LETTER TO EDITOR
Year: 2018 I Volume: 1 I Issue: 2 I Page: 57-58
A Case Of Chronic Radiodermatitis in Adental X-RAY Technician: A Rare Entity
Dr. Tulika Rai11 Dr. Dheeraj Kumar Patwa 2
1 Assistant Professor, Department of Dermatology & Venereology, I.M.S., B.H.U. Varanasi
2 Junior resident, Department of Dermatology & Venereology, I.M.S., B.H.U. Varanasi
Corresponding Author:
Dr. Dheeraj Kumar Patwa
Email: dr.dkpatwa@gmail.com
How to cite this article:
Rai T, Patwa DK. A case of chronic radiodermatitis in a Dental X-ray technician: A rare entity. JDA Indian Journal of Clinical Dermatology 2018;2:57-58.
Sir,
Dealing with diagnostic X-ray radiation may result in serious health problems, unless protection guidelines are followed. This become prevalent immediately a decade following the invention of X-ray radiation, where it had not been known that accumulative exposure to X-ray radiation may carry huge health hazard. Due to occupational accidents, radiography workers may be rarely exposed to high dose of ionizing radiation and acute radiodermatitis may develop after the exposure. After an asymptomatic period of which can last several months, poikiloderma, sclerosis, necrosis, and ulceration of the skin may be observed as clinical features of chronic radiodermatitis.
A case report of 40 year old male, working as a dental radiographer for 12 years (1996-2008) developed thickening was over skin of thumb and fingers, and blackening was over bilateral thumbs nails for 8 years. After 2 years he developed ulcers and thinking over fingers and thumbs, a dermatologist prescribed topical steroid and lesions improved with in two month but blackening and thickening didn’t improve. He presented with ulceration on fingers and blackening of nails. On examination, atrophy of skin, loss of hair appendages, poikiloderma and scar was present over bilateral thumb and a nonhealing ulcer with purulent discharge over right index finger was present (fig.1 and 2). Systemic examination was with in normal limit. Histopathological examination showed a fairly circumscribed focus of mild epidermal hyperplasia with disorderly arrangement of keratinocytes in lower half of epidermis. There was mild nuclear pleomorphism and occasionally dyskeratotic cells and mitotic figures were also seen. The stratum corneum showed alternating zones of orthokeratosis and parakeratosis which spares follicular infundibula. The dermis showed a moderately dense patchy lichenoid lymphocytic infiltrate underlying this focus [fig.3].Topical and oral antibiotics were prescribed for two weeks. Potent topical steroids were prescribed thereafter. There was mild improvement clinically and patient is on regular follow up. We report this case because of rarity.
 |
Figure 1: Clinical photograph of a technician showing ulceration of right index finger |
 |
Figure 2: Nail and skin changes of thumb |
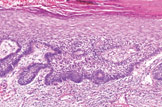 |
Figure 3: Histopathology(H&E stain 40X): Stratum corneum shows alternating zones of orthokeratosis and parakeratosis and dermis shows a moderately dense patchy lichenoid lymphocytic infiltrate, Mild nuclear pleomorphism , dyskeratotic cells and mitotic figures and fairly circumscribed focus of mild epidermal hyperplasia with disorderly arrangement of keratinocytes in lower half of epidermis. |
Late skin effects can develop months to years after the exposure to radiation. The main cutaneous reactions that characterize chronic radiodermatitis are skin atrophy, fibrosis, pigmentation changes, telangiectasia, necrosis and secondary malignant skin tumours. The underlying mechanism behind chronic skin reactions is based on an extended inflammatory reaction and is prolonged for months to years afterwards. Inflammatory cytokines (e.g. IL-1a, IL-6, TNF-a) are responsible for this reaction. In addition, TGF-ß and platelet-derived growth factor are upregulated in irradiated skin. These cytokines enhance tissue fibrosis by activating fibroblasts and inducing synthesis of extracellular matrix proteins and metalloproteinase, as well as the formation of telangiectasia. The prolonged inflammatory reaction induces skin atrophy and necrosis via the accumulation and activation of leucocytes at the irradiated area [1].
Management of ulcerations and necrotic wounds in chronic radiodermatitis is general wound care guidelines are the most important. These include the application of wound dressings that absorb the wound exudate and protect the wound from environmental damage and bacteria to prevent secondary infections. For patients with very moist wounds, hydrogel or hydrocolloid dressings can be used. These dressings do not adhere to wounds, are absorbent and can easily be replaced. For infected wounds, silver-containing dressings can be used. Chronic ulcerations need to undergo selective and careful debridement in order to clean the wound and stimulate the healing process [2, 3]. In some severe cases, surgical interventions are necessary in which skin-flaps are used [4].
In general, dental radiography has a little dose and risk for the individual patient and dental workers provided that the principles of protection are applied; it is less dangerous in comparison to a few days of natural background radiation to which we are all constantly exposed [8].Dental radiography doses and risks are minimal unless dealt without being cautious, which is the case of the radiographer presented here.
References:
1. Spalek M. Chronic radiation-induced dermatitis: challenges and solutions. Clin Cosmet Investig Dermatol 2016; 9:473–482.
2. Hymes SR, Strom EA, Fife C. Radiation dermatitis: clinical presentation, pathophysiology, and treatment 2006. J Am Acad Dermatol 2006; 54:28–46.
3. Wong RK, Bensadoun RJ, Boers-Doets CB, Bryce J, Chan A, Epstein JB, et al. Clinical practice guidelines for the prevention and treatment of acute and late radiation reactions from the MASCC Skin Toxicity Study Group. Support Care Cancer 2013; 21:2933–2948.
4. Veness M, Richards S. Bolognia J, Jorizzo J, Schaffer J. Radiotherapy. Dermatology. New York, NY: Elsevier; 2012.
5. Abbott P. Are dental radiographs safe? Aust Dent J 2000; 45:208-13.

Respected casino https://biamo.bet/ that pays. Prompt payouts, pay any way you want. Many different online games, slots. Huge selection of sports betting, online streaming, work all over the world. Click and win with us
anastrozole 1mg brand oral anastrozole 1 mg anastrozole buy online
I agree with your point of view, your article has given me a lot of help and benefited me a lot. Thanks. Hope you continue to write such excellent articles.
Your article gave me a lot of inspiration, I hope you can explain your point of view in more detail, because I have some doubts, thank you.
levitra lowest price In observational studies, the relationship between blood pressure and end stage renal disease ESRD is direct and progressive
Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks. nimabi
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://www.binance.info/kz/join?ref=FIHEGIZ8
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article. https://accounts.binance.com/el/register?ref=T7KCZASX
Your article helped me a lot, is there any more related content? Thanks!
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
п»їbest mexican online pharmacies: cmq pharma – medicine in mexico pharmacies
medication from mexico pharmacy
https://cmqpharma.com/# mexican mail order pharmacies
buying from online mexican pharmacy
I like this website very much, Its a really nice office to read and incur info.Blog range
canada ed drugs: best canadian pharmacy – legitimate canadian pharmacy
mexican drugstore online: mexican mail order pharmacies – mexican online pharmacies prescription drugs
pharmacy com canada canadian pharmacy prices canadian pharmacy online store
https://indiapharmast.com/# Online medicine order
mail order pharmacy india: indian pharmacy paypal – best online pharmacy india
top 10 online pharmacy in india: Online medicine home delivery – cheapest online pharmacy india
reputable mexican pharmacies online: mexico drug stores pharmacies – mexican rx online
medication from mexico pharmacy mexican mail order pharmacies reputable mexican pharmacies online
https://canadapharmast.com/# my canadian pharmacy reviews
certified canadian international pharmacy: canada pharmacy 24h – pharmacy canadian superstore
buying from online mexican pharmacy mexico drug stores pharmacies mexico drug stores pharmacies
online pharmacy india: online pharmacy india – buy prescription drugs from india
top online pharmacy india: п»їlegitimate online pharmacies india – best india pharmacy
mexico pharmacy: mexican pharmaceuticals online – mexico pharmacies prescription drugs
http://foruspharma.com/# buying from online mexican pharmacy
medication from mexico pharmacy: mexico pharmacy – mexico pharmacy
http://ciprodelivery.pro/# cipro ciprofloxacin
doxycycline 100 mg price uk: doxycycline 100mg tablet price in india – doxycycline 75 mg tab
https://ciprodelivery.pro/# ciprofloxacin 500mg buy online
http://doxycyclinedelivery.pro/# doxycycline 50 mg
generic clomid without insurance: where can i buy clomid no prescription – can i get cheap clomid without insurance
http://clomiddelivery.pro/# cheap clomid pill
buy amoxicillin 500mg capsules uk: where can i buy amoxicillin over the counter uk – can you buy amoxicillin over the counter
https://paxloviddelivery.pro/# paxlovid buy
https://amoxildelivery.pro/# amoxicillin cephalexin
paxlovid pharmacy: paxlovid pill – paxlovid generic
http://clomiddelivery.pro/# get generic clomid without dr prescription
clomid without a prescription: where can i buy clomid pills – cost clomid pills
http://ciprodelivery.pro/# cipro
http://amoxildelivery.pro/# amoxicillin 500 mg for sale
amoxicillin no prescipion: cheap amoxicillin 500mg – buying amoxicillin online
doxycycline 200 mg price in india: doxycycline 150 mg price – where can i order doxycycline