CASE REPORT
Year: 2018 I Volume: 1 I Issue: 1 I Page: 30-31
A case of Phakomatosis Pigmentovascularis type IIb with seizures
Rohit Gupta1, Ashok R Wadhwani1, Kishor Singh1, Sanjay K Kanodia1
1Department of Dermatology, NIMS Medical College, Jaipur.
Corresponding Author:
Dr Rohit Gupta
Department of Dermatology,
NIMS Medical College, Jaipur-Delhi Highway,
Jaipur (Rajasthan) 303121
Email-id: roh.gupta51@gmail.com
How to cite this article:
Gupta R, Wadhwani AR, Singh K, Kanodia SK. A case of Phakomatosis Pigmentovascularis type IIb with seizures. JDA Indian Journal of Clinical Dermatology. 2018;1:30-31.
Abstract:
Phakomatosis pigmentovascularis (PPV) is a genetic disorder characterized by association of capillary malformation with pigmentary nevi. We hereby report a rare presentation of PPV with Sturge-weber syndrome (SWS), Klippel-trenaunay syndrome (KTS) and Nevus of Ota (PPV typeIIb) in a 7 – year old female child.
Key words: Phakomatosis pigmentovascularis, Sturge weber syndrome, Klippel trenaunay syndrome, nevus of Ota, mongolian spots
Introduction:
Phakomatosis pigmentovascularis (PPV) is a rare genetic disorder characterized by association of capillary malformation with pigmentary nevus. Five types of PPV are described with further subtype ‘a’ for cutaneous involvement only and subtype ‘b’ for cutaneous as well as systemic involvement.1,2 Sturge-Weber syndrome (SWS) is a neurological disorder characterized by facial capillary malformation with ipsilateral ocular and brain anomalies.3Klippel-trenaunay syndrome (KTS) is defined as limb capillary venous malformation (CVM) associated with progressive overgrowth of the affected extremity and anomalies of venous system.4 Nevus of Ota are bluish, patchy, dermal melanocytosis that affects the sclera and the skin around the eye.
Case Report:
A 7-year old girl child came to outpatient department with complaints of asymmetry of left half of body and red patch on left side of face since birth along with history of seizures. She was full term vaginal delivery in hospital with birth weight of two kilograms. Her developmental milestones were normal. Her body weight was 15.7 kgs. and height was 108 cms. Examination revealed non-blanchable erythematous patch of port wine stain on left side of face in the distribution of all V1, V2 and V3 branches of trigeminal nerve (Fig.1). Multiple aberrant mongolian spots were present on trunk and back (Fig.2).
 |
Figure 1: Shows port wine stain and Hypertrophy of left half of face. |
 |
Figure 2: Shows aberrant multiple mongolian spots. |
The patient had hypertrophy of left side of body with enlargement of left half of face, left lower limbs and left half of genitalia (Fig. 1,3,4,5). There was engorgement of veins on left lower abdomen crossing the mid-line. Higher mental functions including speech were normal. She had limping gait and motor examination was normal. The eye examination revealed bluish discoloration of sclera on both side consistent with Nevus of Ota. (Fig.5).
 |
Figure 3: Shows gross enlargement of left foot. |
 |
Figure 4: Shows hypertrophy of left half of external genitalia & engorgement of veins. |
 |
Figure 5: Shows nevus of ota in both eyes. |
Magnetic resonance imaging (MRI) of the brain showed cerebral hemiatrophy on left side with loss of white matter more significant in temporo-parieto-occipital region with mild peritrigonal FLAIR hyperintensity (Fig.6). Color doppler studies of lower limbs showed chronic thrombosis of left deep venous system with formation of superficial collaterals in left inguinal region and upper part of left thigh. Right lower limb venous system was normal. Ultrasonography of abdomen was normal. Complete blood count, bleeding & clotting profile, liver function tests, renal function test were normal.
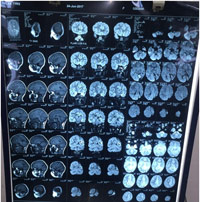 |
Figure 6: MRI Brain shows cerebral hemiatrophy on left side with loss of white matter more significantly in temporo-parieto-occipital region with mild peritrigonal FLAIR hyperintensity. |
Discussion:
Ota et al1 in 1947 coined the term “Phakomatosis pigmentovascularis” and reported associations between cutaneous venous malformations and pigmented nevi. Further studies proposed that the vascular and pigmentary anomalies arises as a result of a genetic concept called twin spotting.2,3 PPV was further delineated in five types with subtype ‘a’ for cutaneous involvement only and subtype ‘b’ for cutaneous as well as systemic involvement. Also, among five types of PPV, type II (Phakomatosis cesioflammea) was the most common with 75% reported cases.4,5,6 However Goyal T et al5 reported first case of Phakomatosis cesioflammea (typeIIb) from India in a 4- year old girl child. The largest series of PPV was published by Cordisco et al7, who presented 25 patients in Argentina. In that, type IIb was the most common type. In another study it was reported that the most common association with extra cutaneous presentations was with the Sturge-Weber syndrome (SWS) and with the Klippel-trenaunay syndrome (KTS), individually or combined.8 Okunola et al.9 reported two cases of Phakomatosis pigmentovascularis type IIb in association with external hydrocephalus. Pradhan S et al10 reported a case of Phakomatosis pigmentovascularis Type IIb with Sturge–Weber syndrome and cone shaped tongue. Jahangir et al.11 reported a case of Phakomatosis pigmentovascularis with lower limb vascular abnormalities in a young Kashmiri male child.
Our patient had PWS, hypertrophy of left half of the face, trunk, extremities and external genitalia with venous engorgement on left lower abdomen and history of seizures. The color Doppler studies of lower limb showed chronic thrombosis of left deep venous system. MRI of the brain showed cerebral hemiatrophy on left side with loss of white matter more significant in temporo-parieto-occipital region. The case is being reported for its rarity and unusual presentation.
References:
1. Ota M, Kawamura T, Ito N. Phakomatosis pigmentovascularis (Ota). Jpn J Dermatol 1947; 52: 1–3.
2. Tadini G, Restano L, Gonzalez-Perez R, et al. Phacomatosis pigmentokeratotica: report of new cases and further delineation of the syndrome. Arch Dermatol 1998; 134: 333-7.
3. Happle R. Allelic somatic mutations may explain vascular twin nevi. Hum Genet 1991; 86(3): 321-2.
4. Redondo P, Bastarrika G, Aguado L, et al. Foot or hand malformations related to deep venous system anomalies of the lower limb in Klippel-trenaunay syndrome. J Am Acad Dermatol 2009; 61(4): 621-8.
5. Goyal T, Varshney A. Phacomatosis cesioflammea: First case report from India. Indian J Dermatol Venereol Leprol 2010; 76(3): 307.
6. Gupta K, Gupta LK, Mittal A, Khare AK, Mehta S, Balai M. Phacomatosis cesioflammea in a 5-week-old infant. Indian J Paediatr Dermatol 2016;17:48-9.
7. Cordisco MR, Campo A, Castro C, et al. Phakomatosis pigmentovascularis: report of 25 cases. Pediatr Dermatol 2001; 18: 70.
8. Garg A, Gupta LK, Khare AK, Kuldeep CM, Mittal A, Mehta S. Phacomatosis cesioflammea with Klippel Trenaunay syndrome: A rare association. Indian Dermatol Online J 2013;4:216-8.
9. Okunola P, Ofovwe G, Abiodun M, Isah A, Ikubor J. Phakomatosis pigmentovascularis type IIB in association with external hydrocephalus. BMJ Case Reports 2012;10.1136/bcr.12.2011.5432, Published Jun 25
10. Pradhan S, Patnaik S, Padhi T, Nayak BP. Phakomatosis pigmentovascularis Type IIb, Sturge – Weber syndrome and cone shaped tongue: An unusual association. Indian J Dermatol Venereol Leprol 2015; 81(6): 614-6.
11. Jehangir M, Quyoom S, Bhat J, et al. Phakomatosis pigmentovascularis with lower limb vascular abnormalities in a young Kashmiri male child-Report of a first child from Kashmir Valley (India) and review of literature. Our Dermatol Online. 2016; 7(1): 87-90.

anastrozole buy online cheap anastrozole 1mg buy arimidex 1 mg without prescription
Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks. nimabi
Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks. nimabi
Pharmacie Internationale en ligne: Medicaments en ligne livres en 24h – pharmacies en ligne certifiГ©es
Achat mГ©dicament en ligne fiable https://kamagraenligne.com/# pharmacie en ligne pas cher
amoxicillin 500 coupon: amoxil doxycyclineca – where can i buy amoxicillin without prec
amoxicillin tablet 500mg
https://azithromycinca.shop/# buy doxycycline without prescription uk
buy doxycycline
Very interesting points you have mentioned,
appreciate it for posting.Raise blog range