CASE REPORTS
Year: 2018 I Volume: 1 I Issue: 2 I Page: 61-63
Carbon Baby Syndrome: A Rare Case Report
Dr. B.B. Mahajan1, Dr. Jyoti Budhwar2, Dr. Parul Chojer3, Dr. Chetna Singla3
1 Professor, Department of Dermatology, Venereology and Leprology, Government Medical College, Amritsar
2 Senior Resident, Department of Dermatology, Venereology and Leprology, Government Medical College, Amritsar.
3 Junior Resident, Department of Dermatology, Venereology and Leprology, Government Medical College, Amritsar
Corresponding Author:
Dr. Parul Chojer
Department of Dermatology, Venereology and Leprology, Circular Road, Government Medical College, Amritsar
Email: parul199019@gmail.com
How to cite this article:
Mahajan BB, Budhwar J, Chojer P, Singla C. Carbon Baby syndrome: a rare case report. JDA Indian Journal of Clinical Dermatology 2018;2:61-63.
Abstract:
Carbon baby syndrome, also known as universal acquired melanosis is one of the causes of diffuse hyperpigmentation of skin and mucosa with only a limited number of cases reported in the literature. Here we report a case of 11 month old female child of universal acquired melanosis. Increased pigmentation as noticed by the parents started over the face, which then gradually progressed over next 4-5 months to involve the whole body. Clinically the case was diagnosed as carbon baby syndrome, thus being reported because of its rarity.
Key words: Carbon baby, Universal Acquired Melanosis
Introduction:
Carbon baby syndrome is an extremely rare condition which is characterised by progressive pigmentation of the skin during childhood, resembling that seen in black races. The major determinant of normal skin colour is the melanin, produced by melanocytes of basal layer of epidermis. Melanin production normally is not maximal in the newborn skin. As a result, all babies, irrespective of race, may look slightly tanned or red in color at birth. Within the ?rst few weeks, racial color becomes more evident because melanin production is stimulated by exposure to light.1 This case is being reported here for its unusual occurrence.
Case Report:
An eleven month old female child born of non-consanguineous marriage was brought to dermatology OPD with complaints of progressive darkening of whole body. Her mother had uneventful prenatal, natal and postnatal periods. The pigmentation was noticed by the parents at the age of 21 days over face and then gradually progressed over next 4-5 months to involve whole body. There was no history of fever, skin infection, darkening of urine, photosensitivity or any other systemic complaints. There was no history of drug intake prior to onset of hyperpigmentation. Past and family history was unremarkable. Elder sisters were normal.
O n e x a m i n a t i o n , c h i l d h a d g e n e r a l i s e d d i f f u s e hyperpigmentation over whole body. Face showed patchy areas of normal skin. The sun exposed areas were darker than sun protected areas (figures 1-4).
Discussion:
There are multiple causes of diffuse hyperpigmentation of the skin in infancy. Classi?cations based on both clinical and histological findings increase the accuracy of diagnosis.
 |
Figure 1-4: Generalised diffuse hyperpigmentation over whole body. Face shows patchy areas of normal skin |
Generalised pigmentation in a child may be seen in a variety of disorders which can be clinically differentiated.1,2 Ruiz- Maldonado described a single case of progressive hyperpigmentation in which a child developed pigmentation at
 |
Figure 5: Dermoscopic examination at 20X magni?cation under polarised light showing accentuation of pigmentation over extremities (red arrow) |
the age of three months and became jet black by the age of 4 years. He described him as “carbon baby”. Histological examination of this patient showed heavy melanin deposition throughout the epidermis with minimal dermal pigmentation. There was no increase in the number of melanocytes.3 Our patients showed similar clinical features. Kaviarasan et al.9 reported a similar case in a 3-year-old Indian girl who developed progressive diffuse hyperpigmentation by the age of 5 months. Histopathology revealed increased melanin deposition in epidermal basal layer.
Furuya and Mishima4 reported a Japanese child with progressive pigmentary disorder. This child developed hyperpigmentation at the age of 3 months. At 4 years of age the child was mentally retarded with partial hyperpigmentation of the body. Biopsy revealed hyperkeratosis, papillomatosis and proliferation of melanocytes. Familial progressive hyperpigmentation has been described in kindred. This condition is characterized by hyperpigmented patches that are present since birth and increase in size and number as the infant grows. Most of the skin and mucous membrane surface show increased pigmentation. Microscopically, the melanin granules are more numerous and larger than normal.5
Familial progressive hyperpigmentation was excluded in our patient as the skin lesions were not seen at birth. Kint et al.6 described two cases of congenital diffuse melanosis in which the patients developed hyperpigmentation shortly after birth which invaded progressively the trunk and limbs. The pigmentation was diffuse on the abdomen but reticulated on the neck and groin. On electron microscopy, they found the melanosomes were not grouped within the keratinocytes but dispersed within the cytoplasm of the epidermal cells.6
A d r e n o l e u k o d y s t r o p h y, a n X – l i n k e d a c q u i r e d neurodegenerative disease characterised by generalized hyperpigmentation with a slowly progressive involvement of the brain and adrenals. Patient develops uniform macular hyperpigmentation which spares the palms and groin area. This disease is characterized by the accumulation of unsaturated fatty acids with a chain of 24-30 carbons, particularly hexacosanoate in the adrenal cortex and in certain sphingolipids of the brain.10
Bronze baby syndrome is a rare acquired generalized pigmentary disorder which occurs in the neonates. It is characterized by gray-brown discoloration and occurs in patients with hepatocellular dysfunction undergoing phototherapy. Porphyrin compound undergoes photo destruction which results in a brown substance that is deposited in the skin.7
In reticulate acropigmentation of Kitamura freckle-like pigmentation appears on the dorsa of hands which spread all over the body later. It manifests in the ?rst two decades of life. In Haber syndrome, there is rosacea-like eruption with keratotic plaques and pitted scars. Acropigmentation of Dohi shows symmetrical dyschromatosis of extremities.
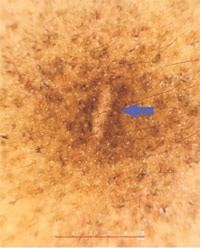 |
Figure 6: Dermoscopic examination at 20X magni?cation under polarised light revealing granular brownish deposits over trunk- epidermal pigmentation (blue arrow) |
Franceschetti-Jadassohn-Naegeli syndrome starts as reticulate pigmentation during the second or third year associated with palmo-plantar keratoderma and hypohidrosis with intolerance to heat. In Cantu syndrome brown macules develop in adolescence on the face, forearms and feet along with hyperkeratosis of palms and soles. In dermatopathica pigmentosa reticularis there is widespread reticulate pigmentation with pigmentary incontinence in histopathology. All these syndromes were ruled out as the pigmentation was not reticulate or punctate in character.
Universal acquired melanosis is a diagnosis of exclusion. It is a progressive condition; long-term prognosis and treatment is not established. Our patient did not have any evidence of in?ammatory condition. We also excluded systemic conditions l ike Addison’ s disease, heavy metal toxicity and hemochromatosis from the history, clinical features and laboratory ?ndings.
The etiology of pigmentation in our case is yet unknown. The following hypothesis can be proposed for its occurrence. The role of excessive production of ß melanocyte-stimulating hormone, abnormal sensitivity of melanocytes towards normal or abnormal endocrine or neural stimuli and ?nally to a genetic mutation, which is not yet detected at the chromosomal level. As “carbon baby syndrome” is a rare case, so it is worthy of reporting.
References:
1. Stefanato CM, Bhawan J. Diffuse hyperpigmentation of the skin: A clinico pathologic approach to diagnosis. Semin Cutan Med Surg 1997;16:61-71.
2. Morelli J, Taieb A, Levine, Flabella R. Pigmentary abnormalities. In: Pediatric dermatology. Schachner LA, Hansen RC 3rd, editors, Mosby: Edinburgh; 2003. p. 501-3.
3. Ruiz-Maldonado R, Tamayo L, Fernandez-Diaz J. Universal acquired melanosis: The carbon baby. Arch Dermatol 1978;114:775-8.
4. Furuya T, Mishima Y. Progressive pigmentary disorder in a Japanese child. Arch Dermatol 1962;86:412-3.
5. Chernosky ME, Anderson DE, Chang JP, Shaw MW, Romsdahl MM. Familial progressive hyperpigmentation. Arch Dermatol 1971;103:581-2.
6. Kint A, Oomen C, Geerts ML, Breuillard F. Congenital diffuse melanosis. Ann Dermatol Venereol 1987;114:11-6.
7. Ashley JR, Littles G, Reddi E. Bronze baby syndrome: A new porphyrin related disorder. Pediatr Res 1983;17:327-30.
8. Wilson-Jones E, Grice K. Reticulate pigmented anomaly of the ?exures (Dowling-Degos): A new genodermatosis? Br J Dermatol 1974;91:6-8.
9. Kaviarasan PK, Prasad PVS, Joe JM et al. Universal acquired mela- nosis (Carbon baby). Indian Journal of Dermatology, Venereology and Leprology 2008;74(1):38
10. M o s e r H W, M a h m o o d A , R a y m o n d G V. X – l i n k e d adrenoleukodystrophy. Nat Clin Pract Neurol 2007;3:140-51.

anastrozole price buy arimidex online buy anastrozole for sale
Good ranking of https://allcasinoaffiliateprograms.com/ casino and sports betting affiliate programs, Super affiliate programs only with us, review, rating
Reading your article helped me a lot and I agree with you. But I still have some doubts, can you clarify for me? I’ll keep an eye out for your answers.
Good ranking of https://24online-casino-affiliate-programs.com/ casino and sports betting affiliate programs, Super affiliate programs only with us, review, rating
The point of view of your article has taught me a lot, and I already know how to improve the paper on gate.oi, thank you. https://www.gate.io/de/signup/XwNAUwgM?ref_type=103
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://www.binance.com/el/join?ref=FIHEGIZ8
Your point of view caught my eye and was very interesting. Thanks. I have a question for you. https://www.binance.com/ur/join?ref=PORL8W0Z
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
hello there and thank you for your info – I’ve
definitely picked up anything new from right here.
I did however expertise some technical points using this site,
as I experienced to reload the site lots of times previous to
I could get it to load correctly. I had been wondering if your web hosting is OK?
Not that I’m complaining, but sluggish loading instances times will often affect your placement in google and can damage
your high-quality score if advertising and marketing with
Adwords. Well I am adding this RSS to my e-mail and
could look out for a lot more of your respective fascinating content.
Make sure you update this again very soon.. Escape rooms hub
Very interesting details you have mentioned, appreciate
it for posting..
mexican online pharmacies prescription drugs: mexico pharmacy – reputable mexican pharmacies online
mexico drug stores pharmacies
http://cmqpharma.com/# buying prescription drugs in mexico
mexican drugstore online