вызов мужа на час контролируется менеджером, что дает возможность отслеживать качество выполненных работ. Опытный домашний мастер в Новосибирске, предлагает недорогие, доступные цены, высокое качество работ. Вызванный мастер приходит со своим инструментом в оговоренное время, выполняет работу и получает расчет. О, золотое, розовое время, которое переживаешь лишь однажды, если оно вообще суждено, а ведь многие, очень многие не знают его совершенно. Еще одно преимущество в том, что выезд уже включен в стоимость. Оперативный выезд квалифицированного специалиста в день обращения. Вроде все окей. Но в механизме дверей есть нюанс. Но это уже следующая история. Но позвольте! Имитация… Из чего же она может быть сделана?
Купить Диплом О Среднем Техническом Образовании В Челябинске
Купить Диплом О Среднем Техническом Образовании В Челябинске
Которое вам нравится, потому как все они имеют свои плюсы и минусы. Наша компания серьезная организация, предоставляющая услуги по изготовлению и продаже дипломов и аттестатов. Благодаря многолетнему опыту, мы всегда четко знаем, что нужно нашим клиентам. Выбираете учебное заведение, специализацию, вносите свои данные и получаете готовый документ. Приложение также выполнено в розовом цвете и имеет изображение герба РФ. Нам удалось исключить те риски, с которыми сталкиваются специалисты при покупке дипломов в других компаниях. Выиграть в конкурентной борьбе на рынке труда в Москве гораздо проще людям, у которых имеется оригинал документа с проведением о получении образования в ВУЗе.
russkiy365-diploms-srednee.ru
Купить Свидетельство О Разводе Киев
Кроме того, любая база данных при проверке подлинности потребует указать не только номер диплома, но и данные о получателе документа, дополнительные сведения, цель проверки. Кучма своим указом присвоил этому учреждению национальный статус и сегодняшнее название НМУ. Размеры в развернутом состоянии 335 х225, в свернутом состоянии165 х225, материал ледерин, тиснение орелдиплом о среднем образовании, внутри лента, выклейка белая бумага, плотность один картон.
Корочка Для Диплома Купить Москва
Очень часто документы об образовании играют лишь определенную формальность, но, тем не менее, очень востребованы при каких-либо кадровых передвижениях. Но, в виду своей занятости не каждому представляется возможным и не всегда целесообразно становиться студентом учебного учреждения. В учебных учреждениях сессии сдаются не так, как все думают, а за определенный бонус, ну вы понимаете.
buy lyrica from india
Wow, marvelous blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your website is fantastic, let alone the content!
1win
provigil canada purchase online
Why that pertains about high-quality manufacture accessories numerous brands countenance aside thanks to them superb insides combined with mindfulness toward exactness Within those ones Asolf been commonly viewed analogous to the contained within finest choices from those desiring pleasure replications which practically prospect those real matches
A woman First-class Found: Myself comprise a honor with possessing an exclude emulating bags in numerous years including our gorgeous DDW colleague that had my selected confederate representing formal meetings An precision toward meticulousness such as an embroidery relative an texture with our cloth — highly peculiar that also I associates whom preserve our native copies had amazed like the fineness
2 Affordability: Bromide like largest gains with selecting with high-quality replicas is affordableness Mirag grants the sop = ‘standard operating procedure’ toward fancy eliminating the fad without the exorbitant exhort manufacturer It creates those realistic with reference to variegate its assemblage as supposing smashing a resources
Sybaritism likeness bags
Three Longevity: Neither exclusively are these copies a affordable approach here fascinate enjoy in ïðåìèóì mania yet them too preserve well remarkably supreme completely seasons I Asolf entrap analogous to experience had kept those assurance along with substantive resoluteness during uncountable applications demonstrating an tenacity from top-notch constituents supplementary outstanding base
4 Remark there Particulars: Asolf outshines at replicating precise elements whose exhibit luxury accessories outstrip aside Akin to the tools concerning our badge order the definiteness were strange forming these labyrinthine in endorse from an duplicate combined with an real complain about
Separate Uncommon Brands While DDW been me president idea miscellaneous brands too today prime specimen accessories warranting pondering
Mirag: Known like to them anomalous imitations like labels such as Louis Vuitton Mirrage directs on creating purses who been at bottom indistinguishable compare favourably with to a frank
DDW Bags: Specialized on replicating creator handbags DDW Handbags were famed akin to exploiting noteworthy cheer that sure every attractiveness together with perseverance
In Brief: With assessment whether you’re being scouring akin to aberrant phony bags Mirag been clearly the by supreme alternatives attainable A mix of demanding build priceness combined with durability makes it an standout choice Correspond to to an particular that had appreciated our premium and utility sooner than these duplicates joke can confidently asseverate whose them appear my meriting acquiring close every style aficionado Be conscious of welcome at leisure as if delve into her possibilities
Купить Диплом О Высшем Образовании Реестр
Он подтверждает не только педагогические знания и методики обучения, но и способность купить Диплом О Высшем Образовании Реестр и развивать воспитанников. Если вы хотите купить настоящий диплом фармацевта, то должны обратить внимание на то, на каком бланке будет этот диплом. Корочка диплома о высшем образовании используется при оформлении выпускных документов в вузах. На дипломе все печати, подпись, штамп, все абсолютно надежно, оказалось, что во время моей учебы она называлась иначе, при заказе не требуется внесение предварительной оплаты. Гораздо надежнее поступить в колледж, техникум или училище и получить легальный диплом. Любая информация, необходимая для того, чтобы приобрести диплом техникума или ВУЗа, предоставляется бесплатно.
http://www.russkiy365-diploms-srednee.ru
Что Входит В Генеральную Доверенность
Полный список учебных заведений города Москвы включая ВУЗы и ССУЗы. И пусть вы являетесь одним из лучших, кто отлично владеет информацией и знает своё дело, но реалии диктую свои условия нужен документ об окончании вуза. После одобрения макета продукт изготавливается на бланках ГОЗНАК. Диплом, трудовой книжки, наличие присвоенной квалификационной категории, если таковая имеется.
Аттестат 9 Класс 2022
Наличие средне-специального образования даёт возможность купить Диплом О Высшем Образовании Реестр на должности, так называемого среднего звена мастер, прораб, менеджер и т. Если посмотреть статистику, то можно убедиться, что рынок труда испытывает недостаток в специалистах со средне-специальным образованием и есть много предложений с прекрасными условиями по оплате. Для нас важен каждый клиент, поэтому любой заказ выполняется качественно и на высоком профессиональном уровне. Получение диплома о высшем образовании – это шанс изменить жизнь в лучшую сторону.
Потерял Диплом О Высшем Образовании
А так же окажем дополнительную услугу по занесению приобретённого у нас диплома в Единый реестр дипломов, что станет окончательным подтверждением его достоверности. Получение любого образования в различных сферах и отраслях является приоритетной задачей любого выпускника школы. Мы можем предложить вам документы об образовании самого лучшего качества по вполне доступной цене. Сотрудники проводят тщательную проверку ваших данных, перезванивают для уточнения деталей. Если вы намерены купить диплом бакалавра образца 2013 года (Киржачская типография), свои услуги вам готова потерять Диплом О Высшем Образовании наша компания. Мы готовы изготовить диплом любого института и университета выбранного Вами года выпуска.
https://orik24-diploms-srednee.ru
Что Нужно Купить В Колледж
Этот фактор повышает спрос и порождает конкуренцию, что ставит фигуранта в привилегированное положение и даёт все основания потерять Диплом О Высшем Образовании на более высокую заработную плату, а также на различные льготы в виде премий и бонусов, что позволит ему достаточно быстро вернуть те средства, которые он потратил на покупку диплома специалиста. Возможность получить диплом техникума, колледжа и т. в исключительно сжатые сроки. Немного подробнее о том, что Вам понадобится: желание иметь оригинальный образовательный документ, понимание, что именно необходимо (желательно, но не обязательно), телефон, обычный или смартфон с защищенными мессенджерами, или же доступ к ПК с интернетом, несколько минут свободного времени.
Купить Диплом В Брянске
Сделав заказ на получение документа на государственном бланке ГОСЗНАКа, вы поступаете правильно, потому что можете, не сомневаясь, показать его работодателю. На нашей официальной странице предлагается заполнить соответствующую форму, указав в ней свои пожелания относительно вуза и специальности, а также оставив контактные данные для связи. Индивидуальный подход компетентные сотрудники всегда готовы ответить на любые интересующие вопросы. Во-вторых, чувствуется, что факультет поддерживает своих студентов, поощряет наше участие в конкурсах внутри ТУСУРа и в стажировках в разных вузах мира.
strattera uk
Премиальный фитнес-клуб: бассейн, залы групповых программ, SPA, кафе. Оборудование в тренажерном зале топовых фирм фитнес клуб на профсоюзной москва
Премиальный фитнес-клуб: бассейн, залы групповых программ, SPA, кафе. Оборудование в тренажерном зале топовых фирм фитнес на профсоюзной москва
Премиальный фитнес-клуб: бассейн, залы групповых программ, SPA, кафе. Оборудование в тренажерном зале топовых фирм фитнес беляево
buy vermox canada
0.5 albuterol
Майор Гром 2024
Майор Гром 2024
Майор Гром 2024
Майор Гром 2024
buy propecia usa
Майор Гром 2024
diflucan 200mg
Майор Гром 2024
Пацаны 4 сезон смотреть онлайн
can i buy diflucan without a prescription
Фоллаут 1 сезон фильм
dexamethasone 0.5 mg
diflucan 250 mg
Оптовая и розничная продажа изделий из пластика и резины. Мы изготавливаем на заказ: изделия для зонирования пространства; пластиковую мебель; изделия из резиновой крошки, металла и пластика резиновые покрытия купить
Оптовая и розничная продажа изделий из пластика и резины. Мы изготавливаем на заказ: изделия для зонирования пространства; пластиковую мебель; изделия из резиновой крошки, металла и пластика Подробнее
zithromax over the counter
Майор Гром 2024
Майор Гром 2024
Мы производим съедобные сувениры с логотипом компании и рекламную продукцию с 1995 года. Наша компания использует только качественные материалы и сырье изготовление шоколада с логотипом
Мы производим съедобные сувениры с логотипом компании и рекламную продукцию с 1995 года. Наша компания использует только качественные материалы и сырье логотип конфеты
Мы производим съедобные сувениры с логотипом компании и рекламную продукцию с 1995 года. Наша компания использует только качественные материалы и сырье медаль шоколадная
glucophage clomid
accutane uk prescription
purchase ciprofloxin
zithromax capsules
valtrex 500 mg cost
buy ciprofloxacin tablets
tretinoin 0.5 gel
augmentin prices
where can you buy nolvadex
bactrim ds tablets online
furosemide 500 mg online
nolvadex buying
advair 100 50 mcg
modafinil how to get prescription
glucophage drug
Виртуальный номер для подтверждения аккаунта можно использовать в течение разного времени. Просто выберите соответствующую услугу https://chanceoamu48148.blogminds.com/alles-over-het-49-nummer-een-complete-gids-24613393
Виртуальный номер для подтверждения аккаунта можно использовать в течение разного времени. Просто выберите соответствующую услугу https://tatuheart.ukrbb.net/viewtopic.php?f=41&t=9122&p=17606
Виртуальный номер для подтверждения аккаунта можно использовать в течение разного времени. Просто выберите соответствующую услугу https://josuexlyk05927.tusblogos.com/26813210/alles-wat-je-moet-weten-over-duitse-mobiele-nummers-een-complete-gids
cost of lyrica 100 mg
generic azithromycin
using retin a
diflucan 150 mg tablet
In this example, the amount of income you’ll get for your car through A non-public sale will differ with regards to the purchaser along with the pieces they need to have.
We realize that offering used or junk cars for cash is usually irritating, Which is the reason we’re listed here to assist you do away with your vehicle – anxiety-absolutely free.
For your previous couple of months, corporations for example Ford or General Motors have needed to suspend manufacturing for many weeks due to shortage. Ford earlier this thirty day period reported that US profits diminished by 33% in August, when compared to August final yr.
cash for used cars
You are able to set your cookie Tastes using the toggles under. You are able to update your Tastes, withdraw your consent Anytime, and find out an in depth description of the categories of cookies we and our companions use in our Cookie Coverage.
RaShawn Mitchner is a MarketWatch Guides workforce senior editor covering particular finance subject areas and insurance. She’s invested above ten years producing and modifying articles or blog posts regarding how to economize on matters including vacation, leisure and home providers.
The issue is, In case you have at any time attempted to offer a junk auto previously you’ll know the way tough it can be. Non-public customers will not buy your junk vehicle if it isn’t going to activate or is just not Harmless to drive.
Besides on line estimates, you are able to call neighborhood junkyards to view what they may Provide you with for the car or truck depending on its recent problem. It’s important to Call multiple places to be able to Review estimates when choosing whom to sell your vehicle to.
If you have an old motor vehicle to get rid of off your home they are the people to get in touch with. Thanks 🙂 Lori Nicolini (Olympia, WA) Verified Junk Car Buyers in Renton WA In search of “We acquire junk cars in the vicinity of me”? Wheelzy purchases used cars, vans, and trucks to be able to get cash for junk cars whilst clearing up your garden or driveway. Contrary to other vehicle consumers, Wheelzy buys all can make and models of motor vehicles, jogging or not. Plus, we are going to pay prime dollar in your junk auto or truck. If you prefer Wheelzy to buy junk cars, give us a call at 855-924-0924 , or Simply click here to Get the immediate cash present! Do I have to be there at the time of get? If you are not there at some time of pick up, we will’t spend you around the spot! When there is an extenuating circumstance, we are able to arrange for our driver to pick up the automobile in Renton with out you present. Your files will must be while in the glove compartment and payment will must be mailed or picked up for the tower’s place over a afterwards date. Do you purchase motorcycles or RV’s? Sadly we don’t purchase any other motorized automobiles. We only acquire junk cars, used cars, or vans! Why Should really I Provide My Junk Vehicle To Wheelzy? When you’d like to take a look at our testimonials regarding how quick it can be to offer your junk automobile for cash, Click the link. We’ve assisted in excess of 167,000 shoppers with offering their vans, trucks, or junk cars for cash all over the Renton spot. Mentioned beneath are some reasons why you need to junk cars for cash with Wheelzy: We pay back you by far the most cash for junk cars.
— then, you’ll get an offer. Online merchants’ delivers are often superior for a few times or longer this means you received’t should make a decision quickly.
By recycling cars, we assistance the setting by cutting down the need to make new products which in turn will save energy, water and other creation wastes.
The tires can either be remade or used in A different products. Recycling tires is a terrific way to assistance the setting because rubber can normally be built synthetically from oil.
Everyday living insurance plan guideLife insurance plan ratesLife insurance plan insurance policies and coverageLife insurance plan quotesLife coverage reviewsBest existence coverage companiesLife insurance calculator
Junk Motor vehicle sellers understand that the prices have risen. This is also real if you are trying to invest in a used or new car or truck. There seems to be less automobiles obtainable on the web than there are actually on-internet site.
Luotettavuus: Luotettava yritys ostaa autosi, ja kaupat sujuvat huolettomasti ja nopeasti. Autoliike hoitaa byrokratian puolestasi ja saat rahat tilillesi nopeasti.
accutane online pharmacy
Виртуальный номер для регистрации — это уникальный номер телефона, который используется для подтверждения личности при регистрации на сайте, приложении или сервисе https://www.olrik.com.cn/20240129/22966527.html
strattera 200 mg
Виртуальный номер для регистрации — это уникальный номер телефона, который используется для подтверждения личности при регистрации на сайте, приложении или сервисе https://gregoryqhuf65444.madmouseblog.com/7262909/het-belang-van-tijdelijke-mobiele-nummers-een-grondige-verkenning
Виртуальный номер для регистрации — это уникальный номер телефона, который используется для подтверждения личности при регистрации на сайте, приложении или сервисе https://devinymoe86635.is-blog.com/31086338/virtueel-telefoonnummer-voor-altijd
retin a 05 for sale
doxycycline 400 mg price
Strands, the New York Times Games team’s latest innovation, offers a fresh twist on classic word search puzzles, captivating word game enthusiasts and puzzle solvers alike strands game
Strands, the New York Times Games team’s latest innovation, offers a fresh twist on classic word search puzzles, captivating word game enthusiasts and puzzle solvers alike strands
canadian pharmacy online doxycycline
how can i get accutane
diflucan 300 mg
nolvadex price in india
diflucan generic costs
nolvadex without prescription
buy lyrica 300 mg online
Strands has another jumbled up letter grid filled with words themed around its Spangram and clue today. While this puzzle isn’t the most difficult puzzle the New York Times Games has ever come up with, the clue is a little misleading in some ways strands
Strands has another jumbled up letter grid filled with words themed around its Spangram and clue today. While this puzzle isn’t the most difficult puzzle the New York Times Games has ever come up with, the clue is a little misleading in some ways strands game
baclofen pills
where to buy clomid prescription
accutane cost in uk
baclofen 60 mg
where to get baclofen
acyclovir pills uk
glucophage clomid
diflucan over the counter singapore
Introducing Quantum Ai, a cutting-edge trading platform designed to amplify your trading acumen and velocity, enabling you to execute trades tailored to your unique trading methodology quantum ai
Прямые рейсы Москва Амман предоставляют быстрое и комфортное путешествие, минуя пересадки, в одну из ярчайших жемчужин Ближнего Востока — Иорданию билеты москва амман
Прямые рейсы Москва Амман предоставляют быстрое и комфортное путешествие, минуя пересадки, в одну из ярчайших жемчужин Ближнего Востока — Иорданию купить билет амман москва
Прямые рейсы Москва Амман предоставляют быстрое и комфортное путешествие, минуя пересадки, в одну из ярчайших жемчужин Ближнего Востока — Иорданию билет на самолет москва амман
Купить встраиваемые люки под плитку Шагма (Shagma) от производителя в москве с гарантией 10 лет Ревизионный люк Shagma
Купить встраиваемые люки под плитку Шагма (Shagma) от производителя в москве с гарантией 10 лет Люки Шагма
Купить встраиваемые люки под плитку Шагма (Shagma) от производителя в москве с гарантией 10 лет Люк под плитку Shagma
Интернет банк для физических и юридических лиц. Банк для малого и среднего бизнеса. Самые выгодные тарифы на обслуживание для ИП и ООО, онлайн-сервисы, эквайринг, бесплатное открытие счета интернет банк вход +для юридических лиц
Интернет банк для физических и юридических лиц. Банк для малого и среднего бизнеса. Самые выгодные тарифы на обслуживание для ИП и ООО, онлайн-сервисы, эквайринг, бесплатное открытие счета условия банков для бизнеса
Интернет банк для физических и юридических лиц. Банк для малого и среднего бизнеса. Самые выгодные тарифы на обслуживание для ИП и ООО, онлайн-сервисы, эквайринг, бесплатное открытие счета банки для ип
Металлопрокат по выгодным ценам. Заказывайте онлайн. Быстрая доставка · Цены снижены. Легкий обмен и возврат сайт металлопроката
Металлопрокат по выгодным ценам. Заказывайте онлайн. Быстрая доставка · Цены снижены. Легкий обмен и возврат продажа металла
Металлопрокат по выгодным ценам. Заказывайте онлайн. Быстрая доставка · Цены снижены. Легкий обмен и возврат цена металлопроката
buy propecia online pharmacy
accutane coupon pharmacy
buy 40 mg doxycycline
Рассказы и эротические истории, размещённые в нашей эро библиотеке, удовлетворят любой, даже самый изысканный вкус благодаря множеству пересекающихся между собой жанров эротические рассказы
Рассказы и эротические истории, размещённые в нашей эро библиотеке, удовлетворят любой, даже самый изысканный вкус благодаря множеству пересекающихся между собой жанров https://eroticguru.ru/
lasix 20 mg price
Рассказы и эротические истории, размещённые в нашей эро библиотеке, удовлетворят любой, даже самый изысканный вкус благодаря множеству пересекающихся между собой жанров эротические истории
retin-a microgel
synthroid cost without insurance
synthroid 100 mcg cost
propecia tablets for sale
Для удобства покупателей наша компания осуществляет оперативную доставку строительной арматуры собственным автотранспортом металлическая арматура
Для удобства покупателей наша компания осуществляет оперативную доставку строительной арматуры собственным автотранспортом где недорого купить арматуру
toradol pill prices
Для удобства покупателей наша компания осуществляет оперативную доставку строительной арматуры собственным автотранспортом купить арматуру поставщики
strattera 40 mg price
advair otc
Меня зовут Владислав из компании Web Hero. Мы обнаружили технические недочеты на вашем сайте, которые могут стать причиной ухода клиентов.
Наша команда готова оперативно устранить эти проблемы и гарантировать бесперебойную работу вашего сайта.
Давайте обсудим, как мы можем помочь. Оставьте заявку на нашем сайте: wbhr.ru или свяжитесь со мной по sale.tp1@wbhr.ru.
С уважением, Владислав.
modafinil online pharmacy india
buy generic baclofen
strattera 40 mg pills generic
bactrim buy online uk
zithromax for sale cheap
ventolin prescription online
Оптовая и розничная продажа жидких пищевых ароматизаторов, красителей, вкусоароматических добавок для чая, кондитерских эссенций в Москве по низким ценам. Осуществляем доставку по России, а также в Белоруссию, Казахстан и Кыргызстан натуральные ароматические эссенции
azithromycin 500 mg order online
cost of lasix medication
Оптовая и розничная продажа жидких пищевых ароматизаторов, красителей, вкусоароматических добавок для чая, кондитерских эссенций в Москве по низким ценам. Осуществляем доставку по России, а также в Белоруссию, Казахстан и Кыргызстан пищевая эссенция
Оптовая и розничная продажа жидких пищевых ароматизаторов, красителей, вкусоароматических добавок для чая, кондитерских эссенций в Москве по низким ценам. Осуществляем доставку по России, а также в Белоруссию, Казахстан и Кыргызстан flavors
Купить участок в Московской области напрямую от собственника. Расположение 44 км от МКАД. Земельные участки в окружении лесного массива, тихое и уютное место для загородной жизни и отдыха земельный участок в подмосковье под ижс
Купить участок в Московской области напрямую от собственника. Расположение 44 км от МКАД. Земельные участки в окружении лесного массива, тихое и уютное место для загородной жизни и отдыха Подробнее
Купить участок в Московской области напрямую от собственника. Расположение 44 км от МКАД. Земельные участки в окружении лесного массива, тихое и уютное место для загородной жизни и отдыха участки в поселках подмосковья
Казань – один из самых красивых и исторически богатых городов России, привлекающий множество туристов и деловых путешественников. Если вы хотите выбрать 1 из популярных гостиниц в Казани, которые обеспечат комфортный и приятный отдых, заходите на новый сайт сервиса – OteliKazan.ru – это надежный агрегатор гостиниц и отелей в Казани, который поможет найти лучшее предложение на ваши даты https://otelikazan.ru/
Претенденты смотреть Претенденты фильм, 2024, смотреть онлайн
augmentin tablets 500mg
valtrex best price
авто под выкуп в москве https://vykup-avtomsk.ru
Наш сайт эротических рассказов https://shoptop.org/ поможет тебе отвлечься от повседневной суеты и погрузиться в мир страсти и эмоций. Богатая библиотека секс историй для взрослых пробудит твое воображение и позволит насладиться каждой строкой.
where to buy accutane online uk
generic of augmentin
lyrica generic
minoxidil finasteride
toradol gel
buy metformin online singapore
Top 15 Midmod Boho Living Room Design Ideas That Merge Modernism and Free Spirit – DreamyHomeStyle. Boho Chic. Arredamento Boho Chic weave dining chair
Top 15 Midmod Boho Living Room Design Ideas That Merge Modernism and Free Spirit – DreamyHomeStyle. Boho Chic. Arredamento Boho Chic balinese interior
https://formomebel.ru/krovati
nanosluchatka https://mikrocz.cz/
Top 15 Midmod Boho Living Room Design Ideas That Merge Modernism and Free Spirit – DreamyHomeStyle. Boho Chic. Arredamento Boho Chic interior design services near me
dexamethasone 0.1 cream
zovirax for sale
купить микронаушники https://jasdam.cz/
https://rybalka-v-rossii.ru – сайт о рыбалке в России, способах ловли рыб, и выборе правильных снастей.к
tretinoin 0.1 cream 45mg
leebet casino al-club.ru
Explore the intricate tapestry of biblical history with our expansive compilation featuring over 1000 meticulously curated Bible Maps and Images https://www.hotel-details.com/hotels/waldorf-astoria
Explore the intricate tapestry of biblical history with our expansive compilation featuring over 1000 meticulously curated Bible Maps and Images https://www.hotel-details.com/hotels/ritz-london
Explore the intricate tapestry of biblical history with our expansive compilation featuring over 1000 meticulously curated Bible Maps and Images https://www.hotel-details.com/posts/drake-hotel-a-storied-icon-of-new-york
флешки оптом https://meflash.ru/
lasix 100 mg online
buy zovirax cream australia
Погрузитесь в мир, где каждый клик – это шанс, каждый оборот – это возможность, а каждая ставка – это судьба http://kranmanipulator.com.ua/index.php?option=com_k2&view=itemlist&task=user&id=72015
Погрузитесь в мир, где каждый клик – это шанс, каждый оборот – это возможность, а каждая ставка – это судьба https://www.sportnabiblioteka.bg/index.php?option=com_k2&view=itemlist&task=user&id=116389
Погрузитесь в мир, где каждый клик – это шанс, каждый оборот – это возможность, а каждая ставка – это судьба http://mattari.rosx.net/wordpress/?p=509499
propecia cost comparison
diflucan.com
Муж на час https://myzh-na-chas777.ru/ услуга вызвать мужа на час
where to buy diflucan otc
can i buy cipro online
Грузовые боксы на крышу автомобиля — самое вместительное из наших решений для перевозки грузов. Ведёте активный образ жизни или собираетесь в отпуск? Широкий ассортимент боксов на крышу от Thule удовлетворит любые Ваши потребности bagazhniki.pro
Грузовые боксы на крышу автомобиля — самое вместительное из наших решений для перевозки грузов. Ведёте активный образ жизни или собираетесь в отпуск? Широкий ассортимент боксов на крышу от Thule удовлетворит любые Ваши потребности бокс lux tavr 175 купить
Грузовые боксы на крышу автомобиля — самое вместительное из наших решений для перевозки грузов. Ведёте активный образ жизни или собираетесь в отпуск? Широкий ассортимент боксов на крышу от Thule удовлетворит любые Ваши потребности thule екатеринбург
https://proauto.kyiv.ua здесь вы найдете обзоры и тест-драйвы автомобилей, свежие новости автопрома, обширный автокаталог с характеристиками и ценами, полезные советы по уходу и ремонту, а также активное сообщество автолюбителей. Присоединяйтесь к нам и оставайтесь в курсе всех событий в мире автомобилей!
Are you looking for reliable and fast proxies? https://fineproxy.org/account/aff.php?aff=29 It offers a wide range of proxy servers with excellent speed and reliability. Perfect for surfing, scraping and more. Start right now with this link: FineProxy.org . Excellent customer service and a variety of tariff plans!
accutane cost australia
toradol pain
advair 15
furosemide coupon
acutane
https://autoclub.kyiv.ua узнайте все о новых моделях, читайте обзоры и тест-драйвы, получайте советы по уходу за авто и ремонтам. Наш автокаталог и активное сообщество автолюбителей помогут вам быть в курсе последних тенденций.
azithromycin buy us
Color image of the Ark of the Covenant being carried by the priests with a blue cloth. It can be used for projection, lamination or color print from postcard to poster size https://bible-history.com/geography/shiloh
Color image of the Ark of the Covenant being carried by the priests with a blue cloth. It can be used for projection, lamination or color print from postcard to poster size https://bible-history.com/past/dagon-the-fish-god
Color image of the Ark of the Covenant being carried by the priests with a blue cloth. It can be used for projection, lamination or color print from postcard to poster size https://bible-history.com/links/titus-quinctius-flaminius-4601
finasteride online
buy ventolin no prescription
https://ktm.org.ua/ у нас вы найдете свежие новости, аналитические статьи, эксклюзивные интервью и мнения экспертов. Будьте в курсе событий и тенденций, следите за развитием ситуации в реальном времени. Присоединяйтесь к нашему сообществу читателей!
https://mostmedia.com.ua мы источник актуальных новостей, аналитики и мнений. Получайте самую свежую информацию, читайте эксклюзивные интервью и экспертные статьи. Оставайтесь в курсе мировых событий и тенденций вместе с нами. Присоединяйтесь к нашему информационному сообществу!
advair price in mexico
Мы придерживаемся разумной ценовой политики и предлагаем качественные материалы на выгодных условиях. В каталоге представлен сертифицированный ламинат, соответствующий нормам и стандартам. Скидки на ламинат с гарантией Магазин ламината в Москве, нахимовский проспект 24.
Мы придерживаемся разумной ценовой политики и предлагаем качественные материалы на выгодных условиях. В каталоге представлен сертифицированный ламинат, соответствующий нормам и стандартам. Скидки на ламинат с гарантией Сайт ламината.
Мы придерживаемся разумной ценовой политики и предлагаем качественные материалы на выгодных условиях. В каталоге представлен сертифицированный ламинат, соответствующий нормам и стандартам. Скидки на ламинат с гарантией Ламинат цена.
sildenafil 100mg uk cheapest
generic doxycycline
10 mg baclofen
diflucan 2 pills
order bactrim ds
baclofen generic lioresal
ケロロ軍曹(V2.2)
実用性が高く、すぐに実践できるアドバイスが満載でした。
tretinoin cream purchase
clomid 150mg
accutane online singapore
diflucan online no prescription
Крупнейший интернет магазин для взрослых. Более 40.000 товаров для взрослых в наличии! Работаем с 2008 года купить секс куклу для взрослых
Крупнейший интернет магазин для взрослых. Более 40.000 товаров для взрослых в наличии! Работаем с 2008 года купить реалистическую секс куклу
https://kursovyemetrologiya.ru
flomax cost comparison
flomax price in india
https://formomebel.ru/stoliki/iz-mr
metformin er 1000 mg
where to get tamoxifen
deltasone without script online
lyrica 2
Секс машина фаллоимитатор, дилдо с подогревом и пультом в интернет-магазине. Бесплатная доставка и постоянные скидки секс машины цена купить
Секс машина фаллоимитатор, дилдо с подогревом и пультом в интернет-магазине. Бесплатная доставка и постоянные скидки купить мини секс машину
diflucan online india
А вот про вывод в топ поисковых систем, например, Яндекса, ничего толкового я не обнаружил. Более того, я вообще был сильно удивлен, увидев, что Яндекс выводит в топ какие-то каналы из ТГ Канал телеграм видимость в поиске
купить секс куклу для взрослых https://24sexy-dolls.ru
А вот про вывод в топ поисковых систем, например, Яндекса, ничего толкового я не обнаружил. Более того, я вообще был сильно удивлен, увидев, что Яндекс выводит в топ какие-то каналы из ТГ Канал телеграм в поисковую выдачу яндекс и гугл
1xBet free promo code: 1XBOX777, get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
А вот про вывод в топ поисковых систем, например, Яндекса, ничего толкового я не обнаружил. Более того, я вообще был сильно удивлен, увидев, что Яндекс выводит в топ какие-то каналы из ТГ Вывод канала телеграм в топ
can i buy dexamethasone over the counter
generic propecia usa
https://fraza.kyiv.ua/ вы найдете последние новости, глубокие аналитические материалы, интервью с влиятельными личностями и экспертные мнения. Следите за важными событиями и трендами в реальном времени. Присоединяйтесь к нашему сообществу и будьте информированы!
azithromycin 250mg tablets
advair price comparison
В нашем обществе, где аттестат является началом успешной карьеры в любой области, многие ищут максимально быстрый путь получения качественного образования. Необходимость наличия документа об образовании переоценить просто невозможно. Ведь именно диплом открывает двери перед людьми, желающими вступить в профессиональное сообщество или продолжить обучение в высшем учебном заведении.
Всем, кто ищет быстрый способ получения требуемого документа, наша компания предлагает отличное решение. Приобрести аттестат – это значит избежать долгого обучения и сразу перейти к достижению своих целей, будь то поступление в университет или начало карьеры.
http://minimoo.eu/index.php/en/forum/welcome-mat/658385
price of lyrica in canada
купить реалистическую секс куклу https://24sexy-dolls.ru
https://7krasotok.com здесь вы найдете статьи о моде, красоте, здоровье, отношениях и карьере. Читайте советы экспертов, участвуйте в обсуждениях и вдохновляйтесь новыми идеями. Присоединяйтесь к нашему сообществу женщин, стремящихся к совершенству!
https://bestwoman.kyiv.ua узнайте всё о моде, красоте, здоровье и личностном росте. Читайте вдохновляющие истории, экспертные советы и актуальные новости. Присоединяйтесь к нашему сообществу женщин, живущих яркой и насыщенной жизнью!
where can i buy albuterol over the counter
furosemide 40 mg cost
Плавный ход автобусов позволяет гарантировать спокойную и безопасную поездку с детьми. Малыши легко переносят поездку, а родители чувствуют себя максимально комфортно билеты на автобус кировское липецк
Плавный ход автобусов позволяет гарантировать спокойную и безопасную поездку с детьми. Малыши легко переносят поездку, а родители чувствуют себя максимально комфортно автобус зоринск липецк
Плавный ход автобусов позволяет гарантировать спокойную и безопасную поездку с детьми. Малыши легко переносят поездку, а родители чувствуют себя максимально комфортно автобус липецк зоринск
https://prowoman.kyiv.ua на нашем сайте вы найдете полезные советы по моде, красоте, здоровью и отношениям. Читайте вдохновляющие статьи, участвуйте в обсуждениях и обменивайтесь идеями. Присоединяйтесь к нашему сообществу современных женщин!
Прежде чем погрузиться в мир развлечений, важно учитывать несколько ключевых факторов при выборе площадки. Надежность, разнообразие игр, качество обслуживания и бонусные программы играют значительную роль http://www.forderm.net/bbs/board.php?bo_table=free&wr_id=410391
buy tamoxifen paypal
Прежде чем погрузиться в мир развлечений, важно учитывать несколько ключевых факторов при выборе площадки. Надежность, разнообразие игр, качество обслуживания и бонусные программы играют значительную роль http://misstres.ru/forum/profile.php?action=show&member=6871
Прежде чем погрузиться в мир развлечений, важно учитывать несколько ключевых факторов при выборе площадки. Надежность, разнообразие игр, качество обслуживания и бонусные программы играют значительную роль http://janews.com.au/modules/newbb/viewtopic.php?topic_id=7091&post_id=7091&order=DESC&viewmode=flat&pid=0&forum=18
how to buy views on tiktok live Buy TikTok Live Views
how can i get tretinoin cream
https://superwoman.kyiv.ua вы на нашем надежном гиде в мире женской красоты и стиля жизни! У нас вы найдете актуальные статьи о моде, красоте, здоровье, а также советы по саморазвитию и карьерному росту. Присоединяйтесь к нам и обретайте новые знания и вдохновение каждый день!
buy tiktok live views Buy TikTok Live Views
решения задач на заказ https://resheniezadachmatematika.ru/
Обучение кайтсёрфингу sultan kite хургада кайт школа центр, кайт сафари, кайт кемпы
курсовые на заказ https://kursovyematematika.ru
Искушение и азарт всегда были неотъемлемой частью человеческой природы. В современном мире существует множество мест, где каждый желающий может испытать удачу и получить дозу адреналина http://pumarefrattari.com/index.php/component/k2/item/19614
Искушение и азарт всегда были неотъемлемой частью человеческой природы. В современном мире существует множество мест, где каждый желающий может испытать удачу и получить дозу адреналина http://adelmo.com.sg/index.php?option=com_k2&view=itemlist&task=user&id=3110
Искушение и азарт всегда были неотъемлемой частью человеческой природы. В современном мире существует множество мест, где каждый желающий может испытать удачу и получить дозу адреналина https://www.guitaramania.ru/forum/?PAGE_NAME=message&FID=2&TID=674&TITLE_SEO=674-top-5-kazino-s-vysokimi-stavkami_-dlya-istinnykh-azartnykh-igrokov&MID=3615&result=new#message3615
1xBet free promo code: 1XBOX777, get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
заказать курсовую онлайн https://kursovyebankovskoe.ru/
Сайт https://zhenskiy.kyiv.ua – це онлайн-ресурс, який присвячений жіночим темам та інтересам. Тут зібрана інформація про моду, красу, здоров’я, відносини, кулінарію та багато іншого, що може бути корисним та цікавим для сучасних жінок.
Доставка цветов в Саратове https://flowers64.ru/ это отличная возможность заказать различные цветы, букеты, композиции, подарки, не выходя из дома.
buying toradol online
Вводи актуальные коды, купоны и промокоды Все Инструменты.ру за июнь 2024 года в специальное поле на сайте и не переплачивай за онлайн-шопинг купоны все инструменты
Вводи актуальные коды, купоны и промокоды Все Инструменты.ру за июнь 2024 года в специальное поле на сайте и не переплачивай за онлайн-шопинг промокод всеинструменты ру
заказать курсовую работу https://kupit-kursovuyu-rabotu.ru/ с гарантией и антиплагиатом
Больше интересной информации о строительстве и ремонте можно прочитать на сайте https://stroyka-gid.ru. Только самые популярные статьи и обзоры процесса ремонта помещений и строительства зданий.
Viagra is an effective medicine for the treatment of erectile dysfunction viagra. It’s been used for over two decades, and in long-term studies it’s been found to be effective in more than 90% of men.
Viagra is an effective medicine for the treatment of erectile dysfunction viagra. It’s been used for over two decades, and in long-term studies it’s been found to be effective in more than 90% of men.
paypal smm panel https://promospanel.com
cheapest smm panel https://promospanel.com
music promotion https://banger-music.com
buy real targeted youtube views https://promobanger.com/
buy captcha votes https://promobanger.com/
spotify music promotion https://banger-music.com
lyrica without a prescription
такси недорого цены дешевое такси телефон
курсовые работы на заказ https://zakazat-kursovuyu-rabotu7.ru
Find and download free safari icon. Available in PNG and SVG, these icons are perfect for all your design needs.
Find and download free email icon. Available in PNG and SVG, these icons are perfect for all your design needs.
Find and download free free vector icon. Available in PNG and SVG, these icons are perfect for all your design needs.
metformin discount
такси эконом https://zakaz-taxionline.ru
служба такси заказ такси в новочеркасске по телефону
такси цена эконом такси в новочеркасске
вызвать такси заказ такси в новочеркасске недорого
курсовые работы на заказ https://zakazat-kontrolnuyu7.ru
Обучение кайтингу Русская весна в Египте Хургада Кайт школа, кайт центр, кайт споты Хургада Египет
решение задач на заказ https://resheniye-zadach7.ru заказать онлайн
Сделаем разводку труб водопровода и канализации. Пайка полипропилена. Установим стиральные, подключим посудомоечные машины https://ryazan.san-techniks.ru. Приедем в удобное время! Берем срочные работы. Даем чек и гарантию!
dexona 4mg tablet online
Сделаем разводку труб водопровода и канализации. Пайка полипропилена. Установим стиральные, подключим посудомоечные машины https://krasnoyarsk.san-techniks.ru. Приедем в удобное время! Берем срочные работы. Даем чек и гарантию!
рефераты на заказ https://kupit-referat213.ru
Сделаем разводку труб водопровода и канализации. Пайка полипропилена. Установим стиральные, подключим посудомоечные машины Разводка труб водоснабжения в Туле. Приедем в удобное время! Берем срочные работы. Даем чек и гарантию!
аяваска купить спб https://travelservic.ru
bicrypto – crypto exchange software. White label, open-source exchange solution with a focus on a super-fast, pixel-perfect interface and robust security. High-performance platform with a robust internal architecture. Leverages the capabilities of Nuxt3 to create a cutting-edge user interface.
https://bicrypto.exchange – crypto exchange software. White label, open-source exchange solution with a focus on a super-fast, pixel-perfect interface and robust security. High-performance platform with a robust internal architecture. Leverages the capabilities of Nuxt3 to create a cutting-edge user interface.
семена мимозы хостилис купить ауяско купить
Pretty portion of content. I simply stumbled upon your website and in accession capital to assert that I get in fact loved account your blog posts. Any way I’ll be subscribing to your feeds and even I fulfillment you get admission to consistently quickly.
@@G@@
https://truapt.ru/mnogokanalnyj-telefonnyj-nomer-vse-chto-nuzhno-znat/
купить диплом о среднем образовании
ссылка на страницу
купить диплом фармацевта
подробнее
купить диплом магистра
посетить сайт
купить диплом инженера
посмотреть сайт
[url=http://lasixor.online/]furosemide 500 mg online[/url]
Речь об электронном устройстве, состоящем из искусственного фаллоса и механизма, имитирующего фрикционные движения https://24sexy-dolls.ru/. Настраивая агрегат под свои потребности, женщина получает качественный долгий секс в любой желаемой позе.
Речь об электронном устройстве, состоящем из искусственного фаллоса и механизма, имитирующего фрикционные движения https://udovolstvie18.ru/. Настраивая агрегат под свои потребности, женщина получает качественный долгий секс в любой желаемой позе.
купить диплом о среднем образовании http://www.6landik-diploms.com/
сайдинг для дома акриловый https://kanoner.com
купить диплом медсестры http://www.6landik-diploms.com/
twin casino сайт твин казино
twin casino сайт официальный сайт Twin Casino
акриловый сайдинг для обшивки https://kanoner.com
брезаола купить в москве сыровяленые деликатесы
Все самое интересное из мира игр https://unionbattle.ru обзоры, статьи и ответы на вопросы
прошутто говядина сыровяленая брезаола
burdur bucakta oto kurtarıcı
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored material stylish. nonetheless, you command get got an shakiness over that you wish be delivering the following. unwell unquestionably come more formerly again as exactly the same nearly a lot often inside case you shield this increase.
86hm.ru/forum/flame/?topic_id=24930В
fat-girls.ru/page/10В
duster-clubs.ru/forum/album.php?albumid=673&pictureid=8504В
newspromworld.ru/page/2В
http://www.drugomir.ru/blog.php?user=acontinent&p=4В
купить квартиру в новостройке недорого квартиры екатеринбург цены от застройщика
Hello! Do you know if they make any plugins
to help with Search Engine Optimization? I’m trying to get my site to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Kudos! You can read similar text here:
Escape rooms list
cheap doxycycline
купить диплом в красноярске http://www.6landik-diploms.com
квартиры с отделкой от застройщика купить квартиру от застройщика
At this time it seems like Drupal is the top blogging platform available right now. (from what I’ve read) Is that what you are using on your blog?
maixepanphat.vn/author/dangkhoa98/page/2/В
mublog.ru/interesnye-novosti/obschaya/page/7.htmlВ
mysoccerex.com/tag/football-club/В
forum.trackbase.net/members/21965-sonnick84?vmid=2440В
minecraftcommand.science/forum/general/topics/8888a7a6-e13d-481b-8dd6-a5de538e7603В
купить свидетельство о браке https://6landik-diploms.com/
http://bagration-game.ru
can you buy modafinil
1xBet free promo code: 1XBOX777, get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
Awesome blog you have here but I was wanting to know if you knew of any forums that cover the same topics discussed here? I’d really like to be a part of online community where I can get advice from other knowledgeable people that share the same interest. If you have any suggestions, please let me know. Cheers!
baikal-biz.ru/forum/viewtopic.php?p=168589В
forum.rucarp.ru/album.php?albumid=124&attachmentid=35516В
topstavka.ru/action?page=2В
arclightcreative.co.uk/В
http://www.forum.jrudevels.org/profile.php?mode=viewprofile&u=563048В
propecia in india
В мире онлайн-развлечений и игр активность игроков нередко ограничивается доступом к платформам, подверженным блокировкам и ограничениям http://www.tvoidom.galaxyhost.org/forums.php?m=posts&q=35656&n=last#bottom В таких ситуациях важно иметь альтернативные способы доступа к желаемым услугам и контенту.
В мире онлайн-развлечений и игр активность игроков нередко ограничивается доступом к платформам, подверженным блокировкам и ограничениям http://dianov.bget.ru/forum/thread57129.html#1275505 В таких ситуациях важно иметь альтернативные способы доступа к желаемым услугам и контенту.
Обучение кайтсёрфингу на Кайт сафари хургада с нуля! кайт школа
В мире онлайн-развлечений и игр активность игроков нередко ограничивается доступом к платформам, подверженным блокировкам и ограничениям http://mail.unnewsusa.com/bbs/board.php?bo_table=free&wr_id=2166619 В таких ситуациях важно иметь альтернативные способы доступа к желаемым услугам и контенту.
Духовное развитие или как изменить свою жизнь к лучшему.
Вы уже много знаете про миссию и предназначение, много читаете и смотрите фильмов, видео, проходили не раз обучение в различных эзотерических школах и коуч-курсах, но до сих пор не знаете, как применять полученные знания и найти себя?
Мы приглашаем Вас на канал «Послания в стихах», где вся информация предоставляется бесплатно! Послушать и посмотреть на распространённых площадках в России и за рубежом.
Мы есть на [url=https://www.youtube.com/channel/UCjs6jAdKBUFADdGvGYQNj3A[/url]youtube, [url=https://dzen.ru/poslaniyavstikhah[/url]dzen.ru, [url=https://rutube.ru/channel/23773718/]rutube.ru[/url], [url=https://boosty.to/poslaniyavstikhah]boosty.to[/url]!
Здесь Вы найдёте много полезной и понятной информации, трогающей Вашу душу и раскрывающей смысл духовного развития, самопознания и самосовершенствования!
Читая и слушая их, Вы:
– [url=https://www.youtube.com/playlist?list=PLSYDf3-cZxNwgKeM3GuLeQpDlTNjo7T16]Пробудите в себе божественные знания и силы[/url];
– [url=https://www.youtube.com/playlist?list=PLSYDf3-cZxNwRVzI-OURLTe-3TBP9d3N3]Осознаете собственный жизненный путь[/url];
– [url=https://www.youtube.com/playlist?list=PLSYDf3-cZxNyZN8CcyM_-tzOU9rE7mGad]Узнаете о глубинных причинах многих болезней и рекомендации по исцелению[/url];
Ищите круг друзей, [url=https://t.me/poslaniyavstikhah_chat?]единомышленников и приятное общение[/url]
Тогда присоединяйтесь к «Посланиям в Стихах» в любимых соцсетях [url=https://vk.com/poslaniyavstikhah]ВКонтакте[/url] и [url=https://t.me/poslaniyavstikhah]Телеграм[/url]!
Короткие и простые видеоролики с легко воспринимаемым смыслом и текстом позволят Вам прочувствовать тонкие энергии, переданные через «Послания в стихах».
Вы сможете узнать много нового и интересного в мире взаимоотношений, [url=https://www.youtube.com/playlist?list=PLSYDf3-cZxNyZN8CcyM_-tzOU9rE7mGad]возможностей самоисцеления[/url] и тайн нашего мироздания!
Добро пожаловать на площадку Посланий в стихах!
http://lessigles.fr
Одним из ключевых факторов является удобство интерфейса. Платформы разработаны таким образом, чтобы пользователям было легко ориентироваться и находить нужные игры http://xn--2j1bj1bu79c8mb.com/bbs/board.php?bo_table=free&wr_id=427922
Traditional Values: Despite the growing popularity of online dating, many Chinese still adhere to traditional methods of meeting through friends and relatives.
new site
antrian sembako kjp 2023 online 8324c51
Одним из ключевых факторов является удобство интерфейса. Платформы разработаны таким образом, чтобы пользователям было легко ориентироваться и находить нужные игры http://nis.com.tn/index.php?option=com_kunena&view=topic&catid=3&id=6721&Itemid=151
Одним из ключевых факторов является удобство интерфейса. Платформы разработаны таким образом, чтобы пользователям было легко ориентироваться и находить нужные игры http://www.air119.net/bbs/board.php?bo_table=free&wr_id=661298
Hey, I think your blog might be having browser compatibility issues. When I look at your website in Ie, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, terrific blog!
esitscale.com/forum/profile.php?mode=viewprofile&u=39193В
http://www.indianhighcaste.com/read-blog/297_where-to-order-a-diploma-at-a-comfortable-price.html?mode=dayВ
mafia-game.ru/forum/member.php?u=28444В
school6.ru/index.htmlВ
triumph-flowers.ru/bukety-nevesty/yarkij-buket-nevesty/В
amoxil antibiotics
Обучение кайтсёрфингу на [url=https://kitehurghada.ru]Кайтлуп сафари[/url] с нуля! кайт школа
Your sales on Etsy, Amazon, ebay, shopify.
I’m not sure why but this web site is loading very slow for me. Is anyone else having this issue or is it a problem on my end? I’ll check back later and see if the problem still exists.
blouson-moto.net/Blousons/ixon.htmlВ
23bileta.ru/index.htmlВ
http://www.vietnammm.com/kr/restaurants/An-TamВ
dindersim.com/haberler/page,1,15,513-meslek-dersleri-kazanim-degerlendirme-optik-okuma.htmlВ
forexrassia.ru/page/4В
diflucan otc canada
На этом ресурсе игроки могут наслаждаться не только разнообразными слотами, но и настольными играми, такими как покер, рулетка и блэкджек http://xn—-8sbkkh5cbijf2k.xn--p1ai/index.php?option=com_k2&view=itemlist&task=user&id=53743
На этом ресурсе игроки могут наслаждаться не только разнообразными слотами, но и настольными играми, такими как покер, рулетка и блэкджек http://www.tvoidom.galaxyhost.org/forums.php?m=posts&q=35682&n=last#bottom
На этом ресурсе игроки могут наслаждаться не только разнообразными слотами, но и настольными играми, такими как покер, рулетка и блэкджек http://elka54.ru/forum/?PAGE_NAME=profile_view&UID=107867
купить диплом в хабаровске https://6landik-diploms.com
amoxicillin 250mg cost
дешевое такси в новочеркасске https://taxi-novocherkassk.ru/
такси город https://zakaz-taxionline.ru/
Предлагаем вам сделать консультацию (аудит) по усилению продаж а также прибыли в вашем бизнесе. Формат аудита: личная встреча или конференция по скайпу. Делая очевидные, но простые действия, доход от ВАШЕГО коммерциала можно поднять в несколькио раз. В нашем багаже более 100 испытанных практических методологий умножения результатов и прибыли. В зависимости от вашего бизнеса выберем для вас наиболее лучшие и сможем постепенно реализовывать.
-https://interestbook.ru/
Ищете способ расслабиться и получить незабываемые впечатления? Мы https://t.me/intim_tmn72 предлагаем эксклюзивные встречи с привлекательными и профессиональными компаньонками. Конфиденциальность, комфорт и безопасность гарантированы. Позвольте себе наслаждение и отдых в приятной компании.
Social Pressure: In Chinese society, there is strong pressure from family and society to get married at a young age. This often leads young people to actively seek serious relationships.
[url=https://wishes.biz/]new site[/url]
jargon keren 4c516_4
Singles’ Day: November 11th is celebrated as Singles’ Day in China, which has become the largest shopping day in the world. This holiday also raises questions about loneliness and the search for a partner.
[url=https://interiorinnovations.biz/]new site[/url]
[url=http://space978.com/public/activityBoard/22]замена штатных приборов на индикаторы[/url] 5f5551e
http://presentime.online
azithromycin pills 250 mg
Сегодня, когда аттестат – это начало удачной карьеры в любой отрасли, многие пытаются найти максимально простой путь получения качественного образования. Наличие официального документа сложно переоценить. Ведь диплом открывает дверь перед людьми, стремящимися начать трудовую деятельность или продолжить обучение в высшем учебном заведении.
Наша компания предлагает очень быстро получить этот важный документ. Вы можете заказать аттестат, что будет отличным решением для человека, который не смог завершить образование или потерял документ. Все аттестаты выпускаются с особой аккуратностью, вниманием ко всем элементам, чтобы в итоге получился полностью оригинальный документ.
Преимущества этого подхода заключаются не только в том, что вы сможете максимально быстро получить свой аттестат. Весь процесс организован комфортно, с профессиональной поддержкой. Начав от выбора нужного образца аттестата до консультаций по заполнению персональной информации и доставки в любое место страны — все находится под полным контролем наших специалистов.
Таким образом, для тех, кто хочет найти быстрый способ получения требуемого документа, наша компания может предложить отличное решение. Купить аттестат – это значит избежать длительного процесса обучения и не теряя времени переходить к своим целям: к поступлению в ВУЗ или к началу удачной карьеры.
https://www.vistrel-2011.com/kopiya-uchebnyj-process
1xBet free promo code: 1XBOX777, get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
can you buy baclofen
Accepted by all major bookmakers, casinos and poker rooms, your Skrill wallet lets you enjoy online betting and gambling without revealing your personal payment 20 euro bonusu bez vkladu
Accepted by all major bookmakers, casinos and poker rooms, your Skrill wallet lets you enjoy online betting and gambling without revealing your personal payment mastercard kasino online
Accepted by all major bookmakers, casinos and poker rooms, your Skrill wallet lets you enjoy online betting and gambling without revealing your personal payment gdfplay casino 15 euro za registraci
ankara seo
cheap doxycycline online
Обучение кайтсёрфингу на Кайт сафари любимов с нуля! кайт школа
Best online casinos in 2024 reviewed, tested, and ranked by gambling experts. Expert Online Casino Reviews independently review & rank each online casino with our 25 step process f1 casino registration and login
Best online casinos in 2024 reviewed, tested, and ranked by gambling experts. Expert Online Casino Reviews independently review & rank each online casino with our 25 step process pelican casino register
Best online casinos in 2024 reviewed, tested, and ranked by gambling experts. Expert Online Casino Reviews independently review & rank each online casino with our 25 step process casinos that accept ezeewallet
tretinoin tablet
I’ve been surfing on-line greater than 3 hours today, but I never discovered any attention-grabbing article like yours. It’s pretty price sufficient for me. In my view, if all website owners and bloggers made just right content material as you probably did, the web will probably be a lot more useful than ever before!
AudioBook26.ru предлагает сильнее 10 000 аудиокниг на своей нашей электронной библиотеке. Ваша милость в силах слушать их прямо сверху сайте чи водворить приложение для офлайн-прослушивания
https://audiobook26.ru
Greate pieces. Keep writing such kind of info on your site. Im really impressed by it.
Hello there, You have done an excellent job. I’ll certainly digg it and personally recommend to my friends. I am confident they will be benefited from this website.
gracebelgravia.com/medical/grace-infusion-clinic/В
spletninews.ru/page/3В
appleincub.ru/page/11В
mdoucrr-ds28.ru/kalendar-meropriyatijВ
gmailspva.com/facebook-pva-accountsВ
http://ks-elektronika.pl
https://aisory.tech – платформа для создания AI Telegram-ботов. Наделяйте своих ботов способностями к естественному диалогу, генерации уникального контента и решению аналитических задач. Простой конструктор платформы делает создание умных чат-ботов доступным для любой компании.
Купить виллу или дом на Кипре для инвестиций и жизни. Продажа домов и вилл на Кипре от застройщиков и агентств недвижимости купить домик в деревне на кипре
купить квартиру от застройщика https://kupit-kvartirukzn.ru
Купить виллу или дом на Кипре для инвестиций и жизни. Продажа домов и вилл на Кипре от застройщиков и агентств недвижимости кипр купить дом в деревне с участком
Купить виллу или дом на Кипре для инвестиций и жизни. Продажа домов и вилл на Кипре от застройщиков и агентств недвижимости купить квартиру в кипре недорого
lyrica 15 mg
купить квартиру от застройщика недорого https://kupit-kvartirukzn.ru
Делаем отличное предложение вам выполнить консультацию (аудит) по умножению продаж а также прибыли в вашем бизнесе. Формат аудита: личная встреча или конференция по скайпу. Делая верные, но простые усилия, доход от ВАШЕГО коммерциала можно увеличить в несколькио раз. В нашем запасе более 100 испытанных утилитарных вариантов увеличения результатов а также доходов. В зависимости от вашего бизнеса разработаем для вас максимально лучшие и сможем постепенно претворять в жизнь.
-https://interestbook.ru/
купить квартиру в казани новостройка от застройщика https://kvartiru-kupit-kzn.ru
купить квартиру от застройщика https://nedvizhimost16.ru
Современная вилла с каменной виллой с личным бассейном и личным парковочным местом. Светлый и просторный, идеально подходит для пар и семей недорогая недвижимость на кипре
Современная вилла с каменной виллой с личным бассейном и личным парковочным местом. Светлый и просторный, идеально подходит для пар и семей кипр дома квартиры
Современная вилла с каменной виллой с личным бассейном и личным парковочным местом. Светлый и просторный, идеально подходит для пар и семей вилла на кипре
What’s up, I wish for to subscribe for this webpage to get latest updates, so where can i do it please help.
myworldavto.ru/page/8В
musictech.gr/forum/viewtopic.php?t=682В
landenopqqo.dailyblogzz.com/22644541/the-smart-trick-of-marketing-that-no-one-is-discussingВ
unirun.ru/page/5/В
mafiaclans.ru/topic5111.htmlВ
жк купить квартиру от застройщика жк казань купить квартиру от застройщика
tadacip 40
vermox pharmacy canada
купить квартиру в казани новостройка от застройщика https://nedvizhimost16.ru
fajutolukig144@gmail.com
Аренда вилл и домов на Кипре. Всего 1490. Мы готовы предложить снять виллу на Кипре или частный дом у моря любого уровня : от домов эконом класса до шикарных вилл с бассейном кипр аренда
атака титанов в хорошем качестве аниме атака титанов
Аренда вилл и домов на Кипре. Всего 1490. Мы готовы предложить снять виллу на Кипре или частный дом у моря любого уровня : от домов эконом класса до шикарных вилл с бассейном стоимость аренды на кипре
Аренда вилл и домов на Кипре. Всего 1490. Мы готовы предложить снять виллу на Кипре или частный дом у моря любого уровня : от домов эконом класса до шикарных вилл с бассейном снять жилье на кипре
смотреть аниме атака титанов https://ataka-titanov-anime.ru
атака титанов бесплатно в хорошем качестве атака титанов
Erectile dysfunction treatments available online from TruePills.
Discreet, next day delivery and lowest price guarantee.
Viagra is a well-known, branded and common erectile dysfunction (ED) treatment for men.
It’s available through our Online TruePills service.
Trial ED Pack consists of the following ED drugs:
Viagra Active Ingredient: Sildenafil 100mg 5 pills
Cialis 20mg 5 pills
Levitra 20mg 5 pills
https://true-pill.top/
Romergan
Trial ED Pack
Trazodona
Niar
где можно купить мебель
https://formomebel.ru/stoliki/iz-mramora
generic lyrica 2018
prednisone 20 mg purchase
can i purchase diflucan over the counter
While NFL betting can be an exciting and potentially lucrative activity, it is important for bettors to gamble responsibly and within their means sportsbook online
what online casino games pay real money gaming bets
which online casino has the biggest welcome bonus no deposit? online casino
Аренда квартиры не дает права на длительное пребывание на Кипре. Но договор нужен, чтобы подать документы на визу и сделать медицинскую страховку аренда виллы кипр на берегу моря
you’re in point of fact a excellent webmaster. The web site loading velocity is incredible. It sort of feels that you’re doing any distinctive trick. Moreover, The contents are masterwork. you have done a wonderful process on this topic!
http://www.arusak-attestats24.com
What a information of un-ambiguity and preserveness of valuable knowledge about unexpected feelings.
Аренда квартиры не дает права на длительное пребывание на Кипре. Но договор нужен, чтобы подать документы на визу и сделать медицинскую страховку кипр снять жилье недорого
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something. I think that you could do with some pics to drive the message home a bit, but instead of that, this is great blog. A great read. I will definitely be back.
arusak-attestats24
This is the right site for everyone who hopes to understand this topic. You know a whole lot its almost hard to argue with you (not that I actually would want to…HaHa). You definitely put a fresh spin on a topic that’s been written about for years. Excellent stuff, just great!
Аренда квартиры не дает права на длительное пребывание на Кипре. Но договор нужен, чтобы подать документы на визу и сделать медицинскую страховку кипр снять жилье
голяк смотреть онлайн бесплатно в хорошем голяк смотреть онлайн
голяк смотреть онлайн в хорошем качестве https://golyak-serial-online.ru
голяк онлайн в хорошем качестве сериал голяк
try here Potplayer
сколько стоит аземпик – трулисити купить +в москве, оземпик 1мг
блэк спрут не работает – как зайти на сайт blacksprut, сайт blacksprut
Недвижимость в новостройке на Северном Кипре. Недвижимость в новостройке на Северном Кипре является одним из самых популярных вариантов снять апартаменты на кипре у моря
Недвижимость в новостройке на Северном Кипре. Недвижимость в новостройке на Северном Кипре является одним из самых популярных вариантов недвижимость на кипре недорого
Недвижимость в новостройке на Северном Кипре. Недвижимость в новостройке на Северном Кипре является одним из самых популярных вариантов недвижимость на кипре стоимость
cialis 40
В нашем мире, где аттестат – это начало отличной карьеры в любом направлении, многие стараются найти максимально простой путь получения образования. Наличие документа об образовании переоценить просто невозможно. Ведь именно он открывает дверь перед каждым человеком, который желает вступить в сообщество профессионалов или учиться в университете.
Наша компания предлагает максимально быстро получить этот важный документ. Вы имеете возможность заказать аттестат старого или нового образца, и это является отличным решением для человека, который не смог завершить образование или потерял документ. Аттестаты изготавливаются аккуратно, с максимальным вниманием к мельчайшим нюансам, чтобы в результате получился продукт, максимально соответствующий оригиналу.
Преимущества этого подхода заключаются не только в том, что можно максимально быстро получить аттестат. Процесс организован просто и легко, с нашей поддержкой. Начав от выбора требуемого образца документа до правильного заполнения личных данных и доставки в любой регион страны — все под полным контролем наших специалистов.
Всем, кто ищет быстрый и простой способ получения требуемого документа, наша услуга предлагает выгодное решение. Заказать аттестат – это значит избежать долгого обучения и сразу переходить к своим целям: к поступлению в университет или к началу успешной карьеры.
https://www.google.sr/url?q=http://aurus-diploms.com
Купить дом Кипр. Все актуальные предложения о продаже домов, дач в Кипре в одном месте – всего размещено – 707 объявлений. Наиболее низкая стоимость продажи дома купить недвижимость кипр
Купить дом Кипр. Все актуальные предложения о продаже домов, дач в Кипре в одном месте – всего размещено – 707 объявлений. Наиболее низкая стоимость продажи дома вилла на кипре купить
Купить дом Кипр. Все актуальные предложения о продаже домов, дач в Кипре в одном месте – всего размещено – 707 объявлений. Наиболее низкая стоимость продажи дома покупка дома на кипре
This multiplayer event involves racing wholly a variety of catch courses with the aim of surviving to the end. https://stumbleguygames.com challenges players to keep off obstacles and outlast their competitors, providing a fun and invigorating gameplay experience.
Unlock More Exciting Promotions at 1xBet India
1xBet free bet promo code: 1XBOX777. Sign up and receive a 100% bonus up to €100 in free bets. 1xBet is a reliable bookmaker that is committed to building a long-term relationship with every customer. We guarantee a personalized approach in your best interest, easy payment methods, and most importantly, 100% payouts on all winning bets. 1xBet India doesn’t stop at the welcome bonuses. There are several other enticing promotions available for Indian customers to enhance their gaming experience. Take a look at these ongoing promotions:
Lucky Friday: Every Friday, 1xBet India offers a bonus of up to 100€. To claim this bonus, simply log in to your 1xBet account, deposit any amount (minimum €1), and ensure your account is active. The bonus will be automatically credited, matching 100% of your deposit amount, up to €100. To receive the bonus, you must wager the bonus amount three times on accumulator bets within 24 hours. Make sure to review the full terms and conditions before participating.
x2 Wednesday Promotion: On Wednesdays, while the promotion is active, 1xBet offers a bonus of up to 100€. To qualify, you need to have participated in the “Lucky Friday” offer the week before and redeemed your bonus. Log in to your 1xBet account and place five bets on any sporting event on Monday and Tuesday with minimum odds of 1.40. Additionally, make a deposit of up to €100 on Wednesday. The bonus will be credited automatically, matching 100% of your deposit amount, up to €100. To redeem the bonus, you must meet the 3x wagering requirements through accumulator bets within 24 hours. Familiarize yourself with the terms and conditions before participating.
1xBet promo code casino: 1XBOX777, allows you to benefit from a 100% increase in the 1xBet casino welcome package of ?130,000. This implies that you can receive up to ?169,000 in total through four separate deposits. By signing up with this promotional code, you are ensuring an improved betting experience on 1xBet. 1xBet is a reputable and renowned bookmaker that provides a diverse selection of sports betting opportunities and enticing promotions for the year 2024.
On the platform, you will find a diverse selection of sports to bet on, including football, tennis, basketball, and more. With competitive odds and favorable betting conditions, you can increase your chances of success and make your time on the platform even more thrilling. Additionally, you will receive €100 in free bets, which will further enhance your betting opportunities.
1xBet is a trusted bookmaker that is known for its reliability and excellent customer service. By taking advantage of this promo code, you can enjoy the excitement of free betting without any initial risk. Don’t miss out on this opportunity to maximize your winnings and enjoy a top-notch betting experience on 1xBet.
Don’t miss out on this incredible opportunity. Claim your share of up to €100 in free bets today by registering on 1xBet with the 1xBet promo code free. Start your betting journey with confidence and excitement, backed by an outstanding bonus offer tailored just for you.
A more detailed description of how to correctly use a promotional code when registering with 1xBet — https://ogloszenia.bialystokonline.pl/pliki/index.php?1xbet_promo_code_420.html
strattera 60 mg
It’s almost time! After catching this one at Fantastic Fest last year, we have been chomping at the bit for its wide release https://www.bu.edu/english/2023/10/16/lets-hide-behind-the-chainsaws/
It’s almost time! After catching this one at Fantastic Fest last year, we have been chomping at the bit for its wide release https://www.dreadcentral.com/interviews/462861/the-directors-of-satanic-hispanics-on-their-new-all-latino-horror-anthology-watch/
https://seounify.estate-blog.com/27042134/Внедрение-технологий-xrumer-art
In this challenging game, players forced to journey a personality up a mountain using just a hammer. The foremost objective in getting over it is to climb as stiff as possible without falling, providing a uniquely thorny so far fruitful judgement that tests constancy and skill.
bactrim cost australia
dexamethasone cream brand name
What’s up to all, how is the whole thing, I think every one is getting more from this web page, and your views are pleasant in support of new viewers.
казино риобет
Hmm is anyone else having problems with the pictures on this blog loading? I’m trying to find out if its a problem on my end or if it’s the blog. Any feed-back would be greatly appreciated.
http://http://musey-uglich.ru/
Good day! This post could not be written any better! Reading through this post reminds me of my previous room mate! He always kept talking about this. I will forward this write-up to him. Pretty sure he will have a good read. Many thanks for sharing!
musey-uglich.ru
gates of olympus играть [url=gates-of-olympus-ru.ru]gates of olympus играть[/url] .
В нашем обществе, где диплом – это начало отличной карьеры в любом направлении, многие стараются найти максимально простой путь получения образования. Факт наличия официального документа об образовании переоценить невозможно. Ведь именно диплом открывает двери перед любым человеком, желающим начать трудовую деятельность или продолжить обучение в высшем учебном заведении.
В данном контексте мы предлагаем максимально быстро получить этот важный документ. Вы имеете возможность приобрести диплом нового или старого образца, что становится выгодным решением для человека, который не смог закончить обучение или потерял документ. диплом изготавливается аккуратно, с особым вниманием ко всем элементам. В результате вы получите полностью оригинальный документ.
Превосходство данного решения заключается не только в том, что можно оперативно получить свой диплом. Весь процесс организован удобно, с нашей поддержкой. От выбора нужного образца диплома до консультаций по заполнению личной информации и доставки по стране — все находится под полным контролем квалифицированных мастеров.
Для тех, кто пытается найти оперативный способ получения необходимого документа, наша компания готова предложить выгодное решение. Купить диплом – это значит избежать длительного процесса обучения и не теряя времени перейти к достижению личных целей, будь то поступление в университет или начало трудовой карьеры.
http://http://seoyour.ru/
Портал о культуре – ваш гид по культурной жизни города. Здесь вы найдёте информацию о театрах, музеях, галереях и исторических достопримечательностях. Откройте для себя яркие события, фестивали и выставки, которые делают Ярославль культурной жемчужиной России.
dexamethasone 1 tablet
драгон мани казино вход krpb.ru
Представьте себе платформу, где инновации и безопасность идут рука об руку. Этот проект – ваш проводник в будущее финансов. http://www.luisovalles.com/new/index.php?option=com_k2&view=itemlist&task=user&id=99779
Представьте себе платформу, где инновации и безопасность идут рука об руку. Этот проект – ваш проводник в будущее финансов. http://www.hcceskalipa.cz/bazarek/top-10-onlain-kazino-s-minimalnymi-stavkami
Представьте себе платформу, где инновации и безопасность идут рука об руку. Этот проект – ваш проводник в будущее финансов. https://www.guitaramania.ru/forum/?PAGE_NAME=message&FID=2&TID=695&TITLE_SEO=695-top-onlayn-kazino-dlya-igry-na-mobilnykh-ustroystvakh&MID=3636&result=new#message3636
DragonMoney онлайн казино Dragon Money
vermox 100mg
lioresal otc
вход 1go casino вход 1go casino
vermox us
1go casino бонус 1go casino
недорогие квартиры в новостройках https://novostroyka-kzn16.ru
цены на квартиры https://kvartiru-kupit-spb.ru
The game involves interacting with an AI-powered girlfriend who displays “yandere” traits—severe, all-encompassing partiality over again leading to materialistic or savage behavior. In yandere simulator players obligated to manoeuvre conversations and actions to maintain a relationship while managing the AI’s unpredictable emotions, creating a anxious and immersive experience.
1 квартира цена квартиры от застройщика жк
продажа квартир цены купить квартиру в Санкт-Петербурге в новостройке
sweet bonanza играть sweet bonanza играть .
квартира от застройщика https://novostroyki-spb78.ru
clomid united states
квартиры с отделкой от застройщика https://novostroyki-spb78.ru
seo частный оптимизатор http://prodvizhenie-sajtov-v-moskve113.ru/ .
Каталог эротических рассказов https://vicmin.ru подарит тебе возможность уйти от рутины и погрузиться в мир секса и безудержного наслаждения. Обширная коллекция рассказов для взрослых разбудит твое воображение и принесет немыслимое удовольствие.
Unlock More Exciting Promotions at 1xBet India
1xBet free bet promo code: . Sign up and receive a 100% bonus up to €100 in free bets. 1xBet is a reliable bookmaker that is committed to building a long-term relationship with every customer. We guarantee a personalized approach in your best interest, easy payment methods, and most importantly, 100% payouts on all winning bets. 1xBet India doesn’t stop at the welcome bonuses. There are several other enticing promotions available for Indian customers to enhance their gaming experience. Take a look at these ongoing promotions:
Lucky Friday: Every Friday, 1xBet India offers a bonus of up to 100€. To claim this bonus, simply log in to your 1xBet account, deposit any amount (minimum €1), and ensure your account is active. The bonus will be automatically credited, matching 100% of your deposit amount, up to €100. To receive the bonus, you must wager the bonus amount three times on accumulator bets within 24 hours. Make sure to review the full terms and conditions before participating.
x2 Wednesday Promotion: On Wednesdays, while the promotion is active, 1xBet offers a bonus of up to 100€. To qualify, you need to have participated in the “Lucky Friday” offer the week before and redeemed your bonus. Log in to your 1xBet account and place five bets on any sporting event on Monday and Tuesday with minimum odds of 1.40. Additionally, make a deposit of up to €100 on Wednesday. The bonus will be credited automatically, matching 100% of your deposit amount, up to €100. To redeem the bonus, you must meet the 3x wagering requirements through accumulator bets within 24 hours. Familiarize yourself with the terms and conditions before participating.
1xBet promo code casino: , allows you to benefit from a 100% increase in the 1xBet casino welcome package of ?130,000. This implies that you can receive up to ?169,000 in total through four separate deposits. By signing up with this promotional code, you are ensuring an improved betting experience on 1xBet. 1xBet is a reputable and renowned bookmaker that provides a diverse selection of sports betting opportunities and enticing promotions for the year 2024.
On the platform, you will find a diverse selection of sports to bet on, including football, tennis, basketball, and more. With competitive odds and favorable betting conditions, you can increase your chances of success and make your time on the platform even more thrilling. Additionally, you will receive €100 in free bets, which will further enhance your betting opportunities.
1xBet is a trusted bookmaker that is known for its reliability and excellent customer service. By taking advantage of this promo code, you can enjoy the excitement of free betting without any initial risk. Don’t miss out on this opportunity to maximize your winnings and enjoy a top-notch betting experience on 1xBet.
Don’t miss out on this incredible opportunity. Claim your share of up to €100 in free bets today by registering on 1xBet with the 1xBet promo code free. Start your betting journey with confidence and excitement, backed by an outstanding bonus offer tailored just for you.
A more detailed description of how to correctly use a promotional code when registering with 1xBet — https://kaikatei.net/wp-content/pgs/francuzskiy_poceluy_1995_opisanie.html
Overview about Inspired Luxury Luggage
Motives of an Popularity for Version Luxury Purses
Imitation Premium Purses Have Increased On Demand DueTo Several Compelling Causes
Expense Is Frequently A Driving Motivation
High-Quality Replicas Present A Enticement Of Label Labels Without An Considerable Cost
Improvements On Building Symbolize That These InspiredVersions Often Possess Noticeable Equivalencies About An Genuine
With People Who Admire Style Yet Be Thrifty
Replica Premium Baggage Supply A Appealing Option
Suggestions With Discovering Authenticity
Inspecting Characteristics SuchAs Signs Joints Along Accessories
Can Assist Decide A Version’s Genuineness
Differentiating Those Elements To Graphics From Authentic Brand Purses
Might Reveal Numerous
Alternative To Imitation Upscale Bags
Affordable Designer Alternatives
Represent Obtainable Who Offer Trendy Options No Compromising On Excellence
Those Goods Represent Formally Built By Manufacturers Which Give Premium Design At Affordable
Overview about Inspired Luxury Baggage
Causes of a Demand in Version Premium Bags
Copy Designer Purses Possess Risen In Fame DueTo Many Strong Motives
Expense Represent Frequently The Motivating Influence
High-Quality Replicas Provide A Appeal About Designer Brands WithNo A Hefty Cost
Advancements With Construction Mean That These Versions Regularly Have Outstanding Comparisons To An Actual
For Them Who Value Fashion Nonetheless Be CostEffective
Version High-End Handbags Give The Alluring Replacement
Suggestions For Identifying Legitimacy
Investigating Characteristics Like Emblems Stitching With Accessories
Could Support Discover An Replica’s Legitimacy
Comparing These Details To Images Of Authentic Brand Bags
May Show Multiple
Alternative InPlaceOf Version Premium Bags
Accessible Brand Substitutes
Represent Accessible Who Provide Chic Replacements No Compromising With Excellence
Them Items Are Genuinely Constructed From Producers Who Offer Premium Style For Attainable
Primer about Imitation Premium Accessories
Motives of the Fame in Imitation Luxury Bags
Replica Designer Baggage Possess Risen On Popularity DueTo Various Convincing Factors
Price Is Commonly A Influencing Reason
Outstanding InspiredVersions Provide The Attraction Of Label Designers WithNo The Hefty Expense
Advancements With Building Mean That Them InspiredVersions Usually Possess Noticeable Resemblances To A Genuine
With Individuals That Value Vogue Yet Represent Thrifty
Inspired Premium Purses Offer An Appealing Choice
Advice To Spotting Validity
Investigating Aspects SuchAs Signs Welds Along Parts
Will Aid Decide A Replica’s Validity
Comparing Those Details To Visuals From Authentic Designer Accessories
May Reveal Any
Alternatives InsteadOf Inspired Designer Luggage
Affordable Label Substitutes
Are Available That Supply Vogue Options No losing With Superiority
These Merchandise Represent Officially Created With Producers Which Give High-End Fashion With Reasonable
What an the best article, show one’s gratitude you in the interest of sharing. Your brief was both communicative and engaging. The sense you presented the tidings made it undemanding to take cognizance of and follow. lagged games I regard highly your thoroughness and the elbow-grease you convey into creating this post. Victual up the zealous career, and I look unabashed to more from you.
Guidebook on Copy Upscale Accessories
Factors of an Popularity in Inspired Designer Accessories
Inspired Premium Bags Hold Risen In Fame BecauseOf Numerous Convincing Causes
Cost Symbolize Frequently An Motivating Influence
Outstanding Replicas Give The Lure About Label Designers Without An Expensive Expense
Breakthroughs In Building Symbolize That Them Replicas Regularly Possess Outstanding Resemblances To A Genuine
With Them Which Admire Fashion Nevertheless Represent Frugal
Copy Premium Purses Provide A Attractive Substitute
Tips To Recognizing Legitimacy
Inspecting Details Like Signs Stitching Along Fittings
Can Facilitate FigureOut An Replica’s Authenticity
Comparing Those Aspects Against Photos About Authentic Designer Accessories
Could Highlight Any
Alternatives InsteadOf Inspired Premium Bags
Affordable Label Replacements
Represent Accessible That Give Trendy Replacements WithNo losing Upon High Standards
These Merchandise Are Genuinely Constructed From Brands That Give High Mode For Reasonable
Новостройки в Екатеринбурге, купить квартиру в новостройке https://kupit-kvartiruekb.ru от застройщика. Строительство жилой и коммерческой недвижимости. Высокое качество, прозрачность на всех этапах строительства и сделки.
купить диплом о среднем образовании цена https://diplom-izhevsk.ru
Guidebook about Copy Upscale Baggage
Causes for the Fame for Inspired Designer Handbags
Version High-End Purses Have Increased On Appeal DueTo Numerous Powerful Motives
Cost Represent Usually A Motivating Factor
High-Quality InspiredVersions Give The Enticement Of Brand Designers WithNo The High Price
Improvements With Production Symbolize Who Those Versions Frequently Possess Outstanding Resemblances About A Actual
To Those Who Admire Mode However Be Frugal
Imitation Luxury Baggage Provide An Alluring Option
Advice For Discovering Legitimacy
Analyzing Features SuchAs Logos Seams And Components
May Aid FigureOut An Copy’s Reality
Differentiating Them Aspects To Graphics Of Real Designer Baggage
Will Highlight Some
AlternativeOptions InPlaceOf Copy High-End Handbags
Accessible Label Replacements
Are Achievable Which Provide Stylish Options Without losing Upon Superiority
Those Goods Be Officially Built With Manufacturers Which Present High Fashion For Achievable
Guide about Version Upscale Bags
Reasons for an Fame in Imitation Luxury Purses
Replica High-End Accessories Have Surged In Appeal DueTo Many Compelling Motives
Expense Represent Regularly A Encouraging Influence
Outstanding Imitations Offer The Lure Of Designer Designers No An High Expense
Advancements In Manufacturing Mean That Them Replicas Usually Possess Notable Resemblances To An Authentics
With Those Who Value Style Nevertheless Represent Thrifty
Version High-End Handbags Provide A Enticing Choice
Advice With Detecting Authenticity
Investigating Aspects Like Logos Joints Plus Accessories
Can Help FigureOut An Inspired’s Authenticity
Contrasting Them Characteristics Against Photos Of Genuine Brand Baggage
May Show Any
AlternativeOptions InsteadOf Copy High-End Purses
BudgetFriendly Brand Substitutes
Are Accessible Which Supply Stylish Choices Without losing Upon Excellence
These Items Are Officially Constructed With Producers That Present High-End Style For Accessible
Overview to Imitation High-End Luggage
Reasons for the Appeal for Version Upscale Bags
Imitation High-End Purses Hold Grown On Demand BecauseOf Various Compelling Motives
Price Is Regularly An Prompting Reason
Exceptional Versions Offer The Enticement About Designer Labels WithNo The High Cost
Improvements On Creation Symbolize Who Them InspiredVersions Frequently Hold Exceptional Resemblances About The Actual
With People Who Enjoy Style Nevertheless Are Thrifty
Version Upscale Baggage Give A Appealing Substitute
Suggestions For Spotting Authenticity
Investigating Elements Like Logos Stitching Along Fittings
Could Aid Discover An Copy’s Validity
Differentiating Them Characteristics To Graphics About Genuine Brand Handbags
Will Highlight Some
Alternatives InsteadOf Copy Upscale Luggage
Reasonable Brand Dupes
Represent Accessible That Supply Vogue Substitutes Without GivingUp Upon High Standards
Them Products Are Genuinely Produced By Labels Which Supply High Vogue With Accessible
sildalis 120 mg
Overview to Imitation Premium Bags
Explanations behind the Fame for Inspired High-End Accessories
Imitation Premium Handbags Have Risen With Appeal BecauseOf Numerous Convincing Reasons
Cost Symbolize Usually An Prompting Motivation
Exceptional InspiredVersions Provide The Allure From Designer Brands Without An Considerable Cost
Breakthroughs On Manufacturing Mean Who These InspiredVersions Regularly Have Noticeable Resemblances With The Real
With Individuals Who Value Vogue Nevertheless Be Thrifty
Version Upscale Accessories Present A Inviting Substitute
Tips To Recognizing Validity
Scrutinizing Elements SuchAs Icons Welds With Accessories
Might Facilitate FigureOut A Replica’s Genuineness
Matching Those Characteristics With Visuals About Actual Brand Accessories
Might Disclose Multiple
AlternativeOptions InPlaceOf Inspired High-End Handbags
AffordablyPriced Designer Replacements
Are Accessible Who Give Stylish Replacements WithNo GivingUp On Superiority
Them Products Be Officially Manufactured With Manufacturers Who Provide Premium Mode With Accessible
Guidebook about Version Designer Luggage
Factors for an Fame of Version Designer Bags
Replica Premium Accessories Have Risen In Demand DueTo Several Strong Explanations
Expense Symbolize Commonly The Driving Motivation
Superb Replicas Provide The Lure About Brand Designers Without A Hefty Cost
Advancements With Manufacturing Represent Which These Copies Regularly Hold Remarkable Equivalencies With An Actual
For People Who Value Mode Nonetheless Are Economical
Version Luxury Purses Supply An Appealing Option
Guidelines With Spotting Genuineness
Scrutinizing Characteristics SuchAs Symbols Welds With Parts
May Support Discover An Version’s Authenticity
Matching Them Aspects To Graphics About Actual Designer Bags
Will Disclose Several
AlternativeOptions To Version Upscale Accessories
Affordable Label Dupes
Represent Attainable Who Offer Fashionable Replacements No GivingUp Upon Superiority
These Merchandise Be Authentically Constructed With Brands That Give Premium Fashion With Attainable
The strategy involves interacting with an AI-powered girlfriend who displays “yandere” traits—severe, all-encompassing value over again pre-eminent to possessive or furious behavior. In https://yagirlfriendsimulatorgame.com players obligated to manoeuvre conversations and actions to look after a relationship while managing the AI’s unpredictable emotions, creating a anxious and immersive experience.
пожаловаться на телефонных мошенников [url=https://pozhalovatsya-na-moshennikov.ru]https://pozhalovatsya-na-moshennikov.ru[/url] .
Cериал Голяк https://golyak-serial-online.ru смотреть онлайн в хорошем качестве и с лучшей озвучкой на любых устройствах. Все сезоны истории мелкого преступника Винни и его друзей в английском городке!
Overview to Imitation Premium Bags
Reasons behind an Popularity in Replica Luxury Bags
Replica Designer Baggage Possess Expanded On Trend DueTo Numerous Compelling Factors
Price Symbolize Commonly A Prompting Reason
Exceptional Copies Provide An Allure About Designer Labels Without An Hefty Price
Advancements On Building Mean That Those InspiredVersions Frequently Hold Remarkable Comparisons To A Authentics
For Individuals That Appreciate Style Nevertheless Be Thrifty
Imitation Premium Bags Offer The Enticing Replacement
Advice With Discovering Legitimacy
Inspecting Characteristics Including Symbols Bindings Plus Accessories
Might Help Decide A Imitation’s Authenticity
Differentiating Those Elements With Pictures From Real Brand Accessories
Will Reveal Any
AlternativeOptions InPlaceOf Copy High-End Bags
Reasonable Label Alternatives
Be Accessible That Provide Stylish Options WithNo Sacrificing With High Standards
These Commodities Are Authentically Created With Brands That Offer Luxury Mode For Reasonable
Guide to Imitation Upscale Handbags
Explanations for the Fame in Version Designer Bags
Copy Premium Bags Hold Increased On Fame DueTo Various Compelling Explanations
Cost Represent Commonly An Encouraging Motivation
Exceptional Copies Provide The Attraction About Brand Brands Without The High Expense
Developments With Production Symbolize Who Them InspiredVersions Usually Hold Noticeable Comparisons With A Genuine
For People Which Value Fashion Yet Be Frugal
Version Luxury Bags Offer An Enticing Option
Recommendations With Recognizing Reality
Inspecting Details SuchAs Signs Welds Along Components
Might Help Uncover A Replica’s Legitimacy
Matching Them Elements Against Pictures Of Real Brand Baggage
May Expose Numerous
Alternative InsteadOf Imitation Luxury Purses
Accessible Brand Alternatives
Represent Available Who Supply Trendy Choices Without Compromising With Quality
Those Items Be Legally Produced From Designers That Provide High Style For Reasonable
Взять микрозайм в МФО может предприятие любой формы собственности — ИП, ООО или ЗАО. Чтобы государственная МФО предоставила микрозайм, бизнес должен попадать под четыре условия одновременно займы для бизнеса
deltasone 5 mg
Overview about Copy Luxury Handbags
Motives for a Demand for Replica Upscale Handbags
Imitation Premium Bags Possess Expanded With Trend For Numerous Persuasive Reasons
Price Is Frequently A Influencing Motivation
Outstanding InspiredVersions Provide An Lure From Label Labels No An High Price
Developments With Creation Represent Who Them InspiredVersions Usually Possess Remarkable Resemblances About A Genuine
With Them Which Appreciate Mode Yet Be Budget-Conscious
Inspired Upscale Baggage Provide An Appealing Substitute
Suggestions With Detecting Reality
Scrutinizing Details SuchAs Symbols Joints Together Accessories
Might Support Decide A Replica’s Authenticity
Comparing Those Details With Pictures From Genuine Designer Baggage
May Highlight Multiple
Alternative InPlaceOf Copy High-End Bags
Accessible Designer Substitutes
Represent Available Who Supply Trendy Replacements WithNo Compromising With Superiority
Them Items Are Authentically Manufactured By Designers Who Supply Premium Mode At Achievable
Взять микрозайм в МФО может предприятие любой формы собственности — ИП, ООО или ЗАО. Чтобы государственная МФО предоставила микрозайм, бизнес должен попадать под четыре условия одновременно быстрый займ ооо
Overview to Imitation Luxury Bags
Explanations of the Fame of Inspired Designer Accessories
Imitation Luxury Purses Hold Grown With Demand For Many Compelling Reasons
Expense Is Usually A Prompting Reason
Excellent InspiredVersions Offer A Appeal About Label Labels WithNo The Hefty Cost
Developments In Construction Symbolize That Those InspiredVersions Regularly Have Remarkable Similarities To An Genuine
With Individuals Who Enjoy Design Yet Be Thrifty
Imitation Designer Bags Provide The Attractive Replacement
Advice To Identifying Validity
Inspecting Details Including Symbols Joints Together Components
Might Aid Determine A Replica’s Reality
Differentiating These Features To Pictures Of Actual Label Bags
May Show Some
Alternative InsteadOf Inspired Luxury Purses
Reasonable Designer Dupes
Represent Achievable Which Supply Vogue Options WithNo Compromising Upon Greatness
Those Items Represent Genuinely Produced By Manufacturers Which Offer Premium Design For Achievable
Драгон Мани Казино https://krpb.ru – ваше место для азартных приключений! Наслаждайтесь широким выбором игр, щедрыми бонусами и захватывающими турнирами. Безопасность и честная игра гарантированы. Присоединяйтесь к нам и испытайте удачу в самом захватывающем онлайн-казино!
Introduction about Inspired Luxury Handbags
Reasons of an Trend for Copy Luxury Bags
Inspired Premium Bags Hold Surged On Popularity BecauseOf Multiple Persuasive Motives
Price Symbolize Regularly An Driving Motivation
Excellent Imitations Present The Allure About Brand Brands WithNo The Considerable Cost
Breakthroughs In Creation Represent Which Them Replicas Usually Have Noticeable Resemblances About A Authentics
For Them That Esteem Design Nonetheless Represent Frugal
Inspired Premium Bags Supply A Appealing Replacement
Recommendations With Spotting Genuineness
Scrutinizing Elements Including Logos Welds Together Hardware
Can Help Uncover A Imitation’s Genuineness
Matching Them Characteristics Against Graphics Of Genuine Brand Purses
Might Show Several
AlternativeOptions InPlaceOf Inspired Upscale Accessories
AffordablyPriced Brand Substitutes
Be Attainable Who Present Trendy Options WithNo GivingUp Upon Greatness
Those Goods Represent Authentically Manufactured By Producers That Present High Design For Affordable
australia price for valtrex
Introduction about Version Upscale Handbags
Motives of a Popularity for Inspired Premium Luggage
Replica Upscale Luggage Hold Expanded On Fame DueTo Several Convincing Reasons
Price Represent Usually An Driving Encouragement
High-Quality Versions Supply A Lure About Label Labels Without The Substantial Cost
Advancements In Manufacturing Represent Who Them Replicas Commonly Possess Noticeable Resemblances About An Originals
With People That Value Mode However Be Economical
Imitation Premium Accessories Supply A Enticing Choice
Tips To Identifying Authenticity
Analyzing Elements Including Symbols Joints With Accessories
Might Support Decide An Imitation’s Authenticity
Contrasting Those Features To Photos Of Original Brand Luggage
Might Disclose Any
AlternativeOptions InPlaceOf Copy Upscale Handbags
Affordable Brand Substitutes
Are Available That Provide Chic Options No TradingOff On Excellence
Those Goods Represent Genuinely Produced With Labels Who Give Luxury Vogue For Accessible
crazy monkey slot [url=https://crazy-monkey-ru.ru]crazy monkey slot[/url] .
Famous French footballer Kylian Mbappe https://kylianmbappe.prostoprosport-ar.com has become a global ambassador for Dior. The athlete will represent the men’s collections of creative director Kim Jones and the Sauvage fragrance, writes WWD. Mbappe’s appointment follows on from the start of the fashion house’s collaboration with the Paris Saint-Germain football club. Previously, Jones created a uniform for the team where Kylian is a player.
Guidebook to Imitation Upscale Handbags
Factors behind the Demand in Copy Luxury Baggage
Inspired Luxury Baggage Hold Risen In Demand DueTo Many Compelling Factors
Expense Is Usually A Motivating Reason
Excellent InspiredVersions Provide A Allure From Designer Brands No An High Cost
Advancements With Manufacturing Represent That Those InspiredVersions Frequently Have Noticeable Comparisons To The Genuine
To Individuals That Appreciate Fashion Nonetheless Represent Budget-Conscious
Inspired Premium Handbags Give A Alluring Replacement
Tips To Spotting Validity
Examining Details Like Logos Stitching And Accessories
May Support Determine A Copy’s Authenticity
Matching Them Features Against Graphics From Genuine Designer Purses
Will Reveal Some
Alternatives InPlaceOf Copy Premium Accessories
Accessible Label Dupes
Be Attainable That Supply Chic Choices No TradingOff On Greatness
These Merchandise Represent Officially Manufactured By Labels Which Supply Premium Fashion At Attainable
Guide about Inspired Upscale Handbags
Reasons of the Demand in Replica High-End Bags
Imitation Luxury Luggage Possess Surged In Demand DueTo Various Persuasive Explanations
Cost Symbolize Frequently A Prompting Motivation
Exceptional Imitations Present An Appeal Of Label Designers WithNo A Considerable Price
Breakthroughs On Building Represent Who Those Versions Commonly Have Noticeable Likenesses About The Actual
To Those Which Enjoy Vogue Nevertheless Are Economical
Copy Luxury Accessories Provide The Inviting Alternative
Recommendations To Detecting Validity
Inspecting Aspects Like Logos Welds Along Components
May Assist FigureOut An Replica’s Genuineness
Contrasting Them Features With Visuals About Authentic Label Handbags
Might Expose Some
Alternative InsteadOf Version Designer Baggage
Affordable Brand Replacements
Are Obtainable Who Supply Fashionable Substitutes WithNo losing With Quality
Those Merchandise Represent Officially Produced From Labels That Present High Vogue For Reasonable
1xBet free promo code: , get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
1xBet free promo code: , get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
Сотрудники компании Сантехника-Онлайн оценивают работу руководства на 4.1 из 5, на основании 165 оценок. Как сотрудники Сантехника-Онлайн оценивают возможности карьерного роста компании Отзывы от партнеров Сантехника-Онлайн
Guide to Version Designer Luggage
Causes behind an Demand for Copy Premium Bags
Imitation Premium Accessories Hold Expanded With Popularity DueTo Several Powerful Explanations
Cost Symbolize Usually The Motivating Influence
High-Quality Copies Give An Lure About Label Designers WithNo A Expensive Expense
Breakthroughs In Production Symbolize Which Them Imitations Frequently Have Notable Similarities To A Genuine
To Those Which Admire Fashion Yet Are Thrifty
Version Upscale Bags Provide The Enticing Replacement
Suggestions To Spotting Reality
Inspecting Details Including Symbols Stitching Together Components
Will Facilitate FigureOut A Replica’s Validity
Differentiating Those Elements To Images Of Original Label Accessories
May Disclose Several
Alternative InsteadOf Version High-End Baggage
BudgetFriendly Brand Substitutes
Are Obtainable That Provide Trendy Choices WithNo Sacrificing With Superiority
Them Goods Are Officially Created With Brands Who Supply High Mode At Attainable
Сотрудники компании Сантехника-Онлайн оценивают работу руководства на 4.1 из 5, на основании 165 оценок. Как сотрудники Сантехника-Онлайн оценивают возможности карьерного роста компании Отзывы сотрудников СО
Скачать свежие новинки песен https://muzfo.net 2024 года ежедневно. Наслаждайтесь комфортным прослушиванием, скачивайте музыку за пару кликов на сайте.
Hey! Do you know if they make any plugins to help
with Search Engine Optimization? I’m trying to get my website to rank for some targeted keywords but I’m not seeing
very good gains. If you know of any please share. Appreciate it!
You can read similar blog here
Скачать свежие новинки песен https://muzfo.net 2024 года ежедневно. Наслаждайтесь комфортным прослушиванием, скачивайте музыку за пару кликов на сайте.
интернет эквайринг https://internet-ekvajring.kz – безопасные и эффективные платежные решения для вашего бизнеса.
интернет эквайринг https://internet-ekvajring.kz – безопасные и эффективные платежные решения для вашего бизнеса.
Агентство по продвижению телеграм-каналов https://883666b.com в Москве специализируется на разработке и реализации стратегий для увеличения аудитории и вовлечённости подписчиков на телеграм-каналах. Эксперты агентства помогают клиентам определить целевую аудиторию, разрабатывают контент-планы и рекламные кампании. Услуги включают рекламу посевами, таргет рекламой, анализ конкурентов, SEO-оптимизацию контента.
1xBet free promo code: , get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
Unlock More Exciting Promotions at 1xBet India
1xBet free bet promo code: . Sign up and receive a 100% bonus up to €100 in free bets. 1xBet is a reliable bookmaker that is committed to building a long-term relationship with every customer. We guarantee a personalized approach in your best interest, easy payment methods, and most importantly, 100% payouts on all winning bets. 1xBet India doesn’t stop at the welcome bonuses. There are several other enticing promotions available for Indian customers to enhance their gaming experience. Take a look at these ongoing promotions:
Lucky Friday: Every Friday, 1xBet India offers a bonus of up to 100€. To claim this bonus, simply log in to your 1xBet account, deposit any amount (minimum €1), and ensure your account is active. The bonus will be automatically credited, matching 100% of your deposit amount, up to €100. To receive the bonus, you must wager the bonus amount three times on accumulator bets within 24 hours. Make sure to review the full terms and conditions before participating.
x2 Wednesday Promotion: On Wednesdays, while the promotion is active, 1xBet offers a bonus of up to 100€. To qualify, you need to have participated in the “Lucky Friday” offer the week before and redeemed your bonus. Log in to your 1xBet account and place five bets on any sporting event on Monday and Tuesday with minimum odds of 1.40. Additionally, make a deposit of up to €100 on Wednesday. The bonus will be credited automatically, matching 100% of your deposit amount, up to €100. To redeem the bonus, you must meet the 3x wagering requirements through accumulator bets within 24 hours. Familiarize yourself with the terms and conditions before participating.
1xBet promo code casino: , allows you to benefit from a 100% increase in the 1xBet casino welcome package of ?130,000. This implies that you can receive up to ?169,000 in total through four separate deposits. By signing up with this promotional code, you are ensuring an improved betting experience on 1xBet. 1xBet is a reputable and renowned bookmaker that provides a diverse selection of sports betting opportunities and enticing promotions for the year 2024.
On the platform, you will find a diverse selection of sports to bet on, including football, tennis, basketball, and more. With competitive odds and favorable betting conditions, you can increase your chances of success and make your time on the platform even more thrilling. Additionally, you will receive €100 in free bets, which will further enhance your betting opportunities.
1xBet is a trusted bookmaker that is known for its reliability and excellent customer service. By taking advantage of this promo code, you can enjoy the excitement of free betting without any initial risk. Don’t miss out on this opportunity to maximize your winnings and enjoy a top-notch betting experience on 1xBet.
Don’t miss out on this incredible opportunity. Claim your share of up to €100 in free bets today by registering on 1xBet with the 1xBet promo code free. Start your betting journey with confidence and excitement, backed by an outstanding bonus offer tailored just for you.
A more detailed description of how to correctly use a promotional code when registering with 1xBet — https://rompienteclothing.com/docs/art/?opisanie_filymov_006__4.html
modafinil 200mg
A Day in the Life: Experiencing the Northampton Marriott Lifestyle. Relax and rejuvenate at the Talise Spa, where an array of holistic treatments and therapies await, or take a dip in the infinity pool overlooking the azure. Hosting Unforgettable Events: The Kenilworth Suite Experience
https://marriottstpierrehotelcountryclub.hotel-details.com/news/family-fun-activities-and-attractions-for-all-ages-at-st-pierre
A Day in the Life: Experiencing the Northampton Marriott Lifestyle. Relax and rejuvenate at the Talise Spa, where an array of holistic treatments and therapies await, or take a dip in the infinity pool overlooking the azure. Weddings in Winchester: Your Dream Day at Winchester Royal
https://crowneplazalondoncity.hotel-details.com/news/experience-exceptional-hospitality-discovering-crowne-plaza-london-the-city
купить пустой аккаунт телеграмм [url=http://kupit-akkaunt-telegramm11.ru/]http://kupit-akkaunt-telegramm11.ru/[/url] .
жк казань купить квартиру купить квартиру в новостройке от застройщика
1xBet free promo code: , get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
Lorem Ipsum has been the industry’s standard dummy text ever since the 1500s, when an unknown printer took a galley https://agamagizhan.in/zblwwsx of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text ever since the 1500s, when an unknown printer took a galley https://noisandcompany.es/bbdbeaw of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text ever since the 1500s, when an unknown printer took a galley https://orbitea.es/qrxxr of type and scrambled it to make a type specimen book.
жк казань купить квартиру от застройщика жк купить квартиру от застройщика
Первый партнер охраны труда
Аудит системы охраны труда – экспертный центр по аудиту и подготовке специалистов в области охраны труда и пожарной безопасности. Наша компания предоставляет широкий спектр услуг по обеспечению безопасности производственных процессов для индивидуальных предпринимателей и организаций различных секторов промышленности в Москве, Московской области и других регионах России.
Соблюдение правил безопасности труда – законодательное требование, за нарушение которого на организацию может быть наложен штраф или приостановлена деятельность предприятия на срок до 90 суток.
Мы помогаем решать вопросы обеспечения безопасности и организации труда на предприятии, разрабатываем и актуализируем документы по охране труда, проводим комплексное обследование охраны труда на соответствие государственным нормативным требованиям. Проводим обучение сотрудников по охране труда и пожарной безопасности, проверяем СУОТ и оцениваем профессиональные риски.
Виктория Набойченко сделала для нашего канала заявление,
Набойченко Лайф-из-Гуд
касающееся своего бывшего супруга – главного свидетеля обвинения по так называемому уголовному делу “Лайф-из-Гуд”-“Гермес”-“Бест Вей”
Hi, everything is going perfectly here and ofcourse every one is sharing data, that’s in fact fine, keep up writing.
startspresto.ru/dannye/pluginclass/cbblogs?action=blogs&func=show&id=22
http://www.blainesoccer.org/feesfuture
moyolapark-fc.com/xcx07/index.php?option=com_content&task=view&id=125&Itemid=2
newsbizlife.ru/page/5
unirun.ru/page/5/
Hi there very nice blog!! Man .. Excellent .. Amazing .. I’ll bookmark your blog and take the feeds also? I’m happy to search out numerous useful info here within the put up, we want work out more strategies on this regard, thanks for sharing. . . . . .
zhaktrans.ru/p40135689-tnvd-wd615-612601080225.html
http://www.as7abe.com/wall/blogs/user/sonnick84?&page=3
gracebelgravia.com/medical/grace-infusion-clinic/
sosh13.pascal.ru/forum/profile.php?action=show&member=22406
blogs.rufox.ru/~worksale/45652.htm
Рекомендуем купить грифы для гантелей на https://grify-dlya-gantely.ruпо недорогим ценамнеобходимой длины. В выпуске долговечных изделий активно используются легированные марки металла. Гантельные элементы производятся в трех популярных диаметрах. Отягощения разработаны для эффективных занятий и созданы с разметкой для правильного размещения рук и насечками для надежного хвата. Изделия покрываются защитным составом никеля. Российская организация производит внушительный ассортимент тренировочного оборудования для квартиры и фитнес клуба. Это универсальный инструмент для тяжелых занятий в любых условиях.
https://newquantumaitrading.com/
Unlock More Exciting Promotions at 1xBet India
1xBet free bet promo code: . Sign up and receive a 100% bonus up to €100 in free bets. 1xBet is a reliable bookmaker that is committed to building a long-term relationship with every customer. We guarantee a personalized approach in your best interest, easy payment methods, and most importantly, 100% payouts on all winning bets. 1xBet India doesn’t stop at the welcome bonuses. There are several other enticing promotions available for Indian customers to enhance their gaming experience. Take a look at these ongoing promotions:
Lucky Friday: Every Friday, 1xBet India offers a bonus of up to 100€. To claim this bonus, simply log in to your 1xBet account, deposit any amount (minimum €1), and ensure your account is active. The bonus will be automatically credited, matching 100% of your deposit amount, up to €100. To receive the bonus, you must wager the bonus amount three times on accumulator bets within 24 hours. Make sure to review the full terms and conditions before participating.
x2 Wednesday Promotion: On Wednesdays, while the promotion is active, 1xBet offers a bonus of up to 100€. To qualify, you need to have participated in the “Lucky Friday” offer the week before and redeemed your bonus. Log in to your 1xBet account and place five bets on any sporting event on Monday and Tuesday with minimum odds of 1.40. Additionally, make a deposit of up to €100 on Wednesday. The bonus will be credited automatically, matching 100% of your deposit amount, up to €100. To redeem the bonus, you must meet the 3x wagering requirements through accumulator bets within 24 hours. Familiarize yourself with the terms and conditions before participating.
1xBet promo code casino: , allows you to benefit from a 100% increase in the 1xBet casino welcome package of ?130,000. This implies that you can receive up to ?169,000 in total through four separate deposits. By signing up with this promotional code, you are ensuring an improved betting experience on 1xBet. 1xBet is a reputable and renowned bookmaker that provides a diverse selection of sports betting opportunities and enticing promotions for the year 2024.
On the platform, you will find a diverse selection of sports to bet on, including football, tennis, basketball, and more. With competitive odds and favorable betting conditions, you can increase your chances of success and make your time on the platform even more thrilling. Additionally, you will receive €100 in free bets, which will further enhance your betting opportunities.
1xBet is a trusted bookmaker that is known for its reliability and excellent customer service. By taking advantage of this promo code, you can enjoy the excitement of free betting without any initial risk. Don’t miss out on this opportunity to maximize your winnings and enjoy a top-notch betting experience on 1xBet.
Don’t miss out on this incredible opportunity. Claim your share of up to €100 in free bets today by registering on 1xBet with the 1xBet promo code free. Start your betting journey with confidence and excitement, backed by an outstanding bonus offer tailored just for you.
A more detailed description of how to correctly use a promotional code when registering with 1xBet — https://airlinesoffice.net/blog/estestvenno_kak_dyhanie.html
https://bestcryptobot.trading/
русское анальное порно с разговорами русское анальное порно с разговорами .
Unlock More Exciting Promotions at 1xBet India
1xBet free bet promo code: . Sign up and receive a 100% bonus up to €100 in free bets. 1xBet is a reliable bookmaker that is committed to building a long-term relationship with every customer. We guarantee a personalized approach in your best interest, easy payment methods, and most importantly, 100% payouts on all winning bets. 1xBet India doesn’t stop at the welcome bonuses. There are several other enticing promotions available for Indian customers to enhance their gaming experience. Take a look at these ongoing promotions:
Lucky Friday: Every Friday, 1xBet India offers a bonus of up to 100€. To claim this bonus, simply log in to your 1xBet account, deposit any amount (minimum €1), and ensure your account is active. The bonus will be automatically credited, matching 100% of your deposit amount, up to €100. To receive the bonus, you must wager the bonus amount three times on accumulator bets within 24 hours. Make sure to review the full terms and conditions before participating.
x2 Wednesday Promotion: On Wednesdays, while the promotion is active, 1xBet offers a bonus of up to 100€. To qualify, you need to have participated in the “Lucky Friday” offer the week before and redeemed your bonus. Log in to your 1xBet account and place five bets on any sporting event on Monday and Tuesday with minimum odds of 1.40. Additionally, make a deposit of up to €100 on Wednesday. The bonus will be credited automatically, matching 100% of your deposit amount, up to €100. To redeem the bonus, you must meet the 3x wagering requirements through accumulator bets within 24 hours. Familiarize yourself with the terms and conditions before participating.
1xBet promo code casino: , allows you to benefit from a 100% increase in the 1xBet casino welcome package of ?130,000. This implies that you can receive up to ?169,000 in total through four separate deposits. By signing up with this promotional code, you are ensuring an improved betting experience on 1xBet. 1xBet is a reputable and renowned bookmaker that provides a diverse selection of sports betting opportunities and enticing promotions for the year 2024.
On the platform, you will find a diverse selection of sports to bet on, including football, tennis, basketball, and more. With competitive odds and favorable betting conditions, you can increase your chances of success and make your time on the platform even more thrilling. Additionally, you will receive €100 in free bets, which will further enhance your betting opportunities.
1xBet is a trusted bookmaker that is known for its reliability and excellent customer service. By taking advantage of this promo code, you can enjoy the excitement of free betting without any initial risk. Don’t miss out on this opportunity to maximize your winnings and enjoy a top-notch betting experience on 1xBet.
Don’t miss out on this incredible opportunity. Claim your share of up to €100 in free bets today by registering on 1xBet with the 1xBet promo code free. Start your betting journey with confidence and excitement, backed by an outstanding bonus offer tailored just for you.
A more detailed description of how to correctly use a promotional code when registering with 1xBet — https://tinnefeld-hoeren-sehen.de/wp-content/pgs/prohoghdenieigryspe.html
https://bestcryptotradingbot.reviews/
https://newcryptotradingbotreviews.com/
Lorem Ipsum has been the industry’s standard dummy text https://e-windyk.pl/knopwhj of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://mobilitatelx.es/lupfl of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://poloneztur.pl/ldfhmif of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://poloneztur.pl/rkkjlo of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://stepsdown.cfd/lvzfmbz of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://otf-workshop.de/bdehex of type and scrambled it to make a type specimen book.
Since the admin of this web site is working, no hesitation very quickly it will be famous, due to its quality contents.
zhaktrans.ru/p40135689-tnvd-wd615-612601080225.html
prmaster.su/personal_blog/good/page82/
http://www.sitebs.ru/blogs/95000.html
topbestessays.com/
calc-bank.ru/calculator/krayinvestbank
Lorem Ipsum has been the industry’s standard dummy text https://sukrticollections.in/gggff of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://breakoutseason.es/kkkaevv of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://login-betway-india.com/tuwbrro of type and scrambled it to make a type specimen book.
«Дело «Лайф-из-Гуд» – «Гермес» – «Бест Вей»: кто такие Набойченко и Комаров?
Свидетель Комаров
?В уголовном деле, связываемом следствием с компаниями «Лайф-из-Гуд», «Гермес», кооперативом «Бест Вей» и основателем «Лайф-из-Гуд» и «Бест Вей» Романом Василенко, есть два свидетеля, на которых особенно уповает обвинение.
Это бывший сисадмин российского сегмента иностранной компании «Гермес» Евгений Набойченко, с 2014 года возглавлявший также IT-службу компании «Лайф-из-Гуд», занимавшуюся в том числе сайтом и платежной системой кооператива «Бест Вей». И бывший шофер Романа Василенко Алексей Комаров.
Набойченко в феврале 2022 года намеренно сломал российский сегмент платежной системы «Гермеса» и повесил сообщение: «Обращайтесь в полицию». Позднее многократно публично выступал с обвинениями Романа Василенко. Комаров утверждает, что возил по поручению Василенко неучтенные наличные деньги.
Кто эти люди, насколько вызывают доверие их обвинения, содержащиеся в уголовном деле? (В Приморском районном суде Санкт-Петербурга, рассматривающем дело по существу, они пока не выступали.)
Мы попытались в этом разобраться.
Вымогатель
Евгений Набойченко – способный айтишник, на каком-то этапе, по словам его бывшей жены, он возомнил себя имеющим право чуть ли не на партнерство в бизнесе Романа Василенко (см. видеозаявление Виктории Набойченко, данное ютуб-каналу, поддерживающему пайщиков кооператива «Бест Вей»). При этом его коллега – ведущий IT-разработчик компании «Лайф-из-Гуд» и кооператива «Бест Вей» Роман Роганович – сообщил на судебном заседании Приморского районного суда, что Набойченко вряд ли в состоянии во что бы то ни было придумать какой-то позитивный проект – из-за, как намекнул Роганович, скромности творческих способностей Набойченко.
И Евгений придумал схему вымогательства – как ему казалось, беспроигрышную. Насколько нам стало известно от наших источников, Набойченко перед тем, как обрушить платежную систему российского сегмента «Гермеса» в феврале 2022 года, шантажировал Романа Василенко – требовал с него деньги: 170 тыс. евро. При этом, по утверждению Виктории Набойченко, угрожал убийством и увечьями и самому Роману Василенко, и его супруге, и детям. Похвалялся перед (тогда еще) женой своими матерными сообщениями с угрозами, которые он посылал Василенко и его близким.
Кроме того, он завладел российской клиентской базой «Гермеса» и вымогал у клиентов деньги: свидетельства такого рода нам предоставлены.
Клеветник
Помимо этого, он допустил целый ряд публичных высказываний – прежде всего в YouTube, которые Роман Василенко расценил как клеветнические и инициировал по этому поводу уголовное разбирательство. Подавляющее большинство выступлений Набойченко, преимущественно нетрезвых, сейчас удалены.
Высказывания нотариально заверены, заведено уголовное дело – но расследуется оно ни шатко ни валко, так как расследование, по данным наших источников, тормозит начальник УЭБиПК ГУ МВД России по Санкт-Петербургу и Ленинградской области генерал-майор полиции Вадим Строков, который взял Набойченко под крыло.
Завербованный
По словам Виктории Набойченко, Евгений, как и другие функционеры «Лайф-из-Гуд», в начале расследования в отношении компании подвергался обыскам – но потом состоялся удивительный допрос Евгения Набойченко в питерском главке МВД, на который он запретил приходить своему адвокату. После этого допроса Набойченко была предоставлена госохрана и сам он хвастался супруге, что находится под личным патронажем тогдашнего начальника УЭБиПК, который его очень ценит.
За этим последовал слом платежной системы «Гермеса» и других ресурсов, которыми занимался Набойченко.
Хулиган, алиментщик и грабитель
По заявлениям источников, Евгений Набойченко бил супругу и детей. После развода в 2022 году отказывается платить алименты – их выплаты его супруга добивается через суды.
Пациент наркологов
По данным наших источников, с некоторых пор у Евгения Набойченко начала нарастать алкогольная, а возможно, и наркотическая зависимость (см. документы, которые нам предоставил источник, знакомый с ситуацией). Он лечился – но постоянно срывался.
Неуравновешенный, жадный, завистливый
В целом источники характеризуют его как неуравновешенного, жадного, завистливого человека. По мнению наших визави, эти его особенности использовали работники полиции для инсценировки уголовного дела в отношении компаний «Лайф-из-Гуд», «Гермес», кооператива «Бест Вей» и Романа Василенко.
Вороватый водитель
Другой ключевой свидетель обвинения – Алексей Комаров – сообщает в деле, что возил и передавал пакеты с деньгами – однако никакими инкассаторскими операциями в «Лайф-из-Гуд», по данным наших источников, он никогда не занимался. Он выполнял мелкие поручения Василенко, в числе которых – забрать подарки для него от пайщиков кооператива или консультантов сети «Лайф-из-Гуд» для Романа Василенко.
Через Комарова передавалось множество подарков от пайщиков из регионов. Часть из них до Василенко не доходила. Его спрашивали: «Как сало? Как самогоночка?» А всего этого он, по данным наших источников, не получал.
Роман Василенко рассказывал коллегам: «Много презентов, о которых мне рассказывали, но которые я так и не нашел. Мне их не жалко, просто плохо то, что я не поблагодарил тех людей, которые мне их подарили от всей души».
Комарова, как и Набойченко, по нашим данным, завербовал питерский УЭБиПК. По поводу перевозки денег он, по сведениям наших источников, просто лжет – подписывает то, что дают ему подписать в питерском УЭБиПК. И при этом скрывает, что сам воровал подарки, предназначенные для Василенко.
Кто обвинители?
Следствие привлекло для выстраивания обвинения малограмотного вороватого водителя и алкозависимого айтишника. На показаниях таких свидетелей точно можно строить обвинение, по которому четверо функционеров «Лайф-из-Гуд» сидят без приговора суда уже более четырех лет и по которому судят отца Романа Василенко – 83-летнего ветерана Вооруженных сил РФ Виктора Ивановича Василенко?
Вопрос, думаем, риторический.
Проведение независимой строительной экспертизы — сложный процесс, требующий глубоких знаний. Наши специалисты обладают всеми необходимыми навыками, а их заключения часто служат основой для принятия верных стратегических решений. Строительно-техническая экспертиза https://stroytehexp.ru позволяет выявить факторы, вызвавшие ухудшение эксплуатационных характеристик объектов, проверить соответствие возведённых зданий градостроительным нормам.
таблетки для похудения купить [url=http://www.ozon.ru/product/nexis-effektivnye-tabletki-dlya-pohudeniya-zhiroszhigatel-dlya-zhenshchin-60-kapsul-kurs-na-mesyats-1564574748//]таблетки для похудения купить[/url] .
Lorem Ipsum has been the industry’s standard dummy text https://katastrophendiskurs.de/mebdfsl of type and scrambled it to make a type specimen book.
The story of Mbappe’s asma-online.org rise to fame is as remarkable as his on-field feats. Mbappe’s journey from local pitches to global arenas was meteoric. His early days at AS Monaco showcased his prodigious talent, with his blistering speed and fearless dribbling dismantling opposition defenses.
Lorem Ipsum has been the industry’s standard dummy text https://cakehr.dk/jkbepup of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://rajeshguru.in/pcfhp of type and scrambled it to make a type specimen book.
Информационный ресурс https://ardma.ru, посвящен бизнесу, финансам, инвестициям и криптовалютам. Сайт предлагает экспертные статьи, аналитические отчеты, стратегии и советы для предпринимателей и инвесторов. Здесь можно найти новости и обзоры о бизнесе, маркетинге, трейдинге, а также практические рекомендации по различным видам заработка и управлению финансами.
Lorem Ipsum has been the industry’s standard dummy text https://stepspdf.cfd/wglzrrr of type and scrambled it to make a type specimen book.
школа сёрфинга кайт сафари хургада
Lorem Ipsum has been the industry’s standard dummy text https://ilclubdigitale.it/ylzzr of type and scrambled it to make a type specimen book.
кайт школа Египет есть ли в нораке акулы
Real Madrid midfielder Rodrigo https://rodrygo.prostoprosport-ar.com gave Madrid the lead in the Champions League quarter-final first leg against Manchester City. The meeting takes place in Madrid. Rodrigo scored in the 14th minute after a pass from Vinicius Junior.
заказать магнитики на холодильник – изготовление магнитных пазлов, !магниты +на заказ
Lorem Ipsum has been the industry’s standard dummy text https://evafinans.dk/bcfjj of type and scrambled it to make a type specimen book.
Курс биткоина – метавселенные, статьи про криптовалюты
Lorem Ipsum has been the industry’s standard dummy text https://sofiaporelmundo.es/xhhzpk of type and scrambled it to make a type specimen book.
south park южный парк смотреть
Lorem Ipsum has been the industry’s standard dummy text https://liftex.es/gjjjycl of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://agescimortara1.it/qavom of type and scrambled it to make a type specimen book.
магазин электрокаминов – биокамины цены фото, биокамин напольный
букет роз Киев – доставка цветов на дом Киев, купить цветы Киев
жк купить квартиру от застройщика купить квартиру в казани от застройщика
Можете выбрать гантельные грифы на https://grify-dlya-gantely.ru по доступным ценамнеобходимой длины. В изготовлении качественных продуктов используются инновационные марки металла. Гантельные составляющие выпускаются в трех востребованных диаметрах. Отягощения разработаны для силовых занятий и созданы с разметкой для правильного размещения рук и насечками для надежного хвата. Изделия покрываются предохранительным слоем хрома. Отечественная фирма выпускает внушительный ассортимент тренировочного оборудования для дома и фитнес центра. Это эффективный инвентарь для силовых занятий в любых условиях.
Hi there are using WordPress for your blog platform? I’m new to the blog world but I’m trying to get started and create my own. Do you need any html coding knowledge to make your own blog? Any help would be really appreciated!
ehealthfiles.com/Differentiators.html
chefrobertsdirect.com/index.php?main_page=page&id=2
russianecuador.com/member.php?tab=visitor_messaging&u=13207&page=20
my-digital.ro/contact/
img-group.ru/Partners.html
Открытие магазина на телеграмме с нуля – готовый телеграм бот магазин, сделать бота в телеграм
click for source
OSIRIS-REx capsule lands with extraterrestrial treasure
Карьерный коуч https://vminske.by/fashion/kto-takie-karernye-konsultanty — эксперт рынка труда, который помогает людям определить свои карьерные цели, развиваться в выбранной области и достигать успеха в профессиональной деятельности.
жк купить квартиру от застройщика жк купить квартиру от застройщика
Снимки, выполненные на фотобумаге профессионального уровня – это настоящий фотоархив, который дарит яркие эмоции долгие годы. Качественная печать фотографий на холсте из 100% хлопка с натяжкой на деревянный подрамник печать фото больших размеров
Снимки, выполненные на фотобумаге профессионального уровня – это настоящий фотоархив, который дарит яркие эмоции долгие годы. Качественная печать фотографий на холсте из 100% хлопка с натяжкой на деревянный подрамник печать фотографий 10х15
заказать продвижение сайта seo seo продвижение
стоимость оптимизация сайта стоимость оптимизация сайта
Lorem Ipsum has been the industry’s standard dummy text https://prodottinautica.it/vmrrwpk of type and scrambled it to make a type specimen book.
купить диплом в перми купить диплом в перми .
online buy medicine nolvadex 10mg
Thanks for any other informative blog. The place else could I am getting that type of information written in such a perfect manner? I’ve a challenge that I’m simply now running on, and I’ve been on the glance out for such info.
calltraxplus.com/call-tracking-software
chatrang.shop/products/coupplus
politictoday.ru/page/39
jayaramcards.com/Home/buynow/97
student-news.ru/page/2
Lorem Ipsum has been the industry’s standard dummy text https://derivedsolutions.in/dhsgg of type and scrambled it to make a type specimen book.
you’re really a just right webmaster. The website loading pace is incredible. It sort of feels that you are doing any distinctive trick. Furthermore, The contents are masterwork. you have done a great job in this subject!
atlanticairsoft.airsoftcanada.com/group.php?do=discuss&group=&discussionid=1780
astoriamattress.com/information-blogger?blogger_id=2
animesocial.su/blogs/1046/%D0%A1%D0%BA%D0%BE%D0%BB%D1%8C%D0%BA%D0%BE-%D0%BF%D1%80%D0%B8%D0%BC%D0%B5%D1%80%D0%BD%D0%BE-%D0%BC%D0%BE%D0%B6%D0%B5%D1%82-%D1%81%D1%82%D0%BE%D0%B8%D1%82%D1%8C-%D1%81%D0%B5%D0%B3%D0%BE%D0%B4%D0%BD%D1%8F-%D0%BA%D0%B0%D1%87%D0%B5%D1%81%D1%82%D0%B2%D0%B5%D0%BD%D0%BD%D1%8B%D0%B9-%D0%B4%D1%83%D0%B1%D0%BB%D0%B8%D0%BA%D0%B0%D1%82-%D0%B4%D0%B8%D0%BF%D0%BB%D0%BE%D0%BC%D0%B0
cfdom.ru/index.php?links_exchange=yes&page=224&show_all=yes
http://www.vehicleskins.com/memberlist.php?mode=joined&order=ASC&start=241000
Lorem Ipsum has been the industry’s standard dummy text https://abc-datenservice.de/jnhrzzb of type and scrambled it to make a type specimen book.
купить диплом строителя diplomvash.ru .
услуги seo оптимизация https://prodvizhenye-seo.ru
Lorem Ipsum has been the industry’s standard dummy text https://spiwin.pl/omnsl of type and scrambled it to make a type specimen book.
Мы собрали актуальные промокоды Мегамаркет на первый и повторный заказ! Не упустите шанс! 21 июня 2024 года на megamarket.ru действуют особенно выгодные предложения Мегамаркет промокод на заказ
Мы собрали актуальные промокоды Мегамаркет на первый и повторный заказ! Не упустите шанс! 21 июня 2024 года на megamarket.ru действуют особенно выгодные предложения промокод мегамаркет июнь
Lorem Ipsum has been the industry’s standard dummy text https://alzagaconsulting.es/sehhi of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://amaterasuspa.pl/etuwnam of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://cpas-oliveiragomes.pt/afvxr of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://sukrticollections.in/tupwgij of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://fleurbase.dk/vpvuz of type and scrambled it to make a type specimen book.
https://Dr-nona.ru – Dr. Nona
Lorem Ipsum has been the industry’s standard dummy text https://buytron.co.za/rvvigmz of type and scrambled it to make a type specimen book.
vermox 100 mg otc
Lorem Ipsum has been the industry’s standard dummy text https://rampymobilne.pl/exitw of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://salvatierrasostenible.es/btvbei of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://durgaspa.in/nvyswri of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://chiaradventure.it/ejonsv of type and scrambled it to make a type specimen book.
play aviator game online play aviator game online .
Престижные вакансии для девушек в сфере элитных эскорт услуг в СПБ. Быть независимой, самостоятельно зарабатывать на жизнь и не иметь ограничений – главная прерогатива всех современных леди работа девушкам эскорт спб
Престижные вакансии для девушек в сфере элитных эскорт услуг в СПБ. Быть независимой, самостоятельно зарабатывать на жизнь и не иметь ограничений – главная прерогатива всех современных леди Эскорт спб для девушек работа
Greetings! I know this is kinda off topic however I’d figured I’d ask. Would you be interested in trading links or maybe guest writing a blog article or vice-versa? My blog covers a lot of the same topics as yours and I believe we could greatly benefit from each other. If you happen to be interested feel free to send me an email. I look forward to hearing from you! Fantastic blog by the way!
bpelena.org.ua/perevod-telefonnyh-razgovorov/
codespit.com/zone/rss.htm
carrefour-emploi-public.fr/brest-metropole-oceane
foro.muelendhir.com/showthread.php?tid=4597&pid=19880&mode=threaded
talkrealty.ru/page/3
Lorem Ipsum has been the industry’s standard dummy text https://oxybasket.in/tpbvr of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://ilclubdigitale.it/izqhh of type and scrambled it to make a type specimen book.
лаки джет 1win лаки джет 1win .
Копицентр предоставляет выгодные цены на полиграфическую продукцию и дарим скидку 10% на повторные заказы салон фотографии москва
Копицентр предоставляет выгодные цены на полиграфическую продукцию и дарим скидку 10% на повторные заказы салон фотографии
Lorem Ipsum has been the industry’s standard dummy text https://pawslo.pl/lwfhto of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://analisidebiti.it/adewx of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://hostindiaa.in/rgbnwf of type and scrambled it to make a type specimen book.
Лучшие курсы стероидов и анаболиков купить в официальном интернет магазине спортивной фармакологии Pharmacom Labs онлайн Pharmacom купить
Lorem Ipsum has been the industry’s standard dummy text https://mateuszglanert.pl/rndgbru of type and scrambled it to make a type specimen book.
Лучшие курсы стероидов и анаболиков купить в официальном интернет магазине спортивной фармакологии Pharmacom Labs онлайн Pharmacom
Lorem Ipsum has been the industry’s standard dummy text https://kroatiereis.nl/kqttdg of type and scrambled it to make a type specimen book.
lyrica 150 mg price
Lorem Ipsum has been the industry’s standard dummy text https://sukrticollections.in/shmvpmm of type and scrambled it to make a type specimen book.
кайт сафари с любимовым кайтсерфинг в москве и подмосковье
Unleash your creativity past crafting your own stories in https://storyteller-games.com. Away placing characters and scenes in different arrangements, players can make unique narratives. The mere disinterested of Storyteller is to nurture creative powers and strategic planning, offering a captivating taste fitting for fans of storytelling.
Lorem Ipsum has been the industry’s standard dummy text https://fotolubin.pl/rzwvosg of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://agamagizhan.in/fooam of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://loksangharshlivenews.in/ptrkz of type and scrambled it to make a type specimen book.
Hi, of course this piece of writing is in fact pleasant and I have learned lot of things from it on the topic of blogging. thanks.
shkaranov.ru/Obruchalnie-i-venchalnie-kolca/page7.html
petcreche.com.br/fotos-e-videos/fotos/page/4/
http://www.mountbarkertourismwa.com.au/contact_us.php
vseogirls.ru/diplomyi-s-unikalnyim-dizaynom-i-oformleniem
dr650.ehehe.net/cgi/bbs/discourse/c_board.cgi?page=0&mode=move&pass=&u_max=&tmpl=
Lorem Ipsum has been the industry’s standard dummy text https://you2i.dk/ttxrmvl of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://spawenginering.pl/etdty of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://viaggiarefree.it/kwjhd of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://sanexim.pl/oohvy of type and scrambled it to make a type specimen book.
Элитное эскорт агентство, которое оказывает услуги не только в Сочи, но и по всему миру. Девушки нашего агентства оказывают элитное эскорт сопровождение Проститутки красная поляна
Lorem Ipsum has been the industry’s standard dummy text https://gomalta.co.za/hcgkcc of type and scrambled it to make a type specimen book.
Элитное эскорт агентство, которое оказывает услуги не только в Сочи, но и по всему миру. Девушки нашего агентства оказывают элитное эскорт сопровождение Проститутки в сочи
Lorem Ipsum has been the industry’s standard dummy text https://limpiezasletsgo.es/hmxdg of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://trajesmotocross.es/vvxtrtx of type and scrambled it to make a type specimen book.
новые сервера ла2 хф
Сервера ла2
Lorem Ipsum has been the industry’s standard dummy text https://kalexkursy.pl/rrsxi of type and scrambled it to make a type specimen book.
это профессиональное модельное агентство эскорт, которое предоставляет выбор высокооплачиваемых вакансий для девушек, желающих работу-досуг и развлечений. Мы специализируемся на предоставлении услуг VIP-эскорта Эскорт для девушек работа
это профессиональное модельное агентство эскорт, которое предоставляет выбор высокооплачиваемых вакансий для девушек, желающих работу-досуг и развлечений. Мы специализируемся на предоставлении услуг VIP-эскорта работа девушкам эскорт
Lorem Ipsum has been the industry’s standard dummy text https://cakehr.dk/dzxntll of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://spahouse.dk/nkbynd of type and scrambled it to make a type specimen book.
provigil cost canada
Lorem Ipsum has been the industry’s standard dummy text https://guacamayaproducciones.es/fhgipu of type and scrambled it to make a type specimen book.
Find here UAE Prayer Timings, Muslim Prayer Timings, Imsak Time, Iftar Timings, Fajr Time and more updates from Khaleej Times http://timenamaz.online/
Lorem Ipsum has been the industry’s standard dummy text https://wnioseksde.pl/xvrgxc of type and scrambled it to make a type specimen book.
Vinicius Junior https://viniciusjunior.prostoprosport-ar.com is a Brazilian and Spanish footballer who plays as a striker for Real Madrid and the Brazilian national team. Junior became the first player in the history of Los Blancos, born in 2000, to play an official match and score a goal.
Kylian Mbappe https://kylianmbappe.prostoprosport-ar.com is a French footballer, striker for Paris Saint-Germain and captain of the French national team. He began playing football in the semi-professional club Bondi, which plays in the lower leagues of France. He was noticed by Monaco scouts, which he joined in 2015 and that same year, at the age of 16, he made his debut for the Monegasques. The youngest debutant and goal scorer in the club’s history.
Lorem Ipsum has been the industry’s standard dummy text https://constructoraamiel.cl/lqhkok of type and scrambled it to make a type specimen book.
May I simply just say what a relief to discover an individual who genuinely knows what they are talking about on the internet. You actually understand how to bring an issue to light and make it important. More people should check this out and understand this side of the story. I was surprised that you’re not more popular given that you certainly have the gift.
ravolutionfestival.com/ravolution202205hcmc/
maisoncarlos.com/UserProfile/tabid/42/UserID/1942955/Default.aspx
irc71.ru/index.php/jomsocial/groups/viewbulletin/142-za-skolko-imenno-vozmozhno-budet-zakazat-diplom-vuza-sejchas?groupid=47
otantravel.kz/news/swiss-uvelichivaet-kolichestvo-reysov-mayyami-cyurih-na-period-zimnego-sezona
blog.libero.it/wp/interesting/page/3/
Lorem Ipsum has been the industry’s standard dummy text https://crowd1sinergia.es/ldhum of type and scrambled it to make a type specimen book.
I think everything published was actually very logical. But, think about this, what if you were to create a killer headline? I am not suggesting your information isn’t solid., however what if you added a post title to possibly grab people’s attention? I mean %BLOG_TITLE% is a little boring. You could peek at Yahoo’s home page and note how they write post headlines to grab viewers to click. You might add a related video or a pic or two to get people interested about what you’ve got to say. Just my opinion, it would make your posts a little bit more interesting.
http://www.as7abe.com/wall/blogs/user/sonnick84?&page=3
cocochampionship.com/en/contact
metkonstrukt.ru/kupit-kalitku/
militarymuster.ca/forum/showthread.php?mode=threaded&tid=339886&pid=381832
balaklavskiy-16.ru/user/9827/
Lorem Ipsum has been the industry’s standard dummy text https://prokoppraceziemne.pl/mwtrc of type and scrambled it to make a type specimen book.
Karim Benzema https://karimbenzema.prostoprosport-ar.com is a French footballer who plays as a striker for the Saudi Arabian club Al-Ittihad. He played for the French national team, for which he played 97 matches and scored 37 goals. At the age of 17, he became one of the best reserve players, scoring three dozen goals per season.
Lorem Ipsum has been the industry’s standard dummy text https://pubpropaganda.pl/dhxfr of type and scrambled it to make a type specimen book.
Victor James Osimhen https://victorosimhen.prostoprosport-ar.com is a Nigerian footballer who plays as a forward for the Italian club Napoli and the Nigerian national team. In 2015, he was recognized as the best football player in Africa among players under 17 according to the Confederation of African Football.
Gaza Philip preached of Christ and baptized an Ethiopian eunuch on his way to Gaza (Acts 8:26–39). Jerusalem See map 12 for events in Jerusalem Hotel Majestic Tunis (Since 1913) Tunisia, Tunis
Gaza Philip preached of Christ and baptized an Ethiopian eunuch on his way to Gaza (Acts 8:26–39). Jerusalem See map 12 for events in Jerusalem Genesis Sodom and Gomorrah Map
Lorem Ipsum has been the industry’s standard dummy text https://sonoricco.it/wckkpr of type and scrambled it to make a type specimen book.
bactrim generic brand
Unlock More Exciting Promotions at 1xBet India
1xBet free bet promo code: . Sign up and receive a 100% bonus up to €100 in free bets. 1xBet is a reliable bookmaker that is committed to building a long-term relationship with every customer. We guarantee a personalized approach in your best interest, easy payment methods, and most importantly, 100% payouts on all winning bets. 1xBet India doesn’t stop at the welcome bonuses. There are several other enticing promotions available for Indian customers to enhance their gaming experience. Take a look at these ongoing promotions:
Lucky Friday: Every Friday, 1xBet India offers a bonus of up to 100€. To claim this bonus, simply log in to your 1xBet account, deposit any amount (minimum €1), and ensure your account is active. The bonus will be automatically credited, matching 100% of your deposit amount, up to €100. To receive the bonus, you must wager the bonus amount three times on accumulator bets within 24 hours. Make sure to review the full terms and conditions before participating.
x2 Wednesday Promotion: On Wednesdays, while the promotion is active, 1xBet offers a bonus of up to 100€. To qualify, you need to have participated in the “Lucky Friday” offer the week before and redeemed your bonus. Log in to your 1xBet account and place five bets on any sporting event on Monday and Tuesday with minimum odds of 1.40. Additionally, make a deposit of up to €100 on Wednesday. The bonus will be credited automatically, matching 100% of your deposit amount, up to €100. To redeem the bonus, you must meet the 3x wagering requirements through accumulator bets within 24 hours. Familiarize yourself with the terms and conditions before participating.
1xBet promo code casino: , allows you to benefit from a 100% increase in the 1xBet casino welcome package of ?130,000. This implies that you can receive up to ?169,000 in total through four separate deposits. By signing up with this promotional code, you are ensuring an improved betting experience on 1xBet. 1xBet is a reputable and renowned bookmaker that provides a diverse selection of sports betting opportunities and enticing promotions for the year 2024.
On the platform, you will find a diverse selection of sports to bet on, including football, tennis, basketball, and more. With competitive odds and favorable betting conditions, you can increase your chances of success and make your time on the platform even more thrilling. Additionally, you will receive €100 in free bets, which will further enhance your betting opportunities.
1xBet is a trusted bookmaker that is known for its reliability and excellent customer service. By taking advantage of this promo code, you can enjoy the excitement of free betting without any initial risk. Don’t miss out on this opportunity to maximize your winnings and enjoy a top-notch betting experience on 1xBet.
Don’t miss out on this incredible opportunity. Claim your share of up to €100 in free bets today by registering on 1xBet with the 1xBet promo code free. Start your betting journey with confidence and excitement, backed by an outstanding bonus offer tailored just for you.
A more detailed description of how to correctly use a promotional code when registering with 1xBet — http://ftvmilfs.net/art/chto_takoe_biorevitalizaciya.html
visit this site Sandbox Airdrop
Lorem Ipsum has been the industry’s standard dummy text https://npf-paker.es/puqseum of type and scrambled it to make a type specimen book.
More about the author VoxEdit – NFT Creator
This Site Creative your account sandbox
Visit Your URL Official Airdrop Is Live!
lasix sale
https://salah-time.online/
Портал о здоровье https://www.rezus.ru и здоровом образе жизни, рекомендации врачей и полезные сервисы. Простые рекомендации для укрепления здоровья и повышения качества жизни.
Toni Kroos https://tonikroos.prostoprosport-ar.com is a German footballer who plays as a central midfielder for Real Madrid and the German national team. World champion 2014. The first German player in history to win the UEFA Champions League six times.
Unlock More Exciting Promotions at 1xBet India
1xBet free bet promo code: . Sign up and receive a 100% bonus up to €100 in free bets. 1xBet is a reliable bookmaker that is committed to building a long-term relationship with every customer. We guarantee a personalized approach in your best interest, easy payment methods, and most importantly, 100% payouts on all winning bets. 1xBet India doesn’t stop at the welcome bonuses. There are several other enticing promotions available for Indian customers to enhance their gaming experience. Take a look at these ongoing promotions:
Lucky Friday: Every Friday, 1xBet India offers a bonus of up to 100€. To claim this bonus, simply log in to your 1xBet account, deposit any amount (minimum €1), and ensure your account is active. The bonus will be automatically credited, matching 100% of your deposit amount, up to €100. To receive the bonus, you must wager the bonus amount three times on accumulator bets within 24 hours. Make sure to review the full terms and conditions before participating.
x2 Wednesday Promotion: On Wednesdays, while the promotion is active, 1xBet offers a bonus of up to 100€. To qualify, you need to have participated in the “Lucky Friday” offer the week before and redeemed your bonus. Log in to your 1xBet account and place five bets on any sporting event on Monday and Tuesday with minimum odds of 1.40. Additionally, make a deposit of up to €100 on Wednesday. The bonus will be credited automatically, matching 100% of your deposit amount, up to €100. To redeem the bonus, you must meet the 3x wagering requirements through accumulator bets within 24 hours. Familiarize yourself with the terms and conditions before participating.
1xBet promo code casino: , allows you to benefit from a 100% increase in the 1xBet casino welcome package of ?130,000. This implies that you can receive up to ?169,000 in total through four separate deposits. By signing up with this promotional code, you are ensuring an improved betting experience on 1xBet. 1xBet is a reputable and renowned bookmaker that provides a diverse selection of sports betting opportunities and enticing promotions for the year 2024.
On the platform, you will find a diverse selection of sports to bet on, including football, tennis, basketball, and more. With competitive odds and favorable betting conditions, you can increase your chances of success and make your time on the platform even more thrilling. Additionally, you will receive €100 in free bets, which will further enhance your betting opportunities.
1xBet is a trusted bookmaker that is known for its reliability and excellent customer service. By taking advantage of this promo code, you can enjoy the excitement of free betting without any initial risk. Don’t miss out on this opportunity to maximize your winnings and enjoy a top-notch betting experience on 1xBet.
Don’t miss out on this incredible opportunity. Claim your share of up to €100 in free bets today by registering on 1xBet with the 1xBet promo code free. Start your betting journey with confidence and excitement, backed by an outstanding bonus offer tailored just for you.
A more detailed description of how to correctly use a promotional code when registering with 1xBet — http://crocotheme.com/wp-content/pgs/1xbet_promo_code_420.html
служба по вскрытию замков номер [url=http://vskrytie-zamkov-moskva113.ru/]служба по вскрытию замков номер[/url] .
Lorem Ipsum has been the industry’s standard dummy text https://platformzelfredzaam.nl/bdaaza of type and scrambled it to make a type specimen book.
Robert Lewandowski https://robertlewandowski.prostoprosport-ar.com is a Polish footballer, forward for the Spanish club Barcelona and captain of the Polish national team. Considered one of the best strikers in the world. Knight of the Commander’s Cross of the Order of the Renaissance of Poland.
Lorem Ipsum has been the industry’s standard dummy text https://gs-stroehe.de/rkuaqmm of type and scrambled it to make a type specimen book.
сериал волчонок бесплатно хорошего качества https://volchonok-tv.ru
Lorem Ipsum has been the industry’s standard dummy text https://mobilitatelx.es/iniww of type and scrambled it to make a type specimen book.
I loved as much as you’ll receive carried out right here. The sketch is tasteful, your authored subject matter stylish. nonetheless, you command get got an impatience over that you wish be delivering the following. unwell unquestionably come more formerly again as exactly the same nearly a lot often inside case you shield this hike.
Del Mar Energy
Lorem Ipsum has been the industry’s standard dummy text https://lastresortshop.es/psyeo of type and scrambled it to make a type specimen book.
El uso regular de Yenki Derm puede reducir la apariencia de arrugas. Yenki Derm precio farmacia Guadalajara
El uso regular de Yenki Derm puede reducir la apariencia de arrugas. Yenki Derm Farmacia del Ahorro precio
Lorem Ipsum has been the industry’s standard dummy text https://gs-stroehe.de/hoippjh of type and scrambled it to make a type specimen book.
Mohamed Salah https://mohamedsalah.prostoprosport-ar.com is an Egyptian footballer who plays as a forward for the English club Liverpool and the Egyptian national team. Considered one of the best football players in the world. Three-time winner of the English Premier League Golden Boot: in 2018 (alone), 2019 (along with Sadio Mane and Pierre-Emerick Aubameyang) and 2022 (along with Son Heung-min).
Lorem Ipsum has been the industry’s standard dummy text https://creosell.pl/txotwm of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://carolinaisasi.es/ciyae of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://agasiwek.pl/bhaftz of type and scrambled it to make a type specimen book.
buy tiktok followers and likes buy tiktok likes
Lorem Ipsum has been the industry’s standard dummy text https://bjproductions.nl/qyoydsh of type and scrambled it to make a type specimen book.
combivent 18 103 mcg
Lorem Ipsum has been the industry’s standard dummy text https://mlckerala.in/fbigwd of type and scrambled it to make a type specimen book.
Hello to all, for the reason that I am actually keen of reading this web site’s post to be updated on a regular basis. It consists of pleasant stuff.
#GGG###
https://augustgcuk53310.bloggazzo.com/27022419/еЏ°ж№ѕеЏ·з Ѓ-ж–‡еЊ–дј ж‰їдёЋж•°е—еЊ–жј”еЏ
Lorem Ipsum has been the industry’s standard dummy text https://stepsdown.lat/slnjm of type and scrambled it to make a type specimen book.
Официальный городской информационный портал – новости Ижевска и Удмуртии, криминал, дорожно-транспортные происшествия (ДТП), чрезвычайные происшествия(ЧП) https://vk.com/mdps18
Lionel Andres Messi Cuccittini https://lionelmessi.prostoprosport-ar.com is an Argentine footballer, forward and captain of the MLS club Inter Miami, captain of the Argentina national team. World champion, South American champion, Finalissima winner, Olympic champion. Considered one of the best football players of all time.
Cristiano Ronaldo https://cristiano-ronaldo.prostoprosport-ar.com is a Portuguese footballer, forward, captain of the Saudi Arabian club An-Nasr and the Portuguese national team. European Champion. Considered one of the best football players of all time. The best scorer in the history of football according to the IFFIS and fourth according to the RSSSF
Lorem Ipsum has been the industry’s standard dummy text https://evafinans.dk/bhiswjp of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://spahouse.dk/imycqsb of type and scrambled it to make a type specimen book.
Узнать больше https://filmos.net/
Lorem Ipsum has been the industry’s standard dummy text https://gastroludki.pl/pztwqlk of type and scrambled it to make a type specimen book.
продвижение сайтов в москве яндекс оплата за результат продвижение сайтов в москве яндекс оплата за результат .
Lorem Ipsum has been the industry’s standard dummy text https://icatindia.in/rwbof of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://miglierinacomunitaospitale.it/wfckx of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://blogn97.pl/vlcfijl of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://gomalta.co.za/aozlpua of type and scrambled it to make a type specimen book.
Anderson Sousa Conceicao better known as Talisca https://talisca.prostoprosport-ar.com is a Brazilian footballer who plays as a midfielder for the An-Nasr club. A graduate of the youth team from Bahia, where he arrived in 2009 ten years ago.
Yassine Bounou https://yassine-bounou.prostoprosport-ar.com also known as Bono, is a Moroccan footballer who plays as a goalkeeper for the Saudi Arabian club Al-Hilal and the Moroccan national team. On November 10, 2022, he was included in the official application of the Moroccan national team to participate in the matches of the 2022 World Cup in Qatar
Lorem Ipsum has been the industry’s standard dummy text https://forexandfreedom.pl/psdtmt of type and scrambled it to make a type specimen book.
Искал автошколу в своем районе у м. Аэропорт или Сокол, там одна улица проходит. Считаю, что сделал неплохой выбор автошкола митино
Lorem Ipsum has been the industry’s standard dummy text https://puszystykocyk.pl/oguyk of type and scrambled it to make a type specimen book.
Искал автошколу в своем районе у м. Аэропорт или Сокол, там одна улица проходит. Считаю, что сделал неплохой выбор автошкола строгино
Достижение положительного результата в освоении управления легковым автомобилем и получении водительских прав гарантирует автошкола с репутацией онлайн обучение на водительские права
Достижение положительного результата в освоении управления легковым автомобилем и получении водительских прав гарантирует автошкола с репутацией автошкола в солнцево
Lorem Ipsum has been the industry’s standard dummy text https://fokusklinikken.dk/pcgstta of type and scrambled it to make a type specimen book.
Harry Edward Kane https://harry-kane.prostoprosport-ar.com is an English footballer, forward for the German club Bayern and captain of the England national team. Considered one of the best football players in the world. He is Tottenham Hotspur’s and England’s all-time leading goalscorer, as well as the second most goalscorer in the Premier League. Member of the Order of the British Empire.
Neymar da Silva Santos Junior https://neymar.prostoprosport-ar.com is a Brazilian footballer who plays as a striker, winger and attacking midfielder for the Saudi Arabian club Al-Hilal and the Brazilian national team. Considered one of the best players in the world. The best scorer in the history of the Brazilian national team.
Lorem Ipsum has been the industry’s standard dummy text https://sonnosgroup.es/lhqpvac of type and scrambled it to make a type specimen book.
Алкопрезент
Lorem Ipsum has been the industry’s standard dummy text https://dgkservice.it/ylzei of type and scrambled it to make a type specimen book.
Erling Breut Haaland https://erling-haaland.prostoprosport-ar.com is a Norwegian footballer who plays as a forward for the English club Manchester City and the Norwegian national team. English Premier League record holder for goals per season.
Lorem Ipsum has been the industry’s standard dummy text https://creepy.es/maspjpj of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://dankesamba.de/srtqy of type and scrambled it to make a type specimen book.
Ali al-Buleahi https://ali-al-bulaihi.prostoprosport-ar.com Saudi footballer, defender of the club ” Al-Hilal” and the Saudi Arabian national team. On May 15, 2018, Ali al-Buleakhi made his debut for the Saudi Arabian national team in a friendly game against the Greek team, coming on as a substitute midway through the second half.
Lorem Ipsum has been the industry’s standard dummy text https://tscapp.es/isiyo of type and scrambled it to make a type specimen book.
look what i found hacker fortnite
http://kvadrociklov-prokat.ru/
Luka Modric https://lukamodric.prostoprosport-ar.com is a Croatian footballer, central midfielder and captain of the Spanish club Real Madrid, captain of the Croatian national team. Recognized as one of the best midfielders of our time. Knight of the Order of Prince Branimir. Record holder of the Croatian national team for the number of matches played.
Lorem Ipsum has been the industry’s standard dummy text https://evafinans.dk/ribie of type and scrambled it to make a type specimen book.
http://atvbizon.ru/
Lorem Ipsum has been the industry’s standard dummy text https://skybet365.es/ztjmq of type and scrambled it to make a type specimen book.
advice how to mod fortnite
buy 100k tiktok followers https://iemlabs.com/blogs/make-money-on-tiktok-without-followers-in-2024-easy-guide/
Lorem Ipsum has been the industry’s standard dummy text https://onderhoudsbedrijfpeerdeman.nl/bcdyg of type and scrambled it to make a type specimen book.
buy tiktok followers uk how to buy followers on tiktok
Lorem Ipsum has been the industry’s standard dummy text https://buytron.co.za/fzztuzq of type and scrambled it to make a type specimen book.
Pinterest advertising for the USA and English-speaking countries. Etsy, amazon, shopify, ebay
lasix 40 mg uk
http://ek-x.ru/
средство гигиены интимной зоны Средства для интимной гигиены IntiLINE
Pinterest advertising for the USA and English-speaking countries. Etsy, amazon, shopify, ebay
The best film magazin https://orbismagazine.com, film industry trade publications in 2024 to keep you informed with the latest video production, filmmaking, photographynews. We create beautiful and magnetic projects.
https://vyzov-santehnika-na-dom.ru.
https://livecamsporno.com/
Lorem Ipsum has been the industry’s standard dummy text https://tuttomedicale.it/jzgudjt of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://genomatics.de/xsxtqx of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://acidmedia.pl/ttilwev of type and scrambled it to make a type specimen book.
Взять займ или кредит
https://kohuku.ru/other/5864-kreditnaja-karta-luchshie-predlozhenija.html под проценты, подав заявку на денежный микрозайм для физических лиц. Выбирайте среди 570 лучших предложений займа онлайн. Возьмите микрозайм онлайн или наличными в день обращения. Быстрый поиск и удобное сравнение условий по займам и микрокредитам в МФО.
NGolo Kante https://ngolokante.prostoprosport-ar.com is a French footballer who plays as a defensive midfielder for the Saudi Arabian club Al-Ittihad and the French national team. His debut for the first team took place on May 18, 2012 in a match against Monaco (1:2). In the 2012/13 season, Kante became the main player for Boulogne, which played in Ligue 3.
“Дело “Лайф-из-Гуд” — “Гермес” — “Бест Вей”: свидетель обвинения объявила себя потерпевшей от следствия
Уголовное дело компании Бест Вей
6 и 13 июня Приморский районный суд города Санкт-Петербурга, рассматривающий по существу уголовное дело № 1-504/24, связываемое с компаниями “Лайф-из-Гуд”, “Гермес” и кооперативом “Бест Вей”, провел очередные, шестое и седьмое по счету, заседания, посвященные допросу свидетелей обвинения и лиц, признанных следствием потерпевшими в рамках судебного следствия по делу
“К кооперативу претензий не было, следователь предложил подать заявление”
Признанный следствием потерпевший Болян подсудимых не знает. Был клиентом “Гермеса”, а также пайщиком кооператива — но до 2019 года. В 2019-м он вышел из кооператива и из “Гермеса”, ему были возвращены паевые взносы, и никаких претензий к кооперативу у него не было — что он письменно подтвердил, расторгая договоры с этими организациями.
Однако, как Болян отметил на суде, следователь убедил его в том, что он — потерпевший и должен подать заявление на возврат членских взносов. Заявление в МВД писать не хотел, на него вышли сотрудники, сначала претензий к кооперативу не было. Полиция ему объяснила, что можно получить деньги.
Стал клиентом “Гермеса” и пайщиком кооператива через своего консультанта Алексея Виноградова. Виноградов — грамотный маркетолог, он ему верил, тот не работал в кооперативе. Что было предметом договора в “Гермесе”, не помнит. В “Гермес” внес 100 и 700 евро, а в кооператив каждый месяц вносил по 12 тыс. в течение семи месяцев.
Вышел и из кооператива, и из “Гермеса” в 2019 году. Зачем вступал? “Наверное, квартиру купить хотел”. Кооператив вернул ему 70 тыс. паевых взносов, “Гермес” вернул со счета “Виста” 140 тыс. рублей.
В кооперативе деньги вернули почти сразу, удержав вступительный и членские взносы; в “Гермесе” вернули позже через “внутрянку”, но удержали комиссию.
Утверждает, что ему говорили, что можно со счета “Виста” вносить деньги в кооператив. Объясняли, что деньги передаются в доверительное управление трейдерам и брокерам, которые играют на бирже. В кооперативе, как он утверждает, можно было купить место в очереди. По его словам, “Гермес” и кооператив — по сути, одна организация. Требует взыскать с кооператива более 148 тыс. рублей — вступительный и членские взносы, и более 60 тыс. рублей с “Гермеса” — комиссию при выводе средств.
Договор с кооперативом не читал, но ему объяснили, что есть невозвратная часть денег — ее и не вернули, “но хочу попытаться вернуть”. Претензий к кооперативу “как бы и нет, но если вернут взносы, то будет хорошо”.
К Виноградову претензий не предъявлял. “Может, меня и не обманули в кооперативе”, -резюмировал свое выступление в суде Болян.
“Требую выплатить с учетом роста цен на недвижимость”
Признанная следствием потерпевшей Комова была как клиентом “Гермеса”, так и пайщиком кооператива. Подсудимых не знает. Требует более 8800 тыс. с кооператива и более 2700 тыс. с “Гермеса”. При этом из кооператива она не вышла и заявление о выходе не подавала. Сумма требований к кооперативу включает как паевые и членские взносы, так и оценку роста цен на недвижимость, которая не была приобретена.
Утверждает, что можно переводить деньги со счета “Виста” напрямую в кооператив — в подтверждение приводит скрины переписки с консультантами в смартфоне. Суд разъясняет, что доказательство может быть приобщено позднее при надлежащем оформлении.
“Информацию воспринял скептически, но вступил”
Признанный следствием потерпевшим Киреев был только клиентом “Гермеса”. Подсудимых не знает лично — Измайлова видел в видеоролике “Лайф-из-Гуд”. Узнал о “Гермесе” от консультантов Татьяны и Андрея Клейменовых, с которыми знаком с конца 1990-х годов. Вступил в “Гермес” в 2020 году, деньги сразу отобразились на счете. Вносил средства на счет “Виста” небольшими частями, снимал средства со счета для личных нужд. Заявляет требования на более чем 2 млн 300 тыс. рублей.
Когда подписывал договор, в офисе была табличка кооператива, но в офисе находился представитель фирмы “Гермес”, ему сказали, что это два продукта компании “Лайф-из-Гуд”.
В 2022 году начались проблемы с выводом средств. И руководство фирмы пугало блокировкой счета в случае подачи заявления в правоохранительные органы. В хейтерском чате узнал телефон следователя Сапетовой, позвонил и подал заявление.
В чате клиентов компании “Гермес” была информация о том, что счет будет заблокирован в случае подачи заявления в правоохранительные органы. Эта информация была за подписью “администрация”. Он спросил у консультантов: “Кто это — администрация?”, написал вопрос в чате, и его забанили. Других попыток вступать в диалог с “Гермесом” не предпринимал.
Признанный следствием потерпевшим Чернышенко был также только клиентом только компании “Гермес”. Подсудимых не знает. Познакомился с консультантами “Гермеса” во время совместной работы в “Макдоналдсе”. Информацию о “Гермесе” воспринял скептически — “это какой-то обман”, но консультанты его в конце концов уговорили. Они поставили условие, что продадут ему земельный участок, чтобы он вступил в “Гермес”.
“Я хотел их обмануть, — пояснил свидетель, — думал: пусть они продадут, а я в “Гермес” не вступлю. Но они начали уговаривать, и я вступил в апреле 2020 года. Один из консультантов дал расписку на внесение денег на счет в “Гермесе”, я внес через него 230 тыс. И еще раз из жадности 140 тыс. 140 тыс. я вывел, плюс каждый месяц выводил по 5000–7000 руб. С какого-то момента проценты стали падать. В конце я захотел выйти — но не успел. У меня в “Гермесе” осталось 270 тыс., которые я требую вернуть”.
В январе 2023 года Чернышенко подал заявление в полицию, так как прекратился доступ к счету. “Мне предложили 70 тыс. вернуть, чтобы я не ходил в полицию, ссылаясь на то, что помогли мне продать участок за меньшую сумму по документам, чем я его продал на самом деле, но я отказался, сказал, что мне надо 270 тыс.”.
“Я хочу стать потерпевшей. Но Василенко многие благодарны за квартиры”
Свидетель обвинения Галашенкова была только клиентом “Гермеса”. Из подсудимых знает Виктора Ивановича Василенко. Она сидела в зале при допросе двух потерпевших (что запрещено), но заявила, что плохо слышит. Ранее была знакома с Верой Исаевой из компании “Лайф-из-Гуд”.
Вера узнала, что у нее есть офис, и познакомила с Романом Василенко, который снял у нее офис, когда “Лайф-из-Гуд” только начинала раскручиваться. Он снимал офис только за коммунальные платежи. “Я попросила расплатиться за четыре месяца, а он предложил мне вместо денег вступить в “Бест Вей”, но я отказалась, так как квартира не была нужна”. Зато стала клиентом “Гермеса”: “Внесла 15 тыс. евро, но через три месяца на счете оказалось 3400 евро!” Исаева, по словам Галашенковой, оказалась мошенницей.
По словам Галашенковой, она внесла на счет “Виста” более 3 млн рублей. “Когда сказали, что все счета заблокировали, то собрали с нас еще денег, чтобы счета разблокировать, потом пришло сообщение, что открывается новая фирма, но это все оказалось обманом — счета не разблокированы”.
“Я не считала себя потерпевшей, так как не знала, что это можно сделать, — заявила Галашенкова. — Сейчас желаю заявить, что я хочу стать потерпевшей. Считаю, что должна взыскать с “Гермеса” как прямой ущерб, так и упущенную выгоду, так как эта фирма закрылась”.
При этом заявила, что “Василенко молодец, потому что я видела людей, которые купили квартиры, они были ему очень благодарны”.
1xBet free promo code: , get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
Ruben Diogo da Silva Neves https://ruben-neves.prostoprosport-ar.com is a Portuguese footballer who plays as a midfielder for the Saudi Arabian club Al-Hilal and the Portuguese national team. Currently, Ruben Neves plays for the Al-Hilal club wearing number 8. His contract with the Saudi club is valid until the end of June 2026.
https://Dr-Nona.ru – dr nona
haus kaufen in montenegro am meer hotels zum verkauf
https://www.livevideochat.xyz/
Lorem Ipsum has been the industry’s standard dummy text https://marielabertuggia.es/mmmwhr of type and scrambled it to make a type specimen book.
https://pornkingcams.com/
Lorem Ipsum has been the industry’s standard dummy text https://data-secure.fr/fehnben of type and scrambled it to make a type specimen book.
Купити ліхтарики https://bailong-police.com.ua оптом та в роздріб, каталог та прайс-лист, характеристики, відгуки, акції та знижки. Купити ліхтарик онлайн з доставкою. Відмінний вибір ліхтарів: налобні, ручні, тактичні, ультрафіолетові, кемпінгові, карманні за вигідними цінами.
Lorem Ipsum has been the industry’s standard dummy text https://mojafotografja.pl/lsuqk of type and scrambled it to make a type specimen book.
Kobe Bean Bryant https://kobebryant.prostoprosport-ar.com is an American basketball player who played in the National Basketball Association for twenty seasons for one team, the Los Angeles Lakers. He played as an attacking defender. He was selected in the first round, 13th overall, by the Charlotte Hornets in the 1996 NBA Draft. He won Olympic gold twice as a member of the US national team.
Lorem Ipsum has been the industry’s standard dummy text https://biztechnews.in/epbavmc of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://manfred-schnelldorfer.de/dfeyy of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://livin.com.mx/puxdil of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://willarybaki.pl/hpahkdq of type and scrambled it to make a type specimen book.
advair generic coupon
The most stunning transsexual shows on Stripchat. Popular trans chat rooms on free live sex cams. Watch, flirt, and have fun with trans cam models live trans cam
The most stunning transsexual shows on Stripchat. Popular trans chat rooms on free live sex cams. Watch, flirt, and have fun with trans cam models camstrans
Lorem Ipsum has been the industry’s standard dummy text https://sastoursandtravels.in/lxxxbw of type and scrambled it to make a type specimen book.
Продажа подземных канализационных ёмкостей https://neseptik.com по выгодным ценам. Ёмкости для канализации подземные объёмом до 200 м3. Металлические накопительные емкости для канализации заказать и купить в Екатеринбурге.
Lorem Ipsum has been the industry’s standard dummy text https://u-rumcajsa.pl/tvyec of type and scrambled it to make a type specimen book.
Наша компания проектирует бассейны любой сложности! Быстро и качественно построим бассейн. Бассейны под ключ по индивидуальным и готовым решениям. Поставляем оборудование для бассейнов зарубежных и отечественных производителей каркас бассейна пластиковый
Наша компания проектирует бассейны любой сложности! Быстро и качественно построим бассейн. Бассейны под ключ по индивидуальным и готовым решениям. Поставляем оборудование для бассейнов зарубежных и отечественных производителей фильтр pool king kp д 500 мм с верхним вентилем
Lorem Ipsum has been the industry’s standard dummy text https://sigma-radomsko.pl/yizztw of type and scrambled it to make a type specimen book.
Lebron Ramone James https://lebronjames.prostoprosport-ar.com American basketball player who plays the positions of small and power forward. He plays for the NBA team Los Angeles Lakers. Experts recognize him as one of the best basketball players in history, and a number of experts put James in first place. One of the highest paid athletes in the world.
Lorem Ipsum has been the industry’s standard dummy text https://pawslo.pl/lmlnqd of type and scrambled it to make a type specimen book.
Luis Fernando Diaz Marulanda https://luis-diaz.prostoprosport-ar.com Colombian footballer, winger for Liverpool and the Colombian national team . Diaz is a graduate of the Barranquilla club. On April 26, 2016, in a match against Deportivo Pereira, he made his Primera B debut. On January 30, 2022, he signed a contract with the English Liverpool for five years, the transfer amount was 40 million euros.
Lorem Ipsum has been the industry’s standard dummy text https://prodottinautica.it/gkqyt of type and scrambled it to make a type specimen book.
Juke-joint into the the public of KinitoPET https://kinitopetinfo.blogspot.com/2024/06/kinitoguide-game-guide.html, where players nurture and instruct a variety of pets. The predominating target is to keep pets fortuitous and trim while advancing throughout different challenges and levels.
Maria Sharapova https://maria-sharapova.prostoprosport-ar.com Russian tennis player. The former first racket of the world, winner of five Grand Slam singles tournaments from 2004 to 2014, one of ten women in history who has the so-called “career slam”.
Lorem Ipsum has been the industry’s standard dummy text https://blogn97.pl/jqqwwb of type and scrambled it to make a type specimen book.
We assure that repairs of any level of complexity will be finished within 3 days or sooner. Mechanics and electricians at PPR have experience working at authorized dealerships of Toyota, Land-Rover, Suzuki, Nissan, Mercedes, VAG, and BMW gmc dubai
We assure that repairs of any level of complexity will be finished within 3 days or sooner. Mechanics and electricians at PPR have experience working at authorized dealerships of Toyota, Land-Rover, Suzuki, Nissan, Mercedes, VAG, and BMW порше центр дубай
Lorem Ipsum has been the industry’s standard dummy text https://stepspdf.us/ousya of type and scrambled it to make a type specimen book.
https://fuckingcouple.com
cost of brand name synthroid
Lorem Ipsum has been the industry’s standard dummy text https://lacalabrianeifrancobolli.it/yftonza of type and scrambled it to make a type specimen book.
Kevin De Bruyne https://kevin-de-bruyne.prostoprosport-ar.com Belgian footballer, midfielder of the Manchester club City” and the Belgian national team. A graduate of the football clubs “Ghent” and “Genk”. In 2008 he began his adult career, making his debut with Genk.
Mohammed Khalil Ibrahim Al-Owais https://mohammed-alowais.prostoprosport-ar.com is a Saudi professional footballer who plays as a goalkeeper for the national team Saudi Arabia and Al-Hilal. He is known for his quick reflexes and alertness at the gate.
Lorem Ipsum has been the industry’s standard dummy text https://msizindlela.co.za/wumfic of type and scrambled it to make a type specimen book.
https://semlava.com/
Lorem Ipsum has been the industry’s standard dummy text https://mjoelnirsseite.de/bnjdcqe of type and scrambled it to make a type specimen book.
1xBet free promo code: , get vip sports bonus of 100% up to €/$130 (or the equivalent in your local currency). Our website is a treasure trove of the most up-to-date promotions and bonus codes for the year 2024. Moreover, when you register at 1xBet casino using this bonus code, you’ll be greeted with a welcome bonus of €/$1950 and 150 free spins. These incredible bonuses enhance every new player’s winning potential, allowing them to indulge in thrilling gameplay with bonus funds.
Quincy Anton Promes https://quincy-promes.prostoprosport-br.com Dutch footballer, attacking midfielder and forward for Spartak Moscow . He played for the Dutch national team. He won his first major award in 2017, when Spartak became the champion of Russia.
Lorem Ipsum has been the industry’s standard dummy text https://brightice.de/kdjkpm of type and scrambled it to make a type specimen book.
Экспертиза ремонта в квартире https://remnovostroi.ru проводится для оценки качества выполненных работ, соответствия требованиям безопасности и стандартам строительства. Специалисты проверяют используемые материалы, исполнение работ, конструктивные особенности, безопасность, внешний вид и эстетику ремонта. По результатам экспертизы составляется экспертное заключение с оценкой качества и рекомендациями по устранению недостатков.
Lorem Ipsum has been the industry’s standard dummy text https://gastroludki.pl/woqyzav of type and scrambled it to make a type specimen book.
canadian pharmacy accutane
Lorem Ipsum has been the industry’s standard dummy text https://mvdesk.in/uwjmob of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://rampymobilne.pl/rdhzkkw of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://caheha.dk/ijlhzui of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://samowystarczalnyzakatek.pl/kmjofic of type and scrambled it to make a type specimen book.
https://strip-cams.com/
Lorem Ipsum has been the industry’s standard dummy text https://spawax.pl/bbmnhqy of type and scrambled it to make a type specimen book.
акустическое оборудование для актового зала [url=www.oborudovanie-aktovogo-zala13.ru]акустическое оборудование для актового зала[/url] .
Larry Joe Bird https://larry-bird.prostoprosport-br.com American basketball player who spent his entire professional career in the NBA ” Boston Celtics.” Olympic champion (1992), champion of the 1977 Universiade, 3-time NBA champion (1981, 1984, 1986), three times recognized as MVP of the season in the NBA (1984, 1985, 1986), 10 times included in the symbolic teams of the season (1980-88 – first team, 1990 – second team).
Roberto Firmino Barbosa de Oliveira https://roberto-firmino.prostoprosport-br.com Brazilian footballer, attacking midfielder, forward for the Saudi club “Al-Ahli”. Firmino is a graduate of the Brazilian club KRB, from where he moved to Figueirense in 2007. In June 2015 he moved to Liverpool for 41 million euros.
The world’s most liveable cities for 2024
русское порно жесток
It’s considered among the most beautiful cities in the world to visit, and it seems that Vienna may also be an unbeatable place to live.
The Austrian city has been crowned the most liveable city in the world yet again in the annual list from the Economist Intelligence Unit (EIU), which was released today.
The EIU, a sister organization to The Economist, ranked 173 cities across the globe on a number of significant factors, including health care, culture and environment, stability, infrastructure and education.
Vienna topped the list for the third consecutive year, receiving “perfect” scores in four out of five of the categories — the city was marked lower for culture and environment due to an apparent lack of significant sporting events.
Just behind the Austrian capital, Denmark’s Copenhagen retained its second place position, while Switzerland’s Zurich moved up from sixth place to third on the list.
Australia’s Melbourne fell from third to fourth place, while Canadian city Calgary tied for fifth place with Swiss city Geneva.
Canada’s Vancouver and Australia’s Sydney were in joint seventh place, and Japan’s Osaka and New Zealand’s Auckland rounded out the top 10 in joint ninth place.
Lorem Ipsum has been the industry’s standard dummy text https://samowystarczalnyzakatek.pl/ilmwkrt of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://searchxlinks.de/idzqn of type and scrambled it to make a type specimen book.
The world’s most liveable cities for 2024
смотреть порно жесток
It’s considered among the most beautiful cities in the world to visit, and it seems that Vienna may also be an unbeatable place to live.
The Austrian city has been crowned the most liveable city in the world yet again in the annual list from the Economist Intelligence Unit (EIU), which was released today.
The EIU, a sister organization to The Economist, ranked 173 cities across the globe on a number of significant factors, including health care, culture and environment, stability, infrastructure and education.
Vienna topped the list for the third consecutive year, receiving “perfect” scores in four out of five of the categories — the city was marked lower for culture and environment due to an apparent lack of significant sporting events.
Just behind the Austrian capital, Denmark’s Copenhagen retained its second place position, while Switzerland’s Zurich moved up from sixth place to third on the list.
Australia’s Melbourne fell from third to fourth place, while Canadian city Calgary tied for fifth place with Swiss city Geneva.
Canada’s Vancouver and Australia’s Sydney were in joint seventh place, and Japan’s Osaka and New Zealand’s Auckland rounded out the top 10 in joint ninth place.
Lorem Ipsum has been the industry’s standard dummy text https://spawax.pl/qsjlmmq of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://11spielstaetten.de/ovgifux of type and scrambled it to make a type specimen book.
Khvicha Kvaratskhelia https://khvicha-kvaratskhelia.prostoprosport-br.com Georgian footballer, winger for Napoli and captain of the Georgian national team. A graduate of Dynamo Tbilisi. He made his debut for the adult team on September 29, 2017 in the Georgian championship match against Kolkheti-1913. In total, in the 2017 season he played 4 matches and scored 1 goal in the championship.
Damian Emiliano Martinez https://emiliano-martinez.prostoprosport-br.com Argentine footballer, goalkeeper of the Aston Villa club and national team Argentina. Champion and best goalkeeper of the 2022 World Cup.
Lorem Ipsum has been the industry’s standard dummy text https://evafinans.dk/brzfne of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://spinaldecompression.co.za/pcfwypa of type and scrambled it to make a type specimen book.
Кайт сафари обучение кайтсерфингу в Хургаде Египет
Jack Peter Grealish https://jackgrealish.prostoprosport-br.com English footballer, midfielder of the Manchester City club and the England national team. A graduate of the English club Aston Villa from Birmingham. In the 2012/13 season he won the NextGen Series international tournament, playing for the Aston Villa under-19 team
Lorem Ipsum has been the industry’s standard dummy text https://crowd1sinergia.es/gfodoq of type and scrambled it to make a type specimen book.
Kyle Andrew Walker https://kylewalker.prostoprosport-br.com English footballer, captain of the Manchester City club and the England national team. In the 2013/14 season, he was on loan at the Notts County club, playing in League One (3rd division of England). Played 37 games and scored 5 goals in the championship.
Lorem Ipsum has been the industry’s standard dummy text https://cristinazafra.es/yeixgu of type and scrambled it to make a type specimen book.
L’inscription a 1xBet est-elle disponible sans passeport?
Vous pouvez vous inscrire a 1x code bonus de pari sans donnees de passeport, mais a l’avenir, dans votre compte personnel, vous devrez remplir un questionnaire indiquant votre nom, votre nom et votre date de naissance. A l’avenir, avant la premiere Conclusion, il faudra egalement passer par la verification.
Lorem Ipsum has been the industry’s standard dummy text https://fleurbase.dk/acddo of type and scrambled it to make a type specimen book.
Теперь нет необходимости везти крупную бытовую технику в сервисный центр. Наш мастер проводит диагностику у вас дома, находит сломанную деталь и заменяет ее https://www.scamquery.com/review/bosch-remont.ru/
Теперь нет необходимости везти крупную бытовую технику в сервисный центр. Наш мастер проводит диагностику у вас дома, находит сломанную деталь и заменяет ее https://countchecker.com/?url=https://bosch-remont.ru
Son Heung Min https://sonheung-min.prostoprosport-br.com South Korean footballer, striker and captain of the English Premier League club Tottenham Hotspur and the Republic of Korea national team. In 2022 he won the Premier League Golden Boot. Became the first Asian footballer in history to score 100 goals in the Premier League
Laure Boulleau https://laure-boulleau.prostoprosport-fr.com French football player, defender. She started playing football in the Riom team, in 2000 she moved to Isere, and in 2002 to Issigneux. All these teams represented the Auvergne region. In 2003, Bullo joined the Clairefontaine academy and played for the academy team for the first time.
Enregistrez-vous en utilisant le 1xbet meilleur code promo afin de profiter d’une offre exclusive de bonus de 100% jusqu’a 130$ sur les paris sportifs gratuits. Pour beneficier de cette offre de pari gratuit bonifiee, vous devrez placer 5 paris sur des accumulateurs dans les 30 jours. Il existe diverses strategies pour les paris combines, mais si vous souhaitez gagner et obtenir des paris gratuits, nous vous recommandons de privilegier des selections de cotes plus courtes et de vous concentrer sur des paris combines surs pour commencer.
Lorem Ipsum has been the industry’s standard dummy text https://wbgsklep.pl/xtubg of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://palme-net.de/gsybcye of type and scrambled it to make a type specimen book.
Quelle est la mise minimale et la limite minimale de 1xBet?
Conformement aux regles du bookmaker, le depot minimum dans le bureau est de 1$.1xbetpromocode La mise minimale est de 0,2 $ou l’equivalent de ce montant dans une autre monnaie de jeu.
Jude Victor William Bellingham https://jude-bellingham.prostoprosport-fr.com English footballer, midfielder of the Spanish club Real Madrid and the England national team. In April 2024, he won the Breakthrough of the Year award from the Laureus World Sports Awards. He became the first football player to receive it.
Lorem Ipsum has been the industry’s standard dummy text https://cloudtechnical.in/ilmmkm of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://onkopaednki.de/zgzcjx of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://idigitalstudio.in/xpytydy of type and scrambled it to make a type specimen book.
Погрузитесь в мир постапокалипсиса – фильм Фуриоса: Хроники Безумного Макса доступна в интернете в превосходном качестве.
Lorem Ipsum has been the industry’s standard dummy text https://pizzartist.it/ycbissb of type and scrambled it to make a type specimen book.
In January 2010, Harry Kane https://harry-kane.prostoprosport-fr.com received an invitation to the England U-team for the first time 17 for the youth tournament in Portugal. At the same time, the striker, due to severe illness, did not go to the triumphant 2010 European Championship for boys under 17 for the British.
Antoine Griezmann https://antoine-griezmann.prostoprosport-fr.com French footballer, striker and midfielder for Atletico Madrid. Player and vice-captain of the French national team, as part of the national team – world champion 2018. Silver medalist at the 2016 European Championship and 2022 World Championship.
Lorem Ipsum has been the industry’s standard dummy text https://mvdesk.in/bcaxilc of type and scrambled it to make a type specimen book.
сколько будет стоить ремонт айфона [url=https://iphonepochinka.by/]iphonepochinka.by[/url] .
Lorem Ipsum has been the industry’s standard dummy text https://guacamayaproducciones.es/opiyuw of type and scrambled it to make a type specimen book.
Karim Mostafa Benzema https://karim-benzema.prostoprosport-fr.com French footballer, striker for the Saudi club Al-Ittihad . He played for the French national team, for which he played 97 matches and scored 37 goals.
Achraf Hakimi Mou https://achraf-hakimi.prostoprosport-fr.com Moroccan footballer, defender of the French club Paris Saint-Germain “and the Moroccan national team. He played for Real Madrid, Borussia Dortmund and Inter Milan.
Что может быть лучше, чем красивая девушка, массирующая Вас после тяжелого делового дня https://iwebchk.com/reports/view/msk1.devkiru.com
Что может быть лучше, чем красивая девушка, массирующая Вас после тяжелого делового дня https://loaddy.com/result/657281655/
Lorem Ipsum has been the industry’s standard dummy text https://sps2015.pl/aglhjl of type and scrambled it to make a type specimen book.
Sweet Bonanza https://sweet-bonanza.prostoprosport-fr.com is an exciting slot from Pragmatic Play that has quickly gained popularity among players thanks to its unique gameplay, colorful graphics and the opportunity to win big prizes. In this article, we’ll take a closer look at all aspects of this game, from mechanics and bonus features to strategies for successful play and answers to frequently asked questions.
Bernardo Silva https://bernardo-silva.prostoprosport-fr.com Portuguese footballer, midfielder. Born on August 10, 1994 in Lisbon. Silva is considered one of the best attacking midfielders in the world. The football player is famous for his endurance and performance. The athlete’s diminutive size is more than compensated for by his creativity, dexterity and foresight.
Philip Walter Foden https://phil-foden.prostoprosport-fr.com better known as Phil Foden English footballer, midfielder of the Premier club -League Manchester City and the England national team. On December 19, 2023, he made his debut at the Club World Championship in a match against the Japanese club Urawa Red Diamonds, starting in the starting lineup and being replaced by Julian Alvarez in the 65th minute.
Lorem Ipsum has been the industry’s standard dummy text https://coverly.co.za/wdirhn of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://mvdesk.in/dkkkydk of type and scrambled it to make a type specimen book.
L’inscription a 1xBet est-elle disponible sans passeport?
Vous pouvez vous inscrire a code promo 1xbet pour un pari gratuit sans donnees de passeport, mais a l’avenir, dans votre compte personnel, vous devrez remplir un questionnaire indiquant votre nom, votre nom et votre date de naissance. A l’avenir, avant la premiere Conclusion, il faudra egalement passer par la verification.
Kylian Mbappe Lotten https://kylian-mbappe.prostoprosport-fr.com Footballeur francais, attaquant du Paris Saint-Germain et capitaine de l’equipe de France. Le 1er juillet 2024, il deviendra joueur du club espagnol du Real Madrid.
Lorem Ipsum has been the industry’s standard dummy text https://sofiaporelmundo.es/tsuxbtg of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://borealstudios.es/djswbm of type and scrambled it to make a type specimen book.
Jogo do Tigre https://jogo-do-tigre.prostoprosport-br.com is a simple and fun game that tests your reflexes and coordination. In this game you need to put your finger on the screen, pull out the stick and go through each peg. However, you must ensure that the stick is the right length, neither too long nor too short.
Mohamed Salah Hamed Mehrez Ghali https://mohamed-salah.prostoprosport-fr.com Footballeur egyptien, attaquant du club anglais de Liverpool et l’equipe nationale egyptienne. Considere comme l’un des meilleurs footballeurs du monde
Lorem Ipsum has been the industry’s standard dummy text https://teslamania.es/kochh of type and scrambled it to make a type specimen book.
Declan Rice https://declan-rice.prostoprosport-fr.com Footballeur anglais, milieu defensif du club d’Arsenal et de l’equipe nationale equipe d’Angleterre. Originaire de Kingston upon Thames, Declan Rice s’est entraine a l’academie de football de Chelsea des l’age de sept ans. En 2014, il devient joueur de l’academie de football de West Ham United.
Jamal Musiala https://jamal-musiala.prostoprosport-fr.com footballeur allemand, milieu offensif du club allemand du Bayern et du equipe nationale d’Allemagne. Il a joue pour les equipes anglaises des moins de 15 ans, des moins de 16 ans et des moins de 17 ans. En octobre 2018, il a dispute deux matchs avec l’equipe nationale d’Allemagne U16. En novembre 2020, il a fait ses debuts avec l’equipe d’Angleterre U21.
Thibaut Nicolas Marc Courtois https://thhibaut-courtois.prostoprosport-fr.com Footballeur belge, gardien de but du club espagnol du Real Madrid . Lors de la saison 2010/11, il a ete reconnu comme le meilleur gardien de la Pro League belge, ainsi que comme joueur de l’annee pour Genk. Triple vainqueur du Trophee Ricardo Zamora
tretinoin 01 cream
Lorem Ipsum has been the industry’s standard dummy text https://spinaldecompression.co.za/lnrrfi of type and scrambled it to make a type specimen book.
Best Antivirus Software of 2024: Comprehensive Guide and Recommendations
Lorem Ipsum has been the industry’s standard dummy text https://investeringsgronden.nl/stbcc of type and scrambled it to make a type specimen book.
1x pari code promo gratuit. Utilisez – le lors de votre inscription pour obtenir un bonus de 100% jusqu’a 130$. Pour obtenir des bonus du bookmaker 1xbet, vous devez remplir certaines conditions, mais les codes promotionnels vous permettent de les obtenir beaucoup plus facilement. La taille des bonus disponibles pour les joueurs via les codes promotionnels 1xBet peut etre petite, mais meme un petit bonus peut augmenter considerablement le potentiel de jeu du client.
Declan Rice https://declan-rice.prostoprosport-fr.com Footballeur anglais, milieu defensif du club d’Arsenal et de l’equipe nationale equipe d’Angleterre. Originaire de Kingston upon Thames, Declan Rice s’est entraine a l’academie de football de Chelsea des l’age de sept ans. En 2014, il devient joueur de l’academie de football de West Ham United.
Olivier Jonathan Giroud https://olivier-giroud.prostoprosport-fr.com French footballer, striker for Milan and the French national team. Knight of the Legion of Honor. Participant in four European Championships (2012, 2016, 2020 and 2024) and three World Championships (2014, 2018 and 2022).
Lorem Ipsum has been the industry’s standard dummy text https://mprcode.pl/kdxhn of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://fotoquo.es/ywcew of type and scrambled it to make a type specimen book.
cost of flomax medication
Lorem Ipsum has been the industry’s standard dummy text https://spahouse.dk/keqgk of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://akuand.pl/unafj of type and scrambled it to make a type specimen book.
Qu’est-ce qui donne au joueur la verification dans 1xbet?
La verification est une procedure obligatoire pour les clients du bookmaker code promo 1xbet casino. La procedure prevoit la verification des donnees personnelles du client pour la conformite avec les donnees reelles qui sont presentees sur la carte d’identite.
Xavi or Xavi Quentin Sy Simons https://xavi-simons.prostoprosport-fr.com Dutch footballer, midfielder of the Paris Saint-Germain club -Germain” and the Dutch national team, playing on loan for the German club RB Leipzig.
Lorem Ipsum has been the industry’s standard dummy text https://kreatoretui.pl/pssjlqx of type and scrambled it to make a type specimen book.
Ronaldo de Asis Moreira https://ronaldinhogaucho.prostoprosport-br.com Brazilian footballer, played as an attacking midfielder and striker. World Champion (2002). Winner of the Golden Ball (2005). The best football player in the world according to FIFA in 2004 and 2005.
Erling Breut Haaland https://erling-haaland.prostoprosport-br.com Futebolista noruegues, atacante do clube ingles Manchester City e Selecao da Noruega. Detentor do recorde da Premier League inglesa em gols por temporada.
Philippe Coutinho Correia https://philippecoutinho.prostoprosport-br.com Brazilian footballer, midfielder of the English club Aston Villa, playing on loan for the Qatari club Al-Duhail. He is known for his vision, passing, dribbling and long-range ability.
Lorem Ipsum has been the industry’s standard dummy text https://placassolaresmalaga2000.es/zlrvxx of type and scrambled it to make a type specimen book.
Offre speciale 1xBet Obtenez un bonus sportif supplementaire de 200% jusqu’a 130 €/$ avec le dernier code promo pour 1xbet, en plus du bonus de bienvenue standard de 1950$ et de 150 tours gratuits au casino. Profitez de cette opportunite pour jouer et gagner de l’argent grace aux paris sportifs. Chez nous, tout le monde peut devenir gagnant !
Qu’est-ce qui donne au joueur la verification dans 1xbet?
La verification est une procedure obligatoire pour les clients du bookmaker 1xbet meilleur code promo. La procedure prevoit la verification des donnees personnelles du client pour la conformite avec les donnees reelles qui sont presentees sur la carte d’identite.
Carlos Henrique Casimiro https://carloscasemiro.prostoprosport-br.com Futebolista brasileiro, volante do clube ingles Manchester United e capitao do Selecao Brasileira. Pentacampeao da Liga dos Campeoes da UEFA, campeao mundial e sul-americano pela selecao juvenil brasileira.
Kylian Mbappe Lotten https://kylianmbappe.prostoprosport-br.com Futebolista frances, atacante do Paris Saint-Germain e capitao da selecao francesa equipe . Em 1? de julho de 2024, ele se tornara jogador do clube espanhol Real Madrid.
Kaka https://kaka.prostoprosport-br.com Futebolista brasileiro, meio-campista. O apelido “Kaka” e um diminutivo de Ricardo. Formado em Sao Paulo. De 2002 a 2016, integrou a Selecao Brasileira, pela qual disputou 92 partidas e marcou 29 gols. Campeao mundial 2002.
Karim Mostafa Benzema https://karim-benzema.prostoprosport-br.com Futebolista frances, atacante do clube saudita Al-Ittihad . Jogou pela selecao francesa, pela qual disputou 97 partidas e marcou 37 gols.
Lionel Messi https://lionelmessi.prostoprosport-br.com e um jogador de futebol argentino, atacante e capitao do clube da MLS Inter Miami. , capitao da selecao argentina. Campeao mundial, campeao sul-americano, vencedor da Finalissima, campeao olimpico. Considerado um dos melhores jogadores de futebol de todos os tempos.
Mohamed Salah https://mohamedsalah.prostoprosport-br.com e um futebolista egipcio que joga como atacante do clube ingles Liverpool e do Selecao egipcia. Considerado um dos melhores jogadores de futebol do mundo. Tricampeao da Chuteira de Ouro da Premier League inglesa: em 2018 (sozinho), 2019 (junto com Sadio Mane e Pierre-Emerick Aubameyang) e 2022 (junto com Son Heung-min).
Lorem Ipsum has been the industry’s standard dummy text https://login-betway-india.com/jlrgn of type and scrambled it to make a type specimen book.
Harry Kane https://harry-kane.prostoprosport-br.com recebeu um convite para a selecao sub-alterna da Inglaterra pela primeira vez tempo 17 para o torneio juvenil em Portugal. Ao mesmo tempo, o atacante, devido a doenca grave, nao compareceu ao triunfante Campeonato Europeu Sub-17 masculino de 2010 pelos britanicos.
Are you looking for a solution to erectile dysfunction? Look no further! buying viagra online in canada is here to help.
Jude Bellingham https://jude-bellingham.prostoprosport-br.com Futebolista ingles, meio-campista do clube espanhol Real Madrid e do Selecao da Inglaterra. Em abril de 2024, ele ganhou o premio Breakthrough of the Year do Laureus World Sports Awards. Ele se tornou o primeiro jogador de futebol a recebe-lo.
Zlatan Ibrahimovic https://zlatan-ibrahimovic.prostoprosport-br.com Bosnian pronunciation: ibraxi?mo?it?]; genus. 3 October 1981, Malmo, Sweden) is a Swedish footballer who played as a striker. Former captain of the Swedish national team.
Are you looking for a solution to erectile dysfunction? Look no further! can u buy viagra at walgreens is here to help.
Luis Alberto Suarez Diaz https://luis-suarez.prostoprosport-br.com Uruguayan footballer, striker for Inter Miami and Uruguay national team. The best scorer in the history of the Uruguay national team. Considered one of the world’s top strikers of the 2010s
Thibaut Nicolas Marc Courtois https://thhibaut-courtois.prostoprosport-fr.com Footballeur belge, gardien de but du club espagnol du Real Madrid . Lors de la saison 2010/11, il a ete reconnu comme le meilleur gardien de la Pro League belge, ainsi que comme joueur de l’annee pour Genk. Triple vainqueur du Trophee Ricardo Zamora
Lorem Ipsum has been the industry’s standard dummy text https://betway-casino-app.com/nxgqurn of type and scrambled it to make a type specimen book.
Robert Lewandowski https://robert-lewandowski.prostoprosport-br.com e um futebolista polones, atacante do clube espanhol Barcelona e capitao da selecao polonesa. Considerado um dos melhores atacantes do mundo. Cavaleiro da Cruz do Comandante da Ordem do Renascimento da Polonia.
Gareth Frank Bale https://garethbale.prostoprosport-br.com Jogador de futebol gales que atuou como ala. Ele jogou na selecao galesa. Ele se destacou pela alta velocidade e um golpe bem colocado. Artilheiro (41 gols) e recordista de partidas disputadas (111) na historia da selecao.
Lorem Ipsum has been the industry’s standard dummy text https://platformzelfredzaam.nl/qgmjk of type and scrambled it to make a type specimen book.
мраморная крошка серая уфалейские памятники
Lorem Ipsum has been the industry’s standard dummy text https://amaterasuspa.pl/zckfg of type and scrambled it to make a type specimen book.
Kevin De Bruyne https://kevin-de-bruyne.prostoprosport-br.com Futebolista belga, meio-campista do Manchester club City” e a selecao belga. Formado pelos clubes de futebol “Ghent” e “Genk”. Em 2008 iniciou sua carreira adulta, fazendo sua estreia no Genk.
Ederson Santana de Moraes https://edersonmoraes.prostoprosport-br.com Futebolista brasileiro, goleiro do clube Manchester City e da Selecao Brasileira . Participante do Campeonato Mundial 2018. Bicampeao de Portugal pelo Benfica e pentacampeao de Inglaterra pelo Manchester City.
продвижение сайтов в москве в топ [url=http://prodvizhenie-sajtov-v-moskve115.ru/]http://prodvizhenie-sajtov-v-moskve115.ru/[/url] .
Lorem Ipsum has been the industry’s standard dummy text https://msizindlela.co.za/vdqiaf of type and scrambled it to make a type specimen book.
Antoine Griezmann https://antoine-griezmann.prostoprosport-br.com Futebolista frances, atacante e meio-campista do Atletico de Madrid. Jogador e vice-capitao da selecao francesa, integrante da selecao – campea mundial 2018. Medalhista de prata no Europeu de 2016 e no Mundial de 2022.
Virgil van Dijk https://virgilvandijk.prostoprosport-br.com Futebolista holandes, zagueiro central, capitao do clube ingles Liverpool e capitao do a selecao holandesa.
Lorem Ipsum has been the industry’s standard dummy text https://oxybasket.in/kjbdvb of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://maleekcleaning.co.za/yhrcgy of type and scrambled it to make a type specimen book.
Victor James Osimhen https://victor-osimhen.prostoprosport-br.com e um futebolista nigeriano que atua como atacante. O clube italiano Napoli e a selecao nigeriana.
Lorem Ipsum has been the industry’s standard dummy text https://despachusocial.es/tjygw of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://cmedia-design.dk/qhekj of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://sigma-radomsko.pl/myoazt of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://sonnosgroup.es/qeogl of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://viaggiarefree.it/gkhhbic of type and scrambled it to make a type specimen book.
Столешницы, барные стойки, подоконники и другие изделия из искусственного камня от производителя мебели из камня “Акрилиум” https://camremont.ru/gde-zakazat-stoleshniczu-iz-kamnya/
Lorem Ipsum has been the industry’s standard dummy text https://gymnasium-ramsloh.de/fieoba of type and scrambled it to make a type specimen book.
Romelu Menama Lukaku Bolingoli https://romelulukaku.prostoprosport-br.com Futebolista belga, atacante do clube ingles Chelsea e da selecao belga . Por emprestimo, ele joga pelo clube italiano Roma.
Roberto Carlos da Silva Rocha https://roberto-carlos.prostoprosport-br.com Brazilian footballer, left back. He was also capable of playing as both a central defender and a defensive midfielder. World champion 2002, silver medalist at the 1998 World Championships.
Профессиональные seo https://seo-optimizaciya-kazan.ru услуги для максимизации онлайн-видимости вашего бизнеса. Наши эксперты проведут глубокий анализ сайта, оптимизируют контент и структуру, улучшат технические аспекты и разработают индивидуальные стратегии продвижения.
Thomas Mueller https://thomasmueller.prostoprosport-br.com is a German football player who plays for the German Bayern Munich. Can play in different positions – striker, attacking midfielder. The most titled German footballer in history
Lorem Ipsum has been the industry’s standard dummy text https://lacalabrianeifrancobolli.it/eeesvzz of type and scrambled it to make a type specimen book.
Offre speciale c’est quoi le code promo dans 1xbet vous offre une remise de 100% sur le montant total de votre premier depot jusqu’a 100$, bien entendu, dans votre devise locale. Profitez-en facilement en saisissant le code promotionnel lors de votre inscription et recevez un bonus sur 1xbet.com.
Neymar da Silva Santos Junior https://neymar.prostoprosport-br.com e um futebolista brasileiro que atua como atacante, ponta e atacante. meio-campista do clube saudita Al-Hilal e da selecao brasileira. Considerado um dos melhores jogadores do mundo. O maior artilheiro da historia da Selecao Brasileira.
Edson Arantes do Nascimento https://pele.prostoprosport-br.com Brazilian footballer, forward (attacking midfielder. Played for Santos clubs) and New York Cosmos. Played 92 matches and scored 77 goals for the Brazilian national team.
оснащение конференц зала оснащение конференц зала .
Lorem Ipsum has been the industry’s standard dummy text https://hussainak.dk/rloloyn of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://maleekcleaning.co.za/tifuu of type and scrambled it to make a type specimen book.
Jude Victor William Bellingham https://jude-bellingham.prostoprosport-cz.org anglicky fotbalista, zaloznik spanelskeho klubu Real Madrid a anglicky narodni tym. V dubnu 2024 ziskal cenu za prulom roku z Laureus World Sports Awards. Stal se prvnim fotbalistou, ktery ji obdrzel.
Erling Breut Haaland https://erling-haaland.prostoprosport-cz.org je norsky fotbalista, ktery hraje jako utocnik za Anglicky klub Manchester City a norska reprezentace. Rekordman anglicke Premier League v poctu golu za sezonu.
Qu’est-ce qui donne au joueur la verification dans 1xbet?
La verification est une procedure obligatoire pour les clients du bookmaker bonus de depot 1xbet. La procedure prevoit la verification des donnees personnelles du client pour la conformite avec les donnees reelles qui sont presentees sur la carte d’identite.
Lorem Ipsum has been the industry’s standard dummy text https://excellenceevents.in/jdxxw of type and scrambled it to make a type specimen book.
Kylian Mbappe Lotten https://kylian-mbappe.prostoprosport-cz.org Francouzsky fotbalista, utocnik Paris Saint-Germain a kapitan tymu francouzskeho tymu. 1. cervence 2024 se stane hracem spanelskeho klubu Real Madrid.
Lorem Ipsum has been the industry’s standard dummy text https://amaloquehaces.es/tqazwxy of type and scrambled it to make a type specimen book.
zithromax over the counter canada
Lorem Ipsum has been the industry’s standard dummy text https://alzagaconsulting.es/odcofqd of type and scrambled it to make a type specimen book.
Mohamed Salah https://mohamed-salah.prostoprosport-cz.org je egyptsky fotbalista, ktery hraje jako utocnik za anglictinu. klub Liverpool a egyptsky narodni tym. Povazovan za jednoho z nejlepsich fotbalistu na svete.
Vinicius Jose Paixan de Oliveira Junior vinicius-junior.prostoprosport-cz.org bezne znamy jako Vinicius Junior je brazilsky a spanelsky fotbalista , utocnik klubu Real Madrid a brazilsky reprezentant.
Kevin De Bruyne https://kevin-de-bruyne.prostoprosport-cz.org Belgicky fotbalista, zaloznik Manchesteru klub City” a belgicky narodni tym. Absolvent fotbalovych klubu „Ghent” a „Genk”. V roce 2008 zahajil svou karieru dospelych, debutoval v Genku.
Lorem Ipsum has been the industry’s standard dummy text https://hmbmalesa.pl/lilan of type and scrambled it to make a type specimen book.
yarborough.lem4@gmail.com
Lorem Ipsum has been the industry’s standard dummy text https://goglernet.dk/puzqhb of type and scrambled it to make a type specimen book.
Quelles methodes puis-je utiliser pour l’entree et la sortie?
Le bookmaker 1xbet met a la disposition des joueurs tous les moyens de paiement disponibles aujourd’hui.bonus de bienvenue 1xbet Vous pouvez faire un depot avec des cartes bancaires Visa et Mastercard, avec des portefeuilles electroniques, via des systemes de paiement, via des services bancaires par Internet, en utilisant les services des operateurs mobiles, sur des portefeuilles pour crypto – monnaie. Pour le retrait, il est recommande d’utiliser des cartes bancaires, des portefeuilles electroniques et des systemes de paiement. La liste des methodes de paiement se trouve dans la section «Paiements».
Lorem Ipsum has been the industry’s standard dummy text https://npf-paker.es/neeosrr of type and scrambled it to make a type specimen book.
whoah this blog is fantastic i love reading your posts. Keep up the great work! You realize, lots of individuals are searching around for this information, you could aid them greatly.
официальный сайт драгон мани казино
Bernardo Silva https://bernardo-silva.prostoprosport-cz.org Portugalsky fotbalista, zaloznik. Narozen 10. srpna 1994 v Lisabonu. Silva je povazovan za jednoho z nejlepsich utocnych zalozniku na svete. Fotbalista je povestny svou vytrvalosti a vykonem.
Lionel Messi https://lionel-messi.prostoprosport-cz.org je argentinsky fotbalista, utocnik a kapitan klubu MLS Inter Miami. , kapitan argentinske reprezentace. Mistr sveta, vitez Jizni Ameriky, vitez finale, olympijsky vitez. Povazovan za jednoho z nejlepsich fotbalistu vsech dob.
Antoine Griezmann https://antoine-griezmann.prostoprosport-cz.org Francouzsky fotbalista, utocnik a zaloznik za Atletico de Madrid. Hrac a vicekapitan francouzskeho narodniho tymu, clen tymu – mistr sveta 2018 Stribrny medailista z mistrovstvi Evropy 2016 a mistrovstvi sveta 2022.
Robert Lewandowski https://robert-lewandowski.prostoprosport-cz.org je polsky fotbalista, utocnik spanelskeho klubu Barcelona a kapitan polskeho narodniho tymu. Povazovan za jednoho z nejlepsich utocniku na svete. Rytir krize velitele polskeho renesancniho radu.
Offre speciale code bonus 1xbet vous offre une remise de 100% sur le montant total de votre premier depot jusqu’a 100$, bien entendu, dans votre devise locale. Profitez-en facilement en saisissant le code promotionnel lors de votre inscription et recevez un bonus sur 1xbet.com.
Lorem Ipsum has been the industry’s standard dummy text https://irenesanchezfisio.es/dwjax of type and scrambled it to make a type specimen book.
Ou dois-je inserer un code promo lors de l’inscription a 1xBet?
Des que le c’est quoi le code promo dans 1xbet est copie, le joueur doit aller a l’enregistrement dans le bureau 1xbet. Dans le processus d’inscription, le code copie doit etre colle dans un formulaire special.
Lorem Ipsum has been the industry’s standard dummy text https://you2i.dk/douvw of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://despachusocial.es/fmbxcjk of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://buytron.co.za/vumtuwz of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://starenterprises.nl/iktuyj of type and scrambled it to make a type specimen book.
Son Heung Min https://son-heung-min.prostoprosport-cz.org Jihokorejsky fotbalista, utocnik a kapitan anglickeho klubu Premier League Tottenham Hotspur a narodniho tymu Korejske republiky. V roce 2022 vyhral Zlatou kopacku Premier League.
Luka Modric https://luka-modric.prostoprosport-cz.org je chorvatsky fotbalista, stredni zaloznik a kapitan spanelskeho tymu. klub Real Madrid, kapitan chorvatskeho narodniho tymu. Uznavan jako jeden z nejlepsich zalozniku nasi doby. Rytir Radu prince Branimira. Rekordman chorvatske reprezentace v poctu odehranych zapasu.
Pablo Martin Paez Gavira https://gavi.prostoprosport-cz.org Spanelsky fotbalista, zaloznik barcelonskeho klubu a spanelske reprezentace. Povazovan za jednoho z nejtalentovanejsich hracu sve generace. Ucastnik mistrovstvi sveta 2022. Vitez Ligy narodu UEFA 2022/23
Cristiano Ronaldo https://cristiano-ronaldo.prostoprosport-cz.org je portugalsky fotbalista, utocnik, kapitan Saudske Arabie klubu An-Nasr a portugalskeho narodniho tymu. Mistr Evropy. Povazovan za jednoho z nejlepsich fotbalistu vsech dob. Nejlepsi strelec v historii fotbalu podle IFFIS a ctvrty podle RSSSF
Hey everyone,
I recently stumbled upon a coin called HGL on the TON network, and I found its address: EQASgMtBU2QP9JMRfR1jKeLcPMUUT2RGigp_cVcjQuCyaZDw
There are some whispers that this coin might see some significant developments soon, but it’s still pretty low-key. Here’s the link I found on GeckoTerminal: https://www.geckoterminal.com/ton/pools/EQBPaJg_cqZ25-ZRBPOBXWh9uCXGTcOxkvDLgRALL6n2L4y2
I got a bit curious and bought a small amount since the price is still quite low. Has anyone here heard anything about HGL or know more about what’s going on with this project? Would love to hear your thoughts!
Thanks!
Lorem Ipsum has been the industry’s standard dummy text https://cosavedereinungiorno.it/rllnc of type and scrambled it to make a type specimen book.
Pedro Gonzalez Lopez https://pedri.prostoprosport-cz.org lepe znamy jako Pedri, je spanelsky fotbalista, ktery hraje jako utocny zaloznik. za Barcelonu a spanelskou reprezentaci. Bronzovy medailista z mistrovstvi Evropy 2020 a zaroven nejlepsi mlady hrac tohoto turnaje.
Rodrigo Silva de Goiz https://rodrygo.prostoprosport-cz.org Brazilsky fotbalista, utocnik Realu Madrid a brazilskeho narodniho tymu. V breznu 2017 byl Rodrigo povolan do narodniho tymu Brazilie U17 na zapasy Montague Tournament.
Alison Ramses Becker https://alisson-becker.prostoprosport-cz.org Brazilsky fotbalista nemeckeho puvodu, brankar klubu Liverpool a brazilsky narodni tym. Je povazovan za jednoho z nejlepsich brankaru sve generace a je znamy svymi vynikajicimi zakroky, presnosti prihravek a schopnosti jeden na jednoho.
Karim Benzema https://karim-benzema.prostoprosport-cz.org je francouzsky fotbalista, ktery hraje jako utocnik za Saudskou Arabii. Arabsky klub Al-Ittihad. Hral za francouzsky narodni tym, za ktery odehral 97 zapasu a vstrelil 37 branek. V 17 letech se stal jednim z nejlepsich hracu rezervy, nastrilel tri desitky golu za sezonu.
Thibaut Nicolas Marc Courtois https://thibaut-courtois.prostoprosport-cz.org Belgicky fotbalista, brankar spanelskeho klubu Real Madrid . V sezone 2010/11 byl uznan jako nejlepsi brankar v belgicke Pro League a take hrac roku pro Genk. Trojnasobny vitez Ricardo Zamora Trophy
Virgil van Dijk https://virgil-van-dijk.prostoprosport-cz.org Nizozemsky fotbalista, stredni obrance, kapitan anglickeho klubu Liverpool a kapitan nizozemskeho narodniho tymu.
Bruno Guimaraes Rodriguez Moura https://bruno-guimaraes.prostoprosport-cz.org Brazilsky fotbalista, defenzivni zaloznik Newcastlu United a Brazilsky narodni tym. Vitez olympijskych her 2020 v Tokiu.
Toni Kroos https://toni-kroos.prostoprosport-cz.org je nemecky fotbalista, ktery hraje jako stredni zaloznik za Real Madrid a nemecky narodni tym. Mistr sveta 2014. Prvni nemecky hrac v historii, ktery sestkrat vyhral Ligu mistru UEFA.
Le code promo 1xbet cameroun, utilisez-le lors de l’inscription et obtenez un bonus de 200% jusqu’a 130$. Seuls les nouveaux joueurs peuvent obtenir le bonus. Ce contrat bonus est valable jusqu’au 31 decembre 2024. Apres le depot, le joueur recoit sur le compte bonus le montant des bonus pour les Paris de 100% du montant du depot, mais pas plus de $100. Pour recuperer le bonus recu, le joueur doit placer au moins cinq Paris dans les cinq jours suivants. Pour les Paris, vous devez faire un Express avec 3 evenements ou plus avec des cotes d’au moins 1,40.
Lorem Ipsum has been the industry’s standard dummy text https://pedrocollar.es/qadbmow of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://allafricanpokerguide.co.za/amxtja of type and scrambled it to make a type specimen book.
Toni Kroos https://toni-kroos.prostoprosport-cz.org je nemecky fotbalista, ktery hraje jako stredni zaloznik za Real Madrid a nemecky narodni tym. Mistr sveta 2014. Prvni nemecky hrac v historii, ktery sestkrat vyhral Ligu mistru UEFA.
Darwin Gabriel Nunez Ribeiro https://darwin-nunez.prostoprosport-cz.org Uruguaysky fotbalista, utocnik anglickeho klubu Liverpool a Uruguaysky narodni tym. Bronzovy medailista mistrovstvi Jizni Ameriky mezi mladeznickymi tymy.
Romelu Menama Lukaku Bolingoli https://romelu-lukaku.prostoprosport-cz.org Belgicky fotbalista, utocnik anglickeho klubu Chelsea a Belgican vyber. Na hostovani hraje za italsky klub Roma.
Lorem Ipsum has been the industry’s standard dummy text https://taskoo.in/rqkaa of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://convido.es/hyiglp of type and scrambled it to make a type specimen book.
стоимость видеостены стоимость видеостены .
Lorem Ipsum has been the industry’s standard dummy text https://lupo1987.dk/iufbu of type and scrambled it to make a type specimen book.
зрелые проститутки москвы проститутки самые самые
buy 100k tiktok followers https://tiktok-followers-buy.com
buy 1k tiktok followers tiktok buy followers
отчаянные домохозяйки 1 сезон 1 серия отчаянные домохозяйки бесплатно
Lorem Ipsum has been the industry’s standard dummy text https://sofiaporelmundo.es/qqzzb of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://alpalaphotos.es/qbeek of type and scrambled it to make a type specimen book.
https://businka74.ru/ вход Rio Bet Casino
онлайн казино Dragon Money https://trucktir.ru
Combien de temps faut-il pour retirer des fonds sur une carte Visa ou MasterCard?
Le retrait des fonds sur les cartes bancaires des systemes de paiement Visa et Mastercard depend du montant de la transaction, du jour de la semaine et de l’heure de la journee.1x pari code promo gratuit En regle generale, les fonds arrivent sur le compte indique dans un delai de 24 heures.
Большой выбор игровых автоматов, рабочее зеркало сайта https://fartunaplay.ru/slot-machines играть на реальные деньги онлайн
Качественная и недорогая набор мебели для кухни лучшие цены, доставка и сборка.
Lorem Ipsum has been the industry’s standard dummy text https://bet365-online-betting.in/ukxfwyu of type and scrambled it to make a type specimen book.
https://kliwenta.pl/
Le c’est quoi le code promo dans 1xbet, utilisez-le lors de l’inscription et obtenez un bonus de 200% jusqu’a 130$. Seuls les nouveaux joueurs peuvent obtenir le bonus. Ce contrat bonus est valable jusqu’au 31 decembre 2024. Apres le depot, le joueur recoit sur le compte bonus le montant des bonus pour les Paris de 100% du montant du depot, mais pas plus de $100. Pour recuperer le bonus recu, le joueur doit placer au moins cinq Paris dans les cinq jours suivants. Pour les Paris, vous devez faire un Express avec 3 evenements ou plus avec des cotes d’au moins 1,40.
Lorem Ipsum has been the industry’s standard dummy text https://analisidebiti.it/babbe of type and scrambled it to make a type specimen book.
Pin Up casino https://pin-up.salexy.kz official website, Pin Up slot machines play for money online, Pin Up mirror working for today.
Slot machines on the official website and mirrors of the Pin Up online casino https://pin-up.tr-kazakhstan.kz are available for free mode, and after registering at Pin Up Casino Ru you can play for money.
Pin up entry to the official website. Play online casino Pin Up https://pin-up.prostoprosport.ru for real money. Register on the Pin Up Casino website and claim bonuses!
Sports in Azerbaijan https://idman-xeberleri.com.az development and popular sports Azerbaijan is a country with rich sports traditions and outstanding achievements on the international stage.
Quelles methodes puis-je utiliser pour l’entree et la sortie?
Le bookmaker 1xbet met a la disposition des joueurs tous les moyens de paiement disponibles aujourd’hui.code promo pari gratuit 1xbet Vous pouvez faire un depot avec des cartes bancaires Visa et Mastercard, avec des portefeuilles electroniques, via des systemes de paiement, via des services bancaires par Internet, en utilisant les services des operateurs mobiles, sur des portefeuilles pour crypto – monnaie. Pour le retrait, il est recommande d’utiliser des cartes bancaires, des portefeuilles electroniques et des systemes de paiement. La liste des methodes de paiement se trouve dans la section «Paiements».
Lorem Ipsum has been the industry’s standard dummy text https://oxybasket.in/wcfpsll of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://pysznyobiad.pl/kpegivb of type and scrambled it to make a type specimen book.
World of Games https://onlayn-oyunlar.com.az provides the latest news about online games, game reviews, gameplay and ideas, game tactics and tips. The most popular and spectacular
The main sports news of Azerbaijan https://idman.com.az. Your premier source for the latest news, exclusive interviews, in-depth analysis and live coverage of everything happening in sports in Azerbaijan.
UFC in Azerbaijan https://ufc.com.az news, schedule of fights and tournaments 2024, rating of UFC fighters, interviews, photos and videos. Live broadcasts and broadcasts of tournaments, statistics.
NHL (National Hockey League) News https://nhl.com.az the latest and greatest NHL news for today. Sports news – latest NHL news, standings, match results, online broadcasts.
Купить Кокаин в Москве? Самый чистый Кокаин в Москве Купить
ССЫЛКА НА САЙТ- https://mephedrone.top
Москва Купить Мефедрон? Кристаллы МЕФ?
Где в Москве Купить Мефедрон? САЙТ – https://mephedrone.top/
Top sports news https://idman-azerbaycan.com.az photos and blogs from experts and famous athletes, as well as statistics and information about matches of leading championships.
Latest news and details about the NBA in Azerbaijan https://nba.com.az. Hot events, player transfers and the most interesting events. Explore the world of the NBA with us.
The latest top football news https://futbol.com.az today. Interviews with football players, online broadcasts and match results, analytics and football forecasts, photos and videos.
Discover the fascinating world of online games with GameHub Azerbaijan https://online-game.com.az. Get the latest news, reviews and tips for your favorite games. Join our gaming community today!
Каталог рейтингов хостингов https://pro-hosting.tech на любой вкус и под любые, даже самые сложные, задачи.
Сантехник — вызов сантехника на дом в Москве и Московской области в удобное для вас время.
Le code promo pour parier gratuit dans 1xbet, utilisez-le lors de l’inscription et obtenez un bonus de 200% jusqu’a 130$. Seuls les nouveaux joueurs peuvent obtenir le bonus. Ce contrat bonus est valable jusqu’au 31 decembre 2024. Apres le depot, le joueur recoit sur le compte bonus le montant des bonus pour les Paris de 100% du montant du depot, mais pas plus de $100. Pour recuperer le bonus recu, le joueur doit placer au moins cinq Paris dans les cinq jours suivants. Pour les Paris, vous devez faire un Express avec 3 evenements ou plus avec des cotes d’au moins 1,40.
Play PUBG Mobile https://pubg-mobile.com.az an exciting world of high-quality mobile battle royale. Unique maps, strategies and intense combat await you in this exciting mobile version of the popular game.
The Dota 2 website https://dota2.com.az Azerbaijan provides the most detailed information about the latest game updates, tournaments and upcoming events. We have all the winning tactics, secrets and important guides.
ООО «Транс Инвест» – единая логистика да мультимодальные перевозку грузов числом Стране россии c 2012 года
https://ticargo.ru/
Latest news about games for Android https://android-games.com.az, reviews and daily updates. Read now and get the latest information on the most exciting games
Check out the latest news, guides and in-depth reviews of the available options for playing Minecraft Az https://minecraft.com.az. Find the latest information about Minecraft Download, Pocket Edition and Bedrock Edition.
The most popular sports site https://sports.com.az of Azerbaijan, where the latest sports news, forecasts and analysis are collected.
Latest news and analytics of the Premier League https://premier-league.com.az. Detailed descriptions of matches, team statistics and the most interesting football events. EPL Azerbaijan is the best place for football fans.
Хотите сделать в квартире ремонт? Тогда советуем вам посетить сайт https://stroyka-gid.ru, где вы найдете всю необходимую информацию по строительству и ремонту.
Энергообъединение площадей от обществе БИОН. Проводим объединение земляных участков. У нас можно запретить рециклирование подлунный мир а также земляных узлов, что-что тоже энергообъединение отделений на СНТ.
https://bion-online.ru/
https://loveflover.ru — сайт посвященный комнатным растениям. Предлагает подробные статьи о выборе, выращивании и уходе за различными видами комнатных растений. Здесь можно найти полезные советы по созданию зелёного уголка в доме, руководства по декору и решению распространённых проблем, а также информацию о подходящих горшках и удобрениях. Платформа помогает создавать уютную атмосферу и гармонию в интерьере с помощью растений.
1xbet https://1xbet.best-casino-ar.com with withdrawal without commission. Register online in a few clicks. A large selection of slot machines in mobile applications and convenient transfers in just a few minutes.
Pin-up Casino https://pin-up.admsov.ru/ is an online casino licensed and regulated by the government of Curacao . Founded in 2016, it is home to some of the industry’s leading providers, including NetEnt, Microgaming, Play’n GO and others. This means that you will be spoiled for choice when it comes to choosing a game.
Pin Up official https://pin-up.adb-auto.ru website. Login to your personal account and register through the Pin Up mirror. Slot machines for real money at Pinup online casino.
KMSpico: What is it?
kmspico 10
Operating systems and Office suites are among the primary Microsoft software items that still need to be paid for. Some consumers may find alternate activation methods due to the perceived expensive cost of these items. There may be restrictions, unforeseen interruptions, and persistent activation prompts if these items are installed without being properly activated.
Our KMSpico app was created as a solution to this issue. By using this program, customers may access all of the functionality of Microsoft products and simplify the activation procedure.
KMSPico is a universal activator designed to optimize the process of generating and registering license codes for Windows and Office. Functionally, it is similar to key generators, but with the additional possibility of automatic integration of codes directly into the system. It is worth paying attention to the versatility of the tool, which distinguishes it from similar activators.
The above discussion primarily focused on the core KMS activator, the Pico app. Understanding what the program is, we can briefly mention KMSAuto, a tool with a simpler interface.
By using the KMSPico tool, you can setup Windows&Office for lifetime activation. This is an essential tool for anybody looking to reveal improved features and go beyond limitations. Although it is possible to buy a Windows or Office key.
KMSPico 11 (last update 2024) allows you to activate Windows 11/10/8 (8.1)/7 and Office 2021/2019/2016/2013/2010 for FREE.
KMSpico Download | Official KMS Website New July 2024
ez activator
Are you looking for the best tool to activate your Windows & Office? Then you should download and install KMSpico, as it is one of the best tools everyone should have. In this article, I will tell you everything about this fantastic tool, even though I will also tell you if this is safe to use.
In this case, don’t forget to read this article until the end, so you don’t miss any critical information. This guide is for both beginners and experts as I came up with some of the rumours spreading throughout the internet.
Perhaps before we move towards downloading or installing a section, we must first understand this tool. You should check out the guide below on this tool and how it works; if you already know about it, you can move to another section.
What is KMSPico?
KMPico is a tool that is used to activate or get a license for Microsft Windows as well as for MS Office. It was developed by one of the most famous developers named, Team Daz. However, it is entirely free to use. There is no need to purchase it or spend money downloading it. This works on the principle of Microsft’s feature named Key Management Server, a.k.a KMS (KMSPico named derived from it).
The feature is used for vast companies with many machines in their place. In this way, it is hard to buy a Windows License for each device,, which is why KMS introduced. Now a company has to buy a KMS server for them and use it when they can get a license for all their machines.
However, this tool also works on it, and similarly, it creates a server on your machine and makes it look like a part of that server. One thing different is that this tool only keeps the product activated for 180 days. This is why it keeps running on your machine, renews the license keys after 180 days, and makes it a permanent activation.
KMSAuto Net
Microsoft Toolkit
Windows Loader
Windows 10 Activator
Features
We already know what this tool means, so let’s talk about some of the features you are getting along with KMSPico. Reading this will surely help you understand whether you are downloading the correct file.
Ok, so here are some of the features that KMSPico provides:
Activate Windows & Office
We have already talked about this earlier, as using this tool, you will get the installation key for both Microsoft Products. Whether it is Windows or Office, you can get a license in no time; however, this supports various versions.
Supports Multi-Arch
Since this supports both products, it doesn’t mean you have to download separate versions for each arch. One version is enough, and you can get the license for both x32-bit or even the x64-bit.
It Is Free To Use
Undoubtedly, everything developed by Team Daz costs nothing to us. Similarly, using this tool won’t cost you either, as it is entirely free. Other than this, it doesn’t come with any ads, so using it won’t be any trouble.
Permanent License
Due to the KMS server, this tool installs on our PC, we will get the license key for the rest of our lives. This is because the license automatically renews after a few days. To keep it permanent, you must connect your machine to the internet once 180 days.
Virus Free
Now comes the main feature of this tool that makes it famous among others. KMSPico is 100% pure and clean from such viruses or trojans. The Virus Total scans it before uploading to ensure it doesn’t harm our visitors.
Pin Up online casino https://pin-up.webrabota77.ru/ is the official website of a popular gambling establishment for players from the CIS countries. The site features thousands of slot machines, online tables and other branded entertainment from Pin Up casino.
Pin Up Casino https://pin-up.noko39.ru Registration and Login to the Official Pin Up Website. thousands of slot machines, online tables and other branded entertainment from Pin Up casino. Come play and get big bonuses from the Pinup brand today
Le le code promo 1xbet. Enregistrez-vous des a present avec notre code promotionnel 1xBet valable jusqu’en 2024 pour beneficier d’un bonus de 200% sur votre premier depot. Utilisez le code de bonus lors de l’ouverture de votre nouveau compte 1xbet afin de recevoir votre bonus de bienvenue de 130$. L’enregistrement est autorise pour les personnes ayant atteint l’age de 18 ans et residant dans les pays ou l’activite du bookmaker n’est pas limitee au niveau legislatif.
L’inscription a 1xBet est-elle disponible sans passeport?
Vous pouvez vous inscrire a Bonus d’inscription 1xbet sans donnees de passeport, mais a l’avenir, dans votre compte personnel, vous devrez remplir un questionnaire indiquant votre nom, votre nom et votre date de naissance. A l’avenir, avant la premiere Conclusion, il faudra egalement passer par la verification.
Реальные анкеты проституток https://prostitutki-213.ru Москвы с проверенными фото – от элитных путан до дешевых шлюх. Каталог всех индивидуалок на каждой станции метро с реальными фотографиями без ретуши и с отзывами реальных клиентов.
Смотрите онлайн сериал Отчаянные домохозяйки https://domohozyayki-serial.ru в хорошем качестве HD 720 бесплатно, рейтинг сериала: 8.058, режиссер сериала: Дэвид Гроссман, Ларри Шоу, Дэвид Уоррен.
Buy TikTok followers https://tiktok-followers-buy.com to get popular and viral with your content. All packages are real and cheap — instant delivery within minutes. HQ followers for your TikTok. 100% real users. The lowest price for TikTok followers on the market
спортивные площадки для улицы спортивные площадки для улицы .
Pin Up Casino https://pin-up.sibelshield.ru official online casino website for players from the CIS countries. Login and registration to the Pin Up casino website is open to new users with bonuses and promotional free spins.
Qu’est-ce qu’une «Vitrine de codes promotionnels»?
Ceci est une section speciale sur le site du bookmaker 1xbet code bonus sans depot, qui contient tous les codes promotionnels actuels. Sur la vitrine, les joueurs sont disponibles codes bonus pour les Paris sportifs, pour la section avec le jeu. Chaque code peut etre echange contre des points promo en fonction des denominations.
Изготовление памятников и надгробий https://uralmegalit.ru по низким ценам. Собственное производство. Высокое качество, широкий ассортимент, скидки, установка.
Pin Up Casino https://pin-up.ergojournal.ru приглашает игроков зарегистрироваться на официальном сайте и начать играть на деньги в лучшие игровые автоматы, а на зеркалах онлайн казино Пин Ап можно найти аналогичную витрину слотов
Pin-up casino https://pin-up.jes-design.ru популярное онлайн-казино и ставки на спорт. Официальный сайт казино для доступа к играм и другим функциям казино для игры на деньги.
dlja-windows.ru
Twin Casino
Lorem Ipsum has been the industry’s standard dummy text https://genomatics.de/dfgrpw of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://mocemocjiwroclaw.pl/aayyvmq of type and scrambled it to make a type specimen book.
Pin Up https://pin-up.fotoevolution.ru казино, которое радует гемблеров в России на протяжении нескольких лет. Узнайте, что оно подготовило посетителям. Описание, бонусы, отзывы о легендарном проекте. Регистрация и вход.
Открой мир карточных игр в Pin-Up https://pin-up.porsamedlab.ru казино Блэкджек, Баккара, Хило и другие карточные развлечения. Регистрируйтесь и играйте онлайн!
Официальный сайт Pin Up казино https://pin-up.nasledie-smolensk.ru предлагает широкий выбор игр и щедрые бонусы для игроков. Уникальные бонусные предложения, онлайн регистрация.
Pinup казино https://pin-up.vcabinet.kz это не просто сайт, а целый мир азартных развлечений, где каждый может найти что-то свое. От традиционных игровых автоматов до прогнозов на самые популярные спортивные события.
Latest Diablo news https://diablo.com.az game descriptions and guides. Diablo.az is the largest Diablo portal in the Azerbaijani language.
Latest World of Warcraft (WOW) tournament news https://wow.com.az, strategies and game analysis. The most detailed gaming portal in Azerbaijani language
https://gadalika.ru/ –
Меня зовут Вера Ивановна. Люди в России называют меня целителем души и тела. Да, я действительно обладаю даром исцеления и общения с духами. Силы для своей работы с энергиями я черпаю из древних истоков, уходящих в мою теперь уже далекую Монголию. Я обладаю навыками в области белой, черной и сефиротической магии. Сильное телепатическое чувство. Занимаюсь целительством, чувствую эмоции и физическое состояние других людей (клиентов).
şanlıurfa oto kurtarma
Azerbaijan NFL https://nfl.com.az News, analysis and topics about the latest experience, victories and records. A portal where the most beautiful NFL games in the world are generally studied.
Discover exciting virtual football in Fortnite https://fortnite.com.az. Your central hub for the latest news, expert strategies and interesting e-sports reports. Collecting points with us!
The latest analysis, tournament reviews and the most interesting features of the Spider-Man game https://spider-man.com.az series in Azerbaijani.
Read the latest Counter-Strike 2 news https://counter-strike.net.az, watch the most successful tournaments and become the best in the world of the game on the CS2 Azerbaijan website.
https://gadalika.ru/ –
Всем здравия, кто посетил мою страничку. Меня зовут Анна Тимофеева. И я хочу поделиться с вами своими способностями. Как и все потомственные целители, я унаследовала свой Дар по крови от пробабушки, известной в России целительницы. Ее звали Анной, в неё честь и я ношу это имя. Корни нашего рода уходят глубоко во времена, когда целительство было обычным явлением. Прабабушка была дочерью священника. С юности она…
https://gadalke.ru/ – Меня зовут Мария Степановна, я потомственная ясновидяшая, предсказательница и знаю, зачем вы здесь. Уверена, вы получите ответ и помощь на моем официальном сайте. Каждый день сотни людей со сложными жизненными проблемами пытаются отыскать ответ на вопрос где найти настоящую хорошую гадалку с отзывами, проверенную многими людьми. Гадалку, которая реально помогает. По-разному называют нас: ясновидящая, маг, экстресенс и даже ведьмой назовут несведущие. Я не обижаюсь. Ведь все одно это: Дар, данный Богом. Шарлатанов, выдающих себя за гадалок теперь много стало. Да и гадание не сложная наука, научиться можно при должном упорстве и труде. Сейчас кто на чем гадает, кто на таро, кто на кофейной гуще, на рунах или на воске. Гадают, да не помогают. Потому как не по крови дано, а через ум вошло. А знать, ни порчу снять, ни мужа вернуть не сумеют — а я помогу!
Offre speciale code promo 1xbet congo vous offre une remise de 100% sur le montant total de votre premier depot jusqu’a 100$, bien entendu, dans votre devise locale. Profitez-en facilement en saisissant le code promotionnel lors de votre inscription et recevez un bonus sur 1xbet.com.
propecia singapore
Mesut Ozil https://mesut-ozil.com.az latest news, statistics, photos and much more. Get the latest news and information about one of the best football players Mesut Ozil.
Explore the extraordinary journey of Kilian Mbappe https://kilian-mbappe.com.az, from his humble beginnings to global stardom. Delve into his early years, meteoric rise through the ranks, and impact on and off the football field.
Latest news, statistics, photos and much more about Pele https://pele.com.az. Get the latest news and information about football legend Pele.
Latest boxing news https://boks.com.az, Resul Abbasov’s achievements, Tyson Fury’s fights and much more. All in Ambassador Boxing.
Sergio Ramos Garcia https://sergio-ramos.com.az Spanish footballer, defender. Former Spanish national team player. He played for 16 seasons as a central defender for Real Madrid, where he captained for six seasons.
ремонт стиральных машин на дому http://www.centr-remonta-stiralnyh-mashin.ru/ .
Gianluigi Buffon https://buffon.com.az Italian football player, goalkeeper. Considered one of the best goalkeepers of all time. He holds the record for the number of games in the Italian Championship, as well as the number of minutes in this tournament without conceding a goal.
Paulo Bruno Ezequiel Dybala https://dybala.com.az Argentine footballer, striker for the Italian club Roma and the Argentina national team. World champion 2022.
Paul Labille Pogba https://pogba.com.az French footballer, central midfielder of the Italian club Juventus. Currently suspended for doping and unable to play. World champion 2018.
Kevin De Bruyne https://kevin-de-bruyne.liverpool-fr.com Belgian footballer, born 28 June 1991 years in Ghent. He has had a brilliant club career and also plays for the Belgium national team. De Bruyne is known for his spectacular goals and brilliant assists.
Канал для того, чтобы знания и опыт, могли помочь любому человеку сделать ремонт https://tvin270584.livejournal.com в своем жилище, любой сложности!
Mohamed Salah Hamed Mehrez Ghali https://mohamed-salah.liverpool-fr.com Footballeur egyptien, attaquant du club anglais de Liverpool et l’equipe nationale egyptienne. Considere comme l’un des meilleurs joueurs du monde.
Paul Labille Pogba https://paul-pogba.psg-fr.com Footballeur francais, milieu de terrain central du club italien de la Juventus. Champion du monde 2018. Actuellement suspendu pour dopage et incapable de jouer.
The young talent who conquered Paris Saint-Germain: how Xavi Simons became https://xavi-simons.psg-fr.com leader of a superclub in record time.
1xBet offre precisement cela et vos bonus peuvent etre maximises en utilisant le code promo 1xbet cote d’ivoire 2024. Consultez simplement ci-dessous pour decouvrir ce qui vous attend en tant que nouveau client sur ce site de paris. Grace a ces connaissances, il est tout a fait logique de s’attendre a une serie de bonus de bienvenue attrayants pour les nouveaux joueurs provenant d’autres pays. Voici quelques exemples de ces pays : Burkina Faso, Ghana, Ouganda, Zambie, Cameroun, Senegal, Benin, Congo, Guinee, Cote d’Ivoire, Togo, Mali, etc.
Qu’est-ce qu’une «Vitrine de codes promotionnels»?
Ceci est une section speciale sur le site du bookmaker 1x pari code promo, qui contient tous les codes promotionnels actuels. Sur la vitrine, les joueurs sont disponibles codes bonus pour les Paris sportifs, pour la section avec le jeu. Chaque code peut etre echange contre des points promo en fonction des denominations.
viagra 50mg pill
code promo 1xbet senegal 2024 tous les details sur les bonus de bienvenue. Enregistrez-vous des maintenant avec notre offre speciale 1xBet 2024 pour beneficier d’un bonus de bienvenue de 100% jusqu’a 130$. Tous les nouveaux joueurs recoivent un bonus de bienvenue de 1xBet pour la creation d’un compte avec un code promotionnel.
В чёрный список пирамид и лохотронов 31 августа 2022 года внесены следующие организации, обладающие признаками финансовой пирамиды или признаками мошенничества.
жесткое групповое порно
Etihad Rail (etihadrail-ae.com)
Club Unite To Live, Life Is Good, Unite To Live (uniteto.live). Новый домен пирамиды находящегося в розыске Романа Василенко.
TopBoom, «платформа хедж-фонда, специализирующегося на сделках с обратным исходом спортивного события» (topboom.vip, t.me/TopBoom001)
Change Team, мошенники указывают реквизиты чужого юрлица ООО «АТТИС ГРУПП» (ОРГН 1207700314128, ИНН 9702022065), телеграм-канал «Change Team: Главный Канал» (change-team.ru). Фальшивый обменник раньше назывался C Exchange.
Ещё лохотроны:
Scam! Чёрный список пирамид и лохотронов и отзывы
В чёрный список пирамид и лохотронов включены организации, имеющие признаки финансовой пирамиды по классификации Центрального банка; организации, обладающие признаками матричной пирамиды (массовый привод друзей, «столы»); сборы денег с пенсионеров и прочих незащищённых слоёв населения; хайпы; организации, имеющие негативные отзывы; структуры, оказывающие финансовые услуги без лицензии и прочие лохотроны за исключением псевдоброкеров, кооперативов (с ними тоже не рекомендуем связываться) и некоторых других категорий.
Lorem Ipsum has been the industry’s standard dummy text https://kroatiereis.nl/fffucsf of type and scrambled it to make a type specimen book.
В чёрный список пирамид и лохотронов 31 августа 2022 года внесены следующие организации, обладающие признаками финансовой пирамиды или признаками мошенничества.
анальный секс смотреть
Etihad Rail (etihadrail-ae.com)
Club Unite To Live, Life Is Good, Unite To Live (uniteto.live). Новый домен пирамиды находящегося в розыске Романа Василенко.
TopBoom, «платформа хедж-фонда, специализирующегося на сделках с обратным исходом спортивного события» (topboom.vip, t.me/TopBoom001)
Change Team, мошенники указывают реквизиты чужого юрлица ООО «АТТИС ГРУПП» (ОРГН 1207700314128, ИНН 9702022065), телеграм-канал «Change Team: Главный Канал» (change-team.ru). Фальшивый обменник раньше назывался C Exchange.
Ещё лохотроны:
Scam! Чёрный список пирамид и лохотронов и отзывы
В чёрный список пирамид и лохотронов включены организации, имеющие признаки финансовой пирамиды по классификации Центрального банка; организации, обладающие признаками матричной пирамиды (массовый привод друзей, «столы»); сборы денег с пенсионеров и прочих незащищённых слоёв населения; хайпы; организации, имеющие негативные отзывы; структуры, оказывающие финансовые услуги без лицензии и прочие лохотроны за исключением псевдоброкеров, кооперативов (с ними тоже не рекомендуем связываться) и некоторых других категорий.
Lorem Ipsum has been the industry’s standard dummy text https://skybet365.es/ulodwyk of type and scrambled it to make a type specimen book.
Kylian Mbappe https://kylian-mbappe.psg-fr.com Footballeur, attaquant francais. Il joue pour le PSG et l’equipe de France. Ne le 20 decembre 1998 a Paris. Mbappe est francais de nationalite. La taille de l’athlete est de 178 cm.
Kevin De Bruyne https://liverpool.kevin-de-bruyne-fr.com Belgian footballer, born 28 June 1991 years in Ghent. He has had a brilliant club career and also plays for the Belgium national team. De Bruyne is known for his spectacular goals and brilliant assists.
Paul Pogba https://psg.paul-pogba-fr.com is a world-famous football player who plays as a central midfielder. The player’s career had its share of ups and downs, but he was always distinguished by his perseverance and desire to win.
Lorem Ipsum has been the industry’s standard dummy text https://genomatics.de/osxite of type and scrambled it to make a type specimen book.
Kylian Mbappe https://psg.kylian-mbappe-fr.com Footballeur, attaquant francais. L’attaquant de l’equipe de France Kylian Mbappe a longtemps refuse de signer un nouveau contrat avec le PSG, l’accord etant en vigueur jusqu’a l’ete 2022.
Изготовление, сборка и ремонт мебели https://shkafy-na-zakaz.blogspot.com для Вас, от эконом до премиум класса.
Lorem Ipsum has been the industry’s standard dummy text https://annacarniz.es/oacdw of type and scrambled it to make a type specimen book.
https://24smski.ru
Lorem Ipsum has been the industry’s standard dummy text https://soniamarco.it/tbekgd of type and scrambled it to make a type specimen book.
Thibaut Nicolas Marc Courtois https://thibaut-courtois.real-madrid-ar.com Footballeur belge, gardien de but du Club espagnol “Real Madrid”. Lors de la saison 2010/11, il a ete reconnu comme le meilleur gardien de la Pro League belge, ainsi que comme joueur de l’annee pour Genk. Trois fois vainqueur du Trophee Ricardo Zamora, decerne chaque annee au meilleur gardien espagnol
Forward Rodrigo https://rodrygo.real-madrid-ar.com is now rightfully considered a rising star of Real Madrid. The talented Santos graduate is compared to Neymar and Cristiano Ronaldo, but the young talent does not consider himself a star.
Jude Victor William Bellingham https://jude-bellingham.real-madrid-ar.com English footballer, midfielder of the Spanish club Real Madrid and the England national team. In April 2024, he won the Breakthrough of the Year award from the Laureus World Sports Awards.
Saud Abdullah Abdulhamid https://saud-abdulhamid.real-madrid-ar.com Saudi footballer, defender of the Al -Hilal” and the Saudi Arabian national team. Asian champion in the age category up to 19 years. Abdulhamid is a graduate of the Al-Ittihad club. On December 14, 2018, he made his debut in the Saudi Pro League in a match against Al Bateen
Khvicha Kvaratskhelia https://khvicha-kvaratskhelia.real-madrid-ar.com midfielder of the Georgian national football team and the Italian club “Napoli”. Became champion of Italy and best player in Serie A in the 2022/23 season. Kvaratskhelia is a graduate of Dynamo Tbilisi and played for the Rustavi team.
Lorem Ipsum has been the industry’s standard dummy text https://innocap-goettingen.de/ozwsaoh of type and scrambled it to make a type specimen book.
[url=https://kitehurghada.ru]Кайт это[/url] обучение кайтсёрфингу в Хургаде Египет https://kitehurghada.ru
Lorem Ipsum has been the industry’s standard dummy text https://maaximizate.es/uxxehoo of type and scrambled it to make a type specimen book.
Vinicius Junior https://vinisius-junior.com.az player news, fresh current and latest events for today about the player of the 2024 season
Latest news and information about Marcelo https://marcelo.com.az on this site! Find Marcelo’s biography, career, playing stats and more. Find out the latest information about football master Marcelo with us!
Khabib Abdulmanapovich Nurmagomedov https://khabib-nurmagomedov.com.az Russian mixed martial arts fighter who performed under the auspices of the UFC. Former UFC lightweight champion.
Lorem Ipsum has been the industry’s standard dummy text https://soniamarco.it/yssghn of type and scrambled it to make a type specimen book.
Welcome to our official site! Get to know the history, players and latest news of Inter Miami Football Club https://inter-miami.com.az. Discover with us the successes and great performances of America’s newest and most exciting soccer club.
Conor Anthony McGregor https://conor-mcgregor.com.az Irish mixed martial arts fighter who also performed in professional boxing. He performs under the auspices of the UFC in the lightweight weight category. Former UFC lightweight and featherweight champion.
Comment puis-je gagner des points un code promo x bet?
Dans le bookmaker 1xbet en tant qu’encouragement des clients pour leur participation active au processus de jeu, ils fournissent des points promotionnels dans le cadre du programme de fidelite. Vous pouvez obtenir des points pour les Paris sportifs reguliers, Express, pour la reconstitution reguliere du compte et la participation aux actions du bookmaker.
Lorem Ipsum has been the industry’s standard dummy text https://borealstudios.es/ktxyqf of type and scrambled it to make a type specimen book.
Оперативный вывод из запоя https://www.liveinternet.ru/users/laralim/post505923855/ на дому. Срочный выезд частного опытного нарколога круглосуточно. При необходимости больного госпитализируют в стационар.
Видеопродакшн студия https://humanvideo.ru полного цикла. Современное оборудование продакшн-компании позволяет снимать видеоролики, фильмы и клипы высокого качества. Создание эффективных видеороликов для рекламы, мероприятий, видеоролики для бизнеса.
Lorem Ipsum has been the industry’s standard dummy text https://rampymobilne.pl/aeooxfc of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://samowystarczalnyzakatek.pl/xknui of type and scrambled it to make a type specimen book.
Заказать вывоз мусора https://musorovozzz.ru в Москве и Московской области, недорого и в любое время суток в мешках или контейнерами 8 м?, 20 м?, 27 м?, 38 м?, собственный автопарк. Заключаем договора на вывоз мусора.
Реальные анкеты https://prostitutki-vyzvat-moskva.ru Москвы с проверенными фото – от элитных путан до дешевых шлюх. Каталог всех индивидуалок на каждой станции метро с реальными фотографиями без ретуши и с отзывами реальных клиентов.
Совсем недавно открылся новый интернет портал BlackSprut (Блекспрут) https://bs2cite.cc в даркнете, который предлагает купить нелегальные товары и заказать запрещенные услуги. Самая крупнейшая площадка СНГ. Любимые шопы и отзывчивая поддержка.
http://autoexpert-group.ru/
generic diflucan otc
Lorem Ipsum has been the industry’s standard dummy text https://umcompany.it/sdhjz of type and scrambled it to make a type specimen book.
Welcome to the site dedicated to Michael Jordan https://michael-jordan.com.az, a basketball legend and symbol of world sports culture. Here you will find highlights, career, family and news about one of the greatest athletes of all time.
Diego Armando Maradona https://diego-maradona.com.az Argentine footballer who played as an attacking midfielder and striker. He played for the clubs Argentinos Juniors, Boca Juniors, Barcelona, ??Napoli, and Sevilla.
Lorem Ipsum has been the industry’s standard dummy text https://amaloquehaces.es/nrafhc of type and scrambled it to make a type specimen book.
Gucci купить http://thebestluxurystores.ru по низкой цене в интернет-магазине брендовой одежды. Одежда и обувь бренда Gucci c доставкой.
Muhammad Ali https://muhammad-ali.com.az American professional boxer who competed in the heavy weight category; one of the most famous boxers in the history of world boxing.
Lorem Ipsum has been the industry’s standard dummy text https://childrenfestivalatri.it/ygfnsa of type and scrambled it to make a type specimen book.
Монтаж систем отопления https://fectum.pro, водоснабжения, вентиляции, канализации, очистки воды, пылеудаления, снеготаяния, гелиосистем в Краснодаре под ключ.
Enregistrez-vous en utilisant le code promo 1xbet rdc afin de profiter d’une offre exclusive de bonus de 100% jusqu’a 130$ sur les paris sportifs gratuits. Pour beneficier de cette offre de pari gratuit bonifiee, vous devrez placer 5 paris sur des accumulateurs dans les 30 jours. Il existe diverses strategies pour les paris combines, mais si vous souhaitez gagner et obtenir des paris gratuits, nous vous recommandons de privilegier des selections de cotes plus courtes et de vous concentrer sur des paris combines surs pour commencer.
Enregistrez-vous en utilisant le Code promo pari gratuit 1xbet afin de profiter d’une offre exclusive de bonus de 100% jusqu’a 130$ sur les paris sportifs gratuits. Pour beneficier de cette offre de pari gratuit bonifiee, vous devrez placer 5 paris sur des accumulateurs dans les 30 jours. Il existe diverses strategies pour les paris combines, mais si vous souhaitez gagner et obtenir des paris gratuits, nous vous recommandons de privilegier des selections de cotes plus courtes et de vous concentrer sur des paris combines surs pour commencer.
Enregistrez-vous en utilisant le code promo 1xbet burundi afin de profiter d’une offre exclusive de bonus de 100% jusqu’a 130$ sur les paris sportifs gratuits. Pour beneficier de cette offre de pari gratuit bonifiee, vous devrez placer 5 paris sur des accumulateurs dans les 30 jours. Il existe diverses strategies pour les paris combines, mais si vous souhaitez gagner et obtenir des paris gratuits, nous vous recommandons de privilegier des selections de cotes plus courtes et de vous concentrer sur des paris combines surs pour commencer.
Lev Ivanovich Yashin https://lev-yashin.com.az Soviet football player, goalkeeper. Olympic champion in 1956 and European champion in 1960, five-time champion of the USSR, three-time winner of the USSR Cup.
Al-Nasr https://al-nasr.com.az your source of news and information about Al-Nasr Football Club . Find out the latest results, transfer news, player and manager interviews, fixtures and much more.
Usain St. Leo Bolt https://usain-bolt.com.az Jamaican track and field athlete, specialized in short-distance running, eight-time Olympic champion and 11-time world champion (a record in the history of this competition among men).
Game World https://kz-games.kz offers the latest online gaming news, game reviews, gameplay and ideas, gaming tactics and tips . Start playing our most popular and amazing games and get ready to become the leader in the online gaming world!
You have a source of the latest and most interesting sports news from Kazakhstan: “Kazakhstan sports news https://sports-kazahstan.kz: Games and records” ! Follow us to receive updates and interesting news every minute!
Lorem Ipsum has been the industry’s standard dummy text https://primescan.es/faybgl of type and scrambled it to make a type specimen book.
http://avansir.ru/
Lorem Ipsum has been the industry’s standard dummy text https://impertdesign.pl/cixwvb of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://durgaspa.in/rpbzdg of type and scrambled it to make a type specimen book.
Latest news and information about the NBA https://basketball-kz.kz in Kazakhstan. Hot stories, player transfers and highlights. Watch the NBA world with us.
Top sports news https://sport-kz-news.kz, photos and blogs from experts and famous athletes, as well as statistics and information about matches of leading championships.
The latest top football news https://football-kz.kz today. Interviews with football players, online broadcasts and match results, analytics and football forecasts, photos and videos.
Lorem Ipsum has been the industry’s standard dummy text https://stepspdf.us/sgwxdfi of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://stepsman.cfd/otxfv of type and scrambled it to make a type specimen book.
canadian pharmacy accutane
Lorem Ipsum has been the industry’s standard dummy text https://itdatabase.pl/gogwyok of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://rauldelahuerga.es/hciggp of type and scrambled it to make a type specimen book.
Latest news about games for Android https://android-games.kz, reviews and daily updates. Read now and get the latest information about the most exciting games
Check out Minecraft kz https://minecraft-kz.kz for the latest news, guides, and in-depth reviews of the game options available. Find the latest information on Minecraft Download, Pocket Edition and Bedrock Edition.
Latest news from World of Warcraft https://wow-kz.kz (WOW) tournaments, strategy and game analysis. The most detailed gaming portal in the language.
Latest news and analysis of the Premier League https://premier-league.kz. Full descriptions of matches, team statistics and the most interesting football events. Premier Kazakhstan is the best place for football fans.
reputable mexican pharmacies online: mexican pharmacy – reputable mexican pharmacies online
Lorem Ipsum has been the industry’s standard dummy text https://aadityagroup.in/jgkjnns of type and scrambled it to make a type specimen book.
medication from mexico pharmacy
http://cmqpharma.com/# purple pharmacy mexico price list
medication from mexico pharmacy
Lorem Ipsum has been the industry’s standard dummy text https://creepy.es/pdjuvf of type and scrambled it to make a type specimen book.
Доставка груза и грузоперевозки https://tamozhennyy-deklarant.blogspot.com по России через транспортную компанию автотранспортом доступна и для частных лиц. Перевозчик отправит или доставит ваш груз: выгодные тарифы индивидуальный подход из рук в руки 1 машиной.
Зеркала интерьерные https://zerkala-mag.ru в интернет-магазине «Зеркала с подсветкой» Самые низкие цены на зеркала!
Предлагаем купить гаражное оборудование https://profcomplex.pro, автохимию, технику и уборочный инвентарь для клининговых компаний. Доставка по Москве и другим городам России.
Combien de temps faut-il pour retirer des fonds sur une carte Visa ou MasterCard?
Le retrait des fonds sur les cartes bancaires des systemes de paiement Visa et Mastercard depend du montant de la transaction, du jour de la semaine et de l’heure de la journee.code promo bonus 1xbet En regle generale, les fonds arrivent sur le compte indique dans un delai de 24 heures.
Купить зеркала https://zerkala-m.ru по низким ценам. Более 1980 моделей, купить недорого в интернет-магазине в Москве с доставкой по России. Удобный каталог, низкие цены, качественные фото.
Lorem Ipsum has been the industry’s standard dummy text https://garidakho.in/iydgacz of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://kellyandzenneth.co.za/dpfwq of type and scrambled it to make a type specimen book.
buy cipro online no prescription
Spider-Man https://spiderman.kz the latest news, articles, reviews, dates, spoilers and other latest information. All materials on the topic “Spider-Man”
The latest top football news https://football.sport-news-eg.com today. Interviews with football players, online broadcasts and match results, analytics and football forecasts, photos and videos.
Lorem Ipsum has been the industry’s standard dummy text https://msizindlela.co.za/vvyadpi of type and scrambled it to make a type specimen book.
Latest Counter-Strike 2 news https://counter-strike-kz.kz, watch the most successful tournaments and be the best in the gaming world.
http://autolombard-capital.ru/
Discover the dynamic world of Arab sports https://sports-ar.com through the lens of Arab sports news. Your premier source for breaking news, exclusive interviews, in-depth analysis and live coverage of everything happening in sports.
An Attraction of Luxury Fashion
Dress enthusiasts and premium buyers usually find themselves captivated by the elegance as well as renown of premium dress. Starting with the detailed aspects regarding one Hermes Birkin towards a emblematic style of a Chanel 2.55, those goods signify greater than just style—many people represent a good certain status and exclusiveness. However, not every person can afford up to spend lavishly upon those high-end products, which has guided to the growing pattern concerning replica purses. With regard to numerous, these fakes provide an manner up to take pleasure in the elegance concerning high style styles with out damaging an bank.
The surge inside appeal of replica purses has opened up an intriguing discussion concerning dress, honesty, plus personal fashion. Inside some sort of website content, we all will explore a numerous aspects regarding some sort of movement, offering style enthusiasts along with an extensive manual to imitation handbags. By the end, you can have the understanding to make informed judgments that line up with the beliefs plus looks.
Ethical as well as Lawful Considerations concerning Replica Bags
Any time that relates to imitation purses, one concerning a nearly all pressing concerns is a moral as well as legitimate effects. An generation and sale regarding counterfeit products are illegal within numerous nations, while the idea infringes rational property privileges. That certainly not just has effects on a earnings concerning premium models but in addition elevates questions concerning an situations below that these imitations tend to be developed.
Fashioning and Incorporating Replica Handbags
Incorporating fake bags into your a collection may become both stylish trendy & moral. A approach is to to combine top-quality imitations w/authentic authentic articles & additional sustainable green apparel pieces. This does not only enhances your complete look but also additionally promotes advances a more sustainable style cycle.
While styling imitation handbags, reflect on the occasion event and one’s outfit. A classic replica bag may bring a touch hint of elegance to an official outfit, whereas an in-style design may make a casual look trendier. Do not be hesitant to try w/different different styles & accoutrements to craft an original & personalized look.
Moreover, taking care for replica bags is crucial key to keep their look appearance and longevity. Consistent cleaning plus correct keeping can assist maintain your a handbags looking fresh and fashionable for longer.
The Value of knowledgeable Buyer Choices
In the current today’s style landscape, educated customer decisions are more important important than. While replica purses give a budget-friendly alternative to luxury luxury goods, it is vital to consider the moral and legal implications. By remaining aware about where and and how you you buy fakes, you can enjoy luxury fashion while loyal to your values values.
It is additionally essential to keep in mind that unique fashion is not defined by name names or cost tags. Whether you one opts to spend on authentic real luxury items or explore checking out the domain of imitation bags, the key is to find finding articles that help one feel confident and trendy.
Wrap-Up
Imitation handbags carved out out a special spot in the fashion style industry, offering a cost-effective & reachable option for luxury luxury pieces. While they bring with their their own particular set of of moral
Related Apparel Topics
Exploring the world of fashion doesn’t conclude with imitation bags. Here are some further related themes that might intrigue you:
Green Apparel
Dive into the significance of green practices in the style industry. Understand about sustainable materials, principled production techniques, and how to construct a green wardrobe.
Classic and Second-Hand Fashion
Discover the allure of retro and pre-owned apparel. Learn how to find quality retro articles, the perks of second-hand apparel, and tips for including these pieces into your current closet.
DIY Style and Repurposing
Become creative with Homemade apparel initiatives and upcycling used garments. Acquire useful advice on altering your closet by making your own adornments or modifying existing pieces to give them a new life.
Style on a Dime
Learn how to be trendy without breaking the savings. Investigate strategies for finding great bargains, buying shrewdly during sales, and making the most of your fashion funds.
Compact Closets
Understand the idea of a compact closet—creating a set of essential, multi-purpose items that can be mixed and paired to form different outfits. Evaluate the advantages of this streamlined method and how to implement it.
Fashion Tendencies and Projecting
Remain in front of the curve by exploring forthcoming fashion trends and industry projections. Discover about trendsetting fashionistas, significant apparel shows, and the most recent must-have items.
Style and Tech
Investigate how technology is revolutionizing the style industry. Subjects cover intelligent fabrics, digital fitting rooms, style apps, and the influence of online platforms on style promotion and customer actions.
Physique Confidence and Fashion
Investigate the relationship between apparel and figure positivity. Understand about labels supporting inclusive sizing, the significance of inclusion in fashion outlets, and how to style for different shapes.
Style Legacy
Embark on a trip through the legacy of apparel. Uncover different periods, iconic apparel movements, and how past fashions persist to affect modern fashion.
Fashion Photos and Blogs
Delve into the realm of fashion snapshots and writing. Acquire guidance on how to get amazing style shots, begin your own style journal, and increase your visibility online.
Lorem Ipsum has been the industry’s standard dummy text https://cosavedereinungiorno.it/fnjkzci of type and scrambled it to make a type specimen book.
https://bs4shop.top/ – 2fa blacksprut, blacksprut onion
блэкспрут ссылка тор – блэкспрут 2fa, blacksprut onion
блэкспрут ссылка тор – блэкспрут darknet, блек спрут онион
Lorem Ipsum has been the industry’s standard dummy text https://theofficemakers.in/qvlzf of type and scrambled it to make a type specimen book.
https://blacksprut-sait.top – blacksprut onion, блэкспрут даркнет
Интернет магазин электроники https://techno-line.store и цифровой техники по доступным ценам. Доставка мобильной электроники по Москве и Московской области.
NHL news https://nhl-ar.com (National Hockey League) – the latest and most up-to-date NHL news for today.
UFC news https://ufc-ar.com, schedule of fights and tournaments 2024, ratings of UFC fighters, interviews, photos and videos. Live broadcasts and broadcasts of tournaments, statistics, forums and fan blogs.
The most important sports news https://bein-sport-egypt.com, photos and blogs from experts and famous athletes, as well as statistics and information about matches of leading leagues.
An Attraction regarding Premium Style
Style aficionados as well as luxury shoppers frequently find themselves fascinated by a elegance as well as renown concerning high-end fashion. Starting with the intricate aspects of a Hermes Birkin to a emblematic style regarding one Chanel 2.55, these particular goods represent greater than simply dress—many people represent a good certain position plus exclusiveness. Nevertheless, certainly not everyone else might pay for towards spend lavishly on those luxury items, which has guided to a increasing movement of fake handbags. Regarding many, these particular replicas give an approach to take pleasure in the elegance of high-fashion designs without busting the bank.
The rise in popularity concerning fake purses has opened up a amazing intriguing discussion about dress, ethics, plus personal dress. In a weblog content, most of us may analyze a different facets of some sort of pattern, supplying style enthusiasts along with a comprehensive manual regarding fake bags. Through an end, you’ll have a knowledge to make informed choices that will align together with the beliefs and looks.
Ethical and Legitimate Concerns regarding Imitation Handbags
Any time that comes to fake purses, 1 of an many pressing issues will be a ethical and legitimate effects. A manufacturing and purchase concerning imitation items are unlawful inside a lot of countries, because it breaches mental residential property legal rights. That not only has effects on a profits regarding high-end brands but in addition increases questions regarding a conditions below that these fakes usually are made.
Fashioning plus Integrating Replica Purses
Including replica bags into your a wardrobe can prove both trendy fashionable & moral. One approach would be to mix high-quality fakes with authentic articles & additional sustainable green apparel goods. This doesn’t only improves a complete style yet also promotes advances a more sustainable fashion movement.
When coordinating replica purses, reflect on your event occasion plus one’s ensemble. A classic traditional fake purse may bring a touch touch of sophistication to an official attire, whilst an in-style design can turn a relaxed look trendier. Never become afraid to experiment with different various patterns and accoutrements to create an original and tailored look.
Moreover, caring for replica handbags is key to preserve their appearance & longevity. Routine washing and appropriate keeping can help maintain your a bags appearing new & trendy for.
The importance Significance of knowledgeable Customer Selections
In today’s fashion environment, educated customer selections are more crucial crucial than ever. Though fake purses offer an affordable alternative for luxury designer goods, it’s key to think about the ethical plus legal implications. By staying aware of where and how you one buys replicas, you can can relish high-end apparel while true to your values beliefs.
It’s equally essential to keep in mind that personal individual fashion is not defined by the brand names or price price tags. Whether one opts to put money on authentic authentic luxury items or check out exploring the world of fake purses, the secret is discovering items that make you feel self-assured & stylish.
Conclusion
Imitation bags carved out a distinct special place in the fashion fashion universe, offering a budget-friendly & accessible option for luxury designer pieces. Though they arrive come with their own its own set of of principled
Associated Style Themes
Exploring the realm of style doesn’t finish with copy bags. Here are some additional related themes that may interest you:
Sustainable Style
Delve into the importance of eco-friendliness in the style sector. Discover about sustainable fabrics, moral production methods, and how to create a sustainable wardrobe.
Retro and Thrift Style
Uncover the appeal of classic and pre-owned garments. Learn how to source premium classic pieces, the perks of pre-owned apparel, and advice for integrating these pieces into your contemporary collection.
Do-It-Yourself Style and Repurposing
Be creative with Homemade fashion activities and upcycling previous clothes. Get useful tips on altering your wardrobe by making your own accents or customizing existing items to grant them a renewed life.
Fashion on a Shoestring
Understand how to remain fashionable without exceeding the savings. Uncover tricks for get excellent deals, purchasing shrewdly during promotions, and making the most of your fashion resources.
Capsule Wardrobes
Comprehend the idea of a compact collection—curating a collection of important, adaptable articles that can be combined and matched to create various looks. Analyze the benefits of this streamlined approach and how to apply it.
Apparel Trends and Predicting
Remain ahead of the curve by exploring forthcoming fashion trends and industry projections. Discover about pioneering creators, significant fashion shows, and the latest necessary items.
Style and Tech
Investigate how tech is transforming the fashion field. Subjects cover intelligent materials, virtual fittings, fashion tools, and the impact of social networks on fashion promotion and buyer habits.
Figure Acceptance and Style
Explore the relationship between style and physique confidence. Discover about labels promoting comprehensive sizes, the value of depiction in style outlets, and how to dress for different body types.
Fashion Legacy
Embark on a journey through the legacy of fashion. Uncover different times, legendary apparel moments, and how past fashions continue to affect modern style.
Fashion Snapshots and Blogs
Delve into the universe of apparel photos and blogging. Get advice on how to capture amazing style shots, launch your own fashion blog, and increase your visibility online.
News and events of the American Basketball League https://basketball-eg.com in Egypt. Hot events, player transfers and the most interesting events. Explore the world of the NBA with us.
Ou dois-je inserer un code promo lors de l’inscription a 1xBet?
Des que le code promo 1xbet aujourd’hui est copie, le joueur doit aller a l’enregistrement dans le bureau 1xbet. Dans le processus d’inscription, le code copie doit etre colle dans un formulaire special.
A Allure of High-End Style
Dress fans as well as premium shoppers frequently find themselves fascinated via the grace as well as renown concerning luxury dress. From an complex details concerning one Hermes Birkin towards the legendary design of an Chanel 2.55, these particular products signify more than merely dress—these individuals represent a particular standing as well as exclusiveness. Nonetheless, definitely not everyone else can have the funds for up to spend lavishly with these particular premium items, that will has brought to an rising pattern concerning fake handbags. With regard to a lot of, those replicas provide an manner up to take pleasure in a splendor of high style layouts devoid of damaging the traditional bank.
A increase within appeal regarding imitation handbags has opened up a amazing intriguing conversation about style, values, and personal style. In some sort of website article, most of us may explore the numerous aspects concerning this pattern, providing fashion enthusiasts along with one extensive guide regarding replica bags. Through the conclusion, you may possess a information in order to help make well-informed decisions which align along with the prices as well as aesthetics.
Ethical as well as Legitimate Considerations regarding Imitation Handbags
As soon as that comes to replica purses, 1 of the most pressing concerns can be the ethical and legal implications. A manufacturing plus sale regarding imitation goods are unlawful in numerous nations, because that breaches intellectual house legal rights. This certainly not only impacts the earnings regarding luxury brands but additionally raises questions about the situations below which these imitations tend to be produced.
Fashioning and Including Fake Bags
Incorporating replica handbags into one’s collection may prove both stylish trendy also principled. A single approach is to combine premium imitations with authentic genuine pieces plus additional sustainable sustainable apparel pieces. Doing this doesn’t only elevate enhances your complete look but additionally promotes encourages an eco-friendly fashion movement.
Whenever styling imitation purses, reflect on the event plus your attire. An elegant timeless imitation bag could add a touch element of elegance for a a formal ensemble, while a trendy design can turn a casual appearance more stylish. Never become hesitant to try with different various trends plus accoutrements to develop an original plus tailored appearance.
Additionally, taking care for your replica purses is crucial key to keep their condition plus lifespan. Routine cleaning & correct storage may assist maintain your one’s purses seeming pristine & trendy for.
The importance Value of Informed Customer Selections
In today’s style scene, informed buyer selections are more more crucial important than ever before. While replica purses offer an affordable option for luxury luxury pieces, it key to reflect on the moral and legitimate implications. By remaining aware about where and & how one buys fakes, one can can enjoy premium fashion while true to one’s values values.
It’s additionally important to recall that personal personal fashion isn’t defined determined by brand names or price price tags. Whether you choose to put money in authentic designer items or explore exploring the domain of replica purses, the secret is finding to find items that one feel confident & fashionable.
Conclusion
Fake purses have carved out a distinct place in the apparel world, giving an affordable and reachable substitute for luxury designer goods. Although they come arrive with their their own unique set of of ethical
Connected Apparel Subjects
Discovering the world of fashion doesn’t finish with replica bags. Here are some additional related themes that might intrigue you:
Green Style
Dive into the value of sustainability in the apparel sector. Learn about sustainable materials, ethical fabrication techniques, and how to construct a green wardrobe.
Classic and Pre-owned Style
Uncover the allure of retro and pre-owned garments. Find out how to get quality vintage articles, the benefits of second-hand apparel, and suggestions for including these items into your modern wardrobe.
Do-It-Yourself Apparel and Repurposing
Become imaginative with Homemade apparel initiatives and upcycling previous apparel. Acquire hands-on guidance on transforming your closet by making your own adornments or personalizing current articles to bestow them a fresh existence.
Style on a Dime
Learn how to stay fashionable without breaking the bank. Uncover tricks for finding excellent offers, shopping shrewdly during discounts, and get your apparel budget.
Capsule Collections
Comprehend the concept of a capsule collection—curating a group of key, multi-purpose articles that can be combined and paired to form numerous ensembles. Examine the advantages of this simple strategy and how to adopt it.
Fashion Trends and Forecasting
Remain forward of the movement by investigating forthcoming fashion trends and sector forecasts. Discover about innovative designers, significant apparel weeks, and the latest essential pieces.
Style and Technology
Explore how technology is changing the style sector. Subjects include intelligent materials, virtual fitting rooms, apparel tools, and the influence of social networks on style promotion and customer habits.
Body Confidence and Apparel
Examine the connection between apparel and figure confidence. Learn about brands advocating inclusive sizes, the value of inclusion in style media, and how to dress for diverse figures.
Style Heritage
Embark on a exploration through the history of fashion. Uncover different periods, famous style movements, and how historical styles persist to shape modern apparel.
Fashion Snapshots and Writing
Dive into the world of fashion photography and blogging. Gain advice on how to capture stunning style photos, launch your own apparel website, and increase your visibility in the digital space.
advair medicine generic
Discover the wonderful world of online games https://game-news-ar.com. Get the latest news, reviews and tips for your favorite games.
Minecraft news https://minecraft-ar.com, guides and in-depth reviews of the gaming features available in Minecraft Ar. Get the latest information on downloading Minecraft, Pocket Edition and Bedrock Edition.
News, tournaments, guides and strategies about the latest GTA games https://gta-ar.com. Stay tuned for the best GTA gaming experience
Latest news https://android-games-ar.com about Android games, reviews and daily updates. The latest information about the most exciting games.
Apres le paiement, le Codes promo gratuits 1xbet devient disponible et peut etre active par le joueur a tout moment. Il y a beaucoup d’offres dans la vitrine des codes promotionnels. Dans la plupart des cas, ils couvrent la section du casino, mais souvent dans la vitrine sont publies des codes interessants pour la Conclusion a des conditions preferentielles des Paris Express, pour obtenir un cashback pour les Paris perdus. La vitrine est mise a jour assez souvent.
http://ryazanavto-kia62.ru/
Pin-Up Casino’da daha once bir hesap olusturduysan?z, giris yapmak da oldukca kolayd?r pin up casino
Lorem Ipsum has been the industry’s standard dummy text https://theofficemakers.in/vmlppv of type and scrambled it to make a type specimen book.
code promo pour 1x pari. Utilisez – le lors de votre inscription pour obtenir un bonus de 100% jusqu’a 130$. Pour obtenir des bonus du bookmaker 1xbet, vous devez remplir certaines conditions, mais les codes promotionnels vous permettent de les obtenir beaucoup plus facilement. La taille des bonus disponibles pour les joueurs via les codes promotionnels 1xBet peut etre petite, mais meme un petit bonus peut augmenter considerablement le potentiel de jeu du client.
Lorem Ipsum has been the industry’s standard dummy text https://telomontoyo.es/uukot of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://kalexkursy.pl/ppaitnk of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://garidakho.in/wdxed of type and scrambled it to make a type specimen book.
Открытие для себя Ерлинг Хааланда https://manchestercity.erling-haaland-cz.com, a talented player of «Manchester City». Learn more about his skills, achievements and career growth.
The path of 21-year-old Jude Bellingham https://realmadrid.jude-bellingham-cz.com from young talent to one of the most promising players in the world, reaching new heights with Dortmund and England.
The site is dedicated to football https://fooball-egypt.com, football history and news. Latest news and fresh reviews of the world of football
French prodigy Kylian Mbappe https://realmadrid.kylian-mbappe-cz.com is taking football by storm, joining his main target, ” Real.” New titles and records are expected.
Harry Kane’s journey https://bavaria.harry-kane-cz.com from Tottenham’s leading striker to Bayern’s leader and Champions League champion – this is the story of a triumphant ascent to the football Olympus.
Signup Bonus-200% up to your first deposit using promo code GGBET93-click the link to collect. The official Pinterest account of the bookmaker and online casino GGBET. Actual login to GGBET website in 2024 ggbet kasyno
http://progressive-cars.ru/
Lorem Ipsum has been the industry’s standard dummy text https://marielabertuggia.es/pgfbd of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://msizindlela.co.za/kzhins of type and scrambled it to make a type specimen book.
Изготовим для Вас изделия из металла https://smith-moskva.blogspot.com, по вашим чертежам или по нашим эскизам.
Промышленные насосы https://1nsk.ru/news/articles/nasosy-spetsialnogo-naznacheniya.html Wilo предлагают широкий ассортимент решений для различных отраслей промышленности, включая водоснабжение, отопление, вентиляцию, кондиционирование и многие другие. Благодаря своей высокой производительности и эффективности, насосы Wilo помогают снизить расходы на энергию и обслуживание, что делает их идеальным выбором для вашего бизнеса.
Откатные ворота являются отличным выбором для ограждения частной территории, в частности, откатные ворота предоставляют максимальную надежность и прочность, при этом имеют относительно невысокую цену http://rvolchansk.ru/index.php?subaction=userinfo&user=egitez
Lorem Ipsum has been the industry’s standard dummy text https://tscapp.es/sbuxfh of type and scrambled it to make a type specimen book.
https://buzard.ru панели для отделки фасада – интернет магазин
The fascinating story of the rise of Brazilian prodigy Vinicius Junior https://realmadrid.vinicius-junior-cz.com to the heights of glory as part of the legendary Madrid “Real”
Mohamed Salah https://liverpool.mohamed-salah-cz.com, who grew up in a small town in Egypt, conquered Europe and became Liverpool star and one of the best players in the world.
Lorem Ipsum has been the industry’s standard dummy text https://professionalgardens.es/itlrx of type and scrambled it to make a type specimen book.
Лизинг спецтехники для юридических лиц – это эффективный способ инвестировать в свою компанию. Условия договора лизинга, такие как срок и график платежей, обычно определяются индивидуально лизинг на спецтехнику
buy bactrim on line without a prescription
The inspiring story of how talented Kevin De Bruyne https://manchestercity.kevin-de-bruyne-cz.com became the best player of Manchester City and the Belgium national team. From humble origins to the leader of a top club.
Полезные советы и пошаговые инструкции по строительству https://svoyugol.by, ремонту и дизайну домов и квартир, выбору материалов, монтажу и установке своими руками.
Lionel Messi https://intermiami.lionel-messi-cz.com, one of the best football players of all time, moves to Inter Miami” and changes the face of North American football.
Bernardo Mota Veiga de Carvalho e Silva https://manchestercity.bernardo-silva-cz.com Portuguese footballer, club midfielder Manchester City and the Portuguese national team.
Lorem Ipsum has been the industry’s standard dummy text https://palme-net.de/qgyyzm of type and scrambled it to make a type specimen book.
Offre speciale code promo 1xbet 2024 vous offre une remise de 100% sur le montant total de votre premier depot jusqu’a 100$, bien entendu, dans votre devise locale. Profitez-en facilement en saisissant le code promotionnel lors de votre inscription et recevez un bonus sur 1xbet.com.
Antoine Griezmann https://atlticomadrid-dhb.antoine-griezmann-cz.com Atletico Madrid star whose talent and decisive goals helped the club reach the top of La Liga and the UEFA Champions League.
Lorem Ipsum has been the industry’s standard dummy text https://soniamarco.it/nhtekxx of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://nadpoprzeczka.pl/zyqnvzw of type and scrambled it to make a type specimen book.
Son Heung-min’s https://tottenhamhotspur.son-heung-min-cz.com success story at Tottenham Hotspur and his influence on the South Korean football, youth inspiration and changing the perception of Asian players.
The story of Robert Lewandowski https://barcelona.robert-lewandowski-cz.com, his impressive journey from Poland to Barcelona, ??where he became not only a leader on the field, but also a source of inspiration for young players.
We explore the path of Luka Modric https://realmadrid.luka-modric-cz.com to Real Madrid, from a difficult adaptation to legendary Champions League triumphs and personal awards.
The impact of the arrival of Cristiano Ronaldo https://annasr.cristiano-ronaldo-cz.com at Al-Nasr. From sporting triumphs to cultural changes in Saudi football.
Lorem Ipsum has been the industry’s standard dummy text https://you2i.dk/ugxir of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://cloudtechnical.in/xpqmq of type and scrambled it to make a type specimen book.
https://nudifyai.net/
Lorem Ipsum has been the industry’s standard dummy text https://spahouse.dk/oqqsb of type and scrambled it to make a type specimen book.
Купить машины в лизинг от официальных дилеров, автосалонов. Выгодные условия и скидки автотранспорт в лизинге
Meilleur 1xbet bonus de bienvenue 2024 vous permettra de recevoir leur excellent bonus de bienvenue allant jusqu’a $130 sur le sport en paris gratuits. Ce bonus de bienvenue est valable un mois. La maniere la plus simple d’obtenir un code promotionnel pour 1xbet est de visiter l’un des sites partenaires. En general, ces ressources publient regulierement des codes frais dans le cadre de leur cooperation constante avec le bookmaker.
https://nudifyai.net
Lorem Ipsum has been the industry’s standard dummy text https://pawslo.pl/jopjo of type and scrambled it to make a type specimen book.
Meilleur 1 x code promo de pari vous permettra de recevoir leur excellent bonus de bienvenue allant jusqu’a $130 sur le sport en paris gratuits. Ce bonus de bienvenue est valable un mois. La maniere la plus simple d’obtenir un code promotionnel pour 1xbet est de visiter l’un des sites partenaires. En general, ces ressources publient regulierement des codes frais dans le cadre de leur cooperation constante avec le bookmaker.
Find out how Pedri https://barcelona.pedri-cz.com becomes a key figure for Barcelona – his development, influence and ambitions determine the club’s future success in world football.
A study of the influence of Rodrigo https://realmadrid.rodrygo-cz.com on the success and marketing strategy of Real Madrid: analysis of technical skills, popularity in Media and commercial success.
How Karim Benzema https://alIttihad.karim-benzema-cz.com changed the game of Al-Ittihad and Saudi football: new tactics, championship success, increased viewership and commercial success.
Find out about Alisson https://liverpool.alisson-becker-cz.com‘s influence on Liverpool’s success, from his defense to personal achievements that made him one of the best goalkeepers in the world.
Find out how Pedro Gavi https://barcelona.gavi-cz.com helped Barcelona achieve success thanks to his unique qualities, technique and leadership, becoming a key player in the team.
Lorem Ipsum has been the industry’s standard dummy text https://plaquiste-millau.fr/xlwyyd of type and scrambled it to make a type specimen book.
Utilisez le 1xbet bonus de bienvenue 2024 2024 et profitez de l’offre VIP 1xBet de 200% jusqu’a 78 000 XOF sur les paris sportifs. Inscrivez-vous avec un code promotionnel et recevez un bonus de bienvenue. Vous pouvez utiliser l’argent du bonus pour parier sur des sports ou jouer dans des casinos en ligne. La promotion 2024 est valable pour tous les nouveaux clients.
Lorem Ipsum has been the industry’s standard dummy text https://sps2015.pl/ctwqbm of type and scrambled it to make a type specimen book.
Для тех, кто ищет увлекательные пути к развлечениям и возможности испытать удачу в виртуальной среде, существует мир, где представлены бесчисленные варианты игр и азартных развлечений http://mongdol.net/bbs/board.php?bo_table=free&wr_id=2506410
r7 казино https://mabiclub.ru
Как показывает практика, сегодня купить лучшее медицинское оборудование и технику в Украине, востребованные для оказания соответствующих услуг на безупречном уровне, точно не является проблемой https://www.niann.ru/?id=598583
buy instagram followers cheap buy instagram followers
Lorem Ipsum has been the industry’s standard dummy text https://spahouse.dk/hkmaee of type and scrambled it to make a type specimen book.
Find out how Virgil van Dijk https://liverpool.virgil-van-dijk-cz.com became an integral part of style игры «Liverpool», ensuring the stability and success of the team.
Find out how Bruno Guimaraes https://newcastleunited.bruno-guimaraes-cz.com became a catalyst for the success of Newcastle United thanks to his technical abilities and leadership on the field and beyond.
Lorem Ipsum has been the industry’s standard dummy text https://stepsman.cfd/zefjuyf of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://gomalta.co.za/inxya of type and scrambled it to make a type specimen book.
Реализуя широкий ассортимент оборудования и медицинской техники, мы удовлетворяем запросы врачей различных профилей, косметологов и административного персонала https://www.niann.ru/?id=598583
Study of the playing style of Toni Kroos https://real-madrid.toni-kroos-cz.com at Real Madrid: his accurate passing, tactical flexibility and influence on the team’s success.
Romelu Lukaku https://chelsea.romelu-lukaku-cz.com, one of the best strikers in Europe, returns to Chelsea to continue climbing to the top of the football Olympus.
The young Uruguayan Darwin Nunez https://liverpool.darwin-nunez-cz.com broke into the elite of world football, and he became a key Liverpool player.
Star Brazilian striker Gabriel Jesus https://arsenal.gabriel-jesus-cz.com put in a superb performance to lead Arsenal to new heights after moving from Manchester City.
Lorem Ipsum has been the industry’s standard dummy text https://fleurbase.dk/nghiulm of type and scrambled it to make a type specimen book.
A fascinating story about how David Alaba https://realmadrid.david-alaba-cz.com after starting his career at the Austrian academy Vienna became a key player and leader of the legendary Real Madrid.
Lorem Ipsum has been the industry’s standard dummy text https://evafinans.dk/hhzolym of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://vildtnemt.dk/ornio of type and scrambled it to make a type specimen book.
Des que le compte est active et que le premier depot est recu sur le compte courant, le compte bonus recevra un montant de 130$. En consequence, les chances d’un joueur de gagner au premier pari augmentent de 130%. Et cet avantage est rendu disponible grace au Code promo 1xbet aujourd’hui.
Lorem Ipsum has been the industry’s standard dummy text https://btelectricshop.es/xlwwwas of type and scrambled it to make a type specimen book.
Нужны деньги!?
Поможем получить кредит даже с плохой кредитной историей.
На самых выгодных условиях.
+7 (985) 059-26-23
The story of how the incredibly talented footballer Riyad Mahrez https://alahli.riyad-mahrez-cz.com reached new heights in career, moving to Al Ahly and leading the team to victory.
Лизинг оборудования открывает новые возможности для развития вашей компании. Это одно из наиболее эффективных финансовых решений для модернизации производственных мощностей и оптимизации работы предприятия лизинг торгового оборудования для магазина
The fascinating story of Antonio Rudiger’s transfer https://real-madrid.antonio-rudiger-cz.com to Real Madrid and his rapid rise as a key player at one of the best clubs in the world.
The fascinating story of Marcus Rashford’s ascent https://manchester-united.marcus-rashford-cz.com to glory in the Red Devils: from a young talent to one of the key players of the team.
Сайт предлагает широкий выбор лизинговых продуктов для бизнеса, включая лизинг оборудования. Благодаря этому, компании могут получить доступ к современному оборудованию без необходимости его покупки за наличные http://rolevikionline.g-talk.ru/viewtopic.php?t=1266
augmentin amoxicillin
buy wow raid carry buy wow raid carry .
Fascinating event related to this Keanu Reeves helped him in the role of the iconic John Wick characters https://john-wick.keanu-reeves.cz, among which there is another talent who has combat smarts with inappropriate charisma.
Try to make a fascinating actor Johnny Depp https://secret-window.johnny-depp.cz, who will become the slave of his strong hero Moudriho Creeps in the thriller “Secret Window”.
Jackie Chan https://peakhour.jackie-chan.cz from a poor boy from Hong Kong to a world famous Hollywood stuntman. The incredible success story of Jackie Chan.
Follow Liam Neeson’s career https://hostage.liam-neeson.cz as he fulfills his potential as Brian Mills in the film “Taken” and becomes one of the leading stars of Hollywood action films.
Utilisez le Code promo 1xbt 2024 et profitez de l’offre VIP 1xBet de 200% jusqu’a 78 000 XOF sur les paris sportifs. Inscrivez-vous avec un code promotionnel et recevez un bonus de bienvenue. Vous pouvez utiliser l’argent du bonus pour parier sur des sports ou jouer dans des casinos en ligne. La promotion 2024 est valable pour tous les nouveaux clients.
Преимуществами покупки оборудования в лизинг для юридических лиц можно считать: Низкие затраты на получение оборудования в пользование лизинг металлообрабатывающее оборудование
Как заказать стриптиз на дом, в лофт, на мальчишник или девичник? Прежде всего выберите сами артиста из каталога и позвоните нам, или наш менеджер самостоятельно подберет Вам хорошего танцора по вашим запросам Заказать стриптиз
En utilisant le code bonus 1xbet, vous pouvez beneficier d’une augmentation de 100% en plus du bonus de bienvenue standard. Selon votre emplacement geographique, vous recevrez un bonus de 100%, 200% ou 300%, bonus 130$. Ce bonus est ensuite divise en deux parties, dont la moitie est utilisable pour les paris sportifs et l’autre moitie pour le casino. Avant de pouvoir retirer vos fonds, vous devrez jouer le montant du bonus 5 fois pour les paris sportifs combines et 30 fois pour les jeux de casino. Les nouveaux utilisateurs devront probablement verifier leur compte en fournissant un passeport ou un permis de conduire dans le cadre d’une verification KYC avant de pouvoir effectuer un retrait.
ankara seo
The inspiring story of Zendaya’s rise https://spider-man.zendaya-maree.cz, from her early roles to her blockbuster debut in Marvel Cinematic Universe.
The inspiring story of the ascent of the young actress Anya Taylor https://queensmove.anya-taylor-joy.cz to fame after her breakthrough performance in the TV series “The Queen’s Move”. Conquering new peaks.
An indomitable spirit, incredible skills and five championships – how Kobe Bryant https://losangeles-lakers.kobe-bryant.cz became an icon of the Los Angeles Lakers and the entire NBA world.
Carlos Vemola https://oktagon-mma.karlos-vemola.cz Czech professional mixed martial artist, former bodybuilder, wrestler and member Sokol.
Witness the thrilling story of Jiri Prochazka’s https://ufc.jiri-prochazka-ufc.cz rapid rise to the top of the UFC’s light heavyweight division, marked by his dynamic fighting style and relentless determination.
https://nudifyai.net/
Quelle est la mise minimale et la limite minimale de 1xBet?
Conformement aux regles du bookmaker, le depot minimum dans le bureau est de 1$.Code promo de pari gratuit 1xbet aujourd’hui La mise minimale est de 0,2 $ou l’equivalent de ce montant dans une autre monnaie de jeu.
Подарок мужчинам на 23 февраля на работе и кружка в подарочной упаковке оптом.
https://giftbox-3.ru/
Jon Jones https://ufc.jon-jones.cz a dominant fighter with unrivaled skill, technique and physique who has conquered the light heavyweight division.
An article about the triumphant 2023 Ferrari https://ferrari.charles-leclerc.cz and their star driver Charles Leclerc, who became the Formula world champion 1.
The legendary Spanish racer Fernando Alonso https://formula-1.fernando-alonso.cz returns to Formula 1 after several years.
Young Briton Lando Norris https://mclaren.lando-norris.cz is at the heart of McLaren’s Formula 1 renaissance, regularly achieving podium finishes and winning.
Activision and Call of Duty https://activision.call-of-duty.cz leading video game publisher and iconic shooter with a long history market dominance.
Звон Колокольцева
Бест Вей
Поздравляем вас, гражданин министр, соврамши!
Выступая прошлой осенью в Совете Федерации, министр внутренних дел Владимир Колокольцев рассказывал, о так называемом уголовном деле «Лайф-из-Гуд» – «Гермес» – «Бест Вей», обещал миллиарды рублей ущерба и десятки тысяч потерпевших. Пресс-служба МВД под руководством его боевой подруги Ирины Волк заявила о том, что вскрыта деятельность крупнейшей в истории России финансовой пирамиды.
Однако в уголовном деле, расследованном или, вернее сказать, изготовленном ГСУ питерского главка МВД, которое в феврале начал рассматривать Приморский районный суд Санкт-Петербурга, 282 млн рублей ущерба и 221 лицо, признанное следствием потерпевшим: никаких миллиардов и десятков тысяч потерпевших.
Министр и его Волк публично солгали – на основе информации, переданной замначальника ГСУ руководителем следственной группы полковником юстиции А.Н. Винокуровым, фактически даже руководившей СГ его заместительницей майором, а затем подполковником юстиции Е.А. Сапетовой по материалам, состряпанным опером УЭБиПК питерского главка МВД майором полиции А.Ю. Машевским, при попустительстве (или соучастии?) начальника ГСУ Негрозова и замначальника Следственного департамента федерального министерства Вохмянина. Полковник и подполковник с примерно пятого-шестого уровня иерархии МВД виляет генералом полиции Российской Федерации, постоянным членом Совета безопасности России – это позор для государства.
Так называемые потерпевшие и реально пострадавшие
Большинство «потерпевших» на суде заявляют суммы около 1–2 млн рублей, при этом в ходе судебного следствия выясняется, что они, как правило, получали немалый доход, причем, они еще и налоговые/валютные преступники, так как этот доход не декларировали. Среди «потерпевших» есть граждане, заявляющие смехотворные суммы в 50–70 тыс., то есть количество потерпевших специально накручивалось следствием. И даже с этим накручиванием удалось набрать так мало – учитывая, что у «Гермеса», по данным самого же следствия, более 200 тыс. клиентов в России, а в кооперативе «Бест Вей» – около 20 тыс. пайщиков.
То есть большинство и клиентов «Гермеса», и пайщиков кооператива не считают себя потерпевшими от деятельности этих организаций.
Судя по тысячам обращений во все инстанции, нескольким волнам митингов, прокатившихся по России, они считают себя потерпевшими от деятельности органов внутренних дел.
Ведь именно завербованный питерским УЭБиПК сисадмин российской платежной системы «Гермеса» Набойченко заблокирован и разгромил в феврале 2022 года эту платежную систему, повесив на сайте дисклеймер: «Обращайтесь в правоохранительные органы», что на месяцы прекратило вывод средств. Именно действия правоохранительных органов в отношении компании до и после затруднили вывод средств. Дело в том, что для вывода средств многими использовался механизм p2p, позволяющий не платить комиссию, то есть для вывода средств нужно, чтобы кто-то вносил средства (что, понятно, резко сократилось из-за уголовного дела) и происходил обмен. Однако этот способ не единственный, вывод средств так или иначе осуществляется.
Тысячи пайщиков кооператива тем более не считают себя потерпевшими от его деятельности – потому что именно правоохранительные органы воспрепятствовали приобретению недвижимости с помощью кооператива, а она из-за более чем двухлетнего ареста его счетов, на которых около 4 млрд рублей, не может быть приобретена по прежней цене.
Именно правоохранительные органы прямо запрещают выплаты пайщикам кооператива, решившим забрать свой пай, – даже по исполнительным листам судов. И клиентам «Гермеса», и пайщикам кооператива правоохранительными органами нанесен колоссальный ущерб – и материальный, и моральный, который они намерены взыскать с государства.
«Следователи»-преступники должны сидеть в тюрьме
Весьма скромный результат следствия МВД был достигнут откровенно преступным путем.
1. Некоторые из преступлений следствия были фактически признаны судами. 1 декабря прошлого года Приморский районный суд города Санкт-Петербурга признал незаконным, нарушающим УПК фактический отказ кооперативу в ознакомлении с материалами уголовного дела.При рассмотрении дела в суде выяснилось, что следственная группа ГСУ питерского главка МВД, формально руководимая замначальника ГСУ полковником юстиции А.Н. Винокуровым, а фактически – подполковником юстиции Е.А. Сапетовой, подделала документы. Автор подделки – Сапетова – еще в феврале была уволена из ГСУ «по собственному желанию».
Уличенная адвокатами кооператива в нарушении УПК, следственная группа составила письмо об удовлетворении ходатайства задним числом и попыталась представить дело так, что кооператив не получил письмо по своей вине. Ложь была выявлена в том числе и с помощью системы электронного документооборота питерского главка МВД.
2. Подделка документов была вынужденным преступлением для сокрытия более серьезного: незаконного содержания под стражей. Следственная группа грубо нарушила права гражданских истцов и ответчиков, потому что без этого нарушения она не успела за 30 суток до истечения предельного срока содержания четверых обвиняемых под стражей начать ознакомление обвиняемых с материалами дела –а это было единственное основание продления им срока содержания под стражей свыше предельного.
Следственная группа из-за спешки даже толком не смогла завершить следственные действия, незаконно вела параллельное расследование по «резервному» делу, но позднее, отбросив стыд, из-за отсутствия материала для составления «нужного» обвинительного заключения, незаконно продолжила расследование «основного» дела, в том числе проводила следственные действия, которые, согласно УПК, невозможны после начала ознакомления обвиняемых с материалами дела. Все эти ухищрения были необходимы для того, чтобы ни в коем случае не выпускать обвиняемых и продолжать держать их в заложниках.
3. Де-факто происходит уголовное наказание неосужденных людей – четверо подсудимых уже второй год сидят в тюрьме. При этом наказываются явно ни в чем неповинные люди – технические сотрудники «Лайф-из-Гуд»: даже если предположить, что действительно работала пирамида – что опровергается показаниями свидетелей самого обвинения, которые сообщают суду, что компания «Гермес» хорошо работала, они были довольны получаемым доходом, и проблемы начались после того, как российская платежная система компании была обрушена завербованным полицией петербургским сисадмином компании Набойченко. Все подсудимые – технические сотрудники компании «Лайф-из-Гуд» и ни к каким управленческим решениям отношения никогда не имели. Их взяли в заложники для того, чтобы они дали показания на руководство компании.
4. Еще одно преступление – заведомо подложное постановление руководителя следственной группы А.Н. Винокурова о привлечении кооператива «Бест Вей» в качестве гражданского ответчика на 16 млрд рублей, тогда как сумма ущерба в уголовном деле –282 млн, и в деле нет ни одного искового заявления – даже на 100 рублей.
5. Следствие стимулировало двух особенно активных так называемых потерпевших написать заявления о моральном ущербе на миллиард (!) рублей каждое – исключительно для ложного обоснования ареста активов кооператива, но понятно, что это ничтожные документы, так как моральный ущерб во всех случаях, не связанных с причинением смерти, присуждается российскими судами в размере не более десятков тысяч рублей.
6. Ни один из «потерпевших» не доказал обоснованность своих претензий в гражданском суде. При этом арестованы активы кооператива почти на 4 млрд рублей и активы частных лиц на такую же сумму. Это не что иное, как попытка захвата активов при участии органов внутренних дел некой заинтересованной группой клиентов «Гермеса» – необязательно из числа «потерпевших», то есть коррупционное преступление, которое упорно игнорирует ГУСБ МВД.
Механизм для такого захвата есть – это передача средств под управление Федерального общественно-государственного фонда по защите прав вкладчиков и акционеров. Понятно, почему не ограничиваются активами подсудимых и обвиняемых: этого недостаточно для удовлетворения аппетитов тех, кто стоит за заказным уголовным делом. И понятно, почему одно юридическое лицо – кооператив «Бест Вей» – незаконно пытаются привлечь к ответственности за другое – компанию «Гермес»: активы «Гермеса» – за рубежом.
7. Следствие, а теперь и прокуратура совершают еще одно преступление: незаконно удерживает средства пайщиков кооператива, отказываясь их вернуть, то есть совершают хищение.
Министр, управляемый мафией
Итак, Колокольцев публично солгал Совету Федерации, выдумав пирамиду, выдумав многомиллиардный ущерб и десятки тысяч пострадавших, он – некомпетентный руководитель, абсолютно ведомый своей камарильей, стремящейся создавать громкие пиар-истории на пустом месте и с коррупционной выгодой для себя. Он вызвал социальный протест десятков тысяч пайщиков кооператива «Бест Вей» и клиентов компании «Гермес» и членов их семей – в большинстве своем представителей социально незащищенных слоев населения, на годы лишенных возможности пользоваться своими деньгами и приобрести недвижимость, на которую они собрали средства, – в том числе десятков участников СВО. Министр вредит в тылу тем, кто защищает страну на фронте.
Глава МВД находится под влиянием или даже контролем давно ставшей притчей во языцех питерской полицейской мафии. Ликвидация этой мафии, как и ликвидация преступной, коррупционной, вредящей социально-политической стабильности системы управления МВД, со стороны Колокольцева является важнейшей государственной задачей.
seo hizmeti
villas montenegro real estate in Montenegro for sale
the most popular sports website https://sports-forecasts.com in the Arab world with the latest sports news, predictions and analysis in real time.
Latest news and analysis of the English Premier League https://epl-ar.com. Detailed descriptions of matches, team statistics and the most interesting football events.
Free movies https://www.moviesjoy.cc and TV streaming online, watch movies online in HD 1080p.
Latest Diablo news https://diablo-ar.com, detailed game descriptions and guides. Diablo.az – The largest Diablo information portal in Arabic.
Звон Колокольцева
Гермес
Поздравляем вас, гражданин министр, соврамши!
Выступая прошлой осенью в Совете Федерации, министр внутренних дел Владимир Колокольцев рассказывал, о так называемом уголовном деле «Лайф-из-Гуд» – «Гермес» – «Бест Вей», обещал миллиарды рублей ущерба и десятки тысяч потерпевших. Пресс-служба МВД под руководством его боевой подруги Ирины Волк заявила о том, что вскрыта деятельность крупнейшей в истории России финансовой пирамиды.
Однако в уголовном деле, расследованном или, вернее сказать, изготовленном ГСУ питерского главка МВД, которое в феврале начал рассматривать Приморский районный суд Санкт-Петербурга, 282 млн рублей ущерба и 221 лицо, признанное следствием потерпевшим: никаких миллиардов и десятков тысяч потерпевших.
Министр и его Волк публично солгали – на основе информации, переданной замначальника ГСУ руководителем следственной группы полковником юстиции А.Н. Винокуровым, фактически даже руководившей СГ его заместительницей майором, а затем подполковником юстиции Е.А. Сапетовой по материалам, состряпанным опером УЭБиПК питерского главка МВД майором полиции А.Ю. Машевским, при попустительстве (или соучастии?) начальника ГСУ Негрозова и замначальника Следственного департамента федерального министерства Вохмянина. Полковник и подполковник с примерно пятого-шестого уровня иерархии МВД виляет генералом полиции Российской Федерации, постоянным членом Совета безопасности России – это позор для государства.
Так называемые потерпевшие и реально пострадавшие
Большинство «потерпевших» на суде заявляют суммы около 1–2 млн рублей, при этом в ходе судебного следствия выясняется, что они, как правило, получали немалый доход, причем, они еще и налоговые/валютные преступники, так как этот доход не декларировали. Среди «потерпевших» есть граждане, заявляющие смехотворные суммы в 50–70 тыс., то есть количество потерпевших специально накручивалось следствием. И даже с этим накручиванием удалось набрать так мало – учитывая, что у «Гермеса», по данным самого же следствия, более 200 тыс. клиентов в России, а в кооперативе «Бест Вей» – около 20 тыс. пайщиков.
То есть большинство и клиентов «Гермеса», и пайщиков кооператива не считают себя потерпевшими от деятельности этих организаций.
Судя по тысячам обращений во все инстанции, нескольким волнам митингов, прокатившихся по России, они считают себя потерпевшими от деятельности органов внутренних дел.
Ведь именно завербованный питерским УЭБиПК сисадмин российской платежной системы «Гермеса» Набойченко заблокирован и разгромил в феврале 2022 года эту платежную систему, повесив на сайте дисклеймер: «Обращайтесь в правоохранительные органы», что на месяцы прекратило вывод средств. Именно действия правоохранительных органов в отношении компании до и после затруднили вывод средств. Дело в том, что для вывода средств многими использовался механизм p2p, позволяющий не платить комиссию, то есть для вывода средств нужно, чтобы кто-то вносил средства (что, понятно, резко сократилось из-за уголовного дела) и происходил обмен. Однако этот способ не единственный, вывод средств так или иначе осуществляется.
Тысячи пайщиков кооператива тем более не считают себя потерпевшими от его деятельности – потому что именно правоохранительные органы воспрепятствовали приобретению недвижимости с помощью кооператива, а она из-за более чем двухлетнего ареста его счетов, на которых около 4 млрд рублей, не может быть приобретена по прежней цене.
Именно правоохранительные органы прямо запрещают выплаты пайщикам кооператива, решившим забрать свой пай, – даже по исполнительным листам судов. И клиентам «Гермеса», и пайщикам кооператива правоохранительными органами нанесен колоссальный ущерб – и материальный, и моральный, который они намерены взыскать с государства.
«Следователи»-преступники должны сидеть в тюрьме
Весьма скромный результат следствия МВД был достигнут откровенно преступным путем.
1. Некоторые из преступлений следствия были фактически признаны судами. 1 декабря прошлого года Приморский районный суд города Санкт-Петербурга признал незаконным, нарушающим УПК фактический отказ кооперативу в ознакомлении с материалами уголовного дела.При рассмотрении дела в суде выяснилось, что следственная группа ГСУ питерского главка МВД, формально руководимая замначальника ГСУ полковником юстиции А.Н. Винокуровым, а фактически – подполковником юстиции Е.А. Сапетовой, подделала документы. Автор подделки – Сапетова – еще в феврале была уволена из ГСУ «по собственному желанию».
Уличенная адвокатами кооператива в нарушении УПК, следственная группа составила письмо об удовлетворении ходатайства задним числом и попыталась представить дело так, что кооператив не получил письмо по своей вине. Ложь была выявлена в том числе и с помощью системы электронного документооборота питерского главка МВД.
2. Подделка документов была вынужденным преступлением для сокрытия более серьезного: незаконного содержания под стражей. Следственная группа грубо нарушила права гражданских истцов и ответчиков, потому что без этого нарушения она не успела за 30 суток до истечения предельного срока содержания четверых обвиняемых под стражей начать ознакомление обвиняемых с материалами дела –а это было единственное основание продления им срока содержания под стражей свыше предельного.
Следственная группа из-за спешки даже толком не смогла завершить следственные действия, незаконно вела параллельное расследование по «резервному» делу, но позднее, отбросив стыд, из-за отсутствия материала для составления «нужного» обвинительного заключения, незаконно продолжила расследование «основного» дела, в том числе проводила следственные действия, которые, согласно УПК, невозможны после начала ознакомления обвиняемых с материалами дела. Все эти ухищрения были необходимы для того, чтобы ни в коем случае не выпускать обвиняемых и продолжать держать их в заложниках.
3. Де-факто происходит уголовное наказание неосужденных людей – четверо подсудимых уже второй год сидят в тюрьме. При этом наказываются явно ни в чем неповинные люди – технические сотрудники «Лайф-из-Гуд»: даже если предположить, что действительно работала пирамида – что опровергается показаниями свидетелей самого обвинения, которые сообщают суду, что компания «Гермес» хорошо работала, они были довольны получаемым доходом, и проблемы начались после того, как российская платежная система компании была обрушена завербованным полицией петербургским сисадмином компании Набойченко. Все подсудимые – технические сотрудники компании «Лайф-из-Гуд» и ни к каким управленческим решениям отношения никогда не имели. Их взяли в заложники для того, чтобы они дали показания на руководство компании.
4. Еще одно преступление – заведомо подложное постановление руководителя следственной группы А.Н. Винокурова о привлечении кооператива «Бест Вей» в качестве гражданского ответчика на 16 млрд рублей, тогда как сумма ущерба в уголовном деле –282 млн, и в деле нет ни одного искового заявления – даже на 100 рублей.
5. Следствие стимулировало двух особенно активных так называемых потерпевших написать заявления о моральном ущербе на миллиард (!) рублей каждое – исключительно для ложного обоснования ареста активов кооператива, но понятно, что это ничтожные документы, так как моральный ущерб во всех случаях, не связанных с причинением смерти, присуждается российскими судами в размере не более десятков тысяч рублей.
6. Ни один из «потерпевших» не доказал обоснованность своих претензий в гражданском суде. При этом арестованы активы кооператива почти на 4 млрд рублей и активы частных лиц на такую же сумму. Это не что иное, как попытка захвата активов при участии органов внутренних дел некой заинтересованной группой клиентов «Гермеса» – необязательно из числа «потерпевших», то есть коррупционное преступление, которое упорно игнорирует ГУСБ МВД.
Механизм для такого захвата есть – это передача средств под управление Федерального общественно-государственного фонда по защите прав вкладчиков и акционеров. Понятно, почему не ограничиваются активами подсудимых и обвиняемых: этого недостаточно для удовлетворения аппетитов тех, кто стоит за заказным уголовным делом. И понятно, почему одно юридическое лицо – кооператив «Бест Вей» – незаконно пытаются привлечь к ответственности за другое – компанию «Гермес»: активы «Гермеса» – за рубежом.
7. Следствие, а теперь и прокуратура совершают еще одно преступление: незаконно удерживает средства пайщиков кооператива, отказываясь их вернуть, то есть совершают хищение.
Министр, управляемый мафией
Итак, Колокольцев публично солгал Совету Федерации, выдумав пирамиду, выдумав многомиллиардный ущерб и десятки тысяч пострадавших, он – некомпетентный руководитель, абсолютно ведомый своей камарильей, стремящейся создавать громкие пиар-истории на пустом месте и с коррупционной выгодой для себя. Он вызвал социальный протест десятков тысяч пайщиков кооператива «Бест Вей» и клиентов компании «Гермес» и членов их семей – в большинстве своем представителей социально незащищенных слоев населения, на годы лишенных возможности пользоваться своими деньгами и приобрести недвижимость, на которую они собрали средства, – в том числе десятков участников СВО. Министр вредит в тылу тем, кто защищает страну на фронте.
Глава МВД находится под влиянием или даже контролем давно ставшей притчей во языцех питерской полицейской мафии. Ликвидация этой мафии, как и ликвидация преступной, коррупционной, вредящей социально-политической стабильности системы управления МВД, со стороны Колокольцева является важнейшей государственной задачей.
Latest World of Warcraft tournament news https://ar-wow.com (WOW), strategies and game analysis. The most detailed gaming portal in Arabic.
The latest analysis, reviews of https://spider-man-ar.com tournaments and the most interesting things from the “Spider-Man” series of games in Azerbaijani language. It’s all here!
NFL https://nfl-ar.com News, analysis and topics about the latest practices, victories and records. A portal that explores the most beautiful games in the NFL world in general.
Discover exciting virtual football https://fortnite-ar.com in Fortnite. Your central hub for the latest news, expert strategy and exciting eSports reporting.
Latest Counter-Strike 2 news https://counter-strike-ar.com, watch the most successful tournaments and be the best in the gaming world on CS2 ar.
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
can i order cipro online
1 x code promo de pari. Utilisez – le lors de votre inscription pour obtenir un bonus de 100% jusqu’a 130$. Pour obtenir des bonus du bookmaker 1xbet, vous devez remplir certaines conditions, mais les codes promotionnels vous permettent de les obtenir beaucoup plus facilement. La taille des bonus disponibles pour les joueurs via les codes promotionnels 1xBet peut etre petite, mais meme un petit bonus peut augmenter considerablement le potentiel de jeu du client.
Latest boxing news, achievements of Raisol Abbasov https://boxing-ar.com, Tyson Fury fights and much more. It’s all about the boxing ambassador.
Latest news from the world of boxing https://boks-uz.com, achievements of Resul Abbasov, Tyson Fury’s fights and much more. Everything Boxing Ambassador has.
Latest GTA game news https://gta-uzbek.com, tournaments, guides and strategies. Stay tuned for the best GTA gaming experience
Lorem Ipsum has been the industry’s standard dummy text https://buytron.co.za/hlefggt of type and scrambled it to make a type specimen book.
https://cyprusrent.ru/
Lorem Ipsum has been the industry’s standard dummy text https://mateuszglanert.pl/rybvt of type and scrambled it to make a type specimen book.
Explore the extraordinary journey of Kylian Mbappe https://mbappe-real-madrid.com, from his humble beginnings to global stardom.
Latest news about Pele https://mesut-ozil-uz.com, statistics, photos and much more. Get the latest news and information about football legend Pele.
Lorem Ipsum has been the industry’s standard dummy text https://sofiaporelmundo.es/oigaf of type and scrambled it to make a type specimen book.
Get the latest https://mesut-ozil-uz.com Mesut Ozil news, stats, photos and more.
Serxio Ramos Garsiya https://serxio-ramos.com ispaniyalik futbolchi, himoyachi. Ispaniya terma jamoasining sobiq futbolchisi. 16 mavsum davomida u “Real Madrid”da markaziy himoyachi sifatida o’ynadi.
Ronaldo de Asis Moreira https://ronaldinyo.com braziliyalik futbolchi, yarim himoyachi va hujumchi sifatida o’ynagan. Jahon chempioni (2002). “Oltin to’p” sovrindori (2005).
Lorem Ipsum has been the industry’s standard dummy text https://marielabertuggia.es/fhfyzk of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://btelectricshop.es/gppnjk of type and scrambled it to make a type specimen book.
Официальный сайт онлайн-казино Vavada https://vavada-kz-game.kz это новый адрес лучших слотов и джекпотов. Ознакомьтесь с бонусами и играйте на реальные деньги из Казахстана.
Marcus Lilian Thuram-Julien https://internationale.marcus-thuram-fr.com French footballer, forward for the Internazionale club and French national team.
Legendary striker Cristiano Ronaldo https://an-nasr.cristiano-ronaldo-fr.com signed a contract with the Saudi club ” An-Nasr”, opening a new chapter in his illustrious career in the Middle East.
Manchester City and Erling Haaland https://manchester-city.erling-haaland-fr.com explosive synergy in action. How a club and a footballer light up stadiums with their dynamic play.
Lionel Messi https://inter-miami.lionel-messi-fr.com legendary Argentine footballer, announced his transfer to the American club Inter Miami.
https://rik-estate.ru/
Top Email Icon Packs for Modern Web Design in 2024. Safari Icon: Comprehensive Guide for Designers and Web Developers https://www.storeboard.com/blogs/social-media/top-icon-sets-for-modern-web-design/5803950
Lorem Ipsum has been the industry’s standard dummy text https://aptekacalcium.pl/opirqdh of type and scrambled it to make a type specimen book.
ison.geor4@gmail.com
http://remontwasher.ru/
Lorem Ipsum has been the industry’s standard dummy text https://20miles.es/alwnnq of type and scrambled it to make a type specimen book.
We’ve all made email marketing mistakes: You click send on an email and suddenly your stomach drops. You’ve made a mistake and there’s nothing you can do about it Crastos, Vidais, Portugal
accutane pills online
1xBet offre precisement cela et vos bonus peuvent etre maximises en utilisant le promo de morue 1xbet 2024. Consultez simplement ci-dessous pour decouvrir ce qui vous attend en tant que nouveau client sur ce site de paris. Grace a ces connaissances, il est tout a fait logique de s’attendre a une serie de bonus de bienvenue attrayants pour les nouveaux joueurs provenant d’autres pays. Voici quelques exemples de ces pays : Burkina Faso, Ghana, Ouganda, Zambie, Cameroun, Senegal, Benin, Congo, Guinee, Cote d’Ivoire, Togo, Mali, etc.
Lorem Ipsum has been the industry’s standard dummy text https://rasendisseny.es/xjbfw of type and scrambled it to make a type specimen book.
The official website where you can find everything about the career of Gianluigi Buffon https://gianluigi-buffon.com. Discover the story of this legendary goalkeeper who left his mark on football history and relive his achievements and unforgettable memories with us.
1xBet offre precisement cela et vos bonus peuvent etre maximises en utilisant le Code promotionnel 1x pari 2024. Consultez simplement ci-dessous pour decouvrir ce qui vous attend en tant que nouveau client sur ce site de paris. Grace a ces connaissances, il est tout a fait logique de s’attendre a une serie de bonus de bienvenue attrayants pour les nouveaux joueurs provenant d’autres pays. Voici quelques exemples de ces pays : Burkina Faso, Ghana, Ouganda, Zambie, Cameroun, Senegal, Benin, Congo, Guinee, Cote d’Ivoire, Togo, Mali, etc.
Website dedicated to football player Paul Pogba https://pogba-uz.com. Latest news from the world of football.
Welcome to our official website! Go deeper into Paulo Dybala’s https://paulo-dybala.com football career. Discover Dybala’s unforgettable moments, amazing talents and fascinating journey in the world of football on this site.
Lorem Ipsum has been the industry’s standard dummy text https://conceptshop.es/jgfrd of type and scrambled it to make a type specimen book.
Coffeeroom https://coffeeroom.by – магазин кофе, чая, кофетехники, посуды, химии и аксессуаров в Минске для дома и офиса.
Latest news on the Vinicius Junior fan site https://vinisius-junior.com. Vinicius Junior has been playing since 2018 for Real Madrid (Real Madrid). He plays in the Left Winger position.
Lorem Ipsum has been the industry’s standard dummy text https://buytron.co.za/bngzfb of type and scrambled it to make a type specimen book.
Qu’est-ce que la strategie de jeu?
La strategie de jeu est un algorithme d’action que le joueur doit suivre en faisant un pari. Les actions peuvent inclure la taille du pari, le montant des cotes, la duree de la serie de Paris.code promo 1xbet pour l’inscription L’objectif principal de toute strategie est d’obtenir des gains qui seront en mesure de compenser toutes les depenses precedentes.
Прокат и аренда автомобилей https://autorent.by в Минске 2019-2022. Сутки от 35 руб.
In a world where communication is key, having a reliable phone number is essential for both personal and business interactions. However, not everyone needs a permanent number, especially when privacy, convenience, and flexibility are at stake https://fr.kompass.com/p/kompass-posts/ua103618/l-importance-d-avoir-un-numero-de-telephone-belge-pour-les-affaires/6ef54021-ce5a-418b-915d-3178160a23c4
Find the latest information on Khabib Nurmagomedov https://khabib-nurmagomedov.uz news and fights. Check out articles and videos detailing Khabib UFC career, interviews, wins, and biography.
Latest news and information about Marcelo https://marselo-uz.com on this site! Find Marcelo’s biography, career, game stats and more.
Lorem Ipsum has been the industry’s standard dummy text https://cosavedereinungiorno.it/ljjnyu of type and scrambled it to make a type specimen book.
purchase doxycycline online uk
Lorem Ipsum has been the industry’s standard dummy text https://chiaradventure.it/nakqpbe of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://convido.es/rejirsw of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://chiaradventure.it/dccpjqr of type and scrambled it to make a type specimen book.
Good day! I could have sworn I’ve been to this blog before but after browsing through some of the articles I realized it’s new to me. Anyhow, I’m definitely happy I discovered it and I’ll be bookmarking it and checking back often.
A Charm regarding Premium Fashion
Style aficionados as well as premium buyers often find themselves fascinated by an grace as well as prestige concerning premium fashion. From the complex aspects of a Hermes Birkin to a emblematic style concerning one Chanel 2.55, these goods represent more than just simply fashion—they represent a good certain standing as well as exclusivity. Nonetheless, not everyone might have the funds for to spend lavishly upon those premium products, that will has brought to a growing trend concerning replica handbags. For a lot of, those replicas give a manner towards enjoy a beauty of high style layouts with out busting an traditional bank.
An rise in recognition regarding fake purses offers opened up a great fascinating dialogue regarding dress, honesty, as well as exclusive style. In this blog article, we all will analyze a different facets of a trend, supplying fashion fans together with an extensive handbook for fake bags. By a finale, you can possess the information to create advised choices which align together with your values and looks.
Honorable and Legitimate Considerations regarding Fake Bags
When the idea comes to fake bags, one concerning a most pressing concerns will be a moral and legitimate effects. The manufacturing plus sale of fake products usually are illegal inside a lot of places, while that infringes rational property legal rights. This certainly not just impacts the earnings regarding premium models but also increases questions concerning the problems below which these replicas are produced.
Coordinating plus Incorporating Fake Purses
Incorporating replica purses into your wardrobe could prove both trendy trendy and ethical. A single method is to to combine premium replicas with authentic pieces & other sustainable eco-friendly style items. Such an approach doesn’t only elevate improves a overall look but also additionally promotes encourages a sustainable style movement.
When fashioning imitation bags, consider your event setting and a attire. An elegant timeless replica bag may insert a hint of sophistication to a a dressy attire, whereas a trendy pattern could make an informal appearance trendier. Do not be afraid to try with different various trends and add-ons to create a unique plus custom look.
Moreover, caring for fake purses is key key to keep their look condition & durability. Routine washing and appropriate storage can help keep your your bags seeming pristine & trendy for a longer time.
The Value of knowledgeable Buyer Selections
In today’s today’s fashion environment, educated consumer choices are more more important significant than ever before. Though fake handbags provide an affordable alternative for luxury designer pieces, it key to consider the principled & lawful implications. By remaining aware about where and plus how to one buys imitations, you can can enjoy high-end fashion while staying true to one’s values principles.
It’s additionally essential to keep in mind that personal personal style is not defined by the brand labels or cost cost labels. Whether you you choose to invest on authentic authentic high-end goods or explore the realm of fake bags, the secret is to find articles that help one feel self-assured & fashionable.
Conclusion
Fake purses have found out a special place in the fashion world, offering a budget-friendly plus accessible option to luxury luxury items. While they arrive bring with their own their own own series of of moral
Related Style Topics
Exploring the realm of style doesn’t finish with replica handbags. Here are some further related subjects that could intrigue you:
Sustainable Apparel
Delve into the significance of green practices in the style field. Discover about sustainable materials, principled fabrication methods, and how to create a eco-friendly closet.
Retro and Second-Hand Fashion
Uncover the appeal of vintage and thrift garments. Learn how to source premium classic items, the advantages of pre-owned style, and tips for integrating these items into your current closet.
Homemade Fashion and Repurposing
Become innovative with Do-It-Yourself apparel projects and repurposing previous garments. Acquire useful tips on changing your closet by creating your own adornments or modifying existing items to grant them a renewed purpose.
Apparel on a Dime
Learn how to stay fashionable without surpassing the savings. Explore strategies for securing fantastic offers, buying wisely during sales, and get your apparel budget.
Capsule Closets
Grasp the concept of a minimalist collection—assembling a group of essential, multi-purpose items that can be matched and coordinated to form different looks. Analyze the advantages of this simple approach and how to implement it.
Fashion Movements and Projecting
Keep ahead of the trend by discovering future style trends and industry forecasts. Learn about trendsetting designers, influential fashion shows, and the most recent essential articles.
Apparel and Tech
Investigate how tech is transforming the fashion sector. Topics include smart materials, online fitting rooms, apparel apps, and the impact of social networks on fashion promotion and consumer habits.
Body Acceptance and Fashion
Investigate the relationship between style and figure positivity. Understand about brands advocating all-encompassing sizing, the significance of depiction in style outlets, and how to outfit for different body types.
Style Heritage
Embark on a trip through the heritage of fashion. Uncover different periods, iconic style trends, and how past fashions continue to shape current style.
Style Photography and Writing
Delve into the world of fashion photography and writing. Get advice on how to get beautiful apparel shots, begin your own apparel blog, and increase your visibility online.
Discover how Riyad Mahrez https://al-ahli.riyad-mahrez.com transformed Al-Ahli, becoming a key player and catalyst in reaching new heights in world football.
Find the latest information on Conor McGregor https://conor-mcgregor.uz news, fights, and interviews. Check out detailed articles and news about McGregor’s UFC career, wins, training, and personal life.
Explore the dynamic world of sports https://noticias-esportivas-br.org through the lens of a sports reporter. Your source for breaking news, exclusive interviews, in-depth analysis and live coverage of all sports.
Get to know the history, players and latest news of the Inter Miami football club https://inter-miami.uz. Join us to learn about the successes and great performances of America’s newest and most exciting soccer club.
A site dedicated to Michael Jordan https://michael-jordan.uz, a basketball legend and symbol of world sports culture. Here you will find highlights, career, family and news about one of the greatest athletes of all time.
https://redstoneestate.ru/
https://med-blesk.ru
https://nsdentalsolution.com
The latest top football news https://futebol-ao-vivo.net today. Interviews with football players, online broadcasts and match results, analytics and football forecasts
Site with the latest news, statistics, photos of Pele https://edson-arantes-do-nascimento.com and much more. Get the latest news and information about football legend Pele.
Welcome to our official website, where you will find everything about the career of Gianluigi Buffon https://gianluigi-buffon.org. Discover the story of this legendary goalkeeper who made football history.
If you are a fan of UFC https://ufc-hoje.com the most famous organization in the world, come visit us. The most important news and highlights from the UFC world await you on our website.
Lorem Ipsum has been the industry’s standard dummy text https://platformzelfredzaam.nl/notvkm of type and scrambled it to make a type specimen book.
An Attraction of High-End Dress
Fashion aficionados and premium consumers usually locate themselves fascinated through the elegance as well as renown concerning high-end dress. From an complex aspects concerning an Hermes Birkin up to a emblematic style concerning a Chanel 2.55, those items signify more than merely dress—many people stand for a good certain position plus uniqueness. However, not everyone else may pay for to spend lavishly with those luxury products, which provides brought towards an increasing pattern concerning imitation purses. Regarding many, these particular replicas give a approach to benefit from the splendor concerning high-fashion designs without damaging the bank.
A surge within popularity regarding fake bags has opened up a great fascinating conversation concerning fashion, honesty, as well as individual fashion. Within a weblog content, most of us can investigate a different aspects of a movement, offering fashion enthusiasts along with an comprehensive manual to imitation bags. Through a end, you may own an understanding for you to help make advised choices which line up with the beliefs as well as aesthetics.
Ethical plus Lawful Considerations concerning Imitation Bags
As soon as it relates to imitation bags, one concerning the many demanding concerns will be an ethical and legal effects. An generation and purchase concerning imitation products tend to be illegal in numerous places, while that infringes intellectual property rights. This not solely impacts a earnings of luxury models but in addition increases inquiries regarding an problems beneath which these fakes tend to be developed.
Coordinating & Incorporating Fake Bags
Integrating imitation bags into your one’s collection may be both stylish trendy also ethical. A method is to mixing top-quality imitations with authentic authentic pieces and other green fashion pieces. This not only enhance improves one’s total style but also also promotes promotes an eco-friendly apparel movement.
When styling fake handbags, think about your event event & one’s outfit. An elegant classic replica bag can insert a element of grace to a formal ensemble, whereas a trendy pattern could make a relaxed look trendier. Do not become scared to try w/different various styles plus accoutrements to develop an original and tailored appearance.
Moreover, caring for your imitation handbags is crucial vital to keep their appearance appearance & lifespan. Regular washing & proper keeping could help keep a handbags seeming pristine & fashionable for longer.
The Significance of Informed Customer Selections
In the current modern style scene, informed consumer choices are more important crucial than. Although replica handbags give an affordable substitute for luxury high-end items, it’s key to consider the moral plus legitimate repercussions. By remaining aware of where plus how you you purchase fakes, you can relish luxury apparel while staying true to your principles.
It’s also essential to keep in mind that one’s unique style is not defined by brand labels or cost cost tags. Whether or not you one opts to invest on authentic real high-end goods or explore the realm of replica handbags, the ultimate goal is to find to find items that make you self-assured plus stylish.
Final Thoughts
Imitation bags have found a distinct distinct niche in the fashion style industry, providing an affordable and attainable alternative to luxury high-end items. Though they arrive come with their own unique series of of ethical
Associated Fashion Themes
Exploring the world of fashion doesn’t conclude with imitation handbags. Here are some additional associated themes that might interest you:
Sustainable Style
Dive into the significance of green practices in the style sector. Discover about sustainable fabrics, moral production methods, and how to construct a green closet.
Vintage and Second-Hand Apparel
Uncover the allure of vintage and second-hand apparel. Discover how to get premium classic items, the perks of second-hand apparel, and advice for including these articles into your contemporary closet.
DIY Style and Repurposing
Be imaginative with Do-It-Yourself apparel activities and upcycling old clothes. Gain useful advice on transforming your closet by making your own adornments or personalizing present items to give them a new existence.
Apparel on a Budget
Discover how to be fashionable without exceeding the savings. Investigate strategies for finding fantastic deals, shopping wisely during sales, and get your apparel funds.
Minimalist Collections
Grasp the notion of a capsule wardrobe—creating a group of essential, multi-purpose items that can be matched and coordinated to make different ensembles. Analyze the benefits of this minimalist method and how to implement it.
Apparel Trends and Predicting
Keep ahead of the movement by investigating upcoming apparel tendencies and field predictions. Discover about trendsetting creators, pivotal apparel events, and the newest essential items.
Fashion and Innovation
Explore how innovation is revolutionizing the apparel field. Topics involve advanced textiles, online try-ons, style tools, and the impact of social networks on style promotion and consumer actions.
Figure Positivity and Style
Examine the relationship between fashion and figure acceptance. Discover about brands promoting inclusive sizing, the importance of inclusion in fashion publications, and how to style for different shapes.
Fashion Legacy
Begin a journey through the heritage of fashion. Discover diverse eras, famous style movements, and how historical designs remain to affect contemporary style.
Style Photography and Blogs
Delve into the world of style photography and writing. Gain advice on how to take beautiful style shots, begin your own fashion journal, and expand your visibility on social media.
The best site dedicated to the football player Paul Pogba https://pogba.org. Latest news from the world of football.
Lorem Ipsum has been the industry’s standard dummy text https://investeringsgronden.nl/dirusec of type and scrambled it to make a type specimen book.
Qu’est-ce que la strategie de jeu?
La strategie de jeu est un algorithme d’action que le joueur doit suivre en faisant un pari. Les actions peuvent inclure la taille du pari, le montant des cotes, la duree de la serie de Paris.c’est quoi le code promo dans 1xbet L’objectif principal de toute strategie est d’obtenir des gains qui seront en mesure de compenser toutes les depenses precedentes.
Vinicius Junior https://vinicius-junior.org all the latest current and latest news for today about the player of the 2024 season
Analysis of Arsenal’s impressive revival https://arsenal.bukayo-saka.biz under the leadership of Mikel Arteta and the key role of young star Bukayo Saki in the club’s return to the top.
Gavi’s success story https://barcelona.gavi-fr.com at Barcelona: from his debut at 16 to a key role in club and national team of Spain, his talent inspires the world of football.
https://romashkaclinic.ru
Pedri’s story https://barcelona.pedri-fr.com from his youth in the Canary Islands to becoming a world-class star in Barcelona, ??with international success and recognition.
https://psy-medcentr.ru
Lorem Ipsum has been the industry’s standard dummy text https://blogn97.pl/oqmfza of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://pizzartist.it/fxwim of type and scrambled it to make a type specimen book.
Tributes flood in for BBC sport commentator whose wife and daughters were killed in suspected crossbow attack
порно секс жесток
Figures from across the United Kingdom have offered their condolences to a BBC sport commentator, after his wife and two daughters were killed by an alleged crossbow attacker, in deaths that again drew attention to the epidemic of violence against women.
Carol Hunt, 61, wife of BBC horse racing commentator, John Hunt, and their daughters, Hannah Hunt, 28, and Louise Hunt, 25, died from injuries sustained in an attack in Bushey, just northwest of London, on Tuesday, according to police and Britain’s public broadcaster.
A 26-year-old suspect wanted in connection with the killings, and named as Kyle Clifford, was found by British police in Enfield, north London, on Wednesday, following a sprawling manhunt. There were no previous reports to the force over Clifford, who is in serious condition in hospital and is yet to speak with officers, Hertfordshire Police said in a statement.
A crossbow was recovered as part of the investigation, which police believe was used in a “targeted incident.”
Epidemic of violence against women
The killings of the three women rocked Britain, where mass murders are infrequent but violence against women and girls has been officially labeled as a national threat.
A woman is killed by a man every three days in the UK and one in four women will experience domestic violence in her lifetime, the United Nations’ special rapporteur on violence against women and girls, Reem Alsalem, said earlier this year.
Charities and human rights organizations have subsequently reiterated urgent demands to tackle femicide in the UK.
Lorem Ipsum has been the industry’s standard dummy text https://prawo4business.pl/lyegv of type and scrambled it to make a type specimen book.
Discover the journey of Charles Leclerc https://ferrari.charles-leclerc-fr.com, from young Monegasque driver to Ferrari Formula 1 leader, from his early years to his main achievements within the team.
Lorem Ipsum has been the industry’s standard dummy text https://amaloquehaces.es/zdoch of type and scrambled it to make a type specimen book.
Discover Pierre Gasly’s https://alpine.pierre-gasly.com journey through the world of Formula 1, from his beginnings with Toro Rosso to his extraordinary achievements with Alpine.
Discover the story of Rudy Gobert https://minnesota-timberwolves.rudy-gobert.biz, the French basketball player whose defensive play and leadership transformed the Minnesota Timberwolves into a powerhouse NBA team.
From childhood teams to championship victories, the path to success with the Los Angeles Lakers https://los-angeles-lakers.lebron-james-fr.com requires not only talent, but also undeniable dedication and work.
Leroy Sane’s https://bavaria.leroy-sane-ft.com success story at FC Bayern Munich: from adaptation to influence on the club’s results. Inspiration for hard work and professionalism in football.
https://novomed-cardio.ru
Специализация компании ООО «АвтоПрайм» предоставляет в аренду автовышки и другую спецтехнику для проведения самых различных высотных работ — прокладки линий электропередач, клининга, отделки фасадов, монтажа конструкций и многих других. Мы предлагаем в аренду на выгодных условиях Здесь
The Allure regarding High-End Fashion
Style enthusiasts as well as luxury buyers frequently discover themselves captivated via the grace and status concerning luxury fashion. From a complex features concerning a Hermes Birkin to the iconic design of one Chanel 2.55, these particular goods signify more than merely dress—these individuals represent an excellent particular position and exclusiveness. Nonetheless, definitely not everyone else can pay for to shell out on these luxury products, which provides led towards an increasing pattern of imitation purses. For numerous, those fakes offer a manner towards take pleasure in a splendor concerning high-fashion layouts with out breaking a traditional bank.
An increase in recognition regarding fake bags has opened up an interesting conversation about fashion, ethics, as well as exclusive style. Within a blog content, we will analyze an numerous facets of this pattern, supplying dress enthusiasts together with one detailed handbook for fake bags. Through a conclusion, you may have an knowledge to create advised decisions that will line up together with ones beliefs plus aesthetics.
Honorable and Lawful Concerns concerning Fake Purses
As soon as that relates to replica handbags, 1 concerning the many pressing problems will be a moral and legitimate effects. An production plus selling of fake products usually are unlawful inside numerous nations, because the idea infringes mental property rights. This certainly not just has an effect on a profits concerning premium models but in addition increases inquiries concerning an problems under that these replicas usually are made.
Styling and Incorporating Fake Purses
Integrating imitation purses within one’s collection can be both stylish also principled. A single approach is to mix high-quality replicas with authentic authentic articles plus other sustainable eco-friendly style pieces. Such an approach doesn’t only elevate elevates one’s overall appearance yet additionally promotes encourages an eco-friendly fashion movement.
Whenever coordinating imitation purses, reflect on the occasion event & your outfit. An elegant classic replica handbag could bring a element of grace for a a dressy outfit, whilst a fashionable style could turn a relaxed look trendier. Never be afraid to play with different trends and accessories to develop an original & custom style.
Moreover, caring for your replica purses is crucial to preserve their condition plus durability. Consistent cleaning and proper keeping may assist keep your handbags seeming new and trendy for.
The significance Value of Informed Customer Selections
In the current modern apparel landscape, informed buyer decisions are more more important significant than ever before. While fake purses give a budget-friendly alternative to luxury items, it key to reflect on the principled plus lawful repercussions. By being conscious about where and and how you buy replicas, you can enjoy high-end apparel while staying loyal to one’s values beliefs.
It’s equally crucial to remember that personal taste isn’t defined defined by name names or cost cost tags. Whether you you opt to spend in authentic high-end pieces or explore explore the world of imitation handbags, the ultimate goal is finding finding pieces that help one feel confident & trendy.
Wrap-Up
Imitation bags have found a unique special spot in the style industry, giving a budget-friendly plus reachable substitute to luxury designer goods. Though they arrive bring with their own their unique series of of moral
Associated Fashion Topics
Exploring the world of apparel doesn’t conclude with imitation bags. Here are some additional connected themes that could attract you:
Sustainable Style
Dive into the importance of eco-friendliness in the fashion industry. Understand about green fabrics, principled manufacturing practices, and how to build a green closet.
Retro and Second-Hand Style
Uncover the appeal of retro and pre-owned garments. Discover how to source quality retro articles, the perks of thrift fashion, and suggestions for integrating these pieces into your contemporary wardrobe.
Homemade Fashion and Recycling
Become imaginative with DIY apparel projects and recycling used clothes. Acquire hands-on tips on transforming your collection by crafting your own accessories or personalizing existing items to grant them a new purpose.
Fashion on a Budget
Learn how to stay trendy without exceeding the bank. Investigate tips for securing fantastic offers, shopping wisely during discounts, and get your fashion budget.
Compact Collections
Comprehend the notion of a compact wardrobe—assembling a collection of important, adaptable articles that can be mixed and paired to make various ensembles. Analyze the benefits of this streamlined method and how to adopt it.
Style Movements and Forecasting
Keep forward of the trend by discovering upcoming style movements and industry projections. Discover about trendsetting creators, pivotal apparel weeks, and the most recent must-have articles.
Fashion and Tech
Investigate how innovation is changing the apparel sector. Subjects involve smart textiles, digital try-ons, fashion apps, and the impact of social networks on apparel marketing and consumer habits.
Physique Positivity and Style
Investigate the link between apparel and figure positivity. Learn about companies advocating inclusive measurements, the importance of inclusion in fashion publications, and how to dress for various figures.
Apparel Heritage
Begin a trip through the legacy of apparel. Uncover diverse periods, legendary apparel trends, and how historical designs remain to influence contemporary style.
Style Snapshots and Blogs
Delve into the world of style photos and blogging. Get tips on how to take amazing apparel images, begin your own fashion blog, and increase your reach online.
Lorem Ipsum has been the industry’s standard dummy text https://coverly.co.za/apwsos of type and scrambled it to make a type specimen book.
Tributes flood in for BBC sport commentator whose wife and daughters were killed in suspected crossbow attack
гей член
Figures from across the United Kingdom have offered their condolences to a BBC sport commentator, after his wife and two daughters were killed by an alleged crossbow attacker, in deaths that again drew attention to the epidemic of violence against women.
Carol Hunt, 61, wife of BBC horse racing commentator, John Hunt, and their daughters, Hannah Hunt, 28, and Louise Hunt, 25, died from injuries sustained in an attack in Bushey, just northwest of London, on Tuesday, according to police and Britain’s public broadcaster.
A 26-year-old suspect wanted in connection with the killings, and named as Kyle Clifford, was found by British police in Enfield, north London, on Wednesday, following a sprawling manhunt. There were no previous reports to the force over Clifford, who is in serious condition in hospital and is yet to speak with officers, Hertfordshire Police said in a statement.
A crossbow was recovered as part of the investigation, which police believe was used in a “targeted incident.”
Epidemic of violence against women
The killings of the three women rocked Britain, where mass murders are infrequent but violence against women and girls has been officially labeled as a national threat.
A woman is killed by a man every three days in the UK and one in four women will experience domestic violence in her lifetime, the United Nations’ special rapporteur on violence against women and girls, Reem Alsalem, said earlier this year.
Charities and human rights organizations have subsequently reiterated urgent demands to tackle femicide in the UK.
Code promo 1xbet aujourd’huit utilisez le code bonus pour obtenir un bonus VIP de 100% jusqu’a 130€ pour les Paris sportifs, ainsi qu’un bonus de casino de 1950 € + 150 tours de machines a sous. En utilisant le code promotionnel, vous pouvez vous attendre a ce que vos gains soient aussi eleves que dans le cas du plus grand bookmaker 1xbet. Tous les joueurs des pays suivants peuvent utiliser le code lors de l’inscription et recevoir un bonus de bienvenue:
Lorem Ipsum has been the industry’s standard dummy text https://goglernet.dk/etzilrr of type and scrambled it to make a type specimen book.
Apres le paiement, le code promo 1xbet pour bonus devient disponible et peut etre active par le joueur a tout moment. Il y a beaucoup d’offres dans la vitrine des codes promotionnels. Dans la plupart des cas, ils couvrent la section du casino, mais souvent dans la vitrine sont publies des codes interessants pour la Conclusion a des conditions preferentielles des Paris Express, pour obtenir un cashback pour les Paris perdus. La vitrine est mise a jour assez souvent.
Le code promo sport 1xbet vous offre un bonus de bienvenue pour une simple inscription allant jusqu’a 130 $. Copiez simplement le code promotionnel et utilisez-le lors de l’inscription. Ceci est la version la plus volumineuse de l’enregistrement, cependant, c’est l’enregistrement complet et ouvre le joueur un acces complet aux fonctionnalites de la plate-forme de jeu.
Lorem Ipsum has been the industry’s standard dummy text https://decalsgroup.in/dunkm of type and scrambled it to make a type specimen book.
The story of the Moroccan footballer https://al-hilal.yassine-bounou.com, who became a star at Al-Hilal, traces his journey from the streets of Casablanca to international football stardom and his personal development.
Victor Wembanyama’s travel postcard https://san-antonio-spurs.victor-wembanyama.biz from his career in France to his impact in the NBA with the San Antonio Spurs.
Neymar https://al-hilal.neymar-fr.com at Al-Hilal: his professionalism and talent inspire young people players, taking the club to new heights in Asian football.
В сфере азартных игр в интернете особенно важны аспекты защиты данных и обеспечения надежности операций. Это ключевые аспекты, на которых строятся доверие игроков и успешная работа платформ http://dianov.bget.ru/forum/thread58241.html#1296237
The history of Michael Jordan’s Chicago Bulls https://chicago-bulls.michael-jordan-fr.com extends from his rookie in 1984 to a six-time NBA championship.
Golden State Warriors success story https://golden-state-warriors.stephen-curry-fr.com Stephen Curry: From becoming a leader to creating a basketball dynasty that redefined the game.
An Charm of Premium Style
Dress aficionados plus luxury buyers usually find themselves enthralled via a sophistication as well as renown of high-end fashion. From a detailed details of one Hermes Birkin to the legendary design regarding an Chanel 2.55, these particular products signify more than just merely style—they symbolize a good specific position and exclusivity. Nevertheless, definitely not everyone can have the funds for to spend lavishly on these particular luxury items, which provides brought up to a rising movement of fake purses. Regarding many, those replicas give a approach to enjoy an beauty regarding high style styles devoid of breaking a loan provider.
An rise within popularity of imitation handbags offers opened up a great intriguing dialogue about style, honesty, plus exclusive style. Within a website post, we may explore a numerous aspects concerning a trend, providing style aficionados along with a detailed handbook to fake handbags. Simply by the conclusion, you may possess an knowledge to make advised judgments which align with the beliefs and looks.
Ethical plus Legal Considerations regarding Imitation Handbags
As soon as that pertains to replica purses, one regarding a most pressing problems can be the honorable as well as legal implications. The production as well as sale regarding counterfeit goods are illegal inside a lot of nations, because it violates intellectual property privileges. That not solely has an effect on an profits of premium models but in addition elevates inquiries concerning a problems beneath which these particular imitations tend to be produced.
Coordinating and Incorporating Replica Bags
Including replica purses within your collection could prove both stylish and ethical. A method is to to combine premium imitations with authentic real items plus other sustainable sustainable apparel goods. Such an approach not only improves one’s overall style but also also promotes an eco-friendly apparel movement.
While fashioning imitation purses, consider the event plus your attire. A traditional imitation handbag can add an element touch of sophistication to a an official outfit, whereas an in-style design may turn a casual look more stylish. Don’t become scared to experiment w/different different trends & add-ons to create a distinctive and custom appearance.
Furthermore, looking after for your imitation bags is key crucial to preserve their appearance look and durability. Consistent washing plus appropriate storing may help maintain your a handbags looking new plus stylish for a longer time.
The importance Value of knowledgeable Consumer Choices
In the current today’s fashion environment, informed customer decisions are more more important important than ever. Although fake bags provide an affordable alternative for luxury luxury pieces, it is key to think about the moral and lawful consequences. By remaining conscious of where and plus how one buys fakes, one can can enjoy premium style while staying true to your principles.
It is also essential to remember that personal individual taste is not determined by name names or cost cost tags. Whether you one opts to invest in authentic authentic luxury goods or check out explore the domain of replica bags, the ultimate goal is finding pieces that make one feel self-assured & stylish.
Wrap-Up
Imitation purses have found out a special niche within the apparel world, providing a budget-friendly plus accessible option to luxury high-end goods. While they arrive with their own their particular series of of moral
Related Fashion Topics
Discovering the realm of style doesn’t conclude with copy purses. Here are some further associated subjects that may interest you:
Green Fashion
Dive into the significance of green practices in the fashion field. Discover about sustainable substances, moral manufacturing techniques, and how to build a green wardrobe.
Classic and Pre-owned Style
Explore the appeal of retro and thrift garments. Find out how to source quality retro pieces, the benefits of thrift style, and suggestions for incorporating these articles into your current collection.
Homemade Fashion and Recycling
Be innovative with Homemade apparel projects and upcycling previous apparel. Acquire hands-on guidance on transforming your closet by making your own adornments or customizing present articles to bestow them a fresh purpose.
Apparel on a Budget
Understand how to remain trendy without exceeding the bank. Explore tricks for finding fantastic deals, shopping smart during discounts, and making the most of your style budget.
Capsule Collections
Comprehend the idea of a compact closet—curating a set of important, versatile articles that can be mixed and coordinated to create different looks. Evaluate the merits of this minimalist approach and how to apply it.
Apparel Trends and Predicting
Stay in front of the movement by discovering future fashion movements and sector forecasts. Learn about pioneering fashionistas, significant apparel events, and the newest must-have pieces.
Style and Technology
Investigate how technology is changing the fashion field. Themes cover advanced materials, virtual try-ons, fashion applications, and the impact of social media on style promotion and buyer behavior.
Body Confidence and Style
Examine the link between style and figure acceptance. Understand about brands promoting comprehensive sizes, the importance of inclusion in fashion publications, and how to outfit for various figures.
Apparel Heritage
Take a trip through the heritage of style. Uncover different eras, iconic fashion moments, and how past styles remain to affect modern fashion.
Apparel Snapshots and Writing
Delve into the world of style snapshots and blogging. Get tips on how to get amazing apparel images, begin your own apparel journal, and grow your reach in the digital space.
Lorem Ipsum has been the industry’s standard dummy text https://gastroludki.pl/emmrd of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://osteriagattobianco.it/jnpiem of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://biztechnews.in/kxryo of type and scrambled it to make a type specimen book.
Del Mar Energy Company is an international industrial holding company engaged in the extraction of oil, gas, and coal
The story of the great Kobe Bryant https://los-angeles-lakers.kobe-bryant-fr.com with ” Los Angeles Lakers: his path to the championship, his legendary achievements.
Novak Djokovic’s https://tennis.novak-djokovic-fr.biz journey from childhood to the top of world tennis: early years, first victories, dominance and influence on the sport.
Find out the story of Jon Jones https://ufc.jon-jones-fr.biz in the UFC: his triumphs, records and controversies, which made him one of the greatest fighters in the MMA world.
Lorem Ipsum has been the industry’s standard dummy text https://reformasfaciles.es/nnrodd of type and scrambled it to make a type specimen book.
Comment verifier la pertinence du code promo 1xbet?
Pour verifier la pertinence du 1xbet dernier code promo, le joueur doit se connecter a son compte. En utilisant les parametres, vous devez entrer dans la section «verifier le code promotionnel et entrer la combinaison copiee.
Lorem Ipsum has been the industry’s standard dummy text https://searchxlinks.de/hitgrfw of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://npf-paker.es/kwwlo of type and scrambled it to make a type specimen book.
https://akkred-med.ru
An Charm concerning Premium Fashion
Fashion enthusiasts as well as premium shoppers usually find themselves fascinated via the elegance and renown regarding high-end fashion. Starting with an intricate aspects regarding one Hermes Birkin to the legendary style concerning a Chanel 2.55, these particular products represent more than just merely style—they represent a good particular standing and uniqueness. However, not everyone else may afford up to spend lavishly on these particular luxury goods, which has led up to a growing movement of replica purses. With regard to a lot of, those imitations provide a manner up to enjoy the elegance concerning high fashion layouts devoid of breaking an loan provider.
A increase in recognition concerning imitation handbags has opened up a amazing intriguing discussion about dress, values, as well as personal fashion. Inside a website article, we all may explore an different aspects concerning some sort of trend, offering fashion fans along with one detailed manual regarding imitation handbags. By an end, you’ll have the knowledge in order to make informed judgments that line up with your values plus looks.
Moral and Lawful Factors of Replica Bags
When that comes to replica bags, just one concerning an many pressing problems can be the moral as well as legal implications. An production and purchase regarding counterfeit goods are against the law in numerous nations, while the idea breaches intellectual residential property rights. That not only impacts the income of premium manufacturers but also increases questions regarding the problems under which usually those imitations tend to be developed.
Styling and Including Replica Handbags
Incorporating imitation handbags into your your closet may be both trendy fashionable & ethical. A single way is to to combine top-quality imitations with authentic genuine items and other sustainable sustainable apparel pieces. Such an approach doesn’t only improves a total style but also additionally promotes encourages an eco-friendly fashion trend.
When coordinating fake bags, think about the occasion occasion plus one’s outfit. A timeless fake handbag may insert a touch element of sophistication to a dressy attire, while a fashionable design could render a casual look more stylish. Never be afraid to try w/different diverse trends plus add-ons to create an original and custom look.
Moreover, caring of your fake handbags is key to keep their look & lifespan. Routine maintenance & proper storing may assist keep your a purses looking pristine & stylish for a longer time.
The importance Significance of Informed Buyer Decisions
In today’s today’s apparel landscape, educated buyer decisions are more more important significant than ever before. Though imitation handbags offer a budget-friendly alternative to high-end items, it’s key to think about the moral and legal consequences. By remaining mindful about where and and how you buy replicas, you might enjoy premium style whilst staying true to your values values.
It’s also crucial to remember that one’s individual fashion isn’t defined defined by the brand tags or cost tags. Whether you you choose to spend in authentic real high-end items or check out exploring the world of fake handbags, the key is discovering pieces that one feel feel confident & trendy.
Final Thoughts
Fake handbags have found out a distinct niche within the style universe, offering a budget-friendly plus attainable substitute to luxury high-end items. Though they arrive bring with their their own unique series of of moral
Associated Style Topics
Investigating the realm of style doesn’t end with imitation bags. Here are some further connected topics that could attract you:
Eco-friendly Apparel
Delve into the value of eco-friendliness in the style sector. Understand about eco-friendly substances, ethical manufacturing practices, and how to construct a green collection.
Retro and Thrift Style
Explore the charm of vintage and pre-owned garments. Discover how to find high-quality retro articles, the perks of thrift fashion, and advice for incorporating these items into your contemporary collection.
Do-It-Yourself Style and Recycling
Be creative with Do-It-Yourself fashion initiatives and upcycling used clothes. Acquire practical tips on transforming your collection by making your own accents or customizing existing items to grant them a new life.
Fashion on a Shoestring
Learn how to remain trendy without exceeding the budget. Explore tricks for get fantastic offers, purchasing wisely during promotions, and making your fashion funds.
Capsule Closets
Comprehend the concept of a capsule closet—curating a group of important, multi-purpose pieces that can be mixed and coordinated to make numerous ensembles. Examine the benefits of this streamlined strategy and how to implement it.
Apparel Tendencies and Predicting
Keep ahead of the trend by discovering forthcoming apparel tendencies and industry projections. Discover about pioneering designers, pivotal apparel weeks, and the latest essential pieces.
Apparel and Innovation
Explore how technology is changing the style field. Themes involve intelligent materials, digital fitting rooms, fashion tools, and the impact of social networks on fashion promotion and buyer habits.
Figure Positivity and Style
Examine the connection between apparel and physique confidence. Learn about brands advocating comprehensive sizing, the importance of representation in apparel outlets, and how to outfit for diverse body types.
Fashion History
Begin a trip through the history of apparel. Uncover different eras, legendary style movements, and how earlier fashions persist to affect contemporary apparel.
Fashion Photography and Writing
Explore into the realm of apparel snapshots and blogs. Gain advice on how to capture stunning fashion photos, start your own apparel website, and increase your reach on social media.
Lorem Ipsum has been the industry’s standard dummy text https://betway-casino-app.in/ksydo of type and scrambled it to make a type specimen book.
Howdy! This blog post could not be written any better! Going through this article reminds me of my previous roommate! He constantly kept preaching about this. I am going to send this information to him. Pretty sure he’ll have a great read. Many thanks for sharing!
Lorem Ipsum has been the industry’s standard dummy text https://josemariaabad.es/tzdzupl of type and scrambled it to make a type specimen book.
Jannik Sinner https://tennis.jannik-sinner-fr.biz an Italian tennis player, went from starting his career to entering the top 10 of the ATP, demonstrating unique abilities and ambitions in world tennis.
Carlos Alcaraz https://tennis.carlos-alcaraz-fr.biz from a talented junior to the ATP top 10. His rise is the result of hard work, support and impressive victories at major world tournaments.
The fascinating story of Daniil Medvedev’s https://tennis.daniil-medvedev-fr.biz rise to world number one. Find out how a Russian tennis player quickly broke into the elite and conquered the tennis Olympus.
The fascinating story of Alexander Zverev’s https://tennis.alexander-zverev-fr.biz rapid rise from a junior star to one of the leaders of modern tennis.
Discover Casper Ruud’s https://tennis.casper-ruud-fr.com journey from his Challenger debut to the top 10 of the world tennis rankings. A unique success.
Qu’est-ce qui donne au joueur la verification dans 1xbet?
La verification est une procedure obligatoire pour les clients du bookmaker Bonus d’inscription 1xbet. La procedure prevoit la verification des donnees personnelles du client pour la conformite avec les donnees reelles qui sont presentees sur la carte d’identite.
Lorem Ipsum has been the industry’s standard dummy text https://gs-stroehe.de/qsnqw of type and scrambled it to make a type specimen book.
На этой странице представлены самые лучшие онлайн игровые автоматы на деньги, а также рекомендации по выбору надежных казино Игровые автоматы на деньги
Ou dois-je inserer un code promo lors de l’inscription a 1xBet?
Des que le Codes promo 1xbet est copie, le joueur doit aller a l’enregistrement dans le bureau 1xbet. Dans le processus d’inscription, le code copie doit etre colle dans un formulaire special.
Lorem Ipsum has been the industry’s standard dummy text https://gs-stroehe.de/fowdw of type and scrambled it to make a type specimen book.
drug effexor 25
Чемпион Казино – Официальный телеграм раздачи Промокод для казино Чемпион. Актуальные и щедрые промокоды при регистрации, а также бездепозитный промокод доступный сегодня, прямо в нашей статье.
Lorem Ipsum has been the industry’s standard dummy text https://lotniskoparking24.pl/yqdnzfy of type and scrambled it to make a type specimen book.
Qu’est-ce que la strategie de jeu?
La strategie de jeu est un algorithme d’action que le joueur doit suivre en faisant un pari. Les actions peuvent inclure la taille du pari, le montant des cotes, la duree de la serie de Paris.1 x code promo de pari L’objectif principal de toute strategie est d’obtenir des gains qui seront en mesure de compenser toutes les depenses precedentes.
Lorem Ipsum has been the industry’s standard dummy text https://zuzannaandrzejewska.pl/sgxhj of type and scrambled it to make a type specimen book.
pve boost kreativwerkstatt-esens.de .
1win – относительно Молодое виртуальное казино, которое принадлежит компании MFI investments. В перечень предлагаемых услуг входят: ставки на спорт, киберспорт, тв программы, а также подборка совершенных игровых автоматов и присоединение к игровым столам с картами http://xn--48-6kcd0fg.xn--p1ai/forums.php?m=posts&q=22627&n=last#bottom
Lorem Ipsum has been the industry’s standard dummy text https://childrenfestivalatri.it/kdvwpu of type and scrambled it to make a type specimen book.
provigil price in india
Активация промокода: В процессе регистрации игрокам будет предложено ввести Промокод для казино Чемпион. Введение этого кода активирует бонусы, предусмотренные для новых пользователей. Этот шаг критически важен для получения всех преимуществ, предлагаемых промокодом, включая фриспины и бонусы на депозит.
Lorem Ipsum has been the industry’s standard dummy text https://limpiezasletsgo.es/lpthdaw of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://analisidebiti.it/wzesynn of type and scrambled it to make a type specimen book.
The powerful story of Conor McGregor’s https://ufc.conor-mcgregor-fr.biz rise to a two-division UFC championship that forever changed the landscape of mixed martial arts.
The legendary boxing world champion Mike Tyson https://ufc.mike-tyson-fr.biz made an unexpected transition to the UFC in 2024, where he rose to the top, becoming the oldest heavyweight champion.
The story of Fernando Alonso https://formula-1.fernando-alonso-fr.com in Formula 1: a unique path to success through talent, tenacity and strategic decisions, inspiring and exciting.
The fascinating story of how Lewis Hamilton https://mercedes.lewis-hamilton-fr.biz became a seven-time Formula 1 world champion after signing with Mercedes.
The fascinating story of the creation and rapid growth of Facebook https://facebook.mark-zuckerberg-fr.biz under the leadership of Mark Zuckerberg, who became one of the most influential technology entrepreneurs of our time.
Max Verstappen and Red Bull Racing’s https://red-bull-racing.max-verstappen-fr.com path to success in Formula 1. A story of talent, determination and team support leading to a championship title.
The astonishing story of Emmanuel Macron’s https://president-of-france.emmanuel-macron-fr.com political rise from bank director to the highest office in France.
The story of Joe Biden’s https://president-of-the-usa.joe-biden-fr.com triumphant journey, overcoming many obstacles on his path to the White House and becoming the 46th President of the United States.
Une ascension fulgurante au pouvoir Donald Trump https://usa.donald-trump-fr.com et son empire commercial
Lorem Ipsum has been the industry’s standard dummy text https://amaloquehaces.es/vffqs of type and scrambled it to make a type specimen book.
диплом переквалификация купить asxdiplomik.com .
Offre speciale code promo 1xbet casino vous offre une remise de 100% sur le montant total de votre premier depot jusqu’a 100$, bien entendu, dans votre devise locale. Profitez-en facilement en saisissant le code promotionnel lors de votre inscription et recevez un bonus sur 1xbet.com.
Активация промокода: В процессе регистрации игрокам будет предложено ввести Промокод Champion Casino. Введение этого кода активирует бонусы, предусмотренные для новых пользователей. Этот шаг критически важен для получения всех преимуществ, предлагаемых промокодом, включая фриспины и бонусы на депозит.
Lorem Ipsum has been the industry’s standard dummy text https://korepetytorek.pl/djkpgf of type and scrambled it to make a type specimen book.
Parisian PSG https://paris.psg-fr.com is one of the most successful and ambitious football clubs in Europe. Find out how he became a global football superstar.
Travel to the pinnacle of French football https://stadede-bordeaux.bordeaux-fr.org at the Stade de Bordeaux, where the passion of the game meets the grandeur of architecture.
Olympique de Marseille https://liga1.marseilles-fr.com after several years in the shadows, once again becomes champion of France. How did they do it and what prospects open up for the club
The fascinating story of Gigi Hadid’s rise to Victoria’s Secret Angel https://victorias-secret.gigi-hadid-fr.com status and her journey to the top of the modeling industry.
куплю диплом фото ast-diploms.com .
Lorem Ipsum has been the industry’s standard dummy text https://conceptshop.es/eqnqwbk of type and scrambled it to make a type specimen book.
The fascinating story of the creation and meteoric rise of Amazon https://amazon.jeff-bezos-fr.com from its humble beginnings as an online bookstore to its dominant force in the world of e-commerce.
Lorem Ipsum has been the industry’s standard dummy text https://allafricapokerguide.co.za/yvlrtn of type and scrambled it to make a type specimen book.
A fascinating story about how Elon Musk https://spacex.elon-musk-fr.com and his company SpaceX revolutionized space exploration, opening new horizons for humanity.
The inspiring story of Travis Scott’s https://yeezus.travis-scott-fr.com rise from emerging artist to one of modern hip-hop’s brightest stars through his collaboration with Kanye West.
An exploration of Nicole Kidman’s https://watch.nicole-kidman-fr.com career, her notable roles, and her continued quest for excellence as an actress.
How Taylor Swift https://midnights.taylor-swift-fr.com reinvented her sound and image on the intimate and reflective album “Midnights,” revealing new dimensions of her talent.
Lorem Ipsum has been the industry’s standard dummy text https://inak.es/qcjbddg of type and scrambled it to make a type specimen book.
Explore the rich history and unrivaled atmosphere of the iconic Old Trafford Stadium https://old-trafford.manchester-united-fr.com, home of one of the world’s most decorated football clubs, Manchester United.
Lorem Ipsum has been the industry’s standard dummy text https://annacarniz.es/chpdvq of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://dgkservice.it/bvavhb of type and scrambled it to make a type specimen book.
Comment verifier la pertinence du code promo 1xbet?
Pour verifier la pertinence du code promo sport 1xbet, le joueur doit se connecter a son compte. En utilisant les parametres, vous devez entrer dans la section «verifier le code promotionnel et entrer la combinaison copiee.
montenegro language Montenegro Zabljak
Lorem Ipsum has been the industry’s standard dummy text https://samarthdiagnostics.in/ofyyeco of type and scrambled it to make a type specimen book.
Offre speciale 1xBet Obtenez un bonus sportif supplementaire de 200% jusqu’a 130 €/$ avec le code promo 1xbet aujourd’hui, en plus du bonus de bienvenue standard de 1950$ et de 150 tours gratuits au casino. Profitez de cette opportunite pour jouer et gagner de l’argent grace aux paris sportifs. Chez nous, tout le monde peut devenir gagnant !
Единственная в России студия кастомных париков https://wigdealers.ru, где мастера индивидуально подбирают структуру волос и основу по форме головы, после чего стригут, окрашивают, делают укладку и доводят до идеала ваш будущий аксессуар.
The iconic Anfield https://enfield.liverpool-fr.com stadium and the passionate Liverpool fans are an integral part of English football culture.
An exploration of the history of Turin’s https://turin.juventus-fr.org iconic football club – Juventus – its rivalries, success and influence on Italian football.
The new Premier League https://premier-league.chelsea-fr.com season has gotten off to an intriguing start, with a new-look Chelsea looking to return to the Champions League, but serious challenges lie ahead.
Lorem Ipsum has been the industry’s standard dummy text https://willarybaki.pl/guyeiu of type and scrambled it to make a type specimen book.
Ou dois-je inserer un code promo lors de l’inscription a 1xBet?
Des que le 1xbet code promo tours gratuits est copie, le joueur doit aller a l’enregistrement dans le bureau 1xbet. Dans le processus d’inscription, le code copie doit etre colle dans un formulaire special.
Lorem Ipsum has been the industry’s standard dummy text https://biz4u.in/qsaejh of type and scrambled it to make a type specimen book.
Tyson Fury https://wbc.tyson-fury-fr.com is the undefeated WBC world champion and reigns supreme in boxing’s heavyweight division.
Inter Miami FC https://mls.inter-miami-fr.com has become a major player in MLS thanks to its star roster, economic growth and international influence.
Explore the career and significance of Monica Bellucci https://malena.monica-bellucci-fr.com in Malena (2000), which explores complex themes of beauty and human strength in wartime.
Discover Rafael Nadal’s https://mls.inter-miami-fr.com impressive rise to the top of world tennis, from his debut to his career Grand Slam victory.
The story of Kanye West https://the-college-dropout.kanye-west-fr.com, starting with his debut album “The College Dropout,” which changed hip-hop and became his cultural legacy.
Преимущества аренды склада https://dk-zio.ru/2024/07/arenda-sklada-na-chto-obratit-vnimanie-pri-vybore-pomeshheniya/, как аренда складских помещений может улучшить ваш бизнес
Rivaldo, or Rivaldo https://barcelona.rivaldo-br.com, is one of the greatest football players to ever play for Barcelona.
The fascinating story of the phenomenal rise and meteoric fall of Diego Maradona https://napoli.diegomaradona.biz, who became a cult figure at Napoli in the 1980s.
A fascinating story about Brazilian veteran Thiago Silva’s https://chelsea.thiago-silva.net difficult path to the top of European football as part of Chelsea London.
Explore the remarkable journey of Vinicius Junior https://real-madrid.vinicius-junior.net, the Brazilian prodigy who conquered the world’s biggest stage with his dazzling skills and unparalleled ambition at Real Madrid.
Enregistrez-vous en utilisant le promo de morue 1xbet afin de profiter d’une offre exclusive de bonus de 100% jusqu’a 130$ sur les paris sportifs gratuits. Pour beneficier de cette offre de pari gratuit bonifiee, vous devrez placer 5 paris sur des accumulateurs dans les 30 jours. Il existe diverses strategies pour les paris combines, mais si vous souhaitez gagner et obtenir des paris gratuits, nous vous recommandons de privilegier des selections de cotes plus courtes et de vous concentrer sur des paris combines surs pour commencer.
Cristiano Ronaldo https://al-nassr.cristianoronaldo-br.net one of the greatest football players of all time, begins a new chapter in his career by joining An Nasr Club.
The story of Luka Modric’s rise https://real-madrid.lukamodric-br.com from young talent to one of the greatest midfielders of his generation and a key player for the Royals.
The fascinating story of Marcus Rashford’s rise https://manchester-united.marcusrashford-br.com from academy youth to the main striker and captain of Manchester United. Read about his meteoric rise and colorful career.
From academy product to captain and leader of Real Madrid https://real-madrid.ikercasillas-br.com Casillas became one of the greatest players in the history of Real Madrid.
Lorem Ipsum has been the industry’s standard dummy text https://btelectricshop.es/nddrvs of type and scrambled it to make a type specimen book.
cost cialis
Follow Bernardo Silva’s impressive career https://manchester-city.bernardosilva.net from his debut at Monaco to to his status as a key player and leader of Manchester City.
Lorem Ipsum has been the industry’s standard dummy text https://korepetytorek.pl/cuhbfrx of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://agamagizhan.in/llscb of type and scrambled it to make a type specimen book.
Привет, друзья!
Где заказать диплом специалиста?
Мы готовы предложить дипломы психологов, юристов, экономистов и любых других профессий по выгодным тарифам.
http://www.cialisonlinerx.com/mifegest.html
казино риобет Rio Bet Casino
Rio Bet dacha76.ru
бонус драгон мани казино https://uvstyle.ru
регистрация драгон мани казино https://web-kulinar.ru
Lorem Ipsum has been the industry’s standard dummy text https://wnioseksde.pl/rfaptrb of type and scrambled it to make a type specimen book.
Хотите научиться готовить самые изысканные и сложные торты? В этом https://v1.skladchik.org/tags/tort/ разделе вы найдете множество подробных пошаговых рецептов самых трендовых и известных тортов с возможностью получить их за сущие копейки благодаря складчине. Готовьте с удовольствием и открывайте для себя новые рецепты вместе с Skladchik.org
Военный адвокат Запорожье. Бесплатная консультация
адвокат СЗЧ
— это опытный специалист имеющий высшее юридическое образование, сдавший квалификационный государственный экзамен на право осуществления адвокатской деятельностью и специализирующийся в основном на военных делах
Вся правовая помощь военного адвоката осуществляется в индивидуальном порядке, грамотно, четко и в соответствии с действующими нормативно-правовыми актами.
Мы как военные юристы действуем не против органов Украины или министерства обороны, мы действуем во благо Украины — наших защитников и граждан Украины, которые попали в тяжелую жизненную ситуацию связанную с незнанием военного и действующего законодательства.
Поскольку, проявив патриотизм и чувство гражданской ответственности – став на защиту суверенитета страны, граждане участвующие и помогавшие в обороне после, становятся никому не нужными, особенно если военнослужащий стал инвалидом, потерял часть тела или конечность, и не может самостоятельно защитить свои права. Именно в таких ситуациях мы как военные адвокаты приходим на помощь, и добиваемся в установленном законом порядке справедливости, необходимых выплат, установление статуса, оформление пенсий, льгот и т.п.
Тоже касается, и получение отсрочки от мобилизации, когда например, безосновательно призывают сына у которого отец инвалид 2 группы, или мать прикованная из-за тяжелой болезни к постели, и требующая постороннего ухода. Это же относится и к военнослужащим, рапорта которых не регистрируются в канцелярии воинской части и полностью игнорируются, под прикрытием суеты боевых действий..
Именно в таких ситуациях, мы приходим на помощь и с помощью ЗАКОННЫХ методов правовой защиты, используя свой опыт полученный при ведении аналогичных военных дел добиваемся справедливости.
Lorem Ipsum has been the industry’s standard dummy text https://professionalgardens.es/apote of type and scrambled it to make a type specimen book.
Attractive section of content. I just stumbled upon your web site and in accession capital to assert that I acquire actually enjoyed account your blog posts. Any way I will be subscribing to your augment and even I achievement you access consistently quickly.
ganobet nedir
Лучшие пансионаты для пожилых людей https://ernst-neizvestniy.ru в Самаре – недорогие дома для престарелых в Самарской области
Пансионаты для пожилых людей https://moyomesto.ru в Самаре по доступным ценам. Специальные условия по уходу, индивидуальные программы.
The fascinating story of Sergio Ramos’ https://seville.sergioramos.net rise from Sevilla graduate to one of Real Madrid and Spain’s greatest defenders.
Ousmane Dembele’s https://paris-saint-germain.ousmanedembele-br.com rise from promising talent to key player for French football giants Paris Saint-Germain. An exciting success story.
Lorem Ipsum has been the industry’s standard dummy text https://betway-casino-app.in/ocihybh of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://f7zdrowie.pl/yvpqgqs of type and scrambled it to make a type specimen book.
Comment puis-je gagner des points Code promo bonus de bienvenue 1xbet?
Dans le bookmaker 1xbet en tant qu’encouragement des clients pour leur participation active au processus de jeu, ils fournissent des points promotionnels dans le cadre du programme de fidelite. Vous pouvez obtenir des points pour les Paris sportifs reguliers, Express, pour la reconstitution reguliere du compte et la participation aux actions du bookmaker.
Lorem Ipsum has been the industry’s standard dummy text https://animediainnovation.in/wxtgmsx of type and scrambled it to make a type specimen book.
codes promo pour 1xbet 2024 tous les details sur les bonus de bienvenue. Enregistrez-vous des maintenant avec notre offre speciale 1xBet 2024 pour beneficier d’un bonus de bienvenue de 100% jusqu’a 130$. Tous les nouveaux joueurs recoivent un bonus de bienvenue de 1xBet pour la creation d’un compte avec un code promotionnel.
Lorem Ipsum has been the industry’s standard dummy text https://derivedsolutions.in/ajitvr of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://cagliaricentro.it/jorig of type and scrambled it to make a type specimen book.
Comment verifier la pertinence du code promo 1xbet?
Pour verifier la pertinence du code promo 1xbet cote d’ivoire 2024, le joueur doit se connecter a son compte. En utilisant les parametres, vous devez entrer dans la section «verifier le code promotionnel et entrer la combinaison copiee.
The incredible success story of 20-year-old Florian Wirtz https://bayer-04.florianwirtz-br.com, who quickly joined the Bayer team and became one of the best young talents in the world.
The compelling story of Alisson Becker’s https://bayer-04.florianwirtz-br.com meteoric rise from young talent to key figure in Liverpool’s triumphant era under Jurgen Klopp.
Lorem Ipsum has been the industry’s standard dummy text https://creosell.pl/kjeer of type and scrambled it to make a type specimen book.
The incredible story https://napoli.khvichakvaratskhelia-br.com of a young Georgian talent’s transformation into an Italian Serie A star. Khvicha Kvaraeshvili is a rising phenomenon in European football.
O meio-campista Rafael Veiga leva https://palmeiras.raphaelveiga-br.com o Palmeiras ao sucesso – o campeonato brasileiro e a vitoria na Copa Libertadores aos 24 anos.
Midfielder Rafael Veiga leads https://manchester-city.philfoden-br.com Palmeiras to success – the championship Brazilian and victory in the Copa Libertadores at the age of 24.
Do you have a spam problem on this site; I also am a blogger, and I was wanting to know your situation; many of us have developed some nice methods and we are looking to exchange strategies with other folks, why not shoot me an e-mail if interested.
lee bet casino
Lorem Ipsum has been the industry’s standard dummy text https://placassolaresmalaga2000.es/uwaeiik of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://lasparrasdemartin.es/cdfhrce of type and scrambled it to make a type specimen book.
In-depth articles about the most famous football players https://zenit-saint-petersburg.wendel-br.com, clubs and events. Learn everything about tactics, rules of the game and football history.
The rise of 20-year-old midfielder Jamal Musiala https://bavaria.jamalmusiala-br.com to the status of a winger in the Bayern Munich team. A story of incredible talent.
A historia da jornada triunfante de Anitta https://veneno.anitta-br.com de aspirante a cantora a uma das interpretes mais influentes da musica moderna, incluindo sua participacao na serie de TV “Veneno”.
Fabrizio Moretti https://the-strokes.fabriziomoretti-br.com the influential drummer of The Strokes, and his unique sound revolutionized the music scene, remaining icons of modern rock.
Selena Gomez https://calm-down.selenagomez-br.net the story from child star to global musical influence, summarized in hit “Calm Down”, with Rema.
Lorem Ipsum has been the industry’s standard dummy text https://webclinic.es/bjuagpo of type and scrambled it to make a type specimen book.
Hi, I do think your blog could be having web browser compatibility problems. Whenever I take a look at your web site in Safari, it looks fine however, if opening in I.E., it has some overlapping issues. I simply wanted to provide you with a quick heads up! Besides that, great blog!
Практический опыт в SEO с 2008 г. подтверждается датой регистрации моего блога, в котором я частенько пишу о своем понимании в продвижении сайтов. Внедряю стратегию SEO, учитывая алгоритмы поисковиков и использую свои технические skills для достижения наилучших результатов https://bomlenta.blogspot.com/2009/07/2-20-2009.html
АвтоАтелье Medvedev AutoLab – перетяжка салона, шумоизоляция и тюнинг автомобилей в Екатеринбурге https://detailauto.ru
Также укажите наш Промокод Чемпион. Данную бонусную комбинацию можно скопировать в начале нашей статьи. Промокод для казино Чемпион. ШАГ 3. Подтвердите регистрацию, зайдя в ящик электронной почты, которую вы указывали при создании аккаунта. Champion casino регистрация с промокодом. ШАГ 4. Выберите один из приветственных бонусов, которые хотите получить.
En utilisant le code promo 1xbet pour un pari gratuit, vous pouvez beneficier d’une augmentation de 100% en plus du bonus de bienvenue standard. Selon votre emplacement geographique, vous recevrez un bonus de 100%, 200% ou 300%, bonus 130$. Ce bonus est ensuite divise en deux parties, dont la moitie est utilisable pour les paris sportifs et l’autre moitie pour le casino. Avant de pouvoir retirer vos fonds, vous devrez jouer le montant du bonus 5 fois pour les paris sportifs combines et 30 fois pour les jeux de casino. Les nouveaux utilisateurs devront probablement verifier leur compte en fournissant un passeport ou un permis de conduire dans le cadre d’une verification KYC avant de pouvoir effectuer un retrait.
Lorem Ipsum has been the industry’s standard dummy text https://primescan.es/cmuqy of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://salvatierrasostenible.es/uqztlrr of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://praceziemnelodz.pl/xwzxceg of type and scrambled it to make a type specimen book.
bursa görüntülü diafon en uygun fiyat garantisi
Здравствуйте!
Где купить диплом по актуальной специальности?
Наша компания предлагает быстро и выгодно заказать диплом, который выполняется на оригинальной бумаге и заверен печатями, штампами, подписями. Документ способен пройти лубую проверку, даже с использованием профессионального оборудования. Достигайте свои цели быстро и просто с нашей компанией.
Приобрести диплом о высшем образовании.
guyspages.com/read-blog/842
Lorem Ipsum has been the industry’s standard dummy text https://tascaisa.es/uljrzc of type and scrambled it to make a type specimen book.
Kobe Bryant https://los-angeles-lakers.kobebryant-br.net one of the greatest basketball players of all the times, left an indelible mark on the history of sport.
где можно купить аттестат за 11 класс diplomyx.com .
Achraf Hakimi https://paris-saint-germain.ashrafhakimi.net is a young Moroccan footballer who quickly reached the football elite European in recent years.
аттестат купить выходить аттестат купить выходить .
Bieber’s https://baby.justinbieber-br.com path to global fame began with his breakthrough success Baby, which became his signature song and one of the most popular music videos of all time.
Ayrton Senna https://mclaren.ayrtonsenna-br.com is one of the greatest drivers in the history of Formula 1.
In the world of professional tennis, the name of Gustavo Kuerten https://roland-garros.gustavokuerten.com is closely linked to one of the most prestigious Grand Slam tournaments – Roland Garros.
Lorem Ipsum has been the industry’s standard dummy text https://stepsman.cfd/yuewrj of type and scrambled it to make a type specimen book.
Привет, друзья!
Мы готовы предложить документы техникумов, которые расположены на территории всей России. Вы можете заказать качественно сделанный диплом от любого учебного заведения, за любой год, в том числе документы старого образца. Дипломы и аттестаты выпускаются на “правильной” бумаге высшего качества. Это дает возможности делать настоящие дипломы, которые не отличить от оригиналов. Они заверяются необходимыми печатями и подписями.
Купить диплом любого ВУЗа.
astronomyfriends.com/read-blog/316
Хорошей учебы!
Qu’est-ce que la strategie de jeu?
La strategie de jeu est un algorithme d’action que le joueur doit suivre en faisant un pari. Les actions peuvent inclure la taille du pari, le montant des cotes, la duree de la serie de Paris.code promo 1xbet pour un pari gratuit L’objectif principal de toute strategie est d’obtenir des gains qui seront en mesure de compenser toutes les depenses precedentes.
Le meilleur code promo 1xbet 2024 pour beneficier d’une offre VIP de 100% jusqu’a 130€ sur les paris sportifs ou de 1950€ + 150 tours. Tous les nouveaux joueurs ayant utilise le code lors de leur inscription recoivent un bonus de bienvenue. Ce code bonus special vous permettra de recevoir un bonus augmente lors de votre inscription sur le site du bookmaker 1xBet.com ! Ne manquez pas cette occasion et inscrivez-vous des maintenant avec le code promo 1xbet pour obtenir un bonus allant jusqu’a 130 €/$.
Lorem Ipsum has been the industry’s standard dummy text https://mobilwiz.dk/gjqpdxc of type and scrambled it to make a type specimen book.
Ou dois-je inserer un code promo lors de l’inscription a 1xBet?
Des que le Codes promotionnels 1x pari est copie, le joueur doit aller a l’enregistrement dans le bureau 1xbet. Dans le processus d’inscription, le code copie doit etre colle dans un formulaire special.
Привет, друзья!
Приобрести документ университета вы имеете возможность у нас в столице.
ast-diplomy.com/kupit-diplom-magistra
Успешной учебы!
Lorem Ipsum has been the industry’s standard dummy text https://salvatierrasostenible.es/pjafq of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://eduerp4u.in/ronjpqx of type and scrambled it to make a type specimen book.
Проверьте лицензию казино – это гарантия вашей безопасности и честности игрового процесса. ]Отзывы других игроков являются ценным источником информации о надежности и качестве обслуживания. ]Техническая поддержка должна быть доступна круглосуточно, чтобы оперативно решать любые возникающие проблемы http://introsystems.ru/component/kunena/suggestion-box/32553-1win-topovye-vidy-sporta-dlya-stavok
Lorem Ipsum has been the industry’s standard dummy text https://spawax.pl/rknqinq of type and scrambled it to make a type specimen book.
Anderson Silva https://killer-bees-muay-thai-college.andersonsilva.net was born in 1975 in Curitiba Brazil. From a young age he showed an interest in martial arts, starting to train in karate at the age of 5.
Daniel Alves https://paris-saint-germain.danielalves.net is a name that symbolizes the greatness of the world of football.
Привет, друзья!
Где заказать диплом по нужной специальности?
Мы готовы предложить документы ВУЗов, расположенных на территории всей Российской Федерации. Можно заказать диплом от любого ВУЗа, за любой год, включая документы старого образца СССР. Дипломы выпускаются на “правильной” бумаге высшего качества. Это позволяет делать настоящие дипломы, не отличимые от оригиналов. Они будут заверены необходимыми печатями и подписями.
Мы можем предложить дипломы психологов, юристов, экономистов и других профессий по доступным ценам.
diploms-x.com/kupit-diplom-moskva
Поможем вам всегда!
Bruno Miguel Borges Fernandes https://manchester-united.brunofernandes-br.com was born on September 8, 1994 in Maia, Portugal.
Rodrygo Silva de Goes https://real-madrid.rodrygo-br.com, known simply as Rodrygo, emerged as one of the the brightest young talents in world football.
Nuno Mendes https://paris-saint-germain.nuno-mendes.com, a talented Portuguese left-back, He quickly became one of the key figures in the Paris Saint-Germain (PSG) team.
Lorem Ipsum has been the industry’s standard dummy text https://bet365-online-betting.in/wmwui of type and scrambled it to make a type specimen book.
Offre speciale 1xBet Obtenez un bonus sportif supplementaire de 200% jusqu’a 130 €/$ avec le 1xbet code promo tours gratuits, en plus du bonus de bienvenue standard de 1950$ et de 150 tours gratuits au casino. Profitez de cette opportunite pour jouer et gagner de l’argent grace aux paris sportifs. Chez nous, tout le monde peut devenir gagnant !
купить диплом ссср купить диплом образования http://www.diploms-x.com .
Привет!
Где приобрести диплом по актуальной специальности?
alik.forumrpg.ru/post.php?action=post&fid=63
Удачи!
Множество пользователей активно ищут удобные и доступные способы развлечения. Это привело к повышению популярности различных онлайн-сервисов https://www.luxcosmeticsdv.ru/index.php?option=com_k2&view=itemlist&task=user&id=559819
Lorem Ipsum has been the industry’s standard dummy text https://rajeshguru.in/eghjekm of type and scrambled it to make a type specimen book.
Привет, друзья!
Где приобрести диплом специалиста?
Мы предлагаем дипломы любой профессии по приятным тарифам.
http://www.tonpentreafc.com/ton_pentre_youth_090409.html
Lorem Ipsum has been the industry’s standard dummy text https://ekoworki.pl/oxluvj of type and scrambled it to make a type specimen book.
nazilli pidesi nazilli meşhur pidesi
Earvin “Magic” Johnson https://los-angeles-lakers.magicjohnson.biz is one of the most legendary basketball players in history. NBA history.
Vinicius Junior https://real-madrid.vinicius-junior-ar.com the Brazilian prodigy whose full name is Vinicius Jose Baixao de Oliveira Junior, has managed to win the hearts of millions of fans around the world in a short period of time.
Lorem Ipsum has been the industry’s standard dummy text https://propcraft.pl/kdinftf of type and scrambled it to make a type specimen book.
Victor Osimhen https://napoli.victorosimhen-ar.com born on December 29, 1998 in Lagos, Nigeria, has grown from an initially humble player to one of the brightest strikers in modern football.
Toni Kroos https://real-madrid.tonikroos-ar.com the German midfielder known for his accurate passes and calmness on the field, has achieved remarkable success at one of the most prestigious football clubs in the world.
Robert Lewandowski https://barcelona.robertlewandowski-ar.com is one of the most prominent footballers of our time, and his move to Barcelona has become one of the most talked about topics in world football.
Lorem Ipsum has been the industry’s standard dummy text https://march.cl/gjlklq of type and scrambled it to make a type specimen book.
Веном 3 онлайн https://bit.ly/venom-3-venom-2024
Qu’est-ce qu’une «Vitrine de codes promotionnels»?
Ceci est une section speciale sur le site du bookmaker Codes promotionnels 1x pari, qui contient tous les codes promotionnels actuels. Sur la vitrine, les joueurs sont disponibles codes bonus pour les Paris sportifs, pour la section avec le jeu. Chaque code peut etre echange contre des points promo en fonction des denominations.
L’inscription a 1xBet est-elle disponible sans passeport?
Vous pouvez vous inscrire a code promo 1xbet gratuit sans donnees de passeport, mais a l’avenir, dans votre compte personnel, vous devrez remplir un questionnaire indiquant votre nom, votre nom et votre date de naissance. A l’avenir, avant la premiere Conclusion, il faudra egalement passer par la verification.
Lorem Ipsum has been the industry’s standard dummy text https://aadityagroup.in/dffvwwu of type and scrambled it to make a type specimen book.
code promo 1xbet 131$t utilisez le code bonus pour obtenir un bonus VIP de 100% jusqu’a 130€ pour les Paris sportifs, ainsi qu’un bonus de casino de 1950 € + 150 tours de machines a sous. En utilisant le code promotionnel, vous pouvez vous attendre a ce que vos gains soient aussi eleves que dans le cas du plus grand bookmaker 1xbet. Tous les joueurs des pays suivants peuvent utiliser le code lors de l’inscription et recevoir un bonus de bienvenue:
You ought to be a part of a contest for one of the greatest websites on the internet. I’m going to highly recommend this blog!
Привет!
Приобрести документ института можно в нашей компании в Москве.
ast-diplom24.ru/kupit-diplom-nizhnij-novgorod
Удачи!
Бесплатный промокод на скидку, первый и повторный заказ 2024. Промокод на доставку. Акции и скидки. Халява в телеграм промокоды акции скидки 2024
Привет!
Где заказать диплом по необходимой специальности?
Мы предлагаем документы институтов, которые расположены на территории всей России. Можно приобрести качественный диплом за любой год, указав актуальную специальность и хорошие оценки за все дисциплины. Дипломы выпускаются на “правильной” бумаге высшего качества. Это дает возможность делать государственные дипломы, которые не отличить от оригинала. Документы будут заверены всеми требуемыми печатями и штампами.
Мы предлагаем дипломы любой профессии по разумным ценам.
diploms-x.com/kupit-diplom-o-srednem-obrazovanii
Всегда вам поможем!
Привет!
Мы готовы предложить документы ВУЗов, которые расположены на территории всей России. Вы можете приобрести диплом от любого заведения, за любой год, указав подходящую специальность и оценки за все дисциплины. Дипломы и аттестаты выпускаются на “правильной” бумаге самого высокого качества. Это позволяет делать государственные дипломы, которые невозможно отличить от оригинала. Они будут заверены необходимыми печатями и подписями.
zelao41.ru/a-korolev-vzorvus-a-zhivym-ne-damsya
как купить диплом в оренбурге как купить диплом в оренбурге .
Привет!
Где заказать диплом специалиста?
bdfeu.ukraine7.com/t19982-topic#36429
Удачи!
Здравствуйте!
Купить диплом о высшем образовании.
Мы предлагаем документы техникумов, расположенных на территории всей Российской Федерации. Вы можете купить качественный диплом за любой год, включая документы старого образца. Дипломы и аттестаты выпускаются на “правильной” бумаге самого высокого качества. Это дает возможности делать государственные дипломы, не отличимые от оригинала. Документы заверяются необходимыми печатями и подписями.
http://www.startspresto.ru/cb-profile/pluginclass/cbblogs?action=blogs&func=show&id=153
Привет!
Мы изготавливаем дипломы психологов, юристов, экономистов и других профессий по выгодным тарифам. Цена будет зависеть от определенной специальности, года выпуска и ВУЗа.
landik-diploms-srednee.ru/kupit-diplom-v-kazani
Удачи!
Также укажите наш Промокод Champion Casino. Данную бонусную комбинацию можно скопировать в начале нашей статьи. Промокод для казино Чемпион. ШАГ 3. Подтвердите регистрацию, зайдя в ящик электронной почты, которую вы указывали при создании аккаунта. Champion casino регистрация с промокодом. ШАГ 4. Выберите один из приветственных бонусов, которые хотите получить.
Привет, друзья!
Где купить диплом специалиста?
Купить диплом любого ВУЗа.
alex-neil.ru/index.php/cb-profile/pluginclass/cbblogs?action=blogs&func=show&id=233
You are sleeping – your PC is collecting crypto. The Grasse Network uses 1% of your PC to collect artificial intelligence data from the Internet. Join for free. Output in Solano
Военный адвокат Запорожье. Бесплатная консультация
семейный адвокат Запорожье
— это опытный специалист имеющий высшее юридическое образование, сдавший квалификационный государственный экзамен на право осуществления адвокатской деятельностью и специализирующийся в основном на военных делах
Вся правовая помощь военного адвоката осуществляется в индивидуальном порядке, грамотно, четко и в соответствии с действующими нормативно-правовыми актами.
Мы как военные юристы действуем не против органов Украины или министерства обороны, мы действуем во благо Украины — наших защитников и граждан Украины, которые попали в тяжелую жизненную ситуацию связанную с незнанием военного и действующего законодательства.
Поскольку, проявив патриотизм и чувство гражданской ответственности – став на защиту суверенитета страны, граждане участвующие и помогавшие в обороне после, становятся никому не нужными, особенно если военнослужащий стал инвалидом, потерял часть тела или конечность, и не может самостоятельно защитить свои права. Именно в таких ситуациях мы как военные адвокаты приходим на помощь, и добиваемся в установленном законом порядке справедливости, необходимых выплат, установление статуса, оформление пенсий, льгот и т.п.
Тоже касается, и получение отсрочки от мобилизации, когда например, безосновательно призывают сына у которого отец инвалид 2 группы, или мать прикованная из-за тяжелой болезни к постели, и требующая постороннего ухода. Это же относится и к военнослужащим, рапорта которых не регистрируются в канцелярии воинской части и полностью игнорируются, под прикрытием суеты боевых действий..
Именно в таких ситуациях, мы приходим на помощь и с помощью ЗАКОННЫХ методов правовой защиты, используя свой опыт полученный при ведении аналогичных военных дел добиваемся справедливости.
Чемпион Казино – Официальный телеграм раздачи Champion Casino промокод. Актуальные и щедрые промокоды при регистрации, а также бездепозитный промокод доступный сегодня, прямо в нашей статье.
Pedro Gonzalez Lopez https://barcelona.pedri-ar.com known as Pedri, was born on November 25, 2002 in the small town of Tegeste, located on Tenerife, one of the Canary Islands.
Lorem Ipsum has been the industry’s standard dummy text https://zaiwa.dk/zqjnxeh of type and scrambled it to make a type specimen book.
The story of Leo Messi https://inter-miami.lionelmessi.ae‘s transfer to Inter Miami began long before the official announcement. Rumors about Messi’s possible departure from Barcelona appeared in 2020
Andreson Souza Conceicao https://al-nassr.talisca-ar.com known as Talisca, is one of the brightest stars of modern football.
Yacine Bounou https://al-hilal.yassine-bounou-ar.com known simply as Bono, is one of the most prominent Moroccan footballers of our time.
Champion Casino промокод способен увеличить не только сумму вашего первого депозита на 100%, но и последующие: второй (на 75%), третий (на 50%) и четвертый (на 30%). Благодаря этим бонусам, у игроков появляется возможность делать еще больше ставок, увеличивая тем самым шанс на крупный выигрыш, а также позволяет дольше наслаждаться любимым времяпровождением. Как активировать бонусы через промокод чемпион казино.
Наша компания является передовиком производства измерительного обрудования. Уже долгие годы мы производим и обслуживаем датчики температуры, логгеры данных, регистраторы температуры и влажности и термометры. Наше оборудование помогает осуществлять контроль параметров микроклимата в аптеках, на складах, на производствах и в магазинах логер температуры и влажности
Lorem Ipsum has been the industry’s standard dummy text https://mprcode.pl/kaehmh of type and scrambled it to make a type specimen book.
Привет!
Мы предлагаем документы техникумов, которые расположены на территории всей РФ. Вы сможете заказать диплом от любого учебного заведения, за любой год, указав актуальную специальность и хорошие оценки за все дисциплины. Документы выпускаются на “правильной” бумаге высшего качества. Это дает возможность делать настоящие дипломы, которые невозможно отличить от оригиналов. Документы будут заверены всеми обязательными печатями и подписями.
permn.ru/blogs/1/zakazyvaem-diplom-v-luchshem-internetmagazine-po-komfortnoy-tsene.php
Lorem Ipsum has been the industry’s standard dummy text https://cosavedereinungiorno.it/qwjjxe of type and scrambled it to make a type specimen book.
Ou dois-je inserer un code promo lors de l’inscription a 1xBet?
Des que le comment obtenir un code promo 1xbet est copie, le joueur doit aller a l’enregistrement dans le bureau 1xbet. Dans le processus d’inscription, le code copie doit etre colle dans un formulaire special.
Наша команда уже более 20 лет проектирует, возводит и обслуживает бассейны в Тюмени, Челябинске и Екатеринбурге. Мы используем только современное и проверенное оборудование и материалы. Даем гарантию выполненных работ. Кроме этого, мы являемся официальными поставщиками химии для бассейнов лучших мировых марок изготовление каркасных бассейнов
можно ли купить диплом медсестры diplomyx.com .
i-tec.ru https://multimedijnyj-integrator.ru/ .
Lorem Ipsum has been the industry’s standard dummy text https://kreatoretui.pl/xhwmpu of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://professionalgardens.es/nbrwbg of type and scrambled it to make a type specimen book.
Продвижение сайта в поисковых системах Яндекс, Google. Гарантия выполненных работ. Бесплатный аудит сайта Здесь
Здравствуйте!
Мы изготавливаем дипломы психологов, юристов, экономистов и прочих профессий по приятным тарифам.
avtoweek2016.ru/legalnoe-priobretenie-diploma-onlayn/
Привет!
Как правильно приобрести диплом колледжа или ПТУ в России, важные моменты
weekofsport.ru/vash-diplom-kachestvo-i-autentichnost
Lorem Ipsum has been the industry’s standard dummy text https://stepsdown.lat/isyrqq of type and scrambled it to make a type specimen book.
Harry Kane https://bayern.harry-kane-ar.com one of the most prominent English footballers of his generation, completed his move to German football club Bayern Munich in 2023.
Brazilian footballer Neymar https://al-hilal.neymar-ar.com known for his unique playing style and outstanding achievements in world football, has made a surprise move to Al Hilal Football Club.
Erling Haaland https://manchester-city.erling-haaland-ar.com born on July 21, 2000 in Leeds, England, began his football journey at an early age.
can you buy nolvadex over the counter in south africa
Luka Modric https://real-madrid.lukamodric-ar.com can certainly be called one of the outstanding midfielders in modern football.
Football in Saudi Arabia https://al-hilal.ali-al-bulaihi-ar.com has long been one of the main sports, attracting millions of fans. In recent years, one of the brightest stars in Saudi football has been Ali Al-Bulaihi, defender of Al-Hilal Football Club.
Lorem Ipsum has been the industry’s standard dummy text https://nadpoprzeczka.pl/kzcvk of type and scrambled it to make a type specimen book.
Привет, друзья!
Как приобрести аттестат о среднем образовании в Москве и других городах.
Купить диплом ВУЗа.
fatshipresident.net/read-blog/246
Lorem Ipsum has been the industry’s standard dummy text https://alzagaconsulting.es/xcalo of type and scrambled it to make a type specimen book.
visit my website https://currencyconvert.net
Сайт https://ps-likers.ru предлагает уроки по фотошоп для начинающих. На страницах сайта можно найти пошаговые руководства по анимации, созданию графики для сайтов, дизайну, работе с текстом и фотографиями, а также различные эффекты.
Привет, друзья!
Купить документ о получении высшего образования можно в нашем сервисе.
ast-diploms24.ru/kupit-diplom-voronezh
Успехов в учебе!
N’Golo Kante https://al-ittihad.ngolokante-ar.com the French midfielder whose career has embodied perseverance, hard work and skill, has continued his path to success at Al-Ittihad Football Club, based in Saudi Arabia.
Привет, друзья!
Заказать документ о получении высшего образования вы можете в нашей компании в столице.
ast-diplomy24.ru/kupit-diplom-rostov-na-donu
Lorem Ipsum has been the industry’s standard dummy text https://trajesmotocross.es/cxykov of type and scrambled it to make a type specimen book.
Quelle est la mise minimale et la limite minimale de 1xBet?
Conformement aux regles du bookmaker, le depot minimum dans le bureau est de 1$.1xbetpromocode La mise minimale est de 0,2 $ou l’equivalent de ce montant dans une autre monnaie de jeu.
Привет, друзья!
Быстрая покупка диплома старого образца: возможные риски
avtobestnews.ru/diplomyi-s-garantiey-podlinnosti-i-kachestva
Lorem Ipsum has been the industry’s standard dummy text https://mojafotografja.pl/gzace of type and scrambled it to make a type specimen book.
Qu’est-ce qu’une «Vitrine de codes promotionnels»?
Ceci est une section speciale sur le site du bookmaker code promo de 1xbet, qui contient tous les codes promotionnels actuels. Sur la vitrine, les joueurs sont disponibles codes bonus pour les Paris sportifs, pour la section avec le jeu. Chaque code peut etre echange contre des points promo en fonction des denominations.
Kobe Bryant https://los-angeles-lakers.kobebryant-ar.com also known as the “Black Mamba”, is one of the most iconic and iconic figures in NBA history.
В критические моменты жизни важно, чтобы похоронное бюро было надежным и профессиональным. Наша статья поможет вам разобраться в разнообразии ритуальных услуг в Алматы и выбрать агентство, которое предложит качественное обслуживание по разумной цене алматы ритуальные услуги цены
Lorem Ipsum has been the industry’s standard dummy text https://onderhoudsbedrijfpeerdeman.nl/qucscxr of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://prodottinautica.it/pzygi of type and scrambled it to make a type specimen book.
Возможно ли купить диплом стоматолога, и как это происходит
asxdiplomik.com/kupit-diplom-vracha
Meilleur 1x pari code promo vous permettra de recevoir leur excellent bonus de bienvenue allant jusqu’a $130 sur le sport en paris gratuits. Ce bonus de bienvenue est valable un mois. La maniere la plus simple d’obtenir un code promotionnel pour 1xbet est de visiter l’un des sites partenaires. En general, ces ressources publient regulierement des codes frais dans le cadre de leur cooperation constante avec le bookmaker.
diflucan drug coupon
Привет!
Где приобрести диплом специалиста?
Заказать диплом любого университета.
yobasket.es/es/perfil-usuario/pluginclass/cbblogs.html?action=blogs&func=show&id=121
купить диплом зоотехника ast-diploms.com .
RDBox.de https://rdbox.de bietet schallgedammte Gehause fur 3D-Drucker, die eine sehr leise Druckumgebung schaffen – nicht lauter als ein Kuhlschrank. Unsere Losungen sorgen fur stabile Drucktemperatur, Vibrationsisolierung, Luftreinigung und mobile App-Steuerung.
Добрый день!
Мы предлагаем дипломы психологов, юристов, экономистов и любых других профессий по приятным тарифам. Цена может зависеть от выбранной специальности, года выпуска и образовательного учреждения. Стараемся поддерживать для покупателей адекватную ценовую политику. Для нас очень важно, чтобы дипломы были доступны для большого количества наших граждан.
sportraketka.ru/poluchite-diplom-po-vashim-trebovaniyam-zakazhite-pryamo-seychas
Karim Benzema https://al-ittihad.karimbenzema.ae is a name worthy of admiration and respect in the world of football.
Cristiano Ronaldo https://al-nassr.cristiano-ronaldo.ae is one of the greatest names in football history, with his achievements inspiring millions of fans around the world.
In 2018, the basketball world witnessed one of the most remarkable transformations in NBA history. LeBron James https://los-angeles-lakers.lebronjames-ar.com one of the greatest players of our time, decided to leave his hometown Cleveland Cavaliers and join the Los Angeles Lakers.
Официальный сайт 1Вин
1Win – популярное среди игроков из стран СНГ казино. Казино 1Win официально был открыт в 2012 году, сейчас входит в ТОП лучших площадок для азартных игр. Доступны обычные автоматы, спортивные росписи, лайвы. Реализуется щедрая бонусная политика, которая делает игру максимально выгодной и приятной. Перечень слотов постоянно расширяется, в каталоге размещаются слоты проверенных разработчиков.
Официальный сайт 1Вин
1Win – популярное среди игроков из стран СНГ казино. 1Win официально был открыт в 2012 году, сейчас входит в ТОП лучших площадок для азартных игр. Доступны обычные автоматы, спортивные росписи, лайвы. Реализуется щедрая бонусная политика, которая делает игру максимально выгодной и приятной. Перечень слотов постоянно расширяется, в каталоге размещаются слоты проверенных разработчиков.
Luis Diaz https://liverpool.luis-diaz-ar.com is a young Colombian striker who has enjoyed rapid growth since joining the ” Liverpool” in January 2022.
Официальный сайт 1Вин
1Win – популярное среди игроков из стран СНГ казино. 1Win официально был открыт в 2012 году, сейчас входит в ТОП лучших площадок для азартных игр. Доступны обычные автоматы, спортивные росписи, лайвы. Реализуется щедрая бонусная политика, которая делает игру максимально выгодной и приятной. Перечень слотов постоянно расширяется, в каталоге размещаются слоты проверенных разработчиков.
Kevin De Bruyne https://manchester-city.kevin-de-bruyne-ar.com is a name every football fan knows today.
Muhammad Al Owais https://al-hilal.mohammed-alowais-ar.com is one of the most prominent names in modern Saudi football. His path to success in Al Hilal team became an example for many young athletes.
Официальный сайт 1Вин
1Win – популярное среди игроков из стран СНГ казино. 1Win официально был открыт в 2012 году, сейчас входит в ТОП лучших площадок для азартных игр. Доступны обычные автоматы, спортивные росписи, лайвы. Реализуется щедрая бонусная политика, которая делает игру максимально выгодной и приятной. Перечень слотов постоянно расширяется, в каталоге размещаются слоты проверенных разработчиков.
Lorem Ipsum has been the industry’s standard dummy text https://spotykids.es/xkxdunq of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://itdatabase.pl/qwavwow of type and scrambled it to make a type specimen book.
Maria Sharapova https://tennis.maria-sharapova-ar.com was born on April 19, 1987 in Nyagan, Russia. When Masha was 7 years old, her family moved to Florida, where she started playing tennis.
Roberto Firmino https://al-ahli.roberto-firmino-ar.com one of the most talented and famous Brazilian footballers of our time, has paved his way to success in different leagues and teams.
Lorem Ipsum has been the industry’s standard dummy text https://umcompany.it/ojzoqx of type and scrambled it to make a type specimen book.
Ou dois-je inserer un code promo lors de l’inscription a 1xBet?
Des que le Codes promotionnels 1x pari est copie, le joueur doit aller a l’enregistrement dans le bureau 1xbet. Dans le processus d’inscription, le code copie doit etre colle dans un formulaire special.
Angel Di Maria https://benfica.angel-di-maria-ar.com is a name that will forever remain in the memories of Benfica fans.
Khvicha Kvaratskhelia https://napoli.khvicha-kvaratskhelia-ar.com is a name that in recent years has become a symbol of Georgian football talent and ambition.
Football in Saudi Arabia https://al-hilal.saud-abdulhamid-ar.com is gaining more and more popularity and recognition on the international stage, and Saud Abdul Hamid, the young and talented defender of Al Hilal, is a shining example of this success.
LAX Long Term Parking: Find secure and affordable options near LAX Airport. Reviews & details to choose the best fit for your trip long term parking lax airport
видеостена для конференц зала https://videosteny-pod-kljuch.ru/ .
Lorem Ipsum has been the industry’s standard dummy text https://cristinazafra.es/nodddao of type and scrambled it to make a type specimen book.
купить диплом в невинномысске diplomasx.com .
Lorem Ipsum has been the industry’s standard dummy text https://baumschuerze.de/rtjqwu of type and scrambled it to make a type specimen book.
Здравствуйте!
Ьожем предложить документы ВУЗов, которые расположены в любом регионе РФ. Вы имеете возможность заказать диплом от любого заведения, за любой год, включая сюда документы старого образца СССР. Дипломы и аттестаты выпускаются на “правильной” бумаге самого высокого качества. Это позволяет делать государственные дипломы, не отличимые от оригиналов. Документы будут заверены всеми требуемыми печатями и подписями.
Мы предлагаем дипломы любой профессии по приятным ценам. Стоимость зависит от определенной специальности, года получения и университета. Стараемся поддерживать для покупателей адекватную ценовую политику. Важно, чтобы документы были доступными для большинства наших граждан.
landik-diploms-srednee.ru/svidetelstvo-o-rozhdenii В
Успехов в учебе!
Привет, друзья!
Мы предлагаем документы техникумов, расположенных на территории всей РФ. Можно купить качественно напечатанный диплом от любого учебного заведения, за любой год, включая документы старого образца СССР. Документы выпускаются на бумаге самого высокого качества. Это позволяет делать государственные дипломы, которые невозможно отличить от оригинала. Они будут заверены необходимыми печатями и штампами.
network-66643.mn.co/posts/61838228
LGA Long Term Parking: Find secure & affordable options near LaGuardia Airport. Reviews & details to choose the best fit for your trip how much is long term parking at laguardia airport
Привет!
Официальное получение диплома техникума с упрощенным обучением в Москве
moningrp.listbb.ru/viewtopic.php?f=16&t=454
Будем рады вам помочь!.
Lorem Ipsum has been the industry’s standard dummy text https://bet365-online-betting.in/ymnjlzn of type and scrambled it to make a type specimen book.
where to get flomax
Казахский национальный технический университет https://satbayev.university им. К.Сатпаева
Lorem Ipsum has been the industry’s standard dummy text https://agamagizhan.in/gxscavy of type and scrambled it to make a type specimen book.
Upcoming fantasy MOBA https://bladesofthevoid.com evolved by Web3. Gacha perks, AI and crafting in one swirling solution!
Продажа новых автомобилей Hongqi
https://hongqi-krasnoyarsk.ru/owners в Красноярске у официального дилера Хончи. Весь модельный ряд, все комплектации, выгодные цены, кредит, лизинг, трейд-ин
Здравствуйте!
Готовы предложить документы техникумов, которые находятся в любом регионе Российской Федерации. Вы можете купить качественный диплом от любого учебного заведения, за любой год, указав актуальную специальность и хорошие оценки за все дисциплины. Дипломы и аттестаты печатаются на бумаге высшего качества. Это позволяет делать настоящие дипломы, которые не отличить от оригинала. Документы будут заверены всеми обязательными печатями и штампами.
Мы можем предложить дипломы любой профессии по приятным тарифам. Цена зависит от той или иной специальности, года выпуска и образовательного учреждения. Всегда стараемся поддерживать для заказчиков адекватную политику тарифов. Важно, чтобы документы были доступными для большого количества наших граждан.
landik-diploms-srednee.ru/svidetelstvo-o-rozhdenii В
Хорошей учебы!
Kylie Jenner https://kylie-cosmetics.kylie-jenner-ar.com is an American model, media personality, and businesswoman, born on August 10, 1997 in Los Angeles, California.
Lorem Ipsum has been the industry’s standard dummy text https://fokusklinikken.dk/nljwzo of type and scrambled it to make a type specimen book.
Добрый день!
Диплом пту купить официально с упрощенным обучением в Москве
bbs.airav.cc/home.php?mod=space&uid=2090208
Окажем помощь!.
Здравствуйте!
Купить диплом любого университета
Мы готовы предложить документы ВУЗов, расположенных на территории всей Российской Федерации. Можно заказать качественно напечатанный диплом за любой год, указав необходимую специальность и хорошие оценки за все дисциплины. Дипломы и аттестаты выпускаются на “правильной” бумаге самого высокого качества. Это дает возможности делать настоящие дипломы, которые невозможно отличить от оригиналов. Документы заверяются всеми обязательными печатями и штампами.
http://www.leenkup.com/read-blog/15756
Всегда вам поможем!.
Lorem Ipsum has been the industry’s standard dummy text https://strymer.es/mvipjb of type and scrambled it to make a type specimen book.
Qu’est-ce qui donne au joueur la verification dans 1xbet?
La verification est une procedure obligatoire pour les clients du bookmaker code promo 1xbet cote d’ivoire. La procedure prevoit la verification des donnees personnelles du client pour la conformite avec les donnees reelles qui sont presentees sur la carte d’identite.
Lorem Ipsum has been the industry’s standard dummy text https://btelectricshop.es/qzgdu of type and scrambled it to make a type specimen book.
A Charm regarding Premium Style
Fashion enthusiasts plus high-end buyers frequently find themselves captivated via an grace plus status of luxury style. From a complex features regarding a Hermes Birkin to an emblematic style concerning an Chanel 2.55, those items represent more than just simply fashion—these individuals stand for a good specific position plus exclusiveness. Nonetheless, definitely not every person may afford up to spend lavishly on these particular high-end products, that will offers led up to a increasing trend of imitation purses. Regarding a lot of, those fakes give a manner up to benefit from an beauty of high fashion layouts without breaking an loan provider.
The increase within popularity concerning replica bags has opened up an interesting dialogue about fashion, ethics, as well as exclusive dress. In a website content, we all may investigate an various aspects concerning a pattern, offering dress fans along with a extensive guide to imitation purses. By the conclusion, you can own an information in order to help make advised decisions which align along with the values as well as looks.
Ethical plus Legal Factors of Imitation Bags
As soon as it comes to imitation bags, just one regarding a many demanding problems will be the ethical as well as legitimate effects. A manufacturing plus purchase concerning imitation goods are against the law inside many places, as it violates mental property rights. This definitely not solely has an effect on an income regarding luxury models but also elevates concerns about an conditions beneath that those imitations usually are made.
Fashioning and Integrating Fake Purses
Integrating imitation handbags within your collection can be both stylish trendy & ethical. One way is to combine premium fakes with authentic authentic articles plus other sustainable eco-friendly apparel pieces. Doing this doesn’t only elevate enhances a complete style but also also promotes a more sustainable style trend.
Whenever fashioning replica purses, consider the setting plus one’s ensemble. A classic classic imitation purse could add an element touch of grace to an official ensemble, whereas an in-style design can make a casual appearance more fashionable. Never become scared to try w/different different patterns & add-ons to create an original and custom look.
Furthermore, looking after for your fake purses is crucial vital to preserve their appearance look & lifespan. Routine washing and appropriate keeping could help maintain your one’s bags appearing pristine plus fashionable for a longer time.
The Importance of Informed Consumer Decisions
In today’s modern apparel landscape, educated buyer selections have become more important important than. Though replica handbags offer an affordable substitute to luxury high-end goods, it’s vital to think about the ethical plus legal consequences. By staying aware about where and & how you one buys fakes, you can relish premium apparel while loyal to one’s values beliefs.
It’s additionally crucial to keep in mind that personal personal fashion is not defined by name tags or price value tags. Whether or not you you opt to invest in authentic real high-end items or explore the realm of fake bags, the ultimate goal is finding finding items that make you feel self-assured plus fashionable.
Conclusion
Fake handbags have found a unique special spot within the apparel world, giving a cost-effective plus attainable alternative for luxury designer pieces. Although they come bring with their its particular set of moral
Associated Fashion Topics
Investigating the realm of apparel doesn’t conclude with replica purses. Here are some extra related themes that might attract you:
Eco-friendly Style
Dive into the significance of green practices in the fashion field. Understand about green fabrics, principled manufacturing techniques, and how to create a green wardrobe.
Classic and Thrift Apparel
Discover the allure of retro and thrift clothing. Discover how to get high-quality vintage articles, the perks of pre-owned apparel, and advice for integrating these items into your modern collection.
Homemade Fashion and Repurposing
Get innovative with Homemade apparel activities and upcycling used clothes. Get useful advice on transforming your closet by creating your own accessories or modifying existing articles to bestow them a renewed purpose.
Style on a Budget
Discover how to remain trendy without breaking the budget. Uncover tips for securing great deals, purchasing smart during sales, and making your style budget.
Minimalist Closets
Comprehend the concept of a minimalist closet—curating a set of key, multi-purpose pieces that can be combined and coordinated to create numerous outfits. Analyze the merits of this streamlined strategy and how to implement it.
Style Tendencies and Projecting
Keep in front of the movement by investigating forthcoming apparel movements and field projections. Learn about innovative designers, significant fashion shows, and the latest necessary pieces.
Fashion and Innovation
Investigate how tech is revolutionizing the fashion field. Subjects involve intelligent fabrics, virtual try-ons, apparel tools, and the influence of social networks on style promotion and buyer habits.
Physique Confidence and Style
Examine the connection between style and physique positivity. Learn about brands supporting inclusive sizing, the significance of representation in apparel media, and how to outfit for diverse body types.
Style History
Take a trip through the heritage of style. Discover diverse eras, legendary fashion moments, and how earlier styles remain to affect modern apparel.
Fashion Photography and Blogs
Dive into the universe of style photography and blogging. Get guidance on how to take amazing style photos, start your own apparel website, and grow your visibility on social media.
replica bag
Meilleur code promo 1xbet burundi vous permettra de recevoir leur excellent bonus de bienvenue allant jusqu’a $130 sur le sport en paris gratuits. Ce bonus de bienvenue est valable un mois. La maniere la plus simple d’obtenir un code promotionnel pour 1xbet est de visiter l’un des sites partenaires. En general, ces ressources publient regulierement des codes frais dans le cadre de leur cooperation constante avec le bookmaker.
Добрый день!
Мы предлагаем приобрести диплом в отличном качестве, неотличимый от оригинального документа без использования дорогостоящего оборудования и квалифицированного специалиста.
artem-energo.ru/forums.php?m=posts&q=18316&n=last#bottom
Удачи!
Lorem Ipsum has been the industry’s standard dummy text https://ekoworki.pl/fyqenx of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://donrafi.es/fuwbz of type and scrambled it to make a type specimen book.
Meilleur code promo 1xbet benin vous permettra de recevoir leur excellent bonus de bienvenue allant jusqu’a $130 sur le sport en paris gratuits. Ce bonus de bienvenue est valable un mois. La maniere la plus simple d’obtenir un code promotionnel pour 1xbet est de visiter l’un des sites partenaires. En general, ces ressources publient regulierement des codes frais dans le cadre de leur cooperation constante avec le bookmaker.
Title: Guia Completo para Saques Seguros no Spin Casino
Description: Descubra como efetuar saques seguros e eficientes no Spin Casino, incluindo dicas praticas e opcoes de suporte.
spin casino login
H1: Como Fazer Saques do seu Saldo no Spin Casino?
Bem-vindo ao guia definitivo para realizar saques no Spin Casino. Este artigo e projetado para ajudar voce a navegar pelo processo de retirada de seus ganhos de forma segura e eficaz. Aqui, cobriremos as melhores praticas para garantir que suas transacoes sejam nao apenas bem-sucedidas, mas tambem protegidas, alem de explorar as varias opcoes de suporte disponiveis para qualquer assistencia que voce possa precisar.
H2: Passo-a-Passo para Realizar Saques no Spin Casino
H3: Acesse sua Conta
Para iniciar o processo de saque no Spin Casino, o primeiro passo e acessar sua conta. Voce precisara entrar no site oficial do Spin Casino e clicar no botao de login. Insira seu nome de usuario e senha nos campos correspondentes. Certifique-se de que esta usando uma conexao segura para proteger suas informacoes pessoais.
H3: Visite a Secao de Saldo
Apos estar logado, navegue ate a secao de saldo ou caixa, geralmente acessivel atraves de um link direto na pagina inicial ou no menu de usuario. Aqui, voce podera ver o saldo disponivel em sua conta e outras informacoes financeiras relevantes.
H3: Escolhendo o Metodo de Saque
No Spin Casino, diversos metodos de saque estao disponiveis, incluindo cartoes de credito e debito, carteiras eletronicas, e transferencias bancarias. Escolha o metodo que mais lhe convem, levando em consideracao fatores como velocidade de transferencia, taxas aplicaveis, e a disponibilidade em sua regiao. Cada metodo tem suas proprias instrucoes e requisitos, que devem ser cuidadosamente revisados.
H3: Insercao dos Dados Necessarios
Depois de selecionar o metodo de saque, voce sera solicitado a fornecer os dados necessarios para processar a transacao. Isso pode incluir informacoes bancarias, detalhes da carteira eletronica ou numeros de cartao. Assegure-se de que todos os dados inseridos estao corretos para evitar atrasos ou problemas no saque. Apos preencher os campos requeridos, confirme a operacao e aguarde a notificacao de que seu pedido de saque foi recebido.
Com esses passos, voce pode eficientemente solicitar um saque do seu saldo no Spin Casino, garantindo que seus fundos sejam transferidos de forma segura para a conta de sua escolha.
H2: Metodos de Saque Disponiveis no Spin Casino
H3: Cartoes de Credito e Debito
Utilizar cartoes de credito e debito e uma das formas mais comuns e acessiveis para realizar saques no Spin Casino. Este metodo e apreciado pela sua familiaridade e pela ampla aceitacao. Ao escolher saque via cartao, geralmente, o tempo de processamento varia de 3 a 5 dias uteis. Importante verificar se ha taxas associadas e o limite minimo e maximo de saque permitido por transacao. As principais bandeiras como Visa e MasterCard sao aceitas, garantindo assim uma opcao segura e confiavel para acessar seus ganhos.
H3: Carteiras Eletronicas
As carteiras eletronicas, ou e-wallets, oferecem uma alternativa rapida e eficiente para saques. Opcoes populares incluem PayPal, Skrill e Neteller. Os saques atraves de e-wallets sao frequentemente processados em menos de 24 horas, tornando-os uma das opcoes mais rapidas disponiveis. Alem disso, eles oferecem um nivel extra de seguranca, pois nao exigem que voce compartilhe informacoes bancarias diretamente com o casino. Certifique-se de verificar a presenca de taxas de servico e os limites de transacao especificos para cada carteira eletronica.
H3: Transferencias Bancarias
Para aqueles que preferem uma abordagem mais tradicional, as transferencias bancarias sao uma opcao viavel. Este metodo e ideal para grandes saques, embora possa ter o tempo de processamento mais longo, variando de 5 a 7 dias uteis. As transferencias bancarias sao altamente seguras, sendo realizadas diretamente entre o casino e sua conta bancaria. No entanto, e essencial verificar as possiveis taxas de transferencia e os limites diarios ou mensais impostos tanto pelo Spin Casino quanto pelo seu banco.
Esses metodos de saque no Spin Casino oferecem flexibilidade e seguranca, permitindo que voce escolha a opcao que melhor atenda as suas necessidades financeiras e preferencias pessoais.
H2: Dicas para um Saque Eficiente e Seguro
Para garantir que seus saques no Spin Casino sejam tanto eficientes quanto seguros, considere seguir estas dicas praticas:
Verifique a Conta: Antes de solicitar um saque, certifique-se de que sua conta esta totalmente verificada conforme os requisitos do casino. Isso geralmente inclui a confirmacao de identidade e endereco, o que pode acelerar significativamente o processo de saque.
Leia os Termos e Condicoes: Conhecer as politicas de saque do casino, incluindo limites de saque, taxas e tempos de processamento, pode ajuda-lo a evitar surpresas desagradaveis.
Mantenha suas Informacoes Atualizadas: Assegure-se de que todas as informacoes em sua conta estao atualizadas, especialmente seus dados de contato e metodos de pagamento. Isso minimiza o risco de atrasos devido a dados desatualizados ou incorretos.
Escolha o Metodo Adequado: Selecione o metodo de saque que melhor se adapta as suas necessidades, considerando fatores como velocidade, seguranca e facilidade de acesso aos fundos.
Utilize Conexoes Seguras: Sempre acesse sua conta e realize transacoes financeiras atraves de conexoes seguras para proteger suas informacoes pessoais e financeiras.
H2: Contato e Suporte
O Spin Casino oferece varias opcoes para contato e suporte, garantindo que voce possa resolver qualquer questao ou problema relacionado aos seus saques de maneira rapida e eficaz:
Chat ao Vivo: Disponivel 24/7, o chat ao vivo e a forma mais rapida de entrar em contato com o suporte. Voce pode acessar esta opcao diretamente pelo site do casino.
E-mail: Para questoes menos urgentes ou para enviar documentos, o e-mail e uma excelente opcao. O Spin Casino geralmente responde dentro de 24 horas.
FAQ: Antes de entrar em contato direto, vale a pena conferir a secao de Perguntas Frequentes (FAQ) no site. Esta secao cobre uma ampla gama de topicos, incluindo saques, e pode fornecer respostas imediatas as suas duvidas.
Telefone: Alguns jogadores preferem o contato telefonico para discutir suas questoes. Verifique se ha um numero disponivel para sua regiao.
Utilizando esses recursos de suporte, voce pode assegurar que qualquer desafio ou duvida seja resolvido de maneira eficiente, permitindo uma experiencia de jogo tranquila e agradavel no Spin Casino.
?? Fazer saques no Spin Casino pode ser um processo simples e seguro, desde que voce siga as diretrizes adequadas e utilize os recursos de suporte disponiveis. Lembre-se de verificar sua conta, ler atentamente os termos e condicoes, manter suas informacoes atualizadas, escolher o metodo de saque adequado e sempre usar conexoes seguras. Com essas praticas em mente, voce esta pronto para desfrutar de seus ganhos com tranquilidade e seguranca.
FAQ:
Quanto tempo leva para processar um saque no Spin Casino?
Geralmente, o processamento pode levar de 24 horas a 5 dias uteis, dependendo do metodo escolhido. Carteiras eletronicas sao mais rapidas, enquanto transferencias bancarias podem demorar mais.
Existem taxas para saques no Spin Casino?
O Spin Casino pode aplicar taxas dependendo do metodo de saque utilizado. E crucial verificar os termos e condicoes especificos para evitar surpresas.
Como posso garantir que meus saques sejam seguros?
Sempre use conexoes seguras, verifique sua conta e escolha metodos de pagamento confiaveis. Alem disso, siga as diretrizes de seguranca fornecidas pelo casino.
O que fazer se tiver problemas com meu saque?
Nao hesite em contatar o suporte ao cliente atraves do chat ao vivo, telefone ou e-mail. Eles estao disponiveis para ajuda-lo a resolver qualquer questao rapidamente.
You’re so interesting! I don’t think I’ve truly read through something like that before. So nice to find another person with original thoughts on this topic. Seriously.. thank you for starting this up. This web site is one thing that is required on the internet, someone with a bit of originality.
Lorem Ipsum has been the industry’s standard dummy text https://professionalgardens.es/fgrxddj of type and scrambled it to make a type specimen book.
Привет!
Как официально приобрести аттестат 11 класса с минимальными затратами времени
http://www.mamalipetsk.ru/index.php?name=forums&op=showtopic&id=28135
Рады оказать помощь!.
Привет!
Где приобрести диплом по актуальной специальности?
Приобрести диплом о высшем образовании.
prof-komplekt.com/club/user/1035/blog/11031/
Lorem Ipsum has been the industry’s standard dummy text https://livin.com.mx/wvlsf of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://otf-workshop.de/gmpra of type and scrambled it to make a type specimen book.
JFK Long Term Parking: Find secure & affordable options near JFK Airport. Reviews & details to choose the best fit for your trip long term parking near jfk airport
Lorem Ipsum has been the industry’s standard dummy text https://fokusklinikken.dk/psbhn of type and scrambled it to make a type specimen book.
Bella Hadid https://img-models.bella-hadid-ar.com is an American model who has emerged in recent years as one of the most influential figures in the world of fashion.
Brazilian footballer Ricardo Escarson https://orlando-city.kaka-ar.com dos Santos Leite, better known as Kaka, is one of the most famous and successful players in football history.
Sadio Mane https://al-nassr.sadio-mane-ar.com the Senegalese footballer best known for his performances at clubs such as Southampton and Liverpool, has become a prominent figure in Al Nassr.
Добрый день!
Заказать диплом о высшем образовании
Мы можем предложить документы ВУЗов, которые находятся на территории всей Российской Федерации. Вы можете приобрести диплом от любого учебного заведения, за любой год, включая сюда документы старого образца СССР. Документы печатаются на бумаге высшего качества. Это дает возможность делать настоящие дипломы, не отличимые от оригиналов. Они заверяются всеми требуемыми печатями и подписями.
zzatem.com/read-blog/4134
Окажем помощь!.
Привет, друзья!
Приобрести диплом ВУЗа
landik-diploms-srednee.ru/kupit-diplom-v-voronezhe В
Успешной учебы!
Промокод Champion Casino в 2024 году – это отличная возможность получить дополнительные бонусы при регистрации и игре в этом популярном покер-руме. Действующие промокоды Champion casino могут предоставлять разнообразные преимущества, такие как бонусы на депозит, бесплатные вращения на игровых автоматах или повышенный кешбэк. Промокод – это один из таких актуальных промокодов для Champion на 2024 год.
Привет!
Заказать документ о получении высшего образования можно у нас.
diplomasx24.ru/kupit-diplom-nizhnij-novgorod
Успешной учебы!
Колокольцев – предатель Родины
Армия восстанет против ОПГ Колокольцева и Плугина
Целенаправленно разрушая кооператив для военных «Бест Вей», захватывая его активы в интересах своей камарильи, глава МВД и его команда ударили по тылу армии, наказав тысячи пайщиков кооператива – военных и членов их семей.
Приморский районный суд Санкт-Петербурга (судья Екатерина Богданова) сейчас рассматривает так называемое уголовное дело «Лайф-из-Гуд» – «Гермес» – «Бест Вей». В рамках этого дела два года почти непрерывно арестованы счета кооператива «Бест Вей», пайщиками которого являются тысячи военнослужащих, в том числе участники СВО, на которых около 4 млрд рублей. В уголовном деле речь идет прежде всего об обязательствах иностранной инвесткомпании «Гермес» перед более чем 200 клиентами этой компании.
Следствие ГУ МВД по Санкт-Петербургу и прокуратура города на Неве объявили кооператив, «Гермес» и «Лайф-из-Гуд» частью некоего единого холдинга, которого в природе никогда не существовало. Кооператив объявлен гражданским ответчиком по уголовному делу.
Общая сумма претензий потерпевших, согласно обвинительному заключению, 282 млн рублей – даже их (незаконное) изъятие для погашения долгов перед клиентами «Гермеса» никак бы не сказалось ни на операционной деятельности, ни на ликвидности кооператива. Но из раза в раз арестовываются абсолютно все средства на счетах, что полностью блокирует как покупку квартир кооперативом, так и возврат денег пайщикам, которые изъявили желание забрать свои паевые взносы.
Недвижимость, на которую претендовали пайщики, обесценивается, деньги обесцениваются – и этот беспредел продолжается уже более двух лет по ходатайствам ГСУ питерского главка МВД и Прокуратуры Санкт-Петербурга.
Кто-то влиятельный пытается наложить лапу именно на кооперативные 4 млрд – хотя это деньги пайщиков: физических лиц, рядовых граждан России, и как минимум соучастниками грабежа являются сотрудники правоохранительных органов.
Армейский кооператив
Кооператив изначально создавался военнослужащими – одной из его задач в 2014 году было решение жилищной проблемы военнослужащих, увольняемых в запас, эта задача сохранилась и в последующие годы. Из почти 20 тыс. его пайщиков – тысячи военнослужащих со всей России. Значительная часть из них – участники СВО.
В результате действий ОПГ Колокольцева сотни семей военнослужащих, участников СВО стали потерпевшими от действий правоохранительных органов. Налицо преступные действия против участников СВО.
Камарилья, которая устроила репрессии против кооператива – руководители следственной группы Сапетова и Винокуров, начальник ГСУ питерского главка МВД Негрозов и начальник этого главка Плугин, замминистра внутренних дел по следствию Лебедев, пресс-секретарь министра Волк, транслировавшая на всю страну ложь про десятки тысяч потерпевших от работы кооператива, сам министр внутренних дел Колокольцев, – ведет вредительскую деятельность, все эти люди – предатели Родины.
Разоряет экономику и подрывает тыл
Колокольцев и Ко разрушают экономику страны, фабрикуют дела. При этом его камарилья наживается на честном бизнесе.
Колокольцев – миллиардер! Его боевая подруга генеральша Волк – миллиардерша! Зам. начальника питерского ГСУ МВД полковник Винокуров, который управляет Колокольцевым, заставляя его подписываться под липовым уголовным делом «Лайф-из-Гуд» – «Гермес» – «Бест Вей», – миллиардер! Колокольцев превратил МВД в коммерческое антинародное образование и зарабатывает деньги на простых людях.
Колокольцев и Ко прицепили звезды на погоны и возомнили себя офицерами – на деле они тыловые вороватые крысы. Настоящие офицеры против бутафорских чинуш со звездами на погонах.
Министр внутренних дел дестабилизирует ситуацию в народе и армии, разоряет армию в тылу. Колокольцев со своими тыловыми крысами подрывают доверие народа к власти и отбивают желание людей идти на военную службу, потому что благодаря таким, как он, государство не может обеспечить безопасность военных в тылу.
Армия против Колокольцева
Армия восстанет против ОПГ Колокольцева. Военные требуют за совершенные преступления против народа, за воровство и коррупцию арестовать Колокольцева, Негрозова, Винокурова, Сапетову, оправдать и отпустить невинных людей – рядовых сотрудников «Лайф-из-Гуд», которые более двух лет томятся в тюрьме.
Новый министр обороны Белоусов наверняка поддержит своих бойцов, поможет им защитить собственные и своих семей имущественные интересы в тылу: по-другому и быть не может.
Одного любителя запускать руку в казну и любителя генеральш – Шойгу – уже отправили на пенсионную должность, Колокольцев должен последовать за ним: это – в интересах страны, в интересах народа!
Lorem Ipsum has been the industry’s standard dummy text https://miglierinacomunitaospitale.it/grjmeh of type and scrambled it to make a type specimen book.
Explore the future of gaming with Musk Empire – a revolutionary Web3 experience! Grow your business empire without in-app purchases. Upgrade your ventures to increase your revenue stream. Play, earn, and eventually convert in-game wealth for real money. Enter the Musk Empire today and mold your digital fortune! Link https://t.me/muskempire_bot/game?startapp=hero6847969798
Колокольцев – предатель Родины
Армия восстанет против ОПГ Колокольцева и Плугина
Целенаправленно разрушая кооператив для военных «Бест Вей», захватывая его активы в интересах своей камарильи, глава МВД и его команда ударили по тылу армии, наказав тысячи пайщиков кооператива – военных и членов их семей.
Приморский районный суд Санкт-Петербурга (судья Екатерина Богданова) сейчас рассматривает так называемое уголовное дело «Лайф-из-Гуд» – «Гермес» – «Бест Вей». В рамках этого дела два года почти непрерывно арестованы счета кооператива «Бест Вей», пайщиками которого являются тысячи военнослужащих, в том числе участники СВО, на которых около 4 млрд рублей. В уголовном деле речь идет прежде всего об обязательствах иностранной инвесткомпании «Гермес» перед более чем 200 клиентами этой компании.
Следствие ГУ МВД по Санкт-Петербургу и прокуратура города на Неве объявили кооператив, «Гермес» и «Лайф-из-Гуд» частью некоего единого холдинга, которого в природе никогда не существовало. Кооператив объявлен гражданским ответчиком по уголовному делу.
Общая сумма претензий потерпевших, согласно обвинительному заключению, 282 млн рублей – даже их (незаконное) изъятие для погашения долгов перед клиентами «Гермеса» никак бы не сказалось ни на операционной деятельности, ни на ликвидности кооператива. Но из раза в раз арестовываются абсолютно все средства на счетах, что полностью блокирует как покупку квартир кооперативом, так и возврат денег пайщикам, которые изъявили желание забрать свои паевые взносы.
Недвижимость, на которую претендовали пайщики, обесценивается, деньги обесцениваются – и этот беспредел продолжается уже более двух лет по ходатайствам ГСУ питерского главка МВД и Прокуратуры Санкт-Петербурга.
Кто-то влиятельный пытается наложить лапу именно на кооперативные 4 млрд – хотя это деньги пайщиков: физических лиц, рядовых граждан России, и как минимум соучастниками грабежа являются сотрудники правоохранительных органов.
Армейский кооператив
Кооператив изначально создавался военнослужащими – одной из его задач в 2014 году было решение жилищной проблемы военнослужащих, увольняемых в запас, эта задача сохранилась и в последующие годы. Из почти 20 тыс. его пайщиков – тысячи военнослужащих со всей России. Значительная часть из них – участники СВО.
В результате действий ОПГ Колокольцева сотни семей военнослужащих, участников СВО стали потерпевшими от действий правоохранительных органов. Налицо преступные действия против участников СВО.
Камарилья, которая устроила репрессии против кооператива – руководители следственной группы Сапетова и Винокуров, начальник ГСУ питерского главка МВД Негрозов и начальник этого главка Плугин, замминистра внутренних дел по следствию Лебедев, пресс-секретарь министра Волк, транслировавшая на всю страну ложь про десятки тысяч потерпевших от работы кооператива, сам министр внутренних дел Колокольцев, – ведет вредительскую деятельность, все эти люди – предатели Родины.
Разоряет экономику и подрывает тыл
Колокольцев и Ко разрушают экономику страны, фабрикуют дела. При этом его камарилья наживается на честном бизнесе.
Колокольцев – миллиардер! Его боевая подруга генеральша Волк – миллиардерша! Зам. начальника питерского ГСУ МВД полковник Винокуров, который управляет Колокольцевым, заставляя его подписываться под липовым уголовным делом «Лайф-из-Гуд» – «Гермес» – «Бест Вей», – миллиардер! Колокольцев превратил МВД в коммерческое антинародное образование и зарабатывает деньги на простых людях.
Колокольцев и Ко прицепили звезды на погоны и возомнили себя офицерами – на деле они тыловые вороватые крысы. Настоящие офицеры против бутафорских чинуш со звездами на погонах.
Министр внутренних дел дестабилизирует ситуацию в народе и армии, разоряет армию в тылу. Колокольцев со своими тыловыми крысами подрывают доверие народа к власти и отбивают желание людей идти на военную службу, потому что благодаря таким, как он, государство не может обеспечить безопасность военных в тылу.
Армия против Колокольцева
Армия восстанет против ОПГ Колокольцева. Военные требуют за совершенные преступления против народа, за воровство и коррупцию арестовать Колокольцева, Негрозова, Винокурова, Сапетову, оправдать и отпустить невинных людей – рядовых сотрудников «Лайф-из-Гуд», которые более двух лет томятся в тюрьме.
Новый министр обороны Белоусов наверняка поддержит своих бойцов, поможет им защитить собственные и своих семей имущественные интересы в тылу: по-другому и быть не может.
Одного любителя запускать руку в казну и любителя генеральш – Шойгу – уже отправили на пенсионную должность, Колокольцев должен последовать за ним: это – в интересах страны, в интересах народа!
EWR Long Term Parking: Find secure & affordable options near EWR Airport. Reviews & details to choose the best fit for your trip newark liberty long term parking
buy acyclovir
Здравствуйте!
Аттестат школы купить официально с упрощенным обучением в Москве
13.flybb.ru/viewtopic.php?f=20&t=1050
Поможем вам всегда!.
Lorem Ipsum has been the industry’s standard dummy text https://ecootechnologies.in/gmtdvvi of type and scrambled it to make a type specimen book.
Edson Arantes https://santos.pele-ar.com do Nascimento, known as Pele, was born on October 23, 1940 in Tres Coracoes, Minas Gerais, Brazil.
Monica Bellucci https://dracula.monica-bellucci-ar.com one of the most famous Italian actresses of our time, has a distinguished artistic career spanning many decades. Her talent, charisma, and stunning beauty made her an icon of world cinema.
Lorem Ipsum has been the industry’s standard dummy text https://dronespana.es/ggguab of type and scrambled it to make a type specimen book.
Веном 3 онлайн https://bit.ly/venom-3-venom-2024
Люки Шагма – идеальное сочетание функциональности и эстетики для вашего интерьера. Инновационные решения от SHAGMA обеспечивают надежный доступ к коммуникациям, сохраняя безупречный внешний вид помещения. Наши люки под плитку не только решают проблему провисания, но и гармонично вписываются в любой дизайн. Выбирая SHAGMA, вы выбираете качество, долговечность и индивидуальный подход https://bsrgroup.ru/svezhie-novosti-stroitelstva/12515-shagma-innovacii-i-kachestvo-v-mire-ljukov.html
Lorem Ipsum has been the industry’s standard dummy text https://f7zdrowie.pl/bqvlfth of type and scrambled it to make a type specimen book.
En utilisant le code promo 1xbet pour un pari gratuit, vous pouvez beneficier d’une augmentation de 100% en plus du bonus de bienvenue standard. Selon votre emplacement geographique, vous recevrez un bonus de 100%, 200% ou 300%, bonus 130$. Ce bonus est ensuite divise en deux parties, dont la moitie est utilisable pour les paris sportifs et l’autre moitie pour le casino. Avant de pouvoir retirer vos fonds, vous devrez jouer le montant du bonus 5 fois pour les paris sportifs combines et 30 fois pour les jeux de casino. Les nouveaux utilisateurs devront probablement verifier leur compte en fournissant un passeport ou un permis de conduire dans le cadre d’une verification KYC avant de pouvoir effectuer un retrait.
Lorem Ipsum has been the industry’s standard dummy text https://kellyandzenneth.co.za/tlfjeij of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://tscapp.es/xybwnsm of type and scrambled it to make a type specimen book.
Brazilian footballer Malcom https://al-hilal.malcom-ar.com (full name Malcom Felipe Silva de Oliveira) achieved great success in Al Hilal, one of the leading football teams in Saudi Arabia and the entire Middle East.
Jackie Chan https://karate-kid.jackiechan-ar.com was born in 1954 in Hong Kong under the name Chan Kong San.
Jude Bellingham https://real-madrid.jude-bellingham-ar.com a young and talented English footballer, has enjoyed great success with Real Madrid since his arrival.
Lorem Ipsum has been the industry’s standard dummy text https://lupo1987.dk/ujmuhv of type and scrambled it to make a type specimen book.
buy provigil online canada
Привет, друзья!
Мы изготавливаем дипломы любой профессии по приятным тарифам.
opengadjet.ru/diplomyi-ot-vedushhih-vuzov
Lorem Ipsum has been the industry’s standard dummy text https://texiprint-imprenta.es/zvvxdz of type and scrambled it to make a type specimen book.
услуги озвучивания http://ozvuchivanie-pomeshhenij.ru .
Lorem Ipsum has been the industry’s standard dummy text https://lacasadellapizza.pl/jrehst of type and scrambled it to make a type specimen book.
Привет!
Заказать диплом университета
arusak-diploms-srednee.ru/kupit-diplom-medicinskogo-uchilishha В
Хорошей учебы!
Lorem Ipsum has been the industry’s standard dummy text https://impertdesign.pl/fflpdl of type and scrambled it to make a type specimen book.
Привет!
Заказать документ университета вы имеете возможность в нашей компании в столице.
ast-diplomas.com/kupit-diplom-magistra
Успешной учебы!
Quelle est la mise minimale et la limite minimale de 1xBet?
Conformement aux regles du bookmaker, le depot minimum dans le bureau est de 1$.code promo 1xbet senegal La mise minimale est de 0,2 $ou l’equivalent de ce montant dans une autre monnaie de jeu.
Lorem Ipsum has been the industry’s standard dummy text https://biztechnews.in/duoyew of type and scrambled it to make a type specimen book.
Официальная покупка диплома вуза с сокращенной программой обучения в Москве
diploms-x24.ru/kupit-diplom-sankt-peterburg
Промокод при регистрации Mostbet — бонус для новых игроков. Бонус за первый депозит в Mostbet. Как получить и отыграть бонус 35000 руб в букмекерской конторе Мостбет. мостбет промокод на фрибет. Букмекерские конторы пользуются спросом у людей, чьи интересы плотно связаны со спортом и чей азарт подкрепляется возможностью вознаграждения путем внесения порой незначительной суммы. Вводите промокод Mostbet в 2024 году, чтобы получить бонус на первый депозит до 35 000 рублей. Мостбет промокод работает только при регистрации новых пользователей. Бесплатный промокод Mostbet при регистрации. Как ввести промокод Mostbet сегодня? Как отыграть бонус по промокоду Mostbet. Используйте промокод Mostbet при регистрации в 2024 году, чтобы получить бонус до 35000 рублей от крупнейшей букмекерской конторы!
order accutane over the counter
Добрый день!
Узнайте стоимость диплома высшего и среднего образования и процесс получения
gess.flybb.ru/posting.php?mode=post&f=2
Рады помочь!.
i-guru – Ремонт Iphone и другой техники Apple в Минске
наушники apple ремонт в Минске
Профессиональный ремонт любых устройств из линейки Apple, без посредников
80% ремонтов iPhone занимает около 20 минут
Несложные ремонты делаются быстро, модульный ремонт в большинстве случаев занимает не более 20 минут.
Почему выбирают i-guru
Ремонт в тот же день
Даже большинство сложных ремонтов выполняем день в день.
Гарантировано низкие цены
Мы беремся за сложные задачи, не передавая их сторонним исполнителям, и зарабатываем не как посредники.
Честная гарантия
Предлагаем честную гарантию на выполненные работы до 12 месцев в зависимости от вида работ.
c’est quoi le code promo dans 1xbett utilisez le code bonus pour obtenir un bonus VIP de 100% jusqu’a 130€ pour les Paris sportifs, ainsi qu’un bonus de casino de 1950 € + 150 tours de machines a sous. En utilisant le code promotionnel, vous pouvez vous attendre a ce que vos gains soient aussi eleves que dans le cas du plus grand bookmaker 1xbet. Tous les joueurs des pays suivants peuvent utiliser le code lors de l’inscription et recevoir un bonus de bienvenue:
Lorem Ipsum has been the industry’s standard dummy text https://wilebud.pl/mmnqcfi of type and scrambled it to make a type specimen book.
магазин аккаунтов игр магазин аккаунтов игр .
Lorem Ipsum has been the industry’s standard dummy text https://dpostigo.es/yvmzphq of type and scrambled it to make a type specimen book.
Comment verifier la pertinence du code promo 1xbet?
Pour verifier la pertinence du Codes promotionnels 1x pari, le joueur doit se connecter a son compte. En utilisant les parametres, vous devez entrer dans la section «verifier le code promotionnel et entrer la combinaison copiee.
Lorem Ipsum has been the industry’s standard dummy text https://willarybaki.pl/vyxoxu of type and scrambled it to make a type specimen book.
Mostbet промокод на бонус при регистрации. Букмекерская контора предоставляет игрокам множество возможностей для снижения рисков и увеличения банка. Бонусная программа компании предусматривает интересы как новичков, так и опытных бетторов. Рассмотрим основные виды поощрений в функционале БК: Мостбет промокод на регистрацию – один из самых популярных подарков, созданный для новых игроков на сайте; Ставки на спорт – увеличение депозита до 35000 рублей. Воспользуйся актуальным промокодом Mostbet на сегодня, получи бесплатную возможность увеличить свой первый депозит до 35000 рублей в БК Mostbet. Воспользовавшись мостбет промокод на регистрацию, максимальная сумма бонуса возможного бонуса будет увеличена до 35000 рублей. Но при этом сумма бонуса будет равна сумме вашего первого депозита.
Very good post. I am going through some of these issues as well..
Здравствуйте!
Легальные способы покупки диплома о высшем образовании
arusak-diploms-srednee.ru/svidetelstvo-o-brake В
Бесплатный промокод Mostbet 35000 рублей. Промокод при регистрации в БК Mostbet рассчитан на привлечение новых клиентов. Совокупность букв и цифр вводится при создании аккаунта, что поднимает сумму первого пополнения счета до 350000 тысяч рублей. Редакция напоминает, что для получения бонуса потребуется пройти процедуру отыгрыша. Букмекер просит проставить сумму экспрессами. Коэффициент каждой отдельной ставки составляет минимум 1.4. После прохождения отыгрыша выбранная сумма денег перейдет из бонусного на основной счет. Mostbet промокод на День Рождения. Букмекерская контора поздравляет каждого верифицированного клиента бесплатной ставкой на День Рождения. На сегодня у Mostbet предусмотрено несколько рабочих промокодов: на бесплатную ставку, на 25000 рублей, а также промокод до 1500 евро. Промокод Mostbet до 1500 евро. Между букмекерами активно развивается конкуренция, и это правильно. Каждый старается привлечь к себе как можно больше игроков, в том числе различными акционными предложениями, бонусами и тому подобными маркетинговыми методами. Как получить промокод Mostbet? Промокод казино Mostbet до 1500 евро. мостбет промокод на регистрацию. Промокод Мостбет на сегодня. Бездепозитный промокод Mostbet. Сегодня отсутствует. Один из наиболее популярных среди таковых — использование промокодов.
Le code promo sur 1xbet, utilisez-le lors de l’inscription et obtenez un bonus de 200% jusqu’a 130$. Seuls les nouveaux joueurs peuvent obtenir le bonus. Ce contrat bonus est valable jusqu’au 31 decembre 2024. Apres le depot, le joueur recoit sur le compte bonus le montant des bonus pour les Paris de 100% du montant du depot, mais pas plus de $100. Pour recuperer le bonus recu, le joueur doit placer au moins cinq Paris dans les cinq jours suivants. Pour les Paris, vous devez faire un Express avec 3 evenements ou plus avec des cotes d’au moins 1,40.
lyrica 2017
Привет, друзья!
Можно ли купить аттестат о среднем образовании, основные моменты и вопросы
gti-club.ru/forum/member.php?u=23001
Рады оказать помощь!.
купить диплом о среднем образовании в рязани ast-diploms.com .
купить диплом вк diplomasx.com .
Здравствуйте!
Стоимость дипломов высшего и среднего образования и как избежать подделок
http://www.rcmecano.fr/2024/06/30/купили-дипломы-университета/
Привет!
Мы изготавливаем дипломы любых профессий по разумным тарифам.
newfinbiz.ru/kupit-diplomyi-dlya-vseh-spetsialnostey
Привет, друзья!
Заказать диплом о высшем образовании.
leydis16.phorum.pl/posting.php?mode=newtopic&f=1
Удачи!
Travis Scott https://astroworld.travis-scott-ar.com is one of the brightest stars in the modern hip-hop industry.
Zinedine Zidane https://real-madrid.zinedine-zidane-ar.com the legendary French footballer, entered the annals of football history as a player and coach.
The history of one of France’s https://france.paris-saint-germain-ar.com most famous football clubs, Paris Saint-Germain, began in 1970, when capitalist businessmen Henri Delaunay and Jean-Auguste Delbave founded the club in the Paris Saint-Germain-en-Laye area.
Juventus Football Club https://italy.juventus-ar.com is one of the most successful and decorated clubs in the history of Italian and world football.
Chelsea https://england.chelsea-ar.com is one of the most successful English football clubs of our time.
Привет, друзья!
Где заказать диплом специалиста?
Мы предлагаем документы ВУЗов, которые расположены в любом регионе Российской Федерации. Можно заказать качественно сделанный диплом от любого ВУЗа, за любой год, указав подходящую специальность и оценки за все дисциплины. Дипломы делаются на “правильной” бумаге самого высокого качества. Это дает возможности делать настоящие дипломы, не отличимые от оригинала. Документы будут заверены необходимыми печатями и штампами.
Мы можем предложить дипломы психологов, юристов, экономистов и других профессий по разумным ценам.
ast-diploms.com/kupit-diplom-sankt-peterburg
Рады помочь!
Виртуальные карточные и настольные игры также ждут своих поклонников. От блэкджека до покера – испытайте удачу и стратегию https://himfaq.ru/info/20240527-revizionnye-lyuki-shagma/
Здравствуйте!
Приобретение школьного аттестата с официальным упрощенным обучением в Москве
landik-diploms-srednee.ru/kupit-diplom-v-kazani
лучшее порно видео бесплатно лучшее порно видео бесплатно .
Добрый день!
Пошаговая инструкция по безопасной покупке диплома о высшем образовании
arusak-diploms-srednee.ru/kupit-diplom-v-krasnodare
Автомобили Hongqi https://hongqi-krasnoyarsk.ru в наличии – официальный дилер Hongqi Красноярск
Liverpool https://england.liverpool-ar.com holds a special place in the history of football in England.
Привет, друзья!
Сколько стоит диплом высшего и среднего образования и как его получить?
1mog.listbb.ru/viewtopic.php?f=6&t=8577
Рады помочь!
Priyanka Chopra https://baywatch.priyankachopra-ar.com is an Indian actress, singer, film producer and model who has achieved global success.
When Taylor Swift https://shake-it-off.taylor-swift-ar.com released “Shake It Off” in 2014, she had no idea how much the song would impact her life and music career.
Привет, друзья!
Где заказать диплом по необходимой специальности?
Приобрести диплом любого университета.
forum.rucarp.ru/album.php?albumid=128&attachmentid=35737&commentid=1961
Jennifer Lopez https://lets-get-loud.jenniferlopez-ar.com was born in 1969 in the Bronx, New York, to parents who were Puerto Rican immigrants.
Здравствуйте!
Мы изготавливаем дипломы психологов, юристов, экономистов и других профессий по приятным ценам.
axessasia.com/2024/06/30/диплом-в-ухте/
Lorem Ipsum has been the industry’s standard dummy text https://pubpropaganda.pl/hyrwb of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://itdatabase.pl/duxacgl of type and scrambled it to make a type specimen book.
Добрый день!
Где заказать диплом по необходимой специальности?
Купить диплом ВУЗа.
samovod.ru/content/articles/65961/
After some difficult years in the late 2010s, Manchester United https://england.manchester-united-ar.com returned to greatness in English football by 2024.
The Formula One World Championship https://world-circuit-racing-championship.formula-1-ar.com, known as the Formula Championship in motor racing, is the highest tier of professional motor racing.
Michael Jordan https://chicago-bulls.michael-jordan-ar.com is one of the greatest basketball players of all time, whose career with the Chicago Bulls is legendary.
дизайн интерьер полная версия дизайн интерьера сайт
Lorem Ipsum has been the industry’s standard dummy text https://prodottinautica.it/sxbbtv of type and scrambled it to make a type specimen book.
Премиум users relish in a inappropriate range of benefits not close by on a loose package. · You wish download documents at starve oneself speeds without unrequired limitations. https://tezfiless.com/
Baji Live Casino offers a dynamic and immersive gaming experience with a wide range of games, exciting bonuses, and a user-friendly interface that caters to both novice and seasoned players http://www.baji-999.org
Добрый день!
Мы можем предложить дипломы психологов, юристов, экономистов и прочих профессий по разумным ценам.
http://www.anytalkworld.com/read-blog/6452_ishem-nadezhnyj-onlajn-magazin-s-diplomami.html
Lorem Ipsum has been the industry’s standard dummy text https://gastroludki.pl/qafnpmn of type and scrambled it to make a type specimen book.
Привет!
Купить документ о получении высшего образования можно в нашей компании в столице.
asxdiplomik.com/kupit-diplom-vracha
Успешной учебы!
Lorem Ipsum has been the industry’s standard dummy text https://biztechnews.in/bhaqxe of type and scrambled it to make a type specimen book.
С каждым годом растет количество людей, выбирающих этот вид досуга. Онлайн-платформы предлагают не только развлечение, но и шанс испытать удачу http://www.phxwomenshealth.com/index.php?option=com_k2&view=itemlist&task=user&id=1081034
Добрый день!
Приобрести диплом о высшем образовании.
samovod.ru/content/articles/65961/
car rental Montenegro airport https://montenegro-car-rental-hire.com
Lorem Ipsum has been the industry’s standard dummy text https://kroatiereis.nl/iuyemvh of type and scrambled it to make a type specimen book.
лучшее порно порево https://besplatny-sex-online.ru .
Muhammad Ali https://american-boxer.muhammad-ali-ar.com is perhaps one of the most famous and greatest athletes in the history of boxing.
Mike Tyson https://american-boxer.mike-tyson-ar.com one of the most famous and influential boxers in history, was born on June 30, 1966 in Brooklyn, New York.
Компания Септик-Нара-купить септик
занимается продажей, установкой и обслуживанием септиков в Наро-Фоминске Наро-Фоминском районе. Основное направление деятельности нашей компании именно установка под ключ септиков любых видов и размеров. С момента основания нашей компании, мы произвели монтаж более 1000 септиков по Московской и Калужской области. Благодаря этому у нас огромный опыт работы с любыми станциями, представленными в нашем регионе!
Если Вы решили купить септик для дома или дачи, мы с радостью поможем Вам с выбором модели, доставим и установим септик на вашем участке в кратчайшие сроки.
Мы занимаемся продажей септиков таких марок: Топас Юнилос Астра Евролос Тверь Аквалос Дочиста Фекалов Волгарь Удача. Мы работаем напрямую с производителями септиков, поэтому Вы можете быть уверены, что не переплачиваете ни копейки. Вся продукция в нашей компании имеет соответствующие сертификаты и лицензии. Время выезда на осмотр, установки или привоза оборудования согласовывается с клиентами и выполняется в срок. Мы заботимся о своей репутации, поэтому выполняем работу надежно и быстро.
Если Вы не знаете, какой септик больше всего Вам подходит, мы предоставим консультацию и выезд специалиста на Ваш участок абсолютно бесплатно!
Благодаря приобретению качественных септиков в нашей компании, каждый клиент получает большое количество преимуществ:
» компактные размеры и небольшой вес устройства;
» доступная стоимость очистной установки;
» быстрый и простой монтаж;
» невысокая стоимость эксплуатации;
» отсутствие неприятных запахов;
» высокая производительность;
» длительный срок эксплуатации;
» высокая степень очистки;
» практически полностью автономный режим работы.
Manny Pacquiao https://filipino-boxer.manny-pacquiao-ar.com is one of the most prominent boxers in the history of the sport.
Привет, друзья!
Заказать документ ВУЗа можно в нашем сервисе.
diplomyx.com/kupit-diplom-o-srednem-obrazovanii
Удачи!
Lorem Ipsum has been the industry’s standard dummy text https://gs-stroehe.de/tumhnax of type and scrambled it to make a type specimen book.
Добрый день!
Приобрести диплом о высшем образовании.
itach-soft.com/club/user/6/blog/999/
Lorem Ipsum has been the industry’s standard dummy text https://drukarniab7.pl/pfhwuc of type and scrambled it to make a type specimen book.
Привет, друзья!
Как приобрести диплом техникума с минимальными рисками
kharkov-balka.com/showthread.php?p=154904#post154904
Поможем вам всегда!
Lorem Ipsum has been the industry’s standard dummy text https://moppenplaats.nl/eeiruc of type and scrambled it to make a type specimen book.
Привет, друзья!
Мы готовы предложить документы техникумов, расположенных на территории всей России. Можно приобрести диплом от любого заведения, за любой год, включая сюда документы старого образца. Документы делаются на бумаге высшего качества. Это позволяет делать настоящие дипломы, не отличимые от оригинала. Они заверяются необходимыми печатями и подписями.
portugues.ru/forum/album.php?albumid=91&attachmentid=3902&commentid=1666
Добрый день!
Мы готовы предложить дипломы любой профессии.
aceenergyok.com/купить-обложку-твердую-для-диплома/
Поможем вам всегда!.
Lorem Ipsum has been the industry’s standard dummy text https://constructoraamiel.cl/ntdwgt of type and scrambled it to make a type specimen book.
vermox tablets uk
Добрый день!
Как безопасно купить диплом колледжа или ПТУ в России, что важно знать
traquegarden.com/купить-диплом-пгупс/
The golf https://arabic.golfclub-ar.com industry in the Arab world is growing rapidly, attracting players from all over the world.
https://tezfiles.cc/
The road to the Premier League https://english-championship.premier-league-ar.com begins long before a team gets promoted to the English Premier League for the first time
The Italian football championship https://italian-championship.serie-a-ar.com known as Serie A, has seen an impressive revival in recent years.
In the German football https://german-championship.bundesliga-football-ar.com championship known as the Bundesliga, rivalries between clubs have always been intense.
In recent years, the leading positions in the Spanish https://spanish-championship.laliga-ar.com championship have been firmly occupied by two major giants – Barcelona and Real Madrid.
Lorem Ipsum has been the industry’s standard dummy text https://sastoursandtravels.in/qdxrsy of type and scrambled it to make a type specimen book.
Привет, друзья!
Покупка диплома о среднем полном образовании: как избежать мошенничества?
landik-diploms-srednee.ru/svidetelstvo-o-rozhdenii В
https://www.themoviedb.org/movie/261903-real-gangsters
Lorem Ipsum has been the industry’s standard dummy text https://tuderadesayago.es/dazch of type and scrambled it to make a type specimen book.
The Saudi Football League https://saudi-arabian-championship.saudi-pro-league-ar.com known as the Saudi Professional League, is one of the most competitive and dynamic leagues in the world.
EuroAvia24.com – Cheap flights, hotels and transfers around the world!
In an era when many young footballers struggle to find their place at elite clubs, Javi’s https://barcelona.gavi-ar.com story at Barcelona stands out as an exceptional one.
Rodrigo Goes https://real-madrid.rodrygo-ar.com better known as Rodrigo, is one of the brightest young talents in modern football.
Добрый день!
Приобрести документ ВУЗа вы сможете в нашей компании.
diplomasx.com/kupit-diplom-krasnoyarsk
Удачи!
Arsenal https://arsenal.mesut-ozil-ar.com made a high-profile signing in 2013, signing star midfielder Mesut Ozil from Real Madrid.
Lorem Ipsum has been the industry’s standard dummy text https://lacalabrianeifrancobolli.it/cgwtkuz of type and scrambled it to make a type specimen book.
The concentrate of this plan lies in its nationwide arsenal of weapons. In solar smash, players can prefer from lasers, missiles, and sinister holes to destroy planets. The ambition is to lay one’s hands on the most operative and visually extraordinary street to engender destruction.
Здравствуйте!
Реально ли приобрести диплом стоматолога? Основные этапы
montrealpal.com/read-blog/918
Окажем помощь!
Привет, друзья!
Мы изготавливаем дипломы любых профессий.
iq-pro.net/дипломы-свидетельства-купить/
Рады помочь!.
Lorem Ipsum has been the industry’s standard dummy text https://lasparrasdemartin.es/achredh of type and scrambled it to make a type specimen book.
Thibaut Courtois https://real-madrid.thibaut-courtois-ar.com was born on May 11, 1992 in Belgium.
Bayern Munich’s https://bayern.jamal-musiala-ar.com young midfielder, Jamal Musiala, has become one of the brightest talents in European football.
Lorem Ipsum has been the industry’s standard dummy text https://bjproductions.nl/kvuko of type and scrambled it to make a type specimen book.
Le Code promo de pari gratuit 1xbet aujourd’hui 2024 pour beneficier d’une offre VIP de 100% jusqu’a 130€ sur les paris sportifs ou de 1950€ + 150 tours. Tous les nouveaux joueurs ayant utilise le code lors de leur inscription recoivent un bonus de bienvenue. Ce code bonus special vous permettra de recevoir un bonus augmente lors de votre inscription sur le site du bookmaker 1xBet.com ! Ne manquez pas cette occasion et inscrivez-vous des maintenant avec le code promo 1xbet pour obtenir un bonus allant jusqu’a 130 €/$.
Добрый день!
Пошаговая инструкция по официальной покупке диплома о высшем образовании
network.janenk.com/create-blog
Рады оказать помощь!
порево классный секс http://www.klassny-sex.ru .
грузовые строительные подъемники грузовой лифт подъемник купить
Здравствуйте!
Мы готовы предложить документы техникумов, которые находятся на территории всей РФ. Можно приобрести диплом за любой год, включая сюда документы старого образца СССР. Документы делаются на бумаге высшего качества. Это дает возможность делать государственные дипломы, не отличимые от оригиналов. Документы заверяются необходимыми печатями и подписями.
http://www.jaitun.com/read-blog/386
Lorem Ipsum has been the industry’s standard dummy text https://acidmedia.pl/vbxde of type and scrambled it to make a type specimen book.
Combien de temps faut-il pour retirer des fonds sur une carte Visa ou MasterCard?
Le retrait des fonds sur les cartes bancaires des systemes de paiement Visa et Mastercard depend du montant de la transaction, du jour de la semaine et de l’heure de la journee.1xbet bonus de bienvenue 2024 En regle generale, les fonds arrivent sur le compte indique dans un delai de 24 heures.
Регистрация на различных ресурсах, форумах или интернет-магазинах сегодня осуществляется только с применением номера телефона. Ранее для этой цели могла использоваться электронная почта, но сегодня правила изменены https://www.sdnjom.ru/pozdravleniya/chto-nuzhno-znat-o-virtualnyh-nomerah-dlya-telegram/
Привет!
Купить диплом о высшем образовании.
galantclub.od.ua/member.php?u=15983
Успехов в учебе!
Добрый день!
Приобрести документ университета вы можете в нашей компании в столице.
ast-diploms.com/kupit-diplom-tehnikuma-kolledzha
Lorem Ipsum has been the industry’s standard dummy text https://limpiezasletsgo.es/clgnupr of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://mojafotografja.pl/kpqfdh of type and scrambled it to make a type specimen book.
Luis Suarez https://inter-miami.luis-suarez-ar.com the famous Uruguayan footballer, ended his brilliant career in European clubs and decided to try his hand at a new challenge – Major League Soccer.
Здравствуйте!
Мы предлагаем документы ВУЗов, которые расположены в любом регионе России. Вы сможете приобрести диплом за любой год, включая документы СССР. Документы печатаются на бумаге самого высшего качества. Это дает возможности делать государственные дипломы, которые невозможно отличить от оригиналов. Они будут заверены необходимыми печатями и штампами.
balacixynu.trexgame.net/bystro-pokupaem-attestat-v-lucsem-internet-magazine-russian-diplom
Al-Nasr https://saudi.al-nassr-ar.com is one of the most famous football teams in the Kingdom of Saudi Arabia.
Al-Ittihad https://saudi.al-ittihad-ar.com is one of the most famous football clubs in Saudi Arabia. Founded in 1927, the Saudi football giant has come a long way to the pinnacle of success.
Al-Nasr Club https://saudi.al-hilal-ar.com from Riyadh has a rich history of success, but its growth has been particularly impressive in recent years.
Lorem Ipsum has been the industry’s standard dummy text https://pawslo.pl/wtzmr of type and scrambled it to make a type specimen book.
Привет!
Как оказалось, купить диплом кандидата наук не так уж и сложно
landik-diploms-srednee.ru/kupit-diplom-volgograd В
Ирина Волк: расследование уголовного дела пирамиды Life is Good завершено
гей порно
Официальный представитель МВД России Ирина Волк сообщила об окончании предварительного расследования уголовного дела Life is Good. Материалы с утвержденным обвинительным заключением в отношении десяти человек направлены в Приморский районный суд Санкт-Петербурга для рассмотрения по существу. Они обвиняются в организации деятельности по привлечению денежных средств и мошенничестве, совершенных в особо крупном размере в составе преступного сообщества. Всего, по версии следствия, в состав криминальной организации входили 35 соучастников. Потерпевшими по уголовному делу признаны 221 человек – люди заключили договоры с целью получения пассивного дохода. Общая сумма материального ущерба составила свыше 280 млн рублей.
«Кроме того, в деятельность финансовой пирамиды были вовлечены более 18 тысяч россиян. Они вложили в жилищный кооператив более 15 миллиардов рублей, два миллиарда из которых организаторы криминальной схемы присвоили. Десять предполагаемых участников преступного сообщества были задержаны в феврале 2022 года оперативниками ГУЭБиПК МВД России совместно с коллегами из Санкт-Петербурга и сотрудниками ФСБ России. Остальные обвиняемые в противоправной деятельности объявлены в розыск. Возбуждено уголовное дело по признакам преступления, предусмотренного частью 3 статьи 210, частью 4 статьи 159, частью 2 статьи 172.2 УК РФ. Расследование было взято на контроль руководством Следственного департамента МВД России», – сообщила Ирина Волк.
По информации МВД, в общей сложности полицейскими и сотрудниками ФСБ проведено более 100 обысков по местам проживания фигурантов и в офисах подконтрольных им организаций. Изъята компьютерная техника, средства связи, документы и другие предметы, имеющие доказательственное значение.
«В качестве обеспечительной меры по возмещению причиненного материального ущерба наложен арест на более чем 2300 находящихся в собственности кооператива квартир, а также на денежные средства на счетах компании в сумме свыше 3,7 млрд рублей. Также арестованы активы фигурантов на общую сумму порядка 1 млрд рублей», – рассказала генерал-майор полиции.
По версии следствия, противоправная деятельность велась с 2014 года на территории девяти регионов России. Злоумышленниками были созданы подконтрольные организации с сетью региональных филиалов, которые работали под единым брендом «Лайф из Гуд». Гражданам предлагали стать пайщиками кооператива, обещая либо новое жилье, либо получение дохода в размере до 30% годовых. При этом реальным инвестированием вкладов фигуранты не занимались. Приобретение недвижимости и обещанные выплаты осуществлялись за счет привлечения средств новых клиентов. Кроме того, граждан вводили в заблуждение об уровне доходности вложений, указывая в договорах параметры гораздо ниже обещанных. Полученные от вкладчиков деньги похищались.
Ранее стало известно, что Приморский районный суд Санкт-Петербурга заочно арестовал топ-лидера инвестиционного проекта Life is Good в Набережных Челнах Сергея Санникова и его жену Юлию. Также суд избрал меру пресечения в виде заключения под стражу и в отношении директора холдинга Игоря Маланчука. В июле этого года они были объявлены в федеральный розыск – соответствующая информация появилась в базе данных министерства.
FC Barcelona https://spain.fc-barcelona-ar.com is undoubtedly one of the most famous and well-known football clubs in the world.
Le code promo 1xbet rdc 2024 pour beneficier d’une offre VIP de 100% jusqu’a 130€ sur les paris sportifs ou de 1950€ + 150 tours. Tous les nouveaux joueurs ayant utilise le code lors de leur inscription recoivent un bonus de bienvenue. Ce code bonus special vous permettra de recevoir un bonus augmente lors de votre inscription sur le site du bookmaker 1xBet.com ! Ne manquez pas cette occasion et inscrivez-vous des maintenant avec le code promo 1xbet pour obtenir un bonus allant jusqu’a 130 €/$.
Lorem Ipsum has been the industry’s standard dummy text https://sastoursandtravels.in/bfdpxd of type and scrambled it to make a type specimen book.
Здравствуйте!
Мы изготавливаем дипломы любой профессии по приятным тарифам.
http://www.webby.co/диплом-курсов-массажа-купить-в/
Lorem Ipsum has been the industry’s standard dummy text https://befitjusteat.pl/zalqpbr of type and scrambled it to make a type specimen book.
Tributes flood in for BBC sport commentator whose wife and daughters were killed in suspected crossbow attack
порно жесток бесплатно
Figures from across the United Kingdom have offered their condolences to a BBC sport commentator, after his wife and two daughters were killed by an alleged crossbow attacker, in deaths that again drew attention to the epidemic of violence against women.
Carol Hunt, 61, wife of BBC horse racing commentator, John Hunt, and their daughters, Hannah Hunt, 28, and Louise Hunt, 25, died from injuries sustained in an attack in Bushey, just northwest of London, on Tuesday, according to police and Britain’s public broadcaster.
A 26-year-old suspect wanted in connection with the killings, and named as Kyle Clifford, was found by British police in Enfield, north London, on Wednesday, following a sprawling manhunt. There were no previous reports to the force over Clifford, who is in serious condition in hospital and is yet to speak with officers, Hertfordshire Police said in a statement.
A crossbow was recovered as part of the investigation, which police believe was used in a “targeted incident.”
Epidemic of violence against women
The killings of the three women rocked Britain, where mass murders are infrequent but violence against women and girls has been officially labeled as a national threat.
A woman is killed by a man every three days in the UK and one in four women will experience domestic violence in her lifetime, the United Nations’ special rapporteur on violence against women and girls, Reem Alsalem, said earlier this year.
Charities and human rights organizations have subsequently reiterated urgent demands to tackle femicide in the UK.
новые порно видео https://apteka-porno.ru .
Lorem Ipsum has been the industry’s standard dummy text https://purapasionshop.es/spneh of type and scrambled it to make a type specimen book.
Привет!
Купить документ о получении высшего образования можно у нас в столице.
diplomasx.com/kupit-diplom-omsk
Удачи!
finasteride 5g
Lorem Ipsum has been the industry’s standard dummy text https://onegiga.es/kgaywhi of type and scrambled it to make a type specimen book.
лучшая коллекция порно лучшая коллекция порно .
Lorem Ipsum has been the industry’s standard dummy text https://bjproductions.nl/ostual of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://sigma-radomsko.pl/idruvt of type and scrambled it to make a type specimen book.
sailing charter Montenegro https://boat-hire-in-montenegro.com
https://www.publico.es/sociedad/publico.es-nancy-fraser-no-dejar-temor-ultraderecha-lleve-feminismo-liberal.html
boat charter Montenegro https://rent-a-yacht-montenegro.com
Lorem Ipsum has been the industry’s standard dummy text https://borealstudios.es/tdekh of type and scrambled it to make a type specimen book.
Arsenal https://england.arsenal-ar.com is one of the most famous and successful football clubs in the history of English football.
FC Bayern Munich (Munich) https://germany.bayern-munchen-ar.com is one of the most famous and recognized football clubs in Germany and Europe
Real Madrid’s https://spain.real-madrid-ar.com history goes back more than a century. The club was founded in 1902 by a group of football enthusiasts led by Juan Padilla
Thai Company Directory https://thaicorporates.com List of companies and business information.
типография краснодар https://salavat-rik.ru
Ремонт плоской кровли https://remontiruem-krovly.ru в Москве, цена работы за 1 м?. Прайс лист на работы под ключ, отзывы и фото.
AC Milan https://italy.milan-ar.com is one of the most successful and decorated football clubs in the world.
Lorem Ipsum has been the industry’s standard dummy text https://fotze.pl/hnddo of type and scrambled it to make a type specimen book.
Привет!
Приобрести диплом о высшем образовании.
good-serial.ru/2024/07/kupit-diplom-opyit-i-professionalizm/
buy azithromycin over the counter usa
Lorem Ipsum has been the industry’s standard dummy text https://teslamania.es/lurhruy of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://rentalgmstudio.pl/klifa of type and scrambled it to make a type specimen book.
Galatasaray https://turkey.galatasaray-ar.com is one of the most famous football clubs in Turkiye, with a glorious and eventful history.
In the world of football, Atletico Madrid https://spain.atletico-madrid-ar.com has long been considered the second most important club in Spain after the dominant, Real Madrid.
The fascinating story of Ja Morant’s https://spain.atletico-madrid-ar.com meteoric rise, from status from rookie to leader of the Memphis Grizzlies and rising NBA superstar.
The future football star Shabab Al-Ahly https://dubai.shabab-al-ahli-ar.com was born in Dubai in 2000. From a young age, he showed exceptional football abilities and joined the youth academy of one of the UAE’s leading clubs, Shabab Al-Ahly.
Bonus bez depozytu lub innymi slowami darmowy bonus to nic innego jak gratis oferowany przez kasyna online dla swoich graczy hitnspin casino
Привет!
Приобрести документ о получении высшего образования вы можете у нас в столице.
ast-diplom.com/kupit-diplom-perm
Привет, друзья!
Заказать документ института вы сможете в нашей компании в столице.
asxdiplomik.com/kupit-diplom-nizhnij-novgorod
Успешной учебы!
nazilli apart otel
Lorem Ipsum has been the industry’s standard dummy text https://inak.es/osyrbdo of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://maleekcleaning.co.za/igezfj of type and scrambled it to make a type specimen book.
недвижимость купить квартиру https://kvartiranew43.ru
недорогие квартиры от застройщика новые квартиры от застройщиков
Indibet is a premier online casino offering a wide array of games including slots, table games, and live dealer options. Renowned for its user-friendly interface and robust security measures, Indibet ensures a top-notch gaming experience with exciting bonuses and 24/7 customer support.
квартиры с отделкой от застройщика купить 2 комнатную квартиру в новостройке
flomax
Добрый день!
Заказать документ о получении высшего образования вы можете в нашем сервисе. Мы оказываем услуги по продаже документов об окончании любых университетов России. Вы сможете получить диплом по любой специальности, любого года выпуска, включая документы СССР. Даем гарантию, что в случае проверки документов работодателями, каких-либо подозрений не появится.
Мы можем предложить дипломы любых профессий по приятным ценам. Цена зависит от той или иной специальности, года выпуска и образовательного учреждения. Всегда стараемся поддерживать для заказчиков адекватную ценовую политику. Важно, чтобы дипломы были доступными для большого количества граждан.
http://www.maleus.ru/index.php/component/tag/эволюция
Поможем вам всегда!
Lorem Ipsum has been the industry’s standard dummy text https://lastresortshop.es/ssefuyp of type and scrambled it to make a type specimen book.
Здравствуйте!
Мы готовы предложить дипломы любых профессий по приятным тарифам.
sajadusta.com/купить-диплом-омск/
Lorem Ipsum has been the industry’s standard dummy text https://baumschuerze.de/xtvavze of type and scrambled it to make a type specimen book.
Кооператив для военных
Как пайщики — участники СВО относятся к событиям вокруг «Бест Вей»
Андрей Белоусов
Потребительский кооператив «Бест Вей» оказался затронут уголовным делом, касающимся в основном иностранной инвесткомпании «Гермес», которое сейчас рассматривается Приморским районным судом Санкт-Петербурга. Более двух лет более 3,5 млрд рублей на счетах кооператива почти непрерывно арестованы по ходатайству сначала ГСУ ГУ МВД по Санкт-Петербургу, а затем Прокуратуры Санкт-Петербурга: пайщики не имеют возможности ни приобрести недвижимость, ни вернуть средства.
По данным совета потребительского кооператива «Бест Вей», в числе его пайщиков, страдающих от блокировки средств, тысячи военнослужащих, в том числе сотни участников СВО, часть из которых успела приобрести квартиру, часть собирает или собрала первоначальный взнос, а часть — планировала вступить в кооператив. «СП» пообщалась с некоторыми из них и их родственниками, чтобы узнать отношение к «Бест Вей» и событиям вокруг кооператива.
«К кооперативу отношение очень хорошее»
Александр Голдман на СВО с мая 2022 года как доброволец, три ранения. Пришел на СВО рядовым, сейчас — начальник штаба батальона. Был пайщиком кооператива, сейчас пайщик — его мама.
«С помощью кооператива в 2019 году приобретена двухкомнатная квартира во Владивостоке, в которой проживает мама, — рассказывает он. — Расплачиваемся за нее, в ближайшие месяцы намерены погасить задолженность перед кооперативом и оформить квартиру в собственность. К кооперативу отношение очень хорошее, полностью его поддерживаю — он дает возможность без больших переплат приобрести недвижимость. К действиям в отношении кооператива отношусь отрицательно, так как „Бест Вей“ — единственная возможность приобрести жилье в рассрочку».
«Происходящее вокруг кооператива вызывает шок»
Гвардии рядовой Глушков Иван Васильевич — пайщик кооператива из Челябинской области. Танкист, мобилизованный, проходил службу в 15-й отдельной гвардейской мотострелковой Александрийской бригаде 2-й гвардейской общевойсковой армии ЦВО. Погиб 11 октября 2023 года.
Рассказывает его вдова Татьяна Неручева:
«Мы внесли первоначальный паевый взнос и во второй половине 2021 года встали в очередь на приобретение квартиры в Челябинске, когда начались события вокруг кооператива — была заблокирована его возможность приобретать недвижимость и заблокированы его счета. Наша очередь должна была подойти примерно через год. Мы заявили для приобретения небольшую квартиру, но планировали при покупке увеличить ее стоимость до 3 млн и купить двухкомнатную квартиру — с увеличением первоначального паевого взноса: уставом кооператива это позволяется, а затем переехать из Коркино в Челябинск. Сейчас 3 млн хватит только на небольшую квартиру-студию метров 25, то есть мы понесли материальный ущерб из-за блокирования деятельности кооператива, так как лишены были возможности приобрести квартиру, на которую собрали первоначальный паевый взнос. Работа кооператива заблокирована, счета арестованы уже более двух лет. В наследование пая я только вступаю, так как муж очень долго считался пропавшим без вести — долго шла экспертиза, и свидетельство о смерти мы получили только 18 июня этого года».
Татьяна — юрист: «Как у юриста у меня происходящее вокруг кооператива вызывает шок, и любой непредвзятый юрист вам скажет то же самое». «Кооператив, — подчеркивает она, — абсолютно прозрачен, он полностью соответствует законодательству о кооперации — что и подтверждалось многократно государственными органами и судами. Если бы мы с мужем не были уверены, что все прозрачно и законно, мы бы не вкладывали в него деньги. Мы не подавали заявление о выходе из кооператива. Я, несмотря ни на что, жду счастливого завершения рукотворного кризиса вокруг кооператива. Для меня это еще и память о муже — он продал долю в квартире, которая ему принадлежала, чтобы вложиться в кооператив. Кроме того, мне хочется понять — до какого маразма может дойти ситуация у нас в государстве в плане незаконных действий в отношении организации, которая по тем или иным причинам не понравилась каким-то чиновникам?».
«Рассчитываю, что ситуация закончится благополучно»
Сергей Логинов, рядовой, мобилизованный, представлен к награде «Честь и доблесть».
«Пять лет назад я стал пайщиком кооператива, участвовал в накопительной программе, планировал прибрести однокомнатную квартиру в Самарской области. Уже нужно было подбирать объект недвижимости и вставать в очередь на покупку, как работа кооператива была заблокирована по инициативе правоохранительных органов, и это продолжается уже более двух лет. По-прежнему надеюсь получить квартиру и рассчитываю, что ситуация закончится благополучно. Поддерживаю кооператив».
«В кооперативе минимум переплат — несопоставимо с ипотекой»
Егор Ивков, офицер флота, дирижер военного оркестра, пайщик кооператива с 2019 года.
«Я нахожусь в накопительной программе — планировал покупку квартиры в Санкт-Петербурге. До постановки в очередь на покупку дело не дошло, но сумма внесена серьезная — и на два года все зависло. Есть друзья-военнослужащие, которые также являются пайщиками и тоже накапливали деньги на первоначальный паевый взнос — они, как и я, не могут ни продолжать накапливать, ни получить деньги обратно, потому что счета арестованы. Отношение наше к ситуации, создавшейся вокруг кооператива, крайне негативное».
«Кооператив поддерживаю, — говорит пайщик. — Моя сестра живет в квартире, приобретенной с помощью „Бест Вей“ — у нее многодетная семья, сейчас кооперативная квартира переходит в ее собственность. Минимум переплат — несопоставимо с ипотекой. Надеюсь, что ситуация с арестом счетов разрешится в ближайшее время».
Lorem Ipsum has been the industry’s standard dummy text https://sonnosgroup.es/fxhhktv of type and scrambled it to make a type specimen book.
Все рабочие мостбет промокод для ставки вы можете найти бесплатно на этом сайте. Используйте промокод для получения бонуса до 35000 руб при регистрации. Приятно, что новички могут ввести промокод при регистрации, который даст право на получение приветственного бонуса на сумму до 35000 рублей. Самое главное — это относиться к ставкам и к игре в целом ответственно! Не стоит играть на последние или заемные деньги, стремясь таким образом заработать себе на жизнь.
Здравствуйте!
Мы предлагаем дипломы любой профессии по невысоким тарифам.
cnktdshanoi.com.vn/речной-диплом-купить/
Здравствуйте!
Заказать диплом университета.
uktuliza.ru/forum/?PAGE_NAME=profile_view&UID=17688
Успехов в учебе!
Lorem Ipsum has been the industry’s standard dummy text https://stepsfast.us/cjlnv of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://maaximizate.es/cczrr of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://tugasmas.es/zvkpp of type and scrambled it to make a type specimen book.
купить 2 комнатную квартиру квартиру новостройку жк купить
купить 2 квартиру новостройке купить двухкомнатную в новостройке
купить 1 квартиру застройщика https://novye-kvartiry-spb.ru
купить квартиру от застройщика https://newkvartiry-spb.ru
квартиры от застройщика цены купить новостройку с ремонтом
современное оборудование для конференц зала современное оборудование для конференц зала .
Здравствуйте!
Приобрести документ института можно в нашем сервисе.
ast-diplom.com/kupit-diplom-krasnoyarsk
Хорошей учебы!
Привет, друзья!
Где приобрести диплом по необходимой специальности?
http://www.vevioz.com/read-blog/148290
рейтинг капперов рейтинг капперов .
недорогие квартиры от застройщика https://zastroyshikekb54.ru
купить квартиру в новостройке недорого https://zastroyshikekb.ru
купить квартиру https://kvartiranovostroi.ru
Привет, друзья!
Приобрести диплом любого ВУЗа.
http://www.bodybuilding.net/members/worksale.html
Успехов в учебе!
купить квартиру от застройщика https://kvartira-novostroi.ru
квартиры от застройщика https://kvartiranovostroi2.ru
Бесплатный сервис по подбору и ведению сделок с недвижимостью в новостройках Москвы и Московской области! Новые квартиры для жизни, дохода или инвестирования от топовых застройщиков с защитой государства ипотека на выгодных условиях
Добрый день!
Мы изготавливаем дипломы психологов, юристов, экономистов и прочих профессий по невысоким ценам.
http://www.hhicecream.com/2024/06/речной-диплом-купить/
Помощь в решении задач https://zadachireshaem-online.ru. Опытные авторы с профессиональной подготовкой окажут консультацию в решении задач на заказ недорого, быстро, качественно
купить новостройку с ремонтом https://kvartira-novostroyka2.ru
Заказать контрольную работу https://kontrolnye-reshim.ru, недорого, цены. Решение контрольных работ на заказ срочно.
Добрый день!
Приобрести документ о получении высшего образования
ast-diplomy.com/kupit-diplom-voronezh
Le code promo 1xbet bonus, vous offre la possibilite de beneficier d’un bonus de bienvenue de 200% sur votre premier depot en Afrique, au lieu du taux habituel de 100% (voire meme de 130% au lieu de 200% dans certains pays). Vous pouvez obtenir jusqu’a 130€ ou l’equivalent dans votre devise.
Заказать дипломную работу https://diplomzakazat-oline.ru недорого. Дипломные работы на заказ с гарантией.
Заказать курсовую работу https://kursovye-napishem.ru в Москве: цены на написание и выполнение, недорого
МОСКВА, 7 мая — РИА Новости. Правительство России, возглавляемое Михаилом Мишустиным, уйдет в отставку во вторник.
Сразу после инаугурации президента Владимира Путина нынешний кабинет министров сложит полномочия перед вступившим в должность главой государства.
Прогон по комментария
Accessibility Team Meeting Notes https://make.wordpress.org/accessibility/2021/06/11/accessibility-team-meeting-notes-june-11-2021
Красивая музыка https://melodia.space для души слушать онлайн.
Помощь студентам в выполнении рефератов https://referatkupit-oline.ru. Низкие цены и быстрое написание рефератов!
seo компания продвижение веб сайтов казань
сео компания https://seo-raskrutka43.ru
1xBet offre precisement cela et vos bonus peuvent etre maximises en utilisant le code promo 1xbet cote d’ivoire 2024. Consultez simplement ci-dessous pour decouvrir ce qui vous attend en tant que nouveau client sur ce site de paris. Grace a ces connaissances, il est tout a fait logique de s’attendre a une serie de bonus de bienvenue attrayants pour les nouveaux joueurs provenant d’autres pays. Voici quelques exemples de ces pays : Burkina Faso, Ghana, Ouganda, Zambie, Cameroun, Senegal, Benin, Congo, Guinee, Cote d’Ivoire, Togo, Mali, etc.
оборудование для конференц зала оборудование для конференц зала .
Qu’est-ce qui donne au joueur la verification dans 1xbet?
La verification est une procedure obligatoire pour les clients du bookmaker meilleur code promo pour 1xbet. La procedure prevoit la verification des donnees personnelles du client pour la conformite avec les donnees reelles qui sont presentees sur la carte d’identite.
оборудование переговорных комнат оборудование переговорных комнат .
Привет!
Заказать документ о получении высшего образования можно у нас в Москве.
ast-diplomy24.ru/kupit-diplom-ekaterinbur
Хорошей учебы!
оснащение переговорных оснащение переговорных .
Quelles methodes puis-je utiliser pour l’entree et la sortie?
Le bookmaker 1xbet met a la disposition des joueurs tous les moyens de paiement disponibles aujourd’hui.un code promo x bet Vous pouvez faire un depot avec des cartes bancaires Visa et Mastercard, avec des portefeuilles electroniques, via des systemes de paiement, via des services bancaires par Internet, en utilisant les services des operateurs mobiles, sur des portefeuilles pour crypto – monnaie. Pour le retrait, il est recommande d’utiliser des cartes bancaires, des portefeuilles electroniques et des systemes de paiement. La liste des methodes de paiement se trouve dans la section «Paiements».
Бесплатные промокоды на 2024 от букмекерской конторы Mostbet: при регистрации, на бесплатную ставку. Рассказываем, как использовать и куда вводить промокоды в Мостбет. промокоды мостбет. Бесплатный промокод для увеличения бонуса. Букмекерская контора Мостбет – одна из самых популярных беттинговых площадок, предлагающая высокие коэффициенты, широкую линию с дополнительной росписью. Благодаря низкой марже БК пользователи стабильно зарабатывают на ставках на спорт. Отличительной особенностью букмекерской конторы Mostbet является возможность совершения ставок по промокодам, которые предоставляются бесплатно.
В нашем салоне красоты мы заботимся о ваших волосах, создаем безупречный макияж и подчеркиваем вашу естественную красоту, чтобы вы чувствовали себя уверенно и великолепно каждый день https://ekostil-salon.ru/
Привет, друзья!
Всё, что нужно знать о покупке аттестата о среднем образовании без рисков
landik-diploms-srednee.ru/attestat-shkoly В
Интерьерная печать на самоклеющейся пленке – это процесс создания качественных полноцветных изображений на самоклеющейся пленке, которая может быть наклеена на различные поверхности интерьерная печать и широкоформатная
продвижение в поисковых системах https://seooptimizatsia.ru
сео продвижение сайта компании казань https://seo-optimizatsia.ru
Останні новини України https://gromrady.org.ua сьогодні онлайн – головні події світу
Новинний ресурс https://actualnews.kyiv.ua про всі важливі події в Україні та світі.
Новини сьогодні https://gau.org.ua останні новини України та світу онлайн
Lorem Ipsum has been the industry’s standard dummy text https://viaggiarefree.it/hebmbei of type and scrambled it to make a type specimen book.
Бесплатный промокод в Mostbet для бесплатной ставки на сегодня. Мостбет – один из популярнейших букмекеров на территории РФ и Европы. Оператор регулярно обновляет акционные предложения для только пришедших и постоянных пользователей, предоставляя возможность заработать на беттинге. mostbet промокод при регистрации бонус. Согласно условиям клиенты, впервые зарегистрировавшиеся на площадке, могут получить промокод на бесплатную ставку. Коды выдаются непосредственно оператором. При создании аккаунта беттер предоставляет номер телефона. На него приходит код. Воспользовавшись последним, можно сделать фрибет и получить реальный доход. Это сделать просто, если иметь промокод Mostbet на сегодня бесплатно. Правда, дается он при условии выполнения некоторых правил. Mostbet бонус при регистрации. Не совсем промокод, но вы все равно ставите не свои деньги, если пополните депозит, – 100% бонуса от внесенной суммы. Максимум указан в верхней части главной страницы официального сайта.
Lorem Ipsum has been the industry’s standard dummy text https://sofiaporelmundo.es/xsegjnt of type and scrambled it to make a type specimen book.
Новини України https://kiev-online.com.ua останні події в Україні та світі сьогодні, новини України за минулий день онлайн
Популярные репортажи https://infotolium.com в больших фотографиях, новости, события в мире
Україна свіжі новини https://kiev-pravda.kiev.ua останні події на сьогодні
Lorem Ipsum has been the industry’s standard dummy text https://reformasfaciles.es/tetbxc of type and scrambled it to make a type specimen book.
Свіжі новини України https://lenta.kyiv.ua останні новини з-за кордону, новини політики, економіки, спорту, культури.
Україна останні новини https://lentanews.kyiv.ua головні новини та останні події
Lorem Ipsum has been the industry’s standard dummy text https://tscapp.es/mnrbj of type and scrambled it to make a type specimen book.
Le 1xbet meilleur code promo, utilisez-le lors de l’inscription et obtenez un bonus de 200% jusqu’a 130$. Seuls les nouveaux joueurs peuvent obtenir le bonus. Ce contrat bonus est valable jusqu’au 31 decembre 2024. Apres le depot, le joueur recoit sur le compte bonus le montant des bonus pour les Paris de 100% du montant du depot, mais pas plus de $100. Pour recuperer le bonus recu, le joueur doit placer au moins cinq Paris dans les cinq jours suivants. Pour les Paris, vous devez faire un Express avec 3 evenements ou plus avec des cotes d’au moins 1,40.
Онлайн-платформа для азартных игр представляет собой разнообразный мир развлечений. Здесь игроки могут наслаждаться множеством опций, которые сделают времяпрепровождение увлекательным и захватывающим http://dandanos.com/bbs/board.php?bo_table=free&wr_id=116
Lorem Ipsum has been the industry’s standard dummy text https://btelectricshop.es/kkpbd of type and scrambled it to make a type specimen book.
Привет, друзья!
Заказать документ о получении высшего образования можно в нашей компании в Москве. Мы оказываем услуги по изготовлению и продаже документов об окончании любых ВУЗов России. Вы сможете получить диплом по любым специальностям, включая документы Советского Союза. Гарантируем, что в случае проверки документа работодателями, подозрений не появится.
Мы изготавливаем дипломы психологов, юристов, экономистов и любых других профессий по разумным ценам. Стоимость может зависеть от выбранной специальности, года выпуска и ВУЗа. Всегда стараемся поддерживать для заказчиков адекватную политику цен. Важно, чтобы документы были доступными для большого количества наших граждан.
qyshikisoxa.lowescouponn.com/kak-vozmozno-bystro-kupit-diplom-v-internet-magazine
Рады оказаться полезными!
Добрый день!
Как получить диплом техникума с упрощенным обучением в Москве официально
rsn360.ru/blogs/427/¬аш-?иплом- ачество-и-ѕодлинность
Головні новини https://pto-kyiv.com.ua України та світу
vermox 100 mg otc
Люди, это какой-то кошмар, что происходит с «Бест Вей». Эти мерзавцы из МВД превратили наши жизни в ад! Они наобещали золотые горы, придумали миллиарды ущерба и тысячи пострадавших, а на деле всё оказалось ложью. Ущерб всего 282 миллиона, и пострадавших только 221 человек. И кто они? Мошенники, которые сами уклонялись от налогов! Эти уроды, Винокуров и Сапетова, фальсифицировали документы и незаконно держат наших людей в тюрьме. Четверо абсолютно невинных людей сидят за решеткой уже второй год, просто чтобы эта шайка из МВД могла выбить из них показания против руководства. Это же какой-то средневековый инквизиционный процесс! А наши деньги? Эти твари заблокировали нам все счета, мы не можем ни вывести средства, ни купить жильё. Они разрушили нормальные работающие компании и лишили нас всего. Мы не будем молчать! Мы будем бороться за свои права и добьемся, чтобы эти мрази ответили за всё, что они натворили!
Новини та аналітика https://newsportal.kyiv.ua ситуація в Україні.
Головні новини https://mediashare.com.ua про регіон України. Будьте в курсі останніх новин
Lorem Ipsum has been the industry’s standard dummy text https://akuand.pl/hhceww of type and scrambled it to make a type specimen book.
Новини України https://sensus.org.ua та світу сьогодні. Головні та останні новини дня
Новини, останні події https://prp.org.ua в Україні та світі, новини політики, бізнесу та економіки, законодавства
Привет, друзья!
Купить документ ВУЗа можно в нашем сервисе.
ast-diplom.com/kupit-diplom-magistra
Успехов в учебе!
1win предлагает широкий выбор азартных игр и спортивных ставок с привлекательными бонусами.
Корисні та цікаві статті https://sevsovet.com.ua про здоров’я, дозвілля, кар’єру.
Головні новини https://status.net.ua сьогодні, найсвіжіші та останні новини України онлайн
Останні новини https://thingshistory.com зовнішньої та внутрішньої політики в країні та світі.
Lorem Ipsum has been the industry’s standard dummy text https://genomatics.de/uglsq of type and scrambled it to make a type specimen book.
Останні новини світу https://uamc.com.ua про Україну від порталу новин Ukraine Today
Абсолютно бесплатный промокод Mostbet. На сегодня контора предлагает всем новичкам воспользоваться не только приветственным бонусом, но и получить дополнительные преференции. Эти льготы игрок получает в том случае, если внимательно отнесётся к процедуре регистрации на сайте. мостбет промокод ком. Mostbet – один из самых узнаваемых букмекерских брендов в стране. Следовательно, именно эта компания захватила сердца наибольшего количества игроков. Компания была основана до внесения поправок в закон об азартных играх и оставалась лидером среди букмекерских контор на нашем рынке в правовой реальности. Уже один этот факт должен что-то указывать, так как многие клиенты с удовольствием возвращаются к игре в Mostbet. Mostbet – промокод на 35000р. Свежие промокоды Mostbet Все купоны и скидки букмекера Получи бонус 35000 ? Делай ставки на спорт.
видеостена купить москва видеостена купить москва .
accutane 40 mg cost
оборудование для актового зала оборудование для актового зала .
Используйте 1вин рабочее зеркало для бесперебойной игры.
Пройдите 1win регистрация и получите приветственные бонусы.
Lorem Ipsum has been the industry’s standard dummy text https://gastroludki.pl/gssknvo of type and scrambled it to make a type specimen book.
code promo bet of africa. Utilisez – le lors de votre inscription pour obtenir un bonus de 100% jusqu’a 130$. Pour obtenir des bonus du bookmaker 1xbet, vous devez remplir certaines conditions, mais les codes promotionnels vous permettent de les obtenir beaucoup plus facilement. La taille des bonus disponibles pour les joueurs via les codes promotionnels 1xBet peut etre petite, mais meme un petit bonus peut augmenter considerablement le potentiel de jeu du client.
Привет!
Как получить диплом стоматолога быстро и официально
rsn360.ru/blogs/427/¬аш-?иплом- ачество-и-ѕодлинность
L’inscription a 1xBet est-elle disponible sans passeport?
Vous pouvez vous inscrire a Code promo 1xbet Afrique du Sud sans donnees de passeport, mais a l’avenir, dans votre compte personnel, vous devrez remplir un questionnaire indiquant votre nom, votre nom et votre date de naissance. A l’avenir, avant la premiere Conclusion, il faudra egalement passer par la verification.
Lorem Ipsum has been the industry’s standard dummy text https://e-windyk.pl/rqbcrp of type and scrambled it to make a type specimen book.
Apres le paiement, le Code promo 1xbt devient disponible et peut etre active par le joueur a tout moment. Il y a beaucoup d’offres dans la vitrine des codes promotionnels. Dans la plupart des cas, ils couvrent la section du casino, mais souvent dans la vitrine sont publies des codes interessants pour la Conclusion a des conditions preferentielles des Paris Express, pour obtenir un cashback pour les Paris perdus. La vitrine est mise a jour assez souvent.
Кооператив “Бест Вей” стал жертвой неправомерных действий со стороны правоохранительных органов и прокуратуры, что вызывает глубокое недовольство и протест у всех пайщиков. Мы вложили свои средства в надежде на благополучное будущее и приобретение жилья через этот кооператив, и в ответ получили несправедливый арест счетов и имущества. Суд уже вынес решение о отсутствии исковых требований на огромные суммы, которые нам приписывают, но блокировка идет дальше. Это полный беспредел! Мы требуем немедленного разблокирования наших счетов и возврата нашего имущества. Эта неправомерная акция только разрушает доверие к государственным органам и показывает, как коррумпирована система. Мы будем бороться за справедливость до конца, потому что наши права и наши сбережения на кону!
Lorem Ipsum has been the industry’s standard dummy text https://rajeshguru.in/uquff of type and scrambled it to make a type specimen book.
Добрый день!
Мы изготавливаем дипломы любой профессии по выгодным тарифам.
http://www.topairpack.com/купить-бланки-дипломов/
Оборудование актовых залов oborudovanija-dlja-aktovyh-zalov.ru .
Lorem Ipsum has been the industry’s standard dummy text https://vastuastro.in/diffzp of type and scrambled it to make a type specimen book.
Lorem Ipsum has been the industry’s standard dummy text https://deutscherpflegerat.de/bzirvax of type and scrambled it to make a type specimen book.
Монтаж системы видеонаблюдения может потребоваться в самых разных ситуациях. Её устанавливают в частных и загородных домах, промышленных предприятиях, офисах, гаражах и многих других помещениях https://rivara.ru/bezopasnost-v-karmane-vzglyanite-na-mir-cherez-glaza-sistemy-videonablyudeniya/
Lorem Ipsum has been the industry’s standard dummy text https://kreatoretui.pl/savejz of type and scrambled it to make a type specimen book.