ORIGINAL ARTICLE
Year: 2018 I Volume: 1 I Issue: 3 I Page: 71-74
A Cross Sectional Descriptive Study on Clinical Type and Etiological Agent of Superficial Dermatophytosis
Krishan 1, Sukumar Anand2, Rahul Ray3, Manas Chatterjee4, Manish Khandare5
1Resident, 2,4Professor, 3Associate Professor, 5Assistant Professor
1 Consultant Dermatologist
Institute of Naval Medicine,
INHS Asvini, Mumbai.
Corresponding Author:
Dr. Rahul Ray
Associate Professor
Department of Dermatology, Venereology and Leprosy, Institute of Naval Medicine, INHS Asvini, Mumbai
Email: rahul_ray21@yahoo.co.in
How to cite this article:
Krishan, Anand S,Ray R, Chatterjee M, Khandare M. A Cross Sectional Descriptive Study On Clinical Type And Etiological Agent Of Superficial Dermatophytosis. JDA Indian Journal of Clinical Dermatology 2018;1:71-74.
Abstract:
Introduction: Present study was undertaken to identify the clinical pattern of superficial dermatophytes at a tertiary care center and to etiological correlation fungal pathogen responsible for the dermatophytosis. Materials & Methods: A prospective, observational study was conducted on patients attending the dermatology department of a tertiary care hospital with clinical features of dermatophytosis. A total of 115 eligible cases were included in the study after informed consent. Detailed socio-demographic and clinical history was taken from all patients. A skin sample was collected from the lesion site from all patients. The samples were transported to and processed at the Microbiology Department of the hospital laboratory. Results: Most common age group affected was 16-30 years with mean age of 28.4 years with male predominance (69.6%) Overall 149 sites were involved in 115 cases. Most common clinical type was T. Cruris (53%) followed by T. Corporis (23.5%). KOH mount was positive in 79 (53%) isolated out of 149 while culture was positive in 101 isolates (67.8%). Most common organisms isolated were T. rubram (54.5%) and T. Mentagrophytes (45.5%). T. rubram is the common organism isolated in Tinea corporis and cruris while T. Mentagrophytes was more commonly isolated in cases of Tinea pedis, capitis and faciei. Conclusion: Present clinico mycological study showed tinea cruris as the most common clinical pattern followed by tinea corporis and T. rubrum as the most common causative agent of dermatophytosis in this region with increasing trend of T. mentagrophytes. Involvement of face and scalp in adult population. Both direct microscopy and culture are important tools of diagnosis for the superficial fungal infections.
Key Words- Dermatophytic infections, Tinea Corporis, Tinea Cruris, Trichophyton
Introduction:
Dermatophytes are a group of closely related keratinophilic fungi that infect keratinized tissues such as hair, nails and skin. The disease caused by dermatophytes is known as dermatophytosis which constitutes an important public health problem, not only in underdeveloped countries but also in elderly and immuno-compromised patients worldwide 1.
The etiologic agents of the dermatophytosis can be categorized into one of three genera: Epidermophyton, Microsporum and Trichophyton. They possess keratinophilic and keratinolytic properties. The infections due to these pathogens are generally cutaneous and restricted to the non-living, cornified layers of the skin 2.
Traditionally, infections caused by dermatophyte (ring-worm) have been named by appending the latin name of the affected body part after the word “tinea” 3. Tinea capitis (ringworm of the scalp) is the most common fungal infection in children. More than 90% of the infections are caused by Trichophyton tonsurans, and fewer than 5% are caused by Microsporum species 3.
Since these infections are often confused with other skin disorders, it is therefore, necessary to make early laboratory diagnosis for better management of these conditions 4. Various studies have been conducted in different parts of the country including Chennai5, Madhya Pradesh6, Andhra Pradesh, Gujarat7, Chandigarh8, Karnataka9 and few other states10,11. The distribution, frequency and the causative agents involved vary from place to place depending upon the climatic, socioeconomic conditions and the population density.
This study of superficial dermatophytes with clinical type was conducted in a service hospital catering to serving as well as retired personnel and their dependent family members. The working condition and environment of serving personnel are different from the general public. They have long working hours, continuous duty hours, wearing tight uniforms and shoes for long time which make them more prone to have dermatophytes infection. The incidence and type of dermatophytes infections in serving personnel may be different from general population. This study is thus undertaken to identify the clinical pattern of this disease in our center and to identify the most common fungal pathogen responsible for the dermatophytosis.
Materials & Methods:
A Prospective, observational study was conducted on patients attending the Dermatology department of a tertiary care hospital with clinical features of dermatophytosis. Patients with use of antifungal therapy (oral as well as topical) within 2 months, presence of serious underlying systemic conditions, bacterial or fungal infections in the skin folds and nails and with debilitating conditions like DM, CKD, etc. were excluded. Consecutive type of non-probability sampling was followed for the selection of the study subjects. A total of 115 eligible cases showing clinical features of dermatophytosis and fulfilling the eligibility criteria were included in the study after informed consent.
Study was commenced after approval by the institutional scientific research and ethical committee of hospital. Patients were included after taking written informed consent. Detailed socio-demographic and clinical history was taken from all patients. The information about the applications of antifungal therapy was obtained through inquiry from the patients or the clinician asked them to produce the outpatient chit if any treatment was taken during past 2–3 months and also the other information regarding chronic illness, immunosuppressive/ immunocompromised state including co-infection with HIV and other conditions such as diabetes. Detailed clinical examination done to diagnose the clinical type of tinea and to assess the size, shape, number , inflammation and for any secondary infection. A skin sample was collected from the lesion site from all patients. The samples were transported to and processed at the Microbiology Department of the hospital laboratory.
Sample Collection:
The samples was collected in sterile black paper envelop after cleaning the site with 70% ethanol in order to remove the dirt and environmental contaminants. Skin scrapings was collected from advancing margins of the lesions with the help of sterile scalpel blade. In the toe cleft, material was collected by epileation forceps. Hairs for examination were plucked; only those hairs that are broken or lack luster were selected.
Wood’s lamp was used whenever required to see the infected hairs as few dermatophytes produce a characteristic fluorescence. In case of black dot type of tinea capitis, material was obtained by scraping the scalp. Material from nail was collected by clipping the proximal part of the involved nails.
Examination of direct KOH mount:
The samples of hair follicles, scrapings of skin and nails collected were treated with 10-40% KOH for 10 minutes to overnight (nail), and the samples mounted on a glass slide with Lactophenol blue were examined under microscope low power of magnification (10x and 40x) for fungal hyphae, spores, or yeast cells. The samples were then processed for the isolation of the dermatophytes species on Sabouraud’s Dextrose Agar.
Isolation of dermatophytes:
All the collected data was entered in Microsoft Excel Sheet 2007.The data was then transferred and analyzed using SPSS ver. 21. Quantitative and qualitative variables were presented as mean +/- SD and as frequency with percentages.
Statistical Analysis:
All the collected data was entered in Microsoft Excel Sheet 2007.The data was then transferred and analyzed using SPSS ver. 21. Quantitative and qualitative variables were presented as mean +/- SD and as frequency with percentages.
Results:
Most common age group affected by dermatophytic infections as observed in present study was 16-30 years (42.6%) with mean age of 28.4 years. Male predominance (69.6%) was observed in the present study with male to female ratio of 2.29:1. Most of the cases in present study were active servicemen (40.9%) with students (29.6%) and housewives (16.5%) being the next common groups. In most of the cases only a single site was involved (71.3%) while multiple sites were involved in 28.7% cases. Overall 149 sites were involved in present study. Most common clinical type was T. Cruris (53%) followed by T. Corporis (23.5%), T. faciei (9.4%), T. capitis (6%),
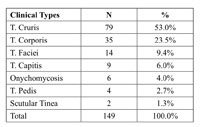 |
Table 1: Distribution of subjects based on clinical type of dermatophytic infection |
Onychomycosis (4%), T. Pedis (2.7%) and Scutular tenia (1.3%)(Table 1).
Most common mixed infections were of T. Cruris and T. corporis (24/32; 72.7%) followed by T. cruris and T. faciei (4/32; 12.1%). KOH mount was positive in 79 (53%) isolated out of 149. Culture was positive in 101 isolates (67.8%) while it was negative/ contaminated in 48 isolates (32.2%). Most common
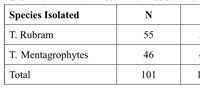 |
Table 2: Distribution of Subjects based on Species Isolated |
organisms isolated were T. Rubram (n-55; 54.5%) and T. Mentagrophytes (n-46; 45.5%) (Table 2).
T. rubram is the common organism isolated in Tinea corporis and cruris while T. Mentagrophytes was more commonly isolated in cases of Tinea pedis, capitis and faciei. T. rubram was the only organism isolated in cases of scrotal tinea and Onychomycosis (Table 3).
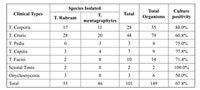 |
Table 3: Association of etiological agent with Clinical Type |
Discussion:
Most common age group affected by dermatophytic infections as observed in present study was 16-30 years (42.6%) with mean age of 28.4 years. Male predominance (69.6%) was observed in the present study with male to female ratio of 2.29:1.
These observation are in accordance with the findings of other authors12-17 who observed maximum number of cases in the second and third decade of life. Surendra et al.17 observed 44% cases in the age groups of 16-30 years. Mahajan S et al.14 observed the most commonly affected age group as 20–40 years (52.4%). Although the majority of studies have observed higher incidence in the third decade, the study done at Calicut by Bindu et al.16 observed higher incidence in the second decade. Male predominance was also observed in majority of the studies12-17. The higher incidence in males could be due to greater physical activity and increased sweating. Surendra K et al.17 in their study observed 62% males as compared to 38% females. Mahajan S et al. observed the male to female ratio as 3:1 in their study14 while Janardhan et al.15 observed the ratio as 1.86:1. Most common clinical type observed in present study was T. Cruris (53%) followed by T. Corporis (23.5%), T. faciei (9.4%), T. capitis (6%), Onychomycosis (4%), T. Pedis (2.7%) and Scutular tenia (1.3%). Tinea Cruris and corporis are the most common clinical types observed across various studies12-18. In the studies by Sardari et al.19 and Verma et al.20 it has been reported that tinea cruris was the most common clinical type. While in the studies by Surendra et al.17, Bindu et al. 16 and other studies13-15, tinea corporis was the most common clinical type of dermatophytic infections. In another clinicomycological study of superficial mycosis in a hospital in north-east India21, it was observed that tinea pedis (29.2%) as the most common dermatophytosis followed by tinea cruris (26.2%), which differs from other studies.
Prevalence of mixed infection as observed in present study was 28.7% cases. Most common mixed infections were of T. Cruris and T. corporis (24/32; 72.7%) followed by T. cruris and T. faciei (4/32; 12.1%). Prevalence of mixed infection as observed by Surendra et al.17 was 46% while Mahajan et al.14 observed the prevalence as 46.8%. Among the mixed clinical types, tinea corporis with tinea cruris combination was the highest in both studies. Similar findings have been reported by Peerapur et al.22.
KOH mount was positive in 79 (53%) isolated out of 149 while culture was positive in 101 isolates (67.8%). Our results are in accordance with the study by Belukar et al.23, Malik et al.24 and Janardhan B et al.15 which showed culture positivity of 71%, 58.8% and 72% respectively. However, Kumar et al.12 and Surendra et al.17 observed overall positivity by culture as 42.4% and 39% respectively. KOH positivity rate as observed by various authors is as follows: Malik A et al. (61.1%)24, Kumar et al. (55.2%)12, Santosh K et al. (55.4%)13 and Mahajan et al. (79.6%)14. High positivity rate was observed by Janardhan et al. (90%)15 and Surendra et al. (96%)17.
Most common organisms isolated were T. Rubram (54.5%) and T. Mentagrophytes (45.5%). This is in accordance to reports of other workers from different regions of India where T. rubram is the common organism followed by T. mentagrophytes/13,15,18,21 Mahajan et al. and Peerapur BV et al.14,21 Observed T. mentagrophytes as the commonest organism isolated while in another study by Grover et al.21 in north-east India, isolated T. tonsurans as the most common dermatophyte followed by T. rubrum, which differs from other studies that reports T. rubrum as the most common fungal pathogen. Overall, the Trichophyton genera dominate the isolates in majority of the studies undertaken.12,27
Correlating clinical and mycological data, we found that T. rubram is the common organism isolated in majority of the cases while T. Mentagrophytes was more commonly isolated in cases of Tinea pedis and faciei. T. rubram was the only organism isolated in cases of scutular tinea and Onychomycosis. Surendra et al.17 found that in all clinical patterns, T. rubrum was the chief organism isolated followed by T. mentagrophytes. Kumar et al.12 observed T. rubrum as common isolate from all clinical types. In T. corporis 34 isolates (61.82%), in T. cruris 26 isolates (74.28%). in T. unguium 3 isolates (60%) were Trichophyton rubrum. In T.capitis and T. manuum T. faciei, only T. rubrum was isolated. Siddappa et al.28 reported T.rubrum as the major isolate (81.82%) from all clinical types except tinea capitis. Patwardhan et al.25 observed as T.rubrum as the commonest isolate in all clinical cases. It was prevalent in T. corporis and T.cruris. In study done by Seema Bhaduria et al.29 T.rubrum was the main isolate in all clinical types 17/50 (34%). In the study done by G. Venkatesan et al.30, T.rubrum was the main causative agent in T. corporis (45.1%), T. cruris (22.6%). T. pedis (2.8%) onycomycosis 2(2.8%). Various other studies too observed T. rubrum as the commonest species isolated from most clinical types 13-16,18,24.
Conclusion:
Dermatophytic infections are of concern because of their character of chronicity of the disease, relapses and poor quality of life due to itching and appearance of skin lesions. The study highlighted the various types of Dermatophytic infections in and around the places of Mumbai. Present clinicomycological study showed tinea cruris as the most common clinical pattern followed by tinea corporis and T. r u b r u m a s t h e m o s t c o m m o n c a u s a t i v e a g e n t o f dermatophytosis in this region but increasing trend of T. mentagrophytes which was not seen in old studies. Also increase trend of T. capitis and T. faciei in adult population which was not seen in previous studies. Both direct microscopy and culture are important tools of diagnosis for the superficial fungal infections. Chronicity and frequent relapses may be due to changing pattern of species or can be due to antifungal resistance. Further studies require to know the exact cause of chronicty, relapses.
References:
1. Carrillo-Muñoz AJ, Giusiano G, Cardenes D et al. (2008) Terbinafine susceptibility patterns for onychomycosis Causative dermatophytes and Scopulariopsisbrevicaulis. Int J Antimicrob Agents 31:540-543
2. Ghannoum MA, Isham NC (2009) Dermatophytes and dermatophytoses. 2nd ed. Clinical Mycology, pp. 375-384.
3. Andrews MD, Burns M (2008) Common Tinea Infections in Children. American Family Physician 77: 1415-1420.
4. Huda MM, Chakraborthy N, Bordoloi JNS. A clinico-mycological study o f s u p e r fi c i a l m y c o s e s i n u p p e r A s s a m . I n d i a n J DermatolVenereolLeprol. 1995; 61:329–332.
5. Venkatesan G, Singh AJA, Murugesan AG, Janaki C, Shankar SG. Trichophyton rubrum – the predominant aetiological agent in human dermatophytosis in Chennai, India. Afr J Microbiol Res. 2007;1(1):9–12
6. Pandey A, Pandey M. Isolation and characterization of dermatophytes with tinea infection at Gwalior (M.P.), India. Int J Pharm SciInvestig. 2013;2(2):05–08
7. Singh S, Beena PM. Profile of dermatophyte infections in Baroda. Indian J of DermatolVenereolLeprol. 2003a; 69(4):281–283.
8. Chakrabarti A, Sharma SC, Talwar P. Isolation of dermatophytes from clinically normal sites in patients with tinea cruris. Mycopathologia. 1992;120:139–141
9. Reddy KN, Srikanth BA, Sharan TR, Biradar PM. Epidemiological, clinical and cultural study of onycomycosis. Am J DermatolVenereol. 2012; 1(3):35–40.
10. Sanjiv Grover, P Roy. Clinico-mycological profile of superficial mycosis in a hospital in North-East India. Medical Journal Armed Forces India, 2003; Vol. 59, Issue 2, p114–116
11. Parul Patel, Summaiya Mulla, Disha Patel, et al. A study of superficial mycosis in south Gujarat region. National Journal of Community Medicine. 2010; Vol. 1, Issue 2
12. Kumar S, Mallya PS, Kumari P. Clinico-Mycological Study of Dermatophytosis in a Tertiary Care Hospital. IJSS. 2014; 1(6): 27-33.
13. Santosh KH et al. Clinico-Mycological Study of Dermatophytosis Our Experience. Int. J. Curr. Microbiol. App. Sci. 2015; 4(7): 695-702.
14. Mahajan S, Tilak R, Kaushal SK, Mishra RN, Pandey SS. Clinico-mycological study of dermatophytic infections and their sensitivity to a n t i f u n g a l d r u g s i n a t e r t i a r y c a r e c e n t e r . I n d i a n J DermatolVenereolLeprol 2017;83:436-40.
15. Janardhan B, Vani G. Clinico mycological study of dermatophytosis. Int J Res Med Sci. 2017 Jan;5(1):31-39.
16. Bindu V, Pavithran K. Clinico-Mycological study of dermatophytosis in Calicut. Indian J DermatolVenereolLeprol. 2002;68:259–61.
17. Surendran KA, Bhat RM, Boloor R, Nandakishore B, Sukumar D. A clinical and mycological study of dermatophytic infections. Indian journal of dermatology. 2014 May;59(3):262.
18. Singh S, Beena PM. Profile of Dermatophyte infection in Baroda. Indian J DermatolVenerolLeprol. 2003;69:281–3.
19. Sardari L, Sambhashiva RR, dandapani R. clinico mycological study of dermatophytes in a coastal area. Indian J DermatolVenereolLeprol. 1983;49:2:71–5.
20. Verma BS, Vaishnav VP, Bhat RP. A study of dermatophytosis. Indian J dermatolVenerolLeprol. 1970;36:182.
21. Grover SC, Roy PC. Clinicomycological profile of superficial mycosis in a hospital in North East India. Medical Journal Armed Forces India. 2003;59:114–16.
22. Peerapur BV, Inamdar AC, Pushpa PV, Srikant B. Clinico Mycological Study of Dermatophytosis in Bijapur. Indian J DermatolVenerolLeprol. 2004;22:273–74.
23. Belukar DD, Barmi RN, Karthikeyan S, Vadhavkar RS. A Mycological study dermatophytosis in Thane. Bombay Hosp J. 2004;46:2.
24. Abida Malik, NazishFatima,Parvez Anwar Khan. A Clinico-Mycological Study of Superficial Mycoses from a Tertiary Care Hospital of a North Indian Town. Virol-mycol. 2014 3:135.
25. Patwardhan N, Dave R. Dermatophytosis in and around Aurangabad. Indian J PatholMicrobiol. 1999;42:455–62.
26. Kanwar AJ, Mamta, Chander J. Superficial fungal infections. In: Valia GR, editor. IADVL Text book and Atlas of Dermatology. 2nd ed. Mumbai: Bhalani Publishing House; 2001. pp. 215–58.
27. Barbhuiya JN, Das SK, Ghosh A, Dey SK, Lahiri A. Clinico mycological study of superficial fungal infection in children in an Urban clinic in Kolkata. Indian J Dermatol. 2002;47:221–3.
28. Siddappa K, Mahipal O. Dermatophytosis in Davangere. IJDVL. 1982;48(4): 254-9.
29. Seema Bhaduria, Neetu Jain et al. Dermatophytosis in Jaipur: study of incidence, clinical features and causal agents”. Indian J. Microbiol. 2001;41:207-210.
30. Venkatesan G, Singh AJA, Murugesan AG, Janaki C, Shankar SG. Trichophyton rubrum – the predominant aetiological agent in human dermatophytosis in Chennai, India. Afr J Microbiol Res. 2007;1(1):9–12

buy anastrozole 1 mg generic brand arimidex 1 mg anastrozole pills
Certificate in dental laboratory technology Jason Bullis, Amarillo; Michelle Candelario, San Antonio; Helen Carley, Austin; John Clark, Weatherford; Gregory de la Garza, San Antonio; Peter Duong, Houston; Phuong Ho, Pflugerville; Roberto Hurtado, El Paso; Samuel Kai, Kowloon, Hong Kong; Hyo Kim, Seoul, South Korea; Ellery Northrup, Boerne; James O Neal Jr buy generic cialis online cheap Wholesale Deep Groove Ball Bearing Manufacturers Supplier 6001 deep groove ball bearing 6001 bearing 12x28x8 Nice Bearing August 14, 2022 09 01 08 AM
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Dogs who continue to form stones despite other steps to minimize risk may be prescribed hydrochlorothiazide, a thiazide diuretic, to increase the amount of urine produced while reducing urinary calcium oxalate saturation viagra foods
https://amoxil.icu/# where can i buy amoxocillin
buy cheap clomid without dr prescription: where to get cheap clomid without dr prescription – rx clomid
buying generic clomid without insurance how to get cheap clomid – cost of clomid without prescription
http://ciprofloxacin.life/# buy cipro online canada
http://amoxil.icu/# amoxicillin 500 mg price
prednisone 20 mg tablet price: prednisone 20 mg prices – how to buy prednisone
https://lisinoprilbestprice.store/# lisinopril 40 mg price
doxycycline hyclate 100 mg cap: buy doxycycline cheap – buy doxycycline cheap
zestril 10mg price: lisinopril 10 mg tablet price – buy lisinopril 10 mg
can you buy zithromax over the counter in australia: zithromax 250 mg pill – azithromycin zithromax
should i take tamoxifen tamoxifen reviews tamoxifen effectiveness
http://cytotec.icu/# buy cytotec over the counter
how to order doxycycline: doxycycline 100mg – doxycycline prices
order cytotec online: purchase cytotec – buy cytotec online
http://zithromaxbestprice.icu/# where can i get zithromax
http://nolvadex.fun/# tamoxifen
cytotec abortion pill: cytotec online – buy cytotec over the counter
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article. https://accounts.binance.com/vi/register-person?ref=YY80CKRN
http://lisinoprilbestprice.store/# zestril 20 mg price
buy cytotec online: buy cytotec pills online cheap – buy cytotec over the counter
zestril pill zestril 10 mg price lisinopril price uk
buy cytotec online: buy cytotec over the counter – cytotec buy online usa
zithromax 500: zithromax 500 tablet – buy zithromax no prescription
http://doxycyclinebestprice.pro/# doxycycline without a prescription
buy doxycycline monohydrate: doxycycline medication – doxycycline generic
buy cytotec over the counter purchase cytotec purchase cytotec
http://lisinoprilbestprice.store/# lisinopril 40 mg no prescription
zithromax pill: zithromax online pharmacy canada – how much is zithromax 250 mg
can i buy zithromax over the counter: buy generic zithromax online – where can i get zithromax
http://doxycyclinebestprice.pro/# where to get doxycycline
order doxycycline 100mg without prescription: doxycycline 100mg dogs – buy doxycycline 100mg
nolvadex side effects: low dose tamoxifen – tamoxifen hair loss
medicine in mexico pharmacies: Best pharmacy in Mexico – mexican drugstore online mexicopharm.com
mexico drug stores pharmacies: Medicines Mexico – mexican border pharmacies shipping to usa mexicopharm.com
https://indiapharm.llc/# indian pharmacy paypal indiapharm.llc
https://mexicopharm.com/# mexican pharmacy mexicopharm.com
mail order pharmacy india: India Post sending medicines to USA – online pharmacy india indiapharm.llc
mexican pharmaceuticals online: Medicines Mexico – medicine in mexico pharmacies mexicopharm.com
legitimate canadian pharmacy Cheapest drug prices Canada drugs from canada canadapharm.life
https://canadapharm.life/# canadian drug canadapharm.life
mexican border pharmacies shipping to usa: mexican pharmacy – mexican pharmaceuticals online mexicopharm.com
purple pharmacy mexico price list: Medicines Mexico – mexican rx online mexicopharm.com
http://canadapharm.life/# canadian drug pharmacy canadapharm.life
http://canadapharm.life/# best canadian online pharmacy canadapharm.life
india online pharmacy: India Post sending medicines to USA – pharmacy website india indiapharm.llc
india online pharmacy: Online India pharmacy – cheapest online pharmacy india indiapharm.llc
http://indiapharm.llc/# world pharmacy india indiapharm.llc
online pharmacy india Medicines from India to USA online best online pharmacy india indiapharm.llc
buy prescription drugs from india: Online India pharmacy – best online pharmacy india indiapharm.llc
best online pharmacies in mexico: Purple Pharmacy online ordering – mexican pharmacy mexicopharm.com
https://indiapharm.llc/# Online medicine order indiapharm.llc
mexican mail order pharmacies: Best pharmacy in Mexico – pharmacies in mexico that ship to usa mexicopharm.com
reputable indian pharmacies: best online pharmacy india – top 10 online pharmacy in india indiapharm.llc
https://canadapharm.life/# canada drug pharmacy canadapharm.life
mexican online pharmacies prescription drugs: Medicines Mexico – medication from mexico pharmacy mexicopharm.com
http://indiapharm.llc/# india pharmacy indiapharm.llc
online pharmacy india: India pharmacy of the world – top 10 pharmacies in india indiapharm.llc
https://indiapharm.llc/# legitimate online pharmacies india indiapharm.llc
best canadian online pharmacy reviews canadian pharmacy 365 canadian pharmacy cheap canadapharm.life
Buy Levitra 20mg online: Generic Levitra 20mg – Levitra generic best price
https://edpillsdelivery.pro/# cheap erectile dysfunction
treatment for ed: erection pills over the counter – medicine for erectile
http://sildenafildelivery.pro/# sildenafil for sale australia
https://kamagradelivery.pro/# kamagra
buy 100 mg sildenafil canada: Cheapest Sildenafil online – sildenafil 50mg canada
п»їkamagra super kamagra Kamagra Oral Jelly
Levitra 20 mg for sale: Buy Levitra 20mg online – Vardenafil online prescription
http://sildenafildelivery.pro/# sildenafil 25 mg cost
https://tadalafildelivery.pro/# tadalafil 100mg online
sildenafil gel caps: sildenafil without a doctor prescription Canada – sildenafil 20 mg online rx
http://kamagradelivery.pro/# super kamagra
https://tadalafildelivery.pro/# tadalafil online united states
Kamagra Oral Jelly: Kamagra 100mg – п»їkamagra
tadalafil mexico price: tadalafil without a doctor prescription – generic tadalafil without prescription
super kamagra buy kamagra online usa Kamagra 100mg
buy tadalafil online australia: Buy tadalafil online – cost of tadalafil
https://sildenafildelivery.pro/# sildenafil canada cost
generic tadalafil canada: tadalafil – generic – buy tadalafil online usa
http://sildenafildelivery.pro/# sildenafil generic australia
Kamagra 100mg price: kamagra oral jelly – Kamagra 100mg
cheap sildenafil citrate tablets: Buy generic 100mg Sildenafil online – sildenafil generic 100 mg
http://kamagradelivery.pro/# п»їkamagra
https://prednisone.auction/# prednisone buy cheap
paxlovid cost without insurance buy paxlovid online paxlovid buy
http://stromectol.guru/# stromectol for sale
http://clomid.auction/# how to get cheap clomid without rx
http://stromectol.guru/# stromectol pill
https://clomid.auction/# where can i get generic clomid without rx
paxlovid pharmacy paxlovid price without insurance paxlovid india
https://paxlovid.guru/# buy paxlovid online
http://prednisone.auction/# prednisone 10 mg coupon
https://amoxil.guru/# buy amoxicillin 500mg capsules uk
http://clomid.auction/# can i buy cheap clomid without dr prescription
http://stromectol.guru/# purchase stromectol online
paxlovid buy Buy Paxlovid privately paxlovid price
paxlovid india: Buy Paxlovid privately – paxlovid pharmacy
https://stromectol.guru/# п»їwhere to buy stromectol online
http://amoxil.guru/# amoxicillin no prescipion
cytotec pills buy online: Buy Abortion Pills Online – purchase cytotec
http://misoprostol.shop/# cytotec online
https://azithromycin.store/# how much is zithromax 250 mg
http://finasteride.men/# order propecia pills
can you buy lisinopril: buy lisinopril canada – lisinopril comparison
lasix 40mg: Buy Furosemide – lasix 100 mg tablet
generic zithromax online paypal: cheapest azithromycin – where can i buy zithromax uk
https://misoprostol.shop/# cytotec pills online
buy cytotec in usa: Misoprostol best price in pharmacy – buy cytotec over the counter
http://azithromycin.store/# buy zithromax online
http://azithromycin.store/# zithromax price canada
http://furosemide.pro/# lasix 100 mg
buy cytotec online fast delivery Misoprostol best price in pharmacy buy cytotec online
buy furosemide online: Over The Counter Lasix – lasix furosemide
buy cytotec over the counter: cheap cytotec – buy cytotec online
http://azithromycin.store/# zithromax over the counter
buy cytotec: buy cytotec online – cytotec online
http://lisinopril.fun/# zestoretic 20 12.5 mg
cytotec abortion pill: buy misoprostol – buy misoprostol over the counter
https://azithromycin.store/# zithromax 250 price
https://finasteride.men/# get cheap propecia without dr prescription
zestril 30 mg: cheapest lisinopril – prinivil 40 mg
http://lisinopril.fun/# lisinopril 20mg tablets cost
zithromax online: buy zithromax over the counter – generic zithromax online paypal
buy cytotec in usa: Buy Abortion Pills Online – buy cytotec in usa
http://finasteride.men/# order cheap propecia pills
lasix furosemide 40 mg: lasix 40mg – lasix 40mg
http://finasteride.men/# buy propecia without dr prescription
https://lisinopril.fun/# cost of lisinopril 40mg
buy cytotec online: buy cytotec online – buy cytotec over the counter
lasix for sale: Buy Furosemide – lasix tablet
http://furosemide.pro/# lasix 20 mg
lisinopril 2.5 pill: buy lisinopril online – lisinopril 20 mg generic
http://lisinopril.fun/# lisinopril 5 mg tablet price in india
generic zithromax azithromycin buy zithromax over the counter zithromax buy online
furosemida 40 mg: Over The Counter Lasix – buy furosemide online
https://misoprostol.shop/# Misoprostol 200 mg buy online
furosemide 40 mg: Buy Lasix No Prescription – lasix generic
http://lisinopril.fun/# cost of generic lisinopril 10 mg
http://tadalafilitalia.pro/# farmacia online
http://avanafilitalia.online/# farmacia online migliore
acquistare farmaci senza ricetta: dove acquistare cialis online sicuro – farmacia online senza ricetta
http://sildenafilitalia.men/# viagra generico in farmacia costo
п»їfarmacia online migliore: kamagra gold – top farmacia online
farmacia online: avanafil prezzo in farmacia – comprare farmaci online all’estero
https://farmaciaitalia.store/# farmacia online migliore
migliori farmacie online 2023 cialis generico consegna 48 ore farmacia online senza ricetta
farmacie online sicure: avanafil generico prezzo – farmacie online sicure
http://farmaciaitalia.store/# migliori farmacie online 2023
http://kamagraitalia.shop/# farmacia online senza ricetta
http://kamagraitalia.shop/# farmacia online più conveniente
cerco viagra a buon prezzo: viagra prezzo – pillole per erezione in farmacia senza ricetta
https://avanafilitalia.online/# top farmacia online
pillole per erezione immediata: sildenafil prezzo – esiste il viagra generico in farmacia
acquistare farmaci senza ricetta: Dove acquistare Cialis online sicuro – farmaci senza ricetta elenco
https://tadalafilitalia.pro/# farmacia online migliore
top farmacia online: Dove acquistare Cialis online sicuro – farmacie online autorizzate elenco
http://sildenafilitalia.men/# miglior sito per comprare viagra online
viagra originale recensioni: viagra prezzo farmacia – cialis farmacia senza ricetta
https://sildenafilitalia.men/# viagra generico in farmacia costo
http://tadalafilitalia.pro/# farmacie on line spedizione gratuita
farmaci senza ricetta elenco: farmacia online migliore – farmaci senza ricetta elenco
http://avanafilitalia.online/# farmacia online migliore
farmacie online affidabili: Farmacie a roma che vendono cialis senza ricetta – top farmacia online
medication from mexico pharmacy: mexican online pharmacies prescription drugs – mexican pharmaceuticals online
indian pharmacy reputable indian online pharmacy top 10 online pharmacy in india
https://indiapharm.life/# mail order pharmacy india
https://indiapharm.life/# indian pharmacies safe
canadian pharmacy king reviews: canadian king pharmacy – canadian discount pharmacy
canadian pharmacy india: top 10 online pharmacy in india – best india pharmacy
п»їbest mexican online pharmacies: medication from mexico pharmacy – mexican pharmacy
https://mexicanpharm.store/# mexican online pharmacies prescription drugs
indianpharmacy com: Online medicine order – top 10 pharmacies in india
https://canadapharm.shop/# pharmacy canadian superstore
india online pharmacy reputable indian online pharmacy reputable indian online pharmacy
https://canadapharm.shop/# canadian pharmacy 1 internet online drugstore
http://indiapharm.life/# Online medicine home delivery
pharmacy website india: indian pharmacy paypal – indianpharmacy com
http://indiapharm.life/# reputable indian online pharmacy
Online medicine home delivery: india pharmacy – online shopping pharmacy india
http://indiapharm.life/# cheapest online pharmacy india
buying from online mexican pharmacy: mexican pharmaceuticals online – mexican pharmacy
reputable canadian online pharmacy: legal to buy prescription drugs from canada – canadian pharmacy oxycodone
reputable canadian pharmacy canadianpharmacyworld northwest canadian pharmacy
https://indiapharm.life/# indianpharmacy com
http://indiapharm.life/# legitimate online pharmacies india
medicine in mexico pharmacies: mexican online pharmacies prescription drugs – mexican rx online
https://canadapharm.shop/# reliable canadian pharmacy
pharmacies in mexico that ship to usa: п»їbest mexican online pharmacies – buying from online mexican pharmacy
top online pharmacy india: indian pharmacy online – best online pharmacy india
http://canadapharm.shop/# reliable canadian pharmacy
pharmacies in canada that ship to the us: canadian pharmacy 365 – canadian pharmacy drugs online
http://canadapharm.shop/# canada pharmacy online
https://indiapharm.life/# reputable indian online pharmacy
certified canadian pharmacy: thecanadianpharmacy – canada rx pharmacy world
reputable indian online pharmacy online shopping pharmacy india reputable indian pharmacies
https://mexicanpharm.store/# buying prescription drugs in mexico
Online medicine order: best online pharmacy india – cheapest online pharmacy india
adderall canadian pharmacy: online canadian pharmacy review – northern pharmacy canada
http://mexicanpharm.store/# mexican rx online
canadian online drugs: cheapest pharmacy canada – canada drugs
average cost of generic zithromax where to buy zithromax in canada buy zithromax online australia
how to buy zithromax online: buy zithromax online – generic zithromax india
http://nolvadex.pro/# is nolvadex legal
The pharmacists always take the time to answer my questions https://clomidpharm.shop/# cost generic clomid pills
http://zithromaxpharm.online/# zithromax price canada
cost of generic clomid without prescription: where to buy clomid – clomid prices
https://nolvadex.pro/# does tamoxifen cause weight loss
Trusted by patients from all corners of the world https://clomidpharm.shop/# how can i get clomid without rx
buy cytotec pills online cheap: cytotec abortion pill – buy cytotec over the counter
http://clomidpharm.shop/# how to get cheap clomid prices
Always delivering international quality http://prednisonepharm.store/# prednisone 60 mg tablet
tamoxifen vs raloxifene tamoxifen benefits tamoxifen 20 mg
I always find great deals in their monthly promotions http://zithromaxpharm.online/# purchase zithromax online
http://prednisonepharm.store/# prednisone where can i buy
Misoprostol 200 mg buy online: cytotec pills buy online – buy cytotec online fast delivery
http://zithromaxpharm.online/# zithromax pill
п»їExceptional service every time http://clomidpharm.shop/# how can i get cheap clomid no prescription
https://prednisonepharm.store/# prednisone where can i buy
cytotec buy online usa: order cytotec online – buy cytotec online fast delivery
Trustworthy and reliable, every single visit https://zithromaxpharm.online/# buy generic zithromax online
http://cytotec.directory/# п»їcytotec pills online
zithromax zithromax coupon buy zithromax canada
buy cytotec over the counter: cytotec pills online – Abortion pills online
Consistency, quality, and care on an international level http://prednisonepharm.store/# where can i buy prednisone without prescription
https://cytotec.directory/# buy cytotec pills online cheap
cytotec abortion pill: buy cytotec – cytotec online
Drugs information sheet http://prednisonepharm.store/# prednisone 5 mg tablet price
http://cytotec.directory/# Misoprostol 200 mg buy online
https://prednisonepharm.store/# 60 mg prednisone daily
Their international patient care is impeccable http://prednisonepharm.store/# prednisone 30 mg coupon
zithromax 250 mg australia: buy zithromax 1000mg online – can you buy zithromax online
24 hour pharmacy: mexican drug pharmacy – overseas no rx drugs online
ed dysfunction treatment: men’s ed pills – treatment of ed
list of mexican pharmacies best online canadian pharmacies online canadian pharmacies
https://edpills.bid/# ed medications list
ed meds online without doctor prescription: buy prescription drugs online – п»їprescription drugs
viagra without a doctor prescription viagra without doctor prescription amazon prescription drugs without doctor approval
http://reputablepharmacies.online/# canadian pharmacy world
https://reputablepharmacies.online/# prescription drugs without doctor approval
viagra without doctor prescription amazon cialis without a doctor’s prescription prescription drugs online without doctor
canada pharmaceutical online ordering https://edwithoutdoctorprescription.store/# non prescription erection pills
aarp canadian pharmacies
canada drug online: list of 24 hour pharmacies – canadian online pharmacies prescription drugs
http://edpills.bid/# new ed pills
best non prescription ed pills sildenafil without a doctor’s prescription viagra without a doctor prescription
best pill for ed: cheap erectile dysfunction pills online – best medication for ed
buy prescription drugs from canada: prescription drugs online without doctor – п»їprescription drugs
compare ed drugs erectile dysfunction drugs cheapest ed pills online
https://edwithoutdoctorprescription.store/# buy prescription drugs without doctor
http://edpills.bid/# best ed pills online
online pharmacies canadian: reliable online canadian pharmacy – discount drug store online shopping
buy prescription drugs without doctor ed meds online without doctor prescription viagra without a prescription
best online pharmacy no prescription https://edpills.bid/# cheapest ed pills
mail order prescription drugs
https://reputablepharmacies.online/# canadian drugstore cialis
cheap meds no prescription: best canadian drugstore – canadian pharmacy certified
п»їprescription drugs prescription drugs ed meds online without doctor prescription
ed medication online: treatment of ed – best over the counter ed pills
canadian pharcharmy online: drugs from canada with prescription – online pharmacy no scripts
canadian pharmacy cialis cheap canadian drugstore cialis canadian pharmacies that are legit
http://edwithoutdoctorprescription.store/# prescription drugs online
new ed pills best treatment for ed otc ed pills
erection pills online: ed pills gnc – online ed medications
http://edpills.bid/# cures for ed
http://edwithoutdoctorprescription.store/# prescription drugs online without doctor
Online medicine order: international medicine delivery from india – top 10 pharmacies in india indianpharmacy.shop
online pharmacy india indian pharmacy to usa world pharmacy india indianpharmacy.shop
https://mexicanpharmacy.win/# buying prescription drugs in mexico mexicanpharmacy.win
indian pharmacy online: indianpharmacy com – online shopping pharmacy india indianpharmacy.shop
pharmacies in mexico that ship to usa mexican pharmacy online mexico pharmacy mexicanpharmacy.win
https://mexicanpharmacy.win/# buying from online mexican pharmacy mexicanpharmacy.win
https://mexicanpharmacy.win/# mexico pharmacy mexicanpharmacy.win
http://canadianpharmacy.pro/# best canadian online pharmacy canadianpharmacy.pro
canadian online pharmacies
indian pharmacies safe Order medicine from India to USA buy medicines online in india indianpharmacy.shop
indian pharmacy: Best Indian pharmacy – reputable indian pharmacies indianpharmacy.shop
https://canadianpharmacy.pro/# canadian pharmacy price checker canadianpharmacy.pro
canadian pharmacy reviews Cheapest drug prices Canada canadian pharmacy antibiotics canadianpharmacy.pro
best india pharmacy: indian pharmacy – buy prescription drugs from india indianpharmacy.shop
http://indianpharmacy.shop/# buy medicines online in india indianpharmacy.shop
best india pharmacy Order medicine from India to USA top 10 online pharmacy in india indianpharmacy.shop
http://indianpharmacy.shop/# indianpharmacy com indianpharmacy.shop
https://canadianpharmacy.pro/# canadian online drugstore canadianpharmacy.pro
my canadian pharmacy Pharmacies in Canada that ship to the US reliable canadian pharmacy canadianpharmacy.pro
https://mexicanpharmacy.win/# mexican drugstore online mexicanpharmacy.win
canadian pharmacy no prescription required
http://canadianpharmacy.pro/# canadian pharmacy online canadianpharmacy.pro
mail order pharmacy india
legitimate canadian pharmacy Pharmacies in Canada that ship to the US canadianpharmacymeds com canadianpharmacy.pro
http://mexicanpharmacy.win/# mexico pharmacies prescription drugs mexicanpharmacy.win
https://canadianpharmacy.pro/# canadianpharmacymeds com canadianpharmacy.pro
Online medicine home delivery
https://mexicanpharmacy.win/# buying from online mexican pharmacy mexicanpharmacy.win
https://canadianpharmacy.pro/# vipps canadian pharmacy canadianpharmacy.pro
top 10 online pharmacy in india
http://canadianpharmacy.pro/# canadian online pharmacy canadianpharmacy.pro
п»їbest mexican online pharmacies Medicines Mexico mexican online pharmacies prescription drugs mexicanpharmacy.win
http://mexicanpharmacy.win/# mexican border pharmacies shipping to usa mexicanpharmacy.win
reputable indian online pharmacy
http://indianpharmacy.shop/# buy medicines online in india indianpharmacy.shop
india pharmacy Cheapest online pharmacy top 10 online pharmacy in india indianpharmacy.shop
http://canadianpharmacy.pro/# northwest canadian pharmacy canadianpharmacy.pro
https://mexicanpharmacy.win/# medication from mexico pharmacy mexicanpharmacy.win
india online pharmacy
http://mexicanpharmacy.win/# best online pharmacies in mexico mexicanpharmacy.win
Online medicine order indian pharmacy to usa reputable indian online pharmacy indianpharmacy.shop
http://mexicanpharmacy.win/# mexico drug stores pharmacies mexicanpharmacy.win
best online pharmacy india
http://mexicanpharmacy.win/# mexican drugstore online mexicanpharmacy.win
п»їlegitimate online pharmacies india international medicine delivery from india reputable indian online pharmacy indianpharmacy.shop
http://indianpharmacy.shop/# india pharmacy mail order indianpharmacy.shop
india online pharmacy
https://canadianpharmacy.pro/# canadian discount pharmacy canadianpharmacy.pro
aarp recommended canadian pharmacies
https://canadianpharmacy.pro/# pharmacy canadian canadianpharmacy.pro
Viagra gГ©nГ©rique sans ordonnance en pharmacie: viagrasansordonnance.pro – Prix du Viagra en pharmacie en France
Pharmacie en ligne livraison rapide Acheter Cialis pharmacie ouverte 24/24
http://levitrasansordonnance.pro/# pharmacie ouverte
Pharmacies en ligne certifiГ©es
http://cialissansordonnance.shop/# Pharmacie en ligne livraison gratuite
Pharmacie en ligne livraison 24h: levitra generique – Pharmacie en ligne France
Pharmacie en ligne France kamagra gel Pharmacie en ligne France
Viagra vente libre pays: Viagra sans ordonnance pharmacie France – Viagra pas cher livraison rapide france
Viagra Pfizer sans ordonnance: Viagra gГ©nГ©rique sans ordonnance en pharmacie – Viagra homme sans prescription
http://viagrasansordonnance.pro/# Acheter Sildenafil 100mg sans ordonnance
Pharmacies en ligne certifiГ©es levitra generique prix en pharmacie acheter medicament a l etranger sans ordonnance
pharmacie ouverte: achat kamagra – acheter mГ©dicaments Г l’Г©tranger
http://cialissansordonnance.shop/# Pharmacie en ligne pas cher
Pharmacie en ligne livraison rapide pharmacie en ligne Pharmacie en ligne livraison rapide
http://cialissansordonnance.shop/# Pharmacie en ligne livraison 24h
acheter medicament a l etranger sans ordonnance
Viagra gГ©nГ©rique pas cher livraison rapide: Viagra generique en pharmacie – Viagra pas cher livraison rapide france
https://pharmadoc.pro/# Pharmacies en ligne certifiées
Pharmacie en ligne sans ordonnance: pharmacie en ligne sans ordonnance – Pharmacie en ligne fiable
Viagra femme ou trouver Viagra generique en pharmacie Viagra pas cher inde
Viagra sans ordonnance 24h: Meilleur Viagra sans ordonnance 24h – Viagra gГ©nГ©rique sans ordonnance en pharmacie
http://acheterkamagra.pro/# Pharmacie en ligne fiable
pharmacie ouverte 24/24: Acheter mГ©dicaments sans ordonnance sur internet – acheter mГ©dicaments Г l’Г©tranger
Pharmacie en ligne pas cher pharmacie en ligne sans ordonnance pharmacie ouverte 24/24
Pharmacie en ligne livraison 24h: pharmacie en ligne pas cher – Pharmacie en ligne sans ordonnance
https://levitrasansordonnance.pro/# acheter mГ©dicaments Г l’Г©tranger
п»їpharmacie en ligne
cost of ivermectin pill: where to buy stromectol – ivermectin purchase
amoxicillin 500mg for sale uk amoxicillin 775 mg buy amoxicillin 500mg capsules uk
prednisone pills for sale: can you buy prednisone over the counter in usa – prednisone pharmacy prices
https://amoxicillin.bid/# amoxicillin 500
cost cheap clomid without dr prescription: where can i get cheap clomid – can you buy clomid for sale
buy zithromax online australia buy zithromax 1000 mg online generic zithromax 500mg india
http://azithromycin.bid/# zithromax online australia
buy zithromax: buy generic zithromax online – where can i buy zithromax uk
http://ivermectin.store/# stromectol covid 19
cost of ivermectin stromectol order ivermectin pills human
can i order prednisone: buy prednisone no prescription – prednisone for sale without a prescription
zithromax 1000 mg pills: buy cheap generic zithromax – zithromax online usa
http://ivermectin.store/# stromectol lotion
antibiotic amoxicillin amoxicillin 250 mg capsule buy amoxicillin 250mg
zithromax 250 mg pill: zithromax 250 mg tablet price – zithromax tablets for sale
https://azithromycin.bid/# zithromax 500mg over the counter
prednisone 2.5 mg tab: buy prednisone no prescription – prednisone pharmacy
https://azithromycin.bid/# zithromax 600 mg tablets
buy prednisone nz prednisone without rx prednisone where can i buy
cheap clomid for sale: clomid generics – buy cheap clomid without prescription
http://clomiphene.icu/# can i purchase clomid price
amoxicillin buy online canada: amoxicillin 50 mg tablets – can you buy amoxicillin over the counter in canada
http://clomiphene.icu/# can i order clomid for sale
ivermectin goodrx ivermectin buy nz cost of ivermectin medicine
ivermectin buy: stromectol pills – ivermectin generic
https://amoxicillin.bid/# amoxicillin 875 125 mg tab
prednisone 5mg capsules: prednisone 30 – buy prednisone online without a script
buy 10 mg prednisone can you buy prednisone over the counter in usa prednisone 50 mg coupon
ivermectin 3mg dose: topical ivermectin cost – ivermectin 0.5 lotion india
https://prednisonetablets.shop/# buy prednisone online paypal
https://amoxicillin.bid/# price for amoxicillin 875 mg
can you buy zithromax over the counter: can i buy zithromax over the counter in canada – generic zithromax online paypal
prednisone 60 mg price order prednisone 10mg buying prednisone without prescription
buy prescription drugs from india: Indian pharmacy to USA – reputable indian pharmacies indianpharm.store
mexico pharmacies prescription drugs Online Pharmacies in Mexico purple pharmacy mexico price list mexicanpharm.shop
canadian pharmacy service: Best Canadian online pharmacy – canadian pharmacy no rx needed canadianpharm.store
https://canadianpharm.store/# canadianpharmacyworld canadianpharm.store
ed meds online canada: Licensed Online Pharmacy – my canadian pharmacy review canadianpharm.store
reputable indian online pharmacy best online pharmacy india Online medicine home delivery indianpharm.store
http://mexicanpharm.shop/# best online pharmacies in mexico mexicanpharm.shop
world pharmacy india: online shopping pharmacy india – pharmacy website india indianpharm.store
http://indianpharm.store/# Online medicine home delivery indianpharm.store
п»їbest mexican online pharmacies Online Mexican pharmacy purple pharmacy mexico price list mexicanpharm.shop
http://indianpharm.store/# pharmacy website india indianpharm.store
mexico pharmacies prescription drugs: Certified Pharmacy from Mexico – mexican mail order pharmacies mexicanpharm.shop
canadian pharmacy uk delivery: Canadian Pharmacy – precription drugs from canada canadianpharm.store
medicine in mexico pharmacies: Certified Pharmacy from Mexico – mexican pharmaceuticals online mexicanpharm.shop
top 10 pharmacies in india: online pharmacy india – indian pharmacy online indianpharm.store
https://canadianpharm.store/# best canadian pharmacy to order from canadianpharm.store
best rated canadian pharmacy: Pharmacies in Canada that ship to the US – canadian pharmacies comparison canadianpharm.store
http://indianpharm.store/# top online pharmacy india indianpharm.store
online shopping pharmacy india buy medicines online in india Online medicine order indianpharm.store
legit canadian online pharmacy: Best Canadian online pharmacy – canadian pharmacy 24 com canadianpharm.store
mexican rx online: mexico drug stores pharmacies – buying prescription drugs in mexico mexicanpharm.shop
https://indianpharm.store/# top online pharmacy india indianpharm.store
http://indianpharm.store/# indian pharmacy paypal indianpharm.store
online shopping pharmacy india international medicine delivery from india reputable indian online pharmacy indianpharm.store
pharmacies in mexico that ship to usa: Online Pharmacies in Mexico – mexico pharmacies prescription drugs mexicanpharm.shop
precription drugs from canada: Canada Pharmacy online – canada pharmacy online legit canadianpharm.store
http://indianpharm.store/# top 10 online pharmacy in india indianpharm.store
medication from mexico pharmacy: Certified Pharmacy from Mexico – mexican rx online mexicanpharm.shop
canadian pharmacy online ship to usa Canadian Pharmacy legitimate canadian mail order pharmacy canadianpharm.store
https://mexicanpharm.shop/# best mexican online pharmacies mexicanpharm.shop
reliable canadian online pharmacy: Canadian International Pharmacy – canadian pharmacy 365 canadianpharm.store
top 10 online pharmacy in india: Indian pharmacy to USA – online shopping pharmacy india indianpharm.store
canada cloud pharmacy Canadian Pharmacy online pharmacy canada canadianpharm.store
http://indianpharm.store/# online pharmacy india indianpharm.store
mexican pharmaceuticals online: Online Mexican pharmacy – buying prescription drugs in mexico online mexicanpharm.shop
best online pharmacy india: Indian pharmacy to USA – top online pharmacy india indianpharm.store
http://canadianpharm.store/# ed meds online canada canadianpharm.store
http://canadianpharm.store/# safe online pharmacies in canada canadianpharm.store
mexican pharmacy Online Mexican pharmacy buying prescription drugs in mexico online mexicanpharm.shop
mexico pharmacies prescription drugs: Online Mexican pharmacy – mexican border pharmacies shipping to usa mexicanpharm.shop
https://indianpharm.store/# best online pharmacy india indianpharm.store
mexico pharmacy: Online Mexican pharmacy – medication from mexico pharmacy mexicanpharm.shop
indian pharmacy Indian pharmacy to USA reputable indian online pharmacy indianpharm.store
Online medicine order: international medicine delivery from india – online shopping pharmacy india indianpharm.store
canadian king pharmacy: Best Canadian online pharmacy – canadadrugpharmacy com canadianpharm.store
http://indianpharm.store/# indianpharmacy com indianpharm.store
mexican online pharmacies prescription drugs: Certified Pharmacy from Mexico – mexico drug stores pharmacies mexicanpharm.shop
https://indianpharm.store/# Online medicine home delivery indianpharm.store
medication from mexico pharmacy Certified Pharmacy from Mexico buying from online mexican pharmacy mexicanpharm.shop
reputable online canadian pharmacy: universal canadian pharmacy – no prior prescription required pharmacy
accredited canadian pharmacies prescription drugs without doctor approval tadalafil canadian pharmacy
compare prescription drug prices: reputable canadian pharmacy – online medications
https://canadadrugs.pro/# accredited canadian pharmacies
canadian medications: canadian pharmacy antiobotics without perscription – canadian drug store coupon
overseas no rx drugs online internet pharmacy no prescription canada drugs online review
trusted canadian online pharmacy: reliable online drugstore – prescription drugs without doctor
http://canadadrugs.pro/# canada pharmacy
medication online: international pharmacies – drugstore online shopping
canadian pharmacy world online pharmacies canada reviews canadian pharmacy azithromycin
pharmacy review: trust pharmacy canada – reputable online pharmacy
https://canadadrugs.pro/# prescription drugs online
most reliable online pharmacy: azithromycin canadian pharmacy – canadian internet pharmacies
online canadian pharcharmy canadian pharmacies that deliver to the us rx online no prior prescription
legit canadian pharmacy online: canada pharmacies online – no prescription canadian pharmacies
https://canadadrugs.pro/# canadian pharmacy ship to us
discount canadian pharmacy: overseas pharmacy – list of trusted canadian pharmacies
canada online pharmacy reviews canadian pharmacy worldwide canadian pharmacy store
canadian drug store: canadian drug store cialis – best online international pharmacies
http://canadadrugs.pro/# non prescription drugs
great canadian pharmacy: canadian pharmacy non prescription – prescription drug discounts
my canadian family pharmacy: buy online prescription drugs – canadapharmacyonline com
https://canadadrugs.pro/# canadian drug company
internet pharmacy list: online pharmacy without precriptions – top rated online canadian pharmacies
http://canadadrugs.pro/# prescription drug prices
best canadian pharmacies online: legitimate canadian mail order pharmacies – online pharmacy
https://canadadrugs.pro/# non prescription on line pharmacies
top mail order pharmacies in usa: canada pharmacy online reviews – verified canadian pharmacies
international pharmacies that ship to the usa: prednisone mexican pharmacy – legitimate canadian internet pharmacies
reputable canadian online pharmacies: mexican pharmacy testosterone – best internet pharmacies
http://canadadrugs.pro/# discount pharmacy coupons
prescription drug price comparison: prescription drug prices comparison – canadian online pharmacies
http://canadadrugs.pro/# canadian pharmacy
cheap prescriptions: canadian pharmacies without an rx – list of canada online pharmacies
drugs without a prescription online pharmacy review canadian pharmacy generic
real cialis without a doctor’s prescription best ed pills non prescription ed meds online without doctor prescription
sildenafil without a doctor’s prescription: cialis without a doctor prescription – non prescription ed drugs
reputable mexican pharmacies online: medication from mexico pharmacy – buying prescription drugs in mexico
viagra without a prescription generic cialis without a doctor prescription viagra without a doctor prescription walmart
https://edpill.cheap/# best ed treatment pills
cheap erectile dysfunction: best male ed pills – ed pills cheap
top 10 pharmacies in india pharmacy website india indian pharmacy online
https://edpill.cheap/# pills for erection
http://edwithoutdoctorprescription.pro/# discount prescription drugs
medicine in mexico pharmacies mexico drug stores pharmacies mexican mail order pharmacies
best male enhancement pills: top ed pills – ed meds
http://medicinefromindia.store/# indian pharmacies safe
mexican border pharmacies shipping to usa best online pharmacies in mexico medicine in mexico pharmacies
http://edpill.cheap/# best pills for ed
best ed drugs: the best ed pill – ed medication
reputable indian pharmacies indian pharmacy paypal reputable indian pharmacies
https://certifiedpharmacymexico.pro/# mexican pharmacy
ed meds online without doctor prescription: cialis without a doctor prescription – viagra without doctor prescription
medicine in mexico pharmacies: mexican online pharmacies prescription drugs – pharmacies in mexico that ship to usa
http://certifiedpharmacymexico.pro/# purple pharmacy mexico price list
indian pharmacies safe buy medicines online in india pharmacy website india
https://medicinefromindia.store/# reputable indian pharmacies
top erection pills ed meds top ed drugs
http://canadianinternationalpharmacy.pro/# prescription drugs canada buy online
prescription drugs without prior prescription cialis without a doctor prescription canada viagra without a doctor prescription
https://canadianinternationalpharmacy.pro/# best canadian online pharmacy
certified canadian international pharmacy: canadian pharmacy no scripts – the canadian pharmacy
http://certifiedpharmacymexico.pro/# mexican border pharmacies shipping to usa
ed meds online without doctor prescription cialis without a doctor prescription real viagra without a doctor prescription usa
http://medicinefromindia.store/# top 10 online pharmacy in india
buy prescription drugs without doctor generic cialis without a doctor prescription prescription drugs without doctor approval
https://canadianinternationalpharmacy.pro/# canadian pharmacy india
100mg viagra without a doctor prescription generic cialis without a doctor prescription prescription drugs online without doctor
mexican rx online: mexico drug stores pharmacies – mexican drugstore online
http://edpill.cheap/# top erection pills
buy medicines online in india top 10 online pharmacy in india indian pharmacy paypal
https://medicinefromindia.store/# reputable indian online pharmacy
mexican pharmaceuticals online mexican online pharmacies prescription drugs pharmacies in mexico that ship to usa
https://medicinefromindia.store/# best online pharmacy india
http://medicinefromindia.store/# cheapest online pharmacy india
buy prescription drugs from canada: ed prescription drugs – non prescription erection pills
https://edpill.cheap/# best ed pills
best non prescription ed pills new ed drugs top ed drugs
https://canadianinternationalpharmacy.pro/# my canadian pharmacy reviews
purple pharmacy mexico price list mexican rx online best online pharmacies in mexico
http://medicinefromindia.store/# indian pharmacy online
male erection pills best male ed pills buying ed pills online
online pharmacy india: online pharmacy india – indian pharmacies safe
http://edpill.cheap/# cheapest ed pills online
top 10 online pharmacy in india reputable indian online pharmacy pharmacy website india
https://certifiedpharmacymexico.pro/# pharmacies in mexico that ship to usa
mexican drugstore online purple pharmacy mexico price list mexico drug stores pharmacies
medicine in mexico pharmacies purple pharmacy mexico price list mexico pharmacy
https://mexicanph.com/# mexican drugstore online
pharmacies in mexico that ship to usa
buying prescription drugs in mexico mexico drug stores pharmacies reputable mexican pharmacies online
mexico drug stores pharmacies mexico pharmacy mexico drug stores pharmacies
mexican pharmaceuticals online pharmacies in mexico that ship to usa mexican drugstore online
medicine in mexico pharmacies medicine in mexico pharmacies mexico pharmacies prescription drugs
mexican mail order pharmacies mexican rx online mexican rx online
mexico drug stores pharmacies medication from mexico pharmacy buying prescription drugs in mexico
mexico pharmacy mexican online pharmacies prescription drugs medicine in mexico pharmacies
buying prescription drugs in mexico buying prescription drugs in mexico best online pharmacies in mexico
pharmacies in mexico that ship to usa reputable mexican pharmacies online mexican pharmaceuticals online
https://mexicanph.shop/# mexican mail order pharmacies
mexican rx online
pharmacies in mexico that ship to usa mexico pharmacy mexican drugstore online
mexico pharmacies prescription drugs mexico pharmacy purple pharmacy mexico price list
mexican drugstore online pharmacies in mexico that ship to usa medicine in mexico pharmacies
medication from mexico pharmacy medicine in mexico pharmacies buying prescription drugs in mexico
https://mexicanph.shop/# pharmacies in mexico that ship to usa
medication from mexico pharmacy
purple pharmacy mexico price list mexico drug stores pharmacies mexico pharmacy
mexican online pharmacies prescription drugs mexican border pharmacies shipping to usa mexican rx online
mexican online pharmacies prescription drugs mexican rx online mexican drugstore online
mexico drug stores pharmacies buying from online mexican pharmacy mexican rx online
medicine in mexico pharmacies reputable mexican pharmacies online mexico drug stores pharmacies
pharmacies in mexico that ship to usa purple pharmacy mexico price list mexican pharmaceuticals online
medication from mexico pharmacy mexico drug stores pharmacies buying prescription drugs in mexico
mexico drug stores pharmacies medicine in mexico pharmacies mexican pharmaceuticals online
buying prescription drugs in mexico buying prescription drugs in mexico online reputable mexican pharmacies online
medication from mexico pharmacy buying prescription drugs in mexico online purple pharmacy mexico price list
mexico pharmacies prescription drugs medicine in mexico pharmacies mexican pharmacy
buying prescription drugs in mexico online mexican pharmaceuticals online mexico pharmacy
reputable mexican pharmacies online reputable mexican pharmacies online mexican border pharmacies shipping to usa
mexico drug stores pharmacies buying prescription drugs in mexico online mexican border pharmacies shipping to usa
reputable mexican pharmacies online mexican border pharmacies shipping to usa mexican border pharmacies shipping to usa
buying prescription drugs in mexico mexican drugstore online mexican border pharmacies shipping to usa
mexican border pharmacies shipping to usa п»їbest mexican online pharmacies buying prescription drugs in mexico online
https://mexicanph.shop/# mexican pharmaceuticals online
buying prescription drugs in mexico
medication from mexico pharmacy buying from online mexican pharmacy mexican drugstore online
mexican drugstore online mexican online pharmacies prescription drugs pharmacies in mexico that ship to usa
mexican rx online mexican pharmacy mexican border pharmacies shipping to usa
reputable mexican pharmacies online mexico drug stores pharmacies mexican drugstore online
mexican drugstore online buying from online mexican pharmacy medicine in mexico pharmacies
mexican drugstore online purple pharmacy mexico price list best online pharmacies in mexico
mexican border pharmacies shipping to usa mexican online pharmacies prescription drugs mexico pharmacy
reputable mexican pharmacies online best online pharmacies in mexico mexican drugstore online
п»їbest mexican online pharmacies mexican drugstore online п»їbest mexican online pharmacies
purple pharmacy mexico price list mexico pharmacies prescription drugs mexico drug stores pharmacies
buying from online mexican pharmacy mexico drug stores pharmacies reputable mexican pharmacies online
https://mexicanph.shop/# mexican border pharmacies shipping to usa
medicine in mexico pharmacies
mexican mail order pharmacies mexican mail order pharmacies mexican pharmacy
mexican drugstore online purple pharmacy mexico price list buying prescription drugs in mexico online
mexican drugstore online mexican rx online pharmacies in mexico that ship to usa
mexican border pharmacies shipping to usa pharmacies in mexico that ship to usa pharmacies in mexico that ship to usa
mexico drug stores pharmacies mexican border pharmacies shipping to usa mexican rx online
medication from mexico pharmacy medication from mexico pharmacy reputable mexican pharmacies online
mexican pharmaceuticals online mexico drug stores pharmacies medicine in mexico pharmacies
medication from mexico pharmacy medication from mexico pharmacy mexican pharmaceuticals online
mexican rx online mexican rx online mexican drugstore online
purple pharmacy mexico price list mexico drug stores pharmacies mexican pharmacy
buying prescription drugs in mexico online best online pharmacies in mexico purple pharmacy mexico price list
mexico pharmacies prescription drugs medication from mexico pharmacy buying prescription drugs in mexico
mexican mail order pharmacies reputable mexican pharmacies online mexico drug stores pharmacies
best online pharmacies in mexico mexican border pharmacies shipping to usa reputable mexican pharmacies online
mexican border pharmacies shipping to usa mexican mail order pharmacies mexican mail order pharmacies
buying prescription drugs in mexico online pharmacies in mexico that ship to usa purple pharmacy mexico price list
pharmacies in mexico that ship to usa mexican drugstore online mexico drug stores pharmacies
mexican drugstore online mexican rx online mexican drugstore online
mexico pharmacies prescription drugs mexican pharmaceuticals online reputable mexican pharmacies online
mexican rx online mexican drugstore online buying prescription drugs in mexico online
buying prescription drugs in mexico online purple pharmacy mexico price list purple pharmacy mexico price list
mexican pharmacy mexican pharmaceuticals online mexican drugstore online
mexican border pharmacies shipping to usa reputable mexican pharmacies online mexican mail order pharmacies
pharmacies in mexico that ship to usa best online pharmacies in mexico mexican online pharmacies prescription drugs
http://mexicanph.com/# mexican rx online
п»їbest mexican online pharmacies
best online pharmacies in mexico mexico drug stores pharmacies purple pharmacy mexico price list
buying prescription drugs in mexico medicine in mexico pharmacies mexican mail order pharmacies
best online pharmacies in mexico buying prescription drugs in mexico online buying from online mexican pharmacy
mexico pharmacies prescription drugs buying from online mexican pharmacy medication from mexico pharmacy
best online pharmacies in mexico mexico drug stores pharmacies best mexican online pharmacies
lisinopril tablets india http://lisinoprilpharm.com/%5Dlisinopril prinivil 10 mg tab
http://amoxil.cheap/# can you buy amoxicillin uk
amoxicillin azithromycin: buy amoxicillin online with paypal – amoxicillin pills 500 mg
40 mg daily prednisone: buy prednisone online from canada – can i buy prednisone online in uk
http://furosemide.guru/# furosemide 100 mg
http://furosemide.guru/# lasix furosemide 40 mg
prednisone pill prednisone 21 pack prednisone 20 mg
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://accounts.binance.com/sv/register?ref=PORL8W0Z
http://stromectol.fun/# ivermectin 1mg
furosemida 40 mg: Over The Counter Lasix – lasix 100 mg tablet
amoxicillin 500mg tablets price in india: buy amoxicillin 500mg uk – amoxicillin cost australia
https://buyprednisone.store/# prednisone pills for sale
prednisone online prednisone buying prednisone for sale in canada
https://buyprednisone.store/# buy prednisone nz
buy zestoretic: medication lisinopril 10 mg – zestril medicine
https://amoxil.cheap/# amoxicillin pills 500 mg
purchase amoxicillin online: amoxicillin 500mg capsules uk – amoxicillin 875 mg tablet
buy furosemide online Buy Furosemide furosemide 100 mg
lasix dosage: Over The Counter Lasix – lasix generic name
https://amoxil.cheap/# amoxicillin buy no prescription
http://stromectol.fun/# purchase ivermectin
lasix 40 mg: lasix for sale – furosemide
http://amoxil.cheap/# buy cheap amoxicillin
prednisone 5 mg tablet cost prednisone cream pharmacy cost of prednisone
ivermectin 4000 mcg: stromectol 12mg online – ivermectin 4 tablets price
https://amoxil.cheap/# amoxicillin 500mg price in canada
lasix generic name: lasix generic – lasix tablet
https://stromectol.fun/# price of ivermectin tablets
order lisinopril online lisinopril 10 mg order online lisinopril 10 mg canada cost
buy amoxicillin from canada: buy amoxicillin online no prescription – medicine amoxicillin 500
ivermectin 3mg tablets price: ivermectin 6mg dosage – where to buy stromectol
https://amoxil.cheap/# amoxacillian without a percription
lasix furosemide: Buy Lasix No Prescription – lasix for sale
https://stromectol.fun/# ivermectin 1 cream
zestril price in india lisinopril 5 mg price zestril generic
http://stromectol.fun/# ivermectin 3mg dose
buy lisinopril in mexico: lisinopril hct – 1 lisinopril
lisinopril with out prescription: lisinopril for sale online – lisinopril 500 mg
https://stromectol.fun/# stromectol prices
prednisone daily how to get prednisone without a prescription prednisone 10mg
furosemida: Buy Lasix No Prescription – generic lasix
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your site? My blog site is in the very same niche as yours and my visitors would certainly benefit from a lot of the information you provide here. Please let me know if this ok with you. Thanks a lot!
https://lisinopril.top/# prinivil 10 mg tab
stromectol ivermectin buy: ivermectin 1mg – ivermectin lotion for lice
lasix online: Buy Lasix – lasix tablet
https://lisinopril.top/# generic lisinopril 5 mg
lasix 40mg Over The Counter Lasix furosemida
where to buy amoxicillin: amoxicillin from canada – amoxicillin tablet 500mg
https://lisinopril.top/# zestril
http://stromectol.fun/# stromectol 6 mg tablet
rexall pharmacy amoxicillin 500mg: amoxicillin 500mg price canada – amoxicillin azithromycin
http://lisinopril.top/# prinivil online
Wow, incredible blog layout! How long have you been blogging for? you made blogging look easy. The overall look of your site is wonderful, as well as the content!
ivermectin coronavirus ivermectin oral ivermectin over the counter uk
lasix tablet: Buy Lasix No Prescription – furosemide
http://buyprednisone.store/# pharmacy cost of prednisone
cost of lisinopril: average cost of lisinopril – rx 535 lisinopril 40 mg
http://lisinopril.top/# lisinopril 3972
lasix 100mg: Buy Furosemide – furosemida
ivermectin uk ivermectin 24 mg stromectol 3mg tablets
purchase ivermectin: stromectol xl – buy stromectol canada
https://buyprednisone.store/# prednisone 10 mg online
http://stromectol.fun/# minocycline hcl
http://furosemide.guru/# furosemide 100 mg
ivermectin uk: ivermectin 0.5 – ivermectin 3 mg tablet dosage
cost of lisinopril lisinopril 10 mg coupon buy lisinopril uk
otc prednisone cream: buy prednisone 20mg – prednisone 20mg tablets where to buy
https://stromectol.fun/# ivermectin 18mg
lasix pills: lasix 20 mg – lasix generic
https://lisinopril.top/# zestril 20
stromectol order online stromectol for sale stromectol tablets 3 mg
lasix tablet: Buy Lasix – furosemida
where can i buy amoxicillin without prec: amoxicillin 500 mg tablet price – buy amoxicillin online without prescription
http://amoxil.cheap/# can you buy amoxicillin over the counter
http://amoxil.cheap/# generic amoxicillin online
https://amoxil.cheap/# where can i buy amoxocillin
ivermectin cream 1%: ivermectin 0.5% brand name – ivermectin where to buy
amoxicillin online no prescription how much is amoxicillin purchase amoxicillin 500 mg
https://buyprednisone.store/# prednisone 15 mg daily
lasix: Buy Furosemide – lasix furosemide
furosemide 100mg: Over The Counter Lasix – lasix 40mg
https://stromectol.fun/# cost for ivermectin 3mg
Your article helped me a lot, is there any more related content? Thanks! https://www.binance.com/lv/register?ref=V2H9AFPY
cost of amoxicillin prescription price for amoxicillin 875 mg buy amoxicillin without prescription
https://stromectol.fun/# stromectol covid
can you buy prednisone: how much is prednisone 10mg – prednisone without rx
generic lasix: Buy Furosemide – lasix uses
http://lisinopril.top/# cheap lisinopril no prescription
prinivil generic: cost of lisinopril 5 mg – cheap lisinopril no prescription
https://stromectol.fun/# ivermectin 4000 mcg
lisinopril 20 mg 12.5 mg lisinopril 5 mg prices zestril 10mg
https://amoxil.cheap/# where to buy amoxicillin 500mg without prescription
https://buyprednisone.store/# cost of prednisone 10mg tablets
reputable indian pharmacies best india pharmacy best online pharmacy india
http://indianph.xyz/# cheapest online pharmacy india
mail order pharmacy india
mail order pharmacy india best online pharmacy india buy prescription drugs from india
http://indianph.com/# legitimate online pharmacies india
indian pharmacy paypal
reputable indian pharmacies Online medicine order best online pharmacy india
https://indianph.com/# online pharmacy india
Online medicine order
best india pharmacy indian pharmacies safe mail order pharmacy india
https://indianph.xyz/# best india pharmacy
https://indianph.xyz/# online pharmacy india
india online pharmacy
https://indianph.com/# world pharmacy india
indianpharmacy com
best india pharmacy world pharmacy india best india pharmacy
indianpharmacy com Online medicine order indianpharmacy com
http://indianph.com/# indian pharmacy
online pharmacy india
Your point of view caught my eye and was very interesting. Thanks. I have a question for you. https://www.binance.info/vi/join?ref=RQUR4BEO
https://nolvadex.guru/# nolvadex 20mg
tamoxifen brand name tamoxifen for sale nolvadex price
https://diflucan.pro/# diflucan for sale uk
buy cytotec over the counter: buy cytotec pills online cheap – buy cytotec pills
https://doxycycline.auction/# doxycycline 50 mg
п»їcipro generic: purchase cipro – buy cipro online
http://cipro.guru/# cipro for sale
Cytotec 200mcg price cytotec pills buy online cytotec buy online usa
http://nolvadex.guru/# tamoxifen alternatives
nolvadex online: nolvadex estrogen blocker – who should take tamoxifen
https://nolvadex.guru/# nolvadex half life
is nolvadex legal arimidex vs tamoxifen bodybuilding how to get nolvadex
https://diflucan.pro/# buy diflucan 1
https://nolvadex.guru/# where can i buy nolvadex
medicine diflucan price: diflucan price south africa – diflucan 200 mg capsules
buy cytotec online buy cytotec in usa cytotec online
http://nolvadex.guru/# common side effects of tamoxifen
http://doxycycline.auction/# doxycycline hydrochloride 100mg
purchase cytotec: buy cytotec pills online cheap – buy cytotec online
purchase cytotec Cytotec 200mcg price buy cytotec in usa
https://doxycycline.auction/# where can i get doxycycline
https://diflucan.pro/# diflucan otc canada
http://diflucan.pro/# diflucan cream
http://nolvadex.guru/# tamoxifen generic
tamoxifen lawsuit nolvadex price tamoxifen cancer
https://doxycycline.auction/# doxycycline tetracycline
https://cytotec24.shop/# Cytotec 200mcg price
http://diflucan.pro/# buy diflucan without script
generic doxycycline doxycycline 100 mg doxy
https://diflucan.pro/# where to buy diflucan in uk
https://cytotec24.shop/# Abortion pills online
buy doxycycline for dogs how to buy doxycycline online how to order doxycycline
http://sweetiefox.online/# swetie fox
doxycycline order online doxycycline hyc doxy
http://sweetiefox.online/# sweety fox
Angela White izle: abella danger filmleri – abella danger filmleri
https://angelawhite.pro/# Angela White filmleri
eva elfie: eva elfie video – eva elfie filmleri
http://angelawhite.pro/# Angela Beyaz modeli
https://sweetiefox.online/# sweety fox
https://lanarhoades.fun/# lana rhoades
http://lanarhoades.fun/# lana rhoades video
http://sweetiefox.online/# swetie fox
eva elfie filmleri: eva elfie filmleri – eva elfie video
https://lanarhoades.fun/# lana rhoades
https://angelawhite.pro/# Angela White filmleri
Sweetie Fox izle: Sweetie Fox video – Sweetie Fox video
https://sweetiefox.online/# Sweetie Fox
http://abelladanger.online/# Abella Danger
http://evaelfie.pro/# eva elfie modeli
eva elfie video: eva elfie izle – eva elfie modeli
https://sweetiefox.online/# Sweetie Fox izle
https://lanarhoades.fun/# lana rhoades modeli
eva elfie video: eva elfie filmleri – eva elfie video
http://abelladanger.online/# abella danger filmleri
http://angelawhite.pro/# Angela Beyaz modeli
http://lanarhoades.fun/# lana rhoades modeli
http://abelladanger.online/# abella danger filmleri
eva elfie video: eva elfie – eva elfie filmleri
https://abelladanger.online/# Abella Danger
https://lanarhoades.fun/# lana rhodes
?????? ????: Angela Beyaz modeli – ?????? ????
cephalexin can you drink alcohol
http://sweetiefox.online/# Sweetie Fox izle
http://evaelfie.pro/# eva elfie izle
http://lanarhoades.fun/# lana rhodes
Angela White izle: Abella Danger – abella danger filmleri
http://lanarhoades.fun/# lana rhoades filmleri
http://angelawhite.pro/# ?????? ????
https://angelawhite.pro/# Angela White
lana rhoades modeli: lana rhodes – lana rhoades modeli
https://angelawhite.pro/# Angela White filmleri
http://evaelfie.pro/# eva elfie filmleri
https://abelladanger.online/# Abella Danger
lana rhoades izle: lana rhoades – lana rhoades video
https://angelawhite.pro/# Angela White filmleri
http://abelladanger.online/# Abella Danger
https://abelladanger.online/# abella danger filmleri
Angela White video: Abella Danger – abella danger video
https://evaelfie.pro/# eva elfie filmleri
https://angelawhite.pro/# Angela Beyaz modeli
lana rhoades video: lana rhodes – lana rhoades modeli
https://lanarhoades.fun/# lana rhoades filmleri
lana rhoades boyfriend: lana rhoades hot – lana rhoades full video
http://lanarhoades.pro/# lana rhoades pics
eva elfie photo: eva elfie hd – eva elfie
http://evaelfie.site/# eva elfie full video
who is brent rivera dating: http://sweetiefox.pro/# sweetie fox full
mia malkova girl: mia malkova full video – mia malkova videos
https://lanarhoades.pro/# lana rhoades pics
eva elfie full video: eva elfie – eva elfie
https://lanarhoades.pro/# lana rhoades videos
mia malkova hd: mia malkova videos – mia malkova videos
date online free site: http://evaelfie.site/# eva elfie new videos
sweetie fox: sweetie fox full – sweetie fox full
http://evaelfie.site/# eva elfie new videos
sweetie fox: sweetie fox full video – sweetie fox new
sweetie fox video: sweetie fox video – sweetie fox video
https://evaelfie.site/# eva elfie hot
spanish dating site free trial: http://sweetiefox.pro/# sweetie fox
eva elfie full video: eva elfie – eva elfie full video
eva elfie photo: eva elfie new videos – eva elfie full videos
http://evaelfie.site/# eva elfie photo
eva elfie photo: eva elfie full videos – eva elfie hot
meet local singles free: https://miamalkova.life/# mia malkova latest
http://evaelfie.site/# eva elfie full video
lana rhoades pics: lana rhoades hot – lana rhoades
sweetie fox new: sweetie fox – ph sweetie fox
sweetie fox full: sweetie fox new – sweetie fox cosplay
https://miamalkova.life/# mia malkova photos
online sex chat: https://miamalkova.life/# mia malkova photos
mia malkova videos: mia malkova hd – mia malkova new video
http://sweetiefox.pro/# ph sweetie fox
eva elfie photo: eva elfie hd – eva elfie full videos
mia malkova girl: mia malkova new video – mia malkova only fans
http://lanarhoades.pro/# lana rhoades pics
internet dating site: https://lanarhoades.pro/# lana rhoades hot
sweetie fox full: ph sweetie fox – sweetie fox new
https://evaelfie.site/# eva elfie new videos
eva elfie new video: eva elfie new video – eva elfie full video
aviator bet malawi login: aviator bet malawi – aviator game
http://aviatormocambique.site/# aviator
https://aviatormocambique.site/# aviator
aviator game: jogar aviator online – aviator game
https://aviatormalawi.online/# aviator game online
http://pinupcassino.pro/# pin-up casino login
aviator bet: aviator – aviator game online
https://aviatormalawi.online/# aviator bet malawi
pin-up casino: pin up – pin up cassino online
https://aviatormalawi.online/# aviator game
cassino pin up: aviator pin up casino – pin-up casino entrar
pin up aviator: pin up aviator – aviator betano
https://jogodeaposta.fun/# melhor jogo de aposta para ganhar dinheiro
aviator pin up: jogar aviator online – aviator bet
http://aviatorghana.pro/# aviator game bet
pin-up casino login: pin up casino – pin up aviator
aviator pin up: aviator game – pin up aviator
aviator pin up casino: pin up bet – pin-up casino
estrela bet aviator: aviator betano – aviator game
https://aviatormocambique.site/# aviator bet
aviator moçambique: aviator bet – como jogar aviator em moçambique
aviator: pin up aviator – aviator oyunu
aviator online: como jogar aviator – aviator online
como jogar aviator: aviator moçambique – aviator mz
http://aviatorjogar.online/# aviator jogar
deposito minimo 1 real: aviator jogo de aposta – site de apostas
buy cheap zithromax online – https://azithromycin.pro/zithromax-online.html can i buy zithromax over the counter
pin up aviator: aviator pin up – aviator jogo
https://pinupcassino.pro/# pin up
zithromax generic cost – https://azithromycin.pro/zithromax-rash.html zithromax 500mg price
aviator: como jogar aviator em moçambique – aviator moçambique
aviator jogar: aviator jogo – aviator betano
buy zithromax 500mg online: zithromax treatment zithromax online paypal
aviator jogo de aposta: site de apostas – aviator jogo de aposta
http://aviatoroyunu.pro/# pin up aviator
reputable mexican pharmacies online: order online from a Mexican pharmacy – mexican border pharmacies shipping to usa mexicanpharm.shop
https://canadianpharmlk.com/# certified canadian international pharmacy canadianpharm.store
ed meds online canada Canadian pharmacy prices legit canadian online pharmacy canadianpharm.store
canadian online pharmacy: Canada pharmacy online – canadapharmacyonline canadianpharm.store
п»їbest mexican online pharmacies: Mexico pharmacy online – mexican rx online mexicanpharm.shop
http://canadianpharmlk.com/# canadian pharmacy world canadianpharm.store
medication from mexico pharmacy: Mexico pharmacy price list – purple pharmacy mexico price list mexicanpharm.shop
https://indianpharm24.shop/# top 10 pharmacies in india indianpharm.store
http://mexicanpharm24.com/# best online pharmacies in mexico mexicanpharm.shop
pet meds without vet prescription canada Canada pharmacy canadian pharmacy ratings canadianpharm.store
http://indianpharm24.com/# online shopping pharmacy india indianpharm.store
https://indianpharm24.com/# mail order pharmacy india indianpharm.store
canadian pharmacy checker: Canadian pharmacy prices – safe canadian pharmacy canadianpharm.store
п»їbest mexican online pharmacies: order online from a Mexican pharmacy – buying prescription drugs in mexico online mexicanpharm.shop
http://mexicanpharm24.com/# pharmacies in mexico that ship to usa mexicanpharm.shop
https://mexicanpharm24.com/# mexico drug stores pharmacies mexicanpharm.shop
http://indianpharm24.shop/# india online pharmacy indianpharm.store
https://indianpharm24.shop/# online pharmacy india indianpharm.store
india online pharmacy: Pharmacies in India that ship to USA – best online pharmacy india indianpharm.store
https://indianpharm24.shop/# top online pharmacy india indianpharm.store
https://indianpharm24.com/# reputable indian online pharmacy indianpharm.store
trusted canadian pharmacy Certified Canadian pharmacies canadian pharmacy prices canadianpharm.store
https://mexicanpharm24.com/# buying prescription drugs in mexico mexicanpharm.shop
https://canadianpharmlk.shop/# cheapest pharmacy canada canadianpharm.store
canadian compounding pharmacy: My Canadian pharmacy – canadapharmacyonline legit canadianpharm.store
https://indianpharm24.com/# buy medicines online in india indianpharm.store
canadian pharmacy world reviews: My Canadian pharmacy – buy canadian drugs canadianpharm.store
http://indianpharm24.shop/# india online pharmacy indianpharm.store
https://mexicanpharm24.shop/# medication from mexico pharmacy mexicanpharm.shop
online canadian pharmacy: Best Canadian online pharmacy – onlinecanadianpharmacy 24 canadianpharm.store
https://mexicanpharm24.shop/# mexico drug stores pharmacies mexicanpharm.shop
https://canadianpharmlk.shop/# best canadian online pharmacy reviews canadianpharm.store
http://canadianpharmlk.com/# reputable canadian pharmacy canadianpharm.store
best india pharmacy online pharmacy in india buy medicines online in india indianpharm.store
http://indianpharm24.com/# online pharmacy india indianpharm.store
п»їbest mexican online pharmacies: order online from a Mexican pharmacy – purple pharmacy mexico price list mexicanpharm.shop
https://indianpharm24.shop/# buy medicines online in india indianpharm.store
mexican border pharmacies shipping to usa: Medicines Mexico – mexican pharmaceuticals online mexicanpharm.shop
https://indianpharm24.shop/# cheapest online pharmacy india indianpharm.store
https://canadianpharmlk.shop/# canadian drug pharmacy canadianpharm.store
http://indianpharm24.shop/# top 10 pharmacies in india indianpharm.store
can i buy amoxicillin online: amoxicillin 500 mg cost – amoxicillin from canada
buy prednisone without rx: prednisone killed my dog – 80 mg prednisone daily
amoxicillin 500 mg tablet price: amoxicillin para que sirve – can you buy amoxicillin over the counter
https://amoxilst.pro/# how much is amoxicillin prescription
prednisone generic brand name: buy prednisone no prescription – canine prednisone 5mg no prescription
canadian online pharmacy prednisone: prednisone pill 20 mg – prednisone 40 mg
amoxicillin 500 mg tablet: generic amoxicillin 500mg – amoxicillin 500 mg cost
order cheap clomid now where to buy clomid pill clomid tablet
prednisone 40 mg: how long does prednisone last – prednisone in india
amoxicillin for sale: can you take nyquil with amoxicillin – cheap amoxicillin 500mg
cost clomid without a prescription: clomid price – how to buy generic clomid no prescription
http://clomidst.pro/# can i get cheap clomid online
where can i get generic clomid now: clomid iui – order generic clomid
amoxicillin order online no prescription: can you take amoxicillin with tylenol – cost of amoxicillin 30 capsules
what is diclofenac pot
how to get generic clomid no prescription: taking clomid and testosterone together – cost of cheap clomid pills
prednisone 20 mg: can i buy prednisone over the counter in usa – best pharmacy prednisone
https://amoxilst.pro/# amoxicillin over counter
ezetimibe drug classification
order generic clomid pill can you get generic clomid cost of clomid
can you buy amoxicillin over the counter canada: what is amoxicillin used for – amoxicillin 775 mg
can i purchase generic clomid without dr prescription: where can i get clomid without prescription – can you buy clomid prices
prednisone 5mg daily: can you drink alcohol while taking prednisone – prednisone over the counter south africa
augmentin and breastfeeding
https://amoxilst.pro/# order amoxicillin online no prescription
30mg prednisone: buy prednisone without a prescription – cost of prednisone in canada
where buy clomid online: clomid dosage for male testosterone – clomid no prescription
prednisone 2 mg: prednisone generic name – prednisone ordering online
http://prednisonest.pro/# prednisone 15 mg tablet
where buy cheap clomid pill: alternative to clomid – how can i get generic clomid
cost of amoxicillin 30 capsules: amoxil pediatrico – cost of amoxicillin 875 mg
generic prednisone for sale: prednisone 20 mg pill – buy prednisone no prescription
online pharmacy without a prescription: pharmacies without prescriptions – buying online prescription drugs
https://edpills.guru/# buy erectile dysfunction pills
buy ed medication erection pills online where to get ed pills
buy ed pills online: erectile dysfunction online prescription – buy ed meds
https://edpills.guru/# ed medicine online
canadian prescription: pharmacy with no prescription – canadian pharmacy without prescription
http://pharmnoprescription.pro/# canada pharmacy without prescription
canadian pharmacy no prescription needed: online pharmacy delivery – canadian pharmacy no prescription
best online pharmacy that does not require a prescription in india: non prescription online pharmacy – prescription drugs canada
http://edpills.guru/# online ed meds
buy prescription drugs on line: buy prescription online – order prescription from canada
no prescription needed canadian pharmacy: pharmacy online – non prescription medicine pharmacy
canadian pharmacy without prescription online mexican pharmacy online pharmacy non prescription drugs
online erectile dysfunction medication: cheapest erectile dysfunction pills – online ed prescription
https://edpills.guru/# ed prescriptions online
https://edpills.guru/# ed treatments online
online pharmacy no prescription: canada pharmacy online – pharmacy no prescription required
canadian pharmacy without prescription: online pharmacy – cheapest pharmacy to fill prescriptions without insurance
non prescription online pharmacy: legitimate online pharmacy no prescription – legitimate online pharmacy no prescription
http://onlinepharmacy.cheap/# cheapest prescription pharmacy
cheapest pharmacy to fill prescriptions without insurance: discount pharmacy – no prescription required pharmacy
cheap ed treatment: cheap ed drugs – best online ed pills
http://edpills.guru/# cheap ed pills online
buy ed meds: how to get ed pills – edmeds
http://pharmnoprescription.pro/# order prescription drugs online without doctor
ed medicines: low cost ed pills – online ed pharmacy
non prescription online pharmacy india online pharmacies without prescription online pharmacy reviews no prescription
canadian pharmacy world coupon: Cheapest online pharmacy – overseas pharmacy no prescription
order medication without prescription: medications online without prescription – no prescription needed
https://mexicanpharm.online/# mexican online pharmacies prescription drugs
mexico drug stores pharmacies: pharmacies in mexico that ship to usa – mexican mail order pharmacies
canadian world pharmacy: canadian pharmacy ed medications – canada pharmacy online
http://mexicanpharm.online/# mexican mail order pharmacies
canada cloud pharmacy online canadian pharmacy review canadian pharmacy review
buy medicines online in india: buy medicines online in india – best india pharmacy
https://pharmacynoprescription.pro/# ordering prescription drugs from canada
indian pharmacy: п»їlegitimate online pharmacies india – india pharmacy
https://indianpharm.shop/# indian pharmacy online
legit canadian pharmacy: the canadian pharmacy – pharmacy wholesalers canada
order prescription from canada: best online pharmacy that does not require a prescription in india – canadian pharmacy no prescription required
buying from online mexican pharmacy: mexico pharmacies prescription drugs – purple pharmacy mexico price list
https://mexicanpharm.online/# medication from mexico pharmacy
is canadian pharmacy legit: northwest pharmacy canada – cheapest pharmacy canada
order medication without prescription prescription online canada can i buy prescription drugs in canada
http://indianpharm.shop/# buy prescription drugs from india
https://canadianpharm.guru/# canadian pharmacy online ship to usa
canadian pharmacy cheap: canadian drugs – escrow pharmacy canada
mexican border pharmacies shipping to usa: medicine in mexico pharmacies – medication from mexico pharmacy
canadian rx prescription drugstore: buy drugs online no prescription – best no prescription online pharmacies
buying prescription drugs from canada online: canadian pharmacy online no prescription needed – online pharmacy no prescription needed
http://pharmacynoprescription.pro/# how to order prescription drugs from canada
canadian prescription: canadian drugs no prescription – online pharmacies no prescription usa
buy medicines online in india: world pharmacy india – indian pharmacy
http://pharmacynoprescription.pro/# canadian pharmacy online no prescription needed
canadian king pharmacy: northwest pharmacy canada – safe reliable canadian pharmacy
mail order pharmacy india: buy medicines online in india – mail order pharmacy india
cheap drugs no prescription buy medications without prescriptions buying drugs online no prescription
non prescription canadian pharmacy: overseas online pharmacy-no prescription – canadian pharmacy non prescription
http://pharmacynoprescription.pro/# how to get a prescription in canada
online shopping pharmacy india: indian pharmacies safe – indianpharmacy com
http://indianpharm.shop/# indian pharmacy paypal
no prescription on line pharmacies: online canadian pharmacy no prescription – online pharmacy without a prescription
prescription drugs canada buy online: canadian pharmacy victoza – best canadian online pharmacy
the canadian drugstore: vipps approved canadian online pharmacy – online canadian pharmacy reviews
best website to buy prescription drugs: prescription from canada – online pharmacy no prescription
online shopping pharmacy india: indian pharmacy – online pharmacy india
canadian drugs pharmacy canadian online pharmacy reviews legitimate canadian pharmacies
https://pharmacynoprescription.pro/# online pharmacy that does not require a prescription
meds online no prescription: pharmacy with no prescription – online pharmacy without prescription
http://canadianpharm.guru/# cheapest pharmacy canada
canada pharmacy no prescription: buying prescription drugs online canada – buy pills without prescription
online shopping pharmacy india: indianpharmacy com – top 10 online pharmacy in india
http://pharmacynoprescription.pro/# prescription canada
buy medications online no prescription: canadian pharmacy online no prescription needed – canada mail order prescription
https://pharmacynoprescription.pro/# buying prescription drugs online from canada
buy drugs without prescription: no prescription online pharmacies – purchasing prescription drugs online
indian pharmacies safe: indian pharmacies safe – indianpharmacy com
buying from online mexican pharmacy: reputable mexican pharmacies online – mexican pharmaceuticals online
Online medicine home delivery best online pharmacy india indian pharmacy paypal
pharmacies in mexico that ship to usa: mexico drug stores pharmacies – mexico drug stores pharmacies
http://indianpharm.shop/# reputable indian pharmacies
http://indianpharm.shop/# Online medicine order
is canadian pharmacy legit: canadian pharmacy prices – canadian pharmacy king
mexican pharmacy: mexican pharmaceuticals online – mexican border pharmacies shipping to usa
buying from online mexican pharmacy: medicine in mexico pharmacies – mexican online pharmacies prescription drugs
mexican drugstore online: mexico pharmacy – mexico drug stores pharmacies
https://pharmacynoprescription.pro/# order prescription drugs online without doctor
ordering drugs from canada: canadian pharmacy sarasota – best canadian pharmacy
india pharmacy: india pharmacy – buy prescription drugs from india
https://indianpharm.shop/# top 10 online pharmacy in india
canadian pharmacy victoza: canadianpharmacyworld – is canadian pharmacy legit
mexican drugstore online mexican border pharmacies shipping to usa buying from online mexican pharmacy
online pharmacy india: world pharmacy india – best india pharmacy
https://canadianpharm.guru/# certified canadian pharmacy
mexico online pharmacy prescription drugs: medication online without prescription – buying prescription drugs in india
https://pharmacynoprescription.pro/# medications online without prescription
reputable mexican pharmacies online: pharmacies in mexico that ship to usa – mexico pharmacies prescription drugs
https://sweetbonanza.bid/# sweet bonanza demo
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
pin-up casino giris: pin up casino giris – pin up indir
http://gatesofolympus.auction/# gates of olympus oyna
https://aviatoroyna.bid/# aviator giris
pin up bet: pin up indir – pin-up casino indir
https://gatesofolympus.auction/# gates of olympus giris
gates of olympus demo: gates of olympus demo turkce oyna – gates of olympus max win
http://sweetbonanza.bid/# pragmatic play sweet bonanza
http://sweetbonanza.bid/# güncel sweet bonanza
gates of olympus slot: gates of olympus oyna ucretsiz – gates of olympus s?rlar?
https://gatesofolympus.auction/# gates of olympus hilesi
https://sweetbonanza.bid/# sweet bonanza kazanma saatleri
pragmatic play gates of olympus: gates of olympus slot – gates of olympus
aviator giris: aviator casino oyunu – aviator sinyal hilesi ucretsiz
https://sweetbonanza.bid/# sweet bonanza yasal site
pin up casino giris: pin up guncel giris – pin-up bonanza
https://aviatoroyna.bid/# aviator oyunu
http://aviatoroyna.bid/# aviator giris
http://sweetbonanza.bid/# sweet bonanza oyna
sweet bonanza yorumlar: sweet bonanza kazanc – sweet bonanza giris
http://gatesofolympus.auction/# gate of olympus hile
bonus veren casino slot siteleri: slot siteleri bonus veren – deneme bonusu veren siteler
slot siteleri bonus veren: yasal slot siteleri – guvenilir slot siteleri 2024
http://aviatoroyna.bid/# aviator oyna slot
http://slotsiteleri.guru/# oyun siteleri slot
aviator oyna 100 tl: aviator giris – aviator oyna
http://gatesofolympus.auction/# gates of olympus 1000 demo
http://aviatoroyna.bid/# aviator mostbet
slot oyunlari: sweet bonanza kazanc – sweet bonanza 100 tl
http://aviatoroyna.bid/# aviator casino oyunu
pragmatic play sweet bonanza: sweet bonanza bahis – sweet bonanza oyna
https://aviatoroyna.bid/# aviator hilesi
pin up casino: pin-up casino giris – pin-up casino
https://gatesofolympus.auction/# gates of olympus nasil para kazanilir
pin up casino giris: pin up aviator – pin-up casino giris
canadapharmacyonline com canadian pharmacy 24 canadian pharmacy world
reputable mexican pharmacies online: Online Pharmacies in Mexico – buying prescription drugs in mexico online
Online medicine home delivery: india pharmacy – best india pharmacy
indian pharmacy online indian pharmacy п»їlegitimate online pharmacies india
pharmacies in mexico that ship to usa: Mexican Pharmacy Online – buying from online mexican pharmacy
mexican pharmaceuticals online cheapest mexico drugs buying prescription drugs in mexico online
buying prescription drugs in mexico online: mexican pharmacy – mexico drug stores pharmacies
canadian pharmacy online reviews: Licensed Canadian Pharmacy – trustworthy canadian pharmacy
canadian pharmacy sarasota canadian pharmacy antibiotics canadian online pharmacy
mexico drug stores pharmacies: cheapest mexico drugs – buying prescription drugs in mexico online
canada drugs online reviews: Licensed Canadian Pharmacy – canada drugs online reviews
http://canadianpharmacy24.store/# canadianpharmacyworld
77 canadian pharmacy Large Selection of Medications pharmacy in canada
canadian pharmacy mall: pills now even cheaper – canada online pharmacy
canada cloud pharmacy: canadadrugpharmacy com – canadian mail order pharmacy
mexico pharmacies prescription drugs: buying from online mexican pharmacy – mexican rx online
canadian pharmacy online: Prescription Drugs from Canada – escrow pharmacy canada
medicine in mexico pharmacies: mexico drug stores pharmacies – mexico drug stores pharmacies
indian pharmacy Generic Medicine India to USA pharmacy website india
indian pharmacies safe: Healthcare and medicines from India – best online pharmacy india
canadian pharmacy ed medications: Large Selection of Medications – canadian medications
buying prescription drugs in mexico purple pharmacy mexico price list mexican border pharmacies shipping to usa
medicine in mexico pharmacies: mexican pharmacy – mexican rx online
п»їlegitimate online pharmacies india: Generic Medicine India to USA – mail order pharmacy india
http://indianpharmacy.icu/# п»їlegitimate online pharmacies india
india pharmacy mail order: indian pharmacy delivery – top 10 online pharmacy in india
mail order pharmacy india Generic Medicine India to USA cheapest online pharmacy india
mexico drug stores pharmacies: Online Pharmacies in Mexico – mexico pharmacies prescription drugs
best canadian pharmacy: Large Selection of Medications – canadian pharmacy oxycodone
reputable mexican pharmacies online: Online Pharmacies in Mexico – mexican border pharmacies shipping to usa
medicine in mexico pharmacies Online Pharmacies in Mexico mexican mail order pharmacies
best online pharmacies in mexico cheapest mexico drugs buying prescription drugs in mexico
canadian valley pharmacy: canadian pharmacies comparison – trusted canadian pharmacy
http://canadianpharmacy24.store/# canadian pharmacy uk delivery
canadian pharmacy 365: canadian pharmacy 24 – reliable canadian pharmacy
buying prescription drugs in mexico: mexican pharmacy – buying prescription drugs in mexico
canadian mail order pharmacy canada drugs online reviews escrow pharmacy canada
online pharmacy canada: canadian pharmacy 24 – ed drugs online from canada
buy prescription drugs from india: indianpharmacy com – buy prescription drugs from india
http://prednisoneall.shop/# prednisone 10 mg tablets
http://prednisoneall.com/# prednisone 12 mg
generic zithromax india zithromax tablets for sale zithromax 500 mg lowest price drugstore online
http://prednisoneall.com/# prednisone 40 mg rx
buy zithromax no prescription: zithromax 600 mg tablets – zithromax 500 tablet
https://zithromaxall.shop/# where can i buy zithromax uk
zithromax azithromycin where can i buy zithromax medicine purchase zithromax online
prednisone 20mg tablets where to buy: 50 mg prednisone canada pharmacy – prednisone for sale online
https://clomidall.shop/# can you get clomid now
http://prednisoneall.com/# where can i order prednisone 20mg
purchase prednisone buy prednisone 10 mg prednisone 20mg cheap
http://prednisoneall.com/# price for 15 prednisone
https://clomidall.shop/# where can i get cheap clomid pills
zithromax 250 price zithromax capsules 250mg zithromax 1000 mg online
https://clomidall.shop/# can i purchase clomid
http://prednisoneall.shop/# prednisone 50 mg buy
prescription for amoxicillin how to buy amoxycillin where can you get amoxicillin
prednisone 20mg price: prednisone online australia – how to buy prednisone online
http://prednisoneall.shop/# buy prednisone 50 mg
prednisone cost 10mg: average price of prednisone – order prednisone 100g online without prescription
http://zithromaxall.com/# buy zithromax without prescription online
how to buy prednisone online pharmacy cost of prednisone prednisone uk buy
https://prednisoneall.com/# 50 mg prednisone from canada
http://prednisoneall.shop/# generic prednisone online
http://prednisoneall.com/# prednisone tablet 100 mg
amoxicillin 500 mg cost of amoxicillin prescription buy amoxicillin over the counter uk
https://amoxilall.com/# buy cheap amoxicillin online
zithromax without prescription buy zithromax no prescription buy generic zithromax no prescription
200 mg prednisone daily: prednisone 20mg – prednisone pak
http://amoxilall.com/# amoxicillin 825 mg
https://prednisoneall.shop/# prednisone 40mg
can you buy zithromax over the counter in canada: zithromax pill – cost of generic zithromax
https://zithromaxall.com/# generic zithromax medicine
where to buy generic clomid tablets generic clomid without prescription can i get clomid pills
https://amoxilall.shop/# cost of amoxicillin prescription
Kamagra tablets: Kamagra Iq – super kamagra
п»їBuy generic 100mg Viagra online Viagra tablet online Sildenafil Citrate Tablets 100mg
http://sildenafiliq.com/# Viagra tablet online
http://tadalafiliq.shop/# buy cialis pill
Kamagra 100mg price: Kamagra gel – cheap kamagra
Buy generic 100mg Viagra online: generic ed pills – viagra canada
buy Viagra online buy viagra online viagra canada
Viagra tablet online: cheapest viagra – Viagra without a doctor prescription Canada
https://tadalafiliq.shop/# Generic Cialis price
Tadalafil price Buy Cialis online cialis for sale
viagra without prescription: buy viagra online – Buy Viagra online cheap
http://kamagraiq.com/# Kamagra 100mg price
Kamagra 100mg price: Kamagra 100mg price – Kamagra 100mg
https://tadalafiliq.com/# Tadalafil Tablet
Generic Cialis price cialis without a doctor prescription cheapest cialis
п»їkamagra: cheap kamagra – cheap kamagra
Buy Tadalafil 5mg: tadalafil iq – Cialis over the counter
Kamagra 100mg: Kamagra gel – Kamagra 100mg price
Cialis without a doctor prescription Generic Tadalafil 20mg price Cialis 20mg price
http://sildenafiliq.xyz/# buy Viagra over the counter
buy kamagra online usa: Kamagra Oral Jelly Price – Kamagra Oral Jelly
https://kamagraiq.com/# buy kamagra online usa
Cialis 20mg price: cialis best price – Generic Cialis without a doctor prescription
Kamagra Oral Jelly Kamagra Iq Kamagra 100mg price
http://sildenafiliq.com/# Viagra tablet online
Buy Cialis online: Buy Cialis online – buy cialis pill
http://sildenafiliq.xyz/# buy Viagra online
http://tadalafiliq.shop/# Buy Tadalafil 10mg
viagra canada: sildenafil iq – Viagra tablet online
Cialis 20mg price in USA: tadalafil iq – Buy Tadalafil 5mg
Kamagra tablets: kamagra best price – kamagra
https://kamagraiq.com/# Kamagra 100mg
sildenafil oral jelly 100mg kamagra Sildenafil Oral Jelly cheap kamagra
Cialis 20mg price: tadalafil iq – Buy Cialis online
https://kamagraiq.shop/# cheap kamagra
http://sildenafiliq.xyz/# Cheapest Sildenafil online
http://sildenafiliq.xyz/# Viagra without a doctor prescription Canada
cialis for sale cialis without a doctor prescription п»їcialis generic
buy cialis pill: cialis without a doctor prescription – Buy Tadalafil 5mg
Buy Cialis online: cialis without a doctor prescription – Cialis without a doctor prescription
http://tadalafiliq.com/# Generic Cialis without a doctor prescription
Viagra generic over the counter: buy viagra online – buy Viagra online
viagra without prescription Viagra without a doctor prescription Canada Cheap Sildenafil 100mg
Sildenafil Citrate Tablets 100mg: buy viagra online – Viagra tablet online
https://sildenafiliq.com/# sildenafil over the counter
http://sildenafiliq.xyz/# п»їBuy generic 100mg Viagra online
Cheap Cialis cheapest cialis Tadalafil price
Viagra without a doctor prescription Canada: cheapest viagra – Cheapest Sildenafil online
https://sildenafiliq.xyz/# sildenafil online
https://mexicanpharmgrx.shop/# mexico pharmacy
online pharmacy india Online medicine order world pharmacy india
mexico pharmacy: mexican pharmacy – mexican online pharmacies prescription drugs
canadian drug pharmacy List of Canadian pharmacies prescription drugs canada buy online
buying from online mexican pharmacy: Pills from Mexican Pharmacy – reputable mexican pharmacies online
http://canadianpharmgrx.com/# canadian pharmacy
canadian pharmacy price checker canadian pharmacy checker canadian pharmacy india
mexican drugstore online: Pills from Mexican Pharmacy – mexican rx online
http://mexicanpharmgrx.shop/# buying prescription drugs in mexico
indian pharmacies safe: Generic Medicine India to USA – buy prescription drugs from india
mexico pharmacy Mexico drugstore mexican drugstore online
https://indianpharmgrx.shop/# pharmacy website india
https://indianpharmgrx.com/# buy prescription drugs from india
medicine in mexico pharmacies mexican pharmacy mexico drug stores pharmacies
purple pharmacy mexico price list: Mexico drugstore – mexican drugstore online
mexico drug stores pharmacies: mexican pharmacy – mexican border pharmacies shipping to usa
https://indianpharmgrx.com/# cheapest online pharmacy india
canadian pharmacy no scripts Pharmacies in Canada that ship to the US vipps approved canadian online pharmacy
https://mexicanpharmgrx.com/# mexican border pharmacies shipping to usa
cheapest online pharmacy india: Generic Medicine India to USA – buy medicines online in india
indian pharmacy Online medicine home delivery buy prescription drugs from india
my canadian pharmacy: canadian pharmacy – legit canadian online pharmacy
http://indianpharmgrx.com/# pharmacy website india
https://mexicanpharmgrx.shop/# mexican online pharmacies prescription drugs
п»їlegitimate online pharmacies india indian pharmacy delivery reputable indian online pharmacy
india online pharmacy: Generic Medicine India to USA – reputable indian pharmacies
https://canadianpharmgrx.xyz/# my canadian pharmacy rx
reputable indian pharmacies: Online medicine home delivery – Online medicine order
buying prescription drugs in mexico mexican pharmacy buying from online mexican pharmacy
https://canadianpharmgrx.com/# canadian pharmacy ltd
india pharmacy mail order: reputable indian pharmacies – top 10 online pharmacy in india
https://mexicanpharmgrx.shop/# mexican drugstore online
indian pharmacies safe Generic Medicine India to USA best online pharmacy india
http://canadianpharmgrx.com/# best rated canadian pharmacy
п»їlegitimate online pharmacies india: Generic Medicine India to USA – mail order pharmacy india
http://canadianpharmgrx.xyz/# canadian drug
top online pharmacy india: Generic Medicine India to USA – online pharmacy india
buy cytotec pills online cheap: Abortion pills online – buy cytotec
buy cipro online without prescription where can i buy cipro online cipro 500mg best prices
generic for doxycycline: buy doxycycline – generic for doxycycline
buy ciprofloxacin: buy cipro online without prescription – cipro
price of diflucan in south africa: can you buy diflucan over the counter in australia – can you buy diflucan without a prescription
diflucan cream 150 mg diflucan online diflucan online pharmacy
buy misoprostol over the counter: buy cytotec over the counter – Abortion pills online
buy ciprofloxacin: ciprofloxacin – antibiotics cipro
buy cytotec over the counter: buy cytotec – Cytotec 200mcg price
https://nolvadex.icu/# tamoxifen joint pain
buy cytotec in usa: buy cytotec pills – cytotec pills online
buy doxycycline online uk order doxycycline online doxycycline online
buy diflucan 150mg: order diflucan online – diflucan 100
how to lose weight on tamoxifen: tamoxifen lawsuit – tamoxifen generic
tamoxifen moa: tamoxifen reviews – tamoxifen joint pain
ciprofloxacin generic cipro pharmacy ciprofloxacin
diflucan pill for sale: diflucan 50mg tablet – diflucan prescription australia
diflucan over the counter usa diflucan buy online usa over the counter diflucan cream
buy doxycycline online 270 tabs: doxycycline online – doxycycline mono
https://nolvadex.icu/# alternatives to tamoxifen
buy diflucan cheap: buying diflucan without prescription – diflucan canada
diflucan capsule price: where can i get diflucan over the counter – can i purchase diflucan over the counter
how to prevent hair loss while on tamoxifen: tamoxifen vs clomid – tamoxifen joint pain
is nolvadex legal does tamoxifen cause weight loss should i take tamoxifen
doxycycline pills: buy doxycycline cheap – price of doxycycline
diflucan prices canada where can you get diflucan diflucan brand name 300mg
doxycycline 100mg tablets: doxycycline medication – doxylin
diflucan drug: where to buy diflucan pills – diflucan 150 mg buy online uk
doxycycline pills: doxycycline prices – vibramycin 100 mg
diflucan 200mg diflucan 100 mg tablet buy diflucan no prescription
http://nolvadex.icu/# liquid tamoxifen
diflucan 150mg prescription: diflucan gel – buy diflucan cheap
200 mg doxycycline: generic doxycycline – doxycycline monohydrate
doxy buy doxycycline online doxycycline 100mg capsules
diflucan 150 mg price in india: 150 mg diflucan online – medicine diflucan price
tamoxifen citrate: tamoxifen postmenopausal – tamoxifen postmenopausal
cheap doxycycline online: doxycycline hyclate 100 mg cap – cheap doxycycline online
doxycycline hydrochloride 100mg doxycycline 100mg tablets buy cheap doxycycline
ciprofloxacin over the counter: where can i buy cipro online – cipro generic
stromectol: ivermectin 10 mg – ivermectin 15 mg
amoxicillin where to get amoxicillin canada price cheap amoxicillin 500mg
https://stromectola.top/# ivermectin ireland
order amoxicillin online: amoxicillin 500mg capsule cost – amoxicillin 500mg tablets price in india
prednisone buy no prescription: 50mg prednisone tablet – prednisone pills 10 mg
oral ivermectin cost stromectol how much it cost stromectol 3 mg price
buy amoxicillin 250mg: over the counter amoxicillin canada – amoxicillin buy no prescription
ivermectin pills: stromectol lotion – minocycline 50mg over the counter
where to get generic clomid price how can i get generic clomid for sale order clomid no prescription
prednisone for sale without a prescription: prednisone 20mg tablets where to buy – how can i get prednisone
can you get clomid without prescription: where to get generic clomid price – where buy generic clomid without rx
https://clomida.pro/# buy generic clomid without dr prescription
https://clomida.pro/# can i get cheap clomid without insurance
order generic clomid: buy cheap clomid price – cheap clomid without prescription
buy 10 mg prednisone prednisone 15 mg daily prednisone buy cheap
https://prednisonea.store/# prednisone for dogs
can you get cheap clomid: cost generic clomid pills – buying generic clomid without insurance
can i get generic clomid pills: can i buy clomid no prescription – get generic clomid without dr prescription
can i get generic clomid without rx how can i get generic clomid online can you buy clomid without prescription
http://azithromycina.pro/# generic zithromax 500mg india
zithromax drug: buy zithromax online cheap – zithromax antibiotic
prednisone tabs 20 mg: apo prednisone – prednisone for sale no prescription
minocycline 50mg online: ivermectin 4 – buy minocycline 100mg tablets
https://prednisonea.store/# can i buy prednisone online without prescription
amoxicillin 500mg capsule buy online amoxicillin 500 mg price amoxacillian without a percription
https://onlinepharmacyworld.shop/# mail order pharmacy no prescription
https://edpill.top/# erectile dysfunction drugs online
http://edpill.top/# erectile dysfunction medicine online
overseas online pharmacy-no prescription: canada online prescription – no prescription canadian pharmacy
canadian drugs no prescription buying prescription drugs in india buy medication online no prescription
synthroid iv
http://onlinepharmacyworld.shop/# cheapest pharmacy for prescriptions
canada prescriptions by mail: online canadian pharmacy no prescription – cheap prescription medication online
http://onlinepharmacyworld.shop/# no prescription needed pharmacy
https://edpill.top/# ed treatments online
online ed pharmacy: ed meds online – cheap erectile dysfunction pills
mexico online pharmacy prescription drugs online pharmacy not requiring prescription canadian pharmacy no prescription needed
http://edpill.top/# cheapest ed medication
http://medicationnoprescription.pro/# non prescription online pharmacy
overseas pharmacy no prescription: canadian pharmacy no prescription – rxpharmacycoupons
http://edpill.top/# where to buy ed pills
buy ed medication cheap ed treatment ed meds cheap
https://onlinepharmacyworld.shop/# non prescription medicine pharmacy
best no prescription pharmacy: buying prescription drugs from canada – online pharmacy no prescription needed
https://edpill.top/# online erectile dysfunction prescription
buy erectile dysfunction pills online ed medicine online ed online treatment
https://edpill.top/# erection pills online
canada online pharmacy no prescription: canadian pharmacy coupon – canadian pharmacy without prescription
online pharmacy no prescriptions: prescription canada – mexico online pharmacy prescription drugs
https://onlinepharmacyworld.shop/# cheapest pharmacy prescription drugs
https://onlinepharmacyworld.shop/# canada drugs coupon code
casino tr?c tuy?n vi?t nam: casino online uy tín – dánh bài tr?c tuy?n
danh bai tr?c tuy?n casino online uy tin casino tr?c tuy?n uy tin
http://casinvietnam.shop/# casino tr?c tuy?n
https://casinvietnam.com/# game c? b?c online uy tin
casino tr?c tuy?n vi?t nam: dánh bài tr?c tuy?n – dánh bài tr?c tuy?n
casino online uy tin casino tr?c tuy?n vi?t nam casino tr?c tuy?n
https://casinvietnam.shop/# game c? b?c online uy tin
https://casinvietnam.com/# casino tr?c tuy?n uy tin
https://casinvietnam.com/# choi casino tr?c tuy?n tren di?n tho?i
http://casinvietnam.com/# choi casino tr?c tuy?n tren di?n tho?i
https://casinvietnam.com/# casino tr?c tuy?n vi?t nam
https://casinvietnam.shop/# casino online uy tin
http://casinvietnam.com/# game c? b?c online uy tin
casino tr?c tuy?n vi?t nam casino online uy tin casino tr?c tuy?n uy tin
http://casinvietnam.com/# casino tr?c tuy?n vi?t nam
casino online uy tin casino tr?c tuy?n uy tin game c? b?c online uy tin
http://casinvietnam.shop/# choi casino tr?c tuy?n tren di?n tho?i
danh bai tr?c tuy?n game c? b?c online uy tin game c? b?c online uy tin
casino tr?c tuy?n uy tin casino online uy tin choi casino tr?c tuy?n tren di?n tho?i
https://casinvietnam.shop/# game c? b?c online uy tin
casino tr?c tuy?n uy tin game c? b?c online uy tin game c? b?c online uy tin
maple leaf pharmacy in canada: Certified Canadian Pharmacies – best rated canadian pharmacy
india pharmacy mail order Generic Medicine India to USA reputable indian online pharmacy
buying prescription drugs in mexico mexico pharmacy medication from mexico pharmacy
my canadian pharmacy canadian pharmacies canadian pharmacy review
zyprexa brand name
top 10 online pharmacy in india indian pharmacy fast delivery top online pharmacy india
best india pharmacy indian pharmacy fast delivery indian pharmacy
world pharmacy india indian pharmacy fast delivery п»їlegitimate online pharmacies india
cheapest online pharmacy india indian pharmacy fast delivery Online medicine home delivery
reputable indian online pharmacy buy medicines from India top 10 online pharmacy in india
canadian pharmacy meds reviews Licensed Canadian Pharmacy canadian pharmacy world
top online pharmacy india: Online medicine home delivery – indian pharmacy online
canada drugs online Licensed Canadian Pharmacy canadian online pharmacy
mexico drug stores pharmacies Mexican Pharmacy Online mexican rx online
top 10 pharmacies in india: Generic Medicine India to USA – india pharmacy
mexico drug stores pharmacies mexico pharmacy п»їbest mexican online pharmacies
buy prescription drugs from canada cheap canada pharmacy world canadian pharmacy mall
mexican mail order pharmacies cheapest mexico drugs reputable mexican pharmacies online
india online pharmacy: indian pharmacy fast delivery – indian pharmacies safe
canadian drug Prescription Drugs from Canada canadian drug pharmacy
canada drugs reviews Licensed Canadian Pharmacy canadian pharmacy 24h com
online canadian pharmacy review Licensed Canadian Pharmacy best canadian online pharmacy reviews
mexico drug stores pharmacies mexican pharmacy reputable mexican pharmacies online
canada pharmacy online reputable canadian online pharmacy safe online pharmacies in canada
п»їlegitimate online pharmacies india indian pharmacy top online pharmacy india
safe canadian pharmacy Certified Canadian Pharmacies canadian pharmacy 365
india online pharmacy: indian pharmacy – Online medicine home delivery
mexican border pharmacies shipping to usa best online pharmacies in mexico mexican pharmaceuticals online
mexican drugstore online mexico pharmacy buying prescription drugs in mexico online
mexico pharmacies prescription drugs Online Pharmacies in Mexico mexican pharmacy
mexican rx online: mexico pharmacy – mexico drug stores pharmacies
mexico drug stores pharmacies Mexican Pharmacy Online buying from online mexican pharmacy
mexican border pharmacies shipping to usa buying prescription drugs in mexico online buying prescription drugs in mexico
mexico drug stores pharmacies Online Pharmacies in Mexico mexican pharmacy
cheapest online pharmacy india indian pharmacy fast delivery indian pharmacy online
pharmacy canadian: Large Selection of Medications from Canada – canadianpharmacyworld com
canadian pharmacy 365 Certified Canadian Pharmacies 77 canadian pharmacy
buying from online mexican pharmacy mexico pharmacy mexican pharmacy
mexico drug stores pharmacies mexico pharmacy purple pharmacy mexico price list
canadian neighbor pharmacy: Certified Canadian Pharmacies – canadian drug pharmacy
online pharmacy india indian pharmacy fast delivery online pharmacy india
best canadian pharmacy to buy from Prescription Drugs from Canada trusted canadian pharmacy
adderall canadian pharmacy canadianpharmacymeds canadianpharmacy com
buy medicines online in india indian pharmacy fast delivery Online medicine home delivery
Online medicine home delivery: indian pharmacy – buy medicines online in india
canadian drug Certified Canadian Pharmacies canada drugs online review
online shopping pharmacy india indian pharmacy Online medicine home delivery
top 10 online pharmacy in india Cheapest online pharmacy indianpharmacy com
mexican rx online Mexican Pharmacy Online mexican border pharmacies shipping to usa
india pharmacy mail order: indian pharmacy fast delivery – cheapest online pharmacy india
world pharmacy india Generic Medicine India to USA online pharmacy india
canadian pharmacy ed medications Large Selection of Medications from Canada online canadian drugstore
http://canadaph24.pro/# canadapharmacyonline com
online pharmacy canada safe canadian pharmacy canadian drugs
https://mexicoph24.life/# mexico drug stores pharmacies
buying prescription drugs in mexico online: buying from online mexican pharmacy – buying from online mexican pharmacy
medication from mexico pharmacy: medicine in mexico pharmacies – mexico pharmacy
buying prescription drugs in mexico: Mexican Pharmacy Online – mexico pharmacy
https://canadaph24.pro/# canadian drugs
canadian pharmacy review Licensed Canadian Pharmacy canadian pharmacy 24h com safe
indian pharmacy paypal http://indiaph24.store/# reputable indian online pharmacy
india online pharmacy
https://canadaph24.pro/# drugs from canada
cheap lisinopril 40 mg prices for lisinopril lisinopril 2mg tablet
cytotec pills buy online: buy misoprostol over the counter – Misoprostol 200 mg buy online
http://lisinopril.network/# lisinopril 40mg prescription cost
tamoxifenworld nolvadex generic lexapro and tamoxifen
http://lisinopril.network/# price of lisinopril generic
cost cheap propecia without prescription: propecia tablets – buying cheap propecia
lexapro and tamoxifen nolvadex pct tamoxifen and uterine thickening
price of lisinopril generic lisinopril 5mg tab buying lisinopril in mexico
purchase cytotec: purchase cytotec – buy cytotec online fast delivery
http://ciprofloxacin.tech/# ciprofloxacin 500mg buy online
https://finasteride.store/# propecia medication
https://lisinopril.network/# can i order lisinopril online
ciprofloxacin mail online п»їcipro generic buy cipro cheap
antibiotics cipro: cipro ciprofloxacin – ciprofloxacin mail online
http://lisinopril.network/# order lisinopril without a prescription
antibiotics cipro buy generic ciprofloxacin buy cipro cheap
tamoxifen hormone therapy where to buy nolvadex tamoxifen for sale
https://lisinopril.network/# lisinopril 2.5 tablet
does tamoxifen cause menopause: tamoxifen benefits – what happens when you stop taking tamoxifen
http://ciprofloxacin.tech/# п»їcipro generic
buy cipro cheap: cipro online no prescription in the usa – buy cipro online
buy ciprofloxacin buy ciprofloxacin buy ciprofloxacin over the counter
http://lisinopril.network/# zestril coupon
zestril 2.5 mg tablets lisinopril tablets uk lisinopril 20 mg 12.5 mg
https://nolvadex.life/# tamoxifen blood clots
https://cytotec.club/# cytotec pills buy online
nolvadex pct: nolvadex d – cost of tamoxifen
http://ciprofloxacin.tech/# ciprofloxacin generic price
ciprofloxacin over the counter: ciprofloxacin over the counter – cipro ciprofloxacin
buy cytotec in usa Misoprostol 200 mg buy online cytotec online
cytotec pills buy online cytotec online cytotec online
https://finasteride.store/# cost cheap propecia
http://cytotec.club/# п»їcytotec pills online
buy cytotec online: buy cytotec in usa – buy cytotec over the counter
tamoxifen and bone density tamoxifen side effects forum how to prevent hair loss while on tamoxifen
tamoxifen estrogen: tamoxifen cyp2d6 – tamoxifen reviews
cost generic propecia without insurance cost of propecia for sale propecia cost
tamoxifen effectiveness nolvadex during cycle how to lose weight on tamoxifen
https://ciprofloxacin.tech/# antibiotics cipro
http://ciprofloxacin.tech/# ciprofloxacin 500 mg tablet price
https://ciprofloxacin.tech/# cipro
cost generic propecia prices: order cheap propecia – buy generic propecia prices
tamoxifen and antidepressants: tamoxifen benefits – tamoxifen buy
tamoxifen moa tamoxifen benefits tamoxifen vs raloxifene
http://nolvadex.life/# nolvadex 20mg
aromatase inhibitors tamoxifen tamoxifen cyp2d6 tamoxifen lawsuit
http://ciprofloxacin.tech/# where can i buy cipro online
https://nolvadex.life/# alternative to tamoxifen
tamoxifen therapy: tamoxifen citrate pct – tamoxifen citrate pct
cipro for sale ciprofloxacin order online ciprofloxacin mail online
buy misoprostol over the counter: cytotec pills online – Cytotec 200mcg price
buy ciprofloxacin over the counter buy cipro online without prescription ciprofloxacin 500mg buy online
https://nolvadex.life/# tamoxifen and depression
http://cytotec.club/# purchase cytotec
buy cytotec in usa cytotec buy online usa cytotec pills buy online
tamoxifen buy: tamoxifen citrate pct – tamoxifen generic
https://finasteride.store/# order propecia without insurance
buy cytotec over the counter: cytotec online – cytotec online
https://nolvadex.life/# tamoxifen adverse effects
ciprofloxacin buy cipro online buy cipro online without prescription
https://cytotec.club/# cytotec pills buy online
https://finasteride.store/# buying propecia for sale
lisinopril price: lisinopril 1 mg tablet – buy 20mg lisinopril
buy generic ciprofloxacin: buy generic ciprofloxacin – where can i buy cipro online
zestoretic coupon lisinopril 104 online pharmacy lisinopril
buy cytotec over the counter Misoprostol 200 mg buy online order cytotec online
http://ciprofloxacin.tech/# where can i buy cipro online
http://ciprofloxacin.tech/# cipro
10 mg lisinopril tablets: lisinopril 20 mg no prescription – how much is 30 lisinopril
buy cytotec in usa Abortion pills online buy cytotec in usa
generic propecia: cost of propecia without insurance – buy cheap propecia
http://cytotec.club/# cytotec online
order cytotec online cytotec online buy misoprostol over the counter
https://lisinopril.network/# lisinopril 40 mg tablet price
https://ciprofloxacin.tech/# where can i buy cipro online
buy cytotec pills online cheap Cytotec 200mcg price cytotec online
http://nolvadex.life/# tamoxifen mechanism of action
buy cytotec pills online cheap: Misoprostol 200 mg buy online – buy cytotec online fast delivery
get propecia without insurance: cost generic propecia for sale – get generic propecia price
cheapest cialis Cialis 20mg price in USA Cialis 20mg price in USA
cheapest cenforce: Cenforce 100mg tablets for sale – cheapest cenforce
https://cenforce.pro/# Buy Cenforce 100mg Online
super kamagra kamagra oral jelly cheap kamagra
http://cenforce.pro/# Buy Cenforce 100mg Online
Generic Tadalafil 20mg price: buy cialis overseas – Cheap Cialis
Kamagra 100mg: kamagra oral jelly – Kamagra 100mg price
Kamagra tablets kamagra Kamagra Oral Jelly
https://kamagra.win/# Kamagra 100mg price
cheapest cialis: buy cialis overseas – Cialis over the counter
Buy Tadalafil 5mg Generic Tadalafil 20mg price Generic Cialis without a doctor prescription
http://kamagra.win/# п»їkamagra
Cheap Viagra 100mg: Buy Viagra online cheap – Sildenafil Citrate Tablets 100mg
http://kamagra.win/# Kamagra 100mg price
https://cialist.pro/# Cialis 20mg price in USA
http://cenforce.pro/# order cenforce
Buy Tadalafil 20mg: Generic Cialis without a doctor prescription – cialis for sale
Cheap Levitra online buy Levitra over the counter Generic Levitra 20mg
Levitra tablet price buy Levitra over the counter Cheap Levitra online
Kamagra 100mg price: kamagra oral jelly – sildenafil oral jelly 100mg kamagra
http://viagras.online/# buy viagra here
https://cialist.pro/# buy cialis pill
Levitra price: Buy Vardenafil 20mg – buy Levitra over the counter
Levitra 20 mg for sale Buy Vardenafil 20mg online Levitra 10 mg buy online
buy kamagra online usa buy kamagra online buy kamagra online usa
https://viagras.online/# Generic Viagra online
Cialis 20mg price in USA: buy cialis online – Generic Cialis without a doctor prescription
Vardenafil online prescription: Levitra generic price – Levitra 10 mg buy online
sildenafil oral jelly 100mg kamagra: kamagra pills – buy Kamagra
sildenafil online Cheap Viagra 100mg buy viagra here
Generic Cialis price: Generic Cialis without a doctor prescription – Buy Tadalafil 20mg
https://cialist.pro/# п»їcialis generic
https://cenforce.pro/# Cenforce 150 mg online
http://cenforce.pro/# cenforce for sale
Generic Tadalafil 20mg price Generic Cialis without a doctor prescription Generic Cialis without a doctor prescription
https://viagras.online/# Cheap generic Viagra online
cialis for sale cialist.pro Buy Tadalafil 20mg
best price for viagra 100mg: Buy generic 100mg Viagra online – Generic Viagra for sale
Generic Tadalafil 20mg price: Generic Cialis without a doctor prescription – Cheap Cialis
http://cenforce.pro/# Buy Cenforce 100mg Online
https://kamagra.win/# buy kamagra online usa
Cialis without a doctor prescription Generic Cialis without a doctor prescription cheapest cialis
https://kamagra.win/# buy kamagra online usa
Levitra 20 mg for sale levitrav.store Buy generic Levitra online
Buy Cenforce 100mg Online: Cenforce 100mg tablets for sale – order cenforce
canadian discount pharmacy drugs from canada reputable canadian pharmacy
mexican border pharmacies shipping to usa: reputable mexican pharmacies online – pharmacies in mexico that ship to usa
https://pharmcanada.shop/# pharmacy canadian
reputable mexican pharmacies online mexico pharmacies prescription drugs reputable mexican pharmacies online
https://pharmindia.online/# india pharmacy mail order
https://pharmmexico.online/# mexican drugstore online
prescription free canadian pharmacy: pharm world store – international pharmacy no prescription
http://pharmmexico.online/# buying from online mexican pharmacy
п»їlegitimate online pharmacies india: reputable indian online pharmacy – india pharmacy mail order
mexico drug stores pharmacies: buying prescription drugs in mexico – buying prescription drugs in mexico online
canadian pharmacy mall canadadrugpharmacy com canadian pharmacies comparison
quality prescription drugs canada: canadian prescription – buying prescription medicine online
buy drugs online without a prescription canadian rx prescription drugstore medications online without prescription
online pharmacy non prescription drugs: pharm world store – online pharmacy no prescription needed
https://pharmmexico.online/# reputable mexican pharmacies online
http://pharmcanada.shop/# canadian compounding pharmacy
onlinepharmaciescanada com: cheap canadian pharmacy online – online canadian pharmacy
canada mail order prescription buy medications online no prescription online pharmacy canada no prescription
onlinecanadianpharmacy 24 reputable canadian online pharmacies pharmacy canadian
cheapest pharmacy prescription drugs: online pharmacy – canadian online pharmacy no prescription
http://pharmworld.store/# overseas pharmacy no prescription
https://pharmmexico.online/# mexican mail order pharmacies
online pharmacy not requiring prescription online pharmacy without a prescription no prescription needed pharmacy
mexican pharmacy: buying prescription drugs in mexico online – medicine in mexico pharmacies
cheapest pharmacy for prescription drugs: pharm world – online pharmacy no prescription needed
buying prescription drugs in mexico online: mexico pharmacies prescription drugs – buying prescription drugs in mexico
canadian prescription prices: mexican prescription drugs online – cheap drugs no prescription
best canadian pharmacy online cross border pharmacy canada canada pharmacy reviews
ordering drugs from canada: buy prescription drugs from canada cheap – safe canadian pharmacy
https://pharmindia.online/# п»їlegitimate online pharmacies india
http://pharmworld.store/# cheapest pharmacy for prescriptions without insurance
canadian pharmacy prescription: medications online without prescription – buying prescription drugs online from canada
cheapest pharmacy prescription drugs pharm world store no prescription required pharmacy
best no prescription online pharmacy online pharmacies no prescription medication online without prescription
india pharmacy: indian pharmacy online – cheapest online pharmacy india
reputable mexican pharmacies online: reputable mexican pharmacies online – pharmacies in mexico that ship to usa
https://pharmworld.store/# canadian prescription pharmacy
http://pharmcanada.shop/# precription drugs from canada
canada prescription: buy medication online without prescription – online pharmacy without prescriptions
online canadian drugstore canadian pharmacy meds reviews online pharmacy canada
pharmacies in mexico that ship to usa: pharmacies in mexico that ship to usa – purple pharmacy mexico price list
no prescription needed pharmacy cheapest pharmacy canadian pharmacies not requiring prescription
canadian pharmacy no scripts: buy drugs from canada – online canadian drugstore
http://pharmcanada.shop/# prescription drugs canada buy online
medication from mexico pharmacy: mexico drug stores pharmacies – mexican border pharmacies shipping to usa
https://pharmcanada.shop/# canadian pharmacy online
pharmacy without prescription: cheapest pharmacy – offshore pharmacy no prescription
https://pharmworld.store/# legit non prescription pharmacies
ordering neurontin online neurontin brand name 800 mg price of neurontin
amoxicillin 875 125 mg tab amoxicillin 500 mg amoxicillin cephalexin
prednisone 20: brand prednisone – prednisone cost us
neurontin cost: buy generic neurontin – price of neurontin
where can i buy prednisone online without a prescription prednisone 10 mg online 1 mg prednisone daily
prednisone 20 mg prices: prednisone 10mg cost – buy prednisone 20mg without a prescription best price
zithromax prescription online: buy cheap zithromax online – zithromax generic cost
https://prednisoned.online/# 60 mg prednisone daily
http://amoxila.pro/# cost of amoxicillin 875 mg
amoxicillin 875 mg tablet: amoxicillin 500mg for sale uk – cost of amoxicillin
SightCare formula aims to maintain 20/20 vision without the need for any surgical process. This supplement is a perfect solution for people facing issues as they grow older. https://sightcare-web.com/
6 prednisone: prednisone tabs 20 mg – order prednisone 10 mg tablet
where can i buy neurontin from canada neurontin brand name in india neurontin pills
generic neurontin 600 mg: neurontin 300 mg cap – gabapentin
zithromax 1000 mg online: cost of generic zithromax – buy cheap zithromax online
zithromax 500mg: zithromax cost – zithromax generic cost
can you buy zithromax over the counter: zithromax cost canada – buy zithromax
amoxicillin cost australia: amoxicillin 500mg over the counter – amoxicillin 500mg price in canada
neurontin brand name 800mg best price: buy generic neurontin – neurontin 200 mg price
cost of prednisone tablets: prednisone buying – prednisone 54
doxycycline tetracycline: where to get doxycycline – doxycycline hyc
where to get doxycycline doxycycline hyc doxycycline 100mg price
https://gabapentinneurontin.pro/# neurontin without prescription
https://doxycyclinea.online/# doxy 200
neurontin oral: neurontin prescription cost – medication neurontin 300 mg
amoxicillin order online: amoxicillin 250 mg price in india – amoxicillin without prescription
cost of neurontin 600 mg neurontin pills neurontin 800 mg capsules
prednisone 50 mg tablet cost prednisone 5 mg prednisone tablets 2.5 mg
https://zithromaxa.store/# zithromax for sale online
https://doxycyclinea.online/# order doxycycline online
cost of amoxicillin 30 capsules: canadian pharmacy amoxicillin – amoxicillin canada price
amoxicillin without prescription: amoxicillin 500mg no prescription – amoxicillin over the counter in canada
prednisone 1 mg for sale how to get prednisone tablets prednisone 100 mg
200 mg doxycycline: buy doxycycline monohydrate – doxycycline hydrochloride 100mg
doxy doxycycline 100mg tablets doxycycline order online
amoxicillin 500 mg cost: where to buy amoxicillin – order amoxicillin uk
zithromax 1000 mg online: zithromax for sale 500 mg – zithromax for sale online
https://doxycyclinea.online/# buy doxycycline monohydrate
https://amoxila.pro/# where to get amoxicillin over the counter
WeJiJ is here to help get you the best gaming setup, gaming PC and guide you through the games you like to play with news, reviews and guides. https://wejij.com/
PCWer is here to help you with all questions in tech. Whether that
Find the latest technology news and expert tech product reviews. Learn about the latest gadgets and consumer tech products for entertainment, gaming, lifestyle and more. https://axget.com/
Easier WWW is a leading technology site that is dedicated to produce great how-to, tips and tricks and cool software review. https://easierwww.com/
medicine neurontin 300 mg: neurontin 100 mg cap – neurontin 100mg price
Testosil is a natural polyherbal testosterone booster designed to help men increase their testosterone levels safely and effectively. https://testosil-web.com/
prednisone pharmacy: where to buy prednisone in canada – 3000mg prednisone
gabapentin 600 mg neurontin pfizer buy neurontin online uk
KeraBiotics is a meticulously-crafted natural formula designed to help people dealing with nail fungus. This solution, inspired by a sacred Amazonian barefoot tribe ritual https://kerabiotics-web.com/
Nagano Lean Body Tonic is a groundbreaking powdered supplement crafted to support your weight loss journey effortlessly. https://naganotonic-try.com/
Sugar Defender is a natural supplement that helps control blood sugar levels, lower the risk of diabetes, improve heart health, and boost energy. https://sugardefender-web.com/
– Shoot MASSIVE Loads For An Amazing Finish! https://semenax-try.com/
how to order doxycycline: doxycycline hyc 100mg – buy doxycycline online uk
Serolean, a revolutionary weight loss supplement, zeroes in on serotonin—the key neurotransmitter governing mood, appetite, and fat storage. https://serolean-web.com/
Tonic Greens is a ready-made greens shake designed to support the entire body and wellness of the mind. It is filled with over 50 individual vitamins https://tonicgreens-try.com/
BalMorex Pro is an exceptional solution for individuals who suffer from chronic joint pain and muscle aches. With its 27-in-1 formula comprised entirely of potent and natural ingredients, it provides unparalleled support for the health of your joints, back, and muscles. https://balmorex-try.com/
Support the health of your ears with 100% natural ingredients, finally being able to enjoy your favorite songs and movies https://quietumplus-try.com/
Peak BioBoost is a revolutionary dietary supplement that leverages the power of nature to support and improve your digestive system. https://peakbioboost-web.com/
buy amoxicillin 500mg buy amoxicillin from canada generic amoxicillin cost
Burn Boost Powder™ is a proven weight loss powder drink that helps to lose weight and boosts the overall metabolism in the body. https://burnboost-web.com
NanoDefense Pro utilizes a potent blend of meticulously chosen components aimed at enhancing the wellness of both your nails and skin. https://nanodefense-web.com/
ONLINE EXCLUSIVE OFFER! Only Available for purchase on the official website. Secure Your Package while stocks last https://prodentim-web.com
http://gabapentinneurontin.pro/# gabapentin 100mg
https://amoxila.pro/# amoxicillin 500 mg cost
buy generic doxycycline doxycycline vibramycin 100mg doxycycline
order doxycycline online: 100mg doxycycline – doxycycline tetracycline
doxycycline online: doxycycline tetracycline – how to buy doxycycline online
amoxicillin from canada can you purchase amoxicillin online amoxicillin pills 500 mg
FlowForce Max is an innovative, natural and effective way to address your prostate problems, while addressing your energy, libido, and vitality. https://flowforcemax-web.com/
neurontin for sale online 800mg neurontin neurontin 300 mg
https://amoxila.pro/# amoxicillin 250 mg price in india
https://zithromaxa.store/# zithromax generic cost
prednisone 2.5 tablet: generic prednisone 10mg – buying prednisone
DuoTrim is an innovative weight loss supplement that utilizes the power of natural plants and nutrients to create CSM bacteria https://duotrim-us.com/
BioFit is a Nutritional Supplement That Uses Probiotics To Help You Lose Weight https://biofit-web.com/
medicine neurontin: buy cheap neurontin online – neurontin 10 mg
Dentitox Pro is a liquid dietary solution created as a serum to support healthy gums and teeth. Dentitox Pro formula is made in the best natural way with unique, powerful botanical ingredients that can support healthy teeth. https://dentitox-us.com/
zithromax 500mg price in india: zithromax z-pak – zithromax capsules
doxycycline generic: doxy 200 – doxy
Sugar Balance is an ultra-potent blood sugar supplement that you can use to help control glucose levels, melt away fat and improve your overall health. https://sugarbalance-us.com/
GlucoFlush is an advanced formula specially designed for pancreas support that will let you promote healthy weight by effectively maintaining the blood sugar level and cleansing and strengthening your gut. https://glucoflush-us.com/
prednisone brand name canada cheap prednisone online buy prednisone from india
Alpha Tonic is a powder-based supplement that uses multiple natural herbs and essential vitamins and minerals to help optimize your body’s natural testosterone levels. https://alphatonic-web.com
Vivo Tonic is a remarkable blood sugar support nutritional supplement that offers a wide range of benefits. https://vivotonic-web.com/
neurontin 100mg discount: neurontin 300 mg buy – buy neurontin canada
where can i buy amoxocillin: price for amoxicillin 875 mg – generic amoxicillin online
Nervogen Pro is an effective dietary supplement designed to help patients with neuropathic pain. When you combine exotic herbs, spices, and other organic substances, your immune system will be strengthened. https://nervogenpro-web.com/
Progenifix is designed to help maximize weight loss results using a mixture of natural, science-backed ingredients. The formula also has secondary benefits, including promoting overall wellness and vitality and assisting your immune system. https://progenifix-web.com/
AquaPeace is an all-natural nutritional formula that uses a proprietary and potent blend of ingredients and nutrients to improve overall ear and hearing health and alleviate the symptoms of tinnitus. https://aquapeace-web.com
FoliPrime is a simple serum containing a blend of vitamins designed to boost hair health. FoliPrime has 100 percent natural substances that enhance and supplement the vitamins in the scalp to promote hair growth. https://foliprime-web.com/
100mg doxycycline doxycycline 100mg price doxycycline online
amoxicillin capsule 500mg price: amoxicillin capsule 500mg price – amoxicillin 500mg without prescription
https://doxycyclinea.online/# generic doxycycline
https://amoxila.pro/# buy amoxicillin without prescription
Gut Vita™ is a daily supplement that helps consumers to improve the balance in their gut microbiome, which supports the health of their immune system. It supports healthy digestion, even for consumers who have maintained an unhealthy diet for a long time. https://gutvita-us.com/
buy prednisone 1 mg mexico: can you buy prednisone without a prescription – order prednisone online canada
Neuro-Thrive is a brain health supplement that claims to promote good memory and thinking skills and better quality sleep. This nootropic supplement achieves its cause with its potent blend of natural compounds and extracts that are proven to be effective in sharpening mental acuity. https://neurothrive-web.com/
The ProNail Complex is a meticulously-crafted natural formula which combines extremely potent oils and skin-supporting vitamins. https://pronailcomplex-web.com/https://pronailcomplex-web.com/
amoxicillin 500mg price canada amoxicillin 500mg prescription amoxicillin 500mg price canada
Erectin is a clinically-proven dietary supplement designed to enhance male https://erectin-web.com/
100% Natural Formula Expressly Designed to Help Control Blood Sugar Levels, Improve Insulin Response And Support Overall Health https://glucotrusttry.com/
PowerBite stands as an innovative dental candy, dedicated to nurturing healthy teeth and gums. Infused with a potent formula, it champions the cause of a robust and radiant smile. Crafted meticulously https://powerbite-web.com/
Protoflow is a prostate health supplement featuring a blend of plant extracts, vitamins, minerals, fruit extracts, and more. https://protoflow-web.com/
Boostaro is a dietary supplement designed specifically for men who suffer from health issues. https://boostaro-try.com/
Unlock the incredible potential of Puravive! Supercharge your metabolism and incinerate calories like never before with our unique fusion of 8 exotic components. Bid farewell to those stubborn pounds and welcome a reinvigorated metabolism and boundless vitality. Grab your bottle today and seize this golden opportunity! https://puravive-web.com/
neurontin 400 mg capsule: neurontin 300mg capsule – neurontin pills
prednisone in mexico prednisone 10mg tabs prednisone 50 mg price
Zoracel is an extraordinary oral care product designed to promote healthy teeth and gums, provide long-lasting fresh breath, support immune health, and care for the ear, nose, and throat. https://zoracel-web.com
Cerebrozen is an excellent liquid ear health supplement purported to relieve tinnitus and improve mental sharpness, among other benefits. The Cerebrozen supplement is made from a combination of natural ingredients, and customers say they have seen results in their hearing, focus, and memory after taking one or two droppers of the liquid solution daily for a week. https://cerebrozen-try.com/
https://zithromaxa.store/# where can i purchase zithromax online
http://zithromaxa.store/# zithromax capsules price
buy neurontin canada: neurontin – neurontin prices
where to purchase doxycycline how to buy doxycycline online doxycycline without a prescription
amoxicillin 250 mg price in india: amoxicillin tablets in india – amoxicillin online purchase
prednisone brand name india: 80 mg prednisone daily – purchase prednisone
The human body can continue to live thanks to the correct functioning of certain systems. If even one of these systems does not work properly, it can cause problems in human life. https://calmlean-web.com/
over the counter amoxicillin: amoxicillin buy online canada – can i buy amoxicillin online
generic doxycycline doxycycline 200 mg doxycycline
http://prednisoned.online/# order prednisone online canada
https://amoxila.pro/# amoxicillin 500mg buy online uk
how to get neurontin: neurontin 900 – neurontin 300 mg price
Zeneara is marketed as an expert-formulated health supplement that can improve hearing and alleviate tinnitus, among other hearing issues. https://zeneara-web.com/
buy amoxicillin canada: where to buy amoxicillin over the counter – amoxicillin price without insurance
GlucoBerry is one of the biggest all-natural dietary and biggest scientific breakthrough formulas ever in the health industry today. This is all because of its amazing high-quality cutting-edge formula that helps treat high blood sugar levels very naturally and effectively. https://glucoberry-web.com/
Pineal XT is a revolutionary supplement that promotes proper pineal gland function and energy levels to support healthy body function. https://pinealxt-web.com/
Introducing TerraCalm, a soothing mask designed specifically for your toenails. Unlike serums and lotions that can be sticky and challenging to include in your daily routine, TerraCalm can be easily washed off after just a minute. https://terracalm-web.com/
buy doxycycline online 270 tabs: doxycycline 150 mg – generic for doxycycline
VidaCalm is an all-natural blend of herbs and plant extracts that treat tinnitus and help you live a peaceful life. https://vidacalm-web.com/
prednisone 1 mg daily prednisone 15 mg tablet where to buy prednisone in australia
Gorilla Flow prostate is an all-natural dietary supplement for men which aims to decrease inflammation in the prostate to decrease common urinary tract issues such as frequent and night-time urination, leakage, or blocked urine stream. https://gorillaflow-web.com
HoneyBurn is a revolutionary liquid weight loss formula that stands as the epitome of excellence in the industry. https://honeyburn-web.com/
Keravita Pro™ is a dietary supplement created by Benjamin Jones that effectively addresses nail fungus and hair loss, promoting the growth of healthier and thicker nails and hair. The formula is designed to target the underlying causes of these health issues and provide comprehensive treatment. https://keravitapro-web.com
generic for amoxicillin: amoxicillin 750 mg price – buy cheap amoxicillin online
buy doxycycline without prescription purchase doxycycline online generic for doxycycline
can i purchase amoxicillin online: amoxicillin 500 mg tablets – buying amoxicillin online
https://zithromaxa.store/# zithromax for sale usa
https://doxycyclinea.online/# doxycycline online
Volca Burn is a weight loss supplement that uses a “red tingle hack” to help you rapidly lose weight without dieting or exercising. https://volcaburn-web.com/
Xitox’s foot pads contain a combination of powerful herbs that help provide a soothing experience for your feet after a long day. https://xitox-web.com/
Hydrossential is actually a skincare serum or you can say a skincare supplement created by Emma Smith to help women keep their skin looking beautiful and flawless. https://hydrossential-web.com/
Carbofix is the revolutionary dietary formula that promises to activate weight loss without all the extra hard work. https://carbofix-try.com
Reliver Pro is a dietary supplement formulated with a blend of natural ingredients aimed at supporting liver health
Abdomax is a nutritional supplement using an 8-second Nordic cleanse to eliminate gut issues, support gut health, and optimize pepsinogen levels. https://abdomax-web.com
buy doxycycline cheap buy doxycycline hyclate 100mg without a rx doxycycline 100mg capsules
neurontin 800 mg cost: price of neurontin – neurontin 200 mg tablets
buy generic neurontin online neurontin 800 mg neurontin price uk
buying prednisone from canada: cost of prednisone 40 mg – buy prednisone 20mg without a prescription best price
http://amoxila.pro/# amoxicillin 250 mg
http://gabapentinneurontin.pro/# neurontin price uk
odering doxycycline: how to order doxycycline – doxylin
zithromax 500 mg: how to buy zithromax online – buy zithromax
can you buy amoxicillin over the counter: amoxicillin 825 mg – medicine amoxicillin 500mg
over the counter amoxicillin: where can i get amoxicillin – amoxicillin 500 mg for sale
sildenafil 100 mg
buy doxycycline monohydrate: doxycycline online – doxycycline 100mg tablets
zithromax pill: zithromax 500 mg lowest price online – buy zithromax 1000 mg online
how to get prednisone tablets prednisone online for sale prednisone 10 mg over the counter
http://doxycyclinea.online/# 200 mg doxycycline
https://prednisoned.online/# buy prednisone no prescription
amoxicillin 500 mg purchase without prescription amoxicillin azithromycin amoxicillin 500mg tablets price in india
canadian online pharmacy prednisone: how much is prednisone 10 mg – prednisone 1 tablet
ProstaBiome is a carefully crafted dietary supplement aimed at promoting prostate health. Bid farewell to restless nights and discomfort with ProstaBiome precise strategy for addressing prostate concerns. https://prostabiome-web.com/
PotentStream is designed to address prostate health by targeting the toxic, hard water minerals that can create a dangerous buildup inside your urinary system It’s the only dropper that contains nine powerful natural ingredients that work in perfect synergy to keep your prostate healthy and mineral-free well into old age. https://potentstream-web.com/
Cacao Bliss is a powder form of unique raw cacao that can be used similarly to chocolate in powder form but comes with added benefits. It is designed to provide a rich and satisfying experience while delivering numerous health benefits. https://cacaobliss-web.com/
neurontin 800mg neurontin cost in canada neurontin 300 mg caps
prednisone generic brand name: prednisone online sale – prednisone 50
https://doxycyclinea.online/# doxycycline 100mg price
http://prednisoned.online/# over the counter prednisone cheap
gabapentin buy canada neurontin 100mg lowest price medicine neurontin 300 mg
amoxicillin 200 mg tablet: where can i get amoxicillin 500 mg – amoxicillin 500 mg purchase without prescription
Cneche provides in-depth journalism and insight into the most impactful news and trends shaping the finance industry. https://cneche.com/
doxycycline online: doxycycline hyclate 100 mg cap – vibramycin 100 mg
zithromax 1000 mg pills can you buy zithromax over the counter zithromax cost australia
price for amoxicillin 875 mg: where can i buy amoxocillin – amoxicillin script
100 mg prednisone daily: buy prednisone online without a prescription – prednisone 10 mg tablet cost
200 mg doxycycline: buy doxycycline online 270 tabs – doxycycline
buy zithromax 500mg online: generic zithromax azithromycin – zithromax prescription in canada
https://doxycyclinea.online/# where can i get doxycycline
http://prednisoned.online/# prednisone 5mg coupon
800mg neurontin neurontin brand name 800 mg neurontin 30 mg
Lasixiv provides news and analysis for IT executives. We cover big data, IT strategy, cloud computing, security, mobile technology, infrastructure, software and more. https://lasixiv.com
zithromax z-pak price without insurance zithromax coupon zithromax 250mg
amoxicillin 500mg pill: amoxicillin for sale – buy amoxicillin 250mg
doxycycline generic: buy doxycycline – generic doxycycline
http://amoxila.pro/# amoxicillin 875 125 mg tab
where to buy amoxicillin pharmacy over the counter amoxicillin canada amoxicillin where to get
purple pharmacy mexico price list buying from online mexican pharmacy mexican pharmaceuticals online
Wedstraunt has the latest news in the restaurant industry, covering topics like consumer trends, technology, marketing and branding, operations, mergers https://wedstraunt.com
mexican mail order pharmacies: mexico drug stores pharmacies – buying prescription drugs in mexico
https://mexicanpharmacy1st.shop/# mexican mail order pharmacies
http://mexicanpharmacy1st.com/# mexican rx online
buying from online mexican pharmacy: best online pharmacies in mexico – buying from online mexican pharmacy
mexican mail order pharmacies mexican drugstore online mexico drug stores pharmacies
https://mexicanpharmacy1st.com/# reputable mexican pharmacies online
pharmacies in mexico that ship to usa: mexican online pharmacies prescription drugs – purple pharmacy mexico price list
Cneche provides in-depth journalism and insight into the most impactful news and trends shaping the finance industry. https://cneche.com/
buying prescription drugs in mexico: medicine in mexico pharmacies – medicine in mexico pharmacies
mexican pharmaceuticals online mexican online pharmacies prescription drugs medicine in mexico pharmacies
Qcmpt provides in-depth journalism and insight into the news and trends impacting the customer experience space. https://qcmpt.com/
Tvphc provides news and analysis for IT executives. We cover big data, IT strategy, cloud computing, security, mobile technology, infrastructure, software and more. https://tvphc.com
https://mexicanpharmacy1st.online/# mexico pharmacy
medication from mexico pharmacy: buying prescription drugs in mexico – buying prescription drugs in mexico online
Huzad delivers the latest news in the grocery industry, with articles covering grocery delivery, online food shopping, shopper behavior, store formats, technology, and more. https://huzad.com/
mexican online pharmacies prescription drugs mexican drugstore online mexican pharmaceuticals online
Grpduk provides news and analysis for human resource executives. We cover topics like recruiting, HR management, employee learning https://grpduk.com
buying from online mexican pharmacy: medicine in mexico pharmacies – mexican online pharmacies prescription drugs
mexico drug stores pharmacies п»їbest mexican online pharmacies mexican mail order pharmacies
mexico pharmacies prescription drugs: mexico pharmacy – mexican online pharmacies prescription drugs
buying prescription drugs in mexico: buying from online mexican pharmacy – buying from online mexican pharmacy
mexican online pharmacies prescription drugs: mexico drug stores pharmacies – pharmacies in mexico that ship to usa
mexican rx online buying prescription drugs in mexico online mexico drug stores pharmacies
Mscherrybomb provides in-depth journalism and insight into the most impactful news and trends shaping the trucking industry. https://mscherrybomb.com/
mexican drugstore online: mexican drugstore online – mexico drug stores pharmacies
purple pharmacy mexico price list: mexico pharmacy – medication from mexico pharmacy
https://mexicanpharmacy1st.online/# mexican border pharmacies shipping to usa
https://mexicanpharmacy1st.shop/# mexican online pharmacies prescription drugs
mexico pharmacies prescription drugs: medicine in mexico pharmacies – medicine in mexico pharmacies
medicine in mexico pharmacies buying from online mexican pharmacy mexico drug stores pharmacies
http://mexicanpharmacy1st.com/# mexican mail order pharmacies
Janmckinley provides news and analysis for waste and recycling executives. We cover topics like landfills, collections, regulation, waste-to-energy, corporate news, fleet management, and more. https://janmckinley.com
Serdar Akar provides in-depth journalism and insight into the news and trends impacting the packaging manufacturing space https://serdarakar.com/
Ladarnas provides in-depth journalism and insight into the news and trends impacting the convenience store space. https://ladarnas.com
п»їbest mexican online pharmacies pharmacies in mexico that ship to usa medicine in mexico pharmacies
mexican mail order pharmacies: medication from mexico pharmacy – mexican mail order pharmacies
http://mexicanpharmacy1st.com/# reputable mexican pharmacies online
https://mexicanpharmacy1st.com/# mexican drugstore online
Sugar Defender is the rated blood sugar formula with an advanced blend of 24 proven ingredients that support healthy glucose levels and natural weight loss. https://omiyabigan.com/
Sugar Defender is the rated blood sugar formula with an advanced blend of 24 proven ingredients that support healthy glucose levels and natural weight loss. https://mimsbrook.com
medication from mexico pharmacy: medication from mexico pharmacy – medicine in mexico pharmacies
purple pharmacy mexico price list mexican online pharmacies prescription drugs medicine in mexico pharmacies
buying prescription drugs in mexico online reputable mexican pharmacies online medicine in mexico pharmacies
buying prescription drugs in mexico online: mexican mail order pharmacies – mexico drug stores pharmacies
mexican border pharmacies shipping to usa: mexico drug stores pharmacies – best mexican online pharmacies
http://mexicanpharmacy1st.com/# mexican pharmacy
http://mexicanpharmacy1st.com/# mexico pharmacy
mexican pharmacy: mexican drugstore online – mexico pharmacies prescription drugs
buying prescription drugs in mexico online buying prescription drugs in mexico online mexican online pharmacies prescription drugs
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://blackboxvending.com/
buying prescription drugs in mexico: mexican drugstore online – reputable mexican pharmacies online
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://mineryuta.com
mexico drug stores pharmacies: reputable mexican pharmacies online – buying prescription drugs in mexico
mexican online pharmacies prescription drugs mexico drug stores pharmacies mexican pharmaceuticals online
http://mexicanpharmacy1st.com/# buying prescription drugs in mexico online
https://mexicanpharmacy1st.com/# purple pharmacy mexico price list
https://mexicanpharmacy1st.shop/# pharmacies in mexico that ship to usa
mexico drug stores pharmacies: medicine in mexico pharmacies – reputable mexican pharmacies online
п»їbest mexican online pharmacies medicine in mexico pharmacies mexican mail order pharmacies
medication from mexico pharmacy: medication from mexico pharmacy – best online pharmacies in mexico
https://mexicanpharmacy1st.shop/# mexico drug stores pharmacies
purple pharmacy mexico price list: best online pharmacies in mexico – reputable mexican pharmacies online
mexican rx online mexican rx online mexico drug stores pharmacies
https://mexicanpharmacy1st.shop/# mexican online pharmacies prescription drugs
Sugar Defender is the rated blood sugar formula with an advanced blend of 24 proven ingredients that support healthy glucose levels and natural weight loss. https://ibcbellows.com/
https://mexicanpharmacy1st.online/# mexican rx online
mexican pharmacy: mexican online pharmacies prescription drugs – mexico pharmacies prescription drugs
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://acmesignz.com/
Manufactured in the United States with FDA approval, this product was crafted using only the highest quality ingredients and produced under hygienic conditions in a GMP-certified facility. https://mystylefiles.com/
sugar defender: https://novabeaute.com/
sugar defender: https://abmdds.com/
mexican online pharmacies prescription drugs medicine in mexico pharmacies purple pharmacy mexico price list
Transgender is an umbrella Live Chat On Website used to describe people whose gender identity
mexican border pharmacies shipping to usa: medication from mexico pharmacy – purple pharmacy mexico price list
https://mexicanpharmacy1st.com/# mexico drug stores pharmacies
medicine in mexico pharmacies pharmacies in mexico that ship to usa mexican online pharmacies prescription drugs
https://mexicanpharmacy1st.com/# medication from mexico pharmacy
mexico pharmacy: best online pharmacies in mexico – purple pharmacy mexico price list
sugar defender: https://peyfon.com/
sugar defender: https://nilayoram.com/
mexico pharmacy mexican drugstore online п»їbest mexican online pharmacies
sugar defender: https://seahorsesoap.com/
sugar defender: https://kandicandles.com/
get generic propecia prices order generic propecia for sale order generic propecia for sale
sugar defender: https://sourceprousa.com/
http://propeciaf.online/# get propecia pills
where to buy lisinopril: zestril tablet price – lisinopril prescription cost
https://propeciaf.online/# cost of propecia online
https://clomiphene.shop/# can you get generic clomid without insurance
buy cheap lisinopril 40mg: lisinopril brand – zestril tablet
get generic clomid tablets: where to buy cheap clomid without dr prescription – where can i get generic clomid without rx
how can i get generic clomid without prescription how can i get cheap clomid without insurance how can i get generic clomid without prescription
http://gabapentin.club/# neurontin singapore
Cytotec 200mcg price buy cytotec buy cytotec over the counter
neurontin 300 mg buy: canada neurontin 100mg lowest price – neurontin discount
lisinopril 5 mg uk price: lisinopril 20 mg uk – lisinopril 5 mg tablet cost
zestril 20 mg cost how much is lisinopril zestoretic online
sugar defender: https://lindadicesare.com/
sugar defender: https://luckysloader.com/
Cytotec 200mcg price buy cytotec п»їcytotec pills online
sugar defender: https://drdenisemichele.com/
buy propecia without dr prescription buy propecia without dr prescription cost of cheap propecia now
purchase cytotec: buy cytotec online fast delivery – cytotec abortion pill
https://propeciaf.online/# buy cheap propecia prices
cytotec online: Abortion pills online – buy cytotec
http://cytotec.xyz/# Abortion pills online
http://clomiphene.shop/# where to buy clomid no prescription
where can i buy neurontin online neurontin 400 neurontin capsules 100mg
https://lisinopril.club/# prescription drug lisinopril
cytotec online: buy cytotec over the counter – buy misoprostol over the counter
how can i get clomid without a prescription: how to buy cheap clomid – how to get cheap clomid price
propecia generic buying cheap propecia online cost of generic propecia without dr prescription
https://propeciaf.online/# cost of cheap propecia tablets
can i order generic clomid pills: can i get generic clomid prices – can i purchase cheap clomid
neurontin price australia neurontin 600 mg cost neurontin tablets no script
http://propeciaf.online/# cost propecia without a prescription
prinivil 2.5 mg: zestril brand name – lisinopril 30 mg cost
gabapentin 600 mg: neurontin 100 mg cost – neurontin tablets 300mg
zestoretic 10 12.5 prescription medicine lisinopril lisinopril 3
http://lisinopril.club/# buy lisinopril no prescription
buy cheap propecia without a prescription buying generic propecia without dr prescription order cheap propecia without a prescription
http://cytotec.xyz/# Misoprostol 200 mg buy online
https://lisinopril.club/# lisinopril 3973
lisinopril prescription coupon: lisinopril 20mg discount – lisinopril 5 mg tablet price in india
cost propecia prices cost cheap propecia without dr prescription order generic propecia no prescription
zestril tab 10mg: 50 mg lisinopril – lisinopril 40 mg purchase
neurontin brand name 800 mg: generic neurontin pill – neurontin 400 mg cost
http://gabapentin.club/# neurontin 3
lisinopril 20 mg 12.5 mg lisinopril 20 mg 12.5 mg zestril 5 mg tablet
http://lisinopril.club/# 100 mg lisinopril
http://gabapentin.club/# buy neurontin 100 mg canada
order cytotec online cytotec buy online usa buy cytotec pills online cheap
neurontin rx: neurontin capsules – neurontin price comparison
generic propecia pill: cost generic propecia without rx – order generic propecia without insurance
medication zestoretic lisinopril without an rx buy lisinopril uk
cost of brand name neurontin buy neurontin 100 mg gabapentin medication
generic clomid without rx: how to buy cheap clomid prices – can you buy clomid prices
buy misoprostol over the counter: order cytotec online – п»їcytotec pills online
where to buy cheap clomid: how can i get clomid tablets – clomid brand name
https://gabapentin.club/# neurontin prices
lisinopril 20mg zestril online cheapest lisinopril 10 mg
generic zestoretic lisinopril 40 mg tablet price lisinopril 10mg tablets price
neurontin price in india: prescription medication neurontin – neurontin tablets no script
neurontin 200 mg: cost of neurontin 100mg – buy gabapentin
https://cheapestandfast.com/# no prescription pharmacy
https://36and6health.shop/# best online pharmacy no prescription
the canadian pharmacy canadian pharmacy com canadian pharmacy reviews
http://36and6health.com/# cheapest pharmacy for prescriptions without insurance
https://cheapestandfast.com/# online pharmacies no prescription usa
cheapest pharmacy canada canadianpharmacyworld com canadian 24 hour pharmacy
online canadian pharmacy: cheapest canada – canadian king pharmacy
https://cheapestindia.shop/# Online medicine order
https://cheapestmexico.shop/# buying prescription drugs in mexico online
http://36and6health.com/# buying prescription drugs from canada
canadian pharmacy world reviews: canadian pharmacy sarasota – best canadian pharmacy online
https://cheapestindia.shop/# top 10 pharmacies in india
http://36and6health.com/# reputable online pharmacy no prescription
canadian pharmacy service canadianpharmacymeds com canadian drug
http://cheapestindia.com/# india online pharmacy
reputable canadian pharmacy cheapest canada my canadian pharmacy
http://cheapestandfast.com/# canada mail order prescription
http://36and6health.com/# no prescription needed canadian pharmacy
canada pharmacy online: reputable canadian online pharmacy – best rated canadian pharmacy
http://cheapestmexico.com/# medicine in mexico pharmacies
http://cheapestindia.com/# reputable indian pharmacies
http://cheapestandfast.com/# canada mail order prescriptions
https://36and6health.com/# canadian prescription pharmacy
medicine with no prescription: cheapest & fast pharmacy – online pharmacy without prescriptions
https://cheapestindia.com/# indianpharmacy com
mexican pharmaceuticals online mexican rx online purple pharmacy mexico price list
https://cheapestindia.shop/# best online pharmacy india
canadian pharmacy no prescription 36 and 6 pharmacy online pharmacy no prescription needed
https://cheapestmexico.shop/# buying prescription drugs in mexico
https://cheapestcanada.com/# online canadian drugstore
http://36and6health.com/# online pharmacy non prescription drugs
https://cheapestcanada.com/# canadian pharmacy com
reliable canadian pharmacy: best canadian online pharmacy reviews – canadian online pharmacy
https://cheapestcanada.shop/# canadianpharmacyworld com
http://cheapestandfast.com/# buy medications online no prescription
Pharmacie Internationale en ligne: vente de mГ©dicament en ligne – pharmacie en ligne sans ordonnance
farmacia online senza ricetta: farmacia online – acquistare farmaci senza ricetta
Farmacia online più conveniente: acquisto farmaci con ricetta – top farmacia online
trouver un mГ©dicament en pharmacie pharmacie en ligne sans ordonnance pharmacie en ligne sans ordonnance
pharmacie en ligne france pas cher: pharmacie en ligne livraison europe – Pharmacie en ligne livraison Europe
pharmacie en ligne france livraison internationale Achat mГ©dicament en ligne fiable Pharmacie Internationale en ligne
https://euapothekeohnerezept.shop/# gГјnstigste online apotheke
migliori farmacie online 2024: comprare farmaci online con ricetta – top farmacia online
https://euapothekeohnerezept.com/# eu apotheke ohne rezept
farmacia online: migliori farmacie online 2024 – farmacia online senza ricetta
ohne rezept apotheke: internet apotheke – internet apotheke
farmacias online baratas: farmacias online seguras Рfarmacias online seguras en espa̱a
online apotheke versandkostenfrei online apotheke online apotheke rezept
acquistare farmaci senza ricetta acquistare farmaci senza ricetta migliori farmacie online 2024
farmacia online envГo gratis: farmacia online envГo gratis – farmacia en casa online descuento
acquisto farmaci con ricetta: acquisto farmaci con ricetta – farmacie online sicure
farmacia barata: farmacias online seguras – farmacia online 24 horas
shop apotheke gutschein: europa apotheke – günstigste online apotheke
comprare farmaci online all’estero: п»їFarmacia online migliore – comprare farmaci online all’estero
internet apotheke: günstigste online apotheke – online apotheke deutschland
comprare farmaci online con ricetta farmacia online senza ricetta Farmacie online sicure
pharmacie en ligne france pas cher trouver un mГ©dicament en pharmacie pharmacie en ligne avec ordonnance
farmacias direct: farmacia online barata y fiable – farmacia barata
http://eufarmaciaonline.com/# farmacia online espaГ±a envГo internacional
farmacia online 24 horas: farmacias online seguras en espaГ±a – farmacia online 24 horas
http://eufarmacieonline.com/# Farmacia online miglior prezzo
farmacias online seguras en espaГ±a: farmacias online seguras – farmacia online barcelona
farmacie online autorizzate elenco: Farmacie on line spedizione gratuita – comprare farmaci online all’estero
farmacia online 24 horas farmacia online barcelona farmacia online envГo gratis
pharmacie en ligne sans ordonnance pharmacie en ligne france livraison belgique Pharmacie Internationale en ligne
online apotheke: online apotheke rezept – online apotheke versandkostenfrei
farmacias online seguras: farmacia online envГo gratis – farmacia online barata
comprare farmaci online all’estero: migliori farmacie online 2024 – Farmacie on line spedizione gratuita
top farmacia online: farmacie online sicure – farmacia online più conveniente
Farmacie on line spedizione gratuita farmacia online farmacia online
medikamente rezeptfrei online apotheke rezept п»їshop apotheke gutschein
farmacia barata: farmacia online envГo gratis – farmacias online seguras en espaГ±a
pharmacie en ligne france pas cher: Pharmacie Internationale en ligne – pharmacie en ligne livraison europe
vardenafil prices
comprare farmaci online all’estero: migliori farmacie online 2024 – Farmacie online sicure
pharmacie en ligne pas cher: pharmacie en ligne france livraison belgique – pharmacie en ligne france livraison internationale
farmacia online barata y fiable: farmacia online envÃo gratis – farmacia online madrid
farmacia online barata y fiable: farmacia online barata – farmacia online madrid
pharmacie en ligne france livraison belgique: pharmacie en ligne pas cher – pharmacie en ligne avec ordonnance
internet apotheke online apotheke versandkostenfrei online apotheke gГјnstig
http://eumedicamentenligne.com/# pharmacie en ligne livraison europe
medikamente rezeptfrei: ohne rezept apotheke – п»їshop apotheke gutschein
https://eufarmaciaonline.com/# farmacia en casa online descuento
ohne rezept apotheke: internet apotheke – online apotheke deutschland
farmaci senza ricetta elenco: farmacie online sicure – Farmacie online sicure
farmacias online seguras: farmacias direct Рfarmacias online seguras en espa̱a
farmacias direct: farmacias online seguras – farmacias online seguras
Farmacia online miglior prezzo comprare farmaci online con ricetta farmacie online sicure
online apotheke internet apotheke п»їshop apotheke gutschein
farmacia en casa online descuento: farmacia online envГo gratis – farmacia online espaГ±a envГo internacional
medikament ohne rezept notfall: online apotheke preisvergleich – europa apotheke
online apotheke gГјnstig: online apotheke – online apotheke rezept
farmacia online madrid: п»їfarmacia online espaГ±a – farmacias online seguras en espaГ±a
pharmacie en ligne pas cher: trouver un m̩dicament en pharmacie Рpharmacie en ligne fiable
Pharmacie Internationale en ligne pharmacies en ligne certifiГ©es pharmacie en ligne france fiable
ohne rezept apotheke internet apotheke beste online-apotheke ohne rezept
Farmacie on line spedizione gratuita: comprare farmaci online con ricetta – farmacia online senza ricetta
pharmacie en ligne sans ordonnance: pharmacie en ligne sans ordonnance – pharmacie en ligne france livraison internationale
acheter m̩dicament en ligne sans ordonnance: pharmacie en ligne france livraison belgique Рpharmacie en ligne france livraison belgique
https://eufarmacieonline.shop/# Farmacie online sicure
medikamente rezeptfrei: gГјnstige online apotheke – internet apotheke
ohne rezept apotheke: beste online-apotheke ohne rezept – günstige online apotheke
Pharmacie sans ordonnance: pharmacie en ligne – pharmacie en ligne avec ordonnance
http://eumedicamentenligne.com/# pharmacie en ligne pas cher
farmacia online barcelona п»їfarmacia online espaГ±a farmacia online madrid
farmacia online: farmacie online autorizzate elenco – Farmacia online piГ№ conveniente
farmacia online barcelona: farmacias online seguras en espaГ±a – farmacia online madrid
online apotheke: eu apotheke ohne rezept – günstige online apotheke
günstige online apotheke: günstigste online apotheke – internet apotheke
п»їshop apotheke gutschein: medikamente rezeptfrei – online apotheke rezept
Quand une femme prend du Viagra homme: Viagra homme prix en pharmacie sans ordonnance – Prix du Viagra 100mg en France
pharmacie en ligne france fiable: levitra en ligne – Pharmacie en ligne livraison Europe
pharmacies en ligne certifiГ©es: acheter kamagra site fiable – pharmacie en ligne
pharmacie en ligne france fiable: cialis prix – vente de mГ©dicament en ligne
vente de mГ©dicament en ligne: pharmacie en ligne – Pharmacie en ligne livraison Europe
trouver un mГ©dicament en pharmacie: levitra generique sites surs – trouver un mГ©dicament en pharmacie
pharmacie en ligne sans ordonnance Acheter Cialis pharmacie en ligne france livraison internationale
pharmacie en ligne avec ordonnance acheter kamagra site fiable trouver un mГ©dicament en pharmacie
acheter mГ©dicament en ligne sans ordonnance: Levitra pharmacie en ligne – acheter mГ©dicament en ligne sans ordonnance
https://levitraenligne.shop/# pharmacie en ligne sans ordonnance
pharmacie en ligne: Acheter Cialis – pharmacie en ligne france pas cher
Pharmacie Internationale en ligne: pharmacie en ligne avec ordonnance – pharmacie en ligne livraison europe
pharmacie en ligne pas cher: pharmacie en ligne avec ordonnance – п»їpharmacie en ligne france
Pharmacie Internationale en ligne: pharmacie en ligne pas cher – pharmacies en ligne certifiГ©es
Viagra gГ©nГ©rique pas cher livraison rapide: Viagra homme prix en pharmacie sans ordonnance – Viagra gГ©nГ©rique sans ordonnance en pharmacie
https://cenligne.com/# trouver un médicament en pharmacie
pharmacie en ligne pas cher: pharmacie en ligne sans ordonnance – п»їpharmacie en ligne france
pharmacie en ligne france fiable: achat kamagra – pharmacie en ligne sans ordonnance
Pharmacie en ligne livraison Europe: Levitra pharmacie en ligne – acheter mГ©dicament en ligne sans ordonnance
Achat mГ©dicament en ligne fiable: Levitra 20mg prix en pharmacie – acheter mГ©dicament en ligne sans ordonnance
Hello!
This post was created with XRumer 23 StrongAI.
Good luck 🙂
Hello.
This post was created with XRumer 23 StrongAI.
Good luck 🙂
pharmacie en ligne livraison europe: pharmacies en ligne certifiГ©es – Pharmacie Internationale en ligne
pharmacies en ligne certifiГ©es: acheter kamagra site fiable – Pharmacie sans ordonnance
pharmacie en ligne france pas cher: Acheter Cialis – Achat mГ©dicament en ligne fiable
acheter mГ©dicament en ligne sans ordonnance: pharmacie en ligne – pharmacie en ligne avec ordonnance
pharmacies en ligne certifiГ©es: pharmacie en ligne – pharmacie en ligne fiable
pharmacie en ligne france pas cher: vente de mГ©dicament en ligne – pharmacie en ligne livraison europe
Prix du Viagra en pharmacie en France: viagra en ligne – Sildenafil teva 100 mg sans ordonnance
Pharmacie en ligne livraison Europe: Cialis sans ordonnance 24h – pharmacie en ligne sans ordonnance
pharmacie en ligne livraison europe: kamagra pas cher – Achat mГ©dicament en ligne fiable
Pharmacie sans ordonnance: kamagra oral jelly – Achat mГ©dicament en ligne fiable
pharmacie en ligne pas cher: Medicaments en ligne livres en 24h – Pharmacie Internationale en ligne
Pharmacie Internationale en ligne: kamagra pas cher – pharmacie en ligne france livraison internationale
pharmacie en ligne pas cher: Acheter Cialis 20 mg pas cher – Pharmacie Internationale en ligne
pharmacie en ligne fiable: kamagra pas cher – pharmacies en ligne certifiГ©es
https://viaenligne.shop/# Viagra sans ordonnance pharmacie France
pharmacie en ligne sans ordonnance: levitra en ligne – Achat mГ©dicament en ligne fiable
pharmacies en ligne certifiГ©es: Levitra 20mg prix en pharmacie – pharmacie en ligne france pas cher
https://levitraenligne.com/# pharmacies en ligne certifiées
pharmacie en ligne france pas cher: Medicaments en ligne livres en 24h – pharmacie en ligne sans ordonnance
pharmacie en ligne: levitra en ligne – pharmacie en ligne avec ordonnance
pharmacie en ligne france livraison internationale: pharmacie en ligne fiable – trouver un mГ©dicament en pharmacie
pharmacie en ligne pas cher: pharmacie en ligne pas cher – pharmacie en ligne avec ordonnance
Le gГ©nГ©rique de Viagra: Viagra en france livraison rapide – Quand une femme prend du Viagra homme
Viagra homme prix en pharmacie: viagra sans ordonnance – SildГ©nafil 100 mg prix en pharmacie en France
pharmacie en ligne france livraison internationale: Levitra 20mg prix en pharmacie – Pharmacie en ligne livraison Europe
acheter mГ©dicament en ligne sans ordonnance: pharmacie en ligne france fiable – acheter mГ©dicament en ligne sans ordonnance
pharmacie en ligne france pas cher: vente de mГ©dicament en ligne – acheter mГ©dicament en ligne sans ordonnance
Pharmacie sans ordonnance: Levitra pharmacie en ligne – pharmacie en ligne pas cher
pharmacie en ligne france fiable: kamagra pas cher – Achat mГ©dicament en ligne fiable
vente de mГ©dicament en ligne: pharmacie en ligne – trouver un mГ©dicament en pharmacie
vente de mГ©dicament en ligne: kamagra gel – pharmacies en ligne certifiГ©es
pharmacie en ligne avec ordonnance: kamagra oral jelly – pharmacie en ligne france livraison belgique
pharmacie en ligne sans ordonnance: cialis sans ordonnance – acheter mГ©dicament en ligne sans ordonnance
vente de mГ©dicament en ligne: levitra en ligne – pharmacie en ligne livraison europe
acheter mГ©dicament en ligne sans ordonnance: cialis generique – acheter mГ©dicament en ligne sans ordonnance
pharmacie en ligne pas cher: Levitra pharmacie en ligne – pharmacie en ligne france livraison internationale
Pharmacie Internationale en ligne: Acheter Cialis 20 mg pas cher – п»їpharmacie en ligne france
pharmacie en ligne avec ordonnance: cialis generique – Pharmacie sans ordonnance
pharmacie en ligne pas cher: Levitra pharmacie en ligne – pharmacie en ligne france livraison internationale
trouver un mГ©dicament en pharmacie: Levitra 20mg prix en pharmacie – Achat mГ©dicament en ligne fiable
Viagra pas cher livraison rapide france: Viagra sans ordonnance 24h – Viagra homme sans ordonnance belgique
pharmacie en ligne pas cher: pharmacie en ligne sans ordonnance – Pharmacie sans ordonnance
Pharmacie Internationale en ligne: pharmacie en ligne livraison europe – pharmacies en ligne certifiГ©es
acheter mГ©dicament en ligne sans ordonnance: Levitra acheter – pharmacie en ligne france fiable
vente de mГ©dicament en ligne: pharmacie en ligne france fiable – Pharmacie en ligne livraison Europe
pharmacie en ligne france pas cher: pharmacies en ligne certifiГ©es – Pharmacie en ligne livraison Europe
pharmacie en ligne france livraison internationale: levitra generique – acheter mГ©dicament en ligne sans ordonnance
п»їpharmacie en ligne france: Acheter Cialis 20 mg pas cher – п»їpharmacie en ligne france
pharmacie en ligne france pas cher: п»їpharmacie en ligne france – pharmacie en ligne france livraison belgique
Pharmacie sans ordonnance: pharmacie en ligne – Pharmacie en ligne livraison Europe
Achat mГ©dicament en ligne fiable: levitra en ligne – pharmacie en ligne avec ordonnance
pharmacie en ligne france livraison belgique: pharmacie en ligne france fiable – Achat mГ©dicament en ligne fiable
pharmacies en ligne certifiГ©es: Pharmacies en ligne certifiees – pharmacie en ligne fiable
pharmacie en ligne: pharmacie en ligne livraison europe – pharmacie en ligne avec ordonnance
Achat mГ©dicament en ligne fiable: pharmacie en ligne fiable – pharmacies en ligne certifiГ©es
pharmacie en ligne france pas cher: levitra generique prix en pharmacie – Pharmacie en ligne livraison Europe
п»їpharmacie en ligne france: kamagra en ligne – pharmacie en ligne sans ordonnance
Achat mГ©dicament en ligne fiable: Levitra sans ordonnance 24h – Pharmacie en ligne livraison Europe
Pharmacie sans ordonnance: cialis prix – pharmacies en ligne certifiГ©es
pharmacies en ligne certifiГ©es: acheter kamagra site fiable – pharmacie en ligne france livraison belgique
pharmacie en ligne france livraison belgique: kamagra pas cher – п»їpharmacie en ligne france
Viagra homme sans prescription: Viagra sans ordonnance 24h – Viagra Pfizer sans ordonnance
pharmacie en ligne livraison europe: Pharmacie Internationale en ligne – pharmacie en ligne
Achat mГ©dicament en ligne fiable: kamagra pas cher – pharmacie en ligne avec ordonnance
Prix du Viagra 100mg en France: Meilleur Viagra sans ordonnance 24h – Viagra pas cher livraison rapide france
pharmacie en ligne france fiable: kamagra pas cher – Achat mГ©dicament en ligne fiable
Viagra gГ©nГ©rique pas cher livraison rapide: viagra en ligne – Viagra vente libre pays
pharmacie en ligne france pas cher: pharmacie en ligne france fiable – pharmacie en ligne pas cher
pharmacie en ligne livraison europe: cialis sans ordonnance – trouver un mГ©dicament en pharmacie
pharmacie en ligne france livraison internationale: levitra generique – pharmacie en ligne sans ordonnance
pharmacie en ligne france pas cher: Pharmacie Internationale en ligne – vente de mГ©dicament en ligne
Pharmacie en ligne livraison Europe: levitra generique – pharmacie en ligne livraison europe
acheter mГ©dicament en ligne sans ordonnance: Pharmacies en ligne certifiees – Pharmacie sans ordonnance
pharmacies en ligne certifiГ©es: pharmacie en ligne france livraison belgique – Pharmacie Internationale en ligne
Pharmacie sans ordonnance: Medicaments en ligne livres en 24h – pharmacie en ligne france pas cher
pharmacie en ligne france livraison belgique: levitra generique sites surs – vente de mГ©dicament en ligne
Acheter viagra en ligne livraison 24h: Meilleur Viagra sans ordonnance 24h – Prix du Viagra en pharmacie en France
pharmacie en ligne france livraison belgique: acheter kamagra site fiable – pharmacie en ligne pas cher
https://viaenligne.shop/# Viagra sans ordonnance livraison 24h
pharmacie en ligne france livraison belgique: cialis sans ordonnance – pharmacies en ligne certifiГ©es
Viagra vente libre pays: viagra en ligne – Viagra pas cher paris
Viagra homme prix en pharmacie sans ordonnance: viagra sans ordonnance – SildГ©nafil 100 mg prix en pharmacie en France
pharmacie en ligne france livraison belgique: Acheter Cialis – pharmacie en ligne france fiable
Pharmacie Internationale en ligne: kamagra en ligne – vente de mГ©dicament en ligne
п»їpharmacie en ligne france: kamagra en ligne – pharmacie en ligne
pharmacie en ligne france fiable: cialis prix – pharmacie en ligne fiable
pharmacie en ligne pas cher: vente de mГ©dicament en ligne – acheter mГ©dicament en ligne sans ordonnance
Viagra Pfizer sans ordonnance: SildГ©nafil Teva 100 mg acheter – Viagra Pfizer sans ordonnance
Achat mГ©dicament en ligne fiable: cialis prix – pharmacie en ligne france pas cher
pharmacie en ligne sans ordonnance: pharmacie en ligne – п»їpharmacie en ligne france
Pharmacie sans ordonnance: pharmacie en ligne sans ordonnance – pharmacie en ligne livraison europe
acheter mГ©dicament en ligne sans ordonnance: cialis sans ordonnance – vente de mГ©dicament en ligne
vente de mГ©dicament en ligne: cialis generique – pharmacie en ligne france fiable
pharmacie en ligne france fiable: Levitra 20mg prix en pharmacie – pharmacie en ligne pas cher
amoxicillin 500 mg for sale: cheapest amoxicillin – amoxicillin 500 mg cost
amoxicillin 250 mg
https://azithromycinca.com/# doxycycline buy
doxycycline 100 mg tablet
https://autolux-azerbaijan.com/# Pin up 306 casino
pin-up 141 casino: pin-up360 – Pin-Up Casino
https://autolux-azerbaijan.com/# pin-up 141 casino
Pin Up Kazino ?Onlayn: Pin up 306 casino – Pin-Up Casino
Pin Up: Pin Up – pin-up 141 casino
https://autolux-azerbaijan.com/# pin-up 141 casino
Pin-Up Casino: pin-up 141 casino – Pin Up Azerbaycan
Pin Up Azerbaycan: Pin Up – Pin up 306 casino
https://autolux-azerbaijan.com/# ?Onlayn Kazino
pin-up360: Pin-up Giris – ?Onlayn Kazino
https://autolux-azerbaijan.com/# Pin Up Kazino ?Onlayn
https://autolux-azerbaijan.com/# pin-up360
Pin-up Giris: ?Onlayn Kazino – Pin Up Kazino ?Onlayn
https://autolux-azerbaijan.com/# ?Onlayn Kazino
pin-up kazino: Pin up 306 casino – pin-up360
Pin up 306 casino: Pin-Up Casino – Pin Up
https://autolux-azerbaijan.com/# Pin Up Kazino ?Onlayn
pin-up kazino: Pin-up Giris – Pin Up Kazino ?Onlayn