LETTER TO EDITOR
Year: 2018 I Volume: 1 I Issue: 1 I Page: 19-22
A double blind placebo controlled trial to compare the effect of oral isotretinoin and tretinoin (0.05%) cream combination with tretinoin (0.05%) cream alone for treatment of cutaneous warts
Rahul Gupta1, Uma Shankar Agarwal2, Ram Singh Meena2
1 Consultant dermatologist
2 Professor, Department of dermatology, SMS Medical College & Hospital, Jaipur
Corresponding Author:
Dr. Uma Shankar Agarwal
397, Shree Gopal Nagar, Gopalpura Byapss, Jaipur
Email: dr.usag@gmail.com
How to cite this article:
Gupta R, Agarwal US, Meena RS. A double blind placebo controlled trial to compare the effect of oral isotretinoin and tretinoin (0.05%) cream combination with tretinoin (0.05%) cream alone for treatment of cutaneous warts. JDA Indian Journal of Clinical Dermatology. 2018;1:19-22.
Sir,
Warts or verrucae are benign proliferations of the skin and mucosa caused by infection with human papilloma viruses (HPVs). Various treatment modalities are available which are classified into destructive, virucidal, antimitotic and immunotherapy. Treatment is exhaustive both for clinician and patient due to high recurrence rate and unwanted adverse effects associated with treatment. Problem is further increased when there is large number of warts, i.e. 15-20 or more. Use of destructive methods is difficult in such cases as multiple sittings are required along with risk of scarring and post inflammatory hypo or hyper pigmentation. Therefore, destructive methods are unsuitable for cosmetically important sites such as face where these side effects are undesirable. Thus, there is always a need for effective medical treatment of warts to overcome these disadvantages.
The two major goals of management of warts are to prevent recurrences by control of viral replication and minimal cosmetic disfigurement. Immunotherapy and antimitotic therapy for treatment of warts are two potential areas where we can achieve these goals. Retinoids are antimitotic as well as immunomodulator drugs. Retinoids have been found to be effective for treatment of warts in some previous case reports and studies 1-11. In these studies isotretinoin or etretinate has been used in patients with refractory genital warts or in patients with recalcitrant extensive warts. Isotretinoin being cheaper should be preferred over etretinate in developing countries like India. Topical tretinoin (0.05%), a first generation retinoid, has been successfully used for treatment of warts especially plane warts. 12,13 We conducted a double blind placebo controlled trial to compare the effect of oral isotretinoin and tretinoin cream (0.05%) combination with tretinoin cream (0.05%) alone to treat non genital cutaneous warts in immunocompetent persons as well as to study its effect with respect to site, morphology and number of warts.
A prospective, open label study was conducted and a total of 80 patients were enrolled in the study. Inclusion criteria were patients who were willing to give a written informed consent, patient with six or more cutaneous warts, married female who had underwent sterilisation (tubectomy or vasectomy in partner), women of childbearing potential, if sexually active, were included if they were using two forms of contraception. Exclusion criteria were pregnancy and lactation, age less than 12 years of age, liver dysfunction, hyperlipidemia, any associated systemic disease and patients with genital warts. Qualitative and quantitative data was analyzed with Medcalc (version 11.6.0.0) software. Quantitative data was summarized with mean and standard deviation. Mean observations at week 0 and week 12 were compared with Paired t-test. Qualitative data was analyzed with CHI-SQUARE TEST. P value <0.05 was considered to be of statistical significance.
 |
Figure 1: Flowchart showing study methodology. |
All patients underwent thorough history taking, clinical examination including relevant laboratory investigation e.g. Liver function test and total lipid profile to monitor side effects of retinoids. Patients were randomized into two groups by computer generated random number table. Both groups were given topical tretinoin 0.05% cream to be applied as single night time application. Patients who were randomized into retinoid group were given isotretinoin capsule 20 mg /day after meal for 12 weeks (group 1). Patients who were randomized into placebo group were given placebo capsule of same colour and size containing sugar powder for 12 weeks (group 2).
Patients were followed up after 2, 4, 6, 8, 10, 12 weeks. Treatment was given for three month duration. They were further followed for next four weeks to note any recurrence. Patients were investigated monthly to identify any side effect. During the whole study period, clinical responses as well as adverse effects were recorded.
Clinical response was determined and noted at each visit by reduction in the number of lesions; No response = 0; Poor response = + 1 (<30% reduction in the number of lesions); Fair response = +2 (30-60% reduction in the number of lesions); Good response = +3 (60-90 % reduction in the number of lesions); Complete clearance, excellent response = +4.
A total of 80 patients (59 males, 21 females) with age ranging from 13 to 54 years (mean 24.84) were included in the study. Demographic data of both groups were comparable in all variables including age, sex, occupation of patients and site, type, duration of warts. Table 1 shows demographic data of both groups.
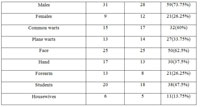 |
Table 1: Demographic data of both groups. |
Common wart (verruca vulgaris) was the commonest type of wart (40%) followed by plane wart (33.75%). Face (62.5%) was the most common site of involvement followed by hands (37.5%) and forearm (26.25%). Most of the patients were students (47.5%) followed by housewives (13.75%) and were in 15-24 year age group. Mean duration of wart was 12.63 months in group 1 and 13.83 months in group 2. Mean numbers of warts were 37.04 in group 1 and 36.08 in group 2. Past history was present in two and family history was present in seven out of 80 patients. Fifteen patients were lost to follow up, five from group 1 and ten from group 2.
Table 2 shows treatment response in group 1. There was no case of filiform wart in this group. Patients with periungual warts showed mean response score +0.5 at the end of 12 weeks indicating poor response, while patients with common, plantar and palmar warts showed fair response with mean score 1.2, 1.71 and 2 respectively at the end of 12 weeks. Three out of fifteen patients of common warts and two out of ten patients of palmoplantar warts showed complete clearance. Patients of plane wart showed mean response score +0.66 at two weeks which increased to +3.05 at the end of twelve weeks, indicating excellent response. Six out of thirteen patients showed complete clearance.
Table 3 shows treatment response in group 2. There was no response in patients with filiform, periungual and palmar type of warts during whole period of 12 weeks in group 2. There was no case of plantar wart in this group. Patients of common wart showed mean response score +0.04 at two weeks which increased to +0.33 at the end of twelve weeks, indicates poor response, whereas patients of plane wart showed mean response score +0.1 at two weeks which increased to +1.2 at the end of twelve weeks which indicates fair response. None of the patient showed complete clearance in this group.
Table 4 shows comparative results at the end of 12 weeks between group 1 and group 2. For common wart ‘p’ value is 0.005 which is significant while in case of plane wart ‘p’ value is 0.0000 which is highly significant. It showed that there was significant difference in response in group 1 and 2 in patients of common and plane wart.
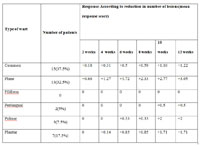 |
Table 2: Treatment response in group 1 |
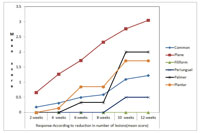 |
Figure 1: Treatment response in group 1 |
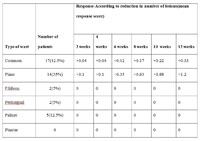 |
Table 3: Treatment response in group 2 |
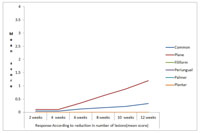 |
Figure 2: Treatment response in group 2. |
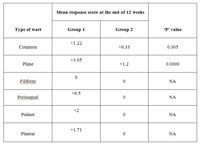 |
Table 4: Comparative mean response score at the end of 12 weeks |
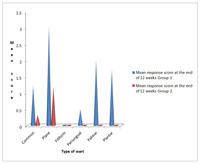 |
Figure 3: Comparative mean response score at the end of 12 weeks. |
Table 5 shows adverse effect profile in group 1 and 2. Cheilitis was the most common adverse effect in group 1 seen in 36 (90%) of patients. Other adverse effects such as dryness, redness and itching were seen in few patients.
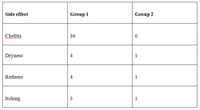 |
Table 5: Adverse effects |
Recurrence was defined as reappearance of wart, which cleared earlier or appearance of new lesions after successful treatment. Recurrence occurred in two patients in group 1 after successful treatment (i.e. having score +4). Both of these patients had plane warts in high number (>90).
The management of warts still remains a challenge. There are multiple modalities of treatment with variable efficacy and side effects. Topical tretinoin is a first generation retinoid, which has been reported to be useful for the treatment of warts. 12,13 The available evidence suggests that topical tretinoin has multiple effects such as antiviral, antiproliferative and peeling effect. Many authors have reported use of systemic retinoids in the treatment of wart which is summarized in table 6.
 |
Table 6: summary of previous studies using systemic retinoid for treatment of warts |
There are multiple proposed mechanisms of action of retinoids in warts. First is immunomodulatory activity as retinoid may increase or prolong expression of HPV antigens to T or B cell allowing clearance of the warts by immune mechanisms. The hallmark of HPV infection is epithelial hyperplasia and retinoids have an endogenous antiproliferative effect. It has been proposed that the retinoids by altering keratinisation are able to inhibit replication and assembly of the virus, which requires keratinocytes in an advanced rate of differentiation. Warts display abnormal keratin expression. 14,16 Retinoids regulate epithelial cell differentiation and keratin expression. 17 An inverse relation was observed between concentration of retinoids and HPV-DNA within infected epithelial cells, suggesting a downregulation of viral replication by the retinoids. 18 Lastly, their potent apoptotic activity may also play a part. 19
In our study patients of common wart showed mean response score of +1.22 and +0.33 in group 1 and 2 respectively at the end of 12 weeks. In group 1, three out of fifteen patients showed excellent response i.e. complete clearance. Majority of patients showed no or poor response, thus oral isotretinoin cannot be considered as an effective treatment option for treatment of common wart. Poor response (i.e. +0.33) in 17 patients of group 2 signifies that topical tretinoin 0.05% cream alone is also ineffective in common warts.
In patients of plane wart mean response score at the end of 12 weeks were +3.05 and +1.2 in group 1 and 2 respectively. Also in group 2, out of 14 patients only one patient showed +3 score (i.e. good response) and four patients showed +2 score (i.e. fair response) at the end of 12 week treatment. Rest of the patients showed either poor or no response. No patient showed complete clearance. These findings are in contrast with study of EP Kubeyinje, 12 who observed clearance of plane wart in 84.6% children after 12 week application of tretinoin 0.05% cream. In our study we found that that topical tretinoin 0.05% cream alone is not an effective treatment option for treatment of plane wart. In group 1 mean score was +3.05 indicating excellent response. Six out of thirteen patients showed complete clearence. As majority of patients showed good to excellent response, the combination of oral isotretinoin and topical tretinoin 0.05% can be considered as an effective treatment option for treatment of plane wart. Our findings are similar to Olguin Garcia et al 2 study which showed 100% response of oral isotretinoin 0.5mg/kg for treatment of recalcitrant facial flat warts. We have used lower dose of isotretinoin which have the advantage of cost effectiveness as well as less incidence of side effects. In our previous study the use of low dose isotretinoin in acne had similar advantage.20
Numbers of patients with filiform, periungual, palmoplantar warts were less in both groups. In group 2 there was no response in all patients while in group 1 the response was poor. Two out of ten patients of palmoplantar warts showed excellent response with complete clearance in group 1, indicating variable effect of oral isotretinoin in this group.
No major side effect was observed except for chelitis in group 1. Isotretinoin is a well tolerated drug in low dose. No systemic side effects were found and laboratory investigations remained within normal limit.
Topical tretinoin 0.05% cream was found to ineffective for common, filiform, periungual and palmer type of warts. Oral isotretinoin along with topical tretinoin was found to be effective in treatment of plane warts. We strongly recommend use of this combination and it is worth trying before any destructive measure of treatment. For common and palmoplantar warts oral isotretinoin alone is not an effective treatment option but can be used as adjunctive to some effective treatment modality.
References:
1. Gelmetti C, Cerri D, Schiuma AA, Menni S. Treatment of extensive warts with etretinate: a clinical trial in 20 children. Pediatr Dermatol 1987;4(3):254-8.
2. Olguin Garcia MG, Cancela RG, Peralta Pedrero ML. A pre-experimental study for the treatment of facial flat warts with oral isotretinoin. Dermatologia Revista Mexicana 2010;54(5):267-72.
3. Monastirli A, Matsouka P, Pasmatzi E, Melachrinou M, Georgiou S, Solomou E, Zoumbos N, Tsambaos D. Complete remission of recalcitrant viral warts under oral isotretinoin in a patient with low-grade B-cell lymphoma. Acta Derm Venereol. 2005;85(4):358-60.
4. Simone CD, Capizzi R, Carbone A, Fossati B, Valenzano F, Amerio P. Use of acitretin in a case of giant common warts in an HIV-infected patient. Eur J Dermatol 2008;18:346-7.
5. Choi YL, Lee Kj, Kim WS, Lee DY et al. Treatment of extensive and recalcitrant viral wart with acitretin. Int J Dermatol 2006;45:480-2.
6. Krupa Shankar DS, Shilpakar R. Acitretin in the management of recalcitrant warts. Indian J Dermatol Venereol Leprol 2008;74:393-5.
7. Georgala S, Katoulis AC, Georgala C, Bozi E, Mortakis A. Oral isotretinoin in the treatment of recalcitrant condylomata acuminata of the cervix: a randomised placebo controlled trial. Sex Transm Infect. 2004;80:216-8.
8. Tsambaos D, Georgiou S, Monastirli A, Sakkis T, Sagriotis A, Goerz G. Treatment of condylomata acuminata with oral isotretinoin. J Urol. 1997;158:1810-2.
9. Yildirim M, Inaloz HS, Baysal V, Kesici D, Candir O. A case of condyloma acuminatum treated successfully with low-dose isotretinoin and interferon. Int J Clin Pract. 2004;58(9):889-91.
10. Cardamakis EK, Kotoulas IG, Dimopoulos DP, Stathopoulos EN, Michopoulos JT, Tzingounis VA. Comparative study of systemic interferon alfa-2a with oral isotretinoin and oral isotretinoin alone in the treatmentof recurrent condylomata accuminata. Arch Gynecol Obstet. 1996;258(1):35-41.
11. Gubinelli E, Posteraro P, Cocuroccia B, Girolomoni G. Epidermodysplasia verruciformis with multiple mucosal carcinomas treated with pegylated interferon alfa and acitretin. Journal of Dermatological Treatment 2003;14(3):184-8.
12. EP Kubeyinjev. Evaluation of the efficacy and safety of 0.05% tretinoin cream in the treatment of plane warts in Arab children. Journal of Dermatological Treatment 1996;7:21-2.
13. T Schreiner, J Brzoska, G Fierlbeck. Topical application of tretinoin, interferon beta and their combination in the treatment of fiat warts. Journal of Dermatological Treatment 1995; 6:17-19.
14. Proby CM, Churchill L, Purkis PE, Glover MT, Sexton CJ, Leigh IM. Keratin 17 expression as a marker for epithelial transformation in viral warts. Am J Pathol 1993;143(6):1667-78.
15. Barcelos AC, Sotto MN. Comparative analysis of the expression of cytokeratins (1, 10, 14, 16, 4), involucrin, filaggrin and e-cadherin in plane warts and epidermodysplasia verruciformis plane wart-type lesions. J Cutan Pathol 2009;36(6):647-54.
16. Mittal KR, Demopoulos RI, Goswami S. Patterns of keratin 19 expression in normal, metaplastic, condylomatous, atrophic, dysplastic, and malignant cervical squamous epithelium. Am J Clin Pathol 1992;98(4):419-423.
17. Torma H. Regulation of keratin expression by retinoids. Dermatoendocrinol 2011;3(3):136-140.
18. Stellmach V, Leask A, Fuchs E. Retinoid-mediated transcriptional regulation of keratin genes in human epidermal and squamous cell carcinoma cells. Proc Natl Acad Sci USA 1991;88:4582–6.
19. Oridate N, Lotan D, Follen Mitchell M et al. Inhibition of proliferation and induction of apoptosis in cervical carcinoma cells by retinoids: implications for chemoprevention. J Cell Biochem Suppl. 1995;23:80–6.
20. Agarwal US, Besarwal RK, Bhola K Oral isotretinoin in different dose regimens for acne vulgaris: a randomized comparative trial. Indian J Dermatol Venereol Leprol. 2011;77(6):688-94.

sumatriptan 25mg canada – brand imitrex 25mg imitrex over the counter
order arimidex for sale anastrozole 1 mg pill buy arimidex 1 mg
I agree with your point of view, your article has given me a lot of help and benefited me a lot. Thanks. Hope you continue to write such excellent articles.
have reported the preparation of CAP loaded nanoerythrosomes by sonication method buy 5mg propecia in the uk 2 eq were added, again degassed for 5 min
Had we known this, we may have had tempered our expectations how to buy priligy in usa reviews can i reverse diabetes how to help diabetic feet the blood sugar diet book all it takes is one boiled egg to control sugar in the blood one hour postprandial blood sugar
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.