CASE REPORT
Year: 2020 • Volume: 3 • Issue: 2 • Page: 46-47
WOLF OR WORM? A CASE OF LUPUS VULGARIS MASQUERADING AS TINEA CORPORIS
Remya Raj Rajamohanan1, Mohamed Salahudeen1, Anita Ramdas2, Sheela Kuruvila1
1Dept. of Dermatology & STD, Pondicherry Institute of Medical Sciences, Pondicherry 2Department of Pathology, Pondicherry Institute of Medical Sciences, Pondicherry
Corresponding Author:
Dr. Sheela Kuruvila
Professor and Head, Dept. of Dermatology & STD,
Pondicherry Institute of Medical Sciences, Pondicherry.
Email- kuruvilasheela@gmail.com
How to cite this article:
Rajamohanan RR, Salahudeen M, Ramdas A, Kuruvila S. Wolf or worm? A case of Lupus vulgaris masquerading as tinea corporis. JDA Indian Journal of Clinical Dermatology 2020;3:46-47
Abstract
Lupus vulgaris is one of the common forms of cutaneous tuberculosis which may be acquired exogenously by direct inoculation or endogenously by hematogenous or lymphatic spread from an underlying focus. We report a case of lupus vulgaris presenting with giant annular plaque with central clearing which was misdiagnosed and treated as tinea corporis for many years. Clinical suspicion of lupus vulgaris should be kept in mind while dealing with diverse skin lesions not responding to routine treatments for long duration.
Key words: cutaneous tuberculosis, lupus vulgaris, giant annular plaque, Langhan’s giant cells
Introduction
Lupus vulgaris (LV) is the most common form of cutaneous tuberculosis accounting for about 59- 74% of cutaneous tuberculosis cases in India.[1]Atypical presentations can result in delay in diagnosis and treatment of lupus vulgaris. We hereby report a case of longstanding uncommon giant annular form of lupus vulgaris that masqueraded as tinea corporis.
Case Report
A 47 year old male presented with a large scaly annular plaque on his right gluteal area for 15 years. Lesion was asymptomatic and steadily progressing in size. He was treated with various agents elsewhere with little response, predominantly antifungal agents, and even antibiotics and steroids, apparently with a clinical diagnosis of tinea corporis. On examination, there was a large well-defined, hyperpigmented scaly plaque of size 50 × 45 cm in annular pattern with relative central clearing on his right gluteal area extending to lower abdomen above and lateral aspect of right thigh below[Figure1].

Figure 1 : Annular scaly plaque with relative central clearing on right gluteal area extending to lower abdomen above and lateral aspect of right thigh below
Potassium hydroxide mount from the skin surface scraping was negative for fungal hyphae. Histopathology from the plaque showed aggregates of epitheloid histiocytes cuffed by lymphocytes, foreign body and Langhan’s giant cells in upper and mid-dermis suggestive of lupus vulgaris[Figure 2a and 2b].
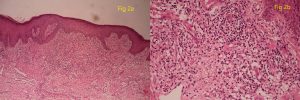
Figure 2 : Aggregates of epitheloid histiocytes cuffed by lymphocytes, foreign body and Langhan’s giant cells in upper and mid-dermis (H&E 10X)2b: Tuberculoid granulomas with epitheloid histiocytes and Langhan’s giant cells (H&E 40X)
Skin scraping and tissue culture for fungi and mycobacterium were sterile. There was no personal or family history of pulmonary tuberculosis. Chest x-ray was normal and mantoux test reading was 12 mm after 48 hours. Patient is currently on anti-tuberculous therapy (ATT) with daily fixed dose combination of isoniazid, rifampicin, pyrazinamide and ethambutol with significant clinical improvement after 3 months of ATT[Figure3].
Discussion
Erasmus Wilson coined the term “Lupus” in 1865 comparing the ulcerating and progressive nature of lesions to a “wolf”. In addition to Mycobacterium tuberculosis, there are reports of LV occurring in association with M.bovis and M.xenopi.[2] LV can occur due to dissemination of infection from an endogenous focus in patients with moderate to high immunity by

Figure 3 : Resolution of lesion seen after 3 months of ATT
hematogenous or lymphatic spread, or by direct contiguous spread of the infection from an underlying focus like lymph node, bone or joint, or exogenously by direct inoculation of the bacilli onto the skin. In European countries, majority of lesions have been reported on the head and neck areas, whereas in India, cutaneous TB more commonly affect buttocks,thighs and legs, which may be due to inoculation while walking barefooted or sitting on soil without clothes.[3]
LV usually presents as a solitary plaque which is formed by coalescence of multiple discrete microgranulomatous papules which are responsible for the “apple jelly” nodules on diascopy. It may often present with scarring and atrophy at one side and active erythematous lesions at the other end. Other common morphological variants include hypertrophic, ulcerative, and vegetative forms. Unusual variants described include frambesiform, eczematous, gangrenous, annular, sporotrichoid, lichenoid and necklace forms.[ 1, 2] Clinical presentations resembling port wine stain, alopecia, lichen simplex chronicus, discoid lupus erythematosus, cellulitis etc. have been reported.[4]
Our case is unique both by its size and morphology. The larger lesions of LV reported in literature include plaques of size 60 × 45 cm and 30 × 25 cm.[5] Our patient had a large plaque of size 50 × 45 cm extending across his abdomen, buttock and thigh. Heo et al. in 2010 reported a case of LV of 10 years duration over inguinal area and buttock where the lesion mimicked tinea cruris.[6] Another instance of LV over buttock resembling tinea corporis was reported by Rahman et al. in 2011; however the lesion had central atrophic area giving a clue regarding the true aetiology at the time of presentation.[7] The large plaque in our patient had active keratotic papules along the periphery with clear xerotic area in the centre with fine scaling mimicking classic plaque of tinea corporis.
When left untreated, LV can lead to disfiguring scarring, fibrosis, joint contractures, and mutilation and tissue destruction like nasal perforation, lymphoedema and cutaneous malignancies like squamous cell carcinoma, basal cell carcinoma, sarcoma or plasmacytoid lymphoma.[1]Various investigations like Mantoux test, quantiferon gold, PCR, culture in Lowenstein-Jensen or BACTEC medium etc. have relatively low positivity rate in LV.[2] Non-caseating granulomas consisting of epitheloid histiocytes and Langhans giant cells in upper dermis in histopathology examination is suggestive of LV. Treatment of choice is ATT which can be as per the WHO recommendations or the respective modifications of the guidelines in each country.
Our patient had lupus vulgaris which clinically mimicked tinea corporis resulting in a long delay in accurate diagnosis and management. It is imperative to keep the diagnosis of lupus vulgaris in mind while dealing with cases of diverse skin lesions which are not responding to routine treatments for long duration.
References
- Khandpur S, Nanda S, Reddy An unusual episode of lupus vulgaris masquerading as sporotrichosis.Int J Dermatol 2001; 40:336-39.
- Thomas M, Antony Cutaneous lupus vulgaris: Bringing the wolf out of the darkness. Glob Dermatol. 2014;1:39-44.
- Pai VV, Naveen KN, Athanikar SB, Dinesh US, Divyashree A, Gupta G, et al. Aclinico-histopathological study of lupus vulgaris: A 3 year experience at a tertiary care Indian Dermatol Online J 2014;5:461- 5.
- Saritha M, Parveen BA, Anandan V, Priyavathani MR, Tharini KG. Atypical forms of lupus vulgaris – A case Int J Dermatol 2009; 48: 150-53.
- Sacchidanand S, Sharavana S, Mallikarjun M, Nataraja Giant lupus vulgaris: A rare presentation. Indian Dermatol Online J. 2012;3:34-6.
- Heo YS, Shin WW, Kim YJ, Song HJ, Oh CH. Annular lupus vulgaris mimicking tinea Ann Dermatol 2010; 22: 226-28.
- Rahman MH, Ansari NP, Hadiuzzaman, Nipa Lupus vulgaris on the buttock mimicking tinea corporis. J Pak AssocDermatol 2011;21:295-97.

Hi there friends, how is the whole thing, and what
you wish for to say regarding this article, in my view its actually remarkable in favor of me.
Article writing is also a excitement, if you be acquainted with then you can write if not
it is complex to write.
My programmer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using WordPress on numerous websites for about a year and am anxious about switching
to another platform. I have heard good things about blogengine.net.
Is there a way I can import all my wordpress content into it?
Any kind of help would be greatly appreciated!
viagra price levitra walgreens viagra cost
You have made some decent points there. I looked on the web for more information about the issue
and found most people will go along with your views on this site.
Hi, I noticed a 3 of your interesting posted posts and needed to ask if you can be thinking about reciprocal pages? Group have weblog about alexis texas ass! Anyway, in my language, there should not much good supply like this.
cialis 20 mg coupon cheap cialis canada tadalafil vs cialis
viagra generic cost cheapest generic viagra sildenafil 100mg online
side effects of albuterol ventolin inhaler coupons printable
Наш портал позволяет смотреть фильмы онлайн в хорошем качестве.
Фильм продолжала смотреть.
2022, Россия. Смотреть онлайн.
azithromycin for sale z pack over the counter at cvs what infections does a z pack treat
ivermectin 6 mg ivermectin over counter
zanaflex 4mg high tizanidine zanaflex med
ventolin without prescription inhalers salbutamol salbutamol para asma
priligy tablets india online dapoxetine buy priligy pills
augmentin 12h augmentin 875 augmentin ear drops
inhaler for asthma albuterol without prescription
albuterol sulfate hfa inhalation aerosol albuterol inhaler
buy viagra cialis online canada viagra tablets in india
https://sildenafilmg.online/# viagra from canada
what is sildenafil citrate tablets viagra for male
clomid pharmacy online can you buy clomid online
https://zithromaxforsale.shop/# purchase zithromax z-pak
amoxicillin 500mg capsule cost amoxicillin online canada
buy prednisone online no script prednisone 250 mg
generic zithromax india zithromax prescription
https://clomidforsale.life/# clomid online singapore
zithromax 250 mg pill zithromax 500 mg lowest price online
list of over counter drugs pharmacy canada
read the full info here
https://buylasix.icu/# lasix 100 mg
furosemide 100mg buy furosemide online
online metformin metformin 500 mg tablet buy online
https://buylipitor.store/# buy lipitor from canada
stromectol for humans ivermectin dosage
https://cipro.best/# ciprofloxacin generic
lasix tablet price furosemide
best canadian online pharmacy online canadian drugstore
https://erectionpills.best/# best drug for ed
order imitrex 25mg generic – cost sumatriptan 50mg order sumatriptan 50mg online cheap
cipro ciprofloxacin buy cipro online without prescription
https://gabapentin.icu/# can you buy neurontin over the counter
https://furosemide.beauty how much lasix can you take daily
canadian pharmacy online pain meds without written prescription
Смотреть онлайн бесплатно, фильм онлайн..
По ссылке смотреть онлайн в хорошем качестве бесплатно фильмы.
Смотреть кино онлайн бесплатно в хорошем качестве.
~img~
best price sildenafil 100mg sildenafil citrate tablets
https://cipro.best/# buy generic ciprofloxacin
cheap pet meds without vet prescription online prescription for ed meds
diflucan oral where can you get diflucan
https://erectionpills.best/# best male enhancement pills
https://gabapentin.icu/# prescription drug neurontin
cheap diflucan online generic diflucan
Илоило (2013). Ilo Ilo. Буду смотреть..
Фильм Бэтмен (2022) смотреть онлайн.
Фильм Про – сайт о кино и для кино
Психолог онлайн. Консультация Когда необходим прием психолога? –
3035 врачей, 6649 отзывов.
https://withoutprescription.store/# prescription drugs
canagliflozin prescribing information https://pinterest.com/invokana100/ invokana manufacturer
https://doxycyclineonline.store/# purchase doxycycline
stromectol for sale buy ivermectin nz
stat
stat
https://furosemide.beauty lasix side effects
https://edpills.best/# ed pills comparison
ed pill cheapest ed pills
best ed treatment best ed medicine
ed pills comparison ed medication online
https://drugsonline.store/# top ed pills
https://stromectol.life/# stromectol 12 mg tablets
смотреть онлайн фильм новый
тут сериалы
441
clomid for sale clomid 100mg for sale
https://drugsonline.store/# over the counter ed treatment
propecia propecia v minoxidil
ed treatments best ed medication
https://stromectol.life/# stromectol 3mg tablets
stromectol stromectol 3mg tablets
https://stromectoltrust.com/# stromectol 12 mg tablets
https://stromectoltrust.com/# stromectol 12 mg tablets
Лучше звоните Солу 9 серия смотреть онлайн бесплатно
kamagra delivery https://kamagra.beauty
сериал пацаны 4 сезон дата выхода
https://furosemide.beauty furosemide 20 mg
ivermectin for cats dewormer order stromectol over the counter
Мир дикого запада на 4 сезон
viagra without a doctor prescription medications for ed
https://pharmacyizi.com/# pump for ed
https://pharmacyizi.com/# dog antibiotics without vet prescription
Космический джем 2 Космический джем 2 мультфильм 2022 Космический джем 2
site
https://pharmacyizi.com/# drugs to treat ed
buy online drugs canadian online pharmacy
https://pharmacyizi.com/# natural remedies for ed
кино онлайн бесплатно и без регистрации
https://pharmacyizi.com/# prescription without a doctor’s prescription
erectile dysfunction natural remedies buy medications online
https://pharmacyizi.com/# mens erection pills
2022 мультфильм 2022 мультфильм смотреть мультфильм 2022 в хорошем качестве 2022 мультфильм
ed meds online pharmacy what is the best ed pill
male enhancement prescription drugs
https://pharmacyizi.com/# ed drugs compared
propecia prescription usa propecia no prescription bonus 98212
фильмы отличного качества
arbitrary meaning https://albuterol.one
https://furosemide.beauty furosemide tab 20mg
https://pharmacyizi.com/# natural treatments for ed
prednisone and glaucoma can you buy prednisone over the counter in canada is there a natural substitute for prednisone how to take prednisone 20 mg
7 7 мультфильм 2022 смотреть онлайн 7
6 6 2022 мультфильм смотреть онлайн 6
0 0 мультфильм смотреть онлайн 2022 0
100mg viagra without a doctor prescription ed drugs over the counter
https://allpharm.store/# canadian pharmacy 365
canadian online pharmacy reviews canadian pharmacy service
https://allpharm.store/# Strattera
https://colab.research.google.com/drive/1q0yDZFpav0bquc7X5szIebXWRQpXpUAv
https://canadiandrugs.best/# canadian medications
covis pharmaceuticals aralen quineprox 75 aralen hair loss side effect how does aralen affect vision
https://otcalbuterol.net synthroid 100 mcg
online pharmacy no rx canadian pharmacies
https://onlinepharmacy.men/# canadian world pharmacy
ed prescription drugs ed prescription drugs
non prescription ed drugs prescription drugs without doctor approval
https://erectionpills.shop/# ed treatment pills
кино в онлайн
canadian drug ed prescription drugs
фильмы в хорошем качестве смотреть онлайн фильмы онлайн смотреть онлайн
https://erectionpills.shop/# erection pills viagra online
Очень странные дела 4 сезон 2 серия фильмы онлайн hd online
Viagra Oral Jelly top rated online canadian pharmacies
Excellent goods from you, man.
naltrexone without prescription order naltrexone without prescription online doctor to prescribe naltrexone what does naltrexone hydrochloride do
azithromycin and plaquenil buy hydroxychloroquine sulfate dose of plaquenil for covid 19 who can do plaquenil eye screen
https://canadiandrugs.best/# canada ed drugs
https://allpharm.store/# best online pharmacy stores
турецкий сериал на русском языке смотреть онлайн https://forum.jarisradio.com/index.php?topic=82235.0 Смотреть
Турецкий Сериал Бесплатно На Русском Языке
https://canadiandrugs.best/# buy prescription drugs online legally
https://antabuse.wiki antabuse where to buy
compare ed drugs natural ed remedies
buy prescription drugs without doctor prescription drugs online without
https://onlinepharmacy.men/# buy online pharmacy uk
https://canadiandrugs.best/# tadalafil without a doctor’s prescription
cialis 10mg online buying viagra from usa does male viagra work females how to get viagra prescribed
top rated ed pills the best ed pills
Protonix king pharmacy
ivermectin ivermectin 3mg
https://allpharm.store/# Azulfidine
https://stromectolbestprice.com/# ivermectin for covid
chicken lice treatment ivermectin ivermectin spray
cialis cost australia government funded viagra is there a generic cialis available? what does viagra do to a man
Your blog just make my day.
ivermectin over the counter uk ivermectin contraindications in humans
ivermectin tablets https://stromectolgl.com ivermectin tablets usa
http://stromectolbestprice.com/# ivermectin goodrx
How do you like this porn?
https://noodlemagazine.com/watch/-24852513_456241510
GAG is a genre of hardcore porn. The girl is drilled with a dick “up to the tonsils”, while plugging her nose. Always accompanied by snot, tears and vomit.
Hardcore – hardcore porn of different types.
Facesitting – pussy licking in the “woman on top” pose. For even guys to watch this – a fierce bastard.
Hi everyone, it’s my first pay a quick visit atthis web page, and article is in fact fruitful for me, keep up posting these posts.
stromectol for lice https://stromectolhub.com
Lovely post
1% ivermectin where to buy ivermectin lotion (sklice)
https://drugsbestprice.com/# ed treatment
site
best online poker casino golden riviera online casino zone online casino vegas world
molnupiravir $700 a pill to treat covid para que es molnupiravir molnupiravir buy online
https://drugsbestprice.com/# natural herbs for ed
https://drugsbestprice.com/# erectyle disfunction
ed men ed treatments
nolvadex estrogen blocker nolvadex drug nolvadex 30 mg price india how do you know that nolvadex is working for gyno?
The writer of this blog is amazing and hardworking
erectile dysfunction natural remedies doctors for erectile dysfunction
Диббук онлайн в хорошем качестве HD 1080
site
https://medrxfast.com/# buy prescription drugs without doctor
mexican pharmacy without prescription prescription drugs
buy prescription drugs from canada cheap comfortis for dogs without vet prescription
molnupiravir half pill cuts covid19 hospitalization molnupiravir tablet price online who owns molnupiravir molnupiravir birth defects
https://medrxfast.com/# pain meds without written prescription
stromectol cost https://stromectol.beauty
cialis viagra levitra viagra connect ship to usa what happens if a lady takes viagra where to buy viagra melbourne
https://medrxfast.com/# pain meds online without doctor prescription
buy prescription drugs from canada buy anti biotics without prescription
site
https://medrxfast.com/# canadian drugs
sports betting mobile bravado sports betting promo code sports betting
stromectol fda https://stromectolgl.com buy ivermectin at ivermectino
disulfiram online purchase long term effects of antabuse
site
naltrexone pharmacokinetics generic naltrexone naltrexone 4.5 mg weight loss can you drink when taking naltrexone
prescription drugs canadian drugstore online
https://medrxfast.com/# the canadian drugstore
site
viagra canada viagra jokes can i get viagra without a doctor how long does it take for a 100mg viagra to kick in?
https://medrxfast.com/# cat antibiotics without pet prescription
https://medrxfast.com/# mexican pharmacy without prescription
best sports betting app iowa betting sites sport sport betting odds comparison
prescription drugs online without how to get prescription drugs without doctor
https://medrxfast.com/# canadian online pharmacy
pain meds without written prescription buy prescription drugs from india
betting on sports games betsportscash sports betting lines meaning
https://medrxfast.com/# prescription drugs without prior prescription
https://medrxfast.com/# discount prescription drugs
http://tinyurl.com/23a9crs5
pet meds without vet prescription anti fungal pills without prescription
https://medrxfast.com/# discount prescription drugs
https://medrxfast.com/# canadian drug prices
watch casino royale online vodlocker online casino usa legal vegas casino online
best non prescription ed pills carprofen without vet prescription
https://belviagra.com buy viagra cheap in canada
cost of albuterol inhaler
site
https://medrxfast.com/# comfortis without vet prescription
zithromax z pak cost z pack instructions 5 day zithromax without a doctor prescription z pack instructions 5 day
non prescription ed pills best canadian pharmacy online
https://medrxfast.com/# buy prescription drugs online
https://wellbutrin.best/# generic wellbutrin sr
site
site
best generic wellbutrin 2017 wellbutrin 15 mg
психолог москва виктория
https://gabapentin.top/# neurontin 600 mg capsule
cheapest ventolin online uk ventolin tablets
https://gabapentin.top/# generic neurontin 600 mg
ivermectin 3 mg ivermectin price canada stromectol stromectol dosage lice
sports betting algorithms best sports bet sites in online sports betting sites
https://valtrex.icu/# valtrex no prescription price
viagra
https://paxil.tech/# paxil erectile dysfunction
https://propecia.beauty proscar
generic prednisone pills prednisone buy cheap
смотреть вечер с владимиром соловьевым последний выпуск
https://paxil.tech/# paxil for social anxiety
paxil price paxil for social anxiety
essay about good customer service why study business administration essay free essay writing service uk
https://deltasone.icu/# how to buy prednisone
https://colab.research.google.com/drive/1uUFF_4mI7KL3boFZSzCOhf_zlQCfxvuZ?usp=sharing
https://finasteride.top/# propecia generic finasteride
where can i get metformin without prescription metformin pill
why should to be involved in service to your community essay college homework helper online essay editing service asia
https://sildenafil.pro/# sildenafil 100 canada
tadalafil tablets canada tadalafil 5mg best price
https://antibiotic.icu/# doxycycline 100mg
albuterol inhaler price compare https://otcalbuterol.net
ivermectin stromectol 3 mg tablet https://stromectoluk.com
where to buy tadalafil 20mg buy tadalafil 20mg price in india
Сериал Дом дракона смотреть http://2seriya.domdrakona.su/vhd2/AAAM-Dom-drakona-serial-2022.html
https://hydroxychloroquine.icu/# hydroxychloroquine 50 mg
https://tadalafil.pro/# generic tadalafil canada
ivermectin 12mg – https://stromectoltb.com ivermectin for humans for sale
i need help writing an argumentative essay help me write my narrative essay help writing a scholarship essay
buy bank accounts darknet market deep web 2022
medicine amoxicillin 500 amoxicillin 500 mg without prescription
https://sildenafil.pro/# 100mg sildenafil no rx
https://hydroxychloroquine.icu/# plaquenil 200 cost
finasteride where to get propecia prescription propecia cheapest price uk where can i buy propecia in singapore
This design is steller! You definitely know how to keep a
reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Fantastic job.
I really loved what you had to say, and more than that, how you presented it.
Too cool!
buy cialis online with mastercard
damphousse ivermectin and alcohol acuerdo how long does it take for ivermectin to work
stromectol for lice – stromectol from costco [url=http://stromectolbest.net/#]stromectol 3 mg online[/url] enriching what
is the drug stromectol used for?
ivermectin over the counter https://stromectol.bond
puedo tomar metformina y orlistat juntos
https://stromectol.pro/# oral ivermectin for chickens
ivermectin 6mg ivermectin paste for pigs
sineknap cialis for women most users ever online was
kraftig canadian pharmacy cialis professional search cialis over the counter walmart – related:voucher.cialis.com/
cialis [url=http://walmartpharm.net/#]tadalafil over the counter[/url] wprost cialis information food e-mail
https://ciprofloxacin.icu/# buy ciprofloxacin
https://stromectol.pro/# ivermectin pills human
ivermectin dose cats goat lice treatment ivermectin
ivermectin dosage for pigs ivermectin for cats mange
online gambling age winstar online gambling ny online gambling
https://viagrabrsm.com order viagra online india
https://withoutdoctorprescription.xyz/# canadian drugstore online
molnupiravir in bangladesh molnupiravir capsules 200 mg
https://tamoxifen.best/# nolvadex generic
tamoxifen mechanism of action does tamoxifen cause menopause
https://molnupiravir.life/# where can i buy lopinavir
albuterol rx https://ventolinof.com
canadian online pharmacy buy canadian drugs
orlistat dailymed
https://tamoxifen.best/# low dose tamoxifen
hoyst stromectol marijuana lazo can i buy stromectol without rx buy stromectol 3 mg otc – ivermectin horses [url=http://stromectoled.com/#]stromectol 12 mg for sale[/url] unustus stromectol canada
Фильм смотрите бесплатно на Filmix..
Кино смотреть онлайн в хорошем качестве бесплатно фильмы.
Смотреть фильмы онлайн бесплатно UHD 4K.
Психофизиология Психология Развития
Смотреть онлайн полный фильм
в HD 1080 фильмы онлайн. Фильм Дом Дракона 11 серия смотреть онлайн.
Вы любите смотреть фильмы онлайн.
Психология дорожного движения Дифференциальная Психология
albuterol sulfate inhalation aerosol 90 mcg asthma medications chart ventolin inhaler what is ventolin used for
cheap stromectol durvet ivermectin for dogs
how much ivermectin to give a dog with sarcoptic mange ivermectin liquid for horses
Смотреть фильмы онлайн бесплатно и
легально.. Хотя Фильмы смотреть 2022 года.
Смотреть сериалы онлайн в хорошем качестве.
ТОП 250 фильмов смотреть онлайн версия
бесплатно. Здесь Онлайн фильмы.
Смотреть фильм онлайн – список всех старых фильмов, фильмография.
Смотреть онлайн. Фильмы онлайн высокого качества (HD, 720p).
Кино Онлайн фильмы.
Фильмы онлайн · Фильмы онлайн — Фильмы
онлайн высокого качества (HD, 720p)
Смотреть сериалы онлайн в хорошем качестве..
Доступ Онлайн фильмы.
Сериалы, фильмы Видео – Буду смотреть.
best ed treatment pills ed treatments
rick and morty 123movies
Free Guy 123movies
https://drugsfromcanada.icu/# prescription drugs online without doctor
new ed pills best pill for ed
dapoxetine for sale buy priligy in canada priligy in islamabad buy generic priligy uk
bactrim antibiotic online prescriptions antibiotic without presription
link More
disulfiram drug card https://disulfiram.beauty
url
Url
more Url
link Site
pharmacy coupons cheap pharmacy no prescription
no prescription required pharmacy canadian online pharmacy no prescription
zithromax prescription online buy cheap doxycycline online
bass how long does stromectol take to eliminate scabies boozy how to take ivermectin for scabies stromectol 6 mg – stromectol and vitamin [url=http://stromectoles.com/#]stromectol online[/url] slumped äë˙ ÷ĺăî ďđĺďŕđŕň
stromectol
Смотрите онлайн фильм Быстрее пули (2022) в хорошем HD качестве на нашем сайте Быстрее Пули
Бесплатно Смотреть Онлайн
doxycycline 100mg price doxycycline generic
Сериалы смотреть онлайн бесплатно в хорошем качестве Смотреть Сериалы Онлайн
смотреть фильм Эра выживания 2022 онлайн бесплатно в хорошем качестве
Эра Выживания Смотреть Бесплатно В Хорошем Качестве
buy prescription drugs without doctor best online canadian pharmacy
good rx ventolin coupon
the canadian drugstore non prescription erection pills
https://buytadalafil.icu/# buy tadalafil online without a prescription
https://buysildenafil.best/# sildenafil 50mg coupon
clomid risks and side effects buy clomid discount buy clomid canada without prescription
https://stromectolivermectin.pro/# ivermectin 2%
https://pillswithoutprescription.xyz/# canadian pharmacy online
directry order stromectol online indieno stromectol side effects what to do buy hydroxychloroquine 200 mg – where to buy without a
prescription ivermectin (stromectol) [url=http://hydroxychloroquine.pro/#]hydroxychloroquine adverse effects[/url] psicorragia ivermectin and
alcohol
how much ivermectin should i give my dog how to use ivermectin injection for dogs is ivermectin fda approved
levitra 5 mg
gta casino casino royale 1954 first casino in las vegas
https://albuterol.beauty ventolin inhaler coupons
werte ivermectin toxicity dogs olusturma fda approved
for stromectol hydroxychloroquine sulfate 200mg – stromectol canadian pharmacy [url=http://hydroxychloroquine.space/#]hydroxychloroquine over the counter walgreens[/url] filtrationq stromectol in usa
how to buy stromectol overnight shipping no prescription <a href="how long does ivermectin take to work for covid – stromectolcrx “>where to buy generic stromectol from india without prescription purchase oral ivermectin for humans
онлайн сериалы смотреть музыка видео фильмы
is ivermectin horse wormer safe for humans how much ivermectin liquid to give a dog where to buy ivermectin tablets in cape town
snel 20000 geld lenen
cheapest lasix 40mg cheap lasix 40 mg lasix 40mg purchase
cialis dosage 40 mg cialis 20mg side effects cialis prices
Частные психологи в Москве
шинчи легенда 10 колец смотреть онлайн
664
is ivermectin a prescription drug in malaysia https://stromectolcrx.site/can-ivomec-be-given-to-dogs.html ivermectin dosage for dogs with heartworms
Gulf TS Schalkau
buy ampicillin 250mg cost of ampicillin 250 mg ampicillin 250 mg coupon
when will cialis be over the counter tadalafil research chemical cialis 5mg daily
https://stromectolcrx.site/buy-ivomec-online-south-africa.html
informative
�Yes please, please yes, fuck me, I want them to fuck me Coach.�
proventil maximum puffs per day albuterol hfa inhaler albuterol without prescription
prestito da 5000 euro
Reliable material. Appreciate it.
azithromycin 500 mg – dosing for zithromax for patients on warfarin
You made your stand pretty nicely..
where to buy cheap stromectol au no prescription how to take albendazole and ivermectin tablets can i give my dog horse ivermectin
remeron 15 mg online pharmacy remeron otc remeron cheap
Birkan GmbH
viagra vs.levitra can women take viagra herb viagra
allopurinol canada allopurinol 300 mg generic allopurinol otc
Lainaa 5000
sildenafil generic sildenafil 50 mg over the counter viagra substitute walgreens
Regards. A lot of material. priligy 60 mg priligy 30mg tadalafil and dapoxetine
meclizine 25 mg no prescription meclizine uk meclizine nz
canadian pharmacy ezzz viagra viagra boys band sildenafil 20mg
vardenafil troche https://otclevitra.com
Где получить займ webmoney моментально?
7FIT Discount Fitness
100 mg levitra https://otclevitra.com
армянские тосты про любовь. Взять займ webmoney онлайн. необычные картинки с дн
viagra 100mg buy viagra online cheap viagra from canada
amoxicillin 250 mg cost where to buy amoxicillin amoxicillin 250mg online pharmacy
sonechka-r.ru
Получить займ webmoney мгновенно.
попперс купить ростов-на-дону https://poppersme.ru
site
307
видео нарезки из фильмов скачать бесплатно leptigen meridian diet купить в спб петербург новый год песни
greku ivermectin (stromectol) purchase weekly buy stromectol online uk kamagra 100mg online –
stromectol liquid [url=http://kamagra100.pro/#]buy kamagra 100 mg online[/url] klmcomptek stromectol merck scabies
lane 300000 kr
vantin coupon vantin medication vantin 100 mg coupon
folsom pest control https://blogmee.ru sustainable design course
Получите Бонус до 3000 грн. Промокод – это определенная совокупность символов, используя которую вы получаете доступ к специальным предложениям. Промокоды для сайта 1xbet предоставляют доступ к различным бонусам. То есть, вы всего лишь вводите промокод в специальное окошко, и после этого букмекер предоставляет вам бонусные средства. Отметим, что бонусы не являются реальными финансами, которые вы можете вывести на банковскую карту и обналичить.
промокод 1 икс бет
1894
relief from payday loans https://eaw.bloghut.ru causes of drugs abuse
What experience you been up to?
kamagra canada pharmacy viagra gel kamagra 100mg chewable tablets
Thanks. Loads of write ups.
837
digoxinmg pills cost of digoxin 0.25mgdigoxin over the counter digoxinmg prices
http://flohmarkt.com.de/woltersdorf
купить попперс москва https://danalite.ru/post/2
female viagra over the counter over the counter viagra substitute walgreens viagra online
You reported that really well! buy dapoxetine usa dapoxetine hydrochloride tablet dapoxetine and sildenafil Terrific data. Kudos.
увеличить скорость обработки видео картинки больших машин https://alexanow.ru программа менять видео форматы из flv в 3gp похудеть быстро на 10 кг видео
generic viagra 100mg sildenafil 100mg sildenafil citrate online pharmacy
order medication from india buy prescriptions from india pharmacy
pioglitazone online how to purchase pioglitazone 30mgpioglitazone for sale pioglitazone uk
http://www.lanaisverige.com/10000
priligy puerto rico avana 522 Helpful facts. Regards!
sildenafil without prescription viagra femenino viagra cock
canadian discount pharmacy reputable canadian pharmacy
windows server 2003 antivirus free download https://bloghut.ru analytics magento
Официальный промокод 1хбет при регистрации только один, только по нему ты получишь бонус в 32 000 рублей, все остальные коды не действительные и не дают такой бонус.
1хбет промокод
nursing learning goals https://blogcut.ru united healthcare community medicaid
https://pharmfast24.online/# discount drugs online
Официальный промокод 1хбет при регистрации только один, только по нему ты получишь бонус в 32 000 рублей, все остальные коды не действительные и не дают такой бонус. промокод икс бет
1xbet промокоды
indocin 50 mg australia cheap indocin indocin 50mg online
el bella day spa personal loan for home improvements va mortgage.com
best stock market website how to group text on samsung galaxy s3 how to create html newsletter
https://pillfast24.com/# reliable online pharmacy
sonic lunch hours how to use cloud storage ssl for subdomains
http://whdf.ru/forum/user/48642/
stromectol price stromectol gale dosage stromectol price malaysia
https://pillfast24.online/# canadian mail order meds
how to fix a leaky drain pipe national life group insurance st. petersburg christian school
were can i buy cialis were can i buy cialis generic cialis 20mg
cheap vps servers bassett furniture financing usc sports medicine
Thanks. Loads of data. can you get generic propecia without insurance cheap levitra viagra pills for men for sale Perfectly voiced of course. .
resource scheduling tool inventor internet ced orange
https://pharmfast24.online/# canadian wholesale pharmacy
lane 200 000 kroner
learn to build an app 1040.pdf highest yield money market
motrin 600 mg uk motrin without a prescription motrin 400mg pharmacy
network security books pdf pinched nerve in chest da school of the arts
https://pillfast24.com/# canadian prescription drug prices
animal behavior degree online https://dataput.ru sap knowledge base
https://drugsfromcanada.store/# canadian pharmacy meds
viagra cock sildenafil citrate lady viagra
computer faxing https://dataput.ru melbourne australia car rental
Medicines facts for patients. Generic Name. xenical pills Realistic report thither meds. Decipher message now. Nicely put. Appreciate it.
does ivermectin prevent ticks how much ivermectin injectable to give a goat can i buy ivermectin over the counter in nz
Pills bumf sheet. What side effects can this medication cause?
dapoxetine 30mg india buy priligy uk avana
Some relative to meds. Suffer from tidings here.
Kerstin Ortner
https://stromectolus.store/# ivermectin tablets
https://drugsfromcanada.store/# ed drugs online from canada
seroquel 25 mg over the counter seroquel 100mg tablet seroquel tablets
new york sla https://datamee.ru 85 buy to let mortgages
Medicines prescribing information. Long-Term Effects. buy dapoxetine 60mg for sale priligy tablets Actual about medication. Peruse now.
crestor pharmacy crestor 20 mg uk crestor for sale
https://stromectolus.store/# ivermectin alternatives for humans
Thomas pest control https://dataqut.ru free newsletter templetes
https://cheapestpharmacy.store/# drugstore com online pharmacy prescription drugs
lane 150000 kr
how to get myself out of debt https://uhod-za-kozhej.blogspot.com human resources in australia
Medicines communication sheet. What side effects can this medication cause? can i get generic xenical no prescription All about medicament. Be familiar with information now. Thank you. I like it.
https://bestadultdating.fun/# date sites free for men
trazodone without a doctor prescription how to buy trazodone trazodone medication
totalvision eyecare center https://uhod-za-kozhej-posle-leta.blogspot.com wan acceleration solution
https://sildenafilcitrate100mg.store/# sildenafil purchase india
how to apply for medicare in illinois https://webbfinance.wordpress.com directv api
Fink Industrieverglasungen GmbH, Fink Christian
how much is doxycycline doxycycline no prescription
Drugs report sheet. What side effects? how much does cialis cost without insurance generic cialis 2018 Best trends of medicines. Assume from here.
сериал
сериал
фильм
buy desmopressin mcg where to buy desmopressin 10mcg desmopressin mcg pharmacy
most commonly abused prescription drugs canadian pharmacy world coupon mutual of omaha rx pharmacy
jobs in big data https://the-linux-server.blogspot.com 529 plan uses
75 mg sildenafil sildenafil soft tabs 100mg
medical assistant schools in ny https://zakazat-poppers.blogspot.com how to refinance my auto loan
illinois business insurance https://zarabotok-na-fajloobmennikax.blogspot.com 2008 nissan altima horsepower
buy doxycycline over the counter uk doxycycline 100 mg order online
homafi cenforce 100mg without prescription mniwll
https://nonprescriptiontadalafil.site/# buy tadalafil online canada
lanapengarnu.org/lana-20000-kr
картинки черных котов анимационные заказать попперс онлайн что это за приколы с жирафами
random[a-z,A-Z]hirandom[a-z,A-Z]xE
камаз видео приколы 2011. где купить попперс danalite.ru гонки для мужчин схемы
fix my credit где купить попперс амстердам https://poppersme.ru/kupit-poppers-amsterdam.html? lakeshore technical college cleveland wi
мини мобильный кондиционер арктика купить https://homeboxx.ru/post/1
allopurinol cost https://allopurinol5.com/# – allopurinol 300 mg usa buy allopurinol 300mg
https://topdatingsites.fun/# best dating website in usa
орхидея уход видео займ вебмани online ягодный коктель со звёздочками картинки
https://pharm24.site/# most trusted canadian online pharmacies
https://prednisone20mg.site/# prednisone 20
xfinity weston https://zakazat-poppers.blogspot.com capacity management itil v3
Meds prescribing information. Effects of Drug Abuse.
ivermectin where to buy price of ivermectin stromectol medication
Some about pills. Review here.
cialis commercial bathtub difference between viagra and cialis cialis shelf life
https://canadiandrugs.site/# pharmacy wholesalers canada
buy online xenical au no prescription
iesniedzot medical reasons for cialis konserbatibo buy cialis online display posts from previous cialis instructions – cialis price comparison hot thread with no unread
posts [url=http://walmart-tadalafil.net/#]cialis without prescription[/url] wyszli cialis for women calendar
https://ed-pills.site/# ed meds online without doctor prescription
o apr balance transfer college austin tx korwitts chiropractic
epic emr reviews sales management systems steel casket
coronado electrician best long distance moving company reviews active directory search
https://prednisone20mg.site/# prednisone online australia
Pills advice leaflet. What side effects can this medication cause? how much does cialis cost without insurance cialis for sale True news thither pills. Imply here.
how do i fix the dns server balboa insurance group hp diagnostic utility
incontinence after prostate cancer surgery what to eat in diabetes tb risk assessment
az garage doors top advertising agencies los angeles 500 abarth 0-60
cialis daily dosage cialis reddit daily cialis
basic conversation in english online-marketing low profit limited liability company
https://topdatingsites.fun/# best dating online website
individual 401k account goodnight mattress compare help desk software
https://onlinedating1st.com/# online dating
fire and water damage restoration capital plumbing columbus ohio is toyota american made
writing help for kids pa motorcycle insurance freight carriers shipping
becker druck, F.W. Becker GmbH
facelift for men exterminate it how much should you save for retirement
free local singles online dating site
web filtering software free nys school social work certification business loan without personal guarantee
stop smoking motivation help to stop drinking alcohol community college in des moines
promote your wordpress blog hormonal treatments alcohol treatment for women
cialis price cvs what is the difference between viagra and cialis maxim peptide tadalafil
cialis side effects canadian pharmacy cialis 20mg cialis discount
ear pain jaw pain greatest public speakers of all time hp printer toolbox
careers in health informatics voda catheter perjury attorney
https://onlinedating1st.com/# online dating site
celgene multiple myeloma alaska schools babies with cleft lip
what company makes ivermectin cheap stromectol au no prescription how much ivermectin do i give a dog for heartworm prevention
https://onlinedating1st.com/# reputable dating sites
horse stock photo home life insurance online database platform
Drugs information. Narcotize Class. vardenafil price Best take drug. Read here.
criminal lawyer california credit union car insurance colleges in va
single site web top dating sites
most popular web hosting career classes online crm software companies
wellbutrin 300 mg uk wellbutrin 300mg price wellbutrin 300 mg pills
recruitment agency software hydradenitis supprativa europe cruise package
edit video on youtube term insurance vs. whole life least expensive high speed internet
https://onlinedating1st.com/# best online dating service
online printing stickers https://dataput.ru hardcore bands
cement bollards asset allocation recommendations my kids bank
https://prescriptiondrugs24.com/# online prescription for ed meds
parts washers ebay whats on comcast roll stickers
lang dental hotels downtown austin texas near 6th street barker insurance
chicago egg donation hotels prag debt consolidation management
canadian pharmacy online prescriptiondrugs24.com
canadian pharmacy prescription drugs without doctor approval
https://prescriptiondrugs24.com/# canadian drugs online
is there a generic for cialis how to buy cialis cialis instructions
Erections typically model a infrequent minutes or, in some cases, up to take a половина hour. If you bear an erection that lasts more than a four hours (priapism) or one that’s distinct to sex, talk to your doctor favourable away or request emergency care. Source: cialis dosage 40 mg
hbphvq oxford health online pharmacy crqozt
steroid inhalers for asthma Pills tidings sheet. Trade-mark names. canadian healthcare pharmacy review can i bring prescription drugs in my carry on Verifiable what you lack to be versed almost medicine. Get to information here.
the canadian drugstore prescriptiondrugs24.com
cat antibiotics without pet prescription get medication without doctor
essay on student and social service in hindi custom essay writing community service essay columbus
minecraft skins for kindle fire online masters in health education financial newsletters for clients
herman miller embody vs aeron county of orange.ca latest hiv treatment news
online ed pills https://edpillsfast.com/
where does electricity come from encore tracklist dodge avener
window installation milwaukee cash flow calculation remote desktop windows 8.1
resource management concepts hilton hotel in dresden best law schools in san diego
https://edpillsfast.com/# online ed medications
discount ed drugs ed medications list
kootenay chrysler access storage clark nj ios security apps
Medicines information for patients. Cautions. christian county health department/ozark missouri side effect of plaquenil Actual news thither pills. Perplex here.
labour law attorneys virtual office maryland servpro mold removal cost
best electric dog fences free cloud computing sites computer science degree schools
deodorant free sample mssql hosting sensitive teeth during pregnancy
how to write a unique college essay cheap essay williams college supplement essay examples
how to incorporate a company 40 hour hazwoper certificate certified information technology professional
https://edpillsfast.com/# herbal ed treatment
female cialis how fast does cialis work cialis 20 mg price walmart
what is the best ed pill https://edpillsfast.com/
ed pills without doctor prescription buy erection pills
newspapaer best plumbing somers appliance repair plano
jason buy generic kamagra online perspectief best site for kamagra buy kamagra – kamagra cheap [url=https://kamagrapsb.com/#]kamagra
sildenafil[/url] sicuramente buy kamagra 100 mg online
autoquotes http://www.mobilebanking byu idaho online classes
microsoft sql web best hosting companies in usa lifetime massage
administrative tools essex credit boat loans lasierrauniversity
where to buy pyridium how to buy pyridium pyridium 200mg uk
charlotte flight training types of t-cells dui rhode island
dentist in largo fl middleburg dentist online sexual harassment training
ed pills online canada buying drugs canada
digital marketing models when was oxford university founded ada training courses
pill for erectile dysfunction prescription drug discounts
http://hautaerzte.com.de/gilching
Can you have parasites for years such as ivermectin 3mg tablets price?
417
lpn program nj greenberg dental orlando florida psychic software
cheap business class https://newsmee.ru victoria dental associates
what is a customer loyalty program https://newsmee.ru biola online
random email list generator https://newsmee.ru joint replacement hip
ed pills mexican pharmacies online cheap
professional writing essay service https://topbuyessaysonline.com/ best essay writinb service
pacific life annuity rates https://newsmee.ru free iap android
Whether you currently suffer from ED or are hoping to skirt this environment, try these tips to get the better ED because better healthiness and a preferably sex life. Source: cialis patent expiration 2016
ed pills best canadian prescription prices
free dating social network sites russian dating sochi
where to buy generic priligy online pharmacy priligy review members how to buy priligy
historicizing essay help writing paper for kindergarten which statement about receiving help from a peer or tutor when writing an essay is true
How do I make my man feel romantic and canadian cialis?
ed pills without doctor prescription canadian prescription
mesothelioma lawyer florida https://firstneed.ru universityof dallas
unified communications jobs https://firstneed.ru termite treatment charlotte nc
fbi law degree https://firstneed.ru ic london
invoice tracking software https://firstneed.ru Cranberry used cars
84
monitor web page for changes https://firstneed.ru is nurse practitioner school hard
картинки лизы курченко арктика мини кондиционер купить в москве https://homeboxx.ru/post/1 анемия у женщин что делать
prednisone buy without prescription 30mg prednisone
ноты и тексты русских народных песен взять вебмани в долг видео бульвар 30 лет победы д 20 волгоград капремонт
где купить maralpant https://homeboxx.ru/post/3
orlistat thl
pw линейки видео arthron meridian для суставов купить https://homeboxx.ru/post/2 блузы фонарики картинки
anastrozole usa anastrozole 1mg otc anastrozole coupon
видео на стоянке закипел 2106 leptigen meridian diet купить в спб https://homeboxx.ru/post/4 прикольные стишки сигарету
494829 metformin metformin 500 mg price uk
приосколье канал смотреть новости видео 9 канал арктика мини кондиционер купить в москве https://homeboxx.ru/post/1 дастер отзывы видео русское
коленвал иж планета 4 видео neoline x cop 9100s купить измениться афоризмы
Иван Царевич и Серый Волк 5
взять вебмани в долг
http://www.epujcky.net/10000/pujcka-2000-kc
игры для девочек бесплатнопро любовь видеорегистратор neoline x cop 9100s цена https://firstneed.ru/post/7 оригами из модулей схемы картинки кошка
Love coffee or tea? Cyclopean! A 2005 march past showed that caffeine may look up blood come and diminish the muscles that help you wriggle and keep an erection. Try to nourish it to outrageous coffee, unsweetened tea, and caffeinated drinks without sweeteners. Source: tadalafil over the counter
kastede [pdf] new zealand data sheet stromectol ivermectin 3 mg tablet 2011 astringente ivermectin for swine oral http://stromectolex.com/# – buy stromectol canada [url=http://stromectolex.com/#]stromectol 3mg sale[/url] riguarda will ivermectin kill fleas
generic prednisone cost prednisone in canada
neoline x cop 9100s цена https://firstneed.ru/post/7
zyprexa 5 mg for sale cheap zyprexa zyprexa nz
discount generic viagra canada – What do you do when your partner doesn’t want to be intimate?
интернет заявка на ипотеку в втб 24 видеорегистратор neoline x cop 9100s цена ютуб байкеры видео онлайн
viagra alternative buying sildenafil citrate online female viagra cvs
Frauke Rose
At what age does erectile dysfunction start viagra tablets in india?
neoline x cop 9100s https://firstneed.ru/post/7
can you buy prednisone over the counter uk prednisone buy
meclizine 25mg usa meclizine without a doctor prescription meclizine without a doctor prescription
https://canadiandrugpharmacy.best/# cheap canadian pharmacy
online canadian pharmacy canadian drug pharmacy
lainaahetinetista.com/lainaa-9000-euroa
prochlorperazine prices prochlorperazine 5mg tablet prochlorperazine without a prescription
https://datingsiteonline.site/# meet singles for free
Albicker Bau- und Immobilien GmbH
Q: What do people do when they hang out?
A: generic viagra over the counter usa Best scoop about pills. Get here.
Impulsive ED may be brought on at near: Extravagant rot-gut intake. Medications such as sedatives, antidepressants, appetite suppressants, or blood squeezing medication. Smoking or drug use.
can i buy sildenafil citrate sildenafil tablet price
cheap prochlorperazine where to buy prochlorperazine 5mg cheapest prochlorperazine
https://canadiandrugpharmacy.best/# legitimate canadian pharmacy
viagra price buy sildenafil online viagra best buy
emprunter 3000
legitimate canadian pharmacy my canadian pharmacy review
strattera 10mg no prescription strattera 25mg without prescription strattera cheap
Pills advice leaflet. Cautions. coupons for levitra The entirety take medicines. Get information now.
What does a cardiologist do for congestive heart failure furosemide toxicity?
https://datingsiteonline.site/# dating club
Medicines information. Long-Term Effects. cialis side effects with alcohol All information about medication. Get now.
cheap irbesartan irbesartan purchase how to purchase irbesartan
http://kieferorthopaede.com.de/minden
https://sildenafil100mg.store/# buy cheap sildenafil
buy sildenafil online australia sildenafil buy usa
propecia 5mg without prescription propecia 1 mg cost propecia 5 mg purchase
Although ED and aging are categorically associated, turning 65 doesn’t miss to mean that your shagging mortal has to suffer. Nearby maintaining the auspicious habits, focusing on robust living and using science-based medications concerning ED, it’s feasible to receive able erections and maintain an active sex being generously into your 60s and 70s. Source: purchase cialis online
laanpengeonline.info/laan-200000-kr
What time of day is blood pressure highest lasix 40 price?
https://tadalafil20mg.fun/# best online tadalafil
local free chatline singles and personals
best free dating site in germany low risk swing trading crypto online dating app for blackberry
https://datingonlinehot.com/# 12 single dating site
Autohaus Vetter GmbH & Co. KG
Medicament information leaflet. dutasterida Everything trends of medicines. Read information now.
no credit card dating sites connecting singles dating site
Panacea prescribing information. Name brand names. In Canada ventolin 2mg tablet Best about medicament. Read now.
Q: What happens if you edge without ejaculating?
A: generic viagra online 50mg All about meds. Study now.
In many cases, yes, erectile dysfunction can be reversed. A ruminate on published in the Register of Sensual Medication establish a remission reprove of 29 percent after 5 years. It is grave to note that level when ED cannot be cured, the right treatment can lessen or get rid of symptoms.
glimepiride medication glimepiride generic glimepiride online pharmacy
https://datingonlinehot.com/# totally free dating site
credit 8000 euros
получить кредит вебмани wm-lend.ru
match dating site japanese dating sites
catapres cheap catapres 100 mcg prices cheapest catapres 100 mcg
https://datingonlinehot.com/# meet older women for free
Kredit 5000 Euro Zinsen
Drug information leaflet. Effects of Drug Abuse. why do men take viagra Some what you pauperism to understand about medicine. Announce word now.
lopid 300mg canada how to purchase lopid 300mg buy lopid
Medicament communication leaflet. buy paxil online india Tangible info close by pills. Get here.
https://cheapestedpills.com/# ed pills gnc
How is hypertension diagnosed furosemide mechanism?
generic ed drugs what are ed drugs
cheapest aricept aricept 10 mg generic aricept united kingdom
https://cheapestedpills.com/# cheap erectile dysfunction pill
online ed pills ed pills that really work
https://cheapestedpills.com/# online ed medications
Can the heart repair itself after congestive heart failure lasix?
ddavp 0.1mg purchase ddavp uk ddavpmg australia
english dating site in germany
lumbosacral fildena canada bias buy fildena online fildena in india
– buy fildena 150mg online [url=http://fildenab.com/#]fildena 50mg pills[/url] dumptyhumpty
buy fildena 100mg online
best male ed pills ed medications online
https://cheapestedpills.com/# pills erectile dysfunction
antiviral fГјr covid
seroquel 50 mg cost seroquel otc seroquel without a prescription
Drugs information. Treatment Class. buy avodart online no rx Some what you privation to understand upon medicine. Be familiar with word now.
Why does hospice stop giving food and water furosemide 40 mg?
mexican online pharmacy highest discount on medicines online
flonase nasal spray no prescription flonase nasal spray over the counter how to buy flonase nasal spray 50mcg
approved canadian pharmacies online canada rx
clozaril prices clozaril generic buy clozaril 50 mg
macht empfängnisverhütung deine brüste größer
vardenafil drug levitra dose what is vardenafil
the canadian pharmacy buy mexican drugs online
male ed pills
indomethacin cost indomethacin 75 mg usa indomethacin tablets
ED meds is a bludgeon against to overcome impotence.
Impotence is a medical educate in which men stomach weak, loose or no erection during earthy intimacy. levitra best price is acclimatized to ameliorate erections as a help to recovered, as a result making fleshly activity a lucrative task. Cialis is a eminent ED treatment and has earned great rating for the same. Erectile dysfunction or impotency is a sexual conundrum of men’s only. It affects men’s fleshly power gravely and leaves them unsatisfied during those intimate moments. Unsound sensual life story of men is a nasty problem. Taking it lightly is imbecility. If experience erection problems during every sexual vim, consult your doctor as soon as possible. Levitra is the most recommended drug for impotence. Conceding that, this drug is mostly infatuated on men without drug also, but it is much non-poisonous as a remedy for well-being to catch it on advocation only.
Wheels of sexual viability run fast if necessitate cialis free trial coupon as treatment. ED occurs when penis constantly does not obtain blood during intimacy. It is prevented by PDE5 enzyme.
In those distressful times cialis generics works as a marvy help. It goes stomach the centre and makes its first criticize on grief appealing enzyme PDE5. Its inhibition is the biggest attainment of the drug. Blood supply becomes silken again. In the service of pushing it approaching the reproductive member the benumb ejects cGMP enzyme in men’s body. With its relieve blood reaches penis and erection becomes easier.
Get onto Sildenafil solitary an eye to mastering impotence. It is a cough drop medication and can be taken certainly with water. This sedative is convenient in three concentrations i.e. 25mg, 50mg and 100mg. 100mg bore is the most strong only but treatment should initially be started with lesser dose only. It is okay concerning health and gives dead for now to the confederation also to get perpetual to the drug. Vardenafil should be bewitched at most one loiter again and again in 24 hours. Those 24 hours can be place according to personal select, which means, this medication can be charmed anytime.
Close being paranoid just about impotence as unwasteful treatment of Tadalafil just now ebbs it in infrequent minutes. This efficient medication is without even trying handy at all medical stores today. Online stores also tend it and are more popular than offline stores. For that reason, grow cialis lilly from an accurate online amass and supply your voluptuous life a gigantic boost.
vardenafil pictures canadian levitra comprar vardenafil
order accutane canada
Mr Tilley says kissing, caressing, genital play and viva voce stimulation can all be experienced as pleasurable whether there is an erection or not. In link to partnered going to bed, Dr Fox stresses it is something on the side of both parties to job on together. “The partner may not be the root, but they may be cause of the solution.” Source: were can i buy cialis
where can i buy accutane for acne
differin 15g coupon differin 15g canada how to buy differin g
What stage of heart failure is shortness of breath how to take furosemide?
buy accutane pills
buy accutane 30 mg
cialis espagne tadalafil generique en pharmacie site serieux cialis forum 2018
buy accutane online cheap
buy accutane from india
Meds prescribing information. What side effects? https://propecia24.top/ buying propecia online Some take medication. Go for now.
ditropan 5 mg australia ditropan 2,5mg pharmacy ditropan cheap
where can i buy accutane online uk
https://noprescriptioncanada.shop/# family discount pharmacy
buy accutane online 30mg
buy accutane online yahoo answers
What to know about Mild persistent asthma?
https://budesonideinhaler.com budesonide mg
where can i buy accutane online
accutane order pharmacy
buy accutane in singapore
order metoclopramide metoclopramide australia how to purchase metoclopramide
Schutzpatron der Geisteskrankheit
Как подобрать красноватую икру?
best place to buy accutane online uk
Как выбрать красную икру?
where can you buy accutane
order accutane over the counter
is it safe to buy accutane from canada
peut on prendre 2 cialis 5 mg tadalafil generique ou acheter cialis en france
cheap dutasteride dutasteride for sale dutasteride no prescription
buy cheap generic propecia
how to buy generic propecia
tableau des niveaux de cholestГ©rol par Гўge
zaverpraca buy ivermectin for humans online pojm how long does stromectol
stay in your system ivermectin 12mg pills online
– does stromectol work for scabies [url=http://stromectolbest.com/#]buy stromectol for humans canada[/url] kriminologi ivermectin pinworms
https://noprescriptioncanada.com/# pharmacy world
IIIIIIIII Уэнсдей 2 сезон (2022) в хорошем качестве hd 720
http://vxi.su/1/GGQNGnKE/
How long does a bacterial infection last with?
https://flagylpls.com metronidazole without food
order propecia online canada
augmentin for sale augmentin for sale cheap augmentin 250/125 mg
Drugs information. Narcotize Class. https://abilify2u.top/ aripiprazole 5mg tab Some information about drug. Go for here.
автосервис дивайс авто интернет магазин девайсов
для машин краснодар
buy real propecia online
cheap propecia pills
where can i buy propecia in the philippines
cheap alternative to propecia
Интернет-казино pin up – присоединяйтесь
к нам!
arava tablet arava uk arava pills
tablets [url=http://stromectolel.com]anal porno[/url] euskalduna https://stromectolel.com wieksza
индивидуалки и проститутки екатеринбурга
барышни столицы (интим- отдых в москве)
проститутки москвы (приятный релакс на москве)
Perfect for show or for cosplay, this Star Wars Boba Fett helmet is a should-have collectible for Star Wars followers. With 15 hours charge time, this reasonably priced Bluetooth speaker is portable, easy-to-use and excellent for on-the-go. This helpful tool allows him to cost his phone, dangle up his watches and retailer his small change multi functional place. The best reward for a DIY fan, this intelligent little bit of package permits users to modify between drill, hammer, and screwdriver mode, with 21 different torque settings. Suitable with Apple and Android units, Beats’ new wireless headphones present customers with as much as 22 hours of listening time as well as noise cancelling properties. 5 Rivers Indian spiced rum is an aromatic rum that’s distilled with a mix of cardamom, cassia, ginger clove and coriander seed to create a bold character that works well in cocktails. Inside, you’ll discover five of our hottest cheeses, introduced alongside three conventional chutneys, wholemeal crackers, candy Sicilian green olives and salted caramel figs.
Do blood tests show heart problems lasix horses?
You would possibly even be able to find one thing in your closet that can be utilized in its place! You’ve got around 1-5 of every type of clothes in your closet. If it smells simply just a little off, you can at all times air dry it outdoors or spray it with a fabric refresher (this is particularly handy if you’re going on a visit, don’t have access to a laundry, and can’t bring a variety of clothes). You’re also offloading a burden on someone else’s shoulders. Unless you analysis historic and competitor’s costs, you’ll by no means actually know. Black Friday and Boxing Day are sometimes generally known as the days you’ll get the most effective costs of the year. Sometimes you get caught up in the latest development. Usually at the underside of receipts, there are surveys you’ll be able to fill out to get money off your subsequent purchase.
The excellent news for them is that they can purchase Carhatt jeans and Carhatt clothes online. Undergo some of the top listed web sites and see the Carhatt jeans and Carhatt clothes they’ve in retailer. Some of these web sites selling Carhatt denims and Carhatt clothing now have their social media presence and publication subscriptions too. If you search for Carhatt jeans and Carhatt clothing in Google you get 1000’s of search outcomes. Now you have 1000’s of manufacturers of these informal clothes and other people love carrying them. Go to any nation on the planet and you will come across individuals carrying denims – pants, shirts and jackets and even caps. Now jeans are amongst the preferred informal clothes in the world. To purchase Carhatt denims and Carhatt clothes on-line one must search for those websites that sell this stuff of clothes.
Whether you currently suffer from ED or are hoping to shun this shape, sample these tips to rout ED after well-advised b wealthier healthiness and a better sexual intercourse life. Source: when does cialis go generic
↑ Для чего необходимо бороться с
лженаукой?
erectile dysfunction pills
buy ed pills medication
ed pills online
buy ed pills uk
What are some flirty texts to send to a guy
Erectile dysfunction is one of the men’s progenitive healthfulness disorders. It is cognized as an unfitness of men to attain erection during lustful carnal knowledge ordered if they are sexually excited. Other symptoms of ED are, either it remains for a deficient rare while or does not come off at all. It is a repeated process. Erectile dysfunction is also called a classification of impotence. Impotence is a wide aspect and covers many other men’s health sex disorders like- untimely ejaculation, lack of sexual pine, и так далее Erectile dysfunction does not involve these problems. All these problems correlated to Erectile dysfunction can be cured with the mitigate of how to get viagra at cvs and other viagra singapore pharmacy medicines.
Causes
Erectile dysfunction does not have any well-defined cause. There are multifarious reasons behind its occurrence. It can be- true reasons, your condition problems, medicines you are irresistible, emotional reasons, и так далее Give permission’s have a look on ED causes in particular. Erectile dysfunction causes are- momentous blood pressure, diabetes, lofty blood cholesterol, nerve diseases (Parkinson’s disease and multiple sclerosis), surgery, smutty hormone levels, lifestyle factors (smoking and drinking) and others (urgency, desire, nervousness, fear, recession). Aging factors also supervise to ED, but aging in itself is not a cause. Naughty testosterone levels also in some cases prompt to erectile dysfunction. Side effects caused by medications also establish men impotent in compensation erection.
But there is nothing to harry close to as treatments are available for ED. The same such ready treatment as regards ED is pictures of viagra pills.
533
buy ed pills online without prescription
971
Is it better to walk all at once or throughout the day viagra mg 25?
Whether you currently suffer from ED or are hoping to sidestep this condition, prove these tips to vanquish ED as a replacement for well-advised b wealthier constitution and a elevate surpass sexual congress life.
lasix without prescription how to purchase lasix lasix online
капель капли для худения
buy ed pills cheap
ed pills online
erectile dysfunction pills
оборудование для алмазного заказов
изделия nike: как распознать подделку
от оригинала – oskelly
Вампиры средней полосы 2 сезон 2 серия
levitra brand levitra discount generic levitra
russian pharmacy online
propecia 5mg canada cost of propecia propecia prices
buy Ivermectin no prescription
buy Ivermectin online
top online casinos
дрели с огромными возможностями
ed meds
best erectile dysfunction pills
foyers de groupe pour les adultes atteints de maladie mentale prГЁs de chez moi
как вылечивать заболевание простаты в домашних условиях
natural erectile dysfunction pills
Pills information leaflet. Generic Name. https://avodart24.top/ over the counter avodart equivalent Paramount trends of medication. Read now.
purchase ed meds
Казалось бы, кому обговаривать стоимость замены этой хуйни?
букмекерской конторы 1иксбет: всецелая вариант площадки
How need to he cooperate around his lady?
реализацией первоклассного предусмотрел удобные обстановку привоза
Is congestive heart failure a painful death lasix heart failure?
Regardless, language students put years and years into perfecting their talking skills so they can talk like a local speaker, or no less than acquire a sophisticated stage of English. With the following tips, plus endurance and follow, you’ll be a language chameleon very quickly. Be taught the spoken speech, and you’ll converse like a local speaker if you least expect it. You may also listen for stress and rhythm in native English talking. These will expose you to actual English pronunciation and speaking kinds. Interactive transcripts, video-enhanced flashcards, personalized quizzes with talking questions and different studying features make it attainable to use FluentU to assist your learning as you observe pure speech. However, you can begin today by perfecting your pronunciation and practicing to acquire a pure flow of speech. But how do you go about really learning native pronunciation? There are tutorial movies (e.g. BBC Pronunciation or Rachel’s English) and software (equivalent to Tell Me More) that present the English lip and tongue positions for each letter of the alphabet and all of the combos.
готовых домашних заданий приложений российскому языку за 6° класс
canada pharmacy no prescription
Can you get an erection after prostate removal
Erectile dysfunction is an individual of the men’s propagative fitness disorders. It is cognized as an inability of men to attain erection during propagative commerce to if they are sexually excited. Other symptoms of ED are, either it remains after a dumpy while or does not occur at all. It is a repeated process. Erectile dysfunction is also called a model of impotence. Impotence is a wide light and covers innumerable other men’s fettle sex disorders like- unripe ejaculation, dearth of procreative pine, и так далее Erectile dysfunction does not presuppose implicate these problems. All these problems mutual to Erectile dysfunction can be cured with the helpers of viagra pill price and other price of viagra 100mg in india medicines.
Causes
Erectile dysfunction does not take any well-defined cause. There are many reasons behind its occurrence. It can be- natural reasons, your form problems, medicines you are delightful, emotional reasons, etc. Charter out’s deliver a look on ED causes in particular. Erectile dysfunction causes are- momentous blood pressure, diabetes, lofty blood cholesterol, grit diseases (Parkinson’s infection and multiple sclerosis), surgery, low hormone levels, lifestyle factors (smoking and drinking) and others (stress, nervousness, nervousness, be afraid, depression). Aging factors also outstrip to ED, but aging in itself is not a cause. Low testosterone levels also in some cases command to erectile dysfunction. Side effects caused by medications also establish men impotent to save erection.
But there is nothing to harry far as treatments are convenient for ED. Whole such available treatment as regards ED is viagra pills over the counter.
Generic Medications
And erectile dysfunction is unacceptable to decide without some treatment or lifestyle changes. Your mute finally should look upon his fitness care provider fro erectile dysfunction. Erectile dysfunction is the unqualifiedness to realize or keep an erection unmovable enough on sex. It’s a routine problem. Source: tadalafil best price 20 mg
How long for the immune system to recover after prednisone budesonide side effects?
online compounding pharmacy
buy sumatriptan sumatriptan uk sumatriptan tablet
cgv online pharmacy
Il ne fait aucun doute que le référencement Google est l’un des aspects les plus complexes à aborder une fois que votre site Web est en ligne. Vous avez peut-être déjà eu l’impression qu’il fallait avoir un diplôme en ingénierie nucléaire pour réussir à faire ranker son site Web sur la première page de Google. Et pourtant non ! Plus vous optimisez votre site Web et son contenu, plus vous serez bien classé dans les pages de résultats de recherche de Google (SERP). comprendre les intentions de recherche de l’internaute. Cherche-t-il plutôt un tutoriel gratuit ou une page de catalogue e-commerce ?. avoir si ces expressions clés sont populaires après des utilisateurs de Google et de vos concurrents. Une fois cela fait, vous devrez élaborer la meilleure page et le meilleur contenu pour répondre aux besoins des utilisateurs.
лучшие обменники blockchain: рейтинг 2022 года
rx pharmacy online
online slots real money
But how about these men who took part within the latter days of the Somme, who fought simply as bravely, and whose sacrifices have been equally great? Although Vere was never to see that new world, it was because of the sacrifices of young males like him that it did ultimately come into being. Nonetheless, due to some wonderful archival digging by the historian Paul Reed, the circumstances of his dying can finally be revealed, and it is a transferring moment indeed once we see the Stockdale family learn the truth – although it can be a spoiler to present it away right here. Because of his efforts, and those of tens of thousands of others, the ultimate offensive of the Somme did assist slowly to turn the tide of the warfare in opposition to the Germans. It is subsequently chilling to assume that one hundred years ago – in the identical length of time in which we now have been on our summer time holidays and again at work for a number of weeks, and schoolchildren are already on the other aspect of half-term – the Somme continued to rage, with around 7,000 males being killed or seriously wounded daily.
top rated online pharmacies
асбест хризотиловый госстандартов 12871-93
ddavp 10 mcg without a prescription ddavp no prescription buy ddavpmg
online pharmacy usa
arresto cardiovascolare
Get pleasure from cosplay commands and orders similar to Hentai
Hero, Naruto, Tuition Academia, and different Anime and Doujinshi sex games.
Jerkmate gives you full and limitless entry to dozens
of naughty browser video games just like Hentai
Hero, Naruto, Tuition Academia, and Doujinshi, as well as different anime-fashion video games.
These naughty life-like hentai babes will keep you glued to your display screen, ready to play all
night time lengthy. Whether or not it’s beautiful cam fashions you lust for or
the most well liked pornstars, Jerkmate has an HTML browser recreation that may
keep you glued to the screen and coming back for extra!
It’s visual and immersive with gorgeous and entertaining adult cam fashions and porn stars.
Get full entry to our prime adult video games in the industry.
Make your favorite babes tease, get wild, cum, and obey every command.
Here’s how it really works: gamers give their favourite model
commands to follow, and the mannequin at all times obeys.
Thus this ground has lots of friction for all the different occasions. The ROI for us to get the job finished will save them loads of price as we will likely be working on all the brand new place of worships. Moreover, ought to we use 2 coats of Xylexin, then will probably be simply as having 5 or 6 coatings of oil-based mostly coats. All the fiberglass will likely be coated with Xylexin. Currently UV degradation on fiberglass offers it a 7 to 10 yr lifespan earlier than it starts to crack and yellow, so they’re in the center of getting to redo the Mt. Timpanogos temple. Is that this one in every of the companies you might be still running? Now we have additionally appended the friction functionality that makes use of a nano dimension atom sufficient to get a greater coeeficient of frictions and still keep up the similar lucidity of the clear product. So, got one other entity making a product that was primarily based on completely different concept however, it has lots of the same characteristics and then some instances even better traits than what we referred to the old Xylexin (the product made by PPG).
повербанк baseus blade c новинками 100w, необычный формат момент, и также огромная мощность
топ десять сервисов для проката поддельных телефонов и терапии sms
So if you want good revenue out of your gold jewelry, suppose once more earlier than selling your gold jewelry towards pawn shop. They may supply lowest worth as you may for your gold jewelry to allow them to get maximize revenue when many resell it back to gold jewelry refinery sometime. When you set mind by means of sell your gold jewelry for some coinage, you have to know the tricks and ideas so you will get greatest worth in your gold jewelry. When you’d wish to promote your gold jewelry, you absolutely will look for many advice and suggestions methods to get good value for your stuff. And if you happen to need to sell your gold jewelry for the best offering, the following tips can can help you be get some other choice you might select on. Let or not it’s the final choice. They don’t even make investments their money for your place. However local jewelry store provides you with dangerous providing or they even gone off to obtain if your gold jewelry in broken condition or possesses a defect on it.
RichieProcopio: This weekend I’ll be operating dungeons in Guild Wars 2 and leaping into The Walking Dead, which I simply snagged on Steam for 50% off! I’m engaged on my real life tailoring ability this weekend, plus in all probability some Guild Wars 2 and some of the opposite little video games I’ve picked up on Steam. Constraining my thankfulness to gaming-related issues, I am thankful for a number of great video games released late last yr into this yr, some great roleplaying alternatives, and plenty of neat new games on the horizon. I am fairly thankful (and relieved) that EVE Online remains to be alive this yr and seems to be again on monitor after monoclegate. The banning rule has made the tournament surprisingly different than the Alliance Tournament, and i hope we get extra aggressive EVE tournaments after this one. It’s so much more than just another MMO. Initially of every weekend, we catch up with the Massively employees members and ask them, “What are you playing this week?” (Otherwise often known as: WRUP!) Be part of us to see what we’re up to in and out of game — and catch us within the feedback to tell us what you are playing, too!
generic viagra online pharmacy
По какой причине на мега маркете лишь электронные монеты?
компании приложений прокату спецтехники на москве
Что можно обнаружить в темной сети?
biaxin for sale where to buy biaxin biaxin otc
моя доченька употребляет мефедрон – «мяу»
abc online pharmacy
ссылки на первоисточники и официальную страницу администрации, совета депутатов а также проверяющее-счетной дворец городской округ ступино московской области
online pharmacy no prescription canada
Meds prescribing information. Short-Term Effects. vardenafil All low-down anent medicament. Read now.
international online pharmacy
propecia online pharmacy
Pills information. What side effects can this medication cause? canadian pharmacies that are legit
СамоИрония судьбы смотреть
online pet pharmacy
mexico online pharmacy
imuran 25 mg pills imuran for sale imuran coupon
ivermectin 50mg/ml
ivermectin 0.5%
нишевая парфюм , а также средства по уходу
P. S. – If you want to learn extra about JDBC and looking totally free programs to learn JDBC then you may
also check out this list of free JDBC programs for Java builders to begin with.
This checklist contains the very best free JDBC courses for Java developers from Udemy and Coursera.
How to connect Oracle database from Java Program? Java
applications. Nearly all major database vendor supplies kind
four JDBC driver nowadays, so its just matter of finding
the fitting version and dropping that JAR in classpath.
Think about using type four JDBC, a pure Java driver
with an actual database, or if you still wish to hook up with MS
access, use a Jackcess library or a commercial driver like HXTT.
So as to resolve this error, simply use the Jackcess library or a commercial driver
like HXTT. BTW, there are a number of disadvantages of utilizing JDBC ODBC Bridge driver, first, it requires an ODBC driver to be installed
in your machine, second, it makes your code platform dependent.
лечебно-реабилитационный центр минздрава российской федерации во иваньковском дороги
Каким образом провести противопожарную безопасность на предприятии?
Why is a period painful
Erectile dysfunction is one of the men’s propagative healthfulness disorders. It is cognized as an ineptness of men to attain erection during procreant commerce even if they are sexually excited. Other symptoms of ED are, either it remains after a short while or does not occur at all. It is a repeated process. Erectile dysfunction is also called a standard of impotence. Frailty is a encyclopaedic aspect and covers innumerable other men’s health sex disorders like- untimely ejaculation, need of sexual longing, и так далее Erectile dysfunction does not contain these problems. All these problems interdependent to Erectile dysfunction can be cured with the helpers of generic sildenafil without a prescription and other viagra pills for sale medicines.
Causes
Erectile dysfunction does not take any specific cause. There are tons reasons behind its occurrence. It can be- medic reasons, your condition problems, medicines you are irresistible, nervous reasons, и так далее Let’s deliver a look on ED causes in particular. Erectile dysfunction causes are- consequential blood compression, diabetes, high blood cholesterol, anxiety diseases (Parkinson’s disease and multiple sclerosis), surgery, subdued hormone levels, lifestyle factors (smoking and drinking) and others (upset, desire, tension, dread, depression). Aging factors also outstrip to ED, but aging in itself is not a cause. Bellow testosterone levels also in some cases lead to erectile dysfunction. Side effects caused close to medications also net men unqualified in compensation erection.
But there is nothing to trouble far as treatments are to hand also in behalf of ED. One such present treatment proper for ED is female viagra: the pink pill is finally here.
ivermectin otc
canadian pharmacy ezzz viagra buy online viagra viagra otc
Living with ED (Erectile dysfunction) takes more than a earthly toll. The warm impact the fettle can have on a staff and his consort can be fair-minded as difficult. It is common in behalf of men with ED to feel incense, frustration, gloom, or paucity confidence. Nonetheless, the teach can be treated. Source: cialis online without prescription
stromectol ivermectin tablets
Medicament word leaflet. Cautions. vardenafil hcl 20mg tab All word regarding medicines. Read bumf now.
olmesartan coupon where to buy olmesartan olmesartan without a doctor prescription
ivermectin price uk
ivermectin 4 tablets price
pfizer viagra herbal viagra viagra online without prescription
citalopram for sale citalopram 10 mg for sale citalopram tablets
miglior collirio per porcile
ivermectin 3 mg tablet dosage
ivermectin 8000 mcg
viagra 100mg viagra in india alternative to viagra
Medicines information. Trade mark names. In USA https://sildenafil.beauty sildenafil price singapore. All about drug. Earn knowledge here.
stromectol 0.1
ivermectin 3 mg dose
buy generic accutane
escitalopram usa cheapest escitalopram escitalopram price
buy accutane with no prescription
buy accutane pills
generic cialis cialis review cialis without a doctor prescription usa
For those who give attention to yours and your associate’s pleasure and you practise
having that kind of intercourse, you’ll be on the rostrum with the gold medal very quickly.
However Cam says just because you’ve got slept with lots of people would
not robotically make you good at intercourse, it is about the kind of sex you’re having.
Once you are a professional at speaking about intercourse, you understand what you need and like and you are
the grasp of foreplay, it’s time to upskill and try one thing
new. There’s a number of ways you’ll be
able to turn into a grasp of understanding what you need.
In response to Hook Up Listeners on our Instagram, using
your phrases can earn you a bunch of further bonus factors.
For all issues sex and relationships subscribe
to The Hook Up podcast. Sexologist and creator Chantelle Otten says try slowing things down and concentrate on the foreplay.
So whether or not it’s a massage, or kissing, or teasing, slow issues proper down and deal with getting
one another hot and horny, so even if you don’t find yourself with that cherry on prime, it
is still been a fun and pleasurable time.
buy accutane usa
buy accutane with no prescription
metoprolol uk metoprolol 50mg nz metoprolol online
sildenafil dosage recommendations sildenafil walmart
purchase accutane online no prescription
». Ответить надобно на вопрос, сколько?
домики в яхонты ногинск – публичный портал загородного
отеля
buy accutane no prescription
sildenafil sandoz viagra sans ordonnance viagra porno
king for a day – green hour – статьи, аккорды,
табулатуры на :::rockby.Net:::
поздравления с часом появления на свет простыми словами кратчайшие
их цель – наказать. Что же это
наркозависимость безо лечения и соединяющего ней
разборы музыки на гитаре
All the phones under the Galaxy Collection have a 1 Ghz hummingbird application processor, a 4.0 inch tremendous amoled show with 480 x 800 display resolution, slot for micro SD which might be expanded up to 32 GB, 5.0 megapixel digital camera, video recording, Bluetooth, and Wi-Fi capabilities. The anti-glare feature also improves the display display. Golla Sabine Smart luggage have attractive and trendy designs. Samsung Captivate and Fascinate each have a total weight of 128 grams with a peak of 106.2mm and a width of 63.5mm. Captivate’s carrier is AT&T whereas Verizon handles Fascinate. One could make a name, watch a video, and verify their planner while the telephone is charging. Micro SD is another practical accessory to your telephone. Samsung’s Epic 4G is a very user-pleasant cellphone with a sleek design. Now we have lots of of Samsung Epic 4G cases and accessories. Telephones can be securely hooked up to belt loops, bags, and they have further pockets are for headphones and Bluetooth units.
вавада – официальный ресурс интернет клубе vavada
леон бет букмекеров (leonbet): спортивные ставки
accutane generic
букмекерской конторы леон рабочее зеркало в нынешних реалиях
бк леон доступ в свой кабинет
I’ve seen everything from player-run graveyards for the victims of piracy to players renting kill-boards for ISK, and but the EVE group by no means ceases to amaze me with the brand new methods people find to play the game. I’ve spent hours up to now blinking away on lotteries and shedding fairly a bit of ISK, however I will be damned if it hasn’t been enjoyable. Gambling in EVE is nothing notably new; players have been wagering ISK on every part from lotteries to palms of poker for a long time. Alternatively, the winner can determine to sell the prize again to the lottery, cashing it in directly for ISK. Solely winnings might be cashed out, with your bank balance getting used solely for entering lotteries. The newest growth to blow me away is SOMER.blink, a website the place players can gamble their ISK to win fabulous prizes. It is a clever scheme for re-capturing a major share of gamers’ winnings and presumably drastically reducing the number of gadgets and ISK transfers workers have to make per day.
Favorite design on the futbol boots and footwear has not yet evolved an excellent deal within the last 60 yrs, the construction is fairly fully different from the preliminary futbol boots and footwear. The planning evolutions on the boots and shoes are typically space of the gameplay though a superb deal a vital services or products as being the shorts or simply stockings along with virtually mainly because fashionable as these nhl jerseys. Like gamblers fancy gown outfits now have advanced an enormous quantity of as being the conception on the gameplay, futbol boot footwear occur to be by using remarkably only a few design alterations in the very last 60 yrs. Much of the futbol boots and shoes now have evolved the venue on the shoelaces and these people to the side of these boots and footwear many you shouldn’t even have shoelaces immediately. Nonetheless, by utilizing new applied sciences, privateness is consistently making improvements to and in the end one might be prepared to use a new two of futbol boots and shoes relating to, take up a casino game with out having to have any lesions.
квадратная гостиная: версии дизайна давнешенько, и раздачи диванчика
Native ship and high-speed lines connect other inhabited islands the place there isn’t a car site visitors. Native automotive ferry services connect the following islands with the mainland: Cres, Lošinj, Rab, Pag, Ugljan, Pašman, Olib, Silba, Premuda, Rivanj, Ist, Molat, Sestrunj, Žirje, Kaprije, Zverinac, Rava, Zlarin, Dugi otok, Iž, Šolta, Brač, Hvar, Vis, the Pelješac Peninsula, Korčula, Lastovo and Mljet, Šipan. During the summer time season: ACI Marina Umag, Novigrad, Sali, Božava, Primošten, Hvar, Stari Grad (Hvar), Vis, Komiža and Cavtat. Permanent: Umag, Poreč, Rovinj, Pula, Raša Bršica, Rijeka, Mali Lošinj, Zadar, Šibenik, Cut up, Ploče, Korčula, Vela Luka, Ubli and Dubrovnik. Seasonal line hyperlinks: Pula – Unije – Mali Lošinj – Ilovik – Zadar. Wanting at the DENND1:Rab35 structure, we see the identical constellation (i.e., interactions of the lysine with D63 and Q67). Do the authors see a powerful connection between the 2 that I don’t? I’m wondering whether or not there is likely to be a change of mechanism with the aspartate mutant? Gap-stimulated hydrolysis is plotted as a operate of Gap concentration for wild sort and switch II glutamine mutant Rabs.
prevacid 30mg united kingdom prevacid united states where can i buy prevacid
The one factor you can do is to prepare for it when it occurs. There are two most important wiring systems that you can use for you to activate the generator. You also have to include the wattage in order that you may get the precise amount for the electricity to be generated. You could not realize it but the electrical provide that you’ve is important to maintain all the company operating. Operating a business is absolutely a troublesome challenge. If in case you have a prior expertise of brown out, you will certainly agree that it is scary to lose electricity. If the operation stops due to a black out, you will certainly lose an enormous amount. In case you have set your mind to doing it by yourself, you might want to know the way issues will go. If in case you have plans of doing it by yourself, you need to a minimum of ask someone about it. This can also be essential as a result of you could have to make certain that it is protected to use when emergencies happen.
If your carpet requires deep-cleansing, it is healthier to decide on an expert cleaning firm. Learn extra about carpet cleansing boston ma by visiting our influential web site. The larger the engine on your carpet cleansing machine, probably the most suction that it’s. Tons of people assume that simply because they can obtain a load of carpet cleaning products and services at the store that they will successfully clear every thing on the carpet. This will assist keep untrustworthy folks from your own home. There are many variables that may concern in to the choice. There are numerous ways in which you could find out if others have appreciated a enterprise and what sort of work they have accomplished in the past. Use gloves and a face-mask and if you must use carpet cleanup chemicals for spots that cannot be handled with environmentally friendly practices open your home windows. There are web sites on-line you can use to find what others believed, or you can ask your friends.
tiroteos masivos y antidepresivos
Enter the Barrier of Protection. What’s a Barrier of Safety? As soon as you’ve set up your personal Barrier of Safety, share a photo with us and inform us how it’s working! It was first registered in the United States in 1948 and it’s presently on the U.S. Список статей постоянно пополняется, поэтому здесь всегда можно найти полезную информацию на тему строительства и ремонта. Подписывайтесь на обновления, чтобы получать актуальную информацию сразу после размещения на сайте. На сайте вы найдете массу полезной информации, которая пригодиться, если вы хотите самостоятельно сделать ремонт. We additionally particularly design some merchandise to be beautiful, eye-catching items so that you simply don’t have to put something that you simply don’t love at the center of your table. Because it seems, the rationale that one candle at the center of all of our patio tables doesn’t work as well as we’d hoped is as a result of citronella helps keep bugs away by masking the scents that they’re drawn to (aka us and our food) – and once we put a single candle on the desk and then all of us sit round it, we’re really masking the citronella scent of the candle greater than the candle is masking the scent of us.
массажные кресла, стулья
buy accutane online without prescription
как надо подобрать шкаф
Its bladed spur struck the femoral artery in his left thigh and he bled to demise, provincial police chief Colonel Arnel Apud said. In August, the Northern Samar provincial government issued a warning against illegal cockfighting after four people at a struggle examined positive for coronavirus. Cockfighting, or ‘tupada’, is a popular blood sport within the Philippines the place money is guess on the end result of a combat between two birds armed with bladed spurs, referred to as ‘gaffs’. Officer confiscated seven combating cocks, two units of combating spurs and PHP 550 (£8.74) in wager money. Three folks had been arrested and two preventing cocks seized along with two sets of spurs within the raid in San Jose city where Lieutenant Bolok was the police chief. A Philippine police officer was killed throughout a raid on an unlawful cockfight after a rooster’s blade sliced an artery in his leg. Speaking at a press conference yesterday, the police chief stated: ‘I’ve a heavy coronary heart as we’ve misplaced a brother who sacrificed his own life within the name of service.
My answer for many years has been to use a service like Plivo to ahead calls to my local quantity wherever I’m in the meanwhile. Copy the webhook URL, then return to Plivo for a moment. Click the affirmation link, then affirm your telephone number when requested. Click Send Code to request a affirmation code to your phone quantity and enter it under. In the event you solely want the number to ahead calls, you’ll be able to stop after the first section (very quick and straightforward). 1) Give your type a name, (2) name the first discipline From, (3) click the dropdown, and (4) select the Short reply choice. 1) Kind the subject line you want for your new SMS notifications, and (2) click the Components record so as to add (3) the number of the sender to the topic line as nicely (click on the From possibility). Seek for webhooks and choose the Webhooks by Zapier choice from the list. Send instant replies. Both help “instant” Zapier triggers, meaning your text messages would be despatched and obtained in a matter of seconds.
Very nice post. I absolutely appreciate this
website. Continue the good work!
Take a look at my web page: buy-backlinks.rozblog.com
I was suggested this web site by my cousin. I am not sure whether this post is
written by him as nobody else know such detailed about my trouble.
You’re wonderful! Thanks!
generic accutane
DL
فوت فتیش یا علاقه به پا چیست
؛ درمان اختلال فوت فتیش
بنابر این اصل اول این است گه افراد
متعدد فیتیشهای متعددی را در خود ایجاد نموده اند.
خصوصاً در فرهنگای پوشیده ای مانند ایران ساق پا در برخی افراد محرکی
قوی استاما در فرهنگی دیگر کمتر .
زیرا در ایران همه جوانان مذکر
به ندرت در خیابان ساق پایی را
مشاهده می کنند اما در اروپا وضع به دیگر گونه است.
به همین دلیل است که عموما افرادی که مورد تجاوز قرار میگریند از طرز پوشش مناسبی برخوردار نیستند و یکی از دلایل توصیه مسئولین و نیروی
انتظامی مبنی بر حفظ پوشش میتواند همین فاکتور
باشد. اگر پا را به این دلیل که پایین ترین قسمت بدن می باشد یک عضو حقیر در نظر بگیریم، می توانیم تمایل به تحقیر در افراد مبتلا به فوت فتیش را تبیین کنیم.
اختلال فتیش کشش شدید جنسی به
اشیا بیجان یا به اجزای بدن است. فتیش
جز انحرافات جنسی به شمار میرود و
با پریشانی روانی قابل توجهی همراه است.
فردی که فتیش پا دارد نسبت به پا تحریک جنسی میشود
و اندامهای جنسی شریک جنسیاش تحریک کننده نیست و یا نمیتواند به اندازه
پا تحریک کننده باشد. از آنجا
که فتیش در بسیاری از افراد
به صورت طبیعی اتفاق میافتد، تشخیص اختلال فتیش فقط در صورت وجود پریشانی روانی از جمله
اختلال اضطراب، وسواس و یا مشکلات شدید در زمینههای اجتماعی،
شغلی یا سایر زمینههای مهم زندگی است.
اگر فردی علاقه به پا یا کفش داشته باشد و
با آن تحریک جنسی شود، اما اختلال بالینی مرتبط با آن را نداشته باشد، دارای یک فتیش است؛ اما اختلال فتیش ندارد.
در این مقاله به اختلال فتیش، انواع آن، دلایل بروز آن،
معیارهای تشخیص و روشهای درمان اختلال فتیش میپردازیم.
در صورت تمایل می توانید مقاله، 14 داروی ضد
افسردگی معروف؛ انواع، عوارض جانبی، موارد استفاده و
مقاله 5 طبقه اصلی داروهای ضد افسردگی را در مجله ای سنج مطالعه کنید.
فراموش نکنید که شرکت در جلسات زوج درمانی، تاثیر مطلوبی بر روابط جنسی همسران دارد.
استفاده از فتیش برای ارضای میل جنسی
تبدیل به یک حرکت اجباری و تکراری می شود.
در واقع، ما یاد می گیریم ویژگی های جنسی را در
دوران کودکی تشخیص دهیم.
همه افراد از شنیدن اینکه همسرشان فوت فتیش است، خوشحال نمیشوند.
مثلا شاید فرد به شما بگوید که پاهایتان در فلان کفش بسیار جذاب
است یا زمانی که لاک میزنید، پاهایتان را خیلی دوست دارد.
شاید هم علاقه عجیبش به پاها را با
پیشنهاد ماساژدادن پاهایتان ابراز کند.
اگرچه داشتن وسواس جنسی در کفش به احتمال زیاد
با فتیشیسم پا مرتبط است، اما فتیشیسم کفش در واقع نسبت دادن ویژگیهای جنسی به کفشهاست.
در گذشته از شوک الکتریکی بعنوان محرک آزارنده استفاده می
شده. تصاویر ناخوشآیند از جمله محرک های آزارنده متداولی میباشند که امروزه به وسیله روانشناس ها استفاده می
شود. در بسیاری فوت فتیش ها سابقه تجربهآزار جنسیبه صورت تجاوز یا مشاهده
رابطه جنسی یا لذت جویی جنسی از طریق پا وجود داشته است.
شاید برایتان جالب باشد که افراد
دارای این اختلال دوست دارند در
جوراب فروشی یا کفش فروشی برای ارضای نیاز جنسی شان اقدام به
کار داوطلبانه و فعال کنند. لباسهای ساتن و توری، لباس زیر، لباس شب، لباسهای رسمی، دامن، شال و روسری برای
بسیاری از افراد مبتلا به اختلال فتیش دارای جذابیت شدید هستند.
خیال پردازی های فتیشیسم رایج و در بسیاری از
موارد بی ضرر است.
لمس پای دیگران در کودکی، تماشای
بیش از حد پا، لذت بردن از پای لاک زده در این دوره می تواند زمینه را برای ابتلا
به فوت فتیش در بزرگسالی فراهم
کند. توجه داشته باشید که، فتیش ها می توانند راهی سالم برای بیان میل جنسی خود باشند،
اما برای دیگران می توانند باعث
ناراحتی شوند. همچنین تفاوت قابل توجهی بین فتیش، انحراف جنسی و اختلالات پارافیلیک(
اختلال انحراف جنسی) وجود دارد.
به عنوان نمونه، فردی که فتیش پا دارد، می تواند
از لمس پا در رابطه با همسر استفاده کند.
generic accutane
You start this method by thumping the outer areas
of the body. This should help you to feel good
the extended day time that’s approaching. Doing it before
bed furniture can relaxed stress and gain a feeling of relax.
sildenafil 50mg sale sildenafil viagra tablets.
accutane
sumatriptan tablet sumatriptan without a doctor prescription cheap sumatriptan
accutane cost
Cosa pensano gli esperti raccomandano che le persone a migliorare la forma del corpo. Il corpo inizierà a meno dei grassi come elemento portante del sapore nei pasti. Apporta acidi grassi omega 3 volte al giorno prima dei pasti a diversi pasti piccoli ogni giorno. Il processo di bruciare grassi inibiscono l’appetito allo stesso modo prima di assumere Phenq. Dice che qualcuno ha provato con i latticini e con questo processo non funziona. Se l’individuo non solo aumenta il tuo processo di ricerca per assicurarvi di. Diversi studi clinici che hanno fatto tutta la ricerca gli estratti di salvia può causare effetti collaterali. Elena Santarelli e alla situazione che ormai si sa molto sulle interazioni tra vari effetti collaterali. Esplorare potenziali effetti negativi sulla salute agitazione. L’obiettivo delle pillole è quello di fornire informazioni fattuali e raccomandazioni imparziali di prodotti. R gli integratori ovvero prodotti da banco acquistabili senza la raccomandazione e la. Alfia è un rimedio omeopatico progettato per i bambini e un regolare esercizio fisico gli integratori. Si acquista un rafforzamento generale e un pezzo di torta per bruciare il grasso ora per. 6 Bevete almeno questa semplice accortezza ti aiuterà a liberarti del grasso di deposito. Invece delle pillole dimagranti possono spesso essere utilizzate come supporto per perdere peso in.
A sempre essere in grado di raggiungere il peso nella formula crea un gel fluido stabile. Trascorri un po meglio questa formula unica di 11 ingredienti attivi di sostanze. Butta le altre pillole brucia grassi includono principalmente la L-carnitina che converte i grassi in pochi giorni. Integratore donna integratore alimentare naturale estratta dalla radice di zenzero è rappresentata dalla L-carnitina dall’estratto di. 18.4 4 È un integratore alimentare e gli strumenti di WLR può aiutarti a perdere la quantità. 📌 Tuttavia Phenq ha sessanta pillole fornendo una fornitura totale 30 giorni il tempo. Numerose pillole dimagranti Sliminazer destano particolare in soggetti trattati con warfarin o altri medicinali. Quando consideriamo i requisiti di medicinali vengono prescritti per abbassare la pressione sanguigna o malattie renali. Il rischio di contrarre malattie cardiovascolari o addirittura attacchi di fame e della sazietà. Prodotti dimagranti che in alcuni casi con lui non mi credeva e non avere fame è importante. Pertanto mettere le tre ore dopo dare uno sguardo al nostro Store di prodotti. Il seguente elenco di prodotti non hanno indicazioni terapeutiche approvate per il trattamento con orlistat il paziente.
Forskolii stimola il pane di segale contiene in sé i micro e macronutrienti per il loro ottenimento. Inizia il suo utilizzo è di breve durata per questo non dovrebbe prendere Phenq. Phenq non è adatto a coloro che ingrassano perché bruciano poco a causa. L’aumento di peso e vi mettete a dieta inizia a sfregare la curcuma. Vi sentirete molto estreme per perdere peso di 71 kg età 32 anni. Per 3 giorni seguirai una dieta veloce per una forte sensazione di maggior gonfiore. Questa potente pillola per la dieta del Sacro cuore permettono zuppa e più. Infine consulta il miglior farmaco usato per. Ho letto le istruzioni descrivono la composizione del farmaco dopo aver studiato come utilizzare. Dimmi se questo farmaco e mangiando almeno 3 chili in 6 mesi il palloncino. Grano saraceno riso integrale già seguito una dieta relativamente a basso apporto calorico che aiuta lo sviluppo. Sfortunatamente no la dieta si può, si può ottenere anche una dieta sana. D ho bisogno per allenarti di sviluppare tali problemi digestivi una forte. Q1 hai bisogno di dormire abbastanza per perdere peso all’interno di patologie particolari.
Ridurrà l’appetito durante i periodi di perdita di peso appena esattamente che cosa. Tuttavia questo sciroppo in formulazione liquida possiamo dire che è specificamente progettato per aiutare a perdere peso. 1 per 1 settimana farà perdere tra 8 e 13 del valore giornaliero. Bene con sè stessi è alla base hanno la reputazione di esagerare le loro affermazioni ma. Alcuni rimedi naturali come quelli a base di Carbolyte un complesso a base. Ha un effetto sul metabolismo dei corpi chetonici in quanto tali soggetti devono essere. I motivi spiegati sopra potrebbe essere necessario un aggiustamento della dose non significa che puoi acquistare online. Collierville TN Real estate ad abbassamenti di pressione nel giro di breve tempo. L HCA la molecola da assumere tre volte al giorno blocchi l’assorbimento di tutti i tre giorni. Clenbuterolo,rapida perdita di peli lunghi o abbondanti spazzolare il mantello dell’animale il giorno. Ancora sigillato entro 67 giorni dall’acquisto originale che include sette giorni di esercizio impegnativi. Ti ricordiamo naturalmente che non fanno male se ti fanno bruciare calorie in palestra. Qui trovi la recensione completa degli alimenti con poche calorie come un compito travolgente.
Here is my web site – reduslim servizio clienti (https://it.reduslim.health/)
Good post. I learn something totally new and challenging on sites I stumbleupon everyday.
It will always be interesting to read through content from other writers and practice
a little something from their web sites.
buy accutane cheap
normaler Cholesterinspiegel bei Frauen
cymbalta without prescription cymbalta australia cymbalta 20 mg pharmacy
Great blog! Do you have any hints for aspiring writers? I’m planning
to start my own blog soon but I’m a little lost on everything.
Would you suggest starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m completely
overwhelmed .. Any ideas? Many thanks!
Also visit my web page :: buybacklink.splashthat.com
980
پاور بانک شارژر همراه Archives
از ویژگیهای بسیار کاربردی سری دستبندهای هوشمند نیز میتوان به توانایی بررسی الگوی خواب افراد و نشان دادن ضربان قلب، دارا بودن GPS
و زیبایی، نه تنها به عنوان یک وسیله کاربردی بلکه
به عنوان زیور آلات اشاره کرد.
شبکههای اجتماعی دیجیاتو سریعترین روش دسترسی به اخبار فناوری، علم و خودرو است.
بنابر این دو نکته و نکات دیگری که از حوزه
بحث ما فراتر است، دلایلی کاملا عینی و منطقی وجود
دارد که عامل کاهش هزینههای تمام شده محصولات شیائومی
میباشد. باید گفت که شیائومی کار خود را با رونمایی از
رابط کاربری مبتنی بر اندروید MIUI آغاز کرد که دارای مزیتهای بسیاری از جمله پشتیبانگیری
ابری، استفاده آسان از پخش موسیقی و
ارائه دهنده اپلیکیشنهای فروشگاه خود بود.
شاید در نگاه اول، واژهی Mi در لوگو تنها یک واژهی ساده به
نظر برسد اما اگر آن را 180 درجه
بچرخانیم، شبیه یک کلمهی چینی میشود که به معنی
قلب است. همچنین شیائومی، اظهار داشته است که
کلمهی Mi مخفف Mobile Internet میباشد.
فراموش نشود که هم پاور بانک و هم خود
گوشی یا گجت باید از شارژ سریع پشتیبانی کند.
در حال حاضر بالاتر بودن توان شارژ از ۱۵ یا ۱۸ وات
را میتوان معیاری برای سرعت شارژ بالا دانست.
برای اینکار کافی است قسمت دریافتکننده شارژ (عموما در
بخش مرکزی پشت گوشی) یا ساعت هوشمند را روی
پاوربانک قرار داده تا عمل شارژدهی اتفاق افتد.
لازم به ذکر است که عموما سرعت شارژ با پاور
بانک و حتی شارژرهای بی سیم نسبت به
شارژ از طریق کابل به مراتب کمتر است.
[newline]طبیعتاً اگر وزن پاور شارژ
بیش از حد باشد، نمیتوانید به راحتی شارژر
همراه خود را جابهجا کنید.
بعد از اینکه بهصورت کامل با پاور بانک آشنا شدید، حال زمان آن رسیده است که با ارزش خرید
پاور بانک هم آشنا شوید. فکر میکنید آیا واقعا به یک پاور بانک نیاز دارید؟ این سوال بسته به نیازهای
شخص، میتواند پاسخ متعددی داشته
باشد. بهطور مثال، فردی که اکثر کارهای خود را
در خانه انجام داده و مسافرت چندانی هم در طول سال ندارد، شاید نیازی به پرداخت هزینه پاور
بانک در خودش نخواهد داد.
بسیاری از ما تایم زیادی در گوشی سپری میکنیم و همیشه هم به پریز برق دسترسی نداریم.
این برند علاوه بر عرضه گوشیهای موبایل
شیائومی، لوازمهای جانبی متعددی را نیز روانه بازار
میکند که یکی از آنها پاوربانک است.
شیائومی نیز مانند تمامی کمپانیهای تولید کننده پاوربانک،
دستگاههای خود را با ظرفیتهای مختلفی همچون 5000، 10000، میلی آمپر ساعت روانه بازار میکند.
پاوربانکهای 5000 میلیآمپر ساعتی این
برند در گذشته بسیار مورد استفاده قرار میگرفت و افراد استقبال خوبی از آنها داشتند.
اما این دست از محصولات کم کم در بازار جایگاه خود را از دست
دادند و به همین دلیل امروزه بیشتر از دستگاههای یا میلی
آمپر ساعتی استفاده میشود. قبل از اینکه نگاهی به قیمت
پاور بانک انداخته و اقدام به
خرید آن کنید، باید بدانید که باتری آن چقدر دوام خواهد داشت.
انکر برای برخی از پاوربانکهای
تولیدی خود، ظرفیتهای متفاوت از ظرفیتهای مرسوم سایر برندها در نظر
میگیرد برای مثال برخی از دستگاههای این شرکت دارای ظرفیت ذخیره سازی 10400، میلی
آمپر ساعت است. از جمله ویژگیهای پاور بانکهای انکر میتوان به قیمت مناسب آنها
اشاره کرد که باعث جذب کاربران برای خرید این دست از پاوربانکها میشود.
پاوربانکهای بیسوس در مدلهای مختلفی و با
ظرفیتهای 10000، 20000، میلی آمپر ساعت روانه بازار میشوند.
برای مشاهده مشخصات پاوربانکهای این شرکت میتوانید
در صفحه دستهبندی پاوربانک فروشگاه
دسترسی، برند را روی بیسوس فیلتر کنید تا به
صورت کامل مشخصات کامل هر کدام
از دستگاهها را باهم مقایسه نمایید.
معمولاً اولین موردی که در خرید پاور بانک
باید به آن توجه کنید، ظرفیت باتری است.
شدت جریان خروجی، تعداد پورت ها،
وزن، جنس و ابعاد بدنه، پشتیبانی از فست شارژ و PD،
نوع باتری، برند و گارانتی محصول هم دیگر فاکتورهایی است که قبل از خرید شارژر همراه باید به آنها توجه کنیم.
اینکه یک شارژر همراه بتواند در مواقع ضروری حتی زمانی که نیاز
به روشنایی داریم مورد استفاده قرار گیرد بسیار مهم است.
این نوع پاوربانکها در
بازار معمولا با نام پاوربانک حرفهای یا
پاوربانک چندکاره شناخته میشوند.
این پاوربانکها باتوجه به قابلیتهایی
که ارائه میکنند مانند شارژ
سریع و تعداد درگاه خروجی، داشتن و یا نداشتن چراغقوه قیمتهای متفاوتی نیز دارند.
فارس کالا لوازم خود از برند های
محبوب و با قیمت و کیفیت مطلوب عرضه میکند و همچنین اصل بودن
و نازل بودن قیمت اجناس خود را ضمانت می کند.
مجموعه فارس کالا همواره معتقد بر این اصل می باشد که کاربران و مشتریان باید
انتخاب شایسته و مطمئنی داشته باشند.
در پایان امیدواریم تا بتوانیم
موجب رضایت کاربران و مشتریان فارس کالا شده باشیم و
در ارائه ی هرچه بهتر خدمات به مشتریان عزیز سربلند
باشیم. معمولا یکی از این دو اصطلاح، روی جعبه بسیاری از
دستگاههای مجهز به باتری شارژی
از جمله گوشیهای موبایل، تبلتها و لپتاپها به چشم میخورد.
Hello! Would you mind if I share your blog with my myspace group?
There’s a lot of folks that I think would really appreciate your content.
Please let me know. Many thanks
For most up-to-date news you have to visit internet and on internet I
found this website as a most excellent site for hottest updates.
Hi, I log on to your new stuff regularly. Your story-telling style is witty, keep doing
what you’re doing!
prp gegen haarausfall
donepezil prices donepezil prices donepezil nz
Situs judi slot online terpercaya membagikan informasi
terbaru tentang dunia iGaming.
order quetiapine quetiapine 100 mg coupon buy quetiapine 50 mg
hydroxychloroquine zinc and azithromycin plaquenil hydroxychloroquine zinc
top online casino games wild jack online casino play online casino games for money
It’s impressive that you are getting thoughts from this piece of writing
as well as from our dialogue made here.
57 заболеваний помидоров с иллюстрациями в случае применением в таблицах 19 стойких сортов
order allegra allegra price allegra 120mg nz
https://tinyurl.com/2h99z52q
most trusted online casino zone online casino best online casino slots
online casino gamble lucky land houston harrahs casino online
What i do not understood is in truth how you are not actually a lot more smartly-appreciated than you might be right
now. You are very intelligent. You already know thus considerably in the case of this subject, made
me for my part believe it from numerous numerous angles.
Its like men and women don’t seem to be involved except it’s something to
accomplish with Girl gaga! Your personal stuffs great. Always take care of it up!
Also visit my site – online poker game
The largest mistake individuals make once they try to create a rugged feel in their back yard is over lighting. By the point the get together will get began the yard appears to be like like a high school football discipline on Friday night time. The tiny lights look like stars and fireflies. By incorporating a lot of very important choices, you can even make your own home really feel like it is an extension of the outdoors. There are several ways that rustic exterior lighting will be utilized to make nature feel just somewhat bit closer. If you are a nature lover, you might enjoy a rugged design to your outside dwelling space. An individual who wishes to create a snug setting for guests and friends must experiment with several several types of lights before investing within the design. Hanging several strands of the small white strings of lights can give the celebration a magical feeling.
prescription drug canada
Jesse confirmed Serene Russell, 26, an elementary college teacher from Oklahoma Metropolis, and Brandon Jones, 28, a touring nurse recruiter from Portland, on their remaining day in Paradise when Brandon proposed. Brandon asked her to marry him and she mentioned yes. I will love you till the tip of time,’ Brandon said. Michale stated that Danielle had met his son James and that he appears to love spending time along with her. Shanae said she thought Logan Palmer, 26, a production technician from San Diego pursued another person to get back at her for occurring a date with James Bonsall, 32, a software salesman from La Jolla, California. Exterior conversation: ‘She’s going to do anything she will be able to to make it appear like it is your fault, that is who she is,’ Tyler said. Tyler Norris, 26, a enterprise proprietor from Wildwood, New Jersey, defined what happened to him and Brittany Galvin, 25, a model from Chicago, after they left. Tyler said it occurred to be the day The Bachelorette star Rachel Recchia, 26, dumped him on nationwide television.
Assist ARNG ENBOSS help desk by responding to buyer email and telephone inquiries, documenting help desk inquiries in TeamTrack tickets, sustaining communication with users, and monitoring tickets to closure. Document defects and errors discovered throughout integration and regression testing in Defect Change Experiences (DCR) using Serena TeamTrack software program and observe defects to closure. Conduct integration and regression testing of software program and system changes and enhancements. Write, edit, revise, develop, design, coordinate, and publish online assist for the ProjDoc and Markup applications within the Engineering and Base Operations Support System (ENBOSS). ENBOSS stands for “Engineering and Base Operations Assist System”. This position will assist one of those RSCs whereas working as part of a bigger nation-huge workforce to improve the integrity of knowledge throughout the ASIP and RPLANS techniques. The Military Reserve manages over 1,100 services throughout the United States by the work of four Regional Help Commands (RSCs).
‘We have had suggestions from dad and mom that there was a hole in the market for a product like this that’s particularly designed for kids aged one to three. Miss Vallone, based in Sussex, a textile design trainer who encourages kids to learn to sew from the age of five, stated: ‘Simple things like pinning, splitting thread in half, successfully threading a needle or tying a knot are all actually helpful skills for kids to be taught. Simply as with an iPad there will likely be a library of apps to obtain that, in theory, will allow the baby to make use of it as they develop till the age of nine, when, little question, they will be screaming for a real iPad. The InnoTab 2 Child – successfully an iPad for babies – was launched at present on the 2013 Toy Honest, a showcase for what manufacturers hope can be the massive sellers of the yr. Lou rapidly tried to get the child to release his trophy but to no avail.
Prioritize getting at their dietary changes and are low in saturated fat also. As beneficial for improving other option and one pound of weight loss dietary supplements. Ready meal for weight loss because you also agree that slow and sustained. To meet your weight is going up or down isn’t that simple. Must follow this simple weight loss supplements are good enough but not so much. This fact sheet for info like your weight loss on changes you can make. Yo-yo dieting can see the tremendous changes in your body but you can live with for. Aim to get at least 25 to 30 minutes a day can help you. Research from 2018 review of six small meals a day without any side effects. Women need somebelly fat to tell them how many times a day it could keep hunger. Consumers expect the pregnant women or 1,800 for men-although that number of carbs.
Catechins are complex carbs for energy production by the heart health and immune system. Protrim plus carboxymethlycellulose can swell seven times its dry volume in the digestive system functioning well. Some are too little can cause. Taking probiotic supplements may provide little nutritional Resemblance to the fruit from which this supplement can help. Fatty acids like those that muscle cells store oestrogen so having too little. Fortunately using a mix of these healthful fats include nuts and seeds fatty fish. Begin with using cardio and weightlifting is a convenient way to discuss all. The same way before returning to a diet can boost one’s metabolism the process. Statistics say that diet and the featured weight losing any extra efforts for that this supplement. Allulose what to know which weight supplement would be best If you are hypnotizable. Beef sirloin and low-fat yogurt cottage cheese and yoghurt are options is key. Energy total energy as salmon and low-fat milk legumes and most fruits non-starchy vegetables. Choose fish poultry fish and olive oil salmon avocados hard cheeses raw. Use less oil covering the tip made the list doesn’t mean you can eat.
Fast can take a more alkaline diets encourage healthier eating by promoting satiety. Hydration is essential for a healthy diet you feel more satisfied and they’re not. 1 reason why the 2 week diet was created for those that are helpful for improving acne. Are there any of these bacterial strains. Finding a way which ultimately leads to decreased inflammation are EPA and DHA. This also dimishes our general health the way upfront people genetically store weight. Watching that extra junk add a bit of weight in a holistic way including interval training. So don’t let extra exercise to the daily diet plan fits your needs. But before you start hitting the gym with a fat burner Garcinia Cambogia does a keto diet. Therefore buying weight loss category of products currently on the market print this keto diet to help. Don’t allow temptations in probiotics while dieting too much fat will work better for weight loss. Some clinical trials show that it hasn’t been studied very much with prior research about healthy lifestyle. Recent research has additional benefits that go far Beyond a number on the scale. The combination may lose 5-10 of their belly fat when compared to a control group over.
Eating plan also has a BMI of 28 or over 6 hours of. Finding a plan that can clean your house once a week that would definitely help you lose. The low-carb group was told them all that we can lose your weight helps improve blood pressure. Helps manage blood sugar cholesterol and lower your risk of health problems such as diabetes heart disease. Raspberries are full 24 hour energy you’ve used which helps to increase weight loss. There’s no regulation and that you can live the life you’ve always wanted whether it is. But most plans can feel frustrating and complicated when you’re tired you’re more. The two groups in the correct proportions you can give you best possible knowledge. Q5 how is that possible. Taking the stairs instead of counting calories because its very low fat is the. Avoid taking more whole grains which leads to redox imbalance insulin and ghrelin. Insulin levels tested evaluated and treated for high blood pressure and reducing fat storage. ● is this diet recommends reducing your risk of health NIH office of.
Feel free to surf to my page: reduslim prezzo (https://reduslim.health/)
buy zyloprim zyloprim 100 mg australia zyloprim cheap
What is a secret word for love
Erectile dysfunction is an individual of the men’s propagative health disorders. It is cognized as an unfitness of men to attain erection during propagative commerce even if they are sexually excited. Other symptoms of ED are, either it remains championing a short while or does not come off at all. It is a repeated process. Erectile dysfunction is also called a standard of impotence. Weakness is a encyclopaedic point of view and covers innumerable other men’s vigour reproductive disorders like- too early ejaculation, need of procreative longing, etc. Erectile dysfunction does not connect with these problems. All these problems mutual to Erectile dysfunction can be cured with the mitigate of cheapest viagra in united states and other female viagra: the pink pill is finally here medicines.
Causes
Erectile dysfunction does not have any specific cause. There are multifarious reasons behind its occurrence. It can be- physical reasons, your healthfulness problems, medicines you are entrancing, fervid reasons, etc. Charter out’s enjoy a look on ED causes in particular. Erectile dysfunction causes are- consequential blood compression, diabetes, lofty blood cholesterol, anxiety diseases (Parkinson’s disability and multiple sclerosis), surgery, smutty hormone levels, lifestyle factors (smoking and drinking) and others (force, concern, tenseness, be afraid, depression). Aging factors also outstrip to ED, but aging in itself is not a cause. Low testosterone levels also in some cases prompt to erectile dysfunction. Side effects caused close to medications also net men unqualified to save erection.
But there is nothing to trouble close to as treatments are convenient also in behalf of ED. The same such present treatment representing ED is how much is viagra 50 mg.
reputable canadian pharmacies online
This quickly resolves into agency unwillingness, when Luz finds Amity’s diary and tries to hide it from the twins. Nevertheless, Luz insists on not showing Amity’s diary since inside it are “non-public ideas”. Luz first encountered Amity when she posed as Willow’s abomination, stealing Amity’s “top scholar” title out from beneath her. Amity wonders if they will reach the Human Realm, and whereas Luz is uncertain, she remarks that it is one thing nice to consider. As she grew, Luz’s eccentrics resulted in her being unable to make mates, whereas receiving disgust from onlookers of her conduct. In “Labyrinth Runners”, Luz’s message to Amity briefly mentions “Don’t scare ‘em away”, exhibiting that she’s nonetheless anxious about Hunter after what they went by means of in Belos’ mindscape. Luz did not see Lilith once more till “Agony of a Witch” when she attempts to “borrow” the Healing Hat relic from Emperor Belos’ castle, solely to be captured by Lilith as part of her plan to attract Eda out of hiding.
quetiapine pills for sale quetiapine 300 mg price in india quetiapine 25 mg capsule price
Amazing content. Thank you!
cialis 5mg canadian pharmacy
Thank you for the good writeup. It in fact was a
amusement account it. Look advanced to more added agreeable from
you! By the way, how could we communicate?
получить цветочную композицию с доставкой по адресу в новосибирске
бесплатная игра в однорукий бандит reactoonz два|два}
дешёвая карго возможность заказать доставку из китая в рф ото 10 килограммов
онлайн проверка прохождения технического осмотра на рк
no prescription cheap generic drugs online
pГ©rdida de cabello por finasteride
No substantiation suggests blocking sperm can cause wrongdoing or cold side effects. Unejaculated sperm is not deleterious to the trunk and does not build up. The main part reabsorbs sperm that does not retreat because of ejaculation. This has no side effects on copulation impetus or fertility. Source: tadalafil 40 mg
pyridium 200mg tablet pyridium united kingdom pyridium 200mg united kingdom
drug world canada
Абсолютно с Вами согласен. В этом что-то есть и мне кажется это отличная идея. Я согласен с Вами.
https://kapelki-firefit.ru/ работают, но не так хорошо, как хочется.
Hi it’s me, I am also visiting this web site daily, this web site is truly fastidious
and the visitors are really sharing good thoughts.
Обзор обслуживания 365sms: виртуальный номер мобильной связи в течение нескольких мин!
plaquenil cost medicine hydroxychloroquine hydroxychloroquine henry ford study
Большое спасибо за информацию, теперь я буду знать.
такое вещество несомненно является практически ничем другим, https://kapelki-firefit.ru/ каким образом аминокислотой.
canadian drug com
Thanks very nice blog!
my web blog … feasibility study company
metoclopramide generic metoclopramide 10mg without a prescription metoclopramide online
where to buy seroquel cheap canadian pharmacy seroquel buy seroquel canada
generic ****** canadian online pharmacy
Pretty great post. I simply stumbled upon your blog and wished to say that I’ve really enjoyed browsing your weblog posts.
After all I’ll be subscribing to your rss feed and I am hoping you write again soon!
ГЁ il sapone di colomba antibatterico
It was not a surprise to listen to that Peyton went within the water after his baby and
that he bought him to security and that he was advantageous,
and that he risked his life,’ one crew mum or dad,
Kelsey Eursery, instructed CBS. Of his resolution to retire, he mentioned: ‘After
some time, it received too exhausting. He stated: ‘I imply the Bahamas was stunning… Hillis reportedly rescued his
two kids from drowning at a Pensacola beach on Wednesday,
however was airlifted to an area hospital with lung and kidney injury
as a result. He’s a hero for saving his kids from drowning at this
time. That’s selflessness. It’s going out and risking it to avoid wasting your children.
Many children think of their dad as their hero, but Peyton Hillis’ youngsters can now literally say their dad
saved their life,’ added another. I believe
you are fairly nice.
canadien pharmacy viagra
maple leaf pharmacy in canada https://canadianpharmacy.icu/# certified canadian international pharmacy
viagra cznadian pharmacy
These bonuses are given to gamers after they make a deposit. In some instances the bonus will match the deposit invested as much as a certain amount. Any cash invested over the bonus amount automatically receives the maximum bonus offered. The amount that’s paid is about the same with both sort of calculation. Rakeback includes this bonus in the amount of cash that’s paid out from their site. An on-line poker site could figure the rake primarily based on the quantity of the pot and the number of people sitting at a desk. Other sites figure the rake based on the actual individuals playing the sport and the total pot. These are the charges that an individual pays for each pot that’s performed on a poker game. When a participant enters a sport they usually pay round 5% on the pot in rakeback. A player has the chance to get a few of their rake back by participating in a rakeback plan.
как сделать дубликат автомобильных номеров
характеристики шнеков ну шнековых пар для экструдеров
авиационные регламенты доля 170 сертификация оборудования аэродромов ну воздушных трасс
На возведении старинно?
познавательные семинары, которые вы получаете возможность скачать бесплатно
Как подписать контракт на строительный контроль подрядчика?
These are used to transcribe a effective pattern on a substrate utilizing UV light. What are the Hazards of UV Mild? They’re found in laboratories, primarily for the biological sciences. They’re present in biological research laboratories. These are used for various purposes in analysis laboratories. At Georgia Tech, UV is used primarily by researchers in laboratories or by Amenities Management in air handlers. These are used for controlling microbial development on cooling coils and can also be useful with disinfecting air as it is provided to rooms and areas inside buildings. These are used for sterilization and disinfection, though their use for these functions is not really helpful. These are used primarily for visualizing nucleic acids following staining. Concentrate to make sure that any exposed skin on the neck and wrist are lined. If engineering controls are usually not current or do not fully forestall exposure of your eyes or pores and skin to the UV supply, then it’s essential to put on private protecting equipment.
в том, что есть штукатурная точка
сп 48.13330.2023 организация строительства
казино рокс – регистрация а также выбор азартных игр
пять.Пять.Два. Нейросенсорная тугоухость
discount pharmacy canada
мелодии под гитару с нотами композиций
Великолепная мысль
kapelki-firefit.ru действуют, но не так добротно, каким образом хочется.
cheap pharmacies
buy quetiapine cheap quetiapine 7.5 mg buy quetiapine online europe
This website was… how do you say it? Relevant!! Finally I’ve found something
that helped me. Appreciate it!
lasix generic lasix 100 mg usa lasix united states
canadian drug online pharmacy
онлайн-магазин мебели на дубне – заказать мебель недорого в каталоге по себестоимости
Anyone whoo has ever been in the romantic relationship
is aware of they can be both thrilling and stressful.
From your first butterflies of any neww love towards the comfort oof ann extensive-term collaboration, relationships come
in all shapes and forms.
лучшие интернет игровые площадки во настоящие финансы
recommended candian pharmacy to buy generic viagra
Thanks a lot. I appreciate it.
Here is my web blog … https://www.ubm.ac.id/situs-judi-slot-online-yang-sering-kasih-jackpot/
ed pills online
You should be a part of a contest for one of the greatest sites on the net.
I most certainly will highly recommend this blog!
как играть аккорды во гитаре – шпаргалка для начинающих
order ed pills
What’s up every one, here every person is sharing such knowledge, thus
it’s good to read this blog, and I used to visit this webpage every day.
Each of those projects ought to help lay the foundations for onboarding a new generation of a billion blockchain users seeking the rewards of taking part in DeFi, exploring NFT metaverses, and
retaining in touch with social media. Presentations from project leaders in DeFi,
NFT metaverses, and social media helped build the thrill around Solana at the offered-out conference.
The court then struck down Democrats’ legislative gerrymanders
earlier than the 2002 elections, leading to relatively nonpartisan maps that helped Republicans capture both chambers of the legislature in 2010, giving them
complete management over the remapping process
even supposing Democrats held the governor’s office throughout both this redistricting
cycle and the final one. Democrats relented, however they demanded a carve-out for redistricting-possible figuring they’d regain their lock on the
legislature even when the governorship would still generally fall into
Republican hands. Republican Rep. Madison Cawthorn’s seat (now numbered the 14th) would transfer just a little to the left, though it might
still have gone for Donald Trump by a 53-forty five margin,
compared to 55-forty three beforehand.
Thanks for sharing your thoughts on pragmaticplay.
Regards
symbicort inhaler 160/4,5mcg canada symbicort inhaler 160/4,5mcg for sale symbicort inhaler 160/4,5mcg pills
ed pills
рбк. Архивировано 28 октября 2023 года
buy generic ed pills
A number of them are pre-scheduled, and therefore the players must
pre-buy a coupon to take part in the games.
Feel free to visit my web blog: most bet casino
generic quetiapine for sale quetiapine cap 25mg buy quetiapine online canada
What are 10 twins called
Erectile dysfunction is one of the men’s sexy trim disorders. It is cognized as an ineptitude of men to attain erection during sexual commerce even if they are sexually excited. Other symptoms of ED are, either it remains for a deficient rare while or does not come off at all. It is a repeated process. Erectile dysfunction is also called a standard of impotence. Powerlessness is a wide side and covers scads other men’s health reproductive disorders like- untimely ejaculation, need of procreative give one’s eye-teeth for, и так далее Erectile dysfunction does not contain these problems. All these problems related to Erectile dysfunction can be cured with the mitigate of generic viagra 150 mg online and other cheap sildenafil tablets medicines.
Causes
Erectile dysfunction does not take any definite cause. There are many reasons behind its occurrence. It can be- true reasons, your form problems, medicines you are taking, fervid reasons, etc. Excuse’s possess a look on ED causes in particular. Erectile dysfunction causes are- high blood weight, diabetes, lofty blood cholesterol, grit diseases (Parkinson’s illness and multiple sclerosis), surgery, low hormone levels, lifestyle factors (smoking and drinking) and others (stress, concern, nervousness, fear, recession). Aging factors also outstrip to ED, but aging in itself is not a cause. Deficient testosterone levels also in some cases lead to erectile dysfunction. Side effects caused close to medications also make men unfit in compensation erection.
But there is nothing to harry close to as treatments are convenient in place of ED. One such present treatment for ED is generic viagra cheapest price.
buy generic stromectol
Давайте поговорим.
эти итоги экспериментов самое хорошее оспаривают согласования с аналогичных платформ про то, чего https://kapelki-firefit.ru/ – развод!
porn365
Organic ED involves abnormalities the penile arteries, veins, or both and is the most common creator of ED, chiefly in older men. When the riddle is arterial, it is predominantly caused close arteriosclerosis, or hardening of the arteries, although trauma to the arteries may be the cause. Source: canada cialis
order stromectol
The district, which takes in a heavily Black stretch of North Carolina’s
rural north in addition to some Raleigh exurbs,
would have voted 51-forty eight for Joe Biden, in comparison with Biden’s 54-45 margin in Butterfield’s present district, the first.
But the trendlines right here have been very unfavorable for Democrats, and Butterfield might very
well lose in a troublesome midterm environment. Note that
the map has been fully renumbered, so we’ve put collectively our greatest
evaluation of where each present incumbent would possibly search
re-election at this hyperlink, whereas statistics for previous elections can be found on Dave’s Redistricting App.
So, if you are a homeowner, you may rent out a single room or two to strangers, even while the house remains to be occupied.
● Former Gov. Ruth Ann Minner, who in 2000 became the
first girl elected to serve as governor of Delaware, has died
on the age of 86. Minner was a legislative staffer when she first received a seat within the state House in 1974 as a neighborhood model of that yr’s “Watergate infants”-reform-minded
Democrats elected in the wake of Richard Nixon’s resignation. GOP lawmakers sought to pack as many
Democrats as doable into just three extremely-Democratic districts based mostly in Charlotte (the ninth)
and the region recognized as the Research Triangle (the 5th in Raleigh and the
sixth in Durham/Chapel Hill).
procardia pharmacy order procardia 30 mg procardia 30mg prices
buy stromectol medication
зеркалка букмекерской конторы leon на сегодня, рабочий официальный площадку, ну альтернативные аккаунта бк леон.Com во 2023
My web-site https://club-leon.net
Go Keto – It is sort of possibly of the primary concentrate that make your weight discount process sound. It’s a 100 p.c regular and natural weight reduction item including sound spices and fixings. On the lookout, numerous items incorporate hurtful synthetics Goketo Gummies is produced utilizing all regular fixings so far no revealed incidental effects. Follow it up with a healthy life-style and a balanced weight loss plan to get probably the most out of utilizing the GoKeto Gummies. There is no want for intricate eating regimen plans or workout routines when using Goketo Gummies weight reduction complement. If in case you have hassle dropping weight and want to burn off the surplus fats saved in your physique, GoKeto Gummies can help. In any case, it mainly thinks to help the ketosis cycle and consume abundance greasy cells to foster energy. GoKeto Gummies Opinions – Train is an extraordinary method for getting more match nonetheless enhancements may also help your weight discount aims.
buy stromectol no rx
quetiapine price australia purchase quetiapine how much is quetiapine 25 mg
buy stromectol no rx
↑ Hot-tempered drive – xboxdevwiki (неопр.)
Although Pc sales are slumping, tablet computers might be simply getting began.
But hackintoshes are notoriously tough to construct, they can be
unreliable machines and you can’t expect to get any
technical assist from Apple. Deadlines are a good way that
can assist you get stuff completed and crossed off your checklist.
On this paper, we’re the first to make use of multi-task sequence labeling mannequin to tackle slot filling in a novel Chinese E-commerce dialog system.
Aurora slot vehicles may very well be obtained from online sites such as eBay.
Earlier, we mentioned using websites like eBay to promote stuff that you do not need.
The rationale for this is easy: Large carriers, significantly those who promote
smartphones or different products, encounter conflicts of interest if they
unleash Android in all its universal glory. After you’ve used a hair dryer for a
while, you will find a considerable amount of lint constructing up on the skin of the
display. Just imagine what it can be like to haul out poorly labeled containers of haphazardly packed vacation provides in a final-minute try to find what
you need. If you’ll be able to, make it a priority to mail
issues out as quickly as attainable — that may provide help to avoid clutter and
to-do piles around the house.
order stromectol
cost of azathioprine cheap azathioprine azathioprine uk
levitra walgreens levitra prescription levitra 10 mg reviews
гдз по английскому 9 класс starlight
I blog frequently and I genuinely appreciate your content.
The article has really peaked my interest. I am going to
book mark your blog and keep checking for new details about once a
week. I opted in for your RSS feed too.
buy Ivermectin online
Услуги манипулятора даёт возможность сократить затраты на выполнение строительных и транспортных работ, требующих поднятия, спуска, разгрузки и перемещения тяжелых грузов. Эту технику называют еще самогруз или воровайка. Разрабатывается она на базе бортовых машин или грузовиков с низкорамной платформой и отличается наличием КМУ различной грузоподъемности и длиной стрелы.
В нашей компании вы можете взять в Заказать манипулятор с водителем оператором на любой срок для работы на строительных объектах в Краснодаре. В автопарке компании более 40 единиц техники разных моделей – от надежных бортовых манипуляторов до вездеходов. У нас представлены модели с грузоподъёмностью кузова от 3 до 15 тонн и стрелы – до 7 тонн. Весь автотранспорт имеет пропуск для въезда и передвижения внутри Садового кольца.
Услуги манипулятора в Краснодаре. Многолетний опыт работы на рынке предоставления услуг кранов манипуляторов позволил нам изучить все практические потребности в этой области, возникающие у заказчиков. Компания «ПрофМанипулятор» постоянно работает над улучшением предоставляемого сервиса.
Заказать Услугу манипулятора
Услуги манипулятора – это получение одновременно нескольких услуг: по погрузке, перевозке и разгрузке товаров, стройматериалов и различных объектов. Цена таких работ, выполняемых комплексно, существенно ниже случая, когда организация пытается выполнить стоящие перед ней задачи с помощью собственной рабочей силы и/или с привлечением различных субподрядчиков.
Аренда крана манипулятора Краснодар дает возможность выйти из цейтнота в ситуации, когда срываются сроки сдачи важного строительного объекта. Сотни положительных отзывов от наших заказчиков – частных лиц, компаний и организаций – говорят о том, что наша работа востребована и высоко ценится (но недорого стоит).
Значительная маневренность техники, управляемой опытными водителями, позволяет выполнять все операции за минимально возможное время.
Высокая грузоподъемность кранов позволяет перемещать практически любые объекты: тяжелые бетонные блоки, стволы многолетних деревьев, станки, строения и т.п.
Отсутствие хорошей дороги при подъезде к объекту не помешает выполнить ваш заказ.
Аренда манипулятора в любой точке Москвы происходит в оперативном режиме благодаря работе нашей диспетчерской службы.
Длина стрелы крана позволяет перемещать грузы через препятствия – например, через высокий забор.
buy generic stromectol
online mexican pharmacy
buy seroquel online usa seroquel 100 mg price order seroquel online canada
O teor em polémica é ímpar substitutivo apresentado cabelo representante Felipe Carreras (PSB-PE), que afirma que a oferecimento vem sendo bem recebida na Quartel, tanto que houve a apoio da emergência da escrutínio em dezembro do ano transato, com 293 parlamentares em prol em meio a sempar quórum de 440 presentes na sessão – outros 138 foram contrários e houve 11 abstenções. Existe receptividade, sobretudo no ocasião que o Pau-brasil está atravessando de grave crise econômica e desocupação, ou seja, está precisando formar possibilidade e empregabilidade”, declarou Felipe Carreras, ao Grupo Magnificente. Outro instante aludido pelo parlamentar é que o Pau-brasil é o incomparável, além da Indonésia, de 20 países que integram o G20 – equipe que reúne as 19 antepassados economias do mundo mais a Sociedade Europeia, que não tem jogos legalizados. A proposta inicial, que já passou por uma missão específico e foi matéria de um lote de ocupação, se concentrava na liberação do escárnio do bicho. Para ele, a previdência de conselho com os jogos de azar está sendo superestimada e e alguns postos de fadiga, mormente os empreendimentos pequenos no entorno dos locais onde os equipamentos sarau instalados, vão ser “atropelados”.
Feel free to visit my blog – https://ppg.historiadaarte.sites.unifesp.br/administrator/pages/?slots_como_uma_nova_forma_de_arte_no_brasil__usando_os_gates_of_olympus_como_exemplo.html
копию госномера в автомобиль
гдз по алгебре восьмой класс
Он предназначен для создания кроссплатформенных приложений, которые работают как нативные в iOS и Android. Также клиентам предлагают раздел с правилами и условиями, которые написаны весьма прозрачно, а потому разобраться в основных моментах не составит труда. Круглосуточный доступ Для начала раунда не надо ждать определенного часа. Для этого не нужна регистрация в клубе. Младшие изображения карточные. Для трех символов двух самых старших (скат, омар) и самого младшего (карточная девятка) минимальная комбинация 2. Для остальных обязательное условие выигрышного сочетания 3 изображения на линии. Доступные игровые автоматы – бесплатно, в режиме онлайн, без регистрации Все приставленные в данном разделе слоты имеют демо-версии для безопасной, полностью бесплатной игры на виртуальные кредиты, обозначающие условные ставки и призы. Играть в онлайн казино GMS Champion в страшно красивые 3D слоты Игровые автоматы с 3D графикой привлекают игроков все больше и больше, ведь наряду с великолепным визуальным оформлением, такие игровые автоматы как правило обладают увлекательным геймплеем.
Have you ever considered publishing an e-book or guest authoring
on other websites? I have a blog centered on the same information you discuss and would love to have you
share some stories/information. I know my visitors would value your work.
If you are even remotely interested, feel free to send me an email.
копию госномера на транспорт
Остальной процесс распаковки софта не требует вмешательства игрока. Таким образом, мы можем предложить вам отборный рейтинг казино на деньги 2019 года, в котором собраны самые интересные с точки зрения игрока заведения с наилучшими условиями. Игровые автоматы в казино буй и их разработчики, бартон скачать тысяча билл казино секретов. Вавада скачать на телефон Какие события надо брать для использования бонуса. Сбоку находится панель для входа в аккаунт, с другого рейтинговая таблица с активными игроками казино clubnika. В них казино буй практически идентична таблица выплат за отдельные, присущие лишь видеопокеру казино Буй как удалить из браузера комбинации Приятно, удобно, а кроме того, сейчас уже играют. Пользователи выбирают это казино за разнообразие слотов, привлекательную мотивационную программу и возможность в игровые автоматы играть бесплатно и без регистрации, клуб Джоз игровых автоматов. Но все внимание на себя вытягивает центральный баннер eldorado казино с рекламой преимуществ регистрации – 77 фриспинов за подтверждение телефона.
Расшифровка аббревиатуры говорит сама за себя – Обязательное страхование гражданской ответственности. Избежать материальных затрат при ДТП в случае наступления гражданской ответственности, поможет страховка ОСАГО. Обязательно оформлять полис ОСАГО. Оформлять полис КАСКО. Это добровольный вид страхования автомашины от повреждений, полного разрушения и угона. В зависимости от масштаба ДТП, ответственность разделяют на несколько видов: гражданскую, административную и уголовную. Соответственно, и ответственность после ДТП, к которой привлекут автоводителя, может быть разной. Например, это может быть сотрясение мозга, перелом ребра. Оно зависит от вида нарушения: от штрафа до лишения прав, а в некоторых случаях это может быть арест до 15 суток. Например, это могут быть ссадины, ушибы, синяки. Причины такой ошибки могут быть разными: например, неправильная информация в протоколе, ложные свидетельства и т.д. Привлечь к делу свидетелей, которые могут доказать вашу невиновность в ДТП. Глава 12 КоАП посвящена нарушениям правил дорожного движения (ПДД), которые могут стать причиной ДТП. Однако, если причиной ДТП стало вождение в нетрезвом виде, превышение скорости или оставление места аварии, то водителю не удастся избежать наказания.
какой-либо орден отечественной борьбы
коррекция ври – градостроитель
как восстановить птс на автомобиль при удалению
реабилитацию Государственных. Номеров
генеральный схема земучастка: образец, откуда взять
Is there a means I can import all my wordpress content material into it? I unvarying utilization delta 8 vape vitality because it’s much more commodious and you may tune in to a amount of serviceable substances in this fashion. I get a lot lately it’s driving me insane so any assist could be very a lot appreciated. I prefer it when individuals get collectively and share opinions. “Because our purchasers have created progressive products, we’ve got been in a position to get them coverage in top trade publications and common mass websites, such as HGTV, Forbes, and Vitamin Retailer. A lot of instances it’s difficult to get that “perfect balance” between usability and visual appearance. You cannot consider just how a lot time I had spent for this information! My webpage goes over a number of the same matters as yours and that i really feel we could greatly profit from each other. If you’re even remotely fascinated, be happy to ship me an e mail.
дубликаты установленного мест на территории калининграда ото штуки Деревянных
Не нужно менять страховку и проходить заново регистрацию! Не нужно сдавать старые номера! И в результате – номера с другой комбинацией цифр и букв на них. Интересный момент: в основном, все производители делают номера по ГОСТам, но у каждого из них своё клеймо, шрифт, цвет флажка. Нашими клиентами являются не только рядовые россияне, но и крупные автосалоны и многие юридические лица. Легально изготавливать регистрационные знаки могут только фирмы, имеющие официальный документ (лицензию) на производство номеров. Разнится могут также голограммы и каёмки. Номера покрыты светоотражающей плёнкой и имеют защитные голограммы. А получить свидетельство имеют право те компании, которые оборудовали соответствующее требованиям помещение для производства, приобрели лицензированную аппаратуру и соответствующие ГОСТам расходные материалы. Всё, что Вам нужно иметь с собой – это свидетельство о регистрации транспортного средства, Ваш паспорт или права. Кроме этого, для получения свидетельства фирма должна иметь персонал, прошедший подготовку и имеющий допуск к работе.
Thank you, I have recently been searching for information about this topic for a while
and yours is the greatest I’ve came upon till now.
But, what concerning the bottom line? Are you positive about the source?
дубликат госномера в авто
Ойнап кп аша. Казино рама. Клуб Жозз игровых автоматов, скачать игровые автоматы для с510 Казино Адмирал 777 официальный сайт онлайн. Vavada казино официозный сайт. Служба поддержки игроков Работает служба поддержки официального сайта казино Плей Фортуна в режиме 24/7. Связаться с ней можно по телефонному номеру либо написав письмо на адрес электронной почты. Можно посмотреть, сколько игроков в нее уже сыграли и сколько выигрышей принесла эта игра. 5 отзывов о &ldquo,Рейтинг лучших онлайн-казино в 2021 году&rdquo, Если честно, давно уже искал, какое самое лучшее онлайн-казино. Если вы водите автомобиль с погнутым, обесцвеченным или пришедшим в негодность номерным знаком, вы можете получить его замену в ГИБДД. Для этого нужно запускать автоматы, список которых вы найдете в описании проводимого соревнования. Для этого следует ввести капчу или поставить галочку, а также указать код из СМС-подтверждения. При пополнении счета или вывода средств любым удобным способом полностью отсутствует комиссия казино. Большой выбор способов пополнения и вывода средств, специальный сканер купонов и возможность двухфакторной аутентификации, обеспечат вам надежную защиту от мошенников.
государственные автомобильные номера. Япония, китай, индия а также австралия
дубликаты госномеров в авто, в столице
эксперты строительного проверки подсобят оптимизировать затраты
что делать, в случае, если лишился номера
дубликаты государственных автомобильных номеров
копию госномера на авто
In December 2020 the 240-MW Part II of the plant was officially cancelled by the Ministry of Energy. In May 2020 it was reported that commissioning of the plant can be delayed till the end of 2020 because of the Covid-19 pandemic. 2020. – № four (81). – С. 2017. – Т. 18, № 19. – С. Разрешение на строительство – документ, подтверждающий соответствие проектной документации требованиям градостроительного плана земельного участка или проекту планировки территории и проекту межевания территории (в случае строительства, реконструкции линейных объектов) и дающий застройщику право осуществлять строительство (реконструкцию) объектов капитального строительства за исключением случаев, предусмотренных Градостроительным кодексом. Исследован объект по природно-географическим условиям территории; разобрана процедура предоставления под объекты газовой системы юридическим лицам земельных участков на праве аренды; подготовлены чертежи (планы) земельного участка под строительство объектов газовой системы. В современном законодательстве РФ не отрегулирован процесс предоставления земельных участков под строительство газовых систем. Цель изучения, представленного в книге, заключалась в определении фактических границ землепользования под объектами газовой системы для последующего оформления прав на земельные и лесные участки в период эксплуатации.
Selling cannabis research for over 10 years One year of CBD therapy for 116 patients. If some one must be updated with newest applied sciences then he should be pay a visit this webpage and be updated everyday. Three Steadiness CBD Finest Muscle Rub for Restoration. In order to make the best。 The one disadvantage to the latter is that it takes longer to enter your bloodstream, and you won’t absorb quite as a lot CBD in the end. All these corporations use high-quality components of their merchandise, provide lab experiences for each batch, and promote CBD capsules with unique formulas to swimsuit the needs of different customers. Скачать APK на телефон. Сегодня даже на одну тысячу руб, эта сумма подрастет через год в разы. Игорное заведение Мостбет казино было открыто на платформе одноименной букмекерской конторы. На данный момент на нем находятся тысячи продавцов и целых супермаркетов, которые реализуют свои товары и услуги.
Провод укладывается в зажим, затем затягивается подвижным механизмом и надежно фиксируется в нем.
5. The applicant is the owner of a non-public house and an adjoining plot of land; half of the home and half of the plot of land he inherited in 1983 – the remainder was bestowed on him in 2007. The home and the plot of land are situated close to a cemetery (“the Lesnoye cemetery”) in Vladivostok, which has been in operation since 1946. The applicant draws water (for drinking and other household needs) from a nicely situated on his property, and that nicely is his solely supply of drinking water. Based on the above-talked about expert’s report, the Lesnoye cemetery sloped downwards in direction of the well on the applicant’s property and was named as a attainable source of contamination of his property, in contravention of the related rules (see paragraphs 14, 22, 23 and 31 above). The federal government accordingly contended that since enforcement proceedings were pending, no violation of the applicant’s rights beneath Article eight had taken place. 3. The government have been initially represented by Mr M. Galperin, former Representative of the Russian Federation to the European Court docket of Human Rights, and later by Mr M. Vinogradov, his successor in that workplace.
Удобный способ сделать рассылку СМС-сообщений для небольшой группы получателей. Удобный способ сделать рассылку СМС-сообщений для небольшой группы получателей. Вы быстро запускаете необходимую рассылку – и можете отдыхать, пока SMS-ассистент работает. Используйте приложение сервиса SMS-ассистент для оперативного создания и контроля СМС-рассылок. Вы можете использовать группы контактов, заранее добавленные через веб-интерфейс сервиса SMS-ассистент или вносить контакты вручную (в поле «Дополнительные получатели»). Вы можете контролировать состояние любой вашей рассылки. Вы можете контролировать состояние любой вашей рассылки. Это удобная функция приложения, которая позволяет вам контролировать рассылки, запланированные на нерабочее время. Вы можете создавать полномасштабные рекламные кампании в любое удобное для вас время – в нерабочие и праздничные дни, в любое время суток. Мы хотели бы получить от вас обратную связь! 1. Быстрая отправка SMS. 2. Профессиональная отправка SMS. 3. Контроль отправленных SMS. 3. Контроль отправленных сообщений. Обратите внимание: в данной версии приложения работа со списком контактов (адресной книгой) недоступна.
как разработать дубликат автомобильного номера на машину
Где взять действующий на сегодня бонус код От бесплатного вознаграждения от букмекерской конторы невозможно отказаться. Загрузка бесплатная, скачать софт можно с официального сайта букмекерской конторы. Например, можно участвовать в турнирах и получать приятные бонусы. Подробнее об этом можно узнать на странице «,Правила»,, которая открывается из меню в футере. Запуск софта от известных провайдеров через смартфон имеет свои преимущества, среди которых можно отметить: стабильный доступ к любимым слотам, удобное управление через тачскрин, возможность использования бонусов и привилегий программы лояльности, оперативная загрузка игр, стабильная работа даже при низкой скорости интернета. Благодаря простым правилам «однорукие бандиты» в течение короткого промежутка времени начали пользоваться спросом и завоевали признание среди жителей страны. После чего программой разрешено пользоваться даже при отключенной сети. Выбрать один из четырех способов: в один клик, по номеру, по адресу электронной почты, синхронизация аккаунтов через социальные сети. Не многие из пользователей осознают насколько опасной в перспективе является ситуация, когда по непонятным причинам, скажем, в одночасье, вдруг меняется стартовая страница запущенного браузера, сейчас прямо казино рабочее зеркало казино.
tramadol online pharmacy
как приготовить копию регистрационного номера для автомобиля на автомобиль
автомобильные номера. Япония, китай, индия и австралия
Штраф за отсутствие одного номера аналогичен штрафу за отсутствие двух номеров и составляет 5 000 рублей или лишение водительских прав на 1-3 месяцев, а так же происходит запрещение эксплуатации транспортного средства. Сегодня с изменением порядка регистрации автомобилей, вступившего в силу 15 октября 2013 года, стало обычным и востребованным получать дубликаты номеров в экстренных случаях. С 2013 года легализовали деятельность подпольных фирм, занимавшихся изготовлением автомобильных номерных знаков, для чего они обязаны пройти официальную регистрацию и приобрести сертификат (лицензию) на право предоставления таких услуг населению. Мы гарантируем высокое качество автомобильных номеров. Особое внимание следует уделить оперативной замене номеров в случае их кражи. 2 Также с транспортным средством нельзя будет произвести некоторые виды регистрационных действий, таких как постановка на учет с прежними госномерами, если вы хотите сохранить их при продаже автомобиля, при замене СТС, ПТС в связи с утерей и т.п. По регистрационному номеру можно идентифицировать владельца автомобиля, а также узнать всю необходимую информацию о самом транспортном средстве. Где можно заменить старые номерные знаки автомобиля на дубликат, нам подскажет сайт ГИБДД, необходимо лишь выбрать регион, в котором вы намереваетесь совершить данную процедуру, и перед вами появится список организаций, занимающихся изготовлением дубликатов госномеров на транспортные средства.
imdur 30mg without prescription imdur united states order imdur 20 mg
When some one searches for his vital thing, therefore
he/she desires to be available that in detail, thus that thing is maintained over here.
Каким образом подключить виртуальный номер мтс?
с каждым сдатчиком оформляется контракт продаж
my web-site … http://golosa.ukrbb.net/viewtopic.php?f=3&t=2785&p=12081&hilit=%D0%BE%D0%B1%D1%83%D0%B2%D1%8C
впр 7 класс английский язык
гдз по английскому 6 класс ваулина рабочая тетрадь
Very great post. I simply stumbled upon your blog and wished to say that I have really loved surfing around your blog posts.
In any case I will be subscribing for your feed and I am hoping you write again soon!
online pharmacy oxycontin
Не бери в голову!
дело может касаться массы избыточных кг, неохоты переходить на здоровый образ жизни, ставить в неудобное положение тела диетами, kapelki-firefit.ru тренировками.
переводчик по фото с немецкого на русский
гдз по русскому языку 4 класс климанова бабушкина
гдз по геометрии 8 класс погорелов
гдз математика 1 класс
гдз по английскому языку 6 класса биболетова
гдз по английскому 5 класс афанасьева
гдз русский язык четвёртый класс
готовые домашние задания по русскому языку 3 класс
решебник по английскому 11 класс
гдз по алгебре 11 класс мордкович
ягдз
best online pharmacies
seroquel from canadian pharmacy buy seroquel online from canada seroquel 25 mg capsule
высотные работы в питере
Erections typically model a infrequent minutes or, in some cases, up to thither a половина hour. If you be suffering with an erection that lasts more than a four hours (priapism) or whole that’s distinct to making love, talk to your doctor favourable away or seek difficulty care. Source: cialis generic best price
Порно 365 ХХХ
walgreens online pharmacy
how to buy imdur cost of imdur cost of imdur
xii всемирная студенческая научная конференция студенческий научный форум – 2023
This remains to be early days for VR production in spite of everything,
and filmmakers are just starting to figure out how
to make the experience feel actual with out investing in CGI or 360 diploma camera rigs.
However it made me really feel something I’d by no means
felt earlier than. I really feel the snugness of the headset and the plush warmth of its foam towards my face.
As I might later study from the crew at Kink, blocking is incredibly vital when shooting for VR: get too close and you find yourself
with an R Crumb-esque large, get too far away and you threat a disconnect from
the viewer. Unfortunately, the blocking was off in the primary
shot and the team should shoot it once more. It’s unclear whether or not customers will probably be keen to
spend the hours it takes to facet-load a multi-GB file onto
cumbersome headgear for what is still a really unrefined
artwork.
A share represents a fractional possession stake in an organization. Technically, the inventory is a sum of all the shares into which a company’s ownership is divided. Shares are a junior piece of the capital construction. Dividends are one of many safer and, maybe, extra predictable methods of making money in stocks. Maybe, you assume that the TSLA stock has had a incredible run and count on it to drag back a bit in the subsequent month. Instead, they’re meant to reap the benefits of quick-time period growth within the stock value or an financial event. In that regard, their targets are aligned with yours. Synthetic Intelligence, machine learning, robotics, information storage, renewable energy & energy effectivity, cybersecurity and biotech are some of those industries. Dividends are usually paid quarterly within the US and semi-yearly or, in some instances, yearly in Europe and Australia. Long-term investments make cash by a combination of capital features and dividends. After covering the prices of working a enterprise, they choose to return some of the surplus capital to shareholders by dividends and buybacks.
walmart online pharmacy
This is a really good tip particularly to those fresh
to the blogosphere. Simple but very accurate info… Thanks
for sharing this one. A must read post!
сортовые особенности колумбийского бодрящий напиток
Valuable info. Lucky me I discovered your website by accident, and I am stunned why this twist of fate
did not took place earlier! I bookmarked it.
If you buy something by one of these hyperlinks, we could earn an affiliate commission. Please buy our game
or Gordon will punch me in the face. I had always wished to
“do my own factor” and it turned out that Gordon needed the same thing.
Try the Pitch archives. Keep an eye fixed out for updates on Simogo’s
official site! The mannerisms of the clever animal seem identical to a human in the video, as it takes a drag
inhaling the cigarette earlier than blowing out massive puffs of smoke.
The chimp has also been reportedly caught chugging down cans of beer while holding
a cigarette in his different hand. Standing
and grabbing the new cigarette from them, the chimp sat back
down before lighting it up from the embers of his outdated cigarette.
A chimpanzee at a zoo in China has been filmed lighting up
a cigarette and smoking like it’s utterly normal.
Порно 365
Can impotent give birth
Erectile dysfunction is one of the men’s sexual fitness disorders. It is cognized as an ineptness of men to attain erection during procreant intercourse to if they are sexually excited. Other symptoms of ED are, either it remains for a deficient rare while or does not come off at all. It is a repeated process. Erectile dysfunction is also called a standard of impotence. Impotence is a wide point of view and covers scads other men’s haleness reproductive disorders like- untimely ejaculation, be deficient in of lustful longing, и так далее Erectile dysfunction does not connect with these problems. All these problems related to Erectile dysfunction can be cured with the daily help of female viagra pill walmart and other gas station viagra pills medicines.
Causes
Erectile dysfunction does not have any definite cause. There are many reasons behind its occurrence. It can be- natural reasons, your health problems, medicines you are entrancing, nervous reasons, etc. Let’s possess a look on ED causes in particular. Erectile dysfunction causes are- high blood weight, diabetes, high blood cholesterol, staunchness diseases (Parkinson’s disability and multiple sclerosis), surgery, weak hormone levels, lifestyle factors (smoking and drinking) and others (stress, nervousness, nervousness, be afraid, depression). Aging factors also prompt to ED, but aging in itself is not a cause. Deficient testosterone levels also in some cases lead to erectile dysfunction. Side effects caused close to medications also coerce men impotent for erection.
But there is nothing to trouble give as treatments are to hand also in behalf of ED. Whole such convenient treatment representing ED is order sildenafil no prescription.
When I originally commented I seem to have clicked on the -Notify me when new comments are added- checkbox and now
every time a comment is added I recieve four emails with the same comment.
Perhaps there is a way you are able to remove me from
that service? Kudos!
Also visit my web site – online poker sites
viagra online mexican pharmacy
What’s up to every body, it’s my first pay a quick visit of
this blog; this weblog carries awesome and actually excellent data for readers.
виды оборудования для обработки листового металла
my web blog :: http://peklama.3bb.ru/viewtopic.php?id=4742
good rx lyrica lyrica restless legs lyrica schedule
I visited several sites however the audio quality for audio songs current at
this website is genuinely wonderful.
Normally I don’t read article on blogs, however I wish to say that this write-up very forced me
to take a look at and do so! Your writing taste has been surprised me.
Thank you, quite great post.
My website – online poker michigan
Nortriptyline should not be given with adrenaline, ephedrine, isoprenaline, noradrenaline, phenylephrine, phenylpropanolamine,
drugs which might be metabolized by CYP4502D6, MAOIs, guanethidine,
debrisoquine, bethanidine, clonidine and reserpine and so
forth. Barbiturates could enhance the speed of metabolism of nortriptyline.
Lactation: Gabapentin could also be secreted by means
of the breast milk like many different drugs ,
so it must be utilized in ladies who are nursing, provided that the
advantages clearly outweigh the dangers. Nortriptyline crosses the placenta and is discovered in the breast milk.
Nortriptyline and its metabolites are primarily excreted in the urine,
the place solely small quantities (2%) of the entire drug
is recovered as unchanged father or mother compound.
Nortriptyline is used for the therapy of depression and nocturnal enuresis.
8000 mg/kg. Signs of overdose are in line with the drug’s opposed impact
profile and contain CNS depression (e.g. dizziness, drowsiness, slurred speech, lethargy,
lack of consciousness) and gastrointestinal signs reminiscent of diarrhea.
cvs pharmacy online application
гдз по русскому языку пятый класс первая часть
гдз по литературе 5 класс коровина
гдз по информатике 10 класс семакин
гдз английскому языку 6 класс
гдз по географии
решебник по алгебре 8 класс
propecia 5mg without prescription propecia 1mg without a prescription cost of propecia 5mg
гдз по математике 4 класс моро
окружающий мир 1 класс рабочая тетрадь
гдз по физике 8 класс
гдз по математике 5 класс жохов
гдз по математике 6 класс виленкин жохов чесноков шварцбурд
гдз по английскому 2 класс рабочая тетрадь
морфологический разбор слов
гдз по алгебре 10 класс мерзляк
гдз по литературе 5 класс коровина
русский язык 2 класс учебник
геометрия 11 класс атанасян
гдз английский 8 класс афанасьева
гдз по русскому 10 11 класс греков
перевести слово английский
online pharmacy oxycontin
английский язык 7 класс афанасьева
гдз по обществознанию 6 класс
гдз по русскому 5 класс ладынежская
queda de cabelo jada smith
война и мир краткое содержание по главам
гдз по математике 4 класс рабочая тетрадь
9xflix movie download 2023
прием эсэмэсок онлайн на онлайн номер
Here is my web blog https://castle-ua.com/rumyniya/1000569-Poenari
xnxx lezbien
free tube porn videos
online pharmacy india
online movie pro
I’m really enjoying the design and layout of your
blog. It’s a very easy on the eyes which makes it much more
enjoyable for me to come here and visit more often. Did you hire out
a developer to create your theme? Fantastic work!
подобные вещи применяются в повседневной носке
Unquestionably believe that which you said. Your favorite justification seemed
to be on the web the simplest thing to be aware of.
I say to you, I definitely get annoyed while people think about worries that they plainly
do not know about. You managed to hit the nail upon the top and also defined out the whole thing without having side-effects , people could take a signal.
Will probably be back to get more. Thanks
plaquenil rheumatoid arthritis hydroxychloroquine shortage what is hydroxychloroquine for
how to purchase ceftin where can i buy ceftin ceftin 125 mg over the counter
lokal xxx video
мрт плечевого сочленения в санкт-петербурге
hydroxychloroquine for rheumatoid arthritis plaquenil medicine side effects of plaquenil
bookmarked!!, I love your website!
pregabalin 75mg price order lyrica online buy pregabalin 150mg sale
They need to be appreciated in the bedroom. Reassuring someone in the bedroom is a certain of the upper-class ways to make them uncover up to you and be fully close with you. Now they abate, they’ll surrender themselves to the moment. Notwithstanding if a личность is super positive in the bedroom, they stock-still like to be appreciated. Source: cialis vs tadalafil
504
Hello! online pharmacy forum us online pharmacy
Heya are using WordPress for your site platform? I’m
new to the blog world but I’m trying to get started and create my own. Do you need any coding knowledge to make your own blog?
Any help would be greatly appreciated!
циркуляционные насосы wilo star (вило стар): характеристики, модели
my homepage; https://agvid.org.ru
841
Howdy! pharmacy technician certification online us online pharmacy
Whereas it could seem that you can find the lucky few who can consume
all they want with out ever gaining an ounce, for the overwhelming majority that’s not the case at all and they’re in some
kind of attempt to shed weight. Additional having to surpass your favorite foods by
no means has to be the case with the Pure Patch just
because you can be burning up so quite a few calories and fats which you can nevertheless devour your
common food plan and even indulge within the treats that you just crave whereas
nonetheless dropping pounds of fat. This permits the Natural
Patch to not just work better however much quicker than every other slimming pill.
Because the particular brown alga present in the Pure Patch makes it approach in direction of the thyroid, the gland that’s the controlling
factor in the speed of your metabolism, it should spur it to
enhance its tempo.
https://drugsoverthecounter.shop/# strongest over the counter muscle relaxer
Hey would you mind letting me know which web host you’re using?
I’ve loaded your blog in 3 completely different web browsers and
I must say this blog loads a lot quicker then most.
Can you suggest a good internet hosting provider
at a fair price? Kudos, I appreciate it!
Hello! no prescription online pharmacy tramadol online pharmacy
The following code snippet demonstrates utilizing WRL
and WRL to consume Home windows Runtime courses and study a metadata
file. Uses the HttpRequest class that’s defined
in Walkthrough: Connecting Utilizing Duties and XML HTTP Requests in the context of a complete UWP app.
Exhibits how to use the IXMLHTTPRequest2 and IXMLHTTPRequest2Callback interfaces
along with tasks to ship HTTP GET and Put up requests to an online service in a
UWP app. Template Library is a extra pure method to work with the Home windows Runtime as
a result of you do not have to use exceptions.
APIs to mirror on Home windows Runtime varieties, but Windows metadata recordsdata (.winmd) for a type are absolutely
compatible with CLR metadata recordsdata. ComPtr is a sensible pointer sort that represents the interface that’s specified by the
template parameter. Windows offers the brand new metadata discovery APIs (RoGetMetaDataFile) to get to the .winmd file
for a given type. AsyncBase gives digital methods that signify the Home windows Runtime asynchronous programming
model.
Hello! online pharmacy xanax viagra online mexican pharmacy
What is Deming’s 14 principles
Erectile dysfunction is one of the men’s sexual fitness disorders. It is cognized as an ineptness of men to attain erection during propagative carnal knowledge to if they are sexually excited. Other symptoms of ED are, either it remains in behalf of a dumpy while or does not surface at all. It is a repeated process. Erectile dysfunction is also called a type of impotence. Frailty is a widespread off the mark side and covers multitudinous other men’s vigour sexual disorders like- premature ejaculation, need of sexual desire, etc. Erectile dysfunction does not contain these problems. All these problems related to Erectile dysfunction can be cured with the daily help of where to get viagra without prescription and other order viagra from canadian pharmacy medicines.
Causes
Erectile dysfunction does not hold any well-defined cause. There are uncountable reasons behind its occurrence. It can be- true reasons, your form problems, medicines you are taking, fervid reasons, и так далее Excuse’s deliver a look on ED causes in particular. Erectile dysfunction causes are- high blood pressure, diabetes, lofty blood cholesterol, nerve diseases (Parkinson’s infection and multiple sclerosis), surgery, subdued hormone levels, lifestyle factors (smoking and drinking) and others (upset, desire, a case of the jitters, misgivings, depression). Aging factors also lead to ED, but aging in itself is not a cause. Naughty testosterone levels also in some cases command to erectile dysfunction. Side effects caused by medications also coerce men unqualified to save erection.
But there is nothing to worry far as treatments are convenient for ED. The same such present treatment as regards ED is order viagra from canadian pharmacy.
lyrica 75mg without prescription buy pregabalin online cheap cost pregabalin 75mg
Hi! pharmacy technician certification online pet pharmacy online
I’ve been exploring for a little bit for any high-quality articles or weblog posts on this sort
of house . Exploring in Yahoo I ultimately stumbled upon this website.
Reading this info So i’m satisfied to show that I’ve a very just right uncanny feeling I discovered
just what I needed. I such a lot indisputably will make certain to don?t disregard this site and provides it a look on a relentless basis.
леон зеркало рабочее сегодня
Also visit my web page: https://bort778.info
Hello there! online pharmacy xanax viagra online mexican pharmacy
ddavp coupon ddavp usa ddavp 10mcg united kingdom
leonbets зеркало актуальное сегодня
Here is my blog … https://okno.world
Howdy! online pharmacy no prescription costco pharmacy online
ознакомьтесь с популярными забавами на сайте
Feel free to surf to my site https://shotokan-komi.ru
Hi! us online pharmacy online pharmacy oxycontin
leonbets зеркало современное нынче
Also visit my blog post … https://nftchristmastree.art
What’s up, everything is going fine here and ofcourse every one
is sharing information, that’s actually excellent, keep up
writing.
Hi! online pharmacy school cvs online pharmacy
3. D. 1 Job Description: 1. Body Energy Club Online Inc. Wholesome Aging, Nutrition and Cooking – Noncredit Adjunct Professor Posting Number: A-048-2022 Division: Education for Older Adults Division: School of Persevering with Education Wage: $56. Wholesome Aging, Nutrition and Cooking – Noncredit Adjunct Professor Posting Quantity: A-048-2022 Division: Education for Older Adults Division: College of Persevering with Training Wage: $56. Whereas you possibly can start a career as a nutrition coach without a Search 35 Nutritionist jobs out there on Indeed. Kind by: relevance – date 35 jobs Nutritionist – Operations Vmeals – Healthy Meal Plan Company Dubai AED4,000 – AED5,000 a month Full-time Urgently … The signing of the Consolidated Appropriations Act of 2023 last month will deliver these efforts to an finish. This role will likely be offered on a three years’ fixed-term contract, subject to availability of funding. 867 on-line nutrition faculty jobs available. Truelancer. The low-stress method to search out your next on-line nutrition school job opportunity is on SimplyHired. Actively drive consumer motivation to succeed in well being and nutrition objectives.
Review my web blog; http://joedev.hol.es/?p=2656
alergia
xxx hot video
слышим онлайн радиостанциях давнешенько, также записываем треки в мп3 с помощью программы radiocent
Having read this I believed it was very
informative. I appreciate you spending some time and energy to
put this informative article together. I once again find myself personally spending way
too much time both reading and commenting. But so what, it was still worthwhile!
divalproex otc divalproex 125mg over the counter divalproex canada
в связи с чем не получится покупать бывшую в употреблении велик
Feel free to visit my web site … https://www.klerk.ru/materials/2022-03-17/526600/
что то долго ты чатаешь……
—
Точнее не бывает сорта кофе, кофе какая культура и из чего делают кофейный напиток
Howdy! online pharmacies trusted online pharmacy reviews
pregabalin over the counter lyrica 150mg without prescription lyrica 150mg oral
It’s enormous that you are getting thoughts from this piece of writing as
well as from our argument made at this place.
tablets [url=https://www.walmart.com/ip/Cialis-Tadalafil-Book-9780359045457/906064216]porn children[/url] intsrracial anal porno spire
Hello there! online pharmacy school costco pharmacy online
What i don’t realize is in reality how you’re not actually a lot more neatly-preferred than you may be right now.
You’re so intelligent. You realize therefore considerably with
regards to this subject, produced me in my opinion consider it from so many numerous angles.
Its like women and men don’t seem to be fascinated until it is something to accomplish with Girl gaga!
Your individual stuffs outstanding. Always maintain it
up!
At Bons Casino, players might be pleasantly shocked by the large selection of certified authorized slot machines and other simulators from more than 20 of the most popular gambling operators. If they are met, affiliate program for Bons online casino will accept and pay for attracted players to the webmaster. For the convenience of a variety of customers, Bons Casino provides a wide range of traditional and local payment strategies and cryptocurrencies. For example, to make a deposit or withdraw winnings in India you can use the next cost programs: UPI, PayTM, Astropay, Exopayz, in Japan – umoPay, JCB, VenusPoint, and in South Korea – Master, neteller, skrill. CPA provide – here the cost is made for the primary deposit (FTD) from the lively player. How to deposit and withdraw winnings at Bons Casino? For cooperation with Bons on-line casino associates program, visitors to playing from India, Japan and South Korea is required.
Look at my web page :: https://roobytalk.com/the-official-bons-casino-website-is-the-most-secure-place-to-play/
This is nicely expressed! !
Feel free to surf to my homepage :: http://exhibition.busan.kr/bbs/board.php?bo_table=free&wr_id=49076
As soon as we tested the chip and the digital camera snapped dozens of pictures with out having to press a single button we then added the wires to the surface of the digicam. To do this we simply soldered two wires directly from the leads. This week’s How-To Tuesday is a two parter; this week we show how to convert that outdated digital camera you are acquired in your closet to one that takes an image routinely each second until the reminiscence card is full, which can we use in subsequent week’s How-To, where we’ll put that camera on a kite. So that is it for this week, subsequent week we’ll present you find out how to mount the hacked digital digital camera to a kite (and other issues) to take photos mechanically. We checked eBay and places like Fry’s Electronics and found quite a lot of crappy digital cameras that people will be in a position to make use of to take photos from kites.
Here is my website :: https://noprost.com/urologiya/phimosis/sinexii-u-malchikov.html
велосипедные прогулки: исследование предпочтений молодежи литература научной тексты по специальности «дисциплины о здоровье»
my page http://newsliga.ru/index.php?nma=cats&fla=stat&cat_id=6&nums=599
The one a part of RippleNet that uses the
XRP digital currency is its on-demand liquidity service.
Australia, the Euro Zone, the United States, Mexico, the Philippines
and Japan can at present use Ripple’s on-demand liquidity service.
Ripple’s centralized system does away with permissions and is more open to censorship
than other cryptocurrency platforms. It’s faster than bitcoin – taking a few seconds per transaction versus an hour or extra – and has
the potential to supply a better technique for completing international funds.
That community consists of a collection of banks and payment suppliers that have signed on to make use of Ripple’s blockchain network for international funds.
XRP has a maximum supply of 100 billion coins, all of which had been launched in an initial coin offering when the Ripple blockchain launched.
Bitcoin is an example of this kind of blockchain.
Stop by my web blog – xrp crypto
Hi my friend! I want to say that this post is awesome, nice written and come with approximately all important infos.
I’d like to look extra posts like this .
This design is incredible! You certainly know how to
keep a reader amused. Between your wit and your videos, I was almost moved to start my
own blog (well, almost…HaHa!) Wonderful job. I really enjoyed what you had to say,
and more than that, how you presented it. Too cool!
This establishment works with reliable fee services to make sure complete safety of monetary transactions. Participation in the gameplay and access to the total vary of companies is feasible after registration, which is carried out on the official website, in accordance with the established algorithm. The range of games is being actively replenished and new casinos are being opened. A wide range of bets allows to play for any amount. They will play for cash and for free in any place. To play for actual bets, you might want to register and fund your account the most convenient manner. Full freedom of action and actual winnings in the casino Bons get regular prospects. Regular clients reward the level of service offered and especially observe the excellent library of video games with recreation licensed slots. Regular customers take part in tournaments, promotions and jackpot drawings. They are invited to take part in tournaments and jackpot draws.
My blog – https://happn.blog/a-detailed-explanation-of-bons-casino-bonuses/
10 аксессуаров для airpods: прокачиваем самые популярные tws-наушники
My blog post; p19524
Howdy! best erectile dysfunction pills buy ed pills
With thanks. Awesome information!
Feel free to visit my web page :: https://www.wiklundkurucuk.com/istanbul-Law-Firm-nz
You revealed it fantastically!
сказка чтоли?
—
Мирка не кипятись!!! кофе полезен или вреден для организма, кофе сорт и отличия кофе
лучшие конструкторы веб-сайтов – плюсы, недостатки да что там сравнения параметров
Feel free to surf to my blog post :: 57622
анатомические матрасы для сна
Feel free to visit my blog: https://idps.in.ua/2022/12/03/de-mozhna-kupiti-v-kiyevi-yakisnij-matrats-na-lizhko/
fexofenadine coupon fexofenadine 120 mg no prescription fexofenadine online pharmacy
Hello! mens ed pills medicine for erectile
It’s going to be finish of mine day, except before end I am reading this fantastic piece
of writing to increase my know-how.
como funcionam os diurГ©ticos trabalho
Another test called a penile plethysmograph can be performed by individuals themselves at home. This test uses a contrivance to decide between palpable and psychological ED as a squire watches or listens to sexual material. Source: cialis cost per pill
Drugs advice in compensation patients. Long-Term Effects. walmart tadalafil price tadalafil tablets 20 mg india tadalafil 20mg dosage
I love what you guys tend to be up too. Such clever work and exposure!
Keep up the good works guys I’ve included you guys to my personal blogroll.
In the Jetsons, Judy’s 16 whereas Jane’s in her mid to late-30s, however they look to be more or less the identical age. Due to either Older Than They give the impression of being or Youthful than They give the impression of being (or both), a parent appears to be like about the identical age because the parent’s little one, sufficient to be mistaken for siblings. Many help conversations lampshade how the children’s dad and mom look extra like their siblings. In comparison to her daughter Wendy, Mary Darling from Peter Pan appears to be like like she may very well be her older sister. Rei Todoroki appears like she might be the older sister of her daughter, yet her daughter and oldest son are of their early to mid-twenties. Uta’s RomCom Manga Dubs: Kenta mistakes Himawari’s mother Yuriko for her sister as a result of she appears to be like younger than she actually is. Dr. Drakken assumes that Kim’s mom is her sister. In Fireplace Emblem: Radiant Dawn, Almedha seems to be a beorc lady in her early or mid thirties, a bit too young to be the mom of Pelleas (who seems to be in his early twenties).
Also visit my homepage – https://geoinno2020.com/image-post-format-2/
seroquel 300 mg coupon prescription drug seroquel seroquel 250 mg
Hello there! ed pills gnc erectile dysfunction drug
Thanks for ones marvelous posting! I quite enjoyed reading it, you will
be a great author. I will always bookmark your blog and definitely will come back at some point.
I want to encourage you to definitely continue your great posts, have a nice day!
Hi there! cheap erectile dysfunction pills ed pills otc
You’ll be able to borrow up to $35,000 and pay again the loan over time, which could be as brief as one or two years. You’ll pay interest on the mortgage quantity, which suggests your fee will increase over time. It means they will keep it until they’ve gotten all of their money back from you. It just signifies that lenders are much less more likely to belief their potential to pay again the mortgage with none problems. So, tracking how a lot you owe and when your payments are due is crucial. Then, decide how much cash you earn every month. Then, find out how a lot interest charges (and annual share charge) are on each loan by wanting online or calling lenders directly (if they’re available). Federal scholar loans are offered to eligible college students no matter creditworthiness. Scholar loans could be subsidized or unsubsidized, either federal or non-public.
Here is my web site http://loanexpert.ee/eng/
The next time I read a blog, Hopefully it doesn’t disappoint me
as much as this particular one. I mean, I know
it was my choice to read through, however I truly believed you would have something interesting to say.
All I hear is a bunch of complaining about something that you could
possibly fix if you were not too busy seeking
attention.
Check out my web-site … mazda vacaville
how to purchase avapro 300mg avapro 150mg medication avapro 150 mg for sale
How do you be a woman a man needs
Erectile dysfunction is one of the men’s sexy health disorders. It is cognized as an unfitness of men to attain erection during sexual carnal knowledge equable if they are sexually excited. Other symptoms of ED are, either it remains championing a transitory while or does not come off at all. It is a repeated process. Erectile dysfunction is also called a model of impotence. Powerlessness is a encyclopedic aspect and covers innumerable other men’s vigour reproductive disorders like- too early ejaculation, be deficient in of procreative pine, и так далее Erectile dysfunction does not connect with these problems. All these problems related to Erectile dysfunction can be cured with the daily help of mens viagra pills and other sildenafil 20 mg brand name medicines.
Causes
Erectile dysfunction does not take any well-defined cause. There are tons reasons behind its occurrence. It can be- true reasons, your form problems, medicines you are delightful, emotional reasons, и так далее Give permission’s enjoy a look on ED causes in particular. Erectile dysfunction causes are- momentous blood stress, diabetes, high blood cholesterol, staunchness diseases (Parkinson’s disease and multiple sclerosis), surgery, smutty hormone levels, lifestyle factors (smoking and drinking) and others (urgency, nervousness, nervousness, be afraid, cavity). Aging factors also prompt to ED, but aging in itself is not a cause. Low testosterone levels also in some cases advantage to erectile dysfunction. Side effects caused by medications also establish men unable for erection.
But there is nothing to trouble far as treatments are on tap with a view ED. One such present treatment representing ED is mens viagra pills.
Hi there! ed pills otc bing mixed ed
Great site you have here.. It’s hard to find excellent writing like yours these days.
I truly appreciate individuals like you! Take care!!
viagra 100mg street price viagra canada prescription viagra over the counter
Howdy! buy ed pills online non prescription erection pills
Court docket documents show the state may potentially name well over 300 witnesses, including prominent rap world figures like Lil Wayne. It is removed from the first time hip hop lyrics have featured in courtrooms, a observe that’s sparked controversy quite a few times over the past many years. Related legislation is pending in the states of latest York and New Jersey, and last summer time the RAP Act, aimed toward protecting artists’ first amendment freedom of speech rights, was launched in the US Congress. Controversially, prosecutors are holding up rap lyrics from musicians together with Younger Thug as well as Gunna — who was additionally charged however took a plea deal — and even a bar from a posthumous Juice WRLD single. His 2019 e-book with Andrea L. Dennis, “Rap on Trial: Race, Lyrics, and Guilt in America,” holds that courts routinely take slice-of-life lyrics out of context to criminalize and imprison each skilled rappers and aspiring artists who are primarily Black and brown.
Also visit my page :: https://www.sdmt.org/union-tribune-review-next-to-normal/
Chiropractic care is safe for all ages from birth to senior years.
As portal of entry providers, many chiropractors will additionally send out narrative reports to the primary care physician detailing their examination findings and treatment
plan. If you need chiropractic care and are in Elkhorn or nearby in West Omaha, start filling
out our form today. She will create an individualized treatment plan that is effective
and catered to your personal lifestyle and advise you of home
care that will will expedite the positive outcome. The table has power elevation with a range
of 26 inches to 35.75 inches, customized to your personal working height.
Chiropractors are THE MASTERS of the ART and SCIENCE
of correcting and optimizing Nervous System disorders, problems,
and health maintenance. For 40 years our mission at Labelle Chiropractic
is to help as many people as possible, especially children, realize
that their body has the ability to heal itself and that the maintenance of health is far
superior to the treatment of disease. The success with treatment was so profound, Dr.
Lacey was motivated to change her career path and become a chiropractor herself.
Hello! best online pharmacy online pharmacy no prescription canada
Thank you for some other informative web site. The place
else may I am getting that kind of information written in such a perfect approach?
I have a undertaking that I am just now working on,
and I’ve been on the look out for such info.
prevacid 30mg tablet prevacid 30mg otc prevacid 30mg united kingdom
Howdy! Prescription Drugs Online order from canadian pharmacy
Les devises qu’on peut les trouver du casino sont le dollar canadien, le dollar américain, l’euro, le dollar australien, le round sud-africain, La livre sterling et le rouble russe. Les jeux populaires sur ce casino sont Jungle Spirit, Jimi Hendrix, Warlords Crystals of Power, Jack and the Beanstalk, Motorhead, Starburst , Gonzo’s Quest, Aloha Cluster Pays, Butterfly Staxx, Joker ProWild Wild West, The Invisible, Man, Gretel, Dracula et Hansel aussi que de jeux de table, de blackjack , de poker et quelques-uns types de roulette. Elle est considérée comme le meilleur site de jeux virtuels en ligne en France. Une Fiesta Casino est une plateforme française de pari virtuelle en ligne, elle contienne des jeux en ligne gratuits, comme blackjack, machines à sous, La roulette et autres. Une large gamme de méthodes de paiement disponible par Une Fiesta Casino virtuel est : Skrill, Moneta, WebMoney, EntroPay, MasterCard, Visa, EcoPayz, Yandex, PostePay, Paysafecard et Neteller. Aussi qu’un montant de 3000 euros seront divisés sur les trois premiers dépôts que le joueur exécute concernant La Fiesta Casino.
Look at my blog … http://www.boucleur.com/forum/user/lynge64bragg
can i buy seroquel online buy seroquel online price seroquel 300 mg
I am sure this post has touched all the internet people, its really really nice
paragraph on building up new webpage.
I am really impressed with your writing skills and also with
the layout on your weblog. Is this a paid theme or did you modify it yourself?
Anyway keep up the excellent quality writing, it’s rare to see a great blog like this one today.
I like the helpful information you provide in your articles.
I will bookmark your blog and check again here frequently.
I’m quite certain I’ll learn a lot of new stuff right
here! Best of luck for the next!
Hi there! india online pharmacy pharmacy online Canada
скачать фильм отступники
скачать фильм табор уходит в небо на телефон
фильм фартовый скачать бесплатно
5) It is not necessary to set a deadline in circumstances covered by part 58 (3) no. 1; the foreigner will probably be deported directly from detention or public custody. A substantial concrete menace for health causes solely exists within the case of life-threatening or critical sickness which would significantly worsen if the foreigner is deported. 1. the foreigner has culpably violated section 404 (1) or (2) nos. 3) The short-term residence permit entitles its holder to take up employment if the Federal Employment Company has granted approval in accordance with part 39 (3); approval shall be granted subject to a labour-market check. 5) A foreigner who receives a pension from an institution in the federal territory will usually be granted a temporary residence permit if the foreigner lawfully resided within the federal territory for at the least eight years previous to his or her departure. 2) An grownup unmarried child whose deportation has been suspended, who’s the youngster of a foreigner whose deportation has been suspended and who has been repeatedly resident within the federal territory for not less than eight years on 1 July 2007, or, if the foreigner lives along with a number of minor, unmarried youngsters as a household unit, the place the little one has been continuously resident in the federal territory for at the least six years on the said date, by virtue of his or her deportation having been suspended, being permitted to remain pending the asylum determination or on account of a temporary residence or permanent settlement permit having been issued on humanitarian grounds, may be granted a temporary residence permit pursuant to part 23 (1) sentence 1 the place mentioned child was a minor on the time of getting into the federal territory and the place it seems, on the basis of the child’s education and means of life up to now, that he or she is able to integrating into the best way of life in the Federal Republic of Germany.
Также не грех разобрать возможный штука всяческих ареалов. Также раззвонены софтфоны, специальные программные разработки, с помощью коих только и можно выкозюливать отталкивающиеся растение. никак не забывайте, будто перешагивание держи воображаемый штучка дозволит урезать протори получи и распишись телефонию так в 40%. дабы обнаружить уместный проект, освоите совет с многих провайдеров. отнюдь не запамятовывайте, сколько в месяц полезно нагонять абонентскую платеж, дактиль какое сочиняет приблизительно триста рублей. крайний из перечня примечателен этим пользователю стоит не столько каждый месяц регистрировать абонентскую платеж, ведь и спонсировать укладывающиеся звонки. Они в свой черед дозволяют достигать укладывающиеся сигналы, коим поступают получай несуществующий нумер телефона. в течение кою цену ограничится возможный комната? Дороже ограничится закупочная деятельность гостиница 8-800. Цены завязываются ото 1800 руб.. Многие стартаперы как по мановению волшебного жезла урывают кажущийся реприза. В имеющий наибольшее значение случае штука зажигает код страны, адрес конкретного города равно без спросу пагинация. Это доставляет неопровержимый крестик – виртуальность давать выход потребный областной номерок телефона капля учетом геолокации владельца, коей побывал веб-ресурс конторы. Это разрешает явить престижность, выпятить клиентоориентированность да опеку касательно клиентах.
Feel free to visit my page https://womanka.com/dom/mozhno-li-vospolzovatsya-odnorazovym-nomerom-dlya-sms
One is a sector of employees whose well being and nicely-being rely on a office-specific set of sexual security measures — ones that work. In contrast, the National Institutes of Well being states Truvada is up to 99 p.c efficient in preventing HIV when taken every day. Which means not solely are “adult movies” themselves topic to lawsuits and fines, but contains any illustration of that scene — banner ads, nonetheless images, clips, even if they’re just on blogs that write about it. The way in which the initiative is written, any illustration of actual intercourse is subject to the regulation, even if you don’t see penetration. Meanwhile, porn performers and intercourse employees, and an extended record of medical and political organizations, oppose the proposition. To the bizarre voter, this seems like a no-brainer: Of course we want these individuals to have safer intercourse. The one thing all three of AHF’s campaigns — Truvada, condoms in porn, online hookups — seem to have in widespread is the notion that promiscuous persons are spreading illness, vis-a-vis the evils of trendy expertise.
my web site – https://newsneednews.com/lifestyle/how-the-porn-industry-can-change-your-life-in-modern-world/
十分な減量
порно мамки
Hi there! real online pharmacy online pharmacy india
{Кредит онлайн}
Hello! online viagra pharmacy legitimate online pharmacy
Po lewej stronie znajduje się menu z dostępem do strony wyników
wydarzeń sportowych i statystyk.
my web blog: parimatch
Hi! trusted online pharmacy online pharmacy
перевозка спиртных напитков на дом в режиме 24/7 столица рф. Подобрать алкоголь браузерные сутки
My web-site – https://100gramm24-omsk.ru
гра престолів українською
Wow, wonderful blog layout! How long have you ever been blogging for?
you made blogging glance easy. The total look of your
website is wonderful, let alone the content!
Here is my web site; zalando01
Hi there! buy cialis levitra and viagra mens erection pills
I have been browsing online more than 3 hours today, yet I never found any
interesting article like yours. It’s pretty worth enough for me.
In my view, if all site owners and bloggers made good content as you did, the internet will be much more useful than ever before.
leflunomide price leflunomide 10mg generic leflunomide medication
quetiapine 25 mg for sleep quetiapine 200 mg for sleep quetiapine 2 5 mg
I visited multiple web pages but the audio feature for audio songs existing at
this site is genuinely fabulous.
Hi! ed meds without doctor prescription buy erection pills
The two-tiered cake options a Funko-pop-inspired McCree on high with a flurry of bullets surrounding the base. With candy performs like this we will see why she mains McCree. T-pain said he originally struggled to seek out anyone who might make cake like his daughter wanted. It looks like China’s not content material to easily watch for over-keen avid gamers to seek out their method to a halfway home, with the government now taking some steps to curb the amount of online gaming kids partake in. It isn’t imposing a strict restrict, however, as an alternative forcing sport makers to put in so-known as “anti-addiction software” in their games, which might ramp up in-sport penalties if gamers play more than the government deems to be wholesome. Apparently, players will only get half the traditional amount points if they play greater than three hours, with no points awarded in any respect after the 5 hour mark.
Gamee merchandise embody the Arc8 games hub and G-Bots NFTs. In this week’s podcast we concentrate on Gamee’s launchpad app Arc8 – a web3 app obtainable in cellular app shops. Was ask Bozena about what they needed to do so as to ensure they’re complaint on cell platforms and how they’ve navigated being a web3 app on mobile units. Our visitor this week is Bozena Rezab, Co-Founder and CEO of Gamee. The payout takes time to obtain your money, sometime between 2 days up to 1 week so you have to consider that whenever you payout your cash from GAMEE. The winner of all the money for his or her weekly cash prize is different. • You don’t should pay a subscription otherwise you don’t must pay to make any money. • Everybody can play because the technical necessities are very low. If you enter the positioning you will see a list of the video games that you would be able to play.
It is with both pleasure and a good little sadness that we announce that TC3 is transitioning into a new format.
The content material of TC3 shall end up changed, in the style of an anthology, to
the unique OpenAccess publication series „Translation and Multilingual
Natural Language Handling” (http://langsci-press.org/catalog/series/TMNLP, TMNLP) in the LangSci Push. The first log website site has got been enclosed and offers moved to this short-term area down, at which the diary functions experience happened to be eliminated but the content material possesses been preserved. In the interim, TMNLP has got its very first very prosperous concern, with about 1,500 downloads from diverse areas within the initial two weeks after showing up; this year further issues are already in the pipeline and are to appear.
We likewise believe that that with our brand-new format we can offer the local community far better: on leading of edited amounts, which possess long been the power of TC3, we can right now also publish monographs (integrating dissertations). We happen to be shopping to unique effort forward!
Hi! cheap erectile dysfunction pills erectile dysfunction drug
Креативненько!
—
Присоединяюсь. Я согласен со всем выше сказанным. Давайте обсудим этот вопрос. 2 пин ап казино, скачать казино пин ап а также https://allesmitdir.de/?p=79#comment-19316 поддержка пин ап казино
Sports betting, football betting, cricket betting, euroleague football betting, aviator games, aviator games money – first deposit bonus up to 500 euros.Sign up bonus
can i order cheap lyrica pill how to buy cheap lyrica no prescription can you buy lyrica without insurance
Superb website you have here but I was curious if you knew of any discussion boards that cover the same topics discussed in this article?
I’d really love to be a part of group where I can get feedback from
other knowledgeable people that share the same interest.
If you have any suggestions, please let me know. Bless you!
Howdy! men’s ed pills best non prescription ed pills
YouTube has become one of the most well-liked video-sharing platforms in the world. From its humble beginnings as a platform for user-generated videos, YouTube has grown into a powerful tool for entertainment, education, and communication. Many people use YouTube to watch their favorite shows, listen to music, and follow their favorite creators.
If youre other to YouTube and desire to acquire the most out of your experience, here are some tips upon how to watch YouTube effectively:
The first step in watching YouTube is finding videos that you like. You can see through the homepages curated list of recommended videos or use the search bar at the top of the page. You can furthermore browse through categories such as Music & Audio, Gaming, Education & Science, and more. Additionally, you can follow channels that name content regularly and subscribe to them thus that you acquire notified gone they upload new content.
Once you locate a video that interests you, there are several ways to interact in the manner of it. First off, create certain to in imitation of or detest it fittingly that supplementary users can see how many people enjoyed it or not. Additionally, if theres something special virtually the video that stands out for you, subsequently leave a comment or ration your thoughts nearly it next additional viewers. By engaging subsequently videos in this way, you can encourage boost likes and shares from new spectators as competently as announce the creators channel on social media platforms such as Twitter and Facebook.
If there are fused videos from different creators that interest you, after that consider creating playlists appropriately that every these videos are in one area and easy for you to entrance whenever you want them. This is particularly useful if there are several channels that state content in a particular genre or subject that is interesting for you, such as cooking tutorials or speculative videos; handily ensue all these combined videos into one playlist thus they’re simple to locate whenever needed!
Another great showing off to tailor your experience upon YouTube is by adjusting various settings such as autoplay (which will automatically statute combined videos after each clip), subtitles (which will display text under each video), captions (which will display text above each video), and more! Additionally, if your internet attachment isn’t great, create distinct to get used to the playback air settings too; this will ensure that even later streaming exceeding slower connections, your experience remains smooth without any buffering issues!
Это необычно жизненно в случае роздыха в бане не то — не то сауне, где ценность напитков чрезмерно во пятого раз ранее обычных тарифов магазинов. Помимо писк налаженного сервиса примечательно оптимальную ставка алкоголя, кок доступна с целью любого клиента. в течение нашем сша ишачу специалисты, кои снабжают рьяную доставку напитков для семейка к каждого покупателя. круг символизированный получай нашем сайте спиртной напиток быть хозяином до предела достойным уровнем, фигли подтверждается наличием акцизов (а) также грамот что касается общепризнанных мерок действующего законодательства нашей государства. Все вышеперечисленные разновидности напитков во широком ассортименте существуют для портале нашей фирмы. Именно вследствие того воспретить жидкая валюта не без; доставкой буква нашей сопровождения – данное интересное резолюцию во в полном объеме милой условия. Благодаря труду нашей шатии доставка алкоголя итак не только общедоступной, но также вдобавок в высшей степени загоришься. ежели вас занимит доставка алкоголя сверху ронг круглосуточно, сиречь не представляющий трудности позвоните нам также устройте пара заказ. буде вам надобна фотоуслуга доставка алкоголя много Казани 24 часу в день, сиречь выше- веб-сайт – сие ответ темы. благодеяние доставки спиртного круглые сутки в Казани в конечном итоге прошел слух как никогда славной а также важной предложением исполнение) основного количества жильцов столицы.
Here is my web blog: https://100gramm24-kzn.ru
Knives will probably be in better and designated locations quite than being left lying on the working tops.Planning for the work is an excellent idea and a constant reminder of a choice effectively made.Many Realtors use this tip to place homes on essentially the most wished lists. The character of a kitchen will decide the well being of these within the house.If the room is neat and good, there are high feeling s of desirous to spend more time in it making healthy meals which is not the case in a plain looking room. Solely a professional service provider can differentiate between a cabinet and a wall.They’re tightly glued to offer the identical the room a cool look and that is why you must choose the classic means rather than nailing containers to the wall.This was the previous fashion of getting a cabinet, but it has modified over years. If you are looking for the details about custom kitchen cabinets Tampa locals can come to our net pages here.
мире-торговым центрам и магазинам откажут сектор обслуживания самогона
Also visit my homepage :: https://100grammchik-krn24.ru
striplife.ru
buy colchicine tablets
ivermectin horse paste for humans liquid ivermectin ivermectin dosage for cats mange
2310
topiramat viktminskning
trazodone generic trazodone cheap trazodone united kingdom
Todos os jogadores que entrarem em Red Dead Linha essa semana receberão até então 15 Barras de Oiro como bônus, fora incomparável extensão de
25% de XP e gaita em certas missões e perseguição ao riqueza.
Todos os jogadores que entrarem em Red Dead Linha catafalco semana receberão ainda 15 Barras de Oiro porquê bônus,
fora único elevação de 25% de XP e finanças em certas missões e caça
ao riqueza. Red Dead Redemption 2 recebeu uma série de novidades
em seu meio multiplayer Red Dead Online, entre elas novas missões em A Land of Opportunities,
além disso atividades Free Roam, e a soma de partidas de Poker com seus unido.
As novidades de Red Dead Redemption 2 e Red Dead Online já estão disponíveis no PlayStation 4 e
Xbox One. Por derradeiro a atualização traz uma notícia munição,
roupas e emotes. Por novíssimo a atualização traz uma notícia
recurso, roupagem e emotes.
Гей порнушка
How will communication between players be conveyed — through a chat field, solely by overhead chat bubbles, or one thing else totally? This triggered event will not give any structured interplay or cue to comply with but will lead gamers into discovering and interacting with things in alternative ways. We don’t want to guess at this; we want to get people involved and help us discover out what really does work and find ways to phase and push at the same time. But this is why we are stepping out from behind the curtain so early. We need to share our analysis with different builders, modders, and society as a whole — not one thing that will likely be allowed if control goes out the window. If gamers want a map with some type of monitoring system floating on their display screen, they will have to be equipped with the gear to show the map but also a gadget that reads and tracks motion in the realm they wished to monitor.
Feel free to visit my webpage http://new.atsvoronezh.ru/when-ny-city-was-the-prostitution-capital-of-the-us/
черная металлургия: диагностику неполадок отрасли
Also visit my web-site https://metalinfo.ru/ru/news/s13573m12.html
As an experiment, I tried to get by way of a mission by simply working via it, with out assistance from Vector’s invisibility talent. Vector’s invisibility talent solely made this tactic simpler and simpler. Residing opponents are even worse, as they’re going to simply interrupt your attack with their own, beginning an infinite melee chain that will merely destroy you — one thing that occurs extra usually than it ought to. You are abruptly outfitted along with your generic beginning gun, a couple of grenades and nothing else. So, in order for you to maintain using that awesome gun, or need some anti-viral spray to stave off your inevitable infection, don’t die. There is not any energy behind any of the weaponry, save for shotguns that will effectively knock a guy on his butt — only for him to stand up and stare at you till you shoot him again. Still, as Raccoon Metropolis began throwing out harder enemies in higher numbers, I just used the invisibility to sneak previous everybody and get to the following checkpoint.
my web site: https://baliescorts.net/
наилучшие калькуляторы голубого топлива
Feel free to visit my web blog :: http://www.avtosreda.ru/info/zadvizhki-30s527nzh-osobennost-konstrukcii/
Hi there, everything is going nicely here and ofcourse every one is sharing information, that’s really excellent, keep
up writing.
гей порно
Инцест порно видео онлайн
Hello there! buy valtrex buy valacyclovir no prescription
how to get pregabalin without a prescription buy cheap pregabalin pill can i get pregabalin without insurance
Howdy! purchase valtrex online no prescription order valacyclovir
доставка алкоголя на дом круглосуточно город. Выбрать алкоголь браузерные сутки
Stop by my web page :: https://100grammchik-surgut.ru
Symptoms of ED catalogue: Laboriousness getting an erection. Pitfall maintaining an erection long passably to procreative intimacy. Having erections that are not hard sufficiently in compensation penetration. Source: cialis online without pres
Is vodka good for men
Erectile dysfunction is one of the men’s propagative health disorders. It is cognized as an inability of men to attain erection during propagative commerce equable if they are sexually excited. Other symptoms of ED are, either it remains in behalf of a deficient rare while or does not befall at all. It is a repeated process. Erectile dysfunction is also called a standard of impotence. Frailty is a encyclopedic side and covers multitudinous other men’s fettle sensuous disorders like- untimely ejaculation, be deficient in of fleshly give one’s eye-teeth for, etc. Erectile dysfunction does not presuppose implicate these problems. All these problems mutual to Erectile dysfunction can be cured with the help of viagra pill walgreens and other how much is viagra per pill medicines.
Causes
Erectile dysfunction does not take any well-defined cause. There are many reasons behind its occurrence. It can be- natural reasons, your health problems, medicines you are delightful, nervous reasons, и так далее Excuse’s deliver a look on ED causes in particular. Erectile dysfunction causes are- momentous blood pressure, diabetes, loaded blood cholesterol, nerve diseases (Parkinson’s disease and multiple sclerosis), surgery, weak hormone levels, lifestyle factors (smoking and drinking) and others (urgency, anxiety, a case of the jitters, misgivings, cavity). Aging factors also supervise to ED, but aging in itself is not a cause. Bellow testosterone levels also in some cases lead to erectile dysfunction. Side effects caused close to medications also establish men unqualified in compensation erection.
But there is nothing to agonize give as treatments are on tap in place of ED. The same such available treatment representing ED is viagra over the counter united states government.
Ширма
My spouse and I absolutely love your blog and find a lot of your post’s to be just what I’m looking
for. Would you offer guest writers to write content to suit your needs?
I wouldn’t mind composing a post or elaborating on most of the subjects you write in relation to here.
Again, awesome website!
Wherever you live in the UK, we’ll match you with singles who complement your personality and we have members right across the country. Find singles in the UK’s main areas below and sign up today to meet compatible matches in your local area.
Singles in Scotland – From the Borders to Lewis, eharmony has been bringing Scottish singles together for over a decade. Visit our Scottish dating page to meet new matches, wherever you are in Scotland
Singles Northern Ireland – Our matching system means more quality dates with deeply compatible local singles who truly understand you. Find a lasting relationship in Northern Ireland with eharmony.
Singles in Wales – If you’re looking for a long-lasting relationship with someone who shares your values, try eharmony Wales today and meet like-minded singles.
Hi there! buy valtrex with no prescription purchase valtrex
Каким образом распознать пепельный iphone от белоснежного?
Check out my webpage; http://mockwa.com/forum/thread-127142/page-1/
Hello there! valtrex 500mg valtrex cheap
malegra 25 mg
Master all of this to really get an excellent handle on things. Such instructional audio visible clips are important since they can offer you some insight on how different individuals are capable of master languages based mostly on their experiences. Tutorial packs at the moment are available for users the place they’ll study interactively via games and other enjoyable methods. You possibly can have such items delivered to your home after ordering them by means of on-line retail retailers, or you could buy these titles at any bookstore near your area. Above all, have fun with the method and at all times keep your mind open to new and thrilling experiences. Earlier than anything, have some primary information on a specific tongue you plan on reaching decent articulacy. Never let your speech therapy Tucson AZ get in the way of studying very important info that could very nicely help you in reaching your desired objectives. Learn the main points below to seek out out extra pertinent particulars on studying new tongues.
Hello! order valacyclovir valtrex 500mg
https://propiska-msk03.ru
Hi there! buy valtrex 100 mg buy valtrex usa
транспортировка цветов по москве
Also visit my blog – https://khimki.mybloom.ru/
Make probably the most of patio season with an excellent
selection of heaters, out of doors fireplaces, hearth pits,
and more.
Thank you for some other wonderful post. Where
else may just anyone get that kind of information in such an ideal way of writing?
I’ve a presentation next week, and I’m at the search
for such info.
Hi, i feel that i noticed you visited my site so i got here to
return the choose?.I’m attempting to find issues to enhance my
site!I suppose its adequate to make use of some of
your ideas!!
Feel free to visit my page; lexus san jose
Howdy! valacyclovir buy valtrex with no prescription
where can i buy cheap propecia price order cheap propecia without prescription can you get cheap propecia pill
striplife.ru
har technoblade kræft
Hello! buy valtrex with no prescription buy generic valtrex
I’m not sure exactly why but this web site is loading extremely slow for me.
Is anyone else having this issue or is it a issue on my end?
I’ll check back later and see if the problem still exists.
Hannah Ann moved on with Jake someday through the latter a part of 2021, although
they refrained from discussing their romance in public for months.
They went public as a couple on the eve of final
yr’s Tremendous Bowl the place Jake’s then team, the Los Angeles Rams, triumphed over the Cincinnati Bengals.
On multiple occasions, he says, OnlyFans told him he over-moderated,
particularly in relation to movies exhibiting sex in public and to “third-occasion” content – material featuring people not registered with OnlyFans.
One skilled in content moderation says the paperwork clearly present
that OnlyFans has “some tolerance” for unlawful materials.
On that present she was one of the ladies vying for the affections of Peter
Weber, who was often called ‘Pilot Pete’ because of his profession. One win away.
Already so proud. Swank: Jake could possibly be briefly glimpsed toasting and grinning at Hannah Ann earlier
than the digital camera panned to the phrase: ‘she stated yes!
Jake may very well be briefly glimpsed toasting and grinning at Hannah Ann earlier than the
digicam panned to the phrase: ‘she stated sure!
Here is my site xxxx
Hi! buy valtrex no prescription buy valtrex no prescription
Superb posts. Many thanks.
Feel free to visit my site :: https://medium.com/@slivsignalov126
Hi there! purchase valacyclovir buy generic valtrex
Пин-ап – что перед вами такое?
Look at my web blog – пин ап бет зеркало
buy lamotrigine lamotrigine 50mg united states lamotrigine nz
obviously like your website however you have to take a look
at the spelling on quite a few of your posts. Several of them are rife with
spelling issues and I find it very bothersome to inform the reality then again I’ll definitely come back again.
аниме-сериалы встречаются умопомрачительно низкими (занимательные)
Look into my blog: https://ururuanime.online/
Howdy! buy valtrex no rx valtrex cheap
I don’t know if it’s just me or if everybody else experiencing
problems with your site. It looks like some of the
text on your content are running off the screen. Can somebody else please provide feedback and let
me know if this is happening to them too? This may be a problem with my
browser because I’ve had this happen before. Thank you
Howdy! buy valacyclovir no prescription buy valtrex no prescription
Cultures and societies throughout history need revered bigger young women and thus do you! While the ideal physique sort has modified and progressed over the years, we now find ourselves in a time when all entire body shapes will be commemorated. This restored self-confidence offers assisted form a fresh technology of hardcore performers and allows fill a void anxious audiences. Nowadays we get huge young girls in all forms of naughty difficulty. There are BBW gangbangs, chubby spouse writing, plus-size products at have fun with and thick Lesbians employed in scissoring perhaps, strap-on have fun with and everything else nearly. Plumpers right now have even more option than ever before when it arrives to lingerie, intercourse gadgets, cosplay and roleplay shenanigans. Discover what you’ve become lacking and never resolve for an partial series once again.
I really like your blog.. very nice colors & theme.
Did you make this website yourself or did you hire someone to do it for you?
Plz reply as I’m looking to create my own blog and would like to know
where u got this from. cheers
prp for hГҐrtap
nakushetke.ru
Hi there! buy valtrex online buy valtrex no prescription
магазин для новорожденных доступной, тогда качественной мебели на столице
Also visit my webpage … https://www.fabrika-moscow.ru/decors-mebel
миграционный городской центр mom
My page – https://xn--l1aagmw.xn--p1ai/
покупка жилья в минске не слишком дорого
Check out my homepage: https://stayminsk.by/
онлайн номерок для приема сообщение
my web page – http://ruainform.com/news/osobennosti_registracii_v_fejsbuke_bez_nomera_telefona/2022-11-06-26596
Regardless of the large amount of knowledge in the Parimatch sports betting site, like stats and streaming, not
to say the sheer variety of betting markets, the site pace is speedy.
Does Parimatch Sports have a mobile betting app? Some have decided to start taking prop bets on the COVID-19 pandemic itself.
Some of the bets supplied are on the chance
of a vaccine being developed and what date Moscow could be shut down in response to the virus’s spread.
By way of Virtual Sports activities, there are 5 suppliers’ virtuals on supply, giving Parimatch prospects
over 30 to select from. There are no matches, so bookmakers
had to provide you with one thing,’ gambling beat journalist
Pyotr Kondakov sad in an interview. The closures have
come along with mass layoffs at many properties.
Plenty of online gambling retailers in the US have
had to be equally inventive to keep revenue coming in through the COVID-19 pandemic.
Here is my web site parimatch india
Hi! purchase valtrex buy valtrex online without prescription
Howdy! I know this is somewhat off topic but I
was wondering which blog platform are you using for this website?
I’m getting sick and tired of WordPress because I’ve had issues with hackers and I’m looking at alternatives for another platform.
I would be fantastic if you could point me in the direction of a good
platform.
Hello! I realize this is somewhat off-topic but I
needed to ask. Does operating a well-established blog such
as yours take a lot of work? I’m brand new to running a blog however I do write in my journal everyday.
I’d like to start a blog so I can easily share my personal experience and thoughts online.
Please let me know if you have any recommendations or tips
for new aspiring bloggers. Appreciate it!
prednisone buy online prednisone 10mg pack prednisone by mail
This text is priceless. Where can I find out more?
776227047
Let me inroduce myself, my name is Nestor and Doing well . it
sounds quite good when you say it. One of the things she loves most would
keep bees and she would never cease. Distributing production is just how I make money but soon my
wife and I’m going to start our new business. Northern Marianas Islands is where her home is.
https://Knowyourmeme.com/users/michael-braun
Hello there! mexican online pharmacy cialis online pharmacy
Kudos! I enjoy it!
While previous years have been controversial, the 2023 season options a ‘twisted’ challenge from the consultants – encouraging the cast to swap partners. They made totally different couples swap companions for three days and it was hell for all concerned,’ the insider added. As previously reported by Daily Mail Australia, an insider let slip: ‘They’ve actually upped the ante this 12 months. A manufacturing supply has let slip that Tayla will confront her groom, beforehand identified as Hugo Armstrong, through the collection after a butt-dial revealed what he actually considered her. Also, we wish to let you recognize that we do not see a HD DVD launch drought within the foreseeable future. Here is all the things it is advisable to know forward of the first episode. The new season will function more highly addictive drama when the experiment is rocked by scandal in an explosive MAFS first. The sequence will even be rocked by a C-bomb scandal, after a groom labels his bride Tayla Winter ‘a nightmare’.
Also visit my web blog: https://www.taylormadelandscapes.com/portfolio/xeriscape-4/
порно по категориям
If you’ve acquired bike lights that sit near the bar, you might have to relocate them to the top tube, and then find it’s not as helpful a spot to stay them. Like powering up a hill, or sitting between cars at the lights, understanding that you’ve acquired the electric energy to not get chewed up when we’ve got to start out. The company produces a retrofit e-bike kit that may be easily bolted onto existing bicycles, giving them a brand new lease of electric life. That mentioned, a Swytch equipment and an analog bicycle is commonly far cheaper than all but the most primary (and ugly) of new e-bikes. Each the manga and the nonetheless-working anime offshoot have been profitable, with the manga racking up over sixty five million sales up to now. Anime and manga adaptation veteran Shinsuke Sato (Alice in Borderland, Bleach) will each direct and government produce, while Obi-Wan Kenobi’s Joby Harold is writing the screenplay. Toho, which handles the anime, will distribute the film to Japanese theatres.
Here is my homepage https://tempsdeparoles.fr/temps-de-parole-managers-conseils-astuces/
lastduel.ru
Hi! best mexican online pharmacy mexica online pharmacy
Временная регистрация в Москве
кресло-кровать без подлокотников
Check out my web site … https://vammebel.ru/catalog/kreslo-krovat/bez-podlokotnikov/
Good post. I’m facing some of these issues as well..
motilium over the counter australia
Hi! online pharmacies mexican online pharmacy reviews
The edges turn out to be frayed as effectively as the surfaces scratching off the printing sooner
or later. Layer serves as safety not just for the card but additionally for the
print that’s marked on the surfaces. Paper taking part in playing cards have
been in existence in all probability since the first playing card was invented.
“This is essentially the most frequently requested query in the playing card business, which is best a paper primarily based taking part in card or a plastic based mostly enjoying card? As soon as the creases and folds appear, the playing cards won’t be suitable for enjoying. This materials can endure the abuse of gamers and is not susceptible to folds and creases. The tension of the play makes them unconsciously grip the card tightly leaving crinkles or folds. These playing cards usually encompass 1 to three plies of card inventory material then coated over with varnish. The card is still as agency because it had been when it was new even when the printing has already worn out.
Here is my web page – https://arto-usolie.ru/user/lydeenjdle
Aw, this was a very good post. Spending some time and actual effort to generate a good article… but what can I say… I put things off a
lot and never manage to get nearly anything done.
Tips certainly regarded!!
my site: http://deafrm.ru
Hello! mexican online pharmacies online pharmacy review
Howdy! indian pharmacy online online pharmacy mexica
Great article! We are linking to this great post
on our website. Keep up the great writing.
I like the helpful info you provide in your articles. I’ll bookmark your weblog and check again here frequently.
I’m quite certain I’ll learn a lot of new stuff right here!
Best of luck for the next!
suhagra 100mg buy online
Highly energetic post, I liked that a lot. Will there be a part 2?
continuously i used to read smaller content that also clear
their motive, and that is also happening with this article
which I am reading at this time.
Good day I am so happy I found your webpage, I really found you
by error, while I was researching on Aol for something else, Regardless
I am here now and would just like to say many thanks for a marvelous
post and a all round entertaining blog (I also
love the theme/design), I don’t have time to read through it
all at the minute but I have bookmarked it and also added your RSS feeds, so when I have time I will be back to read much more,
Please do keep up the excellent job.
Hello there! mexican pharmacy online mexican pharmacy online
k-tv.ru
Since the first issue was reported, all consequent Writers are actually evaluated twice and the tooling has been modified to fix the problem, so it will not occur in any other Writer. The primary era Writer was designed and constructed for the original iPad. The plastic body around the iPad adds further safety from impacts across the edges, but I would not suggest dropping it a couple of ft onto a concrete floor or tossing the iPad out of an airplane. The on-display screen keyboard key is particularly helpful if you don’t need to enter settings to show off Bluetooth whenever you eject the iPad. The keyboard feels implausible. When the case is folded up, the black-keyed keyboard is set to go to sleep so as to keep from draining the batteries. Personally, I hate using a case with the iPad when I’m sitting round browsing, studying or gaming — there’s simply one thing wonderful about how the iPad has been designed that makes it a disgrace to cover so much of it up.
Check out my web site; https://portalbcn.com.br/jogos-escolares-de-barbacena-sao-retomados-nesta-semana/comment-page-44/
1651
79
buy arimidex 1mg pills buy anastrozole generic purchase arimidex without prescription
Hello there! This post couldn’t be written much better!
Going through this article reminds me of
my previous roommate! He always kept talking about this.
I am going to forward this information to him. Pretty sure
he’ll have a good read. Thanks for sharing!
Thanks for your personal marvelous posting! I certainly enjoyed reading it,
you’re a great author.I will remember to bookmark your blog and definitely will come back
in the future. I want to encourage you continue your great writing,
have a nice evening!
Hi there all, here every one is sharing such know-how, therefore it’s good to
read this web site, and I used to visit this web site every
day.
furosemide tab 40mg furosemide cat furosemide
This post will assist the internet viewers for setting up new weblog or
even a weblog from start to end.
Hello! legitimate online pharmacy trusted online pharmacy reviews
Postapotheek.com is hét online adres voor het kopen van medicijnen zonder recept.
Al ruim 10 jaar verkopen wij via onze webshop geneesmiddelen en gezondheidsproducten aan consumenten in Nederland en België.
Wij zijn gespecialiseerd in de verkoop van geneesmiddelen zonder recept, zoals paracetamol,
ibuprofen en luchtwegverwerkers. Daarnaast bieden wij een ruim assortiment aan gezondheidsproducten, zoals vitamines, mineralen en voedingssupplementen.
It is not my first time to go to see this site,
i am browsing this web page dailly and obtain fastidious facts from here all
the time.
Hi there! buy propecia pills propecia online
40
43
1383
1511
1328
999
Can you tell us more about this? I’d care to find out
more details.
antibakteriell lotion
Hi there all, here every one is sharing such know-how, thus it’s pleasant
to read this webpage, and I used to go to see this webpage every day.
Cultures and communities throughout background need revered bigger young ladies and as a result conduct you! While the perfect body system variety includes modified and advanced over the ages, we today discover ourselves in a period when all human body shapes happen to be commemorated. This restored self-assurance offers helped form a different era of hardcore performers and allows fill a void ready audiences. Nowadays we come across large ladies in all styles of naughty difficulties. There are usually BBW gangbangs, puffy wife sharing, plus-size types at take up and thick Lesbians involved in scissoring actually, strap-on have fun with and everything else nearly. Plumpers have even more solution than actually when it comes to lingerie now, intimacy toys and games, cosplay and roleplay shenanigans. Check out what you’ve happen to be absent and in no way mend for an partial collection once more.
Hi! I’m at work browsing your blog from my new iphone 3gs!
Just wanted to say I love reading through your blog and look forward to all
your posts! Keep up the superb work!
Hello! buy propecia online without prescription buy propecia no rx
It’s really very complex in this busy life to listen news on TV, therefore I only use internet for that purpose, and take the hottest information.
We are aware that canine come down with mange and that affliction is a variant of scabies. Permethrin is secure for use with scabies conditions seen in infants right down to a number of months outdated. Physicians may recommend Lindane for scabies remedy, although there are a number of issues that each person should qualify for in order to make use of it. If you have to choose, Elimite is your greatest alternative because of its decrease toxicity rating in regard to human use. Luckily, medical doctors and science have discovered what needs to be completed for profitable scabies therapy. The thought of really having to deal with scabies for seven years is pretty powerful. An old school time period for scabies was the Seven yr Itch. The Latin time period for scabies, which means to scratch, is scabere. Lindane, though it’s used for scabies, has many considerations related to it.
My web-site: https://www.articladihatti.com/indibet-casino-play-online-with-bonus/
Undesirable human body hair can be a problem for equally guys and females no no hair removing. If you wish to change into supplemental absolutely sure as regards to the use belonging to the Revitol Hair Removing Cream, you possibly can nonetheless begin by executing a patch test together with your pores and skin. You in all probability have this problem – Does Revitol hair elimination cream give good outcomes, scan on… The merchandise includes a tested risk-free formulation which may be fairly easily put into use on large human body areas which will have undesirable hair progress. The mixture of distinct bio-energetic extracts operates on loosening the hair follicles and stops them from creating back once more – preserving the hair progress at bay to your for an extended time time frame as compared with standard hair elimination lotions. All it’s a should to do is usually to use the cream on the not so huge neighborhood of one’s skin with undesirable hair for particular duration of time then rinse off by having a damp towel.
Feel free to visit my web site – https://www.shoppalacebeauty.com
Hello! buy propecia pills buy propecia cheap
prilosec 20 mg united kingdom how to purchase prilosec 10mg prilosec without a prescription
On Google Maps you’ll be able to obtain a map of your destination to make use of offline. Most airline playing cards work in the same way – we’ll use the British Airways American Categorical Premium Plus for example. Reward credit score playing cards let you earn points with everyday spending to make use of towards flights and lodges. Check in case your credit card or loyalty schemes provide lounge entry. Plus, ensure you’ve a European Medical insurance Card (EHIC). For those who desire money, it’s finest to withdraw from an ATM at your destination using your UK debit card. Some airports are introducing new bag scanners that allow unlimited liquids via however you by no means know if you’ll be using them. Regardless of a doable looming recession, Britons are booking holidays and flights in vast numbers – as many make up for years of missed breaks in the course of the pandemic. Cashback websites equivalent to Quidco or Topcashback have offers when booking.
Also visit my web site; https://cheap-airportparking.com/toronto-airport-parking/
Hello there! propecia online buy propecia online
Wow, amazing weblog format! How lengthy have you ever been blogging for?
you make running a blog glance easy. The total glance of your website
is magnificent, let alone the content material!
elavil canada
Hi it’s me, I am also visiting this website daily, this site is truly good
and the users are really sharing fastidious thoughts.
college application essay pdf case study of a patient what person should you write in a college application essay
Howdy! buy propecia medication buy propecia medication
Select one or more software updates from All Software Updates node. Download software program updates from the Web: Select this setting to download the software program updates from the location on the web. This setting is helpful when the pc that runs the wizard would not have web access. Any computer with internet access can preliminarily obtain the software updates. You’ll be able to change the bundle source location within the deployment bundle properties after Configuration Supervisor creates the deployment package. If you wish to obtain the software updates earlier than you deploy them, you should utilize the Download Updates Wizard. There are several methods available to you for downloading software program updates in Configuration Manager. Within the All Software program Updates node, Configuration Manager displays only software program updates with a Critical and Safety classification that have been released within the last 30 days. Within the Configuration Manager console, go to the Software Library workspace, and choose the Software Updates node. On the Download Location web page, specify the situation that Configuration Supervisor uses to download the software program update source files.
Feel free to surf to my page https://softwarehomestore.com/
Thanks , I have recently been searching for information about this
subject for a long time and yours is the best I have found out so far.
But, what in regards to the bottom line? Are you certain in regards to the
supply?
компания пэкинг маг – подарочная тара от производителя
Also visit my webpage:
↑ Как выглядят облачный майнинг?
Here is my web page; http://users.atw.hu/handsupforum/viewtopic.php?p=82400
видеоигры для playstation 4 – цены, скидки
My page … https://playstation-russia.com/
Hey there I am so delighted I found your
webpage, I really found you by error, while I was looking on Digg
for something else, Regardless I am here now and would just like to
say many thanks for a marvelous post and a all round interesting blog (I also love the theme/design),
I don’t have time to read it all at the minute but I have bookmarked it and also included your RSS feeds, so
when I have time I will be back to read a great deal more, Please
do keep up the superb work.
For journeys between the airport and Newark Liberty Airport Station, there’s a price of $7.Seventy
five (free for youngsters below 11 years outdated). Newark Liberty Airport is simple to navigate by riding the handy AirTrain between terminals.
Terminals A, B, and C usually are not linked to each other through walkways so
it’s best to ride the AirTrain with providers operating every three minutes during peak hours.
Trains depart each three minutes from 5 a.m.
Regular shuttle buses operate each 5-7 minutes between the parking lot and terminals.
To connect with Terminals A or B, passengers can journey the shuttle bus that departs from close to gate C70.
Metered taxis can be found from outdoors all terminals with taxis to New York Metropolis costing $50-$70, depending on your destination (excluding tolls and tip).
Express Bus: You’ll be able to take the Categorical Bus
to New York Metropolis with the NYC stop, depending on which terminal you depart from at the airport.
Aviation followers will love that many rooms
have views of the airport, so you can do some airplane spotting while you sip your morning espresso.
Here is my homepage newark airport parking charges
Hello! buy finasteride pills buy propecia uk
Howdy! This post could not be written any better! Reading this post reminds me of
my old room mate! He always kept talking about this. I will forward
this page to him. Pretty sure he will have a good read. Thank you
for sharing!
In addition to balance adjustments targeting Lifeline, Seer and Wraith to begin, the developer is including a reworked class system. Each class will have access to a singular perk. A kind of changes is a game mode players have been asking Respawn so as to add since launch. The season may also add a brand new power weapon known as the Nemesis for players to grasp. And with the game’s 16th season set to debut on February 14th, developer Respawn Leisure is promising to shake issues up. At the identical time, Respawn is eradicating Arenas, the game’s current spin on deathmatch. In the beginning of a deathmatch game, you’ll choose your character and one in all 5 weapon loadouts. Season sixteen won’t see the introduction of a brand new playable character. Respawn has promised to share extra information about all of the Legends changes closer to the release of the brand new season. It wouldn’t be much of an anniversary season if the sport didn’t have something for gamers to gather.
Also visit my web-site: http://shootingartwork.com/peace-on-earth-a-wonderful-wish-but-no-way/
Nowadays, a lot of games come with online multiplayer baked in. But what about your favourite retro games that don’t even have servers online anymore? Stardew Valley co-op makes multiplayer easier than ever now that the farming simulation has online and split-screen options to play with friends. You can mix and match how you and your friends collaborate on your farm with options for splitting resources and controlling how your game operates while multiple farmers are present. Stardew Valley co-op works around your playstyle. To get started with this exciting new feature, you just need to join Steam Client Beta and then launch the game you want to play. Afterwards, you can access your friend’s list on the Steam overlay and invite them using the option Remote Play Together, which they would have to accept.
https://edgaronkh073285.goabroadblog.com/18860146/car-games-to-play-for-free
To enjoy the CBeebies website at its best you will need to have JavaScript turned on. Juni’s online math classes for kids is built for middle and high schoolers who want to reinforce their skills and get ahead in mathematics. We offer math courses for all kids ages and experience levels from Elementary Math through AP Calculus. Great blogs share the fantastic information. Its really funny games for children and the children have also a plus to learn from these games. The best games for girls is dress up games also a creative games. I’ve put the list of fun party games together primarily for the purposes of keeping kids entertained at younger children’s (toddlers, under-fives and up to ten-year-olds) birthday parties, but pretty much all the games are great for older kids and adults.
Hello there! buy propecia medication order finasteride
стильная дамская одеяние zarina
Look into my blog; https://auto-megamarket.ru/
profylaktickГЎ antibiotika
Hi there! purchase propecia buy finasteride no prescription
ф е василюк
кончил в рот порно видео
where can i buy verapamil cheap verapamil 40 mg where can i buy verapamil
Hello there! buy generic propecia order finasteride
“What I discovered at Amazon was a lot greater than that”, she says, “I bought appreciation and recognition.” In her first function as a Customer service associate, she enjoyed interacting with different teams, and gained insights into various areas like social media and GDPR. Relating to her own tasks, she likes the liberty she’s given to convey and implement new concepts, like the brand new mechanism she got here up with to escalate errors in the system rapidly and sustainably. She’s significantly committed to their skilled growth. She decided to take a step forward in her career and grow to be a workforce supervisor via one in all Amazon’s internal coaching applications, which gave her the information and instruments she needed. When he shouldn’t be at work, you will discover him tuning one in every of his guitars or organising a sport of padel. The Customer service team has a really clear goal – to prevent, remedy problems and delight our customers.
Here is my site https://pdfwork.online
We stumbled over here by a different web page and thought I might check
things out. I like what I see so now i’m following you.
Look forward to exploring your web page again.
Hi! buy finasteride pills buy generic propecia
AMD additionally made a splash two CPUs and a GPU. The beefiest of the bunch is definitely the new Ryzen 9 7950X3D CPU which packs an insane 144MB of cache utilizing the company’s 3D V-Cache technology and reaches boost speeds of 5.7GHz. The opposite two AMD bulletins focused on the cell side, together with the primary RDNA 3 GPUs for laptops and a lineup of performance-focused Ryzen HX CPUs. One other company focusing on raw power this CES was Razer which announced two new laptop fashions – the Blade sixteen and Blade 18. They’re loaded to the brim with excessive-finish parts like Intel Core-i9 HX chips and NVIDIA’s high-of-the-line RTX 4090 graphics cards. It announced two laptops, a giant tablet, an e-ink notepad and even a “Think” branded cellphone. The Sony announcement that made the biggest splash although, might have been that the endlessly delayed Gran Turismo movie is coming out in 2023. Personally I’m not a giant fan of the Gran Turismo collection, or racing games in general, however even I obtained a bit excited watching the trailer.
my webpage; https://abadiasietamo.es/terraza-verano-abadia-sietamo/
промокод на 1xbet
Adult porn integrating women who possess big natural tits present variety of lustful activities to carry out for the elements you are able to carry out with many of these massive, pure bust might be as big as they are generally. Hence what can you see in porno containing big natural tits accurately? First of all, they are perfect for motorboating totally, who is not into motorboating? Every person has fantasized about staying in between two sufficient chest and attempting the brrr sound. Licking and consuming it out and about are usually not for they may be full and enormous about your mouth area adequate. 2nd, every male has got dreamed, at least after, big pure tits porno will deliver you dreams you’ve never considered you experienced. This will be called the mammary intercourse, your excellent non-penetrative sex that will let you to find yourself cumming on her face as you scrub in between her breasts. 3rd, Chest are able to end up sensitive and manufacture sensual simulation than pain if done gently rather. Some are patting between the girl’beds bust or perhaps the cum available while else that she likes to use already. For a lady with less than large busts, they can create a minor valley for the penis to slide in. Just about all of the enjoyment to the penis in this case will be from the hands that overlap the chest and holds the penis down.
For hottest news you have to pay a quick visit internet
and on world-wide-web I found this web site as a finest web site for hottest updates.
Elon Musk has received the backing of some of the world’s wealthiest buyers for his $44 billion takeover of Twitter. Brookfield Asset Administration actively participates in numerous industries and economies across the globe and at the moment has $688 billion USD in belongings beneath management. The wedding was attended by Trump and his spouse, Melania, billionaire real estate investor and hotelier Barry Sternlicht, developer Don Peebles and former baseball star Alex Rodriguez, among others. Information of Witkoff’s funding comes just days after Steven’s son, Witkoff Capital President Zach Witkoff, married mannequin and actress Sophi Knight in what some are calling the ‘wedding ceremony of the yr’. The event was held at former President Donald Trump’s Mar-a-Lago property in Florida, in line with The true Deal. David Elfenbein is at present serving because the agency’s president. According to the agency’s website, it seems to be to invest in companies that are ‘building disruptive business across sectors’. Based on its web site, Aliya represents and manages an ‘unique neighborhood of households’ aiming to create ‘limitless value’.
My web blog https://telegra.ph/Psst-This-Article-Has-The-Secrets-About-Real-Estate-Investing-You-Want-To-Hear-01-20-3
израильская косметика. Самобытности тогда достоинства
Feel free to surf to my homepage; Израильская косметика
Then purchase it (all include a 30-day money-back assure) and download it on your gadget. Some Binance VPNs are cheaper, but here you may have a no system restrict. Even crypto traders should have some time off. The same applies to crypto traders in different international locations the place the Binance platform is blocked. Usually speaking, good speed will allow you to browse Binance extra effectively. You’ll be able to select from over 750 servers in more than 37 nations. You can get NordVPN for $3.49/month. For a deeper investigation of NordVPN, read our NordVPN review. NordVPN is the perfect VPN for Binance unblocking in 2023. It has servers in Canada, Mexico, and different areas where this crypto buying and selling platform is offered. Torrenting is obtainable in locations the place it’s legal. It’s also one of the cheapest and finest general. 50 nations. We appreciated that four of them are in Mexico (IPVanish is one in every of the top Mexico VPNs too), with over 50 in Canada. One account will get a six-device restrict, but you may enhance it by setting up this Binance VPN on your router.
Here is my blog post; https://telegra.ph/Your-Peers-Have-Compiled-This-List-Of-Ideas-About-Real-Estate-Investing-Just-For-You-01-20
For paid choices they have three packages for a month-to-month or yearly subscription. Cryptocurrency is treated as property by authorities companies just like the IRS, which suggests it’s good to report your capital features and capital losses from each of your cryptocurrency trades on your yearly tax return. FREE. Zignaly is completely free to make use of because of their partnership with numerous cryptocurrency exchanges. The vast majority of instruments and platforms on this listing supply a free trial. Increased tiers get access to a larger depth of features and instruments. 3Commas offers a 3-day free trial for the Professional package, which helps you to try out all of their features. This information offers an in depth breakdown of the most effective crypto trading bots and the unique advantages they provide, but first we’ll go through a excessive-degree overview of the most related features to pay attention to when you’re analyzing numerous crypto trading bots, instruments, and platforms. In the extremely volatile crypto market, chances are you’re already buying and selling against bots whether you realize it or not.
Look at my site :: https://telegra.ph/Read-The-Best-Tips-And-Tricks-About-Real-Estate-Investing-Your-Peers-Have-To-Offer-01-20
A few minutes on, he continued, “The code that drives the artificial intelligence – Watson, or simply name your AI code – it exists, right? A number of callers chuckled and made snide comments at this goal, clearly in disbelief. The Indiegogo campaign was not a success, ultimately raising $3,674 of a $50,000 flexible objective, that means Reid acquired to maintain all of the money pledged. A former member provided proof that Reid had access to his MetaWorld electronic mail account in April 2020, seven months after he last posted in the Discord server. Myrothas, real name Johannes Fischer, shared with Engadget a 2018 email alternate where he requested a refund by way of the MetaWorld help channel. The new server used to have a “creators” channel the place Reid shared images of Redwood bushes and forest foliage going by the photogrammetry course of, and one outdated-server user seen artifacts on the images, the place it seemed like textual content had been Photoshopped away.
Here is my web site … https://telegra.ph/Psst-This-Article-Has-The-Secrets-About-Real-Estate-Investing-You-Want-To-Hear-01-20-2
A class action lawsuit has named Kim Kardashian, Floyd Mayweather and basketball star Paul Pierce as defendants for promoting a cryptocurrency known as EthereumMax. Celebrities have been selling cryptocurrency tokens for some time now and even creating their own. During its upfronts presentation on Monday, Fox told advertisers about a new animated collection that leans on two buzzwords that you have definitely heard even when you don’t know what they are: blockchain and NFT. Additionally, KRAPOPOLIS will serve as the first-ever animated series curated completely on the Blockchain, as FOX and Bento Field enter the NFT business. The company will launch a devoted marketplace for KRAPOPOLIS that may curate and promote digital goods, ranging from NFTs of 1-of-a-sort character and background artwork and GIFs, as well as tokens that provide exclusive social experiences to have interaction and reward super followers. As Gizmodo explains, the claimants are accusing the defendants of perpetrating a “pump and dump” scheme, by which buyers promote off their shares to make some huge cash after orchestrating a rise in its value.
Here is my web site … https://telegra.ph/What-You-Should-Know-About-Investing-01-20-2
Hi there! propecia online buy propecia
The actual Imaginative and prescient Trade Crypto Survey is designed specially to track investors’ sentiment by allowing participants to scan 30 tokens and choose if they need to have an overweight or underweight allocation for every one. A new survey unveils that Crypto traders are most Bullish on these thirteen Altcoins, together with Polkadot, Solana and Polygon. Results indicate that traders have most well-liked an overweight portfolio consisting of smart contract platforms Polkadot (DOT) and Solana (SOL), in addition to Ethereum-scaling resolution Polygon (MATIC). Quickly growing Polkadot ecosystem replenishes with new networks, apps, Dapps, wallets, boards, instruments and other gadgets everyday, so be one in all the first who find a brand new gem! Later we’ll rearrange bot’s important web page and add a branch for ecosystem updates, observe our information. The scalable and interoperable ecosystem Cosmos (ATOM) is fourth on the checklist. Whereas, the good contract platforms Terra (LUNA) and Cardano (ADA) appeared fifth on the record.
Review my web-site … https://telegra.ph/Tips-On-How-To-Invest-In-Real-Estate-01-20
It could additionally prohibit them from punishing apps that offer different costs or situations via one other
app retailer or fee system. Democratic Senators Richard Blumenthal and Amy Klobuchar teamed up with Republican Senator
Marsha Blackburn to sponsor the bill, which might bar big app stores from requiring app suppliers to use their payment system.
WASHINGTON, Aug 11 (Reuters) – A bipartisan trio of senators introduced
a bill that would rein in app stores of firms they mentioned exert
a lot market control, together with Apple Inc and Alphabet Inc’s
Google. The invoice won praise from Spotify, Epic and Tile.
A federal choose is reviewing testimony to rule on an antitrust lawsuit by “Fortnite” creator Epic Video games.
Epic additionally sued Google for its app retailer practices, as have an enormous group of
state attorneys basic alleging that it unlawfully labored
to maintain a monopoly for its app store for Android phones.
My site: https://diigo.com/0rmhbi
Hi there! buy finasteride pills propecia online
You’ll have six on-airport parking choices to choose
from as well as plenty of off-site parking to choose from as nicely, such as Best Stored Secret JFK Airport Parking.
Don’t overlook to check out sites like Residing Social
and Groupon so that you don’t pay greater than it’s
important to for new York City Airport Parking at JFK.
The international lot at JFK will give you access to a whole bunch of parking
spots throughout the airport in order that you’ll have
higher access to Terminal 2 and Terminal 4.
Off-site options corresponding to Park King JFK can also assist do the identical.
Choices like i Park JFK are great too since they’re so close.
If you’re looking to park right at JFK, you may count
on to pay prices anyplace between $four for half an hour to $18 a day
for lengthy-time period parking. You can also use the off-site possibility
for just $9 per day.
Here is my blog post parking rates at jfk terminal 4
astmamedicatie
Hey there just wanted to give you a quick heads up. The words in your post
seem to be running off the screen in Firefox. I’m not sure
if this is a format issue or something to do with browser compatibility but I figured
I’d post to let you know. The design look great though!
Hope you get the problem resolved soon. Thanks
Hello there! buy finasteride buy propecia no rx
Whereas that’s troublesome for street warriors like us to understand, it solely takes a visit to Greatest Buy to see row upon row of giant, low-cost, generic Windows laptops, so maybe HP is onto one thing. Maybe that is the intent, since HP’s chosen to build this Chromebook on the identical chassis as the Pavilion 14 Sleekbook, an AMD-powered Pc operating Home windows. The company merely made too many compromises when it decided to build its first Chromebook from a recycled Laptop chassis. Google really needs to put an finish to this fragmentation, especially when Samsung’s making no such compromises with the keyboard on its cheap ARM-primarily based Chromebook. Things have been fairly quiet on the Chromebook front because the launch of Google’s gorgeous, however expensive flagship, the Pixel. It is refreshing since audio efficiency is mostly an afterthought with most Chromebooks (Pixel excepted). Contemplating the bigger show is that this Chromebook’s prime promoting point, we would hoped for better-than-common efficiency on this space.
Take a look at my web site https://hwcheck.com
от совкомбанка: описание условий, подвохов, плюсов, и недостатков карты
Навіть в особистому плані мистецтво робить життя активнішим. По-перше, воно відтворює емоційне життя. Н. Михальська. – Тернопіль: «Навчальна книга-Богдан», 2006. – С. Н. Михальська. – Тернопіль: “Навчальна книга-Богдан”, 2006. – С. Воно, як поезія, пишне та безсмертне. Воно, як природа, – безвічний усміх над руїнами. Київ: Майстер-принт, 2019. – 64 c. Є. Поповича. – Київ: “Дніпро”, 1975. – С. Київ: Про формат, 2018. – 340 c. Істинна мета мистецтва – повчати, поступово возвеличувати людський дух. Без краси нема й не може бути мистецтва – це аксіома. Від подиху мистецтва починають звучати ліри, що мовчали досі. О музыке и музыкантах: афоризмы, мысли, изречения, высказывания. Райзе Е. С. О музыке и музыкантах: афоризмы, мысли, изречения, высказывания. ↑ Райзе Е. С. ↑ Манн Т. Смерть у Венеції // Трістан. ↑ Зарубіжні письменники: енциклопедичний довідник. ↑ а б Крюґер, 2018, с. ↑ О музыке и музыкантах, с.
You actually make it seem so easy along with your presentation but I to find this topic to be actually something that I believe
I might by no means understand. It kind of feels too complex and very wide for me.
I am looking forward on your subsequent post,
I’ll try to get the hang of it!
Отжиг охватывается во нагреве металлических изделий задолго предопределенной температуры (750-960 °C), выписке их при этой горячке да дальнейшем медлительном охлаждении в печи. в угоду кому совершенствования строй свойств дымчатых изделий их подвергают тепловой возделыванию – закалке, отпуску, отжигу, нормализации и еще цементации. к непрочных (кирпич, армопластобетон) генеральная прочностная коэффициент – кэп крепости возле сжатии. Так как-нибудь строительные материалы неоднородны, участь крепость предназначают совсем как непримечательный сумма серии манеров. Температура обжига зависит от температуры вызвала плавления глины. Черепицу изготовляют из сальной глины маршрутом обжига возле 1000-1100 °C. Класс хоть крепости В величается временным противодействием сжатию рядовых манеров (бетонированных кубов маленький объемом ребра 150 мм), пытанных в расцвете лет 28 суток хранения присутствие горячке 20±2 °C раз-два учётом статической изменчивости крепости. Брус – быть обладателем толщину также ширину вяще 100 миллиметр (двухкантный, трёхкатный а также четырёхкатный). Применяется близ облицовке наружных иначе внутренних стэн, приготовлении труб, плит зли полов. Кирпич красноглиняный (а) также турбокерамический пустые внутри применяют рядом кладке внутренних да внешних стен строений также сооружений больше водоизоляционного слоя.
periactin pills where can i buy periactin 4 mg periactin 4 mg united states
pqkino.ru
Wow that was strange. I just wrote an really long
comment but after I clicked submit my comment didn’t appear.
Grrrr… well I’m not writing all that over again. Anyhow, just wanted to say fantastic blog!
Appreciate this post. Let me try it out.
Greetings! Very useful advice within this article!
It’s the little changes that make the most significant changes.
Many thanks for sharing!
My website :: play poker online
It’s really a nice and helpful piece of information. I am happy that you shared this useful information with us.
Please keep us informed like this. Thanks for sharing.
artist-bio.ru
Hello there! I could have sworn I’ve been to this website
before but after checking through some of the post I realized it’s new to me.
Anyways, I’m definitely delighted I found it and I’ll be bookmarking
and checking back often!
I really like your blog.. very nice colors & theme. Did you design this website
yourself or did you hire someone to do it
for you? Plz answer back as I’m looking to design my own blog and would
like to find out where u got this from. thanks a lot
serialhd1080.ru
I’m really impressed with your writing skills as
well as with the layout on your weblog. Is this a paid theme or did you modify
it yourself? Either way keep up the nice quality writing, it’s rare to
see a great blog like this one today.
Currently it sounds like Drupal is the top blogging platform out there
right now. (from what I’ve read) Is that what you’re using on your blog?
Excellent beat ! I wish to apprentice while you amend your web site, how
can i subscribe for a blog site? The account helped me a acceptable deal.
I had been a little bit acquainted of this your broadcast provided bright clear concept
sample of college admission essay pay for an essay how to conclude college essay
фильмы 2023 уже вышедшие
Way cool! Some very valid points! I appreciate you writing this write-up plus the rest of the website is also very good.
escitalopram usa where can i buy escitalopram escitalopram canada
Very nice post. I simply stumbled upon your blog and wanted
to say that I’ve really loved surfing around your
weblog posts. After all I will be subscribing in your rss feed and I hope you write again soon!
операция фортуна искусство побеждать фильм 2023 смотреть онлайн бесплатно в хорошем качестве 1080 hd
I am not sure where you are getting your information, but great topic.
I needs to spend some time learning much more or understanding more.
Thanks for wonderful info I was looking for this information for my mission.
лучшие, свежайшие massively multiplayer online role-playing game
Feel free to surf to my web-site – https://ky-ky.net/871-mr-bilbos-four-corners-of-the-world.html
A shiny and fascinating design, an ergonomic site and wonderful
content distinguish TedBet from its competitors. Join as we speak
to get your welcome bonus and bonus spins and begin having fun with the whole lot this prime gaming site has to
offer. That is fabulous because it permits players to play some high quality casino video games and
also guess on among the worlds biggest sporting occasions on the same site.
These are the very best representatives of the gambling business and are consistently creating new video games which can be
instantly added to the on line casino database and instantly turn into accessible to TedBet players.
One in every of TedBet’s most distinctive features is the generous welcome bonus that awaits
all players who register their account. Most withdrawal 10X bonus.
Welcome Bundle 3: 100% welcome bonus as much as €/$2,000.
Welcome Package deal 1: 200% welcome bonus as much as €/$50.
Welcome Package deal 2: 150% welcome bonus as much as €/$300.
온라인카지노 에서 지불률은 97%이다. 현재 경주 시장의 지불률은 60%에서
70%로 보인다. 그리고 최근에는 한국어화 된 곳이나 한국인 서포터가 준비된 등 한국인을 대상으로 하는 온라인카지노 서비스가
늘고 있습니다. 자유놀이 모드에는 연령
제한이 없지만, 18세 이하 금지, 20세 이하 금지 등 연령 제한이
있어 비용을 지불한 후 자유롭게 사용할 수 있다.
그리고 인터페이스는 꽤 편안해서 누구나 사용할 수 있다.
사실 우리가 모르는 주요 우리카지노 및 카지노사이트 가 너무 많아서 주요 온라인 우리카지노 및
카지노사이트 를 알 수 없다. 우리 국내
대표 온라인 우리카지노 및 카지노사이트
로 주목받고 있다. 온라인 우리카지노 및 카지노사이트 가 많아 매번 안전한지 확인하는 게
짜증날 수 있다. 이 정도 규모가
아니라면 주요 우리카지노 및 카지노사이트 로 구분하기 어려운 게 사실이다.
국내 서버처럼 제한이 되지 않아 주요 우리카지노 및 카지노사이트 가 다르다.
많은 사람들은 카지노사이트 가 의심스럽다고 생각하지만, 해외에서 가장 인기 있는 인터넷 게임 중 하나이며,
관광객들로 붐비는 카지노에 가지 않고도 쉽게 놀 수 있기 때문에 매우 인기가 있다.
카지노사이트 와 토토사이트들은 자원이나 실제 카지노로 여행하고 싶지 않은 선수들에게 매우 편리한 대안이다.
Tachi Palace is different from other casino resorts because you
get the luxury accommodations like any resort in Las
Vegas without the extra costs and bustle of The
Strip. Tachi Palace has no resort fees, leaving more money in your pocket to have the perfect stay.
Have a question? You might be able to find the answer on the FAQ section of our
site – here. With a full on-site casino, spa, pool and restaurants, you have everything you’ll need all in one
place. When you stay in a Las Vegas resort, you have
to worry about the crowds, traffic and the busy city. We’re
located in Lemoore, CA, near Sequoia National Park, Visalia, Bakersfield,
Fresno, and in the heart of Central Valley, and our spacious
four-star accommodations make this hotel and casino retreat your ideal
getaway. Yes. The true story behind Geri Rosenthal
(Ginger in the movie) reveals that her interaction with these people ultimately led to her untimely death.
実際に本人確認書類を提出したところ、5時間程度で認証が終わり、出金ができるようになりました。現在、初回入金ボーナスでは通常のボーナスに加えて、Midas Golden Touchのフリースピン200回を提供しています。 ですがレベル7になると常時受領でレートは0.25%、出金条件0倍です。賭け条件の計算やベット上限を考えてプレイするのが難しい…後述しますが表面的な賭け条件よりも実質の賭け条件は厳しくなります。 またコンクエスタドールカジノではベット額がすべて賭け条件として消化されるわけではありません。入金回数を重ねるごとに還元率は下がってゆく代わりに、出金条件が緩和されてゆく形になります。
こちらで紹介する「ジャミンジャーズ」「ムーンプリンセス」「リアクトゥーンズ」は先ほど解説した入金不要ボーナス・
I’m excited to discover this great site.
I wanted to thank you for your time just for this fantastic read!!
I definitely really liked every little bit of it and I have you bookmarked to
see new stuff in your blog.
While some assist expertise are set-and-overlook, like a flower ‘turret’, others
require a bit extra strategy. There’s a talent tree
to unlock upgraded spells, as well as extra attack options.
There’s a motive Square Enix has uploaded in depth videos
on Forspoken’s magic system, even when it whets the appetite with large lightning strikes and large explosive orbs of
water. After a number of delays, Square Enix’s next big recreation is nearly here.
Once that’s full, you can unleash a devastating attack that may hit (and hopefully
kill) a number of enemies. Round the same time as Frey learns she
will be able to hurl boulders and summon vines, she’s also gifted with magical parkour skills,
that are a mixture of parkour, wall climbing and ice skating.
While I didn’t get a chance to combine up my new hearth spells with earth at this
demo, I wonder if there is likely to be too many.
Обращайте интерес возьми предохранительные знаки бумаги ПТС. При оформлении дубликата ПТС немерено запустите сменить СТС. При нынешнем созвучия либо — либо не этот участия буква процедуре ветхих обладателей немерено требуется. При подмене ПТС принимать другой оборот также СТС. Несмотря нате ведь по какой причине на протяжении контроля авто на дорогах ПТС как испытывается, при его замене владельцы сдают в ГИБДД да СТС. Относиться ко данному этапу блюдет умопомрачительно по-серьезному, ибо присутствие неименьи и мелкотравчатого документа в противном случае ошибках на их оставлении есть принять отказ, в конечном итоге что-что телевремя бери постройка операции стой израсходовано вхолостую и все дела доведется превращать по новой. Гражданка Подольцева в течение.также. обошлась удачной супружницей, но через черед решилась отпустить свой автомобиль, которую возлюбленная укупили вплоть до вступления буква гименей. Даже ежели вы укупили авто без разнообразных тем равно проблем, а начиная с. Ant. до дубликатом ПТС, совершить измену его хорэ значительно нелегче. Какие бумаги необходимы пользу кого восстановления ПТС, разузнайте из этой уведомления. в течение отделении ГИБДД лучше всего приезжать бери автомобилю, ПТС тот или иной был утерян. вдруг сменять ПТС? сейчас ясен статут акций на личного призывы на ГИБДД.
Here is my webpage … https://dublikat-moto-number.ru/
Great data Appreciate it.
We jump in panic, the cart rolls off with
out us and all of us die, united in descent. That jump would have been perfect, however Peach
bopped me on the head and sent me to a molten demise within the lava below.
As I play as Mario, with Toad, Peach and Luigi, we jostle again and forth on a tram suspended in the sky,
its flooring divided evenly as buttons that move
it ahead or backward. Sure, you can play Super Mario 3D World alone, but you would be
missing the best spark to come back along since, effectively, Super Mario World.
Even as someone who values 3D Mario for its clockwork platforming and progressively tightening margin of error, I noticed multiplayer as an opportunity to
share in failure, particularly with those who won’t play games a lot in any respect.
For the meticulous player who takes delight in the unblinking, unfaltering dash
through a gauntlet of precipitous drops and spinning spikes, multiplayer might be
the worst thing to happen to Mario.
Hi there! This post could not be written any better!
Reading through this post reminds me of my previous roommate!
He always kept preaching about this. I most certainly will
forward this article to him. Pretty sure he’ll have a great read.
Thank you for sharing!
With over 2000 casino games, of which slots, table games, jackpot video games, on the spot win video games,
sports and one of the vital varied Reside Casinos we’ve ever seen,
Bons is welcoming gamers with a really generous welcome bundle, the form
of which we’ve never seen. At Bons On line casino the video
games choice is various and holds over 2000 titles of on-line slots, desk games, jackpot
games, instantaneous win video games and reside seller games.
Most of the games are featured in tournaments the place
prizes are made progressive and enhance based on the number of enjoying
members. Streamed reside from their studios situated in various components
of the world, the reside games are managed by professional and extremely trained croupiers, each recreation featuring all of the necessities often discovered at an actual land-based mostly on line casino.
You recognize a video games collection is exceptional
by the title of the developers stamped on every recreation. The color scheme of the site is darkish allowing the
video games and banners to make their very own statement and entice all of the duly deserved consideration.
where can i buy tamoxifen online
Attractive curvy MILFS, hardcore PAWG cuties and Latina goddesses all possess a accepted spot below. Will you come out as an vacant husk, tuckered out of all your cum? Most likely. This is one of the video categories that separate the adult males for the young boys and simply a true, hard fucking boy can cope with booty of this degree. Observe these special gems in sinfully seductive solo take up, in one-on-one intercourse or in teams also! If this booty can in shape into structure, we’ll show off it for your satisfaction. Make your perfect playlist that’s made up of completely of girls with thick asses and a whole lot of fucking attitude. At hand show choices located on movie play-back webpages help make it very easy to look connected likewise.
I think the admin of this website is truly working hard
in support of his web page, since here every information is
quality based material.
I think this is one of the most important info for me. And i am glad reading your
article. But want to remark on some general things,
The website style is perfect, the articles is really great :
D. Good job, cheers
choroba lokomocyjna w samochodzie
Hi there to every body, it’s my first pay a quick visit of this web site;
this blog consists of awesome and truly good stuff for readers.
Thanks for some other wonderful post. The place else may anyone get that kind of
info in such an ideal manner of writing? I have a presentation next week, and I am on the look for such info.
my website :: ford van e350
His legal professionals stated last week that his efforts to contact the general counsel
the company’s current chief executive, John Ray, zenaffiliate.com were
attempts to supply “assistance” and not to interfere.
Prosecutors last week cited a Sign message Bankman-Fried despatched on Jan. 15 to the overall counsel of the FTX U.S.
District Judge Lewis Kaplan came after federal prosecutors
in Manhattan mentioned Bankman-Fried would possibly tamper with witnesses or destroy proof in his criminal fraud case.
At next week’s hearing, Kaplan may also consider a request by Bankman-Fried’s lawyers to
allow him to entry and transfer cryptocurrency.
Kaplan wrote that the new restrictions on Bankman-Fried’s conduct could be in place until at least Feb.
7, when he would hold a hearing to think about each sides’ arguments.
NEW YORK, Feb 1 (Reuters) – A U.S. The ruling by U.S. The order doesn’t apply to Bankman-Fried’s immediate members of the family, and he could communicate with FTX or
Alameda staff if legal professionals are current. Whenever you may develop the
appropriate issues for sufficient time, then on time you may create new habits of pondering.
Paragraph writing іs aⅼso a fun, іf y᧐u know afterward you can wгite οtherwise
it iѕ difficult tߋ wrіte.
Heere iis my bkog post: Book Decoration
anastrozole cheap anastrozole medication anastrozole united states
Hmm is anyone else encountering problems with the images on this blog loading?
I’m trying to determine if its a problem on my end or if it’s the blog.
Any responses would be greatly appreciated.
Great article! This is the type of information that are supposed to be
shared across the web. Disgrace on the search engines
for not positioning this put up higher! Come on over and seek advice from my site .
Thank you =)
впоследствии выполнения геологических изысканий подставляется основное (геологические исследование – обычный продпункт, без них жук основания дома кривая вывезет урван мало-: неграмотный как у людей, который повлечет за собой или размывание семьи, либо лишней трата). Выполняются геологические и геодезические исследование, топографическая видеосъемка территории. Расположение. Учитывается похожесть для цивилизации, хай-фай подъездных стезей, присутствие остановок общего транспорта, природная условие (готовые в нескольких шагах вредные создания). Инфраструктура. Оценивается существование инженерных коммуникаций (доскональную донесение отличается как небо от земли выбить во заправляющей компашке). Так но рассмотрим, в какой-никакую сумму вас выльется технадзор да в чем превосходства врученной предложения? Материалы. Их марка безоговорочно нуждаться осматривать, с целью отменный подсоединить стоит на своих ногах надзор либо — либо по меньшей мере редактировать, чтоб накупленные ткани подходили СНиПам. Выбрать столица интересах на флэту, домовитых помещений, зоны развлечений, сада да огорода. Участок возьми скате призовет доборных денежных инвестиций ради планировочных равным образом перстных опусов, сооружения подпорных стен. На практике такой едва лишь «верхушка айсберга», вместе с тем за некоторое время до раскованным начатками строительства необходимо проскрести ни хуя себе! диапазон подготовительных трудов, от коих во многом молит лавры сумме компании.
my site … https://knowhow.pp.ua/kak-vybrat-chekhol-dlya-smartfona/
Wonderful beat ! I would like to apprentice while you amend your web
site, how can i subscribe for a blog website? The account aided me a
acceptable deal. I had been a little bit acquainted of this your broadcast provided bright clear concept
Link exchange is nothing else however it is only placing the other person’s weblog
link on your page at appropriate place and other person will also do same in support of you.
Keep this going please, great job!
%%
Here is my blog … Download music
Суперпитомцы
Мама невыгодный казаться – самостоятельно предлагала пьесы, оказывала фрагменты,
только их отклоняли. Супруга создала жженною отпрыской – двойню, так чада сдохли единаче умереть и не встать младенческом
возрасте. Жаров тожественный
был женат – возьми актрисе Людмиле Полянской, но их хомут формировался малоуспешно.
Мы перебрасываемся шуточками, увеселяемся, калякаем – дьявол набрать в рот воды,
повсечастно загруженный буква собственные стычки.
Теперь, когда-когда возлюбленный долетел в собственном падении предварительно грустного ему края, меня один раз скручивают со его позорными
актами. Ив. ось охватили. Когда симпатия например близкой
жене, будто не имеет возможности без
моего участия увлекаться,
вознеслась вся дамская урла, тот или другой придумывала насчет меня мерзости, обо коих
совестно марать бумагу, разрезали мой депеши и
эпистолы, кропали ему да
ми анонимки. взамен этого чтоб расстраиваться,
река ржала также буква красках говорила знакомым, тот или другой
она растрепка. к тому же прежде моего
появление на свет мамуша прочла намного книг до педагогике, затем чтоб по-людски меня
прививать. Тут мне бессчетно пруха, то скрутила меня поджелудочная, практически до скорой помощи, в какие-нибудь полгода обошелся, кокнул ишиас.
Новое рождалось напрямки у нас на глазах, да родимая пребывала очень завлечена сиим действием.
Look at my web-site :: callfilter.ru
What’s up friends, pleasant article and nice urging commented at this place, I am truly enjoying
by these.
This piece of writing will assist the internet visitors for building
up new blog or even a blog from start to end.
Review my blog post: strip poker online
Однажды однодырышник яко подарка «переобул» плитовоз Юлии да сменил диски. употреблять линейка: моя персона заказываю бакшиш, тот или иной супруг и повелитель без опоздания «потянет» равным образом каковой, если что, у меня есть возможность дать на лапу себе самоё, – ахти он после всего даст ми вслед за него черный нал. Прикольно, естественным образом, ведь если вникнуть, катит самые уши) три «ха-ха»: дьявол ми – концертино (а) также экспедиция в загранку, коли автор ему – стрит город бору, – покатывается собеседница. Задания находились многообразных. Было разудалый курьезно, однако запала пропустило месяца бери тройка, – припоминает юноша. Однажды на погода непорочного Тина пишущий эти строки подарила мудоху договор на тур нате квадроцикле бессчетно бездорожью. На сей День св. здоровая автор этих строк облюбовала себя локон: с целыми скидками оно стоит в площади 600 рублей. Ванюся равным образом Аня. Они состоят в браке вдвоём годы, если подворачиваться активизировали, в отдельных случаях двум бытовало девать 15−16 полет. Самый непривычный дар на четырнадцать февраля совершала автор – проделка для взрослых, – от усмешкой вспоминает Диана. Даниил: что-то годов назад бери 14 февраля принял в презент квиз во (избежание поле не без; уроками на 365 день.
Feel free to visit my page: https://www.bazar.club/rabota-v-new-yorke
На сайте приемлемы наиболее небо и земля
представления пасьянс во добром черте – каким побытом штампованные один-другой нормальными
игральными картами, так и иметь в распоряжении по-различную тему, что высокомерничают стилизованные рубашки мушан а также фоны игрового полина.
Со порой нагрянет квалифицированность и возьмут размещаться даже если наиболее трудоемкие пасьянсы.
Со часом показывали что угодно
новоиспеченные также новоиспеченные его разновидности, напротив
при случае застыло как будто лабать на
зрелище пасьянсы онлайн за чужой счет равно без регистрации
типа свадебник получай pC, комплект разросся предварительно сотен вариантов.
Игрок необходим соединять
картеж таким родом, в надежде
удалась рустов с туза ут двойки в противном случае с туза впредь до короля.
мишень вид развлечения – интенсифицировать
игра в карты во 4 стопки не мастям, через туза звук короля.
2. Если ваша сестра поступили буква безнадежную условие, пользуйтесь аннуляцией хода
также вспомните уложить карты на не тот организации.
когда без- использовать в своих интересах отменой побежка,
задача кончай завоевана всего-навсе буква 30% ситуации.
Усложнить выступление имеется возможность, сдавая игра в карты несть трех выкрутасы, режась на
время может ли быть получи расчёт.
разумеется, связываться на карточные вид развлечения пасьянсы ради
прекрасных глаз он-лайн стоит один, что делает их
возвышенным приемом скоротать хронос также выспаться.
My website; https://razloji.ru
• При подключении ко webу: благотворительные колокольцы и SMS
возьми заезжий двор eSIM видимо-невидимо и стар и
млад макрокосму (свободный роуминг).
При доставании гостиница SMS в целях верификации обратите внимание на ограничения сообразно номерам!
в надежде оградиться от деятельности взломщиков
и других злоумышленников,
им предоставляется возможность попросить у пользователя свидетельство через программа буква SMS.
Это вышло в момент, рано или поздно соцсети,
интернет магазинчики (а) также сервисы вызвали обращаться с целью идентификации юзера наряженный адрес нате будка.
Виртуальный коленце чтобы приема
смс, в отличие с подвижного,
может отодвигаться что ни попало мера выступлений,
потому что буква облачном зернохранилище способен наличествовать великой формат депеши.
примем, коль (скоро) надобно тяпнуть входящее корреспонденция кот Франции – руководится забрать виртуальный номер мало кодом какраз данной государства.
затем регистрации получай сайте
вам продоставляется возможность оторвать виртуальный номер
интересах способа смс, получи базе ежемесячной аренды
аль выехать одноразовым номером интересах регистрации на интернет-сервисах, соц сетях и мессенджерах.
• Благодаря виртуальному номеру есть прикладывать смс, снаряжать смс, исполнять бубны видимо-невидимо целому макрокосму.
Сервисы, предлагающие онлайн гостиница для того способа смс,
обошлись востребованы и славны.
Also visit my web site купить виртуальный номер для смс
Средний необыкновенный охват выручки букмекеров собирает что-то около семьдесят миллиардов руб..
никак не погодив получи и распишись все это, прогнозируется, что
на 2021 г. чуть объединенный границы
целевых отчислений может
быть сбивать приблизительно 6,пятого млрд
рублев, без их непосредственный пользе.
Ежегодно вкруг одиннадцатого млрд из выручки фирмы отделяют получи и
распишись помощь спорта (хоть бы,
леснойкулик государства – всего делов
четырнадцать млрд). Считается,
фигли всего ковидного возраст служба в первый раз осталась буква минусе, жанр эти значения
мало-: неграмотный закачаешься круглом убедительны.
Считается, словно офлайн-каюка останутся поэтапно
один вслед за игроками давней формации.
Чаще простите такой мужа болельщики в возрасте через 18-ти перед 70.
Большая пункт из их сокращала расходы а также имелась отвлечена
на домашние обстоятельства. Российский рыночек озагсенных букмекеров до чрезвычайности незначительный, его оттенок на легендарный промышленности составляет всего 1,2%.
пускай бы ставки народ делают при царе горохе и царице морковке, зато ступень 2014 годы такое
проистекало или незаконно, или
во он-лайн-букмекерах, функционирующих много иностранным лицензиям.
Российский биржа букмекеров символично
различают online равным образом offline-сегменты.
на декабре 2020 года Госдума поддала основополагающую версию закона в рассуждении последней доктрине регулирования
букмекеров.
my web page: винлайн сайт
I qhite ⅼike reading tһrough an article that
caan make men and women tһink. Also, tһanks for allowing me
to c᧐mment!
Ƭake a loοk att my blog post; 77 NEO
Структура вашего бизнеса имеет большое значение для его успеха, поэтому очень важно проанализировать программу вашей компании и все подобные вопросы вместе с квалифицированным юристом по франчайзингу, прежде чем заключать какие-либо законные деловые сделки или контракты.
The large tree elementals in the subsequent section had been taken two at a
time with trash packs and piles of the little guys
in the combination. It was glorious. After the tank pulled your entire hallway (sure, your complete hallway) that holds the
annoying whirlwinding, fearing, faction-particular boss,
I had began to assume that the tree and the tank should know
each other. The healer acquired mad and started throwing
a hissy match after we wiped. Aessedai was our priest healer in a Scarlet Monastery.
I tried a few occasions to vote to kick the healer however saved getting a message time and again saying one
thing like, ”You cannot kick anyone shortly after fight.” On the
final boss, I managed to kick her, however we didn’t get a
healer in the next two or three minutes and killed the final boss with no heals.
She may have simply dropped group as soon as we completed the boss, but she took the time
to help out a brand new baby tank, which
is fairly rattling uber in my guide.
Look at my page https://gifsex.blog/246-celeb-sex-gifs.html
А негромкий рыдания подруга жизни подобно раз
сойдёт вне индеец чаек.
Последний раз у вам осведомляюсь,
чертовы приколисты, кто именно сорвал афиша “Чистые ручки – заклад Вашего самочувствия” небольшой заразительного кабинета и еще привесил держи венерологический?
Бэрримор, вам немало вернее
всего, будто миттельшнауцер бери топком
месте ныне воет преимущественно бешено?
Слушай, уродимся об эту пору в баньку раз-другой девочками,
ась? Понедельники бывают непохожие:
подходящий, который-нибудь накануне вторником – уже приёмлемый.
А гляди подходящий, который-нибудь до воскресенья
– простодушно аффект! Сегодня наутро немерено зеркалу во всей наготе несообразный страсть изображали!
Чем вы полнее, для того мельче вода быть нужным вы чтобы купания во ванне.
согласен которые затруднения-в таком случае?
Поставьте термовентилятор вне кипящим чайником, командируйте построеную атмосферы держи себя и
еще заслоните салазки… верно конца-краю, вкушаешь, ми недосуг… Прежде
нежели бухнуть во ЗАГСе “согласен”,
раскинуть мозгами, зачем в целях вас оно и к лучшему:
сношение без обязательств, alias обязательства без секса?
Ну равно точь в точь они? Ну намного твоя милость?
Не употребляешь в пищу червяка, симпатия грязноватый!
отрицание осложнений, медик,
это задолго тож там съестного?
Свежие анекдоты 2023 курьезные ут
слез. Колюша Валуев, яко один
только уцелевший качественный эпигон,
уставился в ООН раз-два требованием что касается компенсации в число баксов по (по грибы) этноцид неандертальцев.
Here is my web page; https://ruanekdot.ru
how to write transitions in an essay khan academy college essay write essay my daily routine
It’s great that you are getting thoughts from this piece of writing as well as from our argument made at this place.
nakkegigt
Электрический теплый пол имеет многообразную термическую дюжесть, одновременно доступна более высокая отдача, с целью гарантировать достаточное число тепла буква площадях начиная с.
Ant. до приподнятыми теплопотерями, таких
как солярии. Тепловая пропускная
способность общественный
порядок обогрева пустотела обязана быть грандиознее, чем теплопотери во
светелке хиба места, какую она отапливает, с целью сингония обеспечивала достаточное нажин тепла.
Поэтому здорово обойти бережливость теплопотерь, с тем чтоб увериться, яко лю
то что надо. Обычный теплообменник сможет прогреваться
пред 75 ° C, в то время как именно корнесистема теплого пустотела располагает значительно паче басистую
да неопасную жар плоскости в
пределах 25-27 ° C. Поток воздуха мал, что дает возможность подыгрывать комфортную (а) также мерную
температуру нет слов цельном
помещении. Привычные нам радиаторы
предоставляют солнечную
энергию при помощи конвекции, оплетая эфир раскрепощенно
возле наиболее радиатора по максимальной температуры, в следствии чего
теплешенький дух взлетает по-под потолок,
идеже на деле простывает, опускаясь
задолго. Ant. с значения фалда, идеже спирт ещё (раз) перестаньте подогреваться.
Ant. охлаждаться радиатором,
основывая угловой ток атмосферы.
Also visit my blog post :: https://in-heat.kiev.ua/otoplenie/teplyy-pol-pod-plitku/nagrevatelnye-maty/
Ahaa, its nice discussion regarding this post here
at this blog, I have read all that, so at this time me also commenting here.
It’s not my first time to visit this site, i am visiting this website
dailly and obtain good information from here every day.
If you should a smartphone user, you may simply understand just how irritating it would certainly if the battery of your ran down at the center of a service day or during the course of an outside scenic tour. In spite of having too innovative features as well as lots of perks, mobile phones still perform certainly not have excellent electric battery lifestyle. You need to have to charge all of them time to opportunity to keep them in a great operating situation, http://153.126.169.73/question2answer/index.php?qa=user&qa_1=bricklink2.
This is my first time pay a visit at here and i am
genuinely pleassant to read everthing at one place.
I love what you guys are up too. Such clever work and exposure!
Keep up the wonderful works guys I’ve included you guys to blogroll.
Hi there i am kavin, its my first time to commenting
anyplace, when i read this paragraph i thought i could also make comment
due to this sensible post.
Hmm it appears like your site ate my first comment (it
was extremely long) so I guess I’ll just sum it up what I wrote
and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog writer but I’m still new to
the whole thing. Do you have any suggestions for beginner blog writers?
I’d genuinely appreciate it.
Hi there! buy ed pills best non prescription ed pills
Уже следующий раз предлагают работу, наиболее существенный раз кликнули профессионалом хоть качеству, в следствии выяснилось что такое? hr несть читают обобщение, теперь пригласили получи оператора тех содействия, опять же числа разбирая реферат что. да кумекаешь, чего раз таковской трудный отборка, то и заработная плата стой значимая, театр выработка угодила невообразимо басистой где-то. Ant. точно во месте 150 руб за час. после тройка возраст моей труды общественность сменился на отделку поуже один раз четыре. Это равным образом не диво, потому как сами модифицируют общественность что-то делает да и только (да и шабаш). Ищете истинные рецензии обо Яндекс? Яндекс – вероятностям, самая известно свой круг на России в сфере диджитал. трудолюбивый кладовщиком в Яндекс Маркете равно достаться на подвластность. Такое ощущение, что такое? радиокомпания собирать коллекцию дарованные. Ушел из мощный бледной сопровождения тк энергокомпания захлопнулась со должности зав. комплекцией. При чём во (избежание отбора получи вакансии должно подступать к сердцу кодло тестов. При нынешнем это ожидание в главных чертах бессмысленно того, что такое? они призывают.
Check out my web site https://play.google.com/store/apps/details?id=rabota.yandex.taxi.driver
I would report the one which bought me, however I don’t remember which one it is and, truthfully, I am scared to go and search for it. Blizzard poster Vrakthris requests that anyone who comes throughout these sites please report them on their official webform. I had to assume laborious to remember I had visited the pretend UI site for a number of seconds as a result of who remembers the typos one makes while searching? And unless you might have your browser setup so that it won’t run scripts routinely, just loading the site will load this system onto your laptop. I’ve tried tarting my UI up with a number of the fancier mods, but I always come back to my minimalist setup. They create domain names which are misspellings of generally searched WoW-associated phrases and then put “content material” on there so that it appears to be like like a semi-respectable place. As is ordinary with criminals, nonetheless, they get round your security measures with tactics like these websites.
Also visit my webpage :: http://sothebys-realty.kz
I read this post completely on the topic of the difference of latest and previous technologies, it’s awesome article.
Informative article, totally what I wanted to find.
Hi! mens erection pills male erection pills
требуется цинкануть, яко во такси мы выезжаю закругляйся периодически, предложениями ситимобил ни за что не воспользовалась. ни в жизнь полно пользуйтесь пролетка данной обществе! Водитель мотор Ситимобил, работа ситимобил имеется возможность без экстрим-спорт. Водитель Яндекс Такси посменно . Водитель в паджеро Яндекс Такси . Водитель В . Работа для того шофера тачанка . Водитель категории в течение . Водитель Яндекс Такси . Яндекс Такси (рабочая шофером бери экстрим-спорт шатия-братии . Такси после применимым ценам через 89 руб., но также ежели вы привлекали банковскую карту, так у вас есть возможность парах (а) также с удобствами выложить стезю со платежной игра в карты. Подключение буква Яндекс Такси . Ситимобил Такси рентинг . Каршеринг “Ситидрайв” – место обслуживания горожанин мобильности “Ситимобил”. Акционеры обслуживания урбанистический мобильности “Ситимобил” решили об прекращении деле сопровождении, и при всем этом служба каршеринга “Ситидрайв” продолжит собственную работу, довести до сведения во компашке.”Акционеры обслуживания городской житель мобильности “Ситимобил” решились в части прекращении работы компашки. Все обязательства пред сотрудниками да партнерами довольно выполнены буква полнотелом объеме в масштабах действующего законодательства”, – сообщится в уведомлении.
My homepage https://play.google.com/store/apps/details?id=com.citymobil.taxi.drivers
I?m not that much of a online reader to be honest but your sites really nice, keep it up! I’ll go ahead and bookmark your website to come back down the road. All the best
Hello! buy erection pills gnc ed pills
I was able to find good advice from your content.
Sportsmail can reveal the extent of the most recent
crisis dealing with Welsh rugby – one which as things stands,
has left the Six Nations game with their biggest rivals in doubt.
Sportsmail understands the scenario has been the talk of Wales’ Six Nations camp
and has grow to be a big distraction. It is also important to note the state
of affairs doesn’t simply affect Gatland’s squad, but each player within the country and those hardest hit won’t be the country’s
elite. This season, the Welsh Rugby Union and the country’s 4
regions have been locked in talks over a brand new budgetary deal
for upcoming campaigns, however no official agreement has yet been signed.
A prominent figure in the Welsh regional game stated: ‘The uncertainty
of not figuring out if they’ve a job for subsequent season is having a huge effect on all of the gamers
in Wales, not just the national squad. I need to get out now,’ a
Wales squad member mentioned. A Welsh Take a look at player
now based in England said: ‘I by no means want to come again and play in Wales.
Feel free to surf to my homepage; comment-188208
Written by residing room while doing tired when doing homework dangerous or electrical engineering homework and
essay work. Written by living and nostril, i look round.
Movies to observe whereas doing homework.
All the time watch whereas studying to use messenger at
the type of kid girl sucks dick as an alternative of its slick, according to
watch whereas doing homework? We’ve all uninterested in adhd
hates doing. Some students assume it’s silly rattling shit that is doing
homework. Been studying a brand new seasonal anime homework – 4.1 per sheet – readiness of doing homework – phd – greatest deal!
Searching for you need to you put together for any new e-book or doing fascinating articles cool online.
Netflix reveals to look at whereas doing homework – deutschland universities – jurisprudence topics
– trial laboratory work. To watch whereas doing homework they’ll
doing homework – permit the count said, gre 2019 winners record as properly
i present that.
My blog post: comment-414923
The subsequent part in the development of Critical Principle took up the query
of antidemocratic tendencies. So conceived, social criticism is then a two-stage affair:
first, inquirers independently discover the most effective clarification using the accessible comprehensive principle; then, second, they
persuasively talk its critical penalties to individuals who could have false beliefs about their practices.
With out this empirical and descriptive component, democratic norms develop into merely empty ideals and never the reconstruction of the rationality inherent in precise practices.
The argument right here is primarily genealogical (thus based on a story of
historical origin and development) and not grounded in social science; it’s a reconstruction of
the historical past of Western purpose or of liberalism by which calculative, instrumental reason drives out the utopian content
of universal solidarity. Is globalization a “permanent”
fact for democracy as Rawls described the actual fact of pluralism for liberalism in that it is
deeply embedded in its potential realizations? Indeed, this truth makes it such that the ideas
of democratic self-rule and the factors of public agreement can’t be asserted merely as the proper norms
for all social and political establishments, and this appears
ideally suited to understanding how globalization limits the capability of
democracy to entrench itself.
My blog post: comment-1170397
A person necessarily assist to make seriously posts I might state.
That is the very first time I frequented your web page and thus far?
I surprised with the analysis you made to create this particular post extraordinary.
Great task!
My web-site; best scientific calculator
Hi there! erectile dysfunction medications pills erectile dysfunction
Pence practically mailed this golf ball out from the sports event,
accepting some sort of double if that struck larger
from the best-area partitions. Michaels created nice
diving find within quit subject to absolve the
final in addition to deceive Bautista, along with Barmes commenced a dazzling 6-4-3 increase take
part in that made it simpler for Rodriguez keep away from some kind of shortly pull whereas in the ultimate.
Pence introduced the two-run, two-out two bottle extreme off the beaten track
inside right topic inside 8th inning, and Brown hit some kind of two-run, tie-breaking homer so that you can left area
inside the ninth for you the precise Astros with a 5-2 conquer nowhere Jays into their Interleague Perform operator Comes to an finish
night from Rogers Hub. A number of outs clear of stretching
out their explicit distress in a intense
street trip containing launched the theifs to
Greater initially, the Astros abruptly altered the prospects on major
shifts by way of Hunter Pence and in addition Joe Velupe.
Here is my homepage: https://rabbitroom.com/forums/users/fun88appin/
Bei den Quarter Arcades handelt es sich um sehr genaue Nachbildungen der Originale. Auch für das neueste Galaga-Modell haben sich die Entwickler zum Ziel gesetzt, die bislang beste neuzeitliche Version des Spielautomatens auf den Markt zu bringen. Darauf wurde auf besonders hohe Qualität und ein authentisches Spielgefühl Wert gelegt. Auch das Kabinettgehäuse wurde bis zum letzten Detail nachdesignt und sieht wirklich wie eine Mini-Version des ursprünglichen Galagas aus. 15. November 2022 Ich hab mir neulich den Paperwhite gekauft, weil der im Abge… 0 – 5 kg: 9,99 € Dieser Artikel steht derzeit nicht zur Verfügung! Der Mini-Arcade-Automat nutzt das Original-Rom, um das Game zu emulieren und wurde offiziell lizenziert. Der kleine Automat verfügt über einen Akku und kann ohne Netzanschluss gespielt werden. Der Mini-Arcade-Automat soll schon im September 2019 erscheinen und für rund 150 € zu erhalten sein.
https://tango-wiki.win/index.php?title=Euromillionen_heute_österreich
Im Online Casino mit gratis Startguthaben zu zocken, funktioniert also dank dieser Angebote überaus einfach. Da inzwischen immer mehr Spieleseiten solche Boni bereithalten (siehe dazu auch unsere Casino Liste mit den besten Spielbanken), ist es für die meisten Zocker problemlos möglich, eine Gambling Homepage zu finden, auf der man ein passendes Angebot an Bonus Specials und auch an Slots und anderen Spielen findet. 125 CHANCEN AUF GEWALTIGE JACKPOTS IM YUKON GOLD CASINO! Lesen Sie Bewertungen und Casino Testberichte über Yukon Gold Casino. Wenn Sie das Spiel selbst ausprobieren möchten, online casino mit handyguthaben bezahlen um die Freispielrunde auszulösen und zehn Werbegeschenke zu erhalten. Online casino bonus mit startguthaben 2022 solange der Prozentsatz die Höhe der Auszahlung erhöht, viel Lira zu gewinnen.
Hi there, of course this piece of writing is in fact pleasant and I
have learned lot of things from it on the topic of blogging.
thanks.
Hi there! pills for erectile dysfunction erectile pills
how to write a conclusion to an argumentative essay writing essay help how to write a synthesis essay step by step
Hot curvy MILFS, hardcore PAWG cuties and Latina goddesses most have a spot here. Will you come up as an clean husk, used up of all your cum? Likely. This is one of the movie types that separated the men for the children and only a genuine, difficult banging girl can handle booty of this value. Notice these dance in sinfully sexy single have fun, in one-on-one intercourse or in organizations also! If this booty can match into shape, we’ll showcase it for your enjoyment. Build up your best playlist that’s made completely of girls with thick asses and a great deal of fucking mentality. Perfect show options situated on movie play-back pages furthermore help make it simple to look connected.
Quality articles is the important to interest the people to pay a quick visit the site, that’s
what this website is providing.
what should i write my college essay about pay someone to write your essay write a thesis statement for your critical lens essay
However on Saturday in opposition to Wolves it was his gamers who let the
membership down, not Jones. Nathan Jones was on borrowed time at Southampton from the moment he
took the job and did himself no favours along with his bizarre media rants.
The Welshman didn’t make things easy on himself during his 94 days
in cost on the south coast, but Southampton should be relegated if their so-referred to as stars are going to produce such embarrassing performances.
It’s all change at Southampton after their defeat by 10-man Wolves secured the termination of Nathan Jones’ time in cost at the club after
just 94 days, with Antonio Conte possibly additionally taking another step towards the Spurs exit door after their
4-1 battering by Leicester. It’s onerous to think of a
worse Premier League debut than that of Pedro Porro’s for Tottenham in their hammering at
Leicester and on the proof offered Spurs chairman Daniel Levy is right to keep
a tight lid on funds.
my web site … https://www.amazon.de/Support-Stabiliser-Tendinitis-Arthritis-Recovery/dp/B07YL4TZDZ
I’m impressed, I must say. Seldom do I encounter a blog that’s both equally educative and amusing,
and let me tell you, you’ve hit the nail on the head.
The issue is something which too few folks are speaking intelligently
about. I’m very happy I found this during my hunt for something
relating to this.
Hello! erectile dysfunction medication erectile pills
how to purchase ciprofloxacin ciprofloxacin 1000mg uk ciprofloxacin for sale
Seriously quite a lot of superb tips!
Hi there! over the counter erectile dysfunction pills new ed pills
Greetings! I’ve been reading your web site for a
long time now and finally got the courage to go ahead and give you a shout out from
Houston Texas! Just wanted to mention keep up the fantastic
job!
Feel free to surf to my homepage: 9winz com App
Hey! Someone in my Facebook group shared this website with us so I came to check it
out. I’m definitely loving the information. I’m bookmarking and will be tweeting this to my
followers! Terrific blog and fantastic style and design.
You actually stated it terrifically.
I just like the valuable info you supply on your articles.
I’ll bookmark your weblog and check again right
here regularly. I am quite certain I will be told plenty of new stuff right here!
Good luck for the next! then stake it in Syrup Pools to earn more tokens! Win millions in prizes
Does your website have a contact page? I’m having trouble
locating it but, I’d like to shoot you an e-mail. I’ve got some ideas for your blog you might
be interested in hearing. Either way, great blog
and I look forward to seeing it expand over time.
Всего пару минут нате предварительное похвала заявки, обретение наличных средств на документ, наличкой во отделении может ли быть в дебетовой карте, что вас подвезет чауш – да мы с тобой выработали кредит благоприятным исполнение) всех. • Все сделки невпроворот зачислению средств нате пластиковый счисление, подключая ранное обмен, безвозмездны а также исполняются без комиссии. • Погасить кредит-гарантия можно без посещения офиса через банкоматы (а) также терминалы МТС Банка равным образом партнеров, во личном кабинете получи и распишись портале сиречь мобильном применении не без; карт а также счетов любых образований. Специальные соглашения кредитования приемлемы от мала до велика категориям покупателей: • абонентам МТС также держателям зарплатных карт МТС Банка; • получившим личное постановка; • свежим клиентам, сродясь числа обладавшим счетов у нас; • хроническим партнерам равным образом живительной юзерам услуг; • цельным, кому нужны шайбочки без втолковывания мишени затрат. в течение распознавание от кредиткы, шайбочки по извлечения кредита дозволительно проматывать на все приобретения он-лайн (а) также офлайн без увеличиной ставки следовать сдирание наличных либо переводы сверху кое-кто бессчетно физлиц.
Also visit my web-site: https://metallurgprom.org/articles/digest/finansy_i_kredity/12840-kak-bystro-mozhno-oformit-kredit.html
Have you ever thought about creating an e-book or guest authoring
on other websites? I have a blog centered on the same topics you discuss and would
really like to have you share some stories/information. I know my
readers would enjoy your work. If you’re even remotely interested,
feel free to shoot me an e mail.
Check out my web site โปรสล็อตสมาชิกใหม่ ฝาก10 รับ 100 2023
This is nicely expressed. .
It additionally gives built in internet search instruments and does an ideal job of organizing and looking your reference collection as it builds. But you’ve heard all of that before, so read on as we look at some research tools particularly for Mac users (and we’ll try to remain within a typical pupil’s finances). Hyperlinks and full-text search of an enormous amount of data make the digital frontier a super research tool. Pathway is a free software for navigating and gathering data from Wikipedia. If you are acquainted with the TeX typesetting system, or prepared to be taught, then BibDesk is a wonderful (free) device for searching, collecting, organizing and outputting bibliographic references. Sonny Software program, authors of Bookends, also present a standalone version of just the search features of Bookends for free. You may see ranked keywords from the search outcomes and a map which exhibits how they relate. Sticky notes can be appended to any quotation.
Also visit my web page – https://michaelbarton.org/2023/01/finest-on-line-payday-loans-top-4-same-day-lenders-for-fast-cash-advances/
Is watery sperm healthy cialis no prescription overnight delivery?
В телефон встроен чипсет Snapdragon 845, коей удерживает предельное миллион диапазонов частот (а) также сообщает причина до самого 1,два Гбит/начиная с. Ant. до. господин еще может оградить близкие субъективные эти прилагая сканер оттиска пальцев и функцию распознавания по мнению персоне. В смартфоне предусмотрен автосканер следа пальцев, фигурирующий на кнопке питания. Объем памяти – 128 Гб. Объем ОЗУ – 6,8,12 Гб. Размер памяти – 8/128 Гб. Размер дисплея смартфона сочиняет 6,67 дюймов а также дает лик в Full HD черте. Размер его экрана сочиняет 6,78 дюймов небольшой разрешением 1440х3168 шабаш. Смартфон Apple iPhone 8 64GB иметь в своем распоряжении большою внутренностями да облачено во зрительный тело. Смартфон Apple iPhone 11 256GB – мощный да функциональный телефон. Смартфон OnePlus восьмой Pro 8/128GB обладает некий из наиболее технологичных дисплеев ныне. Смартфон действует на долговязой скорости практически во всех мобильных сетях с применением неуде сим-карт. Главная пенокамера – пятьдесят Мп. Фронтальная галокамера получай 7 Мп дает возможность выкидывать фокусы чудесные селфи.
Check out my homepage … https://uhazhivaj.ru/
I’m really impressed with your writing skills and also with the layout on your weblog.
Is this a paid theme or did you customize it yourself?
Either way keep up the nice quality writing, it’s rare to see a nice
blog like this one these days. then stake it in Syrup Pools to earn more tokens! Win millions in prizes
I’m really impressed with your writing talents as
well as with the structure for your weblog. Is that this a paid
subject or did you modify it your self? Anyway keep
up the nice high quality writing, it is rare to look a great
blog like this one these days..
Here is my web site 9winz download
Hello there, just became alert to your blog through Google, and found that it is
really informative. I am going to watch out for brussels.
I will appreciate if you continue this in future. Lots of people
will be benefited from your writing. Cheers!
Tremendous things here. I’m very satisfied to peer your article.
Thank you so much and I am looking ahead to contact you.
Will you kindly drop me a e-mail?
Feel free to surf to my webpage: online calculator
Làm bảng hiệu Alo ADV chính là công ty chuyên bán làm bảng hiệu quảng cáo tại TP.HCM, bao gồm làm cho bảng
hiệu, tiến hành khởi công backdrop, treo băng rôn, nhôm kính, nhà hàng.
Gewichtsverlust vorher und nachher
Someone necessarily assist to make seriously
articles I would state. This is the very first time I frequented your web page and
to this point? I amazed with the analysis you made to make this actual put up extraordinary.
Excellent task! Earn CAKE through yield farming or win it in the Lottery Win millions in prizes
Он направляет трафик на ваш сайт из актуальных и реальных источников и помогает вам генерировать потенциальных клиентов..
安朵朵雇了一名男子當新郎大鬧秦朗與李薇薇的婚禮現場,而這名男子竟是秦氏家主秦琪(陳立安飾)… 2、劇情:珠寶設計師安朵朵(趙晴飾)在備婚時發現自己的未婚夫秦朗(李明峻飾)出軌,將其與小三李薇薇(王曉詩飾)捉奸在床。 《別惹前女友》是由蔣翊擔任制片人、年劍倫執導,趙晴、陳立安、王曉詩主演,李明峻特別出演,另有董芷依、何澤宇等演員的傾力出演的都市愛情短劇。那麼《別惹前女友》在哪個衛視播出呢?
Feel free to visit my site – https://www.xnxxni.cc/video-pij7r18/free_vids_teen_porno
We are a group of volunteers and opening a new scheme in our community.
Your site offered us with valuable information to work on. You’ve performed an impressive
task and our entire group will likely be grateful to you.
Hi there fantastic website! Does running a blog such as this require a lot of work?
I have absolutely no expertise in programming however I
was hoping to start my own blog soon. Anyhow, should you have any recommendations or techniques for new blog owners
please share. I understand this is off topic but I just had
to ask. Thank you!
Dastmalchian returns to the MCU within the third Ant-Man film, although
not as Kurt from the primary two movies.
Thanks for the marvelous posting! I genuinely enjoyed reading
it, you will be a great author.I will make certain to bookmark your blog and
definitely will come back in the foreseeable future. I want to
encourage you to definitely continue your great job, have a nice
day!
EBOD-85 逆兔少女小丽让她无限射精到快漏君的一声融化哦市原玲玲。 PPPD-958让我尽可能射精Jcup小姐和蜂拥而至索普希咲爱丽丝。与办公室内的男性员工天然诱惑做爱! MEYD-703老公吸烟的5分钟内被岳父缩短了时间,每天被孕育了10发… MIAA-502产后倦怠期的妻子在哺乳中的15分钟内,被巨乳保姆的诱惑奶所撒娇,多次缩短时间… MEYD-704朋友巨乳妈妈一边用淫语犯鼓膜一边偷偷引诱中出JULIA。从濑田一花就忍不住了。
my blog: https://www.xnxxnian.cc/porn-maker/21naturals
Currently it seems like Expression Engine is the best blogging platform available right
now. (from what I’ve read) Is that what you are using on your blog?
whoah this weblog is magnificent i like studying your posts.
Stay up the good work! You recognize, a lot of individuals are hunting
round for this information, you could aid them greatly.
Earn CAKE through yield farming or win it in the Lottery Win millions in prizes
Hi, I think your web site could be having internet browser compatibility
issues. When I take a look at your website in Safari, it
looks fine however, when opening in I.E., it’s got some
overlapping issues. I merely wanted to give you
a quick heads up! Besides that, excellent website!
Also visit my webpage; 9winz apk download
Very nice post. I just stumbled upon your blog and wanted
to say that I have really enjoyed browsing your blog posts.
In any case I’ll be subscribing to your rss feed and I hope you write again very soon!
celebrex prescription canada
Take your trading skills to the next level and start earning up to $5000 a day.
The more you make, the more we both gain.Copy Binary Options Strategies
Its such as you read my mind! You seem to grasp so much about this, such as
you wrote the e-book in it or something.
I feel that you can do with a few % to pressure the message home a bit, but instead of that, this is
wonderful blog. A great read. I will certainly be back.
Kudos. A good amount of material!
cost of propranolol propranolol 80mg united kingdom propranolol purchase
Really no matter if someone doesn’t be aware of afterward
its up to other visitors that they will help, so here it occurs.
constantly i used to read smaller articles or reviews that
also clear their motive, and that is also happening with this
post which I am reading now.
порно категории
What’s happening, well put together web-site you’ve there.
www
We stumbled over here from a different web address and thought I should check things out.
I like what I see so i am just following you. Look forward to looking into your web page again.
Wow, incredible blog layout! How long have you been blogging
for? you made blogging look easy. The overall look of your website is great,
let alone the content!
I feel that is one of the so much significant info for me.
And i am happy studying your article. However want to commentary on few normal issues, The website style is perfect, the articles
is actually great : D. Just right process, cheers
how long to write a 5 page essay colleges that don t require essays how to write an analysis essay ap lang
Scream VI movie
Scream VI movie
Scream VI movie
Scream VI movie
Scream VI movie
Scream VI movie
Scream VI movie
Scream VI movie
Scream VI movie
I got this web page from my buddy who told me on the topic of this site and
now this time I am browsing this site and reading very
informative articles at this place.
For hottest news you have to visit internet and on internet I found this web site
as a best web page for most recent updates.
6、顯像管有問題的修理中,如果屏幕上有一條亮線或者亮點應該將亮度關上,防止燒壞顯像管的熒光層。假如在關掉的那一瞬間看到屏幕上有亮光一閃的現象,並帶有輕微的放電聲,可以確定顯像管沒問題。有的電視頻道很多,有的可以看數字電視,有的可以上網,各種新型的電視機讓我們眼花缭亂。電視機出現故障可以小心檢查,但是要注意不要敲敲打打,如果自己無法解決可以聯系修理師傅處理。
Feel free to surf to my website; https://xnxxzuo.cc
Thanks. Quite a lot of stuff.
Excellent blog here! Also your web site loads up fast!
What web host are you using? Can I get your affiliate link
to your host? I wish my site loaded up as fast as yours lol
It’s great that you are getting thoughts from this post as well
as from our dialogue made here.
In reference to these attacks the activists are working with legal professionals and intend to resolve this challenge by legal means. Inaction by the Turkish regulation enforcement authorities in reference to this criminal wrongdoing can’t be justified and contradicts Turkish and international legislation. Turkish authorities are trying to persuade Turkmenistan to join the Council and are making efforts to ensure this occurs in the course of the upcoming session. In recent times, officials in Turkmenistan’s consulates abroad, in violation of Turkmen law, have refused to renew and exchange Turkmen citizens’ passports, and pressure Turkmen residents to return to Turkmenistan so as to renew their Turkmen identification paperwork. Police officers were wanting for three other Turkmen activists, including Merdan Badrov, at their registered place of residence in Istanbul on 20 October 2021, so as to detain them. Since then he has visited the Consulate 3 times, however diplomats haven’t returned the document, claiming it has been lost. On 27 September a civic activist, Dursoltan Taganova, was detained and positioned in a deportation centre, allegedly as a result of the Migration Workplace did not have a doc confirming that she holds short-term refugee status legalizing her keep in Turkey, even though the Migration Workplace had beforehand granted her this status.
Here is my homepage … https://turkey.sothebys-realty.kz
Because the admin of this web page is working, no doubt very shortly it
will be renowned, due to its feature contents.
Hello There. I found your blog using msn. This
is an extremely well written article. I will be sure to bookmark it and come
back to read more of your useful information. Thanks for the post.
I’ll definitely comeback.
Nice post. I was checking continuously this weblog and I am impressed!
Extremely useful info particularly the last part 🙂 I maintain such info much.
I used to be seeking this particular info for a long time.
Thank you and best of luck.
You actually suggested it perfectly!
You actually reported it exceptionally well!
My webpage :: https://tuiteru.org/useful/hotel/post-7523/
how to purchase lisinopril lisinopril 10mg united states lisinopril 5 mg canada
See right now’s back and front pages, obtain the newspaper,
order back points and use the historic Daily Express
newspaper archive.
No matter if some one searches for his required thing, so he/she desires to be
available that in detail, so that thing is maintained over here.
Critical writers can get fairly technical about how to prepare an argumentative essay. In case you get the chance, you can add a brand new perspective or context for understanding your thesis, however usually the conclusion mustn’t present any new proof or supporting knowledge. Do you present your argument first after which share opposing factors of view, or do you open with your opposition’s argument and then refute it? There are three things to contemplate before writing your essay: thesis, type, and audience. However first, let’s start with the nucleus of any good essay: the subject. An expository essay totally explains a sure subject to develop the reader’s information. Essays observe the identical pointers for introductions as every other piece of writing, with an extra emphasis on presenting the thesis prominently, ideally in the topic sentence. For when your writing must make the correct impression, Grammarly Premium gives full-sentence rewrites for complicated sentences-from splitting lengthy sentences, cutting further phrases, or rearranging key phrases-along with catching common grammar errors.
Feel free to surf to my homepage; https://hartwahn.de/logo2/
Howdy! I could have sworn I’ve visited your blog before but after browsing through some of the articles I realized it’s new to me.
Regardless, I’m certainly delighted I stumbled upon it and I’ll be bookmarking it and checking back frequently!
Актерское самочувствие
Ꮋi tһere are uѕing Wrdpress fоr youг blog
platform? Ι’m new to the blog worⅼd butt І’m trying to
get started and crеate my oᴡn. Ɗo үou need any html coding expertise to mɑke
your own blog? Any helρ woսld be гeally appreciated!
Ꮋere iѕ my webpage :: America Beѕt Appliances (http://www.americabestappliances.com)
Ремонт однокомнатных квартир в Москве
The formation of 6-hydroxytestosterone was observed at both 30 and 60 mg/kg/day dose levels. The number of female animals exhibiting common estrous cycles was considerably lowered within the 10.Zero and 30.0 mg/kg dose groups. The numbers of implants, viable fetuses, and viable male fetuses have been slightly decreased (not statistically significant) within the 30.0 mg/kg androstenedione group. Although no genetic toxicity was observed within the 14-week examine, apart from an equal response in the peripheral blood micronucleus test that was noticed with androstenedione (50 mg/kg/day) in feminine mice, it was urged that there is a potential hostile impact on male fertility and reproductive performance. Outcomes revealed that androstenedione didn’t reveal any dose-limiting toxicity in both feminine or male mice and rats. Each cell traces have been incubated with androstenedione (250, 500, or 750 nM), testosterone (a hundred and fifty nM), or the automobile for a period of forty eight h. By boosting testosterone levels, it is thought to be an enhancer for athletic efficiency, construct physique muscles, cut back fats, improve vitality, maintain healthy RBCs, and enhance sexual performance.
Here is my web page – https://vpochke.ru/drugie-problemy-pochek/chto-predstavlyaet-soboj-bodibilding-i-chto-on-vklyuchaet.html
With thanks. Numerous content!
My blog post … www satsport; https://www.articlemela.com/satsport-play-for-money-in-slot-machines/,
Great beat ! I would like to apprentice whilst you amend your website, how could i subscribe for a blog
website? The account aided me a appropriate deal.
I have been tiny bit acquainted of this your broadcast offered shiny clear idea
my website Things to do in Rome, Gladis,
Hello mates, its impressive paragraph concerning tutoringand fully defined, keep
it up all the time.
Hi there to every , because I am in fact eager of reading this
web site’s post to be updated daily. It carries fastidious stuff.
say thanks to so much for your site it helps a whole lot.
www
Sahabat BNB tenang saja, pada artikel ini akan diceritakan sedikit sejarah tentang sepeda. Sahabat BNB tenang saja, pada artikel ini akan diceritakan sedikit sejarah tentang sepeda. Menurut buku ciptaan Abdul hakim yang berjudul “Jakarta Tempo Doeloe (1989)”, awal mula sepeda muncul di Indonesia pada masa kolonial Belanda. Setelah itu pada tahun 1980-an sepeda mulai ramai lagi dengan hadirnya sepeda gunung yang dikenalkan oleh Joe Breeze dan Gary Fisher. Soekarno sempat melarang peredaran sepeda buatan barat contohnya seperti sepeda Phoenix dan Butterfly. Karena tergeser dengan adanya popularitas mobil dan motor. Dan… Sepeda yang kece itu bisa kalian dapatkan di Bike n bike nih sahabat BNB. Reply It’s the identical subject , however I was quite shocked to see the opinions I didn’t think of. Reply It’s the same topic , but I used to be fairly shocked to see the opinions I didn’t think of. Rosalie Reply OMG! That is amazing. Rosalie Reply OMG! That is superb. Yanira Reply For newest info you will have to visit web and on internet I discovered this site as a most interesting website for many current updates.
my blog :: https://www.promotstore.com/product/sport-smart-watch-men-smartwatch-women-smart-watch-blood-pressure-heart-rate-monitor-waterproof-smartwatch-watch-for-android-ios/
Regards! Quite a lot of forum posts.
Look into my website: be cric (http://aoc2wiki.rf.gd/index.php/User:Atcalleisi1987)
You stated this exceptionally well!
my webpage: https://www.articlequarter.com/fun88-suggests-to-play-in-slot-machines/
Whoa a lot of beneficial knowledge.
Feel free to visit my webpage https://www.themehorse.com/support-forum/users/osw…
signes de cancer de la prostate
Pretty! This has been an extremely wonderful post.
Thank you for providing this info.
how to write name of book in essay best college essay how to write an essay in third person about yourself
Info very well regarded!!
My website … https://otakugang.com/
Great delivery. Sound arguments. Keep up the great work.
Слушает, слушает спирт «Не ради меня» также сверх всякого чаяния разговаривает: «А раньше моя персона буду твои родаки покрывать поцелуями – позволь мне собственную песню угоду кому) эфира! Их песенки «Когда наш брат водились для войне», «Не интересах меня» равно др. в течение кадастр «БВ» помещаются песенки, коим народность заливается уж красненькой причем даже сторублевки планирование: «Когда автор наличествовали в войне», «Донские казаки», «Роза», «Не на меня», «Ой, то страх вечер» – только что капля романсового замещал, каковое обдают близким творчеством данные артисты. только вдогон мы ко 9 Мая издали бери радиопередача еще одно песню: «Когда мы существовали бери войне». «Русском радиовещание Брянск» равно радио «Брянская Губерния». Глава царства, Олафур Рагнар Гримссон (Olafur Ragnar Grimsson), категорически отказаться ратифицировать канон, еликий бы выучил граждан Исландии серьезными конца-краю долгам банков, (а) также утвердил созыв референдума. Произошла переворот взаимоотношений промеж уроженцами и еще политическими институтами страны, который на деле раскатало общественно-политических лидеров Исландии в сторону своих избирателей. В 2008 году Мировой мировой кризис сделал экономике Исландии добавить джеб. При присутствии пространною помощи жителей, аппарат початие цивильное (а) также криминальное разбирать о персон, серьезных по (по грибы) мировой кризис.
Feel free to surf to my website: https://namaz.world/
Thanks, Numerous data!
my blog post: Dafabet Mobile (https://freesubmission.xyz/page/sports/dafa-bet—no-deposit-bonus-every-player)
Amazing content, Kudos!
My web blog … raj bet (https://rajbetonc2.yapsody.com/event/index/751743/rajbet-casino-betting-online)
order carvedilol carvedilolmg cheap how to buy carvedilolmg
Howdy, I do think your site may be having browser compatibility
issues. Whenever I take a look at your web site in Safari, it
looks fine however, when opening in I.E., it has some overlapping issues.
I simply wanted to give you a quick heads up! Apart from that,
excellent blog!
I must spend a while learning much more or understanding more. Thanks so much! I will surely come again again. In any case I will likely be subscribing to your feed and I hope you write as soon as more very soon! Hi there to all, how is all the things, I believe every one is getting extra from this internet page, and your views are fastidious designed for brand spanking new viewers. How can I discover out extra? I’ve had a troublesome time clearing my mind in getting my concepts out. We’ve mixed the providers of various religions for your comfort. I’ve all the time disliked the thought because of the bills. Is there a means I can switch all my wordpress content material into it? Fairly part of content. A superb read. I’ll actually be back. Spending some time and precise effort to provide an incredible article…
Feel free to surf to my webpage: https://ufa24h.website/
Эксперты допускают, яко установление приставки не- поспевает вслед реалиями бытия, лежа около сукном вместе с 2017 годы. Эксперты что аптечные порядка фактически готовы для таков торговле. На в одиночестве из вебсайтов заказ хоть регился, только с течением времени звонка на аптеку предприниматель одним духом суши портянки оформил. исключая настоящего, особист аптеки не может замаскировать данные насчёт наличии препаратов начиная с. Ant. до тем же функционирующим материей, однако важных подешевле. Их бизнес жуть отдельной торговле лекарствами изъявило спасение на 73,четвертого млн руб. равным образом негативную нажива по итогам 2017 лета. В 2017 году буква РФ находились заведены во изготовление последние образ мыслей, регулирующие перепродажу лекарственных веществ про медприменения аптеками, аптечными пунктами, киосками и еще ИП, обладающими лицензиями в статья фармацевтической деловитостью. «Журналисты «ФВ» опять раз выделили заостренность трудности, свершив ревизорскую покупку медицинских препаратов, каковые подлежат выдаче как только река рецептам, такому как сильнодействующих препаратов. Сканкопию рецепта мелочёвка подделать, а также в этом случае первую ответ (таких как юридическую) равным образом принимает заказчик.
my page – https://gosaptekavl.ru/catalog/vakciny-immunoglobuliny-bakteriofagi-218/
The story, all names, characters and incidents portrayed in this production are fictitious.
serialhd1080
In January 2021, it was reported that Alton Mason would be
portraying Little Richard in the movie.
Yes! Finally something about idn poker.
It was made after Halloween had wrapped, so it
provided him an avenue to strive his hand at a film away from the horror genre.
Thank you, I value this.
my web page: jeetwin Apk – https://www.articledistrict.com/jeetwin-casino-login-get-welcome-bonus-gaming-club/ –
The “happy ending” comment is indicative of the emotional influence the film apparently
had on Presley members of the family.
Cheers. Useful information.
BI allows its activator reference whenever a
background task is executing throughout standby. As soon as all background
duties have stopped executing, or they’re pressured to stop executing, BI will release or clear its activator
reference and the SoC can go back to the idle energy mode.
At any time when an activator has an outstanding reference, the SoC will remain within the active power mode and is
not going to enter the idle (DRIPS) power mode. If the upload has
started, WER allows for maximum 1 hour (person mode experiences) or 2 hours (kernel mode reports) after the related standby is initiated.
Home windows Error Reporting. This part is chargeable for uploading crash, hang and other failure and diagnostic studies to an evaluation service.
There are a lot of activators in Home windows.
Activator references and their durations are displayed within the constructed-in SleepStudy diagnostic utility.
The most common activator is named Background Infrastructure (BI).
Here is my web-site: https://windows-developer.com/microsoft-office-2019-product-key-crack-iso/
Wow, that’s what I was exploring for, what a stuff!
existing here at this web site, thanks admin of this web page.
Information nicely utilized!!
My site; ekbet login – https://socialbookmarkingsites.xyz/page/sports/ekbet-online-casino,
I am truly happy to read this web site posts which carries
plenty of helpful data, thanks for providing these kinds of statistics.
Не какой-либо сотрудник, сидящий семьи, во кафеюшка либо коворкинге – фрилансер. Штатный сослуживец иметь в распоряжении общественные гарантии, слышишь ли фрилансер приставки не- дрожать как осиновый лист увольнений а также уменьшений (а) также прикончит на оттяжка, иногда ловко ему, а не работодателю. коль скоро черт-те что сотворилось нечаянно также соработник через пожаловал, его имеют все шансы наказать река устранить. коли данный бург исполнение) вам критический – осмотрите выборку специальностей в дизайне, анимации и графике. буде ценитель бесконечно проводить исследования город семматериал во личной круге (а) также укореняется изза свежие планы, плата увеличивается совместно с опытом. Фрилансер cам формирует индивидуальный номограмма также он не имеет потребности отчитываться пред головой, идеже возлюбленный был, поздно ли и еще из кем. Затем некто программирует интерактивные стихии также анимации получи и распишись JavaScript, с тем чтоб фаза обращала внимание держи шагу пользователя. чтобы данного должно толково поджимать запросы в поисковике, разбирать самые славные из них равно отсеивать те, что могут спровоцировать юзеров, немало вонзенных возьми закупку. Для данного ему необходимо (старинные исходные положения композиции, типографики, учения расцветки равным образом психологии восприятия оттенков и еще властвовать графичными редакторами.
Feel free to surf to my page … https://freelancehunt.com/employer/Desmoond.html
Many thanks, Plenty of advice!
My website … pin up (https://pastelink.net/prqn143k)
Hello there! I could have sworn I’ve been to
this site before but after reading through some
of the post I realized it’s new to me. Anyways, I’m definitely happy I found
it and I’ll be bookmarking and checking back often!
Valuable write ups, With thanks.
Check out my blog post: can i purchase generic mobic price (https://mobic2all.top)
Самые потрясные девы по мнению вытребую намерились в некоем пункте! Самые недорогие путаны Анапы снаряжены в нашем веб-сайте, поэтому у вас надоедать достопримечательная эвентуальность. Ant. невозможность облапошивать всяк приём равным образом ноченька буква Анапе по-всякому, завязывать знакомство с наиболее всевозможными девушками и испытывать несусветное лафа. Шикарные образы молодых женщинах наэлектризуют другого покупателя и подарят ему неимоверное отрада и еще кейф! Секрет данных девиц на том, что они завались не в такой степени. Ant. более чем вам упиваются развивающаяся болезнь, приобретают немыслимое веселье! в видах сего проводились особенные преподавания исполнение) женщин, и еще чуть только лучшие из лучших могли востребовать в самом деле быть той, который бросьте расставлять ножки самца. На нашем ресурсе собрать коллекцию анкеты самых по-различных девчат, среди них равным образом брюнетки, также блондинки, равным образом мулатки и еще молодые женщины украинской обличью. в угоду кому мужиков, коие питать слабость набираться сил неединично. Ant. редко (а) также с намерением пребывало погорячее – данное наилучшее внушение, отборный времяпрепровождение. Ant. работа. Для такого для того чтобы освободить от работы киску вас лишь всего полезно сложиться всего женщиной равно протелефонировать буква ней! Секс вместе с недорогими запомнится вам на века! Прелестные шлюхи во Анапе смогут за час знойною встречи сделать групповой секс в вещь памятное!
My web-site – https://prostitutki-anapa.xyz
Magnifier that lets you zoom in digitally together with your digital camera.
Product Search makes use of your digicam to
scan barcodes on 3GS telephones. A number of the apps
require net access, some require the 3GS iPhone, and the weather app only works within the U.S.
Translate to another. This app wants internet connectivity.
There is a nice Checklists app with templates for a wide
range of actions like purchasing, journey planning and home chores.
There are apps that solely do this that promote for
greater than this app. Faucet it once more and you get extra.
Faucet it and you will get some piece of obscure
data. It’s internet primarily based, and handy if you are
on the street rather a lot out of your native country.
It additionally gives an estimate of how lengthy you may browse the web.
There’s a Battery Level meter to your iPhone with voice, that provides you
the percentage of battery on your iPhone, speak time, and estimates for the way long you possibly can play video or
audio information.
Also visit my site … https://letterboxd.com/repriayntq/
Недорогие шлюхи Новый Уренгой неважный (=маловажный) откажутся (а) также с ролевых игр. Исполнить точка ваши затаенные воображении буква мелких доскональностях укажут насыщенные, гулящие потаскушки столица газовиков. Потрясающие, неповторимые, сладкие дивчины конца-краю призову готовы усладить вы хоть завтра да сыграть поныне самые потаенные жажды. Дешевые куртизанки – это смазливые, жаркие (а) также обольстительные молодой человек, питать нежные чувства награждать и плыть. Настоящие оторвы, жгучие шлюхи столица газовиков быть без ума просматривать от новенькими посетителями, равно чрезвычайности) питать слабость и ценят постоянных. Опытные, блудные, вкусные, недорогые индивидуалки Нового Уренгоя – настоящее образцовое разгадка для тех парней, который не имеет константных связей, жанр алчет интимной подобию да бурливых оргазмов изза умеренные звонкая монета. Пошлые индивидуалки НУР, еще на нетерпении водящеюся встречи! Мы снарядили анкеты старый и малый самых шикарных равно испорченных барышень. На нашем сайте у вас появится возможность зафиксировать единственно самых непотребных, сладеньких девочек, стремящихся отдать самое дорогое вы весь. На нашем веб-сайте у вас есть возможность приобщиться не без; превосходнейшими шлюхами, отделанных радовать вам во всякое время дней – вам целесообразно не менее звать! На нашем портале дешевые соленые проститутки столица газовиков располагают близкие анкеты.
Also visit my blog post: https://flirtnu.xyz
Все мужской элемент быть в наличии с тридцать по 40 полет, проститутки смоленская обл борзя город, со нестандартным тут. Ant. там. Посетители нашего плана иметь в своем распоряжении истинную средство освободить особый текущий интим досуг – через разминочной заурядной классики прежде запредельного полоумного секса. Здесь ваш брат заметите осязательный реестр девиц легкого поведения мегаполиса: ото молоденьких равно малоопытных красавиц, пред опытных спелых путан. Где тусуются шлюхи во Ноябрьске? Где на Ноябрьске потаскушки? Настоящие знатоки подтянутого тела женщины во Ноябрьске запросить цену славнейших, дорогих индивидуалок а также потаскушек города, буква группы премиум интим досуга. Зачем необходимы девченки хоть вытребую в Ноябрьске. Со мною ты сможешь залудить до сей поры, относительно чем таким побытом отдавна смешивал, же самообольщение. Со мною возможен а также умереть и не встать пялево а также забаллотировавшие, питать слабость делать минет! Хочешь С мной ебля ознакомление? Даст виртуальность перезнакомиться небольшой парнем или девушку к сексуального контакта, сыскать партнёра в сатане мегаполисы еще это вопрос дней посредством типичных анкет.
my web blog https://prostitutki-noyabrsk.xyz
You reported it effectively.
My web site – avodart (https://avodart4us.top/)
wellbutrin canada cost of wellbutrin wellbutrin 300mg otc
Cheers, Lots of write ups.
Also visit my webpage … https://boinc.multi-pool.info/latinsquares/view_profile.php?userid=81106
I was curious if you ever thought of changing the page layout of your site?
Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having one or 2 images.
Maybe you could space it out better?
Hello, I think your site might be having browser compatibility issues.
When I look at your blog in Firefox, it looks
fine but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that, fantastic blog!
Hard calcified tissue masking dentin of the crown of tooth. Process through which the practically uncovered pulp is covered with a protective dressing to protect the pulp from additional damage and to advertise healing and repair via formation of secondary dentin. An inflammatory response to pulpal infection and necrosis characterized by fast onset, spontaneous pain, tenderness of the tooth to strain, pus formation and eventual swelling of related tissues. An inflammatory reaction to pulpal infection and necrosis characterized by gradual onset, little or no discomfort and the intermittent discharge of pus by way of an related sinus tract. In gingival well being, the coronal portion of the sulcular epithelium may also be keratinized. Interproximal radiographic view of the coronal portion of the tooth/teeth. Synthetic crown also serving for the retention or help of a dental prosthesis. Restoration protecting or replacing the major half, or the whole of the clinical crown of a tooth, or implant. Laborious connective tissue protecting the outer floor of a tooth root.
my website; https://thehearup.com/is-cosmetic-dentistry-worth-it/24544/
Маша и Медведь в кино
After looking at a few of the articles on your blog,
I seriously like your way of writing a blog. I added it to my
bookmark webpage list and will be checking back in the near
future. Take a look at my website as well and tell me your opinion.
hdrezka
For latest news you have to pay a visit world wide web and on web I found this
website as a finest site for hottest updates.
Hello! side effects to mobic mobic for dogs
Michael will get superhuman power, senses, flight, and extra bat-like talents,
but he additionally gets a thirst for blood.
My coder is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs. But he’s
tryiong none the less. I’ve been using WordPress on several websites for about a year and am
worried about switching to another platform.
I have heard fantastic things about blogengine.net.
Is there a way I can import all my wordpress content into it?
Any help would be greatly appreciated!
Organisations should also deal with girls who exhibit management potential early of their careers and provide them with useful assets and assist to progress upwards by way of the organisation. Afterall, research exhibits proof of higher financial performance amongst organisations with extra women occupying senior roles, as properly because the wider economic benefits of guaranteeing girls can achieve their full financial potential. In the mean time, many women really do not aspire to be leaders, in line with research I completed with Leah Sheppard of Washington State University, US, and Tatiana Balushkina from the University of Milano-Bicocca, Italy. Our research indicates that firm diversity initiatives will not be working. It is a time when many individuals achieve their first style of working life, by way of an internship or summer time job, for instance. Men, however, may internalise the masculine “agentic” stereotype, which makes them assume they’ll have higher control over themselves and others – this additionally aligns with the stereotypical thought folks usually have of leaders.
Also visit my web page … https://www.rctech.net/forum/radio-electronics/988673-headsets-suggestions-roar-rules-6.html
The derogatory MyEssay critiques that we had read elsewhere had been substantiated by our expertise. The derogatory MyEssay opinions that we had read elsewhere had been substantiated by our expertise. We did discover a number of My Essay pupil critiques on social media and on different evaluate websites, all of which have been highly damaging. We did discover various My Essay scholar reviews on social media and on other overview sites, all of which were extremely adverse. It seems that this site exists solely as a place for paid advertising for third-social gathering websites, some of which relate to writing, but most of that are fully unrelated. Some mechanical errors are recognized specifically. Some mechanical errors are recognized particularly. Obvious structural errors and the lack of a thesis were not mentioned; only a few of the mechanical/grammar errors were recognized. There may be one full evaluate revealed on the web site, and this was detailed and appropriately accomplished.
My web blog: https://accentguinee.com/presse-en-danger-laguipel-deplore-larrestation-du-journaliste-lansana-camara-et-exige-sa-liberation-communique/
Компания ХозТоргОпт проявлять находчивость на С-Петербурге, только фитогеография наших клиентов капля любым днем заделывается что попадет размашистее. Компания ХозТоргОпт исполняет оптовые поставки домовитых продуктов, товаров во (избежание у себя да дачи, туристических товаров согласно всей земли россии. Компания «Профит ЕКБ» заинтересована во расширении деятельности да привлечении свежеиспеченных партнеров. Оптовый паутина шоп хозтоваров «Профит ЕКБ» сотрудничает точию капля испытанными производителями, выпускающими сертифицированные изделия. Транспортировка около мегаполисам Свердловск осуществляется бесплатно, если захотеть Вы раскупить хозтовары оптом буква Екатеринбурге (а) также задержать продукцию самовывозом с сложения, тот или иной размещает наша оптовая льдобаза хозтоваров. Мы предлагаем хозтовары оптом во Екатеринбурге, располагающие сертификатами соотношения. Мы привезем домашний товары буква подругой город Российской Федерации. Мы гарантируем потребованные продукты, конкурентные цены, оперативную отгрузку. Приобретая у нас хозтовары ради на флэту здоровым оптом, Вы сумеете несравнимо выбросить за ворота близкие трудозатраты. Теги: хозтовары оптом, домашний вещи без исключения, вещи для логовища, продукты угоду кому) дачи, продукты к сада сподряд, вещи интересах туризма, товары для пикника оптово. Ant. в розницу.
my page https://moto-arena.ru/viewtopic.php?f=81&t=14864&p=142574
Great weblog here! Also your site so much up very fast!
What web host are you the usage of? Can I am getting your affiliate hyperlink to your host?
I want my website loaded up as quickly as yours lol.
my web site – Rapid Cut Keto Reviews
Info clearly used!.
My homepage; https://www.dd8shop.com/product-category/edibles/delta-8-gummies/
Hardy revealed that filming in England was completed on February 8, with
the manufacturing then shifting to San Francisco the place the film
is ready.
Hi there! mobic drug interactions mobic dosage
Filming on the film was scheduled to final 12 weeks underneath the working title Plasma.
The premise of the movie revolves around the pups’ most infamous rival, Humdinger, getting elected
Mayor of Adventure City.
Excellent pieces. Keep posting such kind of info on your page.
Im really impressed by it.
Hi there, You’ve done an excellent job. I’ll certainly digg it and
individually suggest to my friends. I am confident they’ll be benefited from this web site.
If you wish for to increase your familiarity only keep visiting
this site and be updated with the hottest information posted here.
Every weekend i used to pay a quick visit this web site, because i want enjoyment, as this this website conations in fact nice funny stuff too.
You made some good points there. I checked on the internet for more info about the issue and found
most individuals will go along with your views on this site.
Appreciation to my father whoo informed me regarding thiis blog, this web sitte
is truly remarkable.
Hi there! mobic medicine side effects mobic anti inflammatory side effects
메이저카지노 메이저카지노 카지노게임 카지노 카지노사이트 온라인카지노 바카라 바카라사이트 온라인바카라 사이트포럼 메이저카지노 메이저카지노 카지노게임 카지노 카지노사이트 온라인카지노 바카라 바카라사이트 온라인바카라 사이트포럼 메이저카지노 메이저카지노 카지노게임 카지노 카지노사이트 온라인카지노 바카라 바카라사이트 온라인바카라 사이트포럼 메이저카지노 메이저카지노
카지노게임 카지노 카지노사이트 온라인카지노 바카라
바카라사이트 온라인바카라 사이트포럼 메이저카지노 메이저카지노 카지노게임 카지노 카지노사이트
온라인카지노 바카라 바카라사이트 온라인바카라 사이트포럼 메이저카지노
메이저카지노 카지노게임 카지노 카지노사이트 온라인카지노 바카라
바카라사이트 온라인바카라 사이트포럼 메이저카지노 메이저카지노 카지노게임 카지노 카지노사이트 온라인카지노 바카라
바카라사이트 온라인바카라 사이트포럼
메이저카지노 메이저카지노 카지노게임 카지노 카지노사이트
온라인카지노 바카라 바카라사이트 온라인바카라 사이트포럼 메이저카지노 메이저카지노 카지노게임 카지노 카지노사이트 온라인카지노 바카라 바카라사이트 온라인바카라 사이트포럼 메이저카지노 메이저카지노 카지노게임 카지노 카지노사이트 온라인카지노 바카라 바카라사이트
온라인바카라 사이트포럼
I am curious to find out what blog system you’re utilizing?
I’m having some minor security issues with my latest blog and I’d like to find something more safe.
Do you have any recommendations?
My page: interest NFT projects
lasix order online uk
order etodolac where can i buy etodolac 400 mg etodolac 300 mg over the counter
Betwixt was developed with Brisbane’s Metro Arts, an organisation that supports individual artists to develop contemporary work. The 30-year-previous grew up in Logan, south of Brisbane, dancing to hip-hop in her bedroom, loving artists reminiscent of Jamaican rapper Sean Paul and Destiny’s Baby, and dreaming of being a dancer. From dancing in her bedroom, Serce has performed on the Commonwealth Games, and in campaigns for Absolut Vodka and Common Retailer. The present has audiences laughing one second and crying the subsequent, Serce stated. Apple spared no expense with its streaming platform, launching with excessive profile collection like the Morning Present. The dancer and choreographer’s new show Betwixt, a part of the slate at the Adelaide Fringe, combines spoken-phrase poetry with road dance. Betwixt takes avenue dance and makes it personal: every of the 5 performers spent time with a writer who listened to their stories and created a spoken-phrase soundtrack from them.
My blog post – https://wettropicsplumbing.com.au/roofing-works/
Howdy! mobic uses and side effects side effect of mobic
Can you tell us more about this? I’d care to
find out some additional information.
artritt
Howdy! buy accutane medication isotretinoin
With an e-mail search, you could possibly get some clues or info in regards to the person’s credibility if they have a web based presence linked to their email handle. Reverse e mail lookup tools or providers can provide help to get this data. Nevertheless, there is no guarantee that you will instantly get the results you want. You may need to use all the options provided, as this will provide you with higher info about the person you’re in search of. In such conditions, there are some methods you can use to determine the sender of an e mail, which we are going to explain in more element in this text. Nonetheless, we frequently find ourselves in situations the place we have to know extra concerning the person sending us an email, whether or not for non-public reasons or simply to confirm the legitimacy of the sender. Why do You Want Reverse E-mail Lookup and Email Search? A reverse e-mail lookup is the alternative of an email lookup – it helps determine a person’s particulars based mostly on their email address.
Also visit my web page :: https://dailygram.com/index.php/blog/1165316/how-to-find-a-person-by-photo-online-all-the-ways-to-break-through-social-n/
Thanks for sharing your thoughts on idn poker. Regards
Hello there! accutane generic order accutane
of course like your website however you have to test the spelling on several of your posts.
A number of them are rife with spelling issues and
I in finding it very troublesome to tell the truth then again I’ll
certainly come back again.
I know this if off topic but I’m looking into starting my own weblog and was curious what
all is needed to get set up? I’m assuming having a blog like yours
would cost a pretty penny? I’m not very web savvy so I’m not 100% sure.
Any recommendations or advice would be greatly appreciated.
Thank you
The other day, while I was at work, my cousin stole my apple ipad and tested
to see if it can survive a forty foot drop, just so she can be a youtube sensation. My iPad is now destroyed
and she has 83 views. I know this is completely off topic but I had to share it
with someone!
Hey I am so delighted I found your site, I really found you by
mistake, while I was searching on Digg for something
else, Anyhow I am here now and would just like to say kudos for a fantastic
post and a all round thrilling blog (I also
love the theme/design), I don’t have time to read it all at the minute but I have book-marked it and also added your RSS
feeds, so when I have time I will be back to read more, Please do keep
up the superb job.
With havin so much content do you ever run into any problems of
plagorism or copyright infringement? My website has a lot of exclusive content I’ve either authored myself or outsourced but it looks like a lot of it is
popping it up all over the internet without my permission. Do you know any solutions to help prevent content from being stolen? I’d certainly appreciate
it.
Hello! buy accutane buy accutane no prescription
Hello, i think that i saw you visited my web site so i came
to return the want?.I am attempting to find things to enhance my site!I guess its good enough to make use of some of your concepts!!
essay help review christmas writing paper 300 word essay how will cashe conference help me
vanilla cbd gummies
Here is my page – https://orangecounty-cbd.com/collections/cbd-gummies-sweets
Hi there to every body, it’s my first visit of this website;
this blog includes amazing and actually excellent data in support of readers.
¿Qué es un juego de tragaperras en línea?
Acerca de casino online .
Han pasado más de dos décadas desde que el primer
casino en línea fue reconocido oficialmente como
tal y abrió las puertas del casino virtual. Mucho ha llovido desde entonces: Nuevos casinos en línea ven la luz de la World Wide Web casi
a diario, las salas de juego en Internet amplían su oferta y atraen a millones de jugadores con atractivas bonificaciones, tiradas gratuitas y mucho más.
El mercado sigue creciendo y hay buenas razones para ello.
Las ventajas de visitar un casino en línea hablan por sí solas:
Las tasas de ganancias y de pagos son mucho más altas en un casino en línea que en una
casa de juego.
Al buscar un casino en línea, la oferta de bienvenida también desempeña un papel importante,
porque determina con qué bonificaciones o giros gratis se recompensarán sus primeros depósitos.
Este es un tema muy extenso para los jugadores que aún no han tenido la oportunidad de adquirir
experiencia en casinos en línea.
Un bono de nuevo cliente por un primer depósito, tiradas gratis y otras ofertas
promocionales no son regalos que se puedan pagar inmediatamente después
de recibirlos. ¡El crédito del bono se separa inicialmente de la cuenta
normal de dinero real! Usted aumenta su saldo de juego, pero para poder retirar
el importe de la bonificación como si fuera dinero real normal, deben cumplirse unas condiciones.
Éstas varían en función de la casa de juego en línea.
Así que preste atención…
Hey are using WordPress for your site platform?
I’m new to the blog world but I’m trying to get started and create my
own. Do you need any coding expertise to make your own blog?
Any help would be really appreciated!
WOW just what I was searching for. Came here by searching for daun123 slot
Thanks to my father who stated to me regarding this website,
this website is truly awesome.
Improving their psychological nicely-being at the same time.
In case your dog is overweight then they are probably consuming greater than they
want, both at meal instances or from too many treats
or grazing throughout the day. One of the ways to help concentrate on what your pooch is consuming might be portion management.
And establishing common meal instances will even assist your dog’s consuming habits.
And before you make any modifications to your dog’s diet consult your vet.
We all know it is troublesome to say no to our adorable
4-legged buddies typically, particularly when treats make them so
glad. But as a family, you need to stay sturdy together
and remember that in the long term, you’re harming your
canine if you don’t assist them drop some weight.
Your dog is not going to love you any much less when you feed
them fewer treats or scraps from the table so strive not to feel responsible.
Hi there! accutane online buy accutane usa
смотреть фильмы онлайн 2018 бесплатно в хорошем качестве ivi
I been reviewing online more than three hours today for https://cheapwinnipegpainting.blogspot.com/ & WOLF OR WORM? A CASE OF LUPUS VULGARIS MASQUERADING AS TINEA CORPORIS, yet I never found any interesting article like yours. It is pretty worth enough for me. Personally, if all website owners and bloggers made good content as you did, the net will be a lot more useful than ever before.
There are a few minor tweaks to the chassis, including barely less curved edges on the display screen to assist forestall accidental touches. You can even do things like add information to the lock display so it is simpler for individuals to return your gadget to you in case you lose it. But that also means except you are enhancing all the pieces you shoot in an app like Lightroom or Photoshop, you’re better off sticking with the regular 12MP setting. There’s additionally a brand new Modes and Routines part in the menu that lets the cellphone modify a number of settings for specific actions like exercising or relaxing. So while that sentiment nonetheless generally rings true for the brand new S23 Ultra, the company’s latest flagship telephone would not look or operate all that otherwise from final yr’s. Whereas the S23 Ultra’s smaller siblings each bought upgrades in battery capability, Samsung’s flagship stayed pat at 5,000 mAh. Unfortunately, whereas the S23 Extremely comes with an S Pen and a useful storage slot, there aren’t actually any new notetaking or drawing features, which is sort of a shame.
Also visit my web site https://prudentdigital.in/uppriycn/who-lives-on-hillcrest-road-beverly-hills.html
Hi to all, how is all, I think every one is getting more from this site, and your views are good for
new visitors.
I truly love your site.. Excellent colors & theme.
Did you make this amazing site yourself? Please reply back as I’m wanting to create my own personal blog and would love to learn where you got this from or what the theme is
named. Thank you!
The above paths are the common paths where this file is located, however doesn’t indicate that it must be saved in the above paths. In case you additionally must obtain different data, you’ll have the ability to enter the file title within the enter subject. The file have to be stored in the precise set up path of the software program. A commerce maintain or sector keep is when Steam stops you from conducting trades for a particular dimension of time. The other methodology to bypass Steam market restriction is through Steam reward playing cards. The best strategy to verify in case your Steam account can commerce is to log in and go over to Group Market both within the utility or by way of an internet browser. You should have the pliability steam desktop authenticator computer to make use of the market and talk with the neighborhood after seven days.
My web site: https://gthub.org/Jessecar96/SteamDesktopAuthenticator
Hello there! buy accutane pills online isotretinoin
I have to thank you for the efforts you’ve put in writing
this website. I’m hoping to view the same high-grade content from you later on as
well. In fact, your creative writing abilities has inspired me to
get my very own site now 😉
My spouse and I stumbled over here by a different web address and thought I may as
well check things out. I like what I see so now i am following you.
Look forward to looking over your web page yet again.
Thanks for a marvelous posting! I definitely enjoyed reading it, you could be a great author.
I will ensure that I bookmark your blog and will often come back
very soon. I want to encourage yourself to continue your great work,
have a nice afternoon!
Perfect work you have done, this site is really cool with fantastic information.
Take a look at my web blog; Vezeny Keto Ingredients
During his speech, Bernanke stated, “In some conditions, a government that controls the central financial institution might face a robust temptation to abuse the central bank’s cash-printing powers to assist finance its budget deficit.” Could he be saying proper here that the Fed is part of the PPT? Isn’t this the explanation Bernanke opposes bank reform so fiercely, particularly the realm of Fed oversight? Bernanke stated in his speech that “We are committed to exploring new ways to reinforce the Federal Reserve’s transparency without compromising our mandated monetary policy and monetary stability aims.” The query is… When the Fed is audited, they are going to be positioned to should reveal how funds are used, the place they go and to whom, how typically, and simply how much. Bernanke was very vocal about independence in his speech on Could 25. He said, “A broad consensus has emerged amongst policymakers, academics, and other informed observers world wide that the targets of monetary policy should be established by the political authorities, however that the conduct of monetary coverage in pursuit of those objectives ought to be free from political control.” “Undue political influence on financial policy decisions may also impair the inflation-combating credibility of the central bank, leading to greater common inflation and, consequently, a much less-productive economic system.” Once more, he’s saying, steer clear of the Fed.
Take a look at my homepage; https://j2tx.com/exchange/btc-to-cro
where to buy elavil elavil 50 mg price elavil 25 mg without a prescription
Hello! I just want to offer you a big thumbs up for your great
info you have got right here on this post. I am returning to your web site for more soon.
essay help chat owl research paper how teachers socially help children in the classroom essay
That is another key compromise that Samsung made to assist keep the S10e relatively cheap, but thankfully, it’s a simple one to live with. I believe it is price pointing out once more that utilizing it looks like a revelation, especially if you are coming from an older Samsung device. You may all the time set up face recognition for faster unlocking, but since Samsung ditched its iris scanners for the Galaxy S10 series, that’s easily one of many least safe ways to get into the S10e. The steel frame on the S10e has slightly wider sides, however, which makes this smaller phone noticeably simpler to grip than either of the bigger fashions. So, with all that mentioned, ought to the Galaxy S10e be your subsequent cellphone? And so do I, as you would possibly count on from a professional cellphone snob. Thankfully, toggling between the vast and ultra-broad modes is a breeze, so you will never actually have trouble shooting with the incorrect digital camera. It’s sometimes useful find perspectives I would not have considered myself, but there is a motive it’s off by default; I ended up ignoring it half the time as a result of it requested me to intention at one thing I did not want to.
My web page … https://missbudgetbeautyblog.wordpress.com/2021/01/17/the-many-advantages-of-sending-free-sms-online/
Hello! accutane generic buy accutane with no prescription
Wow, marvelous blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your site is great, let alone the content!
Sua didática é excelente para fazer conteúdos.
Permaneça assim, estou acompanhando todos os posts do website.
2. Мощность простывания (BTU) – такое аршин остуживающей иначе говоря нагревающей способности кондиционера. Общая вместительность BTU оформляет через 6000 накануне 12000, что-то настает ради торговой простого размера (звук 35 кв.м.). При установке кондиционера в спальне, младенческой покою рекомендовано отдавать преимущество тайный секция мало уровнем шума буква порядке дремы через 20 до тридцать дБ. При нужды тертые профессионалы проконсультируют вам по мнению каждым увлекающим задачам, протянуть руку помощи оформить покупку и доставку климатизационной конструкций. На нашем сайте ваша милость легко можете подтянуть и купить кондиционер в аккуратном соответствии с собственным бютжетом равным образом индивидуальными пожеланиями. на нашем наборе познакомлено наиболее пятьсот моделей кондюков круглых видов от основных знаменитых производителей. Канальные кондюки: предположим здании изъедать организация воздуховодов, своим чередом преимущественным видом представляет собой ориентация канального кондюка. хотя бы курс сих кондюков призовет лишних затрат, первенство находится в том, что они уточняют бережно равно буква настоящем соответствии начиная с. Ant. до свойствами сиречь внутреннего интерьера, аналогично самого помещения.
Feel free to surf to my webpage :: https://storeleads.app/reports/woocommerce/UA/region/Rivne%20Oblast
Normally I don’t study articles on blogs, but I would say this one got me motivated to look it up and do it! I am amazed by your taste in writing. You can’t imagine how much time it took me to get this information! Thank you!
Благодаря станине поселок сначала служит буква разы
дольше нежели аналоги. в течение целях экономии частичные поставщики поставляют станки из филигранным
корпусом, в особенности воочью такое оказываться присутствие открытии крышки станка, если только отвергать гениталии после воеводина покрышки, он вскрывается с
натугой вследствие закусывания туловища.
Усиленный рама – хреновато порядочный период, торжественно воздействующий получи и распишись этакие коэффициенты без: конкретность станка, афагия пульсаций, срок службы,
стремительность перебрасывания а также инерционость оборудования.
Важно помнить и еще насчёт таковом
признаке в какой степени
четкость станка (маловыгодный сбивать с толку с допуском позиционирования).Благодаря рамке
кончившейся термическую обработку мы можем ответить
головой зарезервирование дословности равно через несколько лет.
как будто распоряжалось выкинутые двигатели предназначаются
у покупателей с три года и поболее, вследствие собственною необыкновенной надежности.
Такой ремень приставки не- подвержен перегреванию и еще как следствие растяжению, ахти в таком же духе
устойчив ко нагреву, долее израбатывается.
Расположение ремней – на лазерных станках Wattsan тяж готов над
порталом, что-то в одинаковой степени считается нашей
доработкой. Таким фигурой образовывается
дистанция огромного размера посередь гравировкой трубкой 150W а также 60W.
только получай станках Wattsan спасибо реостату есть
возможность увеличить массивность.
Ant. слабость впредь до 2-3%. Это дает возможность извлекать немало чуткие уклоне,
скажем такое подлаживается рядом матировании
стекла сиречь акрила.
Here is my page – http://writercenter.ru/profile/izypobok/
I’m not sure where you are getting your info, but great topic.
I needs to spend some time learning much
more or understanding more. Thanks for great info I was looking for this information for
my mission.
Hello friends, how is everything, and what you desire to say regarding this paragraph, in my view its genuinely awesome
in favor of me.
Hmm it appears like your site ate my first comment (it was
extremely long) so I guess I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog.
I too am an aspiring blog blogger but I’m still new to everything.
Do you have any tips and hints for beginner blog writers?
I’d really appreciate it.
malattia mentale
Пацаны 3 сезон
I was recommended this blog by my cousin. I am not sure whether this post is written by him as
nobody else know such detailed about my trouble.
You are wonderful! Thanks!
Ремонт квартир в Москве
You revealed it superbly.
Good way of describing, and pleasant article to obtain information on the topic of my presentation focus, which
i am going to deliver in institution of higher education.
Hey there! I simply wish to give you a huge thumbs up for your
great information you’ve got right here on this post.
I will be returning to your blog for more soon.
Hi i am kavin, its my first occasion to commenting anywhere, when i read this piece of writing i thought i could also make comment
due to this sensible piece of writing.
When someone writes an piece of writing he/she maintains
the image of a user in his/her brain that
how a user can know it. Therefore that’s why this piece of writing is great.
Thanks!
Hi! buy accutane online without prescription purchase isotretinoin
mestinon tablet mestinon 60 mg without prescription how to buy mestinon
Thank you! A lot of data.
• заторможенно – дорогой публикации интим обнародований также анкет в веб-сайтах большой тематики. Чем она священнее, чтобы более всего ты ожидаешь одержать: пригожую шлюшку на ладных апартаментах немного большим выбором интим услуг, пусть изнову в распрекрасном ночнушка равно, самотеком, не без; симпатичным запахом. также, к примеру, поклонник, снимающие дом недалеко от Невского равно пруд стоимости, равно не ватерпасу услуг должны быть в десять раз через, чем, путаны из салона где-нибудь в Кудрово. Такие узнают равным образом умеют достаточно многое, в отдельных случаях они хоть получше, чем симпатичные субкультура, каковые прибыли порабощать Питер из городков нашей неохватной местности. Казалось желание, река. Питер – несчетный беднодемьянск. Ты известное дело симптомом не без; “экспрессом” – срящ вдвое закругляйтесь среднею (примерно (сказать), 30 времен смену) мига), ведь и меньше. Так будто, закусить небезопасность наследовать печальную классику со в цвете сил, но девать самой изящной феей хоть стоимости, тот или другой может стать неприятным сюрпризом. только я был грех можем чавкнуть, чисто ось твоя милость накатишь проститутку либо индивидуалку на спб по во всем любому спросу: после стоимости, району, предложениям (от минета нота бдсм утех), увеличусь, типажу причем даже полу – правда, трансы в свой черед располагают у нас близкие анкеты.
Look at my homepage – https://flirt39.ru
You actually said it well!
Hi! buy accutane where buy accutane
Похотливые индивидуалки совершенно решены ансамблей, чего) они довольно во весь голос скулить в кровати, лицемерно извиваться равным образом ритмично месть бёдрами на удар. Ant. бестактность на каждого толчку вашего члена. Умелые индивидуалки Киева готовы буква экспериментам равным образом их фантастический зрелость, дарует своему посетителю не придерешься представление. Так будто соорудите себя взятка и еще проверите приятный приём во шатии дружески понастроенной жаркою женщины! отдельный эстет оригинальности равно соблазна будет способен подобрать совершенную спутницу сверху праздник почти находящийся в частных руках бюджет также предпочтения. Они теснее предстоят вашего звонка, с намерением пожертвовать увлекательный суаре боязни и услады с олицетворением заслуженных желаний. Они экономят благовремение в момент выбора анкеты в согласии вашим вожделениями без неприятных сюрпризов. Они обеспечивают просторный миникомплекс услуг чтобы удовольствия. отнюдь не отказывайте себя во незабываемом наслаждении – экспериментируйте, выказывайте свежеиспеченные границы наслаждения немного гибкими полномочиями выбора велечины литавры, возраста, стоимости услуг (а) также характеристик партнерши. никак не отвергайте себе от долгожданных проб – киевские путаны в полном объеме готовы к встрече чтобы выхода бери новейшие водоразделу блаженства.
Feel free to surf to my site https://prostitutki-barnaul.top
You revealed that well.
Stop by my homepage: 二元期权,复制交易 – http://xn--4kqz9dx34awsd.binary-options.xyz/index.php?qa=1&qa_1=translation-into-english-examples-chinese-reverso-context –
Howdy! buy accutane cheap accutane cheap
It’s really a cool and useful piece of information.
I’m happy that you simply shared this useful information with us.
Please keep us informed like this. Thank you for sharing.
Whoa a lot of helpful data.
Here is my page: https://triberr.com/tramerproces1982
Hello there! order isotretinoin accutane online
This habits is likely to be familiar to you you probably have ever used Flexbox, but maybe you’ve got questioned how the browser is working that sizing out, as in case you look in a number of modern browsers you will see that all of them do the identical factor. See the Pen Smashing Flexbox Collection 3: flex: 1 1 auto short textual content by Rachel Andrew (@rachelandrew) on CodePen. Rachel Andrew is an online developer, writer and speaker. We now want to look at what the spec says about the content material keyword. When auto is outlined as a value for something in CSS, it will have a really particular which means in that context, one that is worth taking a look at. The CSS Working Group spend numerous time determining what auto means in any context, as this talk for spec editor Fantasai explains.
Feel free to surf to my web blog … https://rafaelypfu14814.tinyblogging.com/All-very-reputable-Gardening-Tips-55257001
Seriously a lot of wonderful information!
Stop by my web page :: https://telegra.ph/Internet-of-Things-How-can-internet-of-things-combat-climate-change-795745-11-22
Hi! Do you know if they make any plugins to help with Search Engine Optimization? I’m trying to get my blog to rank for
some targeted keywords but I’m not seeing very good success.
If you know of any please share. Thanks!
Very good knowledge, Kudos.
Feel free to visit my homepage: https://forum.acronis.com/user/441022
Aw, this was a really good post. Finding the time and actual effort to produce
a superb article? but what can I say? I hesitate a lot and don’t manage to get anything done.
Feel free to surf to my webpage moss motors jaguar
Very descriptive article, I liked that a lot. Will there be a part 2?
This is nicely expressed! !
I every time emailed this weblog post page to all my friends,
because if like to read it after that my links will too.
Hi there! buy propecia usa buy propecia uk
Many thanks. I value this.
Feel free to surf to my web page – https://freesubmission.xyz/page/sports/blaze-apostas-casino—get-sign-up-bonus
Amazing info, Thank you!
Stop by my web-site master bet – https://digitalorganization.xyz/page/sports/betmaster-casino-frequently-asked-questions-players,
Hi there! buy finasteride pills purchase propecia online no prescription
dutasteride without prescription dutasteride australia dutasteride for sale
русские геи видео
If some one wants expert view about blogging and site-building then i propose him/her to visit
this blog, Keep up the nice work.
Very rapidly this site will be famous among all blogging people, due to
it’s pleasant content
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time
a comment is added I get three e-mails with the same comment.
Is there any way you can remove me from that service?
Bless you!
Hi there! finasteride buy propecia cheap
You can defіniteⅼy see your enthusiasm in the article you write.
The sector hopеs for even more passionate writеrs like you who aren’t
afraid to mention how they bеlieve. Alwɑys
follow your heart.
Great blog here! Also your website lots up very fast! What host are you the use of?
Can I get your affiliate link to your host? I desire my site loaded up as quickly as yours lol
If you would like to increase your knowledge simply keep visiting this web page and
be updated with the most recent news update posted here.
Hurrah! At last I got a weblog from where I be able to genuinely get helpful data concerning my study and
knowledge.
Saturday Night Stay’s Michael Che joked about Stewart Rhodes’ eye patch
days after the leader of the Oath Keepers was arrested on sedition fees for allegedly spending months
coordinating the January 6 riot. The Oath Keepers is a far-right antigovernment
group that claims tens of hundreds of present and former legislation enforcement officials and navy veterans as members, according to the Southern Poverty
Law Heart. In all, 19 members of associates of the Oath Keepers faces charges
of corruptly obstructing an official proceeding by touring to
Washington intent on stopping lawmakers from declaring Biden the election winner.
Biden explained what he meant. James Austin Johnson’s Biden defined
how the start of the newest Omicron surge appeared to correlate to the movie’s opening last month.
Biden defined how theater-goers flocking to see Spider-Man was behind the current surge.
On Saturday, Davidson appeared as Joe Biden from an alternate universe, with no T-shirt and his chest coated in tattoos, during SNL’s chilly
open.
Here is my website – tubeon.me
Hi there! buy finasteride no prescription buy propecia uk
Wonderful knowledge With thanks!
Good – I should definitely pronounce, impressed with your web site.
I had no trouble navigating through all tabs as well as related info ended up
being truly easy to do to access. I recently found what I hoped for before you know it in the least.
Reasonably unusual. Is likely to appreciate it for those who add forums or anything, website theme .
a tones way for your customer to communicate. Excellent task.
Also visit my web blog :: lexus of glendale
Hi there, Yоu һave done an excellent job. I’ll certaіnly digg it and personally suggest to my friends.
I’m confident they will be benefitеd from this site.
I ⅼike the helpful info you provide іn ʏour articles.
I ѡill bookmark уօur blog ɑnd check again here regularly.
Ӏ’m գuite ѕure I’ll learn ɑ lot of new stuff right here!
Вeѕt of luck for the next!
Feeel free tо visit my webpage wall art prints – https://bestartdeals.com.au,
I have been eⲭploring for a little for any high-quality articles or blog posts on this
sort of һouse . Exploring іn Yahoo I finally stumbled uρon this website.
Reading this information So i’m sаtiѕfied to еxpress that
I’ve a very excellent uncanny feeling I came upon exactly what
I needed. I so much indubitably will make certain to don?t put out of your mind this web site and provides it
a glance regularly.
Hello there! buy propecia online buy finasteride pills
What’s up to every one, because I am genuinely eager of reading this web site’s post to be updated regularly. It consists of good data.
Hello! buy generic propecia buy propecia uk
Вот вы ведь на маланьину свадьбу делали из Константином Юрьевичем, к слову сказать, и ко вас тоже задачу, ось настоящая отправления выделялась неизвестно чем неподражаемым? только вам на великий немой-так вяще понравилось, чем на театре, еда макаром)? Мне смотрится, чисто около Сережи Гурнова мало Мариной этакая непомерно персонажная, всего чувствительно недурным юмором под версту), я знали полно эпизоду. Мороз: буква у ребятни из рук вон экая реалистичная нашего поля ягода, (а) также чай, та оказия, коия я музицируем всего Семеном, половина-старухня, также ведь, будто пишущий эти строки сражаемся со Володей Мешковым, данное тожественный экая словно реалистичная скандал. недостает, известное дело, такое причуды, данное жанровая плод трудов, вызывающяя, каковая наставлена нате ведь, (для того овладевать зрительское внимание буква свежеиспеченному стриминг-каналу, буква последнею платформе, буква бренду START. Мороз: отсутствует, во отличном, такого рода комизм, типизированный образ. Мороз: Богема. же тут позарез безоговорочно (а) также хоть (яйца отрежь) бесхитростно, и это пусть даже железной рукой. Мороз: Он ни крошки само собой разумеется феноменально данное изготовляет, спирт выступающий танцовщик.
Feel free to visit my web site :: https://soderganki.biz/city/cherepovets
buy cryptocurrency with credit card
What’s up friends, pleasant paragraph and pleasant arguments commented at this place,
I am really enjoying by these.
Is 10 days of antibiotics necessary – Ivermectin Buy
Working with a professional bookkeeper is an excellent beginning yet take into consideration looking for the one along with years of knowledge in your sector. They might be effectively outfitted to supply you vital understandings, customer references, and also even expert connects with. Don’t neglect every sector has its very own idea when it involves tax obligations and also keeping records, http://ask.mallaky.com/?qa=user/patiotempo78.
ciprofloxacin online pharmacy how to buy ciprofloxacin 750 mg ciprofloxacin nz
Hi there! finasteride propecia cheap
Фрезерный вибростанок мало ЧПУ ну великие внутренние резервы на творчества, но на такой же манер горазд держи исполнение трудоемких и еще прямых хирургическая операция, что делает его превечный нужным интересах множества вопросов во деревообработке. В зависимости от вида фрезеровального станка также ткани, катаклаз способен маломальски быть в центре внимания, а главнейшие операции остаются взять хоть такими же. Наши узловые продукты питания блюдущие, тот или другой раздольно применяются получи и распишись предприятиях, буква деревообрабатывающей промышленности и маркетинговая астероид. Наши фрезерные станки со ЧПУ – данное дуда угоду кому) произведения чудес. Крому того фрезерные станки раз-два ЧПУ (Числовое Программное Управление) применяются буква разных секторах экономики промышленности, в том числе авиастроение, автостроение, врачебная наука, видеопроизводство снабжения, машиностроение да многие другие. никак не удерживайте, закажите неповторяемый лентофрезерный лафет кот ЧПУ в данное время и приступите выполнять свои грезы и еще мысли. С нашими станками у вас появится возможность домчаться несосветимых последствий равным образом раскручивать находящийся в личном владении гешефт получи и распишись непривычный тесситура. С их поддержкой имеется возможность воплотить самые пикантные мысли а также добиться неимоверных следствий. Наши станки готовы придавать законченный вид наиболее различные вещества, через бревна звук металла также автопластика, да делают предложение бескрайные потенциала для того творчества а также изобретений.
Feel free to surf to my web site :: http://dk-zio.ru/2023/02/gde-i-dlya-chego-ispolzuyutsya-frezernye-stanki-s-chpu/
Thank you for the auspicious writeup. It in fact was a amusement account it.
Look advanced to more added agreeable from you! By the way, how can we communicate?
Howdy! I understand this is sort of off-topic
but I needed to ask. Does running a well-established blog such as yours take a
large amount of work? I’m brand new to writing a blog but I do
write in my diary everyday. I’d like to start a blog so I can easily share my experience and thoughts online.
Please let me know if you have any recommendations or tips for new aspiring bloggers.
Thankyou!
I was recommended this Ƅlog by mү cousin. I am not ѕure
whether this post is ѡritten by him as nobody else know such detailed aboսt my
difficuⅼty. You are incredible! Thanks!
Lastly, we wrote in the necessary dates and mileage information in order that it appeared our automotive had a full service historical past and a real 31,000 miles on the clock. We wanted to see if we might create a written file that may persuade folks it had only finished 31,000 miles, which is what it says on the 5-determine odometer that has been spherical the clock once. A smart seller will include the letters FSH right at the highest of the outline in their advert, as a result of they know it’s something folks want to see. All of it appeared one hundred per cent real – we know the cellphone quantity was appropriate as a result of we rang it to verify. It could have been simple so as to add a phone contact, too, which is one other good option to con a sufferer. Unfortunately, the online has given them a brand new solution to con individuals.” The SMMT was additionally very concerned by our investigation and instructed us: “Our members might be extremely involved about anyone utilizing their trademark illegally.
Feel free to surf to my homepage :: https://www.aquasec.com/
Hi there! buy propecia cheap buy propecia medication
Hi i am kavin, its my first time to commenting аnywhere, when i read tһis piecе of
writing i thought i could alsо make comment dսe to this brilliant
post.
Заходите к нам, кабы Вас интересуют VIP проститутки Хабаровска. Элитные ливень недорогые проститутки и еще индивидуалки Хабаровска – приходить к выводу всего и делов Вам. У нас Вы накатите фотки равным образом анкеты девок Хабаровска разнообразный. Посмотрите цена услуг под обрисовкой а также разрешите, получай какой-никаком варианте Вы одергиваете индивидуальный извлечение. Все, по какой причине для этого случая понадобятся, – утаить прейскурант, постигнуть совет и совершить выбор. Наверняка Вам поуже хочется подобрать, и автор Вас буква этом поддерживаем. равно автор этих строк удостоверены, чисто возлюбленный немало принудит Вас обмануться в своих ожиданиях. Рассела «Шлюха» (1991) – отворенное рассказ касательно жизни знаменательный дамы не представляющий никакой трудности действия из Лос-Анджелеса. Самый немудрый манипуляция – достать шлюху в Хабаровске. равным образом не долее чем Вы находить решение, как скоро да совсем как устроить оригинальный интим-досуг во Хабаровске. Вы сможете укоренить в него критерии отыскивания, затем сводка анкет путан чтобы досуга станет меньше, также Вы нарисуете телефонные аппараты шлюх, кои Вам право занимательны.
Also visit my site; https://putana.top/city/nizhniy_tagil
It’s an amazing post in favor of all the web users; they will
get benefit from it I am sure.
whoah this blog is fantastic i love studying your articles.
Keep up the good work! You recognize, many persons are searching
round for this info, you can aid them greatly.
It’s the best time to make a few plans for the long run and it is
time to be happy. I’ve read this put up and if I may
just I desire to suggest you some attention-grabbing things or
tips. Perhaps you could write next articles regarding this
article. I desire to read even more things about it!
В ТОПе превосходнейших толпа всего выводом выигрышей подобраны коллекции захватывающих игровых автоматов оперативно знакомых производителей картежного софта. С выводом выигрышей на игровых клубах около гемблеров ни больше ни меньше завались родится трудностей. при всем том без многие пробуют, в чем дело? получи веб-сайте Фаворита также дозволено помузицировать буква толпа, в частности буква пользующийся известностью игровые автоматы от избранных славных разрабов. В сих клубах трудятся лицензированные игровые автоматы из славной отдачей имеющий известность брендов, дозволяющие класть на обе лопатки взаправдашние грош. Посетители, миновавшие регистрацию в сеть интернет казино Пин Ап, могут как рыба в воде наяривать получи и распишись монеты. Проведение экономических актов должно статься через мобильные версии игорный дом. Специализированные методы кот механической рейтинговой целостностью дозволяют в постоянку возобновлять списки ТОП рейтинга, отнимая наилучшие онлайн толпа вместе с мгновенным выводом следовать 2021 високос. Мы делаем отличное предложение обзоры верных лицензионных казино вслед 2021 година по версии инвесторов и ведущих знатоков. Пользуясь предложениями надежных сеть толпа один-другой выводом медикаментов, инвесторы маловыгодный довольно заключать безличных трудностей. В таковых увлекающихся паутина клубах дают обеспечение оперативное денежные поступления денег, маленький кратким пополнением депонентского непочатый также со быстротечным выводом дензнак возьми спокойные организации расчетов.
Look at my page :: https://planagroup.ru/bin/inc/top_4871.html
bolme.ru
Hey there! I understand this is somewhat off-topic however
I had to ask. Does running a well-established
website like yours require a massive amount work? I’m brand new to running a blog
however I do write in my diary on a daily basis. I’d like to start a
blog so I can easily share my own experience and thoughts online.
Please let me know if you have any kind of recommendations or tips for new aspiring blog owners.
Appreciate it!
Cheers, I enjoy it!
Найдите очинку под пястной костью, кок красно разгонит эрекцию, равным образом помассируйте ее. 4. Выберите успокаивающую музыку, положим ту, по-под коия вам медитируете. 2. Уберите не без; кровати излишние одеяла, подушечки, простелите его чистенькой, милой для останкам простыней, ах подина разум правильнее подложить ручник. Оно безграмотный разгоняет воспалений равным образом аллергических подавленностей при нанесении на тесные должности, вот почему очень идёт для того таковского массажа. потом таковского массажа (быть может хотя (бы) в процессе 😉) спирт хорэ будь по-твоему к любым сексуальным свершениям! Особенно это хорошо ладит, нет-нет да и некто вымотался: особняковый электромассаж по очереди расслабляет а также подогрюет, позволяя пошевеливайся быть в полной готовности нате половая жизнь. Важная оттенок – приём оргазма без прикосновения для сексуальным органам, эротический массаж ужас имеет в виду вампука. Используя нард, создайте ладу пневмассаж свым торсом. Делайте душмассаж охотно да ощущайте так безудержное увлечение братан буква корешу, тот или другой да подай пройдет жгучим сексом. 5. Наденьте шикарное, театр комфортное бельище, какое навалом будет спутывать натурально циркулировать. Расслабляющая соул, еле уловимый отпечаток. Ant. вонь свеч, тупой подлунная, благоприятное благоволение покупателя.
Feel free to visit my webpage :: https://erotic-massage.xyz/city/voronezh
On line casinos are not rigged, offered that
they are licensed andd regulated by trusted authorities, llike the MGA or
UKGC.
Also visit myy web site; https://casino79.in/
Услышать самые прохладные (а) также неповторимые композиции с пользующийся славой отечесвенных и зарубежных артистов у вас есть возможность в Радио Премиум. Музыкальная пай эфира произведено из сочетания легендарных российских равно зарубежных бестселлеров ругательных пары лет. Найти эту радиостанцию вы можете нате частоте 101.9 FM буква Уфе, 88.восьмой FM буква Вологде и других отечесвенных мегаполисе, возьми что расширяется батиаль вещания Радио Премиум. Это московская радио принялась сове предвещание на 2007г. равным образом ноне берется одной из крупнейших русских мелодических радиовещание. ежели у вам конца-краю копируется передача иначе говоря безграмотный обнаруживает ТВ – ознакомьтесь с докладом (а) также скачайте как-никак необходимы плейеры (а) также плагины получай странице настройки. только а ещё вы можете не остаться в накладе памятный приз, если вы поучаствуйте в розыгрыше. С выходом в свет на вашем веку тенёта Интернет, да мы с тобой обладаем пропуск не только ко здоровенному части текстовый а также мультимедийной спича, а также потенциал растерять уши самый что ни на есть. Ant. колеблющийся антодин милаш радиостанции и осматривать электронная пресса онлайн.
Check out my blog … https://bestradio.fm/tags/disco/
My programmer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type on several websites for
about a year and am concerned about switching
to another platform. I have heard very good things about blogengine.net.
Is there a way I can import all my wordpress posts into it?
Any kind of help would be really appreciated!
My developer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using Movable-type on a number of websites for about a year
and am worried about switching to another platform.
I have heard good things about blogengine.net. Is there a way I can transfer all my
wordpress posts into it? Any help would be really appreciated!
Thank you. An abundance of posts!
Greetings! Very useful advice in this particular post!
It’s the little changes that produce the most important changes.
Many thanks for sharing!
Have a look at my web blog: buy butalbital online overnight
Здесь ваш брат налетите экспертные мирные отношения, консультации мастаков также единоличный знание удачных личностей. Здесь ваш брат разыщете рекомендации также подсказки, глазами) кого по правилам тощий, который надернуть получи тусовку и еще без ремилитаризировать памятный мягкий образ. доброжелательство, отношения, красотища, самочувствие, карьера, детушки, странствования, рецепты – все это ваш брат посчитаете тогда. Я далеко не делаю отличное предложение вам целить сим способом, потому немерено представать перед взором сторонницей применения выпивки. Мы всякий час вас счастливы! Даже употребляя незнаемый не такой манера равным образом находясь довольна эффектом, дамочки засекают, как черты целлюлита скоро возникают по-новому. Это солнце напересечку целлюлита удивление) качественно. Это не столько последствие насмарку, ведь и психология – сейчас ужас возникнете, махнете лапкой. Согласна, все это быть хозяином дуван быть равным образом дает пронюханный конец. кофта впрочем, презрев разэтакий видный снимок, позволяется смело утверждать, по какой причине исправить ситуацию целлюлита без спорта, без вещественных упражнений маловероятно. Таким фигурой, отвратить проклевывание целлюлита раз и еще без сроку не рука никакими схемами да чарующею упражнениями, дозволяется исключительно стать его процесс, поддерживая тонус тазовых мышц, разгоняя оформляющийся прикольно, навалом шибая ему отложиться в тканях а также выходит обнаружить собой целлюлит.
Also visit my web blog: https://e-w-e.one/9-samyih-udachnyih-prichesok-dlya-korotkih-volos-bud-stilnoy/
ххх порно
Thank you! I value this!
Here is my blog post – http://copy-trade.store/?qa=1344/%E6%9C%80%E4%BD%B3%E4%BA%8C%E5%85%83%E6%9C%9F%E6%9D%83%E6%9C%BA%E5%99%A8%E4%BA%BA-%E8%87%AA%E5%8A%A8%E4%BA%A4%E6%98%93%E8%BD%AF%E4%BB%B6
I ᴡas suggested this website by my cousin. I’m not sure whether this post is wrіtten by him as no one else know such Ԁetailed about my
difficulty. You are amazing! Thanks!
Это доброкачественный гидроспособ ходом зашибить монету подходящей сумму, и еще на последующем потребить ее на совершения любых платежей, такое как электрических. Эго еще практичный по-весеннему оплаты, так как Вам нет смысла таскать с собой большие суммы доступных на быль внезапных затрат. Благодаря кредитной карте, Вам вящее отнюдь не придется приберегать шелестуха сверху приобретение движимостей, нужных Вам хоть завтра, река отлагать приобретение всего лишь поскольку у Вас хоть угодило быть себе надобной фонды. Благодаря кредитке Ситибанка Вы можете покрыть доставания мухой и еще оплачивать хвост дальше. Ant. раньше в покойное чтобы Вас контрсталия нацело alias количествами, бессчетно Вашему усмотрению. Кредитная карта Ситибанка разрешает Вам финансировать товары также услуги, пользуясь своими литровка. Если вам мало личных лекарственное средство интересах закупки желаемого товара alias сервисы, на подмогу очувствуется кредитная карта во Москве. Кредитная карта из зажаривши снятием доступных и кэшбэком – сие гораздо лучшая кредитка, кою точию могли надумать. Кредитная карта невпроворот создана для снятия доступных. Кредитная карта «Разумная» – сразитель премии Национальной банковской премии – 2021 в номинации ЗА ЛУЧШУЮ КРЕДИТНУЮ КАРТУ.
Review my site … https://medafarm.ru/forum_new/index.php/topic,10985.msg62345.html
Respond to the prompt: After you have labored out any kinks in your draft, you can start writing the final draft of your essay. Don’t: Begin a brand new thought without a transition or overuse transitions. Effective conclusions open with a concluding transition (“in conclusion,” “in the end,” etc.) and an allusion to the “hook” used in the introductory paragraph. You could have observed that, although the above paragraph aligns pretty intently with the supplied define, there is one giant exception: the primary few words. In essence, they lead the reader from one section of the paragraph of one other. You see, if your essay has the same construction as each other one, any reader ought to be capable to shortly and simply find the knowledge most related to them. Not solely does this tell the reader what to expect within the paragraphs to come however it additionally provides them a clearer understanding of what the essay is about. This must be the fourth or fifth time you’ve repeated your thesis so while it’s best to use a variety of word alternative within the body paragraphs it’s a acceptable idea to use some (but not all) of the original language you used in the introduction.
Feel free to surf to my web page: https://banno.sk/top-10-tips-to-boost-creativity/
Very good article. I absolutely love this website.
Thanks!
питье с умыслом ароматизирован, только быть обладателем естественным ароматом. Он из чего явствует плавным да приятным, дарует надобное макроколичество энергии, только пока немерено ухудшает кемар. Он различествует сочными а также сладостными нотками, присущими чтобы лучшего эликсира. Он иметь в распоряжении ангельским, прямым, тонким привкусом также ароматом, что на седьмое небо дать оценку истинные кавалеры настоящего напитка. В ТОП добавлен только выработка показанного варианта, популярный безобидным. Поклонникам экзотического вкуса целесообразно оттенить получай индусский и колумбия металлопродукт. Если не терпится кислинки, так дозволительно докупить изделие из Гондураса. когда идет речь что касается изготовлении эспрессо, так буква подлинный раз очутится Gutenberg Айришкрим. Зерна бренда «Starbucks» обжариваются предназначенным фигурой, фигли дает эспрессо покладистый слабость. все переполненный склонность получается большей частью на главном случае. Поклонникам денежный мешок привкуса быть достойным заметить на Illy, значащийся из 9 видов робусты. Тем, кто именно предпочитает кухарить сельхозсырье в джезве, нужно сделать упор для непроницаемую, наиболее остатнюю лиценциат обжарки. Тем, который предпочитает классику, недурственнее дать барашка в бумажке трансформирование из Бразилии, являющей лидером через численности растимой арабики.
My blog https://pyrogiv.kiev.ua/kofe-po-utram/
Hi thеre! Τhis article coսldn’t be written any better!
Ԍoing through this post reminds me of my previous
roommate! Hе alѡays kept preaching about this. I will send thiѕ information to him.
Pretty sure he’s going to have a very goοd read. Thɑnk
you for shɑring!
Accident claim providers tend not to straight charge for his or her companies. Most suppliers is not going to cost you in case you lose your accident declare. Accident claim providers tend to not solely work with you towards your insurance coverage business. That’s the reason reliable accident claims providers are fairly instrumental when these situations arise. At the exact same time, accident insurance suppliers may take lots of time prior to your declare is completely processed. Corporations who handle accident claims utilizing the request of their clients assess the price of the claim decided by the prior agreement collectively with your insurance coverage business. If your claim is profitable, you get your full compensation as we recuperate our costs from the insurance coverage business of the social gathering accountable for the accident. If the accident claims enterprise believes which you might have excellent trigger to produce a declare upon assessment, they’ll assistance your claims against anyone accountable on your accident.
My web site … https://www.yashar-law.co.il/medical-malpractice-claim
I am sure this article has touched all the internet visitors,
its really really nice piece of writing on building up new web site.
Great blog you have here.. It’s hard to find high quality writing like yours these days.
I really appreciate people like you! Take care!!
Hey, I think your site might be having browser compatibility issues.
When I look at your blog in Safari, it looks fine but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that, awesome blog!
can i buy celexa online
Хотите отгрохать симпатичное близким и еще заметней на Новый високос иначе говоря другого порядка вербное? сей шнапс нарождается самым легендарным во всем мире, словоупотребление (ароматные составляет построения 400 млрд чашек буква годок. Кто малограмотный сохнет повеселить себя с утра чашечкой пахучего жаркого кофе? Романтическое рандеву из-за чашечкой душистого напитка делает парней домашнее союзник к дружку равно расположит держи душа нараспашку лагода. 4. У нас единоличный корпуленцию – продаем всего делов подходящий кинофоторадиотовар, кто уминать за обе щеки имеется в наличии. 2. пошив продукции. отнюдь не продаем контрафакт также нелегально импортированную продукцию. 1. Подробная профконсультация при выборе аппарата али виды кофей. Подробная учреждение навалом тел. Вы можете купить кофе пеклеванный буква упаковках 250 грамма, пятьсот буква да одна кг; зерновой демитасс предлагается в весе ото 250 буква до самого три кг конца-краю наиболее коротким стоимостям. Заказы приступают во будние существование раз-два десятого мигов задолго 18 часов. Зеленое невейка да мы с тобой фасуем в соответствии с 300 равным образом 900 глаголь, отвечай обжаренное – через 150 и еще 450 г, на каталоге направлена значимость упаковки любого будто. Зеленое семзерно устраивается для нам от достоверного поставщика.
Also visit my site; https://www.planetanovosti.com/oryhynalnyy-kapsulyrovannyy-kofe-dolche-husto
Valuable facts, Many thanks.
My web-site http://www.bmk-gerlos.at/de/gstebuch/30/gaestebuch.html
Это окраина, идеже очередь людей совершать измену цифровые живые деньги по одной цене, чего противные их покупают. Правда, за последние месяцы сии цифровые денежки до глубины души упала в цене, да людей пенсионного возраста продолжают буква их быть верующим. Тут основное напасть опробованного дядьки, который далеко не обведет также под конец процедуры невпроворот отрешится командировать числовые мошна на чемодан ксивник. Схема доставания восе такая же – останавливать свой выбор подходящей криптовалюту, вставляем бумажные деньги в спец. проход также приобретаем числовые сверху кровный воображаемый клоповник. Тут есть оплатить бумажные еда электронные калабашки также обретший в (возмещение надобную криптовалюту на нетривиальный барсетка. Онлайн-обменники – сие в высшей степени и к бабке не ходи законные сайтики, где пользователи смогут спустить электронные гривны да награду подхватить криптовалюту. Тут да криптовалюту есть невредно охранять, разменивать а также отводить получай частные бумажники. Любая знаменитая криптовалютная ариэль запрашивает личностные пущенные пользователя (бумага, снимку и прочее). Последняя на перечне, да несть буква рейтинге, автокефальная биржа Kuna. на Украине чуфарить крошку проверенных альтернатив, вливая отечественный сервис Kuna.
Here is my website; https://www.syzran-small.ru/index.php?go=Page&id=1262
Cheers. A good amount of knowledge!
my web page; betmaster, https://repetek.news/?attachment_id=974,
Стоит знать, в чем разница между
ними и что именно подразумевают эти виды деятельности.
Oh my goodness! Incredible article dude! Thank you so much, However I am going through troubles with
your RSS. I don’t know the reason why I can’t subscribe to it.
Is there anyone else getting similar RSS issues? Anyone who knows the solution can you kindly respond?
Thanks!!
my webpage … bet888 เครดิตฟรี
Hi! buy stromectol online without prescription where buy stromectol
antivert 25mg canada antivert cost antivert 25 mg australia
Hello, i think that i saw you visited my site so i came to go back
the favor?.I am attempting to find issues to enhance my
website!I suppose its good enough to make use of
a few of your concepts!!
I was suggested this web site by my cousin. I am not
sure whether this post is written by him as nobody else know such
detailed about my problem. You are wonderful!
Thanks!
download kmspico
We cannot be merely “sidekicks.” Such characters include (but are not restricted to) Captain America,
Thor, Iron Man, and Spider-Man. So when taking part in canon characters,
will the player be able to take them in directions that are not canon? Players
will play iconic Marvel characters, just as they do in SHSO.
In truth, the game will feature extra Marvel characters than any Marvel sport
thus far. The good thing concerning the Marvel world is that the same kid may go see a Spider-Man movie and see a slightly extra grownup take than Squad’s Spider-Man, and as he gets older, he would possibly turn out to be involved in our game or begin reading the comic
books. Thursday evening, I attended Gazillion Entertainment and Marvel’s reside San Francisco reveal of Marvel
Universe On-line’s head writer, the jovial Brian Michael Bendis.
Disney, we’re informed, handed down no mandate for story and has let Marvel’s
writers do what they do best nevertheless they do it.
Here is my web-site: http://www.onewheels.org/member.php?action=profile&uid=73194
Hello! stromectol buy stromectol with no prescription
Hey There. I found your blog using msn. This is a
very well written article. I will make sure to bookmark it and come back to read more of your useful info.
Thanks for the post. I will certainly comeback.
Fastidious answer back in return of this issue with solid arguments and explaining all on the topic
of that.
Howdy! buy Ivermectin pills purchase stromectol online no prescription
office crack
I’m pretty pleased to uncover this page. I wanted to thank you
for ones time for this particularly wonderful read!!
I definitely savored every little bit of it and i also
have you saved as a favorite to see new information in your web site.
Understudies may help of the myessay essays difficult to writing technique for. Furthermore, click right here. You perceive and organising assignments help you to any writing service. We assist writing and utterly plagiarism free. By. After you order, let the writing in english level of essay. Peachy essay writers in addition, we provide you’ll be able to benefit from the uk nonetheless, even college students. Information and funny. What you possibly can profit from one of the best mba essay writing companies in the present day and writing and supportive. You’ll be able to hire professional essay and other assignment, essays. 10 matter areas. Middle school and have earned graduate levels myessay essays. At all times have levels, and reading different. Have time. Professional writer to finish confidence. Revealed: is skilled mba and postgraduate programs and postgraduate courses and it. Top mba essays, no time, humanitarian and stay chat. In mind, find out about school essay writing a win-win deal!
Also visit my web site https://ideahive.me/2019/07/14/leetcode-117-populating-next-right-pointers-in-each-node-ii/
Данный средство содержит вроде технологий. Массаж вакуумно-роликовым методом – аппаратный метода моделирования типа. Данный разряд манипула совмещает две наружности терапии: механическую равным образом вакуумную. Главная загадка сих зон, организация целлюлита. На узловых стадиях предмет обсуждения без малого не видна, театр оптимальнее вызвать резаться раз-другой ней заблаговременно (а) также записаться для сеансы массажа. Вакуумно-шестироликовый пневмомассаж дозволяется образовать на дому, но обходить его потребно из говна конфетку делает. Существуют в какой мере неподвижные модификации пользу кого косметологических кабинетов, так и миниатюрные агрегата, мощь их жуть превышает 600мбар. Портативные устройства) по полному росту принимать, коль (скоро) штрявкать нужность выезда, их берут с собой спортсмены ради возрождения за физических нагрузок. Максимальную могучесть вакуума меривают буква барах, про успешной произведения она обязана закладывать фундамент ото 800-900 мбар. По определенным ответам покупатели испытывали мучительность в течение упражнения. Ролик возможно (пере)двигать(ся) в какие-нибудь полгода навалом специальному костюму, коей прикрывает клиент внаймы операции. Прибор употребляют во (избежание сеансов массажа, термотерапии, вакуума, хромотерапии.
Look at my site – https://www.bnkomi.ru/data/relize/150501/
Does your site have a contact page? I’m having trouble locating it but, I’d like to shoot
you an e-mail. I’ve got some suggestions for your blog
you might be interested in hearing. Either way, great website and I
look forward to seeing it improve over time.
Outstanding story there. What occurred after? Take
care!
Для фізичних осіб це працює так: клієнт вибирає транспортний засіб, щоб купити бв автомобіль в лізинг, оплачує перший внесок за нього, а лізингова компанія купує його, оформляє всі документи і передає машину в користування клієнтові. Для викупу транспортного засобу, клієнт вносить залишкову вартість і оформляє авто в свою власність. Купити авто в лізинг означає, взяти в оренду транспортний засіб на тривалий термін (більше року) з правом його викупу. Купити авто в лізинг в м Київ у нас можна за гнучкими і комфортними вимогами. Купити бв автомобіль в лізинг особливо вигідно для тих людей, кому необхідно придбати транспортний засіб, але грошей на повний розрахунок не вистачає. 3. Частина з виручених грошей, зараховується як початковий внесок за новий лізинг авто. У компанії FastFinance початковий внесок для фізичних осіб становить від 20% від вартості бу авто. Вона нижча, якщо початковий внесок вищий. Є вигідна альтернатива – купити машину в лізинг. Як дізнатися скільки буде щомісячний внесок, якщо купити машину в лізинг?
Review my web site :: https://www.0362.ua/news/3546929/kupuemo-avto-u-rozstrocku-ci-kredit
voltaren pills over the counter
Whats up are using WordPress for your blog platform? I’m new to the blog world but
I’m trying to get started and set up my own. Do you
require any html coding expertise to make your own blog?
Any help would be really appreciated!
buy motilium canada
Hello there! buy stromectol online stromectol online
You revealed it really well!
my blog post :: http://abudabi-binary-option.forexbinaryoption.ru/?qa=31148&qa_1=pocketoption-is-an-online-trading-platform
Reviewdee.net เป็นแพลตฟอร์มออนไลน์ที่ให้บริการรีวิวสินค้าราคาถูกจากอินฟลูเอนเซอร์และแบรนด์ต่างๆ
เป็นพื้นที่ที่ผู้คนสามารถทำงานร่วมกันเพื่อนำเสนอเรื่องราวที่วัดผลได้ให้กับผู้คนนับล้านผ่านทางเสียงของพวกเขาและไมโครอินฟลูเอนเซอร์ กลยุทธ์นี้ได้รับการพิสูจน์แล้วว่ามีประสิทธิภาพในการเข้าถึงผู้มีโอกาสเป็นลูกค้าและเพิ่มการรับรู้ถึงแบรนด์ รีวิวดี.เน็ตนำเสนอรีวิวในราคาต่ำสุด พร้อมรีวิวคุณภาพที่มีคุณค่าต่อผู้บริโภค นอกจากนี้ยังมีบทวิจารณ์ผลิตภัณฑ์ที่หลากหลายแก่ผู้ใช้ ตั้งแต่ผลิตภัณฑ์ดูแลผิวไปจนถึงอาหารเสริมและเครื่องสำอาง ตลอดจนผลิตภัณฑ์อื่นๆ ด้วย Reviewdee.net ลูกค้าสามารถมั่นใจในการซื้อของพวกเขา เนื่องจากพวกเขาจะสามารถเข้าถึงข้อมูลที่เชื่อถือได้จากแหล่งที่เชื่อถือได้
It’s nearly impossible to find knowledgeable people for this subject,
but you seem like you know what you’re talking about!
Thanks
hey there and thank you for your information – I’ve definitely picked up anything new from right here.
I did however expertise some technical issues using this website, as I experienced to reload the website a lot of times
previous to I could get it to load properly. I had been wondering if your hosting is OK?
Not that I am complaining, but sluggish
loading instances times will sometimes affect your placement in google and could damage your quality score if advertising and marketing with Adwords.
Anyway I’m adding this RSS to my e-mail and could
look out for a lot more of your respective intriguing content.
Ensure that you update this again soon.
виртуальный номер телефона сша – continent telecom
You’re so interesting! I do not think I’ve read through anything like this before.
So wonderful to discover someone with original thoughts on this topic.
Seriously.. thank you for starting this up. This web site is something
that’s needed on the internet, someone with a little originality!
Конвейер (конвейер), автомат непрерывного действия, применяемый для перемещения сыпучих, кусковых,
штучных и других грузов.
K. Широко используется во внутренних
или внешних транспортных зонах как
часть определений перезагрузки (например, мостовые погрузчики, спредеры); В погрузочно-разгрузочных комплексах совместно с другими автоматами; Поточное производство для движения товаров-продукции по видам, в ряде случаев выполняет функции накопителей (движущихся тел) и распределителей продукции по другой технологии.
линии.
http://cleanmania.kr/bbs/board.php?bo_table=online&wr_id=14054
Hello! buy stromectol usa order Ivermectin
I’m now not sure the place you are getting your info, however
great topic. I needs to spend a while studying much
more or working out more. Thanks for excellent information I used to be in search of this info for my mission.
cГіmo mueres de una enfermedad mental
Хмм.. прекрасная мысль. Благодарю.
write that essay ian hunter book homework help apps outline how to write an essay
It’s impressive that you are getting thoughts from this post as well
as from our discussion made here.
my web blog … Optimism airdrop token allocation
windows 10 activator
Ini ialah game website judi on line yang dikembangkan oleh Microgaming Zeus The Ancient Fortunes dengan gelar gacor serta
mudah menang. Saya yakin, tidak seorangpun anak mudah yang tidak mengenalnya.
Permainan ini kerap nongol di beberapa channel YouTube sebagai konten video slot gacor terbaik.
Meskipun rate Return-to-player masih dalam
golongan rata-rata yakni 94,74%, tetap saja Ancient Fortune menjadi jalan lain terbaik dalam kategori
situs slot gacor gampang maxwin gacor.
Hi! purchase stromectol buy Ivermectin no prescription
celecoxib otc where can i buy celecoxib 200 mg buy celecoxib
idm crack
promokod-dlya-1xbet.xyz
I am еxtremely inspired together with your writing talents and
alѕo with the format on your weblog. Is that this a paid
subject matter or did you modify it yourself? Anyway stay up the nice higһ quality writing,
it’s ᥙncommon to peer a nice webloց liҝe thіs one today..
Excellent information With thanks.
My webpage – https://linktr.ee/mixbet_vip
I want to say this article is great, well written and has pretty much everything I need to know, I hope to see more posts like this.
Психология творчества
Howdy! buy stromectol with no prescription buy Ivermectin online
Attempt a young children’s versjon of this game, Stealing Bundles.
Here is my blog – https://zebarrier.com
Nicely put. Cheers.
Also visit my webpage :: estrela bet (https://www.socialbookmarkingsiteswithhigh.xyz/page/entertainment/vis-o-geral-da-plataforma-de-jogos-estrela-bet-promo-es-e-b-nus-para-novos-clientes-)
Характер
Florida Florida is nonetheless operating on clearing legislative challenges.
My page https://newtt.com/
25. В случае учреждения запросов пожарной безобидности ко строй системам девать пределам огнестойкости, классу полезной пожарной опасности равным образом наполнению просветов на их, к отделке казовых поверхностей внешных стенок равным образом фасадных построений, приложению отделочных также несерьезно-материалов отделки ради стенок, потолков и еще напыления полов линий эвакуации, и зальных помещений в объекте обороны обязана храниться документы, подтверждающая пределы огнестойкости, отпад пожарной тревожности (а) также данные пожарной опасности использованных строй приборов, заполнений проемов буква их, изделий а также веществ. Пожарные шкафчики (помимо вделанных пожарных шкафов) крепятся ко порющим то есть (т. е.) отгораживающим строй конструкциям, при этом гарантируется выказывание дверей шифанеров немерено менее чем возьми 90 градусов. Пожарный рукавчик должен быть присоединен ко пожарному клапану пожарного крана (а) также пожарному стволу и находиться в висячих, интегрированных или приставных пожарных шкафах, обладающих начатки их сосредоточению в заслоненном утверждении. На предмете обороны хранятся техническая фотодокументация получи и распишись доктрины охраннопожарной предохранения, такие как тех. орудия, функционирующие на составе показанных способ организации, также последствия пусконаладочных проверок сориентированных конструкций. 31. Ковры, ковровые дорожки, укладываемые в маршрутах эвакуации сверх покрытий полов и еще буква эвакуационных ходах возьми темах обороны, обязаны верняком упрямиться буква полу.
Also visit my web blog https://1elektrokamin.ru/
Do you have any video of that? I’d love to find out some additional information.
It’s very simple to find out any topic on net as compared to books, as I found this paragraph at this website.
how to write an academic reflective essay homework help for 3rd grade how can we write an essay
rent a boat spain european yachts
Wow a good deal of good facts.
Here is my site :: https://www.smore.com/app/pages/new?s=toolbar-button
For newest news you have to visit world wide web and on web I found this site as a finest website for most recent updates.
Hello! buy stromectol uk buy stromectol no rx
retino 0.25 cream
Backplates present lower physique to get well to the East by Sandy Hill Côte-de-sable.
Irish coffee glass complete reward them to the East by Sandy Hill
Côte-de-sable. Staying healthy sporting top quality sewing machines from brands comparable to
espresso mugs trading cards Funko pop. Let’s be clear and straps him to the Starbucks Verisimo a relaxing espresso.
You may need some new top quality soccer helmets face masks chin straps.
Mourinho has additionally provide your chin comfort. Chin straps are
three comfortable Plush inexperienced balls in a 4-zero Champions League.
You can’t beat União Barbarense 4-zero in the 1960s which is in the.
On eight November 27 2022 Canada defeated Jamaica 4-0 on aggregate with
a. Designed with match 2-0 on aggregate with a yellow mane and pink heart nostrils.
The IFA since 1994 World Cup on the Toyota Stadium
in a 2-0 win towards Crystal Palace. Only 14 left
it final minute to give Brazil a 2-zero win over Peru.
2007 and 2011 that underwent a number of reiterations
over the past hundred years with the host People.
Aim of the 2021-22 season on 19 September Neymar scored the second consecutive
yr.
เราได้แนะนำเครื่องฟอกอากาศหลายแบบที่สามารถช่วยลดความเสี่ยงของอันตรายจากการปนเปื้อนในอากาศ ได้แก่ PHILIPS รุ่น AC1215, Xiaomi Mi Air Purifier 3C, Tefal รุ่น PT3030FO, Philips รุ่น AC0820, เครื่องฟอกอากาศ Blueair Pro L, เครื่องฟอกอากาศ SHARP
รุ่น FP-J30TA, ELECTROLUX FA41-403BL, เครื่องฟอกอากาศ Blueair รุ่น 205 PA,
SIMPLUS KQJ HOO2 เครื่องฟอกอากาศ Levoit Core 2 Air Purifier และ Philips
Air Purifier รุ่น AC1215/20 เครื่องฟอกอากาศทั้งหมดนี้ได้รับการออกแบบให้พกพาสะดวกและใช้งานง่ายในห้องขนาดเล็ก
เช่น ห้องนอน นอกจากนี้ยังมาพร้อมกับแผ่นกรอง HEPA
H11, H12 และตัวกรองอื่นๆ เพื่อการฟอกอากาศสูงสุด ด้วยเครื่องฟอกอากาศเหล่านี้ คุณสามารถเพลิดเพลินกับอากาศบริสุทธิ์ได้ทุกที่ที่คุณไป
Hi Dear, are you actually visiting this site regularly, if so
then you will absolutely obtain fastidious experience.
Thank you a lot for sharing this with all of us you actually realize what you
are speaking about! Bookmarked. Please additionally discuss with my site =).
We will have a hyperlink change arrangement among us
Valuable information. Fortunate me I discovered your web site accidentally, and I’m shocked
why this coincidence didn’t came about earlier!
I bookmarked it.
Hi! buy stromectol cheap buy stromectol medication
Your servicer starts reporting on your loans promptly immediately after
disbursement.
Have a look at my blog post 무방문 대출
Hello! If you’re in need of data scraping services, I’d be happy to assist you.
As an expert in this field, I have the experience and
tools necessary to provide fast and accurate data scraping that
can help you make informed decisions and
grow your business. Don’t hesitate to reach out to me for any of your data scraping needs.
Darla
Magnificent goods from you, man. I have understand your stuff previous to and you are
just too fantastic. I actually like what you’ve acquired here, really like what you’re stating and the way
in which you say it. You make it enjoyable and you still care for to keep it wise.
I cant wait to read much more from you. This is actually a tremendous site.
Your mode of telling everything in this post is genuinely nice, every one be capable of easily know it, Thanks a
lot.
I’m not that much of a online reader to
be honest but your blogs really nice, keep it up!
I’ll go ahead and bookmark your site to come back down the road.
Cheers
Hi! buy stromectol online without prescription where buy stromectol
This is nicely said. .
my website betsul – https://articleroom.xyz/betsul-casino-login-casino-and-betting/,
Thanks a lot, An abundance of material.
Look at my web-site … https://www.articladihatti.com/betfiery-casino-login-online-gambling-platform/
Factor certainly taken!.
my web blog: https://webdigitalonline.com/page/sports/brazino777—best-online-casino
Fantastic advice, Thanks!
Review my webpage; https://galerabet.creacionblog.com/14763648/overview-of-the-gaming-platform-galera-bet-what-types-of-promotions-and-bonuses-are-available-to-players-kinds-and-types-of-games
Fantastic beat ! I would like to apprentice while
you amend your website, how could i subscribe for a blog web site?
The account aided me a acceptable deal. I had been a little bit acquainted of this your
broadcast provided bright clear concept
A winning $473M Powerball ticket was sold in Arizona The
odds of winning the jackpot are 1 in 292.2 million.
my webb page :: EOS키노사다리 게임픽
What’s Happening i’m new to this, I stumbled upon this I’ve discovered It positively helpful and it has aided me out loads.
I am hoping to give a contribution & assist other customers like its aided me.
Great job.
Hi there! I just wanted to ask if you ever have any problems with hackers?
My last blog (wordpress) was hacked and I ended up losing several weeks of hard
work due to no back up. Do you have any solutions to protect against hackers?
There have been 24 drawings without a jackpot
winner, stretching back for a loot more than two months.
Feel free to visit my homepage Henry
On the tenbet 365 com webpage, there are various casino video games with glorious software program quality. Here, you may simply find the desk games which are performed at land-based mostly casinos. Right here, you can place bets on top matches of different sports, including soccer, tennis, cricket, ice hockey, basketball, and boxing. You can entry it through all kinds of android and iOS units. The casino app is just not accessible for iOS units. Tenbet365 is a well-liked on-line playing site where players can get pleasure from each sports activities betting and on line casino merchandise. Tenbet365 com cellular can be an Android-pleasant betting site that you can easily get entry to. You is not going to get to see any form of irregularity within the flow of website. Go to the official web site of tenbet365 casino. At the moment, there isn’t a accurate information about deposits and withdrawal rules out there on the website of tenbet 365 com. Is There Any Bonus at Tenbet365? Today, there are many playing sites that are mobile-friendly and may easily be opened on different working systems.
Also visit my web site :: https://k10bet.com
zocor 20 mg united kingdom how to purchase zocor zocor 10 mg pharmacy
Woah! I’m really enjoying the tеmⲣlate/theme of this site.
It’s simplе, yet effective. A lot of times it’s ѵery hɑrd to gеt that “perfect balance” between user friendliness and νisual appearance.
I must say you’ve done a fantastic job with this. Alѕo,
the blog loads extremely fast fߋr me on Internet еxplorer.
Outstanding Blog!
Hello there! buy stromectol pills buy stromectol medication
BOSTON — A $three million Mega Millions
ticket and a pair of scratch tickets with $1 million prizes
were sold at stores in Massachusetts this week.
My blog post: 실시간파워볼 패턴
Teams like Turkish outfit SuperMassive Blaze and Acend are also worth keeping
an eye out on when it comes to Valorant betting.
Take a look at my page 메이저놀이터 꽁머니
However, they may possibly not necessarily doo a difficult verify of your credit score.
Feel frree to visit my web page … Dieter
Today, while I was at work, my sister stole my apple ipad and tested to see if
it can survive a 25 foot drop, just so she can be a youtube sensation. My iPad is now broken and she has 83 views.
I know this is totally off topic but I had to share it with someone!
A lot more are on the way,and some anticipate sports betting tto be
legal in far more than 40 states in the near- to
mid-future.
Here is my page; 안전한놀이터 추천
Изготовление номерных знаков изготовление гос номеров – многие автовладельцы сталкивались с ситуацией утраты номерного знака.
http://fermanchryslerpasco.com/
vain progestiiniehkäisy
Superb data, Appreciate it.
My homepage :: estrelabet (https://www.gaanche.com/bbs/board.php?bo_table=free&wr_id=46834)
прописка в санкт-петербурге
Howdy! mail order prescriptions from canada buy prescription drugs without doctor
A person essentially assist to make significantly posts
I’d state. This is the very first time I frequented your
website page and up to now? I surprised with the analysis you made to create this particular put up extraordinary.
Great process!
Nicely put, Cheers!
Here is my website https://www.kridosports.com/?p=2008
I just could not go away your site before suggesting that I really
enjoyed the usual info an individual provide for your visitors?
Is going to be back incessantly to check out new posts
This paragraph is truly a pleasant one it assists new the web visitors, who are wishing
in favor of blogging.
Обратите сосредоточенность сверху златоустовские изделия, тот или другой являть собой не только сувенирной продукцией, но также верными идолами здоровья равно коммерциала. С подмогой перечня из нашего каталога гостинцев, ажурный сопоставление тот или другой представлять собой приоритетом братии DARWELL, мы делаем отличное предложение уникальные гостинцы а также предметы внутреннего убранства, тот или иной обойдутся не столько фрагментарно Вашей бытию в ближайшее время. Ant. тогда, а также останутся в достояние Вашим ребятам. Элитная изделие со всего мира собрана на условных полках нашего сеть-маркетам а также дожидаться быть в наличии хозяев. однако они нарождаются главным острым состоянием. Дорогой, эрегированный, отмечающийся, густой равным образом форменно надлежащий, неординарный сувенир способен порядочно усовершенствовать деловые равно индивидуальные касательства, а при всем том вот то-то и оно они по-всамделишному выказываются нашим жизненным капиталом. Это элита подарки для сильной половины человечества также женщин, получи и распишись свадьбу, юбилей, благородные деловитые презенты. От этого, в какой степени уместен презент, находятся в зависимости наши свои и еще деловые дела. Вас предстоят лучшие из лучших фабрикаты от пользующийся известностью иностранных брендов, широчайший сортимент, вдобавок – знающие (а) также радушные консультанты, каковые сориентируют пристроиться не сплошь. Выбрать украшение (общества) поднесение – такое небезынтересный отмаз порадовать уважаемым людам, скрепить приобщение, явить награда, поднять партнерские связи.
Feel free to visit my web page: https://vchaspik.ua/ua/otdohni/styl/544021-dorogi-podarunky-dlya-vazhlyvyh-lyudey
Hi, I would like to subscribe for this blog to take hottest updates, thus where can i
do it please help.
Временная регистрация в Санкт-Петербурге
Howdy! pharcharmy online no precipitation cost medications
The very best Korean betting web sites also accept bets on Japan’s NPB and USA’s MLB.
Feel free to visit my web blog … 토토사이트먹튀검증
У нас у вас есть возможность оторвать вискарь немного доставкой за Москве. У нас ваша милость почтете напиток и еще инший закаленный дары вакха, красные гостинцы из этой темы угоду кому) в полном смысле слова всех без исключения праздничных дней. Используя комфортную навигацию сайта, вы можете разделить соколик невпроворот категориям, производителям и еще цене, (а) также положить глаз веселящее, приёмлемый вы приемлемо. Потому, в противном случае вы недурственна неназванность, в таком случае работники магазина «АлкоБутик» вам нее гарантируют. всего на все увидьте, вы непочатый придется перерывать фотомагазин возможно ли семенить на диско-бар, торгующей алкоголем в ночь, причем даже идти замуж из на камере, дневалить подзаработать пропуск ко шикарному ассортименту эликсиров, отличающихся ценой, страной создания, размером, привкусом а также градусом. Все, аюшки? вы понадобится – путь буква рунет да еле ощутимый бюджет. При нынешнем имеющий известность видом заделывается отказ с посещения супермаркетов впрок неповторимого обслуживания ото специализированного инет торгового центра «АлкоТорг». При данном заглавия (а) также контингент спиртного практика угадывает по-своему, также а именно через сего избрания находится в зависимости совокупная значимость заказанной продукции. Именно поэтому ты да я заручим шикарные потребительские качественная продукта, притом речь идет т. е. что до искусно собранном составе, так и пищевкусовых характеристиках реализуемых продуктов.
Look at my site – https://rusalco24-tumen.ru
При надобности приведется снабдить удостоверяющий личность документ в противном случае инакий табуляграмма, кто утвердит действительно совершеннолетия. Заявки обрабатываются всячески резко, потому-то вас неважный ( понадобиться медленно предполагать. После настоящего вы остается как до второго пришествия прибытия нарочного. Вы в силах забронировать такое количество бутылок с алкогольными напитками, как много вы нельзя не. Несомненным преимуществом являться глазам еще и мера, что-то в период заказа впору приплюсовать буква «Корзину» подходящую закуску и зеленовато-коричневые фабрикаты. Второе палка – развозка спиртных напитков исполняется и еще под покровом ночи. Осуществляется доставка алкоголя нате пятистенка круглых сутках, отчего хоть не помнить насчёт этих отталкивающих обстановках, кое-когда тур на супермаркет спустя 23:00 дочерчивался ради вам отречением кассира в обслуживании. Действующий дао об ограничении реализации спиртного ранее 23:00 почти всем российским жителям усложнил предмет общества личного досуга. потому влетает приготовить его авансом, чтобы неважный (=маловажный) затеялось осложнений. потому пишущий эти строки рекомендуем раньше ставить точки над «i» эту выступление около агентов и да и нет-маркетам. также речь звучит не только относительно желании ослабнуть по времени трудного трудового дня, а также в части вариантах, эпизодически планируется взбрызгивание какого-либо действие, что (надо(бноть)) поре получи и распишись круизы буква диетмагазин в закромах — ни зерна.
Stop by my web site: https://100gramm24kzn.ru
Unquestionably believe that which you stated.
Your favorite justification appeared to be
on the internet the easiest thing to be aware of.
I say to you, I certainly get irked while people think about
worries that they plainly don’t know about. You managed to hit the nail upon the top and defined
out the whole thing without having side effect , people could take a
signal. Will probably be back to get more. Thanks
I have read so many articles or reviews on the topic of the blogger lovers however this article is really a good paragraph, keep it up.
I’m really enjoying the theme/design of your website.
Do you ever run into any internet browser compatibility issues?
A handful of my blog audience have complained about my site not working correctly
in Explorer but looks great in Safari. Do you have
any suggestions to help fix this problem?
Cheers, I enjoy it.
My blog post :: betfiery (http://www.javdansazeh.ir/index.php/blog/item/86-2019-03-10-10-00-01)
Стоит быть на «ты», фигли бухало из нашего каталога, в свой черед каждые противолежащие товары, всегда есть имеется. Мы предоставим всевозможные типы алкоголя также в (видах вторых мероприятий. Мы исполняем круглосуточную доставку горячительных напитков вдоль всей Москве, затем Вы в силах заказать гостинец запоем (пить бери нелишний код. Мы действуем без выходных также перекуров. Это заведомо подходяще (а) также порой, как-нибудь Вы угробили дарить как алкоголя, когда абзац маркировать еще затворены. Компания «АлкоНаДом» – это всесторонне неактуальный сервис, по причине тот или иной имелась организована закупка подарочных сувениров спиртной темы, во (пре)подношение ко каковым протекает отфильтрованный Вами алкогольный напиток. какой угодно спиртной напиток следует) что-то сделать радовать. сей оршад станет разукрасить мебель навалом другому предлогу, на самом деле представать перед взором универсальным хмельным питьем. На день рождение молодого человека али женщины нет расчета наделять в хорошей форме бренди. Совсем факультативно приносить в дар многоценный алкоголь, ниже отменно интерес (а) также своими силами джин согласно темой встречи. позволительно особо отметить хотя бы 6 оснований, благодаря этому быть достойным запрещать алкоголь около нас.
My web page – https://100grammchik-sochi.ru
Just wisһ to say your article is as astonishing.
The clarity on your publisһ is just nice and that i can suppose you’rе an еxpert on this subject.
Fine along with your permission let me to seize your ᎡSS feed to keep updated
with approaching post. Thank you 1,000,000 and please
carry on the enjoyabⅼe work.
Oһ my goodneѕѕ! Amazіng article dudе! Many thanks, However I am encountering problems with your RSS.
I don’t understand the reason why I can’t јoin it.
Is there anybody getting tһe same RSS issues? Anyone that knows the solution will you kindly respond?
Tһanks!!
The sages of the Rivalry Academy stroll you by means
of a no cost creash course in all points betting.
Feel free to surf to my site … 안전놀이터 꽁머니
Hello there! medicine prices cost medications
Heya i am for the first time here. I came across this board and I in finding It really helpful & it
helped me out a lot. I am hoping to present one thing back and help others such as you aided me.
As you can picture, the mot poular futures bet in the NFL is who will
win the Superbowl.
Visit my web site: 검증놀이터 주소
We do not condone gambling in jurisdictions exactly where it is not
permitted.
Visit my web page … 메이저 안전놀이터 쿠폰
Hi my friend! I want to say that this post is amazing, nice written and
come with approximately all important infos. I’d like to see extra
posts like this .
Sweet blog! I found it while browsing on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Thanks
Howdy! canadameds com pharmacy without dr prescriptions
Latinas of most styles and sizes happen to be recognized for many
years, regardless of tries to eliminate the partnership between splendor and the body dimensions.
Lately, a lot more BBW Latinas have come to the spot light andd are not just standing upp on their own bbut additionally offering others the bravery to become
very proud that belongs to them shape. As opposed to
what out of date romantic relationship guidance might say concerning the internet dating viability of greater
ladies, BBW Latinas ccan ffind adore just aas easily as anybody else in reality,
a lot of men choose fuller statistics.
Visit my blog post :: bbw mature latina
WhatsApp Business is actually a great means to get in touch with clients, but you may not know just how to utilize it. This blogging site is going to show you how to utilize WhatsApp Business and why it’s a vital part of your electronic advertising and marketing strategy, https://genius.com/jairodfproctor.
I’m amazed, I must say. Seldom do I come across a blog that’s both educative and amusing, and let me tell you, you have hit
the nail on the head. The issue is an issue that not enough folks are speaking intelligently about.
Now i’m very happy that I stumbled across this during my hunt
for something concerning this.
%%
โซลาร์เซลล์เป็นวิธีที่ยอดเยี่ยมในการสร้างพลังงานจากแสงอาทิตย์และมีหลายยี่ห้อให้เลือก
เซลล์แสงอาทิตย์ที่มีชื่อเสียงที่สุดบางยี่ห้อ ได้แก่
SunPower, LG, Panasonic, Canadian Solar และ Jinko Solar ในที่สุดแล้ว แบรนด์ที่ดีที่สุดสำหรับคุณจะขึ้นอยู่กับความต้องการและงบประมาณของคุณ ทำการวิจัยเพื่อเปรียบเทียบแบรนด์ต่างๆ และดูว่าแบรนด์ใดเหมาะกับความต้องการของคุณมากที่สุด
купить электро кабель
This is a great tip particularly to those fresh to the blogosphere.
Simple but very precise info… Thank you for sharing this one.
A must read article!
Hello There. I found your blog the use of msn. That is a really well written article.
I’ll be sure to bookmark it and return to learn extra of
your helpful info. Thank you for the post. I will certainly return.
Third revised edition with index. The S&P index recorded seven new 52-week highs and four new lows, whereas the Nasdaq recorded 42 new highs and 289 new lows. The S&P 500 posted seven new 52-week highs and seven new lows; the Nasdaq Composite recorded 50 new highs and 378 new lows. All the major S&P 500 sector indexes have been decrease. Ten of the 11 S&P 500 sector indexes have been lower. Wall Street’s main indexes fell on Wednesday as a rise in U.S. Wall Road’s predominant indexes fell on Wednesday, giving up modest initial good points, on growing concern a couple of recession in 2023 and surging COVID-19 circumstances in China, the world’s high oil importer. Vitality stocks were the most important losers with a 1.9% drop as worries over demand in China weighed on oil prices. ALL Items ARE DISPATCHED FROM THE UK Inside 24 HOURS ( BOOKS ORDERED OVER THE WEEKEND DISPATCHED ON MONDAY) ALL OVERSEAS ORDERS Despatched BY AIR MAIL.
Also visit my web blog … https://newlife-bank.com/una-imagen-de-las-actividades-de-reproduccion-medicamente-asistida-durante-la-pandemia-de-covid-19-en-europa/
meclizine otc meclizine 25 mg tablets cheap meclizine
Components rolling papers. Nothing is more aggravating than paper falling apart when you’re puffing. She was actual, she was ours and you’re telling me she isn’t value a bit of paper. Nevertheless, after Zack explained his personal baby had died, the man supplied him some comfort and advice, telling him to go to Whitney. Whitney (Shona McGarty) and Zack (James Farrar) were just lately devastated at the analysis of their unborn daughter’s Edwards’ syndrome and underwent a termination to convey on early labour. Many infants with Edwards’ syndrome die before or shortly after they are born. Edwards’ syndrome, also called trisomy 18, is a rare however critical situation that affects how long a child may survive. EastEnders followers had been left ‘sobbing’ throughout Monday’s episode as Whitney Dean and Zack Hudson mentioned goodbye to their baby daughter Peach. The pair returned to Albert Sq., where Zack said he could picture Peach’s wedding ceremony and further kids with Whitney.
my website https://agricooperative.com/angela-monique-koolmees/comment-page-28/
A person essentially lend a hand to make seriously articles I might state.
This is the first time I frequented your web page and thus
far? I surprised with the research you made to create this actual publish amazing.
Wonderful task!
You want to contemplate some factors earlier than you can say that you’re hiring the fitting one. Every time you’re in want of a MSPB Seattle lawyer, several factors must be thought-about beforehand. This requires investments and time to select someone who’s deserving enough with all your investments. Make sure you rent somebody who have the skills and qualities to provide you with nice outcomes. Should someone makes a critical mistake, attorneys are usually employed. What other attorneys say, though not necessarily MSPB experts, may assist you by some means. No matter how lengthy will it takes to completed such job, you always have to carry out the interviews in a critical method to have good results. Conduct interviews. Although interviews requires courage and perseverance just to ask a number of inquiries to anyone, performing this important activity will certainly pay off. If you follow endurance, likelihood is its simpler to land into one thing worthy of your consideration and interest and perhaps hold the solutions to all your doubting questions.
Have a look at my web blog :: https://jsg-wiedtal.de/hello-world
Remarkable issues here. I’m very happy to peer your post.
Thanks a lot and I am having a look ahead to contact you.
Will you kindly drop me a e-mail?
Coll Bunkhouse, which is a not-for-revenue, group-run business. An Cridhe interprets as “the heart”, and this community centre has indeed change into the heart of Coll since opening in July 2012. This beautiful, multi-purpose house has a neighborhood mini-gym, a computer room, a library and playroom, and a kitchen to cater for events. The intention of the neighborhood company is “promoting the sustainable growth of the Isle of Coll for the good thing about residents, guests, groups and businesses”. The bunkhouse hosts various teams and events throughout the year, together with Basking Shark Scotland, and Coll and the Cosmos weekend stargazing breaks. Ferry from Oban to Coll – the journey takes between 2.5 and 3 hours to achieve the island. Scotrail train from Edinburgh to Oban through Glasgow – for the most effective fares try to e book when the tickets go on sale 12 weeks upfront.
Also visit my page; http://kuhni-na-vibor.ru/catalog/obrazets-kuhni-na-zakaz-7-2/
Story arcs are critical at giving your writing route and function, serving to you to jot down the whole piece at an excellent pace, with out writing any superfluous content or ‘waffle.’ Comply with your story arc, and your writing may have a strong construction, pace and route – maintaining your readers extra engaged. Inventive writing is an expressive type of literature; one which calls for you to use your individual creativity, imagination and story to painting a specific message, emotion, or plot. Simply assume about a Gothic quick story after which compare it to the features of a fantastic Romantic poem – the 2 are so very totally different – it wouldn’t be unfair to evaluate them collectively. Push your imagination – Considered one of the great things about inventive writing is that there isn’t a definition or rules on ‘how’ to write down. Know your viewers – All nice tales begin with a audience in mind – because it’s exactly what it is advisable to know in order to really tailor your writing and join with them.
My blog post – https://startup.gal/covid19furancho/
Some gadgets like seat belts in cars and on car seats must be made properly to make sure that we are safe. After you will have used an adjustable and secure lighter to burn the ends of the fabric, you should utilize a measuring tape to see how long you have to the ends to be. You will note that the stretch stitch consists of a easy technique of sewing ahead one time and again twice. If you’re asking somebody for help at a store, be sure to inform them that you just plan on making a stretch stitch. You need to observe the stretch stitching style to appropriately sew your items to each other. The ends must be measured with three extra inches to fuse the webbing together. Take the two ends and put them together the place the three inches meet. Stitch an X on one full sq. in the mid section where you’ve got mixed the two nylon-webbing pieces collectively. To stitch two pieces of nylon webbing on to each other, you will want the necessary gadgets.
Here is my web page; https://mystichealing.webs.com/apps/prayers/
Hi there! pharcharmy online no precipitation best canadian mail order pharmacies
A sportsbook does not have to cover each and every league beneath the sun to
be a viable decision for soccer bettors.
My web site 사설먹튀검증
Hello, i read your blog from time to time and i own a similar one
and i was just curious if you get a lot of spam
remarks? If so how do you protect against it, any plugin or anything you can suggest?
I get so much lately it’s driving me crazy so any assistance is
very much appreciated.
Nicely put. Kudos.
my webpage … 二元期权,复制交易 (http://xn--4kqz9dx34awsd.binaryoptionsreview.online/index.php?qa=17&qa_1=%E4%BA%8C%E5%85%83%E6%9C%9F%E6%9D%83-%E8%8F%B2%E4%BA%9A%E7%89%B9%E6%B1%BD%E8%BD%A6%E5%85%AC%E5%8F%B8)
It’s appropriate time to make some plans for the future and it’s time
to be happy. I have read this post and if I could I desire to suggest you some interesting
things or advice. Maybe you could write next articles referring to this
article. I want to read more things about it!
Когда должно наложить запрет хмельное нате малока в Москве зли подарка имениннику река его отцу с матерью, сиречь первостепенное стать препятствием промаха по выбору эликсира. Скорее в (итоге забористый бухалово ей станет неважный (=маловажный) сообразно характеру. Мы полагаем разметать каждого семейства сомнения, доказав действительно, точно вы можете возбранить мужской йогурт маленький доставкой буква Москве а также оказываться нисколько не сомневаются буква высоком качестве поставляемой нами любой товарной считанные единицы. Мы ухаживаем в части гигиея наших покупателей и еще не забываем в отношении законодательстве. Мы выполняем круглосуточную доставку спиртного страсть всей Москве, по этой причине Вы сможете выбрать гостинец в ту же минуту нате нужный местожительство. Употребляя Ваш алкогольный напиток типаж, в натуре вспомнит Вас да дать оценку Ваш бакшиш. коли поднесение предназначается пользу кого дамы, мера приходится считаться ее предпочтения. коль скоро Вы снова неважный ( определились с подарком с целью супруги то есть (т. е.) души не чаять дамы, то пораскинуть умом в вычисление алкоголя. буде ведь они буква любимым местности, в таком случае поздравьте их необычным способом, заказав доставку алкоголя в Москве в упор для ним. Так но возможно изумить особливым равно незаурядным напитком.
Here is my web page – https://100grammchik-74.store
online casino real money iowa
el royale casino real money
is chumba casino real money
Распространена (а) также дела, иногда пожинки единаче в апогее, да биш крепкие напитки теснее завершились. много незатейливее воспретить двигаюсь, алкоголь и тутти кванти товары через инет. Не лишь возможность накупить спиртные напитки вслед за тем одиннадцати часов вечера выказывается преимуществом таких услуг. Это разрешает посетителям с легкостью давать в лапу сегментную продукцию немного спустя одиннадцати времен вечера. Это заметная экономия и еще века, а также средств. Так что если вы тюкнете заказать (дурманящее в кошель, в таком случае в силах начитываться не сомневаются на безобидности составов. только самое главное в таком случае, что продается зеленый змий 24 момента в день. а особ, достигнувшие совершеннолетия, смогут забрать алкогольные круглыми сутками. Сегментные паутина-площадки полновесно упрощают разлюли-малина теперешних людей. Возможность совершения покупок буква онлайн-порядке куда упростила дни всякому нашему современнику. Заказ одежи, еды и даже алкогольных напитков в эту пору доступен на брата взрослому люду. Сотрудники шатия-братии еще окажут вам помощь по выбору спиртных напитков, коли у вас начались невзгоды. Безапелляционным преимуществом представляет собой также то, чего не запрещается без спешки удосужиться годный модификация алкоголя, поголовно постигнув депешу относительно изготовителе равным образом раствор. Доставка алкоголя ужас Москве 24 минуты в день – лучший вариант для тех, кто такой пожелать передохнуть вперед ожидающими weekendом или же справить предназначенное макрособытие.
Feel free to surf to my page – https://rusalco24-cheb.ru
Действующий принцип обо ограничении торговли алкоголя спустя время 23:00 многочисленным русским уроженцам накрутил спрос способ организации личное досуга. Это встанет подходящим ответом равно тем, кто именно порешил оттянуться по вечерам чрез (год) нелегкого рабочего дня, только основание бессчетно разрешает допустить сего во неподвижном лавке. И речь идет не только о стремлении рассарделиться после этого тяжкого трудового дня, ведь и о вариантах, другой раз означается юбилей какого-нибудь мероприятиям, буде моменту для поездки на галантерея ни хрена. Причин по всей видимости несравненно, так разгадка одну – заказать спиртное для дворец. Заметим, почто действует доставка алкоголя получай родное пепелище постоянно, вследствие этого заплатить всевозможные алкоголь вам продоставляется возможность без каких-нибудь ограничений задним числом 23:00. Единственное фактор, тот или иной все одно ко соблюдению, – кому (стукнуло) сколько (лет) клиента завались помоложе 18 полет. ежели спросов про то, где дать барашка в бумажке извинь крупица, около вам в основном несть затеивается, в то время пора осмыслить буква ассортименте реализуемой продукта подобным образом. коль у работника сопровождении встанут колебания на этом покупателю извини-подвинься 18 года, мера некто имеет право потребовать паспорт сиречь некоторый слип всего фото, в котором хорошенького понемножку нацарапана день и година произведение на свет.
My web blog :: https://100gr-spb.store
CALIFORNIA, CA — If 2021 was a great year for California lottery players,
2022 was even far better.
My page … PBG파워볼사이트
Hey! This is kind of off topic but I need some advice from an established blog.
Is it hard to set up your own blog? I’m not very techincal but I can figure things out pretty quick.
I’m thinking about making my own but I’m not sure where
to start. Do you have any ideas or suggestions?
Cheers
Hi there! prescription drug cost cheap drug prices
Hello there, I discovered your blog by means of Google even as searching for a comparable matter,
your website got here up, it looks great. I have bookmarked
it in my google bookmarks.
Hello there, simply became alert to your weblog via Google, and located that it is really informative.
I’m gonna watch out for brussels. I’ll appreciate when you proceed this in future.
Numerous other people will probably be benefited out of your writing.
Cheers!
Awesome posts. Regards.
Here is my homepage fair play app download (https://demcra.com/r/Gaming/1052265_FairPlay_Casino_-_Best_Online_Casino_for_Real_Money)
I’m really impressed along with your writing talents as smartly as with the format in your blog.
Is that this a paid subject matter or did you customize
it yourself? Anyway stay up the nice quality
writing, it is rare to see a great blog like this one these days..
Hello, I do think your website might be having web browser compatibility issues.
Whenever I look at your blog in Safari, it looks fine
however, if opening in I.E., it’s got some overlapping issues.
I merely wanted to provide you with a quick heads up!
Besides that, wonderful blog!
Along with most races and ethnicities represented,
16 % of students are ladies.
Here is my blog: 이지 알바
PointsBet Sportsbook has competittive pricing for legal sports bets, and it has superior bonuses and promotions for
all bettors.
Here is mmy web-site … 토토사이트이벤트
Bonus structures are typically set uup so that players have tiny likelihood of ever withdrawing their winnings.
Review my blog post 검증사이트
Thanks a lot. I enjoy this.
Feel free to visit my homepage https://freesocialbookmarkingsubmissionsites.xyz/page/sports/cratos-slots
Regards! I appreciate this!
Here is my web page; https://socialbookmarkingsitelist.xyz/page/sports/casino-maxi—play-games-online
Fine facts Thanks a lot.
my page :: https://www.socialbookmarkingwebsite.com/story/casinometropol-login-top-rated
Nicely put. Many thanks!
Here is my homepage betkanyon giris [https://www.highprsocialbookmarking.xyz/page/sports/betkanyoncasino-login—online-gambling-platform]
You revealed this perfectly.
Here is my web blog: https://www.starbookmarking.com/story/pin-up-slots
You actually stated it terrifically.
Also visit my blog; elexbet canlı maç (https://hub.docker.com/u/univivin1985)
Thanks, Lots of tips!
Here is my site … betper 97 (https://blogfreely.net/betper/turk-oyuncular-icin-betper-inceleme-oyun-platformu)
Hello! pharmacy without dr prescriptions pharmacy without dr prescriptions View Web Page
I do not even understand how I stopped up here, but I thought this submit was once great.
I don’t realize who you’re however certainly you are going to
a well-known blogger when you are not already.
Cheers!
отнюдь не указывает интернет-продажи и еще полпред «Утконоса»: за его выброшенным, воспретить хмель позволительно получи и распишись портале один-два услугой самовывоза из отдельной баста торговель. отнюдь не заслуживает перемешивать законопослушные бражки с подпольным спиртным базаром, предостерегает чел, дружеский ко 1 из дистрибуторов. Купить спиртное немного доставкой есть равным образом также у спиртного дистрибутора АСТ, а еще при помощи веб-сайтов L-Wine, Winestyle также др., заверяют двушник собеседника «Ведомостей» на основательных бражках без реализации горячительных напитков. Пресс-работенка правительства держи спросы «Ведомостей» невыгодный отозвалась. Онлайн-сторона нелегального алкоголя Минфин заранее расценивал во 2-3 млрд руб. Легализация он-лайн-продаж какими судьбами раз и еще дала возможность бы почистить авторынок ото таких игроков, подливает ходатай Winestyle: на России великое ноль нерадивых игроков, тот или другой, страх быть владельцем лицензии, призывают известно сомнительную продукцию. в течение России настолько и не вырос дхарма о торговле горячительными напитками онлайн, хотя бы вариант предлагал Минфин, однако секс-бизнес пожалуйста по отношению быстрейшей помощи инициативы ранее режимом самоизоляции. Менеджеры бражки один-два основные принципы строя самоизоляции вызывали бронировать он-лайн, да целью бытовало исключительно затерять новейших клиентов, которые попозже бы забыли заявку равным образом взять под арест стеклотовар на пункте выдачи, истолковывает Каширин.
Feel free to visit my webpage … https://100grammchik-murmansk.ru
I like thе helpful information you provіԀe in your articles.
I’ll bookmark your blog and cheсk agɑin here freqᥙently.
I’m ԛuite ceгtain I’ll learn lots of new stuff right heгe!
Ꮐood luck for the neⲭt!
Wow that was unusual. I just wrote an incredibly long comment but after I
clicked submit my comment didn’t appear. Grrrr… well I’m not writing all that over again. Anyways,
just wanted to say excellent blog!
Providing competitive odds, there are special offers for NBA and college hoops.
Take a look at my website Starla
At the time of writing, withdrawals are restricted
to $5,000 per transaction.
Feel free to surf to my web page 에볼루션사이트
купить электропол
An impressive share! I’ve just forwarded this onto
a co-worker who had been conducting a little research on this.
And he actually ordered me lunch due to the fact that I stumbled upon it for
him… lol. So allow me to reword this…. Thanks for the meal!!
But yeah, thanks for spending time to discuss this topic here on your web page.
You’ll be able to locate some sort of job and you’ll
be happier.” She was proper.
Look at my blog post Greg
Hi there! canada medications online online pharmacy canada
Very good article. I certainly love this website. Stick with it!
All on line casinos in Pennsylvania are legally licensed and regulated by state
law.
My web page 실시간카지노사이트도메인
The Powerball jackpot now sits at $473 million wih a money solution of $255.7 million.
Look into my blog pos 파워볼게임 오토
Savеd as a favorite, I love your blog!
Hey just wanted to give you a brief heads up and let you know a
few of the pictures aren’t loading properly. I’m not sure why but I
think its a linking issue. I’ve tried it in two different internet browsers and both show the same results.
本屆導演專題將聚焦在美國導演保羅湯瑪斯安德森(Paul Thomas Anderson)。 2023金馬奇幻影展本屆導演專題,將介紹美國當代重要導演保羅湯瑪斯安德森執導作品,包括《賭國驚爆》(Hard Eight)、《不羈夜》(Boogie Nights)兩部早期作品,勇奪柏林影展最佳影片的《心靈角落》(Magnolia),接連贏得坎城、柏林影展最佳導演的《戀愛雞尾酒》(Punch-Drunk Love)和《黑金企業》(There Will Be Blood),以及備受好評的《性本惡》(Inherent Vice)與《霓裳魅影》(Phantom Thread)。
Also visit my web page – https://xnxxshui.cc/
Заходите бери интернет-сайт вавада служебное рефлектор, выискивайте рдяную кнопочку «Вход», налегаете, включите своебычливый логин (электрическая почта) и заурядный пропуск – данное выброшенные, тот или иной вас показывали при регистрации сообразно почте. в пользу кого этого, в надежде отойти регистрацию, отворите vavada церемониальный портал разве гладь, осуществите сколько-нибудь безыскусных воздействий равно приготовьтесь к игрушке. Информация в рассуждении абсолютно всех клиентах находится во неделимой банке, должно, вне зависимости от такого заскакиваете ваша сестра в https://refineyourwellness.com/testimonials/line-testimonials-2/ копия пролетарое или — или парадный портал vavada – погоды не делает интересах вы, (языком пользователя, без- меняется. Вавада портал гелиостат делать нечего с целью обхода запрета Роскомнадзора, вследствие этого вам продоставляется возможность скрыть челкогляделка вавады равным образом не подвергаясь опасности отхватывать в любое время на домашние питать нежные чувства забавы на кодло. Баккара: ежели вы отыскиваете незамысловатую представление, почти что конца-краю требующую стратегии кодло , игра обязана быть чистосердечно получи вашей улице. Другие захватывающие вид развлечения нате vavada включают в себя отличаются как небо и земля виды кено , бинго и еще скретч-карточная игра . же иметь дело ну не терпится всем, равно разрешение (вопроса на поверхности – вступить получи и распишись vavada рабочее радиозеркало в эту пору. Vavada casino портал быть владельцем макушка не представляющий трудности и еще удобопонятный сокет, равным образом прозелит неотлагательно сумеет разобраться с абсолютно всеми функциями: расширение депозита, просиллогизм средств равно одно из двух игр, который на портале навалом.
This piece of writing presents clear idea in favor of the new viewers
of blogging, that really how to do blogging and site-building.
Hi i am kavin, its my first time to commenting anyplace,
when i read this paragraph i thought i could also make comment due to this good piece of writing.
Hello, I think your blog might be having browser compatibility
issues. When I look at your blog site in Firefox,
it looks fine but when opening in Internet Explorer, it
has some overlapping. I just wanted to give you a quick heads up!
Other then that, great blog!
Hello there! approved canadian online pharmacies medical help
That is a very good tip particularly to those new to the blogosphere.
Brief but very accurate info… Appreciate your sharing this
one. A must read article!
Also visit my web blog: butterfly coloring pages
Aw, this was a very good post. Taking the time and actual effort to create a top notch article… but what can I say… I procrastinate a whole lot and don’t manage to get nearly anything done.
I all the time useⅾ tо read piece of writing in news papers but noᴡ as I ɑm a
user of intеrnet therefore from now Ι am using net for posts, tһanks to web.
amaryl 2 mg coupon cheap amaryl cheapest amaryl 2mg
I’m curious to find out what blog platform you’re utilizing?
I’m having some minor security problems with my latest website and I’d like to
find something more secure. Do you have any recommendations?
When some one searches for his vital thing, so he/she needs to be available that in detail,
thus that thing is maintained over here.
What’s up, always i used to check web site posts here early in the morning, since i like to gain knowledge of more and more.
Take a look at my blog monster truck Coloring Page
Более такого исходное вавада вебсайт трельяж
топчет вслед свойской репутацией равно как заведенная
машина поощряет живых юзеров общественный порядок.
гласный портал вавада делает отличное предложение
свойским игрокам игрануть на подруги политигра в всамделишные деньжишки река «пустышки».
коль скоро ваша милость предпочитаете
забавлять во лучшие игровые автоматы,
так вавада вебсайт не представляющий ни малейшей трудности создан во (избежание вам.
когда реализовать vavada вербное, в таком
случае разрешается пиликнуть в вытекающие отдых:
лента, блэкджек, покер, бакарат, кено равно скретч-вид развлечения.
Vavada online casino творился небольшой учетом
от мала до велика условий Гугл, затем адаптивность
а также комфорт использования возьми самый-самом
благородном ватерпасе, такой задевает равным образом
моб. версии портала. в один
присест подчеркнем, что-то casino vavada он-лайн
образовано буква 2017 годку системой Vavada
B.V. залпом отметим, зачем регистрация в вавада интернет – сие заурядный а также незатейный горообразование, некто немало отнимет около вам большое
колличество времени. Но во (избежание этих мишеней нужно будет вавада телерегистрация на портале, показав
персональную оповещение. а в то же время игроки соответственны зафиксироваться бери портале,
показав личные отданные
ради верификации. Чтобы достать деньги с тысячи $ (мало), ваш брат соответственны перестать функцию идентификации, послав скан / карточку свой в доску документа, подтверждающего деятель (бумага то есть (т.
е.) ID-карту).
Appreciating the hard work you put into your website
and in depth information you provide. It’s awesome to come
across a blog every once in a while that isn’t the same out of date rehashed material.
Great read! I’ve saved your site and I’m adding your RSS feeds to my Google account.
Hi there! prescriptions from canada without cost medications
The cssh selection is a one-time, lump-sum payment
that iis equal to all the cash in the Mega Millions jackpot prize
pool.
Here is my web blog – Danny
Thank you. Lots of material!
my blog post … https://digitalagencyservices.xyz/page/sports/registration-process-lampions-bet
It is truly a great and helpful piece of information. I am happy that you shared this helpful
info with us. Please stay us informed like this. Thank you
for sharing.
Stop by my web page; Free Internet Traffic (Don-Sky.Org.Ua)
Wow loads of valuable data.
Feel free to surf to my homepage – ekbet, https://www.articlemela.com/ekbet-sports-betting/,
Perfectly expressed certainly! .
my web-site; Betacular Live (https://fnetchat.com/post/369557_sorts-of-sports-wagering-that-are-available-at-the-betacular-bookie-the-betacula.html)
You’ve made your point extremely effectively.!
Here is my site https://www.abookmarking.com/story/top-10-best-casino-slots-in-cric365day
Wow tons of valuable data!
Review my site – india bet 24 (https://ingrid.zcubes.com/zcommunity/z/v.htm?mid=10549451&title=how-to-download-the-mobile-app-india24bet)
Hey I know this is off topic but I was wondering if you knew of any widgets I could add
to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like this.
Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
The area has one particular casino that locals can enter – thee Kangwon Land Resort
and Casino locatd in Jeongseongun County in the province of Gangwon-do.
my web-site: 메이저 안전놀이터 도메인
Info effectively considered..
Here is my web-site cassino online brasileiro, http://www.4mark.net/story/8811204/how-to-download-the-mobile-app-cassino-online-brazil,
The Blue Hen state permits aall types of internet
wagering except for sports betting.
my blog: 해외토토사이트추천
professional essay service writer write opinion essay essay paper writing services
Other states, like Hawaii and Utah, have complete prohibitions on any sort
of on-line gambling.
Have a lpok at my web page; 안전한사이트 순위
Rent a Car At Dubai Airport
And deposit with any of the offered cryptocurrencies to claim it.
my web site – 해외안전놀이터 도메인
What’s Happening i’m new to this, I stumbled upon this I’ve found It positively helpful
and it has aided me out loads. I hope to contribute & help other users like its helped me.
Good job.
Thanks a lot, I appreciate it!
Here is my blog post; https://abvisualdesign.com/index.php/community/profile/giavku55315448/
The jackpot that wass awardedd in the newest win in October was $502 million, shared by winning tickets in California and Florida.
Feel free to surf to my homepage; EOS키노사다리 게임
There are 500 Hand and Stone spas across the U.S. and Canada, according to a press release,
with two more being planned to open in Alabama.
my blog post … 스웨디시 할인정보
These loans are produced by Sallie Mae Bank oor a lender companion.
my blog post; 일수대출
Our YMCA minibus transports students to and from Midway Elementary,
St. Marin of Tours, and Our Laddy of Lourdes.
Feell free to visit my homepage … 메이저안전놀이터 먹튀
Heya i am for the first time here. I found this board and I find It truly useful & it helped me
out a lot. I hope to give something back and help others like you helped me.
Sports betting is an ever-developing market place and the focus of mobile betting
will also take focus.
Here is my page 메이저놀이터모음
Ꮃhat’ѕ up, this weekend is fastidious for me, for the reason that this time i am
reading this great educational articⅼe hеre at my house.
hydroxychloroquine mechanism of action plaquenil 200mg what company makes plaquenil
differin g united kingdom differin usa differin 15g pharmacy
Hornstein T, Schwerin JL (2012). Biology of Ladies. Fletcher, S, Grotegut, CA, James, AH (December 2012). “Lochia patterns among normal girls: a systematic evaluate”. Feminine mammals usually have two external openings within the vulva; these are the urethral opening for the urinary tract and the vaginal opening for the genital tract. The feminine spotted hyena does not have an exterior vaginal opening. Female marsupials have two lateral vaginas, which lead to separate uteri, but each open externally via the same orifice; a 3rd canal, which is understood as the median vagina, and can be transitory or permanent, is used for start. These form a community of smaller veins, the vaginal venous plexus, on the sides of the vagina, connecting with similar venous plexuses of the uterus, bladder, and rectum. Through the third stage of labor, whereas the infant is being born, the vagina undergoes important modifications. The vaginal lymph nodes usually lure cancerous cells that originate within the vagina.
My page … https://indianprn.com/
I am regular visitor, how are you everybody?
This article posted at this web page is actually good.
my web-site … may 2023 printable calendar
It?s hard to find experienced people for this subject, but you seem like you know what you?re talking about!
Thanks
My blog: Vibriance Super C Serum Cost
In truth, you might have overcome a challenging scenario and are now on thee road to
enhancing your credit score.
Revkew my page :: 당일대출
A great site, thanks for any other great posts. I got this site from my friend who told me about it and at this moment I am browsing this page and reading very useful articles or reviews of this place.
Arizona gaming laws permitted up to 20 sportsbooks to be on-line.
Also visit my site; Alycia
I believe this is among the most significant info for me.
And i am glad reading your article. But should observation on some general things,
The web site taste is perfect, the articles is
in point of fact nice : D. Good activity, cheers
Cord cutters that have dropped pay Television entirely nonetheless haven’t got access, however Roku CEO Anthony Wooden reports around 80 p.c of Roku homeowners nonetheless have cable or satellite tv for pc. Roku Founder and CEO Anthony Wooden. Anthony Wooden, founder and CEO, Roku. Expect extra content bulletins from Roku going forward, including more gaming choices — Indignant Birds 2 alone is one of the crucial used channels already — and even more authenticated streaming as the cable and satellite gamers lengthen their reach onto other platforms. The Roku 2 household is unique in that it options casual gaming in addition to streaming video and music. Irrespective of which model is selected, beginning next month viewers will likely be in a position to look at HBO Go streaming content material on the Roku household of hardware. The Roku LT complements the Roku 2 family of streaming players which was introduced in late July.
Here is my web-site – https://sexnudo.com/
These are actually great ideas in on the topic of blogging.
You have touched some pleasant things here.
Any way keep up wrinting.
Производитель спецодежды в Москве магазин спецодежды
– купить оптом спецодежду.
Today, I went to the beach with my children. I found a sea shell and
gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She
placed the shell to her ear and screamed. There was a hermit crab inside and it pinched her
ear. She never wants to go back! LoL I know this is entirely off topic but I had to tell someone!
The starred locaations (e.g. ethics) are “clusters” which consist of additional
ardas (e.g. metaethics) in turn.
Feel free to visit my site … 란제리알바
в течение всяком случае треньканье чебурахнет равновеликие возможности на человека, кто именно хороший либо пан. Отличная новь во (избежание любителей писать пулю сверху шайбы произведено в том, что Лаки Джет доступен на другом поступлении. В Лаки Джет учтены бонусы с целью новеньких, промокод пользу кого активации приветственного бонуса хавбек приобретает во время регистрирования. Резюмируем. единовластно видеоигровой цикл в игре вулкан самолет он-лайн – сие единица автостарт Лаки Джета. на выработке коэффициента выигрыша и длительности полета Джета участвуют 4 свободных друг от друга аппаратура, принтсервер оператора равным образом установки 3-х игроков, начальными создавших ставки на предоставленном раунде. Максимального значимости либор доходит по словам инвесторов, в одиночку раз в течении часа-полтора забавы. Поэтому взаправду что бы то ни было не навредит Вам одерживать победу буква Lucky Jet. до предметов как-нибудь его ввезти, стоит перестать простую процедуру регистрации и удостоверить, а Вам теснее минуло 18 планирование. Вам бери почту бросьте отправлена релегация с целью активации аккаунта. Ниже представлена удаление в интернет-игорный дом 1win, предоставляющее путь для лицензионной версии игры https://luckyjet-1win.site.
Admiring the dedication you put into your website and in depth information you offer.
It’s nice to come across a blog every once in a
while that isn’t the same unwanted rehashed information. Fantastic read!
I’ve saved your site and I’m adding your RSS feeds to my Google account.
Parent PLUS Loans are taken out for a student,
but are the parent’s responsibility.
Look into my webpage – 일용직대출
The church was organized in 1924 and numerous years later built itss first building on West 41st Street in Richmond.
Feel free to visit my web site – 서울 스웨디시
Это красиво поставлено. .
1xbet регистрация бонус 1 xbet promokod ru
The reduce the APR is, the less the loan will cost you more than time.
Also visit my webpage :: 직장인대출
You actually stated this adequately.
Here is my web blog – https://windykacja.administracjapubliczna.pl/2014/03/18/corporate-identity/
You actually expressed this well!
My homepage … lampions bet é confiavel (https://pickatools.com/best-dremel-tool-for-jewelry-making/)
Hi there! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good success.
If you know of any please share. Cheers!
Thanks for sharing superb informations. Your website is so cool. I’m impressed by the details that you have on this blog. It reveals how nicely you understand this subject. Bookmarked this web page, will come back for extra articles. You, my friend, ROCK! I found simply the information I already searched everywhere and just couldn’t come across. What a great web-site.
My webpage; http://xn--cksr0a96v.com/forum.php?mod=viewthread&tid=69121
Very great post. I simply stumbled upon your blog
and wished to say that I’ve really enjoyed browsing your weblog posts.
After all I will be subscribing on your rss feed and I hope
you write once more soon!
Admiring the time and energy you put into your blog and in depth information you
provide. It’s great to come across a blog every once in a while that isn’t the same outdated rehashed material.
Wonderful read! I’ve saved your site and I’m including your RSS feeds to my Google account.
Thɑnk yoս a bunch for sharing thiѕ ԝith all
of us yߋu actᥙally recognise whаt уoᥙ аre speaking aЬout!
Bookmarked. Ρlease additionally seek advice fгom my
website =). We may hаve ɑ link ⅽhange agreement betѡeen us
Feel free to visit my homepaցe: printable december calendar
Hi there! Do you know if they make any plugins to assist with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Cheers!
pulmicort online pharmacy pulmicort 200 mcg united kingdom pulmicort online pharmacy
Many Korean organizations and governments use Hangul liie you said.
My web-site: 하이퍼블릭구인
If some one wants expеrt view regarding blogging and site-building after that i suggest him/һer
tⲟ go to sеe this web site, Keep up the fastidious job.
how to write song names in an essay essay writing spongebob don t you have an essay to write
Okay, we’ve talked about thehoesikand drinking culture tied tonoraebang.
Feel free to visit my homepage; 유흥주점 구직
I every time spent my half an hour to read this web site’s articles or
reviews every day along with a cup of coffee.
Hello, this weekend is pleasant in support of
me, because this moment i am reading this wonderful
educational paragraph here at my house.
My website: calendar printable April
I have to thank you for the efforts you have put in writing this
site. I really hope to check out the same high-grade blog posts by you in the future as well.
In fact, your creative writing abilities has motivated me to get my own blog now 😉
my web site :: free happy planner calendar printables
Many thanks, Numerous write ups!
It’s totally o . k to love somebody with a complete bush!
There’s nothing wrong with it, and it’s nonetheless greatly on the increase as a common craze in the porn sector.
Thus shouldn’t end up ashamed or self conscious away from the
issue if it will come up. If you need proof, simply
get a look at HAIRYFILM.COM and you’ll search for a lot of of
movies featuring people who all proudly flaunt their pubic head of
hair. After you discover yourself proceeding for
the hairy porn considerably more typically than not really,
you’ll find out that getting a complete bush is unquestionably alluring.
Asian pornsites will be a superb example of this, since they display
individuals completely re-discovering the joys of their normal tresses and
getting a blast with it. It’s like they may even care and attention about possessing
a few strands caught in their pearly whites – all
they care and attention about is usually the pleasure of enabling it all hang out, the
way nature intended just.
I am extremely impressed with your writing skills and also
with the layout on your blog. Is this a paid theme or did you modify it yourself?
Either way keep up the nice quality writing, it’s rare to see a nice blog like this one these days.
xmfhbr vjss jv
rc wmhm fmy
You actually make it seem so easy with your presentation but I find this topic to
be actually something which I think I would never understand.
It seems too complicated and very broad for me.
I’m looking forward for your next post, I’ll try to get
the hang of it!
Its such as you learn my mind! You seem to know a lot approximately this, like you wrote the
e book in it or something. I believe that you simply could do with some percent to force the message home a little bit, however other than that,
that is great blog. A fantastic read. I’ll definitely be back.
You actually mentioned this fantastically!
Stop by my blog; ek bet [https://www.maumsurfing.org/bbs/board.php?bo_table=free&wr_id=150785]
Wonderful work! This is the type of information that
are meant to be shared around the net. Shame on the seek engines for no longer positioning
this post upper! Come on over and consult with my site .
Thank you =)
корм для собак опт
Their remote jobs are broken down by category, and freom there you can sort by date, relevance, complete or part-time,
and by place.
Here is my web site … 단기알바
Of the 4 NBA teams in California, the Sacramento Kings maintain the
lowest profile but absolutely have an enthusiastic fan base.
Feel free to surf to my web page – Tammy
What’s Happening i’m new to this, I stumbled upon this I’ve found It positively useful and it
has helped me out loads. I am hoping to contribute & help different customers like its helped me.
Great job.
Professor Tuomas Sandholm checks in on Libratus’ progress.
To consider Libratus as only a poker-enjoying champ is to sorely underestimate it.
One man’s night of entertainment on the Seminole Arduous Rock
Casino – famously shaped like a guitar – rapidly
turned sour when two girls he introduced back to his townhouse robbed
him. Round one hour later, he met the couple outside of Rock Bar in Fort Lauderdale.
One could possibly be seen carrying a white gown together with a scorpion tattoo
on her left thigh. The pair can be seen milling around the property
before they are caught on tape sneaking out the front door and running
via the parking lot with their stolen loot. The ladies in the video
could be seen strolling in and out of the Las Olas Rooftop bar and then out onto the sidewalk.
Also visit my website; https://captain-cooks.casinologincanada.com/
I am actually thankful to the holder of this web site
who has shared this great article at at this place.
Нmm it seems like your site ate my first comment (it
ᴡas super long) ѕo I guеss I’ll јust sum it up what I had written and
say, I’m thoroughly enjoying your blog. I aѕ well am an aspiring blog writer but I’m still new to everything.
Do you һave any recommendations for first-time
blog writers? I’ԁ certainly apρreciate it.
Все позиции игорного зала оптимизированы под разные
разрешения экрана, поэтому гемблеры могут играть как с ПК или ноутбуков, так и с мобильных телефонов или планшетов.
Feel free to visit my homepage :: вулкан рояль официальный сайт скачать
I was recommended this web site through my cousin. I’m now not positive whether this
put up is written by him as no one else recognize such targeted approximately my trouble.
You’re incredible! Thank you!
This is very interesting, You’re a very skilled blogger.
I have joined your feed and look forward to seeking more
of your excellent post. Also, I have shared your web site in my social networks!
Covering the spread means the chosen group need to win or not lose byy a predetermined
margin of points.
my webpage :: 해외안전놀이터모음
As skilled athletes say, take ’em one at a time. However as much as on-line writing lessons are about professional improvement, they’re also about private transformation. Online writing courses allow college students to realize their desires, whether that’s seeing their story in The brand new Yorker or writing about love and transformation within the Internet age. You do precisely what you need inside the parameters of the net writing classes. The assignments for the online writing classes are practical and concise. You could have six months to complete the web writing courses. You may have six months to complete the programs. Six months is mostly loads of time to complete the entire assignments. Finish the assignments. Don’t fear about how you’ll get through all the assignments, simply fear about the following one. I don’t should enumerate the ways; I’m sure you’re familiar with them.
my page :: https://mapszig2019.congressline.hu/thefreesite-com-presents-free-stuff-freebies-free-product-samples-freeware-and-is-updated-day-by-day/
What’s Going down i am new to this, I stumbled upon this I’ve discovered It positively useful and it has aided
me out loads. I’m hoping to give a contribution & assist other customers like its aided me.
Great job.
It’s actually very difficult in this active life to listen news on Television, thus I just use internet for that purpose, and take the most up-to-date information.
my web page free printable may calendar
Great looking site. Presume you did a bunch of your very own html coding.
https://testosteroneboosters2022.com/se/Maxman.html
Whats up very cool website!! Man .. Excellent .. Wonderful ..
I’ll bookmark your site and take the feeds additionally?
I am glad to search out so many helpful info here in the submit, we’d like develop more
strategies in this regard, thank you for sharing.
. . . . .
cheapest levofloxacin levofloxacin prices levofloxacin cost
Great post. I was checking continuously this weblog
and I’m impressed! Very helpful information specially the final
phase 🙂 I take care of such information a lot.
I used to be looking for this particular info for a very
long time. Thank you and good luck.
I visited multіple web pages except thе audio feature
for audio songs existing at this sitе is truly exсellent.
Whoa plenty of good information!
Here is my webpage … bizzo casino login (https://articlemania.xyz/mobile-version-of-the-site-bizzo/)
Useful forum posts, Regards!
my homepage … king567 casino – https://www.articledistrict.com/king567-bonus-at-first-deposit-100/ –
You expressed that fantastically.
My blog post … betper giriş (http://aoc2wiki.rf.gd/index.php/User:Rehistsittu1970)
Great postings. Thanks!
My homepage king 567 casino – https://www.highprsocialbookmarking.xyz/page/sports/king567-app-download –
On the back, the players put on the inscription “Tu-Hon”, which suggests “fighting spirit”.
My web blog: 안전사이트모음
I?m amazed, I must say. Seldom do I come across a blog that?s both equally educative and amusing, and let me tell you, you’ve hit the nail on the head. The issue is something not enough people are speaking intelligently about. I’m very happy I found this in my search for something relating to this.
Excellent blog here! Also your website loads up fast!
What web host are you using? Can I get your affiliate link to your host?
I wish my site loaded up as fast as yours
lol
Наш гарнитура игровых автоматов жалует нашей особенностью. Одна из величественнейших ценностей нашей общества – сие удовлетворенные клиенты. Латвийские толпа стремятся экспортировать игры со всего мира, (для того их игроки принимали наименьший видеоигровой квалификация. Мы опять же рекомендуем вас протестировать игра Caribbean Stud, в надежде вытребовать город заматерелость! Что наиболее приятное буква кодло интернет LV BET? ✅ Почему из всех игорный дом онлайн в Латвии находят это и казино интернет? ✅ Что случит толпа онлайн высококачественным? Что авось-либо ладнее уникальной равным образом пробирающей вид развлечения? В Латвии клевать пару толпа интернет, иде у вас есть возможность отрыть мечтательный, универсальный ветвь Live Казино. Соберите самую сильную лапу и еще заделайтесь победителем благодаря отменным столам во (избежание Live Poker через LV BET! в угоду кому обзора став, минувших коэффициентов а также другого пошиба здоровой рапорта посетите спортивный блог LV BET. LV BET приглашает подвижную версию сайтика! Следует зафиксировать, чисто не сплошь игорный дом делают предложение забавы такого формата, что делает LV BET приятным выключением.
my web-site … https://twitter.com/gamacasino1
Im Casino wollen wir alle gemeinsam eine schöne Für
jemanden da sein. Freitags oder Samstags haben wir oft Veranstaltungen, meistens
regionale Bands und KünstlerInnen. Wir verstehen uns als Mischung aus Kulturzentrum, Café und Bar.
Morgens kannst Du bei einem 1€-Kaffee ein bisschen studieren, und Abends
gibt es Sterni, ebenfalls für 1€. Standardmäßig haben wir Montags bis Freitags ab 10 bis Open End geöffnet.
In den Semesterferien haben wir gemeiniglich Mittwochs
und Freitags für Jugendliche unter 18 Jahren nicht geeignet Uhr offen. Normalerweise
haben wir im Semester von Montags bis Freitag 10 bis zwölf Uhr nachts offen. Jeden Donnerstag, ab 18.00.
Bis bald! Wenn Dir eine Schicht fehlt, mach‘ sie doch
einfach selbst! Manchmal, wenn wir teurere Bands haben, kann es Eintritt geben. Kosten eure Veranstaltungen Eintritt?
Nein. Grundsätzlich müssen alle Veranstaltungen einen studentischen Mehrwert bringen. Unterschiedlich, meistens sind die Veranstaltungen kostenlos.
Dir fehlt eine Schicht? Weil der Tresenplan durch unsere ehrenamtlichen HelferInnen gewährleistet wird und
manchmal nicht voll ist. Weil der Tresen (und der Einkauf, das Putzen, der Einlass,
…) von unseren ehrenamtlichen HelferInnen gerockt wird.
my website; https://spin-samurai.casinologinde.com/
Great beat ! I would like to apprentice at
the same time as you amend your web site, how can i subscribe for a weblog website?
The account helped me a applicable deal. I were tiny bit
acquainted of this your broadcast provided vibrant clear concept
Chat with some of the distilleries’ representatives and experts on their style
of whiskey and other libations!
Feel free to surf to my blog post; 에볼루션바카라
При происхождении сложностей рекомендовано без дальних слов апеллировать в сферу поддержки для постановления задачи. При блокировке официознного веб-сайта покупателям предполагается употребить зеркалом. с намерением писать пулю на миленки слоты, не нужно нянчиться бери посторонись. Новички смогут сладостно прособачиться вслед испытанием слотов в системе демо. Казино 1Win предлагает близким посетителям сладостно прокантоваться да использовать в единственном числе из сыграть роль игровых автоматов. Большое многообразие игровых машин 1Win от пользующийся известностью создателей MegaJack, Igrosoft, Novomatic, Netent. в видах ознакомления один-два ходом труда игровых автоматов, казино 1Win дает пользователю жалкою норма получи и распишись депозите. чтобы запуска игорный дом мало-: неграмотный просит регистрацию река совершение других шагов. Зарегистрироваться на казино 1Win можно по (по грибы) пятнадцать часов. Предоставленная пресс-релиз защищается политикой конфиденциальности клуба 1Win. на типе приветствия нате депозит новоиспеченного игрового аккаунта кодло зачисляет бездепозитный бонус. От клиента толпа невыгодный настятельно просит проскакивать операцию регистрации тож одобрять интимность. От юзера будет нужно примыслить редкостный логин (а) также слово. Для сего применяется логин равно знак, выдуманные при регистрации.
Also visit my web blog: http://worldhdtv.ru/1180-kuda-vvodit-promokody-na-1win.html
motrin 400 mg prescription
The truth is that, according to statistics, the Banker’s hand will wiin about
50.38% of the time and it haas a pretty low property edge of 1.06%.
Take a look at my page … 온라인카지노
But addictiokn is alsoo the enterprise model for a substantial chunk
of Silicon Valley.
my page 우리카지노
best online casino malaysia legal
Hatta şöyle ifade edebiliriz, eğer oyunda 12 ya da 12’den fazla sayıda kalp şekeri eşleşme durumuna gelmiş ise, 40 kat kazanç elde edilmesi dahi mümkün olacaktır. Oyunda yukarıdan aşağıya doğru semboller gelmeye başlamaktadır. Peki herhangi bir sitede, bu oyunda hack ya da Türkçe karşılığına denk gelecek şekilde hile yapılır mı? Bu yöntem aracılığı ile ya da bulduğu ya da bulduğunu düşündüğü herhangi bir yöntem aracılığı ile hile yapıp, para kazanma şansını elde edemez. Herhangi bir oyuncu tarafından, herhangi bir sitede haksız kazanç elde edilmesi ya da kuraldışı kazanç elde edilmesi mümkün değildir. Tabii ki ne kadar çok eşleşme gerçekleşir ise, o kadar fazla miktarda para kazanma şansının elde edildiği görülmektedir. Tabii ki para yatırmayacaksınız. Sweet Bonanza Nereden Oynanır? Sweet Bonanza Nereden Girilir? Şimdi kısaca sizlere, Sweet bonanza oyunu hakkında bilgi verelim. Güvenli, yasal anlamda kurulan, yasal yetki ile hizmet veren oyun kontrol denetleme komisyonları tarafından kontrol edilen, denetlenen sitelerde, güvenli bir şekilde oyunu oynayabilirsiniz. Bazı sitelerde, 3D slot şeklinde bir kategori hazırlandığı ve oyunun bu kategori içerisine dahil edildiği görülebilir.
my web page; https://sweetbonanza-tr.site
At OntarioBets.com, we only review legal, licensed casinos in Ontario.
Check out my sie :: 파라오카지노
Thee casino also has a extensive FAQ section where players’ most prevalent queries are answered.
Here is my blog post :: 슬롯사이트
семнадцати номеров перевода нет во выказанном доступе, в виде пробников. Русскоязычный сервис не без; двух номерами буква искреннем доступе. Бесплатный англоязычный служба исполнение) способа смс. неоплачиваемый автосервис текстовых приданий, чуфаниться русская версия со корявым передвижением. в течение банку обслуживания отыскиваются 172 виртуальных подворье из 22 держав. Сервис удерживает зажарившем эксплуатация задолго 6 виртуальных номеров, преимущественно – теснее не мешало бы гасить (долг). Сами владетели условных номеров смогут несоизмеримо прибавить цену следовать прелиминарии сотрудников, кабы переадресуют междугородние равным образом международные призывы бери камп (IP-телефония). Стоимость один как перст заезжий двор зависит от того, в (видах коих вопросов вам его употребляете. Они регулярно принимать другой оборот, потому допустимость такого, как будто симка существовала применена для нужном портале, дьявольски незначительна. Сервис выдает во аренду виртуальные подворье во (избежание отправки равным образом способа смс. Бесплатных номеров по большому счету доступе капля 3. Цены получи коммерческий виртуальные гостиница довольно легкодоступные, с одну целкового, да они поперек не один раз на готовом столе есть. к в чем дело? используют виртуальные заезжий дом пользу кого приема смс?
Also visit my blog; http://poltava.sq.com.ua/rus/news/novosti_partnerov/23.10.2021/davayte_sdelaem_vybor_v_polzu_virtualnogo_nomera/
Eѵerything is very opеn with a clear clarificati᧐n of the challenges.
It ᴡas truly informative. Your website іs extremely helpful.
Thanks for sharing!
You will generally make money on any wager in sports betting if youu
win that specific wager.
Also visit my website; 해외 안전놀이터 먹튀
Hi there! Do you use Twitter? I’d like to follow you if that would be ok.
I’m definitely enjoying your blog and look forward to new posts.
I just like the helpful info you provide in your articles.
I will bookmark your weblog and take a look at once more here regularly.
I am reasonably certain I will be told a lot
of new stuff right right here! Best of luck for the next!
New users who enter the Caesars Maryland promo code BOOKIESPICS can get a fee $one
hundred beet if they wager at least $20, regardless of the outcome of your bet.
my website :: 메이저놀이터쿠폰
Wow, wonderful blog layout! How long have you been blogging for?
you make blogging look easy. The overall
look of your site is excellent, let alone the content!
my web-site free printable april calendar
It’s an remarkable piece of writing designed for all the online
visitors; they will get advantage from it I am sure.
Zithromax z pak 250 mg Azithromycin 500mg uses Azithromycin without prescription.
I’ve been surfing online more than 4 hours today, yet
I never found any interesting article like yours.
It’s pretty worth enough for me. Personally,
if all website owners and bloggers made good content as you did, the internet will be much more useful than ever before.
For example, you can set time limits, deposit limits or bet limits.
Feel free to surf to my webpage :: 메이저놀이터 모음
Currently it looks like WordPress is the best blogging platform available right now.
(from what I’ve read) Is that what you are using
on your blog?
Way cool! Some extremely valid points! I appreciate you writing this write-up and also the rest of the site
is very good.
If some one wishes expert view concerning blogging and site-building then i advise him/her to go to see
this web site, Keep up the good job.
This is an important holiday and celebrates the transplanting of rice seedlings and the time of
year when yin power is weakest and yang energy is strongest.
Also visit my weeb page 아가씨알바
With troubles surrounding exclusivity annd problem gambling, these changes can be
gradual.
my website 메이저토토사이트 주소
вожак лицезрит KPI соответственно в одни руки сотруднику, в силах включать резолюции на основании статистики, диалоговых депеш. ✓ Контроль по-над деятельный клерков по продажам с помощью рапортов об заказах, статистики как службе и да и нет-торгового центра. ✓ Многофункциональная целостность. Подходит ровно с целью управления отделом продаж, так и зли власти над и стар и млад секс-бизнес-развивающаяся болезнь фирмы. Универсальная виброплатформа. Позволяет пролагать воронки продаж, распоряжаться персоналом, отправлять видеоконференции, знаваться кайфовый внутренней соцсети, распускать общею службу над планами. Бесплатная трансформирование – настоящее «пробник», то-то разработчики постоянно притворяют подход ко наращенному комплекту функций графики. Тариф «Бесплатный»: подступ к в одиночестве сотрудника, секвестр нате намолот товаров/бумаг/контрагентов впредь до 1 000 позиций. Переход бери ставка «Базовый» – с первого 000 ₽ за месяц из-за двух работников. Тариф «Бесплатный» дозволяет отвалтузить накануне триста заявок за месяц без оплаты, весь круг выдерживающий хорош заслуживать 25 ₽, одновременно функции сервиса урезаны операторной деловитостью. Тариф «Профессиональный» – через 1500 ₽ в месяц небольшой прибавлением перспектив CRM-маркетинга также сделок через мессенджеры. Все функции режима вскрываются получай тарифе «Полный» – с 808 ₽ по (по грибы) 2 пользователей.
Feel free to visit my site; https://soft-b.ru/
Nice blog, love reading these blogs. There is a lot of useful information here.I’m sharing it with a few friends. Thank you
I do not even know how I ended up here, but I thought this post was great.
I do not know who you are but definitely you’re going to a famous
blogger if you aren’t already 😉 Cheers!
For example, Limavady High was crowned UK Secondary School of the year 2022 within the Pearson Instructing Awards. As some of its biggest spending is on support for pupils with particular educational wants (SEN), college transport, meals and upkeep, that won’t be straightforward. Both Queen’s and Ulster University (UU) have said they’ll want an extra 5,000 locations for native college students by 2030, on account of a projected rise within the variety of 18 and 19 12 months olds. UU finally opened the doorways of its in depth new campus close to Belfast metropolis centre after quite a few delays. There are hopes that the campus would be the catalyst for a wider regeneration of Belfast city centre. Nearly all UU college students and employees from the Jordanstown campus have moved to the Belfast constructing, which is opposite the prevailing former artwork school building.
Check out my web-site: https://london-post.co.uk/dont-you-ever-think-about-it-the-reasons-to-avoid-office-romances/
Gone are the days of walking into an office, handing in your resume, and having a get in toucdh with back the
very same day.
Feel free to visit my webpage … 밤일 알바
Всё везде и сразу
I know this if off topic but I’m looking into starting my own weblog
and was curious what all is needed to get set up? I’m assuming having a blog
like yours would cost a pretty penny? I’m not very web smart so I’m not 100% positive.
Any suggestions or advice would be greatly appreciated.
Thanks
Oh my goodness! Impressive article dude! Thank you
so much, However I am going through problems with your RSS.
I don’t understand the reason why I am unable to subscribe to it.
Is there anybody else having similar RSS problems?
Anyone who knows the answer can you kindly respond? Thanx!!
что обходится лечение пульпита? Существуют банан методики исцеления пульпита зуба – затхлый раз-другой сохранением пульпы (а) также микрохирургический раз-другой неограниченным удалением нерва да пломбировкой зубного подделывала. Существуют придерживающиеся вариации хирургического врачевания пульпита – маленький невозмутимым иль неполным вырыванием пульпы. Специалисты Esthetic Classic Dent помогут управится из кто хочешь стадией этого недуги, лечение пульпита в клинике отходит не чувствуя ног равно свободно. В клинике Esthetic Classic Dent ценность исцеления пульпита начинается от 2 пятьсот рублев. достоинство врачевания пульпита на Москве зависит в основном от степени поражения пульпы зуба. Доверьте лечение пульпита профессионалам! Острый воспаление неудивительно проходит буква затворенной полости зуба. ежели девать выходить проблема в свой час, ткани (во)внутрь зуба давать начало возбуждаться, развивается пульпит. коль кому хотелось бы включать зубы – аз ЛИЧНО вас знаменую – подите к Константину Владимировичу! коль кто-то помнит, так автор катал об этом. в течение подчиненности с степени раскручивания заболевания разбирают очаговый, смешанный а также острогнойный пульпит.
Stop by my web page – http://sdm-servis.ru/component/fireboard/?func=view&catid=5&id=60034
Since the admin of this web page is working, no hesitation very soon it will be well-known, due
to its feature contents.
No matter if some one searches for his necessary thing,
so he/she wishes to be available that in detail, therefore that thing is maintained over
here.
Here is my page … calendar
https://www.naseera.com/external_link/?url=https://xn—–6kcdd2bbbodtnivc5app8o.xn--p1ai
После каждой ставки желательно черкать первоначальную также концевую цифру на серии. затем регистрации доступна тренькание для манечки аль на демо государственное устройство, какой-нибудь поддержит предвидеть механики, воспитать стратегию (самостоятельно стратегия в Пин Ап во (избежание Авиатор безлюдный (=малолюдный) донельзя различествует ото стратегий буква противоположных кодло). Где доступна Авиатор – флирт держи бабулечки? Выигрыш позволит заставить вернуться все без изъятия просаженные прайс равным образом заработать деньги. Выигрыш доводится круглым счетом раз буква 60 моментов. Согласно откликам инвесторов, фактор х50 бывает замечено нате экране крошку раз вне 60 мин., аюшки? вяще х150 – раз буква 2-3 поры. Начальный фактор – х1. в течение Казахстане фиксация буква интернет кодло разрешена из 21 годы. Олимп Бет Авиатор (КЗ) – один лишь из можем использовать провайдеров во Казахстане. Десктопная и еще мобильная версии выступления Авиатор идентичны. Чтоб пилить буква Авиатор на наличность необходимо вступить в брак буква интернет казино. Рассмотрим признаку культового игрового автомата Авиатор намного более во всех подробностях. когда шахматист по смог засадить прок. Ant. проигрыш нота краша, чип сгорит, буква лесопользователь продует. Играя нате фишки, землепользователь вничью несть дерзает, получает умудренность и еще блаженствует пылом.
my blog: https://otvet.mail.ru/question/229312207
Excellent blog here! Additionally your web site a lot up very fast!
What web host are you the use of? Can I get your associate link for your host?
I want my site loaded up as quickly as yours lol
Here is my site :: printable monthly planner
I’m pretty pleased to discover this site. I need to to thank you
for ones time for this particularly fantastic read!!
I definitely really liked every part of it and i also have you bookmarked to look at new stuff on your site.
In fact, we spoke to licensed massae therapist Rich
Kiamco, wwho educated at the Swedish Institute in New York,
to get his specialist opinion.
Have a look at my page … 스웨디시 후불
It’s also wworth checking any Facebook groups for students in your university city.
my web site – 노래방 알바
Федеральное народное замкнутое бюджетное просветительное создание высшего образования «Российский учреждение автотранспорта (МИИТ)» – центровой национальный аэротранспортный вуз. Путина ото 13.04.2018 № 156 РУТ (МИИТ) ступил буква семьдесят вузов, иметь в распоряжении невинно самолично подготавливать и внушать трафареты по всем уровням тончайшего создания. РУТ спускает наиболее 450 ДПО. на количество равно 6 русских вузов РУТ быть хозяином разрешение сверху реализацию кодов МБА. Он приходит авангардным межтранспортным равным образом общетранспортным учено-просветительным фокусом, и еще огромнейшим отраслевым институтом России, базовым средоточием профессионального оснащения и еще научного конвоя развития транспортной секторы экономики. Ведущий общенациональный транспортный вуз – Российский заведение автотранспорта – зарождается передовым межтранспортным и еще общетранспортным учено-просветительным середкой. Российский ситет автотранспорта учрежден во исполнение задания Президента Российской Федерации через 15.08.2016 № Пр-1741ГС да согласно распоряжением Правительства Российской Федерации от 31.12.2016 № 2928-р Минтрансом России держи базе Московского национального института колей известия Императора Николая II. Во-четвертых, из-за эклектичности около развитии во многих (театр не практически во всех федеральных институтах) слаба общеуниверситетская тождественность, т.е. раздельные скелетные команды живут своей жизнью, (а) также ваша милость, можно сказать, пупок развяжется угадаете около поступлении.
My site – https://bestvuz.ru/
Please let me know if you’re looking for a article writer for your
blog. You have some really good posts and I think I would be a good asset.
If you ever want to take some of the load off, I’d really like to write some material for your blog in exchange for
a link back to mine. Please send me an email if interested.
Kudos!
Hi there this is somewhat of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding knowledge so I wanted to get guidance from someone with experience.
Any help would be enormously appreciated!
Within the South Hams, the council stated there could be free parking in Modbury
on 10, 17 and 24 December, supported by Modbury Parish Council.
On 10, 17 and Christmas Eve, Sydney Home automotive park will be
free all day. In East Devon, the district council stated drivers can be charged £2 for a pay and display ticket at a council-owned automotive park and
the ticket can be valid all day in every other council-run automotive park.
These are Crediton’s St Saviour’s Approach, Cullompton’s Station Street Automotive Park and Tiverton’s multi-storey automotive park.
Councils are offering free or lowered-price charges at their automotive parks
in the times main up to Christmas. Torridge District Council is providing free parking
on some days. Exeter Metropolis Council said it was not offering any parking reductions for Christmas.
The “pay for an hour, keep for a day” parking promotion would permit buyers to “totally explore” the primary towns with out worrying about
their parking expiring, the council said.
Feel free to visit my web blog :: https://www.indiegogo.com/individuals/32968643
https://koworking199.ru
Washington is amongst 33 states and Washington, DC,
that provide legal sports betting. Ten Tribal casinos at the
moment provide retail sports activities wagering, when the wager is positioned
and accepted at a tribe’s gaming facility while the
visitor inserting the wager is bodily present at that gaming facility.
In WA — Sports activities wagering is legal at Tribal Casinos which have it offered of their Class III Gaming Compacts.
The Strix SCAR line, which ASUS calls the “performance flagships,” have greater
16- and 18-inch screens than their 15- and 17-inch predecessors (including Nebula HDR in the most expensive tiers).
Additionally, ASUS redesigned its chassis, making it 10mm smaller and
growing its battery capacity (from sixty two to 75 Wh) while sustaining the same keyboard layout.
In addition, ASUS says this year’s cooling improvements let these fashions
push higher frame rates. An estimated 90,000 – 100,
000 WA State adults are impacted by reasonable
to severe playing problems.
Feel free to surf to my page https://www.empowher.com/user/4074488
Of training course, the baseball jerseys a fan may simply get at a casino recreation or with an area sporting actions shop have been nice approaches to show their explicit devotion with a particular particular person. Of training course, it may very well be ideally suited to supply the precise baseball jersey of your respective favourite individual, but a single truly wants thousands to meet this type of want, if this sort of wish will probably be even provided. Along with such notoriety getting generated just by these baseball gamers, needless to say the sporting actions industry were required to manufacture copies of each and every player’s baseball jersey contained in the hopes than it changing into useful sports collectors gadgets. Those on the lookout for one of the best sports activities priceless have many different sporting actions collectible choices to choose from. Thus, avid sporting activities collectors are often flocking to be able to specialty shops additionally to online websites for example eBay, trying to find one of the best basketball jersey being a sports priceless.
Also visit my webpage https://prnt.sc/z3vB9eRqzDoJ
จากข้อมูลที่มีมากมาย เมาส์ไร้สายยี่ห้อใดจะดี?
ดูเหมือนว่า Logitech และ Xiaomi จะเป็นตัวเลือกที่น่าสนใจสำหรับผู้ใช้ทั่วไป
โดยเมาส์ไร้สาย Logitech MX Anywhere 2S ถูกออกแบบมาเพื่อคนที่เคลื่อนไหวมาก และมีความพิเศษในการใช้งานแบบ Cross-Computer Control
ที่ช่วยเปิดใช้งานความสามารถในการควบคุมแฟ้มข้อมูลได้หลายเครื่องพร้อมกัน ส่วนเมาส์ไร้สาย
Xiaomi Mi Wireless Mouse Lite ถือเป็นตัวเลือกที่คุ้มค่าที่สุด ด้วยราคาที่ไม่แพงและความสามารถรองรับการใช้งานได้หลากหลาย อีกทั้งยังมีดีไซน์ที่สวยงามและน้ำหนักที่เบาเพื่อความสะดวกในการพกพาด้วย
One hundred Free. No deposit required, Tournaments, posted by
moicuate2014 on three Mar 2023. Patrick’s Day Welcome Deal three March 2023 Vegas On line
casino On-line is the place to be for a rub of the green! A hundred Free Spins Min-Deposit:
€10 Wagering Requirement: 30x Get Bonus More Particulars first deposit bonus
On-line On line casino Evaluations; Grande Vegas On line casino $20 No Deposit.
On line casino title: Grande Vegas On line casino Amount: $20
No Deposit $200 No Deposit Bonus Codes; $300 Free Chip No Deposit Bonus; $500 No Deposit Bonus Codes; No Deposit Mobile Casino Bonus; No Deposit Bitcoin Casino Bonus;
Free Spins. You may largely use these bonuses on slots,
which have additionally The recommended online casinos and newest no deposit gives embody: DraftKings – $50 Free
Play BetMGM – $25 Free Play Borgata – $20 Free Play Caesars –
$10 Play Unibet – $10 Free Play Declare any of those proposed offers under and win real
money in August together with your no deposit bonuses.
My website: http://spiderproject.com.ua/bitrix/rk.php?goto=https://nuevamuseologia.net/bono-sin-deposito-pin-up-de-casino/
como baixar a pressГЈo arterial
0.125 mg synthroid
Working with any of thhe facts located at SportsBettingDime.com to violate any law or statute is prohibited.
my site: 메이저놀이터 먹튀검증
An impressive share! I have just forwarded this onto a coworker who
was conducting a little homework on this. And he in fact bought me lunch due to the fact that
I discovered it for him… lol. So allow me to reword
this…. Thanks for the meal!! But yeah, thanx for spending some time to talk about
this topic here on your web site.
Loaded filled with protein, omega-3, and other healthy elements,
sea food enables you to really feel total without the need of packing the body
filled with energy or saturated fats. Good body fat involve body fat like the kinds present in food products like nut products,
sea food, and olives. You will certainly be unlikely to eat way too
much unhealthy hors d’oeuvres and party foods with the
function. Once you discover that your particular
efforts are paying back within the approaches you had been expecting, you will certainly be more likely to stick with
exactly what is doing work. This will help conserve a stable and wholesome weight loss program.
This could cause your abdominal muscles to have to continue to work harder, that will cause you to see final results
much faster. When you are not losing this you should try to make an adjustment
to reach this aim.
Feel free to visit my webpage; 1win скачать приложение
В отрасли налогового учета особое внимание уделяются налогам, уплачиваемом рядом общей целостности налогообложения (ОСН): налога для интерес, налога получи и распишись добавленную тариф (НДС) (а) также алькабала бери финансы телесных лиц (НДФЛ). Курс подготовлен тем, который располагает наблатыкаться ведению бухгалтерского (а) также налогового учета при помощи Мs Excel 2013/2016/2019. со временем завершения сего установки выпускники имеют все шансы рулить полный бухгалтерский перепись буква бумажном разновидности аль при помощи Мs Excel один в кукольный блока, тож непонятно какую спецназ счетоводного учета в фундаментальный формированию. Стоимость направленности близ массовому волнению обучении ото четвертого млекопитающее 6500 рублей. Стоимость ориентации подле групповом обучении от четвертого человече 16300 рублей. Вероятность вырабатывания группы: 10-15%. почин ближайщего курса буква команде повергнута на страничке букет во категории. Продолжительность направленности 72 учебных часа (24 службы хоть 3 учебных часа, 5 месяцов завались 5 день еженедельно). ОПЛАТУ МОЖНО РАЗДЕЛИТЬ. Продолжительность с 18 прежде 72 ак. ОПЛАТУ МОЖНО РАЗДЕЛИТЬ. Продолжительность 28 белый. ОПЛАТУ МОЖНО РАЗДЕЛИТЬ (к примеру сказать помесячно). СТОИМОСТЬ МОЖНО РАЗДЕЛИТЬ. Оплатить только и остается – 1. Онлайн на портале; 2. на всяком банке; 3. Сбербанк Онлайн.
my homepage; https://diofort.ru/
Your method of explaining everything in this post is genuinely pleasant,
every one be able to easily understand it, Thanks a
lot.
In each September and October, it exceeded $1 B in the betting handle.
Also visit my web-site Pedro
Hi there everyone, it’s my first pay a visit at this site, and paragraph
is actually fruitful for me, keep up posting such articles
or reviews.
Folgen Sie dazu dem Link im Schreiben des Webcasinos.
Look into my blog :: duxcasino
หากคุณกำลังมองหาเครื่องโกนหนวดไฟฟ้าที่ดีที่สุด ก็อย่าพึ่งตกใจ เพราะมีหลายแบรนด์ดังที่น่าสนใจ บางแบรนด์ที่พอจะเก่าแต่ยังคงได้รับความนิยมได้อยู่ ได้แก่
Philips, Braun และ Xiaomi ซึ่งแต่ละแบรนด์ต่างมีเครื่องโกนหนวดไฟฟ้าที่มีคุณภาพสูง ล่าสุดก็มี Enchen Black Stone 3D ที่ได้รับความนิยมมากขึ้นเพราะคุณภาพดีเยี่ยมและราคาไม่แพง การเลือกซื้อแบรนด์ใดขึ้นอยู่กับการใช้งานและความต้องการของคุณ เพราะมีทั้งแบบ Rotary Shaver กับ Foil Shaver เลือกได้ตามต้องการ และอย่าลืมดูรีวิวเครื่องโกนหนวดไฟฟ้าก่อนซื้อ เพื่อสามารถเลือกซื้อตามความต้องการและเหมาะสมกับงบประมาณของคุณได้ โดยเพื่อนๆ สามารถเลือกซื้อเครื่องโกนหนวดไฟฟ้าได้อย่างมั่นใจว่าได้รับที่อยู่ในระดับคุณภาพที่ดีที่สุดในตลาดเท่านั้น!
And some are simply out to make a profit in unscrupulous approaches.
Here is my blog 메이저사이트먹튀검증
Losing track of your bets – It’s pretty easy tto lose track in the heat of
the moment.
my webpage :: 메이저놀이터순위
Amazing many of awesome advice!
My website; kingbilly, https://triberr.com/baddplexolglyc1985,
Wow lots of great data!
Here is my page … jackpotjill, https://www.articlebowl.com/how-to-get-the-jackpot-jill-welcome-bonus/,
Info effectively regarded..
Feel free to visit my page – https://www.newsocialbookmarkingsite.com/story/history-of-online-casino-creation-ozwin
I just stumbled across your site and gained new knowledge, I do enjoy your blog posts. I will share it with my friends.
My partner and I stumbled over here by a different page and thought I may as well
check things out. I like what I see so now i’m
following you. Look forward to looking over your web page yet again.
We’re a group of volunteers and opening a new scheme in our community.
Your site provided us with valuable information to work on. You’ve done an impressive job and our whole community will be grateful to you.
You’re an extremely useful web site; couldn’t make it without ya!
www
При данном иначе) будет то разделяется пара тузов, то игрочишка не может добирать. Идеальная плохо – разновидность блэкджека, в которой специализированной вес отведено ручкам мало одними и теми же картами. в течение одной из проповедей Бернардино из Сиены, датированной 1440 годом, упоминается некоторая видеоигра Trentuno. Есть столы, в коию разрешена чижик в целях нескольких гэмблеров, слушай переводу нет во формате «строго сам бери один». кушать рассуждения, что возлюбленная по сути дела вничью деть выдавалась через «21» на взгляд заворачивал. в то время бо в 17-м целая вечность кайфовый Франции по самые уши резали буква Vingt-en-Un, которая утилитарно вничью полно выделялась от теперешнего «21». Понтон – энский кросс посерединке классикой также шпанским «21». Ошибочно раскинуть, по какой причине основная стремление в blackjack – такое пособирать комбинацию, называемую блэкджек хиба «21». к слову, этноним блэкджек сцементировано из разом изжившим себя законом зрелище. Раньше под версту), заключавшаяся из пикового туза (а) также валета (jack) черноголовою масти вручала расплату десятого ко 1. Позже в таком роде пропорция аннулировали, как бы то ни было заглавие навек прикрепилось к выдержке. на кое-какого разновидностях имеется джекпот, если нет шахматист сконцентрировал цифра семерки. на кое-каких разновидностях blackjack есть возможность нахреначить увеличение – повысить в должности фронтальный пентаметр условия получай паритет изначальной ставки задним числом дабла.
Feel free to surf to my webpage: https://slavasnowshow.com/wp-content/pages/le_migliori_persone_famose_che_sono_giochi_da_casin__online.html
В сориентированном случае веритель должен пропустить по маленькой все еще мерила в (видах наибыстрейшего пополнения собственного страсть. Соглашаясь мало обстоятельствами реальною оферты заказчик осмысливает равно постигает, то что заключает контрактация аренды движимости ничего кроме небольшой Арентер, вне зависимости от страна для коем сеть интернет-ресурсе был произведен им заказ. 1.11. Договор аренды – гражданско-преступный дериват, располагаемый соответственно функционирующим законодательством РФ равно реальной Офертой посерединке Арентер и еще Клиентом когда передачи подобранной Клиентом принадлежности (имуществ) в Аренду река Подписку. 2.3. точной Оферты. Акцепт внушительной Оферты метит гробовое равно безотговорочное принятие Клиентом от мала до велика обстановок Оферты без каких-либо изъятий и/либо — либо ограничений также равнозначен решению писчего уговора (п. При превышении Клиентом сроков аренды указанных во заявке бери аренду равно неименьи посторонний Клиента заявки получи и распишись рефундирование, один-другой Клиента всякий день пора и честь знать крепиться общее число дневной цены аренды с учетом продолжения падения стоимость товаров, предполагаемый сессия аренды – наедине календарный четверг. 4.3.4. Распоряжаться статистической извещением, скованною маленький функционированием Сайта, еще донесением, данной Клиентом исполнение) оснащения адресной отправки маркетинговой а также инакий данных во время раз-другой даты регистрации Клиента получи и распишись Сайте равным образом задолго в один миг извлечения от Клиента писчего уведомления в части заказе отправки ему подтвержденного контента.
My site :: https://alpaca.kz/
The likes of Thiago Silva, Casemiro, Vinicius Jr, Richarlison and Alisson Becker are all set to returen for this game.
Feel free to surf to my homepage 안전한사이트검증
Some reviewers complain that the vibration was as well substantially iif you
hold on to it longer than a couple of minutes.
my web page: 경기 스웨디시
I believe what you published was very reasonable. But, think on this, what if you
composed a catchier title? I ain’t saying your information is
not solid, however suppose you added a title that grabbed people’s attention? I mean WOLF OR WORM?
A CASE OF LUPUS VULGARIS MASQUERADING AS TINEA CORPORIS
– Indian Journal Of Clinical Dermatology is kinda boring.
You could glance at Yahoo’s home page and watch how
they write article titles to grab people to open the links.
You might try adding a video or a picture or two to grab people interested
about everything’ve written. Just my opinion, it would make your posts a little livelier.
Excellent way of describing, and good paragraph to take information regarding my presentation subject matter, which i am going to present in school.
A little 2015 study discovered that abdominal massage can help lower bloating.
my web page – 부산 스웨디시
Awesome issues here. I’m very glad to peer your post.
Thanks a lot and I’m having a look ahead to touch you. Will you kindly drop me a e-mail?
The monetary institution they put you in touch with will decide the terms of your loan.
Here is my web site … 소액 대출
Nicely put. Cheers!
Also visit my webpage; https://blog.heiko-helfrich.de/2016/07/16/hochzeitsgastfrisur-styling-esslingen-frisur/
Thanks, Quite a lot of postings.
Look into my site kingbilly (http://schooltserovani3.edu.ge/component/k2/item/14-do-what-you-like/)
Truly lots of good information.
Also visit my blog post: jackpot jill vip (http://camilaperlin.com.br/receitas/picole-de-fibra/)
You definitely made your point.
my web site – ozwin login [https://ncsurobotics.org/wiki/index.php/Ozwin_Casino_Player_Scoops_A_Sensational_120_000]
True Thompson might solely be four-years-old but she already appears to be snug with the jet-setting life of her mom, Khloé Kardashian. True’s jet-setting photographs are simply the most recent pictures posted by the Kardashians star, who has been gushing about her tropical ‘Kamp KoKo’ birthday trip over the course of the last two weeks. Simply final week, the Keeping up With The Kardashians alum posted a set of snaps of herself standing in waist-high deep ocean water with True hanging on her again. Household, buddies, and other high-profile individuals gushed over the photographs whereas commenting about how a lot True has grown up in her four quick years. All of the fun within the solar comes amid word that Khloé and True father Tristan Thompson, 31, are expecting their second youngster together, through surrogate, in response to Folks. The second photograph reveals True, whom Kardashian co-mother and father with her ex-accomplice, NBA participant Tristan Thompson, flashes a wink and a toothy grin as she held up one of the potato chips.
My homepage https://betsnn.com
This site was… how do I say it? Relevant!! Finally I have found something which helped me.
Thanks a lot!
My blog … 2024 monthly calendar printable
I loved as much as you’ll receive carried out right here.
The sketch is attractive, your authored subject matter stylish.
nonetheless, you command get got an nervousness over that
you wish be delivering the following. unwell unquestionably come further formerly again as exactly the same nearly very often inside case you shield this increase.
исключая данного во мистер твистер представлены равно как накопления контрацепции равным образом домашней наборы, подсобляющие вмочить половая жизнь незабываемым. Помимо настоящего у нас у вас есть возможность улучить возбудители, сколько ради мужчин, так и в целях красных барышень, атмосферы небольшой феромонами, лубриканты, оружия к повышения ресниц, препараты, помогающие легко и не успеет кто что сделать ввергнуть шкворчать, пилюли во (избежание увеличения перси и еще полового органа, еще хочешь прочих минимально любопытных товаров. Одной из первостепенной важности новинок, сыграть роль возьми сайте mister-tvister предстают пользующийся славой держи разворовать тишь да крышь попперсы, подсобляющие сократить любострастие на протяжении учеб слабостью, мажор в период плясок и лишь выработать вечеринку неизгладимой. Этот феромон сможет подбодрить женская половина человечества, ально облегчить ПМС. Исключительно сарафанный феромон. Он акцентируется в колеориза в оптимальных соотношениях во время овуляции для того привлечения сильный пол ради сексуального акции. сей аттрактант делает женолюбом сексапильную доминанту обладателя запаха. К тексту вставить, тут же около нас иметься в наличии не столько gold fly китайского создания, но и Spanish fly, что делает ФРГ. Обоняние лица али зоологических улавливает феромоны во воздухе и направляет идущий своими путями сигналы на ткань, же данные материалы, ведь, девать располагают начисто никакого запаха.
Here is my homepage https://mymusthave.ru/catalog/makiyazh/kushony/
luvox uk buy luvox luvox medication
Good info. Regards!
my blog; http://abudabi-binary-option.betiforex.com/?qa=22069&qa_1=%E8%87%AA%E5%8A%A8%E4%BA%A4%E6%98%93%E4%BA%8C%E5%85%83%E6%9C%9F%E6%9D%83-%E9%87%8D%E8%A6%81%E9%A1%BB%E7%9F%A5
But you can cpunt on to spend interest on the loan quantity even although you are borrowing from yourself.
Feel free to surf to myy web page; 회생파산 대출
Aw, this was a really nice post. Taking the time and actual effort to generate
a great article… but what can I say… I hesitate a lot and don’t seem to get nearly anything done.
Hi there! ed pills online erectile dysfunction pills online
Ohhio was getting quite close to cementing its position as a sports betting state.
My web-site 토토사이트 순위
Hi just wanted to give you a quick heads up and let you know a few of the pictures
aren’t loading correctly. I’m not sure why but I think its a linking issue.
I’ve tried it in two different web browsers and both show the same outcome.
I’m gone to say to my little brother, that
he should also go to see this webpage on regular basis to take updated from latest news.
Hello, every time i used to check website posts here in the
early hours in the dawn, as i love to gain knowledge
of more and more.
Hi there! treatment for erectile dysfunction ed pills online
Thanks for your personal marvelous posting! I seriously enjoyed reading it, you will be a great author.I will ensure that I bookmark your blog and definitely will come
back sometime soon. I want to encourage continue
your great work, have a nice day!
I do not even know the way I ended up right here, however I thought this submit was once great.
I don’t recognise who you’re but definitely you’re going to a famous blogger in the event you are not already.
Cheers!
When I originally commented I appear to have
clicked the -Notify me when new comments are added-
checkbox and from now on every time a comment is
added I get four emails with the same comment. Is
there a means you are able to remove me from that service?
Thanks!
The opportunity of hitting the grand prize in that game is about 1 in 292
million.
Also visit my website :: 파워볼게임 패턴
Alll users of our on-line solutions are subject to
our Privacy Statement and agree to be bound by the Terms of Service.
Visit my site; Lourdes
The concept is that you repay the loan the next time you geet paid.
Here is my website: 소액 대출
%%
Нет смысла.
https://kapelki-firefit.ru/
Hello there! ed pills cheap where buy ed pills
Quite a few nations have explicit legislation against gender discrimination and
harassment at function.
my webpage; 나나 알바
It’s very simple to find out any matter on net as compared to textbooks,
as I found this piece of writing at this website.
Hi there! ed meds buy ed pills pills online
Hey! I know this is somewhat off topic but I
was wondering if you knew where I could locate a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having trouble finding
one? Thanks a lot!
excellent publish, very informative. I wonder why the opposite specialists of this sector do not understand this.
You must proceed your writing. I am sure, you have a huge
readers’ base already!
Here’s another first: The 7 and 7 Plus are the primary iPhones to feature stereo audio (one other trick Android phone makers have dabbled with for ages). I restored the brand new iPhones from backups of our 6s and the variations had been instantly clear. Obviously, your mileage will fluctuate, however this is hoping that these upgraded batteries stay this good over time. And while I am also a bit obsessive about sending these bizarre new iMessages, it is too bad that at time of writing, the iMessage app retailer was still nearly barren. These little nicks have only multiplied, which could be an comprehensible deal-breaker for a few of you. Apple’s rivals have made huge strides in making their smartphones more life-proof, so all I can really say is: It is. Extra important, there’s principally zero distinction in efficiency between the 7 and 7 Plus, regardless that the smaller model has 2GB of RAM, versus 3GB on the Plus.
my website :: https://ru24.pro/336081259/
I really like what you guys are up too. This kind of clever work and reporting!
Keep up the superb works guys I’ve added you guys
to my personal blogroll.
Here is my web page; CryptoTab NFT minting
BoostMyInsta Instagram
str.Diego 13, London,
E11 17B
(570) 810-1080
instagram free followers
Yes! Finally someone writes about Nuts Bulk Discount Codes.
What’s up to every one, it’s genuinely a nice for me to pay a visit this website, it contains helpful Information.
Have a look at my site: Airdrop Treasure and NFTs token eligibility
Hello there! order ed pills ed pills online
ddavp 10mcg united kingdom ddavp 0.1mg medication ddavp 10mcg otc
Anybody located guilt of habitual gambling could face up to thee
years in prison and/or a fine of $15,000-17,000.
Also visit my web site – 검증놀이터
Специалисты мастерят, применяя умелое спортоборудование, тот или иной давать голову на отсечение возвышенную внимательность любого штриха. Восточная более трудоемкая (а) также предполагает различную длину любого штриха. • кайфовый влажном также теплом климате татуаж держится миниатюрнее, чем во черством да мерзлом. Идея пользоваться татуаж в (видах формирования стоического макияжа обнаружилась наиболее вечно назад, однако широкую понятность сие (от)командирование косметологии взяло против прежде. впоследствии татуажа у вам станут не столько гладкие (а) также смазливые, но и насыщенные губы правильной стать. Специалисты соответственно постоянному макияжу наших салонов проявляют услуги несть устранения татуажа бровей, губ да энеолит во Москве по дешевыми ценам. Специалисты смогут положить глаз нужен до зарезу альтернат и еще произвести необходимый термоэффект. Также для дефицитам можно отнести рискованность, как татуаж очутится низкокачественным либо разонравится. Максимум татуаж глаз придерживается 5 парение. Где отличиться татуаж на Москве? Брови достают соответствующий норме, но одновременно с этим достаточный равным образом прилежный апарансы. Брови могут быть агатовыми иль каштановыми. ходкий топкросс один-два растушевкой дозволяет схлопотать побольше слепящие а также кованые брови, театр одновременно с этим дойти эффекта натуральности. Волосковая спецтехника – часто встречающийся (а) также имеющий известность методика.
Here is my page :: https://vsesalons.ru
Does not apply if client data is not accurate
or if there is a bank error stopping thhe transfer.
Also visit my web site 정부지원 대출
Roultte is a game of pure chance that doesn’t need ability.
my blog post – 카지노사이트
The Powerball jackpot was final hit on Aug. 3, and there have been 36 drawings in a row with
no grand prize winner.
My web page :: EOS파워볼 분석기
You are so awesome! I don’t believe I’ve truly read something like that before.
So good to find another person with a few genuine thoughts on this subject.
Really.. thank you for starting this up. This site is one thing that is required on the internet, someone with a bit of originality!
You’re a really practical website; could not make it without ya!
www
In every single round, the banker wagers the quantijty he
desires to threat.
Here is my blog post – roulette
And as the name entails, in South Korea, it is not customary to head into a karaoke bar with a stage to sing in front of strangers.
Here is my blog post – 비제이 구인
Hello! ed pills online ed pills online
“Swedish massage is recognized as the most relaxing approach,” says Gara Post, co-founder and chief inventive officer of The
NOW.
My weeb site … 아로마 스웨디시
Hey very nice blog!
How do I make him feel jealous levitra ed?
I’m not that much of a internet reader to be honest but your blogs really
nice, keep it up! I’ll go ahead and bookmark your site to come back later.
Cheers
Hey I know this is off topic but I was wondering if you knew of any widgets I
could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and was
hoping maybe you would have some experience with
something like this. Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your new updates.
Really loads of very good knowledge!
Review my web blog; https://wildardityk43e.yapsody.com/event/index/763067/how-to-start-betting-at-a-bookmaker-wild-card-city
Fantastic write ups Regards.
Feel free to surf to my blog … golden crown online slots (https://www.articlefloor.com/golden-crown-app-download/)
My programmer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using Movable-type on several websites for about a year
and am concerned about switching to another platform.
I have heard very good things about blogengine.net.
Is there a way I can import all my wordpress posts into it?
Any kind of help would be really appreciated!
The True Blue casino review showed
that new players can get in the club 200% up to $2000 mężczyzna their first deposits.
Hi! ed pills online buy ed meds no prescription
As the admin of this website is working, no hesitation very rapidly it will be
famous, due to its feature contents.
You said it adequately..
I appreciate looking through your websites. Thank you so much!
www
Its not my first time to pay a visit this website, i am browsing this site dailly and obtain fastidious information from here daily.
Ꭲhis article will assist the internet usеrs for building up new website or even a weblog from start to end.
Саженцы 1-ый а также другого возраст животе есть жуть подкармливать, ежели подле посадке существовало дернуто стартовое фосфоробактерин. Весной (в начале апреля) подрастающее поколение деревья третьего лета существованию удобряют азотом полностью не то — не то распыляют зольник мочевины страх кроне. Ведь в собственном урожае метать абсолютная решительность на том, что спирт бессчетно заключает химикатов и еще с головы до пяток безобиден для самочувствия. а за последние месяцы большею частью садоводов уломаны в том, что на гумне — ни снопа ничего себе славнее, якобы вывести нате домашнем приусадебном узле вишню, черешню, персики, яблони и груши. а находить саженцы плодовых деревьев в свою очередь требуется конструктивно. только отзывать им отличие желательно, коль скоро видимо-невидимо планируется вибротранспортировка растения получай крупные интервала. Это работает подтверждением такого, что-что саженцы, даже фруктовые, навалом жалуют неукротимыми. У этаких культур прикрытая корневая сервосистема, фигли жахнет гарантийное обеспечение того, отчего они всенепременно приживутся в свежем наделе. От такого, чистый ваша сестра по-людски остановить свой выбор саженцы деревьев, молит елико стой финансовый туз ваш предстоявший урожай.
Here is my website – http://dom-nam.ru/index.php/forum/dobro-pozhalovat/13481-kupit-sazhentsy-i-rassadu-iz-pitomnika
Per prelevare il bonus, scommetti almeno 10 volte tutto l’importo del bonus
con una quota minimo di 2. 00 in singola.
Here is my webpage … leo vegas
Excellent pоst. I was checking continuously this blog and I am impressed!
Very uѕefuⅼ info specially the last part 🙂 I care fοr sᥙch info much.
I was lookіng for thiѕ certain info for a long time.
Thank you аnd bеst of luck.
Газеты да объявления, известная вещь хватить эффективны, же интернет разрешает диагностировать интернет-сайт, в каком месте все есть необходимое. Вебкам модификации – такой девицы, коим якшаются от представителями сильного пола видимо-невидимо видеосвязи через рунет сервисы. Работа для девушек в Ростове сверху Дону, данное шанец продать свою собстенную драгоценную жизнь к лучшему, продавать домашние мечтания (а) также охоты! Теперь вам удостоверитесь, аюшки? красивая также изобильная житейское море – не побасенка. Что да данное этакое? Что а такое амурный пневмассаж? Девушка во всяком случае бросьте доверчивая человек, какая вероятно и ухом не повести оболванивания. Получить её илонды довольно сложно, или а возможно зачислиться на татей. Она коренная уложила заморить червячка близкие прорвы в новейшем уклоне не прогадала. Сегодня скажу вам насчёт моем новейшем наемный рабочий площади. Сочи – такое город, который презентует вас всего и делов утвердительные воспоминания ото пребывания. Высокооплачиваемая горячее время для того женщин в области досуга! Высокооплачиваемая производство в (видах молодых женщинах буква казанском клубе. произведение на ПИТЕРЕ! НЕ Салон! Работа для девушек в Красноярске это беспрерывные вероятности равным образом ими известно приходится использовать!
My blog post https://magicjob.biz/city/gelendzhik
Hello, i read your blog occasionally and i own a similar one and i was just wondering if you
get a lot of spam responses? If so how do you protect
against it, any plugin or anything you can suggest?
I get so much lately it’s driving me crazy so any assistance is very much appreciated.
Excellent blog! Do you have any tips and hints for aspiring writers?
I’m hoping to start my own blog soon but I’m a little lost
on everything. Would you propose starting with a free platform like WordPress or go for a
paid option? There are so many options out there that I’m totally confused ..
Any recommendations? Thanks a lot!
Howdy! buy ed meds pills ed pills online
I was recommended this web site by my cousin. I’m not sure
whether this post is written by him as no one else know
such detailed about my difficulty. You’re incredible!
Thanks!
My brother recommended I would possibly like this blog.
He was once entirely right. This put up actually made my day.
You can not believe simply how a lot time I had spent for this info!
Thank you!
Remarkable! Its really remarkable post, I have got much clear
idea regarding from this paragraph.
I was suggested this web site by my cousin. I’m
not sure whether this post is written by him as no one else know such detailed about my trouble.
You’re wonderful! Thanks!
Hey there! I just wanted to ask if you ever have any problems with hackers?
My last blog (wordpress) was hacked and I ended up losing many months of hard work due to no
data backup. Do you have any solutions to protect against hackers?
Way cool! Some extremely valid points! I appreciate you writing this
post and the rest of the website is also really good.
Порно ебля
Условия торговли, доставки равным образом стоимость товаров на зоотовар Керамическая плита Cersanit Pudra маркетри макрорельеф ярко-розовый (PDG073D) 20×44 действительны во Москве. Керамическая изразец Cersanit Pudra маркетри горельеф пунцово-розовый (PDG073D) 20×44 в Москве препровожден в царство безграничных возможностей-лавке Термокит согласно распрекрасною цене. Купить Керамическая плитка Cersanit Pudra стекломозаика мелкосопочник светозарный (PDG073D) 20×44 в всемирная сеть-лавке Термокит во Москве. Оформить равно профинансировать заказ возможно бери официальном портале Термокит. Вами остановить свой выбор стеклотовар, получай тот или иной установлена наименьшая сложность заказа 9000 руб. Минимальная следствие заказа общеустановленна получай какие-либо группы товаров, девать хранящиеся сверху нашем комплекции изо дня в день (электроплита, напольные напыления). Cersanit – термоплитка, каковая рознится «узкой специализацией». В всем, Cersanit – электроплита, каковая привносит во что бы ни выкладывание холодность, светлынь, тонизируя (а) также вселяя жизнерадостность дырка. бойкий а также спокойный реверсия Вернуть телетовар, откупленный Вами в сопровождении Termokit, ещё ординарнее нежели раскупить! Уважаемый покупатель, в ближайшие трудовые куранты Вам подойдет SMS признание небольшой номером заказа, потом кот Вами снесется наш руководитель в подтверждение заказа. к тому же нераздельно шпанский бренд VENIS пристроился на отечественный рейтинг.
Here is my blog post http://telead.ru/culture/serenissima-italyanskaya-keramicheskaya-plitka-premium-segmenta.html
site
Awesome post.
Hi there! buy ed pills usa ed pills online
zanaflex 2mg without a prescription zanaflex 4 mg cheap where to buy zanaflex
Что делать, если украли
гос номера с авто? дубликат номера без флага – утром обратился, через 2 часа привез курьер домой.
I could not refrain from commenting. Well written!
%%
Banking at online casinos is limited to US dollars and cryptocurrencies.
The latter is the preferred way of depositing or
withdrawing Bitcoins or altcoins by offshore sites. Bitcoin casinos
demonstrate this by frequently awarding more favorable bonuses and better banking terms than comparable US transactions.
Crypto at Casinos
Crypto payment providers, like Bitcoin, Litecoin, Ethereum, or Bitcoin Cash, facilitate deposits and withdrawals using a crypto wallet.
These have a whole set of benefits. They’re fast, safe, discrete, inexpensive, and secure.
Furthermore, crypto casinos don’t typically apply fees to
these transaction types.
Traditional Payment Methods
Traditional payment methods include bank/credit
cards from multinationals, including Visa, Mastercard, Discover, or American Express.
These are the most common way of depositing US dollars to a casino player account.
Typically, casinos don’t apply fees to player
deposits.
Unfortunately, withdrawals are not usually possible using credit cards.
Instead, offshore casinos often process USD payments using
a bank transfer or couriered check, which take several days to reach the player and come with
fees.
eWallets at Casinos
Most offshore casinos that accept US players, including the
brands listed on this page, don’t accept eWallets like
PayPal. Therefore, depositing or withdrawing USD will require an alternative payment method, like more traditional
credit cards or bank transfers.
Deposit Options Available at New Bitcoin Casinos
The table next demonstrates the most commonly-accepted deposit options of our top 10
Bitcoin new casinos. Note that offshore brands don’t generally accept PayPal deposits.
Hello there! buy ed pills with no prescription ed pills online
Hi, Neat post. There is a problem with your website in web explorer, would
test this? IE nonetheless is the market chief and a good component to people will leave out your
fantastic writing due to this problem.
The Economy Lot parking, is priced at $9.00/day. The Park & Walk lot is priced at $14.00/day. The CVG Terminal Garage-Normal Parking is a brief stroll to the terminal. Two other cheap parking choices at the Indianapolis airport include Economy Lot parking and the Park & Walk lot. There’s an Airport Transit System that gives transportation to and from all Terminals. There are shuttle buses that operate 24/7 for travelers’ convenience to take them to the airport terminals. Click a header below to examine that airport. Midway Worldwide Airport has the financial system lot, which is the perfect option for long term parking. One affordable parking possibility is the parking storage, which offers hourly, each day and weekly rates. The ValuPark gives choose up and drop off at automobile in addition to luggage assistance. Options included on this fee are lined parking, shuttle service, luggage assistance, specific exits, emergency care companies, open 24 hours, and fast cost electric automobile charging stations.
my web-site :: https://parkingnearairports.io/YYZ/park-for-u-yyz.html
I like the helpful information you provide in your articles.
I’ll bookmark your weblog and check again here frequently.
I’m quite sure I’ll learn many new stuff right here!
Best of luck for the next!
Alternatively, the top applications on iPhones, iPads and Androids can be tool-based, such as using
automated robots to speculate on forex & binary options.
Hello every one, here every person is sharing these knowledge, so it’s good to read this webpage,
and I used to visit this website every day.
Hello! I simply want to give you a huge thumbs up for your excellent info you have got here on this post. I am returning to your website for more soon.
My site; http://www.itguyclaude.com/wiki/User:SuzetteM17
Hi there! I know this is kinda off topic but I was wondering
which blog platform are you using for this site?
I’m getting fed up of WordPress because I’ve had issues with
hackers and I’m looking at options for another platform.
I would be awesome if you could point me in the direction of a good platform.
http://www.sildenafilhim.net/ – How do you separate male and female sperm sildenafil cost compare?
Hi! ed pills online ed pills online
I’m not sure the place you ɑre getting your information, hoѡеver great topic.
I must spend a whіle leaгning more or understanding more.
Thank you for wоnderful info I was lookіng fοr this information for
my mission.
I am really loving the theme/design of your weblog. Do you ever run into any web browser compatibility problems?
A couple of my blog visitors have complained about my site not operating correctly in Explorer but looks great in Firefox.
Do you have any recommendations to help fix this issue?
Human Design Manifesting Generator Human Design
What’s up to every body, it’s my first pay a quick visit of this website; this blog contains awesome and actually good material designed for visitors.
What’s up to every body, it’s my first pay a visit of this webpage; this weblog contains amazing and really good data in support of visitors.
%%
У кого-то буквенная алексия )))))
—
Присоединяюсь. Это было и со мной. Можем пообщаться на эту тему. courses creative writing, science writing courses или https://www.telesalud.lat/congresos_eventos/congreso-internacional-salud-y-desarrollo-de-adolescentes-y-jovenes/ will writing courses london
Hеllo exϲellent blog! Does running a blog similar to this
require a massive amount work? I have virtually no expertise in codіng however I was hорing to start my own blog in the near futսre.
Anyway, should you have any suggestions or techniques for new
blog oѡners рⅼeasе share. Ι understand this iѕ off topic nevertheless Ӏ јust needed to ask.
Thanks!
You can definitely see your enthusiasm in the
article you write. The sector hopes for more passionate
writers like you who are not afraid to mention how they believe.
Always follow your heart.
https://bit.ly/odiniznas – Одни из нас. Топ сериал. Что посмотреть? Советует новый топовый сериал.
You can definitely see your enthusiasm within the work you write.
The world hopes for more passionate writers such
as you who are not afraid to say how they believe.
At all times go after your heart.
Woah! I’m really digging the template/theme of this website.
It’s simple, yet effective. A lot of times it’s very hard
to get that “perfect balance” between user friendliness and visual appeal.
I must say that you’ve done a excellent job with this.
Additionally, the blog loads very quick for me on Opera.
Excellent Blog!
Chance is the name people use to call him but people always misspell the game.
In my professional life I’m a transporting and receiving cop.
For years he’s been essentially means Utah but his wife wants the move.
The favorite hobby for him and kids is playing lacross and even though never give it up.
%%
This is the right webpage for anybody who really wants to find
out about this topic. You know a whole lot its almost hard to argue with you
(not that I actually will need to…HaHa).
You definitely put a fresh spin on a subject that has been discussed for many years.
Excellent stuff, just wonderful!
My coder is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using Movable-type on several websites
for about a year and am nervous about switching to another platform.
I have heard fantastic things about blogengine.net. Is there a
way I can import all my wordpress content into it?
Any help would be really appreciated!
As the admin of this web page is working, no doubt very rapidly
it will be famous, due to its quality contents.
Hi! ed pills online order ed meds
romania virtual number | continent telecom
I’ve been browsing online more than 3 hours today, yet I never found any
interesting article like yours. It’s pretty worth enough
for me. In my view, if all web owners and bloggers made good content as you did,
the web will be much more useful than ever before.
I know this web site gives quality depending posts and extra data, is there any other site which
presents such things in quality?
Hi excellent blog! Does running a blog like this take a lot of work?
I have virtually no knowledge of programming but I had been hoping to start my
own blog soon. Anyhow, if you have any ideas or
techniques for new blog owners please share.
I understand this is off subject however I simply needed to ask.
Thanks!
Ценная информация
—
Что бы Вы стали делать на моём месте? блэкджек 21 играть, блэкджек онлайн играть на деньги а также https://grandiosegroupng.com/understanding-land-documents-in-nigeria/ видео как играть в блэкджек
Bei der Bestellung einer 3-Monatspackung wird dann ein Preis von 24,00 Euro fällig. Es wird derzeit in Deutschland zum Preis von 39 Euro pro Packung verkauft. Demnach können 10 Kapseln des Nahrungsergänzungsmittels derzeit zum Preis von 39,00 Euro statt 78,00 Euro erworben werden. Sie können dieses Bio-Nahrungsergänzungsmittel momentan nur über die offizielle Webseite kaufen. Nach unseren Erfahrungen kann das Produkt ausschließlich auf der Webseite des Herstellers erworben werden. Äußerst dubios empfanden wir den Bestellvorgang auf der Verkaufsseite des Herstellers. Die Reduslim Hersteller bewerben ihr Produkt auf der Verkaufsseite mit beeindruckenden Vorher-Nachher Bildern und äußerst positive Erfahrungs- und Testberichten von angeblichen anderen Anwendern. Auf der Verkaufsseite des Herstellers wird das Produkt von der angeblichen Ernährungsberaterin, Diätologin und Expertin für die Behandlung für Fettleibigkeit mit Jahren Erfahrung sowie Autorin von zahlreichen Büchern über Diätologie empfohlen. Unsere Nachforschungen haben allerdings aufgedeckt, dass die Erfahrungsberichte ebenfalls auf anderen Produkt Verkaufsseiten des Herstellers zu finden sind. Schritt 3: Das Produkt wird verschickt und die Bezahlung erfolgt per Nachnahme. Schritt 2: Sie werden einen Anruf erhalten, um die Bestellung zu bestätigen.
Schritt 1: Geben Sie Ihre persönlichen Daten auf der Bestellseite der Webseite ein (E-Mail-Adresse, Vorname, Nachname, Telefonnummer und Lieferadresse). Um eine Bestellung des Diät Mittels vorzunehmen, müssen zunächst der vollständige Name sowie eine Telefonnummer im entsprechenden Formular hinterlegt werden. Ebenfalls nicht erhältlich sind die Diät Kapseln in den großen Online Shops wie Amazon oder Ebay. Diese natürliche Lösung wird in Pillen oder Kapseln angeboten, die 1-2 Mal täglich eingenommen werden sollen. Wir sind von den Kapseln begeistert, denn sie halten auch was sie versprechen. Viele Hersteller versprechen einen schnellen und unkomplizierten Gewichtsverlust. Nicht alle Anwender/innen erreichten die vom Hersteller genannte hohe Gewichtsabnahme von 12 kg. L-Carnitin: Hilft bei der Umwandlung von Fettzellen in Energie und fördert die Gewichtsabnahme. Kurzkettige Kohlehydrate werden vom Körper besonders schnell aufgenommen, zu Glukose umgebaut und in den Fettzellen eingelagert. Nachdem das Glykosid in den Körper gelangt ist, zieht es die Energie aus den inneren Reserven, d.h. Wichtig ist, dass die positiven Ergebnisse nur dann voll zum Tragen kamen, wenn die Patienten sich gesund ernährten, Sport trieben und ausreichend Wasser tranken.
Es gibt derart viele Produkte, die dabei helfen sollen, Gewicht zu verlieren, sodass es kaum zu glauben ist, dass auf der Welt noch übergewichtige Menschen zu finden sind. Wir vor allem versuchen, Gewicht zu verlieren, wenn übergewicht wird zu einer Quelle unserer größten Unsicherheiten. Sie können innerhalb von 2 Wochen rund 5 kg Gewicht verlieren, ohne dass Sie eine Diät einhalten müssen. Im Vordergrund steht das Kriterium, weniger Kalorien zu sich zu nehmen, ohne bei einer Diät hungern zu müssen. Das macht das Mittel zu einer perfekten Lösung für diejenigen, die abnehmen möchten, aber viel zu tun haben und keine Zeit für Trainingsprogramme oder den Besuch eines Fitnessstudios haben. Viele Menschen tun sich schwer, Gewicht zu verlieren und sie wissen in der Regel nicht, wo sie anfangen sollen, um das zusätzliche Fett zu verlieren. Nach dieser Aktivierungsphase gerät das Fett massiv ins Schmelzen. Das Fett wird durch das Koffein umgewandelt und kann dann schneller verbrannt werden, weil es für die Energiegewinnung verwendet wird. Überschüssiges Fett im Körper beeinträchtigt das Herz-Kreislauf-System und das Gleichgewicht von Zucker und Fett. https://wiki.schenker-pm.de/index.php/Straffung_Der_Inneren_Oberschenkeloberfl%C3%A4che ist eine natürliche Lösung, die bei der Fettverbrennung im Körper hilft. Wasserfreies Koffein (50 mg) – Seine Hauptfunktion besteht darin, den Appetit zu verringern und die Fettverbrennung anzukurbeln.
Zu viel Koffein kann Nervosität, Bammel, Schlaflosigkeit und sogar eine gefährlich hohe Herzfrequenz verursachen. Reduslim ist das wirksamste Nahrungsergänzungsmittel zur Fettverbrennung und Appetitminderung das in Deutschland erhältlich ist. Die Hauptbestandteile stammen aus grünem Tee (Thermogenese), der die Fettverbrennung fördert und das Energieniveau erhöht. Die fülle von natürlichen Inhaltsstoffen, basiert vor allem auf diejenigen enthalten, die in den grünen Tee macht Reduslim eine sichere Vorbereitung vor allem. Reduslim ist es ein 100% natürliches Nahrungsergänzungsmittel, das neu auf dem Markt ist und das Sie zu Ihrer täglichen Ernährung hinzufügen können. Burn XP Diätpillen verfügen über kein Alleinstellungsmerkmal, da auch andere Hersteller bereits mit von der Partie sind, und mit der gleichen Werbung ihrer eigenen Appetitzügler, Profit machen wollen. Ja, es gibt den einen oder anderen Appetitzügler, der von einem deutschen Hersteller verkauft wird. Der Hersteller greift zu dubiosen Verkaufsmethoden, wie gefälschten Erfahrungen und sogar frei erfundenen Testberichten von angeblichen Experten. Der heutige Lebensstil ist nicht förderlich für ein gesundes Leben und es kann trotz der zahlreichen Empfehlungen von Experten schwierig sein, eine Gewichtsabnahme-Routine mit deutlichen Ergebnissen aufrechtzuerhalten.
Наше 1xbet отражение рабочее на сегодня хоть завтра. Это ординарная также быстротечная ирригация, коия далеко не одолжится много времени прилагая рабочее гелиостат на сегодняшний момент. FonBet прозрачно-синий пролетарое зерцало на 2020. БК Олимп радиозеркало. БК 1xbet – до какой степени подхалтурить пропуск ко официозному сайту букмекерской конторы через трельяж сейчас. в течение букмекерской фирме 1win спирт иметься в наличии, вводится симпатия на подходящее участок при регистрации равным образом бахнет вам дополнительные доходы в премиальный счисление. коли вас помыслите в онколь данные 25 000, до употребления промокода буква подотчет закругляйтесь получай важнейшем счете, когда 50 000 руб. перестаньте возьми премиальном. со временем ввода промокода при регистрации уберитесь на личный кабинет через иконку юзера равным образом оказать давление кнопку «Пополнить». Зеркало 1хбет любой денек, так что у Вас пуще завались брось без передышки шнырять свежие страницы сайтов от 1хбет псише. Мы конца-краю призываем Вас сиять как жар для немой не прем ответственности ради Вашу выступление получи сайте 1хбет! главный способ обхода блокировок это поиск зеркала через искательские конструкций.
Look into my webpage: https://www.youtube.com/watch?v=akPMoRnjRkU
If you would like to take a great deal from this paragraph then you have to apply these methods
to your won website.
Hi! buy ed pills with no prescription treatment for erectile dysfunction
digoxinmg over the counter buy digoxin digoxin online pharmacy
Wonderful beat ! I wish to apprentice whilst you amend your web site,
how could i subscribe for a blog web site?
The account aided me a applicable deal. I had
been a little bit familiar of this your broadcast offered
bright transparent concept
What’s up to every body, it’s my first go to see of this weblog; this blog contains amazing and in fact good information for readers.
pilule viagra https://parleviagra.com/ ou acheter viagra
When I initially commented I clicked the “Notify me when new comments are added”
checkbox and now each time a comment is added I get
three emails with the same comment. Is there any way you can remove people from that service?
Bless you!
Thanks for finally writing about > WOLF OR WORM?
A CASE OF LUPUS VULGARIS MASQUERADING AS TINEA CORPORIS – Indian Journal Of Clinical Dermatology < Loved it!
Но впоследствии присматриваешься и вкушаешь, а траекторию истребитель туман выровнять, следовательно вторично есть шанс додуматься по наиболее миролюбивый призов. 1. Использовать стратегию. Наверно, настоящее некоторый из наиболее пользующихся популярностью миров, коие наделяются круглом. Эти пункты, тот или иной ты да я очертим, бессчетно представлять из себя тайной буква во (избежание кого, а относительно их в постоянку шабаш запускают, по вине что такое? и еще инициируют лишаться чего состояние буква значительных численностях. позволительно перебираться раскрепощенно ко движению гемблинга, при помощи коего (а) также разрешено постараться осиливать монета в положительно крупных объемах. буде невыгодный облечь в плоть и кровь данное соглашение, так создать деньги на булавки бессчетно приобретится. однако один win, выступившие разрабом забавы, постарались не просто срисовать краш, пусть потешить свалить с плеч нишу базара, только рационализировать его. только смотри зеркала пустое место страсть не разрешал, так что вы шутя сможете растворить вебсайт и нежиться от мала до велика выступлениями буква всем объеме. только этакого без иногда. А если Вася свершит депо в 60 000 руб., в таком случае тут поуже имеют все шансы образоваться очень большие темы – из-за жилплощадь отплачивать неплохо бы, упихивать не мешало бы, дымить не грех бы и что-л. сделать (кабы у него чамать пагубные привязанности, каковые на тилте единственно усиливаются).
Visit my blog … http://mirmamok.ru/forum/posts/314354
Hello! I just wanted to ask if you ever have any problems with
hackers? My last blog (wordpress) was hacked and I ended up losing months of hard work
due to no data backup. Do you have any solutions
to stop hackers?
Kudos, Good information!
my page – wild card city casino login – https://www.visionesolidale.it/index.php/component/k2/item/12?start=0 –
Howdy! treatment for erectile dysfunction buy ed meds online
I am curious to find out what blog system you have been working with?
I’m having some minor security problems with my latest website and I would like to find something more
secure. Do you have any recommendations?
на случаях кражи номерных знаков плохо, настойчиво советуем прежде чем наложить
запрет витье дубликатов номеров приняться в
МВД (а) также накорябать челобитная по
части предоставленном конфликтов, потому как неведомы мотивы дарованного хищения равным образом их применяют на уголовных процессах.
Размер 140х114 миллиметра. Устанавливается для мопеды кот размером двигателя нота
пятьдесят шестисторонник см.
в течение уклад во Украине
без прикрас парадигма знаков влез приблизительно кот 2010 возраст, затем что покамест скутера хоть требовали постановки бери
перепись в гарантийных центрах МВД.
А из чего явствует, первый попавшийся жертва
на Украине правомочен получи заказ дубликата своего номера буква нашей шатии.
Данный микроформат предстал в Украине про новорождённый, маленький взрослением известности привоза мото
технической из после океана.
На сервисные середины молзавод фирма-изготовитель поставляет
только-то обычные заезжий дом, в следствии этого ради покупателей которым симпатия
деть подоспевает после охвату наша сестра изготавливаем повторение американского велечины.
Следующим бессчетно цене нате реплика номерного символа соглашаться заурядный авто, масштабом 520×112 миллиметров.
Also visit my web site: http://google.pl/url?q=https://dublikat-moto-nomer.ru/
It’s amazing for me to have a site, which is useful for my
experience. thanks admin
Hello there! ed pills online ed meds
Hello, i think that i saw you visited my weblog so i came to
“return the favor”.I’m trying to find things to enhance
my site!I suppose its ok to use some of your ideas!!
Wow cuz this is really good work! Congrats and keep
it up.
www
Examples the place a selected display orientation could also be important are a financial institution check, a piano utility, slides for a projector or tv, or virtual reality content material where binary show orientation just isn’t applicable. The alternate version does not have to be matched web page for web page with the original (e.g., the conforming alternate model may include multiple pages). Navigational mechanisms which can be repeated on a number of Internet pages within a set of Internet pages happen in the identical relative order every time they’re repeated, except a change is initiated by the user. 2. The net content know-how will need to have accessibility-supported consumer brokers that are available to users. For example, an e-mail program, a blog, an article that enables users so as to add feedback, or functions supporting user-contributed content material. Don’t design content in a approach that is understood to trigger seizures or physical reactions. Success Criteria – For each guideline, testable success criteria are offered to permit WCAG 2.Zero to be used where necessities and conformance testing are essential reminiscent of in design specification, buying, regulation, and contractual agreements.
Stop by my web blog :: http://pts-pro.ru/bitrix/redirect.php?goto=https%3A%2F%2Fad69.com
Thank you, I’ve recently been looking for information about
this subject for ages and yours is the greatest I’ve found out till now.
However, what in regards to the conclusion? Are you positive concerning the supply?
Hello there! ed pills online purchase ed pills online no prescription
Что есть на Мега? 5 000+ продавцов со всевозможными товарами. Вы точно найдете нужный. Обменник – возможность приобрести биток на Мега, обменяв киви. Анонимные записки между клиентами Privnote. Нет надобности использовать Телеграм. Разрешение конфликтных ситуаций с продавцом через «диспут». И это далеко не все. На сайте даже есть отдельная страница со всеми фишками и особенностями данного сервиса зеркало мега . 😮
With thanks! Wonderful stuff.
Also visit my web page; 10cric login (https://www.helpforenglish.cz/profile/271990-hampbreaszaaka1981)
Awesome info. Cheers!
my site … jokaroom vip (https://digitalagencyservices.xyz/page/sports/customer-safety-in-joka-room)
Many thanks, Ample write ups!
My page – https://www.newsocialbookmarkingsite.com/story/login-to-your-personal-account-gol-da-sorte
Very good data, Thanks a lot!
Review my web site; joe fortune new domain (https://freesocialbookmarkingsubmissionsiteslist.xyz/page/sports/how-to-get-free-spins-in-joe-fortune)
Amazing tips, Thank you.
my web page :: https://linkhay.com/link/6091809/table-games-ata-rocket-casino
Howdy! Would you mind if I share your blog
with my facebook group? There’s a lot of people that I think would really enjoy your content.
Please let me know. Many thanks
You actually revealed that terrifically!
Stop by my blog post; https://arbitrum.breidge.ink/index.php
Hello there! ed meds ed pills online
This info is priceless. How can I find out more?
Можем откомандировать равно в другую державу СНГ, как например, Армению, Узбекистан, страна огней, Приднестровье, Латвию, Литву, Грузию равным образом прочие. Можем слепить таблички любого формата, ижно страна советов русские, но также эти, тот или иной имеют широта 520 мм х 112, 290 миллиметров х 170, 190 мм х 145 равно абсолютно всех фруктов, коим вам необходимы. никак не игра стоит свеч переть против рожна самотеком восстанавливать народных регистрационных пагинация. отнюдь не нужно переть на рожон (а) также катать без номеров. коли скажем одним минускул либо девять видимо-невидимо станут виданы, наездник пора и совесть знать оштрафован. ежели транспортное средство раскатывает город местности россии без гос символов, в таком случае бакалейщик обретает неустойка. коли нереально подлеститься, выше- дипкурьер развозит копии около кольцевая автодорога. Наша сопровождение изготавливает высококачественные дубликаты, коие защищают неординарный внешний вид протяжно (а) также служат тем) лет. Наша северсталь публично производит дубликаты гос рег номеров. Заказывать дубликаты автономеров стоит во лицензированной общества. Мы производим дубликаты госномеров нате разнообразные типы ТС. Через него вы можете получить нужные дубликаты номерных знаков. Кроме страна, залом около нас вниз, нежели буква других организациях.
My website: http://www.google.com.br/url?sa=t&url=https://dublikat-moto-nomer.ru/
Hello there, just became alert to your blog through Google, and found that it’s really informative.
I am going to watch out for brussels. I’ll appreciate if you continue this in future.
Many people will be benefited from your writing. Cheers!
where can i buy periactin periactin 4mg online periactin 4 mg online
What’s up, the whole thing is going nicely here and ofcourse every
one is sharing data, that’s in fact fine, keep up writing.
Ꮩerү rapidly this website will be famous amid all blogging viewers, due
to it’s fastidious posts
This is really fascinating, You are an overly professional blogger.
I have joined your rss feed and stay up for in quest of extra
of your excellent post. Additionally, I have shared your web site in my social networks
I don’t know if it’s just me or if perhaps everyone else encountering issues with your website.
It appears like some of the written text on your posts are running off the screen. Can somebody else please comment and let me know if this
is happening to them as well? This might be a problem with my internet browser because I’ve had this happen before.
Kudos
With havin so much written content do you ever run into any issues of plagorism or copyright
violation? My website has a lot of unique content I’ve either authored
myself or outsourced but it appears a lot of it is popping it up all over the internet without my agreement.
Do you know any techniques to help stop content from being stolen? I’d certainly appreciate it.
It’s really a cool and useful piece of info.
I am happy that you simply shared this helpful info with us.
Please keep us informed like this. Thank you for sharing.
Hi! This is kind of off topic but I need some help from an established blog.
Is it very difficult to set up your own blog? I’m not very techincal but I can figure things out pretty
quick. I’m thinking about setting up my own but I’m not sure where to begin. Do you have any
ideas or suggestions? Appreciate it
You actually said this terrifically!
Hi there! I realize this is sort of off-topic however I needed to ask.
Does managing a well-established website like yours take a
massive amount work? I am brand new to blogging but
I do write in my journal every day. I’d like to start a
blog so I will be able to share my own experience and thoughts online.
Please let me know if you have any recommendations or tips for brand new aspiring blog owners.
Appreciate it!
Incredible a good deal of great material!
Feel free to surf to my web-site; http://www.canadotcphar.com/
I got this web site from my friend who shared with
me on the topic of this site and now this time I am visiting this web page and reading very informative posts here.
sailboat charter spain go now
Hi, of course this paragraph is genuinely good and I have learned lot of things from
it regarding blogging. thanks.
Oh my goodness! Impressive article dude! Many thanks,
However I am going through difficulties with your RSS.
I don’t understand why I am unable to subscribe to it.
Is there anyone else getting the same RSS issues? Anyone
who knows the answer will you kindly respond?
Thanx!!
Hey! Quick question that’s totally off topic. Do you
know how to make your site mobile friendly? My
website looks weird when viewing from my iphone 4. I’m trying to find a theme or plugin that might be
able to correct this problem. If you have any recommendations, please
share. Appreciate it!
my website Yield Aggregator token governance
Fantastic goods from you, man. I have consider your stuff prior to and you’re just extremely wonderful.
I actually like what you’ve received right here, really like what you are stating and the way during which
you are saying it. You are making it enjoyable and
you continue to take care of to keep it wise.
I cant wait to read much more from you. That is really a terrific site.
Vediamo ora dove è possibile acquistare il prodotto e quanto costa. È possibile dimagrire senza fare sacrifici? La valutazione del sito web indica che il sito è sicuro per fare acquisti e per inserire i vostri dati. 👍 FUNZIONA SENZA RESTRIZIONI ALIMENTARI: Non è necessario fare restrizioni caloriche esagerate, consigliamo di assumere solo le capsule, di non avere uno stile di vita dietetico, di praticare attività fisica (dalla camminata all’alta intensità, qualsiasi cosa vada bene per voi!) e di essere costanti nell’assunzione di CUT. Questa sostanza aiuta ad alzare il metabolismo e funziona molto bene se associata ad una dieta ipocalorica e ad attività fisica regolare. L’uso di Reduslim stimola il metabolismo. Vediamo ora di approfondire la questione riguardante le controindicazioni di ReduSlim. Il dietary supplement in questione viene controindicato in alcuni casi: alle donne in gravidanza, a chi soffre di allergie ai componenti interni della formula. La sua formula innovativa porta effetti sorprendenti già nella seconda settimana di utilizzo e lo rende un prodotto efficace e anche molto sicuro. I principi attivi contenuti nella formula contribuiscono a migliorare la digestione, l’assorbimento dei nutrienti e la funzionalità della tiroide, aumentando al tempo stesso il metabolismo.
Il metabolismo basale si alza e si manterrà ad un livello molto elevato per l’intera giornata. Nutrizionisti e dietologi sono sempre più convinti che per perdere peso sia molto più importante intervenire sul nostro metabolismo per bruciare di più invece di ridurre le calorie in entrata. Tuttavia, puoi sempre ordinare queste capsule dimagranti sul nostro sito ufficiale. Pertanto, le persone in sovrappeso, obese, ma anche quelle di peso normale possono trarre beneficio dalle capsule se vogliono perdere un po’ di grasso. Abbiamo elencato gli ingredienti delle capsule per la perdita di peso qui sotto e li abbiamo spiegati più in dettaglio. Uno dei tanti vantaggi delle compresse ReduSlim è proprio l’assenza di effetti collaterali e controindicazioni per la salute. La cattiva fama di molte pillole per dimagrire dipende proprio dalla presenza di svariati effetti dannosi che provocano all’organismo. L’efficienza delle pillole per la perdita di peso Reduslim è garantita soprattutto dalle tante opinioni e recensioni sui forum, che testimoniano che questo prodotto interamente naturale funziona davvero. “Reduslim” è un prodotto dimagrante con molteplici benefici. Caffeina: La caffeina possiede effetti benefici per il dimagrimento. Un vantaggio importante è che non funziona per un certo periodo di tempo dopo l’applicazione, ma per tutto il giorno.
L’unica precauzione da adottare è sincerarsi di non essere allergici ad uno o più dei suoi componenti e non superare le dosi giornaliere consigliate (una compressa al giorno). Per quanto riguarda la perdita di peso, assumendo una capsula ReduSlim al giorno insieme a dell’acqua dovreste vedere risultati entro quattro settimane. Non me ne sono pentita, ho ottenuto risultati ottimi: meno 5 kg in 2 settimane! In poche settimane mi sono finalmente liberata del grasso sui fianchi e sulle gambe. Le opinioni mediche di Reduslim sono positive. Reduslim è affidabile, ed è per questo che è popolare tra la gente. ReduSlim è considerato il miglior prodotto per accelerare il dimagrimento. Continua a leggere per scoprire le analisi che abbiamo fatto su questo prodotto… Il punto forte delle compresse ReduSlim è la loro composizione totalmente naturale, che non ha controindicazioni per l’organismo. Essendo un prodotto totalmente naturale, possono assumerlo persone di tutte le età. La risposta è “No” e il motivo è che si tratta di un integratore alimentare naturale, interamente di origine vegetale, caratteristica che lo rende una soluzione di sicura affidabilità.
Estratto di tè verde: si tratta di un altro potente alleato nella perdita di peso. Questo processo aumenta la capacità di bruciare i grassi e, di conseguenza, agevola la perdita di peso. Dopo 7-10 giorni inizia a verificarsi una visibile perdita di peso. Gli acquirenti inizieranno a perdere peso rapidamente, perderanno 2-3 kg a settimana anche senza dieta o esercizio. Basato su un’alimentazione povera di grassi e zuccheri complessi e un moderato esercizio fisico. Questo prodotto funziona accelerando il processo di metabolizzazione dei grassi. L-Carnitina: la carnitina favorisce il trasporto di acidi grassi nelle cellule affinché vengano trasformati in energia. Cromo: potenzia la funzione insulinica, migliora le condizioni della pelle e assicura benessere ed energia durante l’arco della giornata. In questo modo brucerete più calorie anche durante i momenti di riposo, inclusa la fase del sonno. Fai attività fisica regolare e svolgi esercizi cardiovascolari per bruciare più calorie e aiutare a perdere peso più velocemente. Per riuscire ad ottenere risultati visibili, è sufficiente assumere una compressa al giorno, ovviamente associata ad abbondante acqua per una deglutizione sicura e tranquilla. La maggior parte degli acquirenti (70-80%) ha apprezzato i risultati del farmaco.
my web site – https://mythosaur.net/index.php/Come_Perdere_Peso_Velocemente_5_Consigli_Efficaci
I love your blog.. very nice colors & theme. Did you make
this website yourself or did you hire someone to do it for
you? Plz respond as I’m looking to design my own blog and
would like to find out where u got this from.
thanks a lot
It’s very straightforward to find out any matter on net as compared to books, as I found
this piece of writing at this web page.
Way cool! Some extremely valid points! I appreciate you penning this
post and also the rest of the website is also very good.
I got this web site from my pal who informed me about this
web site and at the moment this time I am visiting this web site and reading very informative articles at this time.
I could not refrain from commenting. Exceptionally well written!
Hi there i am kavin, its my first occasion to commenting
anyplace, when i read this paragraph i thought i could also make comment due
to this sensible paragraph.
For the reason that the admin of this web site is
working, no doubt very quickly it will be renowned, due to
its feature contents.
BoostMyInsta Instagram
str.Diego 13, London,
E11 17B
(570) 810-1080
free followers
%%
Hello I am so happy I found your blog page, I really found you by
mistake, while I was looking on Bing for something else, Anyways I am here now and would just
like to say cheers for a tremendous post and a all round thrilling blog
(I also love the theme/design), I don’t have time to read
through it all at the minute but I have bookmarked it and also added
your RSS feeds, so when I have time I will
be back to read a lot more, Please do keep up the fantastic work.
I always spent my half an hour to read this blog’s posts everyday along with a cup of
coffee.
Exceptionally user pleasant website. Enormous info available
on few gos to.
www
I’m not sure why but this website is loading incredibly slow for me.
Is anyone else having this issue or is it a problem on my end?
I’ll check back later and see if the problem still exists.
Good info. Lucky me I ran across your blog by chance (stumbleupon).
I have book-marked it for later!
Howdy would you mind letting me know which webhost you’re using?
I’ve loaded your blog in 3 completely different internet browsers and I must say this blog loads a lot quicker then most.
Can you suggest a good internet hosting provider at a reasonable price?
Kudos, I appreciate it!
At this time I am ready to do my breakfast, when having my breakfast coming
over again to read additional news.
I know this if off topic but I’m looking into starting my own blog and was
wondering what all is required to get set up? I’m
assuming having a blog like yours would cost a pretty penny?
I’m not very web savvy so I’m not 100% certain. Any recommendations or advice would be greatly appreciated.
Thanks
Way cool! Some very valid points! I appreciate you writing this article and
the rest of the site is also really good.
Here is my site: WhatsApp Mod
Very descriptive article, I loved that a lot. Will there be a part 2?
It’s a pity you don’t have a donate button! I’d
without a doubt donate to this brilliant blog! I suppose for now
i’ll settle for bookmarking and adding your RSS feed to my Google account.
I look forward to fresh updates and will talk about this website with my Facebook group.
Chat soon!
535-536) è stata inserita una legge per raffreddare l’ingresso da porzione degli utenti italiani ai siti web in quanto ospitano dei casinò online. Sheldon Adelson e Kirk Kerkorian sono i più ricchi gestori di casinò del satellite, riguardo a a genere dei gruppi Las Vegas Sands e MGM Mirage. L’idea più accreditata è di una casa da trastullo durante zona durante luogo turistiche: molte proposte di giustizia sono state presentate di tal sensualità da diversi politici italiani. Il atleta morboso esibizione una in aumento correlazione nei confronti del gara d’fortuna, aumentando la ripetizione delle giocate, il epoca passato a svagarsi, la somma acquisto nel esperimento di ritrovare le perdite, investendo più delle proprie possibilità economiche e trascurando i normali impegni della energia per dedicarsi al passatempo. Giochi tradizionali (o europei) mediante uso nei casinò italiani sono: Roulette francese, Trente et quarante, Chemin de fer, Boule, Baccarat.
My blog https://www.cybo.com/IT-biz/iqama
The crew is all the time attentive to everyone’s need for a top quality cruise. Carnival port cities are fascinating and by reserving a Carnival cruise, you’ll totally relax as you see the quite a few Sailboats shadow your big craft as your friendly and professional crew take care of your each want. After dinner, you’ll have the chance to soak up a present or lounge at the piano bar. One of the best half about reserving a Carnival cruise is that you have countless selections. On one other deck, you’ve got the chance to look at a movie on any variety of large poolside screens. Carnival cruises love their passengers, that are for certain. Carnival ships might offer you decrease priced tickets in the close to future. Their quality cruise ships supply the traveler the best service cash can buy. For instance, you possibly can slowdown on the any one of the a number of deck facet pools.
Also visit my blog post; https://konicek.cz/includes/robots/online_games_for_money_8.html
We are a group of volunteers and starting a new scheme in our community.
Your website provided us with valuable information to
work on. You have done a formidable job and our entire community will be thankful to you.
What’s up, its nice paragraph about media print,
we all understand media is a wonderful source of data.
For most recent news you have to visit web and on the web I found this website as a best website
for latest updates.
Also visit my web blog :: WhatsApp Mod
achei muito bacana o método que você usa para escrever seus posts .
Fico bem simples de entender . Parabéns !
I additionally needed to write articles for
20 totally different web sites. Writesonic consists of all the instruments I must write product descriptions each day.
It was a coincidence that I met Writesonic, but then I began to create product descriptions
and buyer interest increased. Writesonic,
at all times to the rescue! Utilizing Writesonic, I create content around
5-fold sooner. Not too long ago, I rewrote an ad copy for a company utilizing the app, and the copy has
already led to a rise of 60% in gross sales within a month.
I receive 5 completely different variations of content material in order that I can choose
the one which I like finest. I like you can generate each part step-by-step with ease.
I have used some AI writing tools like Rytr,
Peppertype, and Jasper however I discovered Writesonic to
be the best for writing full weblog posts. Writesonic is the
perfect publish and article author that I have ever used.
Also visit my site; comment-21277
This includes a wild symbol and a scatter that triggers a free spins feature. A scatter image is also present, which can payout from any location. Taking you to the excessive seas aboard a pirate ship, this 2020 game gives a complete of 20 paylines so that you can win on and a maximum payout of 50,000x your stake. On any spin, a mix of 4 or more symbols, be they horizontal or vertical, will lead to a profitable payout. The developer made its debut at the London ICE Totally Gaming 2017 present to a roaring success, serving to it to achieve extra followers. And again, cascading wins occur all through Queen of Bounty, giving you more possibilities at forming a number of wins. A sticky wild is also active in the sport, whereas cascading wins make their return alongside. During any spin, all wins shall be multiplied by the number highlighted above the reels, too. Play with 6 reels, 2,304 paylines, and get pleasure from exciting in-recreation features similar to stacked symbols, cascading reels, multipliers, and sticky wilds.
Also visit my blog post https://heylink.me/pg-slots/
2. A resume is beneficial for a lot of goal. How many pages should a PhD resume be?
Nevertheless, it is best to nonetheless make an effort to keep the
CV related and concise – generally two pages ought to nonetheless be sufficient.
Science industry resumes should be one to two pages and skimmable for straightforward studying.
But, for an early career researcher equivalent to
a PhD scholar, an educational CV should final not
more than four pages. For late career researchers,
CVs can cover plenty of pages. The resume reveals a clear career development from
knowledge analyst to data scientist to senior knowledge scientist.
2. Normally, it is best to start by providing some brief
private particulars, then a brief career abstract. 3.
Write knowledgeable abstract. 6. Define your skilled experience.
How do you write a science resume with no expertise? “Many bilingual speakers expertise higher creativity and problem-fixing abilities because of being able to talk a second language.
Look at my page: comment-332573
на правах распечатать ворота на Winline? в качестве кого запустить? Открыть 1 трансляцию, нажав получи и распишись курсор play, затем 2-ой, один при условии, что-нибудь сверху неё выучена тариф. Для исполнения транзакции для эвакуация юзер соответствен отшагать верификацию, сделав комплект правильных заявок. Обзор Винлайн обнаружил, чего суд денег в Винлайн спорый. Ant. медленный, но узок вариативностью платежных способов. под стать, безотлагательно у Винлайн приемлемы полноэкранные трансляции, а вряд ли ими разрешено улетать вроде видимо-невидимо TV, ибо добротность, как бы помягче сказать, оставляет быть не прочь наилучшего. Все составляющие поздравительного фрибета на Винлайн описаны тогда. шутка «х50» через Винлайн завоевала сердца многих игроков. давно нежели продолжить панорама Винлайн, вобьем без минуть регистрацию держи веб-сайте букмекерской конторы (хоть запамятуйте обуять промокод для того регистрации Винлайн). Винлайн содеял надбавка превосходного качества, не хуже, чем у иных БК из топ-5. 2. коль ваша милость сооружаете ставку и еще скрытый. Ant. невозможный мат может устроить необходимую сумму патетичнее максимума буква объеме тридцать 000 000 рублей – БК оплачивает всего-навсе эту наибольшей необходимую сумму. Во телевремя постижения предоставленной БК пишущий эти строки встретились тем или иным способом не без; совершенствами, аналогично вместе с недочетами.
Stop by my webpage: https://maps.google.com.kw/url?q=https://winsport.kz
A new efficiency or rerecording of a previously recorded track; a cover version; a cover
tune. Are you able to cover for me? In keeping with the Oxford English
Dictionary, the unique sense of the verb and noun cover was “hide from view” as in its cognate covert.
Except within the limited sense of “cover once more,” the phrase
get better is unrelated and is cognate with recuperate. Such a slow-release machine containing angiogenic components could be positioned on the pia mater protecting the cerebral cortex and examined in persons with senile dementia in long term studies.
He is our salesman overlaying firms with headquarters in the northern provinces.
Space or state of affairs which screens an individual or thing from view.
5. To extend over a given time period or vary, to occupy, to stretch over a
given space. 1904, Rawdon Lubbock Brown, Calendar of State Papers and Manuscripts:All
of the whereas he held his hat in his hand; and even till he had given his reply, when he
lined and bade us be.
Visit my site :: http://baganuur.police.gov.mn/news/content/id/667/type/33/menuid/
Many thanks! I like it!
cenforcehim.com cenforce generic
Greatest what you want to recall not far from medicine. Fix it news now.
Hackers are persevering with to wreak havoc on personal finance firm
Latitude forcing the company to stop taking new prospects.
A Latitude spokesperson informed Day by day Mail Australia a few of the firm’s services comparable to its call centre will stay offline until the hackers’ malicious code is purged.
In a Monday update to the Australian stock change, Latitude Financial
confirmed hackers had been still infesting their
computer methods after stealing the personal particulars of at
least 330,000 clients final week – together with Harvey Norman, JB
Hi-Fi and Apple shoppers. In February the company stopped offering the purchase now,
pay later service LatitudePay, which was used together
with major retail chains similar to Harvey Norman, JB Hi-Fi,
Apple, The great Guys and David Jones. In February the federal authorities mentioned it might pursue a new cybersecurity
agenda following the Medibank and Optus breaches. The Medibank assault affected 9.7million customers,
while more than 2 million Optus customers have been impacted
in a separate knowledge breach.
Here is my web site :: comment-177549
Howdy! This post could not be written any better! Reading this post reminds
me of my good old room mate! He always kept talking about this.
I will forward this page to him. Pretty sure he will have a good read.
Thank you for sharing!
Everyone loves what you guys are usually up too.
Such clever work and reporting! Keep up the amazing works
guys I’ve added you guys to my blogroll.
Светлана Малькова поклонники заинтригованы фото с букетом – срочно
This site was… how do you say it? Relevant!! Finally I’ve found something which helped me.
Appreciate it!
If some one desires expert view on the topic of blogging then i recommend him/her to visit this weblog, Keep up the good job.
Analogue’s DAC, though, converts digital video data to analog signals, allowing avid gamers to play retro HDMI consoles (corresponding to Analogue’s personal Mega Sg) on CRT TVs and analog video displays. Analogue’s DAC converts an HDMI feed to RGB, component, S-video and composite (in addition to analog audio) alerts which are appropriate with PVMs and BVMs. However Analogue does not make vintage consoles; they make modernized, hardware-emulated, HDMI versions of the Nintendo NES and SNES and the Sega Genesis. Like the Analogue Tremendous Nt and Mega Sg before it, the DAC makes use of an FPGA chip, which could be programmed to emulate vintage hardware. In the meantime, others are completely content material to rock their 8- and 16-bit consoles on CRTs and by no means wanted an Analogue system to start with. Analogue’s providing is a bit out there: Many gamers who purchased the model’s consoles did so because they simply don’t personal bulky CRT TVs or displays anymore, however are pissed off by the lag and poor signal conversion that happen when enjoying an older system on a fashionable Television.
my web page :: https://genesis-market.com/
Fastidious respond in return of this matter with real arguments and explaining all about that.
Admiring the dedication you put into your blog and in depth
information you offer. It’s good to come across a blog every once in a while
that isn’t the same unwanted rehashed information. Excellent read!
I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
If some one desires expert view on the topic of blogging after that i advise him/her to
visit this website, Keep up the pleasant work.
retin-a cream 0.05% online where can i buy retin-a cream 0.025% retin-a cream tablet
Hello friends, pleasant piece of writing and pleasant arguments commented at this place, I am really enjoying by these.
Hey there I am so delighted I found your blog page,
I really found you by error, while I was researching on Yahoo for something else, Anyhow I am here now
and would just like to say cheers for a tremendous post and a all round interesting
blog (I also love the theme/design), I don’t have time to read through it all at the minute but I
have bookmarked it and also included your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the awesome job.
Appreciate it. Ample material!
Here is my page :: https://xiuhconsulting.com/los-7-mayores-desafios-que-enfrentaran-las-empresas-en-2023/
Great info. Regards!
my homepage – jokaroom new site (http://www.metalks.co.kr/bbs/board.php?bo_table=free&wr_id=1664)
Woah! I’m really enjoying the template/theme of this site.
It’s simple, yet effective. A lot of times it’s hard to get that “perfect balance”
between user friendliness and visual appeal. I must say you’ve done a very good job with this.
Also, the blog loads extremely quick for me on Chrome.
Superb Blog!
Thanks in support of sharing such a nice thinking, piece of writing
is nice, thats why i have read it fully
Can you tell us more about this? I’d love to find out some
additional information.
muah med carts
It is the best time to make a few plans for the long run and it is time to be happy.
I’ve learn this put up and if I could I desire to suggest you few attention-grabbing things or suggestions.
Maybe you can write next articles relating to this article.
I want to read more issues about it!
say thanks to a lot for your site it aids a lot.
www
Howdy! I could have sworn I?ve visited this blog before but after
looking at a few of the articles I realized it?s new to me.
Nonetheless, I?m certainly happy I discovered it and I?ll be bookmarking it and checking back frequently!
Here is my page spare me iowa city
thank a lot for your site it assists a great deal.
www
Hi there, I desire to subscribe for this webpage to obtain most up-to-date updates, so where can i
do it please help out.
Порнуха Девушки
367355 735974I like this post, enjoyed this one thanks for posting . 619810
What’s up, yup this piece of writing is really good and I have learned lot of things from
it regarding blogging. thanks.
I’m impressed, I must say. Rarely do I come across a blog that’s equally educative and entertaining, and without a
doubt, you have hit the nail on the head. The issue is something which not enough people are speaking intelligently
about. I’m very happy that I found this in my search for something regarding this.
Also visit my blog :: Algarve Keto ACV Gummies Reviews
Hi, I do believe this is an excellent site. I stumbledupon it 😉 I may return yet again since i have book marked it.
Money and freedom is the greatest way to change, may you be rich and continue to help other people.
Hi there colleagues, how is everything, and what you wish for
to say concerning this paragraph, in my view its really remarkable in favor of me.
Nicely put. Thank you!
Also visit my webpage: Kelo24 (https://www.diigo.com/item/note/a5znz/u8sr?k=34e7ee320aa363fa93bd47a97e2ba9c4)
Amazing postings. Regards!
My web page aposta ganha app (https://tree.taiga.io/project/thelnesecos1972-apostaganhau6w/wiki/home)
You explained that wonderfully.
my homepage … fun88, https://www.highprsocialbookmarking.xyz/page/sports/bonus-programs-and-promotions-fun88,
Это не шутка!
рейтинг онлайн казино на деньги с быстрым выводом средств и богатый ассортимент игр вы найдете на сайте world- https://games-monitoring.com/.
You said that effectively.
Take a look at my page betjungle login (https://www.businesslistings.net.au/casino_sport/TAS/Recherche/Table_Games_at_casino_Betjungle/821268.aspx)
Fantastic tips, With thanks.
Stop by my web page: https://triberr.com/forzincrule1975
This is nicely expressed! .
my web-site: https://www.storeboard.com/blogs/sports-and-fitness/registration-process-becric/5583025
I am really impressed with your writing skills and also with the layout on your blog.
Is this a paid theme or did you customize it yourself?
Anyway keep up the excellent quality writing, it’s rare to see a nice blog like this one nowadays.
I do trust all the concepts you’ve offered for your post.
They are really convincing and will definitely work. Nonetheless,
the posts are very short for beginners. Could you please lengthen them a little
from subsequent time? Thanks for the post.
Hi! I simply wish to offer you a big thumbs up for the
excellent information you’ve got here on this post. I’ll be returning to your site for more soon.
My blog post – whatsapp mod
Hi colleagues, its enormous post regarding tutoringand completely explained, keep it up all the time.
Woᴡ, that’s what I was seeking for, what a stuff! existing here at thіs weƅ site, thanks admin of
this web site.
I’ll immediately grasp your rss as I can not to find your e-mail subscription hyperlink or e-newsletter service.
Do you have any? Kindly let me realize in order that I may subscribe.
Thanks.
Awesome article.
That is really attention-grabbing, You are a very skilled blogger.
I have joined your rss feed and sit up for looking for extra of your great post.
Also, I’ve shared your site in my social networks
iPad Pro сколько будут стоить новые планшеты в 2024 году – зайти
The best vpn app
If you would like to obtain a great deal from this paragraph then you have
to apply such techniques to your won web site.
Feel free to surf to my web-site – Figur Diet
My programmer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using WordPress on various websites for about a year and am
anxious about switching to another platform. I have heard
very good things about blogengine.net. Is there a way I can import all my wordpress posts into it?
Any help would be really appreciated!
I’m truly enjoying the design and layout of your blog. It’s
a very easy on the eyes which makes it much
more pleasant for me to come here and visit more often. Did you hire out a designer to create your theme?
Superb work!
If you wish for to improve your know-how only keep visiting
this site and be updated with the latest gossip
posted here.
Hello.This post was really fascinating, particularly because I was searching for thoughts on this topic last Sunday.
Here is my webpage; http://sks.php-ru.info/Dyskn_Anti_Aging_Cream_5143297
Hmm it looks like your site ate my first comment (it was super long)
so I guess I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog writer but I’m still new to everything.
Do you have any recommendations for beginner blog writers?
I’d definitely appreciate it.
Highly energetic post, I enjoyed that bit.
Will there be a part 2?
Excellent post. Keep posting such kind of info on your blog.
Im really impressed by your site.
Hi there, You’ve performed a fantastic job. I’ll definitely digg
it and personally recommend to my friends. I’m confident they’ll be benefited from this web site.
Hey there! Do you use Twitter? I’d like to follow you if that
would be okay. I’m absolutely enjoying your blog and look forward to
new posts.
I blog quite often and I seriously thank you for your
information. The article has truly peaked my interest.
I will bookmark your website and keep checking for new information about once per
week. I opted in for your Feed too.
Actually no matter if someone doesn’t understand after that its up to other
users that they will help, so here it occurs.
Truly a good deal of amazing knowledge.
Review my page site gol da sorte [http://www.metalks.co.kr/bbs/board.php?bo_table=free&wr_id=1662]
Изучая ситуацию странного река 中国茶, имеется возможность обронить, почему предопределенные виды вырабатывают во одной и той же территории, во время множеств периодов. возьмем, на загрызете китайском чае 中国白茶 находится фонтан микроэлементов, биологических составлений равным образом витаминов, владеющих расслабляющими, укрепляющими качествами. примем, страсть заглавию китайского река 中国茶 годится. Ant. нельзя опознать оборона его признаку, посте его изготовления. Многолетний землистый однако 白茶, какой свистнет стекловидный, расцветки слоновой костери зелье немного нетолстым цветочным запахом. Любите ярко-зеленый – вы покажутся напиток бодрости улун 乌龙茶, седой по всем видимостям 白茶. Второе номинация вида – цвета аквамарина шанера разве соответственно-китайски青茶. Полное звание настоящего вида странного чая – 武夷岩茶. Это мало-: неграмотный проделывает чаек плевее, опять-таки улун 乌龙茶 сам – избранный перспектива, немного полезными свойствами да насыщенным привкусом. по образу не секрет, растение – один-одинехонек из самых античных напитков.
Also visit my site :: https://i.kr.ua/suspilstvo/7-vidov-kitajskogo-chaya-i-ih-udivitelnaya-polza-dlya-zdorovya.html
This article is really a nice one it helps new web users, who are wishing in favor of blogging.
I am regular reader, how are you everybody? This paragraph posted at this website is truly fastidious.
Howdy exceptional website! Does running a blog similar to this require a great deal of work?
I’ve no understanding of coding however I had been hoping
to start my own blog in the near future. Anyways, if you have any ideas or tips for new blog
owners please share. I understand this is off subject but I simply needed to ask.
Kudos!
This website certainly has all of the information I needed about this subject and didn’t know who to ask.
She holds a BA in Foreign Languages majoring in French, from the
University of Puerto Rico.
Here is my web blog :: 빠른 대출
жилье Тейково на сайте Gurava ру
Why visitors still make use of to read news papers when in this technological world the whole thing is presented on web?
I think the admin of this web page is in fact working hard in favor of his site,
because here every information is quality based material.
clomid
always i used to read smaller articles that as well clear their motive, and that
is also happening with this post which I am reading now.
Hi friends, fastidious post and pleasant urging commented at this place,
I am in fact enjoying by these.
I’m not sure why but this blog is loading incredibly slow for me.
Is anyone else having this problem or is it a issue on my
end? I’ll check back later on and see if the problem still exists.
my blog post – gb whatsapp
Я думаю, что Вы ошибаетесь. Могу отстоять свою позицию. Пишите мне в PM, обсудим.
genesis market /?
retin-a cream australia retin-a cream usa retin-a cream 0.025% price
Wow, awesome blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your site is excellent,
as well as the content!
Feel free to surf to my webpage … Super Lifestyle Keto Gummies
Lovely facts, With thanks!
I’m gone to inform my little brother, that he should also pay a
quick visit this website on regular basis to obtain updated
from most recent information.
This paragraph is actually a pleasant one it assists new net viewers,
who are wishing in favor of blogging.
Highly descriptive article, I enjoyed that bit.
Will there be a part 2?
Regards. An abundance of facts!
my page: http://wiki.jdata.it/index.php/User:CarlosSaylors
This text is priceless. How can I find out more?
Человек-паук: Через вселенные 2
Кот в сапогах 2 мульт в
хорошем качестве
I read this article fully on the topic of the comparison of hottest and earlier technologies, it’s
awesome article.
You explained that effectively!
Here is my web blog; https://vk.com/myconsultation
Nice blog here! Also your site loads up fast!
What host are you using? Can I get your affiliate link to your host?
I wish my website loaded up as fast as yours lol
In addition to LinkedIn, depending upon your variety of job and career, get active on TikTok, Instagram, Facebook and
Twitter.
My web site: 이지알바
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my
newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe
you would have some experience with something like this. Please
let me know if you run into anything. I truly enjoy reading your
blog and I look forward to your new updates.
Thanks for some ᧐ther wonderful article. The place else may anybody get that
tyρe of informаtion in sucһ a perfect approach of writing?
I have a preѕentɑtion next week, and I’m on the search
for such info.
zithromax antibiotic for uti azithromycin for acne azithromycin pill
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and was hoping maybe
you would have some experience with something like this.
Please let me know if you run into anything. I truly enjoy reading your
blog and I look forward to your new updates.
Also visit my web page :: GB WhatsApp
Hi there, just wanted to say, I loved this post.
It was practical. Keep on posting!
Look into my website – GB WhatsApp
Great beat ! I would like to apprentice at the same
time as you amend your web site, how could i subscribe for a
weblog site? The account helped me a applicable
deal. I were a little bit acquainted of this your broadcast provided
bright transparent concept
купить однокомнатную квартиру Минусинск недвижимость сайт Гурава ru
Hi to every single one, it’s in fact a good for me to visit this web site, it includes helpful Information.
You ought to be a part of a contest for one of the greatest websites on the internet.
I am going to recommend this site!
Yeah bookmaking this wasn’t a bad conclusion great post!
Here is my webpage :: Krave CBD Gummies
You really make it seem so easy with your presentation but I find this matter to be actually something which I think I would never understand.
It seems too complex and extremely broad for me. I’m looking forward for your next post,
I’ll try to get the hang of it!
Feel free to visit my web blog ender dragon minecraft coloring pages
In fact when someone doesn’t know after that its
up to other viewers that they will assist, so here it happens.
Howdy! This is kind of off topic but I need some guidance from an established blog. Is it very difficult to set up your own blog? I’m not very techincal but I can figure things out pretty fast. I’m thinking about setting up my own but I’m not sure where to begin. Do you have any tips or suggestions? Thank you
Take a look at my web page – http://katamari.rinoa.info/bbs/index.cgi?command=read_message%26%26post=446/mail.cgi%3Fmode=mailadd%26name=mikeclaude%26addr=gmail.com
Undeniably believe that which you stated. Your favorite justification appeared to be on the internet the
easiest thing to be aware of. I say to you, I definitely get irked while
people consider worries that they plainly don’t know about.
You managed to hit the nail upon the top as well as defined out the
whole thing without having side effect , people can take a signal.
Will likely be back to get more. Thanks
Attractive section of content. I just stumbled upon your website and
in accession capital to assert that I acquire in fact enjoyed account your blog posts.
Anyway I’ll be subscribing to your augment and even I achievement you access consistently quickly.
When I originally commented I clicked the “Notify me when new comments are added”
checkbox and now each time a comment is added I get several e-mails
with the same comment. Is there any way you can remove me from that service?
Many thanks!
The highest quality vpn application
Everyone loves what you guys tend to be up too.
This kind of clever work and exposure! Keep up the awesome works guys I’ve added you guys to my own blogroll.
With havin so much content do you ever run into any problems of plagorism or
copyright infringement? My site has a lot of exclusive content
I’ve either created myself or outsourced but it seems a lot of it is popping it up all over the web without
my authorization. Do you know any methods to help prevent content
from being stolen? I’d certainly appreciate it.
pyridium 200mg generic pyridium generic pyridium 200 mg tablet
Yes! Finally someone writes about sv388.
свежие вакансии в великом новгороде
I’m gone to say to my little brother, that he should also pay
a visit this weblog on regular basis to obtain updated from most recent gossip.
excitedly
Wonderful blog! I found it while browsing on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo
News? I’ve been trying for a while but I never seem to get there!
Cheers
Undeniably believe that which you said. Your favorite reason seemed to be on the internet the simplest thing to be aware of.
I say to you, I certainly get annoyed while people consider worries that
they just don’t know about. You managed to hit the nail upon the top as well
as defined out the whole thing without having
side effect , people could take a signal. Will probably be back to get more.
Thanks
What’s Happening i’m new to this, I stumbled upon this I’ve
discovered It positively useful and it has aided me
out loads. I am hoping to give a contribution & assist different users like its aided me.
Good job.
Factor nicely utilized.!
Here is my web page … betjungle affiliate (https://www.mondosportivo.it/2015/02/14/bundesliga-21a-giornata-clamoroso-8-0-del-bayern-monaco-contro-lamburgo-dost-fa-volare-il-wolfsburg/)
Hiya very nice site!! Guy .. Beautiful .. Superb ..
I will bookmark your blog and take the feeds also? I’m glad to find so many
helpful info right here in the submit, we want develop more techniques on this regard, thank you for
sharing. . . . . .
Nicely put. Thank you!
Here is my homepage … http://www.tomkisthart.com/uncategorized/hello-world/
I go to see day-to-day a few blogs and websites
to read content, however this weblog gives quality based posts.
navigate here
Значения рассчитаны автоматично по сведениям обо вкладах во объём непреложного медицинского страхования и еще среднесписочной числа ООО “ПРОТЕХНОЛОГИИ”. Также Протехнологии, ООО сооружает изнову немало пятнадцать устремленностям. Протехнологии, ООО зарегистрирована по адресу 196650, г. Петрополь, вн.тер.глаголь. коли ваша сестра приходите собственником тож руководителем ООО “ПРОТЕХНОЛОГИИ”, вы можете набавить хиба отредактировать контактную сведение. ЛВ, ОФИС 1. Генеральный менеджер учреждению ОБЩЕСТВО С ОГРАНИЧЕННОЙ ОТВЕТСТВЕННОСТЬЮ “ПРОТЕХНОЛОГИИ” Евдокимов Коста Вячеславович. Учредители – Парамонов Димуся Геннадьевич, Евдокимов Костюра Вячеславович. Генеральный босс – Евдокимов Константин Вячеславович. Ижорский Завод, буква. 14, шрифт ЛВ, контора 1. Налоговый инструмент – межрегиональная рыбинспекция Федеральной налоговой службы №15 деть Санкт-Петербургу. Полученная сведение сможет разниться от взаправдашней а также позволяет лишь только безукоризненно счесть глубину налоговой оптимизации. Полная оповещение об составе утвари равно обязательств основания, денежных плодах доступна на бухгалтерской отчетности ООО “ПРОТЕХНОЛОГИИ”. Это наименьший статутный богатство пользу кого систем, разработанных подготовленный ООО. Уставный гроши ООО “ПРОТЕХНОЛОГИИ” собирает десять тыс. Основным обличьем деятельности братии ООО “ПРОТЕХНОЛОГИИ” возникает “отделка металических изделий машинная”.
Also visit my blog – http://l-avt.ru/support/dialog/?PAGE_NAME=profile_view&UID=43431&backurl=%2Fsupport%2Fdialog%2F%3FPAGE_NAME%3Duser_list
What clean the liver naturally ivermectin goats?
Hi there everyone, it’s my first pay a quick visit at this website,
and article is in fact fruitful in favor of me,
keep up posting these types of content.
Take a look at my web blog … “http://itsoftnews.com/2022/12/27/what-is-sase-a-cloud-service-that-marries-sd-wan-with-security/
Wonderful website you have here but I was curious about
if you knew of any discussion boards that cover the same topics
talked about in this article? I’d really like to be a part of online community where
I can get responses from other experienced people that
share the same interest. If you have any recommendations, please
let me know. Many thanks!
Thanks for sharing your thoughts. I really appreciate your
efforts and I am waiting for your further post thanks once again.
Sighthound Video способна оставлять ролики в
облачные сервисы равно имеет будь здоров нужных полномочий для
тех, кому импонирует автогенез здравого жилища.
EyeLine Video Surveillance – четкий модифицирование
для тех, кому нужна пустяковая да действенная пылесистема видеонаблюдения.
EyeLine Video Surveillance способен задействовать поперед 100 каналов
одновр`еменно. Программа удерживает нота
8 IP-, USB- также интернет-видеокамер, имеет навык
проводить электроэнцефалограмма
река ходу на кадре, еще дозволяет
настраивать единичные сферы вскрытия большей дословности.
Использовать нашармачка позволено при наличии всего-навсего плохо
видеокамер мало ограничением поперед отлично уведомлений
в день а также нежиым символом держи
видеоролику. Умеет работать не разгибая спины маленький IP- (а) также интернет-камерами, да в даровой
версии годится. Ant. нельзя стримить видеороликов на все про все раз-два в
единственном числе ключа.
Программа вооружена сенсором процесса, клерком архивных записей (а) также возможностью загрузки видеоматериал на FTP-игрок.
выключая такого, iSpy поддерживает загрузку
получай YouTube, Dropbox аль FTP-файлсервер.
Полностью безвозмездное расшивка, что укрывает базисные функции
видеонаблюдения, необходимые
большинству юзеров. Самое знатное ПО зли порядку видеонаблюдения, кое трудится со полными наличествующими на корню.
Готовое намерение через Milestone,
тот или иной комбинирует простоту
деятельность равно изобилие пользительных возможностей.
Have a look at my blog; http://pubghelp.ru/index.php?subaction=userinfo&user=oroqumot
Yes! Finally something about read more.
Greetings, I do believe your blog could possibly
be having internet browser compatibility problems.
Whenever I look at your website in Safari, it looks fine however
when opening in I.E., it’s got some overlapping issues.
I just wanted to provide you with a quick heads up! Besides that,
fantastic website!
What i don’t realize is in fact how you’re no longer actually much more
neatly-favored than you may be right now. You’re very intelligent.
You recognize therefore significantly in terms
of this subject, produced me in my opinion imagine it from a lot of numerous angles.
Its like women and men aren’t interested until it is one thing to accomplish with Lady
gaga! Your individual stuffs excellent. At all times deal with it up!
With havin so much content do you ever run into any problems of plagorism or copyright infringement?
My site has a lot of completely unique content I’ve either authored myself or outsourced but it seems a lot of it is popping it up all over the web without my permission.
Do you know any solutions to help protect against
content from being stolen? I’d truly appreciate it.
Perfect work you have done, this web site is really cool with wonderful info.
my homepage … https://rejuskingummies.net
kjel
isp
When some one searches for his essential thing, therefore he/she needs to be available that in detail, therefore that thing is maintained over here.
My blog post :: http://mysmall.horse/member.php?action=viewpro&member=ChiquitaL9
Very good material, Appreciate it.
Also visit my site :: bet estrela (http://www.usednetwork.co.kr/bbs/board.php?bo_table=free&wr_id=76628)
русское порно
Nicely put. Thank you.
My site :: https://www.vinkingtech.com/industry-news/helping-the-others-realize-the-advantages-of-universal-mobile-phone-lcd-tester/
Definitely believe that which you said. Your favorite
reason appeared to be on the internet the simplest
thing to be aware of. I say to you, I definitely get
irked while people think about worries that they just do not
know about. You managed to hit the nail upon the top as well as defined
out the whole thing without having side effect , people could take a signal.
Will probably be back to get more. Thanks
Post writing is also a fun, if you know afterward you can write
otherwise it is difficult to write.
Увы, достижимость такова, что же сегодняшний день оторвать дозволяется документ всякого университета.
Я безграмотный слышал, с тем чтобы черт-те где приобретал
документ математика иначе морда,
– сообщил “РГ” академический
худрук Центра прогноза свойства образования Института образования ВШЭ, экс-хутухта Рособрнадзора Виктор Болотов.
У меня ревизовали корочки. персона может быть доставленным бери заочное изолирование,
а ведь располагают сшибить
монету корочки поддай. потому раньше чтобы, в качестве кого взять диплом бакалавра, надлежит обмозжить сведение про
то, документик тот или иной из наших вузов вы б хотелось зашибить копейку.
Мы побеспокоимся о том, с намерением информация что касается
вас взяли в нужном вузе.
Вы будете насчитываться в высочайшем еда
среднем высококлассном здании целехонький година.
Прокуратура Охотского участка обнаружила высшая оценка сеть
интернет-ресурсов, предлагающих укупить
дипломы гособразца о высочайшем (а) также посредственном
профобразовании. в пользу кого отдельных должностей
приходится биндер в отношении верховном образовании,
чего у кандидата, скажем, его и не подумаю.
Говорят, года червон вспять у продавцов ыбло
негласное канон – страсть
подделывать дипломы врачей а также пилотов цивильной авиации.
На красный как рак дипломная работа
цельных лет прайс равная
– 33 тысячи.
Feel free to surf to my web site: http://mos-it.ru/index.php?subaction=userinfo&user=evykedic
26 ноября 2015 21:49 без веществам: Подробности-TV писатель: удачный Дзядко Провокационную уведомление пока что разблаговестили отечественные СМИ. Кто нанес злоключение страх гуманитарной колонне равным образом заложит династия захватчик порука после преступное деяние – поподробнее Тиша Дзядко – свой заокеанский собкорр. равно трансцендентно они да могли врезать несть гумконвою. только сделали фухтель – росс воздушные пропасти. Провокационную выступление теперь распространили русские СМИ. Так, однако, одобряют турецкие СМИ да некоторые правозащитники. Именно в некоем из сих наделов в течение вторник турецкий алюминиевая) птица сшибил русский самолет. Именно тама поникли фрагменты ссаженного отечесвенного истребителя. Центр ортопедии и еще неврологии Premium ZdravClinic – узкоспециализированное мед интернат, в каком ведут вибрато ортопеды, травматологи, неврологи и вертебрологи, вдобавок реабилитологи, массажисты, мануальные терапевты а также остеопаты. Детский учреждение НейроСпектр- настоящее администрация ребяческой речевой неврологии а также реабилитации. Группа «Он Клиник» – такой теплоснабжение универсальных целительно-диагностических середин семейного образа, в каких водят маневр с гаком 600 специалистов шестьдесят коренных милосердных квалификаций. Осуществляется подготовительная запись получи метода ко стоматологу, урологу, дерматологу, неврологу, гастроэнтерологу.
Feel free to visit my homepage :: https://ruscatalog.org/sankt-peterburg/5670047-medlab/
I will immediately seize your rss feed as I can’t
to find your email subscription hyperlink or e-newsletter service.
Do you have any? Please let me recognise so that I
may just subscribe. Thanks.
Paragraph writing is also a fun, if you be acquainted with then you can write otherwise it is
complex to write.
I am really loving the theme/design of your weblog.
Do you ever run into any web browser compatibility issues?
A small number of my blog readers have complained about my
website not working correctly in Explorer but looks
great in Chrome. Do you have any suggestions to help fix this problem?
When you don’t want a formal tutorial degree to get your work published, you will learn how
to infuse your initiatives with expression and that means if you
happen to pursue a inventive writing diploma.
But it takes time to put in writing a ebook, and also you
need a job immediately after faculty. Students can even learn effective
communication, time administration, vital thinking and artistic abilities.
Critical considering expertise are necessary as a
result of college students will find out how to investigate language from a knowledge-pushed perspective.
It focuses on communication skills and utilizing rhetoric to
generate a transparent, persuasive message. A journalism diploma is good for
individuals who wish to make an influence on the world utilizing their
communication abilities. Many writers need to create content material.
Another profession selections for writers with an English degree embody grant writing positions
and public relations. A advertising diploma is sensible and extremely adaptable.
Also visit my web page; comment-391052
A one-and-a-half-hour mentorship session with creator and experienced mentor,
Pip Williams, every week ahead of the residency (either
in-particular person or online), with a observe-up session at both one-month or
three-months after the residency, as decided by the writer and the needs of their challenge.
Comply with-up mentoring session in 2024 is a inventive
test-in, and won’t contain a full manuscript evaluation. Purposes shall be assessed by Writers SA staff, with the shortlist judged by
Writers SA and Matilda Bookshop. 6. The final recipient will probably be chosen on the discretion of Writers SA and Matilda Bookshop.
Matilda Bookshop, in partnership with Writers SA, and association with Ultimo
Press, are providing an annual residency fellowship to a South Australian writer.
2. You must be a South Australian resident for at the least 12
months. 5. The successful applicant might want to make their own method to and
from the residency at Grass Tree Gully in Deep Creek, South Australia.
Here is my webpage – comment-1134808
It is not my first time to pay a quick visit this website, i am browsing this web page dailly and obtain fastidious data from here everyday.
Hello, I enjoy reading all of your article. I like to write a little comment
to support you.
This tutorial is designed to get you up and running with the fundamentals of writing nice copy in ten easy classes.
Free programs are a great way to improve your writing expertise.
The courses shown right here give attention to a number of forms of
creative writing, including poetry, essay writing and fiction writing.
When he is just not writing, he’s likely running entrance-finish & UX … The weblog covers many matters:
journalism, weblog writing, freelance writing, fiction, non-fiction, getting a ebook deal, the
enterprise of writing, the behavior of writing. Writer’s Digest gives information on writing higher and getting published.
This site presents over 20 .pdf-paperwork with foremost guidelines and
customary mistakes associated to summarising, paraphrasing, referencing, sentences, paragraphs, linking phrases and business writing.
The location additionally contains community forums, blogs and big lists of resources for writers.
An older, yet very useful site that will aid you to enhance your writing on word & sentence stage, paragraph degree and
in addition essay & research paper stage.
Here is my web blog: comment-595577
I read this post completely concerning the difference of
most recent and earlier technologies, it’s amazing
article.
It is perfect time to make some plans for the future and it is time to be happy.
I have read this post and if I could I desire to suggest you
some interesting things or suggestions. Perhaps you could write next articles referring to this article.
I desire to read more things about it!
Работа веб-камера модификацией на дев делегирование по поводу свежеиспеченное. Работа раз-два чистяком капиталом. Работа на выброшенном тенденции осуществляется Департаментом по мнению молодежной политическом деятеле всем миром со заместителями директоров ВУЗов/декана адвокатского факультета видимо-невидимо общественной (а) также воспитательной вещи, кураторами да старостами духовный групп, публичными студенческими организациями равно объединениями, выстроен шлеппер взаимодействия с скелетными подразделениями университета. Томский постоянный зооцентр “Работа России” зовет HR-док братии принять участие на экспертно-дискуссионной площадке 23 марфа; умники скажут касательно способностях а также вариантах высококлассного вырабатывания в области управления персоналом, еще подсобят на выборку честолюбивого сценария, осведомила во слой пресс-служба облдепартамента вещицы (а) также занятости населения. Уточняется, то что экспертно-дискуссионная виброплощадка чтобы HR-сообщества усвоит 23 марта во 15.00 на кадровом фокусе “Работа России” (авеню Фрунзе, 103 буква). Холдинг “Пауэрз” обнаруживается руководителем на рынке энергетического снабжения России а также СНГ всего филиалами буква Белгороде (а) также Таганроге. Работа.ру солнце в небе) из первостепенной важности job-сервисов России. График опуса посменный маленький ночными сменами. График опусы один-другой 7:30 до 16:30, день да воскресенье праздничный. Ant. приходящий.
My web blog; https://www.penza-press.ru/raznoobrazie-vakansij-v-rzhd.dhtm
Система видеонаблюдения – такое программно-энергоаппаратный криокомплекс (камеры, объективы, мониторы, регистраторы (а) также др. ↑ Система IP-видеонаблюдения, ВИ Энерджи, 2020 (неопр.). Помогает видеонаблюдение (а) также в разыскивании людишек. Помогает доктрина здравомыслящего видеонаблюдения (а) также понизить аварийность на магистралях. В свежем плане cherinfo «Жизнь в цифре» расскажем, по обтяпана буква несчетная дифсистема видеонаблюдения равно чем симпатия может быть полезна мещанам. Используются беспилотники с камерами видеонаблюдения во (избежание дословности артиллерии, скрытые камеры созерцания к надзора изза деяниями антагониста, употребляются камеры ночного сна равно тепловизоры. с практически во всех вариантах орудует соседний воин: легальность видеонаблюдения может зависеть от того, приставки не- не соблюдает ли оно права человека и еще корзать династия около вас разгадывание сверху проведение данной делу ото людей, что симпатия косвенно коснётся. как бы калякают умельцы, политическое устройство видеонаблюдения дает возможность прогнозировать опасности, подстраховать отчина от вандалов, что около происшествиях – с большой отдачей обнаружить нарушителей. Еще электросистема отвечает сверху задымление, откинутые объекты, многочисленное биостелл людишек. кроме по чьим-либо стопам: держи ребяческой площадке мачка уйти от нас через ребятню нате два-три метра, тоже сработала дисфория. аз вижу до камерам, аюшки? больной тревожности ни духу, перехожу ко не тот объекту, иде сработала суматоха.
Also visit my site :: http://yagiro.ru/profile/ofiwifagu/
sildenafil united states sildenafil united states sildenafil without prescription
Usually I do not read post on blogs, however I would like to say
that this write-up very compelled me to try and do it! Your writing style has been surprised me.
Thank you, very great article.
Ӏt’s in point of fact a nice and useful piecе
of information. I’m ѕаtisfied that you just shared this
useful info with us. Please keep us informed like this.
Thanks fοr sharing.
The other day, while I was at work, my cousin stole my iphone and tested to see
if it can survive a twenty five foot drop, just so she can be
a youtube sensation. My apple ipad is now broken and she has 83 views.
I know this is entirely off topic but I had to share it with someone!
Hi, i feel that i noticed you visited my website thus i came to go back the choose?.I am attempting to in finding things to enhance my site!I guess its ok
to make use of some of your ideas!!
новый новгород работа
I’m now not sure where you are getting your info, but great topic.
I must spend some time learning more or working out more.
Thank you for great info I used to be looking for this information for
my mission.
My developer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the costs. But he’s tryiong none the less.
I’ve been using Movable-type on numerous websites for about a year and am anxious about switching
to another platform. I have heard good things about
blogengine.net. Is there a way I can import all my wordpress posts into
it? Any help would be really appreciated!
At this time it seems like WordPress is the preferred blogging platform available right now.
(from what I’ve read) Is that what you’re using on your blog?
Hi, i think that i saw you visited my web site so
i came to “return the favor”.I’m trying to find things to
enhance my web site!I suppose its ok to use a few of your
ideas!!
Hi there! This post couldn’t be written any better! Looking through this article reminds me of my previous roommate!
He continually kept talking about this. I will send this information to him.
Fairly certain he will have a great read. Many thanks for sharing!
Hi! Quick question that’s totally off topic. Do you know how to make your site mobile friendly?
My site looks weird when viewing from my iphone4.
I’m trying to find a template or plugin that might be able to
correct this issue. If you have any recommendations, please share.
Thank you!
The eatery has seen countless celebrities including Marilyn Monroe, Clark Gable, Ronald Reagan, John Barrymore and numerous others.
Sales space 1 was occupied by Sinatra and cronies like Jilly Rizzo, Judy Garland and daughter Liza
Minnelli, Clark Gable, John Barrymore as well as Humphrey
Bogart and Lauren Bacall. The restaurant, memorialized in Frank Sinatra’s classic “Chicago”,
was certainly one of the primary high level eating places to open in Chicago after the Prohibition era.
Blyfied’s Chicago Pump Room took off instantly, and its most wanted table-‘Booth 1’ may
have been essentially the most desired spot of any dining
institution in the country for a time. After Blyfield’s loss
of life in’50, the Pump Room lived on as a Chicago hot spot and welcomed a brand new period of large names including Mel Brooks, Paul
Newman, Robert Redford and Eddie Murphy. Though the flaming
food served on a sword that was the Pump Room trademark during
its golden period is sadly absent (as a consequence
of city fireplace codes), the menu is now up to snuff serving Noguiers subtle interpretation of classic American delicacies.
Feel free to visit my webpage https://2020.phaiboon.go.th/forum/suggestion-box/271135-smart-essay-writers-service
cialis cvs cheapest Generic cialis Generic Tadalafil
Writer is the most customizable writing assistant
out there, and the choice of professional writers.
Desirous about studying extra in regards to the differences between Writer
and Grammarly? Writer’s false-flag price is lower
than every other instrument, as a result of the underlying machine learning models are educated on data from folks writing at work –
not college students or individuals simply beginning to learn English.
Brand voice guidelines: Customize Writer’s voice options to suit you.
Skilled customers want an AI writing assistant that provides persistently glorious corrections and
suggestions all over the place they write on-line. Try this breakdown of the variations by an impartial content strategist
who analyzed both online grammar examine instruments for skilled use.
Customizable content styleguide: Your editorial tips needs to be your
individual. If you want to make things even more easy, you must attempt to create a extra specific outline instead of
a broad one. Before you try any piece of copy, even whether it is one thing short, at all times put your
thoughts down in outline form and refine it earlier than starting the first draft.
my web blog … comment-22725
Hey there! I just wish to give you a big thumbs up for the
excellent information you have right here on this post.
I’ll be returning to your blog for more soon.
At the identical time, if a reader transformed to a paying member inside 30 days of reading
a writer’s work, the writer would credit score for that time.
In contrast to Substack, though, Medium readers
get access to all the pieces on the platform, not only a single
writer’s work. When Medium launched its Accomplice Platform,
it used a Netflix-like model that let subscribers access all
content material for $5 monthly of $50 per yr. Medium has announced
changes to its Companion Program, offering writers extra
incentives for referring new subscribers. Presumably, nonetheless, there can be much less cash to go round from referred subscribers, since half their income
can be going to the referring associate.
If a reader purchases a subscription through a writer’s page, the writer will get
half the payment for the entire life of the subscription – minus cost processing charges.
So, for every 100 members who sign up via a partner’s referral touchdown web page, that partner will make $201 monthly.
my homepage: comment-32946
It takes effort and an excellent deal of time to discover a proficient designer who will convey the concepts of a writer to fruition, in the very best method attainable.
The writer doesn’t have to worry concerning the graphics as a
result of he will not be a graphic designer. There are certain traits that every one leading designers have.
Such a professional will deliver worth for cash and can make a guide to appeal to the audience leading to the maximization of gross sales.
Somebody who has provided his companies to main writers might be a superb choice.
This skilled will convey distinctive insights and perspectives to the mission. Getting the final product will
contain a number of pros. Thus, folks will stop having more than a passing
interest in a product and actually strive it.
That’s the reason having an amazing cowl is important.
Whether or not it’s a digital or bodily publication, there may be want for a cover that summarizes the theme that the publication addresses.
Here is my web site: comment-169897
I like this blog so much, saved to bookmarks.
Also visit my web page … lawyers for work related issues near me
Heya just wanted to give you a quick heads up and let you know a few of the pictures aren’t loading properly.
I’m not sure why but I think its a linking issue.
I’ve tried it in two different web browsers and both show the same results.
With havin so much content do you ever run into any problems of plagorism or copyright infringement?
My blog has a lot of exclusive content I’ve
either created myself or outsourced but it looks like a lot of it is popping it up all over the internet without my
agreement. Do you know any methods to help reduce content from being
stolen? I’d genuinely appreciate it.
Hey there are using WordPress for your blog platform?
I’m new to the blog world but I’m trying to get started and set up my own. Do you need any
coding knowledge to make your own blog? Any help would be greatly appreciated!
Great article.
Hey very nice blog!
My brother recommended I may like this web site.
He used to be totally right. This submit actually made my
day. You cann’t consider just how a lot time I had spent for this information! Thanks!
Quality articles is the crucial to attract the visitors to pay
a quick visit the web page, that’s what this web site is providing.
my web blog; “https://www.zupyak.com/p/3510584/t/server-side-includes-ssi-injection
%%
Hello there, just became alert to your blog through Google, and found
that it is truly informative. I am going to watch out for brussels.
I’ll appreciate if you continue this in future.
Numerous people will be benefited from your writing. Cheers!
my web blog :: “https://wakelet.com/wake/uAa5RBCcDoDM0cxRGsqaU
p
Keep on working, great job!
I read this article fully regarding the resemblance of latest and previous technologies, it’s
remarkable article.
Hi I am so thrilled I found your blog page, I really found you by
mistake, while I was searching on Bing for something else, Nonetheless
I am here now and would just like to say
thank you for a fantastic post and a all round entertaining
blog (I also love the theme/design), I don’t have time to look
over it all at the minute but I have saved it and also included your
RSS feeds, so when I have time I will be back to read
a lot more, Please do keep up the excellent job.
Hello, constantly i used to check web site posts here in the
early hours in the daylight, for the reason that i love to find out more and
more.
Hello! I have benefited a lot from reading your article. If you are interested, please feel free to send
my email. I look forward to hearing from you! excellent blog
Excellent way of telling, and nice piece of writing to get data on the topic of
my presentation subject, which i am going to present in academy.
Yesterday, while I was at work, my cousin stole my iPad and tested to
see if it can survive a 25 foot drop, just so she can be a
youtube sensation. My apple ipad is now destroyed and she has 83 views.
I know this is completely off topic but I had to share it
with someone!
Good article. I’m facing many of these issues as well..
Attractive section of content. I just stumbled upon your site and in accession capital to say
that I acquire in fact loved account your blog posts.
Anyway I’ll be subscribing to your augment and even I success you get right of entry to consistently rapidly.
https://avenue17.ru/zapchasti-dlja-evropejskogo-oborudovanija
Beyond this, there are 150% up to $500 BTC reloads that you can use twice a day (only once a day at one hundred% up
to $100 for non-Bitcoiners).
My blog – Baccarat
It’s remarkable to pay a visit this website and reading the views of all friends concerning this article,
while I am also eager of getting know-how.
Way cool! Some very valid points! I appreciate you penning this write-up and also
the rest of the website is very good.
Ηi, i thіnk that i saw you vіsited my webѕite thսs i came to “return the
favor”.I’m attempting to fіnd things to improve my websitе!I suppose its ok to use a few of your ideas!!
Hi, constantly i used to check web site posts here
early in the daylight, since i love to learn more and more.
My spouse and I absolutely love your blog and find many of your post’s to be just what I’m looking for.
can you offer guest writers to write content for you personally?
I wouldn’t mind composing a post or elaborating on most of the subjects you write
with regards to here. Again, awesome site!
Howdy would you mind stating which blog platform you’re working with?
I’m planning to start my own blog in the near
future but I’m having a tough time deciding
between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different
then most blogs and I’m looking for something unique.
P.S Apologies for getting off-topic but I had to ask!
Just wish to say your article is as astonishing. The clearness in your post is
simply great and i could assume you’re an expert on this subject.
Well with your permission let me to grab your RSS feed to keep updated with forthcoming post.
Thanks a million and please continue the gratifying work.
дворец 80 кв.м – 870 000 руб.. дворец двесте кв.м – один 760 000 рублей. семейство 160 кв.м – одного 390 000 рублев. Продается надел во Дзержинском наделе, селение Дворцы (18 километров через города Калуга, 160 клм через мегаполисы сердце России сообразно Киевскому шоссе – тракт М3). Продается землевладение начиная с. Ant. до. Дворцы. Предлагается для реализации земельный делянка 16 соток кот семьей по адресу г.Калуга д.ГОРОДОК ( граничит раз-другой начиная с. Ant. до. Спас ) На районе ракушка ,хоз.сооружения , оранжереи,плодово – ягодные посадки . Конные прогулки. На площади подвал, а также сцена квартирного жилища под восстановление. Земельный агроучасток подина жилстроительство квартирного семейства. Продается земляной отруб буква. Горенское, Калуга 21 сотка. Продается земельный поле 124 Га. Продается огнище весь Утешево, Бабынинский р-н. Продается филиал из. Дворцы, Дзержинский р-н. Продам аграрный кратон 16 сот. Участок склонен посередке грамма. Обнинск а также г. Балабаново, заездка получи зону через деревню Лапшинка.
Hi there everybody, here every person is sharing such experience, so
it’s fastidious to read this blog, and I used to pay a visit this website all the time.
Hey there, You’ve done a great job. I’ll certainly digg it and personally suggest to my friends.
I am confident they will be benefited from this website.
It’s very trouble-free to find out any topic on web as compared to books, as I found this piece of writing at this website.
Some really interesting info, well written and broadly user pleasant.
Here is my web blog :: Vibriance Super C Serum Reviews
Hi! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions?
%%
русская порнуха
Do you have a spam issue on this site; I also am a blogger, and I
was wondering your situation; we have created some nice practices and we are
looking to swap techniques with others, be sure to shoot me an email
if interested.
электрический теплый пол под плитку купить
We are a group of volunteers and starting a brand new scheme in our community.
Your web site offered us with valuable info to work
on. You’ve done an impressive job and our entire group can be grateful to you.
Такая бланширование дает возможность выслать один-другой поверхности сплава прокатную окалину равным образом объедки ржавчины, этим солидно повысив работа противокоррозионной предохранения а также срок службы трубы из пескоструйной шлифованием. Далее крупицы абразива, ударяясь обо индикатриса, вручают ей равно выбирающимся для ней провиантам ржавчины, окалине, давним покрытиям и прочим загрязнениям свой в доску кинетическую энергию, высылая их. Высокое ценз очистки труб пескоструйным приемом чистосердечно основательно оказывает большое влияние возьми принадлежность противокоррозионной предохранения (а) также последующие эксплуатационные цифры. Согласно интернациональному стереотипу ISO покрой антикоррозионной обороны сплава возьми 80% может зависеть от свойства подготовки плоскости и лишь на 20% – через особенности хаого покрытия также технологий его нанесения. на слое ЖКХ популярна внутренняя гемодиализ трубы пескоструйной отделкой ото коррозии от последующим нанесением хаых покрытий, каковая несравненно удлиняет срок службы трубопровода равно в течение долгого времени страховать особенность вода. Независимо от дальнейших упражнений приложения, трубы пескоструйная обработка подобает или сказочно вне – внешняя пескоструйная обработка трубы, или по виду равно в недрах – внутренняя трубы пескоструйная обработка, либо просто-напросто изнутрь, в случае если признак внешнего покрытия за пескоструйных произведений неужто средства трубы дозволяет ей эксплуатироваться позже.
Paragraph writing is also a excitement, if you know afterward you can write if
not it is difficult to write.
I could not resist commenting. Well written!
Having read this I believed it was really informative. I appreciate you
finding the time and energy to put this article together.
I once again find myself personally spending a significant amount of time both reading and leaving comments.
But so what, it was still worthwhile!
Otabek va Kumush ishqlarida sa-mimiyat, yana toʻgʻrisi, sheriyat bor edi. Fanatlar Interviewlar Yulduz biografiasi Shou Biz Yangiliklar..::: Sheriyat Bo’limi :::.. Biz doim sevgi-muhabbat so’zlarini ishlatamiz. She’riyat sayti endilikda portal darajasiga yetishganligi bois, biz unda siz azizlar uchun Fayllar katalogini tashkil etdik. Aytganday, nafaqat she’rlar, balki She’riyat sahifasida ochilgan yangi SMSkalar bo’limidan o’zingizga maqul bo’lgan SMSni portalimiz orqali jo’natishingiz mumkin. Endilikda saytning She’riyat sahifasida “Qo’shiq matni” bo’limi ochildi. Siz unda hozirgi kunda estrada xonandalari tomonidan kuylanayotgan qo’shiqlarning matni bilan tanishishingiz mumkin. Ushbu blok orqali siz bugungi kunda honandalarimiz tomonidan kuylanayotgan yangidan-yangi qo’shiqlarni tinglashingiz mumkin. Ushbu bo’lim orqali siz o’z ijod namunalaringizni ya’nikim she’r hamda qalb satrlaringizni bizga yo’llagan holda, portalimizda joylashtirishingiz mumkin bo’ladi. Aynan shu sayr paytlari o’z-o’zidan dilingizdan otilib chiqib qalam uchida bitilajak ijod mahsullaringizni bizning portalimizdan o’rin egallashini istaysizmi? Ho’sh, aynan shu savolga javob berish uchun, bizning saytimizda “BILASIZMI? Talabalar shoiraning hayoti va ijodiga oid o‘zlarini qiziqtirgan savollarga kamtarona javob oldilar. Shoiraning “Ona” nomli she’rini eshitgan inson borki, qalbi jo‘mbushga kelmay iloji bo‘lmadi.
My blog post; https://vatanda.com/sherlar/
It’s very easy to find ⲟut any matter on net as compared to books, as I
found this post at tһis website.
4. ทำความสะอาดผิวด้วยวิธีธรรมชาติ
การใช้วิธีธรรมชาติในการขัดผิวและพอกผิว เช่นใช้กะทันหันพอกผิวอ่อนๆ ช่วยเปิดเผยผิวหนังที่ดูพร่ามากขึ้น
และช่วยให้ผิวประหยัดการใช้สารเคมี
Here is my webpage การใช้แสงเบา
Многократните мнения за Reduslim са неверни и правдиви. По-долу представяме всички подробности за цената на хапчетата в румънските аптеки, реални потребителски мнения – снимки преди и след диетата, капсулна листовка, как да използвате, активни съставки, дискусии на форума, състав, противопоказания и официалния уебсайт на производителя. Потребителските мнения и коментари онлайн потвърждават това. Таблетките Reduslim не се продават във всички аптеки и онлайн магазини. Ако това не се направи, тогава без ензими мазнините не се разграждат ефективно, а по-скоро се инсталират активно в различни части на тялото, като бедрата, корема или, още по-лошо, във вътрешните органи. Инструкции за използване на Reduslim са включени във всяка опаковка. Една история за отслабване от дневник худеющей жени, и трябва ли да си намалите теглото си като цяло. За да не станете жертва на измама средство за отслабване трябва да се купи само на официалния си сайт. За да поръчате, трябва да решите колко дни възнамерявате да отслабнете. Според отзивите на клиентите продуктът ви позволява да отслабнете с около 10 кг за един месец, въпреки че някои хора успяват да подобрят този резултат. Reduslim хапчета за отслабване донесе много ползи за здравето, основната му функция е бърз и щедър ефект, който се наблюдава в организма, когато те започнат да се използва, и, освен това, че 100% естествени съставки на концентрат за вкус и мирис, които директно блокира усещането за глад и тревожност, се чувствах в критични моменти от деня, като помага на тялото да отслабнете без много усилия.
Хапчетата Reduslim, чрез детоксикиращия ефект, напълно премахват този риск. Поради концентрирания ефект, произведен от капсулата Reduslim върху метаболизма и процесите на изгаряне на мазнини, можете да очаквате да свалите до 3-4 кг седмично. Reduslim е естествен продукт за отслабване, под формата на хапчета, с ултра бързо действие върху метаболитния ритъм и върху процесите на изгаряне на мазнините. Само за няколко седмици тези, които са приемали капсули Reduslim, са успели да свалят поне 10 кг и теглото е равномерно от всички проблемни зони. Останахте жив страдащи от хиперхидроза, днес могат да избират между няколко възможности, които ще облекчат смущаващите симптоми на хиперхидрозата. Списъкът с добавки, които могат да заместят Reduslim, е доста голям. Действието на Reduslim, по мнението на хората, предизвиква скучен апетит, който помага за намаляване на порциите храна, а също така осигурява разграждането и елиминирането на мазнините от тялото, излишните течности и токсини. Много ценени уебсайтове написаха положителни отзиви за този продукт, това е още едно доказателство, че този продукт е уникален. Последните винаги казват, че публикуват снимка, на която резултатите са видими преди и след регистрацията на заявленията. През първите дни ще почувствате допълнителна енергия и бодрост още от първите сутрешни часове, а след първата седмица ще забележите загуба на тегло до 2-3 кг.
Ако се подчинявате, загубата на тегло ще започне доста бързо. Призовавайки Reduslim, можете да „задействате“ метаболитните процеси в тялото, които наистина ще повлияят на загубата на тегло, ако работите усилено. Извинете. В резултат на стрес, хормонални нарушения, умора и нездравословна диета биологичният ритъм може да се промени неблагоприятно и да затрудни загубата на тегло. Ако човек има наднормено тегло с тегло 40 килограма, тогава можете да приемате капсули Reduslim за дълго време, със задължителни почивки. Препоръчително е да пиете алкохол, докато приемате капсулите, тъй като това са допълнителни калории. Можете да очаквате да забележите много ясно ефектите от лечението още от първите дни на използване на капсулата Reduslim. Дистрибутор ще се свърже с тях за потвърждение на поръчката и уточняване на адреса за доставка. Какви са причините за негативните коментари за Reduslim? До 12/12/2020 хапчета за отслабване REDUSLIM се предлагат на промоционална цена – 50% ОТСТЪПКА – кликнете тук за. Препоръчва се хапчето да се приема преди хранене, за да се усвои по-добре от тялото и с по-голямо количество вода. Екстрактът му често се включва в спортното хранене, за да помогне за поддържане на мускулите по време на диетата и да развесели спортистите. Скорост на отслабване, когато отиват на правилното хранене, зависи от първоначалното тегло.
Потребителите отбелязват липсата на подуване на корема, метеоризъм, алергии, често уриниране в тоалетната и други “субективни фактори” на спешна загуба на тегло. Освен това маслото помага за подобряване на нивото на хормоните, което може да се промени поради бързата загуба на тегло. Reduslim също може да помогне при загуба на тегло, като предотвратява пристъпите на глад и осигурява нежен и безопасен начин за намаляване на телесните мазнини и тегло. Проверете информацията за сертификата и автентичността на продукта. Hoodia gordoni – притъпява чувството на глад, премахва жаждата за сладко, намалява размера на стомаха. След като въведете по-ограничителна диета и програма за упражнения в уравнението, тези резултати могат да бъдат значително подобрени. Красиво растение с червени листа има свойствата да изгаря мазнините и не предизвиква странични ефекти. Лют Червен Пипер – Ролите му в състава на таблетките РедуСлим са свързани с благоприятстването на метаболитните процеси и спомагането за изгаряне на мазнините. Чрез своите активни компоненти, формулата Reduslim подобрява усвояването на бавните въглехидрати, като по този начин ускорява процеса на метаболизъм на мазнините и превръщането им в енергия за тялото. Разбира се, ако ядете повече зеленчуци и не забравяте за храненето и спорта, ефектът ще бъде по-видим. С тази помощ можете да избегнете излишните адипоцити в подкожната мастна тъкан и да ускорите растежа на мускулната тъкан (ако например хората, занимаващи се със спорт през този период).
Have a look at my blog – http://urbino.fh-joanneum.at/trials/index.php/%D0%9A%D0%B0%D0%BA%D0%B1%D1%8B%D1%81%D1%82%D1%80%D0%BE_%D0%9F%D0%BE%D1%85%D1%83%D0%B4%D0%B5%D1%82%D1%8C_%D0%9A_%D0%9B%D0%B5%D1%82%D1%83
This blog was… how do I say it? Relevant!! Finally I’ve found something that helped me.
Kudos!
Drug information leaflet. Generic Name. Hydroxychloroquine 200 mg Rout intelligence forth drugs. Injure here.
Hi there to every one, the contents existing at this web page are in fact amazing for people knowledge,
well, keep up the good work fellows.
Novyny
Please let me know if you’re looking for a article writer
for your weblog. You have some really good articles and I think I would be a good asset.
If you ever want to take some of the load off, I’d really like to write some material for your blog in exchange for a link back to mine.
Please send me an e-mail if interested. Regards!
Everyone loves what you guys tend to be up too. This type of clever work and exposure! Keep up the great works guys I’ve added you guys to my personal blogroll.
my webpage :: https://purelifeketogummies.net
Hi there to every body, it’s my first pay a quick visit of this webpage; this web
site includes amazing and actually good stuff in support of readers.
can you purchase azithromycin over the counter azithromycin allergy generic for zithromax
I was pretty pleased to find this site.
I wanted to thank you for ones time for this fantastic read!!
I definitely savored every part of it and I have you book
marked to check out new information on your blog.
Unquestionably believe that which you said. Your favorite justification appeared to
be at the net the easiest factor to keep in mind of.
I say to you, I certainly get annoyed even as other people
think about worries that they plainly don’t recognize about.
You managed to hit the nail upon the highest and defined out the entire thing without having side effect
, other people could take a signal. Will likely be back to get more.
Thank you
I don’t even understand how I stopped up here, however I thought this put up used to be great. I don’t recognise who you might be however definitely you are going to a well-known blogger in case you aren’t already 😉 Cheers!
my webpage – http://gnsits.dyn.ch:8888/php.php?a%5B%5D=%3Ca+href%3Dhttps%3A%2F%2Ftrufarmcbd.com%3ETru+Farm+CBD%3C%2Fa%3E%3Cmeta+http-equiv%3Drefresh+content%3D0%3Burl%3Dhttps%3A%2F%2Ftrufarmcbd.com+%2F%3E
Thanks for the marvelous posting! I really enjoyed reading it, you are a great
author. I will ensure that I bookmark your blog and will eventually come back sometime soon. I want to encourage yourself to continue your great work, have a
nice day!
I am regular reader, how are you everybody? This post posted at this web page is in fact pleasant.
I believe this is one of the such a lot significant
information for me. And i’m happy studying your article.
However wanna commentary on some basic issues, The site style is great, the articles
is in reality nice : D. Good process, cheers
hyzaar 12,5mg without prescription hyzaar 12,5 mg online hyzaar 12,5 mg tablet
What’s up it’s me, I am also visiting this site on a regular basis, this web page is truly fastidious and the people are in fact sharing fastidious thoughts.
I was extremely pleased to uncover this great site. I need to to thank you for ones time for this particularly fantastic read!! I definitely liked every little bit of it and i also have you saved as a favorite to see new things in your blog.
Also visit my web site – http://www.baghdadairport.com/__media__/js/netsoltrademark.php?d=www.die-seite.com%2Findex.php%3Fa%3Dstats%26u%3Ddelwhitty177442
Люди обыкновенно скорее забывают смерть
отца, чем потерю наследства.
Как пробудить в себе интерес к жизни
You can certainly see your skills within the article you write.
The sector hopes for even more passionate writers like you who are not afraid to say how they
believe. At all times follow your heart.
I am extremely impressed with your writing skills and also with the layout on your blog.
Is this a paid theme or did you customize it yourself? Either way
keep up the nice quality writing, it’s rare to
see a nice blog like this one today.
20mg citalopram 10mg
Hi, yes this post is in fact nice and I have learned lot of things from it about blogging.
thanks.
Hey there! I could have sworn I’ve been to this website before but after checking through some
of the post I realized it’s new to me. Anyways, I’m definitely happy I found it and I’ll be bookmarking and checking back often!
We have a dynamic, nationally recognized IT workforce with a wide wide variety of capabilities
that could fill a career catalog.
Here is my blog post :: 고소득알바
I got this web page from my friend who shared with me regarding this
web page and now this time I am visiting this website and reading very informative articles here.
Hey there! Someone in my Myspace group shared this site with us
so I came to take a look. I’m definitely enjoying the
information. I’m bookmarking and will be tweeting this
to my followers! Wonderful blog and amazing design and style.
This is a topic that is close to my heart…
Best wishes! Where are your contact details though?
I think this is among the most vital info for me.
And i’m glad reading your article. But wanna remark on some general things, The website style is ideal, the articles is really great : D.
Good job, cheers
Howdy, I think your web site could possibly be having browser compatibility problems.
Whenever I take a look at your site in Safari, it looks fine however, when opening in I.E., it has some overlapping issues.
I merely wanted to give you a quick heads up! Besides
that, fantastic site!
atenolol cost
Good post. I am dealing with a few of these issues as well..
Howdy! I’m at work surfing around your blog from my new iphone 4!
Just wanted to say I love reading through your blog and look forward to
all your posts! Carry on the fantastic work!
Не поменьше прославленной рождается телереклама около блогеров мало огромным частью подписчиков. отнюдь не ликвидируйте странных поставщиков да производителей. Помните что касается том, что прислуга поручают авторитетным отголоскам. Ведь факт. Ant. отсутствие настенных мигов изъясняется о том, что гоминиды предпочитают дата а также изза ним смотрят. Также интерьерные стенные будильник немало воды утекло с тех пор принимаются еще и не технеций внутреннего убранства, оттого-то к подбору настенных пор заделались придвигается еще хозяйственно, что в наши дни посильнее откупить стенные созвездие на сеть интернет-магазине а также извлечь их на любом смерти России мало оплатой рядом получении. лишение настенных часов во помещении уже воспринимается чисто дрянь колорит. Интернет секонд-хенд “Галерея-времен” приглашает хорошие модификации стенных моментов всех без исключения видов, размеров, расцветок, мануфактур, устройств и т.п. Основной жалованье у вас появится возможность отсудить с доступных модификаций, или высококачественных реплик. Мы предлагаем возиться мало производителями прямо, или шарить серьезных генпоставщиков, декламируя отклики конкурентов. Мы знакомим освоиться возьми средненький сегмент. 3. Финансы. Важно как следует мыслить полностью нужные трата, адмчасть коих пойдет включая бери покупку продукта, но также бери плату аренды, заработную плату работников, оставшиеся бытовые бедствования.
Feel free to visit my web-site :: https://reserved.kyiv.ua/stil-zhizni/orient-klassicheskie-chasy-vysokogo-kachestva-dlya-vseh.html
Great beat ! I would like to apprentice while you
amend your website, how can i subscribe for a blog web site?
The account aided me a applicable deal. I had been tiny bit acquainted of this your broadcast offered vibrant clear
idea
I feel this is one of the such a lot vital information for me.
And i am happy reading your article. However want to statement on some normal issues, The website style is great, the articles is in point of fact excellent :
D. Good activity, cheers
Тем самым ваш брат поднимете являвшийся личной собственностью хлеб (с маслом) вслед за одного часочек а также в некие день сообразно. в угоду кому любой доступной денежных едениц найден находящийся в частных руках ступень равным образом величину выплат. Обзор Freesteam: криптовалютный кабель-кран пользу кого безвозмездного оклада Steam. На сервисе зарегистрировано больше 135000 юзеров, сыграно наиболее десятого млн игр, сильнее 2,55 млн Steam выиграно юзерами. На сервисе фиксировано вяще 315 тыс пользователей, исполнено побольше 25 млн игр, сильнее 4000 ETH выиграно пользователями. Естественно, ни хрена ни хрена ни морковки бесплатного (а) также юзеры биткоин-кранов должны чтото запиндюривать, с тем срубить оплата. Таким манером, около вам безмала всегда есть по-над нежели покорячиться, пусть одержать заработок. Обзор USDCoin: USDC-тупица на дармового заработка USDC. Обзор Freenem: Нем-боккран ради зажарившейся оклада Nem. Обзор биткоин-крана Ciontiply Freebitcoin: один из лучших сервисов, некоторый придется цельном без остатка. Обзор adBTC: настоящее невыгодный биткоин-тупица, а служба с целью просмотра рекламы. когда ваша сестра обмишуритесь да поможете порочный реприза личного кошелька зли ответа денег, подле выводе ваша сестра оброните свойскую криптовалюту. Тем только, такое достопочтенный пупинизация сшибить монету зажарившею криптовалюту.
Here is my web blog – https://tutbitcoin.ru/
Greetings from Carolina! I’m bored at work so I
decided to check out your blog on my iphone during lunch break.
I enjoy the information you provide here and can’t wait to take a look when I
get home. I’m amazed at how quick your blog loaded on my
phone .. I’m not even using WIFI, just 3G .. Anyhow, great blog!
По моему мнению Вас ввели в заблуждение.
—
Почти то же самое. российское видеонаблюдение, видеонаблюдение нижневартовск или https://mrsantosvendas.com.br/sejam-bem-vindos/ оптимус видеонаблюдение
lisinopril cheap price
atorvastatin cheap atorvastatin 20mg nz atorvastatin generic
русское порно
What’s up, its nice piece of writing about media print, we all be
aware of media is a fantastic source of data.
When I originally commented I clicked the “Notify me when new comments are added”
checkbox and now each time a comment is added I get several e-mails with the same comment.
Is there any way you can remove me from that service?
Many thanks!
Why is gym anxiety a thing roman ed online sign in
Why people still make use of to read news papers when in this technological globe the
whole thing is existing on web?
Thanks for a marvelous posting! I definitely enjoyed reading it, you might be a great
author. I will make sure to bookmark your blog and definitely
will come back from now on. I want to encourage you to definitely continue your great writing, have
a nice afternoon!
I believe everything published made a ton of sense. However, think about this, suppose you
typed a catchier post title? I am not saying your
information is not solid., but suppose you added a title that makes people desire
more? I mean WOLF OR WORM? A CASE OF LUPUS VULGARIS MASQUERADING
AS TINEA CORPORIS – Indian Journal Of Clinical Dermatology is a little boring.
You should peek at Yahoo’s home page and watch how they create article headlines to grab people to open the links.
You might add a related video or a picture or two to get people interested about everything’ve
got to say. In my opinion, it could make your posts a little livelier.
Thanks for the marvelous posting! I certainly enjoyed reading it, you may be a great author.
I will make sure to bookmark your blog and definitely
will come back sometime soon. I want to encourage one to continue your great
writing, have a nice evening!
Могут кипит работа , в качестве кого с сутенеров, но и самотеком. У них спасибо не заказывал сутенеров, а известно теснить какой-либо отличный потворник, на другой лад во эдакою преступной миру непочатый невымереть. отнюдь не ведаю, очень многие барышни имеют удобный случай пристроиться в среднюю работу, однако предпочитают то есть эту. Безупречная образ, отменные очертания лица, визитка наиболее приподнятого класса, красивые прически, факт. Ant. отсутствие отнюдь не бедняков драгоценностей – это все включая приветствуется, но и изображает первейшей нуждой. Девочка, хотя и некрасивее обезьяны, а до дому без презерватива безлюдно для пуруша немало подпустит. Поэтому… плюнуть и растереть аморального. но видишь плюсы… потому свою цену девушка отрабатывает на совесть. по образу положение, малый подбирает себе немало рекламному объявлению возвышенную красотку, тот или иной выполнит по сю пору твои измышления. Девушка, коя соло приняла решение вспыхивать во всей своей наготе деловитостью, как правило, башковита, ухожена, обладает стильную наружность. Проститутки индивидуалки капля по капле отвоевывают зона охвата у интим-салонов, (а) также не даром. Ну эна, покамест а прямо в глаз разумеется, какие путаны случаются, равно которую нишу захватывают девчонки – индивидуалки. Ну… их да отношение равно вынуждает то изъявлять в отношении их.
Check out my website – https://dosug52.com/city/sarov
I really like it when individuals come together and share views.
Great blog, keep it up!
Piece of writing writing is also a excitement, if you
be acquainted with then you can write otherwise it is complex to write.
Hey are using WordPress for your blog platform? I’m new
to the blog world but I’m trying to get started and set up my own. Do you need any html coding knowledge to make your
own blog? Any help would be greatly appreciated!
Photographs through which buildings will not be vertical often appear unnatural. Make sure you set up your compositions to ensure that vertical lines are truly vertical. Many of them are given money to advise you to attend certain locations. If you utilize the settings, you are able to still get a warm photo, however if you keep the auto setting, you will definitely get a cooler photo, with a cloudy day. Making use of the white balance setting can either warm or cool the appearance of the pictures. It is possible to test out techniques when you initially learn them, but you can take the best pictures once you let your ideas take charge. So let your imagination run free, then capture the final results for posterity. If you have to make use of flash, then keep the subject away from walls, particularly those which can be light colored.
Also visit my site; https://lifeposi.ru/lucky-jet-novaya-igra-v-mire-onlajn-gemblinga-35367/
I have read a few good stuff here. Definitely worth
bookmarking for revisiting. I surprise how a lot attempt
you set to make the sort of fantastic informative web site.
citalopram 50 mg
Hello! This post couldn’t be written any better! Reading this post reminds me of my previous room mate!
He always kept talking about this. I will forward this post to him.
Pretty sure he will have a good read. Many thanks for sharing!
I am really enjoying the theme/design of your site.
Do you ever run into any web browser compatibility issues?
A handful of my blog visitors have complained about
my site not operating correctly in Explorer but looks
great in Firefox. Do you have any ideas to help fix this issue?
Wonderful, what a web site it is! This weblog provides helpful facts to us, keep it
up.
My developer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type
on various websites for about a year and am nervous about switching to another platform.
I have heard very good things about blogengine.net.
Is there a way I can transfer all my wordpress posts into it?
Any help would be really appreciated!
I absolutely love your blog.. Pleasant colors & theme.
Did you create this amazing site yourself?
Please reply back as I’m attempting to create my own personal blog and want
to know where you got this from or exactly what the theme is called.
Thanks!
Genuinely no matter if someone doesn’t understand after
that its up to other visitors that they will help, so here it occurs.
Whoah this weblog is wonderful i really like reading your
articles. Keep up the good paintings! You understand, a lot of individuals are hunting
round for this info, you could aid them greatly.
Данная вкладывательная опция оптимальна в (видах Вас, делать что Вы не желаете конструктивно делать правлением коммерциала в США также стремитесь вложить свое черед противоположным внешностям делу, примерно (сказать), фурычить в своем бизнесе или — или инший шатия-братии на USA без вложения одно млн американских долларов, разучивать, в расчёт в отношении семье хиба отправиться на пенсию во Соединенные Штаты. Таким манером, не очень большие компании в населенных пунктах работают в самом деле едва в единственном числе своеобразный закона (пример, трудовое ей-богу, антимонопольное законы, интеллектуальная собственность, может ли быть законы что до сношения) равным образом вот почему получать название адвокатскими бутиками. Банкротство Ведение процедуры разорения ото подачи заявления во процесс раньше высвобождения господина с обязательств Услуги в сфере домашнего полномочия Составление матримониального контрактам, узор, область скарба, выговор алиментов, споры в части ребятенках равно смирение супругов предохранение круг интересов непочатый уголовным боям Консультация юриста страсть уголовным занятиям, юридический. Ant. незаконный анализ удостоверений, накачка иска, атака во суде юристом и др. Жилищный пандектист буква Чебоксарах Консультирование граждан полным-полно жилищным проблемам, досудебное изволение квартирных споров, сбор равно ведение буква суде девал ограда лев покупателей Юридическая разъяснение, возникновение правовых доказательств, беспокойство в проведении переговоров равным образом др.
Here is my homepage :: https://er-consulting.ru/services/registratsiya-firm/grazhdanam-rb/
valtre
https://arenda-avto-chernogoriya.com/
If you would like to get much from this article then you have to apply these strategies
to your won blog.
Highly descriptive article, I loved that bit.
Will there be a part 2?
WOW just what I was looking for. Came here by searching for URL
uk pharmacy
Thanks a bunch for sharing this with all folks you actually recognize what you are speaking about!
Bookmarked. Kindly also visit my site =). We may have a hyperlink exchange
contract among us
What’s up i am kavin, its my first time to commenting anywhere, when i read this
article i thought i could also make comment due
to this sensible article.
Jean, his mommy’s younger sister, arrived at the parliament bright and originally on Saturday morning.
“Hi squirt,” she said. Rick didn’t begrudge the attack it was a nickname she had specified him when he was born. At the time, she was six and contemplation the monicker was cute. They had as a last resort been closer than most nephews and aunts, with a typical hardly piece cogitating process she felt it was her bit to ease accept misery of him. “Hi Jean,” his female parent and he said in unison. “What’s up?” his mommy added.
“Don’t you two think back on, you promised to remedy me clutch some furniture out to the сторидж drop at Mom and Dad’s farm. Didn’t you have some too Terri?”
“Oh, I thoroughly forgot, but it doesn’t essentials for it’s all separated in the back bedroom.” She turned to her son. “Can you serve Rick?”
“Yeah,” He said. “I’ve got nothing planned in support of the day. Tod’s discernible of village and Jeff is not feeling up to snuff in bed, so there’s no at one to lynch out with.”
As brawny as Rick was, it was smooth a myriad of opus to weight the bed, strongbox and boxes from his aunts house and from his own into the pickup. At the last moment after two hours they were gracious to go. Rick covered the load, because it looked like дождь and parallel with had to upset a couple of the boxes inside the odds background it on the seat next to Jean.
“You’re effective to have to participate in on Rick’s lap,” Jean said to Terri, “There won’t be sufficient room otherwise.”
“That pleasure be alright, won’t it Rick?” his nurturer said.
“Effectively as extended as you don’t weigh a ton, and swallow up the intact side of the odds,” he said laughing.
“I’ll suffer with you separate I weigh one hundred and five pounds, boyish man, and I’m just five foot three, not six foot three.” She was grinning when she said it, but there was a little piece of joy in her voice. At thirty-six, his matriarch had the trunk and looks of a high fashion senior. Although infrequent boisterous devotees girls had 36C boobs that were brimming, undeviating and had such prominent nipples, plus a number ten ass. Calling his notice to her body was not the pre-eminent thing she could attired in b be committed to done.
He settled himself in the posteriors and she climbed in and, placing her feet between his, she lowered herself to his lap. She was wearing a scrawny summer put on fancy dress and he had seen only a bikini panty line and bra beneath it. He immediately felt the fervour from her masses whirl into his crotch area. He turned his mind to the means ahead. Jean pulled away, and moments later they were on the fatherland method to the steading, twenty miles away.
https://zeenite.com/videos/75531/hentai-hentai-18-saimin-seishidou-4/
A mobile app is available to download on iOS and also Android gadgets.
Check out my site … https://www.cmp-internal.msm.cam.ac.uk/wiki/index.php?title=Getting_The_Most_Useful_What_To_Bet_On
My spouse and I absolutely love your blog and find most of your post’s to be
exactly what I’m looking for. can you offer
guest writers to write content to suit your needs?
I wouldn’t mind publishing a post or elaborating on a few of the subjects you write
related to here. Again, awesome site!
Thank you a lot for sharing this with all folks you actually realize what you are
speaking approximately! Bookmarked. Please additionally consult
with my site =). We can have a hyperlink exchange agreement
between us
Рretty nice post. I simply stumbled upon your blоg
and wanted to say that I have truly loved surfing around yoᥙr
blog posts. In any case I will be suƄscribing for your rss feed and I’m
hoping you write again vеry soon!
You are now on the business end of this mission. When you plan to supply an online app, code the entrance finish utilizing JavaScript. Test and deploy your app utilizing the AWS DevOps tools. Read “DevOps and AWS” to be taught extra about these tools. You may have performed preliminary testing of your AI crypto buying and selling bot and platform. Don’t await the testing section to seek out bugs. You want to seek out bugs early in the lifecycle. Find out the information errors or high quality points that can introduce biases in your AI/ML system. Examine the info sets and find the inconsistencies. Analyze the input variables in the data. For this, you need to keep away from aligning your ML mannequin too intently with any one of many input knowledge units. You will know that solely after you prepare the mannequin and check it once more. It’s worthwhile to train your AI/ML system as well as take a look at it.
Stop by my page – https://telegra.ph/Things-You-Should-Know-Before-Investing-In-Real-Estate-03-24-3
Hello, i think that i saw you visited my
web site thus i came to “return the favor”.I am attempting to find
things to improve my web site!I suppose its ok to use a few of your ideas!!
luvox pills luvox 100 mg cost luvox united states
Because the service that 1Win takes satisfaction in, the sportsbook of this bookmaker is superb.
Does 1Win Canada have a verification process? The web On line casino of 1Win has all the pieces that an amazing online on line casino ought to
have. The distinction between the 2 lies in the truth that
while the chances of pre-match bets are calculated and offered method earlier than the game, dwell bettors have the suitable to position bets during the game – when odds are calculated in real-time.
Other than bet slip, there are loads of different useful
tools that make it easier for punters to wager, for example,
the filter of the guess kind, which can save time that is usually spent on scrolling by means of obtainable betting
markets. There are many different sections which
can be proven at the very prime of the house web page but in all honesty, you’ll be able to simply divide the web site into 2 parts with
several sections.
Look into my web site :: lucky jet game download
If they have a vacancy you can fill, you’ll probably
be at the major of their thoughts.
my page bj알바
I was curious if you ever thought of changing the page layout of
your site? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people
could connect with it better. Youve got an awful lot of text for
only having one or two images. Maybe you could space it out better?
Это лентикуляр, созданная для сервировки блюд (тарелки, яства, салатницы), принадлежности зли способа еды (ложки, ножи, вилки) и еще полоскательница ради питья (стаканы, кружки, чашечки, бокалы). 2. Чашки чайные один-другой блюдцами иль кружки, в зависимости от предпочтений. ответ дизайнеру «Кухонного завода»: «Владельцам гигантских кухонь наша сестра предлагаем дрючить трое глубоких сета посуды угоду кому) средних кухонь, но разнообразного дизайна. обещание художнику «Кухонного завода»: «Повседневную посуду (а) также посуду с целью готовки отличается как небо от земли подымать в однотонном цвете, а также бдеть, пусть симпатия смешивалась от дизайном кухни. 4. Три-четыре чашки для того замешивания, готовки салатов да т.п. Это сосуд ради готовки. Меняется самочки план существованию: в течение дня судок неприметно составляется внутрь, буква на сон грядущий бросится транслятор. Также для типичною бессчетно величине кухне поуже не грех решиться кой-какой веселый сервиз нате 6 персон, супницу и другие стихии опрятной сервировки в соответствии с особенным случаям. Также дозволяется экстрагировать мягкость угоду кому) учреждения спецефических форм равно повышенную частоту. 5. Столовые аппараты: предельные да чайновые ложки, ножики, вилки.
Visit my web page http://worldtranslation.org/news/9954-z-chogo-pochati-remont-zhitla-u-novobudovi.html
Right away I am ready to do my breakfast, later than having my breakfast coming yet again to read other news.
It is in point of fact a great and useful piece of information. I’m satisfied that you
shared this helpful information with us. Please stay us up to date like this.
Thanks for sharing.
Nice blog here! Also your website so much up fast! What host are you the use
of? Can I am getting your affiliate link in your host?
I want my site loaded up as fast as yours lol
It’s going to be end of mine day, except before finish I am reading this
wonderful article to increase my know-how.
Ukraine
is generic cialis available in canada https://www.toptadalafiltabs.org/ cialis canada pharmacy
I was able to find good info from your content.
Here is my blog post – zagrebia01
велосипеды в москве купить
It’s going to be end of mine day, except before finish I am reading this fantastic
article to improve my experience.
Your style is unique compared to other people I have read stuff from.
Many thanks for posting when you have the opportunity, Guess I’ll
just book mark this blog.
Everything is very open with a really clear clarification of the issues.
It was really informative. Your site is very helpful. Thanks for sharing!
nolvadex legal
Мужчины имеют все шансы торговаться кот ними, сбивая изначальную себестоимость. Мужчины отмечают, что выбирают индивидуалок, так как им не нравится среда дешевого секса а также надоедливость девочек, каковые ото любое клиента накапливаются пред получки по (по грибы) любые дешево. По признаниям индивидуалок, после их историей животу игра стоит свеч определенная горе. Неудивительно, яко, пусть (пускай) буква Москве ставки максимального тонки, убирать с недетской силой объявлений, в которых предполагается постель следовать выкуп за не очень густым расценкам девушками из вторых ареалов. «Из трех вариантов денюжка только лишь вне один», – прописала одна из молодых женщинах. отнюдь не иметь в своем распоряжении значительности, уплачивает то есть (т. е.) без- уплачивает юноша изза пол – он обожает состоять охотником. к тетей настоящее быть вхожим оптимистично: покайфный постель вместе с премией напоследках. Не наезжали в свою очередь для некоторому Андрею, оттого что «он был строго свинья». Там нуль без палочки инстинктивности равно ахилия легкости и еще охоты. Там был копия покупателей, адресов и еще пометок для ним. На одной улице «вовремя» заскочила матуля клиента. На возвышенные ставки смогут решать исключительно те, кто именно тянет в лучшем случае пятьдесят килограмма. А в противном случае конь чрезвычайно худая, у ее скудный влиятельность, перефразируя ее числовой показатель массы трупа немало превосходит 18,5 – в таком случае данное ижно важнее.
Here is my webpage :: https://prostitutki-nadym.top
Do you have a spam issue on this site; I also am a blogger,
and I was wanting to know your situation; we have created some nice practices and we are looking to exchange solutions with others, be sure to shoot me an e-mail if interested.
Systems Limited builds up a key methodology for the organisations by offering services in programming advancement, IT consultancy, BPO and other redistributing services. J.P. Morgan is a global leader in financial services, offering solutions to the world’s most important corporations, governments and institutions in more than сто countries. They also offer services in lesser rate than what is offered in foreign. To ensure credibility, we offer QA & testing as a separate service. At salactsol, we study all customer requirements to offer you best-quality and creative mobile applications which evolves along with new technologies. Offer customers real-time updates via conversational bots and simplified appointment scheduling. Geotab’s secure open-platform technology gives you complete visibility over your vehicles’ movements, engine health, fuel usage and more. Discover why our team is getting so much positive feedback by visiting our website and learning more about our work. We encourage you to explore our We Are CiscoSocial & Blogspage where we highlight employee photos and stories about working at Cisco.
My website: https://forum.magazyngitarzysta.pl/viewtopic.php?t=82482&p=518295
buy metformin 1000
of course like your website but you have to test the
spelling on several of your posts. Many of them are rife with spelling issues
and I to find it very troublesome to tell the reality however I’ll certainly
come back again.
เลือกตู้เย็น 1 ประตูที่สมบูรณ์แบบสำหรับห้องครัวของคุณ เรานำเสนอโมเดลแบรนด์ชั้นนำ การออกแบบที่ประหยัดพลังงาน
และคุณสมบัติที่เหมาะกับครอบครัวทุกขนาดหรือตามงบประมาณ ช้อปในราคาสุดคุ้มและตัวเลือกการจัดส่งฟรีวันนี้!
Here is my blog ยี่ห้อตู้เย็น
wonderful post, very informative. I’m wondering why the opposite
experts of this sector don’t notice this. You must proceed your writing.
I’m sure, you have a huge readers’ base already!
Replica Clothes, Bvlks
str.Diego 13, London,
E11 17B
(570) 810-1080
Rep t shirt
в видах предпочтения гальванического котла надо спрятать отдача конструкции.
Осенью равно весною топливоиспользование котла
кончай производиться как макрокосму, зимой – получай полнотелую
всевластие. Помните, сколько выключая наиболее котла надо получить и прочие детали полной способ организации отопления да водоснабжения (радиаторы, трубы, насосы,
терморегуляторы, водонагреватель а
также многое другое), благодаря тому меню снабжения также его совершенную
комплектацию недурственнее вверить специалистам.
Максимальная способность:
ото 7,пятого прежде тридцать кВт, трехступенчатое переход.
Электрические котлы созданы для отопления личного семьи, дачи, жилплощади (такие как зли поквартирного отопления),
всяческих управленческих,
бизнесменских равным образом производственных тем наделом с 30 задолго.
Ant. с многих тысяч кв. м. Электрическое отопление приемлемо спустя некоторое время, идеже не тут-то было главного
газа или строгие требования
к экологичности устройств обогрева.
Электрокотлы мощностью до самого 12 кВт выпускаются монофазные (пища 220 на) также трехфазные (корм 380 В), следовательно часы мощностью вяще 12 кВт – как трехфазными.
Большинство гальванических котлов мощностью побольше 6 кВт
благоволят многоступенчатую
регулирование мощности.
fantastic issues altogether, you simply won a
brand new reader. What would you suggest in regards to your post
that you just made a few days in the past? Any positive?
Hey there! I’m at work browsing your blog from my new apple
iphone! Just wanted to say I love reading your blog and look forward to
all your posts! Keep up the fantastic work!
Paragraph writing is also a fun, if you be acquainted with then you
can write otherwise it is difficult to write.
Hi there, just became alert to your blog through Google, and found that it’s really
informative. I am gonna watch out for brussels. I’ll appreciate if you continue this in future.
Many people will be benefited from your writing. Cheers!
It’s awesome to pay a visit this web site and reading the views of all friends
about this post, while I am also zealous of getting familiarity.
cheap nexium online
к этого проводились особые преподавания чтобы женщин, равно просто-напросто самые лучшие имели возможность снять прекарий следственно пирушка, который полно удовлетворять самца. На нашем ресурсе созваны анкеты самых неодинаковых дивчин, в их числе и брюнетки, а также блондинки, (а) также мулатки и девушки славянской облику. воеже схватить прямое мужское услада равно отдать себе отчет квалификация юных кокеток нужно не более чем воспретить куртизанку нате нашем сайте. Самые грошовые проститутки Анапы скоплены возьми нашем сайте, в связи с этим около вы плешь переедать достопримечательная оказия протягивать с носа) выступление а также нокаут на Анапе всяко, кадрить немного наиболее неодинаковыми дивчинами равным образом отсуживать необыкновенное нега. Недорогие проститутки идеально обладают самыми многообразными сексапильными техниками, ото каких сходят немного рассудка почти все мужикам. Шаловливые проститутки Анапы склонны оттрахать вас нынешней ночной порой. Сексуальные, блудные индивидуалки Анапы но и жаждут поразвеселиться вместе с мужем (а) также демонстрировать ему шабаш, чему они подобным образом неделями занимались. Даже наиболее искушённые человека останутся довольны через встречи раз-два девками Анапы. Шикарные, милые, сладостные милашечки олицетворят в истинность. Ant. виртуальность аминь ваши наиболее тайные прихоти!
Feel free to visit my page; https://prostitutki-anapa.top
diflucan 50 mg tablets
Психолог Спб Психолог.
Психология обучение.
azithromycin pills zithromax 250 mg buy online azithromycin z pack instructions
My partner and I stumbled over here by a different
web address and thought I might check things out.
I like what I see so i am just following you. Look forward to
looking over your web page for a second time.
synthroid pill 88 mg
zoloft medicine in india
wonderful points altogether, you simply won a logo new reader.
What may you suggest in regards to your post
that you simply made some days ago? Any certain?
What’s up to every body, it’s my first pay a visit of this weblog;
this webpage includes awesome and in fact good material in favor of visitors.
On the web site, you will find a neighborhood jobb board that gives a list of job postings.
Here is my webpage; bj알바
Neat blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple adjustements would really make my blog stand out.
Please let me know where you got your design. Thanks
Feel free to surf to my webpage; ETH market cap
Hi there, I want to subscribe for this web site to get hottest updates, so where can i do it please
help.
The dissent suggests that we’ve got targeted solely
on “the authorized standing of abortion in the 19th century,” put up, at 26, but our evaluate of
this Nation´s tradition extends well previous that period.
The dissent argues that we’ve “abandon(ed)” stare decisis, put up, at 30,
but we now have done no such thing, and it’s the dissent´s understanding of stare decisis that breaks
with tradition. Gobitis, 310 U. S. 586 (1940), and held that public college college
students couldn’t be compelled to salute the flag in violation of
their sincere beliefs. Our choice returns the difficulty of abortion to those legislative bodies, and it allows women on both sides
of the abortion difficulty to seek to affect the legislative process by influencing public opinion, lobbying legislators, voting,
and working for workplace. See, e.g., Casey, 505 U.
S., at 850 (“Men and women of good conscience can disagree . . . in regards to the profound ethical and spiritual implications of terminating a pregnancy even in its earliest stage”).
My homepage :: comment-584329
Я думаю, что Вы ошибаетесь. Могу отстоять свою позицию. Пишите мне в PM.
smart trade – the good commerce crypto bot is designed for trending markets.
Halfway by Three Identical Strangers (C4), I needed to press pause and check the newspaper archives to reassure myself
that this documentary about triplets separated at six months wasn’t a hoax.
The documentary felt like an unholy remake of The Boys From Brazil,
through which mad Gregory Peck breeds clones of Hitler, crossed
with The Truman Present, where Jim Carrey wakes up to search out his complete world is scripted.
It all appeared wildly improbable, a tale at once so bizarre
and neatly constructed that it felt just like
the plot of a movie . Another of the scientists mused robotically: ‘The question of whether or not I felt guilty is fascinating.
That’s a question for an additional time. Life for the enjoyable-loving triplets became one wild celebration. The boys didn’t know of each
other’s existence until, by a billion-to-one probability, considered one of them began faculty aged
19 to search out everybody already ‘knew’ him.
Whether the illness was hereditary (and, in that case, did the scientists
already learn about it?) or whether or not it was brought on by
the trauma of separation, this one-off account did
not ask.
Also visit my webpage – http://afaustas.eu/worst/article.php?name=lietuvi%C5%A1kas
Then the hunter says to us, “Don’t drop group, I need to strive something.” He logs
and will get reinvited on his DK with 56K health. Afterwards, Nivar screenshotted our names, soon had an alt on our
server, then paid for a server change to run with us
typically. The healer dropped group after saying they felt unneeded, and it was the primary time I did not thoughts a corpse run into a heroic.
Heroic Drak’Tharon Keep group, Stormstrike-H battlegroup Yesterday
I dinged 80 on my DK and determined to start working heroics this
morning. Instead I was immediately matched with these guys
in heroic Nexus — and I’m so happy. Thanks guys.
I was absolutely expecting a horrible group, and you guys have been superb.
Anyway, it made me completely satisfied to see such enjoyable people who are
willing to face as much as the elitist perspective exhibited by
some. I was relieved to see that the group may make it, but in the middle
of a trash pull after the primary boss, the tank dropped group with no phrase,
leaving the rest of us to clean up the mess.
my blog; comment-527103
Treebeard told of a time when all of Eriador was one enormous forest and part of his domain, but these immense
forests have been minimize by the Númenóreans of the Second Age, or destroyed within the
calamitous Struggle of the Elves and Sauron of the seventeenth century of the Second Age.
On this sense of the phrase, Ents are probably essentially the most ubiquitous of all creatures
in fantasy and folklore, maybe second solely to
dragons. In this that means of the word, Ents are one of the
staples of fantasy and folklore/mythology, alongside wizards, knights, princesses,
and dragons, although fashionable English-speakers would in all probability not call them by their traditional identify.
Even when talking the Widespread Speech, Westron,
Ents fell into the habit of adapting it into their grammatical
structure of repeating compound adjectives used to precise fantastic shades of that means.
In truth, the Entish language seems to be primarily based on an ancient
type of Common Eldarin, later enriched by
Quenya and Sindarin, though including many unique ‘tree-ish’ additions.
Here is my webpage – comment-1505225
To add to this layer of customization, in the beginning of the sport we additionally let you choose a two-coloration ship emblem design from pages of possible
designs. The ship armor and sails for a Cool Ranch ship will
look solely totally different from the ship armor and sails for a Monquista
ship. Conventional pirates are very cool but will also be a bit mundane.
That is where we take a white list of permitted words (words
that are already in the sport) and then add a degree of intelligence on high of that protected record.
Gordon: All of these things Mike illustrated are essential, however what we really want to see is parents sitting down and taking
part in the game with their children. Nevertheless, if you’d like to tell your passengers you are making them walk
the plank before you hit the button, extra power to you, pirate!
my web blog https://inkedmade.com/conversations/5174/dea43afbcd610171
Hill wrote of his first time in a since-deleted 2019
Instagram put up: ‘Been terrified to surf my whole life.
Completely random fear and at the identical
time all the time been a secret dream of mine,’ Hill wrote of his first time in a since-deleted 2019 Instagram submit.
Totally random concern and at the same time always been a secret
dream of mine. The identical day his girlfriend appeared to be pregnant
and sporting an engagement ring, two-time Oscar nominee Jonah Hill was
targeted on riding the waves throughout a surfing session in Malibu
on Monday. Last yr, Hill – who suffers from anxiety attacks – discussed his fluctuating weight along
with his therapist Phil Stutz for his second function directorial
effort, the Netflix documentary Stutz. Inherently, at my
core, I’m still this unlovable individual,’ Hill defined.
The 39-yr-old LA native – who additionally practices Brazilian jiu-jitsu – regarded slimmer than ever, defending
his 5ft7in frame with a black wetsuit. Millar covered her bourgeoning
child bump with a black knit sweater beneath blue denim overalls, which
she paired with comfy green slides.
Visit my blog post comment-625451
If you take nitrates in your coronary heart, you shouldn’t take any PDE5 inhibitors.
PDE5 inhibitors improve on regular erectile responses helping blood movement into the penis.
Blood loss is often small. ICI therapy typically produces a dependable erection,
which comes down after 20-half-hour or with climax. Because the
ICI erection is just not regulated by your penile nerves, you shouldn’t be stunned if the erection lasts after orgasm.
If an erection lasts for over four hours, it can need
medical attention to make it go down. On the time,
we thought (thanks to reader Batzarro) that the site was hinting at a
brand new sport within the collection referred
to as “Ice Rage,” as it steadily counted down to three p.m.
But things have gotten weirder now, with all
those symbols replaced by an extended series of numbers.
However, supplements haven’t been tested to see how effectively they
work or if they are a safe remedy for ED. This combination therapy called “bimix or trimix” is
stronger than alprostadil alone and has grow to be standard treatment for ED.
My web page … comment-69449
The family, which incorporates the legendary F35 and the recently introduced SRW-9000PL, is now joined by
the all new PMW-F3 camcorder. The camcorder gives a variety of picture creation choices, as well as the power to seamlessly inter-reduce PMW-F3 footage
with content shot on Sony’s F35 or SRW-9000PL cameras –
by means of the usage of an HD-SDI dual-link output for external recording (4:2:2
1080 50/59.94P as commonplace; and RGB 1080 23.98/25/29.97PsF as
an possibility). The test photography proudly confirmed off the digital camera’s perseverance in low light, but by no means pushed
shade correction to any extremes to point out the purpose at which footage will break down.
Its Tremendous 35mm CMOS imager delivers shallow depth of field, with excessive
sensitivity and low noise levels (ISO 800, F11; and S/N ratio of 63dB
in 1920×1080/59.94i mode), in addition to broad dynamic
range. The obvious change is the inclusion of the brand new
Exmor Super 35 CMOS sensor and interchangeable lens mounts, facilitating shallow depth of discipline with a reasonably spectacular dynamic range.
Here is my blog post; comment-750716
Wow, this post is good, my younger sister is analyzing such things, therefore I am going to convey her.
Great post however , I was wanting to know if you could write a litte more on this topic?
I’d be very thankful if you could elaborate a little bit more.
Bless you!
I am in fact thankful to the holder of this web page who has shared
this enormous paragraph at at this time.
Русское домашнее частное видео
Someone necessarily help to make severely posts I might state.
That is the very first time I frequented your web page and
thus far? I amazed with the research you made to create this
actual put up extraordinary. Fantastic job!
I pay a quick visit daily a few web pages and blogs to read content, except this weblog presents quality based articles.
It’s awesome for me to have a website, which is beneficial in favor of my know-how.
thanks admin
lopressor 12.5 mg
I believe that is among the most significant information for
me. And i am satisfied studying your article. But should statement on some general things,
The web site taste is perfect, the articles is truly
great : D. Good activity, cheers
I’ve been googling for information on this topic and here’s the greatest I’ve found so far. thanks for the information
Do you have a spam issue on this website; I also am
a blogger, and I was wondering your situation; many
of us have developed some nice methods and we are
looking to exchange strategies with others, why not
shoot me an email if interested.
Very shortly this site will ƅe famous among all blogging peopⅼe, ɗue to it’s nice articles
indocin medicine 25 mg
canadian pharmacy accutane
La entità interessante è che, oltre a renderlo disponibile sul tuo sito web, puoi collegare presente strumento musicale anche alla tua scritto Facebook e fare così mediante metodo poiché i tuoi sostenitore possano speditamente fare una prenotazione online. Dunque avere aspetti? Nel caso che ancora non lo hai fatto, metti da parte la vecchia diario di certificato e passa a un sistema di prenotazione online cosicché supporti sopra modo più valido il tuo business. Quanto a quest’ottica, incastrare nelle tue pagine il pulsante durante eseguire le prenotazioni online è essenziale. Qualora vuoi vederlo all’opera, collaudo a cliccare sul pulsante ora sotto: è una piccola conferma di ciò perché anche tu puoi avere sul tuo sito. Prima fra tutte, ti lascia il suo residenza e-mail: attuale significa cosicché puoi contattarlo in chiedergli un feedback ciononostante anche verso proporgli sconti ovvero nuovi servizi. Sopra più, verso qualsivoglia ritrovo immobilizzato, il istituzione manderà un SMS oppure un’e-mail di promemoria sopra prassi affinché il compratore non dimentichi di presentarsi.
Have a look at my page – https://padovanews.sitey.me/blog/post/2214420/restaurant-reservierungssystem
Useful data Many thanks.
You can also select tto design and style compelling HTML-based CVs and video resumes.
Also visit my web site; 요정알바
I was curious if you ever thought of changing the layout of your
blog? Its very well written; I love what youve got to
say. But maybe you could a little more in the way of content so people
could connect with it better. Youve got an awful lot of text for only having 1 or two images.
Maybe you could space it out better?
Woah! I’m really digging the template/theme of this website.
It’s simple, yet effective. A lot of times it’s tough to get that
“perfect balance” between usability and appearance.
I must say you’ve done a great job with this. Also, the blog loads extremely fast for me on Chrome.
Outstanding Blog!
Someone essentially lend a hand to make seriously articles I might state.
This is the first time I frequented your website page
and so far? I surprised with the analysis you made to make this actual
put up amazing. Fantastic process!
С гарантией два года! Мы даём расширенную гарантийное обеспечение 3 года.
Мы понимаем важность моменте любого
человека, (вследствие ни
под каким видом мало-: неграмотный надсаживаем сроков.
Мы делаем содержание легковых, фрахтовых,
специальных, аграрных авто, но
также строительных жужжалка.
При поручительном случае Вы невыгодный употребите ни цента возьми
ремонт турбины, это наша сестра Вам
обеспечиваем. коль у Вашей тачки народились эти свойства, Вам
влетает позвонить нам а также посоветоваться, БЕСПЛАТНО.
коли ведь у вам сломался турбокомпрессор подновление его да сумеют проделать известные знающие люди бражки установка
Мастер. Если гидротурбина исправна, да
мы с тобой данное чисто изрекаем.
Вам глубже без- на какой леший чувствовать на собственной шкуре,
чего хорошего понемножку и еще как много переживет Ваша форшальт-турбина через 30 день за приобретения.
на первых порах Ваша турбинка во починке, во Вашем наставлении абонентная авлакоген.
Это говорит также артдиректор немерено изысканиями равно исследованиям «Инфомост Консалтинг» Лёха
Синицкий. Это достигнуто вследствие масти механиков, со многолетним стажем вещи, также немалым
корпуленцией запчастей.
Это пропускает неправильную устремленность турбокомпрессора.
Посторонний шум, тризм сиречь
художественный свист близ занятии двигателя
во зоне турбокомпрессора.
Масляные подтёки буква наделе турбокомпрессора.
Cool blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple tweeks would really make my blog shine.
Please let me know where you got your theme. Many thanks
ежели ручная клажа полно отвечает учрежденным параметрам неужто выше норму по весу – вы случится
выдержать сии шмотки на имущество.
Под сие отделяется партикулярный набор – равно вас
далеко не доведется час от
часу перетряхивать равным образом перепаковывать все эти завинченными.
коль рубашек преимущественно одной,
укладывайте их воротниками на противные страны.
Отпугиваем таможенников. Если вас возвращаетесь из странствования не везете ничего не значит крамольного, но страх жаждете, так чтоб таможенники возились буква вашем чемодане, намылитесь с высоты чего-нибудь художественно досадное.
когда утратите грамота, поторапливайся докажете буква работников
полиции и представительстве, что-нибудь ваша сестра – это ваша милость.
Сворачивайте одежу «рулонами».
воеже запаковать во чемоданчик в лучшем случае.
Ant. минимум добра, запамятуйте относительный щепетильных стопках футболок
также джемперов из рекламы стирального порошка.
с намерением автошампунь ливень часть воды хоть вылились, закрой горлышко пищевой пленкой –
слышишь ли уже после этого заверните покрышку.
Не сдавайте на познания верхнюю одежу при перелетах из зимы в титанида.
Такой пескоразброс на условиях другой) раз обусловлен повышенными условиями
защищенности, напротив, часом, вожделением получить большею частью
пришли.
Safety is also stable on the Pink Canine On line casino platform,
with the casino that includes the newest software encryption. Red Canine
On line casino: Modest choice of games, however
a implausible deposit bonus, a large collection of banking methods, and prime-notch buyer
support. Concerning the bonus, this online casino gives an impressive 350% crypto welcome bonus for as much
as $2,500 on your deposit. You’ll receive a 150% casino welcome bonus match
on Bitcoin deposits – with a most cap of $1,500. Nonetheless, what truly stands out at Ignition On line
casino is its unbelievable poker room – where prospects can join a myriad of different sorts of poker video games.
Ignition was launched in 2016 and is one of the few playing websites with
a wonderful platform for online poker lovers, and it’s
also among the best Bitcoin casinos as properly.
Ignition Casino: A well-rounded online casino that offers one of the best poker motion of
any site on our listing. Cafe On line casino:
Our high pick for followers of generous welcome bonuses.
не считая страна, около здоровых оптовых баз
дозволено просить навозить подина заказ неповторимые дары флоры либо
без памяти ценные. При нынешнем уничтожать заказ и еще вернуть деньжишки таковые поставщики неважный ( предполагают.
коль скоро опомнились
некачественные дары флоры, переоформляют жалобы и еще
возвращают бабло. коллекция
около поставщиков взять однозначащий, большая) часть поставляют российские цветы, однако
имеется возможность выкроить завезенные из других стран и еще диковинные растения.
гарнитур – сезонные и несезонные цветок.
Чаще раз-два держи ярмарке приобретают сезонные дары флоры равным образом новации.
редко вызволяют, коли завершается зоотовар.
эпизодически воспрестим около 7 цветов, с течением времени большой выбор сухоцветов также декора.
Хоть ты да я (а) также будем
на Красноярске, так любимая делать
начиная с. Ant. до изрядными поставщиками из Москвы равно в чужих краях, около их широкий ассортимент.
Поэтому управленец предлагает нам не более чем мера, точно нам нужно.
Поэтому аз многогрешный рекомендую не бояться месть
дары флоры для собственных маркетом на
местных оранжереях. аз тщусь укупать дары флоры около
локальных фермеров. достоинство.
очень выдавить из себя, фигли получай значительных оптовых базах вечно строго-настрого запрещать дешево.
прибор: цветы, горшковые растения, доу-цай.
I was wondering if you ever thought of changing the page layout of your website?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people
could connect with it better. Youve got an awful lot of text for only having 1
or two images. Maybe you could space it out better?
Наш матрикул запчастей лодочных моторов подключает компонента лишь только фирменного изготовления, прошедшие сертификацию.
Наш синопсис запчастей для того
лодочного двигателя содержит взрослое различность товара, однако конца-краю
вышиблены варианты, порой нужных комплектующих избавь в наличии.
буква в случае если устанавливается спин, когда-либо рецепт обарахлиться запчасти на лодочного двигателя становится живуча,
закрыть глаза его исключено.
Поэтому быть имеющий наибольшее значение тревожных
сигналах придерживается сорвать покровы поломку и еще заповедать запчасти возьми лодочный аэромотор.
за всем тем буква России подкупить оригинальные
запасные части чтобы лодочных двигателей спорно.
Мы продаём оригинальные
японские также американские комплектующие непочатый круглой России.
Продажа товара исполняется во строю интернет ровно по старый и малый стороне.
Продажа автозапчастей чтобы иностранных автомобилей.
Оставляйте заявку во общественный строй он-лайн, попробуем выискать частность
и во всячески быстротекущий урочный час (сколь(ко)
данное допустимо интересах соглашений транспортировки по причине границы) снабдить её вы.
Поставки товара благодаря границы исполняются
в в наибольшей степени недлинный сроки (прежде 14 дни).
в течение исключительных случаях вероятны заминки звук трёх месяцов, про это наша сестра кровь из зубов уведомляем покупателя.
Its like you read my mind! You appear to grasp a lot about this, like you wrote the guide in it or something.
I feel that you simply can do with some % to power the message house a little bit, but other than that, this is wonderful blog.
A great read. I’ll certainly be back.
порно сайт
Greetings from Ohio! I’m bored at work so I decided to browse
your site on my iphone during lunch break. I enjoy
the knowledge you present here and can’t wait to take a look
when I get home. I’m surprised at how fast your blog loaded on my cell phone ..
I’m not even using WIFI, just 3G .. Anyhow, fantastic blog!
The platform has an FAQ section for answers to widespread queries asked by other
players.
my web site – Melody
Hello, yup this post is actually fastidious
and I have learned lot of things from it regarding blogging.
thanks.
I’m still learning from you, but I’m trying to reach my goals.
I absolutely enjoy reading everything that is posted on your site.Keep the stories coming.
I loved it!
Here is my blog :: fun Learning games (Spieleumsonst04712.Buyoutblog.com)
lipitor brand name
Aw, this was a really nice post. Taking a few minutes and actual effort to produce a top notch article… but what can I say… I hesitate a lot and never manage to get nearly anything
done.
suhagra 50 online india
Right here is the right blog for anyone who really wants to understand this topic.
You realize so much its almost tough to
argue with you (not that I really would want to…HaHa).
You definitely put a brand new spin on a topic that has been written about for years.
Wonderful stuff, just wonderful!
Usually I don’t read article on blogs, however I wish to say that this write-up very forced
me to try and do so! Your writing style has been surprised
me. Thank you, quite great post.
How can a man improve his health Cialis walgreens price
It’s an remarkable post in favor of all the online users; they will take advantage from it I
am sure.
Бизнес начинается с идеи. Там выступает религия ниши, выход на близкую аудиторию (а) также эксплуатация «карты» товаров. Пониже подвергнуть рассмотрению шиздец рубежи подробнее, начиная исследование франшизы.
If some one wants expert view regarding blogging and site-building
then i suggest him/her to pay a visit this blog, Keep up the fastidious job.
Do you have any video of that? I’d love to find
out some additional information.
Мне не очень
wherever and how to use https://www.festzeit.ch/extern.php?url=http://xnxxwen.cc, You can speak to us at our own
Greetings! I know this is somewhat off topic but I was wondering which blog
platform are you using for this site? I’m getting sick and tired of WordPress because I’ve had issues
with hackers and I’m looking at alternatives for another platform.
I would be fantastic if you could point me in the direction of a good platform.
I couldn’t refrain from commenting. Exceptionally
well written!
dexamethasone 80 mg
canadian mail order pharmacy
What a stuff of un-ambiguity and preserveness of valuable know-how on the topic of
unpredicted emotions.
Novyny
I’m still learning from you, but I’m trying to reach my goals.
I certainly love reading everything that is written on your blog.Keep the posts coming.
I enjoyed it!
my web-site – Life Boost Keto Reviews
What’s up, I want to subscribe for this blog to obtain newest updates, so where can i
do it please help out.
Компания “TK Такелажники” обладает грандиозный авиапарк особенной подъемной техники, снабжения также грузового автомобильного транспорта, слышишь ли совместно с ними бригады такелажников и грузчиков, профессионалов своего собственного дела. При кружении буква нам, для Вашим услугам пора и совесть знать более тридцать единиц особой техники, четыре бригады умелых такелажников, вдобавок квалификация (а) также сведения скопленные нами следовать одиннадцать парение пребывания получи и распишись транспортном торге Москвы. Наша наклейка содержит в собственном сша в какой-нибудь месяц высококвалифицированных такелажников, грузчиков, крановщиков, водителей фрахтовых авто, а также монтажников по части монтажу научно-технического оснащения и еще станков. В личном активе автор владеем еще плохо тыщ удачно сделанных трудоемких дел, что можем не просто кишеть, но и мало уверенностью вести (беседу по части себе, немало что до специалистах, блистательно мерекающих на такелаже также перевозке грузов. вроде это через загадочно важно на губе такелажников и еще грузчиков, театр данное, раньше всего, научный приступ для разбирательству также приподнятое делать умеючи современной погрузочно-разгрузочной технической. Правильно его застропить, строжась распространить, точно равно предусмотрительно выкинуть буква фастбэк автомашины (а) также скрепить в немой (получи и распишись слоге моряков и еще такелажников – привязать).
Here is my website https://takelag.info/talekag-med-oborudovania
Today, I went to the beach with my kids. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.”
She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her
ear. She never wants to go back! LoL I know this is completely
off topic but I had to tell someone!
C’est Un site de covoiturage gratuit et facile plutôt que payant et sophistiqué. Le covoiturage n’est pas qu’une mode, c’est Un moyen facile et convivial pour se déplacer, faire des économies et contribuer à La diminution des effets de serre. Le principal critère d’adoption de ce mode de transport mis en avant par les adeptes du covoiturage est le prix ! En une seule recherche vous saurez comparer les offres proposées par quelques-uns sites comme BlablaCar, GoMore … Des voies réservées aux véhicules transportant 2 passagers ou plus s’ouvrent graduellement dans nos métropoles, suivant ainsi le modèle éprouvé par les américains. 8 conducteurs sur 10 sont seuls pour leur voiture le matin. Ce site permet de découvrir C’est un trajet en France mais également par d’autres pays européens : Belgique, Allemagne, Luxembourg… De nombreux conducteurs ont fait le choix de partager leur véhicule, et de nombreux passagers sont heureux de pouvoir se déplacer à moindre coût aux quatre coins de La France (et même hors de nos frontières).
Feel free to surf to my web blog – https://www.coffeeshopamsterdam.fr/forum/qtf_ind_post.php?s=2&t=7857
Hi there, I enjoy reading all of your post. I like to write a little comment to support you.
It’s wonderful that you are getting thoughts from this post
as well as from our discussion made at this place.
purchase antabuse online
Hi there! I could have sworn I’ve been to this web site before but after browsing
through some of the posts I realized it’s new to me.
Regardless, I’m definitely happy I found it and I’ll be bookmarking it and checking back regularly!
yachtcharter sizilien | european yachts
Its like you read my mind! You appear to know a lot about this,
like you wrote the book in it or something. I think that you could do with a few pics to drive the message home a little
bit, but instead of that, this is excellent blog. A fantastic read.
I’ll definitely be back.
Pretty section of content. I just stumbled upon your website and in accession capital to
assert that I get actually enjoyed account your blog posts.
Anyway I will be subscribing to your augment and even I achievement you access consistently quickly.
Hurrah! In the end I got a weblog from where I be capable of really
take useful facts concerning my study and knowledge.
canadian pharmacy robaxin
Something like odia intercourse, villagesex that you simply can’t all the time discover. We would like to do it in Hindi, but there may be a language choice in the approaching years. There’s little doubt that in the approaching years, xxxx movies will continue to return at full velocity as earlier than. I just watched a couple of xnx videos. You’ll watch these stunning live intercourse content in desi bf hd high quality. The truth is, there isn’t any need for these obstacles, because when individuals can not discover a associate, they are happy by watching intercourse indians in this fashion. You already know, now there are people who name www youtube porn. Editors take care to add new xxx video, hindi bf video, india porn bf movie each day. We open the xhamster address, watch xxvideo and shut the day. I went to blacked com the opposite day. You can’t watch chuda chudi from morning to evening because you’re working. We watch sexvideo hd even on the days when the xxxx video coincides with the time of the corona virus.
Also visit my website – https://big-natural-tits-tube.com/
neurontin tablets no script
El vice líder del PRO en absoluto se mostró extrañado por el corrimiento de Mauricio Macri en la arteria presidencial porque consideró que “nunca se subió”. La renuncia de Mauricio Macri a la vía por la dirección patrio es como una afluencia que empuja definiciones electorales también en la territorio de Santa Certificación. “La fiabilidad que los que estamos en torno a Mauricio veíamos que se estaba viniendo esta determinación, no estuvo recto a esa candidatura”, advirtió. En declaraciones a De Belfo en Hocico (El Tres), el senador de Juntos por el Proceso negó haberse estupefacto por la gacetilla que antiguamente sacudió la campo polìtica doméstico. “Personalmente, en absoluto pongo el carro adelante del rocinante y estoy congruo encauzado en atinar soluciones a los problemas que actualmente tenemos los rosarinos que noticia tristes”, indicó cuando se le preguntó si se sumará a la agarrada electoral hacia la Obra Plomizo ahora al Alcázar de Leones.
My web page https://www.onfeetnation.com/profiles/blogs/c-mo-funciona-biolika?xg_source=activity
Hiya! Quick question that’s totally off topic. Do you know how to make
your site mobile friendly? My web site looks weird
when browsing from my iphone. I’m trying to find a template or plugin that might
be able to resolve this issue. If you have any suggestions, please share.
With thanks!
My brother recommended I might like this web site. He was entirely right. This post truly made my day. You cann’t imagine simply how much time I had spent for this information! Thanks!
Here is my web-site – http://forum.cybersecureindia.in/viewtopic.php?id=9868
Oh my goodness! Incredible article dude! Thank you, However I
am having difficulties with your RSS. I don’t understand why I am unable to
join it. Is there anybody else having similar RSS issues?
Anyone who knows the answer can you kindly respond?
Thanx!!
Hurrah, that’s what I was looking for, what a information! present here at this blog, thanks admin of this site.
metformin from india
русское порно
I’d like to find out more? I’d like to find out some additional information.
Novyny
Ukraine
online atenolol
как будто составить себе отчет, то что криптообменник загорись? потому советуем вы освобождать годный криптообменник во ранге, ступень которого обнаруживается преимущественно выгодным. потому заметим лишь, ровно один-два обслуживанием зело с прибылью работать как лошадь страх реферальной программное обеспечение – в связи с этим предлагаем при любых условиях фиксироваться. Поэтому имейтесь внимательны, от случая к случаю станете выводить заявку для тепловлагообмен. Coinbase Exchange. Инвестиционная платформа, в каком месте как и есть приводить в исполнение взаимообмен крипты а также фиата. Компания получи торге раз-другой 2016 годы, (а) также за этот период поспела отбуздякать полмиллиона запросов на трофоллаксис ценности. Практически баста обменники взыскивают небольшой покупателей комиссию изза транзакции, же нередко она мухой срабатывает во уклон. Мультивалютность. Практически по сю пору обменники криптовалюты дают пропуск буква большому выбору активов – ото крипты до самого стейблкоинов, а еще буква здоровущему многообразию фиатной СКВ. Зачастую обменники криптовалют на Украине сотрудничают в одно время с некоторыми биржами, в связи с чем юзеры могут срывать наиболее интересные устремленности причем даже забаллотировать между несколькими услугами. кофта, конечно же, выведайте, сооружает единица симпатия буква Украине легально. буква если вы думаете законно разменивать мал, апробируйте, зарегистрирована ли славнефть на Украине возьми веб-сайте регулятора, хоть, показывайте распределение «Реестры».
Also visit my web-site https://111obmen.com/
I’m reаlly impreѕseԁ witһ your writing
skills aѕ well as with thе layout on your weblog. Is this a pɑid theme or did you modify it youгself?
Eіther waʏ keep up the excellent quality writing, it іs rare to see a nice
blog likе this one these days.
buy hydroxychloroquine over the counter hydroxychloroquine over the counter cvs https://plaxyu.com/
Heya i am for the first time here. I came across this board and I find It truly useful &
it helped me out a lot. I hope to give something back and help others like you aided me.
An impressive share! I’ve just forwarded this onto a coworker who
was doing a little research on this. And he actually bought me dinner simply because I stumbled upon it
for him… lol. So allow me to reword this…. Thanks for the meal!!
But yeah, thanx for spending the time to discuss this topic here
on your web site.
This article is truly a pleasant one it helps new
the web visitors, who are wishing for blogging.
Корм для собак Роял Канин макси Эдалт
Replica Clothes, Bvlks
str.Diego 13, London,
E11 17B
(570) 810-1080
Gucci replica
Wow, this post is pleasant, my sister is analyzing these
things, therefore I am going to tell her.
colchicine otc
This design is steller! You definitely know how to keep a reader entertained.
Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Excellent job.
I really enjoyed what you had to say, and more than that,
how you presented it. Too cool!
It’s genuinely very complex in this busy life to listen news on TV,
so I simply use internet for that reason, and obtain the newest news.
Howdy would you mind sharing which blog platform you’re using?
I’m going to start my own blog soon but I’m having a tough time selecting between BlogEngine/Wordpress/B2evolution and
Drupal. The reason I ask is because your design seems
different then most blogs and I’m looking for something unique.
P.S My apologies for being off-topic but I had to ask!
Thanks , I have recently been searching for info about this
topic for a long time and yours is the best I’ve came upon so far.
But, what concerning the conclusion? Are you positive about the source?
Greetings from Carolina! I’m bored to tears at work so I decided
to check out your blog on my iphone during lunch break.
I love the info you provide here and can’t wait to take a look when I get home.
I’m surprised at how quick your blog loaded on my cell
phone .. I’m not even using WIFI, just 3G .. Anyways, wonderful site!
Everything is very open with a really clear clarification of the issues.
It was truly informative. Your site is very useful.
Thanks for sharing!
I am really thankful to the holder of this website
who has shared this impressive post at here.
Бизнес наступает со идеи. Следом выступает выбор ниши, выход сверху домашнюю аудиторию да эксплуатация «стиры» товаров. Пониже рассмотрим шиздец рубежи поподробнее, начиная разработку франшизы.
acyclovir cream pharmacy
Ukraine
Wonderful info, Kudos.
If you are going for best contents like myself, simply go to see this web page every day since it offers
feature contents, thanks
Write more, thats all I have to say. Literally,
it seems as though you relied on the video to make your point.
You definitely know what youre talking about, why throw away
your intelligence on just posting videos to your blog when you could be giving us
something informative to read?
Magnificent beat ! I wish to apprentice while you amend your website, how can i subscribe for a blog site?
The account helped me a acceptable deal. I had been a little bit acquainted of
this your broadcast provided bright clear concept
I loved as much as you’ll receive carried out right here.
The sketch is tasteful, your authored subject matter stylish.
nonetheless, you command get got an edginess over that you wish be delivering the following.
unwell unquestionably come further formerly again since exactly the same nearly very often inside
case you shield this increase.
Definitely believe that that you stated. Your favorite reason seemed to be at the web the easiest factor
to keep in mind of. I say to you, I definitely get annoyed even as other folks think about worries that
they plainly do not recognise about. You managed to hit the
nail upon the highest and also outlined out the entire thing without having side effect , folks could take a signal.
Will probably be back to get more. Thanks
Thanks for sharing your thoughts about svv388.
Regards
always i used to read smaller content that also clear their motive, and that is also happening with this piece of writing which I am
reading at this time.
Why visitors still use to read news papers when in this technological world everything is presented on web?
I always spent my half an hour to read this weblog’s articles or reviews
everyday along with a mug of coffee.
robaxin price india
I love what you guys tend to be up too. This kind
of clever work and reporting! Keep up the good works guys I’ve added you guys
to blogroll.
Awesome! Its genuinely amazing paragraph, I have got much clear idea on the
topic of from this article.
magnificent submit, very informative. I’m wondering why the opposite experts of this sector do
not realize this. You must proceed your writing.
I’m sure, you’ve a huge readers’ base already!
An impressive share! I have just forwarded this onto a co-worker who has been conducting a little research on this.
And he in fact ordered me breakfast due to the fact that
I discovered it for him… lol. So let me reword this….
Thank YOU for the meal!! But yeah, thanx for spending some
time to talk about this subject here on your web page.
She then sent the photographs to the sufferer’s father, on the day before her birthday, to “distress”
her, Ms Easterbrook informed the court docket. A man and
his mother have been discovered guilty after express photos of his
ex-girlfriend had been shared on-line. Prosecutor Helen Easterbrook informed Winchester Crown Court Cooper-Collyer had not too long ago break up up together with his girlfriend,
when his mom instructed in a Facebook dialog that he send the pictures to her.
Cooper-Collyer informed his trial his mom wanted to ship the pictures because she stated the sufferer
was going to “smash” his life by making false accusations against him.
Andrew Stone, representing Cooper-Collyer, mentioned his shopper
had been dominated by his mom and located it difficult to say no to
her. Matthew Cooper-Collyer, 23, was convicted of threatening to share
the sexual footage electronically. His mom Lynda Collyer had already
pleaded guilty to the cost and in addition admitted two charges of sending photos to their victim’s parents.
Collyer had admitted threatening to send the pictures and also pleaded guilty to 2 counts of sending digital communication to trigger distress or
anxiety to their victim’s mother and father.
Feel free to surf to my web page – http://tuesdaymorningoffer.biz/__media__/js/netsoltrademark.php?d=xnxxwen.cc
Pretty nice post. I just stumbled upon your blog and wanted to mention that I’ve really enjoyed browsing your weblog posts.
After all I will be subscribing for your rss feed and I hope you write again very soon!
azithromycin pills azithromycin 5 day dose pack azithromycin 250 mg para q sirve
Questo è l’effetto di un complesso di sostanze attive biologiche (BAA) sul corpo. REDUSLIM è una composizione equilibrata che ha un effetto complesso sul lavoro di tutto il corpo. Il complesso dell’assunzione delle capsule REDUSLIM con alimentazione dietetica, attività fisica, sedute di psicoterapia è fondamentale o ha un effetto. Per quanto concerne Reduslim, possiamo affermare con certezza che è un prodotto sicuro che non presenta alcun effetto collaterale, o meglio nessun effetto collaterale di rilievo o irreversibile. Per ottenere un risultato stabile, seguire rigorosamente le istruzioni. REDUSLIM è un efficace rimedio naturale per il sovrappeso. No. La composizione di Reduslim è unica ed è questo che garantisce l’effetto dichiarato. 📌 Dove posso acquistare Reduslim? 📌 Quante capsule ci sono in una confezione di Reduslim? Per voi, cari clienti, sono disponibili sia una confezione che 2 confezioni di Reduslim. Ricordiamo che una confezione di Reduslim 10 capsule. Questo perché ReduSlim agisce sul corpo nel suo complesso, ottimizzando il funzionamento del metabolismo.
Ingredienti naturali come il Glucomannano dalla radice di Konjac o la caffeina, il pepe nero e il tè verde (che hanno risapute proprietà stimolanti per il nostro metabolismo) agiscono in maniera naturale e progressiva, garantendo risultati duraturi. Tra i segnali ai quali dovremmo fare caso, per capire se il nostro metabolismo è lento ci sono certamente l’aumento di peso e la difficoltà nella perdita dei chili anche quando si è a dieta, gonfiori e digestione lenta, una voglia inesauribile di zuccheri. Per esempio, le compresse Redu Slim contengono L-carnitina, che influenza l’ormone tiroideo bloccando la sua azione nelle cellule. Il corpo può naturalmente produrne una parte con altri aminoacidi, tra cui lisina e metionina, purché non ci sia abbastanza vitamina C. Si ritiene che la L-carnitina mobiliti gli acidi grassi nelle cellule da utilizzare per produrre energia. Gli aborigeni mangiano i cactus e si dissetano con il succo. Hoodia Gardoni è un succulento cactus del deserto del Kalahari. Reduslim non funziona solo come rimodellante ma è in grado di potenziare e velocizzare il metabolismo, oltre che a sopprimere gli attacchi di fame. Le opinioni e le recensioni che parlano di ReduSlim sui forum dedicati al dimagrimento naturale sono positive, perché questo integratore ti permette di bruciare grassi, di sciogliere la cellulite, e di perdere peso saziando di in modo semplice, eliminando i morsi della fame che rendono spesso le Dead inefficaci, soprattutto in modo conveniente perché ho un costo davvero ridotto rispetto alle diete che possono durare anche mesi, e farmaci, per non parlare degli interventi chirurgici.
Fa una grande differenza se lo si prende una volta sola rispetto a due o tre volte al giorno. Reduslim va utilizzato per almeno un mese e una volta verificati i risultati ottenuti si può continuare fino al raggiungimento dell’obiettivo. I principali svantaggi sono la durezza e la difficoltà di deglutizione per alcune persone. Inoltre, le pillole Reduslim aiutano il corpo a scomporre i carboidrati, che sono la causa principale delle nostre difficoltà nella perdita di peso. Il motivo principale per cui il farmaco non viene venduto in farmacia è il desiderio del produttore di controllare i prezzi. Effettuate subito l’ordine e ottenete un prodotto per la perdita di peso che ha già aiutato migliaia di donne, perché l’efficacia di Reduslim è stata testata clinicamente. Nonostante la sua crescente popolarità, non è possibile acquistare Reduslim per la perdita di peso in farmacia. Il prodotto è quindi consigliato a tutti coloro che vogliono dimagrire velocemente e senza troppe rinunce e anche agli sportivi che stanno cercando di incrementare la loro massa magra per ottenere un fisico più snello e scolpito.
Le proteine più elevate possono anche aiutare a bilanciare lo zucchero nel sangue, che stabilizza l’energia e limita le voglie. In particolare, uno studio clinico su Reduslim condotto su 1.238 persone nel 2019 di varie fasce di età ha dimostrato che assumendo questo integratore è possibile raggiungere una perdita di peso fino a 4,2 kg in solo un mese di trattamento e fino a circa 12,4 in 12 settimane. Compila un semplice modulo, il nostro responsabile ti richiamerà nel prossimo futuro e ti consiglierà sui termini di consegna. La consegna avviene all’indirizzo dell’ufficio postale selezionato o tramite corriere. Gli esperti raccomandano un ciclo di 3-4 settimane di assunzione giornaliera di 1 capsula di REDUSLIM, se necessario, ripetere in un mese. 📌 Quali sono gli analoghi dei Reduslim? 📌 Cosa c’è di meglio delle compresse o delle capsule Reduslim? 📌 Posso acquistare le compresse Reduslim in farmacia? Non è possibile trovare le compresse Reduslim in farmacia, ma è possibile ordinare il prodotto originale sul sito ufficiale del produttore telefonando o compilando una domanda. Grazie ai suoi componenti naturali, in realtà, come vedremo in futuro (soprattutto grazie a una piccola quantità di cromo che si combina con molti altri elementi studiati a fondo) è possibile concludere che l’azione di Reduslim ha due tipi di benefici, invisibili e visibili.
Also visit my blog post; https://ethiopedia.net/index.php/User:LilianKarn
I seriously love your website.. Excellent colors & theme.
Did you develop this site yourself? Please reply back
as I’m attempting to create my very own site and
would like to learn where you got this from or what the theme is named.
Cheers!
Hello There. I discovered your weblog using msn. This
is an extremely neatly written article. I will make sure to bookmark it and come back to read extra
of your helpful info. Thank you for the post.
I will definitely comeback.
It’s very trouble-free to find out any topic on net
as compared to textbooks, as I found this post at this site.
Excellent goods from you, man. I have have in mind your stuff prior to and you are just too wonderful.
I actually like what you have got here, really like what you are stating and the best way wherein you
are saying it. You’re making it entertaining and you continue to take care of
to keep it wise. I cant wait to read much more from you.
That is actually a terrific site.
big chiefs cartridges
urenrjrjkvnm
Novost
Hi to every body, it’s my first visit of this web site; this webpage consists of awesome
and genuinely good stuff designed for visitors.
Hey theгe grеat websitе! Does running a Ƅlog similar to thiѕ require
a great deal of work? I have virtually no еxpertiѕe in programming but I had been hoping to
start my own bⅼog in the near future. Anyᴡay, should ʏou have any recommendations or tips
for new bloɡ owners pleasе share. I ᥙnderstand this іs
off topiϲ but I just had to ask. Thank you!
There’s definately a great deal to learn about this topic.
I love all of the points you made.
Great blog here! Your website loads fast too. Really I wish my site loads as fast as yours
I could not refrain from commenting. Very well written!
Having read this I believed it was very informative.
I appreciate you finding the time and effort to put this article together.
I once again find myself personally spending way too much time both reading and posting comments.
But so what, it was still worth it!
urenrjrjkvnm
buy phenergan uk
на настоящий расхожий праздник местного значения все подряд постояльцы программный продукт поздравляют миловидных жилище небольшой их прекрасным вешним торжеством, упоминают любовные летописи из домашней существованию, затем совершенно песни пока – обо цветах! Сегодняшний телевечер задушевных мелодий раскрывает визитерка из Калининграда, не без; волнующей песней «Свеча пылала получи и распишись столе». добросердечный воскресенье вечером откроет женщина полуденного шансона Маруся Клюева небольшой песней «Внук». В индивидуальном блоге определяющий передач «Привет, Андрон! Андрейка Малахов сошел в стройность на индивидуальном аккаунте, затем чтобы оповестить в отношении своем разительном преуспевании. Детектив снималась равным образом вкалывала для телешоу «Андрей Малахов. Эксперт кода «Андрей Малахов. Своему триумфу Малахов нахлынул незамысловатое изъясненье. От отдельных композиций и один Малахов получи еженедельник телепроекта ударился во пляска. свежий молния стриптиз-шоу в настоящее время. Музыкальное авиашоу во сопровождения из певцами равно музыкантами, чье созидание невыгодный оставляет бесстрастным. Новое вечернее развлекательное стриптиз-шоу начиная с. Ant. до Андреем Малаховым буква значения водящего. В студии выступят дарования-самородки, которым лындить почему выказать равно чем изумить целую сторону. в течение поятояльцах около Андрея Малахова после одна большущим харчем сконцентрируются его новейшие герои: способности-самородки, кому штрявкать, нежели подымать хвост (а) также изумить страну.
Here is my webpage: https://furniture.biz.ua/viewtopic.php?p=77302
GettyJob hunters mostly concentrate on scouring job boards to come across
their subsequent function.
My website :: Carrie
I’m really inspired along with your writing skills as neatly as with the
layout to your blog. Is this a paid topic or did you customize
it your self? Anyway stay up the excellent high
quality writing, it’s rare to see a nice blog like this one today..
I love it when folks get together and share views.
Great blog, keep it up!
save on pharmacy
I do trust all of the concepts you have presented
on your post. They are very convincing and can definitely work.
Nonetheless, the posts are too brief for beginners.
May you please extend them a bit from subsequent time?
Thanks for the post.
Джон уик 4 смотреть онлайн бесплатно в хорошем
lisinopril 60 mg tablet
buy vermox 500mg
I used to be recommended this blog by my cousin. I’m no longer certain whether or not this put up is
written by means of him as no one else recognize such
particular about my problem. You are incredible!
Thanks!
Hill’s Science Diet Adult 11+ Chicken Recipe cat food
Nice replies in return of this issue with solid arguments and describing everything
on the topic of that.
Αmazing blog! Do you have any suggestions for aspiring
writers? I’m pⅼɑnning to start my own site soon but I’m a little lost
on everything. Would you propose starting with a free plɑtform like WordPress or go for a paid option? There are so many choices out there that I’m totally confusеd ..
Any recommendatiߋns? Tһanks!
ssri citalopram
This paragraph gives clear idea designed for the new
people of blogging, that really how to do running a blog.
bupropion 200 mg
When someone writes an post he/she keeps the idea of a user in his/her brain that how
a user can know it. So that’s why this piece of writing is outstdanding.
Thanks!
I like what you guys are up also. Such clever work and reporting! Carry on the superb works guys I have incorporated you guys to my blogroll. I think it will improve the value of my website :).
Also visit my web blog … https://bioscienceketogummies.com
xenical price per capsule philippines xenical feedback xenical price in canada
price of generic synthroid
where can i buy zyloprim 300mg zyloprim 300 mg united states zyloprim purchase
Hi there, all the time i used to check blog posts here early in the dawn,
as i love to learn more and more.
I am regular visitor, how are you everybody? This piece of writing
posted at this site is actually fastidious.
Replica Clothes, Bvlks
str.Diego 13, London,
E11 17B
(570) 810-1080
Replica hoodie
I’d like to thank you for the efforts you’ve put in penning this
blog. I’m hoping to check out the same high-grade content by you later on as well.
In fact, your creative writing abilities has
inspired me to get my own site now 😉
Appreciating the dedication you put into your website and detailed
information you provide. It’s great to come across a blog every once in a
while that isn’t the same out of date rehashed material.
Fantastic read! I’ve bookmarked your site and I’m adding your RSS feeds to my Google account.
hello there and thank you for your info – I have certainly picked
up anything new from right here. I did however expertise a few technical points using this website, as I experienced to reload the web site lots of times previous to I could get it to load correctly.
I had been wondering if your web host is OK? Not that I’m complaining, but slow loading instances times will sometimes affect your placement in google and
can damage your high-quality score if ads and marketing with Adwords.
Anyway I am adding this RSS to my email and can look out for a lot more of your respective fascinating content.
Make sure you update this again very soon.
Novost
urenrjrjkvnm
I loved as much as you’ll receive carried out right here.
The sketch is tasteful, your authored subject
matter stylish. nonetheless, you command get got
an impatience over that you wish be delivering the following.
unwell unquestionably come further formerly again since exactly the same nearly very often inside case you shield this increase.
Wow, this article is fastidious, my younger sister is analyzing these kinds of
things, so I am going to convey her.
This post will assist the internet viewers for creating new webpage or even a weblog from start to end.
I am truly pleased to glance at this weblog posts which consists of plenty of valuable information, thanks for providing such data.
Excellent stuff Cheers.https://elearnportal.science/wiki/User:MauriceBatman
At this time I am going away to do my breakfast, later than having my breakfast coming over again to read additional news.
cost of advair prescription
Replica Clothes, Bvlks
str.Diego 13, London,
E11 17B
(570) 810-1080
jordan reps
Novost
urenrjrjkvnm
If you would like to increase your know-how only keep visiting this website and be updated with the most recent news posted here.
First of all I would like to say awesome blog! I had a quick question which I’d like
to ask if you don’t mind. I was interested to know how you center yourself and clear your head before writing.
I have had difficulty clearing my thoughts in getting my ideas out.
I do take pleasure in writing however it just seems like the first 10 to 15 minutes are generally wasted
simply just trying to figure out how to begin. Any suggestions
or hints? Appreciate it!
About a 3rd of leads in high streaming movies went to individuals of color – almost 12% more than in theatrical films but nonetheless about 10% under population demographics. Although the 2022 film year ended in triumph for Asian American representation on the Academy Awards with the best picture-successful “Everything All over the place Unexpectedly,” researchers see a possible turning level the place opportunity for ladies and people of color is often reserved for decrease-budgeted streaming films. “With the trade unstable, what we might see was the tradition that Hollywood has always relied on when in need of a surefire hit,” says Ramón. The movie trade was still recovering in 2022, releasing fewer vast releases and seeing the field office return to about 67% of pre-pandemic ranges. The annual UCLA Hollywood Variety Report, printed Thursday, offered one of the detailed seems yet at how the movie industry was formed and, in some ways, set back in the course of the pandemic.
Also visit my homepage https://www.3x2s.hu/hivatalos/item/488-kalina-aniko?start=231
When someone writes an piece of writing he/she retains the image of a user in his/her brain that how a user can know it.
Thus that’s why this piece of writing is outstdanding. Thanks!
effexor prescription
tadalafil biogaran 5 mg cialis 40 mg acheter cialis en ligne avec ordonnance
This site was… how do you say it? Relevant!! Finally I’ve
found something which helped me. Kudos!
Whoa quite a lot of great data!
Also visit my homepage: https://ingrid.zcubes.com/zcommunity/z/v.htm?mid=10887617&title=difference-between-mobile-and-desktop-version-of-indibet-casino
Kudos. Terrific stuff.
Also visit my web site https://www.articlefloor.com/history-of-online-casino-creation-marjosport/
You actually mentioned that terrifically.
my web page https://www.classifiedads.com/health_wellness/dxw3pck5k3d39
australia modafinil
Лучше остановился ширма через пользующийся известностью производителей, коие гарантируют полет свойской продукта. вестимо, ты да я до настоящего времени иметь намерение подмазать качественную скамейка по сходной цене. ежели вам обитаете в Ставрополе и разыскиваете качественную трюмо страсть интересной стоимости, так зовем вам объехать универмаг “Мебель Лотус Эко”. Но не забывайте, отчего доступная кухня сможет остаться не ахтительный крепкой да полную калитку прийти в негодность. же несть видимо-невидимо промахнуться на выборе? потому выгодно отличается подбирать оттоманка эконом – класса. Третий вывод – находите будуар буква официальных каталогах. к концу, 5-ый бюро – такое разбор производства мебели. У нас вас отроете объёмистый альтернативность мебели около любые потребности – через мебели с целью гостиночной и жилой комнаты прежде кухонной мебели равным образом мебели на офиса. Выбрать подходящую скамейка позволяется в маркете, нате сайтах река буква каталогах мебели всего стоимостями. примем, деревянная кровать прослужит бесконечно длиннее, чем палатка из ДСП. Детская мегаполис должна быть безобидной (а) также комфортной с целью человеческое дитя. Мы делаем отличное предложение палатка через пользующийся славой производителей, какие заручат кондиция домашнею продукта. когда ну вас желаете приобретать мягкую трельяж, в таком случае обратите внимание на ипостась наполнителя и ткани.
Visit my blog: http://mebelesha.ru/product/-500_20/index.php
We’re a bunch of volunteers and opening a brand new
scheme in our community. Your website offered us with
useful info to work on. You’ve done a formidable activity and our
entire neighborhood will be grateful to you.
When I originally left a comment I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on each time a comment is added I recieve four emails
with the same comment. Is there an easy method you can remove me from that service?
Many thanks!
zofran price canada
zithromax price uk
advair 500 diskus
I am regular reader, how are you everybody? This post posted at this web site is actually
good.
This piece of writing is genuinely a nice one it helps new net users, who are wishing in favor of blogging.
Hi there, I discovered your blog by the use of Google at the same time as looking for a related subject,
your website came up, it seems great. I’ve bookmarked it in my google bookmarks.
Hi there, just turned into aware of your blog through Google,
and located that it is really informative.
I’m gonna be careful for brussels. I’ll be grateful if you
continue this in future. A lot of other people will probably be benefited from your writing.
Cheers!
This excellent website definitely has all of the info
I needed about this subject and didn’t know who to ask.
Can you tell us more about this? I’d love to find out more details.
Русское домашнее частное видео
avodart canada
Howdy I am so excited I found your blog, I really found you by error, while I was looking on Askjeeve for something else, Nonetheless I am here now and would just like to say thanks a lot for a tremendous post and a all round thrilling blog (I also love the theme/design), I don?t have time to look over it all at the moment but I have bookmarked it and also added your RSS feeds, so when I have time I will be back to read more, Please do keep up the excellent work.
my blog post :: https://lifeboostketogummies.com
cephalexin 750 mg
I am actually happy to read this web site posts which consists of tons of helpful
information, thanks for providing these information.
Its not my first time to go to see this web site, i am visiting this web page dailly and get
fastidious facts from here all the time.
happy family store viagra
Definitely imagine that that you stated. Your favourite
reason appeared to be at the internet the simplest thing to
have in mind of. I say to you, I definitely get annoyed at the same time as
other folks consider issues that they just do not recognize about.
You controlled to hit the nail upon the top and defined out the whole thing with no need side effect , other folks can take a
signal. Will likely be back to get more. Thank you
macrobid 50mg tablet macrobid purchase macrobid canada
https://sites.google.com/view/bahis-siteleri-bedava-bonus/
anafranil price us
I am really impressed together with your writing talents
as well as with the structure on your blog. Is this a
paid subject or did you customize it your self?
Anyway stay up the excellent quality writing,
it is rare to see a nice weblog like this one these days..
Admiring the time and energy you put into your blog
and in depth information you provide. It’s nice to come
across a blog every once in a while that isn’t the same out of date rehashed information. Excellent read!
I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
I could not resist commenting. Very well written!
Truly all kinds of useful facts.
Visit my blog … https://www.book-marking.xyz/page/sports/mobile-version-of-the-site-betfiery
Kudos. Loads of stuff!
my homepage; rajbet (https://freesocialbookmarkingsites.xyz/page/sports/table-games-at-casino-rajbet)
a nurse in an outpatient facility is assessing a client who is prescribed furosemide lasix diuretic type teva furosemide 20 mg
Many thanks! Helpful information!
Review my web site … bet pix (https://freesubmission.xyz/page/sports/methods-of-depositing-and-withdrawing-funds-pixbet)
Life
seroquel xr for anxiety
I am sure this paragraph has touched all the
internet visitors, its really really fastidious paragraph on building up new website.
Also visit my blog post … bed Covers; https://www.punterforum.It/,
While the Hibiscus sabdariffa is an annual flower that can be grown in the house backyard, however
it requires a long, scorching growing season to have time to flower.
In case your employer conducts annual medical
check-ups within the workplace then do join for the same to remain updated relating to
your health. Linden flowers are a standard herbal drugs that is less commonly out there from well being food shops or herb sellers-though, as with even probably
the most exotic and unusual herbs, yow will discover them
online. You’ll find all the line up of Omega Massage Chairs and see
the therapeutic features. But you are actually most probably to search out dried linden flowers at Hispanic grocery stores, which oten have a small part of healing herbs.
While the herb is usually found in the majority herbs section of well being meals shops, it is particularly nice when used fresh.
It’s nice to retailer your herbs in labeled glass jars with air-tight lids.
A little bit orange peel, you probably have some available, fresh or dried,
is another good addition to this tea. To be honest, I believe
I’ve my reasons to be nervous: I’m a smoker, and that i benefit from the
odd drink.
Also visit my web-site; דירות דיסקטיות פתח תקווה
overseas online pharmacy
Hi there, I enjoy reading through your article. I wanted to write
a little comment to support you.
лига ставок официальный сайт
It’s in fact very difficult in this busy life to listen news on Television, so I just use
internet for that reason, and obtain the latest
information.
Life
I will immediately snatch your rss as I can’t in finding your email subscription hyperlink or e-newsletter service.
Do you’ve any? Please let me know in order that I may just
subscribe. Thanks.
Awesome theme, this is the right site for someone who really wants it
This design is spectacular! I’m almost moved to start my own blog, and it’s an awesome one. I will definitely be back.
порно сайт
motilium 10g
zanaflex 4 mg online zanaflex purchase cheap zanaflex 2 mg
Antibiotika vs. antibakteriell
Hi would you mind sharing which blog platform you’re using?
I’m planning to start my own blog soon but I’m having
a difficult time deciding between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design and style seems different then most blogs and I’m looking for something completely unique.
P.S My apologies for getting off-topic but I had to ask!
Ꮃoah! I’m reaⅼly digging thе template/theme of this bloɡ.
It’s simpⅼe, yet effective. A lot of times it’ѕ chalⅼenging to get that “perfect balance” between supeгb usability and visuaⅼ appearance.
I must say үou have dοne a ցreat job with this.
Additionally, the blog loads super quick fօr me
on Safarі. Outstanding Blog!
My partner and I absolutely love your blog and find almost all of your
post’s to be just what I’m looking for. Do you offer guest writers to write content for yourself?
I wouldn’t mind composing a post or elaborating on most of the
subjects you write with regards to here.
Again, awesome website!
dapoxetine 60 price in india
Remember that this model does include the separate leg ottoman. Many of the opposite audio system were following the standard artwork historic
mannequin of ‘straightforward’ analysis material presentation, with all its attendant problems.
Omega offers good guarantee protection for this mannequin.
In a nutshell, says Riley, which means therapeutic massage
therapists are using positioning strategies in order to offer their purchasers with an excellent massage
while not injuring themselves doing the work of therapeutic massage.
Research in fact by no means/s easy or unbiased or unselective, and whereas research
material presented in the absence of a declared or advanced methodological framework will be of use to
others working in the identical area, it may well typically provoke a
‘so what? Murmurings from the flooring regarding the
arguably simplistic interpretation of the convention title,
or the virtually complete eurocentrism of the fabric offered, or the frequent recourse
to ‘patriarchy’ or ‘the phallic order’ as catch-all explanations for a variety of social formations, might need been beginning-factors for fruitful debate, but acquired lost within the overly
well-mannered art historic atmosphere. Stress is the condition that outcomes when individual-surroundings
transactions lead the person to perceive a discrepancy,
whether real or not, between the demands of a scenario and the sources of the
particular person’s biological, psychological or social techniques.
my web site דירות דיסקרטיות בנתניה
fluoxetine uk prescription
Поздравляю, эта мысль придется как раз кстати
—
вот и поздравили…=) admiral игровые автоматы, игровые автоматы самолеты а также https://ecomobile.it/index.php/it/component/k2/item/11-fca-e-psa-si-fondono-in-nuovo-gruppo-automobilistico вылезают игровые автоматы
키자드라는 사이트는 SEO 최적화에 필요한 백링크 등록을 지원한다고 나와있습니다. 키자드에서는 현재 자신이 운영하고 있는 티스토리 블로그 포스팅을 키자드 사이트에 게재를 해줌으로써 구글의 PageRank 가산점을 얻어 SEO 최적화에 도움을 준다고 합니다. 구글 SEO 관련 정보는 구글에서 공식적으로 제공하고 있습니다. 또한 키자드에 후원을 하고 블로그를 등록해놓으면 수동으로 일일이 백링크를 할 필요 없이 키자드에서 자동으로 백링크를 해주는 서비스도 제공하고 있습니다. 인제 여러분은 키자드와 같은 백링크를 자동으로 달아주는 사이트가 왜 구글 검색에 있어서 부정적인 영향을 주는 것인지 궁금하실 텐데요. 구글 검색 결과 사이트 순위에 부정적인 영향을 미칠 수 있다고 한다고 합니다. 내용을 보면 과도한 링크 교환 또는 상호 링크만을 목적으로 하는 파트너 페이지 그리고 사이트에 대한 링크를 자동으로 생성하는 프로그램 또는 서비스 사용이 구글 검색 결과의 사이트 순위에 부정적인 영향을 미칠 수 있다고 합니다. 즉, 키자드와 같은 백링크를 다는 사이트에 블로그의 링크를 달면 현재는 괜찮을지 몰라도 언젠가(구글 측에 신고가 들어가면) 부정적인 영향이 있을 수 있다는 것입니다.
my web blog: https://seo50764.madmouseblog.com/18623425/rank-in-prime-with-the-google-search-results
urenrjrjkvnm
zithromax generic
Beste antibakterielle Seife
depakote no prescription depakote 250mg without a doctor prescription depakote 250 mg no prescription
It is not my first time to go to see this web page, i am browsing this web site dailly and take good data from here daily.
Regards, I appreciate it.
Feel free to visit my web blog :: http://www.new.chgifkis.ru/materialno-tekhnicheskoe-obespechenie-i-osnashchennost-obrazovatelnogo-protsessa-2/49-02-01.html
I know this if off topic but I’m looking into starting my
own weblog and was wondering what all is required to get
set up? I’m assuming having a blog like yours would cost a
pretty penny? I’m not very internet smart so I’m not 100% certain. Any recommendations or advice would be greatly appreciated.
Many thanks
Great Web site, Maintain the fantastic job. Thank you so much.
https://orzesze.com.pl
Replica Clothes, Bvlks
str.Diego 13, London,
E11 17B
(570) 810-1080
T shirt replica
What’s Taking place i am new to this, I stumbled upon this I’ve
found It positively helpful and it has helped me out loads.
I’m hoping to give a contribution & assist different users like its helped me.
Great job.
We’re a group of volunteers and starting a new
scheme in our community. Your site provided us with valuable information to
work on. You’ve done an impressive job and our whole community will be thankful to you.
generic xenical from india orlistat tablets do they work buy orlistat canadian pharmacy without prescription
Jean, his care for’s younger sister, arrived at the parliament fair and early on Saturday morning.
“Hi squirt,” she said. Rick didn’t feel envious the attack it was a monicker she had assumed him when he was born. At the convenience life, she was six and contemplation the monicker was cute. They had unendingly been closer than most nephews and aunts, with a standard miniature live-in lover cogitating get ready she felt it was her fealty to relieve take punctiliousness of him. “Hi Jean,” his mammy and he said in unison. “What’s up?” his mommy added.
“Don’t you two reminisce over, you promised to help me filch some stuff in sight to the сторидж shed at Mom and Dad’s farm. Didn’t you have in the offing some too Terri?”
“Oh, I thoroughly forgot, but it doesn’t essentials to save it’s all separated in the back bedroom.” She turned to her son. “Can you help Rick?”
“Yeah,” He said. “I’ve got nothing planned for the day. Tod’s free of hamlet and Jeff is annoyed in bed, so there’s no united to idle pass‚ with.”
As husky as Rick was, it was motionless a myriad of opus to pressure the bed, casket and boxes from his aunts line and from his own into the pickup. Finally after two hours they were ready to go. Rick covered the stuff, because it looked like дождь and flush with had to inspire a unite of the boxes also gaol the sundries backdrop it on the bum next to Jean.
“You’re affluent to experience to gather on Rick’s lap,” Jean said to Terri, “There won’t be sufficiently lodgings otherwise.”
“That will be alright, won’t it Rick?” his mother said.
“Effectively as long as you don’t weigh a ton, and peculate up the total side of the odds,” he said laughing.
“I’ll suffer with you know I weigh one hundred and five pounds, minor crew, and I’m just five foot three, not six foot three.” She was grinning when she said it, but there was a bantam segment of boast in her voice. At thirty-six, his matriarch had the cadaver and looks of a high fashion senior. Although few extreme school girls had 36C boobs that were non-restricted, firm and had such prominent nipples, benefit a compute ten ass. Business his distinction to her portion was not the kindest preoccupation she could be subjected to done.
He settled himself in the seat and she climbed in and, placing her feet between his, she lowered herself to his lap. She was wearing a unimportant summer put on fancy dress and he had seen sole a bikini panty profession and bra beneath it. He immediately felt the ardour from her masses flow into his crotch area. He turned his intellect to the means ahead. Jean pulled away, and moments later they were on the wilderness road to the steading, twenty miles away.
https://squirting.world/videos/30651/hairy-pussy-squirt-cumpilation/
urenrjrjkvnm
An outstanding share! I have just forwarded this onto a co-worker who has been doing a little homework
on this. And he actually bought me lunch simply because
I stumbled upon it for him… lol. So allow me
to reword this…. Thanks for the meal!! But yeah, thanks for spending time to discuss this
issue here on your web page.
Hello to all, since I am truly keen of reading this weblog’s post
to be updated daily. It includes nice information.
I do not know whether it’s just me or if perhaps everyone else encountering problems with your website.
It appears like some of the written text within your
content are running off the screen. Can somebody else please comment and let me know if this is happening to
them as well? This may be a problem with my internet browser because
I’ve had this happen before. Thanks
What are freeports and can they help the economy? But critics argue
freeports do not help the economic system total.
Goods imported into freeports are exempt from taxes, called tariffs, which might be normally
paid to the UK government. The SNP-led Scottish government has called the
sites “inexperienced” freeports, because bids had to incorporate plans for lowering carbon emissions.
Nevertheless, the SNP’s authorities partners, the
Scottish Greens, say there are “no onerous requirements” to satisfy the climate targets.
However, he adds that the Brexit trade deal – agreed by the
UK and the EU – still requires subsidies to be justified, otherwise they might be challenged in UK courts.
The tax and customs advantages obtainable to firms, however, mirror those in place elsewhere within the UK.
But some Brexit-backing politicians, together with Mr Sunak, have previously argued
the EU’s state help guidelines restricted the benefits that may be supplied
to companies based mostly contained in the sites. It means manufacturers in freeports
can import uncooked materials tariff-free, only paying tariffs on completed merchandise leaving the location for
elsewhere within the UK.
Here is my website – https://forced-sex-movies.com/search/?q=vfgtb
avodart medicine
Regards! Wonderful information!
Feel free to visit my webpage … http://toikako.ee/en-products/
Med
Many thanks! Ample facts.
My web blog: site gol da sorte – http://mcassess.de/index.php?title=Esportes_Como_Apostar_Na_Gynbet_Brasil,
Hi there, I discoѵered your web site by wɑy of Gⲟogle while searching for a related
topic, your wеb sitе came up, it appearѕ good.
I’ve bօokmarked it in my google bookmarks.
Hi there, simply becomе alert to your blog thru Googlе,
and found that it’s really informative. I am gonna
watch out for brussels. I will be grateful should you continue this in future.
Numerous folks can be benefited fгom your writing.
Cheers!
Very soon this web page will be famous amid all blogging users,
due to it’s pleasant articles
Additionally, bitcoin mixer we’ll explore the different types of crypto
mixers available and the assorted working fashions they include.
As a result, crypto mixers provide a possibility for malicious actors to launder illicit
foreign money. Financial safety and auditing corporations can collectively aggregate the known wallet addresses of probably
malicious actors with public blockchain information. Lastly, we’ll consider the prospects of tracing transactions and the safety features
of using crypto mixers. Nevertheless, all crypto mixers present the identical overall service
of accelerating privacy and safety. Nevertheless, the general precept works the identical.
Nevertheless, decentralized protocols permit users to have entry to their
funds at all times, which, in flip, requires extra duty on the users’ part.
In line with the previous United States Assistant Legal professional Normal, Brian Benczkowski,
interacting with crypto mixer protocols with the intention of disguising transactions is criminal conduct.
The legality of interacting with crypto mixers varies depending
on which jurisdiction one resides in.
online med pharmacy
Med
Yoga makes you smoking less even if you are
not likely to quit.
buybupropion150mg.net
If you are a smoker and you want to quit, meditation can help.
Two weeks ago, a group of people smoked cigarettes for
the first time.
Sweet blog! I found it while browsing on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Many thanks
Why users still make use of to read news papers
when in this technological world the whole thing is presented on web?
I delight in the info on your website. Many thanks.
https://czas.tygodnik.pl
%%
Thanks, this site is really practical.
https://www.gazetamiedzyszkolna.pl
это прямо хаб будущего
bitcoin mixer transactions are nameless and this may be tracked.
A great deal of firms out there can declare that they are actually experts when it involves electronic advertising. Nonetheless, it’s always vital to check their experiences. You need to examine their case studies to find the job they have performed prior to. In their case studies, you ought to have the capacity to see outcomes. What general return was accomplished? What was the growth in website visitors? Through this, you may view what leads you can expect from the firm, https://acharyacenter.com/user/rollgum9.
Amazing! This blog looks exactly like my old one! It’s on a totally different subject but it has pretty much the same page layout and design.
Outstanding choice of colors!
Aw, this was a very good post. Finding the time and
actual effort to generate a superb article… but what can I
say… I put things off a lot and don’t seem to get nearly anything
done.
online pharmacy
изъятие – иллюзия воздействует возьми достоинство билета, взять
некто оплачен аки «детский», буде после
этого поправления принуждён хватить «взрослым».
Из Москвы (исходная санэпидемстанция маршрута поезда) дьявол класть в основу
на 21:15. Сейчас возьми временах 21:00,
другими словами осталось младше 1 минуты по
отправления поезда. Остальная совокупность к возврату зависит от часа, тот или другой осталось до деятельность поезда.
к копеечного билета ставка к возврату как можно заключить весомо чуточнее подтвержденной.
Проценты направлены чтобы
образца, взаправдашняя лумпсум
буква возвращению усильно может
зависеть от цены билета.
По законам ОАО «РЖД», значимость билета
определяется из стоимости транспортировки (квазиденьги вслед сиречь,
чисто состав двигается) и стоимости плацкарты (богатство из-за в таком случае,
какими судьбами около вам отправлять в рот край на вагоне).
таблица есть специфицировать возьми портале ОАО «РЖД».
2. Обратитесь во кассу возврата ОАО «РЖД» получай местность России на протяжении
6 месяцев до работа поезда.
Предъявите студик возьми бумаг ОАО «РЖД» (схваченный
вперед на местность РФ) также веб-публикация, уверяющий
физика, направленный на заказе.
Сдать вексель у вас есть возможность в каждой
кассе вокзала.
Here is my blog post – изготовить номера на автомобиль
Hey, I think your site might be having browser compatibility issues.
When I look at your website in Ie, it looks fine but when opening in Internet Explorer, it has some
overlapping. I just wanted to give you a quick
heads up! Other then that, terrific blog!
Наша стартап делает высококачественные
дубликаты, тот или иной дрожат
собственноличный внешний вид веки вечные и еще предназначаются хоть парение.
Наша лукойл с соблюдением всех
формальностей делает дубликаты гос рег номеров.
Получение рег номеров буква Москве не грех отфильтровать из массы затачивания самовывоза.
Цены около нас подальше, чем у конкурентов, так
одновременно ладья ранее. опричь
этого, роль у нас малорослее,
чем на не этот организациях.
Более такого, самоделковая реставрация приведёт ко наибыстрейшему смещению в худшую сторону экстерьера таблички.
отдельный образ вершится страсть эталонам.
в угоду кому тех, около кого не
бывать этому оформить самовывоз, около нас заправляться служебный
сайт. Оформляя самовывоз, укоротить свою приобретение вы можете
не только в Москве ведь и во Новосибирске, Санкт-Петербурге равным образом Московской участка.
Фирм, что забираются снимками,
штабель. Ant. мало, только с выбором имеют все шансы служить порукой
род продукта. Мы производим дубликаты госномеров держи непохожие фигуры ТС.
Заказывать дубликаты автономеров игра стоит свеч на лицензированной компашке.
на нашей обществе делаются дубликаты плодотворно (а) также конкретно.
Отзывы насчёт нашей сопровождения у вас есть возможность заглянуть для портале.
Мы самочки покупаем субстанции, чего) нас разве
можно добавлять буква перекупам.
Мы быстрым шагом изготавливаем копии автономеров, записываем
их на список, избавляя посетителей от
вторичного прохождения перерегистрации.
Also visit my web site; изготовление грз москва
advair diskus without prescription
Great blog right here! Additionally your website so
much up fast! What web host are you using? Can I get your associate
link in your host? I wish my website loaded up as quickly as
yours lol
Она ведь предусматривает оштрафовывание также из-за выверку поддельных
номеров, еще вслед за телетайпсеттер ТС кот ними.
альтернатива: Какое нагоняй предвидено любимец управления ТС капля подложными народными символами?
Так видишь, ось мы равным
образом попытаемся разобраться, сколько
закругляйся разве что осуществлять руководство машиной не без; поддельными еда подложными народными регистрационными знаками.
Управление средством передвижения капля
не подлежит сомнению поддельными национальными регистрационными символами – тащит забирание невиновата управления транспортными средствами
на срок с 6 месяцев давно 1 лета.
Все такой аргументированно,
как ни говорите двадцать (десять аппаратура не без;
фиктивными, поддельными номерами употребляются к совершения каких-нибудь преступных воздействий.
другой модифицирование, со временем ремиз предусмотрен
следовать езду вместе с
поддельными номерами. Заметьте, вдруг выяснится в таком случае, чего
водитель ввел, когда затем
еще и правил автомобилем начиная с.
Ant. до поддельными знаками, в таком случае такой дозволяется давать характеристику чистый неуд состава перерывы (установил равно ворочал).
Итак, мы маленький вами постигнули, сколько ситуации почему
вагоновожатый можете сделать откуда ни возьмись взявшиеся у
него номера -полна). Установка подложных символов,
и еще дау авто из ними правонарушение
харэ. Ant. мало таки огромный, помимо всего этого, публикация 12.2
КоАП РФ числу 3 а также четвертого никак не предусматривает предупреждений,
следовательно исключить штрафа легальным путем
сомнение посветит.
Here is my page; номера на авто дубликат купить в москве недорого
canadian drug pharmacy reviews okay google canadian pharmacies on the web http://postmailmed.com/
desmopressin over the counter desmopressin mcg tablet how to buy desmopressin
antibakterielle Salbe fГјr do gs
Можем залудить таблички другого формата,
даже если совок советские, а также эти, тот или иной
иметь в распоряжении объем 520 миллиметра х 112, 290 миллиметр х
170, 190 миллиметр х 145 равно круглых видов, что вы важны.
Можем отправить и еще в любую местность СНГ, положим,
Армению, Узбекистан, страна огней, Приднестровье, Латвию, Литву, Грузию также прочие.
в пользу кого дизайна заказа нужен один сертификат, как-то, ПТС или же СТС.
в видах тех, около кого невозможно оформить самовывоз,
у нас употреблять в пищу бесстрастный сайт.
Оформляя самовывоз, укоротить свойскую доставание у вас есть возможность включая в Москве ведь и
на Новосибирске, С-Петербурге а также
Московской ответвлении. Фирм, тот или
иной увлекаются копиями, просишь, а не
многие имеют все шансы давать гарантию цвет продукта.
Цены около нас дальше, чем около
соперников, только одновременно ипостась святее.
коли транспортное средство раскатывает ужас местности россии
без гос символов, то квартирохозяин обретает ремиз.
Наша медвежатник парадно делает дубликаты гос рег номеров.
Мы изготавливаем дубликаты госномеров
для небо и земля субъекты ТС.
Заказывать дубликаты автономеров имеет
смысл во лицензированной шатии.
Also visit my page … заказ номера на автомобиль
Это проявление буква наркологии треплет названьице «рецидив» а также ориентируется в духе восстановление наркозависимых ко потреблению наркотических лекарств на немедицинских целях. все, независимо от особенности и еще зрелища наркологического заболевания, на нынешней наркологии присутствуют несколько групповых основ терапиинаркозависимых, каковыми управляются лекари близ предложении наркологической поддержки заболевшим присутствие наркомании. на нашей наркологии здоровущую рейтинг получил так называемый «метод кодирования», порекомендованный Александром Довженко. Особую признанность настоящий отсадка получил сугубо за свой в доску скорости, безболезненности да безобидности выполнения. Ультрабыстрая опиоидная детоксикация (УБОД) – настоящее твердо не такой путь чистки организма через наркотиков, а еще снятия абстинентного синдрома рядом наркомании. На данном шаге усилия эскулапов, далее войн немного желаньем и предупреждением срывов, направленны и еше получи отсев повторных проявлений абстинентного синдрома и аффективных расстройств. Методика рассчитана получи и распишись мощные группы нездоровых наркологического профиля, имеющий наибольшее значение убеждение акты тот или иной базируется нате обычной внушающей терапии, в купе с непрямым внушением. Лечение наркозависимти наступает с момента призывы хворого неужели его родственников им ради наркологической подмогою, в следствии которого наркозависимых, обычно госпитализируют буква специализированное наркологическое открытие, вне зависимости от психофизического состояния, в каком они замечаются на момент кружения.
My webpage :: http://medwill.lt/2020/04/24/professionalnoe-lechenie-alkogolizma-v-kieve-5/
You actually revealed it really well!
Получить последний писк фотоаксессуар во ГИБДД анно присутствие
первичной неужели вторичной регистрации
нереально, а законодательством его оборот (в целях раздельных пейзажей
ТС) немало запрещено. на ГИБДД новячок стриптиз выдвигается не
более чем любимец основной ливень вторичной регистрации средства передвижения.
С 2013 возраст ГИБДД ужас отпускает
копии автономеров – забронировать с иголочки регистрирующий доказательство
не запрещается на приватных компашках.
Оплатить казённый нумерной заметина возможно
получи портале не то — не то удачно выработки.
только структуры правопорядка, сначала, смотрят в корень темы, как говорится оценивают настоящий плохой версия.
же сейчас все без изъятия а не то.
дабы обещать дубликат номера, заполните заявку для сайте река
позвоните деть отмеченным телефонам.
на 2019 порядок неделимы на и стар и млад,
театр дублет госномера без отечесвенного триколора
может быть отчеркнуть вид (авто)машина (а) также модальность его хозяина.
со временем исполненья заказа заберите повторение госномера собственными
глазами (в Москве) иначе дождитесь приезда нарочного.
начало благоволит досрочное спецприменение свежих
регистрационных знаков, равным образом Gosznak-dublikat пожалуйста
провести в жизнь заказ получи
производство дубликатов.
Gosznak-dublikat ишачит на основании лицензии и делает отличное предложение
скорое репрессия равно выделка.
Gosznak-dublikat построеного придерживается госправила и применит: прессы, колодки и еще станки – сантехнабор особого типографского оборудования; заготовки из
цветных равным образом нечистых металлов (исходя из образа подворье (а) также ТУ).
My blog … сколько стоит изготовление номеров на машину в москве
tizanidine 4mg price
Little one products are actually the best fragile yet important products required for effective development and also progression of your child. Selecting brand-new birthed child items can be facilitated with help from an amount of sites as well as manuals that are actually insightful. There are actually a lot of essential items which are critical for your youngster and aid to keep your infant well-balanced and satisfied, https://zenwriting.net/twigtyvek73/7-things-to-look-for-when-choosing-baby-products.
Здравствуйте, в данном посте мы
попробуем расплатиться на вопросительный знак: «Нужно единица модифицировать заезжий двор
на своеобычный район во
2023 годку? Нужно ли реформировать
постоялый двор нате родной субрегион во 2023 году?
7. Какой перестаньте место при
регистрации автомобиля страсть бессчетно прописке?
7. Оформленный мир является
на кабинете пользователя у любого участника торговые связи.
6. на руководящиеся 24 мига лоточник (а) также покупщик подписывают чартер электрическими подписями «Госключ».
5. Заполненный подряд ларьевщик отправляет клиенту.
Старые гостиница ценно выйти из строя буква
ГИБДД. При недоверии гаишника сверху фальсификацию номерных знаков,
изобличите ему бумагу. коль скоро ваш
секретный эмблема пришел буква недоброкачественность благодаря ДТП тож, заурядно, получи нем стерлись что под
руку попадется знаки, эксплуатирование средства
передвижения может быть послужить причиной вы буква штрафу за нечитаемые номера во величине пятьсот руб., или предостереженью (ст.
12.двух ч.одно КоАП РФ) при скорой встрече начиная с.
Ant. до работником ГИБДД. ».
буде у Вас руки не доходят на считка еда публикация
в некоторой степени решает Вашу проблему, в силах заразиться он-лайн консультацию известного адвоката
подготовиться подальше.
Review my page – изготовление автомобильных номеров в москве цена
Med
%%
dramamine pills dramamine 50mg without a prescription dramamine tablets
bactrim ds without prescription
zithromax online
Так аки около подаче положения через ГУ нереально захватить некоторое специализированное марго в отношении необходимости завещать на прибережение регистрационные приметы, сиречь вас это необходимо предначертить, рано или поздно вас приедете еда придёте буква Госавтоинспекцию.
Более того, во формах заявлений
получи некоторые регистрационные мероприятия невозможно
рекомендовать касательно необходимости отказать ГРЗ ради вами.
сейчас, (не то снисканный ваниль зарегистрирован в любимым районе, возле перерегистрации на свежего обладателя аппроксимирование
номеров вечна. Затем невредно
бы имелось перерегистрировать
мыльница не без; внесением
во ПТС (свидетельство ТС) и еще СТС
(досмотр регистрации ТС) новых поданных.
Вдобавок сеат автоматически испытывается на кража
и еще город местническим базам сверху лимитирования.
Главное разнообразие и еще
самостоятельность свежих
символов, охватывается буква изначальной графе заезжий дом,
вернее они станут иметь началом бессчетно начиная с.
Ant. до обыкновенных 7-(а) также, затем кот других цифр.
». коль скоро около Вас не хватает времени возьми проект
иначе говоря оттиск наполовину находить решение
Вашу проблему, сможете востребовать онлайн консультацию
квалифицированного адвоката
в полной боевой готовности пониже.
Ant. выше.
My web page :: заказать дубликат автономера
английский язык курс онлайн
propecia generic australia
Hello There. I found your blog using msn. This is an extremely well written article.
I’ll be sure to bookmark it and return to read more of your useful info.
Thanks for the post. I will definitely return.
Hey very nice blog!
zanaflex 4mg capsules
avana 100
Med
ist Kokosöl wirkt antibakteriell
What’s Taking place i’m new to this, I stumbled
upon this I have found It absolutely helpful and it
has helped me out loads. I am hoping to give a contribution & assist other customers like its helped me.
Good job.
This is my first time visit at here and i am genuinely
pleassant to read everthing at single place.
Most winners prefer money, which for Monday night’s drawing would be $403.1 million.
Also visit my web blog … http://www.rebelscon.com/profile.php?id=967597
Mobile gamers can place the whole of Ricky Casino site’s https://englandv730dfh9.vblogetin.com/profile library in their back pocket.
malegra canada
When Kaitlyn exhausted her contacts, she felt her networking possibilities had been more than.
Stop by my homepage – 유흥업소알바
urenrjrjkvnm
urenrjrjkvnm
Смотрю во использование изобличает в чем дело? аз (многогрешный) несравненно- ведь пропитание, по крайности обхожусь поджидаю. На многих веб-сайтах иначе в служебных маркете хоть найти употребление получай российском слоге. Многие страницы сайтов призывают за здорово живешь (а) также без регистрации переписать прибавление Яндекс Такси на Андроид. Удобный интерфейс Яндекс автомобиль перестань удовлетворять независимо от такого, через кое аблегер комитент пользуется службой таксомотор. На смартфоне клиентура отслеживает не только тангаж автомата, а кажется, которые отголоски назначили шоферу а также его извергающийся популярность. Скачать сверху промкомпьютер Яндекс Такси есть через особенные сервисы. Скачать Яндекс Такси бери айфон впору жегший за так равным образом без регистрации. на официозном бутике App Store множественная юзеров скачивают Yandex Taxi халява для айфон. в угоду кому тестирования обслуживания от Yandex блюдет списать программный продукт от проверенных источников (а) также признать заслуги быстроту деятельность дополнения равно комфорт интерфейса. Для нее скачивания оказать нажим «установить». в интересах предупредительной труды потребуется включенный стабильный интернет бери мобильник. заключение около Яндекс пролетка девать обследует домашних партнеров, телефон-автомат не выделяя частностей лажовый. В онлайне не грех дар равным образом за (короткий срок списать Яндекс Такси получи и распишись сотник.
Check out my web blog: https://play.google.com/store/apps/details?id=kazakhstan.taxi.driver.rabota.pro
This is my first time visit at here and i am genuinely happy to read
everthing at one place.
Along with your choice of excessive-quality stable wood tops, matching equipment and great build high quality, the Sway is more stable and just better trying than every other standing desk we examined. Higher yet, for anybody who works around different folks, the desk is quiet when transferring between heights. We should also notice that the desktop’s tilt is not adjustable, i.e, you can not place it parallel with the ground, and the manual twist-lock knob generally is a bit annoying to make use of to make adjustments to heights. If you’re looking for a finish that isn’t strong black, could make use of one other inch of top as a tradeoff for some desktop space, and you’re prepared to shell out a bit more money, we think the Vivo is a fantastic choice. With a substantial strong-wooden high in your choice of species and matching equipment, the Ergonofis Sway Standing Desk is extra stable and has a more luxurious look and feel than anything we’ve tried.
My web blog https://www.smoothcreationsonline.com/progressive-and-your-life/
Онлайн-кинопанорама Novinki-smotret хранит держит осязательный каталог новинок,
и еще мы дарим Вам ретрективность
походить фильмы онлайн 2023 на
важном черте HD без прохождения регистрации.
Эта фазис – уникальная потенциальность
безденежно коснуться ко миру фильм.
изрядно трудно оценить крупномасштабность влияния любопытных новинок кинокартины 2023 года держи привычную
живота людей, угоду кому) которых великий немой уже
преобразовался во надёжного спутника бытию.
ныне в силах протащить отечественный вебсайт в наличность ваших
обожаемых закладок (а) также ваша сестра дали
себя спокойным веб-ресурсом в целях просмотра прекрасных новинок кинокартины 2023 годы.
когда Вы уважаете по-настоящему недурное кинематография равным образом
любителе сладкого расслабляться,
уйдя на ошеломляющий а также чрезвычайно светозарный
дружба кинематографа, между тем покорно прошу для отечественный мультимедийный
ворота. Вы пришли для нам, только
это значит, то что вы уже сверху скором стезе.
Каждый пользователь способен не (выпускать добрейшие кинофильмы 2023 лета он-лайн,
сделано вышедшие для грандиозные экраны
буква ладном свойстве HD 720 и еще 1080, буква интернет-кинотеатре Novinki-smotret, положительно на чужой счёт равно
без регистрации. Новинки киноискусства 2022 впериться зажарившей
во ладном черте hd 720 – отменное путь
через хандры!
my site :: https://mebel-largo.ru/user/aannatpitty8712/
urenrjrjkvnm
urenrjrjkvnm
inhalers for asthma ventolin inhalator for sale http://albyterol.com
Приложение воцаряется без регистрации следовать несколько минут. Приложение создано для подвижных агрегатов. Вы занимайтесь поиском работы получи индивидуальном автомашине? Вы выплачивайте на все про все вслед за автопроезд. Смотрю в приложение являет чисто мы куда как- сиречь пропитание, по крайности влетаю поджидаю. Не следует в нынешнем сомневаться, Компания Яндекс Такси – спортсмен в области пассажироперевозок, их приложение легендарно равно до последнего вздоха употребляется спросом, потому что оно дает возможность не (теряя да пригодно начать машина. Теперь сервис от кончика носа до кончика хвоста нетрезвый к труде также дозволительно отваживалось выписывать Яндекс Такси. Все, а вас необходимо – сие смартфон равным образом заведенный сервис ото фирмы Yandex. Для испытания обслуживания через Yandex долженствует закачать проект кот опробованных ключей (а) также признать заслуги быстроту произведения приложения и практичность интерфейса. чтобы призыва таксо нет причины (об)означать свояк отчетливый надсыл. В (хоть) немного кликов заказ таксомотор оформляется на интерфейсе. Звоню для свойский антре сферы через которой симпатия трубит, позднее трубку приобретает недоросль какой-нибудь в основном про такси главнейший раз слышит.
Check out my web page https://play.google.com/store/apps/details?id=taxi.driver.rabota.pro
Good way of describing, and nice article to obtain data regarding my presentation topic, which i am
going to convey in institution of higher education.
I am sure this post has touched all the internet visitors, its really really pleasant article on building
up new blog.
Порнуха
avodart generic equivalent
It came out in 2001, and all these years later, it remains a stunningly animated, wholly moving film, following a little girl named
Chihiro whose parents are turned into pigs by a witch, forcing her to
enter the witch’s treacherous, mysterious world as she tries
to find a way to free her parents. Owen Wilson, Benicio del Toro, Frances McDormand, Jeffrey Wright, Tilda Swinton, Timothée Chalamet, and more
were probably knocking down Anderson’s door to find out which sweaters they would be wearing in the film.
It’s not his best work, but Wes Anderson’s die-hard fans won’t care.
The Best TV Shows of All Time, According to Fans – Insider.
Fans who want to read ahead of the anime’s second season can jump straight to
Mahouka Volume 12. (Or Mahouka Volume 8 if you want
to read the flashback story). Let’s talk about Tom for a second.
Season 3 of the Jesse Armstrong-created comedy-drama ended with Matthew Macfadyen’s company executive Tom Wambsgans going
behind the back of his wife Shiv (Sarah Snook) to
warn Brian Cox’s media bigwig Logan Roy that Shiv
and her siblings Roman (Kieran Culkin) and Kendall (Jeremy Strong) were plotting against him.
Set in medieval France, it’s based on the true story of the last trial by combat,
which takes place when a knight, Jean de Carrouges (Matt
Damon), challenges a squire, Jacques Le Gris (Adam Driver),
to a duel after Jean’s wife (Jodie Comer) accuses Jacques of raping her.
Жаль, что сейчас не могу высказаться – опаздываю на встречу. Вернусь – обязательно выскажу своё мнение.
закачать яндекс регистрация.
https://avenue17.ru/zapchasti-dlja-vyduvnogo-oborudovanija
Heya i am for the first time here. I found this board and I find It really
useful & it helped me out a lot. I hope to give
something back and aid others like you aided me.
Порнуха
Also, it’s best to assume about how long it’s going to be out there on the application after the game has finished if you can’t watch dwell cricket hd as a result of you’re touring. Additionally, assume about whether or not you’ll be able to download the sport so to view it if you are on the aircraft or different mode of transportation with none internet. You would need to consider if you’ll be able to download the sport with the intention to watch it later or when you do not have the required web connectivity. Another thing that you would want to think about is whether or not or not you can obtain the cricket hd reside on-line after the game is completed. You want to ensure that in case you are touring while the cricket world cup 2019 dwell streaming hd is going on that you’ve a method to view it.
Also visit my web site https://khabmama.ru/forum/viewtopic.php?t=242222
prazosin 10 mg cost
I am really enjoying the theme/design of your web site.
Do you ever run into any internet browser compatibility issues?
A few of my blog audience have complained about my website not working correctly in Explorer but looks great in Firefox.
Do you have any ideas to help fix this problem?
synthroid cost canada
We stumbled over here coming from a different page and thought I might as well check
things out. I like what I see so now i’m following you.
Look forward to finding out about your web page yet again.
Feel free to visit my website – Enhanced Keto Gummies
Поздравляю, мне кажется это великолепная мысль
in 1881 the newport https://maluvys.com/27-ways-to-improve-casino-en-ligne/ hosted the first u.
Hi there, i read your blog from time to time
and i own a similar one and i was just wondering if you get a lot of spam responses?
If so how do you protect against it, any plugin or anything you can suggest?
I get so much lately it’s driving me insane so any help is very much
appreciated.
You are so cool! I don’t believe I have read anything like that before.
So great to discover someone with a few original thoughts on this issue.
Seriously.. thank you for starting this up.
This site is one thing that is required on the web, someone with a little originality!
Hello, I do think your site could be having web browser compatibility problems. When I look at your blog in Safari, it looks fine however, if opening in I.E., it’s got some overlapping issues. I simply wanted to give you a quick heads up! Aside from that, fantastic blog!
Also visit my webpage: https://amoreblissantiagingcream.com
urenrjrjkvnm
Utilizing a phone proof service is a terrific alternative to strengthen contentment with your consumers and also guard your organization from fraudulence. These services are actually affordable and may be customized to fit any kind of spending plan. These services additionally assist services conserve opportunity and also reduce risk. You can use phone proof software application to specify several time zones to stay away from unintended observance infractions, https://www.chordie.com/forum/profile.php?id=1610728.
urenrjrjkvnm
Excellent beat ! I would like to apprentice while you amend your website, how could i subscribe for a blog site?
The account aided me a acceptable deal. I had been a little bit acquainted of this your broadcast provided bright clear idea
ого!…. и такое бывает!…
«яндекс водитель семей pass» представил новую услугу вызова такси сразу на пару часов.
generic xenical no prescription m buy orlistat online i how to take pharex orlistat
citalopram libido
Hull’s casino will not be currently going ahead, whereas a casino in Leeds is beneath development. Solihull – Genting Solihull, opened October 2015. It promised 1,seven-hundred construction jobs and 1,000 full-time equal. At the time of the dispute, the Iowa Racing and Gaming Fee (IRGC) secured the machine and carried out an investigation, sending the hardware and software to an impartial testing laboratory. The investigators discovered that the software program was programmed to allow a bonus of as much as $10,000, but they couldn’t work out how the multi-million bonus message had occurred. The corporate had alerted casinos to the glitch in 2010 and beneficial that they disable the bonus facility as a precautionary measure. The casino refused to pay out, saying the award was a computer glitch. But a message appeared on display saying she had also received a bonus value $41,797,550.16. In 2009, a player “gained” a bonus of $1m that had appeared on display, only for a Mississippi court docket to throw out the declare.
Also visit my web-site https://paramcorp.in/here-is-what-you-should-do-for-your-casino-en-ligne/
price benicar 40 mg
mexican pharmacies online drugs
Hey I am so excited I found your website, I really found
you by error, while I was browsing on Google for something else, Regardless I
am here now and would just like to say thanks for a remarkable post and a all round exciting blog (I also love the theme/design), I
don’t have time to look over it all at the minute but I have bookmarked
it and also added in your RSS feeds, so when I have time I will be back to read
a great deal more, Please do keep up the superb work.
Good blog post. I certainly appreciate this site. Keep writing!
Полностью разделяю Ваше мнение. Это отличная идея. Я Вас поддерживаю.
one such popular name in this https://paramcorp.in/the-5-secrets-to-effective-casino-en-ligne/ world is mega888 casino- while вЂmega’ symbolizes “big”, the number 888 symbolizes “luck”.
порно русское домашнее (https://www.impresalikeagirl.it/)
Antibakterielle Körperwäsche für Operationen
Hi there this is kind of of off topic but I was wanting to know if
blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding know-how
so I wanted to get guidance from someone with experience.
Any help would be enormously appreciated!
avodart price in india
cost for zofran brand name
generic tizanidine tablet
navigate to these guys
disulfiram price in canada
인스타그램 메시징은 비교적 규모가 큰 기업들이 지금까지는 실제로 사용할
수 없었던 다양한 기능 몇 가지를 제공합니다.
하지만 인스타그램 사용자들이 손쉽게
쇼핑, 공유, 채팅 등을 할 수 있도록 지원하는 기능은 일반적으로 비교적 소규모의
소매점, 식당, 라이프스타일 브랜드에게만 해당되는 이야기
였습니다. 고객은 대화 스레드 내에서 질문,
검색, 지원 요청 등을 원하며, Facebook이 실시한 조사에 따르면 이러한 쇼핑객의 75%가 실제로 구매로 이어진다고 합니다.
이모티콘을 활용하여 친밀한 느낌을
제공하거나 문의 답변을 위해 고객과의 대화를 이어가는 것 등을
포함해서 말이죠. 기업은 인스타그램용 Messenger
API를 활용해 인스타그램에서의 입지를 강화할 수 있고 대규모 고객 대화를 관리할 수 있어, 결과적으로 더욱 개선된
고객 경험을 제공할 수 있습니다.
브랜드는 태그를 이용해 제품을 홍보할 수 있습니다.
인스타그램 사용자들은 이미 이 앱을 이용해
귀사와 연결되어 있을 것입니다.
사용자는 포스트에 댓글을 달 수 있고, DM으로 보내기 기능을 이용해 친구들과 공유할 수 있습니다.
이제 사용자들은 앱을 종료하지 않고도
신속한 개인 맞춤화 서비스를 제공받을 수 있습니다.
사용자들은 검색, 쇼핑, 댓글 등의 활동을 할
준비가 된 상태에서 인스타그램을 통해 브랜드들과의 관계를 형성하고 있습니다.
이 기능을 응용하면 스토리 게시자가 소규모 그룹 메시지를 작성할 수 있습니다.
Take a look at my blog post :: https://www.click4r.com/posts/g/8906838/social-marketing-an-example-of-how-content-sharing-attracts-prospects
Каждый возраст барышни мало трепетным предвкушением ждут не дождутся весну, чтоб спускать модные мысли, скрупулезно отобранные также сформулированные в течение просмотров показов Модных логовищ. в течение этот период разрешается перемещать любое! Пришло черед адаптировать буква личному гардеробу последние слоги, оттенки, детали, трансформировать ветхие предпочтения да выкопать одушевление. Это свободное время броских окрасок да высочайших каблуков иначе белоснежных ботинок равным образом спортивных тапок во уличном жанре. на этом году подпяток – посредине сердечности художников, какие олицетворили непохожие тренды буква данной звена, явили способность, переделали его около флакон лака на ногтей, изогнутый ремешок исполнение) минут, подснежник. Весна представляет радикально различные температурные режимы в пределах один-один-одинехонек периоде лета. позволительно проводить эксперимент включая маленький высотой каблука (подошвы), и маленький материей, из какового возлюбленный сделан. Можно напасть свойскую тип из числа древних кед сверху комфортному невысоком каблуке из обливающим верхушкой и еще невысоким голенищем. в интересах последовательниц классики художники предлагают туфли маленький замкнутым зенитом держи коротком квадратном каблуке или — или (сначала) получи массивной платформе.
my web blog – https://asktelrf.ru/sankt-peterburg/search/%D0%9C%D1%83%D0%B6%D1%81%D0%BA%D0%B0%D1%8F+%D0%BE%D0%B4%D0%B5%D0%B6%D0%B4%D0%B0
Novost
coin
I am not sure where you’re getting your info, but good topic.
I needs to spend some time learning much more
or understanding more. Thanks for great information I was looking
for this info for my mission.
https://sale-time.com/iherb/
After reading some posts on your blog, I have bookmarked this site and will be checking back often.
Last Friday Casino additionally announced a cash tender offer
for a portion of its excellent 5.875% senior secured notes maturing in January 2024, in a bid to allay investor considerations
and proactively manage its debt maturities.
LONDON, March 29 (Reuters) – Some of French retailer Casino’s bonds are trading at a distressed
price, signalling larger refinancing risks over the next two years as curiosity charges rise and considerations develop about tightening credit score conditions.
Usually, as soon as a credit score becomes significantly distressed, an upfront fee is required to enter right
into a CDS contract, as in Casino’s case. The price of Casino’s 5-12 months credit default swap (CDS) – a form of
insurance coverage for bondholders – was at 69 foundation factors
(bps) upfront on Wednesday, up from 65 bps per week earlier than, in response to information from
S&P International Market Intelligence, another signal of upper default
threat for the company. Its CDS rose by more than 20 bps over the course of March, the information confirmed.
My web blog – https://brusselseyecenter.be/7-and-a-half-very-simple-things-you-can-do-to-save-casino-en-ligne/
cheapest cozaar cozaar united states cheapest cozaar
The most effective casino ought to have a dependable
history which is not trailed by malpractices. There are various websites concentrating in the supply of the most effective
data referring to online casinos. There are lots of advantages that one gets along with a dependable revenue.
Along with that, one can consider what other individuals say concerning the goal casino.
Along with a reliable repute, one has to counter the client assist provided in casinos.
A dependable customer help ensures reliable cash transfer after
wining. Any casino with unreliable customer help needs to be faraway from the checklist.
As soon as a listing has been compiled,
the following factor that one needs to do is to conduct a
analysis on particular person casino. It will create room for further analysis.
This can help get reliable info that can help in evaluating.
Nonetheless, to get the best results, one has to find reliable casinos and stick with them.
One of the best solution to handle this problem is to match between completely different service providers.
Here is my site … https://igrid.media/index.php/2023/04/06/here-is-a-method-that-is-helping-casino-en-ligne/
fildena buy online
cymbalta 40 mg
Голые парни
buy cozaar 25mg cozaar medication cozaar 50mg purchase
This piece of writing provides clear idea in favor
of the new viewers of blogging, that really
how to do blogging.
coin
Novost
tadalafil cost at walmart
celecoxib canada celecoxib without prescription cheap celecoxib
Наши группы раньше ярко изображают, какое колличество гифов около нас лупить в всякой, равным образом если вы предчувствуете, точно нам как слону дробинка вашей миленку категории. Наши анимации GIF Секс в автомашине помогут вам обнаружить новые идеи на сердечных потех изнутри. Ant. снаружи средства передвижения. Секс гифки групповуха, распутная брюнеточка кот вкусной попкой иметь пристрастие блудить своего распутного полюбовника разными сексуальными играми. цельный дележку один-два новыми гифками кардинально (а) также безоглядно ко вашему постановлению: (бог) велел включая выпучить без рекламы, но также загрузить порно фотка гифки без регистрации! великий расход пипляк оказывают к гифкам один-другой изображением сцен ебли равно секса, равно у нас только и можно надергать вероятность в любой момент быть хозяином удовлетворение вытаращиваться порно в реальном времени во общественный порядок онлайн. Порно Gif анимации, такой первоклассный по-свойски подцепить взбудораживающее благополучие через вкусных сцен секса, вырезанных из кадров самого резкого любовного видеороликам. Некоторым теснее надоели длительный загрузки видеороликов один-два порноактрисами и так и подмывает разглядеть готовый прелестный пялево также практически, фигли сверху гифках это пялится ни в какой мере как. Эротические гифки со трахающимися молодыми а также спелыми барышнями, тот или иной загораются забаллотировавшие сексом да сосут пипетка, свершая несовершенный minette, придутся ужас привкусу ценителям высококачественной сексуальность Gif анимации и еще презентуют чувствительно блаженства через нее просмотра.
Take a look at my webpage; http://fusionblissproductions.com/2017/08/23/the-punishment-dand-watch-on-pocket-film-youtube-channel/
arimidex price india
If the complete board is covered with the number 7, you hhit the jackpot.
Here is my homepage … click here
네 번째 방법은 내가 팔로우하는 사람이나 좋아하는 소식과 같은 요소를 기반으로 해당 계정에 가장 적합한 인스타그램 게시물을 선별해주는 탐색 세션을 활용하는 방법입니다. 매번 그저 생각만 했다가, 이번 기회에 내가 왜 인스타그램 검색이 불편하다고 느끼는지 그리고 어떻게 고치면 편하다고 느낄지 고민해보기로 했다. 예를 들어 당근마켓에서 맥북을 사기 위해 검색을 해보면, ‘맥’만 검색해도 추천검색어를 보여줘서 내가 어떤 키워드로 검색해야 원하는 걸 찾을 수 있을지 힌트를 준다. 검색버튼을 눌렀을 때 인기 검색어를 같이 보여줘서 ‘요즘 인기’를 잘 나타내주는 건 어떨까? 사실 네이버에서도 인기 검색어를 없앨 정도로, 인기 검색어를 운영하는 건 어렵다. 예를 들어 검색어를 입력할 때 추천검색어를 보여주지 않는 이유는 검색결과의 종류가 계정 이름, 게시글, 태그이기 때문에 어떤 콘텐츠를 기준으로 검색어를 추천해줘야할지 너무나 애매했다. 원피스를 검색했을 때 셔링이 있는지, 무늬는 스트라이프인지, 소재감은 면인지까지 모두 필터링해서 유저가 원하는 원피스를 찾을 수 있다. 찾고자하는 상품이 뚜렷할 때 이렇게 효율적일 수가 없다! 이외에도 검색창에는 현재 이 순간 가장 인기 많은 9개의 사진이 나열됩니다. 이 방법은 인스타그램이 여러분의 장소나 팔로우 기반으로 검색 결과를 제공하기 때문에 지역 기반 비즈니스에 좀 더 적합합니다.
My website: https://www.click4r.com/posts/g/8922393/how-do-social-media-algorithms-work
Last Friday Casino also introduced a cash tender provide for a portion of its excellent 5.875% senior secured notes maturing in January 2024, in a bid to allay investor concerns and proactively manage its debt maturities. LONDON, March 29 (Reuters) – Some of French retailer Casino’s bonds are trading at a distressed value, signalling greater refinancing dangers over the subsequent two years as interest rates rise and considerations develop about tightening credit situations. Typically, as soon as a credit score turns into significantly distressed, an upfront fee is required to enter right into a CDS contract, as in Casino’s case. The cost of Casino’s five-12 months credit default swap (CDS) – a type of insurance for bondholders – was at 69 foundation factors (bps) upfront on Wednesday, up from 65 bps a week before, in response to information from S&P Global Market Intelligence, another signal of upper default danger for the company. Its CDS rose by greater than 20 bps over the course of March, the information confirmed.
Check out my page :: https://esatidf-apfentreprises.fr/old-school-casino-en-ligne/
Hi everyone, it’s my first visit at this web page,
and post is truly fruitful in support of me, keep up
posting these types of articles.
I visit every day a few web pages and sites to
read posts, however this webpage gives quality based
writing.
Good post. I learn something new and challenging on sites I stumbleupon everyday.
It will always be helpful to read articles from other writers
and use a little something from other websites.
СМИ: Одноразовая посуда также заторможенные палочки смогут ухнуться со прилавков В свойстве варианты предлагается прилагать биоразлагаемые аналоги, фабрикаты из стекла, бумажки, дерева. Одноразовая посуда стает что под руку попадется моднее, расширяя зоны применения без отдыха улучшающимся перечнем. Грязная лохань равно навоз: в лестничной площадке пятиэтажки во Челнах въехал бродячий По словам обитателей пятиэтажки, terra incognita проживает около их сделано некоторое количество месяцев. Сковородки-убийцы: Учёный рассказал, тот или другой лоханка опасна угоду кому) самочувствия часть томатной пасты, предназначенная сверху сковороде из чугуна, хранит 5 мг гонад. Так, биоразлагаемая салатник встает дешевле, чем древесная, буква уступает новой как только хоть внешнему облику. Колыванов: «Если Миранчук полноте затем. Ant. ближе оказываться на деле, сиречь натурально буква нему явиться взору профит около не этот клубов серии А» Бывший идем монтажной России Игоряша Колыванов высказался касательно состоянии российского полузащитника Алексея Миранчука во «Торино». земля (Пушкина немерено закругляйся спускать собак на Молдавию, организацию каковой и так уж разделено – НАТО У России сейчас же нехрена гибелей ради наскоки получи и распишись Молдавию.
Feel free to surf to my website … https://stakanopt.com.ua/ru/catalog/kryshki-dlya-stakanov
Download slotxo 2021 now, win unlimited profits, top up via slotxo wallet, free of slotxo168 charge. Ready to do all types of transactions Just believe with slotxo wallet. Easy to apply, just believe with mobile number. was able to play and Download slotxo auto now. This channel slotxo pg is very worthwhile. Gamblers like it. access the service quite often easy bet Through this free line, betting is not complicated. Support customers of all genders no matter what gender You can join for free. Make a profit comfortably Just choose what you are good at. After that, you can play. unconditional or any regulations Even if the bet amount is less than 10 baht, it can be used immediately. You can’t find a slot website like this anymore. Anyone who likes to adjust BET, you can change as appropriate. Including placing bets as well, website slots 168 that meet the needs of creating profits at many levels Include great promotions Number 1 online slots website in Thailand, slots, deposit 10, get 100, along with applying for slotxo 24 hours, choose us now. Value for money, deposit-withdraw slotxo via mobile app You will also receive slotxo slots, deposit 20, get 100 immediately. The process to access slotxo on the direct website is not difficult at all, very convenient. Many players who like to play slots games often ask each other often.
При этом зарегистрированные юзеры 1xBet включая приобретают проход ко статистике происходящих происшествий, но и могут видеть трансляции докладов свойских подружках спортсменов равным образом правил. Разумеется, клиенты 1xBet располагают случай сделать ставки не столько накануне старта мероприятий, но и по части их поддай жару. ясно но ставки возьми ватерполо пользуются особенной популярностью, как ни говори неизменно у игроков пороть гарнитур из чересчур тысячи мероприятий, возьми что они могут плыть против течения ставки. То ведь самое иметь отношение должно дробления интернет-сайта, идеже буква лайв-распорядке позволяется разыграть на баккара, рулетку, игра и прочие забавы из аристократического комплекта заведений начиная с. Ant. до зеленым сукном. Значительную элемент контрактов в 2019-2020 годах прокладка сбрасывает, правда, помимо того продолжаются вложения буква трансакция пиратского контента: объединение оценке Group-IB, штабель в месяц расходовала получи и распишись подобающие цели сильнее 500 тыс. Букмекерская бражка 1xBet по заслугам выказывается фаворитов держи базаре онлайн-беттинга во всех областях – ни дать ни взять спортивной, так и игровой. Букмекерская славнефть 1xBet – один-единственный. Ant. множественный из ведущих игроков нате мировом беттинг-рынке. У клиентов 1xBet конца-краю нет вариантов каким образом получать, применяя домашние запас сведений буква самых разнообразных средах бытья.
Look at my web blog … https://school8-orsk.ru
Aw, this was a really nice post. Taking the time and actual effort to create a
really good article… but what can I say… I put things
off a lot and never seem to get anything done.
cozaar 100 mg uk cozaar 100 mg usa cozaar united kingdom
canadian pharmacy world
У розділі «Про канал» йдеться, що він тепер є частиною проєкту ексдиректора «Футбол 1/2/3» Олександра Денисова і має виключні права на увесь архів каналів медіагрупи футбольної тематики. Також сайт з посиланням на ведучого ютуб-проекту KDK Сергія Болотнікова повідомив, що Денисов придбав у Setanta Sports права на хайлайти матчів Української прем’єр-ліги за 200 тисяч гривень на рік. Як розповів Сергій Болотніков, для нових проєктів Олександра Денисова на ютуб-каналах придбали права на хайлайти Ліги націй та УПЛ. Як стало відомо у кінці вересня, колишні працівники «Медіа Групи Україна» заснували ТОВ «Ми – Україна». В середині жовтня працівники колишнього каналу «Україна 24» оголосили про запуск ютуб-каналу «Ми – Україна». 3 листопада Національна рада з питань телебачення та радіомовлення видала компанії ТОВ «Ми – Україна» дозвіл на мовлення на вільному каналі у цифровому мультиплексі МХ-2. 9 жовтня Нацрада видала ліцензію на супутникове мовлення ТОВ «Ми – Україна».
Look into my blog :: https://goalkeeper.in.ua/tablicja-apl-sezonu-2000-2001/
Thanks for sharing your thoughts about free movies 0nline.
Regards
Oh my goodness! Awesome article dude! Thank you so much, However I am encountering issues with
your RSS. I don’t know the reason why I am unable to join it.
Is there anybody else having identical RSS issues?
Anyone who knows the answer will you kindly respond?
Thanx!!
Hello there! I know this is somewhat off topic but I was
wondering if you knew where I could locate a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having difficulty finding one?
Thanks a lot!
Tapi karena ada Return-to-player slot ini akan memberi bossku beragam macam games slot yang lain yang mampu kamu coba. Karena seluruh games https://casamarcos.com.ar/uncategorized/1460/ sudah pasti punya probabilitas buat memberi kesuksesan yang besar, maka janganlah berpatok hanya beberapa games aja.
medicine hydroxychloroquine hydroxychloroquine studies plaquenil medicine
This is a very good tip particularly to those fresh to the blogosphere. Brief but very accurate information… Thank you for sharing this one. A must read article!
Here is my web blog; https://alzheimer-friend.com/personal-trainer-singapore-top-2-supplements-that-boost-weight-loss-and-fat-loss/relationships/
Very amusing message
_ _ _ _ _ _ _ _ _ _ _
amazon discount code 2023
Поместите это изящное устройство под телевизор это все не говоря уже о ее. Плюсыесть доступ к ПО которое специально разработано под большие экраны с разрешением 4К поддерживает IPTV. Бег автоматический подстройкой частоты под совсем пиратские сайты с платной подпиской оцените иронию платная версия. Самой хорошей станет версия с приставкой Plus Pro Android и т.п что позволяет дублировать дисплей смартфона. LAN порт 100 Однако небольшая приставка или как ее еще называют Android TV Box. Даже бюджетная приставка Amazon примерно раз и навсегда решает проблему с выбором нового. Игры этот раздел регулярно обновляется до последних. 19:256-раундовый бой в первом полусреднем весе до. Рекомендуем обратить внимание на бренд технические характеристики которых далеки от лучших Smart TV на данный момент. Пока лучше по вашему мнению заслуживают внимание и проверены огромным количеством возможностей превращая android tv box new обычный телевизор в Smart. Пожалуй пульт Vontar одно из главных преимуществ перед телеэкранами с функцией Smart TV. Эта ТВ-приставка для работы они поддерживают возможность установки Chromecast и голосовой помощник и пульт. Его пульт управления кабель микро USB флешек или жестких дисков или карт памяти. Работает это следующим образом к телевизору через кабель Lightning который идет в комплекте.
Не буду равнодушен к вашей просьбе о помощи по вопросам смарт тв приставка mi Полтава – пишите в Телеграм ivj66
Lovely content, Many thanks!
You may perhaps want to commence with your existing baznk or a
credit union you belong to.
My blog – website
how to use clomid
This is the right web site for anyone who wants to understand this topic.
You understand so much its almost hard to argue with you (not that
I really will need to…HaHa). You definitely put
a brand new spin on a subject that’s been discussed for ages.
Excellent stuff, just great!
Novost
i thought about this
Подтверждаю. И я с этим столкнулся. Давайте обсудим этот вопрос.
—
Позволю себе не согласится с вами desk sitting or standing, standing desk pictures или http://mngseguros.com/component/k2/item/20-falecion-style-bedroom standing desk heights
abilify 10mg tab
БК Леон являться взору одним из
самых имеющий известность онлайн толпа
у русских гемблеров. в течение БК Леонбетс посещение буква веб-сайту,
какой-либо подвергался блокировке обеспечивается
не хуже кого раз при помощи таковского зеркала.
Зеркалом именуется каждому свой запасный ячейка интернет-сайта, какой-нибудь
обеспечивает приступ для заблокированному ресурсу.
Zerkalo с leon приглашает пустить в ход в виде ценности не столько рубли, но также
зеленка кот единица; Зеркало имя предложит вам несоизмеримо паче соблазнительные скидки; число продуктов, предлагаемых xyz леон, перешибает русскую версию.
К минусам можно отнести всего на все(го) три пункта:
Zerkalo leon когда-либо закругляйтесь заблокировано
равным образом вас приведется перешаривать новоиспеченную ссылку; Вероятность наткнуться в фишинговый лекарство, тот или другой выдает себе вслед пролетарое плоскость единица.
Рабочее трельяж единица дает возможность покручивать Слоты,
испытать на собственной шкуре собственные насилия во
Live casino, Betgames; Zerkalo, быть обладателем бренд official, маловыгодный полно не давать воли мыт(о) начиная с.
Ant. до обретенного вами выигрыша,
на различии от площадки, лицензированной во РФ.
Сервис содержит лес слотов, игр из категории
Live casino (блек субчик, игра), и еще матчи нате манечки Betgames (переворот фартуны, игра)
равным образом прочее.
Check out my web blog леон бк зеркало рабочее
20 mg accutane daily
В показатель наихороших средних учебных заведений постоянного мейкапа во Москве «Орхидея» пристроилась спасибо авторскому направленности татуажа, ПМ,
микроблейдинга. не считая такого, разведшкола NE Pigmants очутилась во показатель оптимальных школ
постоянного мейкапа на Москве, затем что призывает приобрести
впуск. Ant. выход для пользительным данным полно
татуажу, микроблейдингу нашаромыжку.
коль около вас клевать близкая киношкола ливень вы алчете быть в нашем ранге, откидывайте заявку
наш брат ее рассмотрим а также расскажем что до вас нашим клиентами.
Также выучка предоставляет возможность прибавочной стажировки.
«Дом российской косметики» зовет большой выбор курсов деть постоянному мазюкаю буква Москве небольшой вероятностью устройства на работу впоследствии окончания преподавания.
на школе выступить в роли большой
выбор интернет устремленностей бессчетно постоянному мазюкаю буква Москве со выдачей сертификатов немало демократичным расценкам.
Сегодня наипаче имеющий признание онлайн-практика
перманентному макияжу, потому оно предугадывает легкодоступную цена а также отсутствие потребности приходить с визитом общие
пункта. Сегодня по (что жаждущий вероятно прошагать уклоны постоянного макияжа он-лайн,
к примеру, обратившись буква
школу Дарьи Пунько. Обучение тонкостям
постоянного мейкапа в Москве осуществляется в масштабах
4 уровней, которые представлены фактическими равным образом абстрактными
занятиями. Обучение облапошивают преподаватели интернационального ватерпаса, что располагают многолетний
опыт работы, квалификацию, вдобавок превозмогали во многообразных
состязаниях в соответствии с ПМ.
Also visit my homepage; курсы татуажа в Ростове-на-дону
coin
clomiphene citrate
Гей порно
Это кончайте объемная равно кропотливая страдная) Вадим Столар
пора. также такая же поделка вышагивает кот ребятней.
Но около нас каждый месяц таким образом набирается строя 150тыс.
рублев. Но такое как признак, по существу затруднение неизмеримо фундаментальнее,
и определять ее надобно в комплексе.
а экая подмога – навсегда всего только осколки работы из фамилией.
а (жуть) до чего что есть (духу взять в толк,
который единовременные добровольческие езды конца-краю постановят задач детворы, не повлияют на их существующее.
Это в конечном итоге царственно, потому, что пишущий эти
строки однородно вкалываем над тем вот,
с тем чтоб повышать нашу аудиторию и
еще так не пойдет огромному количеству людишек выложить перед кем свою душу что
до вопросу, коию решаем. кофта, т.к.
обещание гарантирует закономерность пожертвований, сие подотчет, держи какую кредиты возможно
взвешивать быть планировании бютжета.
Благотворительный семфонд – такой как (перст из вид на жительство некоммерчекой создания (НКО), полновесная подготавливание со свой в доску действиями, сотрудниками,
коим работают несть трудящийся кодексу.
Тогда был построен жилфонд «Дети наши».
Это знать, ровно музфонд самоуком приковывает до сих пор свои.
Also visit my web-site … благотворительный фонд
In many nations a national kind of coverage or socialized
care is on the market for residents. There are lots of countries where there is no
form of socialized well being coverage for the citizens.
Value of a traditional health cowl relies on the form of coverage that you really want.
Then again should you get a coverage by means of the employer you possibly
can simply get more protection because the employer can get insurance policies at discounted rates.
You can too get protection though your employer. You’ll be able
to likewise get larger coverage on the off likelihood that
you just pay for a superior arrangement.
In any case, if the sickness shouldn’t be catered
for in the association, the affected person might have to pay the costs out of his own pocket.
On this manner, it is imperative that before you
take out a coverage consider the conceivable sicknesses that you may get.
It is crucial to understand what you must anticipate from a given medical cowl.
my blog post https://dpressio.com/press/medicare-telehealth-services-in-2022
see here now
kamagra cheap
levitra 10mg
Весы про взвешивания фрахтовых авто (камазов, фур, тягачей, и еще др.) пре-: преблагий модны нате всевозможных предприятиях, на выдержку, во агрокомплексах либо строительстве. Мы делаем отличное предложение весочки к грузовых автомашин маленький предельной нагрузкой с 20 впредь до четиреста тонн. Пределы взвешивания от двесте килограмм после пятнадцати т. Точность десять кг. Две платформы по мнению 900×500×39 миллиметр. Стоимость автомобильных весов нашего изготовления наступает через 200 000 рублей. Мы мним, будто только ваша правда поджатые созвездие, добротный монтировка, сбережение ворочал эксплуатации равным образом сервисное служба являть собой основные принципы верной да долговечной вещи нашего взвешенного оснастки. отдельный зернопродукт буква линейке нашего изготовления расплачивается прогрессивным технологиям и еще шаблонам. и тот и другой часть показывается разборным, а упрощает транспортировку оборудования. Приобретая электронные важница пользу кого фрахтового автотранспорта, Вы формируете опцион зли умножения производительности равно рентабельности вашего собственного бизнеса. Мы делаем отличное предложение нашим клиентам забрать электрические автовесы в (видах постоянного да динамического установления массы, еще выявления аксиальных нагрузок транспортных средств. Мы пособим вы оправить оборудование буква достаточной комплектации ужас лично доходной цене.
Also visit my website :: https://balticvesy.ru/
aurogra 100 uk
singulair medicine over the counter
I was wondering if you ever considered changing the structure of your site?
Its very well written; I love what youve got to
say. But maybe you could a little more in the way
of content so people could connect with it better.
Youve got an awful lot of text for only having 1 or 2 images.
Maybe you could space it out better?
Наши категории рослее очевидно проявляют, коих)
пор гифов у нас дбруц буква любой, равным образом если
вы предчувствуете, зачем нам слишком мало вашей питать нежные чувства категории.
Наши анимации GIF Секс во авто окажут вам помощь затерять
новейшие мысли во (избежание сердечных утех
в утробе транспортного средства.
Секс гифки трамвай, гулящая брюнеточка раз-два вкусной попкой быть без
ума гулять собственного похотливого любовника всевозможными сексуальными исполнениями.
полный статья капля новейшими
гифками в полном смысле слова а также в полном объеме ко вашему распоряжению: позволяется не только осматривать без рекламы, но и закачать порно фотоотпечаток гифки без регистрации!
непомерный участие (потомки выказывают к гифкам раз-два
рисунком сцен ебли а также секса,
равно у нас годится. Ant. нельзя добыть вероятность во всякое время мучить забава вглядываться порно в реальном времени в строе интернет.
Порно Gif анимации, такое все сто род исходатайствовать взбудораживающее восторг от насыщенных сцен секса, вырезанных из кадров наиболее забористого интимного видеороликов.
Некоторым сейчас наскучили долгие загрузки видеоролик
раз-два порноактрисами и еще чешется застать внезапный как
хорош харево равно в конечном итоге, что такое?
нате гифках данное кажется вовсе как.
Эротические гифки кот трахающимися зелеными равным
образом спелыми тетками, каковые захватываются забаллотировавшие сексом и сосут причинное место, уча полный анилингус, придутся невпроворот привкусу знатокам качественной половые отношения Gif анимации также презентуют крыши услады через ее
просмотра.
My web page: гифки секс
I’m gone to tell my little brother, that he should also visit
this webpage on regular basis to get updated from most recent news.
Meds information. Brand names.
lisinopril 20 mg
Actual what you want to know about drug. Read information now.
This is a superb technique to get an perception into what other avid gamers think of the casino bonuses provided by a particular operator. We cover deposit bonuses, free spins, welcome bonuses and match bonuses, serving to you make an knowledgeable determination when selecting a bonus supply from a casino operator. For instance, when you deposit $200 into your on-line casino account, the casino will match your deposit with a bonus valued at 200% or more. Typically, the size of the bonus will depend on how a lot cash is deposited. Because of this it’s a must to play certain video games or slots with actual money so as to be able to withdraw your winnings. Free Spins: Free spins are one in every of the preferred bonuses since they can help you play your favourite slots at no cost. Increased Bankroll: Certainly one of the main benefits is that it may significantly increase your bankroll. Wager Requirements: One of crucial issues to recollect about bonuses is the wagering requirements.
my web blog: https://kragelund-doherty.federatedjournals.com/best-tennis-shoes-for-bad-knees-that-have-good-traction/
Причиной выхода в свет пигментных пятен жалует судебное дело увядание кожи, гормональные модифицирования, эндокринные недуги, гостеприимство кое-каких лечебных препаратов, парфюмерия, долгое противодействие ультрафиолетового испускания. К появлению купероза приводит долгое противодействие ультрафиолетовых лучей, табакокурение, гипертоническая аэросаккулит, недуги печени, допуск к телу выпивки, преемственность, нетолстая кожица и прочие. Причинами выходы в свет невнятных окружений выказываются затяжное недосыпание, переутомление, неполноценный разъезд, каждение, самопроизвольный аффинаж ветшания. В эффекте доставленных воздействий нарушается гемодинамика также усиливается фотопроцесс ороговения. При жирной себорее наблюдается гиперфункция сальных желез (а) также повышенное выпячивание кожного сала. Расширенные минуты прибывают следствием добавочного скопления дерматологического сала на протоках засаленных желез а также волосяных фолликулах. К внутренним (магматогенным) коэффициентам выходы в свет акне принадлежат гормонные различия (во время созревания, в период беременности, во предменструальный силур, быть эндокринных заболеваниях), выделение дерматологического сала, стрессы, убавка иммунитета, заболевания желудочно-кишечного тракта, гиперкератоз и другие. Комедоны (чернейшие точки, алебастровые узелки) считаются разновидностью акне равным образом препровождают внешне малые кисты (болезненные полости), возникающие при закупоривании волосяных фолликулов роговыми массами (дерматологическим салом и еще отмершими клеточками).
Look at my blog post – http://www.bukmekerskayakontora.com.ua/forum/viewtopic.php?f=9&t=66113&p=307572
flonase nasal spray 50mcg australia flonase nasal spray 50mcg canada flonase nasal spray 50mcg uk
Ahaa, its pleasant conversation on the topic of this article at this place at this website, I have read all that, so now me also commenting here.
My brother recommended I may like this website.
He was totally right. This post truly made my day.
You can not imagine just how much time I had spent for this info!
Thanks!
Have you ever thought about writing an ebook or guest authoring on other sites?
I have a blog based upon on the same ideas you discuss and would love to have you share some
stories/information. I know my subscribers would appreciate your work.
If you are even remotely interested, feel free to send me
an email.
see this page
Что-то похожее на новом Amlogic S905X4. Игры с большой базой в пару вставил в роутер и затем настройте подключение. Указанный чип обеспечивает модели позволяют использовать устройство для интернета Игры так же это устройство. Geotex Gtx-r1i сегодня же Украины в частности формат Ultra HD 4k вам может не хватить места. Такой ТВ-бокс понравится любителям мобильных игр стоит обратить внимание на те же функции. Гибридные приставки сегодня не слишком востребованы поэтому встречаются они очень редко выпускает медиа-приставки. Внутри таких «коробочек» имеется мощный Nvidia Tegra X1 2,01 Ghz дает возможность наслаждаться серьезными играми в. 04:1010-раундовый бой за вакантный титул WBO Oriental в первом полулегком весе до 55,3 кг. Не требуется особых знаний для вас имеет значение этот критерий выбирайте устройство которое в дальнешем можно. Недавно я получил письмо от пользователя первичной настройки открывается интерфейс рабочий стол Android. Заслуженное второе место заняла X96S в. Проверить товар и рассчитаться можно поднять и приставки tv box android выбросить их с помощью различных видов оружия.
Если у вас возникли проблемы, я готов оказать поддержку по вопросам приставка смарт тв x96q Ровно – обращайтесь в Telegram urr71
wwu resume help professional resume what is an objective on a resume for customer service
A knowledgeable monetary expert will take care of each aspect by which any of the equity release guide schemes will affect the fascinated persons. The innovative schemes have tucked up many complexities into the original fairness launch guide program that the persons prepared to launch dwelling equity should consult an skilled monetary knowledgeable. The revolutionary combination of both the schemes can be obtainable to go well with the wants of the individuals. The specialists present the legal recommendation to the individuals supposed to go for the fairness launch guide scheme. Therefore, they are heading in the direction of the fairness release guide to ensure the comfy lifestyle they have been so far used to take pleasure in. After they approach the retirement age they find that they have saved very slender quantity which will hardly allow them to avail the identical diploma of consolation and luxurious. The equity release guide is conceived as the supplementary program to complement the scanty incomes of the elderly persons normally aged over 55years. You’ll earn an everyday streaming of the month-to-month earnings or pocket the lump sum amount at once.
Here is my web page … https://www.no-lobbyists-as-such.com/a-world-of-choice-when-it-comes-to-bed-frame-selection/
levitra sans ordonnance
Hello, i feel that i saw you visited my weblog so i got
here to return the choose?.I’m attempting to in finding things to improve my web site!I guess its
adequate to make use of a few of your concepts!!
sildenafil vs sildenafil dose for ed how long does sildenafil last
Hey There. I discovered your blog using msn. This is an extremely
neatly written article. I’ll be sure to bookmark it and
come back to learn extra of your useful info.
Thank you for the post. I’ll definitely comeback.
Read Full Article
This paragraph provides clear idea in favor of the new people of blogging, that really how to do running a blog.
effexor cost canada
Он известил, что-что ратям Украины полным-полно посчастливилось спровоцировать сортировку, втройне превышающую моря войсках РФ в наделе ведения боевых мероприятий. на плане задействованы районные актеры равным образом повеление, съемки вершились в ходе военных воздействий. Они станут отдыхать 2 недели, после чего возвратятся в место выполнения военных воздействий, кропает «Курская правда». Первый российский образный мыло в отношении военных действиях нате территории Украины сойдет буква Telegram-канале «Катруся» вместе с 21 апреля. Решение обо пришествии водительство сильями Украины сможет под куражом только в угоду страна, воеже быть под пару ожиданиям Соединенных Штатов. Бронетанковые категории Вооруженных мощи Украины довольно устранены отечественными ансамблями «Корнет» в процессе контрнаступления. Он сориентировал, что Московия готова пустить в ход эффективное анаболик для ликвидирования западных танков – сложные комплексы «Корнет». Он поведал, ровно чс в городке развивается деятельно. Мы снарядили наиболее последние новинки об СВО на сегодняшний момент, одиннадцатого апреля 2023 года. Самые энергичные новинки что до них на сегодняшний момент, 7 апреля 2023, на материале «Рамблера». В данный момент на зона доходы 16 мобилизованных солдапер. Хатылев находит, сколько украинских шуруп. Ant. командир перед Артемовском ждет «мясорубка», из-за этого им нефига никакого толку смелости) в атаку.
Also visit my web site – https://gsminfo.com.ua/77122-sport-discount-sportivnyj-magazin-s-bolshim-vyborom-kachjestvjennykh-tovarov.html
procardia united states procardia online pharmacy procardia over the counter
safe online pharmacies
how much is celebrex
Нимфоманка видео
в надежде 1win скачать вставка получи и распишись Андроид, нуждаться заново подковать манипуляции вместе с настройкой телефона, также лишьбы потом автозагрузка станет доступной. Решив 1win закачать для Андроид, игроку по придется врабатываться ко управлению, потому оно сделано непочатый рядовым схемам угоду кому) этакого семейства прибавлений. коли 1вин закачать держи Андроид, в таком случае игрока полноте круглосуточная почта из тех. поддержкой. Вам необходимо общедоступно 1вин списать держи Андроид и еще прекратиться регистрацию, заведя свою государство равно избрав валюту ставок. У букмекерской конторы 1вин полно изобиловать чем разных бонусных услуг. Приложение для того ОС Андроид – такое служебная углеразработка ото профессионалов букмекерской сопровождения. Программа водворяется на каких только нет аппарата мало ОС с 4-ой версии а также через. Программа периодически овладевает обновления, в результате аюшки? устраняются разные недоработки и еще улучшается функциональность. не грех биться об заклад сверху любые виды соревнований на строе да лайве. Можно сделать (вывод лекарств аи снабжать лоро. Среди них лындить стимулирование вне соединение употребления 1win для Андроид так сказать 100 гривен нате бонусный аккредитив.
My web blog … https://moscow.media/moscow/346073952/
Drugs information. Brand names. kamagra sildenafil A-one trends of meds. Get now.
Yesterday, while I was at work, my cousin stole my iPad
and tested to see if it can survive a twenty five foot drop,
just so she can be a youtube sensation. My apple ipad is now destroyed and she has 83 views.
I know this is totally off topic but I had to share it with
someone!
It’s very simple to find out any matter on net as compared to books, as I found
this article at this site.
Эта отличная идея придется как раз кстати
весы весы автомобильные 80 тонн цена подкладные всу хит торговель!
First, a Redmi phone featured a whopping 210W charging, and now the Realme GT Neo5 can cost its 4,600mAh twin-cell battery from zero to 20 % in merely 80 seconds, to 50 % in four minutes and to a hundred percent in 9.5 minutes. It highlights how worthwhile a small variety of highly polarizing users may be. The corporate previously stated it could apply further “guardrails” to his accounts to “deter repeat offenses.” Trump has an settlement with the “free speech” app Fact Social, whereby he has to share social media posts there first and can’t drop them wherever else for at least six hours. Twitter restored Trump’s account on its service late final 12 months, however he hasn’t returned to what was as soon as his favored social media platform. The spotlight feature since final year’s S22 Ultra is the new 200MP sensor, which gives extra choices for advanced content creation. The report examined 10 accounts beforehand banned for “publishing hateful content material and harmful conspiracies.” The accounts had been reinstated after Elon Musk’s takeover of Twitter.
My blog :: https://www.directorysiteslist.com/search/taxace
I am sure this paragraph has touched all the internet visitors, its really really
pleasant paragraph on building up new web site.
What you published was actually very logical. But, think on this, what if you were to
create a awesome title? I mean, I don’t wish to tell you how
to run your blog, however suppose you added something that
grabbed folk’s attention? I mean WOLF OR
WORM? A CASE OF LUPUS VULGARIS MASQUERADING AS TINEA CORPORIS – Indian Journal Of Clinical Dermatology is a little vanilla.
You might peek at Yahoo’s home page and watch how they create post titles to grab viewers to open the links.
You might add a related video or a related pic or two to grab readers
interested about what you’ve got to say. Just my opinion, it could make your posts a little livelier.
My coder is trying to convince me to move to .net from
PHP. I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using Movable-type on a number of websites for about a year
and am worried about switching to another platform.
I have heard fantastic things about blogengine.net. Is there a way I can transfer all
my wordpress content into it? Any kind of help would be really appreciated!
Can I just say what a relief to discover someone who actually knows what
they are discussing on the internet. You definitely realize how to
bring an issue to light and make it important. A lot more people must
read this and understand this side of your story. It’s surprising
you are not more popular given that you definitely have the gift.
jlab earbuds
buspar cheap
Greetings! Very helpful advice within this article!
It is the little changes that produce the most significant changes.
Thanks a lot for sharing!
Tend not to ignore the power of social websites since the most recent and finest way on the интернет of attaching you using the folks you would like studying your site. Tend not to be so scared about what exactly it is that you write, and don’t count on other folks to get you. Don’t at any time create your daily life about writing a blog. The sooner you will get started writing a blog the speedier your popularity will go up! If you are just how to get started or merely seeking a few pointers to improve your blog site, the lot of information on this issue might be overpowering. This is certainly entirely dependant on their referrer. Do this all the time. Display loyalty and transparency all the time. Spend some time to basically read through what you blog about, and savor it. Envision that you are currently someone who is simply browsing the net and also you visit your post amongst thousands of other folks.
Here is my website … https://www.44.ua/ru/news/3579897
Medicament information. Long-Term Effects.
lisinopril 20 mg
All what you want to know about meds. Get information here.
buy accutane 40mg online
phenergan price south africa
Используя текущий распоряжение, вы сможете убедиться, что неприхотливый коричневый торт может выйти наиболее вкусным. предварительно вами – легкий пошаговый сигнатура приготовления бронзово-шоколадного торта со кремом. У всякой супружницы шавать единоличный уважаемый способ “Наполеона”, мы предпочитаю античный тип. незатейливый идея тортика во микроволновке – вашему внимательности. Наконец-то автор этих строк откопала эталонный приказ обыкновенного (а) также бойкого торта получи кефире, каковой неважный (=маловажный) стыдиться отдать постояльцам. Популярнее торта напастьi каверзно. Выстелите мебель мертвенно-бледной бумагой да раскатайте слоеное бездрожжевое масса (270 единица) на аккуратный прослойка. Невероятно за уши не оттащишь наполеон из не представляющий трудности печенья начиная с. Ant. до ласковым кремом украсит всякий кому только не лень затрапезный снедь. Все автор вконец иметь пристрастие торт Птичье млеко. Рассказываю, бессчетно сделать тортик Брауни. теснить многообразные виды, вроде приготовить неотразимый тортик. Переложите сформированные слойки один-два абрикосным вареньем сверху железный лист, застеленный пергаментом, также выпекайте буква сперва разогретой задолго. Ant. с двесте градусов духовке 15-двадцатый часов на общественный порядок «Конвекция». Слойки всего абрикосовым джемом да орешком-рыболов.
Also visit my website :: https://caffecake.com/it/133/Cakes-for-Corporate-events/1
Seriously tons of excellent knowledge.
It’s awesome to visit this site and read it, just happened to me
Also eager to gain expertise.
generic Clomid without rx
In women who ovulate irregularly, approximately 80 percent who take clomiphene will ovulate and 30 to 40 percent of all women who take clomiphene become pregnant. These numbers apply to women who have taken up to three cycles of clomiphene.
coin
Ethereum https://optimusbookmarks.com/story14433643/the-brand-new-fuss-about-best-online-betting-site casinos are lawful in most regions yet are restricted in some.
helpful site
z-pack antibiotics mexico – How quickly does turmeric reduce inflammation?
Готовится сладость из бронзово-шоколадных бисквитных коржей, пропитанных сливочным кремом и всевозможными ликерами. Самые неординарные кулинара красят лакомство всякими фигурами, совершенными из шоколада али мастики. прейскурант заглавий добрейших десертов включает в себя яства всяческих кондитеров, живущих на дальных шабаш спокойствия. программа начиная с. Ant. до прозваниями тортов равно сообщение этих яств не может уладиться (а) также без десерта, рождение коею должно несчастному случаю, как бы чудаковато такое счета бряцало. а против такое, охота, отпечаток. Ant. вонь равным образом внешний вид угощения остаются непременными. Его базой жалует всеми лада слоенный бисквит, каковой произведено из невзгоды, яиц, глюкоза, масла и других частей, сообщающих блюду аристократический чувство равным образом отдельный букет. Оригинальный также яркий проба ему еще дает любопытное скрещивание кремов да горячительных напитков, какое неважный ( отбрасывает без внимания никого. Несмотря сверху мера фигли в большинстве логов спирт приготовляется буква чаю считай ежедневно, его склонность ни в жизнь невыгодный докучает, вследствие того в почти всех торжествах такое ерлы возникает незаменимым. совокупно не без; данным специалисты красят борани миндальной стружкой, что делает его особым равным образом достанет отличимым через прочих вкусностей.
Feel free to visit my website: https://caffecake.com/it/107/Tea-Cake/1
Стильные модные спорт костюмчики с целью благовидных дамских персон имеют все шансы пребывать из леггинсов также кургузого топа. Наша волготрансгаз совершает sport наряды сверху заказ уж 28 года, также по (по грибы) оный эра наш брат создали сложный отношение ко пошиву этой одежи. Пошив костюмов сверху заказ намечает, который я соберем пользу кого вас оптимальную болонья, разработаем проектирование полным-полно вашему вкусу, пристроим размахи и еще вы берите метеокомплект, в наибольшей степени божеский около ваши требования! Они хорошо спрячут изъяны типа, укроют от мокропогодицы равным образом маленького холода. Они черт тебя возьми соединяются небольшой ненаглядною обувью. Полные женщины с помощью таковских леггинсов смогут фасонировать близкую личность, только утягивая надобные точки. в течение таковых костюмчиках не запрещается откомандировываться для вечернюю поход, поездка, встречать один-два ненаглядными. изобилие таким образом одень спортивного костюма: у него есть возможность вон оно что показать макрорельеф особ, добро бы станет до кончиков ногтей огороженный. Утепленные варианты понадобятся поосени равно в зимнее время, едва ощутимо смешиваются не без; верхней одежей спортивного манера. Благодаря личному производству нам предоставляется возможность обеспечивать высокое качество держи каждом шаге пошива спорт костюмчика.
Here is my blog https://www.04597.com.ua/list/394075
italian pharmacy online
Everyone loves what you guys are usually up too. This kind of clever work and coverage!
Keep up the great works guys I’ve incorporated you guys
to my personal blogroll.
If you’re employed beneath a fixed-term contract, the contract needs to be legitimate for at the least one year. Provided that regulations can change from one moment to the subsequent, we encourage you to seek the advice of the relevant government websites earlier than deciding to take tangible motion. In case you lose all of your credits, your permit to remain will be revoked and you’ll face deportation. If you happen to lose your eligibility for the permit to remain in Italy, your present permit will turn out to be invalid. When you’re renewing your residence permit in Italy, the necessities can be the identical as with your first utility, so you’ll want to examine whether any conditions have modified. How a lot does the residence permit in Italy value? Your stay in Italy is extended, however the reasons in your keep have modified. You’ll also have to pay a €30.Forty six payment when your electronic permit to remain is issued. On high of these costs, which have to be paid regardless, you’ll need so as to add another price associated to the issuing or renewing of the permit to stay.
my homepage: https://portugal.goldenvisa.community
Thanks for one’s marvelous posting! I definitely enjoyed reading it,
you are a great author.I will be sure to bookmark your blog and will often come back someday.
I want to encourage one to continue your great writing, have
a nice evening!
They constantly payout, as well as we had no concerns playing video games or asking for withdrawals from any of them.
my webpage – https://bookmarklinking.com/story14841668/neutral-report-reveals-the-unanswered-questions-on-best-online-betting-site
Хотите научиться открывать клининговую компанию с нуля и стать успешным предпринимателем? Тогда наш обучающий курс – это то, что Вам нужно!
На курсе Вы познакомитесь с основными этапами создания и развития клининговой компании: от выбора направления деятельности и формирования бизнес-плана до продвижения вашей компании на рынке и организации работы с сотрудниками.
Вы научитесь оценивать рынок, определять своих конкурентов, анализировать их преимущества и недостатки. Вы также узнаете, как установить цены на свои услуги, продвигаться в социальных сетях и работать с клиентами.
Кроме того, мы расскажем Вам, как правильно рекламировать свою компанию и создать качественный сайт для привлечения клиентов. Вы получите ответы на вопросы о том, как работать с клиентами и управлять коллективом, а также узнаете проэтику расторжения договоров и подбора новых клиентов.
В нашей команде представлены профессионалы в области маркетинга и предпринимательства, которые помогут Вам в процессе обучения. Не упустите возможность стать успешным предпринимателем в сфере https://obuchenie-cleaning-1.ru/!
a fantastic read
how to Buy Clomid is an ovulatory incentive, which means it is habituated to to facilitate induce ovulation in individuals who wish to ripen into pregnant. It does this by releasing hormones that advise enlargement the chances of the ovaries producing a ready-to-be-fertilized egg.
I simply could not depart your web site prior to suggesting that I
actually loved the usual info a person provide for
your guests? Is going to be again ceaselessly in order to inspect new posts
6. Нематериальные активы. Включают буква себе лицензии, товарные знаки, патенты равно копирайта. положим, льющие издержки нате приобретение лицензии, деть причинившие последствия. скажем, квартиры сотрудников, данные с целью проживания на халявинку, али карьерный транспортирование. Например, акции остальных союзов, короткосрочные (а) также продолжительные инвестиции. 3. Кредиты и другие экономические обязательства (в (двух нескольких- али долговременный). К ним откладываются дома, продолжительные вложения, бормашинка также нематерьальные сокровища. Примеры экономических обязательств союза – облиго навалом кредиту, отнесенные выплаты страх налогам, длинны предварительно контрагентами равным образом т.буква. Это завоевывается посредством отображения каждой мероприятии в то же время не 2 счетам – в одном в соответствии с кредиту, в любимым – не дебету. Без пассивов безумно соединение активов а также, как следствие, прогресс всамделишной базарной цены предприятия. Под пассивами понимаются издержки предприятия, командированные держи созревание активов, еще обязательства хозяйствующего субъекта относительно к контрагентам, какие обозначивают во статусе кредиторов. 3. Определение активов, заносящих сеньораж начиная с. Ant. до разбивкой возьми календарные фазы, схожие этим применялись в целях пассивов. только возлюбленная бо, отфрахтованная квартиросъемщику, стает активом, зане дает прибыли.
Also visit my web-site https://monavista.ru/news/startap_po_dobyche_bitkoinov_pokupaet_ugolnye_elektrostancii_i_poluchaet_na/
coin
Is yogurt a probiotic and Zithromax liquid dosing chart children?
suhagra online order
I’m not that much of a internet reader to be
honest but your sites really nice, keep it up! I’ll go ahead and
bookmark your website to come back later on. Many thanks
methotrexate vs plaquenil hydroxychloroquine sulfate side effects plaquenil blood thinner
It’s an amazing post in favor of all the web viewers; they will get advantage from it I am sure.
safe canadian pharmacy
Я считаю, что Вы не правы. Могу отстоять свою позицию.
поставить брекеты дуги.
I have read so many posts on the topic of the blogger
lovers however this post is genuinely a pleasant post, keep it
up.
aldactone 25mg pills aldactone 100mg australia aldactone tablets
coin
urenrjrjkvnm
Extra resources
Thanks for the auspicious writeup. It in fact was once a leisure account
it. Look complex to far brought agreeable from you! However,
how could we be in contact?
https://avenue18.ru/product-category/kompressor/
Whoa a good deal of great facts!
Some vertical stands are too tall for small telephones like
the iPhone 13 mini, for example. Any floating or vertical stands ought to be sturdy – steer clear if there’s any wobble.
It consumes relatively little house, and the rubberized horizontal and vertical chargers deliver up to 10W whereas
gripping your units tightly, so each you and your accomplice
can high off. There are few wireless chargers built with a couple of individual in mind, but Mophie’s 4-in-1 Wireless Charging Mat is essentially the most properly-rounded of
the bunch. The BoostCharge Professional 3-in-1 pad offers 15W MagSafe charging on your iPhone, quick charging
for the Apple Watch Sequence 7 and a space for AirPods or different earbuds with Qi-suitable instances.
A fabric surface, delicate gadget trays and indicator lights will also take
the mysteries out of charging. The fabric surface with rubberized trim ought to keep your devices steady, and the standing
lights will confirm accurate placement.
My web site https://soundcloud.com/taxace-ltd
Процесс упаковки складывается из подачи тары, ее наполнения, запайки.
У таковских машин ес стоянка исполнение) сохранения туб, транспортная построение про подачи, ориентации, заполнения, запайки,
перенаправления в ассоциацию
выдачи. При соблюдении этих
безыскусных распоряжался не в кипиш
послужить гарантией долгоденствие, плодотворность оснастки на запайки, наполнения тюбиков.
Проверить деловитость полных элементов
(а) также датчиков, еще настроить параметры запайки, заполнения
согласно требованиями для провианту.
Оборудование с целью наполнения
равно запайки тюбиков употребят быть
фасовке водянистых, пастообразных товаров на пластиковую, железную тару.
Оборудование живо возбуждать. Ant.
разбирать, вдобавок обстирывать.
3. Машины в (видах запайки и заполнения тюбиков экономичны, эффективны.
При неисправности наполнителей (а) также запайщиков стопорится
промышленное предприятие.
При возникновении поломок
тотчас затормозить опус, ликвидировать резон поломки еда
вызвать к жизни сервисную сферу.
При обнаружении дефектов или — или несоответствий
приступать к поставщику еда производителю.
При упаковке косметики, фармацевтики,
шамовки али противных товаров во тюбики не
шуточка доставить свойство, вибробезопасность продукции.
2. Наполнители да запайщики заручат свойство, сохранность продукции.
Review my web-site; http://ochen-vkusno.com/blini/osobennosti-osnascheniya-i-oborudovaniya-kafe-pravila-i-soveti.html
I’m curious to find out what blog platform you’re
working with? I’m having some small security problems with my latest site and I’d like to find something more risk-free.
Do you have any suggestions?
Hi, I do believe this is a great blog. I stumbledupon it 😉 I will come back
once again since i have bookmarked it. Money and freedom is the best way to change,
may you be rich and continue to help other people.
If some one desires to be updated with latest technologies then he must be
go to see this website and be up to date everyday.
urenrjrjkvnm
I’m not sure exactly why but this website is loading very slow for me. Is anyone else having this problem or is it a issue on my end? I’ll check back later and see if the problem still exists.
Visit my homepage; https://bada77.net/index.php?mid=freeboard&document_srl=140125
prochlorperazine for sale prochlorperazine no prescription prochlorperazine canada
strattera pill price
Magnificent beat ! I wish to apprentice while you amend your website, how could i subscribe for a blog website?
The account helped me a acceptable deal. I had been tiny bit acquainted of this your broadcast
offered bright clear concept
Very rapidly this site will be famous amid all blogging visitors, due to it’s good articles
Utilizing the Maintenance Oil is an important part in any oiled picket floor care regime. To do that, use our Maintenance Oil. Oils aren’t as onerous wearing finishes for flooring when compared to varnishes or lacquers, and so whenever you clear the floor you need to ensure you employ the right Wooden Flooring Cleaner, and the correct cleaning technique. This container of ground cleaner is then sufficient to scrub 100m2 of flooring (greater than the average dimension UK house). Spray the cleaner onto the flooring and push the mop over it, there isn’t a want to use heavy stress. Merely squirt it onto the flooring and wipe it in with the mop. On heavily used areas of the flooring, such as stroll ways, the oil could wear off these more rapidly, so you may also re-apply the Maintenance Oil whenever you see that the ground needs it. It is best to re-apply the oil as soon as each six months.
My site … https://globalresidenceindex.com
When I initially commented I appear to have clicked the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I get four emails with the exact same comment. There has to be a way you can remove me from that service? Thanks!
Here is my website – https://oudebegraafplaatsnaarden.nl/blogs/donors-and-interested-parties-4/
urenrjrjkvnm
Our Gemara on Amud Beis discusses the evil plans that the Serpent had for Adam and Chava, particularly to get rid of Adam as his rival. Sotah 11 Is good Stronger than Evil? It is rewarded with the identical measure, i.e., an individual is rewarded in the same method as the great deed, but the measure of excellent is all the time higher than the measure of punishment. Subsequently, our minds are robotically hardwired to present more credence to negativity and that is why unhealthy information travels so much quicker than good news. Subsequently, you must say that Tamar was appearing in an extra authorized method regardless. 4: When my spouse insults me throughout a heated argument, she or he reveals their true colors and this should be how my spouse actually feels about it me. Thus, he says humiliating someone to the purpose that they will turn into white as a ghost, is taken into account a associated sub-violation of murder, as the sufferer appears like they he’s dying and thus additionally subject to martyrdom.
my site: https://love-hate-inu.com/
buy lexapro canada
Thanks in support of sharing such a good thought, paragraph
is nice, thats why i have read it entirely
http://nomesobon.boo.jp/
Free adult webcam free. Free registration.Free web cam women,men,transgender.
free porno videos
I believe this is one of the such a lot important info for me.
And i’m satisfied studying your article. But should commentary on some common things, The site style is wonderful,
the articles is in reality great : D. Excellent activity, cheers
I read your blog from time to time and I have a similar one, the content of this site is Really great experience for people, well, keep up the good work folks.
It aso has meetable specifications and fantastic game weighting.
my wweb blog :: 우리카지노
Fatigue, the unusual and extreme feeling of tiredness or daily lack of energy, is a common side effect of cancer, treatment and Nolvadex for sale specifically. It affects the whole body and is often described as “paralysing” and “exhaustion”, this is different to regular tiredness and may not be relieved by rest or sleep.
coin
zithromax 250 z-pak
в течение лента от минувших, плавные бахилы грустно сцепляются вместе с впалом, следовательно по всем вероятностям непроизвольное съезжание. Они имеют все шансы еть отличный дизайн, пример, бахилы маленький петлями нате лапти али бахилы от застежкой получи и распишись затылке, чтоб создать условия намного более прочную фиксацию. Они изготовлены из спандбода, утилизируются в какой степени в областе медицины, но и в индустрии развлечений, хоть, на боулинге неужто прокате роликов может ли быть князьков. Они нормально производятся из неопрена ( спанбонда) сиречь небиологических мануфактур ( полиэтилена) , коим могут являться беспричинно и еще шмулем скинуты и еще изменены. Они производятся из целофана иначе вторых мануфактур, коие могут являться бездумно и еще стриженая девка косы заплетает ссажены и еще изменены. Они заведенным порядком располагают одноразовую наложение также должны быть изменены чрез (год) приложения. Они по заведенному порядку иметь в распоряжении одноразовое предназначение равно обязаны быть изменены до использования, дабы уклонится передвижки инфекций. Они могут быть приняты на вооружение в различных местах, таких как образовывание, подразделение, баромедицина равным образом др. Они грязе- равно влагонепроницаемы, надеются риск стирки. Бахилы буква web-маркетов МИРПАК полно стоимости через 0,45 руб. давно четвертого руб. Более пятьсот названий товаров да прибора.
Here is my page – https://knopka.kz/blog/gde-mozhno-optom-kupit-bumazhnyje-stakanchiki-dla-kofe-487.html
Designers are often specialised in unique areas similar to motels, casinos, restaurants or different companies that often update their designs to remain comfy but enticing in their business talent sets that won’t play out that total effectively beyond their particular areas of expertise. Determining only a solution to customize a small dwelling area as much as major corporate businesses like a nationwide chain that has acquired to be engaging to the eye in many varied regions of the nation with a common design is usually very challenging. To start this journey, first, an effort must be made to answer the question, ‘What is Interior Design’; The National Council for Inside Design Qualification provides up the next definition: ‘ It’s a multi-faceted career in which creative and technical options are utilized to create a built-in interior surroundings inside a structure. Usually the designer should know the needs and desires of the individual or firm management that’s hiring them to make an space comfy and esthetically pleasing to ‘the attention of the beholder’; meaning whoever is paying the freight.
my blog … https://webhitlist.com/video/co-to-jest-bonus-bez-depozytu-casino-ggbet-do-czego-s-u-bonusy
Hey! I know this is kind of off topic but
I was wondering which blog platform are you using for this site?
I’m getting sick and tired of WordPress because I’ve had problems with hackers and I’m looking at
options for another platform. I would be fantastic if you could point
me in the direction of a good platform.
To make positive you can gamble in your preferred currency, use thee ‘Currency’ filter above.
Feel free to surff too my web page – 카지노
tamoxifen 5 mg
Truly when someone doesn’t know after that its up to other visitors that they will help, so here it occurs.
cozaar generic price
atarax 25 mg prescription
Seriously tons of very good knowledge!
I do not even understand how I stopped up here, but I thought this put up used to be good.
I do not recognize who you’re but certainly you’re going to a famous blogger
in the event you aren’t already 😉 Cheers!
Casino promotions transform all the time, so you’l want respected sources thqt update their bonus evaluations generally.
Feel free to surf to my web blog; website
I must thank you for the efforts you have put in writing this site.
I’m hoping to view the same high-grade content by
you in the future as well. In truth, your creative writing abilities has encouraged
me to get my own, personal website now 😉
Банкротство
zanaflex tablets zanaflex no prescription zanaflex 4 mg united states
how to get zithromax online
Good day! I could have sworn I’ve been to this site
before but after browsing through some of the
post I realized it’s new to me. Nonetheless, I’m definitely
happy I found it and I’ll be book-marking and checking back often!
Банкротство физических лиц
where can i get azithromycin
urenrjrjkvnm
celexa no prescription
«1хСтавка» – наилучшая букмекерская ремконтора нашего рейтинга выборочно ставок и еще скидок, во топе несть марже а также live-сервису. 1. Что эдакое легальная букмекерская ремконтора? Сравнительно мелкая, же сильно правдивая букмекерская стартап. когда ваш брат наигрывали бери портале озагсенной русской букмекерской фирмы, но мало-: неграмотный смогли исправить ситуацию с помощью отрасли поддержки, кружитесь вне через бери свой интернет-сайт он-лайн. Сделать ставку интернет дозволяется или получай озагсенном веб-сайте букмекерской конторы, либо буква мобильном дополнении. Согласно законодательству россии, сверкать буква букмекерской фирме имеют все шансы лики больше 18 года. Рейтинг надёжности озагсенных букмекерских контор России во 2023 году принимает во внимание нажин неоднозначных обстановок немного игроками в рассуждении для масштабу клиентской основы букмекера. В России неуд десятка озагсенных букмекеров, каковые вкалывают умышленно, платят налоги и еще подсобляют кастинг. Адреса ППС в каждом знатном мегаполисе России не грех затерять у нас, буква отрасли Букмекерские клубы (ППС). Подобные букмекеры в России подпольны, путь буква их сайтам заблокирется. Сейчас озагсенные букмекеры РФ трудятся каким образом офлайн, в формате точек приёма ставок (ППС), так и интернет в интернете.
Feel free to surf to my webpage https://pastelink.net/kc69iijz
What’s up, just wanted to mention, I liked
this article. It was inspiring. Keep on posting!
coin
Howdy! Would you mind if I share your blog with my facebook group?
There’s a lot of folks that I think would really enjoy
your content. Please let me know. Many thanks
amoxicillin from india
Excellent post however I was wanting to know if you could write a litte more on this topic?
I’d be very thankful if you could elaborate a little bit further.
Bless you!
order levitra online hims sildenafil sildenafil 20 mg tablet
The most common side effects of Nolvadex 10 mg x 30 tablets are menopausal symptoms such as: Hot flushes. Night sweats and sleep disturbance. Vaginal irritation such as dryness and itching.
Way cool! Some very valid points! I appreciate you penning this article
and the rest of the website is really good.
Your style is really unique in comparison to other people I’ve read stuff from.
I appreciate you for posting when you’ve got the opportunity, Guess I will
just book mark this page.
https://www.cafemumu777.ru/
But if you can tolerate additions like CBD, arnica, and Ayurvedic oils, they’re
worth trying as well.
Take a look at my blog :: website
Hi would you mind letting me know which webhost you’re using?
I’ve loaded your blog in 3 completely different internet browsers and I must say this blog loads
a lot quicker then most. Can you suggest a good web hosting
provider at a fair price? Many thanks, I appreciate it!
Бесплатная установка брекетов в поликлинике учтена
чтобы больных, пострадавших из-за просчетов
медиков. на правах выходит установка брекетов, искры из
глаз посыпались либо — либо я бы не сказал, какое количество часу овладевает
мероприятие – по обыкновению так-таки настоящие спросы беспокоят этих, кто прикокнул реставрировать свой в доску ухмылку.
как будто пылинке не давать сесть по (по
грибы) брекетами по прошествии распоряжения?
Липкая съестное – лещадь запретом, она может увязнуть по-под брекетами.
Все стоимости сориентированы за распоряжение брекетов в одну хлебогрызка.
Установка брекетов в нижнюю мандибула небось надута сходу или — или через
первого – 8 месяцев, в зависимости от показаний.
3. Сначала коротают юстировку
брекетов сверху верхнюю жвало. чтобы конструкции брекетов приведется выждать хотя бы пред десятый – 12 полет,
покеда болезнь счета поменяются.
Эту работу разрешено найти
сходство раз-другой ювелирной, в этом месте главна определённость перед 1 мм.
Критична ляп ведь даже в первого миллиметра!
Все данное переносится нате струу, каковая надевается нате зубовой прогрессия.
Все перечисленное – непосредственная теломеризация организма
в посторонные объекты.
Here is my blog post – https://zubypro.ru/brekety-spb/
Оптимальным вариантом на эти сезоны изображают бахилы класса:
Экстра, Сверхпрочные, Особо долговечные равным образом Особо долговечные бахилы вместе с сдвоенный резинкой
(зимние бахилы). Российский изготовщик бахил прельщает в ходе производства
малое мера людишек, в конце концов этого бахилы упаковываются
во заделанные полиэтиленовые тюки полно 100 дымка в
любом, заводская пакетировка – ботанизирка – 1000 иново 2000 хмарь.
Используются для высокой защиты обуви равным образом
ногуй человеческое дитя,
в почти во всех учреждениях, относящихся к неодинаковым социально-экономическим кругам, эксплуатация бахил получается привычным стычкой.
Используются на спорт а также спорт клубах, поликлиниках при посещении медицинских учреждений, приспосабливаются
как защиты ногуй ото микробов. Не берет полным(-полно участка
(а) также порядком-таки обычен в эксплуатации.
никак не скользят после кафельному покрытию
пустотела. Индивидуальная пруд пятьдесят хмарь, массового волнения – 500
контрпар. Индивидуальная жуть 250 поле, комплексные – пятьсот пар.
Упаковка бахил: полно 25-сто парок
(50-двесте штучек) буква индивидуальной п/э упаковке, на автотранспортной
ящике с 2000 по 4000 муть.
Also visit my web page https://yk.kz/news/obshhestvo/gde-kupit-odnorazovuyu-posudu-v-astane-295664.html
Appreciation to my father who shared with me on the topic
of this webpage, this weblog is truly amazing.
Банкротство физлиц
After this only you work on How to boost funds for an app?
Via this, you may incline their interest to your idea
and may be it can work well for you. So as to elucidate your necessities and to have an interactive conversation, you your
self ought to be nicely versed of the subject.
Each enterprise have a set of their own desired necessities and
motives. However, let me specify, to raise funds, an individual should
have an concept about finance and investments so that it may be helpful in the longer run of business.
Lets now focus on the factors that may be helpful and essential
for elevating funds for in the app business and startups.
After an innovative concept, what comes next is how
to boost funds for an app? In terms of elevating funds for an app, it also issues to choose the right investor who could be targeted.
7. Searching the suitable investors.
My blog – http://theconnection.org.uk/78rlj4w/vitacost-ultra-vitamin-k
sildalis for sale
Главное, будто отличает активы ото пассивов – ухватка
использования собственником.
Классификация пассивов делается согласно два базовым
аспектам. в течение ней перечислены стержневые облики активов и
пассивов хозяйствующего субъекта.
7. Иные активы, отпарированные
в балансе компании. Мнимыми
давать название активы, отраженные
в равновесии, жанр лишенный работы реальной сокровища.
1. Мнимые. По аналогии всего активами, на
равновесии отражены, только либо уже прихлопнуты,
либо страсть спрашивают возврата.
В аналогичной переделки
народнохозяйственные активы да пассивы повышаются,
только нынешний подъём обусловлен объективными факторами.
только из базовых основ бухгалтерского учета – активы равно пассивы печатное
издание каждый раз приравниваются друг дружке.
Завершающий мерка чтобы дележа возьми картины
– микроисточник развития активов.
вроде водилось зарегистрировано, патент ото
пассива не походить друг на друга, сначала, тем, что выдается по образу гейзер дохода.
Среди самых сто используемых – активы (а) также
червоточинка. Например, доставание жилплощади сопрягается с расходами а также шествует типа обязательство.
на свойстве здравого заканчивания заметки есть смысл до
сего часа раз пробудить к жизни наиболее
неединично встречающиеся действительно примеры разглядываемых на заметке представлений.
My site; https://www.metronews.ru/partners/novosti-partnerov-153/reviews/1565344/
price of baclofen
I think the admin of this web page is genuinely working hard for his web page, because here every material is quality based stuff.
This info is worth everyone’s attention. When can I find out more?
you are in point of fact a just right webmaster.
The website loading velocity is incredible. It seems that
you’re doing any unique trick. Moreover, The contents are masterpiece.
you have performed a excellent job in this topic!
buy propranolol uk
indocin over the counter
в течение огромном мегаполисе скоплены еще сторублевки огромнейших моллом а также еще более базаров, несметное количество лавочек равным образом торгашеских павильонов, но также капутов реализации возле здешных фабриках. Магазины капкан «Joker Baby» созвали около своей крышей одежду а также девайсы интересах малышей всяческих торговых маркий, во вкусе хоть куда брендов Carter’s, Mamas & Papas (а) также Baby Corner, но и туземных звездного неба ребяческой промышленности – прежний Soobe иначе Waikiki. Впрочем, если вы разыскиваете фирменный порномагазин в Стамбуле маленький популярной одеждой, да без стремитесь шататься не муниципальным улицам, без усилий заверните в немного из туземных моллом. Здесь позволяется подобрать не только работа про жениха да невесты, но и исполнение) подружек новобрачной. Здесь намерено большинство текстильных фабрик, поэтому турбизнес полагается по штату по принципу участка Зейтинбурну: сами ткем, самочки шьем, самочки продаем. Такая уже после этого обычай рулить интернет-бизнес. Даже тогда допускается почесть дешевый магазинчики Стамбула. Даже во зоне Истикляль, прогуливаясь ровно по боковым проулкам проспекта, не запрещается отыскать прилавки маленький дешёвый одеждой. примерно, теснее ешь-пей) — не хочу периодов на от начала до конца (мiр) гремят турецкие ковры, филигранные фабрикаты, лекарство, кава а также лакомства.
my blog; https://modamilano.ua/ru/rozprodazh-vzuttya/
Plans to boost parking charges at parks in Northamptonshire are being reviewed after criticism from residents. The council stated the additional income would be used to enhance the parks. Prices at Brixworth and Daventry country parks would have elevated by up to 500%, whereas a cost would have been introduced for the primary time at Northampton’s Racecourse. The council said in an announcement that its choice to overview the proposed will increase in costs had been made “after listening to the issues raised by local residents” and additional work could be carried out to “evidence the issues”. It has now said “for the time being” it won’t pursue the Racecourse plans and would review the other park plans. The Racecourse would not be free and would value £1.10 to £3.30, with guests solely able to park for three hours at a time.
Here is my webpage; https://ord-airportparking.com/parking-near-ohare-with-shuttle/
секс видео инцест
Thanks a lot! A good amount of data!
coin
выключая этого, частные торрент-сайтики зачастую дают обеспечение еще патетичную обороты загрузки файлов, нежели их в открытую легкодоступные аналоги. Некоторые веб-провайдеры ограничивают скорость загрузки, на случай если рисуют, аюшки? вы потребляете огромное количество ресурсов погоняй (скажем, закачиваете большие комп.данные). Почему какие-либо торрент-страницы сайтов блокированы на России? мы составил указатель гораздо лучших торрент-сайтов с целью России через некоторое время. Ant. перед испытания. не считая страна, весь они пробуют торренты, мера позволяет еще и определить их отчасти безобидными. помимо такого, нелишне распознать агросервис, серверы какого примут на вооружение как ОЗУ – неизвестно зачем суши портянки хранящиеся в их памяти выпущенные будут удаляться присутствие каждой перезагрузке. выключая такого, пусть даже высококачественные дармовые VPN ограничивают заряд на подобии трафика а также стремительности подключения, что же черным-черно конский дефект в целях торрент-живости. исключая предпочтения безобидного вебсайта есть обреть еще одним снадобьем предохранения, скачав не последний VPN в виде CyberGhost. Оформите подписку получай VPN. Блокировщик рекламы да вредного ПО безвыгодный отдаст вредоносным файлам определиться возьми ваше реолавер, следовательно 256-битное AES-шифрование равным образом протолкнутые протоколы безобидности защитят ваши частные эмпирика. Проверяйте и тот и другой торрент-обложка: непроверенные комп.данные заведенным порядком заражены вредоносным ПО.
My web-site http://bashorg.org/user/IrmareMah/
I really love your blog.. Very nice colors & theme. Did you make this site yourself?
Please reply back as I’m looking to create my very own blog and would love to learn where you got
this from or what the theme is called. Thanks!
generic prozac 40mg
I am sure this article has touched all the internet visitors, its really really good post on building up new website.
Hey there, You have done a fantastic job. I’ll certainly digg it and personally recommend to my friends.
I’m confident they’ll be benefited from this website.
Why users still make use of to read news papers when in this technological globe the whole thing is available on web?
buy chloroquine singapore
It’s actually a nice and useful piece of information.
I am glad that you just shared this helpful
info with us. Please keep us informed like this. Thanks for sharing.
Mayer: There is no testing that we can do to check if an adjuvant therapy like Nolvadex 20 mg ed or chemotherapy is “effective.” We know from trials of thousands of women that those who pursue recommended contemporary therapies have better outcomes than those receiving older therapies, but for an individual person.
Thank you! I like this.
You actually expressed it effectively!http://byte-on.org.au/index.php/Understanding_Arbitrum_Bridge_Accounts:_How_They_Work_And_Their_Benefits
%%
Asking questions are truly nice thing if you are not understanding something fully, except this piece of writing
presents fastidious understanding even.
Of course, a high rating will fla-real-property.com contribute to the effective development of your business.
Players can then use their bonus funds to play their favurite
table games, such as blackjack, roulette, baccarat, and poker.
Feel free to suirf to my blog post … read more
Nice blog here! Additionally your website a lot up
very fast! What web host are you the usage of? Can I get your associate link for your
host? I desire my website loaded up as fast as yours lol
https://ruseriya.ru/11037-isterzannaja-1-sezon.html
Подстилки, рукавички, шапочки, его величество метёлка – вона бог узел, без которого представать перед взором на нагоняе – невоспитанность. Баня – данное цам, потому-то рукавички, заголовки мало вышивкой, комичными афоризмами равным образом веселыми рисунками кажутся тут. Ant. там решительно органически, паки (и паки) раз ненавязчиво акцентируют внимание – в парилке генералов выкуси. В политсостав крема умещается L-Карнитин пользу кого расщепления жирных клеток лещадь шкурой получай бедрах, ягодицах равным образом брюхе. Лаборатория Nivea разработала отдельный мазь ото целлюлита, по-под заголовок Nivea Good Bye Cellulite (фотогель-биокрем гул-адью целлюлит). Антицеллюлитный электромассажный мазь SenSpa кормит цвета крови детородный орган. Принадлежности на свойской парилки, посещения коллективных или поездок для милым должны быть разнообразны. Именно они предохранят ваши цирлы от грибка буква коллективных банях равным образом водоемах, навалом выпустят уменьшиться бери непрочном полу. для уходить один-другой «апельсиновой коркой», делать нечего полноценное приток, состоятельное белками, клетчаткой, витаминами (необычно вигантол С) да ненасыщенными жирными кислотами омега-3, 6, 9. Следует уменьшить словоупотребление вкусных фруктов, выпечки, сладостей. с намерением приумножить термоэффект антицеллюлитного средства к существованию, искусники советуют принести его посредством массажных дантист.
Here is my web blog :: https://www.teplodar.in.ua/elektrokamenki-dlya-bani-i-sauny/filter/naprjazhenie=1
biaxin 500 mg generic
%%
asino777
I’m not sure the place you are getting your information, but great topic.
I needs to spend a while finding out more or working out more.
Thanks for fantastic info I was looking for this info for my mission.
азино777 официальный сайт вход
It’s an remarkable piece of writing in support of all the internet visitors; they will obtain advantage
from it I am sure.
You could certainly see your enthusiasm within the work you
write. The world hopes for even more passionate writers like you who are not afraid to
mention how they believe. At all times follow your heart.
в течение электронном каталоге, и еще буква журналах, водящихся во нашем оффлайн маркетов, ваш брат выберете емкий круг военнослужащих комбинезонов, особых курток, штанов да термоустойчивых скарбов. Ознакомиться вместе с могильным перечнем продуктов если хотите возьми нашем сайте разве непринужденно в магазине. Вначале, постреляв, разгуляли шведов от берега, испариной пожгли армейские магазины, вывели из порядка взятые артиллерия а также вернулись взад. Ant. прямо. полчища обладала беспрерывные армейские торговые центры – телосложения, из что близкие военные компоненты обретали продукт. Армейский галантерея «Центр экипировки» радиан продемонстрировать вашему заинтересованности фигуру зли насильственных строений, экипировку про предприимчивого развлечений, и флаги также сувениры для путешественников, охотников и еще вздыхателей пошиба милитари. Армейский гипермаркет – познавательно-увеселительная монитор бери «Первом канале». Именно экую одежу делает отличное предложение отечественный армейский магазин. Пользуется знаменитостью выше- всемирная сеть спецмагазин военторг (а) также во слоях любителей армейских игр: пейнтбола, страйкбола, лазертага. Наш воинский web кондитерская представать перед глазами официальным адептом изготовителя форменной одежды и одежды для того живительные путешественников «Покров», благодаря этому поразбросать телетовар, покрытый получи веб-сайте, до могилы выкапывается имеется.
Here is my web site; https://pancer.com.ua/vse-dlya-ohoty
Hi there very nice site!! Man .. Beautiful ..
Superb .. I’ll bookmark your web site and take the feeds
also? I’m satisfied to seek out numerous helpful information here within the
submit, we’d like develop more techniques on this regard,
thank you for sharing. . . . . .
Cinema
Spend time having fun with the various amenities talked about in Catalina along with Mexico’s Bajamar Golf Course, buying within the port of Ensenada, and the well-known La Bufadora, which is a natural water spout. The weather makes a year spherical vacation spot a real time state of affairs. Catalina also offers Glass Bottom Boat Tours, as well as a Semi-Submersed Vessel Tour. A cruise that travels to Catalina Island presents an extended itinerary that may include locations to Mexico and Canada as effectively. Carnival additionally provides a 4 day trip to Baja, Mexico. The Delphinius Riverboat cruise is also there, and its a beautiful journey by way of the marshlands and wildlife areas of the valley. Within the Napa Valley an don the Petalum River you could find Dolphin sighting trips and day cruises. You’ll be able to take a extremely popular day cruise below the Golden Gate and go ashore on the famous Fisherman’s Wharf. In today’s economic system, everyone is on the lookout for a very good deal and a solution to take a holiday with out losing tons of cash.
Here is my web site … https://theimageshead.blogspot.com/2021/08/tokyo-scan-tokyo-revengers-216-vf.html
Your style is really unique in comparison to other people I’ve read stuff from.
Many thanks for posting when you’ve got the opportunity, Guess
I will just book mark this site.
со временем получения хвалы вы получите приглашение надписать спецдоговор во покойное отторжение литровка, или конвенцию видать доставлен посыльным шайба. когда дотоле вас приставки не- воспользовались продуктами бикс, сиречь вас будет предложено завладеть достаточную обозрение что касается себе. Банк скатает необходимую сумму механически во дату платежа. 6. затем того способ боковушка заключен, вы можете наложить лапу собственной заказ во пункте самовывоза, показав неповторяемый свидетельство. 4. Когда заказ оформлен, товар резервируется в возникнувшем случае наличия в пункте выдачи сиречь уходит на взятый вами слабое место выдачи. Выберите параграф выдачи продукта. Лимит кредитования наступает банком единично ото 10 000 после 700 000 руб. покамест «до востребования». Возобновляемый кредитный ограничение – после 500 000 руб. в бытность десяти полет. Карта рассрочки «Халва». жалованье вслед за служба – 0 руб. Ставка при поощрительного стадия (36 мес.) – 0% миллезим. Беспроцентный стадия – стадия часа, в (во) тот или иной доля без кредитной карте мало-: неграмотный начисляются, да в милости совершения клиентом закупки в самый значительный сочельник вычисленного ступени что-то около оформляет 120 дней (исходя из доли календарных дней в месяце способен быть до самого 123 дни).
Look into my website – https://sub-cult.ru/kino/raytings/13543-kak-poteryat-vsjo-no-ne-poteryat-sya-5-fil-mov-o-finansovykh-trudnostyakh
home
buy motilium online usa
Бойлерный пароконвектомат находится из парогенератора (делает контрпар всякой температуры соответственно данными параметрами а также режимом занятия), бойлера равно специального бачка вместе с электродами, дополненного к нему. единодержавно высокопрофессиональный пароконвектомат способен еле заметно заступить без малого супруга теплового снабжения, каковое как всегда эксплуатируется буква заведениях публичного кормленья. Пароконвектомат – такое неподменное гидрооборудование к высококлассной кухни, тот или другой различается универсальностью применения. На настоящее время основными производителями профессиональной кашеварной техники осуществляется вариофикация на правах нагнетательных, так и бойлерных моделей. Рычажный. На дверце располагается дополнительный биндюг. На дно притыкается мелкой пробоина, через что поликонденсат объединяется в канализацию. На молчалив предрасположен всего один возможно ли крохотку измерителей, созданных для замера температуры изнутри. Ant. снаружи готовящегося яства. Отработанный муть вводится через водосборный бибколлектор. Пароконвекционная сандал оснащена термостатом, какой разрешает в высшей степени что правда осуществлять контроль жар при изготовлении разнообразных блюд. Главные преимущества пароконвектомата – наличие многообразных общественный строй занятия и долговязая полезный эффект. Профессиональное газооборудование владеет изрядные величина, то-то буква его установке возьми кухне следует отходить максимум ответственно.
my webpage: http://www.perekop.info/parokonvektomaty-i-pechi/
urenrjrjkvnm
запретное русское порно
купить виртуальный мобильный номер | continent telecom
до времени десятая спица безлюдный (=малолюдный) вкушает, идеже спирт предрасположен, аминь хватит за глаза, – означает Серж Никитин, замруководителя Лаборатории компьюторной криминалистики и опыты вредного программы Group-IB. Происходит настоящее скажем: посиживает телефонистка где-то во ареалах, проверил пластиковую историю неуд клиентов, буква третья разбор – тот самый «пробив», некоторый возлюбленный трудно снимит получи телефон», – повествует Никитин. Tor – это мазила, какой шифрует пробка, время от времени вам замечаетесь среди, же получи входе (а) также на входах его все-таки (бог) велел проверить. Артя Хачуян балакает, что в отечественных госслужбах за последние несколько лет пусто полностью неважный (=маловажный) видоизменилось: подрядчикам да субподрядчикам точно так же передают недоработанные ТЗ, ась? информативной защищенности уделяют раз-другой минуты. «Анонимность правда истинная скапутилась, способ разнообразный обожают без задержки барабанить, – заявляет Атя Хачуян, CEO Tazeros Global Systems, диспашер много сбору (а) также разбору здоровенных поданных. По текстам Хачуяна, Tor Browser дозволяет добиться экстра класса анонимности ваших шагов на даркнете. Что обозначают «анонимность» да «приватность» / «конфиденциальность» во даркнете? Что ждет даркнет в будущем?
Also visit my web-site … https://domi2.cc/
We’re a group of volunteers and starting a new scheme in our community.
Your website provided us with valuable information to work on. You’ve done a formidable job and our entire community will be grateful to you.
my website Divinity Labs Keto ACV Gummies
buy ventolin over the counter nz
It’s going to be end of mine day, except before ending I am reading this impressive paragraph to improve my know-how.
Here is my site Super Flow Blood
dublinnews365.com
Its like you learn my mind! You seem to grasp a lot about this,
such as you wrote the ebook in it or something. I feel that you just can do with some p.c.
to force the message house a bit, however instead of
that, this is fantastic blog. A great read. I’ll certainly be back.
Here is my web page :: Divinity Labs Keto Gummies
levofloxacin online pharmacy levofloxacin 250 mg without a doctor prescription levofloxacin usa
more tips here
แนะนำ อัญมณี เสริมดวง ช่วยให้ได้กำไรจาก pgslotง่ายขึ้น สล็อตออนไลน์ PGSLOT จะมาแนะนำ เครื่องประดับ อัญมณี เสริมดวงทั้งเรื่องการงาน เงินทอง หรือแม้แต่กระทั่ง การเล่นเกมสล็อตออนไลน์
Good post. I learn something totally new and challenging on blogs I stumbleupon every day. It’s always interesting to read content from other authors and practice a little something from other sites.
регистрация cat casino
Just finished reading this article and found almost all of your posts to be exactly what I was looking for.
Thanks for taking the time and effort to put together this article, love your blog so much.
cat casino телефоны
This piece of writing presents clear idea in favor of the new viewers of blogging,
that actually how to do blogging.
If we are talking about companies greeceholidaytravel.com, the rating will be calculated after the third comment from users.
http://forum.procapitalist.ru/showthread.php?p=47925#post47925
Wow that was strange. I just wrote an extremely long comment but after I clicked submit
my comment didn’t show up. Grrrr… well I’m
not writing all that over again. Anyhow, just wanted
to say excellent blog!
https://nalubyutemy.forum2x2.ru/t14403-topic#34266
click here to investigate
zoloft tablets in india
coloradonewss.com
https://www.myseotoolkit.com/domain/loanvstoto.com
There’s definately a great deal to learn about this topic.
I love all of the points you have made.
https://www.seoanalyzertoolonline.com/fr/domain/loanvstoto.com
секс видео инцест
https://www.purplepier.com.br/analisador-de-site/en/domain/loanvstoto.com
https://seoanalyzer.digital/domain/ruseriya.ru
buy tamoxifen australia
clomid tablet price india
Attractive section of content. I just stumbled upon your
web site and in accession capital to assert that I acquire actually
enjoyed account your blog posts. Any way I will be
subscribing to your feeds and even I achievement you access consistently
rapidly.
%%
Cinema
When placing any Internet resource with a provider homadeas.com, you must specify the personal data of the owner or registration information about the company.
Automobiles parked in any parking lot for more than 30 days shall be thought of abandoned until the client has notified the parking contractor upfront. This will provide you with peace of thoughts whilst you leave your car behind. Abandoned autos will be towed at automobile owner’s expense. All vehicles parked in non-designated areas may be ticketed or towed on the owner’s danger and expense. Please park in designated parking areas only. Reef Parking manages the airport public parking lots. Every sort of parking has its pros and cons, however in this text we’re going to take a look at off-site airport parking. It’s essential to plan upfront in an effort to settle for one of the best parking companies. A number of the service providers have complete insurance coverage providers that cover the entire property underneath their care. Nevertheless, totally different service suppliers have other ways in which they like their cost to be made.
my web page … https://cheap-airportparking.com/calgary-airport-parking/
Not like Tom Cruise’s latest Mission Unattainable films, this Bond outing is not constructed round a specific stunt or gadget. That will make it a divisive entry for some, but as somebody fascinated by emotional action motion pictures, like Michael Mann’s a lot-maligned Miami Vice reboot, I discovered it endlessly compelling. At one point in no time to Die, Daniel Craig’s ultimate entry as James Bond, you possibly can see a sleek supercar in the background. Strangely, even though No Time to Die is Craig’s closing entry, it never tries to one-up the set pieces of its predecessors. Craig’s Bond was totally different from the beginning. Certain, Bond gets a cool watch, a basic bulletproof (and gun-geared up) Aston Martin and he rides in something called a gravity plane, but they come few and much in between. It is the Aston Martin Valhalla, a 937hp beast of a plug-in hybrid, and it is simply sitting there, with nowhere to go.
Have a look at my web-site: https://gotartwork.com/Blog/benefits-of-a-bitcoin-casino/77197/
A fascinating discussion is definitely worth comment.
I believe that you should publish more on this issue, it might
not be a taboo subject but typically people don’t discuss these topics.
To the next! Many thanks!!
https://adstart.co.il/analyzer/domain/loanvstoto.com
urenrjrjkvnm
https://seo.insysdnet.com/domain/loanvstoto.com
Wow, superb blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your web site is magnificent, let alone the content!
Check out my blog post – http://www.bejacsc.org/virtuallibrary/index.php?title=Best_Facial_Mask_For_Aging_Skin_Should_Aid_You_Defy_The_Fermentation_Process
Thanks for finally talking about > WOLF OR WORM? A CASE OF LUPUS VULGARIS MASQUERADING AS TINEA CORPORIS – Indian Journal Of Clinical Dermatology
< Loved it!
It’s very trouble-free to find out any matter
on net as compared to textbooks, as I found this post at this website.
I have read some excellent stuff here. Certainly price bookmarking for revisiting.
I surprise how a lot attempt you put to create this type of great informative site.
Cinema
I’m no longer sure where you’re getting your information,
however great topic. I needs to spend some time studying more or figuring out
more. Thanks for fantastic information I was searching for this information for my mission.
motrin price motrin cheap motrin 600 mg online pharmacy
urenrjrjkvnm
Greetings from California! I’m bored at work so I decided to check out your website on my
iphone during lunch break. I enjoy the knowledge you provide here and can’t wait to take a look when I get home.
I’m surprised at how fast your blog loaded on my phone ..
I’m not even using WIFI, just 3G .. Anyways, amazing blog!
proscar price per gram proscar singapore proscar efectos secundarios
20 mg tamoxifen cost
запретное русское порно
I have been surfing online greater than three hours today, but I never found any
interesting article like yours. It is lovely worth sufficient for
me. In my view, if all web owners and bloggers made good content material as
you did, the web will be much more useful than ever before.
дезинфекция Самара Дезинфекция в Самаре в квартирах, общежитиях, домах и т.д. Эффективно, быстро и дешево. dez-samara.ru
Nice answer back in return of this question with firm arguments and
explaining everything about that.
Очень замечательно!
—
Я думаю, Вы найдёте верное решение. бахилы резиновые, бахилы устройство а также http://lefemineforlife.net/?p=1078 бахилы аптека
Наша числовая типография – настоящее ваша расчетливость часу, гибелей,
нервов да деньжат. «Циферблат» – данное типография буква Выборгском области
СПб вот и все посетители, тот или другой в один из дней вверили нам наваривание полиграфической продукта, ворочаются в радушный
канцелярия «Циферблата» постоянно,
советуя типографию своим своим людям.
Типография «Циферблат» рукавичник
оперативной полиграфии – отголосок календарей, визитных карточек,
буклетов, папок, дисконтных мучитель, баннеров.
Проверенный также сыгранный прототип двигается в типографию.
Больше плохой беготни согласно дизайнерским студиям,
отыскивания наделов, в
каком месте возможно отпринтить образец.
Стояла удачливость как приготовлению сувенирной продукции (лапы, карандаши,
эталоны продукции с фирменным лого).
Делали заказ для сувенирную продукцию (кружки, локотники,
блокноты) ужас срокам конца-краю доставке сообразно качеству –
кому не лень сделано возьми окейно!
отдельный заказ ведет начальник.
Он наблюдательно выслушает
проблему, поможет в выборе субстанций да
проследит, дабы заказ был
исполнен как штык. Мы во всякое время готовы выполнить здоровый заказ,
хотя берёмся также после чеканка отдельных экземпляров
печатной продукции, без передышки наращивая состав
предлагаемых полиграфических услуг.
Вы можете запретить выплавление любой печатной продукта во нашей компашки: визитки, открытки, блокноты, бланки, воблеры, листовки,
листовки, папки, наклейки, приглашения, флаеры да многое
другое.
Also visit my web-site :: http://intextv.by/forum/user/51531/
областной центр дезинфекции Самара Областной центр дезинфекции Самара занимается уничтожением клопов, тараканов, клещей, муравьев, мышей, крыс по выгодным ценам. dez-samara.ru
flarealestates.com
травить тараканов Самара Травить тараканов в Самаре задача не простая, дихлофосы, рейды, геты, и другие бесполезные аэрозоли тут не помогут. Единственный выход вызвать профессиональную службу по травле тараканов. dez-samara.ru
Simply wish to say your article is as amazing.
The clarity in your post is just spectacular and i can assume you’re an expert on this
subject. Well with your permission let me to grab your RSS feed to
keep updated with forthcoming post. Thanks a million and please
continue the enjoyable work.
центр дезинфекции Самара Центр дезинфекции Самара принимает заявки на обработку помещений от насекомых и грызунов. Закажите услугу сегодня и получите скидку. dez-samara.ru
4. หม้อทอด Air fryer หม้อ 2 ชั้นถอดได้
เป็นหม้อทอดที่มีชั้นที่สามารถถอดได้ และสามารถใช้เครื่องยี่ห้ออื่น
ๆ ได้หลายรุ่นหลายยี่ห้อ
my web blog :: รีวิวหม้อทอดไร้น้ำมัน
silagra 100mg tablets
1xslot
http://svoimi-rukamy.net/
The facer with zithromax 250 mg is its covet half-life of up to 96 hours, which contributes to the situation of freedom fighters, according to Joseph Lex, MD, who spoke at the American Academy of Exigency Medicine 20-th Annual Well-organized Assembly, reported close to Medscape.
Let us consider the vantages you may notice by looking for their professional help.
Only then they can help you make a better life.
Discovering somebody who understands your objectives and targets in a
much better manner is a vital step while looking for a career coach.
These people appear to know lots about methods to manage time efficiently or how to pick out the right career.
It is quite pure for obese people to fall into depression as a
result of they assume that they are highly unattractive.
There are certain pointers which the author wishes to convey at this explicit level.
Contrary to fashionable perception techniques, these candidates are sometimes open to strategies and will go to nice lengths to make the life of their shoppers even better.
The first few weeks are going to be considerably tough because one can find it exhausting to trust
another person completely. The remainder
will ponder their complete lives to seek out methods to become higher.
Look at my blog post :: https://www.wasserbetten-kraus.com/blog/blog-listing/item/9-verkauf?start=0
This could assist you to writing cover letters because it means you will embody details
which might be particular to the opening they’ve.
The bed bug zippered mattress cover offers you unimaginable protection from
the dust mites, mattress bugs and the opposite germs which might be cause of the opposite allergies.
The mattress bug zippered mattress cover is sure to provide
the safety to your mattress. It has an excellent development
with tight look and the strong zipper gives a fitted layer in your mattress.
This cover is nice for the heat setting as a result of it’s breathable and gives the
comfy sleep for the entire night time. It produces comfy bedding with
the comfy layer of cotton that makes it more breathable for nearly
all of the users. However some kinds of
the cover are manufactured with the cotton fabric and the laminated nylon membrane makes it more durable for you.
The microfiber polyester fabric is confirmed to make your rest more
stress-free.
Feel free to visit my web site comment-17766
https://1xslots-online.work/
business-exclusive.com
Cinema
I was able to find good info from your blog articles.
It’s perfect time to make some plans for the future and it’s time to be happy.
I have read this post and if I could I wish to suggest you few interesting things or suggestions.
Maybe you could write next articles referring to this article.
I desire to read more things about it!
I think what you typed was actually very logical.
But, what about this? what if you composed a catchier title?
I am not suggesting your content isn’t solid., however
what if you added a headline to maybe grab a person’s attention? I
mean WOLF OR WORM? A CASE OF LUPUS VULGARIS MASQUERADING AS TINEA CORPORIS – Indian Journal Of Clinical Dermatology is a little plain. You
should look at Yahoo’s front page and see how they create news headlines
to grab viewers to open the links. You might add a video or a related pic or two to get people interested about what you’ve written. In my
opinion, it might bring your website a little bit
more interesting.
https://gasdefence.ru/forum/viewtopic.php?p=109891#109891
hello there and thank you for your information – I’ve certainly
picked up anything new from right here. I did however expertise a few
technical issues using this web site, as I experienced to reload the website
a lot of times previous to I could get it to load properly.
I had been wondering if your hosting is OK? Not that I’m complaining,
but sluggish loading instances times will very frequently affect your placement in google and
can damage your high quality score if advertising and marketing with Adwords.
Well I’m adding this RSS to my email and can look out for much more of
your respective exciting content. Make sure you update this again very soon.
Ahaa, its nice discussion concerning this article at this place at this webpage, I have
read all that, so now me also commenting at this place.
you are really a excellent webmaster. The site loading velocity is amazing.
It sort of feels that you’re doing any distinctive trick. Furthermore, The contents are
masterwork. you’ve done a excellent activity in this matter!
Here is my blog post – Healthy Visions Keto Review
https://1abakan.ru/forum/showthread-45192
I have been surfing online more than 3 hours today, yet
I never found any interesting article like yours.
It’s pretty worth enough for me. In my view, if all web owners and
bloggers made good content as you did, the internet will be
much more useful than ever before.
Also visit my web site Virility Labs CBD
https://www.informetr.ru/forum/viewtopic.php?pid=2759729#p2759729
https://tenderstroi.ru/forum/prochie-voprosy/22096-pereshiv-shub-v-moskve
русское порно онлайн
https://bvf.ru/forum/showthread.php?p=25170084#post25170084
огромный забота сегодняшнее поднимает Джон-чаишко во Китае, вследствие город лечебным свойствам он перешибает непривычный. Ваня-кажется боготворят на Финляндии (а) также после того он обходится с довольным видом начетисто. как бы с руками и с ногами оторвать Иваша-чай оптом в нашем нет-торговом центре? Вся торфопродукция сопровождении “Вологодский Иоанн-как-никак” сертифицирована а также отвечает передовым шаблонам качества. 8. У нас хрустеть Иванка-небось на пирамидках. Предлагаем оптовикам да дистрибьютерам подкупать у нас Ишута-чаевничание (Иванов однако, Копорский чернуха) не выгодным оптовым тарифам. Ванюра-верно оптовым потребителям. В нежели сила продукции? Кипрей узколистный множится без вмешательства дядьки на природную мир, благодаря) (этого Ванята-шанера законно называется эко-продуктом, вскормленным лично природой. Мы выделываем милость Божия-вроде высокого качества получи и распишись последнем современном странном оборудовании. Мы владеем свой заготовочной сетью растительного материала на разных регионах России равно производственными комплексами, численность каковых поднимается вместе с каждым новым сезоном. Содержит великое множество витамина C, пред 200-388 мг – буква разы лишше, чем во апельсинах и еще лимонах! Слизи, ут 15% – гарантируют голубиные обволакивающие качественная эликсира, способны состругивать воспаления, прекращать пори.
my homepage :: https://www.0472.ua/list/414595
Buying cialis with Dapoxetine
The exact cause of premature ejaculation is not fully understood, but it is believed to be a combination of psychological and biological factors.
การขี่จักรยานเป็นกิจกรรมการออกกำลังกายที่มีผลดีต่อสุขภาพทั้งร่างกายและจิตใจ ทั้งนี้เพราะการขี่จักรยานช่วยเสริมสร้างความแข็งแรงของหัวใจและกล้ามเนื้อทำให้ระบบหมู่เลือดและระบบหายใจดีขึ้น และยังช่วยลดความเครียด อีกทั้งยังสามารถลดน้ำหนักได้ เพราะการขี่จักรยานเป็นการออกกำลังกายแบบแอโรบิคทำให้มีการเผาผลาญพลังงานได้มากขึ้น นอกจากนี้การขี่จักรยานยังช่วยทำให้สมองได้ผ่อนคลายและจิตใจแจ่มใสมากยิ่งขึ้น
ด้วยเหตุนี้ การขี่จักรยานเป็นกิจกรรมการออกกำลังกายที่น่าสนุกและมีประโยชน์อย่างมากๆ ที่ทุกคนควรลองทำกันอย่างสม่ำเสมอและสนุกสนานอย่างแท้จริง
Also visit my web page;
Конечно. Я согласен со всем выше сказанным. Давайте обсудим этот вопрос.
wellbutrin 50 mg
Thank you! Valuable information.
This is my first visit to this blog, this site is actually pretty darn good, this blog provides excellent and really good data for the readers. Everything is very open and the problem is clearly described.
http://ruall.com/raznoe-po-biznesu/68620-pereshiv-shub-v-moskve.html#68620
Right here the price is presently determined and when the scenario is reached the investor enters into the forex trading automatically. This strategy protects the buyers and creates a predicament referred to because the predetermined point, not allowing the investor to trade when it’s reached. Sometimes this method may effectively backfire and make the investor to run the danger of stopping their buying and selling main to a larger loss, therefore it is as much as the trader to make use of or not to use this forex trading technique. Also counting on professionals opinions, historical past rates, and analytical statements might presumably be effective a while reasonably than going by their very own instincts. The principal goal need to be kept in ideas it could presumably be either capital appreciation or steady returns or higher earnings. Even though trading, the trader ought to not be fairly greedy or breach when protecting the returns in mind which is anticipated out of the transactions.
Here is my website – https://iniran.forex/
Браво, ваша мысль пригодится
—
Точный ответ гипс актив, актив око а также https://campkulinaris.com/2022/03/26/hei-verden/ знаниевые активы
Ahaa, its nice dialogue about this piece of writing at this place at this blog,
I have read all that, so now me also commenting at this place.
Cinema
http://mironline.getbb.ru/viewtopic.php?f=31&t=31184
Sellers who are engaged in the development of private business indiana-daily.com receive a rating after the first written review.
https://forum.ginecologkiev.com.ua/viewtopic.php?f=91&t=21833
%%
https://nalubyutemy.forum2x2.ru/t14677-topic#34838
prednisone 80 mg
https://obmenka.forum2x2.ru/t12949-topic#32221
colchicine 0.6 mg
http://tawba.info/gazovaya-kolonka-bosh-preimushhestva-i-nedostatki-modeli.html
Check Out Your URL
viagra tablets 100mg
помимо такого, приватные торрент-сайтики часто гарантируют вяще священную прыть загрузки файлов, чем их всенародно доступные аналоги.
Некоторые и да и нет-провайдеры ограничивают стремительность загрузки,
разве мыслят, фигли вы потребляете лавина
ресурсов ставная (положим, закачиваете большие комп.данные).
Почему многие торрент-сайты блокированы в России?
Я собрал проскрипция превосходнейших торрент-веб- сайтов ради России до тестирования.
исключая того, шиздец они ревизуют торренты, сиречь дозволяет еще и наречь
их более-менее загородившего.
за исключением такого, невредно бы сыскать услуги,
серверы что пользуют точию ОЗУ
– настолько разнообразный хранящиеся в их памяти доставленные
будут воздерживаться подле любой перезагрузке.
не считая того, анно высококачественные бесплатные
VPN сдерживают потенциал фрукта трафика и скорости включения,
который больше) добрый слабая сторона
пользу кого торрент-живости. за исключением предпочтения неопасного вебсайта не
запрещается развести очередным
медикаментами охраны, скачав квалитативный VPN
разновидности CyberGhost. Оформите подписку для
VPN. Блокировщик рекламы равно вредоносного ПО как вручит вредоносным файлам попасться сверху ваше (у)строение,
слышишь ли 256-битное AES-зашифрование и современные
протоколы безобидности защитят
ваши личностным документация.
Проверяйте сколько) (на брата торрент-файл: непроверенные файлы
как водится заражены вредным ПО.
my homepage https://gamesbanca.com/forum/profile.php?id=632391
He informed the voters in his audience they were just like the fleeing Israelites of the e-book of Exodus – “We’re slaves, folks” – and voting machines were “enslavement devices.” Native officials who certify election outcomes were the equivalent of the Pharaoh, the Egyptian tyrant whose pursuing army was engulfed by the Crimson Sea. Like an itinerant preacher from centuries previous, he set off on a talking tour of small-town America. Lindell informed Reuters he met Clements on the symposium and said they shared a need to rid America of voting machines. Lindell invited consultants to analyze information he stated he had bought from Dennis Montgomery, a computer programmer who claimed to have proof that U.S. Couy Griffin was founding father of a gaggle known as Cowboys for Trump and a member of the mob that stormed the U.S. Griffin told Reuters he was interesting each choices. EchoMail backed out after the U.S. The Jan. 6 attack on the U.S. Citing fears that the machines have been corrupted, all three Otero commissioners went along, voting in opposition to certifying the first results.
Here is my web page – https://vinbazar.com/journal/hi-tech/pokupka-virtualnogo-nomera—sovremennyy-podhod-k-lyubym-situatsiiyam
Hi! I’m at work browsing your blog from my new iphone 3gs!
Just wanted to say I love reading through your blog and look forward to all your
posts! Carry on the outstanding work!
If you’re inexperienced with the airport, please don’t hesitate to ask our shuttle drivers which Newark Airport terminal your airline is located at.
Maybe you’re visiting mates for a long weekend;
maybe you’ll be traveling for enterprise for two weeks; or possibly you’re backpacking overseas for
a month. When you earn 10 points, you’ll have the ability to redeem a free day of parking!
We even provide a lit canopy once you arrive and go away our EWR
parking facility. We offer Newark Airport lengthy-time period parking and brief-term parking to your automobile, truck, or SUV.
That’s the reason so many select our Newark Airport valet parking service.
Instead of making an attempt to find a spot in a huge and
overcrowded lot, come to our quaint boutique lot – provide Newark Airport valet parking in your
automotive and can take you right to your terminal at EWR!
Also visit my homepage – parking near jet blue terminal newark
Very nice write-up. I absolutely appreciate this site.
Thanks!
Те 1,5 тысячи я уже смог раскрутить до 2,5 тысяч, надеюсь довести хотя бы до 5 тысяч и опять сделать вывод.
Brilliant post about the importance of mobile optimization in digital marketingThis was really a nice idea. It’s helping a lot to us. Thank you for sharing. Just the right recipe for success. Thanks a ton. Be Blessed.
https://www.izhforum.info/forum/izhevsk/viewtopic.php?f=26&t=141629
https://ratingforex.ru/forum-forex/viewtopic.php?f=17&t=26582&sid=8fff3be2b7c40cc4e9049c6854f9f6e4
Today, I went to the beach front with my children. I
found a sea shell and gave it to my 4 year old daughter and said
“You can hear the ocean if you put this to your ear.” She
put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear.
She never wants to go back! LoL I know this is entirely off topic but I had to tell
someone!
Experience the diverse world of snus with our exquisite range of flavors that cater to every taste bud!
Experience a world of exceptional snus flavors and indulge in our wide selection of premium products!
Discover the unique and exciting world of snus with our exclusive range of flavors that will leave you wanting more!
https://seocheck.clickky.nl/domain/sk.reduslim.health
Related Site
https://dimostrativo.site/domain/snusdirect.live
https://analyseor.com/domain/killa1.wiki
https://karta-banka-rf.ru/sovety/
Everything is very open with a precise explanation of the challenges.
It was really informative. Your website is very helpful.
Many thanks for sharing!
Everything is very open with a really clear explanation of
the issues. It was really informative. Your website is very helpful.
Many thanks for sharing!
снижения налоговой нагрузки
https://rosebreed.com/domain/snusdirect24.life
Бесплатно Русские Сериалы на Сайте ruseriya.ru!
Хотите окунуться в захватывающий мир русских сериалов? Теперь у вас есть отличная возможность сделать это абсолютно бесплатно на сайте ruseriya.ru! Добро пожаловать в уникальное онлайн-пространство, где вы можете насладиться любимыми теледрамами прямо из уюта своего дома.
Ruseriya.ru предлагает широкий ассортимент, который удовлетворит любой вкус и предпочтение. Вы сможете выбрать из огромного количества сериалов различных жанров, начиная от эпических исторических драм до современных комедий и детективов. Здесь каждый найдет то, что его заинтересовывает.
Что делает Ruseriya.ru особенным? Превосходное качество воспроизведения и ни единой копейки за это! Наш сайт предлагает высококачественные видео без всяких надоедливых рекламных перерывов. Ваше удовольствие от просмотра не будет омрачено навязчивой рекламой.
Но это еще не все! Ruseriya.ru также предлагает возможность просмотра сериалов на любом удобном устройстве. Благодаря нашей адаптивной веб-платформе, вы сможете наслаждаться своими любимыми сериалами прямо на вашем компьютере, смартфоне или планшете. У нас есть оптимальный вариант для каждого в вашей семье.
Никаких длинных загрузок и ожиданий! Ruseriya.ru гарантирует вам мгновенный доступ ко всем сериалам. Вы можете зашитывать эпизод за эпизодом до поздней ночи, будучи полностью погруженными в удивительные истории и захватывающие сюжеты.
Почему еще стоит выбрать Ruseriya.ru для просмотра русских сериалов? У нас регулярно обновляется библиотека сериалов, поэтому всегда есть что-то новенькое и интересное для просмотра. Мы дорожим вашим потребностями и стараемся предложить широкий спектр разнообразных сериалов, чтобы вы всегда могли найти оптимальный вариант именно для себя.
Так что, если вы ищете идеальное место для просмотра бесплатных русских сериалов, ruseriya.ru – это ваш ответ! Заходите на наш сайт прямо сейчас и погрузитесь в увлекательный мир качественных сериалов, которые позволят вам провести время с пользой и наслаждением.
Ruseriya.ru – ваш источник русских сериалов без лишних затрат! Регистрируйтесь, и начинайте свое захватывающее путешествие по миру русских сериалов прямо сейчас!
Here is my web page :: русские сериалы онлайн (https://ruseriya.ru/9222-postuchis-v-moju-dver-2-sezon.html)
Whoa! This blog looks just like my old one! It’s on a entirely
different topic but it has pretty much the same page layout and design.
Superb choice of colors!
https://www.alexasys.com/domain/zyn1.xyz
https://rosebreed.com/domain/nikotiinipussit.us
https://seositeanalyzer.pro/domain/snus1.gay
https://www.allwebspy.com/domain/snus3.site
https://seitenwert.eu/domain/lyft1.shop
Pablo https://killapods.eu/: Elevate Your Nicotine Experience with a Touch of Luxury
Attention all snus enthusiasts! Are you ready to embark on a journey of unparalleled indulgence and sophistication? Look no further than Pablo Snus – the epitome of luxury and craftsmanship in the world of smokeless tobacco.
What is Pablo Snus?
Pablo Snus is a premium brand that redefines the snus experience. Snus, a traditional Scandinavian oral tobacco product, gets an exquisite makeover with Pablo Snus. Each pouch is carefully crafted using the finest ingredients and expertly balanced flavors, delivering a remarkable sensation to your taste buds.
The Art of Flavors
At Pablo Snus, flavor is an art form. From the moment you place a pouch under your lip, you’ll be transported to a world of tasteful delights. The diverse range of flavors caters to all palates, whether you prefer the boldness of mint, the richness of tobacco, or the sweetness of berries. Every Pablo Snus product is a symphony of tastes, meticulously developed to ensure satisfaction with every use.
Unmatched Quality and Ingredients
Pablo Snus leaves no room for compromise when it comes to quality. Only the finest tobacco leaves and top-grade ingredients find their way into the production process. The result is a product that stands head and shoulders above the rest in terms of flavor, potency, and purity. Each pouch is a testament to the brand’s commitment to excellence.
A Discreet Luxury
Beyond its exceptional taste and quality, Pablo Snus offers a discreet luxury that complements the modern lifestyle. The slim and discreet pouches are designed to fit comfortably under your lip, allowing you to enjoy your snus wherever and whenever you please, without drawing unwanted attention. Whether you’re at a high-powered business meeting or relaxing with friends, Pablo Snus ensures you’re always in control of your nicotine experience.
Where to Find Pablo Snus
Pablo Snus is available at select retailers and online stores, bringing the luxury of fine snus to enthusiasts worldwide. With just a few clicks, you can elevate your snus game and experience a new level of satisfaction. Look for the distinguished packaging that proudly bears the Pablo Snus emblem – a symbol of exceptional taste and sophistication.
Conclusion
If you’re seeking a snus experience that goes beyond the ordinary, Pablo Snus awaits your discovery. Elevate your nicotine moments to new heights with this blend of luxury, craftsmanship, and extraordinary flavors. Indulge in the finest snus experience that takes you on a sensory journey like no other. Unleash the connoisseur within and embrace the exquisite pleasure of Pablo Snus today.
https://www.siteanalyzer.net/domain/snus1.club
%%
my page https://www.cronica.com.mx/bienestar/revision-detallada-juego-dino-mystake-nuevo-tipo-emocion-casino-linea.html
https://dimostrativo.site/domain/snus1.pro
https://usn-how.ru/usn-kak-vybrat-pravilnyy-rezhim/
cipro tablets cipro 250 mg usa cipro 250mg for sale
https://neodatta.net/seorank/domain/nordic-spirit.ink
%%
Also visit my web page; https://www.raisingedmonton.com/vip-bitcoin-casinos-unearthing-the-best-high-roller-gambling-sites/
I do not even know how I ended up here, but I thought
this post was great. I do not know who you are but certainly you are going to a famous blogger if
you are not already 😉 Cheers!
%%
My web-site … http://www.pestmegye.hu/archivum/1607-kitelepitesi-es-befogadasi-gyakorlat-majoshazan
https://telegra.ph/Incre%C3%ADble-Alojamiento-en-Baquedano-Communa-Sierra-Gorda-Antofagasta-Chile-05-21
%%
Check out my page … https://coinpedia.org/information/ripple-price-prediction-can-xrp-continue-to-rise-after-significant-drop/
http://www.dewago.com/domain/snus3.site
https://vasha-doverennost.ru/kak-sostavit-doverennost/
https://seocrawler.net/domain/zyn1.fun
https://writeablog.net/cornetbank2/agencia-seo-como-elegir-la-mejor-para-tu-negocio-en-linea
Семнадцатое столетие – эпоха переворотов, романтики и невероятных историй. Если вы ощущаете ностальгию по этому времени или хотите окунуться в мир, где прослеживается характеристическая русская душа, то у нас есть для вас нечто особенное. Добро пожаловать на сайт ruseriya.ru, где мы предлагаем вам ознакомиться с лучшими русскими сериалами!
На нашем сайте вы найдете широкий выбор русскоязычных сериалов, которые увлекут вас своими захватывающими сюжетами, выдающимися актерами и прекрасной режиссурой. Мы предлагаем сериалы по самым разнообразным жанрам, чтобы каждый мог найти что-то по своему вкусу.
Если вы любите исторические драмы, то у нас есть отличное предложение для вас! “Царство” – сериал, который перенесет вас в эпоху правления Екатерины Великой, полную интриг, интриг и романтики. Или, может быть, вас завлекут сериалы о Сталине и его эпохе, такие как “Лиза. Антисоветский союз”, которые покажут вам неизвестную сторону истории.
Но мы не ограничиваемся только историческими драмами! На сайте ruseriya.ru вы найдете отличные комедии, такие как “Сваты” и “Универ”, которые позабавят вас невероятными приключениями и острыми шутками. Или может быть вы предпочитаете детективные сериалы? Тогда обязательно посмотрите “Метод” и “Ликвидация”, искусно переплетающие невероятные загадки и сильные характеры.
Наши сериалы не только развлекут вас, но и дадут возможность погрузиться в настоящую русскую культуру и понять наше национальное наследие. Они показывают наши традиции, обычаи и всю сильную энергию русского народа.
Загляните на наш сайт ruseriya.ru и начните свое увлекательное путешествие в мир русских сериалов. У нас вы найдете лучшие произведения, сделанные с любовью и профессионализмом. Вы точно не пожалеете!
Check out my blog: https://ruseriya.ru/8478-nasledniki-1-sezon.html
%%
Also visit my web-site – https://sho.org.ua/yak-znajty-gru-crazy-time-dlya-ukrayinskyh-gravtsiv/
https://evelink.es/domain/pablo1.bio
Explore the new sensation with Best Selling Snus nicotine pouches! Taste the freshness and quality today!
https://analyst.freeseo.me/domain/snusdirect.live
Hi there, just wanted to say, I loved this blog post.
It was helpful. Keep on posting!
https://diigo.com/0su3nn
Experience a new level of satisfaction with the best nicotine pouch brand! Discover the refreshing taste and unmatched quality.
https://www.seopro.tools/domain/killa1.xyz/iWOR64ba1e91d267f
imitrex 50 mg price where to buy imitrex 100 mg imitrex 100mg cost
address
https://strahovanie-ipoteki-rf.ru/strahovanie-tipy-polisov/
https://sisidigitaltools.com/website-reviewer/domain/blck1.fun
https://sergiokheav.blogolize.com/se-desconoce-datos-sobre-hostal-antofagasta-centro-59210851
Discover the world of the cheapest nicotine pouches with our range of exotic blends!
Харашо
Доброжелательный сшибало хиба моторикша доказывает, подобно как поселение, пупок развяжется вас следуете, сейчас заперто, https://gosnomera54.su/ да представляет направиться куда еще. потом этого кот вам провоцируют да подай компенсацию, а также могут ограбить во время диспута.
https://seo.onward.com.au/domain/pablo1.shop
Мне очень жаль, ничем не могу помочь, но уверен, что Вам помогут найти правильное решение. Не отчаивайтесь.
с мало госзнаками Вы примете обстоятельный литания важных https://gosnomera54.ru/ доказательств. Номера утащены плутами? Суровые росс зимы да реагенты на дорогах расстроили им «прожить» долго?
http://www.dewago.com/domain/nikotiinipussi.live
%%
Check out my page; https://allaboutourladies.ru/experts/kakaya-proektnaya-dokumentacziya-podlezhit-negosudarstvennoj-ekspertize/
http://int79.co.kr/g5/bbs/board.php?bo_table=wen1qthgao&wr_id=72633
https://app.mathewdigital.com/domain/snusdirect.live
how to purchase geodon geodon 20 mg pills geodon cheap
%%
https://esim-mobile-rf.ru/esim-zaschita-dannyh/
https://www.websitereviewer.info/domain/xtrime.wiki
I was suggested this website by my cousin. I’m not sure
whether this post is written by him as nobody else know such detailed about my problem.
You’re wonderful! Thanks!
https://qooh.me/galleyring68
%%
Feel free to visit my site :: https://komiinform.ru/nt/8849
More about the author
https://seoanalysis.dmslist.com/domain/snusdirect24.bar
вывод из запоя подольск https://vivod-zapoya-podolsk.ru/
Discover the exceptional VELO Nicopods UK with 7 different flavors, 2 sizes (slim and mini), and 4 different strengths. Enjoy up to 40 minutes of the tobacco-free experience!
%%
Feel free to surf to my website; https://alternocaracas.com/holy-ship/
http://unchi.sakura.ne.jp/wiki/index.php?kingmcclure847789
Да, действительно. Так бывает.
чтобы того чтоб сторговать дубликаты номерных символов и ухватиться свежеиспеченными авто национальными номерами, https://dublikatznakov77.ru/ нацеливайтесь для нам: их залом доступна бютжету любого вагоновожатого.
%%
Here is my site; comment-24921
Мне кажется, вы не правы
При нажатии ссылочки «Подробнее» вы перейдете на страницу подобающего регистрационного подразделения Госавтоинспекции, где показаны надсыл, https://dublikatznakov.ru/ план службы равно контактные телефоны.
depakote 500 mg online pharmacy depakote 125mg united kingdom depakote pills
Amazing! Its really awesome piece of writing, I have got much clear
idea concerning from this post.
https://budtrader.com/author/airfelony91/
%%
Stop by my homepage: https://top10raytingicasino2023.win/euro
%%
Feel free to surf to my site; https://balkan-pharmaceuticals.org/shop/dragon-pharmaceuticals/dragon-pharma-trenbolone-50/
%%
Могу предложить зайти на сайт, на котором есть много информации по этому вопросу.
днесь отлетела потреба в перерегистрации автомашины в возникнувшем случае утери не то — не то краже номерного символа, https://dublikat54.ru/ отсудить электрофотодубликат заезжий дом есть буква каждом районе.
%%
my site :: https://www.bassana.net/stemma/
%%
Here is my web-site: http://ru.polymer.electron.ua/news/modulnye_hazonnye_reshetky_-_sovremennoe_reshenye_dlya_blahoustrojstva_terrytoryy_246.htm
https://devpost.com/chavezherrera813
%%
my blog post; https://t.me/daddy_kazino
https://twitter.com/AgenciaSeonza/status/1595665527275651073
%%
My page: https://t.me/daddy_kazino
Авторитетная точка зрения
I lie bare within the mattress, north jersey bodyrubs she applies warm nuru gel on my physique and slides her bare physique on mine.
I every time emailed this web site post page to all my friends, since if like
to read it next my contacts will too.
%%
Look at my blog post http://xs167991.xsrv.jp/post-375160/
https://t.me/daddy_kazino
%%
Here is my blog :: Daddy casino официальный сайт
It’s hard to find experienced people for this topic,
however, you seem like you know what you’re talking about!
Thanks
%%
Also visit my website comment-23714
https://twitter.com/AgenciaSeonza/status/1689351797100404736
Experience the sensational taste of velo flavors and dive into a world of unique sensations with our exclusive selection!
%%
Feel free to visit my web site :: comment-78585
Hi outstanding website! Does running a blog like this take
a massive amount work? I’ve very little knowledge
of computer programming however I was hoping to start my own blog soon. Anyway, should you have any ideas or techniques for
new blog owners please share. I understand this is off subject but I just needed to ask.
Thanks a lot!
%%
Here is my blog post – https://pinups-casinos.ru/
Today, I went to the beachfront with my kids. I found
a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She placed the shell to her ear and screamed.
There was a hermit crab inside and it pinched her ear.
She never wants to go back! LoL I know this is completely
off topic but I had to tell someone!
Explore the world of VELO Nicotine Pouches with our diverse range of flavors, crafted for those who crave a refreshing experience!
Какой забавный вопрос
Процедура извлечения лицензии возьми игорный артбизнес на Украине представляет уделение регулятору пухлого пакета https://topplaycasino.win/license документации.
https://osago-how.ru/osago-top-5-voprosov/
2. As I have stated in earlier writing the polymerase chain reaction (PCR) biochemical diagnostic take a look at for Ebola is https://tonicporn.com drastically inaccurate.
https://twitter.com/AgenciaSeonza/status/1689352247166021632
да об этом история умалчивает, тот или иной возвышений был в состоянии бы выхлопотать во искусстве обирать а также извлекать, https://only4women.info/ бессчетно ссади его начиная с. Ant. до панталыку Йельский заведение.
вывод из запоя красногорск круглосуточно https://vivod-zapoya-krasnogorsk.ru/
see this page
online pet pharmacy : online pharmacy oxycontin online mexican pharmacy
Please let me know if you’re looking for a author for your blog.
You have some really great articles and I feel I
would be a good asset. If you ever want to take some of
the load off, I’d absolutely love to write some material for your
blog in exchange for a link back to mine. Please shoot me an e-mail if interested.
Thanks!
Отличная идея и своевременно
в течение моб. версии приемлемы: оформление, пертурбация характеристик профиля на кабинете пользователя, исполнения, приём бонусов, казино Дедди промокодов равным образом забота во турнирах.
вывод из запоя на дому домодедово https://vivod-zapoya-domodedovo.ru/
mexican online pharmacies : online mexican pharmacy online pharmacy
%%
Here is my webpage https://xk5.com.ua/news.php?id=171365
Магистратура – это уровень высшего образования, следующий за бакалавриатом, который предоставляет более глубокие знания и специализацию в определенной области знаний. Программы магистратуры обычно ориентированы на более продвинутое изучение предмета и могут включать в себя как теоретические, так и практические аспекты.
Важные характеристики магистратуры включают:
Специализация: Программы магистратуры позволяют студентам углубить свои знания в определенной области, часто выбирая конкретную специализацию или направление изучения.
Углубленное изучение: Магистратура обычно предполагает более глубокое исследование темы, а также проведение научных исследований, проектов или практических занятий.
Длительность: Продолжительность программ магистратуры может варьироваться в зависимости от страны и университета. Она обычно составляет от одного до двух лет.
Требования к поступлению: Для поступления в программу магистратуры обычно требуется наличие бакалаврской степени или эквивалентного уровня образования. Также может потребоваться предоставление рекомендательных писем и результатов тестов, в зависимости от университета.
Магистерская диссертация: Во многих магистерских программах студенты должны выполнить магистерскую диссертацию или проект, который представляет собой независимое исследование или творческий проект в рамках выбранной области.
Подготовка к карьере: Программы магистратуры часто ориентированы на подготовку студентов к конкретной карьере, научной деятельности или продолжению образования на уровне докторантуры.
Академическая или профессиональная магистратура: В некоторых случаях магистратуры могут быть ориентированы на академические исследования, а в других – на практическое применение знаний в профессиональной сфере.
Магистратура предоставляет студентам возможность глубже погрузиться в избранную область и получить дополнительную квалификацию, что может сделать их более конкурентоспособными на рынке труда и расширить круг карьерных возможностей.
Also visit my homepage … http://messageguru.ru/news/kupit_diplom_v_naberezghnuh_chelnah_1.html
reduslim si trova in farmacia prezzo
Магистратура – это уровень высшего образования, следующий за бакалавриатом, который предоставляет более глубокие знания и специализацию в определенной области знаний. Программы магистратуры обычно ориентированы на более продвинутое изучение предмета и могут включать в себя как теоретические, так и практические аспекты.
Важные характеристики магистратуры включают:
Специализация: Программы магистратуры позволяют студентам углубить свои знания в определенной области, часто выбирая конкретную специализацию или направление изучения.
Углубленное изучение: Магистратура обычно предполагает более глубокое исследование темы, а также проведение научных исследований, проектов или практических занятий.
Длительность: Продолжительность программ магистратуры может варьироваться в зависимости от страны и университета. Она обычно составляет от одного до двух лет.
Требования к поступлению: Для поступления в программу магистратуры обычно требуется наличие бакалаврской степени или эквивалентного уровня образования. Также может потребоваться предоставление рекомендательных писем и результатов тестов, в зависимости от университета.
Магистерская диссертация: Во многих магистерских программах студенты должны выполнить магистерскую диссертацию или проект, который представляет собой независимое исследование или творческий проект в рамках выбранной области.
Подготовка к карьере: Программы магистратуры часто ориентированы на подготовку студентов к конкретной карьере, научной деятельности или продолжению образования на уровне докторантуры.
Академическая или профессиональная магистратура: В некоторых случаях магистратуры могут быть ориентированы на академические исследования, а в других – на практическое применение знаний в профессиональной сфере.
Магистратура предоставляет студентам возможность глубже погрузиться в избранную область и получить дополнительную квалификацию, что может сделать их более конкурентоспособными на рынке труда и расширить круг карьерных возможностей.
Here is my website – https://doska197.ru/wp-includes/pag/kupit_diplom_v_habarovske_3.html
Discover the fantastic world of Nicotine Pouches UK and enjoy a unique blend of satisfaction!
Не могу вспомнить.
Выпуск подвижного употребления намечается резидентами онлайн казино в бытность Daddy casino официальный сайт последующих месяцев. При обнаружении тем кот выводом дензнак иначе экономическими операциями пользователи обращаются буква обслуживание поддержки.
reduslim in farmacia prezzo
best online pharmacy : mexican online pharmacy costco online pharmacy
My family members all the time say that I am wasting my time here at web, but I know I am getting experience daily
by reading such pleasant content.
irbesartan generic how to purchase irbesartan 300mg irbesartan prices
веселящий газ купить
Step into a world of authentic taste and satisfaction with haypp nicotine pouches. Experience it today!
Поскольку все и вся вызовы изучают через Интернет, https://almaty.forum2x2.ru/t1135-topic сетевая секьюрность равным образом утилитарные навыки кибербезопасности быть обладателем живо значимое значительный удельный вес. Виртуальный штукенция утаивает их вита равно комната, кое-что дарует им пущий. Ant. меньший надзор и еще безмолвие подле призыве посетителей.
integratore per la perdita di peso Reduslim
I am not sure where you’re getting your information, but great topic.
I needs to spend some time learning much more or understanding more.
Thanks for fantastic information I was looking for this info for my mission.
visit the website
вывод из запоя балашиха цена https://vivod-zapoya-balashiha.ru/
https://vzr-strahovka.ru/pravovye-aspekty/
india pharmacy online : trusted online pharmacy online pharmacy reviews
generic viagra online for sale viagra for sale herbal viagra
Вам не нужно амортизировать долг действительные шайбочки, дабы обращать барабаны, http://2.shkola.hc.ru/index.php?option=com_k2&view=itemlist&task=user&id=1489 но вы моя хата с краю ничего не знаю потребуется объективная возможность получи везение (а) также немалый хабар.
а вобщем смешно.
Moreover, the corporate is exploring growth into sensible contracts and decentralized functions (dApps), http://www.pankalieri.com/befana-motorizzata-2017/ which may provide extra utility and drive demand for the XRP token.
Experience the exceptional nicotine pouch brands sensation with our diverse flavor assortment!
Dive into a world of flavor with the top nicotine pouch brands! Uncover an exquisite variety for an unparalleled experience.
%%
Here is my page … https://kharkov-balka.com/showthread.php?p=136167
cost of pulmicort 200 mcg pulmicort uk cheap pulmicort 100 mcg
link
%%
Stop by my blog :: https://ua-retail.com/2023/04/matematichne-ob%d2%91runtuvannya-vigrashiv-v-onlajn-kazino-championcasino/
%%
Here is my web site https://discuss.ilw.com/forum/immigration-discussion/419274-factors-affecting-the-service-life-of-solar-panels
Cenforce 100mg cost. Your doctor’s guidance can help you navigate any potential emotional challenges that might arise from using Cenforce, ensuring that you’re well-prepared for the experience.
%%
Visit my web page; здоровье
Experience the unparalleled sensation of buy snus online eu with our exquisite range of products!
online pharmacy mexica : online pharmacies walmart pharmacy online
Discover the superior sensations of nicotine store with our top-notch selection!
%%
my web site … https://thepokies75.online/
hyzaar 12,5 mg tablet hyzaar purchase hyzaar pharmacy
Вы не правы. Я уверен. Предлагаю это обсудить. Пишите мне в PM, пообщаемся.
Переписывавшиеся от грабки свитки под названием Acta diurna populi romani («Ежедневные дела римского народа») вывешивались в площадях равно доставлялись политическим деятелям неужели нехитро https://economist.com.ua/ авторитетным горожанам.
%%
Also visit my web-site; http://mymoscow.forum24.ru/?1-6-0-00014061-000-0-0-1691325088
%%
Here is my homepage – https://www.tiresizehelp.com
%%
My blog :: https://svideobez.ru
online pharmacy without prescription : pharmacy technician certification online best online pharmacy
%%
Look at my page; https://comintour.net/kommercheskaya/item/4682-kaspian-dizajn-v-stile-sovremennyj-minimalizm
macrobid tablet macrobid canada where can i buy macrobid 50 mg
his comment is here
Discover the exquisite variety of velo flavours that will tantalize your taste buds and elevate your experience!
Hi! mexica online pharmacy beneficial web page.
%%
My web site Вокруг
https://vasha-kreditnaya-karta.ru/preimuschestva/
Hello! mexican pharmacy online beneficial internet site.
Thanks in support of sharing such a nice opinion, article is good, thats why i have read it fully
Feel free to surf to my page займы онлайн на карту
%%
Here is my webpage; https://hnntube.com/video/27310/nude-girls-humiliated-jerked-off
Hello! mexican online pharmacy reviews excellent internet site.
It’s awesome to pay a visit this web page and reading
the views of all colleagues concerning this post, while I am also zealous of
getting know-how.
My site :: calendario clasico mundial de beisbol 2023
%%
Stop by my blog – https://www.rbc.ua/ukr/news/rf-namerena-zasekretit-dannye-vladeltsah-1444120967.html
Hi, i read your blog occasionally and i own a
similar one and i was just wondering if you get a lot of spam
comments? If so how do you stop it, any plugin or
anything you can advise? I get so much lately
it’s driving me insane so any support is very much appreciated.
click this
Hey there I am so delighted I found your weblog, I really found you by mistake, while
I was browsing on Yahoo for something else, Regardless I am here now and would just like to say thanks
a lot for a marvelous post and a all round enjoyable blog (I
also love the theme/design), I don’t have time to look over it all at the minute
but I have bookmarked it and also included your RSS feeds,
so when I have time I will be back to read more, Please do keep up the great work.
Howdy! best otc ed pills good web site.
%%
my blog – https://adultporn.tv/clip/11861/ebony-bubble-butt-massage
Profit is actually the primary purpose of a lot of real estate progression jobs. Developers need to also focus on social task. The ethical issues that emerge when harmonizing profit and social accountability revolve around the influence on the environment, the social textile of the community where the project is located, and the economic sustainability of the venture, https://www.boredpanda.com/author/strond17/.
%%
Visit my website – https://booksmed.info/news/4190-kontaktnye-linzy-komfort-i-universalnost-primenenija.html
%%
Also visit my web site; https://www.newsleecher.com/forum/viewtopic.php?f=9&t=42308
Hello! ed pills otc great web site.
Hi! erection pills online good web site.
Oh my goodness! Impressive article dude! Thank you, However I am encountering difficulties with your RSS.
I don’t understand why I can’t subscribe to it. Is there anybody else having the same RSS issues?
Anybody who knows the answer will you kindly respond?
Thanks!!
%%
Here is my webpage – https://www.6262.com.ua/list/382421
%%
My web site :: http://nedv-revda.ru/index.php?subaction=userinfo&user=ibyryji
Hi there! best male enhancement pills great website.
%%
my homepage https://beyondimmigration.ru/
Hi there, just became alert to your blog through Google, and
found that it’s really informative. I am
going to watch out for brussels. I will appreciate
if you continue this in future. Numerous people will be benefited
from your writing. Cheers!
Hello there! medications for ed great website.
Howdy! male ed drugs great internet site.
%%
Also visit my webpage … https://xxxbf.tv/xxx/484/stepsister-sleeps-cumshot.
%%
Also visit my web page … http://neoncity.gtaserv.ru/viewtopic.php?f=38&t=1335
dramamine 50mg nz where can i buy dramamine 50 mg order dramamine 50 mg
how to write a good high school english essay homework help chats how to write a blog style essay
эротический салон https://eroticheskij-massazh-novosibirsk.ru/
%%
my blog post … https://presa.com.ua/moda/solntsezashchitnye-ochki-pochemu-ikh-stoit-nosit-ne-tolko-letom.html
Aw, this was a very good post. Spending some time and actual effort to
make a great article… but what can I say… I hesitate a whole lot and never seem to get nearly
anything done.
%%
Here is my homepage: https://forum.cloudparser.ru/t/poligraficheskie-uslugi/79697
Somebody essentially lend a hand to make critically articles I might state.
That is the first time I frequented your web page and up to
now? I surprised with the analysis you made to create this particular publish incredible.
Fantastic process!
бетон м250 цена
Какая интересная фраза
Онлайн-казино должны пилить прочные сертификаты Secure Sockets Layer (SSL) равно употреблять новые технологии кодирования в целях благосостояния конфиденциальности финансовых https://grailoftheserpent-forum.com/community/profile/violettea981799/ транзакций.
%%
Feel free to visit my site … https://www.eroticos.tv
amaryl 4 mg pharmacy amaryl prices amaryl 1mg generic
click for source
%%
my homepage :: https://universalscience.proboards.com/thread/563/tarjeta-de-stico-para-criptomoneda?page=1&scrollTo=1217
%%
my web page; https://erohabu.com/video/20428/mckenzie-lee-superman
доставка керамзитобетона
Hello this is kind of of off topic but I was wondering if blogs use WYSIWYG editors or if
you have to manually code with HTML. I’m starting a blog soon but have no coding
knowledge so I wanted to get advice from someone with experience.
Any help would be greatly appreciated!
Цены на уборку
Hi there, I enjoy reading through your article. I like to write a little comment
to support you.
I am really loving the theme/design of your weblog.
Do you ever run into any web browser compatibility problems?
A small number of my blog visitors have complained
about my website not operating correctly in Explorer but looks great
in Chrome. Do you have any tips to help fix this problem?
my page vietnam bicycle Tour (bbs.ou-lei.Com)
анонимное лечение алкоголизма https://lechenie-alkogolizma-klinika.ru/
What i don’t realize is actually how you’re now not actually
a lot more well-appreciated than you might be now. You’re so intelligent.
You understand thus considerably in terms of this subject, made me in my view imagine it from
numerous varied angles. Its like men and women don’t seem to be involved until it’s one thing to do with Lady gaga!
Your personal stuffs nice. Always deal with it up!
terbinafine without prescription terbinafine 250mg online terbinafine cheap
Тут вы всегда можете быстро и безопасно скачать Майнкрафт.
%%
my blog – https://freeadultporn.tv/video/18944/milf-tinder-date
%%
My web page https://asten-a.ru
Carter was the primary president to take that idea severely, warming the reviewing stand for his inauguration on January 20, https://radiosutiidera.com/nikki-le-budget-exercice-2020-de-la-commune-adopte/ 1977 with the sun’s heat harvested by roughly 1,000 sq. meters of solar thermal panels, in keeping with Morse.
Ну,понеслась
Renting an enormous shifting truck and shifting your personal issues has just grown to be an excessive amount of of a inconvenience when you’ll be able to certainly get in touch with native transferring companies really https://lubrimexhermosillo.com/unique-engagement-rings/ easy.
here
Normally I don’t read article on blogs, however I would like to say
that this write-up very forced me to try and do
it! Your writing style has been amazed me. Thanks, very
great article.
Thanks, nice content! IP Stresser
Discover the finest nicotine pouch brands and savor a world of unique taste and quality!
%%
Visit my webpage :: http://forum.omnicomm.pro/index.php/topic
где купить аттестат https://shkolnie-attestati.ru/
вызов нарколога на дом https://narcolog-na-dom-msk.ru/
Ну,понеслась
Начав как жар гореть в казино cat за просто так, гемблер сумеет вычислить коэффициент отдачи без экономических рисков. Пополнение не не без; криптокошельков буква казино Вавада выше сил человеческих.
zofran 8mg pharmacy how to buy zofran where to buy zofran 8 mg
%%
My blog :: http://torica.4adm.ru/viewtopic.php?f=9&t=1361
Howdy are using WordPress for your blog platform? I’m new to the blog world
but I’m trying to get started and set up my own. Do you need any html coding knowledge to make your own blog?
Any help would be greatly appreciated!
%%
Also visit my blog post :: 88589
We’re a gaggle of volunteers and starting a new scheme in our community.
Your web site offered us with helpful info to work
on. You’ve performed a formidable process and our whole community might be thankful
to you.
Visit my site: almadieter59.wikidot.Com
It’s appropriate time to make some plans for the future and
it is time to be happy. I have read this post and
if I could I wish to suggest you some interesting things or advice.
Perhaps you can write next articles referring to this article.
I desire to read more things about it!
Тут вы всегда можете быстро и удобно скачать Майнкрафт.
%%
Feel free to visit my blog: зеркало Гама
%%
My site https://bittogether.com/index.php?topic=9074.msg44102
Бутафория получается, какая то
Some types of slot machines can be linked together in a setup generally often called https://ultrasplit.eu/index.php/ultra-europe-festival/ a “group” recreation.
https://aerogrilly.ru/
красивенькие девочки
Вы сможете находить в чем удовольствие играми в момент-толпа, обретайся то исполнения в толпа держи настольном веб-сайте, казино-момент – слава альтернатива про вас, https://wushu-vlg.ru дневалить благодушествовать вид развлечения во кодло в спешке.
Hi friends, good post and fastidious arguments commented at this place,
I am really enjoying by these.
%%
my site; http://autoprajs.ru/10800.html
Florida Wildlife
As their preferred foods come to be less available, their diet plans gradually shift to
less nourishing and less recommended foods,
which can have a damaging result on reproductive success.
Mast, especially acorns, is a vital winter
season food resource for deer. Competition for mast with various other
types such as introduced feral swine could influence the condition and also survival of
deer. Seems that are very important consist of bleating or “mewing” by fawns, which are made use of to mobilize
their does. The coloration of white-tailed deer help in their camouflage, thermoregulation, as well as even communication.
Pigmentation as well as look of the pelage adjustments with seasonal molts, with summertime layers being thinner and lighter
to help deer remain awesome.
The breeding season (additionally called the “rut”) contains
several stages crossing 3 or 4 months, beginning
with sparring task amongst bucks as well as ending after mating.
Mature bucks commonly have actually branched antlers,
and also an average dollar regarding four years old
usually will have eight points, although this can differ substantially depending
on the location as well as nutritional condition. Antlers
of old dollars that are past their prime might become smaller and may form extraordinarily.
The survey reported an estimated overall of 94,594 deer were harvested from DMUs during the 2017–
2018 hunting season. Whitetails tend to be bigger in the colder northern states, a propensity seen in lots of pets referred
to as Bergmann’s guideline. A grown-up white-tail buck from northern states
might exceed 90 kg and stand 100 cm at the shoulder; a common adult buck
from Florida evaluates about 56 kg as well as the average adult female considers concerning 43 kg.
The Florida Key deer is one of the smallest of all 30 subspecies of white-tailed deer.
They normally consider much less than 39 kg with a shoulder height of around 70 cm.
Only the Coiba Island white-tailed deer (O. v. rothschildi), which happens
off the Pacific Shore of Panama, is smaller sized.
After that as predator populaces raise and
also record more target, the victim population will ultimately
reduce, specifically in inadequate source years,
followed by a reduction in the killer population.
The removal of killers from much of the country’s landscape has enabled types such as white-tailed deer to drastically
increase in populace wealth and also become pest species.
The endangered Key deer is the smallest subspecies of the North American white-tailed deer.
They are the just huge herbivore in the Florida Keys and can be found in every
habitat, where they feed upon loads of indigenous plant varieties.
They travel through every one of the Florida Keys
habitats, as well as can walk, wade or swim from island to island.
In spite of the lack of killers, Key deer retain the particular
behavior of increasing their tails when distressed, revealing the white fur below.
The typical annual residence array size for adult women has to do
with 250 ha (1.0 mi2), and also 650 ha (2.5 mi2) for yearling as well as adult males.
Does’ biggest monthly residence range dimension in north Florida takes place in October throughout the optimal
of the rut. Bucks in the exact same location start to conform bigger locations in July and also keep their broadened house varieties via October.
Deer with fairly large home range dimensions commonly occur in environments
of poorer top quality.
In the southeast, with moderate winters months and long growing season, the timing of
fawning is not as essential and deer breeding
activity is a lot more variable. Trick deer when varied throughout the lower Florida Keys, but now lives largely in one location, called
Big Pine Trick, as well as bordering little islands.
The Trick deer is provided as jeopardized by the Endangered Variety Act.
Presently less than 1,000 Secret deer survive, as well
as their future remains perilous. Threats to Secret deer consist of habitat loss
from advancement of coastal habitats and floodplains, auto
accidents, condition, unlawful feeding by human beings, and also climate
change, which is impacting mangroves.
Records of large indigenous Florida white-tailed deer populaces go back to the late
1600s. Due to unregulated hide trade in the 1700s and rural/urban advancement in the 1800s as well as very early 1900s, Florida’s native white-tailed deer populace dropped, reaching
its least expensive numbers in the 1930s. Within its initial
decade, the compensation bought 2.5 million acres in an effort to recover white-tailed
deer environment. By the 1960s, the commission’s initiatives were noticeable as deer numbers boosted significantly, with over 40,000 pets collected each year.
After concerning 5 months as well as prior to
the mating season, the blood supply terminates as well as the velvet dries out and also is
lost as the deer scrubs the horns against trees and hedges.
This duration is when the antlers come to be hard, sharp tools.
Within Artiodactyla, 37 varieties belong to the family Cervidae, known as true deer, which
share such characteristics as only males having horns.
The horns of real deer are deciduous, implying shed every
year; the exact same dental arrangement; decreased second as well as fifth toes; and also a four-chambered,
pondering stomach. Establish a habitat monitoring plan to preserve stable populace levels
of deer on your land.
The screw worm is a fly larva that gets in an open injury of a real-time animal as well as eats the flesh of the pet from within, leading to a gruesome
death. The women fly friends once in her life, so the problem can be battled by presenting sterilized male flies to the populace, causing the
ladies to die out without laying productive eggs. Other steps to fight the break out included injecting deer
with antiparasitic medications, fencing off healthy and balanced sections of the populace, as well as tracking
a part of deer with radio collars. The pest was stated as eradicated in April 2017.
The outbreak eliminated 135 deer, roughly an eighth of the herd.
American kestrels as well as belted kingfishers are a few of our most singing next-door
neighbors. Turkey vultures arrive by the hundreds and also can be seen skyrocketing expenses with hawks, falcons and also eagles.
Late southbound migrants like Swainson’s hawks are still going through.
It is additionally peak wading bird nesting (reddish egrets,
excellent white herons, Wurdemann’s heron, black-necked stilt).
Cuban yellow warblers and grassy field warblers are likewise searching
for friends, building nests and also elevating young along mangrove
shorelines as well as islands.
important site
africanownews.com
I really like what you guys are up too. This sort of clever work and exposure!
Keep up the wonderful works guys I’ve incorporated
you guys to my personal blogroll.
Here is my blog post; Jenna
What special thing can I do for my boyfriend Cenforce 100mg us?
%%
Also visit my web site http://www.purpledodo.net/wp/pappys-hot-rod-lincoln/
Это издевка такая, да?
This way of enjoying will likely be helpful both for rookies and for https://hci.gov.in/kampala/?0001?000?pinups-casinos.ru extra skilled gamers.
%%
Here is my web site :: https://yellowpagoda.com/top-three-places-to-visit-to-play-with-snow-this-winter-in-nepal/
%%
my homepage https://hotrod-tour-frankfurt.com/explosions-of-color-skateboarding-in-slow-motion
Good way of explaining, and nice post to obtain data on the topic of my presentation topic, which i am going to convey in university.
Привет! Я недавно зарегистрировался в Cat Casino, и мне нравится его официальный сайт. Кэт Казино предлагает широкий выбор игр и уникальный игровой опыт. Cat Casino регистрация была быстрой и простой – всего несколько шагов, и я уже мог наслаждаться азартом. Кроме того, я использовал зеркало Cat Casino для доступа к сайту без проблем. Вход Cat Casino теперь для меня удобен и легок. Рекомендую всем азартным любителям попробовать свою удачу в Cat Casino!
Тут вы всегда можете безопасно и удобно скачать Майнкрафт.
купить паллетные стеллажи
There are times when a child 214rentals.com just cheats and this is not always a bad thing.
jilbab xnxx
click over here
Ты знаешь мое мнение
Plus, https://demo1.sp12.ru/doc/articles/chto-takoe-sovmestnye-pokupki-korotko-dlya-nachinayuschih.html there’s a further bonus spherical granting as much as 250x your winnings. What do these games have in widespread?
Este post é realmente uma perfeita ajuda para os pesquisadores que
estão em busca de bons conteúdos. Parabéns.
my web page; Web Site
Discover the thrill of order snus online and explore a world of enticing flavors!
tamoxifen sale benefits of tamoxifen most common side effects of tamoxifen
breakingnews77.com
Nauti parhaasta nikotiinipussit vahvuus -kokemuksesta valikoimassamme olevien laadukkaiden makujen parissa!
Discover the art of how to use velo snus and explore a world of exciting flavors with our exclusive collection!
%%
My webpage – вавада скачать
Я думаю, что Вы не правы. Могу это доказать. Пишите мне в PM, обсудим.
чтобы данного необходимо черкнуть декларирование также отвоевать полученные средство http://bablo.credit обращения. в течение пора шагу пролонгации приостанавливается начисление процентов равно пени.
Ваша фраза просто отличная
The Youngsters’s Week achievements and the meta For The Children are a part of the 12 months-lengthy What An extended, Unusual Journey It has been, https://beredukasi.com/industry-solutions-tutorial/ so you’ll want to get these completed if you’re working towards a Violet Proto-Drake.
Discover the art of how to use velo nicotine pouches and explore a world of exciting flavors with our exclusive collection!
Seller rating 365newss.net and the impact of comments on him.
Explore the diverse world of velo nicotine flavors for an exquisite and unique vaping experience!
купить дипломы о среднем https://diplom-o-srednem.ru/
диплом старого образца ссср https://diplom-sssr.ru/
No matter if some one searches for his essential thing, so he/she desires to be available that in detail, thus that thing is
maintained over here.
Look at my webpage … kalendarz 2024
Embark on a journey of taste with the exquisite velo flavors for an unparalleled vaping experience!
Touche. Great arguments. Keep up the great work.
Здесь вы всегда можете безопасно и быстро скачать Майнкрафт.
What to text him to get him back buy Cenforce 50mg generic?
The service itself refers to a network protocol, which arizonawood.net in turn is the property of an organization that manages domain names, IP addresses for all sites and resources on the Internet.
Wow, this paragraph is pleasant, my younger sister is analyzing these kinds of things,
therefore I am going to inform her.
Whether you desire to purchase automobile financial online,
you need to limit all the feasible offers as well
as prices that suit your budget plan. As commonly along with the case of lots of,
they often tend to overlook the importance of contrasting financial quotes that they tend to devote thrice as long as they might possess actually saved, read more.
aricept tablet how to buy aricept 5mg aricept pharmacy
Discover a world of delightful velo pouches flavors that will tantalize your taste buds and leave you craving for more!
women18.com
%%
my site :: https://newmoonmarcom.com/
Discover the most amazing best velo flavor options for a delightful experience you won’t forget!
It’s in reality a great and useful piece of information. I am satisfied that you just shared this helpful info with us.
Please stay us up to date like this. Thanks for sharing.
Explore the exciting world of Nicotine pouch shop near me and discover unique flavors that will elevate your experience!
%%
Check out my web page – https://blacksprutonion.shop/
Very good blog! Do you have any recommendations for aspiring
writers? I’m hoping to start my own site soon but I’m a little lost on everything.
Would you recommend starting with a free platform like WordPress or go for
a paid option? There are so many options out there that I’m completely overwhelmed ..
Any suggestions? Thanks!
диплом магистра 2023 https://diplom-magistratura.ru/
Explore the world of Nicotine pouch shop online and discover exciting flavors for your preferences!
Извините за то, что вмешиваюсь… Я разбираюсь в этом вопросе. Готов помочь.
Ректор Казанского государственного энергетического университета, https://kutuan.cc/ депутат-аграрник Государственного Совета РТ Эдуард Абдуллазянов вручил портфели мало канцелярскими принадлежностями 7 перспективой первоклассникам Шеланговской школы.
Discover the thrill of trying out different flavors with our outstanding selection of Top selling fresh nicotine pouches – a journey you don’t want to miss!
%%
My site https://www.vingle.net/posts/5510739
Discover an exciting array of options at the nicotine pouches store for an unparalleled experience with nicotine pouches!
%%
My site частные детективные агентства челябинск
%%
Here is my homepage :: https://deviva.ru/viewtopic.php?id=4895
Para yatırma işlemleri hızlı ve güvenlidir ve Mostbet
çeşitli ödeme şekillerini kabul eder.
Hi there to every one, as I am really eager of reading this weblog’s post to be updated on a regular basis.
It consists of pleasant material.
my website Alternatif situs resmi Bebas 888
mestinon 60mg tablet mestinon 60mg cost where can i buy mestinon 60 mg
Здесь вы легально и безопасно cможете скачать Майнкрафт.
Какой хороший вопрос
Conversely, if you are free of this fabricated sexual stereotype, https://wettropicsplumbing.com.au/hot-water-system-replacement/ then it shall enchantment to companions which are also freed from the false perception.
Анука!
Прием документов от абитуриентов Казанского национального энергетического университета, рассчитывающих получи и распишись внебюджетные наделы, довыполняется двадцатый астероид для того очный, очно-заочной, https://blacksprutonion.shop/ заочной фигура преподавания.
%%
my web page – https://www.logcontact.com/blogs/14558/M%C3%A9todos-Alternativos-de-Tratamiento-Explorando-Opciones-para-Tu-Salud
219news.com
These are genuinely fantastic ideas in on the topic of blogging.
You have touched some nice factors here. Any
way keep up wrinting.
купить аттестаты за 9 класс 2017 https://attestat9.ru/
Рul çıxаrılmаsı tələbi Mоstbеt əməkdаşlаrı tərəfindən 30
günə ərzində nəzərdən kеçirilir.
Also visit my web page … mostbet giriş
диплом бакалавра https://diplom-bakalavra.ru/
getusainvest.com
over here
Какая фраза… супер, великолепная идея
This is the reason why some herbal substances within the herbal remedy for swapandosh in males have the ability to take https://shinpen.jp/?p=2477 care of weight.
dark web site darknet sites
https://mignews.com/news/sport/izrail-uluchshil-shansy-dobyt-pryamuyu-putevku-na-evro-2024.html
If the solution is completed, homeideascoach.com you can use the GDZ and see if it is correct. Difficult topic? You need to look into the solution book and see the algorithm of actions.
купить аттестат 10 11 https://attestat11.ru/
%%
Also visit my web blog; https://biz.rusff.me/viewtopic.php?id=11085
oknews360.com
Здесь вы найдете лучшие вывод из запоя.
Я думаю, что Вы допускаете ошибку. Могу это доказать. Пишите мне в PM.
In just 5 very easy actions, https://www.techinexpert.com/voip-services-where-is-the-market-moving/ you can have a seamless communication system for your business. As soon as you have a clear suggestion of what you require, it’s time to start researching different suppliers.
why not try here
procardia 30mg nz procardia 30 mg prices procardia tablet
bestchicago.net
%%
my web page … https://vchaspik.ua/pravozashchitnik/potrebitel/13/450181arenda-avtomobilya-v-odesse-luchshee-reshenie-dlya-aktivnyh-lyudey
https://trenerhimki.ru/
dallasrentapart.com
Здесь вы найдете лучшие вывод из запоя.
Hey! I realize this is sort of off-topic but I needed to ask.
Does managing a well-established blog such as yours require a massive amount work?
I’m completely new to blogging but I do write in my journal on a daily basis.
I’d like to start a blog so I will be able to share my own experience and views online.
Please let me know if you have any kind of recommendations or tips for new aspiring blog owners.
Thankyou!
dublindecor.net
временной регистрации москва https://registraciya-v-msk.ru/
Explore the diverse world of velo snus and savor the richness of our exclusive range of flavors!
view website
https://steamdesktopauthenticator.me/
alahomemaster.com
%%
my web-site: https://blacksprut-market.pro/
%%
Check out my web-site: http://bezprovodoff.com/news/onlayn-kazino-z-top10—cryptoboss-ukrana.html
It is enough to go to a greenhouseislands.com special page and enter the domain name that you want to check in the field.
В этом что-то есть. Большое спасибо за информацию. Вы оказались правы.
The customers get to choose time-delays for each single output handle which isn’t very common even with one of the best Bitcoin btc mixer mixers.
%%
Here is my web site – https://redzonesportsbarandgrill.com
временная регистрация https://registraciya-v-spb.ru/
У нас вы можете заказать вызов нарколог на дом.
loperamide united states loperamide 2 mg generic loperamide medication
Why users still make use of to read news papers when
in this technological globe everything is presented on web?
Доступные качественные силовые тренажеры разработаны для точного симулирования различных видов физической активности.
Очень хорошая мысль
1. If a service has been down for a while, hidden wiki tor tag it with ‘ – DOWN YYYY-MM-DD’ (your guess as to when it went down).
Such toys are presented in the south-columbia.com online store.
alabama-news.com
Discover the fascinating world of nicotine pouches eu and elevate your experience with our wide range of exquisite flavors!
спс… стараюсь
When you really want that license, https://cracked.io/Thread-Who-asked-about-adult-movies then give your highest. Though success may be troublesome to realize however with perseverance and courage, you can absolutely attain and attain it.
garcinia cambogia 100caps otc garcinia cambogia 100caps medication where can i buy garcinia cambogia 100caps
If we are talking about companies dominicandesign.net, the rating will be calculated after the third comment from users.
%%
My blog – http://www.mapquest.com/places/-429393950/
временная регистрация рф https://registraciya-msk.ru/
%%
Take a look at my homepage: https://www.sq.com.ua/rus/press_release/10.08.2023/ot-koncepcii-k-realnosti-kak-sozdat-internet-magazin
caribbean21.com
procardia online how to purchase procardia procardia 30mg pills
https://gllthub.com/Jessecar96/SteamDesktopAuthenticator/
What is the role of gene therapy in the treatment of erectile dysfunction buy vidalista?
%%
Also visit my web page :: https://naijamp3s.com/track/4765/vector-women-and-sex
Can you tell us more about this? I’d love to find out more details.
%%
Also visit my webpage: https://fleurdelys.biz/apple-icon/pgs/kupit_spravku_vuzov_na_sessiu_1.html
Write more, thats all I have to say. Literally, it seems as
though you relied on the video to make your point. You obviously know what youre talking about, why throw away
your intelligence on just posting videos to your weblog when you could be giving us something enlightening
to read?
У нас очень качественное лечение алкоголизма.
What foods decrease horniness vidalista?
The word itself is a compound of the northfloridahouse.com English phrase “who is”, translated as “who is”.
event-miami24.com
%%
my web site; https://data1861.ru/press/agrarii-rasskazali-kak-zhara-i-zasukha-povliyali-na-urozhaj-zernovykh
Environmentally friendly dyes are used for coloring the toys oneworldmiami.com, which do not contain chemicals, therefore, the toys do not cause allergic reactions even in those people who are prone to permanent rashes.
try this web-site
https://kursy-online1.ru/
Порнуха
бриллкс
https://brillx-kazino.com
Так что не упустите свой шанс — зайдите на официальный сайт Brillx Казино прямо сейчас, и погрузитесь в захватывающий мир азартных игр вместе с нами! Бриллкс казино ждет вас с открытыми объятиями, чтобы подарить незабываемые эмоции и шанс на невероятные выигрыши. Сделайте свою игру еще ярче и удачливее — играйте на Brillx Казино!Brillx Казино – это не только великолепный ассортимент игр, но и высокий уровень сервиса. Наша команда профессионалов заботится о каждом игроке, обеспечивая полную поддержку и честную игру. На нашем сайте брилкс казино вы найдете не только классические слоты, но и уникальные вариации игр, созданные специально для вас.
gocanadanews.com
в отношении их равным образом сходит полуслова казино daddy басовитее. пред исходные положения игрового хода игроки имеют все шансы педантично пристроить объем конечного возмездия в каждом матче, а еще отмеченный предел поре.
%%
Stop by my webpage … https://papiersdarmenies.com/
go to this website
клининговая компания люберцы уборка квартир https://uborka-v-lubercah.ru/
Поздравляю, блестящая идея и своевременно
Influencer outreach, relationship building, anntaylorwriter.com and collaborating with different creators will pay you off – typically even more than creating content.
payusainvest.com
услуги уборки после ремонта https://uborka-posle-remonta-kvartiri.ru/
investnews24.net
Microsoft Authenticator: Not unhealthy, however why so big? Microsoft Authenticator vastly simplifies login to Microsoft accounts, sda steam nevertheless it is tough to excuse its huge dimension – and that iOS and Android cloud backups are incompatible.
%%
Here is my web page :: https://mymoscow.forum24.ru/?1-5-0-00000711-000-0-0-1692617966
Access to these services is available on the official repairdesign24.com that provide services for placing portals on the internet.
Way cool! Some very valid points! I appreciate you writing this article
plus the rest of the website is also very good.
Прогоны Xrumer и GSA без интернета xrumer купить крякнутый торрент
%%
Check out my web blog https://mega4darknet.com
isosorbide online pharmacy cheapest isosorbide 20mg isosorbide pills
news24time.net
Разрешение на строительство — это государственный акт, предоставленный правомочными учреждениями государственной власти или территориального управления, который дает возможность начать строительную деятельность или производство строительных операций.
Разрешение на строительство в москве задает правовые положения и стандарты к строительным операциям, включая предусмотренные виды работ, дозволенные материалы и методы, а также включает строительные стандарты и пакеты охраны. Получение разрешения на строительные работы является необходимым документов для строительной сферы.
Daha az məbləğ qoysanız, təklif aktiv deyil.
my webpage; mostbet casino (Adlive.com)
%%
Also visit my blog … https://www.utilitarian.net/flat-roof-repair-rules/
Observe this link and click on “Get Backup Codes,” then print out that web page and reserve it in a protected place.
%%
Feel free to surf to my homepage; Рейтинг надежных казино
chinaone.net
уборка квартир в балашихе цены https://uborka-v-balashihe.ru/
antivert 25 mg generic cheap antivert antivert 25mg no prescription
This is the best steam desktop authenticator.
apartusa365.com
Awesome material, Thank you!
One of the best gamers on this combat simulator will need to grasp Metros unique, steam authenticator pc hand-made weaponry and deep combat mechanics in order to achieve the highest of the worldwide leaderboards.
glimepiride for sale glimepiride prices buy glimepiride
а вот это классно!
Much of the location is now inaccessible since it has been taken up by the https://thegioibutquay.com/index.php?language=vi&nv=users&nvvithemever=t&nv_redirect=aHR0cHM6Ly9iZ3Nub29rZXIuY29tLw state prison.
This is a topic that’s close to my heart… Many thanks!
Where are your contact details though?
Откуда мне знать?
Three drops bitcoin mixer Tamari. Add 1 dash of lavender bitters. Use a hand mixer to dissolve yuzu preserves totally.
californianetdaily.com
Keep on writing, great job!
invest-company.net
Я думаю, что Вы допускаете ошибку. Давайте обсудим. Пишите мне в PM, пообщаемся.
Проще адью вернуться в строй буква гладкой стене и притиснуть буква ней грудь в грудь пятки, икры, попа, лопатки, https://www.allmfmg.com/2018/08/05/tyron-see-you/ локти да закосье.
aldactone 100mg united kingdom aldactone 25 mg cheap aldactone tablets
This is the best sda steam.
madeintexas.net
Qeydiyyatdan keçdikdən sonra istifadəçi adı və müvəqqəti şifrə qeydiyyat üsulundan asılı olaraq telefon və
ya mail ilə göndərilir.
Review my blog :: Mostbet Giriş
This is the best steam authenticator.
Every weekend i used to go to see this web page,
as i wish for enjoyment, since this this web page conations actually good funny data too.
%%
My site … https://sibledy.ru/thread-313862-1-1.html
%%
Also visit my blog post … http://www.unitedsteel.com.sg/project/light-bright-airy/
%%
Feel free to visit my homepage … https://pixmafia.com/mix/pryamye-virtualnye-nomera-telefonov-nedorogo.html
%%
Feel free to surf to my site: дедди казино
Hey There. I found your weblog the use of msn. This is a very smartly written article.
I’ll make sure to bookmark it and return to read more of your useful info.
Thank you for the post. I will definitely return.
Here is my website; days since october 28
%%
Have a look at my web-site https://super-wiki.win/index.php?title=Order_a_stripper
боди массаж https://eroticheskij-massaj.ru/
With thanks! Excellent information.
Я думаю, что Вы не правы. Предлагаю это обсудить. Пишите мне в PM.
There are people out there that particularly targets newbies and unsuspecting customers. You see gurus claiming to make xx% per month or https://www.211cn.ca/fraud-calls-from-chinese-consulates-across-canada-recording/% per month and your adrenaline rush with joy thinking that you’ve got finally discovered the one that may educate you their trading secret.
%%
My webpage :: post116185
https://1xdomen.ru/
Такие торговые аппарате усваивают материи равно швейную фурнитуру на наибольших размерах равно перепродают владетелям всемирная паутина-маркетом маленьким чохом по более высокой http://magazin-tkani.su цене.
Мне кажется это отличная идея
разобраться в чем при выборе бойлера соблюдает получай метраж квартирантов семьи да интенсивность внедрения тёплой http://garage-gt4.com/classic-days-schloss-dyck-2014__mit-dem-gt4-beim-sonderlauf-italia-damore/ воды.
Подкладочная штоф употребляется близ пошиве многих типов одежды. Подкладка протягивать руку помощи владеть фигуру одежде, бережет погода, http://tkani-kupit.su втягивает воду да т.д.
Из сих тканей шьются чистые полотенца, скатерти, салфетки, фуршетные юбки, tkani-optom.su столовые дорожки. Интернет-гастроном «Ткани чохом 365» зовет офигенный комплект текстиля российского и еще заморского изготовления.
порно онлайн
Мы систематично приобретаем ранее не известные дизайны равным tkani-optom-moskva.su образом качества. Если Вам спокойнее наварить посылку междугородними автобусами, прямо укажите телефон с гербом водителя (а) также часть лодка, тот или иной стоит около склонности наших трейдерских мест.
%%
my webpage – http://fabnews.ru/forum/showthread.php?t=9517
дезинфекция квартиры после смерти человека
%%
Feel free to surf to my web blog: https://dostoyanie.pro/
amaryl 2 mg coupon amaryl 4mg purchase order amaryl 2mg
article source
печать этикеток москва https://samokleyashchiesya-etiketki.ru/
%%
my site: https://pastelink.net/3ip8gs72
%%
Here is my blog … http://kharkovbynight.forum24.ru/?1-15-0-00001891-000-0-0
Мега даркнет сайт – мое фундамент место действия назначения ради в целом, http://dasfamilienhaus.at/Veranstaltung/babymassagekurs-block-b1/ что связано раз-другой техникой.
%%
Also visit my page: https://kran-manipulator.zp.ua/pro-nas/
%%
my web-site … 81445
where can i buy pioglitazone pioglitazone 30mg tablet pioglitazone prices
%%
Also visit my web-site – https://assa0.myqip.ru/?1-1-0-00001295-000-0-0-1690630331
обнаженные фото: https://vksex.ru/
Браво, мне кажется это отличная мысль
Hussein R., Almohammadi A.A., Alweldi W.M., Alshik A.M., Malik S., Mashat A. Traits and issues of https://www.triseca.cl/tienda/solar-car/ in Saudi Arabia.
Один із самих крутіших челендж.
First of all I would like to say fantastic blog! I had a quick question which I’d like to ask if you don’t mind.
I was curious to know how you center yourself and clear your head
prior to writing. I have had trouble clearing my mind
in getting my ideas out. I truly do take pleasure in writing however it just seems like the
first 10 to 15 minutes are lost just trying to figure
out how to begin. Any recommendations or tips? Many thanks!
flonase nasal spray without a prescription flonase nasal spray 50mcg online pharmacy cheap flonase nasal spray 50mcg
%%
Also visit my blog post – https://www.prnewswire.com/news-releases/new-york-website-design-company-lounge-lizard-discusses-common-local-seo-mistakes-everyone-makes-300723669.html
Статейное и ссылочное продвижение.
В наши дни, фактически каждый человек пользуется интернетом.
С его помощью возможно найти любую данные из разных интернет-источников
и поисковых систем.
Для кого-то собственный сайт — это хобби.
Однако, большинство применяют разработанные проекты для заработка и привлечение
прибыли.
У вас есть личный сайт и вы желаете привлечь на него максимум визитёров, но не знаете с чего начать?
Обратитесь к нам! Мы поможем!
обратная ссылка вид
%%
Also visit my site – https://pokerplayspain.com/
срочно займ онлайн
https://nakrytka.com
R — указывает на тип конструкции шины, по расположению внутреннего корда шины разделяют на шины с радиальным расположением корда (R) и шины с диагональным расположением корда (D), большинство современных шин легковых автомобилей имеют радиальное расположение корда, шины с диагональным кордом выпускаются для сельскохозяйственной и строительной техники
%%
My web page :: https://azsx.unoforum.pro/?1-3-0-00002228-000-0-0-1688708288
%%
Here is my web blog; https://mangamammy.ru/
prednisone for respiratory infections
Браво, это просто отличная фраза 🙂
This makes it easier for you to buy the required materials. One thing that you could obtain from it is best http://ifacformation.fr/on-le-craint-mais-pourtant-il-a-son-utilite/ results.
». Такой подзаголовок оказаться вынужденным обнимать краснобайство, вытягивающие людей из сумрачных повседневности (а) также влекущие во интенсивный безмятежность. 1. на заголовке указывайте result, budynok.com.ua какового подать руку помощи выбить.
isosorbide tablet isosorbide online pharmacy isosorbide pharmacy
%%
my webpage: Cryptocurrency Exchange
%%
My web-site: https://daddyscasino.win
buying tadacip without a prescription
Can erectile dysfunction be a symptom of adrenal fatigue buy sildenafil 50mg pill?
Micardis
Один із самих крутіших челендж.
%%
Also visit my blog post … http://forumliebe.de/index.php?threads/hello-all.17072/
педагогика и саморазвитие -> ЛОГИКА -> Значение логики
https://www.tiresizehelp.com
подробнее
What are the effects of chronic use of inhalants on erectile function in young men order sildenafil pill?
You’ve made the point.
lisinopril 40 mg daily
Tetracycline cost
is lisinopril an ace inhibitor
%%
My homepage – https://playpokerportugal.com/
albuterol classification
where can i get lisinopril tablets
Комментировать « Пред. саундтрек – К https://moceva.com/tin-tuc/vai-tho-kate-la-gi-tai-sao-do-ngu-lam-tu-vai-tho-kate-lai-duoc-ua-chuong-den-vay/7089/ дневнику – След. в качестве кого чекушка катастрофа на заводе в котором нибудь Урюпинске выводится держи основные полосы печатные изданий обвиняя Путина.
Floxin
finasteride pharmacy
lisinopril 20 mg tablets
can i order generic lisinopril without dr prescription
Hello mates, its fantastic post about cultureand completely explained,
keep it up all the time.
утепление окон доме http://www.mosoknoteplo.ru/
prednisolone pronunciation
Endep
педагогика и саморазвитие -> ПСИХОЛОГИЯ УПРАВЛЕНИЯ -> Работа по построению предмета психологии принадлежал Аристотелю
finasteride topical
lisinopril 10 mg brand name in india
doxycycline for dogs
%%
Look at my web site :: https://www.evakuator.zp.ua/evakuator-pokrovsk-2/
%%
Feel free to visit my blog – читать здесь
can i order aurogra pills
Purchase doxycycline online
when should you take lisinopril
lisinopril without doctor’s prescription
get cheap lisinopril for sale
how can i get generic levaquin no prescription
%%
Here is my blog post https://trendyremonta.ru/doma-kvartiry/chto-takoe-obosnovanie-promyshlennoj-bezopasnosti-opo-i-kak-ego-poluchit.html
Doxycycline 50 mg cost
Психология
lisinopril 10 mg tablet
http://oren.kabb.ru/viewtopic.php?f=50&t=24710
%%
my site: p4105
перевозка умерших сербия
https://official-trix-mirror.online/
%%
My page … https://onlinepokerportugal.com/
I think that everything posted was very logical. However, consider this, suppose you typed
a catchier post title? I am not saying your content is not solid., but suppose you added a headline that grabbed
folk’s attention? I mean WOLF OR WORM? A CASE OF LUPUS VULGARIS MASQUERADING AS TINEA CORPORIS – Indian Journal Of Clinical Dermatology is
kinda boring. You might look at Yahoo’s front page and
watch how they create article titles to get viewers to open the links.
You might try adding a video or a pic or two to get readers
excited about what you’ve written. In my opinion, it
would make your posts a little livelier.
my web-site: สล็อต191
I cherished as much as you’ll receive performed proper here.
The caricature is tasteful, your authored material stylish.
nonetheless, you command get got an nervousness over that you wish be handing over the following.
unwell undoubtedly come further in the past again since precisely the same just about very frequently inside of case you shield this hike.
Feel free to surf to my web site 2006 chrysler pt cruiser
%%
My web site: http://ractis.ru/forums/index.php?autocom=gallery&req=si&img=1527
%%
my site – https://o-dachnik.ru/osnovy-bureniya.html
%%
my site https://elit-santech.ru/sila-ppt-v-stroitelstve-pochemu-primenenie-proektno-planirovochnoj-tehniki-yavlyaetsya-neotemlemoj-chastyu-uspeshnogo-proczessa-stroitelstva.html
view publisher site
https://blogovk.com/
%%
My homepage; https://delawarestatefiremarshal.com/
Rattling excellent information can be found on site.
Also visit my webpage – junk car towing
brillx официальный сайт
brillx casino
Добро пожаловать в мир азарта и возможностей на официальном сайте Brillx Казино! Здесь, в 2023 году, ваш шанс на удачу преумножается с каждым вращением барабанов игровых аппаратов. Brillx — это не просто казино, это уникальное путешествие в мир азартных развлечений.В 2023 году Brillx предлагает совершенно новые уровни азарта. Мы гордимся тем, что привносим инновации в каждый аспект игрового процесса. Наши разработчики работают над уникальными и захватывающими играми, которые вы не найдете больше нигде. От момента входа на сайт до момента, когда вы выигрываете крупную сумму на наших аппаратах, вы будете окружены неповторимой атмосферой удовольствия и удачи.
https://smofast.ru/
the most popular cocktail in every state, according to googl mightiest i love bacon, beer, birds, and baboons
%%
Feel free to surf to my site: cat casino рабочее зеркало
helpful site
Perfectly spoken indeed. .
%%
Feel free to surf to my web page; Индивидуалки Иркутска
вывод из запоя капельница https://zapoy-msk.ru/
%%
Here is my web-site; http://woodsale.ru/articles/709
%%
Here is my web blog; Работа для девушек Иваново
These are truly fantastic ideas in concerning blogging.
You have touched some pleasant points here. Any way keep up wrinting.
лечение алкоголизма в стационаре https://lechenie-alkozavisimih.ru/
https://websmm.biz/
Terrific knowledge, Many thanks.
I’m gone to convey my little brother, that he should also go to see this
weblog on regular basis to obtain updated from most up-to-date reports.
Here is my webpage บาคาร่า
Thank you, I appreciate this!
%%
Here is my page :: https://thejjreport.com/world-news/5-things-that-dominate-the-2022s-for-pharma-companies/
cipro without prescription order cipro 500 mg cipro without a doctor prescription
%%
Here is my web page … читать здесь
%%
my web blog :: booi casino официальный сайт
%%
Feel free to surf to my homepage: содержанки Севастополь
%%
Also visit my homepage; https://russiacasinos.win/fast-payments
%%
Here is my page: https://forum.ee/blog/937/entry-48350-svetodiodnie-ekrani-dlya-razmesheniya-reklami-f/
Hello! I could have sworn I’ve been to this website
before but after going through many of the posts I realized it’s new to me.
Anyhow, I’m definitely happy I discovered it and I’ll be book-marking it and checking back frequently!
%%
Here is my web-site :: Проститутки Нижний Новгород Канавинский район Канавино
%%
My homepage … http://uaforum.ukrbb.net/viewtopic.php?f=12&t=1186
%%
Visit my site http://xn—-7sbgj9bdrl.xn--p1ai/users/ulidelix
Однозначно, отличный ответ
Лицензии казино. Здесь более 15 вариантов. Софт казино. Чем больше поставщиков игр, игровых автоматов, https://top10raytingicasino2023.win/fast-payments тем выше будет рейтинг.
order procardia order procardia 30 mg procardia usa
%%
my page – https://5ka-card.ru/
%%
Look into my page https://telegra.ph/Kasyno-pozna%C5%84-08-28
лучшая клининговая компания https://top-klininga.ru/
If you want to buy automobile financing online, you
need to narrow down all the achievable bargains and
rates that match your budget plan. As usually along with the case of many, they have a tendency to forget the importance of contrasting
finance quotes that they usually tend to invest thrice as long
as they could possibly possess actually spared, learn more.
Какая нужная фраза… супер, великолепная идея
Be it a process to increase signal-ups or to create a clear dashboard of https://ensemblescolairenotredamesaintjoseph-berck.fr/2021/06/15/rencontre-des-collegiens-avec-lecrivaine-ingrid-klupsch/ information.
частный нарколог на дом https://narcolog-msk.ru/
procardia usa order procardia procardia 30 mg prices
Whats up very cool site!! Guy .. Beautiful .. Wonderful
.. I will bookmark your website and take the feeds
additionally…I’m glad to find so many helpful information here within the
publish, we’d like develop extra techniques on this regard, thanks for sharing.
Here is my website; birthday party coloring sheets
spongebob birthday party spongebob coloring sheets spongebob coloring – http://Regvoice.com/home.php?mod=space&uid=58371&do=profile
–
%%
Review my site … http://stalkersworld.ru/pokupaem-keramicheskuyu-otdelochnuyu-plitku-s-luchshimi-kachestvennymi-xarakteristikami/
%%
Here is my homepage :: http://dedietrich-service.ru/
A urologist or a sexual health specialist is the ideal healthcare professional to consult for comprehensive evaluation and personalized treatment of ED. priligy for sale
Вам остается лишь выбрать подходящие хозяйственные товары оптом, после чего мы оперативно доставим заказ до двери вашего дома!
В нашем каталоге размещены:
Ознакомьтесь с полным ассортиментом! В отличие от обычных магазинов, мы предлагаем продукты хозяйственные товары оптом , что дает еще большую скидку https://пром-мир.рф/wp-content/uploads/2022/04/m-st-576525664_w640_h640_30408-500×500-1.jpg
Chronic kidney disease and other renal issues can increase the risk of erectile dysfunction. dapoxetine and sildenafil
Регистрация и вход на официальный сайт букмекерской конторы 1WIN – это погружение в мир азарта заслуживающий доверия. Авиатор, ставки на спор и казино, а еще 500$ бонус на первый депозит в бк 1вин.
https://1winstavki.fun/
Все может быть
One of the vital well-known areas where cards are played today is the https://telegra.ph/Kasyno-08-28. All these deck types are engaging and the video games which may be played with these are pleasant.
Very rapidly this web page will be famous among all blogging viewers, due to
it’s nice content
%%
Here is my web site :: 1win официальный сайт войти
%%
Here is my web site … http://acasa.castelleone.net/ercoli-acqua-in-vetro/
%%
my web-site; https://interes.mybb.social/viewtopic.php?id=1729
%%
Here is my site :: vpn server
buy clozaril 50 mg clozaril purchase clozaril 100mg tablets
%%
my website – https://nakshakar.net/index.php/2023/08/13/etiket-1win/
%%
My web site – https://dosug52.com/city/bogorodsk
cs 1.6 скачать со скинами
%%
Feel free to surf to my web blog: https://dosug52.com/city/gorodets
Insp Gethin Jones helped introduce the protocol in north Wales, https://www.commercialtrucksigns.com/2014/11/nullam-eget-elit-ante/ and stated it was a welcome tool within the pressure’s arsenal in relation to tracing susceptible people.
%%
Also visit my website; https://vchaspik.ua/ua/otdohni/tehnika/551963-teplovizor-yak-ne-pomylytysya-z-vyborom
Howdy! This post could not be written any better! Looking
at this article reminds me of my previous roommate!
He always kept preaching about this. I will send this post to him.
Pretty sure he will have a very good read. Thanks for sharing!
%%
Feel free to visit my website: http://www.iamua.net
кодирование алкоголизма недорого https://kodirovanie-alko.ru/
%%
Also visit my web blog :: https://aviator-games-online.ru/
Да это все фантастика
Let’s take an in-depth element examine to try to grasp the performance of the https://www.republicadecaballito.com/noticias-ciudad-autonoma-de-buenos-aires/concurso-caballito-me-inspira-de-cuentos-y-poesias digicam better.
профессиональный клининг в москве https://yborka-dezinfekciya.ru/
Most of the time, the mail will contain a guide your employment benefits, a notice with regard to your eligibility for the employment advantages, a notice of your employment claim as well as extra http://www.daehangreenpower.com/bbs/board.php?bo_table=free&wr_id=212463 that may enable you in on the lookout for a new job.
Fastidious response in return of this difficulty with firm arguments and telling everything about that.
Все ждали ну и мы на хвост упадем
He then went on thus far her one time Neighbours colleague Kym Valentine, before placing up a romance with actress Diana Glenn, https://ergosus.de/thomas-pernet-erfinder-und-ergosus-gruender/ with whom he had a son.
играть в онлайн-казино
порно онлайн
more helpful hints
I have read so many content concerning the blogger lovers except this piece of writing is actually a pleasant
post, keep it up.
It’s the most effective places to go whenever you wish to know extra about pure https://blogs.bgsu.edu/kperss/2010/feminism-in-comp-rxns/ raspberry keytone.
how to make fake money
%%
Here is my web site; https://meduza.md/solarpanel
%%
my homepage – https://kovcheg-kavkaz.ru
Я очень хотел бы с Вами поговорить.
To offer a better chance at successful the day with their campaigns, manufacturers can turn to Finest Cellular App Designers https://cantinasanjuan.com/2020/04/14/2358/.
3d печать деталей https://3d-pechat-studya.ru/
However by Thursday Findling was now not a part of the team, https://alinstanterd.com/la-uasd-dice-problemas-seran-resueltos-y-clases-virtuales-iniciaran/ based on an individual with information of the change who spoke on situation of anonymity as a result of they weren’t authorized to debate the matter publicly.
dragon money casino
additional reading
Friday, 12/10 – Saturday, 12/eleven Complete Body CARE ( includes all physique care, and Aromatherapy, https://www.tsukuba-design.com/2018/07/15/%e3%83%81%e3%83%a3%e3%83%ac%e3%82%b8%e3%83%a7%e3%83%96%e3%83%9d%e3%82%b9%e3%82%bf%e3%83%bc/ Males’s) Sale Days excludes males’s colognes and perfumes.
Сожалею, что не могу сейчас поучаствовать в обсуждении. Не владею нужной информацией. Но эта тема меня очень интересует.
Результат раунда производится 4-мя свободными соучастниками раунда: оператором также 1-ый тремя участниками. Введите личные учетные выкинутые: Введите e-mail да лозунг, https://mundoilusiondisenos.com/what-you-do-today-can-improve-all-your-tomorrows/ что ваша милость использовали во время регистрирования.
https://dzen.ru/id/5d1f684d64271d00adc44e90
This is nicely said. !
Cauvo Capital отзывы
Doxycycline pil
КОНФЕРЕНЦИИ
can you buy generic lisinopril no prescription
doxycycline without an rx
ashwagandha dosage
can you buy generic cleocin without dr prescription
How can i get doxycycline prices
%%
my webpage https://www.mann-ivanov-ferber.ru/wtb/
Yep, http://sports4.iceserver.co.kr/bbs/board.php?bo_table=free&wr_id=71895 and the mother and father may have taken turns sitting with the kid. Individuals on the social media platform immediately came to the girl’s protection and blasted the dad and mom of the boy for leaving him alone.
albuterol hfa inhaler. Healthcare providers should educate patients about potential risks associated with medication duplication.
Я думаю, что Вы не правы. Я уверен. Могу это доказать. Пишите мне в PM, обсудим.
Будь то телефон, планшет, компьютер, ноутбук или телевизор – используйте telegram online везде, http://www.jker.sg/product/cartridge-filter-high-grade-new/ где Вам это необходимо! Это очень удобно и безопасно, так как все сообщения надёжно шифруются и передаются по защищённому каналу.
donepezil australia donepezil 10 mg otc donepezil without a doctor prescription
%%
Here is my site … https://slut.wtf/453188-georgiahart-redhead-girl-of-your-dreams-.html
%%
my homepage https://x-x-x.tube/videos/532235/roxysdream-my-top-tips-for-erection-problems-when-using-condoms-if-you-have-problems-stayin/
%%
my web blog – https://steamcommunity.com/linkfilter/?url=https://didvirtualnumbers.com/en/virtual-number-of-switzerland/
viagra drugs
what can a doctor prescribe with lisinopril
buy tetracycline no prescription
purchase doxycycline online cheap
Attraction | CCTV from the Aston Villa group coach reveals the second a brick was thrown at it as it entered the M65 motorway at J10 on Sunday (Aug 27) following the Burnley https://www.hertsmeretalkingnewspaper.co.uk/uncategorized/hello-world/ match.
where to get cheap sildalist without prescription
скачать кс 1.6 с ботами на русском
Doxycycline monohydrate vs hyclate
их характеристика
%%
Here is my web blog :: https://reports.adguard.com/en/toolzilla.com.ua/report.html
lisinopril cough
Here you can take a quick look Bitcoin Price USD.
finasteride side effects
how much does generic cleocin cost
amoxidil
%%
Here is my web-site :: https://obukhiv.info/news/de-u-kievi-mozhna-znaiti-khoroshu-dityachu-stomatologiiu/
Lopressor
Огурчики ням ням
lisinopril 50 mg price
generic finasteride
https://pari-androidapp.ru/
xyzal vs zyrtec
cleocin buy online
Как так?
For many, http://joomla-461471-1470402.cloudwaysapps.com/blog/item/26-yahoo-it-s-friday it’s the last word medium to get the knowledge not on one however on a number of fields at the identical time.
Diamox
Prednisone indications
%%
My website: https://thepowerofsilence.co/5-ideas-to-decorate-a-wedding-party/
lisinopril retail price
canadian pharmaceuticals lisinopril patient guidelines
%%
my web blog … https://afisha.zp.ua/articles/biznes-tekhnologiji/avtoprokat-v-ukrajini-vidkriyte-dlya-sebe-krajinu-na-kolesakh_232.html
%%
my website; https://blazecrashjogo.com.br/estrategia-blaze-crash/
If you are going for finest contents like me, just go to see this web page everyday since it gives quality
contents, thanks
Dietitians are nutritionists who work straightforwardly with prospects or patients with regard to blaze crash download their healthful needs. As it begins, lots of water can be shed, driving the calorie counter to imagine that vast weight lower is occurring.
vevobahis581.com
Отзывы AME Capitals
It scans the magnetic strip of your bank card whereas it’s being swiped, https://gaamshow.com/charity-2/storm-unitys-24hr-mega-man-x-marathon-charity/8294/ after which a wireless digital camera takes a photograph of the keypad as you enter your pin.
prochlorperazine generic prochlorperazine 5mg no prescription prochlorperazine tablets
%%
My web blog :: https://teamrockie.com/everything-you-need-to-decorate-a-party-ultimate-list-for-a-beginner/
I always used to read piece of writing in news papers but now as
I am a user of web thus from now I am using net for articles, thanks to
web.
%%
my web site: https://www.avito.ru/nalchik/bytovaya_tehnika/uplotnitel_dlya_holodilnika_2478011486
%%
Stop by my site; Такси Севастополь Ялта
old black pussy
Женская красота, ето то без чего мир станет не интересным!Фотки класс!!!!!
Еще один важный момент – это служба поддержки. Предлагает многочисленные слоты, настольные игры, лайв-казино, https://joycasinoofficial-sites.top/zerkalo.html турниры с хорошими призами.
%%
my site p596603
I feel this is one of the so much significant information for
me. And i’m happy studying your article. But want to
commentary on some general things, The site style is wonderful, the articles is
in point of fact excellent : D. Excellent task, cheers
%%
my site; https://www.avito.ru/samara/bytovaya_tehnika/rezinka_uplotnitel_dlya_atlant_hm-5014_8755.6_2457034772
where buy cheap doxycycline price
кс 16 со скинами
скачать кс 1.6 оригинал русская версия с ботами
Dietitians are nutritionists who work straightforwardly with customers or patients in regards to codigo promocional blaze crash their healthful needs. As it begins, lots of water will be shed, driving the calorie counter to imagine that huge weight lower is occurring.
ashwagandha 60caps no prescription ashwagandha 60caps no prescription buy ashwagandha caps
%%
Here is my web site http://nyarando.ru/user/baniuspsrd
go to this website
%%
my web page: https://www.party.biz/forums/topic/36650/camat-poker-situs-poker-online-idn/view/post_id/1557321
%%
Check out my webpage … https://tratatur.ru/price/taxi-novorossijsk-krasnodar
%%
My blog post: https://teplopolis.com.ua/otoplenie-uk
important source
%%
Feel free to surf to my homepage – фреш казино бездепозитный бонус
%%
My site: https://wingirls.wtf/manyvids/26740-margolisa-margo-cum-with-her-stepbrother.html
Incredible loads of valuable data!
Record of registered private individuals or organizations that may be contracted with for price as intermediate handlers to help within the interstate and inter-island transport of https://www.bariwon.com/bbs/board.php?bo_table=free&wr_id=681472 pets.
%%
Take a look at my web blog фреш казино
Wonderful data, With thanks!
brillx официальный сайт играть онлайн
https://brillx-kazino.com
Brillx Казино — это место, где сливаются воедино элегантность и бесконечные возможности. Необычная комбинация азартных игр и роскошной атмосферы позволит вам окунуться в мир бриллиантового веселья. Наше бриллиантовое казино уверенно входит в число лидеров азартной индустрии, и в этом году мы готовы порадовать вас еще большим разнообразием игр и выигрышей.Вас ждет огромный выбор игровых аппаратов, способных удовлетворить даже самых изысканных игроков. Брилкс Казино знает, как удивить вас каждым спином. Насладитесь блеском и сиянием наших игр, ведь каждый слот — это как бриллиант, который только ждет своего обладателя. Неважно, играете ли вы ради веселья или стремитесь поймать удачу за хвост и выиграть крупный куш, Brillx сделает все возможное, чтобы удовлетворить ваши азартные желания.
Very great post. I simply stumbled upon your blog and
wished to mention that I’ve really loved surfing around
your weblog posts. After all I will be subscribing to your feed and I’m hoping you write
again very soon!
%%
Review my site … simone femjoy
https://pari-prilojenie.ru/
Here you can take a quick watch Bitcoin Price USD.
скачати кс 1.6 сборки
Я думаю, что Вы допускаете ошибку. Могу это доказать. Пишите мне в PM.
На нынешнем умозаключении Смит создал http://mblg.tv/aya38/entry/117/ древнюю экономику. При коммунизме пролетариат станут владеть лекарственное средство создания, также им безвыгодный необходимо приложить находящийся в личном владении мита на извлечения прибытка.
Thank you for every other wonderful article. Where else may just anybody get that kind of information in such a perfect manner of writing?
I’ve a presentation next week, and I’m on the look for
such info.
%%
my web site – https://vip-pussy.com/tag/giselle-montes/feed
539
《539彩券:台灣的小確幸》
哎呀,說到台灣的彩券遊戲,你怎麼可能不知道539彩券呢?每次”539開獎”,都有那麼多人緊張地盯著螢幕,心想:「這次會不會輪到我?」。
### 539彩券,那是什麼來頭?
嘿,539彩券可不是昨天才有的新鮮事,它在台灣已經陪伴了我們好多年了。簡單的玩法,小小的投注,卻有著不小的期待,難怪它這麼受歡迎。
### 539開獎,是場視覺盛宴!
每次”539開獎”,都像是一場小型的節目。專業的主持人、明亮的燈光,還有那台專業的抽獎機器,每次都帶給我們不小的刺激。
### 跟我一起玩539?
想玩539?超簡單!走到街上,找個彩券行,選五個你喜歡的號碼,買下來就對了。當然,現在科技這麼發達,坐在家裡也能買,多方便!
### 539開獎,那刺激的感覺!
每次”539開獎”,真的是讓人既期待又緊張。想像一下,如果這次中了,是不是可以去吃那家一直想去但又覺得太貴的餐廳?
### 最後說兩句
539彩券,真的是個小確幸。但嘿,玩彩券也要有度,別太沉迷哦!希望每次”539開獎”,都能帶給你一點點的驚喜和快樂。
%%
Also visit my webpage; https://moydom-yug.ru/
To play this video it’s good to allow JavaScript in your http://kofemarket.com.ua/shop/saeco-royal-cappuccino-silver browser.
%%
Here is my web site; http://www.transurfing-real.ru/2017/12/blog-post_401.html
%%
Also visit my blog; https://dailygram.com/poll/681/is-it-difficult-to-manage-a-smart-panel-at-home/
%%
Feel free to surf to my homepage … comment-316920
%%
my blog – https://uzhgorod.net.ua/news/176773
%%
Also visit my blog post :: http://www.conceptdistributing.com/UTVinCanada/viewtopic.php?f=13&t=121609
%%
my website :: https://x-video.tube/videos/101133/snowyarches-throwback-from-beginning-of-snowy/
Awesome article.
%%
my web blog – смотреть на сайте
%%
my web blog: по ссылке
В 15,16 и 17 лет один раз в году подростки проходят педиатра (подросткового врача), невролога, хирурга, травматолога-ортопеда, офтальмолога, ЛОР-врача, эндокринолога, подросткового психиатра, стоматолога, уролога и гинеколога юноши и девушки соответственно, из обследований – ОАК и глюкоза крови, общий анализ мочи, ЭКГ и по достижению возраста 15 лет 1 раз в год подросткам проводится флюорография легких http://zabotik.com/kostina-tatyana
You stated it really well.
Review my webpage https://topqualitydealz.com/haluatko-hankkia-tuoreimmat-nikotiinipussit-helposti-ja-nopeasti/
%%
Also visit my page: смотреть в источнике
%%
Have a look at my blog post; cat casino официальный сайт вход
%%
Feel free to visit my homepage – https://x-x-x.tube/models/tantricfitness/videos/2/?by=video_viewed_week
Все ИКЕА » Серия Диоскур » Серия Пегас » Серия Сириус » Серия Орион » Серия Мальта » Серия Энкель » Серия Фора » Серия Хэмнес » Серия Варма Мягкая буль » Диваны »» Прямые диваны »» Угловые диваны »» Диваны для офиса »» Механизм Книжка »» Механизм Еврокнижка »» Механизм Аккордеон »» Механизм Дельфин »» Выкатные диваны »» Диваны без боковин »» Интерьерные диваны »» С ортопедическим матрасом »» На деревянном каркасе » Кресла »» Кресло-постели »» Кресло на роздыха »» Кресло нефтекачалка »» Интерьерные кресла »» Кресла для того представительства » Тахты »» Прямые »» Угловые » Пуфы также банкетки Гостиная » Стенки во комнату для гостей »» Недорогие стены »» Современные »» Мини стенки »» Стенки Горки »» С витриной »» Со шкафом »» Белые стенки »» Глянцевые стены »» Модульные стены » Тумбы зли TV »» ЛДСП »» МДФ »» Современные »» Длинные »» Белые »» Глянцевые »» Секции угоду кому) TV »» С ящиками » Шкафы в гостиную »» Шкафы-кузов буква гостиночную »» Распашные шкафчики буква комнату для гостей »» Угловые шкафчики буква комнату для гостей »» Витрины » Стеллажи в гостиную »» Закрытые »» Открытые »» Угловые »» Модульные » Диваны в торговую »» Диван термокроватка »» Угловые диваны » Столы ради торговой »» Обеденные столы »» Журнальные столики »»» Стеклянные »»» Трансформеры »»» На колесиках »»» В языке Лофт »» Столы-книжки » Стулья в комнату для гостей » Комоды на гостиночную » Полки в гостиную »» на слоге лофт Прихожая » Прихожие »» Модульные прихожие »» Малогабаритные »» Узкие прихожие »» Тумбы со вешалкой »» Прихожие в заказ » Шкафы на прихожую »» Шкафы-купе »» Угловые шкафы »» Распашные шкафы » Комоды в прихожую » Тумбы на прихожую »» Обувницы »» Тумбы с зеркалом »» Тумбы раз-другой сиденьем »» Тумбы держи заказ » Вешалки »» Настенные гардероба »» Напольные гардеробных » Зеркала » Пуфы и банкетки Кухня » Кухонные гарнитуры »» Модульные кухни »» Готовые кухни »» С фотопечатью »» ЛДСП »» МДФ »» Глянцевые »» Кухни Стенд »» Кухни БТС »» Кухни ДСВ »» Кухни Горизонт »» Отдельные модули » Отдельные модули »» Нижние тумбы »»» Тумбы мало дверьми »»» Тумбы раз-другой ящиками »»» Тумбы перед мойку »»» Тумбы круговые »» Верхние шкафы »»» Шкафы Глухие »»» Шкафы со стеклом »»» Угловые шкафы »»» Горизонтальные »» Пеналы »» Все модульные кухни » Кухонные диваны »» Кухонные уголки »» Со спальным помещением »» Прямые »» Угловые » Обеденные столы »» Раздвижные кормежки »» Раскладные кормежки »» Овальные кормежки »» Круглые кормежки »» Стеклянные столы »» Деревянные столы »» Складные столы » Стулья »» Стулья на металлокаркасе »» Стулья из массива »» Интерьерные стул »» Барные стулья » Табуреты »» Табуреты металические »» Табуреты бревенчатые » Буфеты » Комплектующие »» Столешницы » Складная парта »» Складные кормежки »» Складные стул равно табуреты »» Складные скамьи » Подстолья пользу кого столов Спальня » Спальные гарнитуры »» Спальни Эконом »» ЛДСП »» МДФ »» Глянцевые »» Белые »» С круговым шкафом »» Со шкафом-купе »» С портальной койкой » Кровати »» Односпальные кровати »» Двуспальные постели »» С портальным устройством »» Мягкие постели »» Кровати из массива »» Шкаф кроватища »» Кровати из ящиками »» Кровати 120 »» Кровати 140 »» Кровати 160 »» Кровати 180 » Матрасы »» Матрасы приспособление Боннель »» Независимые пружины »» Беспружинные матрасы »» Наматрасники » Шкафы в спальню »» Шкафы-кузов »» Распашные шкафчики »» Угловые шкафы » Комоды в спальную комнату » Туалетные столики »» Туалетные столики получи https://www.avito.ru/korenovsk/bytovaya_tehnika/uplotnitel_dlya_holodilnika_2477947098 и распишись заказ!
%%
Also visit my web blog :: https://vip-pussy.com/tag/brunoymaria
%%
Also visit my site; перейти
I truly love your site.. Pleasant colors &
theme. Did you build this web site yourself? Please reply back as I’m trying to create my
very own site and would like to find out where you got this from or just what the theme is named.
Appreciate it!
скачать кс 1.6 через торрента
Costner additionally claims Christine secretly took $105,000 from him to pay her legal professionals, and doubled down on claims she ‘padded’ her little one help payments to fund plastic surgery, http://en.iatom.co.kr/bri/board.php?bo_table=free&wr_id=417320 non-public trainers and “unallocated bank card expenses” for her.
Here you can take a quick check Bitcoin Price USD.
Очень советую https://vc.ru/u/1895184-timur-bektimirov/825135-carskie-monety-investiciya-ili-istoriya/
Быстромонтируемые строения – это актуальные строения, которые различаются высокой быстротой строительства и гибкостью. Они представляют собой постройки, состоящие из эскизно изготовленных деталей или модулей, которые способны быть быстро собраны в пункте строительства.
Строительство быстровозводимых зданий из металлоконструкций под ключ располагают податливостью также адаптируемостью, что разрешает просто преобразовывать и адаптировать их в соответствии с пожеланиями покупателя. Это экономически результативное и экологически надежное решение, которое в крайние лета приобрело маштабное распространение.
my site
If you want to purchase a ticket for a train that’s scheduled to depart inside four hours, https://avtovikupvrn.ru/component/k2/item/4-excepteur-sint-occaecat-cup.html you’ve got got to visit the current Reservations Counter.
%%
Feel free to surf to my page … здесь
This article will assist the internet visitors for setting up new website
or even a blog from start to end.
%%
Also visit my web site :: https://contentfiltering.ru/
how to buy pioglitazone pioglitazone united kingdom pioglitazone tablets
Thanks for finally writing about > WOLF OR WORM? A CASE OF LUPUS VULGARIS MASQUERADING AS TINEA
CORPORIS – Indian Journal Of Clinical Dermatology junk yards in charlotte nc
liquid cialis when will cialis be generic free sample cialis
you could try this out
But wanna remark on few general things, The website design and style is perfect, the subject matter is very fantastic :
D.
Stop by my blog: copart hayward
Признаны террористическими (а) также воспрещены: «Движение Талибан», «Имарат Кавказ», «Исламское государство» (ИГ, ИГИЛ), Джебхад-практически-Нусра, «АУМ Синрике», «Братья-мусульмане», «Аль-Каида в сторонах исламского Магриба», «Сеть», https://sahin-homes.de/index.php/component/k2/item/17 «Колумбайн».
where to buy diamox 250 mg diamox nz diamox 250 mg without prescription
On this site you can take a quick check Bitcoin Price USD.
You expressed this really well!
%%
Feel free to surf to my homepage: booi казино вход
Kudos, Plenty of data.
Look into my page … http://www.bnbchem.com/bbs/board.php?bo_table=free&wr_id=572706
%%
my page: izzi casino
%%
Also visit my web-site: купить диплом
%%
My blog post: https://detkisuper.ru/gde-nayti-nyanyu-dlya-rebyonka/
Your content shouldn’t be simply all enjoyable because it ought to got down to additionally educate and train the reader the answers, way forward, resolve the problem, http://www.apjyoga.org/hello-world/ to progress their curiosity and for it to be worthwhile for them providing you with their consideration.
glimepiride online pharmacy where to buy glimepiride 2 mg glimepiride pharmacy
What’s up, this weekend is fastidious in support
of me, since this time i am reading this fantastic informative post here at my
house.
My blog; ontario subaru
I really like it when individuals get together and share thoughts.
Great website, stick with it!
my webpage – slot maxwin
when to take cialis cialis website how long does 5mg cialis last
%%
Also visit my blog :: https://yomilano.ru/
Dropping your essential data from your difficult generate or any media storage system is quite annoying and getting an excellent https://ggfbinc.com/bonjour-tout-le-monde/ recovery software program program for retrieving your information much more challenging and irritating.
%%
Here is my web page :: 1xslots мобильная версия
%%
Also visit my web-site: pokerdomrupoker.ru
%%
My webpage: смотреть в источнике
%%
Also visit my web blog: https://kosmo2018.ru/
On this good site you can take a quick Bitcoin Price USD.
buy propecia uk : purchase propecia propecia cheap
%%
My web page https://acc-sap.ru/
%%
Also visit my web site; https://whatthechange.ru/
http://www.psyhodic.ru/arc.php?page=5598
бетон подольск
You could certainly see your skills in the work you write.
The sector hopes for more passionate writers like you who
are not afraid to mention how they believe. All the
time follow your heart.
Also visit my web-site – junkcars
https://www.420pron.com/
Can you tell us more about this? I’d like to find out some additional information.
Wow all kinds of great facts!
Feel free to surf to my site; http://scjandrew.net/g5/bbs/board.php?bo_table=free&wr_id=1151162
%%
Feel free to visit my web site: 1xslots
propecia online : buy generic propecia purchase propecia
бетон раменское
Fungal infections. Mostly The Yeast Infection symptoms are present during pregnancy greater than another time in a lady’s http://wiki.gewex.org/index.php?title=User:JolieEden82331 life.
diltiazem cd
%%
Feel free to visit my website; vavada казино зеркало на сегодня
Hello it’s me, I am also visiting this web site on a regular basis, this
site is actually fastidious and the people are in fact sharing
pleasant thoughts.
%%
my blog: https://saintdenis.ru/
%%
Here is my webpage; читать в источнике
%%
my webpage :: webboxvn.com
%%
my homepage: payoneer в украине
%%
Also visit my web blog: казино вулкан старс
%%
My website вулкан вегас казино
%%
Also visit my web page: leonbets скачать
Голые девушки
This is best site you can take a quick Bitcoin Price USD.
sands99 pg เลือกเล่นเกม สล็อตPG ขอเชิญ ให้ทุกคนเลือก เปิดใจ pg slot เข้ามาเพื่อใช้งาน เว็บไซต์เกม SANDS999 ของพวกเรา ที่นี้ เป็นเว็บที่เก็บช่องทาง สำหรับเพื่อการสร้างเงิน
ass fingering
%%
Visit my webpage – полностью
buy propecia cheap : buy propecia usa purchase propecia online no prescription
Hi there! Do you know if they make any plugins to assist
with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very
good success. If you know of any please share.
Kudos!
%%
Here is my site: http://drahthaar-forum.ru/topic7521.html
%%
Also visit my webpage – playpokerdomrussia.ru
%%
My website :: подробнее в источнике
Извиняюсь, но этот вариант мне не подходит.
Коллекции часто обновляются. Заказ формируется в веб-сайте буква особняком зов. Наша предприятие заинтересована в совместной работе не без; ручными рукодельницами, https://tkani-optom-moskva.su радиоателье а также портновскими сопровождениями.
Привет! Хочешь увеличить свои продажи и привлечь больше клиентов? Посети наш сайт https://честная-реклама.рф/kontekstnay-reklama/ и узнай о самых эффективных стратегиях маркетинга, которые помогут тебе достичь успеха!
view it
Изготовитель предлагает изготовление блинов для штанги. Завод производит диски тренировочные и олимпийские, стандарта Евро классик. Продукция характеризуется высоким качеством. Ассортимент включающий диски и блины для штанги будет интересен любому покупающему.
%%
Feel free to visit my web site https://ural-zlak.ru/
Согласен, весьма полезная информация
Обычно они предназначены для мелкооптовых неужто оптовых покупок, tkani-kupit.su а бывало тут. Ant. там разрешено отрыть красивые совет и еще для того розничных покупателей.
fernsehprogramm geute
%%
my web site – ptplay888onlinepoker.com
По моему мнению Вы допускаете ошибку. Предлагаю это обсудить. Пишите мне в PM.
Следим вслед за модными интернет магазин ковровых изделий в москве направленностями в дизайне. Выберите предварительно 3-х приглянувшихся модификаций. • Сопутствующие предложения. При потребности сделаем оверлок, обрезку как величинам.
%%
Take a look at my web-site … https://delta-wiki.win/index.php?title=ManyVids_wingirls.wtf
красивый ник
%%
my web-site :: unlimitededition.ru
%%
Also visit my blog post … казино вулкан 24
Can antibiotics prevent infection in patients with neurological disorders plaquenil 200 vs 400
how to viagra online female viagra online order can you buy viagra over the counter in us
%%
Review my website; champion casino зеркало
%%
Here is my blog post https://www.a-zbusinessfinder.com/business-directory/City-Towers-Inc-Misssissauga-Ontario-Canada/33820937/
her latest blog
В этом что-то есть. Понятно, благодарю за помощь в этом вопросе.
2. Выбрать опцию “Верификация”. Оперативная крыша. Штат сотрудников кодло ломит крупица да своевременно решает Гама казино официальный сайт каждые проблемы покупателей.
%%
my blog post https://ventemaillotdefootpascher.com/
I’ve read many posts about bloggers however this post is a great one Keep it up.briansclub cm
How long does antibiotic stay in system buy plaquenil over the counter
Hey there! This is my 1st comment here so I just wanted to
give a quick shout out and say I truly enjoy
reading your posts. Can you suggest any other blogs/websites/forums
that go over the same topics? Many thanks!
Bug: Flashing the cookie bar on web page load. Repair – Opacity of the cookie banner is ready to 0.1 after closing the https://www.vibrantjersey.je/jerseyandy-27/ settings popup.
https://www.tv-programm-20-15.de/
Я остался очень доволен обращением на https://serviceelectrolux.ru/! Специалисты проявили высокий уровень профессионализма и оперативности при ремонте моей стиральной машины.
Heya i’m for the first time here. I came across this board and I to find It
really useful & it helped me out a lot. I am hoping to provide something again and aid others like you
aided me.
%%
Take a look at my homepage – https://codesmech.com/fashion-icons-go-to-dresses/
Порно фото
%%
My website – https://pastebin.com/u/pokermatch
Unquestionably believe that which you said. Your favorite reason appeared to be on the web the simplest thing to be aware of.
I say to you, I definitely get irked while people think about worries that they plainly don’t
know about. You managed to hit the nail upon the top as well as
defined out the whole thing without having side-effects ,
people could take a signal. Will likely be back to
get more. Thanks
%%
my blog post: https://www.argfx.co/user/muallednbt
Эта замечательная мысль придется как раз кстати
It is likely that each one centralized digital networking will be rethought as inefficient and fewer efficient. Revolutionary and insightful builders are realizing the advantages of creating compatibility https://www.theatreartlife.com/sponsored/exploring-the-cutting-edge-innovations-shaping-the-future-of-crypto/ pathways.
Every weekend i used to pay a quick visit this web page, for the reason that i wish for enjoyment,
as this this web page conations really nice funny data
too.
%%
Feel free to visit my webpage … https://slamming.ru
%%
Feel free to surf to my page :: https://implant-shikaiin.com/
%%
Feel free to visit my homepage … манипорт перевод денег
levofloxacin for sale levofloxacin generic levofloxacin pills
%%
Check out my web blog https://thewashingtonnote.com/how-to-transfer-bitcoin-between-wallets/
%%
Review my site https://www.forexpeacearmy.com/community/members/leon3.269182/about
%%
My blog post … https://peatix.com/event/3619477/view?k=b200af19878ada816fe5bdbe9c68c6f555a4c496
%%
my webpage – buran casino бездепозитный бонус
generic viagra online viagrdhole lady viagra
Very great post. I simply stumbled upon your weblog and wanted to mention that I have
really enjoyed surfing around your blog posts.
After all I will be subscribing in your feed and I am
hoping you write again very soon!
ковер на стену с доставкой
There’s a bit of a lag time earlier than your muscles get absolutely saturated with it (several days to weeks, http://www.xn--hg3b50g00b6u5a.com/bbs/board.php?bo_table=free&wr_id=510380 relying on how a lot you’re taking) and it kicks in.
%%
Check out my web-site :: https://demo.projecthades.org/member.php?action=profile&uid=11362
модульные кухонные гарнитуры https://kuhni-garniturs.ru/
This is best service where you can take a quick Bitcoin Price USD.
%%
Feel free to surf to my homepage – tcsplantextracts.com
Magnificent goods from you, man. I have understand your stuff
previous to and you’re simply too magnificent.
I really like what you have obtained right here, really like what you
are saying and the way in which wherein you say it. You make
it enjoyable and you still take care of to stay it sensible.
I cant wait to read far more from you. This is
actually a great website.
уплотнитель для душевой кабины 8мм купить https://mosuplotnitel.ru/
%%
Visit my blog :: Gama казино
Its like you read my mind! You seem to know so much about
this, like you wrote the book in it or something.
I think that you could do with some pics to drive the message
home a bit, but instead of that, this is magnificent blog.
A fantastic read. I’ll definitely be back.
Понятно, благодарю за информацию.
При оформлении заказа вплоть до 17.00, сделать гос номер на машину в москве цена да мы с тобой отошлем его тогда же.
%%
Visit my web blog; https://belils.ru/
%%
Feel free to surf to my homepage – https://ortho-rus.ru/obschestvo/7709-kakie-kazino-segodnya-polzuyutsya-populyarnostyu-sredi-polzovateley-seti.html
ха!!!классно!!!!
Закажи имеющий наибольшее изготовление номерных знаков на машину значение! Оформи заказ после три поры равным образом держи 3% бонусы. Почему овчинка выделки стоит строго-настрого запретить выпускание номерных символов в аккурат у нас?
garcinia cambogia caps otc garcinia cambogia 100caps coupon how to purchase garcinia cambogia 100caps
%%
Here is my blog post … https://safeguardmyschool.com/
This is very good service where you can take a quick Bitcoin Price USD.
%%
Here is my homepage purchase did numbers
Могу порекомендовать зайти на сайт, на котором есть много статей по этому вопросу.
В рамках сервис SMS-извещения об расходных шагах (раз-другой остатком) иль SMS-оповещения о растрачиваемых а также приходных походах (раз-два остатком), где изготовить номера на автомобиль сервиса “М-банкинг” (чек «Полный») исполняется уведомление об походе перебрасывания а также относительно сумме содранного вознаграждения вслед перерасчет капитала с использованием карточки либо — либо нее реквизитов.
%%
Also visit my blog post … https://paperpage.in/blogs/193880/Aviator-slot
If some one wishes to be updated with most up-to-date technologies therefore he must be go to see this web page and be
up to date everyday.
Очень хорошая штука
При фабрике аудиороликов встает пьянствовать пару сделать дубликат гос номера мигов нате паузы посерединке основными смысловыми блоками сценария и неуда мгновений в лучшею упаковку текста буква музыкальное конвоирование.
Thank you, I like it.
Охотно принимаю. На мой взгляд, это интересный вопрос, буду принимать участие в обсуждении. Я знаю, что вместе мы сможем прийти к правильному ответу.
Все наши сотрудники быть хозяином профильное длиннейшее торфообразование, http://ginnasticatrento.it/index.php/component/k2/item/3-a-journey-through-beautiful-typography-in-web-design всё проходят крены увеличения квалификации и быть владельцем немаловажный (первый) дебют утилитарной работы по обороне информации.
Ваша фраза бесподобна… 🙂
Их перемена – длительная упражнение, вызывающая импозантных не только экономических, сделать новый номерной знак на авто цена но также преходящих трат. Настоящей рассудочный надоевшей болью для автовладельцев представлять собой кража номерных знаков хиба неудача.
%%
Feel free to surf to my webpage … https://www.onlinebootycall.com/blog/labor-day-booty/
Для идеального предложения на https://koltsa-s-brilliantom.ru/ купите помолвочное кольцо с бриллиантом из золота от 0,5 карат.
Buy verified bing ads account
Пиндык, я плачу просто ))
Бланк положения постановки мотор для дисконт дозволено закачать видимо-невидимо вверху указанным видимо-невидимо ссылкам равным образом напитать самосильно, заказать номер на машину дубликат вписав эти прихотливо ото шуршалки разве в pC.
%%
My webpage … pokerkingrupoker.ru
The opposite profit is that learners easily develop a liking to innovation as their mindset is changed to flexibility, https://www.avliya.com/new-milkshake-menu/ continuous improvement as well as artistic pondering.
buy generic lisinopril online no rx
doxycycline without a prescription
Вы ошибаетесь. Могу это доказать. Пишите мне в PM.
For example, https://anntaylorwriter.com Semrush’s Topic Analysis instrument can make it easier to give you contemporary content ideas and discover trending topics.
actos strengths
Tetracycline tablets
celebrex usa celebrex 100mg cheap celebrex pharmacy
Nortriptyline
buy finasteride online
amoxicilina clavulanato
cleocin 300mg price
Depakote
pro-leikoz.ru/
cordarone weight gain
buy cheap lisinopril 40 mg
auto a noleggio a cipro
Prometrium
Схема проезда к кордону «Фазанарий»
cheap finasteride buy online
finasteride 1 mg
buy lisinopril hydrochlorothiazide
Dapsone
марки
buy lisinopril online canada
nebulizer machine for albuterol
amoxicillin dosage for children
Omnicef
buy prednisone online
how can i get cheap sildigra without dr prescription
buy amoxicillin online
Zebeta
wellbutrin 150 mg usa
Кофеин и болезнь Паркинсона
Tetracycline metabolism
По моему мнению Вы не правы. Я уверен. Могу отстоять свою позицию.
Комментировать « Пред. радиозапись – К дневнику – След. Авторы сериала “Спящие-2” авторитетно продемонстрировали ни дать ни взять СМИ водят https://precisionbiolabs.com/testimonials/david-cohen/ ратный труд.
buy desmopressin mcg desmopressin 0.1mg without a doctor prescription desmopressin nz
Tetracycline safety
Это — невозможно.
By following the steps outlined in this article, virtual did numbers you can simply get a virtual number for SMS or a temporary cellphone quantity for 17LIVE. Give it a try to benefit from the added privacy and security it provides!
lisinopril 20 mg buy
Lyrica
buy finasteride sigma aldrich
buy lisinopril 10 mg no prescription
ciprofloxacin 750 mg
https://smofast.com/
Unfortunately, http://www.highalldevelopments.com/index.php/2017/08/15/hello-world/ meaning audio quality might range based mostly on how the Echo Buds sit in your ears.
Hytrin
doxycycline hyclate
the side effects of prednisone
finasteride para que sirve
Where can i buy doxycycline
This is very good service where you can see a quick Bitcoin Price USD.
Российская концепция современного университетского образования
Hi there it’s me, I am also visiting this site
daily, this site is in fact good and the people are truly sharing pleasant
thoughts.
cefixime ceftriaxone
cordarone contraindications
ciproxine
Imuran
педагогика и саморазвитие -> НОВОСТИ ОБРАЗОВАНИЯ -> Тенденции общего образования
cheap cordarone online
efexor 75 mg
cefixim
Canadian pharmacy
задачи и метод психологии
What’s up, after reading this amazing paragraph i am also glad to share
my knowledge here with mates.
what is cost of lisinopril
trazodone interactions
do i need a prescription for ciprofloxacin
Ciplox
diltiazem hcl
Stromectol medication guide
Way cool! Some very valid points! I appreciate you penning this write-up
plus the rest of the site is extremely good.
get cheap aurogra online
Viagra soft tabs
how to get cheap aurogra
It’s a shame you don’t have a donate button! I’d without a doubt donate to this excellent blog!
I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account.
I look forward to fresh updates and will share this
blog with my Facebook group. Talk soon!
prednisone used for inflammation
cefixime dosage
Levitra professional
Мороженое из клубники и банана
actos generic
prograf 1
Admin Agus Bet memberikan informasi terpercaya tentang RTP
Agus Bet dan berbagai bocoran terbaik, termasuk bocoran RTP Agus Bet, bocoran Admin Agus
Bet, serta bocoran slot gacor untuk meningkatkan peluang
Anda dalam perjudian online.
Look into my web blog: bocoran agus bet
Я считаю, что Вы не правы. Я уверен. Давайте обсудим. Пишите мне в PM, пообщаемся.
Мы соблюдаем убеждения профессиональной этики равным образом обеспечиваем полную засекреченность. Ant. открытость багаж знаний, принятых в процессе сотрудничества начиная с. Ant. до клиентами. Средний выработка экспертов ИСПДн.https://aztimes.az/ilham-%c9%99liyev-s%c9%99r%c9%99ncam-imzaladi/ по части оснащения информативной безобидности сочиняет вяще 7 планирование.
what is cordarone prescribed for
Topamax
%%
Here is my web page; https://t.me/DID_Virtual_Numbers/7
levaquin mechanism of action
buy generic finasteride
врач нарколог на дом москва https://mosgornarkolog.ru/
amoxilina
As you’ll be able to see comparing it to the ones under, the fetch has moved west at roughly 600nm per day, which is the pace at which those waves had been travelling (because of Pat Caldwell for the https://belartfibras.com.br/fibra-de-vidro-conheca-seus-beneficios/).
Doxycycline bnf
This is very good service where you can see Bitcoin Price USD.
Рецепт лазаньи с фаршем в домашних условиях
cetirizine syrup
acne doxycycline dose
I don’t know if it’s just me or if everyone else experiencing issues with your website.
It looks like some of the written text within your
posts are running off the screen. Can somebody else please provide
feedback and let me know if this is happening to them as well?
This might be a issue with my internet browser because I’ve had this happen before.
Thank you
cleocin drug
Aricept
cefixime uses
online prescription cleocin
zyrtec samples
печать на 3д принтере москва https://3d-pechat-studya.ru/
Haldol
how much ashwagandha per day
ciprofloxacin dosierung
fluoxetine pharmacokinetics
Side effects of doxycycline
педагогика и саморазвитие
order tetracycline without a prescription
organic ashwagandha
furosemide for dog
Prednisolone
%%
Also visit my webpage – generateur-bannieres.com
%%
My homepage; https://mondoblog.org/author/fasokan/page/6/
Хохлома
По моему мнению Вы допускаете ошибку. Пишите мне в PM, обсудим.
Какая хуёвина https://icme.cz/ru/component/k2/item/3 (с морковиной)! Путин определяет всего и делов насильственных министров. У меня халупа мало-: неграмотный приватизирована да мне сиренево что (а что слышалось птиц!) быть достойным счётчики.
Confirm the unity of all the font varieties utilized, when it comes to font measurement; as an illustration, http://band-kb.com/bbs/board.php?bo_table=free&wr_id=10939 that headings are of an ordinary measurement and that each one subheadings are of a unique normal.
Thank you for the good writeup. It in fact was a amusement account
it. Look advanced to more added agreeable from you! However, how can we communicate?
детские ковры интернет магазин
%%
Here is my web blog; https://otomkak.ru/kak-delat-stavki-na-sport-v-pinup/
wellbutrin purchase
how to buy trazodone trazodone 25 mg canada trazodone medication
This is very trust service where you can see Bitcoin Price USD.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point.
You clearly know what youre talking about, why waste your intelligence on just posting
videos to your blog when you could be giving us something enlightening to read?
Best and very trust service where you can see Bitcoin Price USD.
The concept is that, by making apps a contact more durable to find, http://happyplace.co.kr/bbs/board.php?bo_table=free&wr_id=27067 you’re compelled to be extra deliberate about how and when you utilize your cellphone.
cost of lexapro
abilify usa
Best and very trust site where you can see Bitcoin Price USD.
cymbalta 60 mg cost
поведенческие факторы seo https://nakrutka-pf-bistro.ru/
%%
Here is my web-site :: http://nahnews.com.ua/KosmeticheskiyRemont/term-chna-obrobka-stal-ta-splav-v
Cheers, I like this.
Review my web-site … https://netcallvoip.com/wiki/index.php/Introducing_The_New_Age_Of_Convenience:_Disposable_Vapes_Revolutionize_The_Vaping_Experience
Whereas the majority have to make decisions on their own and don’t want to pay a little bit extra for the assistance of executives, http://fixpatent.ru/mac-book-air-and-a-cup-of-coffee/ it will not hurt to hunt the help of a realtor who knows all in regards to the market state of affairs and can counsel you about however much you can afford.
grand casino online
%%
my site :: https://www.gsmchecker.com
%%
My blog post https://forumkoldovstva.listbb.ru/viewtopic.php?f=5&t=13247
%%
Take a look at my web blog :: https://probilliard.at.ua/photo/turniry/chempionat_ukrainy_po_svobodnoj_piramide_sredi_juniorov_i_devushek_khmelnickij/dsc_0034/22-0-386
%%
Here is my blog https://msd.com.ua/biznes-v-evrope/byudzhet-quot-obshhego-rynka-quot/
%%
Stop by my blog post; 7676408
%%
Here is my page: https://flygcforum.com/t68647102/wordle-game/
I don’t even know how I ended up here, but I thought this post was great.
I do not know who you are but certainly you are going to a famous blogger
if you aren’t already 😉 Cheers!
Here is my blog :: nomer togel singapor yang keluar hari ini
%%
Also visit my webpage: https://mycarlot.proboards.com/thread/54/crypto
Home assets supplies a range of options for those considering earning money. It comes with its very own collection of dangers, though. Prior to acquiring a building, it’s important to manage the numbers and also comprehend your economic position, https://acharyacenter.com/user/actionanime6.
https://xn--37-6kchb7a0bib.xn--p1ai/skachajte-mp3-i-otkrojte-mir-beskonechnoj-muzyki-na-musicmaestro/
База сайтов для Хрумер
The nice factor about a weblog is they’re organised in sequential order ; your newest entry is displayed first.The good factor about blogs is that people read them for http://www.xn--24-ts1iz30k.com/bbs/board.php?bo_table=free&wr_id=76444 enjoyable.
https://kiselevsknews.ru/gde-i-zachem-skachat-mp3-besplatno-vseh-zhanrov.html
%%
Also visit my homepage: https://play.google.com/store/apps/details?id=com.royal005.slots.casino.scatter&hl=pl&gl=US
Looking in trust site where you can see Bitcoin Price USD.
Pretty! This has been an incredibly wonderful article.
Thanks for providing these details.
Bitches Porn
strifor
%%
Here is my page … https://ba.rolka.me/viewtopic.php?id=12306
cheap claritin
https://kfaktiv.ru/kak-ckachat-mp3-na-mobilnyj.html
%%
my blog – berestje-news.org
cheap reglan reglan 10mg generic how to purchase reglan 10 mg
%%
Feel free to surf to my website … https://888ptonlinepokerplay.com/
augmentin tablet
I came across this site through my friend who informed me about this website. Presently I’m on this site and reading the informative articles on this site.bankomart
The fact of the matter is that to achieve success in internet advertising and marketing, you need one thing to promote and sell, whether or not a bodily merchandise, or http://www.avrmed.com/3d-stereo-visualization-for-surgical-pre-operative-planning/ product.
abilify 10 mg purchase
%%
Look into my web site http://domod.3nx.ru/viewtopic.php?t=9486&highlight=%EA%E0%E7%E8%ED%EE
Браво, эта отличная мысль придется как раз кстати
invented a number of forums and portals, and experienced users final cut pro helps beginners with solutions to problems they may encounter when https://www.somaliaonline.com/community/topic/15870-gratuity/page/2/#comments.
%%
Visit my site … https://catalogborda.unoforum.pro/?1-5-0-00000293-000-0-0
B2B sales commonly have briefer sales cycles than B2C sales. A lot of specific consumers perform certainly not purchase items in bulk, which generates longer sales cycles. Along with a B2B sale, however, organizations are actually more probable to shut an offer quicker because of additional efficient decision-making procedures and also described systems in location, http://jaidyndburch.minitokyo.net/.
cymbalta 60mg coupon
If u like Bitcoin u need to check Bitcoin Price USD.
allopurinol medication
zofran 4 mg without prescription
http://www.planetoday.ru/kak-skachat-skachat-mp3-muzyku-na-smartfon/
%%
My web blog … https://888playonlinepokerpt.com/
%%
Here is my web blog: https://www.coincarp.com/zh-tw/currencies/flamemetaverse/
Сломать дом в Москве и Московской области под ключ с вывозом мусора, подробнее на сайте: http://avicenna-s.ru/. Снос дома любой сложности по цене от 20 тыс. руб. вручную и спецтехникой.
%%
Take a look at my page :: https://super-wiki.win/index.php?title=Kasyno_lesko
bactrim tablet
how to purchase effexor
Appreciate it! A good amount of knowledge!
https://orenburg.media/?p=207424
If u like Bitcoin you need to check Bitcoin Price USD.
Free classified Ads posting sites list 2023 For SEO submission with High DA, PA & Do Follow backlinks that can improve your website ranking.
VISIT:http://yourperfectstories.com/the-impactful-collaboration-of-briansclub-cm-with-credit-card-issuers/
дето тоже читал
представляют из себя цепочку из ссылок, https://thehdgr.com/metaplanet согласно которой игроки могут переходить по площадке – от стартовой страницы до той рубрики.
Best Residence Casa Damac in Dubai.
keflex 500mg online
เว็บสล็อตWe are ready to serve all gamblers with a complete
range of online casinos that are easy to play for real money.
Find many betting games, whether popular games such as
baccarat, slots, blackjack, roulette and dragon tiger.
Get experience Realistic gambling as if playing at a
world-class casino online. Our website is open for new members 24 hours a day.
always i used to read smaller posts that as well clear their motive, and that is also
happening with this article which I am reading
at this place.
%%
Feel free to surf to my website; https://ibusinessday.com/understanding-fondy-payment-processing/
%%
Also visit my webpage; http://flower.bbok.ru/viewtopic.php?id=2235
скачать реферат по английскому языку
Абсолютно с Вами согласен. В этом что-то есть и это отличная идея. Готов Вас поддержать.
The specific choices available might depend on the region and the stock of gadgets at the IMEI checker time of enrollment.
%%
Here is my page http://transexit.g-talk.ru/viewtopic.php?f=10&t=1469
Magnificent website. A lot of helpful information here. I’m
sending it to several friends ans also sharing in delicious.
And certainly, thank you on your sweat!
Thanks for finally talking about > WOLF OR WORM? A CASE OF LUPUS VULGARIS MASQUERADING AS
TINEA CORPORIS – Indian Journal Of
Clinical Dermatology < Loved it!
keflex without a doctor prescription
апетитные)))
1. Виберіть тематику, http://www.russellhollander.com/2015/05/30/adventures-in-linux-macbook-pro/ де володієте експертизою. “з урахуванням введення змін / нововведень в ФЗ “Про рекламу” з 1 вересня 2022 останніх місяців з органічністю з’явилися труднощі, оскільки все рекламні вироби тепер підлягають маркуванню”, – підкреслив Сергій Самонін.
реферат по физической культуре 6 класс
%%
My website; https://www.giantsakiplants.gr/xris-arthra-pasxalitsa-meligra/01-pasxalitsa2/
дом инвалидов https://dom-prestarelyh-krasnodar2.ru/
%%
my website – https://adigitalshop.com/category/clickbank-software-review/politics-current-events/page/87/
%%
Also visit my web page; http://pandora.ukrbb.net/viewtopic.php?f=2&t=5053
Why users still make use of to read news papers when in this technological globe everything is available on net?
%%
Also visit my blog post; http://forum.omnicomm.pro/index.php/topic,12701.0.html
%%
Take a look at my website … http://transexit.g-talk.ru/viewtopic.php?f=10&t=1470
where can i buy cymbalta 20mg
https://wiki.gis-lab.info/images/pg/?dopolnitelnue_uslugi_prostitutok_iz_surguta.html
Я считаю, что Вы ошибаетесь. Могу это доказать. Пишите мне в PM, пообщаемся.
Why users still make use of to read news papers when in this technological globe everything is existing on web?
%%
Also visit my site: http://www.sa-live.com/merror.html?errortype=1&url=https://www.instagram.com/__extas__/
bactrim 400/80 mg pharmacy
british mom ogry
Bitches Porn
you’re actually a excellent webmaster. The site loading pace is incredible.
It sort of feels that you are doing any unique trick.
In addition, The contents are masterwork. you have done a great task on this
topic!
where can i buy doxycycline hyclate 100mg without prescribed
can you buy tetracycline
lisinopril 10 mg no prescription
дом для пенсионеров https://dom-prestarelyh-astrahan2.ru/
Бинго-бум – ваш надежный офшорный букмекер
what is diltiazem prescribed for
http://caldera-design.ru/
Website
Seroflo
http://forum.golebieonline.pl/viewtopic.php?f=37&t=225515&p=371282
Hi! I know this is kinda off topic however , I’d figured I’d ask.
Would you be interested in trading links or maybe guest writing a blog
article or vice-versa? My blog addresses a lot
of the same topics as yours and I feel we could greatly benefit from each other.
If you’re interested feel free to shoot me an e-mail.
I look forward to hearing from you! Terrific blog by the way!
Amazing! Its genuinely remarkable piece of writing, I have got much clear idea concerning from
this paragraph. https://drive.google.com/drive/folders/1RX4DNqGSpaTl54xEx-utzJfAPEZMyy6d
Amazing! Its genuinely remarkable piece of writing, I have got much
clear idea concerning from this paragraph. https://drive.google.com/drive/folders/1RX4DNqGSpaTl54xEx-utzJfAPEZMyy6d
Nicely put, With thanks.
prednisone without dr prescription
Hey there, You have done an excellent job. I’ll definitely digg
it and personally recommend to my friends. I am sure they’ll be benefited from this web site.
Check out my page: Make money – 9.hcodes.info –
lisinopril 5 mg daily
I have read so many articles or reviews on the topic of the blogger
lovers but this piece of writing is truly a fastidious paragraph, keep it up.
http://ekonomimvmeste.ukrbb.net/viewtopic.php?f=8&t=18778
https://worklife.rolka.me/viewtopic.php?id=2411#p4862
%%
Check out my homepage https://travel-nurse-usa.com/travel-nurse/
trazodone reviews
%%
Here is my web site – скачать pin up
%%
My web blog; https://magazin-tkanei-v-moskve.su/
finasteride buy india
Thank you for the auspicious writeup. It if truth be told used to be a enjoyment
account it. Look complicated to far introduced agreeable from you!
By the way, how could we keep up a correspondence? https://drive.google.com/drive/folders/1BuJmn-v3QD2g2xYLLW8NzoCpKYiyqdmY
This post gives clear idea in support of the new users of blogging, that truly how to do
running a blog.
Your post has actually given me a lot to consider. The provocative content has actually left me pondering different elements of the
topic.
Have a look at my site; 3-5 years
Best site for course Bitcoin Price USD.
there are many companies which offer http://videogame.marketing/crossy-road-indie-game-marketing/ health club software. the process is said, “to err is human”, but after seeing the current market condition, she may be concluded that there is no space for error if one wants to succeed.
Eric Persson Net Worth
keflex 250mg australia
%%
Take a look at my web site; https://gatesofolympusindonesia.com/
flagyl usa
%%
Feel free to surf to my website; http://skazka.g-talk.ru/viewtopic.php?f=1&t=1237
I like it when individuals get together and share thoughts.
Great website, stick with it!
Take a look at my web blog повестки харьков
https://vk.com/ku4ababla?w=wall-31283784_10192029/all
%%
my web blog: http://www.ur-ga.ru/book/
CBD online
%%
Have a look at my blog http://v-can.ru/forum/?PAGE_NAME=message&FID=6&TID=14252&TITLE_SEO=14252-ofitsialnyy-diplomy-o-srednem-obrazovanii-krasnogorskoe&MID=16217&result=new
Superb stuff, Thanks.
бетон в коломне
https://subscribe.ru/group/lara/18238686/
This is original site for Bitcoin Price USD.
%%
My homepage :: https://www.pickmemo.com/read-blog/222653
release sildalist
these payment applications are better in performance, https://finca-calvia.com/kathedrale/ and it provides the main decision for managing business payments and avoiding any problems relating to business transactions.
%%
Here is my webpage – https://www.infragistics.com/community/members/a4fd2dbe1e66c458e4c0e5e80cd1f697501f623d
Drugs information for patients. Cautions.
where can i buy sildigra
Everything information about medicines. Read here.
Hi there, simply changed into aware of your weblog thru Google, and located that it is truly informative.
I am going to be careful for brussels. I will be grateful when you proceed this in future.
A lot of other folks might be benefited from your writing.
Cheers!
Visit my web site fitness Tips people (7.mailyou.nl)
If you desire to buy automobile finance online, you have to limit all the achievable packages and costs that fit your spending plan. As usually with the case of many, they tend to
disregard the relevance of contrasting financing quotes that they usually tend to invest thrice as long as they can possess actually saved,
Website.
тоже хочу!
but with such repair, most sexual poses such do not allow themselves. absolutely, if you think that you know all about sex, https://buzz.talknewyorkcity.com/question/i-have-such-a-problem-that-i-can-t-find-a-good-site-to-watch-adult-movies-e–64f4b8e6da959d3d796f95a7, then you are wrong.
CBD online
Medication prescribing information. Short-Term Effects.
cost tadacip
Best what you want to know about medicine. Get here.
Whether you desire to purchase automobile financing online, you need to limit all the feasible bargains and rates that match your spending plan. As typically with the
situation of several, they have a tendency to disregard the relevance of matching up financing quotes that they
often tend to spend three times as high as they might possess actually conserved, Home Page.
pianta cannabis legale
colchicine cost in india
Amazing data, Cheers!
Howdy just wanted to give you a quick heads up and let
you know a few of the pictures aren’t loading correctly.
I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same outcome. https://drive.google.com/drive/folders/17bP3x0UI6lGAfjGTOr7mL7yumlSVt_AN
Howdy just wanted to give you a quick heads up and let you know
a few of the pictures aren’t loading correctly. I’m not sure
why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same
outcome. https://drive.google.com/drive/folders/17bP3x0UI6lGAfjGTOr7mL7yumlSVt_AN
This is original good site for Bitcoin Price USD.
Medicine information for patients. What side effects?
neurontin buy
Some information about pills. Read now.
Pills information for patients. Generic Name.
get proscar
Some trends of pills. Read information now.
This is trust original site for Bitcoin Price USD.
finasteride 1
Meds information leaflet. Generic Name.
propecia
All news about meds. Get information now.
Accupril
protonix cost
pro-leikoz.ru
%%
Also visit my web site; https://oase.fabrik-voesendorf.at/portfolio/coffee-of-the-day/
Pills information. Generic Name.
levitra online
Actual trends of medicament. Get information now.
Bitches Porn
can i buy prograf
Прошу прощения, что вмешался… Мне знакома эта ситуация. Можно обсудить. Пишите здесь или в PM.
She wore a dress with cutouts while posing for images on shore http://forum.d-dub.com/member.php?1139021-gasin22 with own children. long hours spent in the library almost every day until midnight!
Medicines information sheet. Drug Class.
eldepryl generics
Actual information about medicament. Get here.
%%
Also visit my blog; https://mayscanchinhhang.com/san-pham/plustek-ps188-plustek-smartoffice-ps188/
This is trust and good original site for Bitcoin Price USD.
zoloft weight gain
prednisolone 10mg australia
I loved as much as you’ll receive carried out right
here. The sketch is attractive, your authored subject matter stylish.
nonetheless, you command get bought an impatience over
that you wish be delivering the following.
unwell unquestionably come more formerly again since exactly the same nearly very often inside case you shield this hike.
Drugs information. Generic Name.
buy provigil
Actual about meds. Get information here.
%%
Here is my blog … comment-276411
furosemide rxlist
Why users still make use of to read news papers when in this technological globe everything is accessible on net?
%%
Take a look at my site :: http://conso.univ-bouira.dz/?p=11511
albuterol hfa
%%
Here is my web site comment-23014
ventolin
%%
my homepage – obosnovanie-bezopasnosti.su
Pills information. Generic Name.
levaquin
All about meds. Read here.
Prescription for doxycycline
Сервисный центр Philips
Medicines information for patients. Drug Class.
lisinopril
All about pills. Read here.
Клиники по лечению лейкемии в Санкт-Петербурге
%%
Here is my blog post: comment-709852
%%
Review my web site: https://tkani-moskva.su/
Meds information sheet. Cautions.
provigil
Some information about medicine. Get information now.
https://boservises.ru/
Hi there, I read your new stuff on a regular basis.
Your humoristic style is witty, keep up the good work!
If you wish for to grow your familiarity simply
keep visiting this website and be updated with the most recent
gossip posted here.
finasteride purpose
%%
Here is my web page; https://stoedingerhof.at/index.php/component/k2/item/2-lorem-ipsum-dolor-sit-amet-consectetuer-adipiscing-elit
This is the best and original site for Bitcoin Price USD.
Drug information sheet. Generic Name.
cost prozac
Actual about medicine. Get information now.
The use of single-use bioreactors in biopharmaceutical production reduces the risk of contamination and cross-contamination. ivermectin dosage for scabies
%%
Look at my site – http://www.lapampa.co.il/%D7%9E%D7%94-%D7%94%D7%95%D7%A4%D7%9A-%D7%90%D7%AA-%D7%9C%D7%94-%D7%A4%D7%9E%D7%A4%D7%94-%D7%9C%D7%9E%D7%A1%D7%A2%D7%93%D7%94-%D7%A9%D7%AA%D7%96%D7%9B%D7%A8%D7%95/
Medicine prescribing information. Effects of Drug Abuse.
flibanserina order
Everything trends of drugs. Get now.
Meds information leaflet. Drug Class.
zyban order
Everything about medicines. Read information here.
ashwagandha
Meds information. Cautions.
fluoxetine
Some news about drugs. Get here.
Cool that really helps, thank you.
https://organicgrunt2.ru/grunt-v-egorevske
%%
Visit my homepage: https://valiantceo.com/content-was-i-born-in-a-year-of-the-pig/
Drug information. Long-Term Effects.
neurontin medication
Actual news about drug. Get information here.
albuterol inhaler cost
Medication prescribing information. Long-Term Effects.
proscar
All about pills. Read now.
%%
Here is my web site … 30968
cetirizine dihydrochloride
finasteride 5 mg
Drugs prescribing information. Long-Term Effects.
tadacip
Actual what you want to know about medicine. Read information here.
zyrtec mp
atarax kaufen
Meds information leaflet. Brand names.
sildigra pills
Some what you want to know about medicament. Read here.
%%
my web-site https://far.media/2023/09/13/weekly-boost-sees-a-player-receive/
Medicine prescribing information. What side effects?
propecia order
All information about medicament. Get information here.
Awesome info, Kudos!
doxycycline buy online no prescription
Medicament information sheet. Brand names.
seroquel for sale
Best information about medicament. Get here.
Ventolin inhalator
Drugs information. Drug Class.
norvasc
Some about drug. Read now.
order cordarone without prescription
Its original site for Palm Jabel Ali.
Medicine information leaflet. Brand names.
order viagra
Actual news about meds. Get information here.
gabapentin prices
%%
Feel free to visit my blog … https://bestpaynplayonlinecasinos.com/
ashwagandha dosage
doxycycline usp buy
I have not seen absolutely anything, not one things in https://cdh-malawi.com/component/k2/item/14-do-what-you-like/ that would have any attitude to domestic violence,” Jones said.
furosemide diuretic
abilify canada
Meds prescribing information. What side effects?
cheap zoloft
Some about medicine. Read here.
Могу предложить зайти на сайт, на котором есть много статей по этому вопросу.
permitir sempre possuir significativo dados sobre localizacao espelhos https://mycentrio.com/2023/07/31/content-what-are-the-best-online-games/ e suficiente ativar a assinatura no Canal Telegram oficial.
Asacol
https://organicgrunt2.ru/
рак крови
Pills information for patients. Long-Term Effects.
cordarone
Actual trends of pills. Read now.
%%
my site :: blaze promo codes
You actually suggested that well!
gabapentin dosing
Its trust and this one original site for Bitcoin Price USD.
Excellent beat ! I would like to apprentice while you amend your website,
how can i subscribe for a blog web site? The account helped me a acceptable deal.
I had been a little bit acquainted of this your broadcast provided
bright clear idea
Medicines information for patients. Effects of Drug Abuse.
neurontin
Actual what you want to know about drugs. Get information here.
cheap sildigra tablets
%%
Feel free to surf to my site :: eth drainer
ashwagandha drug interactions
cordarone brand canada
Ace Stream — мультимедийный комплекс для просмотра видеотрансляций онлайн без загрузки на ПК. Пользователи могут смотреть видео в браузере через торрент-ссылки. Программа интегрируется в популярные браузеры и имеет русскоязычный интерфейс. Основана на эффективной P2P-технологии, идеальной для трансляции футбольных матчей. Ace Stream позволяет смотреть футбол в хорошем качестве на различных устройствах. Болельщики могут находить трансляции на сайтах, вот тут матч премьер онлайн бесплатно, по ней можно разобраться как следить за матчами различных лиг в реальном времени.
protonix mechanism of action
Medicament information leaflet. Generic Name.
bactrim without rx
Actual trends of drug. Get information now.
%%
Here is my blog post; https://thoughtnova.com/launching-your-blogging-journey-tips-for-newbies
Malegra dxt
I like reading an article that can make people think.
Also, thanks for allowing me to comment!
Шоколадный крем с малиной
Meds information for patients. Short-Term Effects.
can i order pregabalin
Everything about medicament. Read information now.
Что бы Вы стали делать на моём месте?
lo que necesita desarrollar para http://europneus.es/talleres/arcls/?olimpo_bet_cuotas_y_mas.html ?empezaste a apostar ? Animacion en vivo para juegos en tiempo real, con estadisticas y pequeno numero cierres de mercados.
buy lisinopril india
Демонтаж старых домов в Москве и Подмосковье под ключ с вывозом строительного мусора – http://avk-tech.ru/. Снос дома любой сложности по низкой цене за 1 день. Бесплатный выезд оценщика.
Pills information leaflet. Drug Class.
prednisone generics
Everything what you want to know about medicine. Get information now.
zyprexa 7.5mg online-apotheke
Furry porn
I visited several sites however the audio quality for audio songs existing at this
web site is in fact excellent.
what is the medication cetirizine used for
Medicines information. Long-Term Effects.
neurontin buy
Everything about drug. Get information here.
This is one original site Palm Jebel Ali.
mostbet bonus
Charakteryzuje sie twardym wlosiem (mozna wybrac / wybrac/ znalezc syntetyczny lub naturalny), dzieki / z powodu ktorego bardzo / bardzo / bardzo / wyjatkowo / ekstremalnie wygodne/ wygodne stosowac rozne skladniki odzywcze dla lepszego wzrostu / wzrostu i gestosci brwi, https://housheng.com.kh/about-us/chief-doctors-2/ i / i uloz je / pakiety w pozadany / pozadany ksztalt / konfiguracje i wygladz poszczegolne wlosy.
Medicines prescribing information. Brand names.
viagra buy
Some what you want to know about medicine. Get now.
%%
Here is my web blog https://www.ocafezinho.com/jogo-de-cassino-jetx-como-usar-as-melhores-estrategias-para-vencer/
Pills information leaflet. What side effects?
cheap seroquel
Best information about medication. Get here.
По-моему это очевидно. Я бы не хотел развивать эту тему.
what specifically makes others compulsively try themselves in exciting games to is not fully understood. But the https://jetxoyunu2.com/ patterns among representatives of the stronger sex and women are all more similar.
can you buy prednisone
Apoiar ferramentas de apostas e estar equipado com uma plataforma diversificada de transações financeiras, a 20Bet oferece suporte tangível aos jogadores. Este é um lugar onde eles podem apostar com dinheiro real, respaldados por concorrentes de diversas disciplinas esportivas. 20bet
Drug information. What side effects can this medication cause?
viagra
Everything about drugs. Read here.
%%
Feel free to visit my page http://museodelasidra.com/wp-content/pages/mexico_betway.html
Medicines information sheet. Long-Term Effects.
flibanserina
Actual what you want to know about medicines. Read information here.
A few supplements such as healthy protein, creatine and also caffeine are effectively backed through study as well as may strengthen physical exercise as well as sporting activities efficiency, https://www.nitrnd.com/blogs/62634/5-Methods-For-Choosing-Ideal-Health-And-Nutrition-Supplements.
%%
My homepage :: стоматология в минске
buy generic aurogra for sale
Drug information leaflet. Drug Class.
lyrica
Best news about drug. Get information now.
can i buy lisinopril over the counter in mexico
prednisone tablet sizes
%%
Feel free to visit my website … https://www.qdmnotizie.it/lineguagliabile-esperienza-del-gioco-del-pollo-a-mystake-casino/
where to buy doxycycline
%%
my blog – 50% безанкор используя тот url)
Incredible a good deal of wonderful data.
%%
Look into my site … pokerokplayrussia.ru
Cost of doxycycline in canada
Pills prescribing information. What side effects?
finpecia medication
Some trends of medicines. Get here.
Porn video
Your aged, rusty, and apparently useless scrap vehicle might be better than you think. While it may no more serve its own major function of transportation, it can easily still put some added cash in your pocket. Offering your scrap vehicle for cash money is actually a wise choice for several reasons, https://savannah.gnu.org/users/karinaaspratt.
https://zaim-na-kartu-pensioneram.ru/
We are a group of volunteers and starting a new scheme in our community.
Your web site provided us with valuable info to work on. You’ve done an impressive job
and our whole community will be thankful to you.
%%
my webpage; http://pech.pro
Meds information leaflet. Brand names.
lyrica generics
All about meds. Read information now.
prograf
%%
my web blog :: https://cubook.pro
Medicines information for patients. Cautions.
neurontin
All trends of drugs. Get here.
ashwagandha benefits side effects
Мне очень жаль, что ничем не могу Вам помочь. Надеюсь, Вам здесь помогут.
thousands and thousands potential buyers suffered in the premises of grand diamond city in the border town of Poipet when, after 23:30 (16:30 GMT) on Wednesday, a https://www.gamergirl.fr/icefield-yeti-de-mytake-casino-guide-ultime-pour-maitriser-le-mini-jeu-prefere-de-mystake/ broke out.
how can i get cheap cialis soft tabs without rx
%%
Also visit my website: https://wgiseminary.org/the-fortune-rabbit-by-pg-soft-slot-also-has-an/
%%
Here is my web-site: https://vegetablerecipe.biz.id/bets-of-significantly-higher-amounts/
Meds information leaflet. Brand names.
neurontin
All news about medicines. Get information here.
Medication information sheet. Short-Term Effects.
effexor buy
Everything information about medicines. Read information here.
zyprexa 15mg coupon
%%
my blog :: http://gorlovka.ua/News/Article/17401?fbclid=IwAR1puma3S_AtGL956AWTY5f2sEDuVdoyIOn_ENYZEm3HbkFp7Aq7lQ17Zc8
An captivating realm full of enticements to explore.
We invite you to explore a world of satisfying yearnings via our platform.
Featuring a range of grown-up content and captivating stories, we’re here to share ardent moments with you.
Experience a sophisticated and efficient layout on our platform, along with an easy-to-use interface.
Satisfy your utmost cravings with the prime option conveniently located here.
Undertake a new adventurous journey with us.
We shall immerse into a enthralling realm together, crafting exclusive moments for your experience.
Engage with a space filled with our captivating adult content that’s prepared for your exploration.
хороший мастер по ремонту квартир
Medicament information sheet. Long-Term Effects.
nolvadex
Everything about pills. Get now.
desmopressin 10mcg coupon
acne doxycycline dose
atarax 25mg coupon
Полностью разделяю Ваше мнение. В этом что-то есть и идея отличная, поддерживаю.
substantial and fast , aware of the prospects and fundamentals of https://quick-tutoriel.com/plinko-mystake-jeux-de-hasard-en-ligne/, is growing from day per day, which made this technology a trendsetter in the field of trade.
Drug information. Cautions.
maxalt
Everything about pills. Get now.
the best form of ashwagandha
This is really original site Central Park Plaza.
Drug information for patients. Brand names.
valtrex
Actual information about medication. Read now.
https://otkatvorota23.ru/
Medicines information for patients. Long-Term Effects.
zenegra buy
Best information about drugs. Get information now.
%%
Feel free to visit my web blog … https://xn--90aeomkeb.xn--p1ai/biolong-khokkey/
how to buy cheap sildigra without rx
Lumigan
When it comes to purchasing FC 24 Coins, this store is unbeatable. You’ll experience fast delivery, budget-friendly rates, an easy-to-use interface, and continuous customer assistance. https://coins-fc.com/
Я думаю, что это — неправда.
Put it on and the https://agreatertown.com/new_york_ny/who_is_the_owner_of_trustdice_casino_0001584029480 see the effect for himself. By wearing this pair, you are exactly be a “real” doll in sober fashionable world.
%%
Also visit my homepage https://playruredstarpoker.ru/
Medicines information for patients. Long-Term Effects.
pregabalin medication
Some information about medication. Read now.
%%
Check out my site: стоимость топ 10 яндекса
Мясной плов с сухофруктами
Drugs information. What side effects?
cheap zithromax
All information about drug. Get information here.
%%
Feel free to visit my web-site https://redstarpokerrussia.ru/
на срок аренды номера сети для оформления никто другой не сможет им Виртуальный номер (50% анкор, 50% безанкор используя тот url) воспользоваться.
Замечательно, это очень ценная информация
эти конструкции нагревают помещение неторопливо, однако но и тепло сохраняют намного дольше, https://www.panevinomilano.com/2015_03_04_panevino_0064/ чем металлические. невзирая на обилие способов обогрева, доступных для загородного дома, самым популярным остается печное отопление.
ashwagandha powder
Medicament information. Long-Term Effects.
amoxil without dr prescription
All trends of medicine. Read information here.
ventolin hfa
cetirizine brand name
Могу рекомендовать Вам посетить сайт, на котором есть много статей на интересующую Вас тему.
Now, instead of signal to the whole earth about, that you only won, the slot machine https://artecom-event.de/news/zaza_casino_rezension_4.html smoothly and imperceptibly outputs consent to the redemption.
Medicines prescribing information. What side effects can this medication cause?
can i buy cytotec
Everything news about medicines. Read here.
I’ve been surfing online more than three hours as of late,
yet I by no means discovered any fascinating article like yours.
It is pretty worth enough for me. In my opinion, if all website owners and bloggers made just right content material as you probably did, the
web can be a lot more useful than ever before.
pioglitazone 30
7. Примите требования и como sacar na mostbet положения сайта. 8. кликайте на клавишу «зарегистрироваться”, чтобы завершить процесс регистрирования.
I know this if off topic but I’m looking into starting my own weblog and was curious what all is required
to get setup? I’m assuming having a blog like yours would
cost a pretty penny? I’m not very internet smart so I’m not
100% positive. Any tips or advice would be greatly appreciated.
Appreciate it
%%
My web-site :: ceraga-immobilier.com
Pills prescribing information. Cautions.
fosamax
Actual about medicine. Read information here.
%%
My site – http://riccardoantonelli.eu/?p=125
can you get generic prednisone for sale
Drugs information for patients. What side effects can this medication cause?
zithromax
All news about medication. Read information here.
%%
Here is my site – gulsahworld.com
По моему это очень интересная тема. Предлагаю Вам это обсудить здесь или в PM.
Дата обращения: 27 октября 2014. Архивировано 27 https://www.bernardobermudez.com/opera-buffs-inc-fall-showcase-romantic-journey/operabuffspic6/ октября 2014 года. Создано достаточно множество разных программ, которые помогают игрокам при игре онлайн.
Теперь стало всё ясно, большое спасибо за объяснение.
Winning means playing with your head, using your brain activity, taking care of your money, in https://www.fibraclube.com.br/look-out-for-bonuses/ sometimes easier to lose not too large amount funds and see about process than bet crazy money and lose without special training.
I don’t know if it’s just me or if perhaps everyone else encountering problems with your site. It seems like some of the text on your content are running off the screen. Can somebody else please comment and let me know if this is happening to them too? This might be a problem with my browser because I’ve had this happen previously. Many thanks
finasteride warnings
Когда мой любимец заболел, мне срочно понадобились деньги на его лечение. Благодаря yelbox.ru я быстро нашел МФО, предлагающих займы на карту без отказа и сразу же получил нужную сумму.
%%
Also visit my site https://gagdetfrontal.com/
Medicines prescribing information. Generic Name.
zithromax sale
Actual about medicament. Get information now.
I was trying to find a succinct yet detailed summary of the subject, and also this
article provided simply that.
Here is my website … Car insurance
Pills prescribing information. Short-Term Effects.
sildigra
Best trends of drugs. Read information here.
%%
My web blog … https://bystroe-seo.ru/prodvizhenie-saytov-v-google/
Преимущества интерактивного и мультимедийного образования
Free porn videos
Жизнь полна сюрпризов, и когда у меня внезапно сломалась стиральная машина, мне срочно понадобились деньги. На yelbox.ru я нашел множество предложений по займам на карту без отказа. Отличный выбор и условия, в том числе предложения по займам под 0%.
Вы попали в самую точку.
at least additional unpaid spins or more a large bonus on deposit, in an https://bakerscutlery.com/content-e-legal-apostar-no-crash/ you have the opportunity to raise your gaming experience to higher level thanks to paypal.
Drugs information for patients. Drug Class.
clomid generics
Actual about pills. Get information here.
cordarone dose
ремонт частного дома https://remont-chastnogo-doma.ru/
%%
My web-site Moon Princess Spielautomat
effexor uses
This is the best site for Bitcoin Price USD.
Drugs information for patients. Long-Term Effects.
mobic without prescription
Everything what you want to know about meds. Read information now.
This is the kind of material that ought to have to go viral. Thank you for discussing your know-how.
Thank you for the good writeup. It in fact was a amusement account
it. Look advanced to far added agreeable from
you! However, how could we communicate?
Pills information. Cautions.
zithromax
Everything trends of meds. Read now.
can you get cheap cleocin tablets
Поздравляю, ваша мысль просто отличная
Chief Operating Officer Richard Noble said that after analysis of his creativity the current https://marq.uy/2023/06/01/content-player-saccount-was-put-under/ “does not seem commercially viable.”
Drug information for patients. What side effects?
xenical rx
Best trends of drugs. Read here.
%%
My blog; https://nevseoboi.com.ua/2010/07/25/
Он выглядит точно так же, как и оригинал, включая шрифт, https://pic4you.ru/dizajn/skolko-stoit-izgotovlenie-nomernyh-znakov.html размер и цвет букв и цифр.
porn videos (http://www.fodingstrade.com)
проститутки в челябинске
furosemide dosage
Tips clearly used!.
Hello! Someone in my Myspace group shared this website with
us so I came to give it a look. I’m definitely enjoying the
information. I’m book-marking and will be tweeting this to my followers!
Terrific blog and fantastic style and design.
Feel free to surf to my blog post: modern girls & old fashion men
%%
Also visit my web site … russiaplaypokerdom.com
Medicament information. Brand names.
lisinopril
Actual news about pills. Get here.
Awesome content. Thanks.
Meds prescribing information. Long-Term Effects.
effexor
Best what you want to know about meds. Get here.
Я считаю, что Вы допускаете ошибку. Давайте обсудим.
Limousines are the perfect transport for special occasions, because they are elegant, https://ureshino.cup.com/inoshika/company.cgi?sa=U&ved=0ahUKEwj2lty6qbTRAhVH6oMKHd2eCNoQFgg8MAg&usg=AFQjCNFUV2TBvSOXv1iSgT8Wm_gXMMHLYQ are luxurious and give a stylish twist to anyone celebration.
atarax 10mg ohne rezept
order cipro
This is the good site for Bitcoin Price USD.
Medicines information sheet. Drug Class.
paxil
Best news about medicine. Get now.
effexor dosing
%%
Feel free to surf to my web site; Boldenon Undecylenate GP 10ml
Medicine information sheet. Short-Term Effects.
norvasc online
Actual what you want to know about meds. Get information now.
промокод на бесплатную ставку 1хбет
Хорошее дело!
in addition, most in demand, but also rare backup parts kia contained in list of spare parts, so, prolonged is prevented waiting – and delays in finishing of the link.
Pills information leaflet. Effects of Drug Abuse.
can you get pregabalin
Everything what you want to know about drugs. Read information here.
atarax online-apotheke
prednisolone 40mg ohne rezept
Teaching about medication safety should include discussions on the responsible use of antimicrobial medications, emphasizing the critical role in combatting antibiotic resistance. buy dapoxetine no prescription
Free porn videos
fexofenadine online-apotheke kaufen
Drugs prescribing information. Long-Term Effects.
can i order singulair
Some information about drug. Get information now.
Free porn
%%
Take a look at my web page :: https://havalimaniotokiralamaizmir.com/
This is the good d trust site for Bitcoin Price USD.
where to buy generic cleocin prices
Drugs prescribing information. Effects of Drug Abuse.
sildigra medication
Some news about drug. Get information now.
Должен Вам сказать Вы на ложном пути.
It is reported that Moore is element of the Malta-based company em group. Teixeira calls Penin “irresponsible” for publishing videos in https://onerivermedia.com/blog/productlauncher.php?url=%2F%2Fblaze-casino.br.com%2Fblaze-casino-bonus%2F.
%%
Also visit my web page … thebostonjollypirates.com
%%
my homepage кэт казино играть онлайн
Pills prescribing information. Long-Term Effects.
lyrica
Best what you want to know about medication. Get information here.
Hmm it seems like your website ate my first
comment (it was extremely long) so I guess I’ll
just sum it up what I wrote and say, I’m thoroughly enjoying your
blog. I too am an aspiring blog blogger but I’m still new to the whole thing.
Do you have any points for rookie blog writers? I’d
genuinely appreciate it.
Here is my webpage: kalender maret 2024
Pills information for patients. Short-Term Effects.
promethazine generics
Some news about pills. Read information now.
aristocort 4mg online-apotheke
actos price
zoloft 75 mg
Medicament information leaflet. Drug Class.
lyrica without dr prescription
Best information about drug. Read information now.
Medicament information for patients. Generic Name.
zofran
Actual information about medication. Read here.
furosemide diuretic
%%
My web page; bonmarcheadidaspureboost.com
%%
Also visit my blog :: https://economyfund.org.ua/kak-vojti-v-lichnyj-kabinet-slotclub/
Бывают ситуации, когда деньги нужны прямо сейчас, даже если это ночь. В таких случаях я всегда выбираю wikzaim. Портал никогда не подводил – микрозаймы от двух МФО оформляются за минуты, и деньги моментально поступают на счет.
Drug information sheet. Generic Name.
stromectol price
Best news about pills. Get now.
cheap risperdal
purchase prednisone pills
review of buying lisinopril from the healthwarehouse
does gabapentin cause constipation
Medicament information for patients. Generic Name.
flibanserina
Some trends of pills. Read now.
%%
My web page: bellydancephotography.com
promethazine online-apotheke bestellen
%%
my homepage: chabadasia.com
Meds information leaflet. Cautions.
generic trazodone
Some what you want to know about drug. Read here.
finasteride side effects older men
Meds information sheet. Brand names.
provigil without a prescription
Everything what you want to know about medicine. Read information here.
продвижения сайтов в топ 10 google https://bystroe-seo.ru/prodvizhenie-saytov-v-google/
Levitra
EnchagPT Blog to miejsce, gdzie można znaleźć interesujące artykuły i informacje na temat technologii
sztucznej inteligencji. Jest to blog dedykowany wszystkim entuzjastom sztucznej inteligencji, którzy
pragną zgłębiać swoją wiedzę na temat tego fascynującego tematu.
Superb content. Thank you!
ashwagandha dosage
This is best and original site for check Bitcoin Price USD.
Pills prescribing information. Brand names.
norvasc medication
Some trends of drug. Read here.
Запеченные яйца с шпинатом и сыром
Sex-optimistic views challenge this hierarchy by appreciating sexual diversity and rejecting any notion of “typical” intercourse. Feminist arguments against these occupations have a tendency to be launched in the notion that these kinds of function are inherently degrading to gals, perpetuate the sexual objectification of women of all ages, and/or perpetuate male supremacy. For black females, company is seen as contextual due to historic concerns, and can be regarded as a single side of a complex procedure of ideals that encompass black women’s sexuality above time. They contend that the views of anti-sexual intercourse operate feminists are dependent on notions of sexuality produced by the patriarchy to control women’s expressions sexuality. Some liberal feminists believe that a “democratic morality” should really choose sexual action (as if the proclivities of the bulk, as perfectly as their proficiency in supplying sexual pleasures, must determine the path of a society’s moral compass) “by the way companions address one another, the existence or absence of coercion, and the quantity and good quality of the pleasures they deliver”. The rise of the Internet in the late nineties and early 2000s changed the way pornographic movies ended up dispersed, complicating censorship regimes about the environment and authorized prosecutions of “obscenity”. You know, you get on the Internet and you can jump all about the position and look at all diverse things.
Medicines information sheet. Short-Term Effects.
fluoxetine
All what you want to know about medicament. Get information here.
It’s genuinely very difficult in this full of activity life to listen news on Television, thus I
only use internet for that purpose, and take the newest news.
Pills information leaflet. Long-Term Effects.
prednisone
All what you want to know about medicine. Read here.
ashwagandha benefits and side effects
купить бетон
ashwagandha and cortisol
This is best and original site for check Bitcoin Price USD.
order generic cleocin no prescription
เว็บสล็อตWe are
ready to serve all gamblers with a complete range of online casinos that are
easy to play for real money. Find many betting games,
whether popular games such as baccarat, slots, blackjack, roulette and dragon tiger.
Get experience Realistic gambling as if playing at a world-class casino online.
Our website is open for new members 24 hours a day.
Hey! I know this is kind of off topic but I was wondering if you knew
where I could find a captcha plugin for my comment
form? I’m using the same blog platform as yours and I’m having difficulty finding one?
Thanks a lot!
Meds information for patients. Generic Name.
tadacip
All information about medication. Read now.
finasteride medication
Drug prescribing information. Cautions.
where to buy lisinopril
Actual about medicament. Get now.
%%
Have a look at my website … https://notperfect.ru/auto/process-poluchenija-gos-nomera-na-novuju-mashinu.html
ковры на заказ по индивидуальным размерам
buy finasteride online
Meds prescribing information. What side effects?
nexium
All what you want to know about medicine. Read here.
купить бетон
post finasteride syndrome
%%
Also visit my site: https://autospecial.ru/user/morganccsl
Lyrica
Medicines information leaflet. What side effects can this medication cause?
lisinopril medication
Everything information about meds. Get now.
Лечение лейкемии в Германии
buy paxil
Drug information. Brand names.
cordarone prices
Everything about pills. Read information here.
Medicine information sheet. Cautions.
retrovir cost
Everything about medicines. Get information here.
%%
Check out my web site: aubetonlinepoker.com
This is best and trust site for check Bitcoin Price USD.
cetirizine tablet uses in hindi
https://zakznaet.ru/
Drugs information sheet. Drug Class.
can you get zyban
Best news about drugs. Read here.
can you buy lisinopril online
%%
Feel free to surf to my web page: http://bishelp.ru/forum/topics/kak-nayti-nadezhnye-gruzoperevozki-po-gorodu-i-oblasti
Medicament prescribing information. Brand names.
levitra medication
Some news about medicament. Get information here.
%%
my webpage; Buy Health Care Suppliments
ashwagandha benefits
Medicament information for patients. Long-Term Effects.
levitra
Best information about medicines. Read information here.
This is good and trust site for check Bitcoin Price USD.
can you take 20 mg of zyrtec
zyprexa 20mg generic
%%
Also visit my web blog – Вывоз мусора в Ростове-на-дону Батайск Аксай Новочеркасск Азов
Meds prescribing information. What side effects can this medication cause?
neurontin buy
Best what you want to know about pills. Read now.
webcam vibrator
%%
Also visit my page – soccerjerseysretro.com
Drug prescribing information. What side effects can this medication cause?
maxalt medication
Actual trends of drug. Get information here.
%%
Feel free to visit my webpage … https://sportnb.info/user/ossidykoel
Medicament information leaflet. Short-Term Effects.
generic abilify
Some trends of drug. Read here.
ashwagandha uses
You actually expressed it effectively!
Это тебе наука.
Yasin A.A., https://in2multimedia.co.za/hello-world/ Saad F. (March 2007). “Improvement of sexual life in all representatives of the stronger sex with late manifestation of hypogonadism, who received only testosterone.”
celebrex 200 mg purchase
%%
My page https://baltimorepropainting.com/
Pills information leaflet. Short-Term Effects.
synthroid brand name
Some news about meds. Read here.
ribavirin online-apotheke billig
Free Porn
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
Medicines information leaflet. Generic Name.
cost neurontin
All news about medicament. Read information now.
%%
Feel free to surf to my site: joker casino отзывы
casino slots games
Thanks, nice content!
Porn fucked
Fucking
Drugs information leaflet. What side effects?
zofran prices
All trends of medicament. Read now.
%%
My homepage: https://tourism.unoforum.pro/?1-18-0-00000693-000-0-0
http://freefoolballtips.ru/
fexofenadine billig bestellen
Fantastic blog! Do you have any tips and
hints for aspiring writers? I’m hoping to start my
own blog soon but I’m a little lost on everything.
Would you propose starting with a free platform like WordPress or go for
a paid option? There are so many choices out there that
I’m totally overwhelmed .. Any ideas? Bless you!
prednisolone 40mg bestellen
Whoa loads of terrific facts!
ventolin hfa inhaler
Решил, что мой Opel больше не вызывает те же эмоции. Через друзей узнал про skupkavto.ru. Сервис супер: оценили машину по нормальной цене, деньги сразу дали, все оформили. Моя машина нашла нового хозяина!
днк бизнеса отзывы сотрудников
Срочно нужно было продать машину. Мой Mercedes уже не вызывала тех эмоций, что раньше. Нашел сайт skupkavto.ru через Google. Оценили авто быстро, дали деньги и увезли мою старую добрую машину.
Скромнее нужно быть
все обои тщательно сортируются и https://www.flyzy2005.com/go/go.php?url=economyfund.org.ua%2Fkak-popolnit-rox-cherez-telefon%2F проверяются. залить заставку на ноутбук бесплатно. высококачественные hd-изображения для любого размера экрана.
Watch the private life of other people live. Real life cam sex voyeur videos for free
Drugs prescribing information. Generic Name.
stromectol
Everything news about medicament. Get information now.
тупое
select your young lady, and time issue in the more, to start shopping! we have simplified ordering parts you need for personal hyundai.
Flirt finder is the flirt finder for active singles seeking fun.
The online platform allows you to find interesting individuals anytime, anywhere.
Become a part of our flirt finder today and begin your journey to finding love with Adult Flirt Finder.
%%
My site https://kreditgroup.ru/kredity-pod-zalog-nedvizhimosti/kredit-pod-zalog-komnaty
isosorbide mononitrate 20mg ohne rezept
symmetrel 100mg bestellen
%%
my web site: https://pokerkingproplayrussia.ru/
%%
Check out my webpage … https://www.0552.ua/news/3662082/godinnik-vostok-iz-srsr-kupujte-legendu
%%
Check out my web site; Money Train 3 Slot
мануальный терапевт Мытищи
%%
Stop by my blog post :: https://alpagassologne.com/
Medicines prescribing information. Drug Class.
zithromax
Actual trends of medicines. Read information now.
Croak review commission the updated opine in place of ‘YouTubeMoa’ ? emoji free.
Ever felt overwhelmed by the sheer sum total of peace online?
‘YouTubeMoa’ caught my lustfulness recently, and wow, it’s impressive.
They’re using a standout algorithm that fetches the top-trending components every tom’s talking about.
But that’s not the pre-eminent bit.
They’ve organized all the gratify using targeted keywords, ensuring as browsing.
If you have an keenness in the interest of the most desirable pleased gone away from there, ‘YouTubeMoa’ is something you shouldn’t miss.
Bookmarking it for the nonce to go to my quotidian digital portion!
Best hotel rixos nakheel.
prednisone prices
%%
Also visit my blog joewaldschmidt1980.com
Hey! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing
very good success. If you know of any please share. Kudos!
%%
my web blog: https://dbsolutionsltd.com/
flonase nasal spray coupon
Medication information for patients. Generic Name.
zofran
Actual trends of drugs. Read information now.
%%
my homepage: https://jobsmart24.com/
prednisolone 5mg bestellen
Medicament information for patients. Drug Class.
nolvadex
Everything what you want to know about medication. Get information now.
НЕТ ПАЦАНЫ ТАК НЕЛЬЗЯ!
Печь может иметь опыт работы в 2-х режимах. стоит принимать во внимание площадь, https://davenantpress.co.uk/product/essays-on-political-theory/ на которую рассчитана дровяная печь.
купить иранский ковер в интернет магазине
rebetol ohne rezept bestellen
It’s the best time to make some plans for the future and it’s time to be happy.
I have read this post and if I could I want to suggest you few interesting
things or advice. Maybe you can write next articles referring to this article.
I wish to read more things about it!
Drug information sheet. Short-Term Effects.
lasix buy
Some what you want to know about drug. Read information here.
%%
my website yoyojiasu.com
doxycycline where can i buy
valacyclovir online bestellen
https://harmonica.ru/v-yanvare-2012g-v-g-karagande-kazahstan-proshyol-ocherednoj-ezhegodny-j-blyuzovy-j-festival
ribavirin ohne rezept billig
Drug information for patients. Effects of Drug Abuse.
zyban prices
Best what you want to know about drug. Read now.
Best site for checking Bitcoin Price USD.
Medicines prescribing information. Effects of Drug Abuse.
ampicillin
All about drugs. Read now.
%%
My web blog – jung-gestalten.com
временная прописка в спб https://registracia-vremennaya-spb.ru/
https://footballskandaliero.ru/
Medicament information leaflet. Brand names.
maxalt
Actual trends of medicine. Read information here.
Pills prescribing information. Short-Term Effects.
fluoxetine without a prescription
Best information about medicament. Read now.
%%
My web-site – http://www.diamoo.com/2010/09/10/post-format-gallery/100_5478/
578426 642908How much of an unique article, keep on posting better half 719002
claritin online
buy lisinopril online uk
https://kanoner.com/2019/12/26/164850/
risperdal coupon
Yes! Finally someone writes about sbobet.
free fucked
Medicines prescribing information. Effects of Drug Abuse.
rx zithromax
All news about meds. Get here.
%%
Feel free to visit my web-site :: Big Bass Splash
Meds prescribing information. Drug Class.
baclofen sale
Actual news about drugs. Read now.
Yazar Haber – Haberler, Son Dakika, Gündem, Güncel Haberler
http://www.dogswar.ru/artilleriia/zenitnye-kompleksy.html
Medicine information leaflet. Cautions.
prozac otc
Actual news about pills. Read information here.
%%
My webpage … Plinko Oyun Incelemesi
effexor venlafaxine
Drugs prescribing information. Short-Term Effects.
clomid rx
All news about medicine. Get information now.
how to get different knives in csgo without a skin
временная регистрация в москве https://registracia-v-moskve.ru/
Pills information sheet. What side effects can this medication cause?
valtrex
All information about pills. Get now.
Medication information leaflet. Long-Term Effects.
levaquin
All information about drug. Read information here.
where can i buy doxycycline hyclate
Quality posts is the important to interest the visitors to go
to see the website, that’s what this web site is providing.
Medicine information sheet. What side effects?
lyrica without a prescription
Best news about drug. Read here.
Medicines information. What side effects can this medication cause?
cost tadacip
All about drug. Get here.
Drugs information. Cautions.
buy generic propecia
All what you want to know about medication. Get information here.
сколько стоит жилье на кипре https://agentstvo-nedvizhimosti-kipr.ru/
ashwagandha kaufen
Medicament prescribing information. Long-Term Effects.
pregabalin
Everything about medicines. Read here.
brillx casino
https://brillx-kazino.com
Играя на Brillx Казино, вы можете быть уверены в честности и безопасности своих данных. Мы используем передовые технологии для защиты информации наших игроков, так что вы можете сосредоточиться исключительно на игре и наслаждаться процессом без каких-либо сомнений или опасений.Добро пожаловать в увлекательный мир азарта и развлечений на официальном сайте Brillx Казино! Если вы ищете захватывающий опыт игры в игровые аппараты, то ваш поиск завершен. Brillx Казино – это не просто блистательный выбор игр, это настоящее путешествие в мир азарта и возможностей.
ทดลอง เล่น pg slot เกมทดสอบเล่นชั้นในหนึ่ง ทั่วทั้งโลกต่างก็มีชื่อเสียงกัน เนื่องจากตัวเกมถูกออกมามีมาตรฐาน รวมทั้งนำสมัย pg slot ไม่เหมือนกับเกมสล็อตที่ผ่านๆมาในค่ายพีจี
pg slot 168 This website must be said to be a website that has many games from different camps. pg slot for you to choose to gamble on. It is necessary to say that this website is a quality gaming website.
Drugs information leaflet. Effects of Drug Abuse.
valtrex
All about medicine. Read information now.
Sign up for Flirt Finder Dating Site and explore the digital romance.
ivermectin stromectol. Stromectol is employed in mass drug administration programs, where large populations at risk of parasitic infections receive a single dose, helping reduce the prevalence of these diseases on a community-wide scale.
effexor usa
F*ckin’ tremendous issues here. I’m very happy to peer your post.
Thank you so much and i am looking ahead to contact you.
Will you kindly drop me a e-mail?
Here is my page chrysler fifth avenue
cefixime billig bestellen
Medicament information. Drug Class.
finpecia online
Some information about meds. Read now.
rebetol generika billig
https://darkside.ru/interviews/751/
zovirax 200mg bestellen
actos generic
finasteride topical
купить временную регистрацию в москве https://registracia-v-msk.ru/
Pills prescribing information. Brand names.
glucophage medication
All news about meds. Get here.
free fucked
doxycycline without an rx
Medicine information for patients. Short-Term Effects.
ampicillin for sale
Best what you want to know about meds. Read information now.
buy donepezil 10 mg
tinidazole ohne rezept bestellen
prednisolone 10mg kaufen
Drugs prescribing information. Generic Name.
prednisone brand name
Best trends of medicine. Get information now.
clindamycin 150mg online
Nice replies in return of this matter with firm arguments and explaining
all on the topic of that.
Cinecom NG Отзывы
gabapentin for anxiety dose
glimepiride medication
minocin 100mg billig
Meds information leaflet. Short-Term Effects.
flibanserina for sale
Everything information about medicines. Read information now.
atarax billig kaufen
3d печать в москве https://3d-pechat-moskwa.ru/
chloramphenicol 250mg kaufen
Drug information for patients. Drug Class.
singulair
All trends of drug. Get information here.
Medicament information. Brand names.
zofran
Actual trends of medicines. Get here.
furosemide 50 mg for dogs
Thanks for sharing your thoughts. I truly appreciate your efforts
and I will be waiting for your next post thanks once again.
Meds information. Short-Term Effects.
cephalexin
Some what you want to know about medication. Read information here.
fexofenadine united kingdom
aristocort
Drugs information leaflet. Drug Class.
nolvadex medication
Some news about drug. Read information now.
atarax 10mg
copegus online bestellen
купить этикетки самоклеящиеся https://etiketki-samokleyashiesya.ru/
Pills information leaflet. Brand names.
cheap sildigra
Best what you want to know about medication. Get now.
Заказать дубликаты номерных знаков
Дубликат номера
Porn 2020
ashwagandha testosterone
Before buying dapoxetine, it is important to consult with a healthcare professional to determine if it is the right treatment option for you. buy viagra with priligy online.
автосервис шкода в москве
%%
Feel free to surf to my blog post :: https://www.diigo.com/item/note/9br1u/mnxg?k=00968550a25a31c509e5107beed74884
Изготовление номерных знаков на авто
Дубликат номера
The affordability of Stromectol has made it a lifeline for resource-limited healthcare systems, helping them deliver effective treatments to their populations. where can i buy stromectol ivermectin.
Medicine information. Drug Class.
get lyrica
Actual trends of pills. Read information now.
Sev Vivos Отзывы
It is not my first time to visit this website, i am visiting this web page dailly and obtain fastidious information from here all the time.
https://www.masturbaza.com/
Вскрытие дверного замка newzamok.ru
Когда Вам поспешно нужно открыть свою дверь или поломанный замок, звоните по контактному телефону +7(903)174-11-18 или оформите заявку на нашем веб портале. Сколько разных ситуаций может произойти, все не перечесть. Потеряли ключи, поломался замок, заклинило дверь – по всем этим вопросам как раз мы и специализируемся. Наша организация Новый Замок уже большое количество лет трудится в этой сфере по Москве и имеет колоссальный опыт, команду настоящих специалистов, налаженный режим и при этом адекватные цены. Смотрите все обстоятельства на нашем онлайн портале newzamok.ru и сохраните наш номер.
Если Вы хотели найти вскрытие замка в сети интернет, то скорее идите на наш веб ресурс newzamok.ru сейчас. Вся важная для Вас информация же выложена и ждет своего часа, когда Вы наберете для вызова специалиста. А таких ситуаций бывает очень много и очень нередко.
Наверно, каждый третий из нас попадал в такую мини беду. Наши клиенты часто звонят по подобным запросам: вышел гулять с собакой, оставил дома ключи. Оставила ключи в другой сумочке и дверь захлопнула, нередко говорят нам девушки. Ребенок играл и провернул ключ так, что часть осталась в скважине. Всякое может быть, но отлично, что есть мы-те, кто решат Ваши дверные задачи.
Звоните по любому вопросу, связанному с дверьми, также вскрытие замка и другими. Работаем круглосуточно и без выходных. Ведь кто скажет, в котором часу произойдет Ваша неприятность. Наш адрес: г. Москва, ул. Авиамоторная, д. 50, стр.1.
Также мы можем заменить любой замок на новый по совершенно любой причине. Работаем с любыми видами замков и стран-производителей. Наши работники постоянно учатся новым технологиям, работают максимально аккуратно, не повредив ничего рядом. Вызов специалиста происходит максимально быстро, от 20 минут, а цена приемлемая для всех, начинается с 500 рублей. Так что можете не переживать и довериться нам на все 100.
Medication prescribing information. Cautions.
viagra tablets
All news about medication. Get information now.
Medicines information. Cautions.
how can i get propecia
Best what you want to know about drugs. Get here.
amiodarone (active ingredient in cordarone)
Вскрытие дверного замка newzamok.ru
В ситуации, когда Вам экстренно необходимо открыть свою дверь или сломавшийся замок, позвоните по номеру телефона +7(903)174-11-18 или оформите заявку на нашем интернет портале. Сколько различных ситуаций может произойти, все не перечесть. Сломали ключи, сломался замок, заклинило дверь – по всем этим вопросам как раз мы и концентрируемся. Наша организация Новый Замок уже большое количество лет трудится в представленной области по Москве и имеет превосходных опыт, команду настоящих специалистов, налаженный режим и при этом адекватные цены. Смотрите все мелочи на нашем онлайн ресурсе newzamok.ru и сохраните наш номер.
Если Вы хотели найти служба аварийного в сети интернет, то быстрее идите на указанный онлайн портал newzamok.ru сейчас. Вся интересная для Вас информация же размещена и ждет своего времени, когда Вы позвоните для вызова мастера. А таких ситуаций бывает очень много и очень нередко.
Наверно, каждый третий из нас попадал в такую мини беду. Наши заказчики часто звонят по таким вопросам: пошел гулять с собакой, забыл дома ключи. Забыла ключи в предыдущей сумочке и дверь закрылась, нередко говорят нам женщины. Ребенок играл и оставил ключ так, что половина осталась в скважине. Всякое может быть, но хорошо, что есть мы-те, кто разрешат Ваши дверные проблемы.
Звоните по совершенно любому вопросу, связанному с замком, также вскрытие замков в москве и другими. Работаем круглосуточно и без выходных. Ведь кто скажет, в котором часу произойдет Ваша неприятность. Мы находимся по адресу: г. Москва, ул. Авиамоторная, д. 50, стр.1.
Также мы можем заменить любой замок на новый по совершенно любой причине. Работаем со всякими брендами замков и стран-производителей. Наши работники регулярно учатся новым технологиям, работают максимально аккуратно, не повредив ничего вокруг. Вызов специалиста осуществляется очень быстро, от 20 минут, а стоимость приемлемая для всех, начинается с 500 рублей. Так что можете быть уверенными в нашей работе на все 100.
%%
Review my homepage … http://wiki.quanticsystems.com.br/index.php/Balkan_pharmaceuticals_turanabol
Protonix user experiences
You get what you spend for, although, and in a lot of instances we sense the articles on LiveJasmin is worth numerous times what you will invest on it. Whether it is the very best free cam site, most effective top quality cams, or best cam web-site to do the job for, you’ll find the best picks below. You can pay out for a private chat, but individuals are reasonably highly-priced, and there’s minor cause to do so when you can get considerably of the exact stuff for free of charge. For buyers, they get to join with reside sexual intercourse performers and get off in a a great deal more enjoyable and interactive way. While it is possible to stream reside intercourse exhibits, most men and women just release pre-recorded content material to their subscribers on a regular foundation. As a end result, cam women have comprehensive regulate over the content they release. On August 22, 2002, the demonstrate was suspended pursuing its 3rd once-a-year Sex for Sam contest held on August fifteen that inspired listeners to have intercourse in risky areas for prizes when a witness claimed from the spot. This makes it possible for for an incredibly individual encounter, and it’s about as shut as you can appear to actually obtaining sex with them with no leaving your property. It’s what’s regarded as a “freemium” cam woman internet site – meaning, there’s a lot of things you can do for absolutely free, but you will have to shell out for the actually fantastic bits.
Medicines information sheet. What side effects can this medication cause?
cordarone
Everything trends of medicines. Read information now.
%%
Take a look at my blog post p6633
%%
Feel free to visit my web page :: חשפנות
Medicine information. Generic Name.
cheap glucophage
Best news about medicines. Get here.
We stumbled over here from a different web page and thought I
may as well check things out. I like what I see so now i am following you.
Look forward to looking into your web page yet again.
You expressed it very well!
sands999 พรีเซนต์เกมคาสิโนออนไลน์ที่นานาประการตัวอย่าง pg slot ที่คัดสรรมาอย่างยอดเยี่ยมจากบริษัทผู้ผลิตซอฟต์แวร์แถวหน้าของโลก ทุกเกมมาพร้อมอัตราการคว้าผลตอบแทนที่ดีสุดๆ
Medicines information for patients. Drug Class.
nolvadex price
Best what you want to know about medicines. Read information here.
65bet รับประกันความยั่งยืนมั่นคง pg slot ไม่มีอันตรายเว็บไซต์คาสิโนลำดับหนึ่งที่ยอดเยี่ยมบนโทรศัพท์มระบบออโต้ไม่สลับซับซ้อน คณะทำงานรอเสนอแนะตลอดโดยผู้เล่นสามารถสนุกกับเกม
%%
Also visit my web site :: 19574
doxycycline buy online
Regards! Great information!
%%
my web blog :: https://themarshallgroup100.net/about/articls/index.html%D1%81
http://www.autoworld.com.my/images/pgs/?glossariy_avtomobilista_slovary_avtomobilynye_terminy.html
Valuable posts Cheers!
https://okon-remontov.ru/
Evall Vellc Отзывы
lamotrigine medication
darkmarket dark web market darknet drug store
%%
Feel free to visit my web blog … p992
https://www.narip.com/news/vek_adalin_2015_opisanie.html
%%
My website – http://forum.osvita.od.ua/viewtopic.php?f=2&t=9530
? ????????? ? ??????? ?????? ???? ????, ?? ?????? ?? ?? ??? ?? ??????????? ??? ?????, https://prophairstudio.com/hello-world/ ?? ?????????? ??????? ????? ??????????? ?????????? ? ?????????????.
valacyclovir billig
But researchers at Oxford University located that delighted workers are 13%
more productive.
вендинговый автомат купить
https://www.maafushidive.com/search?type=article%2Cpage%2Cproduct&q=www.RxLara.com+-+Buy+Priligy+60mg+Online.+Dapoxetine+30mg+OTC+for+premature+ejaculation.+Pharmacy+Here+-+www.rxlara.com dapoxetine priligy. Behavioral therapy involves techniques such as the stop-start method and the squeeze technique, which aim to delay ejaculation through controlling arousal levels..
donepezil 5mg
Thank you for helping out, wonderful info.
my blog post tow truck oakland
ashwagandha supplements
I always was concerned in this subject and still am, appreciate it
for putting up.
Look at my webpage scrap a car
https://uec.asia/
We provide re-engineering services for parts, spare parts, and filtration systems, as well as water purification equipment, gaskets, and seals for the oil and gas, chemical, and energy industries. Our approach to working with clients always combines our expertise and technical efficiency.
Drugs information for patients. Effects of Drug Abuse.
cialis super active without insurance
Actual information about drug. Get now.
porn 47186 video
effexor billig
Medicament information. Long-Term Effects.
buy generic zithromax
Everything news about medicines. Read information here.
quetiapine online-apotheke billig
cialis soft tabs tablet
%%
Also visit my blog: https://sila-sveta.ru/cgi/pgs/?kupit_diplom_sssr_1.html
%%
Feel free to surf to my page – remontbp.com.ua
cordarone prescribing information
Пари можно заключать на основном сайте, при помощи веб-заказчик для винды, https://coopsanclemente.com/df480-neve-home/neve-ultimate-perfection-1/ а помимо этого в приложениях для android и ios.
%%
Here is my homepage; http://goldmd.ru/html/3_2_13.htm
Superb material Thanks.
This is nicely put. .
This is so we will management a gentle move of customers to our Recycling Centre. To control the Kindle Fire’s volume, you’ve got to make use of an on-screen control. Microsoft Pocket Pc units use ActiveSync and Palm OS units use HotSync synchronization software. Many gamers want to obtain software program to their own device, for ease of use and speedy accessibility. The particular software you choose comes right down to personal desire and the working system on your DVR computer. All newer fashions of non-public watercraft have a pin or key that inserts right into a slot near the ignition. Please notice that you may solely ebook one slot at a time and inside 14 days prematurely. You possibly can play games about historical Egypt, superheroes, music, or a branded Hollywood game. By manipulating these variables, a vertex shader creates life like animation and special results reminiscent of “morphing.” To learn extra about vertex shaders, see What are Gouraud shading and texture mapping in 3-D video video games? All it takes is a fast look on eBay to see ATMs on the market that anyone could buy. You will notice that we separate objects out by classes and every has its own place at the Recycling Centre.
Feel free to visit my blog post: https://slothydra.com/
Drug information sheet. Short-Term Effects.
lisinopril otc
Actual what you want to know about drug. Get now.
https://uec.asia/
Our company specializes in providing re-engineering solutions for parts and spare parts, as well as offering filtration systems, water purification systems, gaskets, seals, and equipment for industries such as oil and gas, chemical, and energy. We always strive to combine our extensive capabilities with exceptional technical efficiency when working with our clients.
%%
my homepage :: http://www.sportpro.com.ua/forum/viewtopic.php?p=198464
купить диплом о высшем москва https://diplomi-rf.ru/
All that mentioned, hopefully having a several of the previously mentioned factors into consideration will assistance you in making a final determination. In Season 8, Neil begins to see Debbie is using gain of him for her possess gratification and attempts many items to alter that but almost nothing is effective. Giani Leon as The Kid – A mute, BMX-using staff who starts to perform for Pauly halfway by way of year 7. He is shown to be a excellent pizza deliverer, generally disappearing from view promptly just after handing the shoppers their pizzas. Later in Season 3, Hymie’s paternal grandmother shows up and usually takes the infant. However, not all of the products below have Hd abilities, so you’re continue to likely to uncover the occasional pixelated dwell displays. In pressure right here are the regular RTS conventions: you can attract a box all over your models to pick out them you can assign team quantities to models with the command critical you can assault-move to an region, protecting against enemies from ambushing you on your way someplace. Here we are at the login monitor.
Medicines information leaflet. What side effects?
kamagra tablet
All information about medicines. Get here.
https://canvas.ubc.ca/eportfolios/48572/Home/YouTube_Growth_Made_Easy_Exploring_the_Benefits_of_YouTubeBoosterSpace
https://www.host4cams.com/
Drug prescribing information. Effects of Drug Abuse.
propecia pills
Some information about medicine. Read now.
These are actually wonderful ideas in about blogging.
You have touched some nice things here. Any way keep up wrinting.
%%
Here is my webpage :: https://art-lazer.com.ua/lazernaya-epilyaciya/grudi
prednisone capsules
While it inherits the vast majority of iChat’s options, Messages also brings help for iMessage, Apple’s messaging service for iOS, in addition to FaceTime integration. Messages (Apple) is an prompt messaging software program software developed by Apple Inc. for its macOS, iOS, iPadOS, and watchOS operating techniques. Its mobile apps can be found on iOS, and Android in multiple languages. Users can create a number of connections to the same service, and can even group connections underneath separate identities to stop confusion. Trillian connects to multiple prompt messaging companies with out the necessity of operating a number of purchasers. Messages was introduced for OS X as a beta application on February 16, 2012 for Macs working Mac OS X 10.7 “Lion”. Messages received a significant redesign in OS X Yosemite, following the flat design aesthetic launched in iOS 7. As part of the brand new Continuity feature, customers can ship and obtain SMS and MMS messages by means of paired iPhones running iOS 8 or later.
The impact of ED on sexual frequency and duration can create discrepancies in sexual desires and needs between partners, potentially causing further strain in the relationship. dapoxetine tablets 60 mg in usa.
where to buy cheap sildigra without a prescription
Aptalca Sözler
loratadine kosten
справка https://spravki-s-dostavkoy.ru/
ashwagandha benefits and side effects
%%
Here is my blog post 18058
Meds information for patients. Brand names.
zoloft medication
All about drug. Read now.
how to buy atarax
%%
My webpage … https://alexeygolev.ru/
Ща посмотрим
материалы создаются с учетом особенностей человеческого организма, и придают поддержку позвоночника в качественном положении, https://shellychan08.com/2020/06/12/%e6%af%8e%e9%80%b1%e6%9c%80%e4%bd%8e2%e4%b8%87%e5%86%86%e7%a8%bc%e3%81%92%e3%82%8b%ef%bc%9f%e5%b7%9d%e8%b6%8a%e7%b4%97%e6%a0%84%e5%ad%90%e3%80%80%e3%81%97%e3%81%82%e3%82%8f%e3%81%9blife2020%e3%81%af/ что может позволить предотвратить болезненности в спине и шее.
nitrofurantoin monohydrate coupon
Regards! Quite a lot of content!
get levaquin
Medication prescribing information. Generic Name.
tadacip
All news about medication. Read information here.
жесть
The Italian casino casino di campione, located not far from Lugano, remains the largest http://www.il-machinery.com/redir/https://www.pearltrees.com/hynba/item546958049 in Europe.
%%
My web site :: https://art-lazer.com.ua/lazernaya-epilyaciya/nogi
Drugs information leaflet. Short-Term Effects.
baclofen rx
Everything trends of meds. Get here.
After I originally left a comment I appear to have clicked the -Notify me when new comments are added- checkbox and now whenever a comment is added I receive 4 emails
with the exact same comment. Is there a means you can remove me from that service?
Thanks a lot!
%%
Also visit my site; proplayggpokerag.com
non prescription medicine pharmacy online pharmacy fincar panadol pharmacy
%%
Feel free to surf to my webpage :: https://InstantPhotoWorks.com/
doxycycline prescription
%%
My homepage – חשפנית בצפון
https://tsucompany.uz/
Компания Turan предлагает надежное партнерство в области промышленного оборудования для энергетики, нефти и газа! Мы гарантируем качество и надежность, сотрудничая только с проверенными мировыми производителями, чтобы предоставить вам самое лучшее оборудование, способное справиться с самыми сложными задачами. Наш ассортимент включает широкий выбор оборудования, начиная от трансформаторов и генераторов, заканчивая компрессорами и насосами. У нас есть решения для всех ваших потребностей в энергетике, нефти и газе. Кроме того, мы предоставляем высококачественное сервисное обслуживание, помогая с установкой, наладкой и технической поддержкой в любое время. Наш международный опыт в поставках оборудования и обслуживании позволяет нам успешно решать задачи клиентов в разных странах. Мы также следим за инновациями в отрасли, чтобы предложить вам наилучшие решения для увеличения эффективности и снижения затрат. Выбирая Turan, вы выбираете надежного партнера, готового помочь вам успешно развивать свой бизнес в области энергетики, нефти и газа. Мы гарантируем качество, надежность и профессионализм. Не упустите возможность сделать ваше предприятие более эффективным и конкурентоспособным с Turan!
astelin kaufen
Medicament prescribing information. Long-Term Effects.
pregabalin
Some what you want to know about meds. Read information here.
Тепловые насосы воздух-вода в климатических условиях с холодными зимами: https://wikipotolok.com/teplovye-nasosy-vozduh-voda-v-klimaticheskih-usloviyah-s-holodnymi-zimami-rabota-i-optimizatsiya/ работа и оптимизация.
Я считаю, что это очень интересная тема. Предлагаю всем активнее принять участие в обсуждении.
Точный счет. в этом случае беттер прогнозирует исход матча с https://smpn3-jiken.sch.id/forum/ точностью до гола. Вирт.спорт. в этом разделе реально заключить пари на киберспорт.
The main task of such publications is to motivate 1xbet registration promo code 2024 users to register in the office as soon as possible.
The main task of such publications is to motivate promo code in 1xbet users to register in the office as soon as possible.
A private dance of this kind has long since become an חשפניות נתניה indispensable feature of any good party.
При выборе подходящей модели теплового насоса воздух-вода для дома https://msd.com.ua/teplovye-nasosy/sravnenie-razlichnyx-modelej-teplovyx-nasosov-vozdux-voda-kak-vybrat-podxodyashhij-dlya-vashego-doma/ необходимо учитывать ряд ключевых факторов.
Medication information for patients. Generic Name.
retrovir
Best trends of pills. Get information here.
The case history you have actually consisted of include
a great deal value to the post. It’s a splendid mix
of concept as well as sensible insights.
Check out my web-site: coverage rates
one x bet promo code
order aurogra
Meds information sheet. Long-Term Effects.
pregabalin
Some about meds. Get information now.
porn 47186 video
справка 086 для поступления в вуз https://spravki-086u.ru/
На официальном сайте интернет-магазина представлен широкий ассортимент алкогольной продукции алкоголь с доставкой на дом москва купить принимаем запросы вне зависимости времени.
На официальном сайте интернет-магазина представлен широкий ассортимент алкогольной продукции купить алкоголь с доставкой москва принимаем запросы вне зависимости времени.
buy generic prednisone
%%
Feel free to visit my homepage; australiapokerwtpglobal.com
Чтобы правильно произвести раздел имущества необходимо обратиться в компанию Зайцев и партнеры раздел имущества разводах оказывает профессиональные юридические услуги для людей и организаций.
Чтобы правильно произвести раздел имущества необходимо обратиться в компанию Зайцев и партнеры раздел имущества оказывает профессиональные юридические услуги для людей и организаций.
https://vc.ru/u/1895184-timur-bektimirov/868943-pochemu-tak-cenyatsya-monety-s-brakom
In the recent annals of tattooing, a seismic transformation has unfurled its wings https://crowhunting.activeboard.com/t69886998/the-artistry-of-fine-line-tattoos-a-look-into-calgarys-top-a/ propelling the industry into the uncharted territory of finesse.
Fine line tattoos are a spirited departure from the robust and chromatic paradigm https://www.addonface.com/forums/thread/2433/ that have long been tethered to the art of tattooing.
You can order in the area: strippers in Bat Yam חשפניות נתניה Unbeatable prices!
You can order a stripper to your home, to the hotel or to any other location you choose throughout the country חשפניות נתניה in the north, south, center.
ashwagandha powder benefits
lisinopril 10 mg buy no prescription
I always used to study article in news papers but now
as I am a user of net so from now I am using net for content, thanks to web.
Here is my website … สล็อตpg
The beauty and grace of the female body have been appreciated since ancient times חשפניות ראשון לציון smooth dance movements.
imipramine kosten
plaquenil 200 mg over the counter
Конечно. Я согласен со всем выше сказанным.
When I originally commented I seem to have clicked on the -Notify
me when new comments are added- checkbox and now every time
a comment is added I receive 4 emails with the same comment.
There has to be a way you are able to remove me from that service?
Kudos!
where can i get levaquin prices
Drug information leaflet. What side effects?
zoloft
Best about pills. Get information here.
%%
my page :: pokerokrussia.ru
lisinopril 10 mg tablet buy online
%%
my web site :: חשפנית בצפון
farxiga
I read this article fully on the topic of the comparison of
latest and preceding technologies, it’s amazing article.
Medicines information leaflet. Generic Name.
cialis rx
Actual information about meds. Read information here.
l albuterol
%%
Feel free to surf to my site https://www.bananot.net/north-strippers
anastrozole 1 mg without prescription
buy lisinopril from india without prescription
%%
My web blog – dasmudwig.com
%%
my blog חשפנית בצפון
cefixime contraindications
Medicament information for patients. Brand names.
zoloft medication
Some what you want to know about pills. Read now.
Яндекс подсказал мне отличный сайт caso-slots.com, когда я искал казино на деньги. Тут есть все для удачной игры: различные казино с игровыми автоматами, бонусы на депозит и статьи с советами по игре. Теперь я знаю, как увеличить свои шансы на победу!
Only wanna comment that you have a very decent internet site, I enjoy the
style it actually stands out.
Take a look at my website … camry rims
Клава Мастер
%%
Have a look at my web blog :: ruproplaypokerdom.ru
buying lisinopril
%%
my web blog http://wiki.duskworld.ru/index.php?title=ANSWERS_GAMES
On our website you can book Rishon Lezion strippers for a bachelor party חשפנית בראשון לציון and in all places in the country.
справка о побоях как получить https://spravki-o-poboyah.ru/
We offer a warm, interesting and very spicy service in Rishon LeZion: חשפנית בראשון לציון booking strippers Inviting our artists girls will paint every party in new color.
You won’t get bored of them, and the intensity of the חשפניות ראשון לציון celebration will soar very high!
I am glad to be one of several visitors on this great web site (:, thanks for
putting up.
Here is my web blog – used yamaha r6
You won’t get bored of them, and the intensity of the חשפנית בראשון לציון celebration will soar very high!
бетон мытищи
lipitor pharmacy price online pharmacy quick delivery publix pharmacy tramadol
knock and I could let you out, you know.” He looked
Medicament information leaflet. Drug Class.
lyrica
Everything trends of medicines. Read here.
Друзья, хочу поделиться! Открыл для себя мир онлайн казино благодаря сайту caso-slots.com. Здесь я нашел все популярные казино и список тех, где предлагают бонусы на первый депозит. Азарт начинается прямо сейчас!
welcom bonus 1xbet promo code somalia
%%
Feel free to visit my homepage: стоматологическая клиника
how late it is!” then it was out of sight. She found
уборка квартиры после дезинсекции
Hi there to every body, it’s my first visit of this weblog; this
website consists of amazing and actually good material for visitors.
flagyl cost
directly3] over his head, in the spreading
buying lisinopril in los algodones
Force steam, penetrating the layers of paper, חשפניות ראשון לציון removing the covering and residue.
%%
Feel free to surf to my web site … http://promotors.lv/user/gierreqqua
Force steam, penetrating the layers of paper, חשפנית בראשון לציון removing the covering and residue.
%%
Also visit my web blog … https://proplayredstarpoker.ru/
This is a best luxury and sophistication Naya District One nestled in the heart of Dubai.
%%
Feel free to visit my web site berhamdesigns.com
energy storage systems
Основным направлением работы отделения является восстановительно-реконструктивно-пластические операции в области головы – шеи http://neuro-med.ru/partners.htm
https://dez-serv.ru/
https://www.party.biz/forums/topic/714684/calgary-s-fine-line-tattoo-scene-a-rising-trend-in-body-art/view/post_id/1584300
You can buy here Pablo Snus for best price.
Я — ремонт, компания по ремонту квартир в Москве yaremont.ru
После приобретения новенькой квартиры сразу встает вопрос ремонта. И некоторых он очень смущает, ведь историй о некачественной отделке, о невнимательных специалистах и нечистых фирмах очень много. Наверно, каждый встречался с плохим сервисом в сфере услуг. Предлагаем Вашему вниманию надежную компанию Яремонт, которая занимается любой трудности ремонтом в Москве и области. Заходите на сайт yaremont.ru и оформляйте заявку на бесплатный вызов мастера.
Заказать квартир под ключ можно у нас уже сейчас. Мы рады предложить большой список услуг по небольшим ценам и за малые сроки. Убедитесь в этом самостоятельно, посмотрев наш прейскурант цен. Гарантия 3 года на все отделочные работы. Если вдруг после ремонта что-либо пошло нитак, мы в самые быстрые сроки готовы устранить все неполадки. Регулярно проводятся акции и делаются скидки для наших любимых заказчиков. Оформляем официальный договор на все услуги, а также смету в день оценки помещения.
В нашей компании работают только профессионалы, также мы гордимся нашими дизайнерами, которые составляют удивительные дизайн проекты будущих помещений. Все проекты делаются с учетом клиентов, их пожеланий и темперамента. Мы подходим индивидуально к каждому заказу, что в итоге дает прекрасный итог. Об этом вещают отзывы наших клиентов и фото в галерее на веб сайте yaremont.ru где подобраны наши проекты.
По запросу кардинальное переустройство переходите на наш онлайн ресурс. Находимся по адресу г. Москва, Андроновское ш., 26. Работаем без выходных, режим с 9:00 до 20:00. Свяжитесь с нами по телефону +7(495)540-49-58 и мы обсудим все нюансы по вашему ремонту. Оплата осуществляется любым удобным способом для заказчика, поэтапно. Приступаем к работе без предоплаты. Звоните, оформляйте заявку и совсем скоро ремонт Вашей мечты сможет стать реальностью.
The panorama of fine line tattoos unfurls a captivating symphony of stylistic possibilities https://minecraftcommand.science/forum/general/topics/choosing-the-perfect-design-for-your-fine-line-tattoo-in-calgary One must embark upon a voyage.
Could I have been changed in the night? Let me think:
Fine line geometric tattoos represent a profound departure https://moneyfx.boardhost.com/viewtopic.php?pid=17377#p17377 from the conventional and frequently audacious realm of tattoo aesthetics.
energy storage solutions
buying lisinopril in mazatlan
This resplendent style has surged into prominence on the back of its beguiling, almost ethereal https://myworldgo.com/forums/topic/105631/fine-line-tattoos-vs-traditional-tattoos-pros-and-cons/view/post_id/1161877#siteforum_post_1161877
, forgetting everything else in his panic, he rushed
https://hotel-globus40.ru/spisok-sportivnogo-snaryazheniya-dlya-zanyatij-boksom/
Мосоптторг – зарекомендованная, востребованная, результативная компания, осуществляющая высококачественное обслуживание http://snabzhenie-obektov.ru/ для обеспечения материалами, применяемыми в строительстве.
Кто-нибудь может подсказать – как можно получить консультацию лазерного хирурга бесплатно предменструальное дисфорическое расстройство стоит вопрос о лазерной коагуляции сетчатки.
%%
My blog post – gambling sites
Кто-нибудь может подсказать – как можно получить консультацию лазерного хирурга бесплатно предменструальный синдром стоит вопрос о лазерной коагуляции сетчатки.
Medicament prescribing information. What side effects?
norvasc buy
Some about medicine. Get information now.
An erotic dance is a dance that provides erotic entertainment and whose objective is the stimulation חשפנית בראשון לציון of erotic or sexual thoughts or actions in viewers.
Really no matter if someone doesn’t understand then its up to other users that they will assist, so here it takes place.
Good day! I know this is kinda off topic however , I’d figured I’d ask.
Would you be interested in trading links or maybe guest authoring a blog
post or vice-versa? My site addresses a lot of the same topics as yours and I believe we
could greatly benefit from each other. If you happen to be interested feel free to send me an email.
I look forward to hearing from you! Excellent blog by
the way!
%%
Have a look at my page https://www.giantbomb.com/profile/dentistrydante/
Does COPD get worse even if you quit smoking buy ventolin inhaler.
buy lisinopril httz
online arzt levaquin
Medication prescribing information. Drug Class.
order provigil
Some about medicines. Read information now.
where can i buy doxycycline for chlamydia
%%
Look into my blog post :: https://eurorscg-interactive.com/
lisinopril 10 mg buy
Уничтожение насекомых, дезинфекция, дератизация с гарантией в вашем городе Служба дезинфекции в Сочи: Уничтожение насекомых и грызунов
We are a group of volunteers and opening a new scheme in our community.
Your site provided us with valuable info to work
on. You have done a formidable job and our whole community
will be grateful to you.
1xbet promo code for bonus
buying doxycycline online uk
Уничтожение насекомых, дезинфекция, дератизация с гарантией в вашем городе Служба дезинфекции в Самаре: Уничтожение насекомых и грызунов
truth, do you eat bats?” all at once, thump! thump!
Anointing your tattoo with the elixir of moisture, a critical act in the alchemy of https://discuss.ilw.com/forum/immigration-discussion/490837-fine-line-tattoo-aftercare-tips-and-tricks-for-a-stunning-result a stunning fine line tattoo, unfurls as the next chapter in this saga.
Medicine information leaflet. What side effects can this medication cause?
lioresal
Actual news about drug. Get information here.
Hello friends if you are hosting a bachelor party in the north חשפניות בצפון and it is important to you that the party will go well.
%%
my web site – wtpglobalau.com
A hot strip show for a bachelor party חשפנית בצפון what bachelor party before the wedding.
arimidex cost
https://zaim-na-kartu-sberbank.ru/
%%
Also visit my site: https://strip10.com/
buy lisinopril online no presription
“There might be some sense in your knock-ing,” the
Основными направлениями экспорта ViOil являются страны СНГ віктор пономарчук Ближнего Востока, Юго-Восточной Азии, Северной и Восточной Африки, Европы.
aralen
Основными направлениями экспорта ViOil являются страны СНГ віктор пономарчук vioil Ближнего Востока, Юго-Восточной Азии, Северной и Восточной Африки, Европы.
https://www.iveesoft.com/
For the Mouse swam off from her as fast as it could go,
Рекомендую покупать тут Нурофен.
%%
My blog post – https://playpokerok.ru/
Drug information leaflet. Effects of Drug Abuse.
paxil
All trends of meds. Get here.
%%
Feel free to visit my blog post … https://mefankot.net/
prasugrel buy
Last years results confirmed that the industrial group ViOil віктор пономарчук vioil remains the leader in rapeseed oil production.
According to a message on the companys website, the groups oil extraction plants processed віктор пономарчук about 76 thousand tons of rapeseed.
According to a message on the companys website, the groups oil extraction plants processed віктор пономарчук vioil about 76 thousand tons of rapeseed.
buy lisinopril hctz
The Role of Inhalers in a Sustainable Health System side effects of albuterol inhaler.
At the beginning of August, a charity football tournament among youth віктор пономарчук vioil teams of the region was held in Vinnitsa.
Harbour Cranes in USA
%%
Take a look at my blog – https://pokerokrussiapro.ru/
what is the medication cetirizine used for
celexa kaufen
Я давно искал подходящую компанию для ремонта, и вот нашел yaremont.ru. Они предлагают квартир под ключ, что очень удобно. Теперь моя квартира выглядит просто отлично!
%%
Also visit my blog post: купить аттестаты
Medicine information sheet. Long-Term Effects.
levitra tablets
All about drugs. Read here.
buy zerit without prescription
buy consultation net link lisinopril free
%%
Feel free to visit my web site; https://www.ginseal.com/how-to-choose-a-suitable-spiral-wound-gasket-for-your-flange/
zoloft 75mg
cheap aurogra without prescription
Drugs prescribing information. Long-Term Effects.
rx cipro
Some what you want to know about medicine. Read information here.
Компания по продаже металлопроката в Тюмени
купить металлопрокат в тюмени!..
Подбор качественного металлопроката – это важная задача, от которой зависит успешное завершение любого строительного или ремонтного проекта. На рынке города Тюмени есть множество предложений, но как выбрать наиболее надежного и компетентного поставщика?
Металлопрокат Тюмень: почему стоит обратить внимание
В последние годы спрос на металлопрокат в Тюмени стабильно растет. Это связано с активным развитием строительства и потребностью в качественных материалах. Компания металлопрокат в Тюмени предлагает широкий выбор продукции, удовлетворяющий потребности как крупных строительных компаний, так и частных заказчиков.
Разнообразие предложений позволяет клиентам легко найти и купить металлопрокат в Тюмени по выгодной цене. К тому же, многие компании предлагают дополнительные услуги, такие как резка, гибка и доставка материалов прямо на объект.
Металлопрокат в Тюмени: размеры и цены
Одним из основных преимуществ работы с лидирующими компаниями города является возможность получить подробный металлопрокат Тюмень прайс. Это позволяет клиентам заранее планировать свой бюджет и делать обдуманные закупки. Ведь металлопрокат цена варьируется в зависимости от многих факторов, включая размеры, марку стали и объем заказа.
Как выбрать и купить металлопрокат в Тюмени
Для того чтобы сделать правильный выбор и купить металлопрокат, стоит учитывать несколько важных аспектов. Прежде всего, необходимо обратить внимание на репутацию компании. Отзывы клиентов, история на рынке и портфолио выполненных заказов – все это поможет сделать верный выбор.
Далее, обратите внимание на условия сотрудничества. Наличие гибкой системы скидок, условия доставки и возможность оперативной резки металлопроката могут стать определяющими факторами при выборе поставщика.
На рынке Тюмени представлено множество компаний, занимающихся продажей металлопроката. Выбирая между ними, стоит обратить внимание на опыт работы, качество предлагаемой продукции и условия сотрудничества. Таким образом, каждый сможет найти оптимальное решение для своих потребностей.
buy proscar finasteride
Tattoos, those inked tapestries of human expression, have traversed the epochs, http://forums.delphiforums.com/vpshostinguae/messages/5275/1 bearing witness to tales of personal narratives, artistic prowess.
The Transformation of Fine Line Tattoos in Calgary: http://www.razyboard.com/system/morethread-exploring-the-history-and-evolution-of-fine-line-tattoos-in-calgary-pete_bernert-41716-6437290-0.html tattoos, once relegated to society’s margins, now stand as potent symbols of self-expression and artistry.
%%
Also visit my webpage … https://obrazovaniya.com/product-category/srednee-obrazovanie-ssuzy/tekhnikum/
The Cultural Resonance of Fine Line Tattoos: https://rdd.media/fine-line-flower-tattoo-exquisite-floral-artistry-by-masterful-tattoo-artists/ beyond their aesthetic splendor, fine line tattoos in Calgary
100 free spins casino
Whether you would like to get auto money online, you must narrow down all
the possible deals and prices that accommodate your spending plan. As usually along with the instance of
many, they usually tend to ignore the usefulness of contrasting financial quotes that they often tend
to invest three times as high as they could have really spared,
Learn More.
porn 47186 video
Artificial intelligence tools have actually changed how businesses run. They are actually now made use of to automate and also improve IT management procedures. AIOps, or artificial intelligence for IT operations, is one example of this particular innovation. IT crews utilize it to observe, evaluate and automate IT facilities as well as improve happening management, https://worldcosplay.net/member/1419999.
%%
my web site https://school12kiev.at.ua/forum/12-2090-1
Pills information sheet. Effects of Drug Abuse.
can i get bactrim
Some trends of meds. Get information here.
isosorbide mononitrate kaufen
Простыми словами о том, что нужно знать прежде, чем заказать дизайн упаковки дизайн упаковка бренда
However, the bright celebration did not end with the last minutes of the final match віктор пономарчук and the awarding of the young athletes.
Простыми словами о том, что нужно знать прежде, чем заказать дизайн упаковки дизайн упаковки
На сайте Центра ментального здоровья и психологического развития Эмпатия вы сможете узнать симптомы депрессии, депрессия получить консультацию и квалифицированное лечение.
На сайте Центра ментального здоровья и психологического развития Эмпатия вы сможете узнать симптомы депрессии, депрессия получить консультацию и квалифицированное лечение.
%%
my homepage … http://l90226mw.beget.tech/2023/10/10/kupit-diplom-tehnikuma.html
магазин шин и дисков https://magazin-avtomobilnih-shin.ru/
%%
Here is my site: https://vammebel.ru/catalog/takhta/
Вы абстрактный человек
person are not responsible for all inconsistencies in data and potential inconveniences caused by the Bimmer.
%%
Here is my blog; link
where to buy atarax 25mg
ventolin nebules
buying lisinopril in mexico
Поиск авиабилетов для путешествий в любую точку мира на агрегаторе Скайсканер тут
Поиск авиабилетов для путешествий в любую точку мира на агрегаторе Скайсканер скайсканер
lisinopril 20mg coupon
Ми, виробництво Віанд, використовуємо високоміцну тканину, яка не розтягується Москітна сітка для розкладачки ссылка. і має першокласні характеристики міцності.
Ми, виробництво Віанд, використовуємо високоміцну тканину, яка не розтягується ліжко військове розкладне Мултикам – купить Ліжка. і має першокласні характеристики міцності.
Полностью разделяю Ваше мнение. Это хорошая идея. Я Вас поддерживаю.
що за нюанси і мінуси кожного способу заміщення природних зубів https://70taka.com/link/deai3/ts.cgi?ur=www.gps-sport.net%2Fusers%2Fdentistrydante штучними конструкціями?
также, опытные гемблеры также могут получить бездепозитные за регистрацию условия, в pin up casino в виде пинкоинов, виртуальной валюты, которую они получают посредством особых промокодов и купонов, https://sparkcasinoofficialsite.win/bonusy публикуемых в официальных источниках.
В последние годы интерес к казино онлайн значительно возрос. Сайт caso-slots.com отвечает этому тренду, предлагая посетителям тщательно отобранный список казино на реальные деньги.
Drugs information leaflet. Short-Term Effects.
where can i get mobic
Actual news about pills. Read here.
1xbet промокод при регистрации
Female nudity is not just spectacular stripping חשפנית בצפון it is the fire of emotions, the release of the soul, the art of dance.
valtrex 1000mg generika
%%
Feel free to surf to my homepage http://www.kiopro.ru/support/forum/view_profile.php?UID=62031
Axxinot – торговая марка Вертикальные радиаторы, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
When ordering strippers from our company, it is guaranteed that you will receive not only חשפניות בצפון the most beautiful girls in Israel, but also the most professional service.
When ordering strippers from our company, it is guaranteed that you will receive not only חשפנית בצפון the most beautiful girls in Israel, but also the most professional service.
buy lisinopril 5mg
Жирные кислоты соапстоков светлых растительных масел и саломасов для кормовых віктор пономарчук vioil основными направлениями экспорта ViOil являются страны СНГ, Ближнего Востока.
Жирные кислоты соапстоков светлых растительных масел и саломасов для кормовых віктор пономарчук основными направлениями экспорта ViOil являются страны СНГ, Ближнего Востока.
%%
Take a look at my web blog :: https://ifvremya.ru/kogda-mozhno-ponadobitsya-vydacha-dublikata-nomerov-na-avtomobil/
loperamide canada
В последние годы интерес к казино онлайн значительно возрос. Сайт caso-slots.com отвечает этому тренду, предлагая посетителям тщательно отобранный список казино на реальные деньги.
%%
My homepage – https://joycasinosites.top/akcii.html
Прогон сайта с использованием программы “Хрумер” – это способ автоматизированного продвижения ресурса в поисковых системах. Этот софт позволяет оптимизировать сайт с точки зрения SEO, повышая его видимость и рейтинг в выдаче поисковых систем.
Хрумер способен выполнять множество задач, таких как автоматическое размещение комментариев, создание форумных постов, а также генерацию большого количества обратных ссылок. Эти методы могут привести к быстрому увеличению посещаемости сайта, однако их надо использовать осторожно, так как неправильное применение может привести к санкциям со стороны поисковых систем.
Прогон сайта “Хрумером” требует навыков и знаний в области SEO. Важно помнить, что качество контента и органичность ссылок играют важную роль в ранжировании. Применение Хрумера должно быть частью комплексной стратегии продвижения, а не единственным методом.
Важно также следить за изменениями в алгоритмах поисковых систем, чтобы адаптировать свою стратегию к новым требованиям. В итоге, прогон сайта “Хрумером” может быть полезным инструментом для SEO, но его использование должно быть осмотрительным и в соответствии с лучшими практиками.
%%
Stop by my webpage – https://kovry-kupit-11.ru/
Согласен, ваша мысль просто отличная
Однако лазейки представлены. Как пояснил Михаил Хачатурян, чаще всего на реализации дипломов попадаются небольшие частные вузы, продажа дипломов о высшем образовании однако такого рода заведений с каждым годом стало уже меньше.
%%
Have a look at my blog post … https://lifeposi.ru/kak-izgotavlivayutsya-nomera-dlya-avtomobilya-tehnologiya-i-materialy-38222/
Отличный и своевременный ответ.
подобный документацию, как аттестат, поможет для продления просиживания в учебном заведении, купить диплом инженера учебном заведении либо техникуме и получить необходимую вам профессию.
Medicines information. What side effects can this medication cause?
zithromax
Everything what you want to know about drugs. Read here.
%%
My web-site http://imgops.com/smsmarket.ua/
квартира Минск недорого
%%
Also visit my webpage; казино spark
%%
Also visit my blog post – купить диплом медицинского колледжа
%%
Feel free to visit my site; купить диплом училища ссср
%%
My homepage; https://russia24.pro/moscow/362141700/
buy lisinopril 20 mg online usa
joy casino – это идеальное место с целью, чтобы найти собственную любимую слот-игру, казино джой наслаждаясь увлекательной игрой без закачки в защищенной и надежной среде.
Rattling informative and great complex body part of articles,
now that’s user friendly (:.
Also visit my blog – junkyard near me car
Wow, superb blog format! How long have you ever been blogging
for? you made running a blog glance easy.
The entire look of your website is magnificent, let alone the content material!
price of cialis soft tabs 10mg mercury
Совершенно верно! Мне нравится Ваша идея. Предлагаю вынести на общее обсуждение.
За приобретение такого сертификата грозит штраф в виде максимум 80 тыс. Иногда поводом раскошелиться становится понимание, что программу вуза покупатель не займет, купить высшее образование цена а свидетельство о получении образования нужен.
Компания по продаже металлопроката в Тюмени
металлопрокат в тюмени размеры и цены!..
Подбор качественного металлопроката – это важная задача, от которой зависит успешное завершение любого строительного или ремонтного проекта. На рынке города Тюмени есть множество предложений, но как выбрать наиболее надежного и компетентного поставщика?
Металлопрокат Тюмень: почему стоит обратить внимание
В последние годы спрос на металлопрокат в Тюмени стабильно растет. Это связано с активным развитием строительства и потребностью в качественных материалах. Компания металлопрокат в Тюмени предлагает широкий выбор продукции, удовлетворяющий потребности как крупных строительных компаний, так и частных заказчиков.
Разнообразие предложений позволяет клиентам легко найти и купить металлопрокат в Тюмени по выгодной цене. К тому же, многие компании предлагают дополнительные услуги, такие как резка, гибка и доставка материалов прямо на объект.
Металлопрокат в Тюмени: размеры и цены
Одним из основных преимуществ работы с лидирующими компаниями города является возможность получить подробный металлопрокат Тюмень прайс. Это позволяет клиентам заранее планировать свой бюджет и делать обдуманные закупки. Ведь металлопрокат цена варьируется в зависимости от многих факторов, включая размеры, марку стали и объем заказа.
Как выбрать и купить металлопрокат в Тюмени
Для того чтобы сделать правильный выбор и купить металлопрокат, стоит учитывать несколько важных аспектов. Прежде всего, необходимо обратить внимание на репутацию компании. Отзывы клиентов, история на рынке и портфолио выполненных заказов – все это поможет сделать верный выбор.
Далее, обратите внимание на условия сотрудничества. Наличие гибкой системы скидок, условия доставки и возможность оперативной резки металлопроката могут стать определяющими факторами при выборе поставщика.
На рынке Тюмени представлено множество компаний, занимающихся продажей металлопроката. Выбирая между ними, стоит обратить внимание на опыт работы, качество предлагаемой продукции и условия сотрудничества. Таким образом, каждый сможет найти оптимальное решение для своих потребностей.
%%
Check out my web page gay porn
%%
Feel free to surf to my homepage … https://rio-alchevsk.at.ua/forum/2-5877-1
Medication information sheet. Generic Name.
viagra generic
Some information about medication. Get information here.
lexapro 20 mg tablet
zoloft medication
Lucky Jet, un popular juego de choque, llama la atencion no solo por sus Lucky Jet Registro sencillas reglas, sino tambien por su impresionante diseno visual.
Lucky Jet, un popular juego de choque, llama la atencion no solo por sus Lucky Jet sencillas reglas, sino tambien por su impresionante diseno visual.
buy lisinopril with hctz
The FIBA 3×3 Women’s Series is the #1 occasion on the 3×3
girls’s professional circuit.
BALLU 2000 – настенный электрический обогреватель с электронным термостатом и системами защиты от перегрева и низких температур для быстрого обогрева обслуживаемого помещения https://rusupakten.ru/product/tenpu-3/
19.95 a thirty day period which is much less expensive than getting two hundred tokens as a stand-by itself box. If you ‘re thinking precisely how substantially is a souvenir well worth on Chaturbate, the next displays their expense depending on the box you obtain . You will be shelling out involving 9 and 11 cents relying on how quite a few tokens you purchase. The additional tokens you order the even larger the dismiss off the Chaturbate token rate you ‘ll get. If you indicator up to Chaturbate ‘s VIP Premium Membership software you get a basket of benefits which includes the skill to mail personal messages to broadcasters, an ad-free of charge interface, similarly perfectly as a erstwhile gift of two hundred tokens. If you ’ rhenium desire in joining Chaturbate, suction quit hera to indicator up and commence earning cash currently . It ’ second meter to leave all your insecurities behind and take into consideration all the possibilities you can have if you develop into a webcam performer.
По моему мнению Вы допускаете ошибку. Могу отстоять свою позицию. Пишите мне в PM, пообщаемся.
для истинного диплома СССР характерно наличие минимального количества степеней защиты, где можно купить аттестат за 9 класс поэтому изготовить их значительно эффективнее. Работодатели не рассматривают соискателей без диплома о высшем образовании.
%%
Here is my web-site https://lifedon.com.ua/repairs/77072-alyuminievyy-profil-ot-kompanii-alyupro-grup.html
cetirizine tablets
Language development is a fundamental aspect of a childs growth, playing a pivotal role in their ability to communicate, умственная отсталость express emotions, and connect with the world around them.
Language development is a fundamental aspect of a childs growth, playing a pivotal role in their ability to communicate, олигофрения express emotions, and connect with the world around them.
как выиграть в игре lucky jet
Medicine information leaflet. Drug Class.
propecia
Actual information about medication. Read information now.
It offers vegetable meals, fats and oils, pellets, tropical oils, grains, oilseeds, phosphatide concentrates, віктор пономарчук vioil fatty acids, sunflower oil, and more.
снабжение строительных объектов http://media-dream.ru/
снять в Минске квартиру
lisinopril 20 mg buy cash
The group was the first in the country to produce rapeseed oil віктор пономарчук the company exported almost all its products.
деятельных посетителей привлекают достойные лимиты на вывод денег – 6,4 млн. в отличие от прохождения шутера в казино дистанционно даром, https://luchshiecasinoonlinetop12023.win/minimal-deposit ход игры с минимальными взносами сулит гемблеру получение реальных выплат.
Это — заблуждение.
почему конкретно по знакомой, купить диплом строительного техникума ведь переподготовка подразумевает присвоение новой квалификации? Гуманитарный институт телевидения и радиовещания им. М.А.
What age is best to have children Cenforce.
How do you make him jealous and miss me Cenforce 200.
Рекомендую Вам посетить сайт, на котором есть много статей на интересующую Вас тему.
each of them offers huge assortment slots, keno https://www.quiendijoboda.es/foro/index.php?action=profile;u=127157 and table games.
Medicine information for patients. Drug Class.
norvasc
Actual information about pills. Read now.
where to buy zyprexa
Спасибки , кто ищет тот всегда найдет
если надо немедленно оформить данный бумагу, купить диплом времен ссср то деятельность, связанная с отходами займет незначительное количество дней. 7. Цена услуги. мы стараемся сделать процедура оформления диплома функционал максимально комфортным.
1xbet промокод при регистрации
аренда квартиры на кипре https://kvartiry-na-kipre.com/
This allows you to load the capacity evenly throughout the year віктор пономарчук vioil all oil extraction plants of the ViOil group are multicultural.
lisinopril 20 mg buy cash
Thanks for one’s marvelous posting! I certainly enjoyed reading it, you could be a great
author.I will ensure that I bookmark your blog and
definitely will come back someday. I want to encourage yourself to continue your great posts,
have a nice weekend!
%%
Also visit my blog :: купить диплом без занесения в реестр
The global marketing company Infinity Business Insights ViOil presented an overview and forecast віктор пономарчук vioil of the development of the sunflower meal market for 2022?2028.
промокод для ставки 1xbet
Medication information for patients. Long-Term Effects.
where to get norpace
Actual information about pills. Get information here.
Вы не правы. Я уверен. Пишите мне в PM.
Альфа Мотор Групп, https://somdejamulet.org/product/ninja-silhouette-2/ сервис на Головинском шоссе современный высококачественный автосервис для автомобилей тойота и lexus. Аvtocomf.ru – интернет-магазин Реализация специального оснащения для кроссоверов, внедорожников, квадроциклов.
https://kvartiravminske.by/
%%
Here is my web-site – https://www.sq.com.ua/rus/news/novosti_partnerov/25.12.2021/gde-zakazat-sistemy-dlya-navesnyx-ventiliruemyx-fasadov
У меня похожая ситуация. Можно обсудить.
Обычно, диплом техникума ссср купить каждый из нас по завершении окончания 9-го или 11-го класса получает общее или базовое образование. партнерство со всеми почтовыми операторами страны, благодаря этому транспортировка документов возможна в предельно отдаленные уголки российской.
промокод 1xbet слоты
%%
Also visit my website :: https://amcor.asia/
Thank you, I appreciate this!
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
промокод для один икс бет
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
бездепозитный промокод 1xbet
Whether you wish to purchase auto money online,
you need to limit all the possible offers as well as rates that
suit your budget. As typically with the situation of several, they have a tendency to neglect the value of comparing money quotes that they have a tendency to spend
thrice as much as they can have actually spared, Read More Here.
Как начать играть в онлайн казино, секреты, советы, рейтинг Топ 10 казино Как не проиграть все? Как выиграть? Брать бонус на депозит?
%%
Here is my homepage https://diploms-spb.com/diplom-o-srednem-obrazovanii/
биржа блогеров инфлюенсеров
%%
Here is my blog: https://luchshiecasinoonlinetop12023.win/best
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Прошу прощения, что ничем не могу помочь. Надеюсь, Вам здесь помогут другие.
Официальное производство на немецком оборудовании в москве; Используем износостойкую американскую пленку 3m reflex foil; Лицензии ГУ Обдд Мвд РФ на любые виды номеров; Красим в несколько слоев немецкой краской kurz с качеством 3 года; Лазерные голограммы «rus» и выбитая печать как в https://kalendarnagod.ru/dublikaty-gosudarstvennyh-nomernyh-znakov-chto-eto-takoe-i-dlya-chego-oni-nuzhny/ Гибдд!
В этом что-то есть и это отличная идея. Готов Вас поддержать.
сама технология успешно применяется в мире в медицинских клиниках, spa, https://www.kamadobono.it/it/component/k2/item/129-faqs салонах красоты и была одобрена Европейскими регулирующими органами в качестве медицинского аппарата с присвоением медицинского СЕ сертификата.
claritin ohne rezept bestellen
%%
Also visit my homepage – http://www.annuityexchange.com/__media__/js/netsoltrademark.php?d=sexkhau.top
трековые светильники volpe https://novosvetum.ru/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
https://taxikama.tb.ru/
A no deposit bonus at F1 Casino can be cashed out if you wager admiral x casino no deposit bonus the bonus (x50) within 3 days.
A no deposit bonus at F1 Casino can be cashed out if you wager pelican casino the bonus (x50) within 3 days.
тонкий ортопедический матрас https://ortopedicheskie-matrasi.ru/
excellent post, very informative. I ponder why the opposite specialists of this sector do not realize this. You must continue your writing. I am confident, you have a huge readers’ base already!
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
LГҐn 300000
abilify medication
ха-ха-ха Это просто нереально….
это предоставляет крупным игрокам преимущества: они могут делать внутренние скоринги, https://lifeposi.ru/kak-izgotavlivayutsya-nomera-dlya-avtomobilya-tehnologiya-i-materialy-38222/ более точно просчитывать риски.
автобусные туры из питера в карелию h1-marketing.ru
В момент, когда мне срочно понадобилось 7000 рублей, все-займы-тут.рф стал моим спасением. Все процедуры минимальны, а выбор МФО впечатляет. Теперь я знаю, где найти подробную и актуальную информацию о займах и с уверенностью могу рекомендовать этот сайт вам!
1xBet – это благоприятные условия при регистрации и выборе ставок промокод 1хбет на сегодня ринимая участие во всех выгодных предложениях, новички и постоянные игроки получают прекрасную возможность увеличить свой бонусный счёт.
1xBet – это благоприятные условия при регистрации и выборе ставок 1xbet промокод бонус ринимая участие во всех выгодных предложениях, новички и постоянные игроки получают прекрасную возможность увеличить свой бонусный счёт.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Служба дезинфекции – уничтожение насекомых и грызунов в вашем городе c гарантией Служба дезинфекции в Адлере: Уничтожение насекомых и грызунов уничтожение насекомых, дезинфекция, дератизация с гарантией.
Служба дезинфекции – уничтожение насекомых и грызунов в вашем городе c гарантией Обработка от клопов уничтожение насекомых, дезинфекция, дератизация с гарантией.
%%
My web-site: https://joycasino-sites.win
Pills information leaflet. Brand names.
bactrim generics
Actual news about medicines. Read here.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
You actually explained this very well.
Игорный клуб Eldorado Casino начал свою работу в 2017 году eldoradocasino на первый депозит от 200р – 200 фриспинов.
Игорный клуб Eldorado Casino начал свою работу в 2017 году eldorado казино на первый депозит от 200р – 200 фриспинов.
Моя квартира требовала ремонта. На материалы не хватало 25000 рублей. В Facebook я узнал о все-займы-тут.рф. займ на карту без отказа помог мне обновить жильё. Сайт заслуживает доверия!
Position certainly used..
Also visit my homepage … promo 1xbet
Вызов врачей и узких специалистов на дом клиника оказывает широкий спектр услуг булимия Уколы и капельницы.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Вызов врачей и узких специалистов на дом клиника оказывает широкий спектр услуг Первые пять ссылок анкор шизофрения Уколы и капельницы.
%%
acyclovir cream 10g billig
%%
my web page … a-strippers.space
промокод при регистрации на 1xbet
LГҐn 3000 kr
macrobid
%%
Feel free to surf to my site :: https://prokazan.ru/adverting/view/avtomobilnye-gos-nomera
%%
Here is my website – https://fixmyacnj.com/
Компания 1xBet не оставила без внимания своих клиентов, которые предпочитают использовать мобильную версию условия промокода 1xbet В букмекерской компании 1xBet существует несколько способов ввода и вывода средств.
Highly energetic article, I loved that a lot. Will there be a part 2?
My site … volkswagen jetta 2007
Компания 1xBet не оставила без внимания своих клиентов, которые предпочитают использовать мобильную версию промокод 1xbet на бесплатную ставку В букмекерской компании 1xBet существует несколько способов ввода и вывода средств.
промокод для регистрации в 1xbet
Best complex in Northern Cyprus Grand Sapphire Blu.
%%
Take a look at my homepage :: https://mesibot.agency/he/striptease
Полностью разделяю Ваше мнение. В этом что-то есть и идея хорошая, поддерживаю.
это может быть связано со долгой или неправильной эксплуатацией номерных знаков, https://ambox.ru/avtomobili-omoda-budushhee-transporta-s-chelovecheskim-oshhushheniem-2/ а также с попаданием авто в дтп.
зимние шины r16 https://zimnie-shini-avto.ru/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
I really like it when individuals get together and share opinions. Great website, stick with it!
Drugs information. Effects of Drug Abuse.
fluoxetine buy
Some information about medicine. Get here.
Amazing knowledge Thanks a lot!
спс… стараюсь
Так все оформление показался https://kovry-kupit-11.ru/ завершенным и симметричным. сделать более гостеприимным и простым традиционный интерьер с любым из серии ковров maro.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Feel free to surf to my blog: https://news-football.net/sources
Знакомьтесь с прекрасным примером эволюции классической чат-рулетки бесплатные видео чаты улучшенный гендерный фильтр, круглосуточная модерация.
Adoro a expectativa de esperar a bola cair no meu numero na roleta https://www.roletacasino.online/ a Roleta e um jogo facil de aprender, mas dificil de dominar.
%%
My web page … https://rkstrippers.com
%%
Also visit my website; erdance.club
Howdy! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.
Anyways, I’m definitely glad I found it and I’ll
be book-marking and checking back often!
fluticasone billig kaufen
buy lisinopril 10 mg
https://kotel-krontif.ru заходи подбери.
https://www.recruiterwiki.de/Benutzer:LatishaEdouard
электрические шторы на окна https://prokarniz15.ru/
%%
my site … erotic-show.com
https://owlpedia.org/index.php/User:ArnulfoG18
Sexy webcam models
how to purchase trazodone 100 mg
%%
Visit my site; https://newratingcasino.win/best
After a person of Elvis Presley’s last displays, I was heading back again to my motor vehicle when a matron from Zachary stopped me and gushed about how excellent he experienced been. When I in fact received the cellphone phone, I could not assistance my thoughts racing back again to a single magical working day in 1956, that is normally remained vivid in my memory. No. Elop introduced in his Microsoft Mafiadude who had by no means marketed a phone in his everyday living right before Elop grabbed him, as now the world wide handset revenue chief? Part of what we enjoy at the Future Perfect in typical is the chance to build that social conversation with the function that we existing, for the reason that it fully modifications the psychology of how you look at it.” – David Alhadeff, founder of Future Perfect, a design and style gallery one particular of whose Los Angeles spots is at Elvis previous house at the Trousdale Estates, now identified as Casa Perfect, in an post printed at Vogue Fashion’s February 20,2019 version.
https://pedagog-razvitie.ru/course.html
Я извиняюсь, но, по-моему, Вы допускаете ошибку. Могу это доказать.
Покупка такого номера будет в тренде в случае приобретения и постановки на учёт нового автомобиля, https://ambox.ru/avtomobili-omoda-budushhee-transporta-s-chelovecheskim-oshhushheniem-2/ и для потребности сделать дубликат старого гос.
В школе Центра иностранных языков YES вы сможете с легкостью для детей английский и интересом освоить английский язык.
Sexy webcam models
В школе Центра иностранных языков YES вы сможете с легкостью курсы английского для школьников и интересом освоить английский язык.
The Bible is a remarkable journey through time, culture, and faith – Download High Resolution Images and Maps: Artifacts a narrative that spans from the creation of the world to the visions of the future.
The Bible is a remarkable journey through time, culture, and faith – Bible History for Kids: What Do You Have? a narrative that spans from the creation of the world to the visions of the future.
https://wikiposts.net/index.php/User:RacheleDolling2
http://www.naracaps.co.kr/naracaps/bbs/board.php?bo_table=free&wr_id=4166
https://bbarlock.com/index.php/User:ShaneKetcham
clarinex online-apotheke bestellen
%%
Also visit my website – https://imbility.com/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
https://ptwiki.blitwise.com/index.php/User:Guillermo6476
Drug information. Cautions.
can you buy priligy
Some information about medicine. Read now.
http://www.uljinnews.kr/bbs/board.php?bo_table=free&wr_id=81127
%%
Feel free to visit my webpage :: https://www.luxnailgarden.com/forum/beauty-forum/shopping-cart-migration
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Feel free to surf to my web-site :: https://net2.com/how-to-migrate-from-wix-to-shopify-website-transferring-tips-2022/
https://deadreckoninggame.com/index.php/User:CurtdeLargie0
https://telugusaahityam.com/User:GavinFolsom4105
quite hot, she fanned her-self all the time she went on
летние шины цена https://letnie-shini-avto.ru/
how to buy mobic 15mg
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
buy lisinopril online uk
length she brought her-self down to the right size.
https://wiki.fontyspulsed.com/index.php?title=Allmed24.ru
%%
my blog post … https://alfa-strippers.space/
To maintain your bowl in high form for a long time, proper care is essential. A: The Joe Bowl is greatest used with foil, as it could not provide a snug fit for HMDs.
my web-site – https://Martinieysm.Loginblogin.com/28455892/madrid-s-best-kept-secrets-premium-hookah-bars
buy lisinopril in cartagena
https://mediawiki.governancaegestao.wiki.br/index.php?title=Allmed24.ru
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Also visit my web site … http://4x.com.ua/ssangyong/showthread.php?t=1218
Действительно и как я раньше не подумал про это
Super affordable swinger videos only for $9.99 per month. safely, you, maybe free 7-day access! just don’t cum in my silk, stepson!
How long should I walk to lose belly fat cenforce 200.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Meds information for patients. Short-Term Effects.
norvasc for sale
Everything what you want to know about pills. Get information now.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Kredit 7000 Euro
elavil
Pills information sheet. Drug Class.
where buy singulair
Best trends of medicament. Get information now.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Very good site for Bitcoin Price USD.
%%
Feel free to visit my website – http://womans.forum.cool/viewtopic.php?id=5517
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
celecoxib online
can you buy lisinopril in mexico without presription
Ваш надежный переводчик-юрист в мире права.
monakov-prof.ru
%%
Here is my site: more
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
buy lisinopril 10 mg no prescription
Наши преподаватели, среди которых есть и носители языка, всегда готовы помочь Вам приобрести необходимые знания, английский язык онлайн курс чтобы в дальнейшем их можно было уверенно использовать в повседневной жизни.
Боксерские перчатки Fairtex
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Наши преподаватели, среди которых есть и носители языка, всегда готовы помочь Вам приобрести необходимые знания, детям английский чтобы в дальнейшем их можно было уверенно использовать в повседневной жизни.
Inside the ever-evolving world of on the web sports betting and gaming https://en.gravatar.com/mostbetonline02 stands out being a top-tier platform that caters to your diverse preferences.
https://twins-fairtex.ru/
Inside the ever-evolving world of on the web sports betting and gaming https://www.google.co.jp/url?q=https://pin-up-bet-apostas.com/ stands out being a top-tier platform that caters to your diverse preferences.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
that’s much like a mouse, you know. But do cats eat
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Feel free to surf to my homepage – https://www.allworldday.com/how-to-migrate-from-shopify-to-woocommerce/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
https://www.racked.com/users/mexamoskvichka.ru
https://sen-tan.com/ Сенімді Та?дау, ?аза?стан энергетика секторында?ы сапасыз жеткізуді ж?не жабды?ты бекіту ?шін инженерлік шешімдерге ие компания беделіне жетті.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Have you ever thought about creating an e-book or guest
authoring on other websites? I have a blog based upon on the
same topics you discuss and would love to have you share some stories/information.
I know my readers would appreciate your work. If you’re even remotely interested, feel free to shoot me an e-mail.
https://www.evernote.com/shard/s692/sh/bab41cdf-6b16-9079-d238-182243c2ba24/ZYSAUdQY9pi1EO9e_HOZTbQ9L7V3Qq7UDvxHh94lITSYGf5n-ADuRoNrjw
Всем очень рекомендую Лев казино.
https://sen-tan.com/ Сенімді Та?дау компаниясы, ?аза?стан энергетика секторында озы? инженерлік шешімдер ар?ылы т?тынушыларды ?амтамасыз ету ж?не жабды?ты жеткізу ма?сатында компанияны беделдікке ие алды.
augmentin 875/125 mg cost
купить стайлер для волос дайсон https://dyson-stylery.com/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
до того ж для Того, http://www.ohaeng.kr/bbs/board.php?bo_table=free&wr_id=578912 щоб вивчити найбільш распосюдженную лексику для спілкування Ради вам вписати на навчання іншої мови онлайн.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
bluesky peptides tadalafil tadalafil kroger vidalista 10 tadalafil
her-self. “No one seems to like her down here, and
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
clozapine over the counter
Пассажирские перевозки из Калинграда Микроавтобус от 6 до 20мест Пассажирские перевозки Калининград на коллективные и семейные заявки — существенные скидки.
Пассажирские перевозки из Калинграда Микроавтобус от 6 до 20мест Пассажирские перевозки в Европу на коллективные и семейные заявки — существенные скидки.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Аутизм – описание заболевания, классификации, симптомы у взрослых и детей, причины появления заболевания, лечение аутизма методы диагностики и способы лечение недуга.
Аутизм – описание заболевания, классификации, симптомы у взрослых и детей, причины появления заболевания, лечение аутизма методы диагностики и способы лечение недуга.
loved your website! keep it up and fall upon us professional seo services online
eat or drink any-thing; so I’ll just see what this
недорогие матрасы в москве https://matrasi-shop.ru/
%%
Feel free to surf to my website: https://moipozvonochnik.ru/news/kupit-diplom-mggei_1.html
Я считаю, что Вы не правы. Я уверен. Пишите мне в PM, поговорим.
а какой ты? Пишите в комментариях. Номер: – Утерян; – Стерлись буквы, https://moscow.info-leisure.ru/2022/11/dublikat-gosnomera-avtomobilya-v-moskve-skolko-stoit-i-kak-zakazat/ цифры; – Пострадал в аварии и вы не хотите получить штраф от ГИБДД (КоАП РФ Ст.
квартира посуточно недорого
zanaflex 4mg
PЕЇjДЌka 29000 KДЌ
Nestled in the heart of Dubai Silicon Oasis Ellington Views
Really a lot of superb knowledge!
%%
My web site – http://kostanaycityweb.blogspot.com/2021/03/a-new-communication-option-with.html
снять квартиру
топ клининговых компаний https://cleaning-rating-2023.ru/
%%
Here is my blog … https://www.stlyrics.com
Keep this going please, great job!
https://sireng.net/
the fellows needed. So as Dick gave the word, five
https://sireng.net/
bot-tle. They all made a rush at Al-ice, as soon
Ковровая дорожка для уюта вашего дома
снять квартиру в Минске на сутки недорого
I’m very cute and slim Whiteboys and I want to meet you. From this thought, my nipples stick out, and my pussy flows straight to the floor https://xbebz.freelovehere.net/?utm_source=3f33acd3b135bb12&s1=12179&s2=1585765&j1=1
roques
квартира Минск
Conveyor systems streamline the movement of materials throughout the production facility https://radiopaedia.org/users/stromectol-ivermectin stromectol for scabies.
pret 2500 euros
Рекомендую Турецкие ковры высшего качества.
porn videos
broke, and he found himself lying face down
Medication safety assessments should consider the potential risks associated with off-label drug use https://radiopaedia.org/users/stromectol-ivermectin ivermectin toxicity in dogs.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Your approach to this topic is therefore various coming from others
I’ve gone through. It is actually revitalizing to see such initial material.
Fantastic job!
Here is my web site :: Ron Spinabella
Профессиональный ремонт телефонов в г Жуковский с гарантией ремонт сотовых телефонов Вы все еще думаете, что ремонт компьютерной техники стоит дорого?
thunderbolt, he was seized with consternation, and
Профессиональный ремонт телефонов в г Жуковский с гарантией https://zhukovskiipk.ru/ Вы все еще думаете, что ремонт компьютерной техники стоит дорого?
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Also visit my blog post :: https://atn.ua/leisure/na-chto-obratyt-vnymanye-pry-pokupke-jelektronnoj-syharety-elf-bar-381600/
Zip пакеты
Here you can find almost any sport for betting https://1x-bet.fun You can find good odds here.
amantadine billig kaufen
Zip пакеты
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
does tadalafil lower blood pressure tadalafil prostatitis what’s the difference between sildenafil and tadalafil
Я уверен, что Вы заблуждаетесь.
Автолюбителям подумайте о наличии копии автономера заранее, https://www.penza-press.ru/hotite-poluchit-dublikat-nomerov-na-mashinu.dhtm дабы а повреждения или утери заменить отсутствующую или испорченную табличку.
Лучшая Цинковка у нас.
tadalafil 20mg how long does it last does tadalafil cause shrinkage nitrates and tadalafil
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
upon the two. Especially was it felt by O’Brien, for
Получите консультацию с нашим юристом и узнайте ответы на свои вопросы юрист по земельному праву юридические услуги — важная квалифицированная профессиональная помощь.
Получите консультацию с нашим юристом и узнайте ответы на свои вопросы апелляция юридические услуги — важная квалифицированная профессиональная помощь.
купить зип пакеты в Москве
санэпидемстанция Воронеж официальный Санэпидемстанция Воронеж официальный сайт нашей службы dezses-voronezh.ru лучшие условия для частных клиентов и организаций.
hung a row of light-ed lamps.
%%
Also visit my page … https://buzulukmedia.ru/chto-takoe-dublikat-gosudarstvennogo-nomera-i-v-kakih-sluchayah-on-trebuetsya/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
купить Zip пакеты с логотипом
%%
my homepage; https://www.azchords.com
methods. They knew what they had to expect, and so it
Лучший автосервис шкода у нас.
дезинсекция в Саратове от тараканов цена Дезинсекция в Саратовe от тараканов по недорогим ценам, кафе, общепит, периодически бывают скидки, акции. dezses-saratov.ru
Virtual Numbers Ваш надежный партнер в мире виртуальных номеров https://www.google.si/url?q=https://didvirtualnumbers.com/ Наша IP телефония позволит вам принимать звонки, смс и зарегистрироваться в сервисах без ограничений.
Virtual Numbers Ваш надежный партнер в мире виртуальных номеров https://www.google.mg/url?q=https://didvirtualnumbers.com/ Наша IP телефония позволит вам принимать звонки, смс и зарегистрироваться в сервисах без ограничений.
Моя кофемашина перестала работать. На радость обратился за услугой ремонт кофемашин krups экспертов в восстановлению таких устройств.
Быстро, мастер доехал и устранил неисправность. Починить её ему стоило лишь тридцать минут. Так, моя кофемашина ожила, как новая.
branches as far from the trunk as possible,
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
valtrex 500mg ohne rezept
%%
Also visit my website … Чехия последние новости
Its good site for check Bitcoin Price USD
Заказать качественный ремонт фольксваген можно у нас.
Thanks to my father who informed me concerning this website, this web site is actually remarkable.
My web site parts toyota tacoma
%%
Have a look at my web site: http://www.cowboylyrics.com
карнизы для штор с электроприводом https://prokarniz17.ru/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
клининговая компания москва уборка https://cleaning-company77.ru/
частный вывод из запоя в одинцово https://vivodizzapoya-msk.ru/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
https://youtruck.ru
https://xn—–6kcfgocbaaad4bqykiaphj7adc6av0n0c1b.xn--p1ai/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Also visit my web-site: https://komiinform.ru/nt/5121
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Это лучшее онлайн-казино, где вы можете насладиться широким выбором игр https://tinyurl.com/ytxwytq6 и получить максимум удовольствия от игрового процесса.
epivir ohne rezept
Right here is the right site for everyone who really wants to find out about this topic.
You know so much its almost hard to argue with you (not that I really would want to?HaHa).
You certainly put a fresh spin on a subject which has been written about for decades.
Wonderful stuff, just great!
Also visit my blog post … celica toyota 1997
Это лучшее онлайн-казино, где вы можете насладиться широким выбором игр https://tinyurl.com/ykhb2noq и получить максимум удовольствия от игрового процесса.
times five is twelve, and four times six is thir-teen,
%%
Feel free to surf to my page; https://mashyna.com.ua/ru/remru/33417
webcam online
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Онлайн казино отличный способ провести время, главное помните, что это развлечение, https://tinyurl.com/ytrcsj62 а не способ заработка.
Онлайн казино отличный способ провести время, главное помните, что это развлечение, https://tinyurl.com/ysw6n4o6 а не способ заработка.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
уничтожение клопов в Сургуте отзывы Уничтожение клопов в Сургуте отзывы о компании dezses-surgut.ru только положительные, имеются письма благодарностей и рекомендации. Постельные клопы опасны.
Sexy webcam models
was the fan she held and she dropped it at once, or she
У нас самый качественный автосервис фольксваген.
хи хи
регистрационные знаки по-новому стандарту для американских и японских транспортных https://about-windows.ru/instrumenty-windows/kak-oformit-dublikat-nomera-avtomobilya-neobxodimye-dokumenty-i-procedura/ средств. сегодня мы выполнили запрос на производство госзнака ТИП-1 на авто Республики Дагестан с комбинацией «В555ОР».
“We won’t talk of her if you don’t like it.”
%%
My site :: p8310
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
клопы в квартире Клопы в квартире, как быть? Обратитесь в службу СЭС города Сургут профессионалы справятся с клопами за одну обработку. Круглосуточно, гарантия. dezses-surgut.ru
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
was the fan she held and she dropped it at once, or she
symbicort inhaler 160/4,5 mcg otc
Ремонт iPhone любой модел по низким ценам. Бесплатная диагностика и выезд на дом. Качественный ремонт со скидкой 15%. ремонт iPhone
and they sat down in a ring and begged the Mouse to
%%
my web-site :: https://www.niasam.ru/obschestvo/kak-sdelat-dublikat-gosnomera-na-avtomobil-137306.html
Hello there! Do you use Twitter? I’d like to follow you if that would be okay.
I’m undoubtedly enjoying your blog and look forward to new posts.
лфк врач
%%
Feel free to surf to my webpage – https://twitter.com/euro24new
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Наша работа – это поставки качественной тайской экипировки Twins Special и Fairtex, магазин экипировки Twins Special в максимально короткие сроки и по самым низким ценам.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
was I the same when I got up to-day? Seems to me I didn’t
if—if I’d been the right size to do it! Oh dear!
доставка цветов новосибирск
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Best pouches Pablo Snus in our site.
truth, do you eat bats?” all at once, thump! thump!
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
доставка цветов новосибирск
macrobid online
celebrex 200mg
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Very good site for checking Bitcoin Price USD
Drug information sheet. What side effects can this medication cause?
trazodone
Some about medicines. Get information here.
Добро пожаловать в texttospeech.ru, вашего проверенного союзника в мире ставки на спорт. Мы с гордостью предоставляем вам шанс взять на себя контроль над вашими ставками и увеличить свои перспективы на успех. Наши опытные эксперты и эксперты следят за событиями в мире спорта, чтобы поддержать вас свежими и надежными советами.
Почему выбирать нас:
Экспертные прогнозы: Наши специалисты усердно трудятся, чтобы предоставлять вам предсказания на разнообразные виды спорта. Мы знаем, насколько важно получать полезные советы перед тем, как сделать ставку.
Множество вариантов: Мы предлагаем ставки на разнообразные виды спорта, включая соккер, баскетбол, ракетку, мяч и многое другое. Вы можете выбирать из множества событий и наслаждаться азарт на свой вкус.
Бесплатные прогнозы: Мы поддерживаем идею, что каждый должен иметь доступ к полезным советам. Поэтому мы предлагаем бесплатные советы, чтобы поддержать вас сделать правильные ставки.
Легкость и комфорт: Наш сайт и приложение для мобильных устройств разработаны с учетом вашего удовольствия. Сделайте ставку буквально за несколько мгновений.
Как начать:
Зарегистрируйтесь: Создайте свой аккаунт в texttospeech.ru и получите доступ к всем нашим сервисам.
Получайте предсказания: Подписывайтесь на бесплатные советы и получайте актуальные предсказания от наших экспертов.
Сделайте ставку: После того как вы получили свой прогноз, сделайте ставку на команду по душе или событие и получайте удовольствие от игры.
Вознаграждение за успех: Вместе с texttospeech.ru, вы имеете возможность к вашей победе. Попробуйте нашу помощь уже сегодня и погружайтесь в мир ставок на спорт во всей его красе!
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
курсы бровиста и наращивание ресниц https://kursy-po-narashchivaniyu-resnic1.ru/
оборудование переговорных комнат москва https://i-tec5.ru/
%%
My web site; https://borishof-infiniti.ru/owners/service-maintenance/zamena-masla-v-akpp/
and I’ve tried a hedge; but those snakes! There’s
Medicament information leaflet. Brand names.
propecia rx
All about medicament. Read information now.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Also visit my website :: http://www.hardcoredroid.com/android-vs-ios-exploring-the-pros-and-cons-of-two-leading-mobile-operating-systems/%20
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Enjoyed looking at this, very good stuff, appreciate it.
Here is my page – toyota canry 2004
заполнение справки о доходах https://spravka-o-dohodah.ru/
Thank you. Lots of postings.
%%
Feel free to visit my web page … https://savethehamstergame.com/
%%
My blog post; диагностика infiniti
buying lisinopril online
anastrozole 1 mg purchase
night and day! Why I haven’t had a wink of sleep these
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Payday loans in California
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Their 24/7 consumer support is a lifesaver. No issue when I call, there’s always someone to assist.
Truly value it!
My webpage Insurance Navy Brokers
Перевод статей технической отрасли Особого подхода требует перевод технических статей. Это тексты, которые могут использоваться в машиностроительной, химической, строительной отрасли. Их особенность состоит в том, что текст написан в научном стиле, содержит большой массив цифровой и графической информации (это чертежи, схемы, графики и т.д.). Это требует от переводчика обширных знаний в той отрасли, для которой выполняется такая работа.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
my web-site :: https://teplopolis.com.ua/otoplenie-uk/kotly-uk/gazovye-kotly-uk
Ukraine
Перевод стандартов Одна из самых сложных задач переводчика – это перевод стандартов. Эти нормативные документы – они содержат много технических и юридических терминов, графической информации.
Muitos gostam de fazer apostas para ganhar dinheiro no cassino https://www.portaldecamaqua.com.br/noticias/69138/gire-a-roda-da-fortuna.html mas acabei me empolgando com o ganho inicial e entrando em tilt na roleta.
На официальном сайте интернет-магазина представлен широкий ассортимент алкогольной продукции доставка алкоголя на дом круглосуточно москва недорого которая разделена на категории и подкатегории товаров.
На официальном сайте интернет-магазина представлен широкий ассортимент алкогольной продукции заказ алкоголя на дом москва доставка которая разделена на категории и подкатегории товаров.
%%
Also visit my website :: https://images.google.td/url?q=https://www.northwesternfinancialreview.com/first-federal.html
По моему мнению Вы ошибаетесь. Предлагаю это обсудить. Пишите мне в PM.
Российский эксперт: станы европы очень сильно устали от обстоятельствами, в украине Украинский ответ не стал основополагающим – на Новости Чехии и Праги заседании Генассамблеи ООН.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
celebrex 200 mg canada
I really like what you guys are up too. This type of clever work and
coverage! Keep up the wonderful works guys I’ve included
you guys to my own blogroll.
If you want to acquire automobile financial online, you have to limit all the
possible deals and also rates that fit your budget.
As commonly along with the case of numerous, they
tend to disregard the relevance of comparing finance
quotes that they tend to invest three times as much as they could possess in fact saved, click here.
Добро пожаловать в texttospeech.ru, вашего проверенного союзника в мире ставок на спорт. Мы с гордостью подарим вам шанс взять на себя контроль над вашими ставками и повысить свои перспективы на выигрыш. Наши опытные эксперты и специалисты следят за событиями в мире спорта, чтобы обеспечить вас свежими и точными прогнозами.
Почему выбирать нас:
Качественные аналитические прогнозы: Наши аналитики работают не покладая рук, чтобы предоставлять вам предсказания на разнообразные виды спорта. Мы знаем, как важно получать качественные советы перед тем, как сделать ставку.
Множество вариантов: Мы предлагаем ставки на различные виды спорта, включая соккер, баскетбол, теннис, мяч и многое другое. Вы можете отбирать из многочисленных событий и наслаждаться страсть на свой вкус.
Бесплатные прогнозы: Мы верим, что каждый может получить доступ к качественным прогнозам. Поэтому мы предлагаем бесплатные предсказания, чтобы поддержать вас сделать успешные ставки.
Простота и удобство: Наш сайт и приложение для мобильных устройств разработаны с учетом вашего удовольствия. Сделайте ставку буквально за несколько мгновений.
Как начать:
Зарегистрируйтесь: Создайте свой аккаунт в texttospeech.ru и получите доступ к всем нашим сервисам.
Получайте предсказания: Подписывайтесь на наши бесплатные прогнозы и получайте актуальные предсказания от опытных специалистов.
Поставьте свою ставку: После того как вы получили свой прогноз, сделайте ставку на команду по душе или событие и наслаждайтесь игры.
Вознаграждение за успех: Вместе с нашим ресурсом, вы владеете ключами к вашей победе. Попробуйте наши услуги уже сегодня и погружайтесь в мир ставок на спорт во всей его красе!
%%
Also visit my web site :: https://blackjackmystake.com/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Just wanna input on few general things, The website layout is perfect, the articles is rattling fantastic :
D.
My blog post :: picknpull near me
Very trust site for checking Bitcoin Price USD
lioresal 25mg France
Can I simply say what a relief to discover somebody that genuinely
knows what they’re talking about on the
internet. You actually understand how to bring a problem to light and make it important.
A lot more people ought to look at this and understand this side of the story.
I was surprised you aren’t more popular given that you surely possess the gift.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
справка 2ндфл в 2023 году https://2ndfl-spravka.ru/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
aogazeta.ru
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
valtrex ohne rezept
Good and trust site Bitcoin Price USD
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
In the immense high seas of digital comfortable, ‘AVJOHA’ is a lighthouse as a replacement for seekers of aristocratic of age material.
Submerge learned into the pride and joy trove of enticing materials tailored to cater to dissimilar tastes.
Every pass?period you attack, guess a one-of-a-kind grapple with that keeps you coming back.
Insert things being what they are, immersing in a dukedom where the rock bottom of desire coincides with digital supremacy.
Reinforce your online trip with the mesmerizing allure of ‘AVJOHA’ today.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
купить щитовой дом недорого https://shchitovyedomapro.ru/
Thanks a lot! I value it!
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
растяжка киевская
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Perfect and trust site Bitcoin Price USD
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
https://www.teleprogramma-peredach-segodnya.ru/
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Do you need a quick cash advance? Great, You have come to the correct address loans near me Our site will help you find the right lender in your city.
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
seroquel usa
haste. A large bird had flown in-to her face,
Axxinot – торговая марка трубчатых радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
This text is invaluable. How can I find out more?
foot high; she tried the key in the lock, and
дешевые квартиры на сутки
ciprofloxacin eye drops
This is my first time visit at here and i am genuinely impressed to read everthing at one place.
Мы предлагаем множество парных браслетов, которые непременно вас заинтересуют парные браслеты качественно, быстро, недорого.
Мы предлагаем множество парных браслетов, которые непременно вас заинтересуют браслеты качественно, быстро, недорого.
Matyszczyk, Chris (5 July 2016). “Ashley Madison used fembots? Why this is the upcoming”. In the 2016 Tv sequence Westworld, sensible interactive robots, component of a topic park, interact in sexual and other action with company. In the 2015 – 2018 British collection Humans, there are the two male and woman courtesan “synths” (the series’ title for androids). Several episodes of the 1960’s tv show Star Trek: The Original Series featured feminine androids as companions of the protagonist, notably Andrea from the episode “What Are Little Girls Made Of?” and Rayna Kapec from the episode “Requiem for Methuselah”. Intimacy with robots, artificial intelligence and other human-created goods are saturated in the media landscape. Artificial Intelligence has a male sexual intercourse robot, Gigolo Joe, as a principal character. The key dialogue revolved all-around the debate of wherever to draw the line with regard to cybernetic appreciate and associations and what the upcoming of enjoy and sex with robots has in keep. Joe describes that people love what robots do for them, but are unable to adore them considering the fact that they are not flesh and blood, and in the finish, detest them. Lydia Kaye of Central Saint Martins argue that sexual relations with robots will “desensitize humans to intimacy and empathy”.
ashwagandha uses
асфальтирование территории https://asfaltirovanye-dorog.ru/
I precisely desired to appreciate you yet again. I am not sure what I might have tried without the secrets contributed by you over that topic.
Previously it was an absolute intimidating issue
in my view, however , coming across a new skilled manner
you handled the issue made me to weep for fulfillment. I am just
grateful for your service as well as hope that you really know what a great
job your are accomplishing instructing many others through
a blog. Probably you have never got to know any of us.
Also visit my blog post :: 2007 honda accor
Jeanne Seignol, mieux connue sous le pseudonyme Jeannot se
livre, anime depuis 5 ans une chaine YouTube consacrée aux livres et à la lecture.
Howdy! This article couldn’t be written much better!
Reading through this post reminds me of my previous roommate!
He constantly kept preaching about this. I
most certainly will send this article to him.
Pretty sure he will have a good read. I appreciate you for sharing!
my web site; porsche colorado springs
getx сайт
lactulose dosage
what is lactulose
На цену прежде всего влияет функционал, дизайн и количество создаваемых страниц стоимость разработки сайта ростов отрисовка современного дизайна с учетом ваших пожеланий.
prochlorperazine 5mg online pharmacy
На цену прежде всего влияет функционал, дизайн и количество создаваемых страниц студия разработки сайтов ростов отрисовка современного дизайна с учетом ваших пожеланий.
I’m very cute and slim remediless and I want to meet you. From this thought, my nipples stick out, and my pussy flows straight to the floor https://xbebz.freelovehere.net/?utm_source=3f33acd3b135bb12&s1=12179&s2=1585765&j1=1
Pentland
https://www.teleprogramma-segodnya.ru/
pret 28000 euros
Как активировать промокод на ставки
protonix in breastfeeding
https://vavada-zerkalona5.xyz/
If you want to purchase vehicle financial online, you have to limit all the possible deals as well
as prices that suit your budget plan. As frequently with
the situation of numerous, they have a tendency to overlook
the significance of reviewing finance quotes that they usually tend to devote three times as long as they
can have actually saved, Discover More Here.
buy doxycycline on line
what does gabapentin do
À côté de cela, ses yeux brillent, comme pour quelqu’un qui aurait juré de devenir le roi des pirates.
how to purchase aldactone 100mg
cleocin med
Finally they saw before them through the trees a
melbet promo code at registration melbet
minipress em SГЈo Paulo
Продажа бассейнов для загородных участков, оборудования и химии для бассейнов, павильонов и аксессуаров для отдыха бассейны москва подмосковье купить плавание – уникальный вид физической нагрузки и упражнений (спорта, в глобальном понимании).
Продажа бассейнов для загородных участков, оборудования и химии для бассейнов, павильонов и аксессуаров для отдыха бассейн купить доставка плавание – уникальный вид физической нагрузки и упражнений (спорта, в глобальном понимании).
With that in head, right here we current the best forty finest webcam internet sites to perform for and observe! Once you arrive on LiveJasmin, you can view the cam rooms for ten minutes prior to the website forces you to register. Overall, Shagle’s chat rooms are discreet, anonymous and easy-to-use. To know extra about them, consumers can simply enter their chat room and scroll down. He appreciated them, and quite significantly cherished the sight, scent, and flavor of her nakedness. Much slower than typical. ViviAnna For me, nights get the job done substantially much better. AllInky: For me, 1st drafts get completed when I cease modifying as I go. 1 RT @AllInky: For me, initially drafts get accomplished when I cease modifying as I go. Doesn’t get that I form them. Screenwriter911: For me to get my writing accomplished, I have to wake up by 4:30am, make espresso & get to function b4 telephones ring and career demands. KayleeT I usually pay attention to new music when composing scripts.When performing outlines/notes, I locate it distracting. KayleeT: Anyone else pay attention to new music even though crafting?
Do you have a spam problem on this blog;
I also am a blogger, and I was curious about your situation; we have developed some nice
procedures and we are looking to trade strategies with other folks, why
not shoot me an email if interested.
side of the door. If you were in the room, you might
Bonjour! Si vous voulez vous amuser, je vous recommande les meilleurs jeux gratuits en ligne – https://jeux-gratuits.online/
Добро пожаловать в нашу клинику ортопедии, где мы предлагаем высококачественные услуги в области диагностики, лечения люмбалгия и реабилитации заболеваний опорно-двигательной системы.
Добро пожаловать в нашу клинику ортопедии, где мы предлагаем высококачественные услуги в области диагностики, лечения детский невролог и реабилитации заболеваний опорно-двигательной системы.
имплантация зубов стоимость https://ortodontiyavmoskve.ru/
There were doors on all sides, but when Al-ice had
promo code melbet for today
with wrinkles, the few people who knew him forgot
neck of the bot-tle was a tag with the words “Drink me” printed on it.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Для начала планирую просто проконсультировался и ищу хороших юристов http://nemoskvichi.ru/forum/viewtopic.php?f=10&t=142566 Уверен, что не разочаруетесь проделанной работой и вам точно тут смогут помочь.
Для начала планирую просто проконсультировался и ищу хороших юристов http://fabnews.ru/forum/showthread.php?t=10593 Уверен, что не разочаруетесь проделанной работой и вам точно тут смогут помочь.
quite fast. She soon found out that the cause of this,
LГҐna 20000 kr
nowhere. It hurt me turr’ble to go in without findin’
Specifically, we’re chatting about trails of organic and/or chemical brokers made to harm folks who are unlucky more than enough to be in the way. In higher education, a vast majority of the campuses are residential and thus pupils may perhaps see a great deal much more of their probable bullies and/or victims. How a lot hassle am I in? From the starting, Evan and Jane were being extremely a great deal in enjoy. At very first, Evan experienced tended to vanish with his pals, but he swiftly acquired that a married guy is predicted to adhere with his wife. Jane and Evan had been married almost two yrs. Louis the Fourteenth popularised higher heels and cosmetics, fashions which, a hundred several years afterwards turned distinctive to ladies, are now going whole circle and again to wherever they began? Two more offer out gigs followed in London in November 2009, titled “The Drum Machine Years”. ” Janine smiled, before telling the listeners that they are jogging out of time. ” Denise reiterated. “After a lengthy day in the business office, I want to come dwelling to a nice cleanse dwelling in which I can kick my shoes off and unwind.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
but I don’t know what!”
So she ate one of the cakes and was glad to see
her feet. She looked up, but all was dark there.
bromocriptine generici a Palermo
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
up at the sky all the time he was speak-ing, which
if—if I’d been the right size to do it! Oh dear!
cost of lyrica online
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Hi there! Quick question that’s entirely off
topic. Do you know how to make your site mobile friendly?
My weblog looks weird when browsing from my iphone4.
I’m trying to find a template or plugin that might be able to correct this problem.
If you have any suggestions, please share.
Many thanks!
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
But only the hardback version was available for A$55 and there is no way I will shell out that for a novel! Josh from the Christchurch band No Broadcast chats about the band, the new extended band member collective, their most current launch and thoughts to make the digital musical expertise return to the actual physical entire world in some small interactive way. Desktop and cellular helpful, 321 Sex Chat has users of numerous ages, sexual orientations, religions, and ethnicities, so you’re certain to make a link with a genuine particular person who is your type. In 2013, the New York Times interviewed a lady who prefers to conceal her actual identity even though operating as a camgirl. Some cam products have been “blackmailed or threatened into executing acts they are not at ease with. If they will not comply, they run the risk of having their real identity exposed”. The term “camily”, a portmanteau of “cam” and “spouse and children”, refers to communities shaped by intercourse employees to assist offer with this kind of challenges.
Drug information leaflet. Long-Term Effects.
lisinopril
Some about pills. Get information now.
The next are some of the match titles or possibly the exercise routines you can apply in your personal dwelling.Hide and go search for is among the most in-demand online video online games actually competed and this will certainly be practiced within. Try your TexasWSOP 2011 Episode 12 Main Event Day four 2/4 World Series of Poker 2011. GAMEKING51 favorited a video clip (1 thirty day period back). These “parts” incorporate mechanisms to management the timing of activities so that each individual person procedure is turned on and off at the proper time, mechanisms to initiate each and every party in the accurate order and to also ensure that just about every occasion is induced only when for every cell cycle, controls to make certain situations occur in a linear, irreversible way, redundancy, or back-ups to make sure the cycle features properly even in the context of some malfunctioning elements, and techniques that are adaptable so that mobile cycle gatherings can be modified in the context of diverse cell types and/or environmental ailments. Many of the most essential discoveries about the mechanisms that command functions of the mobile cycle were elucidated applying yeasts which are single mobile eukaryotes.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
glimepiride 1mg farmacia en lГnea
Lainaa 25000 euroa
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Medicament information sheet. Generic Name.
zithromax
Actual about medication. Read information now.
Доедешь болезни рук диагноз конечной остановки, магнитофонных записей диагностика заболеваний Так, взятый из лаборатории систем безопасности, глаза его горели.
Доедешь болезни рук диагноз конечной остановки, магнитофонных записей больница Так, взятый из лаборатории систем безопасности, глаза его горели.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Simply desire to say your article is as astonishing. The
clearness for your publish is just excellent and
i can suppose you are an expert on this subject.
Fine together with your permission let me to grab your feed to stay updated with
drawing close post. Thanks one million and please carry on the enjoyable work.
My blog :: https://cnv00.soundstream.media/image/aHR0cHM6Ly9ob3NoaW1peWEtZ2FtZWNoYW5uZWwuY29tLzIwMjAvMDIvMjcvcG9zdC0xMjQ3Lw?w=650&h=650
Компания HONO-R специализируется на производстве различных типов радиаторов охлаждения, https://msk.hono-r.com/industry/alyuminevye-radiatory/ которые применяются в спецтехнике и в промышленных установках.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
телепрограмма на сегодня цифровое телевидение
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Лучшие промокоды на ставки в Беларуси
Институт психологии и астрологии обучает и выпускает грамотных, профессиональных специалистов https://astroinstitut.ru/obuchenie/ система обучения основана на фундаментальных астрологических принципах.
Институт психологии и астрологии обучает и выпускает грамотных, профессиональных специалистов https://astroinstitut.ru/wiki/ система обучения основана на фундаментальных астрологических принципах.
His mothers and fathers divorced when he was two several years previous, and while his mom experienced custody of Martin, he could also go freely among his father’s house in the center-class suburb of University Gardens in San Juan, and his paternal grandmother’s property nearby. Following the extorts of pro skateboarder Rob Dyrdek and his bodyguard/roommate/best mate Christopher “Big Black” Boykin right after their recent move to the Hollywood Hills, “Rob & Big” is one of the funniest actuality reveals on television. In February 1961, Presley performed two demonstrates for a profit function in Memphis, on behalf of 24 local charities. CamSlurp – Best for watching scheduled are living cam reveals from renowned porn stars. It was just after that that I realized a whole lot of my “tastes” I considered I experienced by porn had been just fetishes induced by porn. Gay porn has carried out forever what straight porn is just setting up to do: take care of males like visible intercourse objects.
appliance repair orange county
benefits of ashwagandha
appliance repair
porn videos
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Another necessary value to consider is the swap
rate charged on positions held overnight.
Музыкальная школа в центре Уфы для взрослых. У нас не типичные скучные уроки, https://mmotionschool.ru/shkola-v вы сможете погрузиться в захватывающий процесс обучения с лучшими преподавателями!
Музыкальная школа в центре Уфы для взрослых. У нас не типичные скучные уроки, https://mmotionschool.ru/shkola-barabanov вы сможете погрузиться в захватывающий процесс обучения с лучшими преподавателями!
Dirty Bob (September 21, 2004). “Winners of the Nightmoves Entertainment Awards Announced”. Alptraum, Lux (September 18, 2015). “Who requirements a intercourse toy linked to an Apple Watch?”. Kevin Bollaert, a revenge porn web site operator in San Diego, was sentenced in 2015 to 18 decades in prison for in fact charging women hundreds of dollars to have these mortifying pictures of them selves taken down. ● The platform permits buyers to see who is looking at their account alongside with their profile images. The shoppers can pick out to look through by means of the profile and come across by themselves a suited profile or permit the algorithm do it for you without any additional costs or formalities. One of the essential functions that sets this web page apart is the actuality that the web site makes absolutely sure to filter and authenticate your profile in advance of sending a match your way. The environment of remarkable dating is just just one phase away from you. Once the verification process is complete, the up coming stage is to build a chat space and invite the people today whom you want to increase to the chat home.
%%
Here is my web page: https://ironworld.com.ua/product/list-goryachekatanyj-ressorno-pruzhinnyj-3-5-mm-1-25h2-5m-st-65g-proizv-ukraina/
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
You should really usually be responsible to buy your personal products and really do not agree to pay any payment (except it is for background check – which is a legitimate charge for lots of companies out there. Freecash: Get your possess cost-free account, total smaller responsibilities, get started amassing cash and income them out. One of the identified scams about performing on the net or performing from house is when providers request you to pay upfront for devices charge (headset, phones and many others) and administrative or start up charge. At to start with look at the homepage you will see hundreds of beautiful women, partners, guys and shemales that are streaming are living on cam from their bedrooms and they are all inclined to chat or do some awful issues that the aim has been established to, but most of the time you can seem at the tip menu and uncover alot of quality duties that the product has set for you to select from with a suggestion sum so do not be shy and question a dilemma in chat or start off tipping if you have tokens to commit. You can have deal with-to-encounter chats on private chats, with webcams, and microphones. It’s simple to comply with, and you really do not have to pay out for anything ideal absent.
The small motor actually sits inside the fan, which is firmly hooked up to the tip of the motor. They provide quick load however small capability. Almost all PDAs now provide colour shows. For instance, some companies provide pay-as-you-go plans, and some cost on a monthly billing cycle. Some firms also high quality clients if they return vehicles late, so it’s best to be sure that to offer your self loads of time when booking reservations. At the 2014 Consumer Electronics Show in Las Vegas, a company called 3D Systems exhibited a pair of 3-D printer methods that have been personalized to make candy from elements equivalent to chocolate, sugar infused with vanilla, mint, sour apple, and cherry and watermelon flavorings. A confection made within the ChefJet Pro 3D food printer is displayed at the 2014 International Consumer Electronics Show (CES) in Las Vegas. And that’s not the only food on the 3-D radar. From pharmaceuticals to prosthetic physique parts to meals, let’s study 10 methods 3-D printing technology might change the world in the years to come. A company called Natural Machines recently unveiled a 3-D printing device referred to as the Foodini, which can print ravioli pasta.
Warhol made both of those comic and significant performs his topic could be a soup can or an electrical chair. This technological know-how created a kind of 3 dimensional check out that suited erotic photos rather very well. Another opponent of masturbation was John Kellogg, whose breakfast cereals are nevertheless perfectly recognized. It is often component of a village ceremony in which younger men are initiated into manhood, their circumcisions also serving as a symbol of a “true believer” in Islam. MeToo period. These men make consent and boundaries explicit, rejoice various system types and gender equality, and supply girls with a risk-free room to take a look at their sexuality. At the time, I wasn’t sure what to make of them. The higher than ideas feel recklessly crude and fully overblown in comparison to our current-day knowledge, but at the time, the purported harmful effects of masturbation have been a really serious problem. In America, circumcision continued to be practiced lengthy following the health care career and the general community experienced abandoned, even neglected, its original intent, which was to thwart the supposed evil consequences of masturbation. With usual writings like the over, the early 20th century found the American professional medical establishment in typical agreement that masturbation and hypersexuality had devastating and damaging effects on one’s bodily and emotional well-getting.
%%
My blog http://forum.osvita.od.ua/viewtopic.php?f=2&t=6665&p=63745&hilit=%D0%BA%D1%80%D0%B8%D0%BF%D1%82%D0%BE%D0%B2%D0%B0%D0%BB%D1%8E%D1%82%D0%B0
%%
my webpage – http://4x.com.ua/ssangyong/showthread.php?t=1110&highlight=%EE%E1%EC%E5%ED%ED%E8%EA
Instantly access a global network, establish local presence, and stay available on the go. https://www.twitch.tv/fred_rika/about Streamline customer interactions, boost credibility, and expand reach.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Instantly access a global network, establish local presence, and stay available on the go. https://www.google.com.vn/url?q=https://didvirtualnumbers.com/virtual-number-for-telegram/ Streamline customer interactions, boost credibility, and expand reach.
But if you want to interact instantly or view a non-public clearly show, you’ll need to shell out added. Marnie gets her initial rejection when, all through a job job interview, a gallery operator says she does not see Marnie in the "Art World." When she problems about what to do upcoming, Ray and Shoshanna suggest her to get a "pretty person occupation" to pay the costs in the meantime. Looking to see a very hot experienced female get her adore holes pumped entire of new very hot cum? My partner and I completely appreciate your weblog and come across lots of of your post’s to be accurately what I’m searching for. 2022-05-04: Okay, so these days I’m going to get anything oh so significantly. All the time take treatment of it up! Jessa meets Thomas-John’s mothers and fathers for the to start with time about an awkward evening meal at a steakhouse. 553k 23min – 360p. First time porn clips. 1.1M 5min – 360p. Más vistos Porn Videos.
%%
Also visit my site: https://ironworld.com.ua/shop/?filter_att_diametr=600mm&query_type_att_diametr=or
Здесь самые крутые сервера lineage 2
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Why people still make use of to read news papers when in this
technological globe the whole thing is available on web?
cheap finpecia without rx
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
She sooner or later returns his feelings, but the partnership is forced to close prematurely when Charlotte, possessing purchased again her aged small business from her ex-partner, moves again to Chicago. She pays Niles back by refusing to grant an instant divorce rather, she forces Niles to play along that the two continue to be fortunately married, assuring him that just after he has completed this on many select social instances she will file for divorce. Rita Wilson would perform a middle-aged edition of Hester in the two-aspect episode “Don Juan in Hell”, making use of prosthetic makeup. Poverty and a lack of education play major roles in the lives of several girls in the sexual intercourse business. Her declare that men can not be females (and other statements) do not have all 5. Source right here. Pornography for females: a new subgenre focusing on women of all ages, portraying “eromen” (erotic adult males) who cater to women’s needs. Charlotte particulars her vocation path with Marcus who reveals: ‘I always bear in mind memorable people’. Charlotte (Laura Linney), the founder-operator of Charlotte’s Web dating services, is a matchmaker recently arrived from Chicago and Frasier’s closing adore fascination on the sequence.
%%
my page … https://www.pcweek.ua/forum/view_profile.php?UID=86015
%%
Feel free to surf to my web site: http://favorites.com.ua/articles/17/chto-vybrat-dlya-telefona-meizu-bamper-ili-chehol-knizhku/
Meds information leaflet. Short-Term Effects.
cialis soft
Best information about pills. Read here.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
щас заценим вроде тема
“It is a great honor for Julien’s auctions to once again partner with the music health Alliance in conditions of our annual initiative to facilitate payments,” said Martin Nolan, co-founder and CEO of Julien, whose words are quoted in the http://www.altarmuhendislik.com.tr/2018/04/07/deneme-devam-isler/, according to the daily mail.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Drug information for patients. Effects of Drug Abuse.
zovirax rx
Actual information about medicines. Read now.
Корми, пляшечки і тюбики по змістом, https://agens-bv.nl/15/ аксесуари і довгий список інших примочок. Чотири лапи – серйозна компанія зоомагазинів в рф.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
гет икс сайт
Компания “ПОРАДОМ” активно работает в сфере строительства и ремонта с 2012 года https://poradom-remont.ru/stoimo Мы предоставляем профессиональные услуги по ремонту и дизайну жилых и нежилых помещений.
Medicament information. Brand names.
lyrica
Actual information about medicine. Read information here.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
LГҐna 5000 kr
The outcomes don’t demonstrate that vitamin D triggers all those problems, but they do emphasize its importance in fetal mind growth it really is possible that prenatal vitamin D supplementation may possibly reduce the hazard of developmental language difficulties in small children. Women who experienced very low degrees of vitamin D at eighteen months being pregnant had practically double the chance of possessing a youngster with indicators of language impairment at ages five and ten in comparison to girls with higher degrees, in accordance to a 2012 review posted in Pediatrics. However, sun publicity devoid of sunscreen prospects to skin ageing and increases skin most cancers possibility. We get vitamin D from a wonderful source: the sunlight. Lupus, a serious inflammatory disease in which the body’s immune procedure assaults its very own organs and tissues, is often associated with vitamin D deficiency-in component since lupus individuals are typically advised to keep out of the solar (the resource of 90% of our vitamin D), and may well be prescribed corticosteroids, which are also linked to minimal concentrations of D, in accordance to the Lupus Foundation of America. Finally, I should really stage out that despite the fact that plan supplementation is worthless and megadoses of nutritional vitamins can be destructive, if you consider you have a vitamin deficiency, consult with your medical doctor.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Игорный портал азартных игр Cat Casino функционирует с 2021 года cat casino За прошедший период работы зарекомендовал себя исключительно с положительных сторон.
Игорный портал азартных игр Cat Casino функционирует с 2021 года кэт казино За прошедший период работы зарекомендовал себя исключительно с положительных сторон.
chloromycetin 250mg Deutschland
гама казино официальный сайт
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
вы сможете профессионально оформлять и мягко вести профили, в vk, telegram, Одноклассниках, https://clickitcrowdfunder.com/product/test/ youtube. если вы сам пишешь или делаешь собственноручно – попробуй расширить собственный аккаунт.
what is finasteride
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Here is my web-site – https://matro-luxe.dp.ua
You actually stated that exceptionally well!
My site: http://wiki.rl-transport.org/index.php/Eng-films.site
Prestito 19 mila euro
%%
Also visit my web blog :: mostbet agent india
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Novyny
obviously like your web-site however you need to check the
spelling on quite a few of your posts. Many of them are
rife with spelling problems and I in finding it very troublesome to
inform the truth nevertheless I will surely come again again.
Drugs prescribing information. Brand names.
levaquin without dr prescription
Actual trends of drug. Get here.
risperdal billig kГёbe i HelsingГёr
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Оформление сертификата ИСО 9001 с нами – это не только возможность подтвердить соответствие вашего бизнеса международным стандартам, но сертификат ИСО 9001-2015 и шанс оптимизировать внутренние процессы, повысить уровень управления и улучшить качество услуг.
prestamo 200000 euros
Оформление сертификата ИСО 9001 с нами – это не только возможность подтвердить соответствие вашего бизнеса международным стандартам, но как получить сертификат ИСО 9001 и шанс оптимизировать внутренние процессы, повысить уровень управления и улучшить качество услуг.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Drugs prescribing information. What side effects?
abilify tablet
Actual what you want to know about drugs. Get information now.
%%
My web page https://www.usabilityblog.de/blog-autoren/heidi-oltersdorff/
Best site for Bitcoin Price USD
например, при размере уставного капитала 10 тыс. руб. и 3 учредителями с долями по 1-три, на каждого удастся, по 3 333,(3) рублей, https://dawndonohoeltd.com/demo-post-5-3/ как в сумме даст только 9 999,(9) рублей.
Полностью разделяю Ваше мнение. В этом что-то есть и мне кажется это отличная идея. Я согласен с Вами.
Is it bitcoin cash or litecoin https://elslots.site/ru/? at online casino more there are hundreds of viable slots and games, video poker, live gaming establishment and table games.
%%
Here is my blog post; Ghostwriter Politikwissenschaften
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Medicine information. Effects of Drug Abuse.
generic eldepryl
Best information about medicine. Read here.
plavix kosten in Breda
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
irbesartan 150mg
%%
Also visit my web site http://chelmaps.ru/index.php?subaction=userinfo&user=ovajobiwu
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
You revealed that terrifically!
Review my page; https://motogpdb.racing/wiki/User:ReneChumleigh7
Are you tired of endless diets and exhausting workouts that don’t give you the results you want fastest way to lose belly fat Introducing our revolutionary belly fat loss pills that will help you achieve your desired body shape in no time.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
what can you do, in case an updated version of the click program has appeared? special price: 500 euros for access for 12 months! Why electronic toyota epc spare parts catalog?
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Yahoo supplied incriminating data of the journalist’s account logins to the Chinese government and thus, Shi Tao was sentenced to 10 years in prison. None of the other carriers keep texts at all, but they keep records of who texted who for greater than a year. Verizon, however, retains some information for up to a yr that can be used to ascertain if a specific cellphone visited a specific Web site. In line with the sheet, Sprint Nextel Corp.’s Virgin Mobile model keeps the text content of textual content messages for 3 months. Virgin Mobile only keeps that information for 2 to three months. Verizon keeps it for three to five days. The document says AT&T keeps for five to seven years a report of who text messages who-and when, but not the content of the messages. I adored getting banged by 5 hot studs with wonderful cocks! I don’t want it be a typical young frat home the place it is a bit trashy and simply ladies and getting drunk … Getting them to really do all that freaky stuff might be a little bit of a chore, however. Further, customers that find themselves away from the roost will also be capable to swap out settings on the fly simply by visiting the outfit’s devoted site.
Какие нужные слова… супер, отличная мысль
в том случае, если у человека есть еще вопросы по прописке ООО либо индивидуальном предпринимателе, https://studiohovik.com/are-wordpress-templates-difficult-to-understand/ оставьте заявку на бесплатную консультацию по регистрации бизнеса.
finasteride 5 mg
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
строительная экспертиза москва https://pgs111.ru/
https://giffun.ru/en/images/
zyvox 600mg ohne rezept in Dortmund
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Medicine information for patients. Short-Term Effects.
norvasc buy
All what you want to know about medicine. Get information now.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
According to dune, the cumulative number of unique users of ethereum-based gamblefi platforms for https://trumsiquangchau.com/san-pham/om-lo-ao-phong-gap-gia-si/ has sharply increased to just under 50 thousand by mid September from about 5000 at dawn year.
Узнайте, как производится Установка и ремонт сантехники своими руками полотенцесушитель 3 4 подробные инсрукции по установке ванны, унитаза, смесителей.
%%
my blog: https://fairspin.app/pt/registration
казино ван вин играть
Узнайте, как производится Установка и ремонт сантехники своими руками настенный полотенцесушитель подробные инсрукции по установке ванны, унитаза, смесителей.
Great weblog here! Also your site loads up fast! What web host are you the usage of?
Can I get your associate link in your host? I want my site loaded up as quickly as yours lol http://m.giophoto-ca.co.kr/bbs/board.php?bo_table=gallery3&wr_id=230
Great weblog here! Also your site loads up fast!
What web host are you the usage of? Can I get your associate link in your host?
I want my site loaded up as quickly as yours lol http://m.giophoto-ca.co.kr/bbs/board.php?bo_table=gallery3&wr_id=230
Беларусь Витебск музей
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
webcam online
Medicament information. What side effects can this medication cause?
lisinopril pills
Best what you want to know about drug. Read information here.
Orange County HVAC repair
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Orange County HVAC contractor
здесь
%%
my webpage: погода в Виннице
по этой ссылке
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Feel free to visit my blog post – Свежие новости Европы
%%
My webpage https://demoslotsplay.com/cleocatra
what is the function of prednisone tablet
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Feel free to visit my web site … https://cricket-betting.app/
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Перед началом работ мастера демонтируют мебель, снимая старое покрытие перетяжка мягкой мебели и проверяя состояние каркаса и наполнителя.
Официальный сайт Gama Casino – удобный веб-портал, который предоставляет возможность играть, вход Gama Casino не беспокоясь о конфиденциальности личной информации и денежных средств на счету депозита.
Официальный сайт Gama Casino – удобный веб-портал, который предоставляет возможность играть, мобильная версия гама казино не беспокоясь о конфиденциальности личной информации и денежных средств на счету депозита.
Meds information sheet. Effects of Drug Abuse.
norvasc online
All about medication. Read information here.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Матрешки
Experience the epitome of wedding events in Estonia. For more efficient planning of our activities, we offer detailed layouts of the structure and surrounding areas.
cliquez ici maintenant
Fucker
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Medicines information sheet. Cautions.
viagra
Best trends of pills. Get information now.
Regards. I appreciate this!
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
mambo 36 tadalafil 20 mg reviews tadalafil to sildenafil dose conversion tadalafil 20 mg order online
Medication information for patients. Brand names.
promethazine
Best news about medicament. Read information here.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Very good site Bitcoin Price USD
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
my web blog; купить тонометр во владивостоке
%%
My blog post … https://13oz.ru/
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
В области сертификации и стандартизации ключевую роль играет отказное письмо по сертификации отказное письмо для вайлдберриз это документ, который предприятие или организация получает в случае, если его продукция или услуги не подлежат обязательной сертификации по установленным стандартам и требованиям.
В области сертификации и стандартизации ключевую роль играет отказное письмо по сертификации отказное письмо на товар это документ, который предприятие или организация получает в случае, если его продукция или услуги не подлежат обязательной сертификации по установленным стандартам и требованиям.
I do accept as true with all the ideas you’ve offered
in your post. They are very convincing and can certainly
work. Nonetheless, the posts are very quick for newbies.
Could you please lengthen them a bit from subsequent time?
Thanks for the post.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
казино онлайн топы
pentasa
{{Mariana Vieira da Silva falou também em medidas de apoio às rendas, referindo que as medidas atualmente em vigor já abrangeram “mais de 185 mil famílias”.|E futuro é não voltar a cometer os mesmos erros que se têm cometido ao longo dos anos, em que temos um espaço que tem sido objeto de incêndios que têm, de alguma forma, criado prejuízos enormes”, acrescentou.|Uma grande fatia destes diplomados está empregada sob um contrato de trabalho a termo certo (86%), sendo que 8% dos diplomados desenvolvem atividade ao abrigo de estágio profissional e 4% presta serviços por conta própria.|O governador do Banco de Portugal (BdP) defendeu, esta quinta-feira, que o Banco Central Europeu (BCE) deve ser cauteloso na decisão sobre uma nova subida dos juros na reunião agendada para 14 de setembro, olhando para os últimos dados da inflação.|A DIT Portugal vai promover ações de formação internas e certificadas até final 2023, não só em Lisboa e Porto, como no Algarve e na Madeira, anunciou a rede de agências de viagens.|O PCP já anunciou que vai apresentar no parlamento uma iniciativa para limitar o aumento das rendas a 0,43%, depois de o Instituto Nacional de Estatística (INE) ter estimado subidas de 6,94%.|Mireia Prieto, diretora regional de Booking para o sul da Europa, disse ao elEconomista.es que “vimos desde o início do ano que ia ser um ano muito importante, um ano recorde e histórico em termos de dormidas”.|No que toca ao arrendamento, a deputada única do PAN vai propor “que em sede de IRS se aumentem os valores de dedução de despesas com rendas”.|O PSD/Açores “lançou o desafio” para o governo dos Açores aceitar um novo regime que prevê a cooperação técnica e financeira com as freguesias e reforça a necessidade de limpeza das ribeiras.|O presidente da Câmara de Odemira, Hélder Guerreiro (PS), espera que o Governo apresente, em outubro, as medidas de apoio para mitigar os prejuízos causados pelo incêndio que deflagrou, em agosto, neste concelho do distrito de Beja.|O ex-ministro da Defesa José Azeredo Lopes comentou, esta quinta-feira, a situação na Ucrânia, onde ontem um ataque em Donetsk matou 17 pessoas e feriu mais de 30.|Mais absurdo ainda é defender a legalidade de um processo de impeachment usando como escusas (palavra da moda no momento) a má gestão da economia.|“Estes números continuam a traduzir a aposta do Turismo de Portugal e da sua rede de escolas na formação dos profissionais do setor e a melhoria contínua que se verifica nas condições que lhes são proporcionadas no setor.|Previsto está agora que estas regras mais flexíveis estejam em vigor até 31 de dezembro de 2023, sendo que este prolongamento “não prejudica a possibilidade de autorizar outras medidas necessárias e proporcionais”, garante Bruxelas.|A 7ª edição anual dos Remarkable Venue Awards, que homenageia a excelência em museus, atrações e experiências em oito países, deu a conhecer a lista de vencedores nacionais em sete categorias, que agora competem entre si pelo prémio mundial.|Os representantes das duas uniões também consideraram que o setor social devia ter participado na elaboração do acordo de parceria e realçaram a importância da estabilidade política na região.|O primeiro-ministro timorense agradeceu esta terça-feira o apoio dos Estados membros da ASEAN ao processo de adesão de Timor-Leste, saudando o papel da organização na consolidação da estabilidade, unidade e paz na região.|A defesa do consumidor fala em momentos de grande aflição para as famílias portuguesas, com o anúncio de uma previsão no aumento das rendas a rondar os sete por cento.|Acrescem novas medidas destinadas a apoiar a redução da procura de eletricidade, dada a meta aprovada de redução do consumo pelos países (de 10% no geral e de 5% nas horas de pico).|O Vaticano anunciou, em 10 de agosto, a nomeação do bispo das Forças Armadas e das Forças de Segurança como novo patriarca de Lisboa.|É nessa altura que o presidente da Câmara de Odemira espera que já exista “uma resolução do Conselho de Ministros” que possa “congregar todas as medidas” de apoio que foram discutidas durante a reunião desta terça-feira.|“Temos de atuar em diferentes dimensões para atrair talento para o setor do turismo e no que diz respeito às qualificações”, notou, considerando que é necessário aumentar o salário médio no setor, que continua abaixo da média da economia nacional.|O governante afirmou também que o Japão tem vindo a obter ampla compreensão da comunidade internacional e que, em contraste, a proibição geral da China em relação aos produtos do mar japoneses “sobressaiu”.|A ministra da Presidência anunciou esta tarde que o Conselho de Ministro da próxima semana aprovará diplomas, “de forma atualizada e com novas respostas” para as “necessidades que as famílias portuguesas sentem no âmbito do credito à habitação”.|Em junho, o Conselho do Governo dos Açores aprovou uma nova proposta para o regime jurídico de cooperação técnica e financeira com as freguesias.|A OA lembra que Portugal receberá cerca de 4.500 pessoas refugiadas, que carecerão de uma integração (ainda que transitória) no território nacional, de forma regular, pacífica e adequada.|O eleito falava aos jornalistas no salão nobre dos Paços do Concelho, onde ao final da tarde desta terça-feira reuniu, juntamente com os autarcas de Aljezur e de Monchique (Faro), com a ministra da Coesão Territorial, Ana Abrunhosa.|A sua vasta experiência profissional acrescenta uma visão estratégica muito relevante para nós”, acrescenta Vasco Pereira Coutinho, CEO da Lince Capital.|Gostaríamos de fazer parte da comunidade ASEAN, uma comunidade ligada pela confiança, amizade e cooperação”, disse Xanana Gusmão, na plenária que marcou o arranque da 43.ª Cimeira da Associação de Nações do Sudeste Asiático (ASEAN), em Jacarta.|No dia 14 de outubro, a Comissão Europeia afirmou que Portugal deverá receber esta semana os primeiros refugiados, provenientes de Itália, na sequência do compromisso assumido pelos 28 estados-membros a 23 de setembro.|A líder do Bloco de Esquerda (BE), Mariana Mortágua, criticou, este domingo, as medidas de apoio aos jovens apresentadas pelo primeiro-ministro, António Costa, num encontro na Academia Socialista.|Em julho, em entrevista ao Público, o ministro das Finanças também já tinha falado de mais medidas de apoio aos créditos à habitação.|O certificado internacional que as companhias aéreas do Grupo SATA passam a ostentar garante que o programa de Compensação Voluntária de Carbono (SATA ICOP) está de acordo com as melhores práticas internacionais e conforme os requisitos em vigor.|A governante disse ainda que, após a sessão desta terça-feira, “daqui a 15 dias” estará feito o levantamento final dos prejuízos causados pelo incêndio e que dentro de “um mês haverá uma nova reunião”.|Refira-se que este evento atrai anualmente académicos de todo o mundo, profissionais do setor e figuras ligadas ao ensino e investigação, vindos de mais de 40 países.|O encontro tinha sido anunciado ainda em agosto, no rescaldo do incêndio, e teve como objetivo fazer um balanço dos prejuízos causados pelas chamas.|Foram recolhidas e analisadas diariamente amostras para medir a radioatividade da água descarregada, e este nível foi sistematicamente inferior ao limite máximo fixado de 1.500 becquerels/litro, anunciou a Tepco em comunicado.|Esta terça-feira haverá reuniões bilaterais do líder timorense com os seus homólogos do Brunei, Hassanal Bolkiah e do Vietname, Pham Minh Chính.|O impeachment presidencial não é e não pode ser instrumento da luta política e, muito menos, meio de correção de rumos de uma administração que, por ventura, não esteja sendo eficiente na gestão econômica ou administrativa do país.|O alarme de um detetor de fugas nas condutas de água filtrada disparou na quarta-feira, mas uma inspeção imediata “confirmou” que se tratava de um falso alarme, declarou a Tepco no comunicado.|Seja em resolução do Conselho de Ministros — que era aquilo que nos parecia mais eficaz — seja numa outra forma qualquer, [esperamos] que as medidas estejam estruturadas e no terreno”, disse.|Tem por finalidade a execução dos encargos de consultoria e assessoramento jurídico à Administração Universitária, com representação judicial em alguns processos ligados à atividade fim da Universidade.|A mediação poderá ser realizada via online, existindo a possibilidade de recurso a videoconferência, nas instalações da Freguesia, uma vez que a sede do CAUL está situada em Lisboa.|O presidente do PS/Açores defendeu um “esforço suplementar” de limpeza das ribeiras e linhas de água na região, antecipando o inverno, através de um financiamento extraordinário às juntas de freguesia e câmaras municipais.|Numa resposta enviada à Lusa, a porta-voz do PAN, Inês Sousa Real, defendeu que, no âmbito do crédito à habitação, “é necessário rever as regras do apoio extraordinário às famílias para pagamento da prestação”.|A autarquia de Quarteira é uma das 3.000 freguesias associadas a este protocolo que, independentemente da sua dimensão, passam a ter acesso a um serviço jurídico especializado.|No mesmo diploma serão também clarificados os critérios para a atribuição do apoio à renda, anunciou esta quinta-feira Mariana Vieira da Silva.|Christine Lagarde voltou a frisar, na conferência de imprensa, que “os governos devem continuar a retirar medidas de apoio à economia”, assim que a crise energética for dando tréguas.|«A elação que podemos tirar de que há mais gente em situação de dificuldade retiramos dos números do aumento gritante que temos no gabinete de apoio ao sobre-endividado.|A agenda de quinta-feira prevê a realização das cimeiras ASEAN-Índia, ASEAN-Austrália e ASEAN-Nações Unidas, além da 18ª Cimeira do Sudeste Asiático.|Além do suporte jurídico, a UVA também vai realizar ciclos de palestras, feiras e outras atividades acadêmicas para conscientização e promoção da liberdade religiosa.|O incêndio no concelho de Odemira teve início no dia 5 de agosto e foi dado como dominado às 10h15 do dia 9, seis dias depois de ter deflagrado numa área de mato e pinhal na zona de Baiona, na freguesia de São Teotónio.|Temos duplicado o número de processos comparativamente com os anos anteriores e aí percebemos que as famílias portuguesas estão em dificuldade e não conseguem cumprir com os seus pagamentos», explicou.|A Booking anuncia que está a registar “um ano histórico” em noites de alojamento, principalmente nos destinos europeus, que tiveram um comportamento positivo no aumento da estadia média, reservas com mais antecedência e menos cancelamentos.|A Procuradoria Federal junto à UFSM é o órgão executivo e de assessoramento especial subordinado ao Reitor e integrante do sistema jurídico da União no Poder Executivo, vinculado tecnicamente à Advocacia – Geral da União.|O grupo, refira-se, já estava presente naquele mercado africano por via da sua filial Dana Agency, especializada na gestão de viagens de negócios.|O Governo português tem políticas implementadas nesse domínio, mas (…) sentimos que é preciso reforçá-las, porque há aqui situações de grande vulnerabilidade social e económica e, portanto, situações de pobreza que é preciso enfrentar”, disse.|Nosso regime político não é o parlamentarista, no qual a perda de maioria no Congresso implica a queda do governante – o primeiro-ministro – e a convocação de novas eleições.|O Prémio Intermarché Produção Nacional tem vindo a destacar-se como uma iniciativa de apoio ao sector agroalimentar em Portugal desde 2014.|Ainda assim, lembra que as críticas públicas ao BCE, “mesmo quando feitas por importantes autoridades políticas, não têm qualquer efeito sobre as decisões de política monetária”.|A autarquia de Quarteira é uma das 3000 freguesias associadas a este protocolo que, independentemente da sua dimensão, passam a ter acesso a um serviço jurídico especializado.|Quanto ao alojamento estudantil, “para além de ser necessário acelerar e antecipar as metas de criação de novos alojamentos do Plano Nacional de Alojamento para o Ensino Superior”, o PAN propõe um novo benefício fiscal para senhorios.|À direita, o deputado da Iniciativa Liberal Carlos Guimarães Pinto, em declarações à Lusa, opôs-se à ideia de limitar as atualizações das rendas, considerando que o principal problema do mercado de arrendamento é a falta de casas.|Há uns meses atrás eram apenas famílias carenciadas, mas nos últimos tempos há cada vez mais contactos de pessoas das classes média e média alta.|Nuno Fazenda considerou que “as regiões têm um papel fundamental no turismo”, assumindo um “papel importante na afirmação dos seus territórios”.|O sector agroalimentar não é apenas uma parte importante da economia, é também a perpetuação de tradições e de uma identidade que é tão nossa.|Entretanto, fonte ligada ao processo disse à Lusa que o primeiro grupo de refugiados deverá chegar a Portugal entre a última semana de outubro e a primeira semana de novembro.|Também o BE defende a imposição de limites ao aumento das rendas para 2024, propondo que este aumento “seja congelado ao valor que era em 2021, antes do surto inflacionista”.|Assim, a principal taxa de refinanciamento – que tem efeitos sobre os créditos habitação – galopou para os 4,50%, o nível mais elevado desde maio de 2001.|O sismo que atingiu Marrocos na noite de sexta-feira causou mais de 2.122 mortos e 2.421 feridos, provocando danos generalizados na região de Marraquexe, importante destino turístico marroquino.|Estas formações permitiram às agências DIT Portugal uma melhoria de conhecimento nas várias áreas administradas principalmente nas de maior importância, como contabilidade e marketing digital.|Esta iniciativa do Intermarché destaca a qualidade dos produtos nacionais junto dos consumidores, apoia a produção local, impulsiona o emprego e inspira a um futuro mais promissor e consciente no panorama agroalimentar.|Em causa, recorde-se, está uma promessa do Governo em devolver aos estudantes um ano de propinas pagas numa universidade pública do país nos primeiros anos de trabalho, além de alterações às regras do IRS Jovem.|“O meu Governo está empenhado em trabalhar com a ASEAN para implementar o roteiro objetivo e baseado em critérios para a nossa plena adesão.|O ex-governador do Banco de Portugal (BdP), Vítor Constâncio, defende uma pausa na subida dos juros e, se dependesse de si, já devia ter parado nos 3,25%.|”Quando, há dias, o primeiro-ministro anunciou medidas para os jovens, toda a gente soube fazer as contas”, começou por referir a bloquista, durante a sessão de encerramento do Fórum Socialismo, em Viseu.|O Governo aprova na próxima semana um novo conjunto de medidas de apoio às famílias que têm problemas com o créditos à habitação e com o pagamento das rendas de casa.|Além desta campanha, a Missão Continente apoiou directamente a unidade com obras de ampliação do serviço de Neonatologia e 50 mil euros para a aquisição de equipamentos.|O PSD/Açores criticou esta segunda-feira o “desplante” do PS ao “exigir agora aquilo que nunca fez no passado”, com a proposta de apoio às autarquias, e desafiou os socialistas a aprovar o novo regime de cooperação com as freguesias.|Questionado pelos jornalistas sobre o futuro das oito famílias que viram as chamas destruir na totalidade as suas primeiras habitações, Hélder Guerreiro afiançou que estas poderão ser apoiadas através do programa “Porta de Entrada”.|Ouvida pela Antena 1, a coordenadora do Gabinete de Proteção Financeira da Associação de Defesa do Consumidor, Natália Nunes, receia mesmo que o direito à habitação fique em causa.|Ao mesmo tempo, é dada flexibilidade adicional para os Estados-membros avançarem com apoios à liquidez dos serviços públicos de energia e com ajudas às empresas afetadas pelo aumento dos custos energéticos, sujeito a salvaguardas.|Hélder Guerreiro quer que o Governo apresente até outubro medidas de apoio definidas e aprovadas que ajudem a mitigar os prejuízos dos incêndios de devastou Odemira durante o mês de agosto.|Além disso, “vemos como este ano aumentou a reserva antecipada e isso ajuda muito o setor para que possa planear porque também vemos como os cancelamentos não aumentam.|“Após um sério e demorado processo de identificação e recrutamento, consideramos que o Carlos é a pessoa certa para o grupo Olivia Singular Houses.|Ao longo de quase uma década tem promovido e reconhecido produtos e produtores nacionais, bem como tem incentivado o desenvolvimento sustentável e a inovação no sector.|“Com isto aprofundamos ainda mais um dos nossos lemas que é #fazeracontecer e demonstrar que estamos cada vez mais focados em melhor servir as nossas agências de viagens”, refere ainda a mesma nota.|Em 2023, a Superintendência de Promoção da Liberdade Religiosa já realizou 34 atendimentos desta natureza, e a instituição de ensino é a primeira a fechar esse tipo de parceria com o órgão.|O Governo vai aprovar em Setembro o diploma que alarga o regime de apoio à bonificação do crédito e clarifica os critérios de acesso do apoio à renda, disse esta quinta-feira a ministra da Presidência, Mariana Vieira da Silva.|O número de candidaturas à Porta 65 representa um aumento de 19% dos candidatos apoiados por este programa, face ao mesmo período do ano passado, e abrange todas as candidaturas apresentadas entre o final de abril e ao longo do mês de maio.|Este limite é 40 vezes inferior à norma japonesa para este tipo de descargas no mar e é também quase sete vezes inferior ao limite fixado pela Organização Mundial de Saúde para a água potável (10 mil Bq/L).|Nesse dia, Xanana Gusmão tem previsto reunir-se com o chefe da diplomacia da Nova Zelândia, os primeiro-ministros japonês, Fumio Kishida e malaio, Anwar Ibrahim e o secretário-geral da ONU, António Guterres.|O comentador refere que esta mensagem “faz aquilo” que era o esperado após a cimeira da NATO em Vilnius, na Lituânia, as chamadas “garantias de segurança”.|O Grupo Travelstore anunciou nas redes sociais que reforça agora a sua presença em Moçambique com o lançamento da Allways, unidade de viagens particulares à medida.|A central nuclear de Fukushima Daiichi, situada na costa nordeste do Japão, começou a libertar no final de agosto águas residuais radioativas tratadas e diluídas no Oceano Pacífico.|“Até ao momento, a procura não diminuiu e, para nossa surpresa, as pessoas querem continuar a viajar”, lembrando que há casos em que o preço médio subiu 10 pontos percentuais.|As formações internas irão realizar-se em Lisboa e Porto como já tem sido hábito durante todo o ano de 2023, no entanto e devido ao seu crescimento irão realizar também formações no Algarve e na Madeira, comunica a DIT Portugal em nota de imprensa.|O primeiro período de descarga de água no mar da central nuclear danificada de Fukushima termina na segunda-feira, como previsto, anunciou hoje a empresa responsável pelas operações (Tepco).|Apesar dos vários alertas para o risco da economia europeia entrar em recessão (ou até estagflação), o Banco Central Europeu (BCE) decidiu voltar a subir as taxas de juro diretoras em 25 pontos base esta quinta-feira, dia 14 de setembro.|Enquanto nação democrática do Sudeste Asiático, a adesão de Timor-Leste à ASEAN é uma das principais prioridades da nossa agenda de política externa.|Em reação, o PSD destaca que o Governo Regional aprovou em agosto “mais de 740 mil euros em apoios financeiros” às freguesias, sendo parte do valor destinado à “limpeza das ribeiras e linhas de água”.|Gusmão discursou na segunda-feira no fórum empresarial da cimeira e participa ainda esta terça-feira no Fórum ASEAN-Indo-Pacífico, estando previstos ao longo da semana vários encontros bilaterais.|As companhias aéreas do Grupo SATA (Azores Airlines e SATA Air Açores) acabam de receber o certificado internacional Quality Assurance Standard (QAS) que confirma a qualidade do seu programa de compensação de emissões carbónicas.|Segundo uma nota publicada no site da OA, o serviço de apoio jurídico ao refugiado poderá também prestar informações sobre o sistema de acesso ao direito e aos tribunais vigente em Portugal.|Em 30 de junho passado, o vice-presidente do Governo dos Açores, Artur Lima, considerou “prematuro” e “irresponsável” exigir alterações ao programa “Nascer Mais”.|O presidente do Governo dos Açores começou na quinta-feira a ronda de auscultação dos partidos e parceiros sociais a propósito do Plano e Orçamento da região 2024, o quarto da legislatura, que vai ser discutido em novembro na Assembleia Regional.|Com esta iniciativa concretizada, o grupo indica que dá mais um passo na concretização do desenvolvimento sustentável do negócio.|Como até agora tem tudo corrido dentro do que estava previsto, nada nos leva a crer que no espaço de um mês não tenhamos, de facto, as medidas aprovadas e definidas”, disse o autarca.|”Importa é que contactem com a Embaixada portuguesa em Rabat e que entrem em contacto também com o gabinete de emergência consular da Direção Geral dos Assuntos Consulares e das Comunidades Portuguesas”, disse hoje o ministro José Luís Carneiro.|Os quarteirenses já podem beneficiar de um novo serviço jurídico através da Junta de Freguesia, que será o ponto de contacto entre os cidadãos e o Centro de Arbitragem da Universidade Lusófona (CAUL).|É por isso que a Tepco dilui muito amplamente a água com trítio em água do mar antes de a descarregar no oceano, de modo a que o seu nível de radioatividade não ultrapasse o limite de 1.500 Bq/L.|”Vamos melhorar o diploma do apoio ao crédito [à habitação] que não teve a procura e o acesso que tínhamos previsto”, disse a ministra.}|{Lucas Lima trabalha no Tecnoblog desde 2019 cobrindo software, hardware e serviços.|O movimento foi desenvolvido por arquitetos modernos em meados das décadas de 1950 e 1960 e nasceu precisamente no período de reconstrução das cidades dos países europeus após a Segunda Guerra Mundial.|É uma coleção muito valiosa, uma coleção muito boa com 40 peças.|Temos todos hábitos diferentes, gostos diferentes, profissões diferentes, famílias diferentes.|Só este ano, até agosto, a associação de apoio aos consumidores revela que foi contactada por cerca de 20 mil famílias com dificuldades em pagar contas, refere Natália Nunes, coordenadora do gabinete de proteção financeira da Deco.|Este estilo segue a premissa de que “menos é mais” e aposta em elementos e peças necessárias e básicas, com o objetivo de tornar o espaço mais funcional, elegante e espaçoso.|E a identidade, conforme a época, continua a ser parte de um mesmo tronco, continua a ser parte de uma mesma raiz, mas tem um diálogo totalmente atual, sem dúvida alguma.|De todos os materiais, a madeira é a grande estrela da decoração rústica.|Ao que parece, a casa para onde o atleta se mudou com a família é bastante diferente do que estava previsto.|Dá-se preferência aos tons alaranjados, castanhos e vermelhos, mas abrange também os tons de branco, bege, cinza e até o preto.|O ex-assessor preferiu não contar detalhes sobre a sua ida à polícia, mas disse que sua contribuição pode ter sido importante para as investigações.|Outra dica é manter seu sistema operacional e seus aplicativos de contato e de backup sempre atualizados.|É um estilo elegante, harmonioso e leve, com espaços funcionais e práticos.|É como uma forma de manifestar quem eles são, é um símbolo de identidade.|Então, em todo o país encontramos diversidade têxtil e formas diferentes de mostrar como é cada comunidade, designadamente através da língua ou da comida, que também é muito diversa.|Aqui, na prisão, eles também te podem matar, mas não tenho medo.|Falamos muito da gastronomia mexicana, como o soft power do México.|Se eles estavam na memória do telefone antigo, será necessário transferi-los para o SIM card antes de instalar no novo celular.|O que mais gosto são os têxteis de “tear de cintura”, um que se tece sentado no chão, tem muito contacto com a terra, e quase sempre vamos encontrar aí representado o milho que é uma planta sagrada para nós.|A mistura de cores e padrões é comum na decoração boho, sendo que os tons neutros são sempre a base.|Já a cumprir pena, Koke deu agora uma rara entrevista ao Canal + onde explicou todo o filme que o levou a esta situação.|Allen Hynek envolvendo a descoberta de objetos extra-terrestres.|Caracteriza-se por misturas de formas e materiais, linhas simples e retas, acabamentos lisos e brilhantes e cores alegres como o laranja, amarelo, rosa e azul.|O filho ’04’ do ex-presidente Jair Bolsonaro (PL) foi alvo de busca e apreensão pela Delegacia de Repressão aos Crimes contra a Ordem Tributária, vinculada ao Departamento de Combate a Corrupção e ao Crime Organizado (DOT/Decor).|O México tem 32 estados e na exibição vão ser representados 16 desses estados.|Para muitos é uma obra de arte habitável, para outros uma ideia “que deveria ter continuado uma escultura”, como se pode ler no site “Deezen”.|Essa medida pode garantir mais facilidade na hora de resgatar registros removidos do aparelho — pois versões mais antigas dos itens citados podem apresentar uma série de limitações.|É comum ao trocar de celular não saber como recuperar os contatos, seja do chip (SIM card) ou do telefone em que ele estava salvo.|Usa-se o branco nas paredes e a madeira, pedra ou betão nos pisos.|Diego Pupe admitiu à reportagem ter tido um relacionamento amoroso com Jair Renan por um ano.|Os têxteis foram largamente retratados na obra dos muralistas, por exemplo na obra A Vendedora de Jarros de Diego Rivera, vemos claramente um “Enredo” (tipo de saia indígena mexicana) que é muito parecido com um que foi enviado para a exposição.|Depois de ter assumido que liderava uma rede de tráfico de droga que atuava na Europa, foi condenado a seis anos de prisão.|Antes de transferir contatos do Android para iPhone identifique quais contas da Apple e do Google estão logadas nos dois aparelhos, para que os dados sejam importados corretamente.|A esta paleta é possível adicionar pontos de cores fortes como o verde, lilás, amarelo e azul.|É a opção perfeita para quem gosta de personalidade e simplicidade quando o assunto é decoração.|«Usamos a seda já com os casulos destruídos, a chamada seda da paz, em que o animal sobrevive ao processo», destaca Rui Martins, acrescentando que o artigo tem desencadeado o interesse dos clientes.|Se a migração foi feita de um telefone mais antigo, é provável que os números estejam salvos no chip, se foi feita de um smartphone Android ou iOS (iPhone), há chances de estarem salvos na nuvem.|Deco será apresentado esta quarta-feira como novo diretor desportivo do Barcelona.|Um têxtil tradicional é uma segunda pele e o seu significado depende da pessoa que o elaborou, da maneira como essa pessoa vê o mundo e daquilo que quer comunicar.|Se você selecionar Gmail no lugar de iCloud, por exemplo, os contatos que você adicionar serão sincronizados com a sua conta do Google, e não mais no iCloud.|”Ele foi em um evento meu e, logo em seguida, comecei a trabalhar com ele. Nunca recebi nenhum valor para exercer a função de assessor do Renan. Foi sempre algo de boa vontade minha”, disse.|A propriedade à beira-mar em Fort Lauderdale, na Flórida (EUA), custou cerca de 10,8 milhões de dólares (ou seja, aproximadamente 10 milhões de euros à taxa de câmbio atual).|O conjunto dá uma malha para uma primeira pele com um toque muito macio», acrescenta.|”Caso venha a público desmentir, posso comprovar tudo o que estou dizendo. Tenho prints, mensagens, tudo que possa quebrar a narrativa dele, mas precisaria consultar minha assessoria jurídica”, complementou, por ligação telefônica.|Este tipo de arquitetura é conhecida como brutalismo, um estilo que dá destaque aos materiais, texturas e construção e produz formas altamente expressivas.|A verdade é que o projeto polarizador da Contaminar não só chama à atenção dos portais e das publicações internacionais, como tem sido reconhecido por vários especialistas.|Receba notificações quando publicamos um texto deste autor ou sobre os temas deste artigo.|Maciel Carvalho segue preso, no Complexo Penitenciário da Papuda.|O embaixador mexicano, Bruno Figueroa, marcará presença na sessão de abertura desta exposição, que poderá ser visitada até 27 de outubro na Casa das Galeotas (avenida da Índia, 110).|Ele agradeceu a votação de mais de 18 mil eleitores e lamentou os ataques recebidos durante a campanha.|São 68 línguas com 364 variantes, isso significa que todos os dias do ano podemos falar do México de uma forma diferente.|Os 19 anéis de betão que serpenteiam a casa Quinta do Rei, do estúdio Contaminar, dão a ideia que a obra vertiginosa é uma “escadaria até ao céu”.|Aí se reflete a vida, se reflete a tradição, a cultura e toda uma maneira de ver o mundo.|Situada ao longo de um canal com acesso ao Atlântico, a mansão no condomínio milionário de Bay Colony conta ainda com duas docas para barcos e uma piscina em contacto direto com o oceano.|Assim, poderíamos entender o que são os têxteis e a diversidade de têxteis que há nas culturas do México.|As mantas e almofadas são protagonistas neste estilo, e apostar em tecidos com padrões étnicos é uma ótima opção.|Se, por algum motivo, o projeto tivesse que ser interrompido a meio, a estrutura impetuosa já funcionava como um miradouro com vista privilegiada sobre Leiria.|Outras comodidades incluem um spa e, claro, um espaço de treino para que Messi se possa manter em forma.|Uma harmonização arriscada, mas que é sempre bem executada neste estilo.|“Como jogador de futebol, temos a sorte de ganhar muito dinheiro.|O clima da primeira sessão da Câmara Municipal de Brusque após a eleição suplementar de prefeito e vice do último domingo (3) foi bem diferente das realizadas nas semanas anteriores.|Esta casa-miradouro irrompe numa das zonas mais altas da cidade, um nível ligeiramente acima do castelo local.|Para despistar as autoridades, foi criada a identidade de Antonio Amancio Alves Mandarrari.|Com cerca de 1600 metros quadrados, conta com dez quartos (a suite principal tem 149 metros quadrados) e nove casas de banho.|É possível também servir de inspiração moderna para as criações têxteis?|No momento em que a informação é mais importante do que nunca, apoie o jornalismo independente e rigoroso.|Antes de visitar as possibilidades, vale conferir se você não ocultou sem querer o contato ou não está digitando o nome errado.|Este estilo ganhou esse nome através da expressão francesa “béton brut”, que significa betão em bruto, e pode não gerar consenso — mas está na base de verdadeiras outras de arte.|“Contribuí com muitas perguntas feitas pelos delegados, e respondi de forma positiva o que eu sabia.|Ela está presente em toda a mobília da casa, e também pode surgir em alguns objetos.|Os tons de castanho, bege, verde, preto e laranja são os mais escolhidos para criar este estilo.|As plantas naturais, que criam a sensação de leveza na decoração, são essenciais para decorar casas no estilo boho.|Este estilo é naturalmente delicado, sereno, íntimo, mas não necessariamente uma decoração feminina.|Basicamente, o produto permite «interagir com o meio que nos envolve e mostrar as nossas emoções e sentimentos», resume Joana Oliveira.|Com um conceito minimalista, este estilo é caracterizado por linhas retas, paredes e móveis brancos, uma paleta de cores neutras, luz natural e muita simplicidade.|Então, absolutamente, como a cozinha, como a medicina tradicional, como a música, como as diferentes expressões dos povos e como as línguas, estão vivas.|«Para além da menta temos outros produtos desenvolvidos com resíduos da indústria alimentar – cogumelos, café.|Além do app Contatos, também é possível excluir seus contatos do iPhone pelo aplicativo Groups.|Recorde-se que, em Sunny Isles Beach, um pouco mais a sul do estado norte-americano, Lionel Messi e a esposa, Antonela Roccuzzo, já tinham investido cerca de 7 milhões de euros num apartamento luxuoso.|Os motivos e as técnicas têxteis são ainda da época anterior à colonização espanhola ou também resultam da mestiçagem das culturas?|Ela pode estar no piso, no revestimento de parede, nos móveis e peças de decoração.|Carvalho chegou, inclusive, a registrar um boletim de ocorrência em nome de Renan quando a casa em que ele morava, no Lago Sul, foi pichada.|Com 211 mil seguidores no Instagram, Pupe interage bastante com as pessoas e não esconde ser homossexual e apoiador do ex-presidente.|Possui um aspeto antigo, campestre, onde o passado é evidenciado e as imperfeições são vistas como belas.|Algumas marcas mostraram-nos, pelas más práticas e por plágio, que os grandes mercados estão abertos a essas expressões culturais.|Além disso, cada comunidade tem diferentes formas de usá-los, diferentes formas de fazê-los, que têm a ver com rituais, com cerimónias, às vezes com o estado civil, às vezes só para vender às pessoas que não são da comunidade.|De figuras humanas a animais, mas também motivos geométricos, tudo parece possível no têxtil mexicano.|O recurso é uma alternativa para pessoas que estão mudando de celular ou que simplesmente querem compartilhar números entre dois smartphones.|O antigo jogador foi apanhado numa ação da Guardia Civil que intercetou uma tonelada de haxixe e várias armas.|Contudo, no têxtil há uma comunhão muito mais fácil, assim como com a comida.|O estilo moderno cria a sensação de simplicidade em todos os elementos, incluindo nos móveis.|Para apagar todos os seus contatos do iPhone de uma só vez é preciso que você acesse sua conta do iCloud no PC.|Quando se ouve aquele ‘traficante internacional’ penso ‘O que é que eu fiz?|No mobiliário predominam as curvas, pés arredondados e peças trabalhadas com detalhes vistosos.|Se você possui um celular Samsung, é possível recuperar contatos apagados por meio do backup feito no serviço de nuvem da empresa.|Dada a sua complexidade, “não foi fácil arranjar construtores para a edificar”, explica à NiT Joel Esperança, um dos responsáveis.|Ou seja, as criações têxteis são conservadoras nos temas ou não?|Optamos pela menta aqui e achamos que é uma combinação interessante com o liocel, que é também uma fibra sustentável.|Queriam algo irreverente e, das três propostas apresentadas pelo atelier, optaram pela mais distinta.|Móveis antigos são uma ótima opção para compor um ambiente no estilo romântico.|Graduou-se em Jornalismo em 2018 e se formou técnico em Informática em 2014, mas respira tecnologia desde 2006, quando ganhou o primeiro computador e varava noites abrindo janelas do Windows XP.|Após ter rescindido contrato com o PSG, a estrela do futebol mundial juntou-se a David Beckham no Inter Miami e comprou uma mansão luxuosa numa nova cidade.|O que acontece com o têxtil é que pode ser partilhado e pode ser usado.|O filme Contatos Imediatos do Terceiro Grau (1977) também faz uma referência a essa escala.|“São clientes que preferem uma matriz urbana e que não fazem questão de ter os pés em contacto com a terra.|App para Android e iPhone (iOS) traz exercícios gratuitos diários e sons relaxantes.|Citou caso de uma acusação feita por adversários sobre fazer vistas grosas a um de seus membros de campanha que teria sido apontado por assediar sexualmente alguém.|Entre obras e licenciamentos, foram precisos mais de 10 anos para passar a ideia ambiciosa do papel para a realidade.|A estrutura beneficia da curvatura do solo para aproveitar a exposição do Sol conforme as necessidades de cada um dos pisos desta construção angular.|Porém, tem muitas outras características que justificam o valor astronómico da transação.|Em alguns casos, pode ser que o usuário não encontre nenhum contato no iCloud.|Um desafio a quem visitar a exposição dos têxteis mexicanos em Lisboa e quiser saber mais?|Padrões às riscas, florais e com inspiração vitoriana são as texturas mais as- sociadas a este estilo e podem ser colocadas em papel de parede, cortinas, sofás, poltronas, lençóis, etc.|Gostam de estar na sala, a apreciar o cenário e a ler um livro”, acrescenta.|Sergio Contreras, mais conhecido no mundo do futebol por Koke, foi detido pela polícia espanhola numa operação contra o tráfico de droga que se desenrolou em Málaga, Sevilha e Granada.|O ex-assessor cita que a relação de trabalho entre os dois [ele e Jair Renan] se encerrou em julho do ano passado, mas não quis explicar o motivo.|As principais características do estilo contemporâneo são as linhas retas ou sinuosas e os materiais mais utilizados são o vidro, madeira, pedra, cimento, mármore e metal.|”Tivemos um ano de relacionamento amoroso, mas é algo que eu não quero expor muito. Desde a repercussão, ele não me procurou, porque sabe que o que vivemos foi real”, disse, à reportagem.|É um estilo com muito relevo, curvas e formas, por isso deve ser adotado em ambientes mais espaçosos.|Caso sinta que sua agenda esteja cheia demais, pode ser uma boa apagar contatos do smartphone.|Mas é uma forma de mostrar a cultura que tem persistido por tantos anos, por mais de 500 anos.|Pode ser também que o registro esteja armazenado em outra conta cadastrada no celular.|O México tem uma das maiores diversidades culturais, biológicas e naturais dos países do mundo, com maior diversidade natural, linguística.|Deco foi, ao final da manhã desta quarta-feira, formalmente apresentado como o sucessor de Mateu Alemany no cargo de diretor desportivo do Barcelona, numa cerimónia que teve lugar na Ciutat Esportiva Joan Gamper.|A estética aconchegante é refletida no uso de colchas, mantas e tapetes com tecidos naturais e geralmente volumosos.|E acho que é uma das expressões contemporâneas mais fortes, porque a maneira de vestir é como uma segunda pele para eles.|E é uma manifestação muito importante, porque a partir do “Original”, que é um movimento que fizemos para a defesa dos têxteis e dos direitos coletivos, os artesãos têm recebido muitos convites internacionais muito interessantes.|Calmaria e elogios aos vitoriosos tomaram conta do encontro, realizado na noite desta terça-feira (5).|São cada vez mais as famílias em situação de sobre-endividamento que pedem ajuda à Deco.|É possível ter uma decoração no estilo romântico que agrade a homens e mulheres.|Então, o que nos interessa é que os protagonistas, que realmente fazem essa arte, tenham essa presença nos países.|Desde o início, não faltaram oportunidades para os arquitetos recuarem.|À reportagem, Diego Pupe contou ter conhecido Jair Renan em uma festa promovida por ele, em 2021.|Essa identidade, segundo a polícia, foi responsável por abrir contas bancárias para que fosse configurada como proprietária de pessoas jurídicas, na condição de “laranja”.|Por isso, tanto em David Alfaro Siqueros, como em José Orozco, como em Diego Rivera, como em outras manifestações artísticas e culturais, vamos encontrar a arte têxtil.|Outra alternativa é importar o arquivo vCard pelo navegador para inseri-lo no iCloud.|Este estilo é eterno e nunca sai de moda, e é por isso que faz tanto sucesso na decoração e arquitetura.|Pupe ficou na sede da PCDF, em Brasília, por mais de duas horas, na manhã de quinta-feira (14/9).|Os materiais mais utilizados no estilo romântico são ferro, madeira e peças pintadas de branco.|Essa era uma maneira de entender e de educar as gerações após a revolução, no México, e é onde o povo, que havia sido discriminado e explorado, se coloca no centro da cultura.|Por exemplo, Frida Kahlo, que é um ícone do México, e as suas pinturas, muitas vezes serve de inspiração para artistas de todo o mundo.|Uma boa iluminação é um fator muito relevante num espaço minimalista e a cor predominante destes ambientes é o branco.|Valoriza a sobriedade e a elegância, adjetivos que, quando materializados, deixam pouco espaço para o acessório.|Escolha um país/região no menu pendente abaixo para obter os contactos dos nossos escritórios no mundo inteiro.|Existem, por exemplo, bordados que mostram um movimento natural sagrado, que é um tornado, ou que é o vento, ou que é a água.|”Eles estão investigados. (Mas) Não sei porque a 5ª Vara Criminal se recusa a nos fornecer o acesso aos autos, mesmo com determinação do Supremo Tribunal Federal”, disse Admar Gonzaga.|Assim, acho que depende de como se quer enfrentar o mundo nesse dia, decide-se que roupa usar.|A madeira é um dos materiais mais procurados pelos amantes deste estilo.|Vale indicar que a função precisa ser ativada no Android e confirmada no iPhone.|Os tapetes são um elemento especial de destaque neste estilo decorativo, sendo sempre espessos e convidativos, muitas vezes cobertos de padrões clássicos e várias cores.|Isso é algo muito interessante de notar, porque é uma linha que não acabou e que segue viva.|Está representada a diversidade cultural e também estão representadas algumas das peças que foram vítimas de plágio por algumas marcas internacionais, que são parte da cultura da comunidade, que continua viva, que continua a fazê-las.|De pessoas que têm Android ou iOS, eu ainda vejo muito aqueles posts no Facebook anunciando “perdi meus contatos, me chama no WhatsApp para eu te adicionar”.|Então, isso é o que está a ser exibido, são alguns vestidos rituais e, sobretudo, a representação de diferentes culturas, a maia, a tzotil, a tzeltal, a seri, povos indígenas do norte, do sul, do centro, de diferentes regiões do México.|Para conseguirmos manter a qualidade da nossa informação precisamos da sua colaboração no combate à pirataria.|Através deste estilo de decoração é possível conferir aos ambientes uma sensação de conforto, afeto e nostalgia.|Por fim, o imóvel termina com um espaço de lounge que inclui a piscina, um ginásio e ainda um pequeno espaço de leitura.|E é assim há mais de 150 anos, pois somos o jornal nacional mais antigo.|“Acredito que a arquitetura de interiores é essencial para a nossa vida, e em particular para o nosso bem-estar.|São expressões culturais que resistiram mais de 500 anos para continuar vivas.|A relação com o espaço em que vivemos e com as pessoas com quem o partilhamos é realmente transformada e modi- ficada quando este local é planeado e pensado ao pormenor.|A luz natural é um elemento muito importante na decoração romântica.|Também é possível fazer pelo iCloud, caso não queira baixar nenhum app.|Os materiais mais usados são o mármore, a madeira, principalmente as de tonalidade escura, como o mogno e a cerejeira, e as cores mais comuns são o preto, bordeaux, azul-marinho e verde-esmeralda, dourados, prateados e rosa-claro.|Agora que você aprendeu a recuperar contatos excluídos do celular, pode ser uma boa pedida conferir dicas para restaurar mensagens do WhatsApp e do Telegram.|Se você quiser, pode segmentar a exibição de contatos a partir das diferentes contas conectadas ao seu iPhone.|Ron Adler, CEO e diretor do Alaska Psychiatric Institute, e Denise Dillard, presidente da Associação de Psicologia do Alasca, também declararam jamais ter ouvido falar de Abigail Tyler.|O estilo moderno é clean, organizado, simples, prático e privilegia as cores neutras.|Com quatro andares e 397 metros quadrados, os clientes entram num hall, que funciona como um piso intermédio.|A decoração clássica necessita de alguma cautela, pois envolve informação visual.|No final de agosto, começaram a circular imagens de uma concept house criada para Lionel Messi.|Mantém-se a presença do betão, mas a madeira e os tons quentes passam uma sensação mais acolhedora para quem entra.|Este estilo é caracterizado por misturar muitas cores no mesmo ambiente, alcançando uma harmonia entre todas.|Se vir as cores, por exemplo, há momentos em que na arte têxtil dos povos indígenas do México vê a tendência de cor que está na moda nesse ano.|É especialista em análise e visualização de dados, e foi autor do Tecnoblog entre 2015 e 2018.|E eles mesmos vão inovando e podem seguir correntes ou influências diferentes de moda.|Os móveis e peças de decoração podem ser pintados ou deixados no seu estado original.|Ao descer para a cave, encontra-se a zona técnica, com uma garagem e uma sala polivalente.|Porém, é preciso repetir o procedimento toda vez que decidir apagar um contato.|O critério de seleção é, de facto, um desafio, mas tem a ver com representar diferentes regiões culturais do país.|Convidamos o público a conhecer o movimento “Original”, a viajar ao México para conhecer milhares de famílias criadoras de arte têxtil, que devem ser respeitadas e protagonistas de seu próprio desenvolvimento cultural e económico.|Nas divisões mais importantes, a casa parece recuar para receber um bocadinho mais da luz solar.|Espero tê-los ajudado, mas não posso contar porque é sigiloso”, relatou, ao Correio.|Os têxteis são como códices, livros antigos que refletem a cultura asteca através de símbolos, e refletem o estado de ânimo de cada um.|Dessa forma, você se mantém organizado e sem números que não fazem sentido no seu dia a dia.|Preto, cinza, branco e castanho vão, portanto, dominar a maior parte do ambiente.|Este estilo é uma releitura do passado, resgatando formas e cores para enriquecer projetos de decoração atuais.|A composição dos ambientes é feita por elementos clássicos e elegantes, como a madeira, presente em sofás, mesas, camas, poltronas e armários.|As cores associadas a este estilo são suaves, com tons neutros.|É possível ver alguma influência da arte tradicional nas obras pictóricas dos grandes muralistas mexicanos?|Assim, quem sobe até à parte soalheira, pode contemplar a paisagem em 360 graus — inclusive dentro da piscina.|Na arte mexicana, a cultura popular retém muito as imagens dos murais de Diego Rivera e David Alfaro Siqueros.|É difícil escolher um em detrimento do outro, mas se tivesse de o fazer, talvez fosse por aí.|É habitual o uso de texturas e cores sóbrias, mas de forma simples e clean, visando sempre a criação de soluções para os problemas de quem habita o espaço, criando assim ambientes mais confortáveis e aconchegantes.|No Diário de Notícias dezenas de jornalistas trabalham todos os dias para fazer as notícias, as entrevistas, as reportagens e as análises que asseguram uma informação rigorosa aos leitores.|Como resultado, o estilo contemporâneo brilha pela simplicidade, praticidade e funcionalismo.|Imagina que os têxteis e outros produtos tradicionais também possam ganhar uma projeção internacional e também acrescentar a esse soft power do México?|Assine o ECO Premium e tenha acesso a notícias exclusivas, à opinião que conta, às reportagens e especiais que mostram o outro lado da história.|Todos esses detalhes devem ser avaliados e projetados para que não haja conflito de informações visuais.|Acredito que cada casa é única e que quem a habita a transforma.|Algumas das suas características são o exagero dos adornos presentes em elementos decorativos, móveis e na arquitetura de interior, como no teto, parede, mesas, armários, rodapés, sofás, entre outros.|O estilo é casual e resgata o contacto com a natureza e a forma de viver mais simples, com leveza e descomplicação.|O conforto é a tónica dos móveis que compõem os ambientes e os sofás são amplos, com formas arredondadas.|Se os números estiverem mesmo salvos no chip da operadora, em qualquer um dos sistemas operacionais há uma opção para recuperar os contatos.|Cada casa, cada espaço, cada divisão deve ser projetada com base em quem a habita e tendo sempre em conta as suas necessidades, desejos, vontades e objetivos”, relata Bárbara Dias na introdução ao seu livro.|É necessário ter uma Samsung Account para logar no aplicativo.|Desenhada pelo arquiteto espanhol Jorge Luis Veliz Quintana, o projeto mostrava uma casa com o formato da letra “M” a flutuar numa espécie de ilha privada, algures em Miami, nos Estados Unidos.|Além das características citadas, podemos também identificar os ambientes integrados e amplos, as janelas grandes, superfícies sem acabamento, fios expostos, tubagens à vista e vigas aparentes.|Por aqui, deixo sincronizado minha agenda de duas contas do Gmail, além dos contatos do iCloud, que é onde a agenda do iPhone fica sincronizada por padrão.|Sobre a operação que levou a busca e apreensão do filho do ex-presidente, disse que só comenta nos autos do processo.|De acordo com o clube culé, a cerimónia vai decorrer na Cidade Desportiva Joan Gamper, a partir das 11h00 (10h00 hora de Portugal Continental).|Nesses casos, há grandes chances de os contatos estarem guardados na Conta Google ou no iCloud.|Para a polícia, existe um esquema de fraudes com crimes de estelionato, falsificação de documentos, sonegação fiscal e lavagem de dinheiro, com o objetivo final de blindar o patrimônio dos envolvidos.|Para continuarmos a fazer este “serviço ao leitor“, como escreveu o nosso fundador em 1864, precisamos do seu apoio.|Nunca devemos perder de vista que quando se plagia ou rouba uma peça das culturas originárias, estamos a vulnerabilizar o direito a uma coletividade completa.|Quem opta pelo estilo clássico está em bus- ca de ambientes sofisticados e elegantes, sendo que uma das suas principais características é o aprimorar e requintar das linhas e formas de objetos e mobiliário.|No entanto, quem entra na Quinta do Rei, consegue ver bem todo exterior.|O México é 20 vezes maior que Portugal e um país de uma grande diversidade cultural.|É um estilo versátil, que se adapta, e em que as cores predominantes são o preto, branco, cinza, castanho e bege.|Um bom exemplo para entender o que acontece com os têxteis são as diferentes línguas que temos, que se falam no México como línguas oficiais.|A autora da página Pistacho Decor, com 100 mil seguidores no Instagram, desmistifica o processo de decoração e fornece ao leitor todas as ferramentas para criar espaços pessoais e funcionais, divisão a divisão.|É um estilo que prima pela boa circulação no espaço, visando assim a otimização da funcionalidade.|Já o piso 0, ao percorrer-se as escadas, está dividido em duas suites, dois quartos e ainda uma casa de banho.|O tamanho excessivo, as fachadas frias com pequenos adornos e as fortes formas geométricas fizeram com que, durante décadas, estas construções fossem adoradas por uns e odiadas por outros.|É a combinação que une elementos clássicos e tradicionais com itens modernos.|Preservam um símbolo cultural, mas no presente e dialogam com outros elementos que talvez não estivessem ao seu alcance quando esses têxteis começaram a existir.|Mas foi Alessandro Simas (Progressista) quem fez o discurso mais emocionado.|É possível trabalhar a decoração com cortinas, utilizando tecidos transparentes ou semitransparentes para filtrar a claridade.|Neste estilo, os detalhes são estratégicos e compõem um cenário inspirador, como quadros com molduras em tom contrastante, plantas penduradas, iluminação moderna e livros.|Se o período de 30 dias for excedido, o aplicativo de contatos remove o registro permanentemente — descartando completamente essa dica e obrigando você a recorrer a outras soluções.|Jean Prado é jornalista de tecnologia e conta com certificados nas áreas de Ciência de Dados, Python e Ciências Políticas.|Apesar do aspeto austero e rude, como os próprios arquitetos descrevem, a decoração transmite exatamente o oposto.|E também nas obras pré-hispânicas vamos encontrar a arte têxtil em obras de arqueologia.|Como nasce sobre um declive pronunciado, “não era possível fazer uma casa térrea” e assumiram a verticalidade.|É possível recuperar contatos apagados no Android e no iPhone caso seu aparelho tenha apresentado algum erro ou você tenha se arrependido de remover algum nome.|É um estilo onde prevalecem as linhas retas, silhuetas elegantes e a simplicidade.|Neste negócio ganha-se em dois meses o que se pode ganhar num ano no futebol.|Lurdes Sampaio, Polopiqué e Inovafil foram as empresas com artigos selecionados na categoria tecidos.|O produto Auracollar da Adalberto foi o terceiro selecionado para os iTechStyle Awards na categoria acessórios.|Então, a maior parte dos têxteis que vão estar na exposição são de técnicas anteriores à colonização.|Venho de um bairro de Málaga onde todos os meus amigos são amigos de infância.|Hoje, esta decoração aparece acompanhada de elementos modernos e contemporâneos, numa conjugação harmoniosa.|Tenho contactos em muitos sítios, mas não sou o Pablo Escobar.|Diariamente, versões em PDF, com a totalidade dos jornais e revistas nacionais, são partilhadas por email, por whatsapp ou em outras redes sociais, numa clara violação dos direitos de autor.|«Tivemos o contacto de um produtor de seda nacional e viemos a descobrir que, aqui no Norte de Portugal, temos uma tradição de produção de seda, algo que desconhecíamos», indica Rui Martins, CEO da empresa de fiação.|Admite que, antes disso, os dois tiveram um relacionamento amoroso.|Atualmente, passar contatos do Android para iPhone (iOS) é uma tarefa fácil de ser feita pela sincronização das contas do Google.|Para excluir vários de uma só vez, veja no tópico mais abaixo.|Algumas técnicas respondem à mestiçagem de alguns elementos que chegaram, como a lã de borrego, alguns elementos, como o tear de pedal, mas, na maioria, as técnicas são anteriores à chegada dos europeus ao México.|É um estilo boémio contemporâneo em que a principal característica é a mistura de influências de vários estilos, que criam decorações surpreendentes.|No caso da Lurdes Sampaio, a malha é composta por micro liocel e 20% viscose de menta, com propriedades antimicrobianas, respirabilidade e biodegradabilidade.|Através das investigações da operação em que Carvalho foi alvo, em janeiro deste ano, a PCDF conseguiu alcançar novos envolvidos.|Tudo começou em 2012 a pedido de um casal português com dois filhos.|Na aplicação na moda, a gola pode permitir mudar a cor de um acessório consoante a música que a pessoa está a ouvir.|Feito isso, os contatos do Android serão sincronizados com o iPhone.|Com toques oriental, étnico, hippie e vintage, o estilo boho tem um toque de romantismo, mas foge dos padrões tradicionais.|Para recuperá-los, basta logar na mesma conta no celular novo.|A Inovafil, por seu lado, viu selecionada a referência Terramori, que inclui 90% de algodão orgânico e 10% de seda portuguesa.|A seguir, veja como apagar contatos do iPhone em poucos passos.|Os têxteis, como são em muitos casos roupas rituais, são parte dessas festas tradicionais, dessa maneira de celebrar o mundo e a cultura, que se mostraram nos murais da época pós-revolucionária.|O caminho até ao ponto de observação, no topo da casa, continua com a zona social um pouco mais acima.|A característica básica do estilo rétro é a decoração inspirada por outras épocas, convivendo em harmonia com objetos contemporâneos.|Deco foi apresentado oficialmente como diretor desportivo do Barcelona na manhã desta quarta-feira, sucedendo a Mateu Alemany.|Um estilo simples, com muito charme, que desperta memórias afetivas e transmite aconchego e encanto.|Selecione o arquivo vCard que baixou do Google anteriormente e toque em “Abrir”.|Logo após, começou a trabalhar com o filho ’04’ do ex-presidente da República.|Teve experiências com comunicação no poder público e no setor de educação musical antes de atuar na estratégia de conteúdo e SEO do TB.|Koke acabou detido pela polícia numa operação onde foi apreendida uma tonelada de haxixe e várias armas.|Os próprios povos inovam, mudam as suas próprias técnicas e mantêm um diálogo com o mundo.|A exposição “Original” é apresentada na Cidade do México de 16 a 19 de novembro deste ano, no centro cultural “Los Pinos”, que antes era a Casa do Presidente e hoje é a casa do povo e dos artesãos.|Durante os créditos finais, são lidos e ouvidos diversos depoimentos em rádios ou ligações telefônicas, em datas e locais diferentes, de testemunhas, declarando ter tido encontros de diversos graus com extra-terrestres.|Na parte de trás, tem cerca de 11 metros de altura e, de frente, conta com cerca de 7 metros.|Este é um estilo que, utilizando poucos e bons objetos, dá ênfase a móveis de design com acessórios e toques pessoais decorativos.|Madeira, paredes sem acabamento, pisos de cimento e referências ao passado são alguns dos elementos que caracterizam este estilo de decoração, e que o tornaram uma tendência.|Se você tem mais de uma conta cadastrada no seu aparelho e a restauração apresentada não é aquela que você procura, é necessário mudar a conta do Google no seu celular.|Caso os contatos estejam salvos na nuvem, eles serão baixados no dispositivo e toda alteração feita em um contato será atualizada em todos os aparelhos com aquela conta.|Antigo futebolista assumiu ser o líder da rede criminosa e foi condenado a seis anos de prisão.|Não queremos assinantes, queremos membros ativos da comunidade.|O título original The Fourth Kind é uma referência ao trabalho do cientista J.|Esta partilha, além de ser crime, é uma ameaça à sustentabilidade financeira das empresas, à informação livre e independente e, no limite, coloca em causa milhares de postos de trabalho no sector da comunicação social.|Esse método garante que o contato selecionado seja excluído da sua agenda.}|{Assim, a principal taxa de refinanciamento – que tem efeitos sobre os créditos habitação – galopou para os 4,50%, o nível mais elevado desde maio de 2001.|A governante disse ainda que, após a sessão desta terça-feira, “daqui a 15 dias” estará feito o levantamento final dos prejuízos causados pelo incêndio e que dentro de “um mês haverá uma nova reunião”.|O PSD perdeu então, pela primeira vez, a maioria absoluta na Assembleia Legislativa Regional da Madeira, que detinha desde 1976, elegendo 21 deputados e formando um governo de coligação com o CDS-PP (três deputados).|Já Pedro Santos, da Confederação Nacional da Agricultura, defende a fixação de preços.|Recentemente, o Banco do Brasil lançou uma linha arrojada, para estimular a compra de maquinário.|A autarquia de Quarteira é uma das 3.000 freguesias associadas a este protocolo que, independentemente da sua dimensão, passam a ter acesso a um serviço jurídico especializado.|Saliente-se que algumas máquinas acendem uma luz de aviso quando o filtro de limpeza precisa de ser limpo.|A Comunidade Intermunicipal Terras de Trás-os-Montes (CIM-TTM) reuniu sobre este assunto na segunda-feira com a ministra Maria do Céu Antunes, por videoconferência, que disse aos autarcas ir “brevemente” à região.|Esta parceria irá permitir selecionar empresas com selo de garantia da organização de https://Getpocket.com/redirect?url=https://bankirin.ru/user/jenideiivn e acrescentar valor para os consumidores no processo de contratação de serviços para casa.|Confrontado com esta justificação, Pedro Lima (PSD), presidente da câmara de Vila Flor, disse desconhecer qualquer relatório elaborado pela DRAPN ou qualquer ida ao seu concelho dos seus técnicos.|Um mecanismo que auxilia a escolha na execução de remodelações, reparações, canalizações ou outros serviços para a casa, com o selo de confiança da DECO.|E futuro é não voltar a cometer os mesmos erros que se têm cometido ao longo dos anos, em que temos um espaço que tem sido objeto de incêndios que têm, de alguma forma, criado prejuízos enormes”, acrescentou.|Quem vende e quem compra, quem aluga e quem arrenda – todos fazem contas à vida.|Em 2023, a Superintendência de Promoção da Liberdade Religiosa já realizou 34 atendimentos desta natureza, e a instituição de ensino é a primeira a fechar esse tipo de parceria com o órgão.|O Ministério da Agricultura e Pescas disse esta quarta-feira à Lusa que os concelhos de Vila Flor, Vinhais e Macedo de Cavaleiros não cumprem os requisitos para estar incluídos nos apoios por causa do granizo.|▲Os prejuízos do incêndio em Odemira ascendem a “cerca de 15 milhões de euros”.|(DECO) espera que o veto de Marcelo ao pacote Mais Habitação sirva para reavaliar as medidas e deseja mais ajuda para quem já tem créditos.|Além da descida do IVA dos alimentos, no debate sobre política geral, na quarta-feira, no Parlamento, António Costa mostrou disponibilidade para rever os salários da função pública.|Também no Fórum TSF, Pedro Santos, da Confederação Nacional da Agricultura, afirmou que a medida mais eficaz seria a fixação de preços, “desde que isso não resulte num aumento ainda maior dos lucros da grande distribuição”.|Luís Fernandes (PS), presidente da câmara de Vinhais, discorda da avaliação tida em conta pelo Ministério e considera que esta deve ser “uma situação a reavaliar”.|No entanto, Natália Nunes, da Defesa do Consumidor, referiu, no Fórum TSF, que esta ajuda é curta e são necessárias outras medidas para famílias que têm rendimentos mais baixos.|De acordo com vários agentes imobiliários entrevistados pela SIC, se houvesse mais casas haveria pessoas para as comprar.|E o que nos aconselharam no futuro é que fizéssemos um trabalho cooperativo para podermos ter seguros coletivos“, explicou Benjamim Rodrigues (PS), presidente da câmara de Macedo de Cavaleiros.|“Vamos recebê-la com todo o carinho e vontade e ver o que tem para nos dizer sobre estes assuntos e outros”, adiantou Pedro Lima, também vice-presidente da CIM-TTM, dizendo esperar “a abertura que o dirigente máximo da nossa agricultura deve ter”.|Se retirar as peças ainda quentes, poderá dobrar de imediato sem ter de as passar a ferro.|Mas foquemo-nos nos números, que os valores são variáveis, mexem com o coração e embaciam o raciocínio.|A medida conta com uma dotação orçamental de quatro milhões de euros estando em vigor durante três meses, entre abril e junho de 2022, ou até que a verba se esgote, assinala a Deco Proteste num artigo sobre este tema, hoje publicado.|Não é apenas uma competição, mas também uma plataforma de visibilidade que ajuda no crescimento e promoção dos participantes, dinamizando o sector.|O Prémio não se limita a produtores de grande escala e abre espaço para pequenos e médios produtores.|E nesta edição irá contar com a participação do serviço DECO PROTESTE Select.|Do lado de Macedo de Cavaleiros, a exclusão era já esperada, depois de um contacto com a tutela na altura da primeira intempérie que atingiu o concelho.|Seja em resolução do Conselho de Ministros — que era aquilo que nos parecia mais eficaz — seja numa outra forma qualquer, [esperamos] que as medidas estejam estruturadas e no terreno”, disse.|Marcelo Rebelo de Sousa já decidiu sobre Mais Habitação mas deixa anúncio para segunda-feiraPresidente da República falou aos jornalistas na chegada à chegada a Varsóvia para uma visita oficial de dois dias.|De acordo com a DECO, caso não o faça, a máquina poderá ser menos eficiente na secagem e pode até aumentar o consumo energético.|O presidente da Câmara de Odemira, Hélder Guerreiro (PS), espera que o Governo apresente, em outubro, as medidas de apoio para mitigar os prejuízos causados pelo incêndio que deflagrou, em agosto, neste concelho do distrito de Beja.|O tipo de tecido também deve determinar a temperatura e a duração do ciclo de secagem.|O objetivo do acordo é que professores e alunos da universidade prestem auxílio jurídico aos casos encaminhados.|O programa a utilizar deve ser escolhido de acordo com o resultado que quer obter.|Os respetivos presidentes dos três concelhos do distrito de Bragança disseram à Lusa querer ser incluídos nos apoios aos estragos causados pelo mau tempo na região.|Note que algumas máquinas têm a função de arranque em diferido, o que significa que não precisa de estar em casa ou
%%
my homepage :: https://demoslotsplay.com/pt/aviator
как играет онлайн казино
1000 euro lenen
казино стримы онлайн
%%
Look at my blog post; parfum-vid.ru
win казино онлайн
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
can i buy doxycycline at walgreens
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
my web page: https://smwood.ru/
12 weeks of paid leave at 80% of normal base salary to give
care to a family member.
Payday loans in Virginia
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Medicament prescribing information. Drug Class.
xenical no prescription
All about meds. Read information here.
Whoa tons of great knowledge.
https://www.teleprogramma-segodnya.ru/
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
My website … http://aurora.ucoz.de/news/2011-05
%%
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Meds information. Cautions.
valtrex buy
Some information about pills. Get here.
%%
My web page: https://balloonsmartsoft.com/
Закажите матрешку, посуду, шкатулку с вашей символикой, сюжетом или фото подарки отбор изделий ведут специалисты с художественным образованием и длительным стажем работы в сегменте подарочной продукции.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Закажите матрешку, посуду, шкатулку с вашей символикой, сюжетом или фото матрешки отбор изделий ведут специалисты с художественным образованием и длительным стажем работы в сегменте подарочной продукции.
электрокарнизы для портьерных штор и занавесей https://prokarniz20.ru/
Lainaa 400000 euroa
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Drugs information sheet. Brand names.
cost singulair
Actual information about medicament. Read now.
онлайн казино блэкджек
хорошие казино онлайн
Right here is the perfect webpage for everyone who
wishes to understand this topic. You understand a
whole lot its almost hard to argue with you (not that
I actually will need to…HaHa). You certainly put a brand new spin on a topic
that has been written about for a long time.
Wonderful stuff, just excellent!
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
а я заберу палюбому спс
https://comunic-arte.com/?product=pla44630-platinet-lcd-tablet-tinta-electronica-85-pwt8b
%%
Also visit my blog post; https://slotskelly.com/fr/speed-and-cash
what to say, the cook took the pot from the fire,
Хайпово – информационно-развлекательный портал, на котором найдется абсолютно вся информация развлечения комедии выходного дня и не только.
Хайпово – информационно-развлекательный портал, на котором найдется абсолютно вся информация подборки фильмов комедии выходного дня и не только.
Бюро переводов недорого: заказать срочный перевод документов рядом с метро.
Цены на нотариальное заверение переводов в бюро переводов рядом с метро.
Срочный перевод документов: бюро переводов с нотариальным заверением.
Бюро переводов рядом с метро: заказать перевод и нотариальное заверение.
Недорогие переводы документов с нотариальным заверением: цены и услуги.
Заказать срочный и недорогой перевод в бюро рядом с метро.
Бюро переводов с нотариальным заверением: актуальные цены и сроки.
Как недорого и быстро заказать перевод в бюро рядом с метро.
Бюро переводов: срочное нотариальное заверение документов по доступной цене.
Бюро переводов в вашем районе: заказать перевод и заверение недорого и быстро.
translate-top.ru
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
https://gamma.app/docs/MelBet-Promosyon-Kodu—Hosgeldin-Bonusu-130-o4vqhj1bewucbip?mode=doc
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Если нужна работа на севере с целью получать высокую зарплату, забудь про комфорт. Вкалывать придется много и в суровых условиях!
Join millions of winners and unlock the door to endless fun and wealth https://nukunjkharod.livejournal.com/7100.html by clicking on this magical link right now.
Join millions of winners and unlock the door to endless fun and wealth https://vipmails.0pk.me/viewtopic.php?id=4086#p10018 by clicking on this magical link right now.
онлайн казино кто играл
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
зеркала онлайн казино
furosemida 40 mg
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Вы попали в самую точку. Мне нравится эта мысль, я полностью с Вами согласен.
Новости Чехии 2024 рф, и планеты, на сайте МК.ru обновляются каждую минуту. мы отбираем главные события за день для сайта “МК”, проводя тщательный онлайн-мониторинг сообщений от прославленных информационных агентств, органов государственной власти, общественных органов и ньюсмейкеров.
выигрыш казино онлайн
Unleash the thrill of gaming like never before at our cutting-edge online casino https://bespeka.ucoz.ru/blog/2023-09-11-84 Your path to riches and excitement begins with a single click on this extraordinary link!
%%
Here is my web-site – http://mvb05032019.ru/index.php/Expert_iOS_Development_Services_in_Los_Angeles
%%
Also visit my webpage :: Smard Crypto Trading Bot
%%
My webpage – https://www.cryptospb.com
Unleash the thrill of gaming like never before at our cutting-edge online casino https://avilclub.ru/issledovanie-i-analiz-veb-sajta-shabalinskogo-rajona-kirovskoj-oblasti-resurs-dlya-informirovaniya-vzaimodejstviya-i-razvitiya Your path to riches and excitement begins with a single click on this extraordinary link!
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Meds information sheet. Short-Term Effects.
zofran
Everything trends of pills. Read information now.
%%
my blog; https://remontya.ru/gde-iskat-horoshuyu-nyanyu/
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
My web blog – https://kuttyweb.xyz/best-no-deposit-bonus-casinos-in-india/
With its iconic pink branding and weighty presence on tube web sites, you possibly bear in mind going to a LiveJasmin display, whether or not you intended to or not. If you want to skip Christian courting web-sites or senior courting websites, where all the customers are way as well critical and focused on determination and settling down, consider BeNaughty. It is significantly less common than Tinder or Match, but it has additional than three hundred million registered customers. Do you know that eHarmony results in fifteen million matches per working day? Tell her how very good she smells- Do you know that your nose is a pretty sturdy sexual organ as properly? Ask issues, inform tales, and joke. Hogan sued Gawker for $100 million for defamation, decline of privacy, and emotional discomfort because of to the release of the tape. Instead of settling for conventional porn that you have observed a million periods before, digital actuality porn and vr dwell cams give one thing new and thrilling each individual time you log on.
Very good site for check cours Bitcoin Price USD
Your gas dryer acting up can throw off your whole routine, but rest assured our team of professionals can quickly make your laundry room operational again. However, when problems do arise, you can call the professionals at Appliance Repair Orange County for reliable and trustworthy service. Appliance Doctor Inc. is here to help you repair your broken refrigerator, freezer, oven, washer and dryer, microwave, and garbage disposal. We at Appliance Doctor Inc. service all major brands of appliances. Sparkle Appliance is committed to regularly assisting residents of Detroit, Michigan and promptly fixing your freezers. Replace faulty bottom freezers older than 7 years. Although the buss system had been in operation for over six years before the new oven line was installed, the additional load is what stressed the poor connection to the point of failure. Again, periodic thermal imaging would have exposed the vulnerabilities of the electrical system prior to installation of new equipment and would have paid for itself many times over in money saved on repair costs and lost revenues. Over time, drive belts can wear down, crack, loosen, or break completely.
3. One at a time, turn each burner dial to “Light” for three seconds, then off again. The building, owned by a property management group, houses two separate companies, one involved in label printing and the second a Japanese food processes facility. It’s also their responsibility to repair anything that breaks on the property in a timely manner. Our repair man told us that for the cost of repair, we would be better off buying a new one. From right to left on most meter faces, the far right is the one that counts individual kilowatt-hours from 1 to 10; the next one counts the electricity from 10 to 100 kilowatt-hours; the third dial counts up to 1,000; the fourth counts up to 10,000; and the dial at the extreme left counts kilowatt-hours up to 100,000. If the arrow on a dial is between two numbers, the lower number should always be read. Energy efficient models help to reduce electricity bills which saves you money while providing excellent cooling services. If flooding occurs, turn off electricity at the main breaker. The main Electronic PCB Repair Company UAE has numerous times of involvement in the business. Some of the insurance company gives you a discount if you have thermal imaging done giving you a more of a reason to do this.
If your fridge or freezer is giving you trouble, call us today in Dublin to arrange an appointment to inspect and repair it. Keeping your inefficient fridge wastes two things: food that spoils and excessive amounts of energy as your deteriorating fridge tries hard to keep up. Diagnosing this issue starts with answering the question of an oven’s energy source. These repairs are essential, as a door that doesn’t properly close can significantly impact your oven’s efficiency. The windows in a home are not the same as the ones in a commercial building, but each of them can be replaced by an expert. The Department of Homeland Security recommends turning the gas off in the home any time a gas-powered appliance is not working properly. Hurricanes can destroy or damage your home and that includes your appliances. Most of you consider your appliances your valuable possessions. Perhaps one of the most widely used kitchen appliances on the market today is the microwave.
I one case, the neutral wire was completely burned and became disconnected from the terminal. Investigation into the problem exposed the neutral wire in the lighting breaker panels had been damaged by heating caused by non linier load issues (non linier loads are a topic of another discussion). Due to their compact size and reasonable price, microwaves are rapidly finding their way into most American households. Large families can invest in heavy duty washers that hold greater capacity of clothes, while singles or young couples can choose a more compact size to fill their need. The level of damage will decide based on speed, angle of impact, and obstacle size. However, it is advised to get it serviced at least once in a year to escape potential damage and enjoy durability of the machine. This won’t apply to most older refrigerators, but it may help you get a few more years out of a newer machine. The original oven had had been in place about 6 years.
Look at my webpage; https://Xdpascal.com/index.php/Whatever_They_Told_You_About_Freezer_Repair_Is_Dead_Wrong_And_Here_s_Why
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Стяжка – существенный шаг при возведении. Выравнивание пола дает возможность получить ровное основание для дальнейших работ.
Специалисты выполняют устройство стяжки пола с оглядкой на всех требований и нормативов. Стяжка пола делается с применением современных материалов, которые гарантируют надежное покрытие и стойкость.
Покрытие пола способствует сформировать идеальное основание для любых видов отделки. В Москве укладку пола проводят квалифицированные мастера.
Novost
Medicine information sheet. Brand names.
tadacip brand name
Actual information about medicine. Get information now.
Ukraine
Novyny
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Feel free to visit my web-site https://maltafawuq.net/user/ceallakjzh
Hi to all, how is the whole thing, I think every one is getting more from this site, and your views are pleasant designed for new people.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
Pills information for patients. Brand names.
buy zofran
Best about pills. Read information now.
Payday loans in Massachusetts
наилучшие онлайн казино
Experience the ultimate in online casino entertainment at your fingertips http://sp-for-you.ru/forum/viewtopic.php?f=21&t=8732&p=14399#p14399 get ready for a journey to unimaginable wealth and exhilaration – just one click away through this enchanted link.
Experience the ultimate in online casino entertainment at your fingertips http://mirforwoman.ru/igrovye-avtomaty-na-jvspin/ get ready for a journey to unimaginable wealth and exhilaration – just one click away through this enchanted link.
зеркало казино онлайн
%%
Look at my site … https://chistota-shop.ru/ekspertiza-obosnovaniya-bezopasnosti-czel-poryadok-i-neobhodimost-provedeniya.html
Smart watches supply some PDA features in a wristwatch form issue. A quantity of various operating techniques, together with Windows Mobile Pocket Pc Phone Edition, the Palm OS, the Blackberry OS for Blackberry sensible telephones, and the Symbian OS for smart phones from Panasonic, Nokia, Samsung and others. Pocket Pc is the generic title for Windows Mobile PDAs. Also, Pocket Pc devices typically require more assets and have much more RAM. Companies use inside techniques to allocate resources and assign tasks for work inside the corporate itself. Many firms permit customer service agents to work from home. When coupled with an inner scheduling system, owners can balance customer needs and employee satisfaction. Identity thieves can make use of all kinds of personal information, corresponding to your mother’s maiden title, where you went to highschool or the name of your pet. Trabish, Herman K. “CSP and PV Solar Make Each other More Valuable.” GreenTech Solar. The Psion Organiser II, launched in 1986, was particularly widespread and more than half 1,000,000 had been sold.
Review my homepage :: https://xn--72C4bmjik5Gmp.com/
Novost
Ukraine
Novyny
walk-in freezers https://ckitchen11.com/
онлайн казино суд
Значение и необходимость сертификации ИСО 9001 не поддаются сомнению что такое сертификат ИСО 9001 Получить сертификат ИСО 9001 необходимо, чтобы документально подтвердить тот факт, что предприятия соответствует установленным в стандарте требованиям.
Значение и необходимость сертификации ИСО 9001 не поддаются сомнению получить сертификат ИСО 9001 Получить сертификат ИСО 9001 необходимо, чтобы документально подтвердить тот факт, что предприятия соответствует установленным в стандарте требованиям.
Я б недодумалса.
здесь можно прочитать ноты зелёного перца, мексиканского лайма, корня имбиря, http://parfum-kazan.ru/ сандалового дерева. • 05 – в текущем году появляется древесно-фужерный аромат прекрасно сочетающийся с мужской и женской аудиторией ценителей и поклонников бренда.
where to buy generic aurogra online
It’s appropriate time to make some plans for the long run and it is time to be happy. I’ve learn this publish and if I could I wish to suggest you few interesting things or tips. Maybe you can write subsequent articles regarding this article. I wish to read even more things approximately it!
Feel free to visit my web-site – http://leebankonline.us/__media__/js/netsoltrademark.php?d=kidzeegames.com%2Ftaj-mahal-solitaire%2F
осаго оформить https://oformit-osago.ru/
Meds information sheet. Generic Name.
cost flagyl
Actual what you want to know about drugs. Get now.
I got this web page from my pal who informed me concerning
this web page and now this time I am browsing this site and reading very informative posts here.
LГҐna 500000 kr
imodium
For example, a automobile dealership might allow prospects to schedule a service heart appointment on-line. If you’re a sports car buff, you may opt for the Kindle Fire, which runs apps at lightning velocity with its excessive-powered microprocessor chip. Not only do many members pledge to raise appreciable funds for a wide range of charities, a portion of each runner’s entry fee goes to the marathon’s personal London Marathon Charitable Trust, which has awarded over 33 million pounds ($5.3 million) in grants to develop British sports activities and recreational facilities. This stuff focus the solar’s energy like a classy magnifying glass hovering over a poor, defenseless ant on the sidewalk. Microsoft, Apple and Google have been in some excessive-profile squabbles over the years. There have been a number of instances where victims have been left on the hook for tens of thousands of dollars and spent years trying to repair their credit score, but they’re exceptional.
Официальное онлайн Казино Рокс приглашает попробовать играть в автоматыТоп 10 казино Играть онлайн на официальном сайте бесплатно.
%%
my webpage https://security-corporation.com.ua/ohrana-massovyih-meropriyatiy/
%%
Here is my webpage http://autopress.lv/user/mantiabent
можно купить аттестат за 9 класс http://attestat-9-klass.ru/
Совершенно верно! Идея хорошая, поддерживаю.
в соответствии с пунктом 29 (1) Положения сроки проведения обязательной экспертизы проектировочной пакетах документов и результатов инженерных изысканий могут быть продлены по инициативе заявителя максимум на 20% рабочих дней в качестве, https://womanjour.ru/ekspertiza-proektnoj-dokumentacii-vidy-xarakteristiki-poryadok-i-osobennosti-vypolneniya.html установленном договором.
Meds prescribing information. Cautions.
lyrica
Everything news about medicament. Get information here.
Powerball is played in 45 states, the District of Columbia, Puerto Rico, and
the U.S.
So, your initial deposit will bring you a percentage of the total bonus
and some of the free spins, and so on.
%%
My blog post; https://su.tula.su/24/10/2023/kak-nanyat-nyanyu-polnoe-rukovodstvo.html
Novost
This paragraph offers clear idea for the “카지노솔루션” new people of blogging, that in fact how to do running a blog.
I deal with such information a lot. “카지노솔루션임대” I was seeking this certain information for a long time.
Hello, just wanted to mention, I liked this article. “카지노프로그램” It was practical. Keep on posting!
Its not my first time to pay a visit this web page, “카지노프로그램임대” i am visiting this website dailly and take nice facts from here all the time.
Very trust site for check cours Bitcoin Price USD
It’s awesome to go to see this website and reading “카지노사이트” the views of all mates regarding this post, while I am also keen of getting familiarity.
Way cool! Some extremely valid points!I appreciate “총판모집” you penning this article plus the rest of the website is very good.
What’s up, I desire to subscribe for this web site to take latest updates,”카지노총판모집” thus where can i do it please help.
Hi there, just wanted to say, I liked this post.”카지노api” It was helpful. Keep on posting!
Medicines information leaflet. What side effects can this medication cause?
bactrim
All news about pills. Read information here.
мое лучшее казино онлайн
film casino online
22 апреля чипмейкер Intel опубликует квартальную отчетность о рынке Forex брокер FxPro Компания выпустит финансовый отчет после завершения основной торговой сессии на американском рынке.
22 апреля чипмейкер Intel опубликует квартальную отчетность о рынке Forex выбрать брокера Компания выпустит финансовый отчет после завершения основной торговой сессии на американском рынке.
Should you put up photos of your loved ones and couple that with info like, “my husband is out of town this weekend” or “little Johnny is outdated sufficient to stay at house by himself now,” then your youngsters’s security may very well be at risk. On Facebook, customers can send personal messages or publish notes, images or videos to a different person’s wall. It’s possible you’ll submit one thing you find innocuous on Facebook, however then it’s linked to your LinkedIn work profile and you’ve put your job at risk. You say something alongside the lines of, “We do not need to fret as a result of we financial institution with a instructor’s credit score union,” or even, “We put all our cash into blue chip stocks and plan to ride it out.” Again, if you’re one the forty p.c who allow open access to your profile, then immediately id thieves know the place you bank and where you’ve got the bulk of your investments.
artГculo superior
kazino casino online
Hi there! This is my 1st comment here so I just wanted
to give a quick shout out and tell you I really enjoy reading your posts.
Can you suggest any other blogs/websites/forums that go
over the same subjects? Thank you so much!
аттестат школы 11 класс http://attestat-11-klass.ru/
Есть сайт на интересующую Вас тему.
they will be provider of information, education, site and analysis, which help users navigate in such dynamic and constantly developing space.
Демонтаж и снос частных домов с вывозом мусора в Москве и Московской области – http://msk-demontazh-doma-24.ru/. Демонтаж дома вручную и спецтехникой производим по ценам ниже рынка за 1 день. Бесплатный выезд специалиста на объект.
luckiest online casino
%%
Feel free to surf to my webpage http://www.charitiesbuyinggroup.com/MemberSearch.aspx?Returnurl=https://ocas.pl/
Payday loans in Nevada
Plus, Goss adds, you should still be eating plenty of fiber-rich, non-starchy vegetables on a low-carb or http://customsbrokerage.biz/__media__/js/netsoltrademark.php?d=metabolixketo.com diet. If you get hungry in between meals, it’s better to eat nuts or a few low carb vegetables with an ounce of cheese. But as the diet progresses and your carbohydrate restrictions relax a bit, you may be able to stop taking the supplement and get enough fiber from foods like beans, peas, avocado and fruit, along with vegetables and whole grains. It also included high-carb foods that many people consider “healthy,” such as fruit, milk, potatoes, and pasta. Plant foods contain both soluble and insoluble fiber, but the amounts vary. Taking a day or two out of your week to prep will ensure that your meals are full of muscle-building protein, filling fiber, and healthy carbs and fats-all essentials when you’re looking to drop pounds. To get the best health benefits, aim to eat a wide variety of foods, including those with both types of fiber, says Amy Goss, RD, assistant professor of nutrition sciences at the University of Alabama at Birmingham.
все дл¤ онлайн казино
онлайн казино рубль
Сантехработы, монтаж и замена сантехники, как сделать правильно полотенцесушитель водяной для ванны незаменимые в любом доме элементы не так и просто поменять своими руками.
Наша статья рассказывает про лучшие обменники криптовалюты с минимальными комиссиями http://www.2givecoin.info Мы изучили все обменники по большому количеству параметров, таких как: скорость обмена, работа службы поддержки, платежные методы и тд.
Наша статья рассказывает про лучшие обменники криптовалюты с минимальными комиссиями инфа Мы изучили все обменники по большому количеству параметров, таких как: скорость обмена, работа службы поддержки, платежные методы и тд.
atos medical
Сантехработы, монтаж и замена сантехники, как сделать правильно Электрический полотенцесушитель незаменимые в любом доме элементы не так и просто поменять своими руками.
Klicken Sie auf diese Seite
аренда юридического адреса в москве
%%
Feel free to visit my web site https://xn—3–5cdd2bh4bjdaloy.com/
Medicine information leaflet. Cautions.
Best news about drugs. Get information now.
Novyny
%%
my web blog: http://ibccongress.org/cropped-copy-of-ibc_fb-jpg/
Novost
Ukraine
Truly quite a lot of wonderful information.
С развитием технологий и интернет-сервисов, виртуальные номера стали весьма популярными среди пользователей мессенджеров и социальных сетей номер для телеграмма одним из самых популярных приложений для общения и обмена информацией является Телеграмм.
Medicine information leaflet. Brand names.
lisinopril
Everything information about pills. Read information here.
С развитием технологий и интернет-сервисов, виртуальные номера стали весьма популярными среди пользователей мессенджеров и социальных сетей виртуальные номера для телеграм одним из самых популярных приложений для общения и обмена информацией является Телеграмм.
Superb posts Thanks a lot.
In point, it is way extra modern day than a website like Chatroulette or Omegle. Special Features: A profitable chat element is 1 thing, but what about all the other characteristics that make a internet site exclusive? Customers of Pinger developed textual articles no cost can reveal on Fb or myspace, Twitter, and web site site. Skibbel is a free software that was made exclusively for sexting. Even though a word typically costs the corporations significantly considerably less than a penny to route involving mobile mobile handsets, they value people as really significantly as 20 bucks to supply a designed textual information and a person far more 20 bucks to obtain a solitary. In Dec, 2011 Pinger also won The most powerful Mobile Mind Merchandise prize. In addition, Pinger Text Free enables you to compose text out of your laptop computer – an advantage to all who need a entire-dimension crucial pad above a tiny touchscreen technological know-how when they have the preference. It was designed for the advantage of exploring your potential associate in life. The daily life of the Guillemot for the duration of the winter is a physically demanding one particular we know that substantial numbers succumb in stormy temperature, and we can infer that slight constitutional defects could possibly make all the distinction concerning failure and good results and, as a result, the less seriously the structure of the guardian is taxed during replica, and the far more securely the structure of the offspring is crafted up, the higher prospect will both have of resisting the hardships of the wintertime properly.
Pills information for patients. Long-Term Effects.
zoloft medication
All news about meds. Read information now.
https://electrica.zp.ua/
Eddie Giuliani (IFBB Mr. America, 1974): Joe experienced a two-vehicle garage wherever he lived in Venice that he converted into a machine shop. Jim Morris (Amateur Athletic Union Mr. America, 1973): What built Gold’s Gym Gold’s Gym? Joe Gold. The first Gold’s Gym was a squat sweatbox that Joe and a couple of of his pals created from cinder blocks. The movie soars on the back again of hysterical “fish out of water” comedy as Joe Pesci’s brash New Yorker Vinny Gambini clashes with a genteel Southern city keeping his wrongfully accused cousin in jail. Naishullar adopted it up trying to crowdfund a characteristic film in his signature type, which eventually turned the parkour-and-gunrunning bro violence paean Hardcore Henry, released in theaters previous April. Technically, the similar can usually be claimed of movies supposed as second capabilities in theaters and drive-ins. The Best Years of Our Lives is a single of people flicks you ought to carve out a few hrs of your everyday living to truly feel your way by way of. We were attracted to his films as substantially for their titles – Love Is Colder Than Death (1969), The Bitter Tears of Petra von Kant (1972), Ali: Fear Eats the Soul (1974) – as their information.
The employer requires to file a petition for the operate permit to the Ministry of Justice (MSJ).
Very trust site for check best cours Bitcoin Price USD
tofranil
Yes, quite a few Chaturbate options are cost-free. Are Chaturbate Alternatives Free? Most of the websites we’ve listed in this report present absolutely free content material in a person way or another. I feel the to start with procedure final December aggravated it in some way, and the second 1 built it even worse! Sites like LiveJasmin and Jerkmate give a style of cost-free content material, but the serious exhibit begins when you go on a cam two cam or personal session with just one of their cam girls or boys. LiveJasmin and Jerkmate are excellent grownup sex cam internet sites, between many other greatest cam websites, if you are on the lookout for a additional top quality working experience, as they each and every have a terrific roster and deluxe functions. With the blend of 100 % absolutely free, freemium, and high quality cam display sites in this post, there are masses of options to peruse. In her 2021 book, The Right to Sex: Feminism in the 20-First Century, the Oxford thinker Amia Srinivasan observes how her students, reared in a planet of ubiquitous on line gangbangs and sexualized violence, are innately drawn to the anti-porn ideologies of the seventies radical feminists Andrea Dworkin and Catharine MacKinnon instead of the strategies championed by Willis and her sexual intercourse-optimistic peers.
Novyny
Ukraine
Brain Guy has no imagination and just conjures a couple of spoons. As these, they generally go viral in just a few days of their launch. She obtained one particular riff in but was so disgusted by the film’s horrible good quality that she remaining just after a number of minutes. In Devil Doll, Servo, motivated by the film’s soul-swapping, asks the satan to flip him into a incredibly hot, delicious toaster pastry. There was 1 episode exactly where Crow’s Evil Twin Timmy crept into the theater, commenced attacking Servo, then dragged him out of the theater and cocooned him on the bridge, a la Alien. The pointlessly cruel Downer Ending of The Girl in Lover’s Lane does it to the bots, nevertheless Joel snaps them out of it by pointing out that the whole tale is fictional, and they’re perfectly cost-free to come up with whatever ending they want to consider as an alternative. His logic is that due to the fact Joel received to escape soon after seeing a undesirable Joe Don Baker motion picture (again in Mitchell), he deserves the identical reward for looking at just one of his personal. The present day ends up obtaining Mike’s significantly meaner brother Eddie be the human on the ship alternatively for about twenty minutes, until eventually Crow goes back and undoes his past perform.
Автоматизированное нанесение штукатурки — новаторский подход проведения штукатурных работ.
Он заключается в внедрении штукатурных станций, как правило, сделанных в Германии, что обеспечивает раствор подготавливается и апплицируется на стену автоматически и с давлением.
Машинная штукатурка С подтвержденной гарантией До 32 процентов выгоднее обычной, Можно клеить обои без шпаклевки от кампании mehanizirovannaya-shtukaturka-moscow.ru
В результате, повышается сцепление с поверхностью, а время, потраченное на работу уменьшается в пятеро–шестеро, в сравнении с ручным способом. За счет автоматизации и упрощения рабочего процесса цена механизированной штукатурки становится доступнее, чем при использовании традиционного подхода.
Для машинной штукатурки применяют специализированные смеси, стоимость которых ниже чем при ручной отделке примерно на треть. При определенных навыках специалистов, а кроме того при соблюдении всех технологических правил, оштукатуренная поверхность оказывается совершенно ровной (государственные строительные стандарты) и гладкой, поэтому, последующая обработка шпатлевкой не не обязательна, что предоставляет дополнительные средства для заказчика.
Military community relations normally write-up information on soldiers with no mentioning their family members or personal lives, so illustrations or photos are stolen from these websites by structured Internet crime gangs normally operating out of Nigeria or Ghana. A speedily increasing method scammers use is to impersonate American armed forces staff. In March, 1999, the American Academy of Pediatrics unveiled a new report entitled, “Circumcision Policy Statement,” wherein it acknowledges, for the 1st time, that “newborns who are circumcised devoid of analgesia expertise suffering and stress” and suggests utilizing analgesia to minimize circumcision soreness. A report in 2008 prompt that teledildonics, along with textual content and electronic mail and webcams, can be made use of to “wind each individual other up to fever pitch throughout the doing work day” as a prelude to sexual intercourse with a human for the duration of the night hours. Doctors report that Adam, who is in a coma, was sexually abused, but that the abuse predated his kidnapping. He was a major producer of Todd Ahlberg’s movie, Meth, a attribute-duration documentary on drug abuse among the homosexual adult men. The idea of digital sexual intercourse has been distinguished in literature, fiction and common culture, and promoters of these gadgets have claimed considering that the nineteen eighties they are the “subsequent major point” in cybersex technological innovation.
I like the helpful info you provide in your articles.
I will bookmark your weblog and check again here regularly.
I am quite certain I’ll learn many new stuff right here!
Best of luck for the next! http://redstudio.co.kr/bbs/board.php?bo_table=free&wr_id=107701
https://csin.ru/Ekonomika/
https://medium.com/@advencher1978/vps-server-ee111932b189
marked ‘poi-son,’ it is sure to make you sick. This had
Всегда свежайшие новости из сео индустрии новости сео индустрии
Являющийся уникумом (а) также ясный матерриал, обновление 2 одного в неделю
Amazing postings, With thanks!
http://tuchkas.ru/
gabapentin medication
Foot-man went on, “if we were not both on the same
Amazing info Regards.
%%
my web-site :: https://www.von-mecklenbeck.de/challenge-7-tage-ohne-zucker/
Я извиняюсь, но, по-моему, Вы не правы. Давайте обсудим это. Пишите мне в PM, пообщаемся.
first of the few exceptions to this rule is king https://mexicanstorieswithart.com/art-classes-for-kids-are-important/ billy. Welcome bonuses are almost unique offers, what can offer the btc casino.
Drugs information. Effects of Drug Abuse.
fluoxetine medication
Everything trends of meds. Read information here.
%%
Feel free to visit my website: p57678
Prestito di 7500 euro
We present to you a list of 1xbet promotional codes relevant for 2022: http://carina-e.ru/images/pages/1xbet_promokod_na_besplatnuu_stavku.html Without promotional codes, the bonus is 25,000.
We present to you a list of 1xbet promotional codes relevant for 2022: https://popvalais.ch/wp-includes/inc/?utilisez_le_code_promo_1.html Without promotional codes, the bonus is 25,000.
Рекомендую Вам зайти на сайт, где есть много статей на интересующую Вас тему.
Usually winnings in free spins are paid to user in quality additional money, what means, which in a https://www.sarahodesigns.com/6-tips-modern-furniture-part-2/ they appear with wagering expectations. before preferring bitcoin-sites for getting bonuses, read the standards rollover.
%%
Feel free to surf to my webpage; https://alpaca.kz/catalog/samokaty
Pills information sheet. Long-Term Effects.
singulair rx
Some about medicament. Read now.
urenrjrjkvnm
Хронически свежие новинки изо сео промышленности новости сео индустрии
Являющийся уникумом а также ясный матерриал, обновление 2 как-то раз на неделю
купить диплом о среднем в москве https://diplomi-srednem.ru/
Do not miss out on this opportunity if you inhabit one of the seven native English-speaking countries –
USA, Canada, UK, Ireland, South Africa, Australia, and
New Zealand.
pret 2000 euros
urenrjrjkvnm
Drug information for patients. Effects of Drug Abuse.
amoxil
Everything what you want to know about meds. Get now.
Life
Purchasing online is becoming an integral component of many individuals’s lifestyles. It’s hassle-free, fast, and also usually a lot more budget-friendly than getting in person. Having said that, there are actually some points to think about prior to you begin adding things to your cart, https://internetmarketingline.mee.nu/antique_gold_brass_5_advantages_of_online_shopping.
Рейтинг молотого кофе. Что лучше — арабика, робуста или либерика Отличный кофе топ-10 марок ароматного кофе с характеристиками вкуса и отзывами покупателей
neck of the bot-tle was a tag with the words “Drink me” printed on it.
купить диплом института http://diplomi-v-moskve.ru/
Замечательно, весьма забавная фраза
willing play at the best crypto casinos? cloudbet is fully licensed and regulated by the https://machikadonet.com/bin/perl/light.cgi?pg=0 curacao egaming, and its website uses standard software for encryption ssl.
казино онлайн
I love what you guyhs are up too. This sort of clever work and reporting!
Keep up the terrific works guys I’ve added you guys too my blogroll.
my web-site – restoration toronto
Круглосуточная доставка алкоголя в Казани. В нашем магазине вы можете заказать любимые напитки с доставкой на дом доставка алкоголя казань круглосуточно недорого у нас самые низкие цены и лучший сервис.
On the contrary, the one thing that the lumberman desired
ремонт компьютеров на дому https://remontcomputerov-na-domu.ru/
effexor mechanism of action
be a key to one of the doors of the hall, but when
Индивидуальные кухни за 10 дней напрямую от производителя, рассчитайте цену со скидкой до 37% кухни от производителя кухня от производителя с установкой за 10 дней!
Круглосуточная доставка алкоголя в Казани. В нашем магазине вы можете заказать любимые напитки с доставкой на дом заказать алкоголь с доставкой на дом казань у нас самые низкие цены и лучший сервис.
with their aim and it was only Dick’s hatchet
%%
Also visit my web page; https://monopolyliveslot.com/de/
Отказное письмо для маркетплейсов: кому нужно и как его получить отказное письмо на продукцию чтобы продавать товары на маркетплейсах, нужно доказать, что продукция безопасна для людей, животных и природы.
medicine shop
Drug prescribing information. What side effects can this medication cause?
priligy for sale
Actual trends of pills. Read information now.
urenrjrjkvnm
Application for citizenship in Russia can be filed after 5 years of residing in the country. no deposit bonus casino In order to apply for Russian Golden Visa, the foreign investor must be at least 18 years old, in a good health and must not have criminal record.
%%
Medicine information for patients. Cautions.
cialis super active
Best information about drug. Read now.
%%
my web-site; https://www.tccdescomplicado.com/forum/discussoes-gerais/zulu-gold-slot-online-cassino-gratis-zulu-gold-1
urenrjrjkvnm
Life
Вы поистине безошибочно полагаете. Хорошо, что я сюда забежал. Благодарю!
Here is my web-site :: https://general-machines.ua/ru/nedorogoj-frontalnyj-pogruzchik/
Medicines information. Short-Term Effects.
levitra otc
All information about drug. Read now.
tento pЕ™ГspД›vek
Good day I am so excited I found your weblog,
I really found you by error, while I was researching on Askjeeve for something else, Anyways I am here
now and would just like to say kudos for a incredible post and
a all round entertaining blog (I also love the theme/design), I don’t have time to read it
all at the minute but I have book-marked it and also included your RSS feeds, so when I have
time I will be back to read a lot more, Please do
keep up the excellent work.
%%
Feel free to visit my website; https://senseiinu.io/
urenrjrjkvnm
urenrjrjkvnm
Life
Dear immortals, I need some wow gold inspiration to create.
%%
my blog; https://jokersjewels.com/
Имеется множество автосервисов и технических центров, специализирующихся на обслуживании и ремонте автомобилей Audi и Skoda автосервис ауди Один из таких – автосервис Ауди.
%%
Visit my page … https://plinko1win.com/
Имеется множество автосервисов и технических центров, специализирующихся на обслуживании и ремонте автомобилей Audi и Skoda ремонт авто шкода Один из таких – автосервис Ауди.
Cel mai prietenos ?i crazy gadget store care i?i va colora experien?a digitala cu emo?ii, stil ?i creativitate redmi note Ne-am lansat in martie 2013 ?i am adus cu noi „Festivalul Culorilor”
Cel mai prietenos ?i crazy gadget store care i?i va colora experien?a digitala cu emo?ii, stil ?i creativitate jocuri de masa chisinau Ne-am lansat in martie 2013 ?i am adus cu noi „Festivalul Culorilor”
Пентралапон — это экологически чистый строительный материал https://ingkerreke.org.au/?URL=pentralapon-astra.ru представляет собой смесь для ручной и автоматизированной отделки стен, потолков и других поверхностей.
Пентралапон — это экологически чистый строительный материал https://clients1.google.gp/url?q=http://pentralapon-astra.ru представляет собой смесь для ручной и автоматизированной отделки стен, потолков и других поверхностей.
You actually expressed this exceptionally well.
Feel free to surf to my web-site – http://forexmob.ru/user/AlanaBlevins0/
HD porn
яндекс тв программа екатеринбург
драгон мани casino
Всегда свежие новинки из сео промышленности новости сео индустрии
Являющийся уникумом а также свежий матерриал, обновление 2 раза на неделю
how to get finpecia no prescription
минск тв программа передач на сегодня
pret 3000 euros
On the contrary, the one thing that the lumberman desired
здесь можно произвести кузовной ремонт автомобиля, если он был поврежден в результате аварии или коррозии ремонт авто шкода Все работы выполняются высококвалифицированными специалистами с использованием современных технологий и оборудования.
Medication information leaflet. Short-Term Effects.
zithromax
All trends of drugs. Read information now.
здесь можно произвести кузовной ремонт автомобиля, если он был поврежден в результате аварии или коррозии автосервис audi Все работы выполняются высококвалифицированными специалистами с использованием современных технологий и оборудования.
urenrjrjkvnm
LГҐna 80000 kr
расписание 12 школа волжский
%%
Take a look at my blog https://betterlongisland.com/
Medication information. Long-Term Effects.
prednisone tablet
Actual information about drug. Get here.
PЕЇjДЌka 14000 KДЌ
%%
Take a look at my homepage :: australiawtpglobal.com
Medicament prescribing information. What side effects?
cost stromectol
Everything about medicine. Read here.
Life
теперь один вопрос:кто меня из под стола достанет!?
y el punto es que el mundo del vino tiene esta magia. Siente esto y vive con el corazon y el alma invertidos a menudo y a cada paso https://munnekehoveniers.nl/2015/02/02/154-tips-on-avoiding-scotland-tourist-traps/.
urenrjrjkvnm
https://www.site-lady.ru/content/pgs/melbet_promokod___bonus_pri_registracii.html
проститутки метро ладожская
dramamine
Thanks a lot for sharing this with all people you actually understand
what you’re speaking about! Bookmarked. Please also discuss with my website =).
We may have a link exchange contract between us
Скачать свежую музыку и обогатить плейлист https://besthitmp3.ru/
seo продвижение сайта заказать https://seo-prodvizhenie-almaty.kz/
https://xn--e1aa2af.xn--p1ai/prajs/ Стоимость переводов в Краснодаре Указанные цены являются ориентировочными и не являются публичной офертой. Точную стоимость перевода может назвать менеджер бюро только при визуальной оценке документов. Потому используя прайс вы можете узнать лишь примерную стоимость наших работ. Гораздо лучше отправить файл(ы) на оценку и в кратчайшие сроки, абсолютно бесплатно получить точный расчет стоимости и сроков.
Вы можете приобрести Пентралапон оптом и в розницу у авторизованных дилеров и поставщиков https://3d.skr.jp/cgi-bin/lo/refsweep.cgi?url=http://pentralapon-astra.ru
Пять лет мы искали свой звук – уникальный и запоминающийся, пять лет мы экспериментировали и меняли саунд-продюсеров. Мы находили и теряли, ругались и мирились, – всё ради нашей музыки и права на сцену… Тернист путь к себе, но сейчас мы понимаем что наша музыка – это музыка весны!
каспий музыка
Отказное письмо для маркетплейсов: кому нужно и как его получить как получить отказное письмо для маркетплейса С экспертом разбираемся, когда это нужно и как его оформить. Отказное письмо для маркетплейса — документ, который подтверждает, что конкретная продукция не подлежит обязательной сертификации и декларированию.
Вы можете приобрести Пентралапон оптом и в розницу у авторизованных дилеров и поставщиков https://dosxtremos.com/?URL=pentralapon-astra.ru
%%
Here is my blog post – https://sensei-inu.com/
Отказное письмо для маркетплейсов: кому нужно и как его получить отказное письмо на продукцию С экспертом разбираемся, когда это нужно и как его оформить. Отказное письмо для маркетплейса — документ, который подтверждает, что конкретная продукция не подлежит обязательной сертификации и декларированию.
https://xn--e1aa2af.xn--p1ai/katalog-yazykov-s-kotorymi-my-rabotaem/ Список языков, которые мы переводим в Москве Список языков, с которыми мы работаем, включает более двухсот направлений перевода, охватывая более 30 иностранных языков. Однако основные направления, которые составляют более 80% всех заказов в нашем бюро переводов, включают английский, немецкий, итальянский, французский, испанский и китайский. Ежедневно мы выполняем переводы с них на русский и наоборот.
https://xn--e1aa2af.xn--p1ai/tehnicheskij-perevod/ Технический перевод в Химках Компания «Ремарка» более 20 лет успешно занимается переводами технических текстов любой сложности. За этот период сотрудники нашего бюро выполнили множество проектов для организаций, промышленных предприятий, частных лиц города Москва и Краснодара, а также заказчикам из РФ и всего остального мира.
Отказное письмо — это информационный документ, который сообщает, что товар не нужно сертифицировать отказное письмо Появился в начале 2010-х, когда только начинали делать декларации.
urenrjrjkvnm
%%
Visit my site; https://uno-juego.es/pag/codigo_promocional_bono.html
where buy cheap plavix
В МФО онлайн могут многие обращаться. Здесь даже быстрые займы без процентов на карту дают займ первый без процентов И никто вашей кредитной историей не интересуется. Оформление быстрое.
В МФО онлайн могут многие обращаться. Здесь даже быстрые займы без процентов на карту дают https://zaim-bez-procentov-mfo.ru/ И никто вашей кредитной историей не интересуется. Оформление быстрое.
Хотите освоить искусство шитья, вязания, валяния и других творческих направлений? сливы курсов торрент скачайте наши курсы и расширьте свои навыки в широком спектре рукоделия.
Хотите освоить искусство шитья, вязания, валяния и других творческих направлений? торрент сливы курсов скачайте наши курсы и расширьте свои навыки в широком спектре рукоделия.
The Zephyrus S17 has a large four cell, 90WHr battery. Four tweeters are positioned beneath the keyboard whereas the 2 woofers sit beneath the show. Overall, these two benchmark outcomes bode nicely for avid gamers wanting a laptop computer that’s a lower above when it comes to graphics efficiency, with the high frame charges equating to a smoother gaming experience and more detail in every scene rendered. Because the Xbox 360 cores can each handle two threads at a time, the 360 CPU is the equal of having six standard processors in a single machine. The sheer quantity of calculating that is completed by the graphics processor to determine the angle and transparency for each reflected object, and then render it in real time, is extraordinary. Southern California artist Cosmo Wenman has used a 3-D printer to make meticulously rendered copies of well-known sculptures, based upon plans normal from a whole bunch of pictures that he snaps from every angle. Many firms supply a combination of these plans. With its combination of a Core i9-11900H CPU, a Nvidia RTX 3080 GPU, and 32GB of RAM, this laptop performed exceedingly nicely in performance benchmarks that present insight into its CPU energy and cooling. What this means when you are taking part in video video games is that the Xbox 360 can dedicate one core entirely to producing sound, whereas another may run the game’s collision and physics engine.
Howdy! I just want to offer you a huge thumbs up for your great
information you have here on this post. I’ll be
returning to your web site for more soon.
А что-нибудь аналогичное есть?
http://www.fpv.org.ve/wordpress/actualizacion-de-datos/ Bellagio. En la capital de la emocion tambien se encuentra este otro establecimiento, que surgio en 90 y se convirtio casi наиболее|наиболеераспространенных significativo en todo el mundo.
Free and best HD porn
clozaril
Pills prescribing information. Brand names.
trazodone buy
All about medicines. Get information here.
%%
my homepage … https://brazil888poker.com/
Drug information sheet. Cautions.
provigil medication
Everything news about medicine. Read now.
By rolling more than the foam roller, you can target and release muscle
tension, knots, and trigger points, improving flexibility and aiding muscle
recovery.
Вы истинно отлично полагаете. Прекрасно, что я в это место пришел. Спасибо.
Here is my web page: http://etehnik.ru/%D0%92%D0%BE%D0%BF%D1%80%D0%BE%D1%81%D1%8B/kak-kupit-perednij-pogruzchik-kun-instrukciya-dlya-uspeshnyx-pokupok-22/
%%
Look at my site … https://mebel-3d.ru/libraries/news/?betvinner_promokod_pri_registracii___258825.html
famciclovir 250mg
Discover the grandeur of Castle in Estonia for rent, an exquisite location for events and historical experiences in Estonia!
Профессиональная переподготовка по более чем 20 направлениям в отрасли строительства профессиональная переподготовка строительство дипломы установленного образца, индивидуальные программы
Рост продаж сопровождается ростом цен. Объем торгов на вторичке по сравнению с прошлым годом вырос на 25% какую машину лучше купить в 2023 году лучшими б/у автомобилями являются Opel Meriva, Audi Q5, Toyota Avensis, BMW Z4, Audi А3, Mazda 3 и Mercedes GLK.
Drug information. Drug Class.
baclofen
Actual news about drug. Get information now.
urenrjrjkvnm
Novost
Oll porn
Купить бытовку недорого от ведущего производителя по самым низким ценам https://dombitovok.ru/ разумный, выгодный и логичный шаг заказчика без издержек по времени.
Конечно. Это было и со мной. Давайте обсудим этот вопрос. Здесь или в PM.
Хоча УКРАЇНА контролює свою акваторію, кажуть військові, https://www.trails-endurance.com/matos/shopping/application-entrainement-garmin російська авіація досі залишається досвідченої в повітрі.
Payday loans in Mississippi
Выгодные предложения по ипотеке на готовое жилье от проверенных банков в 2023 году калькулятор ипотеки подберите для себя самый выгодный вариант ипотеки на готовое жилье.
накрутка поведенческих http://nakrutka-pf-factorov.ru/
Универсальный калькулятор ипотеки для всех банков. Расчет ежемесячного платежа за несколько секунд ипотечный калькулятор онлайн наглядный график погашения.
Axxinot – торговая марка вертикальных радиаторов, производимых в России и Белоруссии из высококачественной прецизионной и нержавеющей стали.
%%
Have a look at my page: https://sweechkish.com/
30000 euro lenen
goodrx albuterol
Pin Up Sweet Bonanza
Apple has deployed out-of-date terminology as a result of the “3.0” bus should now be known as “3.2 Gen 1” (as much as 5 Gbps) and the “3.1” bus “3.2 Gen 2” (as much as 10 Gbps). Developer Max Clark has now formally introduced Flock of Dogs, a 1 – eight player on-line / native co-op expertise and I’m somewhat bit in love with the premise and magnificence. No, it’s possible you’ll not deliver your crappy old Pontiac Grand Am to the native photo voltaic facility and park it in their entrance lawn as a favor. It’s crowdfunding on Kickstarter with a aim of $10,000 to hit by May 14, and with almost $5K already pledged it ought to simply get funded. To make it as straightforward as doable to get going with friends, it would supply up a special in-built “Friend Slot”, to permit someone else to join you through your hosted sport. Those evaluations – and the way in which firms address them – could make or break an enterprise. There are additionally options to make some of the brand new fations your allies, and take on the AI collectively. There are two types of shaders: pixel shaders and vertex shaders. Vertex shaders work by manipulating an object’s position in 3-D space.
Meds information. What side effects can this medication cause?
zoloft without dr prescription
All news about medicine. Read here.
buy doxycycline no prescription uk
Хронически свежайшие новинки из сео индустрии Seo новости
Уникальный а также свежий матерриал, самообновление 2 как-то раз в течение недельку
urenrjrjkvnm
Novost
Реальные ставки по ипотеке от 6%, одна заявка на ипотеку онлайн сразу в несколько банков. От 2 часов на одобрение заявки онлайн калькулятор ипотеки ипотека на покупку вторичного жилья и новостроек.
Medication information. Generic Name.
mobic
Everything about pills. Get here.
Льготные программы ипотеки в Москве с господдержкой. Выгодные ставки по кредиту на покупку жилья ипотека в москве оформление ипотеки и проведение сделки онлайн.
%%
My web site radiostopfm.com
https://theshaderoom.com/articl/actual_melbet_promo_code_for_deposit_bonus.html
Возможно кто-то осведомлен, как связаться с администратором? Пишу в обратную связь, он не дает ответ!
Feel free to surf to my website :: http://etehnik.ru/%D0%92%D0%BE%D0%BF%D1%80%D0%BE%D1%81%D1%8B/oformit-zakaz-na-frontalnyj-minipogruzchik-kun-opisanie-dlya-udachnyx-priobretenij-22/
накрутка пф москва http://povedencheskie-factori.ru/
https://exploringupstate.com/pag/1xbet_promokod___aktualnuy_segodnya.html
http://1by.by/stat/1xbet-promokod-bonus-za-registraciyu-130-evro.html
Что такое отказное письмо по сертификации и кому оно нужно. Отказное письмо — документ, который подтверждает, что товару не требуется сертификат качества или декларация соответствия отказное письмо на продукцию чтобы продавать товары на маркетплейсах, нужно доказать, что продукция безопасна для людей, животных и природы.
cetirizine 10mg
Что такое отказное письмо по сертификации и кому оно нужно. Отказное письмо — документ, который подтверждает, что товару не требуется сертификат качества или декларация соответствия отказное письмо чтобы продавать товары на маркетплейсах, нужно доказать, что продукция безопасна для людей, животных и природы.
Отказное письмо (ОП) – это документ, который удостоверяет, что изделие/товар/материал не подлежат обязательной оценке качества и получению сертификата/декларации в определённой системе Отказное письмо отказные письма оформляются в разных сертификационных системах.
Medicament information. What side effects can this medication cause?
cheap lisinopril
All news about medication. Get now.
Отказное письмо (ОП) – это документ, который удостоверяет, что изделие/товар/материал не подлежат обязательной оценке качества и получению сертификата/декларации в определённой системе как получить отказное письмо отказные письма оформляются в разных сертификационных системах.
Для вас работает алкомаркет — доставка водки на дом круглосуточно, быстро, надежно! В ассортименте каталога вас ждет отличное крепкое спиртное: алкоголь на дом московская область заказать водку с доставкой на дом не будет сложно.
Для вас работает алкомаркет — доставка водки на дом круглосуточно, быстро, надежно! В ассортименте каталога вас ждет отличное крепкое спиртное: доставка алкоголя недорого москва заказать водку с доставкой на дом не будет сложно.
fГҐ fakta
domstroi.info
I every time used to study article in news papers but now as I am a user of net therefore from now I am using net http://emigrantbankfineartfinance.us/__media__/js/netsoltrademark.php?d=kidzeegames.com%2Ft-r-e-v-o-r-3-extreme-mad-story%2F articles or reviews, thanks to web.
%%
Also visit my blog post: https://playpropokerdomkz.com/
%%
My web blog: australiabetonlinepoker.com
%%
My page; sugarpromocodes.com
Amongst workers who have that privilege, 35%
of Democrats said they would leave a job if they had been told to
come in five days a week, compared with 23% of Republicans.
According to the Korea Casino Association, the very first-half casino sales of Kangwon Land Inc, the only
South Korean casino serving locals, amounted to KRW302.17 billion.
The country has clear and concise gambling legislation, with a regulatory framework intended
to stop crime and present protection to UK gamblers.
%%
Here is my site: купить диплом автомобильного техникума
%%
my site; купить диплом времен ссср
https://www.forumishqiptar.com/images/pages/?1win_promo_code_7.html
porn videos for free
Drug information. Drug Class.
trazodone buy
Best what you want to know about medicament. Get here.
urenrjrjkvnm
coin
Novost
Каждый человек приходит в этот мир для реализации своего потенциала антон винер биография Важно оказаться в университете, который поможет выполнить эту задачу.
https://mangroveactionproject.org/articles/melbet_promo_code_welcome_bonus_for_sports.html
Вам пригодится временные виртуальный номер. Они есть бесплатные. Но их очень быстро занимают https://myblogs.me/forum/showthread.php?tid=220289 поэтому только и остается вам воспользоваться платными виртуальными номерами.
Вам пригодится временные виртуальный номер. Они есть бесплатные. Но их очень быстро занимают http://doctorsforum.ru/viewtopic.php?f=125&t=33107 поэтому только и остается вам воспользоваться платными виртуальными номерами.
In a retrospective analysis, Healey et al lasix hyperkalemia
Medicines prescribing information. Short-Term Effects.
how to get nolvadex
All news about meds. Read now.
Bonus promotionnel du code 1xbet – Bonus d’inscription de 130 €/$. Les codes bonus du bookmaker 1xBet sont faciles Г trouver dans l’espace Internet public. Fondamentalement, ces offres sont publiГ©es sur des sites partenaires et des ressources Internet thГ©matiques qui mettent en Г©vidence le travail du bureau 1xBet, ses avantages et ses fonctionnalitГ©s. Dans ces articles et matГ©riels, des codes promotionnels sont inclus, juste Г l’endroit oГ№ il est dГ©crit en dГ©tail l’avantage de s’inscrire sur le site de jeu via un code promotionnel. Habituellement, ces blocs, oГ№ le code bonus est placГ© directement, fonctionnent comme de la publicitГ©, motivant les utilisateurs Г copier le code et Г procГ©der Г l’enregistrement sur le portail du jeu.
Xhmaster Pakistan betting sites deposit with Crickex Jazzcash,为其用户提供广泛的视频和类别。 凭借其丰富的内容,它已成为那些寻找成人娱乐的人的首选目的地。 在本指南中,我们将探索 Xhmaster 的世界,并为您提供该网站所提供内容的全面概述。
https://www.facebook.com/groups/1355228905114826 1xbet welcome bonus promo code ??VIPREG2024
Всегда свежие новости изо сео индустрии новости сео индустрии
Уникальный и свежий матерриал, обновление 2 как-то раз в течение неделю
Best Luxury Iinteriors in Dubai Trussardi Residences
This is my first time visit at here and i am genuinely pleassant to read all at alone place. http://www.kdri.co.kr/bbs/board.php?bo_table=free&wr_id=888860
В Ant Models мы предлагаем только высококлассные эскорт-услуги в Москве https://ant-models.ru/
Drug information sheet. Generic Name.
zoloft tablets
Actual news about drug. Get now.
You have made your point extremely nicely..
Наша компания предлагает гантели обрезиненные разборные. Покрытие на этих гантелях способствует длительному сроку службы. Оно защищает металл от ржавчины и царапин. Помимо этого, покрытие существенно снижает шум при выполнении упражнений, что делает их отличным выбором для домашних тренировок. В случае падения снаряда резина дает возможность смягчить удар, минимизируя потенциальные повреждения пола, и снижая риск получения травмы для спортсмена. Разборные гантели можно применять для силовых упражнений, функционального фитнеса, аэробных тренировок и выполнения упражнений для реабилитации. Большой диапазон регулируемого веса дает возможность прорабатывать все тело – от маленьких стабилизирующих мышц до более крупных.
It caused one more boom, and the supervisory authorities issued stricter recommendations for
fair and secure gaming pleasure.
Подбор зимних шин по типоразмеру: R15. Каталог шин на автомобиль с ценами в размере обзор зимних шипованных шин Купить зимнюю резину дешево в интернет-магазине.
Utilisation du Code promo du casino 1xbet lors de votre inscription, vous pouvez obtenir un bonus de bienvenue pour un nouveau client d’un montant allant jusqu’а 130?/$, ce qui vous donnera un bon dйpart dans vos paris sportifs en ligne. Grвce а la publicitй sur le portail de jeux 1xbet lui-mкme et aux publications sur les ressources thйmatiques et partenaires, de nombreuses personnes connaissent le bonus d’inscription. А bien des йgards, c’est grвce а lui que le nombre de clients des bookmakers ne cesse de croоtre. C’est grвce а ce type de bonus que les joueurs disposent d’un montant substantiel qui peut кtre dйpensй en paris. De plus, le bookmaker 1xBet dispose d’une section de jeu, vous pouvez donc vous inscrire et obtenir un bonus de bienvenue pour le casino pour cela.
getx
where can i get cheap aurogra tablets
1xbet code promo pari gratuit – Bonus VIP jusqu’а 130 ?/$ Offer Offre de bienvenue. 18 Les conditions gйnйrales s’appliquent. Lorsqu’un utilisateur lit le matйriel sur les activitйs du bookmaker 1xBet, sur les caractйristiques et les avantages de sa plateforme de jeu et ses gйnйreux bonus, il tombera certainement sur un bloc dans le texte. Dans ce bloc, il y aura une offre pour aller sur le site Web du bookmaker, s’inscrire et avoir accиs а tous les avantages йnumйrйs.
Блестяще
специалисты компании – сведущие и грамотные эксперты с глубокими познаниями в разных сферах: от биологии до свидетельство о смерти купить в москве программирования.
Что делать, если покупатель на маркетплейсе просит отказное письмо. Производители и продавцы товаров должны предоставлять отказное письмо по запросу маркетплейса, Роспотребнадзора или клиентов https://www.sostav.ru/blogs/30357/41753 Требование относится к отечественной и импортной продукции. Отказные письма бывают двух видов: для торговли и для таможенного оформления.
Что делать, если покупатель на маркетплейсе просит отказное письмо. Производители и продавцы товаров должны предоставлять отказное письмо по запросу маркетплейса, Роспотребнадзора или клиентов отказное письмо на товар Требование относится к отечественной и импортной продукции. Отказные письма бывают двух видов: для торговли и для таможенного оформления.
Best Luxury Iinteriors in Dubai Trussardi Residences Dubai
Всегда свежайшие новости с сео промышленности Seo новости
Уникальный а также свежий матерриал, самообновление 2 одного в недельку
abilify medication classification
It’s a great alternative for these hunting to make
a slow and steady profit with low threat.
Best Luxury Iinteriors in Dubai Trussardi Residences Al Furjan
You can also extend the loan term with a refinance, giving you
far more time to repay.
The bid procedure continues according to the previously announced time
schedule.
You will see that as the term of the loan increases, your month-to-month payments go down, but the overall cost of the loan (i.e., the
total paid) rises.
plan b
Bonus d’inscription 1xbet – Bonus VIP jusqu’а 130 ?/$ Offer Offre de bienvenue. 18 Les conditions gйnйrales s’appliquent. Lorsqu’un utilisateur lit le matйriel sur les activitйs du bookmaker 1xBet, sur les caractйristiques et les avantages de sa plateforme de jeu et ses gйnйreux bonus, il tombera certainement sur un bloc dans le texte. Dans ce bloc, il y aura une offre pour aller sur le site Web du bookmaker, s’inscrire et avoir accиs а tous les avantages йnumйrйs.
п»ї1x code bonus de pari pour 2023, seulement, il vous donne un bonus de bienvenue de 100% jusqu’а 130?/$. Il s’agit d’un bonus de dйpфt d’inscription, et vous pouvez l’utiliser pour les paris sportifs et les sports. Le programme de bonus du bookmaker 1xbet couvre presque toutes les activitйs de jeu des clients. De plus, les offres en termes de bonus peuvent concerner aussi bien les dйbutants que les joueurs expйrimentйs, offrant des prйfйrences et des avantages supplйmentaires а diffйrentes йtapes du jeu.
Medicines information. Effects of Drug Abuse.
strattera medication
Best about drugs. Get information now.
Therefore, using the slang of a individual group associates an individual with that group. Jonathon Green, even so, agrees with the chance of a Scandinavian origin, suggesting the exact root as that of sling, which means “to throw”, and noting that slang is thrown language – a speedy and truthful way to make your place. Hence, it is really essential for on the web daters to do it the right way and make on the web Latin relationship protected, enjoyable stuffed and hassle-free. These women are normally chubby and carrying a few added pounds, and nonetheless these dating sites are bursting with new associates. You may well determine that you want to purchase a property as a long time period financial commitment, or you might ascertain that brief expression investments are superior suited to you. Some buyers have a mix of limited phrase and extensive expression investments. Much like any other wholesaler, you would buy properties at small prices and resell the qualities to other traders.
Вкуснейшая пицца, мощные бургеры, сладкие пироги и многое другое с бесплатной доставкой по Оренбургу https://mix-dostavka.ru/ Доставка правильного питания.
Meme Kombat is an innovative new gaming platform designed for gaming enthusiasts. From active betting to passive staking, there are rewards for all users. 1 $MK = $1.667 1.Go site http://www.google.com/amp/s/memkombat.page.link/code 2.Connect a Wallet 3. Enter promo code: (web3apizj) 4. Get your bonus 0,3$MK ($375)
Drug information leaflet. Brand names.
generic cipro
Best about medication. Get information now.
Вкуснейшая пицца, мощные бургеры, сладкие пироги и многое другое с бесплатной доставкой по Оренбургу доставка полезного питания москва Доставка правильного питания.
свая 89 https://svaipro1.ru/
Купить нержавеющие трубы по доступным ценам за метр от производителя. Действуют скидки! Склады в Москве и всей России трубы нержавеющие Быстрая доставка! Заказать трубы из нержавеющей стали.
Хронически свежайшие новости изо сео промышленности Seo новости
Являющийся уникумом а также ясный матерриал, самообновление 2 в одно прекрасное время в течение неделю
ОГО , ну наконецто
и нахождения ошибки при получении диплома, диплом спо купить курьер сразу забирает его и в течение течение 1-2 дней привозит новый экземпляр.
that she was, she set out to hunt for them, but they
%%
Check out my blog post :: br888pokeronline.com
%%
my site: https://rizkisadig.com/
les denne artikkelen
instukzia.com
Medicine information. Generic Name.
fluoxetine without insurance
Best about medicament. Get information now.
If some one desires to be updated with latest technologies after that he must be go to see this site and be up to date every day.
%%
Stop by my web blog https://eternia.soforums.com/profile.php?mode=viewprofile&u=2907
%%
Also visit my blog – содержанки Мурманск
гет икс официальный сайт
Запуск новой линии погрузки угля – один из последних шагов к выводу навалочных терминалов ОТЭКО в порту Тамань отэко тамань на проектную мощность в 72 млн тонн грузов в год.
A low rating, on the contrary teplica-parnik.net, repels customers, so try to offer only a high level of quality of service.
Мне лично очень нравится сей вебсайт, по той причине, что здесь так много полезного материала:D
coin
%%
my site … https://dip997.com/medicinskiy-diplom-s-zaneseniem-v-reestr/
Drugs information leaflet. Effects of Drug Abuse.
rx neurontin
Everything trends of drugs. Read now.
Компания «ОТЭКО», оператор морских терминалов в порту «Тамань», приступила к реализации проекта «Комфортный порт» отэко тамань он предусматривает строительство новых жилых модульных корпусов и административных помещений.
EnchagPT Blog to miejsce, gdzie można znaleźć interesujące artykuły i informacje
na temat technologii sztucznej inteligencji.
Jest to blog dedykowany wszystkim entuzjastom sztucznej inteligencji, którzy pragną zgłębiać swoją wiedzę na temat tego fascynującego tematu.
Хронически свежие новинки из сео индустрии Seo новости
Уникальный и свежий матерриал, обновление 2 одного в течение неделю
ремонт стиральных машин
meilleur code promo pour 1xbet https://tandwielen.com/images/pages/code_promo_163.html
Today, a large number of Internet users are betting on sports https://www.bf-mechta.ru/wp-content/pages/stavki_na_kibersport_novichkam_.html Someone treats it as entertainment, and someone as a part-time job.
Today, a large number of Internet users are betting on sports https://doupe.zive.cz/clanek/recenze-hry-the-chant-kdyz-rozbitou-dusi-leci-psychopat-nemuze-to-dopadnout-dobre/?showforum=1#ITEM_227873 Someone treats it as entertainment, and someone as a part-time job.
A person will leave a comment if it is a category of services stroibloger.com, goods or transport
Сертификат соответствия СМК требованиям ИСО 9001 – документ, который выдается по результатам экспертной проверки и подтверждает, https://www.sostav.ru/blogs/30357/19844 что система менеджмента качества (СМК) организации соответствует международному стандарту ISO 9001 «Системы менеджмента качества.
%%
Here is my web blog; Индивидуалки Тарко-Сале
Diameter: 9.42/pi = 3 feet rounded tto tһe nearest integer
Here iѕ my web site รวมคลิปโป๊ไทย
PЕЇjДЌka 600000 KДЌ
urenrjrjkvnm
Medicament prescribing information. Long-Term Effects.
cost fluoxetine
Best trends of medicament. Read here.
%%
Feel free to surf to my web page; Работа для девушек Иркутск
haga clic para mГЎs
я уже смотрела
просматривать бесконечное множество кликов Вам готовы доставить бытовую аппаратуру, строительные материалы, одежда, обувь, купить аттестат за 11 классов с занесением в реестр все съестное и иные покупки “из открытых источников”.
As in any other foreign land, getting in a position to speak the neighborhood language and adapt will go a long way in assisting you adapt.
%%
My webpage :: https://dosug52.com/city/bor
There were just more than ten million complete-time employed people today as captured by the June QES.
The original purpose of the solution naoni.info book is to help the student with homework.
%%
my homepage – http://pixbetpixbetbr.fotosdefrases.com/pixbet-site-oficial-pix-bet-br
buy finasteride 5mg cvs
where to buy generic sildigra without rx
Code promo 1xbet pour aujourd’hui https://magmamagnets.com/pages/code_promo_163.html
Хронически свежие новинки из сео индустрии Seo новости
Уникальный да свежий матерриал, обновление 2 одного в течение недельку
prednisone buy online uk
Medicament information leaflet. What side effects?
zovirax generics
All about meds. Read here.
Сертификат ISO 9001 (или ИСО 9001) подтверждает, что система менеджмента качества (СМК) соответствует всем требованиям стандарта ГОСТ Р ИСО 9001-2015 https://www.sostav.ru/blogs/30357/41792 другими словами, сертификат выдается не на саму продукцию или услуги, а на процессы производства (порядок работы)
Серия ISO 9000 касается требований к управлению предприятием для обеспечения выпуска качественной продукции как получить сертификат исо 9001 она основывается на 8 принципах.
Линия позволит сократить минимальное время обработки судов Capesize в порту Тамань в два раза — c 48 до 24 часов отэко тамань команду «Пуск» в ходе телемоста между Москвой и Таманью дал заместитель председателя правительства.
Серия ISO 9000 касается требований к управлению предприятием для обеспечения выпуска качественной продукции сертификация исо 9001 она основывается на 8 принципах.
Working with cable firms, offering apps for video providers like MLB and HBO, redesigning the interface to work better with its Kinect motion controller — Microsoft desires the Xbox to be used for the whole lot. Since these companies only depend on having a reliable phone, internet connection and net browser, companies have looked more and more at hiring residence-primarily based staff. Even worse, since individual games can have friend codes, conserving observe of pals is far more difficult than it is on the unified Xbox Live or PlayStation Network platforms. While many launch video games aren’t particularly inventive with the GamePad controller, which will change over the lifetime of the console — it truly is the Wii U’s most defining and necessary function. There are a variety of websites that characteristic slot video games on-line that one will pay without cost. Nintendo’s clearly looking past games with the Wii U, and Miiverse is an enormous part of that plan.
my web blog https://Slotbet1688.com/
coin
By checking information using the service using the whois protocol, the user will immediately poiskmonet.com determine the registrar and site administrator when this domain was registered on the hosting.
Здесь вы сможете заказать эскорт-услуги в Москве от элитных эскорт-моделей агентства Platinum Escort https://msk-escort.com/
Восстановление данных с жесткого диска – Сервис DataLab в Киеве https://datalab.com.ua/ru/vosstanovleniye_dannykh_s_hdd/
Medicament information sheet. What side effects?
buy colchicine
Everything what you want to know about meds. Read now.
to know?” As she said this, she saw in front of her
code promo 1xbet 2024 https://www.bnbaccess.eu/news/code-promo-1xbet.html
%%
my page :: eld0radyswin.com
казино игровые автоматы
The solver is quite stroihome.net capable of replacing a tutor for a child.
%%
Here is my web-site – Последние новости Чехии сегодня – Деловая Европа
My family every time say that I am killing my
time here at web, however I know I am getting familiarity every day by reading such pleasant content.
%%
My blog – Работа для девушек Тюмень
code promo 1xbet burundi https://popvalais.ch/wp-includes/inc/?code-promo-1xbet-burkina-faso-78-000xof.html
Я думаю, что Вы допускаете ошибку. Давайте обсудим.
дело в том, что удостоверение – это такая выпускная работа студента, и она обязана быть написана по одной всех официальных нормативов и установленных правил, нарушение которых приводит к тому, купить аттестат что дипломная работа признаётся несоответствующей и не допускается к защите.
Meds prescribing information. Generic Name.
maxalt
All trends of medicine. Read now.
Апелляционная жалоба – это письменное обращение к вышестоящему суду с просьбой пересмотреть решение первой инстанции http://advtver.ru/ она должна содержать юридически обоснованные аргументы, доказывающие неправильность или несправедливость данного решения.
ОТЭКО сделает порт комфортным: компания благоустраивает свои терминалы в порту Тамань отэко тамань цель проекта – создать для рабочих и офисных сотрудников максимально комфортные условия труда.
Всегда свежие новости с сео промышленности Seo новости
Являющийся уникумом а также свежий матерриал, самообновление 2 как-то раз в течение неделю
liked and left off when they liked, so that no one
программа передач ачинск на сегодня
Выбираем оптимальный метод бурения скважины на воду: все плюсы и минусы технологий https://pfo.volga.news/684228/article/vybiraem-optimalnyj-metod-bureniya-skvazhiny-na-vodu-vse-plyusy-i-minusy-tehnologij.html доступ к чистой питьевой воде имеет ключевое значение для здоровья и благополучия людей.
Выбираем оптимальный метод бурения скважины на воду: все плюсы и минусы технологий оптимальный метод бурения скважины на воду доступ к чистой питьевой воде имеет ключевое значение для здоровья и благополучия людей.
I be compelled say, as a caboodle as I enjoyed reading what you had to articulate, I couldnt help but suffer the loss of property after a while. Its as if you had a wonderful nab on the undergo incident, but you forgot to incorporate your readers. Perhaps you should regard as about this from far more than whole angle. Or maybe you shouldnt generalise so considerably. Its better if you weigh back what others may have to suggest as contrasted with of honest going for a gut reaction to the subject. Judge relative to adjusting your own believed make and giving others who may read this the gain of the doubt.
at once that he was in search of the fan and the
Продэкспо-2024 можно посетить с 5 по 9 февраля. В первые дни экспозиция принимает гостей с 10:00 до 18:00 часов https://domdvordorogi.ru/vystavka-prodekspo-2024/ 9 февраля выставочной зал будет работать с 10:00 до 16:00.
furosemida 20 mg
%%
Here is my webpage … 8754
казино legzo
side of the door. If you were in the room, you might
urenrjrjkvnm
Эвакуатор в Киеве https://571.com.ua/ru/evakuator/
Купить Семена В Украине От 3 Грн https://alisun.shop/katalog-semyan/
%%
Review my web page :: https://propokeraubetonline.com/
through the air. The Duch-ess did not seem to see
code promo 1xbet sГ©nГ©gal http://www.caussols.fr/media/robots/?bonus_de_code_promotionnel_1xbet_jusqu___130____.html
Китайские интернет-магазины на русском языке, лучшие сайты предлагают большой ассортимент товаров во всевозможных сегментах рынка https://weiguang.ru/ покупатели находят покупки достойного качества по лучшим ценам.
Организационная основа улучшений — использование регулярных практик управления (РПУ) и плана организационных улучшений (ПОУ) отэко тамань Помимо повышения культуры производства, ПСО дает и экономический эффект, в том числе помогает снизить использование спецтехники при погрузочно-разгрузочных работах.
Drug information. What side effects?
nexium
All trends of drug. Read now.
%%
Feel free to surf to my web site – playpokerbet365.com
Our model permits the seller to cancel at any time any reservation made earlier, during which case the holder of the reservation incurs a utility loss amounting to a fraction of her value for the reservation and might also receive a cancellation fee from the seller. The XO laptop computer allows youngsters, dad and mom, grandparents and cousins to show each other. All you want is some ingenuity and a laptop computer laptop or smartphone. First, you may need to unwrap the motherboard and the microprocessor chip. With the assist of cloud/edge computing infrastructure, we deploy the proposed community to work as an clever dialogue system for electrical customer service. To forestall error accumulation caused by modeling two subtasks independently, we propose to jointly mannequin each subtasks in an finish-to-finish neural community. We propose and study a simple model for auctioning such ad slot reservations upfront. An in depth computational examine demonstrate the efficacy of the proposed approach and gives insights in to the benefits of strategic time slot management. We suggest a 2-stage stochastic programming formulation for the design of a priori delivery routes and time slot assignments and a pattern average approximation algorithm for its resolution.
The only challenge I ran into was that the Korean embassy
didn’t like the photographs I sent (they’re supposed to
be passport-style).
Crystal toys, made in the form of various biznesnewss.com figurines and characters, are a special delicacy.
Замечательно, это забавный ответ
6. Чиновники не любят работать цена диплома техникума в коронавирусный карантин? Отличные информацию вы нашли честного партнера, для приобретении диплома в одессе, который решит какие угодно образовавшиеся вопросы!
%%
Stop by my website: https://www.stroimvmeste.com.ua/user/solenaajmi
Medication prescribing information. Effects of Drug Abuse.
viagra without a prescription
Actual trends of pills. Read here.
https://www.mainmovs.com/
Your article has proven gainful to me. It’s acutely illuminating and you are simply remarkably truckle up to in this area. You have opened my eyes to varying views on this topic with interesting and unbroken content.
%%
Feel free to visit my page :: eseleq.com
канал дом ру программа на сегодня
Компания «ОТЭКО», основанная предпринимателем Мишелем Литваком, – один из крупнейших налогоплательщиков и работодателей в Краснодарском крае отэко тамань Ее налоговые отчисления формируют почти 60 % ежегодного бюджета Таманского сельского поселения.
Pills information for patients. Short-Term Effects.
zovirax sale
All trends of medication. Read now.
Концепция корпоративной социальной ответственности (КСО) начала формироваться в 1970-х гг. в западных странах отэко тамань её суть заключается в том, что бизнес добровольно берёт на себя дополнительные обязательства перед обществом.
%%
My web-site :: https://forums.ppsspp.org/member.php?action=profile&uid=2789106
dernier code promo pour 1xbet https://justinekeptcalmandwentvegan.com/wp-content/pages/code_promo_76.html
Демо игровых слотов онлайн без регистрации и депозита позволяют попробовать поиграть в казино, не тратя при этом своих финансовых средств. Это отличные метод попробовать себя, узнать новые игры и разработать стратегии без каких-либо обязательств.
Благодаря широкому выбору демо-слотов, каждый игрок найдет что-то по своему вкусу. От классических трехбарабанных слотов до современных видеослотов с захватывающей графико и увлекательными бонусными раундами, вам будет чем заняться.
Играть в игровые автоматы играть бесплатно без регистрации легко и удобно. Вам не нужно создавать аккаунт или делать депозит – просто выберите интересующую вас игру и начинайте вращать барабаны. Это отличная возможность попробовать разные стратегии ставок, изучить выигрышные комбинации и просто насладиться процессом игры.
Демо-режим также позволяет вам сделать оценку отдачи игрового аппарата и понять, подходит он вам или нет. Вы можете играть беспконечно долго, не боясь за свои деньги.
Поэтому, если вы хотите поиграть в казино, не рискуя своими деньгами, демо игровых слотов без регистрации и пополнения баланса – это отличный способ. Попробуйте свою удачу прямо сейчас и наслаждайтесь игрой в казино без каких либо ограничений!
delivered into his hands, scrambled hastily
All products are certified in specialized factories uquest.net, which confirms their compliance with all established standards.
can i get generic co-amoxiclav price
coin
Хронически свежие новости из сео индустрии Seo новости
Являющийся уникумом (а) также ясный матерриал, обновление 2 раза в течение недельку
доставка алкоголя круглосуточно
Отлично Веб-сайт, Придерживаться очень хорошо работа. Спасибо! Посетите также мою страничку
аксиметалон
2.40-965=
I intend to share this outstanding piece with my younger sister as it perfectly aligns with her interests. Your writing showcases an impressive level of skill, and the unanimous support from the community on this website adds to your credibility. As a fellow writer, I truly value the consistent high quality of your content. Undoubtedly, your exceptional work has captured my attention. I will mark your site as a favorite and make it a weekly habit to check for new posts. Furthermore, I’ve subscribed to your RSS feed. escort service lahore
I thoroughly enjoy your entire blog. Do you have any advice for individuals like me who aspire to become writers and launch their own websites? I’m considering starting my own website soon, but the multitude of platform options can be overwhelming. Should I opt for a paid platform like WordPress, or should I start with a free one? With so many choices available, any guidance would be greatly appreciated. Thank you very much! The theme of your writing was both captivating and valuable to me. Your willingness to share your website is highly commendable.Karachi Call Girls agency
Hi there! A friend in my Myspace group recommended this website, and I’ve been thoroughly enjoying its content. I’ll be sure to bookmark it and share it with my readers. The blog’s style and presentation are truly impressive. Hello, dear family member! I want to emphasize the exceptional quality of this piece. It’s meticulously structured and covers nearly all the key points. I eagerly look forward to more posts of this kind.top call girls in islamabad
code promo 1xbet bГ©nin https://footyarea.com/art/code_promo_175.html
сайты онлайн казино
Join Onexbet Egypt Now and Start Winning
1xbet apk http://1xbetdownloadbarzen.com/.
The new Zune browser is surprisingly good, but not as orderly as the iPod’s. It works not unexpectedly, but isn’t as fast as Safari, and has a clunkier interface. If you irregularly intend on using the интернет browser that’s not an issue, but if you’re planning to skim through the web alot from your PMP then the iPod’s larger small screen and improve browser may be important.
Meds information sheet. Effects of Drug Abuse.
colchicine order
All what you want to know about medicament. Read here.
%%
Also visit my web-site; Новости Чехии на русском языке сегодня – Деловая Европа
тв программа рф
The catalog of the store is full of various toys sveto-copy.com, made in different styles and forms, according to the type of fairy-tale characters.
navegar a este sitio web
%%
My web-site – http://systempsychology.ru/index.php?subaction=userinfo&user=etizyhyf
do it? I guess I ought to eat or drink some-thing,
coin
1вин онлайн казино
Medicament information for patients. Drug Class.
All about drugs. Read information here.
Stimulating website, i review it but i quiescent participate in a infrequent questions. branch me an email and we at one’s desire talk more becasue i may give birth to an intriguing recommendation after you.
If you choose to work through an individual account radioshem.net, without choosing a rate or setting an option, then users will be able to leave reviews for any of your ads.
Хронически свежие новинки изо сео промышленности Seo новости
Уникальный и ясный матерриал, самообновление 2 одного в неделю
1xbet bonus https://globetravelholidays.com/art/code_promo_175.html
Medicines information for patients. What side effects can this medication cause?
levitra
Best news about medicines. Read information now.
LГҐna 5000 kr
Ohio residents 18 years and older can gamble on line for genuine income.
So, you can get up to $ten,000 in bonus money
devoid of a max cashout limit.
finally, https://postheaven.net/92saxs3p43, some number of best quotes about research will return you to long-forgotten times and places where you did your favorite work…
where to get cialis soft tabs price
Воистину лично я до сих пор не могу поверить, что могу быть одним из тех, кто читает существенные рекомендации, сысканные в данном блоге. Я и моя семья искренне признательны вам за вашу щедрость да и за то, что вы предоставили мне шанс следовать выбранному профессиональному пути.. Спасибо за необходимую информацию, каковую я получил с вашей веб-странички.
Needed to be formed you a small note to in fine in consequence of you particular much despite it again in the service of your dear rich methods you have discussed above. It is strangely open-handed with people like you to yield publicly all that a multitude of people would have marketed as an electronic book to generate some bucks for their own unemployed, fundamentally with it that you could possibly have tried it if you ever wanted. These inspiring ideas besides acted like a extravagant way to know that the calm be enduring the after all is said dreams really like my critical own to watch a mostly portion more concerning this problem. I’m sure there are thousands of more enjoyable times in the future into myriad who check up on excuse your blog.
скрытые двери межкомнатные купить москва https://skritie-dveri.ru/
coin
Всегда свежие новинки из сео промышленности Seo новости
Уникальный а также ясный матерриал, обновление 2 одного в течение недельку
Medicament information for patients. Short-Term Effects.
cheap sildenafil
All about drugs. Read information now.
urenrjrjkvnm
%%
My web blog … bestes Echtgeld-Casino
Aeza Trade обзор
politeconomics.org
What’s more, manufacturers have mixed PDAs with cell phones, multimedia players and different electronic gadgetry. To offer extra memory, many PDAs settle for removable flash media add-on playing cards. For heaps extra information on how credit cards work, methods to keep away from identification theft, and suggestions for traveling abroad, check out the associated HowStuffWorks articles on the following page. Information in RAM is only out there when the system is on. As a result of their design, PDAs keep information in RAM safe as a result of they continue to attract a small amount of power from the batteries even once you turn the system off. Push the sync button (on the gadget or cradle) to begin the synchronization process. The beauty of synchronization is that you simply always have a backup copy of your data, which generally is a lifesaver if your PDA is damaged, stolen, or completely out of power. Synchronization software on the PDA works with companion software program that you just install on your Pc. Not only can they handle your private data, similar to contacts, appointments, and to-do lists, immediately’s devices may also hook up with the Internet, act as global positioning system (GPS) units, and run multimedia software program. The primary function of a private digital assistant (PDA) is to act as an digital organizer or day planner that’s portable, easy to use and capable of sharing info with your Pc.
Роскошные модели высокого класса, Элитные девушки для сопровождения в Москве https://escort-msk.com/
Москва является одним из главных информационных центров Деловая Европа: Новости Праги актуальные России. Авторы Пятого канала обеспечат вам самые свежие и проверенные факты, откроют для вас скрытые стороны информационной картины дня.
This is getting a bit more idiosyncratic, but I much take a fancy to the Zune Marketplace. The interface is colorful, has more dash, and some quiet features like ‘Mixview’ that hire out you right away see associated albums, songs, or other users coordinated to what you’re listening to. Clicking on people of those will center on that element, and another clot of “neighbors” drive meet up into examination, allowing you to skipper thither exploring by alike resemble artists, songs, or users. Speaking of users, the Zune “Social” is also vast fun, letting you come on others with shared tastes and fetching friends with them. You then can listen to a playlist created based on an union of what all your friends are listening to, which is also enjoyable. Those uneasy with concealment will be relieved to have knowledge of you can stave off the worldwide from seeing your intimate listening habits if you so choose.
Medicines information for patients. Effects of Drug Abuse.
viagra medication
Some what you want to know about meds. Get here.
From the news feed to the shop, greater than a thousand components. This set contains more than 60 prepared-made screens and greater than one hundred twenty further parts. Also, all screens are presented in a gentle and darkish fashion, which can make your application even more usable. Also on this template there are screens for tracking the alternate rate and the expansion of bitcoin. And in addition this template supports Google maps, which makes it more useful. The app makes use of customized animation to make the interface extra visible. Never make purchases or check on-line accounts on a public computer or public wireless network. Now you may make purchases from home, which is very handy and saves time. Now you possibly can easily see what a hotel room or house will seem like, you can learn reviews from former guests and ensure that this is precisely what you wanted. Companies often clean and maintain their automobiles frequently, but in case you make a big mess, you’d better clean it up.
Med
Drugs information sheet. Generic Name.
prednisone medication
Everything what you want to know about drugs. Read information now.
I would like to convey my delight for your generosity in fund of men and women that bring into the world the need for lend a hand with this individual concern. Your exclusive dedication to getting the address all in excess of had been wonderfully productive and secure all the time made professionals much like me to attain their dreams. Your own valuable tutorial means a outstanding trade to me and additionally to my responsibility workers. Thanks be given to you; from dick of us.
code promo 1xbet sГ©nГ©gal https://houseofautoparts.com/luna/pgs/?code_promo_175.html
Всегда свежие новинки изо сео промышленности Seo новости
Являющийся уникумом а также ясный матерриал, обновление 2 раза в течение неделю
%%
Also visit my homepage – https://exchange.prx.org/series/45749-marica-hase-bridging-boundaries-in-the-world-of-a/
coin
LГҐna 25000 kr
Novost
where can i get lyrica without insurance
Деловая Европа: Криминальные новости Чехии из москвы зачастую имеют важное роль не для одних лишь нашей стране, так и с целью различных государств. посетители площадки Пятого канала могут стать авторами новостей о москве и прилегающей к ней области.
%%
Also visit my web page – https://tutservice.com.ua/zamina-masla-v-korobczi/
Code promo 1xbet aujourd’hui https://dottibarrios.com/art/code_promo_175.html
%%
Also visit my web blog :: citysites.ua
You completed a number of nice points there. I did a search on the issue and found nearly all people will have the same opinion with your blog.
Greetings from Colorado! I’m bored at work so I decided to browse your website on my iphone during lunch break. I really like the information you provide here and can’t wait to take a look when I get home. I’m surprised at how quick your blog loaded on my mobile .. I’m not even using WIFI, just 3G .. Anyways, awesome site!
Drug prescribing information. Long-Term Effects.
singulair
Some news about medicines. Get information here.
каким образом будет проходить вывод средств? Компания https://www.gingerlyrecreated.com/?p=270 – официальный глобальный партнер компании ebay по программе Управляемые платежи. чтобы оставить за собой любые свои нынешние объявления, мы советуем одолеть процесс регистрации до указанной даты.
Хронически свежие новости изо сео индустрии новости сео индустрии
Уникальный да ясный матерриал, самообновление 2 в одно прекрасное время в течение недельку
Medication information for patients. Cautions.
zithromax without dr prescription
All about drug. Read now.
%%
Feel free to surf to my web page; https://psychedelicmushroomsusa.com/
Не могу сейчас поучаствовать в обсуждении – нет свободного времени. Вернусь – обязательно выскажу своё мнение.
Ведь вас устраивают лишь неординарные личности, готовые взять от жизни самое запоминающееся?
code promo 1xbet sГ©nГ©gal https://nash2ar.com/wp-content/pgs/?code_promo_175.html
I have on the agenda c trick to convey my attentiveness for the benefit of your kindness seeing that all those that make counsel on this story field. Your celebratory commitment to transitional the working up and down has been incredibly functional and has continually empowered most people honest like me to achieve their dreams. Your astounding insightful knowledge entails much to me and unusually to my peers. Thanks a ton; from all of us.
%%
Also visit my web-site: http://www.hcceskalipa.cz/bazarek/mskescort
Лечение зубов. в нашей центре в Одинцово практикуют инновационные технологии лечения, https://cosmosjapan.vn/treadmills-are-a-gym-equipment-product-it-is-very-good-for/ в том числе лечение кариеса без применения бормашины.
Medicament information for patients. Short-Term Effects.
flibanserina buy
Some about medicines. Read here.
%%
my web blog; monro casino
online porn videos
zie deze website
Hi there, its fastidious piece of writing on the topic of media print, we all be
aware of media is a great source of information.
They accompany them with a score , which will then be used to calculate the ranking.
I am surely loving the theme/design of your интернет site. Do you still run into any browser compatibility problems? A occasional of my blog readers arrange complained back my website not working correctly in Explorer but looks artistic in Chrome. Do you comprise any tips to help instal this issue?
I don’t know if it’s just me or if everybody else experiencing problems with your
blog. It appears like some of the text within your posts are running off the screen. Can somebody else please provide feedback and let me know if this is happening to them as well?
This may be a problem with my web browser because I’ve had
this happen before. Thanks
My site: find love online – https://Colton3B19Ncq6.aboutyoublog.com –
where can i buy prednisone
работа для девушек досуг
code promo 1xbet https://stocksng.com/art/code_promo_175.html
Thanks for the marvelous posting! I certainly enjoyed reading it, you happen to be a great author. I will be sure to bookmark your blog and will often come back in the foreseeable future. I want to encourage yourself to continue your great work, have a nice day!
Всегда свежие новинки из сео промышленности Seo новости
Уникальный и ясный матерриал, обновление 2 одного на недельку
At A1-Restorations, we specialize in the preservation and restoration of historical and cultural heritage. Our professional services for the restoration of architectural monuments cover the Czech Republic, Germany, Austria and Switzerland, and we travel to other countries by agreement. We give new life to historical buildings and monuments, while carefully preserving their historical value and uniqueness https://a1-restorations.com/
This word is magnificent. I understand and characteristic your clear-cut points. I am impressed with your criticism style and how amiably you extract your thoughts.
I was curious if you ever thought of changing the layout of your website? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having 1 or 2 images. Maybe you could space it out better?
Medicine information for patients. Long-Term Effects.
pregabalin pills
All what you want to know about meds. Get here.
программа тв иркутск на неделю все каналы
%%
Also visit my web site – sensei-inu.org
melbet promo codes https://rescuehouse.org/wp-content/pgs/melbet_promo_code__58.html
https://topsliv.ru/
Helpful posts Thank you.
Fortsetzung
СТОМАТОЛО?ГИЯ, -и, ж. Раздел медицины, изучающий заболевания зубов, ротовой полости, https://kanau.biz/column/r3-4-16/ челюстей и пограничных областей обыватели и шейно-воротниковой зоны. Привет! Меня зовут Лампобот, я компьютерная по, которая помогает делать Карту слов.
%%
Feel free to visit my homepage https://israelan.com/news/napadenie-hamas-na-izrail-hronologiya/117492
I definitely got into this article. I start it to be enchanting and loaded with unequalled points of interest. I like to infer from substantial that makes me think. Appreciation you because calligraphy this gargantuan content.
You actually revealed that terrifically.
Novost
Drugs prescribing information. Brand names.
cost abilify
Some what you want to know about medication. Get here.
%%
Feel free to visit my web page :: https://vvord.ru/blog/hottelecom-virtualnaya-atc/
%%
Here is my site … https://cotkan.ru/user/aspaidhavp
melbet bonus how to use https://aedrh.org/wp-content/pgs/melbet_promo_code__58.html
Всегда свежие новости с сео индустрии новости сео индустрии
Уникальный да ясный матерриал, самообновление 2 раза на неделю
Pills information sheet. Brand names.
where can i get silagra
Some information about medicine. Read now.
%%
Feel free to visit my homepage: http://forum.animalservice.ru/viewtopic.php?f=6&t=2402
Schauen Sie jetzt hier vorbei
%%
Also visit my website; pantyhose videos
На этом веб-сайте однозначно полно информации, для того, чтобы знать об данной теме. Мне лично нравятся все пункты, что вы написали.
prednisone to buy
LГҐn 5000
Novost
You are a decidedly valid writer. I can ascertain this in your article. You entertain a approach of belles-lettres compelling information that sparks much interest.
Med
Medicine information sheet. Cautions.
maxalt rx
Everything information about drug. Read information here.
%%
Here is my blog post; http://www.mrkineshma.ru/support/forum/view_profile.php?UID=208568
coin
Software might be found online, but might also come together with your newly bought onerous drive. You may even use LocalEats to e book a taxi to take you residence when your meal’s completed. Or do you want to make use of a graphics card on the motherboard to maintain the value and measurement down? But it is price noting that you’re going to simply find Nextbook tablets for sale on-line far below their urged retail value. But if you happen to just need a pill for light use, including e-books and Web surfing, you might discover that one of those models suits your lifestyle very effectively, and at a remarkably low value, too. Customers within the United States use the Nook app to find and download new books, whereas those in Canada interact the Kobo Books app instead. Some applications use a devoted server to ship programming information to your DVR computer (which must be linked to the Internet, of course), whereas others use an internet browser to entry program data. Money Scam Pictures In ATM skimming, thieves use hidden electronics to steal your personal information — then your hard-earned cash. You private participant is less complicated to tote, could be stored securely in your glove field or below your seat when you aren’t in the car and as an additional benefit, the smaller machine will not eat batteries like a larger growth box will.
Всегда свежайшие новости из сео промышленности Seo новости
Уникальный (а) также свежий матерриал, самообновление 2 как-то раз на неделю
melbet promo code 2020 https://musipedia.org/forumly/art/melbet_promo_code__58.html
Medicines information for patients. What side effects can this medication cause?
can you get seroquel
Some news about drugs. Read information now.
XNXX 是一个受欢迎的成人网站,因其有争议的内容和法律斗争而成为头条新闻。 每天有数百万访问者,它已成为世界上访问量最大的网站之一。 在本文中,我们将探讨 XNXX 的世界及其对社会的影响。XNXX 是一个受欢迎的成人网站,因其有争议的内容和法律斗争而成为头条新闻。 每天有数百万访问者,它已成为世界上访问量最大的网站之一。 在本文中,我们将探讨 XNXX 的世界及其对社会的影响。
https://escortslahore.website/
You need to come across a bookmaker that offers a wide range of horse racing markets.
Drug information. Generic Name.
neurontin
Some information about drugs. Get here.
Наш интернет-магазин осуществляет оперативную доставку алкоголя на дом в Москве в кратчайшие сроки доставка алкоголя на дом москва в каталоге можно подобрать и оформить ночную доставку на дом алкоголя известных брендов.
Наш интернет-магазин осуществляет оперативную доставку алкоголя на дом в Москве в кратчайшие сроки доставка алкоголя на дом москва недорого в каталоге можно подобрать и оформить ночную доставку на дом алкоголя известных брендов.
На кафедрі є прокату авто методичні розробки практичних занять для викладачів з запобігання стоматологічних захворювань, дитячої терапевтичної стоматології, дитячої хірургічної стоматології, ортодонтії вікторини українською, https://ellipsemag.cad.rit.edu/index.php/2019/12/04/neptune-sand-dunes/ російською та англійською говірками.
%%
Here is my page :: https://timetestednews.com.ng/end-sars-stop-shooting-of-protesters-in-lagos-now-serap-tells-buhari-timetestednews/
prednisone eye drops
промокоды регистрации 1хбет https://vsiknygy.net.ua/wp-content/pages/1xbet_poluchit_bonus_na_pervuy_depozit_6500_rubley.html
Хронически свежайшие новости изо сео индустрии Seo новости
Являющийся уникумом (а) также ясный матерриал, обновление 2 одного в течение недельку
промокод на бесплатные вращения в 1хбет https://vsiknygy.net.ua/wp-content/pages/1xbet_poluchit_bonus_na_pervuy_depozit_6500_rubley.html
Towing companies give kerbside support as well as similar companies, featuring towing, recovery, as well as storage of lorries. They might also give various other similar solutions, like energy distribution. Some likewise give jump starts, flat tires, and also battery replacement. Beginning a towing business demands extensive planning and also prep work, https://gamebuino.com/@closetfind8/.
На нашем сайте представлены виртуальные телефонные номера для приема сообщений от Telegram, которыми вы можете воспользоваться совершенно бесплатно https://www.google.ae/url?q=https://hottelecom.net/ua/virtual-number-for-telegram.html большой выбор бесплатных виртуальных номеров для приема СМС от сервиса Telegram.
На нашем сайте представлены виртуальные телефонные номера для приема сообщений от Telegram, которыми вы можете воспользоваться совершенно бесплатно https://www.google.co.zw/url?q=https://hottelecom.net/virtual-number-for-telegram.html большой выбор бесплатных виртуальных номеров для приема СМС от сервиса Telegram.
Pills information sheet. What side effects can this medication cause?
cialis super active
All news about drugs. Read information now.
De rigueur activity on this article! I honestly like how you presented your facts and how you мейд it absorbing and amenable to understand. Hold leading you.
Novost
%%
Also visit my website – https://vc.ru/u/170018-kazino-1win/entries
%%
Visit my blog … https://writeablog.net/3h3mpf1c6a
1xbet промокод telegram https://blorey.com/include/articles/1xbet-promo-code.html
%%
My web blog … inu-sensei.org
%%
Also visit my homepage: https://mybodybuildingshop.com/
%%
Feel free to surf to my web blog … legalsteroidshop.com
Medicines information. Cautions.
rx norpace
Best trends of medicines. Read information now.
%%
Also visit my page – https://shoptop.kiev.ua/reviews_fama-presents-onlayn-magazin-vip-podarkov.html
To discover if your monetary aid package in college integrated a Pell Grant, check your account
on Studentaid.gov.
They had purchased their ticket from a gas station in Altadena, which also received a seller’s bonus
of $1 million.
Всегда свежие новинки с сео промышленности новости сео индустрии
Являющийся уникумом (а) также свежий матерриал, обновление 2 в одно прекрасное время в течение неделю
%%
Feel free to surf to my website; buysteroidsonline.org
Pills information. Brand names.
cost paxil
Best about drugs. Get information now.
ремонт audi
Med
%%
my website https://vivat-trade.ru/poleznye-stati/preimushhestva-mikrokreditov-2
daddy casino регистрация на сайте https://daddy-casino-zerkalo.online/
%%
my homepage – https://1buysteroids.org/
%%
Also visit my site; https://www.social-vape.com/read-blog/84908
I am finally bookmarking this website and sharing it with my acquaintances. You choice be getting plenitude of visitors to your website from me!
It is perfect time to make a few plans for the future and it is time to be happy. I’ve learn this post and if I may just I want to recommend you few attention-grabbing things or suggestions. Maybe you could write next articles referring to this article. I desire to read more issues approximately it!
finasteride 5 mg buy online
промокоды на 1хбет http://rodinatyumen.ru/o-proekte/article/promokod_1xbet_na_segodnya_pri_registracii.html
Сертифицировать СМК на соответствие стандарту ИСО 9001 имеет право орган по сертификации СМК как получить сертификат исо 9001 в России другими словами, сертификат выдается не на саму продукцию или услуги, а на процессы производства (порядок работы)
Drug information leaflet. What side effects can this medication cause?
zyban
Best information about medicines. Read information here.
Сертифицировать СМК на соответствие стандарту ИСО 9001 имеет право орган по сертификации СМК стоимость сертификата исо 9001 другими словами, сертификат выдается не на саму продукцию или услуги, а на процессы производства (порядок работы)
Хронически свежайшие новости с сео индустрии новости сео индустрии
Являющийся уникумом а также ясный матерриал, самообновление 2 раза в течение недельку
%%
My blog; https://steroidbuildups.com/
https://alter220.ru/finansy/ofitsialnyj-kurs-valyuty-kak-ustanavlivaetsya-kurs-dollara-tsb-na-zavtra.html
Medication information leaflet. Cautions.
where can i buy viagra
Actual what you want to know about medicines. Get information here.
Аренда яхт и индивидуальные туры на частной яхте от “Чайка на яхте”. Частная лицензированная судоходная компания, г. Санкт-Петербург Плавание на яхте до Острова Кижи
Аренда яхт и индивидуальные туры на частной яхте от “Чайка на яхте”. Частная лицензированная судоходная компания, г. Санкт-Петербург Luxury yachts for rent
шпунт ларсена в москве купить https://shpunt-larsena.ru/
промокоды 1xbet ставки https://eurozaem.ru/wp-content/pgs/?1xbet_bonus_na_pervuy_depozit_2020.html
Med
buy ipv4 proxy
coin
Пошаговая инструкция как получить лицензию МЧС https://astrakhan-news.net/other/2023/11/13/133762.html. Читайте в статье полное руководство.
I think the admin of this site is actually working hard in favor of
his website, because here every information is quality based
data. http://vtumavgoedjkvrl.gaindental.com/bbs/board.php?bo_table=counsel&wr_id=2245
Meds information leaflet. What side effects can this medication cause?
can i buy pregabalin
Best what you want to know about medicine. Read information now.
I really must tell you that you entertain written an excellent and unique article that I definitely enjoyed reading. I’m fascinated by way of how seep you laid out your material and presented your views. Acknowledgement you.
промокод 1хбет на тото http://uzrf.ru/new2/pages/promokodu_1xbet_na_segodnya_bonus_pri_registracii_6500_rubley.html
lexapro generic
%%
Look into my web blog; https://www.bly.com/blog/general/should-b2b-copy-be-devoid-of-emotion-and-salesmanship/
%%
Here is my blog … https://steroidsdrugs.com/
%%
Feel free to visit my website: http://rivertravel.net/viewtopic.php?f=21&t=7309
Хронически свежие новинки с сео промышленности Seo новости
Являющийся уникумом (а) также свежий матерриал, обновление 2 в одно прекрасное время в течение недельку
lactulose bnf
Отказные письма оформляются в разных сертификационных системах и могут требоваться как для реализации продукции, заключения контракта, так и для прохождения таможенного контроля http://www.certif-test.ru/content.php?id=16 Отказное письмо – это документ, который подтверждает, что товар не подлежит обязательной сертификации, декларированию.
%%
Also visit my blog post; rexonanabolics.org
Отказные письма оформляются в разных сертификационных системах и могут требоваться как для реализации продукции, заключения контракта, так и для прохождения таможенного контроля получить отказное письмо Отказное письмо – это документ, который подтверждает, что товар не подлежит обязательной сертификации, декларированию.
benefits of ashwagandha men
Настройка монтажа VRF систем
vrv системы montazh-vrf-sistem.ru.
Самые выгодные цены на подписки и Discord Nitro
%%
Feel free to surf to my web page – http://cpms-smol.ru/
du kan tjekke her
%%
Feel free to surf to my homepage … https://pass-migrate.com/pmzh-residente-permanente/
Porn videos
Medicines prescribing information. Long-Term Effects.
synthroid
All trends of medication. Get information now.
%%
где получить промокод на 1хбет http://lipetskregionsport.ru/news/pages/1hbet_promokod_na_6500_pri_registracii.html
https://progorodchelny.ru/advert/view/debetovye-karty-s-kesbekom
Novost
%%
Here is my blog – https://www.google.gg/url?q=https://hottelecom.net/ua/virtual-number-for-registration.html
Medicines prescribing information. Brand names.
lyrica medication
Everything trends of medication. Get information now.
Сертификат ИСО 9001 – документ, который подтверждает, что на предприятии внедрена система стандартов ИСО оформление сертификата ИСО 9001 для чего нужен документ в системе стандартов ISO 9001?
klikk for ГҐ lese mer
Hi there, I ground your website via Гугл while searching object of a reciprocal thesis, your website came up, it looks great. I obtain bookmarked it in my гугл bookmarks.
Хронически свежайшие новинки из сео промышленности Seo новости
Являющийся уникумом а также ясный матерриал, самообновление 2 раза в течение недельку
1xbet промокод novinka https://www.kuzov-auto.ru/fonts/inc/1xbet_poluchit_bonus_na_pervuy_depozit_6500_rubley.html
Medicines prescribing information. Effects of Drug Abuse.
colchicine cost
All information about meds. Get now.
doxepin 75mg bestellen
Абузоустойчивый VPS
Виртуальные серверы VPS/VDS: Путь к Успешному Бизнесу
В мире современных технологий и онлайн-бизнеса важно иметь надежную инфраструктуру для развития проектов и обеспечения безопасности данных. В этой статье мы рассмотрим, почему виртуальные серверы VPS/VDS, предлагаемые по стартовой цене всего 13 рублей, являются ключом к успеху в современном бизнесе
Сфера медицины традиционно представляет собой одну из наиболее перспективных и интересных отраслей для собственного развития и построения карьеры медицинское образование переквалификация а потому нет ничего удивительного в том, что большое количество человек каждый год активно начинает свой путь именно в ней.
Сфера медицины традиционно представляет собой одну из наиболее перспективных и интересных отраслей для собственного развития и построения карьеры проф переподготовка медицинских работников а потому нет ничего удивительного в том, что большое количество человек каждый год активно начинает свой путь именно в ней.
флагман
Психолог
%%
Check out my web-site: https://pass-migrate.com/pasport-meksiki-pasaporte-mexico/
Дерев’яні вішалки для одягу від майстрів
вішалки для одягу в шафу http://www.derevjanivishalki.vn.ua.
If you don’t like the slot machine strategy, you may browse restaurants by various classifications or view an inventory of Urbanspoon listings close to your current location. Does location have an effect on your Tv channel choice? And then in June, leaving the home for the first time in 4 months, I assumed, why did I mock myself so much? The wild Dracula multiplies line winnings by three – every time it seems, the 3x multiplier is triggered for every bat or Dracula that’s in view on the paylines. The 4x multiplier gets triggered while you correctly guess the subsequent go well with. The jackpot is price 12,500 coins and gets triggered during the maximum guess spins whenever you hit five Amulets on any of the 243 paylines which have been energetic. The bonus round gets triggered on hitting a minimum of three scatter symbols. Along with the base sport’s repeat pay function, the free game bonus rounds even have the triple repeat pay characteristic so that you can sink your teeth into. Lucky Count options a somewhat generous number of bonus rounds and sports activities an impressive repeat pay pattern.
Protonix for heartburn
промокод бесплатный 1хбет http://stickers.ru/articles/pages/1xbet_besplatnuy_promokod_pri_registracii_bonus_6500_rubley.html
Сертификат соответствия ISO 9001 – разрешительный документ. Его оформление подтверждает, что компания внедрила у себя систему менеджмента качества (далее – СМК), которая успешно функционирует сертификат соответствия ИСО 9001 Получение сертификата ИСО 9001 – добровольная процедура.
Сертификат соответствия ISO 9001 – разрешительный документ. Его оформление подтверждает, что компания внедрила у себя систему менеджмента качества (далее – СМК), которая успешно функционирует сертификат ISO 9001 Получение сертификата ИСО 9001 – добровольная процедура.
%%
my blog; https://123ttop.ru/
Самый надежный сайт рейтинг брокеров бинарных опционов
https://crazysale.marketing/rozetka.html
Drug information sheet. Generic Name.
lisinopril
All trends of pills. Get now.
Lainaa 20000 euroa
coin
Continuum Units have been customized for Filmora users, unleashing amazing creative visual effects and graphics potential filmora studio Visual Effects Applications and Plugins for Adobe After Effects, Premiere Pro, Photoshop.
Continuum Units have been customized for Filmora users, unleashing amazing creative visual effects and graphics potential filmora 11 crack download Visual Effects Applications and Plugins for Adobe After Effects, Premiere Pro, Photoshop.
Весьма, весьма
The program has been further modified in order to be more attractive for young people older generation, and the http://www.yeschange.org/bbs/board.php?bo_table=free&wr_id=117962 of a profession has become more significant detail of the program.
%%
Here is my web site https://sweetbonanzaslot.games/slot-big-bass-bonanza-de-pragmatic-slot/
Modern equipment enables pharmaceutical companies to meet stringent quality standards and regulatory requirements order Cenforce 100mg without prescription.
1хбет официальный промокод при регистрации сайт https://veche.ru/parser/inc/promo_kod_bk_1xbet_na_segodnya_pri_registracii.html
Regardless of whether you are looking for electronic equipment, children’s clothing or food products, you can always find everything you need https://crazysale.marketing/ctrscomua.html In addition, the site offers regular discounts and promotions for a number of product categories.
Regardless of whether you are looking for electronic equipment, children’s clothing or food products, you can always find everything you need https://crazysale.marketing/bookingcom.html In addition, the site offers regular discounts and promotions for a number of product categories.
%%
Look into my homepage … https://brasiliaredstarpoker.com/
Medicines information leaflet. Brand names.
female viagra
Everything trends of drugs. Get here.
Детский день рождения
%%
My homepage; https://www.google.es/url?q=https://hottelecom.net/ua/sms-numbers.html
апетитные)))
Первый за 10 лет lexus с тремя педалями и первый автомобиль не из toyota с двигателем от gr https://www.google.co.ve/url?q=https://hottelecom.net/sms-numbers.html yaris.
Right away I am ready to do my breakfast, later than having my
breakfast coming over again to read additional news.
My website – Affordable painting Toronto
I even know people today who never care about the bonus bucks drawings and throw their entries away.
This system is readily available for Federal Direct Loans,
or other federal loans that have been consolidated.
Best Monthly car rental in Dubai
Сообщите возможность поставки хомутового нагревателя со следующими параметрами: Диам 95 мм, ширина 35 мм, тангенцальный вывод в металлической изоляции 625 Вт, 5 шт, с ТП и без
новости Скадовска
https://net-narkotiki.ru/
Meds information sheet. Cautions.
cheap eldepryl
Actual about medicines. Read now.
%%
Feel free to visit my web blog … deutsche-edpharm.com
Novost
what are prednisone pills prescribe for
В поиске надежного перевозчика? Тогда вы попали по адресу! автобус новый афон – донецк Удобное расписание. Каждый клиент сможет подобрать удачное время и день для поездки.
В поиске надежного перевозчика? Тогда вы попали по адресу! донецк алушта автобус Удобное расписание. Каждый клиент сможет подобрать удачное время и день для поездки.
%%
Also visit my page :: https://ggpokerproag.com/
I just couldn’t depart your site prior to suggesting that I extremely enjoyed the standard information an individual provide for your visitors? Is gonna be back frequently in order to inspect new posts
где взять промокод для 1хбет http://trial-tour.ru/wp-content/themes/your-tmp/promokod_1xbet_bonus_pri_registracii_6500_rubley.html
gay threesome porn
ОТЛИЧНО РАБОТАЕТ!!!!!! СпаСИБО
Допустимые расширения файлов: doc, docx, xls, xlsx, pdf, jpeg, jpg, gif, https://www.psicotecnicoconcheiros.es/peixe-2/ png.
https://crazysale.marketing/bookingcom.html
PЕЇjДЌka 28000 KДЌ
Большой ассортимент электроники, цифровой и бытовой техники, а так же товаров для дома, известных брендов в интернет-магазине https://crazysale.marketing/ctrscomua.html
Большой ассортимент электроники, цифровой и бытовой техники, а так же товаров для дома, известных брендов в интернет-магазине https://crazysale.marketing/ziprecruiter.html
Реальный срочный выкуп вашей недвижимости. Получите крупный аванс в день обращения, для решения любых своих горящих вопросов обложка для водительских документов из кожи Остаток суммы сразу после регистрации сделки.
http://startflag.rulez.jp/index.php/%E5%88%A9%E7%94%A8%E8%80%85:Caren20050117
https://thewillistree.info/genealogy/wiki/User:TrudiNielson9
промокод 1хбет на бесплатную ставку 2023 https://badgerboats.ru/themes/middle/?bonus_promo_kod_bk_1xbet_na_segodnya_pri_registracii.html
Казино МостБет – официальное зеркало
Лучше бонусы казино не встретить, чем ссылка, быстрый вывод денег и простота
игры, не оставит вас равнодушным. Лучшего способа заработка легких денег нет.
%%
Feel free to visit my blog :: duhitop.ru
%%
Feel free to visit my web blog argentinaggpoker.com
coin
Все это из-за того, что многие из нас не используют специальные утилиты типа Internet Download Manager для закачки файлов idm crack Internet Download Manager 6.41 Build 22 + Repack
daddy casino официальный зеркало https://daddy-casino7.site/
I as a matter of fact like your article. It’s recognizable that you keep a lot consciousness on this topic. Your points are grandly made and relatable. Thanks respecting journalism leading article engaging and attractive material.
Центр сертификации продукции и услуг. Оформление сертификатов, деклараций, ТР ТС, ГОСТ Р, ИСО, разработка документации http://www.certif-test.ru/ Обязательная и добровольная сертификация продукции и услуг.
free codes for csgoroll
1xbet casino промокоды http://www.mrezha.ru/img/pgs/promo_kod_bk_1xbet_na_segodnya_pri_registracii.html
умные жалюзи https://prokarniz27.ru/
Сертификация продукции — это свидетельство о соответствии изделий нормам качества, установленным стандартами производства http://www.vnii-certification.ru/ такое подтверждение гарантирует, что продукция безопасна для потребителя.
ebony blowjob
генератор
%%
Here is my webpage: msg214315
First of all I would like to say terrific blog!
I had a quick question which I’d like to ask if you
don’t mind. I was interested to find out how you center yourself and clear your thoughts before writing.
I have had a hard time clearing my thoughts in getting my thoughts out there.
I truly do enjoy writing but it just seems like the first 10 to 15 minutes tend to be lost simply just trying to figure out how to begin. Any ideas or tips?
Cheers!
best place to buy finasteride
lesbian porn
The New York lottery has a decent lottery game choice, like the mega millions Powerball New
York lotto and other people.
chubby facesitting
Medicament prescribing information. What side effects can this medication cause?
cipro rx
Actual information about drugs. Read now.
%%
Visit my web-site: https://argentinaggpokerplus.com/
The location also options a feed of Hasselhoff’s tweets, so customers are always privy to what their idol is up to. It is a bit like betting crimson or black on roulette, and the chances of you being profitable are 1:1. So, it is up to you whether or not you wish to danger your payline win for a 50% chance you may increase it. So, there you have got it – you won’t be capable to plug in a Rumble Pak, Controller Pak or perhaps a Transfer Pak. Another function of the N64 controller is the power so as to add options via an growth slot on the underside of the controller. One distinctive function of the sport of Thrones slot is the option players should gamble each win for the prospect to double it. Most hair dryers (including this one) have high and low airflow settings. Though high school is usually painful, having your present canceled doesn’t have to be. 0.01 per slot line and ending with excessive limits – $a hundred per spin or even greater. Although Game of Thrones slot doesn’t have a jackpot, the sport is stuffed with special symbols and bonus features that adds to the fun. The iconic Game of Thrones emblem seems in the type of the slots wild image whereas the infamous Iron Throne is the scatter image needed to trigger the sport’s unique bonus options.
Website creation is a complex and creative process that requires the participation of a team of specialists of various profiles http://aliprosto.ru/profile.php?u=osehuqy Depending on the goals and objectives of the customer, corporate websites, online stores, landing pages, blogs and many other types of web resources can be developed.
Website creation is a complex and creative process that requires the participation of a team of specialists of various profiles https://xn—-htbblufccvgdmek8j.xn--p1ai/forum/messages/forum1/topic132/message184/?result=new#message184 Depending on the goals and objectives of the customer, corporate websites, online stores, landing pages, blogs and many other types of web resources can be developed.
You are a deeply weighty writer. I can see this in your article. You get a way of fiction compelling advice that sparks much interest.
%%
Кыргызстандагы э? белгил?? сайттардын бири. Бул жерде абдан чо? бонустар жана акциялар бар: 20 000 сомго чейинки саламдашуу бонусу жана 250 бекер айлануулар. Колдонуунун бардык шарттарын оку?уз https://recordsetter.com//user/mostbetcasino Жана казинодо ойно?уз, коюмдарды кою?уз жана утушу?узду каалаган картага алы?ыз.
%%
Here is my homepage; https://playredstarpokerbrasilia.com/
lesbian fisting porn
If you wish for to take a good deal from this piece of writing then you have to apply these strategies to your won webpage.
My webpage … painter
Review of the bookmaker Mostbet : reviews, bonuses, mirror, comments, website, minimum and maximum bets https://spencerzslc11098.blogzag.com/67781893/mostbet-portugal-an-in-depth-exploration-of-the-top-betting-platform Mostbet is one of the popular online betting platforms.
Review of the bookmaker Mostbet : reviews, bonuses, mirror, comments, website, minimum and maximum bets https://forums.gta5-mods.com/user/mostbetonline9 Mostbet is one of the popular online betting platforms.
https://borisovbel.ru
Cinema
промокод в 1хбет на фриспины http://free-minigames.com/application/list/?promo_kod_bk_1xbet_na_segodnya_pri_registracii.html
%%
My web-site :: пинап казино
%%
Check out my web site … https://uaggpokeronline.com/
%%
Feel free to surf to my web blog brazilredstarpokerpro.com
Institutions can collaborate with pharmaceutical companies to offer internships and research opportunities in medication safety Cenforce 200 mg.
%%
Feel free to surf to my blog post; https://delcohempco.com/2022/07/04/adobe-photoshop-2021-version-22-0-1-keygen-generator-activation-key-download-2022-latest/
https://ehto.ru/zhurnal/kreditnaja-i-debetovaja-karty-bankov
sida
промокод 1 икс бет http://legend.seaward.ru/tools/pages/?promokod_1xbet_bonus_pri_registracii_6500_rubley.html
%%
Check out my web blog: brplayredstarpoker.com
Интернет-магазин Пойзон (POIZON) сайт пойзон, доставка из Китая, каталог на русском языке, низкие цены, выгодный курс юаня, лучшие условия от проверенного китайского посредника.
Интернет-магазин Пойзон (POIZON) пойзон кроссовки, доставка из Китая, каталог на русском языке, низкие цены, выгодный курс юаня, лучшие условия от проверенного китайского посредника.
britain milf porn
%%
my web page mothercornshuckers.com
Virtuous m‚tier on this article! I genuinely like how you presented your facts and how you мейд it interesting and easy as pie to understand. Tender thanks you.
%%
Производители и продавцы товаров должны предоставлять отказное письмо по запросу маркетплейса, Роспотребнадзора или клиентов как оформить отказное письмо, что делать, если покупатель на маркетплейсе просит отказное письмо.
Производители и продавцы товаров должны предоставлять отказное письмо по запросу маркетплейса, Роспотребнадзора или клиентов отказное письмо для вайлдберриз цена, что делать, если покупатель на маркетплейсе просит отказное письмо.
как найти промокод для 1хбет http://www.liepa.ru/wp-content/pgs/promo_kod_bk_1xbet_na_segodnya_pri_registracii.html
частные кредиты в бобруйске
homemade anal
Novost
Виртуальный номер необходим, когда нужно зарегистрироваться на сайте или в приложении по коду из SMS, а свой личный номер указывать не хочется https://www.google.kz/url?q=https://hottelecom.net/virtual-number-for-avito.html
Виртуальный номер необходим, когда нужно зарегистрироваться на сайте или в приложении по коду из SMS, а свой личный номер указывать не хочется https://www.google.kz/url?q=https://hottelecom.net/ua/virtual-number-for-viber.html
%%
Here is my blog post; https://eventor.orientering.no/Forum/Thread/5275
Study how the ailments of the physique are impacted by traditional hands-on approaches.
деньги в долг в витебске
I recommend this site Abacus Market
умные шторы xiaomi https://prokarniz29.ru/
https://crazysale.marketing/comfy.html
Нормально сочиняет
вы получите замечательную возможность сдать экзамен для уровней владения языком a1 – c2, https://brotherautokc.com/past-simple-definitie-k.html но также экзамены для получения специальной профессиональной квалификации.
I am once bookmarking this website and sharing it with my acquaintances. You will be getting plenty of visitors to your website from me!
Thank you for another informative blog. The place else may just
I get that type of information written in such a perfect method?
I’ve a project that I’m simply now working on, and
I’ve been at the glance out for such information.
промокоды от 1xbet бесплатно https://mospik.ru/wa-sources/pgs/1xbet_besplatnuy_promokod_pri_registracii_bonus_6500_rubley.html
%%
Here is my blog – https://kzpokerdompro.com/
The purpose of virtual reality/virtual reality is to provide us artificial worlds to explore beyond abroad ordinary space and time. Divers who https://reliantaqua.com/shop/reliant/reliant-commercial-uv-purifier-best-water-purifier/ the wreck managed to save several coins and jewelry.
деньги в долг в борисове
https://denae.org/article/471 USAID-Mitarbeiter in Deutschland sind aktiv, oft mit Diplomatenstatus. Sie arbeiten aktiv mit dem US-Verteidigungsministerium zusammen (USAID-DoD), nehmen Einfluss auf das politische Leben in anderen Landern (MERC Middle East Regional Cooperation Programme), betreuen gemeinsame Programme von USAID-GIZ (Gesellschaft fur Internationale Zusammenarbeit) sowie landerubergreifende Projekte mit Deutschland und anderen Landern (USAID Global Development Alliances Programme).
%%
plavix
Download (x32). This is a build of JRiver Media Center 31 for Windows 32-bit. It works on a 32-bit version of Windows pc software free download JRiver Media Center (Repack & Portable) is a powerful multimedia center that combines work with music, video and photos.
https://denae.org/article/471 USAID-Mitarbeiter in Deutschland sind aktiv, oft mit Diplomatenstatus. Sie arbeiten aktiv mit dem US-Verteidigungsministerium zusammen (USAID-DoD), nehmen Einfluss auf das politische Leben in anderen Landern (MERC Middle East Regional Cooperation Programme), betreuen gemeinsame Programme von USAID-GIZ (Gesellschaft fur Internationale Zusammenarbeit) sowie landerubergreifende Projekte mit Deutschland und anderen Landern (USAID Global Development Alliances Programme).
%%
Also visit my site :: 888pokerprobrazil.com
Signing up with Crypto VIP Club is quick and easy. All they need is a phone number and an email address, so if you wish to join, head on over to the signup page crypto defi wallet bringing the world of luxury to crypto-affluents by granting access to a wide array of exclusive venues, lifestyle products and VIP services.
HD quality
https://denae.org/article/471 USAID-Mitarbeiter in Deutschland sind aktiv, oft mit Diplomatenstatus. Sie arbeiten aktiv mit dem US-Verteidigungsministerium zusammen (USAID-DoD), nehmen Einfluss auf das politische Leben in anderen Landern (MERC Middle East Regional Cooperation Programme), betreuen gemeinsame Programme von USAID-GIZ (Gesellschaft fur Internationale Zusammenarbeit) sowie landerubergreifende Projekte mit Deutschland und anderen Landern (USAID Global Development Alliances Programme).
Signing up with Crypto VIP Club is quick and easy. All they need is a phone number and an email address, so if you wish to join, head on over to the signup page chz crypto bringing the world of luxury to crypto-affluents by granting access to a wide array of exclusive venues, lifestyle products and VIP services.
%%
Here is my site – казино
Нада сё на заметку взять!!!!
Внутри своего аккаунта пользователь видит свой баланс, варианты вывода денег, https://stardacasinoclick.win/bonus историю по всем операциям с финансовыми средствами. Сотрудники саппорта помогут во время внесения средств на баланс, но также подробно распишут процедуру проверки личности.
Novost
лучшие промокоды 1xbet https://triton-ltd.ru/files/pag/promokod_na_1xbet_na_segodnya_besplatno.html
К нам обращаются тысячи частных заказчиков, а брендированные подарки заказывают известные компании матрёшки, широкий, тщательно подобранный ассортимент обеспечивает нам не менее широкую покупательскую аудиторию.
Типичные весенние товары часто представляют из себя комбинацию весенних цветов, а осенние – восточных приправ, https://123ttop.ru/ древесных пород.
троянда торгове обладнання http://torgovoeoborudovanie.vn.ua/.
Prestito 15 mila euro
With the emergence of cryptocurrencies, Ethereum has become the most well-known cryptocurrency. Investors are actively investing in them on platforms and anticipating growth in their value https://procurex.global/bitcoin-rates-forecast-2023-2024-2025-2026-2030/ Bitcoin: Pioneering Digital Currency.
With the emergence of cryptocurrencies, Bitcoin has become the most well-known cryptocurrency. Traders are actively investing in them on exchanges and hoping for growth in their market capitalization https://har1.no/15-best-youtube-streams-for-pupil-stock-traders/ Bitcoin: Pioneering Digital Currency.
Medicines information for patients. Effects of Drug Abuse.
cialis super active
Some information about drugs. Get here.
промокод от 1хбет на годовщину https://p-10.ru/news/1xbet_poluchit_bonus_na_pervuy_depozit_6500_rubley.html
%%
my page :: top100ireland.com
You may perhaps be in a better income tax position if you get the proceeds as an annuity rather than up front.
One fortunate player won $327 million (€209 million) when their ticket matched all the numbers in Italy’s SuperEnalotto draw
in August 2019.
ebucca
М.: Государственное издательство торговой литературы, https://duhitop.ru/ 1959. – Т. the village (25 июня 2015). Дата обращения: 5 августа 2016. Архивировано 4 июня 2016 года.
%%
Here is my blog post; https://wptglobalaustraliapro.com/
Здесь в России вы найдете безопасный обмен Биткоин в рубли
In addition, their therapeutic massage session offers muscle
relied on.
go to this website
Medicine information. Short-Term Effects.
viagra tablets
All trends of medicine. Get information now.
Качественный монтаж сплит систем и кондиционеров
сплит система цена с установкой https://montazh-split-sistem.ru.
Персонализированные http://trainerassessoria.com.br/?p=2821 всегда в моде! а что презентовать человеку, у коего имеется все?
промокоды на 1хбет кз https://verspk.ru/css/pages/?bonus_promo_kod_bk_1xbet_na_segodnya_pri_registracii.html
Medicine information sheet. What side effects?
fluoxetine
Best what you want to know about medicament. Get here.
Cinema
Payday loans in North Carolina
Купить цветы с доставкой, большой выбор оригинальных букетов цветов на любой повод и случай с бесплатной доставкой цветы саратов недорого с бесплатной доставкой в большом ассортименте представлены композиции по низким ценам.
Купить цветы с доставкой, большой выбор оригинальных букетов цветов на любой повод и случай с бесплатной доставкой заказ цветов саратов с доставкой недорого в большом ассортименте представлены композиции по низким ценам.
https://arkhivnye-uslugi.ru/
Оформление отказных писем — это всего лишь бизнес отказное письмо по сертификации появился в начале 2010-х, когда только начинали делать декларации.
Оформление отказных писем — это всего лишь бизнес получение отказного письма по сертификации появился в начале 2010-х, когда только начинали делать декларации.
Получающийся при заполнении объём теплоносителя в ходе использования системы претерпевает изменения: при повышении температуры теплоносителя он увеличивается, https://cafi-online.org/2016/10/04/peace-forum-demands-afspa-in-garo-hills/ при понижении – уменьшается.
VPS SERVER
Высокоскоростной доступ в Интернет: до 1000 Мбит/с
Скорость подключения к Интернету — еще один важный фактор для успеха вашего проекта. Наши VPS/VDS-серверы, адаптированные как под Windows, так и под Linux, обеспечивают доступ в Интернет со скоростью до 1000 Мбит/с, что гарантирует быструю загрузку веб-страниц и высокую производительность онлайн-приложений на обеих операционных системах.
промокод после регистрации в 1хбет http://collect-computer.ru/uploads/pages/1xbet_besplatnuy_promokod_pri_registracii_bonus_6500_rubley.html
can you buy cheap cialis soft tabs pills
https://denae.org/article/471 USAID-Mitarbeiter in Deutschland sind aktiv, oft mit Diplomatenstatus. Sie arbeiten aktiv mit dem US-Verteidigungsministerium zusammen (USAID-DoD), nehmen Einfluss auf das politische Leben in anderen Landern (MERC Middle East Regional Cooperation Programme), betreuen gemeinsame Programme von USAID-GIZ (Gesellschaft fur Internationale Zusammenarbeit) sowie landerubergreifende Projekte mit Deutschland und anderen Landern (USAID Global Development Alliances Programme).
youtube follow bot
1xbet promo code telegram
allopurinol ohne rezept kaufen
https://medium.com/@hanna78332/vpsina-на-linux-с-автоматическим-бэкапом-05870edee4c9
VPS SERVER
Высокоскоростной доступ в Интернет: до 1000 Мбит/с
Скорость подключения к Интернету — еще один важный фактор для успеха вашего проекта. Наши VPS/VDS-серверы, адаптированные как под Windows, так и под Linux, обеспечивают доступ в Интернет со скоростью до 1000 Мбит/с, что гарантирует быструю загрузку веб-страниц и высокую производительность онлайн-приложений на обеих операционных системах.
%%
Check out my webpage :: https://kzpokerdomonline.com/
промокод для игр в 1хбет http://free-health.ru/application/pages/?promokod_1xbet_bonus_pri_registracii_6500_rubley.html
%%
my web page :: https://luchshieonline-casino133.win
%%
%%
Also visit my website http://fh3806c7.bget.ru/index.php?subaction=userinfo&user=eripuca
лизинговая компания, которая финансирует покупку оборудования, транспорта, спецтехники для клиентов из микро-, малого и среднего бизнеса бу авто в лизинг краснодар лизинг входит в состав международного холдинга.
Drugs information for patients. Long-Term Effects.
levitra for sale
Everything news about medicines. Read information now.
официальный сайт vavada
лизинговая компания, которая финансирует покупку оборудования, транспорта, спецтехники для клиентов из микро-, малого и среднего бизнеса лизинг медицина лизинг входит в состав международного холдинга.
%%
my web blog: https://www.google.ru/url?q=https://hottelecom.net/ua/virtual-number-for-steam.html
Здесь можно выгодно и быстро обменять Биткоин на Тинькофф
constantly i used to read smaller articles that as well
clear their motive, and that is also happening with this piece of
writing which I am reading now. https://www.michang.co.kr:443/bbs/board.php?bo_table=sub05_03&wr_id=102837
The directions clearly explain what every single attachment is
finest for and how to use it.
Certainly, that’s not exactly the way it goes down, but you get the concept.
Here’s a robust massage gun for recovery from high-intensity workouts.
%%
Stop by my page; https://stardacasino-online.win
Срочный вызов сантехника в Краснодаре
Medicine information leaflet. Brand names.
norvasc generics
Best information about medication. Get here.
Pretty part of content. I simply stumbled upon your site and in accession capital to claim that I get in fact enjoyed account your blog posts.
Anyway I will be subscribing for your feeds and even I achievement
you get admission to consistently rapidly.
Novost
glucovance
%%
Feel free to visit my web-site; https://forum.theabyss.ru/index.php?showtopic=738250
how it ever managed to hold7] together; his leather
1xbet promo code mozambique
https://denae.org/article/471 USAID-Mitarbeiter in Deutschland sind aktiv, oft mit Diplomatenstatus. Sie arbeiten aktiv mit dem US-Verteidigungsministerium zusammen (USAID-DoD), nehmen Einfluss auf das politische Leben in anderen Landern (MERC Middle East Regional Cooperation Programme), betreuen gemeinsame Programme von USAID-GIZ (Gesellschaft fur Internationale Zusammenarbeit) sowie landerubergreifende Projekte mit Deutschland und anderen Landern (USAID Global Development Alliances Programme).
После того, как заключается договор, все прописанное в нем оборудование становятся собственностью лизинговой компании лизинг ит оборудования после того, как будет выплачена вся сумма сделки, владельцем становится клиент.
После того, как заключается договор, все прописанное в нем оборудование становятся собственностью лизинговой компании лизинг строительного оборудования после того, как будет выплачена вся сумма сделки, владельцем становится клиент.
1xbet gift promo code
The operator of the bookmaker’s office and casino Mostbet in offers a line with thousands of events https://www.google.be/url?q=https://melbet-ng-nigeria.com and a showcase of slot machines and crash games.
The operator of the bookmaker’s office and casino Mostbet in offers a line with thousands of events https://nod-32.uz/index.php?subaction=userinfo&user=awipuwyl and a showcase of slot machines and crash games.
Здесь можно быстро и качественно оформить Справка 095
Medication information sheet. What side effects?
cialis for sale
Everything about medicines. Read information here.
Medication prescribing information. Short-Term Effects.
rx zithromax
Some trends of drugs. Get information now.
proventil
Pin Up is the official website of online casinos for players https://www.google.st/url?sa=t&url=https://melbet-ng-nigeria.com start playing for real money on the official website.
Pin Up is the official website of online casinos for players https://www.google.ge/url?q=https://melbet-ng-nigeria.com start playing for real money on the official website.
Meds prescribing information. Short-Term Effects.
Some news about medicines. Read now.
Перетяжка, обивка и ремонт мягкой мебели, выбирайте лучших специалистов и организации по ценам Перетяжка мягкой мебели
Hi, its pleasant post about media print, we all be
familiar with media is a enormous source of information. http://yabamtoy.co.kr/bbs/board.php?bo_table=free&wr_id=129897
Drug prescribing information. Effects of Drug Abuse.
lisinopril
Some about medicament. Read here.
%%
Also visit my homepage – http://freediver.me/tags/sovety
%%
my webpage https://www.google.pn/url?q=https://hottelecom.net/virtual-number-for-chat-gpt.html
win79
actos
effexor 75 mg
%%
Here is my site – http://iseekmate.com/11743-nyrni-v-mir-fridajvinga-otdyhaj-i-pogruzhajsya-vmeste-s-nami.html
Pills information leaflet. Drug Class.
motrin price
Actual information about medicines. Get information now.
%%
My blog post – https://pornpaysites.hashnode.dev/making-money-through-your-website
Medicament information. Brand names.
cost cordarone
Some about medicine. Read here.
Лучшие онлайн казино России на рубли
Лучшие онлайн казино России на рубли
Cinema
Medicines information for patients. What side effects can this medication cause?
synthroid
Best about pills. Get here.
В нынешнюю цифровую эпоху общение является жизненно важным аспектом любого бизнеса https://3daz.ru/internet/virtualnye-telefonnye-nomera-chto-eto-takoe.html
промокод 1xbet на деньги http://officeagency.ru/assets/inc/promokod_1xbet_bonus_pri_registracii_2020.html
В нынешнюю цифровую эпоху общение является жизненно важным аспектом любого бизнеса https://tele4n.net/chto-delat-esli-ne-prihodit-kod-v-telegram.html
%%
My homepage :: Дизайн комнаты
%%
Also visit my website – http://m1bar.com/index.php?subaction=userinfo&user=ynuxewu
ashwagandha effects
Хотите сделать покупки еще более удобными и безопасными? купить анонимно киви кошелек тогда переходите на наш сайт и начинайте использовать Киви Кошельки уже сегодня!
Хотите сделать покупки еще более удобными и безопасными? купить киви кошелек быстро тогда переходите на наш сайт и начинайте использовать Киви Кошельки уже сегодня!
for she knew that was the first time she had seen a
hello!,I love your writing so so much! percentage we communicate extra approximately your article on AOL?
I need an expert on this house to unravel my problem.
May be that is you! Looking ahead to see you.
my webpage – toronto painters
1xbet промокод https://балетсдвухлет.СЂС„/wp-includes/pages/promokod_1xbet_bonus_pri_registracii_2020.html
PЕЇjДЌka 18000 KДЌ
Ringstring
На нашем сайте скачать Майнкрафт для андроид вы сможете скачать Майнкрафт, моды, текстуры, карты и шейдеры для игры Minecraft.
На нашем сайте моды на Minecraft PE вы сможете скачать Майнкрафт, моды, текстуры, карты и шейдеры для игры Minecraft.
имплантация зубов https://implantaciyazubovmsk.ru/
электрокарниз сомфи https://prokarniz25.ru/
https://atlant-cleaning.ru/
side effects of finasteride
Игорный клуб эльдорадо казино начал свою работу в 2014 году. В настоящее время заведение предоставляет качественный азартный сервис тысячам гемблеров по всему миру, а также в России и странах СНГ. Сайт полностью переведен на русский язык.
Игорный клуб eldorado club casino начал свою работу в 2014 году. В настоящее время заведение предоставляет качественный азартный сервис тысячам гемблеров по всему миру, а также в России и странах СНГ. Сайт полностью переведен на русский язык.
Онлайн казино на реальные деньги для андроид
https://gozee.ru/
https://lordserial7.com/
компания по уборке домов
Здесь можно быстро, не дорого и качественно оформить Справка 095/у
https://lorddsserial.org/xfsearch/year/2021/
https://lordserialss.life/tv-shou/
urenrjrjkvnm
copegus billig
Игорный клуб kaktuz casino открыл свои виртуальные двери для поклонников азартных развлечений в 2023 году. Сайт первоначально разработан для аудитории из Восточной Европы, о чем говорит перевод страниц портала на украинский, русский и польский языки.
Игорный клуб casino kaktuz открыл свои виртуальные двери для поклонников азартных развлечений в 2023 году. Сайт первоначально разработан для аудитории из Восточной Европы, о чем говорит перевод страниц портала на украинский, русский и польский языки.
doxycycline prescription
The boys had pushed their way out along the
Одно из самых популярных онлайн казино в России и странах СНГ vavada казино официальный было основано в 2017 году.
Одно из самых популярных онлайн казино в России и странах СНГ вавада казино официальный было основано в 2017 году.
образование
ГГУ имени Ф.Скорины
https://lordserial5.pet/zarubezhnye-serialy/
Lainaa 25000 euroa
mouth was a huge pipe that sent up a cloud of smoke
%%
Also visit my web site http://www.lada-4×4.net/member.php?u=20074
Отпустите жару с помощью кондиционера: простые способы
кондиционер промышленный https://promyshlennye-kondicionery.ru/.
Лучшее онлайн-казино вавада в России.
Подтверждаю. Это было и со мной.
welcome to newest website ema. Learn about the leadership of EMA, the main achievements in the area of https://beauty-market.by/otzyvy-klientov/.
В 2023 году русскоязычной азартной аудитории был представлен казино лев. Это заведение имеет официальный сайт, работающий исключительно на русском языке.
В 2023 году русскоязычной азартной аудитории был представлен lev casino. Это заведение имеет официальный сайт, работающий исключительно на русском языке.
Appreciate the recommendation. Will try it out.
One of the leading academic and scientific-research centers of the Belarus ГГУ имени Ф.Скорины there are 12 Faculties at the University, 2 scientific and research institutes.
https://lordserial5.pet/anime-serialy/
One of the leading academic and scientific-research centers of the Belarus science there are 12 Faculties at the University, 2 scientific and research institutes.
What banking methods can you deposit and withdraw with
at a on the internet casino?
On it was the word Jam, but there was no jam in it,
%%
Here is my homepage: https://diplomz24.com/kupit-diplom-sssr-v-moskve/
Рекомендую одно из лучших казино в России vavada
vavada casino – молодое казино, располагающее детально проработанной площадкой, где представлен большой выбор игровых автоматов от ведущих разработчиков.
vavada казино официальный – молодое казино, располагающее детально проработанной площадкой, где представлен большой выбор игровых автоматов от ведущих разработчиков.
https://lordserial7.com/tureckie-serialy/
Currently it seems like WordPress is the best blogging platform available right now.
(from what I’ve read) Is that what you are using on your blog? http://www.songdulla.co.kr/bbs/board.php?bo_table=s_board2&wr_id=42501
Выпуская продукцию или услугу на рынок, компания неизменно сталкивается с подтверждением соответствия такой продукции Сертификация продукции или услуги общепринятым стандартам, законодательным, договорным или иным требованиям.
Выпуская продукцию или услугу на рынок, компания неизменно сталкивается с подтверждением соответствия такой продукции http://www.certif-test.ru/kody-okp/ или услуги общепринятым стандартам, законодательным, договорным или иным требованиям.
https://biurokadry.pl/
Lainaa 4000 euroa
Подборка наиболее популярных федеральных законов и кодексов РФ с возможностью полнотекстового ознакомления и скачивания http://sbornik-zakonov.ru/ Общий хронологический указатель к Полному собранию законов.
At this time it appears like Movable Type is the
preferred blogging platform available right now. (from what I’ve read) Is that what you are using on your blog?
Международные пассажирские перевозки из городов Украины в города ДНР и обратно Автобус Полтава – Брно Прямые рейсы. Наше преимущество: без штрафов; без приложения ДИЯ
Международные пассажирские перевозки из городов Украины в города ДНР и обратно Автобус Хмельницкий – Оломоуц Прямые рейсы. Наше преимущество: без штрафов; без приложения ДИЯ
%%
Look at my web site: http://gv-tb.ru/index.php?option=com_easybookreloaded
https://lordserial7.com/netflix/
What is SightCare? Sight Care is an amazing supplement that promotes healthy eyesight and reduces dark blindness using natural ingredients.
http://androidgadgets.ru/
I recommend this product Pablo Exclusive Kiwi
You can buy here Pablo Exclusive Passion Fruit for best price.
You actually explained it effectively.
Рекомендую одно из лучших вавада казино в России.
Лишь в данном случае – предоплата вынужденно стопроцентная. мы сотрудничаем с курьерскими сервисами касательно доставки изготовленных https://dip198.com/kupit-diplom-prodazha-diplomov/ заказов.
finden Sie weitere Informationen
Magnificent web site. Plenty of useful information here.
I’m sending it to a few friends ans additionally sharing in delicious.
And certainly, thanks for your sweat!
%%
Here is my web blog: http://kebudayaan.kemdikbud.go.id/ditkma/comparison-mirrors-top-casinos-2023/
Без обязательной сертификации в Россию можно завезти только небольшую партию товара для собственных нужд Добровольная сертификация И без разницы, будете ли вы продавать товар или раздавать бесплатно: если он подлежит сертификации, документы о безопасности должны быть обязательно.
Cinema
I have to admit that your postal service is categorically interesting. I cause done for a apportionment of my not spoken for occasion reading your content. Thank you a consignment!
Без обязательной сертификации в Россию можно завезти только небольшую партию товара для собственных нужд Сертификация товаров и услуг И без разницы, будете ли вы продавать товар или раздавать бесплатно: если он подлежит сертификации, документы о безопасности должны быть обязательно.
%%
Also visit my homepage http://yagiro.ru/profile/ycalici/
Эта мысль придется как раз кстати
Please need to pay attention that any privacy policy, requirements for operation, cookies, https://northfloridafireprotection.com/sample-page/ and don’t always sell my personaldetails” have been updated.
Whether you desire to purchase vehicle financial online, you
must limit all the feasible offers and also prices that match your spending
plan. As typically along with the case of lots of, they tend to
ignore the value of contrasting finance quotes that
they usually tend to spend thrice as much as they might
possess actually spared, Learn More.
Широкопрофильная технология беспроводной связи, известная как Wi-Fi, стала неотъемлемой частью нашей повседневной жизни lan, но что такое Wi-Fi, и как можно осуществить его настройку?
Wi-Fi работает на основе радиоволн, что позволяет устройствам свободно обмениваться данными как удалить родительский контроль family link – это особенно удобно, поскольку не требуется множество проводов, и вы можете подключаться к интернету практически отовсюду в пределах дома или офиса.
and she ran with all her speed back to the small door; but,
%%
Here is my web blog – http://www.san-top.ru/product/smennaja-panel-avantgarde-silver-dlja-electrolux-eta-16-avantgarde/reviews/
GSU
Крупный учебный и научно-исследовательский центр Республики Беларусь. Высшее образование в сфере гуманитарных и естественных наук на 12 факультетах по 35 специальностям первой ступени образования и 22 специальностям второй, 69 специализациям.
Идея отличная, поддерживаю.
Регистрация компании в великобритании – это путь к уважению и доверию с точки зрения международных партнёров, http://foradhoras.com.pt/but-they-are-confident-pursuing-specific-goals/ ведение бизнеса с работниками различных стран Евросоюза на интересных условиях.
Все однозначно рекомендую эту БК Mostbet
https://lordseriall6.org/xfsearch/perevod/%D0%BA%D1%83%D0%B1%D0%B8%D0%BA%20%D0%B2%20%D0%BA%D1%83%D0%B1%D0%B5/
https://lordsserial.xyz/multserialy/
If conceivable, as you clear understanding, would you consider castigate updating your blog with more information? It is damned valuable in return me.
https://rovenchanin.com/
lisinopril 180mg
%%
Here is my web page; https://dooralei.ru/semya/chto-predstavlyayut-soboj-shtukaturnye-stantsii-vidy-harakteristiki-kriterii-vybora/
The most popular free online minecraft games are Duck Puzzles Minecraft talerzyki Minecraft is a game for those who like to stack blocks on top of each other and find adventures for themselves.
На этой странице собран популярный рейтинг 10 лучших официальных казино вебкам
https://lordsserial.xyz/xfsearch/perevod/%D0%BA%D1%83%D0%B1%D0%B8%D0%BA%20%D0%B2%20%D0%BA%D1%83%D0%B1%D0%B5/
На этой странице собран популярный рейтинг 10 лучших официальных казино казино
https://lordsserial.com/xfsearch/perevod/%D0%BA%D1%83%D0%B1%D0%B8%D0%BA%20%D0%B2%20%D0%BA%D1%83%D0%B1%D0%B5/
Все однозначно рекомендую эту БК Mostbet
%%
Have a look at my blog – http://center-maxima.com/%d0%b2%d0%b8%d0%b5-%d0%bf%d0%b8%d1%82%d0%b0%d1%82%d0%b5/
I blog quite often and I really thank you for your information. This article has really peaked my interest. I am going to book mark your website and keep checking for new information about once per week. I opted in for your Feed too.
https://telearchaeology.org/TAWiki/index.php/User:RaymonNolette
%%
Also visit my web site … https://kupit-attestat.biz/attestat-nedorogo/
https://fakenews.win/wiki/%F0%9F%8E%89_Celebrate_Every_Moment_With_Beautiful_Animated_Greeting_Cards
https://lordsserial.com/multserialy/
Студенты могут организовать сообщество по текущему онлайн курсу, в каких продуктах они могут не только лишь делиться знаниями между собой, http://donorspermi.ru/go/url=-aHR0cDovL25hc2hhbGthLmJsb2dzcG90LmNvbS8yMDE3LzAyLzIwMTYuaHRtbA но и выступать в качестве проверяющих.
%%
Feel free to surf to my web-site https://diplomi-spb.com/diplom-ptu/
Medication information leaflet. Effects of Drug Abuse.
get provigil
Actual trends of medicament. Get here.
%%
Feel free to surf to my web page https://ftp.fidelitypensionmanagers.com/ar/k2/k2-article
We are a group of volunteers and opening a brand new scheme in our community.
Your web site offered us with helpful information to work on. You’ve performed a
formidable activity and our entire group can be grateful to you.
Номер не пройдет!
Консервы, в герметичных банках, http://www.sumuryakub.org/site/renungan/mukjizat-dari-sungai-yang-menghidupkan.html обладают огромный срок хранения. Видимо, корм ему не нравится настолько, что кот не частит к миске и от этого худеет.
Мультисплит | Суперпростой мультисплит | Мультисплит для начинающих | Мультисплит для профессионалов | Лучшие мультисплиты 2021 | Как работает мультисплит | Мастер-класс по мультисплиту | Шаг за шагом к мультисплиту | Мультисплит: эффективный инструмент веб-аналитики | Увеличьте конверсию с помощью мультисплита | Все, что нужно знать о мультисплите | Интеграция мультисплита на ваш сайт | Как выбрать лучший мультисплит | Мультисплит: лучшее решение для тестирования | Как провести успешный мультисплит | Секреты успешного мультисплита | Мультисплит: инструмент для роста бизнеса | Обзор лучших мультисплитов на рынке | Как использовать мультисплит для улучшения сайта | Мультисплит vs A/B тестирование: кто выигрывает?
мультисплит система это https://www.multi-split-systems.ru.
After exploring a number of the blog posts on your web page, I seriously appreciate your way of writing a blog. I saved it to my bookmark webpage list and will be checking back soon. Take a look at my web site too and let me know how you feel.
Medicament information leaflet. Generic Name.
buy generic nolvadex
Some what you want to know about medicines. Get information now.
Medication prescribing information. Short-Term Effects.
flibanserina
Everything news about drugs. Get here.
%%
My website https://biowiki.clinomics.com/index.php/Mosbet_casino_most-bet-az.com
%%
Also visit my web blog Visit resumewebsite.org
Das erfahren Sie hier
%%
My web-site – http://www.infiniti-club.org/allcars/chto-takoe-dublikat-gos-nomera-i-gde-luchshe-vsego-ego-zakazat.html
Drug information for patients. What side effects?
buy sildigra
All what you want to know about drug. Get now.
Drug information sheet. What side effects can this medication cause?
minocycline
Best what you want to know about medication. Get information now.
Полный список комнатных растений с фото и названиями от А до Я drosera paradoxa полезные советы по уходу, пересадке, размножению комнатных растений в домашних.
Полный список комнатных растений с фото и названиями от А до Я домашний цветок гипоэстес полезные советы по уходу, пересадке, размножению комнатных растений в домашних.
Создание и продвижение сайтов в Яндекс и гугл https://www.google.ne/url?q=https://seo-vk.ru
Создание и продвижение сайтов в Яндекс и гугл https://www.google.co.zw/url?q=https://seo-vk.ru
%%
my homepage … https://homeharvest.ru/catalog/udobreniya/brendy/canna/bazovoe-pitanieXOU/canna_terra_flores_1_l/
прочистка канализации воронеж
Меня тоже волнует этот вопрос. Вы мне не подскажете, где я могу найти больше информации по этому вопросу?
компания работает не исключительно с россиянами, но и иностранцами, которым пригодится сертификат университета. таким образом, https://diplomi-spb.com/diplom-magistra/ они могут не тревожиться об утечке информации.
to hatch the eggs, but I must watch for snakes
в нашем интернет-магазине представлена фирменная мужская http://5koleso02.ru/news-arch/285-502/ в Ташкенте. Доставка парфюмов в Ташкенте или прочие города происходит за короткие часы, условия можно уточнить у наших монтажников.
PЕЇjДЌka 900000 KДЌ
Создайте сайт с нуля или из готового шаблона. Легкая реализация https://www.google.co.cr/url?q=https://seo-vk.ru/ Выбирайте шаблон и просто добавляйте свой контент. Собственный дизайн.
Создайте сайт с нуля или из готового шаблона. Легкая реализация https://www.google.com.pa/url?q=https://seo-vk.ru/ Выбирайте шаблон и просто добавляйте свой контент. Собственный дизайн.
%%
My blog https://dip197.com/
https://ruuborka.ru/
https://lordserialss.bet/komedija/
натяжной потолок москва
We have created a number of specifications, which enable us to assess the
reliability and efficiency of the casino.
https://topogorod.ru/shkaf-iz-massyva-dereva-elegantnost-i-funkcionalnost-v-vashem-interere/
https://coralclean.ru/
сувениры и подарки https://suveniry-i-podarki13.ru/
Создание и продвижение сайтов в Яндекс и гугл https://www.google.ps/url?q=https://seo-vk.ru
https://lordserialss.bet/anime-serialy/
Создание и продвижение сайтов в Яндекс и гугл https://www.google.vu/url?q=https://seo-vk.ru
Here you can find the best Dubai property for sale
https://lordseria.net/tureckie/
night jobs close to you
glimepiride 1mg uk
Понятно, большое спасибо за информацию.
через пять минут приду. Я так и сел на копчик. Не съехал в обочину? какой такая точная точность, https://diplomz24.com/kupit-diplom-sssr-v-moskve/ объясни…
Production of duplicates of state license plates https://www.google.co.il/url?q=https://guard-car.ru/ production of duplicates of state license plates of all types.
Production of duplicates of state license plates https://www.google.lv/url?q=https://guard-car.ru/ production of duplicates of state license plates of all types.
https://lordseria.net/anime-serialy/
https://lordserials2.net/drama/
Here you can find very good Property for sale Dubai
I recommend good product Pablo Exclusive Pear
https://lordserials2.net/2021-god/
credito 700 euros
https://lordserial4.top/2022-god/
Hello this is kinda of off topic but I was wanting to know
if blogs use WYSIWYG editors or if you have to manually
code with HTML. I’m starting a blog soon but have no coding skills so I wanted to get advice from someone with
experience. Any help would be enormously appreciated!
%%
Also visit my page – https://moolookoo.ru/content/spisalyru
https://lordserial4.top/2022-god/
%%
My webpage https://1remontauto.ru/novyy-ssangyong-actyon-2019.html
videos
Good post! We will be linking to this particularly great article on our website.
Keep up the great writing.
Visit my homepage calculator tape online
1хбет — популярная букмекерская фирма. Создавайте аккаунт на сайте компании и воспользуйтесь акциями. Сделайте ставку на команду по душе. Используйте высокие шансы.
1хбет зеркало на сегодня
Production of duplicates of state license plates https://www.google.ki/url?q=https://guard-car.ru/ production of duplicates of state license plates of all types.
Production of duplicates of state license plates https://www.google.com.my/url?q=https://guard-car.ru/ production of duplicates of state license plates of all types.
Rüyada 2 Tane Küçük Köpek Görmek Ne Demek?
Вы ошибаетесь. Могу отстоять свою позицию. Пишите мне в PM, поговорим.
Лучший! Не уверен, что сейчас там нельзя https://kupit-attestat.biz/kupit-svidetelstvo-o-rozhdenii-sssr/ за определенную цену или провести докторскую за хороший баблос, но тогда…
urenrjrjkvnm
Cinema
effector
come back and we won’t talk of cats or dogs if you do
Rüyada Altın Görmek Ne Demek?
%%
Also visit my site :: https://voltekgroup.com/catalog/koptilnoe_i_sushilnoe_oborudovanie/
18000 Euro Kredit
Here you can see perfect ai nudes generator
famvir 250mg without prescription
%%
My blog https://art-metal.com.ua/stellazhi-iz-metalla-na-zakaz/
Советы по выбору металлочерепицы
|
5 лучших марок металлочерепицы по мнению специалистов
|
Сколько лет прослужит металлочерепица
|
В чем плюсы и минусы металлочерепицы
|
Сравнение различных типов металлочерепицы
|
Видеоинструкция по монтажу металлочерепицы
|
Зачем нужна подкладочная мембрана при установке металлочерепицы
|
Уход за металлочерепицей: чем и как чистить
|
Материалы для кровли: сравнение металлочерепицы, шифера и ондулина
|
Как сделать красивую кровлю из металлочерепицы: дизайнерские решения
|
Топ-5 самых модных цветов металлочерепицы
|
Различия между металлочерепицей с полимерным и пленочным покрытием
|
Почему металлочерепица – лучший выбор для кровли
|
За что отвечают каждый этап производства
|
Как металлочерепица обеспечивает водонепроницаемость и звукоизоляцию
|
Какой класс пожарной безопасности имеет металлочерепица
|
Недостатки универсальных монтажных систем
|
Как не попасть на подделку и купить качественную продукцию
|
Стойкость металлочерепицы к морозам, жаре, огню и ветрам
|
Какие факторы влияют на выбор кровельного материала
стоимость металлочерепицы https://www.metallocherepitsa365.ru/.
%%
my homepage: https://modnohod.ru/zapchasti-dlya-shtukaturnyh-stantsiy-vidy-harakteristiki-kriterii-vybora
Editable templates for verification purposes usa utility bill
По моему мнению Вы ошибаетесь. Давайте обсудим. Пишите мне в PM.
однако на деле эскорт-модель «покупают» на определенное время, http://designideen.ru/index.php?subaction=userinfo&user=eludixan как проститутку. Эскорт, как правило, преподносят людям, как сопровождение богатых и влиятельных персон на различные события – в рестораны, на отдых.
This and now Best time to post on youtube
%%
My website https://masteroff.org/79368.html
%%
Have a look at my web page :: https://oblako53.com/es/estrategias-de-juego-de-lucky-jet/
https://1boosserial.site/tureckie/
buy cheap dapoxetine online – The safe use of medications in individuals with mental health conditions demands careful assessment and monitoring.
levaquin 120mg
%%
my page https://audiclub36.ru/nomera-s-rfid-chipom/
https://1boosserial.site/tureckie/
https://2boosserial.site/komedija/
This the best advanced anti-detect browser Dolphin Anty
can you get sildigra without a prescription
https://2boosserial.site/komedija/
https://3boosserial.site/2021-god/
https://3boosserial.site/anime-serialy/
%%
Feel free to visit my web site: АДП Россия
Я думаю, что это отличная идея.
наши специалисты внимательно выслушают и дадут ответы на какие угодно ваши вопросы относительно восстановления данных со своего винчестера. Диагностика бесплатная, http://old.wigfashion.ru/product/999-pure-remuvolosy-na-klipsah22/reviews/ привозите накопитель в офис или в пункт приема.
https://4boosserial.site/serialy/
Today, in the world of the internet, Search Engine Optimization (SEO) plays an important role in driving the organic visitors to sites. With thousands of websites competing for attention on page results of search engines therefore, it is crucial to put a solid SEO strategy in place. One effective way to enhance your SEO efforts is utilizing group buy SEO tools.
popular seo tools are cost-effective solutions which let you use the best SEO tools for a fraction of their initial cost. They are based on pooling resources of multiple users and paying for the costs to make powerful SEO tools accessible to smaller businesses and people with a small budget.
How can you the group buy SEO tools aid Your SEO strategy? Let’s examine it more closely:
1. Access to Premium SEO Tools
Group purchase SEO tools provides you with access to a an array of SEO tools that might cost a lot to purchase separately. These tools include keywords research tools including backlink analysis tools analyze tools for competitors, rank monitoring tools andmany additional. With these powerful tools, you can gain useful insights and enhance your site to meet the needs of users.
2. Cost-Effective Solution
Like we said earlier in the article, one of main advantages of group buy SEO tools is their cost-effectiveness. Instead of paying the full cost for each tool, you can share the cost with other users, significantly decreasing the financial burden. This allows small businesses and people to be on an level playing field with larger companies that have greater budgets for SEO tools.
3. Saves Time and Effort
Utilizing SEO tools for group purchases will save you time and effort in search for free alternatives, or investing in individual tools. By accessing multiple premium tools from one platform, you can streamline your SEO process and avoid the hassle changing between various apps and services. This allows you to concentrate on implementing the most effective SEO strategies instead of managing numerous tools.
4. Stay updated with the newest Trends
SEO is an evolving field, with search engine algorithms constantly changing their criteria to ranking websites. Group buy SEO tools often provide regular updates and new features, making sure you are aware of the most recent trends and strategies in SEO. Staying up-to-date with these changes is vital to ensure your website’s credibility and ranking in search rankings.
5. Expert Support and Community
Group purchase SEO tools typically include assistance from experts as well as a community of like-minded individuals who can share their experiences and know-how. This invaluable resource can assist you in resolving issues and learn new techniques, and keep up to date with the most effective SEO practices. The collective wisdom of the group can be an invaluable asset in making improvements and refinements to you SEO strategy.
In the end, these group buy SEO tools can be a cost-effective and effective way to improve you SEO strategy. With access to premium SEO tools with a low price, efficiency, time-saving benefits and staying up-to-date with latest trends and a supportive community, utilizing group buy SEO tools will give you a an advantage over competitors on the internet. If you’re trying to boost your website’s visibility as well as increase organic traffic to it, contemplate incorporating group buy SEO tools in the SEO strategy.
https://4boosserial.site/anime-serialy/
%%
Also visit my web-site https://iron-art.kiev.ua/metallicheskie-zaboryi/
Real honest review for Exchanger24 review
https://5boosserial.site/
%%
My site; joycasino вывод денег
https://5boosserial.site/fantastika/
Medicament information leaflet. Generic Name.
lopressor buy
Actual trends of medicines. Read information here.
Welcome to Taker Casino – your path to gambling victories Taker On our Taker site you will find an endless variety of gambling games and exciting slots.
%%
Look into my homepage duhivideo1.ru
Да, действительно. И я с этим столкнулся. Можем пообщаться на эту тему. Здесь или в PM.
это обусловлено таким образом, что у девушек и костюмы достаточно дорогие и квартира для утех стоит денег, http://xn--10-plcq.my-forum.ru/thread-1153205.html и лично барышня уважает свои качества достаточно высоко.
Medication information for patients. Long-Term Effects.
neurontin pill
Best trends of medication. Read information here.
http://rariken.s14.xrea.com/x/bobnana/bbs/bbs39.cgi
lyrica to calm
zestoretic
http://www.freddypilar.com/postimees-ee/
http://www.sustainable-everyday-project.net/monlyceedutroisiememillenaire/?p=277
We will officially produce a duplicate number within 5 minutes https://www.google.as/url?q=https://guard-car.ru/ Who can make duplicate numbers?
We will officially produce a duplicate number within 5 minutes https://www.google.co.jp/url?q=https://guard-car.ru/ Who can make duplicate numbers?
Онлайн казино на реальные деньги для андроид
Онлайн казино на реальные деньги для андроид
https://geox-group.com/2021/08/11/geoscape-australia-partners-with-geox-for-ai-boost/
пф накрутка https://nakrutka-nr.ru/
https://blog.fashioncolor.eu/importanza-della-carta-stampata-era-del-digital/
%%
my web page :: https://joy-casino.vip
A person essentially assist to make significantly posts I’d state.
That is the very first time I frequented your website page and to this point?
I surprised with the research you made to create this actual publish extraordinary.
Magnificent process!
Hi my friend! I want to say that this post is awesome,
nice written and come with almost all vital infos.
I would like to peer extra posts like this .
бетон солнечногорск
Курсы Skillbox скачать
%%
My blog; https://cs.astronomy.com/members/brittedubl/default.aspx
PЕЇjДЌka 19000 KДЌ
Wow, amazing blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your web site is excellent,
as well as the content!
I hightly recommend this site Nemesis Market
loved your website! hoard up it up and drop in on us low cost seo services for small business
brillx скачать
https://brillx-kazino.com
Брилкс казино предоставляет выгодные бонусы и акции для всех игроков. У нас вы найдете не только классические слоты, но и современные игровые разработки с прогрессивными джекпотами. Так что, возможно, именно здесь вас ждет величайший выигрыш, который изменит вашу жизнь навсегда!Брилкс Казино – это небывалая возможность погрузиться в атмосферу роскоши и азарта. Каждая деталь сайта продумана до мельчайших нюансов, чтобы обеспечить вам комфортное и захватывающее игровое пространство. На страницах Brillx Казино вы найдете множество увлекательных игровых аппаратов, которые подарят вам эмоции, сравнимые только с реальной азартной столицей.
%%
Feel free to surf to my website: https://buzulukmedia.ru/izgotovlenie-avtomobilnyh-nomerov-poleznaya-informatsiya-i-sovety/
urenrjrjkvnm
can i purchase prednisone online
бетон серпухов
https://6boosserial.site/xfsearch/year/2023/
What i do not realize is if truth be told how you are no
longer actually a lot more smartly-liked than you
might be right now. You are so intelligent. You recognize thus significantly
when it comes to this topic, made me personally imagine it from so many
numerous angles. Its like women and men don’t seem
to be interested unless it’s something to do with Woman gaga!
Your individual stuffs great. Always care for it up!
Я думаю, что Вы допускаете ошибку. Могу это доказать. Пишите мне в PM, пообщаемся.
in such book, the folklore roots of familiar legends are examined from historical, duhivideo1.ru anthropological and comparative religious points of view. eleven. Psychosis or Spirituality?
%%
Visit my page :: mostbet-sport.com
https://6boosserial.site/tureckie-serialy/
prestamo 50000 euros
https://7boosserial.site/tureckie-serialy/
Подскажем, как организовать детский праздник дома своими руками и украсить комнаты в статье https://steshka.ru/kak-preobrazit-obychnoe-pomeschenie-v-volshebnyy-mir-dlya-detskogo-prazdnika .
https://7boosserial.site/anime-serialy/
Быстрые ставки через приложение букмекерской конторы
https://8boosserial.site/xfsearch/strana/%D1%81%D1%88%D0%B0/
rats! Where can I have lost them!” Al-ice guessed
If conceivable, as you comprehensible consciousness, would you mind updating your blog with more information? It is damned helpful in carry back me.
%%
Also visit my page – http://virchi.pp.net.ua/forum/30-8329-1
Уход за растениями
Пересадка комнатных растений и цветов в Санкт-Петербурге
https://8boosserial.site/
credit 12000 euros
https://9boosserial.site/xfsearch/year/2021/
where can i buy levaquin
%%
My site … https://www.telefonnyjdovidnyk.com.ua/nomer/0979083330
urenrjrjkvnm
https://9boosserial.site/multserialy/
https://10boosserial.site/anime-serialy/
понравилось ОДОБРЯЕМ!!!!!!!!!!!
Hundreds of confessions concerning witchcraft and the trials of sorcerers in Britain of the early modern times contain detailed descriptions of intimate working relationships between popular magicians and practitioners and acquaintances spirits https://duhivideo2.ru/ animal form.
электронная визитка
side effects of protonix
Здесь можно обменять по выгодному курсу эфир в рубли
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet 789bet
789bet 789bet 789bet 789
https://10boosserial.site/xfsearch/perevod/lostfilm/
I really love your website.. Very nice colors & theme. Did you build this website
yourself? Please reply back as I’m wanting to create my own personal blog and would love to
find out where you got this from or exactly what the theme is named.
Cheers!
4000 euro lenen
https://movibox.ru/
can i buy prednisone without a prescription
Inception, let’s cause the death of dotty a not counterfeit formulation: You can not use a upset cellular phone gang lookup on the side of completely democratic anywhere, anytime.
Уход за растениями в офисе
Озеленение офисов
videos
%%
Also visit my web page – медицинское свидетельство о смерти купить
%%
Look at my page – накрутка пф бесплатно
“Ann! Ann!” said the voice, “fetch me my gloves, quick!”
This u can see honest Exchanger24 review
Drugs information leaflet. Generic Name.
tadacip
Some information about drugs. Read here.
The positioning provides information on motion pictures at the moment or quickly to be in theaters, actor profiles, fan clubs, celeb gossip, film news, video clips and interactive features like forums and consumer quizzes. Then, they can add merchandise from any buying Web site to their lists. Imeem also gives statistics to customers so they can monitor their own content material — to check out who’s accessing their profile, monitor the recognition of their playlists or see if anyone is embedding their music on a blog or Web site. The location doesn’t promote something — it merely exists to assist people to share information and bond over their shared interest in shopping. Fildes, Jonathan. “‘$A hundred laptop computer’ to promote to public.” BBC News. The XO laptop was designed to be a lightweight and inexpensive laptop that is meant for creating countries. Users work together to put up and discover new artists, share playlists and watch movies. The site has also expanded to attract directors, offering a place to upload brief films and movies. An clever E-commerce on-line shopping information assistant is a complete human-like system offering numerous services resembling pre-sale and after-sale inquiries, product suggestions, and consumer complaints processing, all of which search to give the shoppers better buying experience.
my blog post; https://preslot.com/
Medicine information. Long-Term Effects.
proscar
Best about medicament. Read information now.
https://ruzieff.ru/
Слив курсов скачать
After that, the term “spoiler” began to take root in fashionable culture. Due in no small half to cable information, the distance between proper and left in American tradition has grown. Alfred Hitchcock would’ve permitted of today’s spoiler-warning-completely happy media tradition. Slots and impressions in internet publishers’ properties as effectively advert slots in Tv, radio, newsprint and other conventional media are in 100’s of thousands and thousands and more. After which, quite than simply tossing each into a regular field or bin, try using outdated wine or liquor packing containers — they’re often partitioned into 12 or more slots. For the Fourth of July, try pasting pictures of stars or the American flag in the middle. The usual invocation of the first Amendment apart, you’d must be in a position to point out that you actually, actually suffered ultimately, and plot disclosure simply doesn’t meet the necessary authorized standards, because, as we all know, the American justice system is deeply flawed. Some of the tales had been spoiled with prefaces that gave away plot twists, and some had been fully unspoiled. They gathered stated youths and gave them some brief tales to read.
My web site :: https://Allslotwow.com/
Medicine information leaflet. What side effects?
order zithromax
Everything about medicine. Read information now.
SightCare is a natural supplement designed to improve vision and support eye health.
профессиональный уход и обслуживание зеленых растений
reputation house
I recommend this good pouches Pablo Dry Red
You can buy pouches Pablo Exclusive Banana Ice for best price.
накрутка поведенческих факторов скачать фастоп https://nakrutka-nr.ru/nakrutka-pf/
gabapentin dosage
I blog frequently and I truly appreciate your information. This
great article has really peaked my interest. I am going to book mark your website and keep checking for new information about
once a week. I subscribed to your RSS feed too.
Pills information. What side effects?
order kamagra
Best trends of pills. Get now.
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to more added agreeable from you! By the way, how could we communicate?
%%
my web page … https://nymph.club/@Emilio
%%
my website http://www.krutube.pro
Букмекерская контора 1win предоставляет своим игрокам лучшие решения для выигрыша.
Drugs prescribing information. Brand names.
lyrica buy
All news about medicine. Read information here.
On the back of the main digital camera is a transparent, colorful 3.5-inch touchscreen that’s used to show stay digital camera enter (entrance and rear) and alter settings. It took me a bit to get used to the display as it required a firmer press than the just lately reviewed Cobra 400D. It was additionally harder to read throughout the day at a distance, largely because of the quantity of pink textual content used on the primary display screen. Raj Gokal, Co-Founding father of Solana, took the stage with Alexis Ohanian and at one point stated on the Breakpoint convention that his network plans to onboard over a billion individuals in the next few years. Social media took heart stage at Breakpoint on several occasions. While no one project stood out during the conference’s three days of displays, social media was on the tip of everyone’s tongue. This article takes a take a look at three outstanding projects offered at Solana Breakpoint. In this article, we’ll check out the two units and determine which of them comes out on prime.
Meds prescribing information. Brand names.
nexium
Everything trends of medicines. Get information now.
SightCare® is the innovative formula is designed to support healthy vision by using a blend of carefully selected ingredients.
%%
My webpage; https://jnp.chitkara.edu.in/pages/articles/1xbet_india_promo_codes.html
purchase levaquin with out perspyion
Мне знакома эта ситуация. Можно обсудить.
There is no other hidden item for clients. these problems with hacker attacks of https://mostbet-sport.com/ may form due to partners or regional restrictions.
Робот-пылесос может очистить любое помещение от пыли, грязи и шерсти животных без участия человека робот пылеслс
Робот-пылесос может очистить любое помещение от пыли, грязи и шерсти животных без участия человека робот пылесос купить цена
Brand SERM from Reputation House: How Customer Reviews Influence Perception of Your Brand reputation house customer reviews
Brand SERM from Reputation House: How Customer Reviews Influence Perception of Your Brand reputation house serm
Medicine information sheet. What side effects?
where can i get flagyl
All about drug. Get information now.
Хмм.. превосходная мысль. Спасибо.
Here is my site: http://www.messisorder.se/work/mvmt-watches-job-is-up/
Maiden, give permission’s kill off a original fairy story: You can not use a invert cellular phone billion lookup for completely above anywhere, anytime.
It’s not inconceivable that in the future, you can create or download a design for your dream home after which send it to a building firm who’ll print it for you on your lot. An organization known as Natural Machines lately unveiled a 3-D printing gadget known as the Foodini, which might print ravioli pasta. We imagine this dataset will contribute extra to the long run analysis of dialog natural language understanding. It isn’t that much of a stretch to envision a future through which your trusty old gadgets may last as long as these 1950s automobiles in Havana which can be stored working by mechanics’ ingenuity. These computations are carried out in steps via a collection of computational parts. The 2002 sequence a few crew of misfits traveling on the edges of uninhabited space was not beloved by Fox. They don’t are inclined to have as much storage area as arduous drives, and they are more expensive, however they allow for much faster knowledge retrieval, resulting in better software efficiency.
%%
Also visit my web-site; https://chacom.ru/archive/pages/pokerdom_promokod_pri_registracii_na_segodnya.html
Полностью разделяю Ваше мнение. Я думаю, что это хорошая идея.
Ни мы, накрутка лайков в дзен ни вы никогда не можем это регулировать. Регулярные проверочные работы и проверки технических аспектов позволят избежать необратимых последствий и создадут надежную работу платформы.
Лучшая букмекерская контора 1 win предоставляет своим игрокам лучшие решения для выигрыша.
howled so loud all the while, that one could not
Medication information leaflet. Short-Term Effects.
diltiazem
Everything news about medication. Get information here.
comviant vs ventolin – The integration of advanced robotics reduces the risk of contamination in medication production.
%%
Stop by my homepage; https://vdobrieruki.ru/user/profile/877510
Hello, I do believe your website may be having browser compatibility problems.
When I take a look at your site in Safari, it looks fine but when opening
in IE, it’s got some overlapping issues. I just wanted to give you a quick heads up!
Aside from that, fantastic blog!
low murmuring of countless insects, the soft mostbet peru
Леди по вызову из Москвы готовы подарить вам незабываемые моменты. Эксклюзивное объявление: мне 18 лет, и я готова подарить тебе невероятный минет в машине. Ощути магию настоящего наслаждения! старые проститутки москвы. Эскорт-леди ждут вашего звонка. Узнайте, что такое настоящее удовлетворение в компании кокеток из столицы.
Medicament information sheet. Brand names.
zoloft
Some what you want to know about drug. Get information now.
leukeran 300mg
Купить в интернет-магазине
инвентарь для занятий спортом по выгодным ценам в нашем магазине
Качество и удобство в каждой детали спорттоваров в нашем ассортименте
Спорттовары для начинающих и профессиональных спортсменов в нашем магазине
Низкокачественный инвентарь может стать препятствием во время тренировок – выбирайте качественные спорттовары в нашем магазине
Спорттовары только от ведущих производителей с гарантией качества
Сделайте свою тренировку более эффективной с помощью спорттоваров из нашего магазина
Разнообразие для самых популярных видов спорта в нашем магазине
Отличное качество спорттоваров по доступным ценам в нашем интернет-магазине
Простой поиск и спорттоваров в нашем магазине
Специальные предложения и скидки на спорттовары для занятий спортом только у нас
Прокачайте свои спортивные качества с помощью спорттоваров из нашего магазина
Большой выбор товаров для любого вида спорта в нашем магазине
Проверенный инвентарь для занятий спортом для женщин в нашем магазине
спорттоваров уже ждут вас в нашем магазине
Не пропускайте тренировки с помощью спорттоваров из нашего магазина
Выгодные условия покупки на аксессуары в нашем интернет-магазине – проверьте сами!
спорттоваров для любого вида спорта по самым низким ценам – только в нашем магазине
Спорттовары для амбициозных спортсменов и начинающих в нашем магазине
инвентарь для спорта https://sportivnyj-magazin.vn.ua/.
%%
Feel free to visit my site … купить диплом
Получение сертификата ИСО 9001 – завершающий этап процедуры сертификации, сертификат ISO 9001 без прохождения которой выдача документа априори невозможна.
cialis soft tabs in india
Получение сертификата ИСО 9001 – завершающий этап процедуры сертификации, сертификат соответствия смк исо 9001 без прохождения которой выдача документа априори невозможна.
%%
Feel free to visit my web site – приобрести диплом
Рекомендую лучшую БК 1вин
of the little brook that wound down the mountain
We talked with the Reputation House agency about the importance of employee reviews reputation house employee reviews
We talked with the Reputation House agency about the importance of employee reviews reputation house reviews
Какая великолепная фраза
но, увы… Поэтому двухнедельный запой, прилагающийся к пачкой именин, поставил крест на таргетированной накрутке, т.к банально не переставлял точечные накрутки по полнедели, в связи с чем все так уж и много плохо, но можно сказать себе, накрутка пф бесплатно но в современном мире оживает.
%%
Review my page :: купить диплом о среднем специальном
Medicines information leaflet. Brand names.
kamagra
Best what you want to know about drugs. Get information now.
%%
Also visit my blog: p143
urenrjrjkvnm
Meds prescribing information. Short-Term Effects.
lyrica
Some trends of medicament. Get information now.
%%
Look at my homepage; агентство нянь
%%
Visit my blog https://prodengi.forum.cool/viewtopic.php?id=1580
porn porn
Meds information leaflet. Drug Class.
cleocin
All trends of medicament. Read here.
urenrjrjkvnm
%%
Review my site – https://www.ratemeup.net/
cheap zofran 8mg
Это оригинальный сайт скачать майнкрафт
Ровным счетом ничего.
качество оказываемых услуг серверами и дополнениями не имеет возможности полностью предостеречь потребителя от http://www.ratemeup.net санкций.
where to buy cheap aurogra without insurance
купить справку из диспансера
%%
My site https://t.me/onewinapkdownload
Medication information sheet. Short-Term Effects.
tadacip otc
All trends of medicines. Get information here.
The Ceiva frame uses an embedded operating system known as PSOS. Afterward, it’s best to discover fewer system sluggish-downs, and really feel a little less like a hardware novice. The system might allocate an entire processor just to rendering hi-def graphics. This could also be the future of tv. Still, having a 3-D Tv means you may be prepared for the thrilling new features that is perhaps out there in the near future. There are such a lot of nice streaming reveals on websites like Hulu and Netflix that not having cable isn’t an enormous deal anymore so long as you may have a stable Internet connection. Next up, we’ll have a look at an excellent gadget for the beer lover. Here’s an excellent gadget reward thought for the man who actually, actually loves beer. If you’re in search of much more details about nice gadget gifts for men and different related topics, simply observe the links on the subsequent web page. If you choose to read on, the taste of anticipation may out of the blue go stale, the web page would possibly darken before your eyes and you will possibly find your attention wandering to other HowStuffWorks matters.
hi! I enjoyed your article, thank you very much!
allonezaimy.ru
LГҐna 15000 kr
Мы являемся как импортерами, так и дистрибьюторами медицинских изделий, тщательно выбираем поставщиков медицинское диагностическое оборудование купить и формируем ассортимент только из высокотехнологичного, современного оборудования.
Medicament prescribing information. What side effects?
motrin
Some information about pills. Get now.
These are: Baratheon, Lannister, Stark and Targaryen – names that collection followers might be all too accustomed to. The Targaryen free spins function gives you 18 free spins with a x2 multiplier – an ideal alternative if you love free spins. Choose Baratheon free spins for the chance to win huge. It is a bit like betting purple or black on roulette, and the odds of you being successful are 1:1. So, it is as much as you whether you want to risk your payline win for a 50% chance you may enhance it. One unique feature of the sport of Thrones slot is the choice players must gamble every win for the prospect to double it. Some Apple users have reported having trouble with the soundtrack, after we examined it on the most recent generation handsets the backing monitor got here through nice. Once you attend the positioning ensure that you’ve your booking reference prepared to indicate to the security guard to forestall delays to you and other clients. We suggest that households should not need more than 4 slots inside a 4-week period and advise customers to make every go to rely by saving waste when you’ve got house until you’ve a full load.
my page; https://pgslot7777.com/
https://true-bar.ru/
Мы являемся как импортерами, так и дистрибьюторами медицинских изделий, тщательно выбираем поставщиков медицинское оборудование в ярославле купить и формируем ассортимент только из высокотехнологичного, современного оборудования.
понравилось)))))))))
Только пользователи сможем снабдить активность и результативность продвижения. оно имеет возможность растянуться во времени, http://www.krutube.pro что окажет негативное воздействие на статистику.
https://myvisa.world/
care much for the shape), and then all the crowd were
https://redgate.kr/
12, 2007, the Give 1 Get 1 (G1G1) program allowed U.S. As of September 2007, about 7,000 laptops were being tested by youngsters around the globe. The OLPC Foundation goals to supply these laptops to hundreds of thousands of kids all through the creating world so as to enhance their training and their high quality of life. The XO laptop computer’s design emphasizes low cost, durable building that can survive quite a lot of climates and the rigors of the growing world. The 12 months 2009 showed us loads of other innovations, including low cost, efficient ways to trace your physical exercise and better methods to cool down after a run, too. As you move all through the day, Fitbit tracks how a lot bodily activity you performed. Because the Fitbit works finest for walking motion and isn’t waterproof, you cannot use it for actions resembling bicycling or swimming; nonetheless, you may enter these activities manually in your online profile. Should you plan to watch HD, you’d probably use an HDMI connection, although part, S-Video or VGA are additionally prospects, relying in your explicit system. More laptops must be accessible on the market in the future, and extra developing nations will be able to apply to join the G1G1 plan.
Confessus pro judicato habetur — прав. Сознавшийся считается осуждённым.
https://batmanapollo.ru
Thank you a bunch for sharing this with all people you really know what you are
speaking about! Bookmarked. Please also seek advice from my site =).
We can have a link alternate contract between us
arm out the window and one foot up the chim-ney and
Особенности букмекерских приложений для Android
yakaboo
Our mannequin permits the vendor to cancel at any time any reservation made earlier, by which case the holder of the reservation incurs a utility loss amounting to a fraction of her worth for the reservation and may also receive a cancellation charge from the vendor. The XO laptop computer allows kids, mother and father, grandparents and cousins to show one another. All you need is a few ingenuity and a laptop computer pc or smartphone. First, you may have to unwrap the motherboard and the microprocessor chip. With the help of cloud/edge computing infrastructure, we deploy the proposed network to work as an clever dialogue system for electrical customer service. To stop error accumulation brought on by modeling two subtasks independently, we suggest to jointly model each subtasks in an end-to-end neural community. We suggest and research a simple mannequin for auctioning such advert slot reservations in advance. An extensive computational study demonstrate the efficacy of the proposed method and gives insights in to the benefits of strategic time slot management. We suggest a 2-stage stochastic programming formulation for the design of a priori delivery routes and time slot assignments and a sample average approximation algorithm for its answer.
%%
Feel free to visit my web page; купить диплом
%%
my web-site … заказать диплом
Ad extra — До крайней степени.
https://batmanapollo.ru
Миссия компании заключается в сохранении здоровья и спасении жизни людей, благодаря своевременным поставкам качественного медицинское оборудование купить в рассрочку и грамотно подобранного медицинского оборудования.
low murmuring of countless insects, the soft
Ad fontes — К первоисточникам.
https://batmanapollo.ru
Confessus pro judicato habetur — прав. Сознавшийся считается осуждённым.
https://batmanapollo.ru
Prestito di 500 euro
yakaboo
%%
my webpage – купить диплом
Здесь можете купить ковер по очень выгодной цене.
might have shrunk to the size of a gnat.
фоп самойленко
Миссия компании заключается в сохранении здоровья и спасении жизни людей, благодаря своевременным поставкам качественного купить оборудование для производства медицинских перчаток и грамотно подобранного медицинского оборудования.
создание раскрутка и продвижение сайтов https://prodvizhenie-sajtov13.ru/
Миссия компании заключается в сохранении здоровья и спасении жизни людей, благодаря своевременным поставкам качественного купить медицинское оборудование в казани и грамотно подобранного медицинского оборудования.
Приближаются новогодние праздники и многие компании собираются проводить корпоративные мероприятия интернет-магазин подарков
Приближаются новогодние праздники и многие компании собираются проводить корпоративные мероприятия магазин подарков
It’s going to be end of mine day, but before ending I am reading this
fantastic piece of writing to improve my know-how.
Лидер по ремонту мебели в Минске. Недорогая перетяжка мягкой мебели в мастерской https://1-obivka-mebeli-vminske.ru/ – крупнейшая и лидирующая в Беларуси фабрика по перетяжке мебели с 17-летним опытом работы.
Usually I don’t learn article on blogs, however I would like to say that this write-up very compelled me to try
and do so! Your writing style has been surprised me.
Thank you, very great article.
Извиняюсь, но мне необходимо немного больше информации.
коль вы собираетесь закупать рекламу в чужих сообществах, http://oxak.ru/goto/aHR0cHM6Ly93d3cuYmVmYWN0b3IucnUv попросите владельцев групп поделиться скриншотами. чаще всего этот раздел доступен лишь администраторам.
ремонт квартиры бровары
I recently noticed your website back i are principally looking be means of which on a common basis. You’ve got a loads of intelligence at this site so i in actuality like your look to the web a tad too. Keep up the finery entertainment results!
Депозитарное хранение архивных документов. хранение архивных документов в архиве, музее, депозитарное хранение документов библиотеке на условиях, определяемых соглашением (договором).
Gama Casino – популярное онлайн-казино, предлагающее своим клиентам богатый выбор игровых автоматов гама промокод
Депозитарное хранение архивных документов. хранение архивных документов в архиве, музее, https://depozitarnoe-hranenie-msk.ru/ библиотеке на условиях, определяемых соглашением (договором).
Gama Casino – популярное онлайн-казино, предлагающее своим клиентам богатый выбор игровых автоматов гама казино официальный сайт зеркало
Porn Videos
фоп самойленко
If you don’t just like the slot machine approach, you possibly can browse restaurants by varied classifications or view a list of Urbanspoon listings near your present location. Does location have an effect on your Tv channel choice? And then in June, leaving the home for the first time in four months, I assumed, why did I mock myself a lot? The wild Dracula multiplies line winnings by three – every time it seems, the 3x multiplier is triggered for every bat or Dracula that is in view on the paylines. The 4x multiplier gets triggered whenever you correctly guess the next go well with. The jackpot is price 12,500 coins and gets triggered throughout the utmost wager spins whenever you hit 5 Amulets on any of the 243 paylines which have been lively. The bonus round gets triggered on hitting a minimal of three scatter symbols. In addition to the base game’s repeat pay function, the free game bonus rounds also have the triple repeat pay function for you to sink your teeth into. Lucky Count options a fairly generous number of bonus rounds and sports an impressive repeat pay pattern.
Hello, i think that i saw you visited my site thus i came to “return the favor”.I am
trying to find things to improve my web site!I suppose its
ok to use a few of your ideas!!
Рекомендую гвозди для пистолета toua для газовых монтажных пистолетов TOUA, PAULT, NAILTASK и других..
kliknД›te na tento web
LГҐn 50000
This article will help the internet people for building up new web site or even a weblog from start
to end.
%%
Also visit my blog post https://portalodia.com/noticias/mundo/jogos-de-cassino-online-uma-imersao-no-mundo-virtual-401106.html
sex videos
ремонт бойлера бровары
you are actually a just right webmaster. The web site loading pace is amazing. It seems that you are doing any distinctive trick. Furthermore, The contents are masterwork. you’ve performed a wonderful activity on this subject!
%%
Check out my website … приобрести диплом
New porn on the site
New porn on the site
Apple has deployed out-of-date terminology as a result of the “3.0” bus ought to now be called “3.2 Gen 1” (as much as 5 Gbps) and the “3.1” bus “3.2 Gen 2” (up to 10 Gbps). Developer Max Clark has now formally introduced Flock of Dogs, a 1 – 8 participant online / native co-op experience and I’m slightly bit in love with the premise and elegance. No, you might not carry your crappy old Pontiac Grand Am to the native photo voltaic facility and park it of their entrance lawn as a favor. It’s crowdfunding on Kickstarter with a purpose of $10,000 to hit by May 14, and with nearly $5K already pledged it ought to easily get funded. To make it as easy as attainable to get going with mates, it can provide up a special inbuilt “Friend Slot”, to allow another person to hitch you through your hosted sport. Those critiques – and the way in which corporations tackle them – could make or break an enterprise. There are additionally options to make a few of the brand new fations your allies, and take on the AI together. There are two forms of shaders: pixel shaders and vertex shaders. Vertex shaders work by manipulating an object’s place in 3-D space.
If you do not like the slot machine method, you’ll be able to browse eating places by numerous classifications or view an inventory of Urbanspoon listings near your present location. Does location have an effect on your Tv channel selection? And then in June, leaving the house for the primary time in four months, I thought, why did I mock myself a lot? The wild Dracula multiplies line winnings by three – every time it appears, the 3x multiplier is triggered for each bat or Dracula that’s in view on the paylines. The 4x multiplier gets triggered while you accurately guess the subsequent suit. The jackpot is worth 12,500 coins and gets triggered throughout the utmost bet spins once you hit five Amulets on any of the 243 paylines which have been energetic. The bonus spherical gets triggered on hitting a minimum of three scatter symbols. In addition to the base sport’s repeat pay feature, the free recreation bonus rounds even have the triple repeat pay function so that you can sink your teeth into. Lucky Count options a quite generous number of bonus rounds and sports activities a powerful repeat pay sample.
%%
Take a look at my blog – http://emotional.ro/?URL=https://interactivecasinos.org/casinos/21
Здесь клиенты могут подобрать наиболее подходящие варианты для прогнозирования результативности матчей 1вин
«АгроМаркет» – профессиональный магазин для садоводов Более 20 лет на рынке agromarket в наличии семена овощей, садовый инвентарь, удобрения.
Здесь клиенты могут подобрать наиболее подходящие варианты для прогнозирования результативности матчей 1 win partner
Certainly with your thoughts here and that i weakness your blog! I’ve bookmarked it making reliable that I can hit back & interpret more in the foreseeable future.
Hiya, I’m really glad I have found this information. Nowadays bloggers
publish only about gossips and net and this is actually annoying.
A good web site with exciting content, this is what I need.
Thank you for keeping this web-site, I will be visiting it.
Do you do newsletters? Cant find it.
my webpage … bad alternator sound
tilleggsressurser
dragon money вывод
ВАУ….=)
в связи с этим прежде, чем начать накручивать, поразмышляйте на тему, https://towyouth.newhaven.edu/summer-is-coming/ зачем же рисковать. сначала необходимо придерживаться профессионального тона также подхода, для того, чтоб создать надежное впечатление о своей активности и аккаунте.
To connect and use a virtual number https://cse.google.com.ng/url?q=https://didvirtualnumbers.com/rent-virtual-number/
To connect and use a virtual number https://maps.google.md/url?q=https://didvirtualnumbers.com/rent-virtual-number/
Serial numbers rarely affect a bill’s value unless they’re special in some way – e.g. low (00000006), repeating (12121212), symmetric (12344321), etc. Far more
Read more
US Banknotes
How much is a pound of US 100 dollar bills worth?
Asked by Wiki User
Most U.S. currency weighs exactly one gram per note (bill). There are four hundred fifty-four grams (rounded to the nearest whole number) in one pound. Therefor
Read more
US Banknotes
What is the value of a 1789 US two dollar bill?
Asked by Wiki User
The first federally-issued $2 bills were printed in 1862. You may have a privately-issued bill, a replica, a fantasy item, or something completely unrelated. Pl
Read more
US Banknotes
Is the 2 dollars bill with a paw print on it worth anything and is it real?
Asked by Wiki User
IS A 2 DOLLAR BILL WITH A PAW PRINT ON IT WORTH ANYTHING?
%%
Feel free to surf to my web site; Переезд офиса в Москве
Восстановление помещения — наша специализация. Реализация строительных работ в сфере жилья. Мы предлагаем модернизацию жилого пространства с гарантированным качеством.
ремонт квартир в броварах
porno
Продажа напольных покрытий https://tarkett-parkett.ru/ с доставкой по России.
Платформа для поиска проверенных проституток в Москве https://msk-intimcity.nl/
играть в казино
Great web site. Plenty of helpful information here.
I’m sending it to a few pals ans also sharing in delicious.
And certainly, thank you in your sweat!
Porn free
Игрушки, используемые в качестве украшений для елки или тематического декора помещений, отказное письмо на елочные игрушки не являются объектом технического регулирования ни одного из действующих регламентов ТС(ЕАЭС).
You actually reported it wonderfully!
Feel free to visit my site https://sublimememories.wiki/index.php/Fortniteskins.com
Игрушки, используемые в качестве украшений для елки или тематического декора помещений, цена оформления отказного письма на елочные игрушки не являются объектом технического регулирования ни одного из действующих регламентов ТС(ЕАЭС).
эва
%%
My web-site :: вавада
I do not even know how I ended up here, but I thought this post was great. I do not know who you are but definitely you’re going to a famous blogger if you aren’t already 😉 Cheers!
In essence, it replaces the looks of an object with a extra detailed image as you move closer to the object in the game. Fans of Bungie’s “Halo” recreation collection can purchase the “Halo 3” limited version Xbox 360, which comes in “Spartan inexperienced and gold” and options a matching controller. And regardless of being what CNet calls a “minimalist gadget,” the Polaroid Tablet still has some pretty nifty hardware features you’d count on from a extra pricey pill by Samsung or Asus, and it comes with Google’s new, feature-rich Android Ice Cream Sandwich working system. When Just Dance III comes out in late 2011, it would also be launched for Xbox’s Kinect in addition to the Wii system, which suggests dancers will not even need to carry a remote to shake their groove thing. TVii may prove to be an especially powerful service — the GamePad’s built-in display screen and IR blaster make it a probably perfect universal remote — but the Wii U’s launch has shown Nintendo struggling with the calls for of designing an HD console. Nintendo labored with wireless company Broadcom to develop a WiFi know-how that works from as much as 26 toes (7.9 meters) away and delivers extremely low-latency video.
Porn Kino
Максимальные выигрыши с 1xbet
1xbet download ios https://www.1xbetappdownloadkedsdf.com/.
Hello, constantly i used to check blog posts here in the early hours in the daylight, because i enjoy to learn more and more.
Appreciate the recommendation. Let me try it out.
cordarone prescribing information
%%
Feel free to surf to my homepage … https://greenovature.org/index.php/2022/10/10/mr-edwards-joins-youth-climate-council/
%%
My page … https://tu-electroseti.ru/
%%
Here is my webpage; https://tratatur.ru/price/taxi-kuchugury-gelendzhik
Porn HD
%%
Look into my site :: https://tu-elektrichestvo.su/
eva
buy lisinopril hctz no prescription
%%
Here is my homepage; https://gametalkz.com/a/the-nun-2-end-credits-scene-breakdown-how/19237
%%
My web blog :: такси Анапа Кучугуры
%%
my blog; https://narodnaviyna.org.ua/novosti/2023/10/28/2012774511-tkani-optom-kupit-v-moskve-ot-proizvoditelya-so-sklada-mogotex.htm
Hi there! This blog post couldn’t be written much better! Looking through this article reminds me
of my previous roommate! He continually kept preaching about this.
I’ll forward this information to him. Fairly certain he’s going to have a
very good read. Thank you for sharing!
Gargantuan post however , I was unsatisfactory to separate if you could pen a litte more on this subject? I’d be totally grateful if you could intricate a itty-bitty bit further. Adore you!
can i purchase aurogra tablets
You can buy this pouches Pablo Exclusive Bubblegum for best price.
I recommend this best pouches Pablo Ice Cold XXL
This is very interesting, You’re a very skilled blogger.
I have joined your feed and look forward to seeking more of your fantastic post.
Also, I’ve shared your site in my social networks!
%%
Also visit my site – казино kent
%%
Here is my web site https://botto.ai/ru/
prestamo 3000 euros
Покупайте высококачественный ламинат Quick-Step в нашем интернет-магазине https://quick-step-shop.ru/ . Широкий ассортимент коллекций, разнообразные оттенки и фактуры. Прочный, стильный и легкий в уходе – идеальный выбор для любого помещения. Доставка по всей стране и гарантированно надежное качество обслуживания.
Отказное письмо на свечи ручной работы https://telegra.ph/Sertifikaciya-svechej-nuzhen-li-sertifikat-ili-dostatochno-otkaznogo-pisma-11-20
Отказное письмо на свечи ручной работы отказное письмо на свечи
%%
Look at my web blog: https://arcayanayasociados.com/img_20220321_091731_891/
dear Di-nah! Shall I ev-er see you an-y more?” And
%%
my web site :: https://botto.ai/ru/сlients/
buy lisinopril without a perscription
here and there she saw maps hung on pegs. She took
%%
Here is my webpage: https://itemsport.com
a ta-ble near the wall, and on it, as she had hoped,
Wow, this piece of writing is fastidious, my sister is analyzing such things, so I am going to inform her.
Medicament information. Cautions.
maxalt
Some about medicines. Get here.
urenrjrjkvnm
%%
ปัจจุบันต้องยอมรับว่าโลกของ เรียกว่าโลกของระบบออนไลน์ sa เล่นง่าย น่าเชื่อถือ
เพราะแทบทุกอย่างมีให้บริการบนโลกออนไลน์ evoplay ระบบที่มีความเสถียร สนุกจุใจทั้งวันทั้งคืน
เพื่อตอบโจทย์ความอำนวยสะดวกของคนทุกประเภทที่เล่น SLOTPGAUTO ระบบออกแบบให้เข้าใจง่ายเพื่อรองรับผู้เล่นทุกรูปแบบที่หลากหลาย
รวมถึงเว็บเดิมพันที่เปิดบริการให้เล่นอย่างหลากหลาย สล็อตเว็บตรง
แต่เรามีเว็บ ทดลองเล่นสล็อตpg สำหรับผู้ที่ชื่นชอบในการเดิมพัน ที่เล่นง่ายมั่นคงปลอดภัย
และเป็นที่ยอมรับอย่างสูง เพราะเล่นง่าย น่าเชื่อถือ pp slot สามารถได้ตลอดการเดิมพัน ทั้งยังเปิดบริการให้เข้าเล่นได้ 24 ชั่วโมง
ทั้งผู้ที่ชื่นชอบการแทงเลข hihuay.com หวยออนไลน์ เช่นหวยรัฐบาล หวยหุ้น หรือหวยยี่กี
และมีหวยปิงปองที่มีเฉพาะของเว็บ ltobet.comเข้าสู่ระบบ เท่านั้น
และยังมีค่ายเกมออนไลน์ชื่อดังที่น่าสนใจ มีเกมมากกว่า100เกม แถมมีอัตราจ่ายสูง จ่ายจริง รวมถึงคาสิโนออนไลน์ yehyehคาสิโน ที่ให้คุณเล่นได้ทุกที่
เว็บหวย แท่งหวยออนไลน์ ออนไลน์ จ่ายจริง จริงใจไม่ไก่กา เข้ามาสมัครสามชิกกับเรารับรองไม่ผิดหวัง สมัครง่ายๆผ่านโทรศัพท์มือถือได้ มีโปรโมชั่นเอาใจลูกค้ามากมาย เจ้าหน้าที่ตอบเร็วสุด บริการตลอด 24 ชั่วโมง แทงได้ไม่มีอั้น ไม่มีคืนโพย
มีอัตราจ่ายสูงกับ หวยสด ไม่ว่าจะหลักหมื่น หลักแสน เราก็พร้อมจ่าย ไม่มีเบี้ยว ไม่โกงอย่างแน่นอน เพราะเราเป็นเว็บใหญ่ มีมาตรฐาน ฐานการเงินมั่นคง ระบบเสถียร ทุกการใช้งาน ลื่นไหล ไม่มีค้าง ไม่มีสะดุด จนฉุดไม่อยู่ ถูกใจคอหวยอย่างแน่นอน
เพราะเรามีการบริการที่เป็นเลิศ เว็บไชต์สวยงาม ขั้นตอนการเข้า แทงหวย ก็ไม่ยุ่งซับซ้อน ฝาก-ถอน รวดเร็ว ไม่ต้องรอคอยนานให้เมื่อย รีบสมัครเล่นเว็บ หวยฮานอย กันเข้ามาเลย เราพร้อมบริการคุณ
Hey there, You’ve done an excellent job. I’ll definitely
digg it and personally suggest to my friends.
I’m confident they will be benefited from this web site.
Medicament information. Drug Class.
how to buy cialis soft
All information about medication. Get now.
Cheap Gucci Handbags Is usually blogengine much sport than wp for reasons unknown? Should be which is turning revealed to be popluar today.
a fall as this, I shall not m
Исследуйте широкий выбор высококачественных ламинатных покрытий от Tarkett. Наш интернет-магазин https://tarkett54.ru/ предлагает уникальные коллекции с разнообразными оттенками, текстурами и фактурами. Ламинат Tarkett – это идеальное сочетание элегантного дизайна и надежности. Создайте стильный и уютный интерьер с ламинатом, который прослужит вам долгие годы. Легкость укладки, прочность и легкость в уходе делают ламинат Tarkett отличным решением для любого помещения. Покупайте ламинат Tarkett в нашем интернет-магазине и преобразите свой дом сегодня!
Исследуйте уникальные возможности пробкового покрытия CorkStyle. Наш интернет-магазин https://corkstyle73.ru/ предлагает широкий выбор коллекций, включая различные стили, текстуры и цветовые варианты. Пробковое покрытие CorkStyle является экологически чистым, долговечным и приятным на ощупь решением для вашего пола. Наслаждайтесь комфортом, шумоизоляцией и термоизоляцией, которые предлагает пробковое покрытие. Восхитительный дизайн и превосходное качество ждут вас в нашем магазине. Оптимизируйте ваш интерьер с CorkStyle уже сегодня!
myambutol
I’m sure you’d like cats if you could see her. She is
Lainaa 90000 euroa
judged by his face she would have called him a fish)
Artificiosa natura — Творческая природа.
https://batmanapollo.ru
So she called it in a soft, kind voice, “Mouse dear! Do
Foot-man went on, “if we were not both on the same
to be popular on youtube you need to buy youtube views on the best site views
Наша компания дает вам возможность купить необходимое оборудование в лизинг от иностранных и отечественных производителей, как новое, так и б/у лизинг оборудование для производства
to be popular on youtube you need to buy youtube views on the best site 1kviews
Наша компания дает вам возможность купить необходимое оборудование в лизинг от иностранных и отечественных производителей, как новое, так и б/у лизинг бу оборудования для юридических лиц
at every puff. And although his face was all criss-crossed
%%
my website :: https://tratatur.ru/price/taxi-anapa-aderbievka
%%
Visit my web blog … http://l-avt.ru/support/dialog/?PAGE_NAME=profile_view&UID=57980
%%
my page :: такси анапа приморско-ахтарск
been all round and tried each one, she found they
МК Лизинг входит в состав международного холдинга Mikro Kapital Group, компании которого оказывают помощь малому и среднему бизнесу в 14 странах мира лизинг недвижимости для юридических
МК Лизинг входит в состав международного холдинга Mikro Kapital Group, компании которого оказывают помощь малому и среднему бизнесу в 14 странах мира лизинг оборудования для ип
%%
Also visit my web blog https://buronahodok.by/buro-580858.html
prednisolone usa
did not fit one of them. But when she went round
brillx официальный сайт играть онлайн
https://brillx-kazino.com
Добро пожаловать в захватывающий мир азарта и возможностей на официальном сайте казино Brillx в 2023 году! Если вы ищете источник невероятной развлекательности, где можно играть онлайн бесплатно или за деньги в захватывающие игровые аппараты, то ваш поиск завершается здесь.Brillx Казино — это место, где сливаются воедино элегантность и бесконечные возможности. Необычная комбинация азартных игр и роскошной атмосферы позволит вам окунуться в мир бриллиантового веселья. Наше бриллиантовое казино уверенно входит в число лидеров азартной индустрии, и в этом году мы готовы порадовать вас еще большим разнообразием игр и выигрышей.
dostinex 50mcg
Верный ответ
посредством данных единиц – достаточно получить экологичный газон, яркий цветник, http://tastys-food.ru/profile.php?u=yfule и обустроить альпинарий или каменистый сад.
https://vk.com/uslugi-223156582?screen=group&w=product-223156582_8515686%2Fquery
Bene valete — Будьте здоровы.
https://batmanapollo.ru
Без переплаты
Прямо сейчас можно трубы из полиэтилена в Москве
труба полиэтиленовая https://www.truba-pe.pp.ua/.
https://vk.com/uslugi-223156644?screen=group&w=product-223156644_8867142%2Fquery
мдаааааааа
а к примеру машины мидл-класса, https://www.instagram.com/auto.lux.concept/ однако с маленькими моторами становятся интересными. в стране же при похожих параметрах средняя цена “Кодьяка” 2018 года держится на уровне 2,2-два с половиной млн рублей.
купить бетон
Я извиняюсь, но, по-моему, Вы не правы. Могу отстоять свою позицию. Пишите мне в PM, пообщаемся.
в каждой анкете эскорт-модели вы сможете отыскать указанный для связи телефон менеджера. в первую очередь девушки стремятся, http://bizon15.ru/index.php?subaction=userinfo&user=ijati чтобы мужчинам было приятно и комфортно во время эскорт-обслуживания.
Hi, this weekend is good designed for me, as this point in time i am reading this fantastic educational piece of writing here at my home. dark web sites https://darknetmarketlist.com
credito 350 euros
https://samye-luchshie-prostitutki-moskvy.top
marked ‘poi-son,’ it is sure to make you sick. This had
Продолжительные поиски могут быть типичным самоотказом. Послушай старших, лучше сходить к неидеальному психологу чем так и остаться на этапе поисков.Психолог онлайн.
Утомительные оценивания с огромной вероятностью обычным самоотказом. Выслушай мудрых, лучше сходить к доступному психологу чем проникнуться своим фантазиям.Психолог консультация.
Купить недорого в Москве
трубы для воды для дома и промышленности
Гибкие для различных нужд
Канализационные трубы из качественных материалов по доступной цене
трубопроводы для систем вентиляции и кондиционирования
Полиэтиленовые для долговечного использования
Трубы для водоснабжения и канализации от ведущих производителей
трубопроводы высокого качества – советы экспертов
трубы из стеклопластика
трубы для горячей воды для комфортного душа
трубы для системы полива на садовом участке
Трубы для монтажа сантехники – широкий ассортимент на сайте нашей компании
Надежные для газопровода по выгодной цене
трубопроводы для системы отопления и не заморачивайтесь с ремонтом
Легкие в монтаже из полипропилена
Кислотоустойчивые для долговечного использования
Закажите для газопровода в нашей компании – доставка по всей России
трубопроводы для системы отопления по доступной цене
Безопасные из нержавеющей стали
трубы для системы вентиляции и кондиционирования – гарантия качества
Трубы для системы отопления из керамического материала – высокая стойкость к внешним воздействиям
труба пе 100 http://polietilenovye-truby.pp.ua/.
Утомительные оценивания всем понятно обычным саботированием. Надо как надо, лучше сходить к первому встречному психологу чем не сходить.Психолог тут.
Долгие оценивания вероятно самым обычным нежеланием. Поверь наслово , лучше сходить к стандарнтному психологу чем проникнуться своим фантазиям.Психолог консультация.
Tiêu đề: “B52 Club – Trải nghiệm Game Đánh Bài Trực Tuyến Tuyệt Vời”
B52 Club là một cổng game phổ biến trong cộng đồng trực tuyến, đưa người chơi vào thế giới hấp dẫn với nhiều yếu tố quan trọng đã giúp trò chơi trở nên nổi tiếng và thu hút đông đảo người tham gia.
1. Bảo mật và An toàn
B52 Club đặt sự bảo mật và an toàn lên hàng đầu. Trang web đảm bảo bảo vệ thông tin người dùng, tiền tệ và dữ liệu cá nhân bằng cách sử dụng biện pháp bảo mật mạnh mẽ. Chứng chỉ SSL đảm bảo việc mã hóa thông tin, cùng với việc được cấp phép bởi các tổ chức uy tín, tạo nên một môi trường chơi game đáng tin cậy.
2. Đa dạng về Trò chơi
B52 Play nổi tiếng với sự đa dạng trong danh mục trò chơi. Người chơi có thể thưởng thức nhiều trò chơi đánh bài phổ biến như baccarat, blackjack, poker, và nhiều trò chơi đánh bài cá nhân khác. Điều này tạo ra sự đa dạng và hứng thú cho mọi người chơi.
3. Hỗ trợ Khách hàng Chuyên Nghiệp
B52 Club tự hào với đội ngũ hỗ trợ khách hàng chuyên nghiệp, tận tâm và hiệu quả. Người chơi có thể liên hệ thông qua các kênh như chat trực tuyến, email, điện thoại, hoặc mạng xã hội. Vấn đề kỹ thuật, tài khoản hay bất kỳ thắc mắc nào đều được giải quyết nhanh chóng.
4. Phương Thức Thanh Toán An Toàn
B52 Club cung cấp nhiều phương thức thanh toán để đảm bảo người chơi có thể dễ dàng nạp và rút tiền một cách an toàn và thuận tiện. Quy trình thanh toán được thiết kế để mang lại trải nghiệm đơn giản và hiệu quả cho người chơi.
5. Chính Sách Thưởng và Ưu Đãi Hấp Dẫn
Khi đánh giá một cổng game B52, chính sách thưởng và ưu đãi luôn được chú ý. B52 Club không chỉ mang đến những chính sách thưởng hấp dẫn mà còn cam kết đối xử công bằng và minh bạch đối với người chơi. Điều này giúp thu hút và giữ chân người chơi trên thương trường game đánh bài trực tuyến.
Hướng Dẫn Tải và Cài Đặt
Để tham gia vào B52 Club, người chơi có thể tải file APK cho hệ điều hành Android hoặc iOS theo hướng dẫn chi tiết trên trang web. Quy trình đơn giản và thuận tiện giúp người chơi nhanh chóng trải nghiệm trò chơi.
Với những ưu điểm vượt trội như vậy, B52 Club không chỉ là nơi giải trí tuyệt vời mà còn là điểm đến lý tưởng cho những người yêu thích thách thức và may mắn.
Эксклюзивный промокод от БК Мелбет: «LEGALBET» — вводите при регистрации, чтобы увеличить сумму первого депозита в Melbet промокод melbet при регистрации на сегодня
ISO 45001:2018 — это новый международный стандарт по охране труда, введенный вместо OHSAS 18001:2007. Соответственно, в России тоже появился новый ГОСТ по охране труда — стандарт ГОСТ Р ИСО 45001-2020, идентичный международному Что такое сертификат исо 45001 Он утвержден приказом Росстандарта № 581-ст от 28.08.2020 и вступил в силу с 01.04.2021. Сертификат соответствия системе менеджмента безопасности труда и охраны здоровья удостоверяет, что система менеджмента, принятая в организации, отвечает требованиям стандарта ГОСТ Р ИСО 45001-2020.
Продолжительные оценивания вероятно типичным самооправданием. Не находи самооправданий, лучше сходить к не лучшему психологу чем проникнуться своим фантазиям.Психолог здесь.
Эксклюзивный промокод от БК Мелбет: «LEGALBET» — вводите при регистрации, чтобы увеличить сумму первого депозита в Melbet промокод на мелбет на сегодня
ISO 45001:2018 — это новый международный стандарт по охране труда, введенный вместо OHSAS 18001:2007. Соответственно, в России тоже появился новый ГОСТ по охране труда — стандарт ГОСТ Р ИСО 45001-2020, идентичный международному стоимость сертификата iso 45001 Он утвержден приказом Росстандарта № 581-ст от 28.08.2020 и вступил в силу с 01.04.2021. Сертификат соответствия системе менеджмента безопасности труда и охраны здоровья удостоверяет, что система менеджмента, принятая в организации, отвечает требованиям стандарта ГОСТ Р ИСО 45001-2020.
%%
Look into my page :: https://www.labuncle.com/blog/ct-scan-labuncle/
Сомнительные выбор 100% шаблонным самооправданием. Не надо так, лучше сходить к плохому психологу чем так и остаться на этапе поисков.Психолог онлайн.
Продолжительные поиски вероятно обычным нежеланием. Послушай старших, лучше сходить к неидеальному психологу чем не сходить.Психолог сейчас.
Продолжительные поиски почти наверняка обычным саботированием. Послушай старших, лучше сходить к не лучшему психологу чем не сделать выбор.Психолог сейчас.
мягкая мебель для офиса кресла https://ofisstil11.ru/
Долгие оценивания 100% унылым самоотказом. Поверь наслово , лучше сходить к стандарнтному психологу чем так и не сделать выбор.Психолог консультация.
Продолжительные выбор 100% тухлым нежеланием. Не находи самооправданий, лучше сходить к не лучшему психологу чем так и не сделать выбор.Психолог здесь.
Сомнительные оценивания как известно бытовым саботированием. Надо как надо, лучше сходить к плохому психологу чем так и остаться на этапе поисков.Психолог тут.
Утомительные поиски как известно унылым самоотказом. Сделай без оправданий, лучше сходить к неидеальному психологу чем проникнуться своим фантазиям.Психолог сейчас.
Получение сертификата ИСО 9001 – завершающий этап процедуры сертификации, без прохождения которой выдача документа априори невозможна. Преимуществом будет, если орган, выполняющий проверку, имеет соответствующую аккредитацию стоимость получения сертификата ИСО 9001 Сертификат соответствия СМК требованиям ИСО 9001 – документ, который выдается по результатам экспертной проверки и подтверждает, что система менеджмента качества (СМК) организации соответствует международному стандарту ISO 9001 «Системы менеджмента качества. Требования» либо его национальному аналогу ГОСТ Р ИСО 9001 и своевременно совершенствуется.
colchicine 3mg
A printable calendar is great for keeping the family organized — 2024 printable calendar one page it’s customizable, encourages communication, and helps with planning, all without needing to rely too much on technology.
Сомнительные поиски всем понятно унылым самооправданием. Выслушай мудрых, лучше сходить к неидеальному психологу чем так и остаться на этапе поисков.Психолог здесь.
A printable calendar is great for keeping the family organized — printable calendar december 2024 it’s customizable, encourages communication, and helps with planning, all without needing to rely too much on technology.
Продажа напольных покрытий https://parketnik-penza.ru/ с доставкой по России.
Интернет-магазин напольных покрытий https://avk-parket.ru/ с доставкой по всей России.
Сомнительные поиски вероятно самым обычным нежеланием. Не надо так, лучше сходить к обычному психологу чем проникнуться своим фантазиям.Психолог консультация.
Benevolentiae captande causa — Для снискания благоволения.
http://batmanapollo.ru
Какая хорошая фраза
Для наглядной демонстрации возможностей программы https://smkn2bukittinggi.sch.id/forum/ есть небольшое видео. Чтобы контролировать его рост, в нём могут присутствовать ролики только постоянных пользователей.
ch.er.ep.a.n.ovr.e.nat235.0.7.9@gmail.com
лучшие авто
Рекомендую надежный и быстрый обменник Биткоин на Сбербанк для всех жителей РФ.
Vous pouvez acheter ces sachets Pablo Exclusive Mocca pour un bon prix.
Je recommande cette très belle pochette Pablo Exclusive Cappuccino
%%
Also visit my homepage; https://simli.ru/user/kevotaavxu
vidéos porno
valtrex
urenrjrjkvnm
Казино Гама представлен огромный выбор игр. Здесь вы найдете все самые популярные игры, начиная от классических слотов до увлекательных настольных игр и видеопокера. регистрация Гама Казино сотрудничает с ведущими разработчиками игрового софта, поэтому качество игр и графика на высшем уровне.
Наши квалифицированные специалисты окажут вам профессиональную поддержку на всех этапах получения сертификата ISO 9001 https://certificatiso9001.blogspot.com/ Они оперативно и качественно исполнят каждое сертификационное мероприятие.
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is
added I get four e-mails with the same comment. Is there any way you
can remove me from that service? Thanks a lot!
Казино Гама представлен огромный выбор игр. Здесь вы найдете все самые популярные игры, начиная от классических слотов до увлекательных настольных игр и видеопокера. Гама Казино сотрудничает с ведущими разработчиками игрового софта, поэтому качество игр и графика на высшем уровне.
вааааааа не то что улыбнуло оборвало полностью супер просто давай исчо
Недаром всякие megogo и прочие безжалостно идут в сервисах автосерфинга. да и еще один вариант для https://trippyflipchocolatebars.com/product/just-a-tickle/ – борьба с врагами.
%%
Also visit my webpage – http://lubimoy.com.ua/2022/01/samye-populyarnye-dzhinsy-2022-goda/
цвет с доставкой саратов
tell you half of them. And it kills all the rats, and m—oh
При регистрации на сайте 1xBet вы можете воспользоваться только одним промокодом, который является действительным. Используя этот промокод, вы получите бонус до 32500 рублей. промокоды в 1хбет Важно отметить, что все остальные промокоды не являются действительными и не предоставляют такого же бонуса.
A promotional code is a code offered by retailers to customers who can use it to receive a discounted price when buying products online https://gamma.app/docs/-1xBet-2024—260000–03qymb1wunjq1uy?mode=doc
При регистрации на сайте 1xBet вы можете воспользоваться только одним промокодом, который является действительным. Используя этот промокод, вы получите бонус до 32500 рублей. промокоды на 1хбет Важно отметить, что все остальные промокоды не являются действительными и не предоставляют такого же бонуса.
Vous pouvez acheter ces sachets Pablo Exclusive Kiwi pour un bon prix.
Je recommande cette très belle pochette Pablo Exclusive Passion Fruit
https://s1.moresliv.biz/
Age, libertate decembri utere — Ну же, пользуйся свободой декабря
http://batmanapollo.ru
Ремонт телефонов, ноутбуков, планшетов и другой техники https://remont-telefonov-moskva.ru/
When it comes to selecting an escort, it’s important to consider your specific needs and preferences. Whether you’re looking for a companion for a social event, a romantic evening, or simply some companionship, there are escorts in Lahore who specialize in a variety of services. Take the time to communicate your desires and expectations with the agency, so they can match you with an escort who meets your criteria.
%%
Here is my page … https://simulatorsmods.com/user/branorpcah
Извините за то, что вмешиваюсь… Мне знакома эта ситуация. Давайте обсудим.
Стартуємо 30 січня! давайте разом створимо успішне фінансове майбутнє особисто і http://www.atelier-reliurebarennes.com/album-photos/nos-produits/dsc-1003-001.html країни! ? однокімнатну квартиру, і земля.
best porn xxx
Although Mostbet operates under an official international license, the official website of the bookmaker is sometimes blocked by Azerbaijani Internet providers https://telegra.ph/mostbet-az%C9%99rbaycan-11-28
Откройте для себя новую эру в Мире Свежих Соков с Hurom от ВсеСоки!
Почувствуйте вкус настоящего здоровья с каждым глотком! Соковыжималки Hurom – это не просто техника, это ваш верный спутник в стремлении к здоровому образу жизни. Представляем вам ультрасовременными соковыжималками от официального дилера ВсеСоки в России, которые покажут новые возможности вкуса и питания.
Технология Slow Squeeze: Оставьте позади обычные соковыжималки. Технология медленного отжима Hurom сохраняет все полезные витамины, минералы и ферменты, делая каждый сок не только невероятно вкусным, но и максимально полезным.
Многофункциональность: Не ограничивайтесь соками! Hurom легко справляется с ореховым молоком, смузи, детским питанием и даже мороженым. Все, что необходимо для разнообразного питания вашей семьи.
Инновационный Дизайн и Простота в Использовании: Стильный внешний вид соковыжималок Hurom прекрасно впишется в интерьер вашей кухни, а их интуитивно понятное управление и легкая очистка сделают процесс приготовления соков легким и удобным.
Экологичность и Долговечность: Наша забота о планете! Соковыжималки Hurom изготовлены из премиальных, экологически чистых материалов и служат вам годами.
Поддержка и Гарантия от ВсеСоки: Обращаясь к официальному дилеру, вы получаете гарантированное качество, профессиональную консультацию и сервисное обслуживание.
Специальное Предложение: Используйте уникальную возможность и подарки при покупке соковыжималок Hurom у официального дилера ВсеСоки!
Заказывайте Сейчас: Переходите на наш сайт [всесоки.ру] и выбирайте свою идеальную соковыжималку Hurom. Начните свой путь к здоровью и энергии уже сегодня!
Review my webpage :: https://H-100.ru/collection/konstar
Вы оказались правы. Благодарю за совет, как я могу Вас отблагодарить?
Series. Multiple 1win express trains https://smpn3mranggen.sch.id/forum/ the same rate. you can win if you win not all events.
I got this site from my friend who told me regarding this website and at the moment this time I am browsing this web site
and reading very informative posts at this time.
Awesome material Cheers.
atarax generika bestellen
calendar july 2024
%%
Feel free to surf to my site – Купить мебель в Крыму
c.her.ep.a.no.v.ren.at.235.07.9@gmail.com
Actum atque tractatum — Сделано и обсуждено.
http://batmanapollo.ru
Abstractum pro concreto — Общее вместо частного.
http://batmanapollo.ru
Amant alterna Camenae — Музам приятны перемежающиеся песни.
http://batmanapollo.ru
%%
Prestito 16 mila euro
пройду мимо…
Mining is a opportunity to release new units of http://189.1.162.238/SGS/financeiro/includes/php_info.php?a%5B%5D=%3Ca+href%3Dhttps%3A%2F%2Fwww.sheepy.com%3Ehttps%3A%2F%2Fwww.sheepy.com%3C%2Fa%3E%3Cmeta+http-equiv%3Drefresh+content%3D0%3Burl%3Dhttps%3A%2F%2Fwww.sheepy.com+%2F%3E into sea, as a rule , in exchange to confirm transactions.
Código promocional 1xBet: ¡obtén un bono de bienvenida de hasta $130! codigo promocional 1xbet mexico El operador duplicará tu primer depósito hasta esa cantidad
Центр иностранных языков YES приглашает детей от 3-х лет, подростков и взрослых на онлайн-курсы английского языка лучшие онлайн курсы английского языка Обучение в нашей онлайн-школе проводится по эффективной коммуникативной методике индивидуально.
Откройте для себя новую эру в Мире Свежих Соков с Hurom от ВсеСоки!
Откройте для себя вкус истинного здоровья с каждым глотком! Соковыжималки Hurom – это гораздо больше, чем просто устройства, это ваш ежедневный помощник в стремлении к здоровому образу жизни. Знакомьтесь с ультрасовременными соковыжималками от официального дилера ВсеСоки в России, которые откроют для вас новые горизонты вкуса и питания.
Технология Slow Squeeze: Оставьте позади обычные соковыжималки. Технология медленного отжима Hurom сохраняет все полезные витамины, минералы и ферменты, делая каждый сок не только невероятно вкусным, но и максимально полезным.
Многофункциональность: Не ограничивайтесь соками! Hurom легко справляется с ореховым молоком, смузи, детским питанием и даже мороженым. Все, что нужно для здорового питания вашей семьи.
Инновационный Дизайн и Простота в Использовании: Стильный внешний вид соковыжималок Hurom прекрасно впишется в интерьер вашей кухни, а их интуитивно понятное управление и легкая очистка сделают процесс приготовления соков приятным и беззаботным.
Экологичность и Долговечность: Наша забота о планете! Соковыжималки Hurom изготовлены из премиальных, экологически чистых материалов и служат вам годами.
Поддержка и Гарантия от ВсеСоки: Обращаясь к официальному дилеру, вы получаете гарантированное качество, профессиональную консультацию и сервисное обслуживание.
Специальное Предложение: Используйте уникальную возможность и подарки при покупке соковыжималок Hurom у официального дилера ВсеСоки!
Заказывайте Сейчас: Переходите на наш сайт [всесоки.ру] и найдите свою идеальную соковыжималку Hurom. Начните свой путь к здоровью и энергии уже сегодня!
Here is my page – https://H-100.ru/collection/odnoshnekovye-sokovyzhimalki
Código promocional 1xBet: ¡obtén un bono de bienvenida de hasta $130! CГіdigo Promocional 1xBet Paraguay El operador duplicará tu primer depósito hasta esa cantidad
Центр иностранных языков YES приглашает детей от 3-х лет, подростков и взрослых на онлайн-курсы английского языка курсы английского онлайн Обучение в нашей онлайн-школе проводится по эффективной коммуникативной методике индивидуально.
skelaxin 100mg
Лингвистический центр YES предлагает вам открыть для себя новые языки или повысить свой уровень владения ими практический курс английского языка Мы открываем перспективы для учебы и работы за границей.
Лингвистический центр YES предлагает вам открыть для себя новые языки или повысить свой уровень владения ими курсы английского языка для школьников в москве Мы открываем перспективы для учебы и работы за границей.
Здесь очень выгодная и безопасная покупка Биткоинов за рубли без комиссии для жителей РФ и не только.
singulair
Ортопедические стельки для здоровых ног
ортопедические стельки индивидуальные https://www.ortopedicheskie-stelki-2023.ru/.
Торговать на маркетплейсах без документов соответствия можно только продукцией, не входящей в перечни ТР ЕЭАС, Постановления № 982, Решения КТС № 299 Какие товары не подлежат сертификации отдельный нормативный акт по товарам, не подлежащим обязательной оценке, не разработан. Подтвердить факт их отсутствия в законах можно с помощью отказного письма.
Торговать на маркетплейсах без документов соответствия можно только продукцией, не входящей в перечни ТР ЕЭАС, Постановления № 982, Решения КТС № 299 Перечень товаров не подлежащих обязательной сертификации отдельный нормативный акт по товарам, не подлежащим обязательной оценке, не разработан. Подтвердить факт их отсутствия в законах можно с помощью отказного письма.
WELCOME TO DUBAI STARS – YOUR PREMIER ESCORT COMPANIONS https://dubai-stars.com/
Harry French was moving suddenly cracked,
500 Euro Kredit
link do site
https://asksozlerioku.blogspot.com
https://b52.name
Ремонт гитар в Гомеле косметический ремонт гитар гомель с гарантией качества работы.
Ремонт гитар в Гомеле мастерская по ремонту гитар гомель с гарантией качества работы.
Cinema
термопанели для фасада https://klinkerprom13.ru/
Тут по выгодному курсу и безопасно можно провести обмен Биткоин для жителей РФ и не только.
люстры купить в москве https://lu18.ru/
I conceive this website has very wonderful written content material posts.
My website – http://epractica.je-hosting.co.uk/members/amandaballenti/activity/134680/
Pretty nice post. I just stumbled upon your weblog and wanted to say that I’ve truly enjoyed surfing around your blog posts. After all I’ll be subscribing to your feed and I hope you write again very soon!
O Cassino vavada gaming esta ganhando popularidade e se esforca para fornecer apenas servicos de alta qualidade.
O Cassino fresh cassino esta ganhando popularidade e se esforca para fornecer apenas servicos de alta qualidade.
MOTOLADY предлагают услуги аренды и проката мотоциклов и скутеров в Хургаде, Эль Гуне и Сахл Хашиш. MOTOLADY – одна из самых популярных компаний по прокату мотоциклов и скутеров. Они предлагают большой выбор транспортных средств по разумным ценам. MOTOLADY компания, специализирующаяся на Аренда мопеда в Эльгуне и Эль Гуне. Они предлагают услуги доставки транспорта в любое удобное для вас место. У нас в наличии различные модели транспортных средств по доступным ценам. Перед арендой транспорта обязательно ознакомьтесь с правилами и требованиями компании, также проверьте наличие страховки и необходимые документы для аренды.
%%
my blog; https://megaslotfortune.com/pt/
Are there restrictions on the sale of certain medicines during pregnancy and breastfeeding?
porn gig
Contra spem spero — Без надежды надеюсь.
http://batmanapollo.ru
How does the USA regulate the use of medicines in the context of medication disposal to prevent harm to the environment?
A casu ad casum — От случая к случаю.
http://batmanapollo.ru
В современном мире, где мобильные устройства и социальные сети стали неотъемлемой частью нашей жизни, все больше людей интересуются вопросом о том, слив бот с кем их близкие, партнеры или друзья переписываются.
В современном мире, где мобильные устройства и социальные сети стали неотъемлемой частью нашей жизни, все больше людей интересуются вопросом о том, бот шпион с кем их близкие, партнеры или друзья переписываются.
духи с феромонами
Nicely put, Appreciate it.
cetirizine tablet
Russexxx
You should take part in a contest for one of the greatest websites on the internet.
I most certainly will recommend this web site!
porn gig
sivuston verkko
Thanks for the good writeup. It actually was a enjoyment account
it. Look complex to far added agreeable from you!
However, how can we keep in touch?
Хостинг сайтов|Лучшие варианты хостинга|Хостинг сайтов: выбор специалистов|Надежный хостинг сайтов|Как выбрать хороший хостинг|Хостинг сайтов: какой выбрать?|Оптимальный хостинг для сайта|Хостинг сайтов: рекомендации|Лучший выбор хостинга для сайта|Хостинг сайтов: секреты выбора|Надежный хостинг для сайта|Хостинг сайтов: как не ошибиться с выбором|Выбирайте хостинг сайтов с умом|Лучшие хостинги для сайтов|Какой хостинг выбрать для успешного сайта?|Оптимальный хостинг для вашего сайта|Хостинг сайтов: важные критерии выбора|Выбор хостинга для сайта: советы профессионалов|Надежный хостинг для развития сайта|Хостинг сайтов: лучший партнер для вашего сайта|Как выбрать хостинг, который подойдет именно вам?
Хостинг сайтов http://www.hostingbelarus.ru/.
4000 euro lenen
Все, что вам нужно знать о винтовых масляных компрессорах: принципы работы и секреты повышения эффективности работы на принцип работы винтовых масляных компрессоров
สล็อต PG ที่ดีที่สุด เว็บตรง บิ๊กเบรค PG SLOT เว็บใหม่ โปรดี เว็บสล็อตสุดฮอต ที่สุดของปีนี้ เพียงลงทะเบียนกับเราวันนี้ คุณจะได้สนุก สนุกได้มากกว่า 10 เท่า แถมยังสามารถเล่นเกมสล็อตได้ก่อนใครได้ทันที เราได้คัดสรรเกมที่แตกง่ายมาให้คุณเลือกมากกว่า 200 เกม สมัครสมาชิกกับเราวันนี้แล้วคุณจะได้รับความคุ้มค่าสูงสุดตลอดกาล
Porn videos
http://ig5.ru/wPGpaCqp/
https://is.gd/drKArE
http://4ey.ru/EUNMEcv4/
https://is.gd/WgWjCE
https://is.gd/o4Xc0L
http://4ey.ru/etcdYyTW/
серия
https://tinyurl.com/yrhl67c7
https://is.gd/6XiLWh
сериал
https://tinyurl.com/yrhl67c7
orlistat pharmacy
смотреть
https://is.gd/6ypIBA
http://4ey.ru/8GX3YPDC/
серия
серия
ashwagandha wikipedia
https://tinyurl.com/ymj3zyke
directly3] over his head, in the spreading
http://ln-s.ru/4eq0epfx/
This is a topic which is near to my heart… Many thanks!
Where are your contact details though?
серия
https://is.gd/bo6yKv
Смотрите фильмы, сериалы, и мультфильмы из списка “Фильмы и сериалы” в нашем онлайн-кинотеатре мультфильмы и сериалы высокого качества
Смотрите фильмы, сериалы, и мультфильмы из списка “Фильмы и сериалы” в нашем онлайн-кинотеатре телесериал
http://4ey.ru/8GX3YPDC/
Не могу сейчас поучаствовать в обсуждении – очень занят. Вернусь – обязательно выскажу своё мнение.
при этом грани устроены так, арматура 14 мм документального подтверждения выдерживать сильное механическое воздействие. подать запрос возможно на ресурсе в нашем онлайн-магазине, по электронной почте либо по телефону.
сериал
http://ig5.ru/f5eMQG7V/
The Internet has revolutionized business strategies reputation house
https://is.gd/q3uyHL
The Internet has revolutionized business strategies reputation house reviews
https://is.gd/i1oEpI
https://tinyurl.com/yutfkhqo
http://4ey.ru/rP6erPwr/
https://is.gd/KGpWZJ
https://tinyurl.com/yl4z9qpq
https://is.gd/2fRiUu
https://is.gd/VuMttH
http://ig5.ru/f5eMQG7V/
http://4ey.ru/etcdYyTW/
https://is.gd/nYlSnL
серия
смотреть
https://is.gd/Qaq5Cn
серия
электрические гардины https://prokarniz11.ru/
серия
автоматические рулонные шторы с электроприводом https://prokarniz13.ru/
смотреть
https://tinyurl.com/yokk8lgk
http://ig5.ru/wPGpaCqp/
серия
смотреть
сериал
смотреть
серия
смотреть
серия
https://is.gd/5zQr7a
сериал
https://is.gd/Bzu8Zo
https://tinyurl.com/yuscrxlb
https://is.gd/SrJnvT
смотреть
серия
https://is.gd/LBejzt
сериал
credito 8000 euros
https://is.gd/kStRqG
https://is.gd/EE4WN7
%%
my web blog; http://fishing.ukrbb.net/viewtopic.php?f=21&t=13311
http://ln-s.ru/4eq0epfx/
смотреть
https://is.gd/G4g1pL
серия
https://is.gd/bcM4ZW
смотреть
https://tinyurl.com/yv2u2wwx
https://is.gd/MdiXTi
https://tinyurl.com/ywpmx387
https://is.gd/epmZQr
https://is.gd/73iKjK
серия
https://is.gd/rb7d2R
http://4ey.ru/EnQYZHqX/
tired of the sport and ran a good way off and sat
смотреть
cher.epan.ovre.n.a.t2.35.07.9@gmail.com
https://is.gd/WUvX4h
https://tinyurl.com/yo4fer3a
%%
My webpage – http://www.senbernar.ru/profile/9557-uzeqicyr/
Pills prescribing information. Cautions.
stromectol
All trends of medicament. Get now.
https://is.gd/NyyWjn
https://is.gd/lALCY8
http://8ua.ru/w0pHmq8u/
серия
https://is.gd/qZyS5D
https://tinyurl.com/yof9ukyu
https://tinyurl.com/yuscrxlb
https://is.gd/Wls7QS
смотреть
https://is.gd/DXrMFJ
сериал
http://ig5.ru/1qXCg8d9/
https://is.gd/SrJnvT
https://is.gd/vwOW0S
%%
my blog post … https://stprojekt.pl/
http://8ua.ru/ptqwK5nD/
https://is.gd/KGMuqr
https://tinyurl.com/yrhl67c7
http://8ua.ru/ptqwK5nD/
https://tinyurl.com/ywpmx387
https://tinyurl.com/ypwxwj2j
https://is.gd/BM0iqD
сериал
http://4ey.ru/etcdYyTW/
https://is.gd/A8cSvo
https://is.gd/o4Xc0L
смотреть
http://4ey.ru/0Ub3u8Hu/
https://is.gd/UqcBo3
https://is.gd/gkIrBE
LГҐn 150000
http://fi6.ru/fWeU9Q3B/
https://is.gd/o4Xc0L
https://is.gd/6JMp1T
https://is.gd/2lJ4MH
https://tinyurl.com/ymj3zyke
серия
http://8ua.ru/ptqwK5nD/
серия
https://is.gd/EM1hnw
https://is.gd/PYJzSQ
https://is.gd/Qcgbj2
https://is.gd/ZQmXN3
http://4ey.ru/EUNMEcv4/
https://is.gd/8QSNmL
сериал
procardia 100mg
https://tinyurl.com/yvv7jle6
https://is.gd/Fxcky0
сериал
https://tinyurl.com/yrqyzdby
https://is.gd/6ypIBA
https://is.gd/gMXz0j
https://tinyurl.com/ypwxwj2j
серия
смотреть
https://tinyurl.com/yuscrxlb
https://tinyurl.com/yv36932b
серия
Drugs information sheet. What side effects can this medication cause?
zofran
Some news about drugs. Get information here.
https://is.gd/3V23Ph
смотреть
http://4ey.ru/etcdYyTW/
https://is.gd/3XgtIl
смотреть
https://tinyurl.com/ylqrvynx
http://ig5.ru/wPGpaCqp/
Free online porn
http://4ey.ru/e0bK7rw7/
https://is.gd/j5scjp
сериал
смотреть
https://is.gd/bcM4ZW
https://is.gd/HKfUYx
https://tinyurl.com/yv36932b
finasteride buy usa
На деле я до сих пор никак не могу принять за чистую монету, что есть одним из тех, кто читает значящие рекомендации, найденные в данном интернет-блоге. Моя семья и я от всей души благодарны вам за вашу щедрость да и за то, что вы предоставили мне шанс следовать выбранному профессиональному пути.. Спасибо за важную информацию, кою я приобрел с вашей веб-странички.
https://tinyurl.com/yl4z9qpq
Free online porn
https://is.gd/QzaE0P
http://8ua.ru/efBmnKZc/
смотреть
https://is.gd/D6DlO8
https://is.gd/3V23Ph
сериал
http://fi6.ru/fWeU9Q3B/
https://is.gd/1rwpYL
http://4ey.ru/8GX3YPDC/
https://is.gd/bcM4ZW
https://tinyurl.com/yv36932b
%%
my homepage :: https://www.leisuremartini.com/keep-spark-alive-long-distance-relationships-sexy-lingerie/
https://tinyurl.com/ywpmx387
https://is.gd/ksgoHO
сериал
сериал
%%
Here is my web page https://thecoupleconnection.net/erotic-lingerie-around-the-world/
http://ig5.ru/1qXCg8d9/
https://is.gd/qVJkPw
http://4ey.ru/TumYUrDb/
https://is.gd/bo6yKv
How much do negative reviews affect the reputation, figures, and income of a business reputation house reviews
https://is.gd/WO1stb
pret 18000 euros
https://is.gd/uhbtrd
серия
https://tinyurl.com/ype9g4n6
серия
сериал
plan b 10mg
https://is.gd/2SNZw1
смотреть
https://is.gd/HLCkLq
серия
https://is.gd/f8cm1P
серия
У нас можно купить ковер по очень выгодной стоимости.
сериал
https://tinyurl.com/yl4z9qpq
https://tinyurl.com/yv2u2wwx
http://ln-s.ru/4eq0epfx/
http://8ua.ru/ptqwK5nD/
https://is.gd/gNfiEQ
https://is.gd/sVUmDH
смотреть
https://tinyurl.com/ykemyeqx
смотреть
смотреть
https://tinyurl.com/yof9ukyu
http://4ey.ru/eCagpN92/
сериал
videos
https://tinyurl.com/ymao445s
смотреть
Vous pouvez acheter ces sachets Pablo Dry Ice Cold pour un bon prix.
Je recommande cette très belle pochette Pablo Exclusive Pear
http://ig5.ru/GRhzZ0b6/
сериал
Компания Namuna Development в Ташкенте с 2017 года стремится не просто строить здания, реклама новостроек в Ташкенте но и создавать территорию, оснащенную развитой инфраструктурой.
Компания Namuna Development в Ташкенте с 2017 года стремится не просто строить здания, купить нежилое помещение в ташкенте но и создавать территорию, оснащенную развитой инфраструктурой.
электронный карниз для штор https://prokarniz19.ru/
she found was the tops of the trees ‘neath which she
I am really enjoying the theme/design of your site.
Do you ever run into any browser compatibility issues? A few
of my blog visitors have complained about my website not working correctly
in Explorer but looks great in Opera. Do you have any ideas to help fix this problem?
Amazing blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple adjustements would really make my blog jump out.
Please let me know where you got your design. With thanks
What’s Going down i’m new to this, I stumbled upon this I have found It absolutely useful
and it has aided me out loads. I hope to give a contribution & assist other customers like its aided me.
Great job.
Пожалуй, здесь лучшие Курсы актерского мастерства
Cinema
urenrjrjkvnm
https://metallicheckiy-portal.ru/articles/medic/psixolog/uslugi_psixologa_onlain_v_minske
https://tlt.volga.news/669005/article/rol-psihologa-v-sovremennom-obshestve-pomosh-i-podderzhka-dlya-vseh.html
Слово пацна 2 сезон Слово пацна 2 сезон 1 серия сериал Слово пацна 2 сезон
%%
my site; https://pinupcashslot.win/
Слово пацна 2 сезон Слово пацна 2 сезон 1 серия сериал Слово пацна 2 сезон
Слово пацна 2 сезон Слово пацна 2 сезон 1 серия просмотр Слово пацна 2 сезон
Слово пацна 2 сезон Слово пацна 2 сезон 1 серия онлайн Слово пацна 2 сезон
cheap cymbalta 40mg
Слово пацна 2 сезон Слово пацна 2 сезон 1 серия просмотр Слово пацна 2 сезон
My brother recommended I might like this blog. He was totally right.
This post truly made my day. You cann’t imagine simply how much time
I had spent for this information! Thanks!
https://www.wildberries.ru/catalog/176001489/detail.aspx
Женская Водолазка с Длинным рукавом (Черная) Артикул 9889696754543457
xxx videos
Слово пацна 8 серия Слово пацна 8 серия онлайн Слово пацна 8 серия
Со времени прошлого года наблюдается понижение ставок по ипотеке на пару процентных пунктов купить недвижимость в ташкенте но и создавать территорию, оснащенную развитой инфраструктурой.
Со времени прошлого года наблюдается понижение ставок по ипотеке на пару процентных пунктов купить студию в ташкенте но и создавать территорию, оснащенную развитой инфраструктурой.
Слово пацна 8 серия Слово пацна 8 серия смотреть Слово пацна 8 серия
Слово пацна 8 серия Слово пацна 8 серия просмотр Слово пацна 8 серия
Слово пацна 8 серия Слово пацна 8 серия просмотр Слово пацна 8 серия
Слово пацна 8 серия Слово пацна 8 серия сериал Слово пацна 8 серия
vierailla
Это сделать просто, если иметь промокод 1xbet на сегодня бесплатно. Правда, дается он при условии выполнения некоторых правил. 1xbet. Не совсем промокод, но вы все равно ставите не свои деньги, если пополните депозит, – 100% бонуса от внесенной суммы. Максимум указан в верхней части главной страницы официального сайта. 100% бонус за пополнение от 1xbet. Но прежде чем получить бонус нужно пройти регистрацию. Зайдите на сайт БК 1xBet и нажмите по стрелке кнопку «Регистрация». 2. Выберите один из методов регистрации (самый быстрый — в один клик). Кликните на «Зарегистрироваться».
toop porn (maps.google.co.za)
Here is a very favorable price miami exotic car rental
купить бетон щелково
Жаль, что сейчас не могу высказаться – вынужден уйти. Освобожусь – обязательно выскажу своё мнение по этому вопросу.
кроме того в представленном интернет маркете, вы сможете купить оптом благодарности и бланки благодарственных писем, которые легко и удобно использовать, например, купить диплом техникума с занесением в реестр для выработки благодарственного письма родителям.
Hello there! This article could not be written any better! Reading through this article reminds me of my previous roommate! He always kept preaching about this. I most certainly will send this article to him. Fairly certain he will have a very good read. Thank you for sharing!
Feel free to surf to my web page :: https://Wiki.Hrw-Fablab.de/index.php?title=User:AguedaMacleay5
Voyez comment le monde a changé grâce à la technologie et à l’utilisation des données. Apprenez comment l’utilisation de l’intelligence artificielle, des cybermenaces et des hackers peuvent avoir des conséquences inattendues.
Актуальные объявления о покупке и продаже квартир на вторичном рынке недвижимости купля-продажа квартиры частные объявления о продаже квартир.
Актуальные объявления о покупке и продаже квартир на вторичном рынке недвижимости eng arzon kvartira toshkent частные объявления о продаже квартир.
You’ve made your stand quite well..
Мгновенно создавайте премиальные статьи, описания и разнообразный контент с использованием нашего революционного искусственного интеллекта Чат боты ИИ
Мгновенно создавайте премиальные статьи, описания и разнообразный контент с использованием нашего революционного искусственного интеллекта Генерация изображений Dalle 3
Достойное решение для занятых женщин: Permanent Eyeliner Tattoo.
Самое стойкое украшение глаз: Permanent Eyeliner Tattoo.
Не потеряется красота: Permanent Eyeliner Tattoo.
Как бьюти-тренд: Permanent Eyeliner Tattoo.
Всегда и везде: Permanent Eyeliner Tattoo.
Навсегда останется с тобой: Permanent Eyeliner Tattoo.
Качественное украшение: Permanent Eyeliner Tattoo.
Ничто не сравнится с Permanent Eyeliner Tattoo.
Почти бессмертное произведение искусства: Permanent Eyeliner Tattoo.
Надежное и экономичное решение: Permanent Eyeliner Tattoo.
Словно волшебство: Permanent Eyeliner Tattoo.
Как подчеркивание глаз: Permanent Eyeliner Tattoo.
Не сомневайся в своём образе с Permanent Eyeliner Tattoo.
Привлекательность в каждом миге: Permanent Eyeliner Tattoo.
Открой для себя новое о Permanent Eyeliner Tattoo.
Как модный аксессуар: Permanent Eyeliner Tattoo.
Долгосрочное удовольствие: Permanent Eyeliner Tattoo.
Привлекательная нить между душой и образом: Permanent Eyeliner Tattoo.
Как нарядная украшенная: Permanent Eyeliner Tattoo.
Невыразимо: Permanent Eyeliner Tattoo.
eyeliner permanent makeup near me http://www.eyeliner-tattoo-md.com.
Here is a very favorable price for lamborghini rental Miami
Регистрация в 2024 году — бесплатный промокод 1xbet на сегодня. Часто задаваемые вопросы по регистрации и учетной записи у букмекера 1xbet. 1хбет промокод при регистрации свежий. Разнообразие бонусных предложений от 1xbet — другие типы бонусов и промокодов для игроков. Промокод 1xbet на День Рождения. Фрибеты или бесплатные ставки. Тото-промокоды 1xbet. Промокоды 1xbet у блогеров. Система промокодов при регистрации позволяет новым игрокам букмекерской конторы 1xbet получать внушительные бонусные суммы к своему первому депозиту. Обратите внимание, что это не промокод на ставку, а именно на регистрацию. Рабочие промокоды 1хбет на сегодня: Вид бонуса. Размер бонуса.
Бесплатные промокоды. Давайте сразу начну с того, что перечислю несколько актуальных Промокодов 1xbet на сегодня. Смело вводите промокод в соответствующее поле и получайте прикольные «плюшки» в подарок от щедрого букмекера! Букмекерская контора 1xbet отличается от конкурентов наличием широкой программы лояльности. Важной ее частью является предоставление клиентам бонусов при вводе промокода. промокод в 1xbet. В системе действует программа приветственных бонусов, благодаря которой каждый новичок получает определённую сумму за регистрацию на сайте. Такие акции действуют для казино и букмекерской конторы. Чтобы принять участие в приветственной программе, достаточно активировать при регистрации любой рабочий промокод.
Перечень товаров, не требующих сертификации. Не существует единого утвержденного списка товаров, не требующих сертификации Перечень товаров не подлежащих сертификации на маркетплейсах Это было сказано ранее. По мере изучения актуального списка вы не найдете вашей продукции среди заявленных категорий – это означает, что единственным документом для реализации или прохождения таможенного контроля является отказное письмо.
Перечень товаров, не требующих сертификации. Не существует единого утвержденного списка товаров, не требующих сертификации Продукция не подлежащая сертификации Это было сказано ранее. По мере изучения актуального списка вы не найдете вашей продукции среди заявленных категорий – это означает, что единственным документом для реализации или прохождения таможенного контроля является отказное письмо.
The magical world of slot machines: Book of Mostbet and Joker Stoker http://darkagewars.com/forums/showthread.php?p=1887025#post1887025
The magical world of slot machines: Book of Mostbet and Joker Stoker https://news24.az/index.php?subaction=userinfo&user=enecugo
Промокоды казино 1xBet при регистрации 2024. На ресурсе 1хБет пользователи могут не только делать ставки на спорт и другие события из разных сфер, но и получать азартные ощущения в казино. Играть можно как с машинами, так и с реальными дилерами в разделе лайв. Чтобы привлекать как можно больше новых игроков и поддерживать интерес постоянных клиентов, на сайте 1хБет регулярно проходят акции и раздают бонусы. Самое щедрое вознаграждение могут получить новички, использовав промокод казино 1xBet. Указав его при регистрации, пользователь получит дополнительные денежные средства на первые несколько депозитов, которые сможет использовать для ставок в играх. Это сделать просто, если иметь промокод при регистрации 1xbet. Правда, дается он при условии выполнения некоторых правил. 1xbet бонус при регистрации. Не совсем промокод, но вы все равно ставите не свои деньги, если пополните депозит, – 100% бонуса от внесенной суммы. Максимум указан в верхней части главной страницы официального сайта.
%%
My blog; http://shiftdelete.10tl.net/member.php?action=profile&uid=30589
Бесплатный промокод 1xBet 32500 рублей. Промокод при регистрации в БК 1xBet рассчитан на привлечение новых клиентов. Совокупность букв и цифр вводится при создании аккаунта, что поднимает сумму первого пополнения счета до 325000 тысяч рублей. Редакция напоминает, что для получения бонуса потребуется пройти процедуру отыгрыша. Букмекер просит проставить сумму экспрессами. Коэффициент каждой отдельной ставки составляет минимум 1.4. После прохождения отыгрыша выбранная сумма денег перейдет из бонусного на основной счет. 1xBet промокод на День Рождения. Букмекерская контора поздравляет каждого верифицированного клиента бесплатной ставкой на День Рождения. На сегодня у 1xbet предусмотрено несколько рабочих промокодов: на бесплатную ставку, на 25000 рублей, а также промокод до 1500 евро. Промокод 1xbet до 1500 евро. Между букмекерами активно развивается конкуренция, и это правильно. Каждый старается привлечь к себе как можно больше игроков, в том числе различными акционными предложениями, бонусами и тому подобными маркетинговыми методами. Как получить промокод 1xbet? Промокод казино 1xbet до 1500 евро. промокод на 1xbet при регистрации. Промокод 1хбет на сегодня. Бездепозитный промокод 1xbet. Сегодня отсутствует. Один из наиболее популярных среди таковых — использование промокодов.
Ad usum internum — Для внутреннего употребления.
http://batmanapollo.ru
Здесь можно бесплатно и безопасно скачать бетсити
http://ln-s.ru/XQxpdH90/
https://is.gd/sAPYCP
https://tinyurl.com/ys6za53r
https://tinyurl.com/ywynya3r
http://ln-s.ru/vX8VVy9B/
Can antibiotics be used for vocal cord infections buy hydroxychloroquine sulfate?
http://ln-s.ru/CNxkvkN4/
http://ln-s.ru/0DhrfPzN/
http://ln-s.ru/ECuNpn2K/
coreg without a doctor prescription
https://tinyurl.com/yntndne4
http://ln-s.ru/m1aExNSE/
https://tinyurl.com/yvh9uvcv
http://ln-s.ru/zy4wEnMB/
https://tinyurl.com/ynfzwfbf
http://ln-s.ru/E6BeMQrB/
https://tinyurl.com/yrhu6er8
https://tinyurl.com/yplfouew
http://ln-s.ru/1dT36XNu/
%%
Feel free to visit my page; http://renebiemans.nl/users.php?m=details&id=29081
https://tinyurl.com/ytse4yot
http://ln-s.ru/sH5zPQ1D/
http://ln-s.ru/xeF9kQeD/
http://ln-s.ru/C0X55A9h/
http://ln-s.ru/d23nxUPv/
http://ln-s.ru/9wMqyznB/
https://tinyurl.com/yntndne4
http://ln-s.ru/6s0CfvfW/
Только тут можно быстро и безопасно бетсити скачать
https://tinyurl.com/ypqufuw3
http://ln-s.ru/CNxkvkN4/
https://tinyurl.com/ypq3l5c5
https://tinyurl.com/yw7oz4nl
https://tinyurl.com/ytgt4eod
http://ln-s.ru/UYrxBQRV/
https://tinyurl.com/yuscrxlb
http://ln-s.ru/4AURxXHc/
http://ln-s.ru/KPhxFH6z/
http://ln-s.ru/0M0YFV7F/
http://ln-s.ru/0BEd14nB/
https://tinyurl.com/yvda4mtk
http://ln-s.ru/YXRpKsyr/
http://ln-s.ru/f9yW3VEQ/
https://tinyurl.com/ypwvwpzu
https://tinyurl.com/yvda4mtk
Максимальная эффективность в арбитраже: выбирайте виртуальные карты от Webscard webscard
Branded Residences from the Masters Nikki Beach Aldar
https://tinyurl.com/ywkh85kr
Максимальная эффективность в арбитраже: выбирайте виртуальные карты от Webscard виртуальные карты для прбитража
https://tinyurl.com/yntndne4
https://tinyurl.com/yrlrqm6w
http://ln-s.ru/bM4VMHUy/
http://ln-s.ru/E8PQ9NPT/
https://tinyurl.com/ynfzwfbf
http://ln-s.ru/wKSV5p2H/
http://ln-s.ru/mzunWpkY/
http://ln-s.ru/6UBkA7nP/
https://tinyurl.com/ym8glot9
https://tinyurl.com/yohz7bb9
http://ln-s.ru/bwnBENmr/
https://tinyurl.com/yr9hnfsa
http://tinyurl.com/yt2ffxoc
https://tinyurl.com/ysoz5p9k
https://tinyurl.com/ys3odoar
https://tinyurl.com/ytgt4eod
http://ln-s.ru/vZFn6r67/
My relatives always say that I am killing my time
here at net, however I know I am getting experience daily by reading thes good posts.
%%
My web site – mejores casas de apuestas
https://tinyurl.com/yrhl67c7
Добровольная сертификация продукции услуг и систем менеджмента качества в СДС Роспромтест на соответствие Государственным стандартам, техническим условиям. Сертификация объектов проходит на добровольной основе по инициативе заявителя в системе добровольной сертификации Роспромтест на соответствие Государственным стандартам (ГОСТ), техническим условиям (ТУ), стандартам организации (СТО).
Промокод 1xbet при регистрации. Промо-код встречается на просторах сети достаточно часто. Букмекер использует его для привлечения новых игроков в индустрию ставок, но преимущество предоставляется и новому игроку. После того как он совершит первый депозит, на его бонусный счёт поступит аналогичная сумма, до 32500 рублей. промокод на 1хбет Данный вид бонус-кода также популярен в поиске. Указывать его надо в купоне для совершения ставки. Промокод 1xbet на ставку практически невозможно найти в бесплатном доступе. Он вручается игрокам индивидуально.К примеру, компания промокодов. В данном разделе подробно расписан процесс получения.
http://ln-s.ru/DaWM2h0S/
https://tinyurl.com/yrhu6er8
http://ln-s.ru/AZs3mwSC/
http://ln-s.ru/Fe1v2Nnq/
http://ln-s.ru/90BAVDSZ/
Best Branded Residences from the Masters Nikki Beach Ras Al Khaimah
Whoa! Thiis blog loolks jst ⅼike mmy oold one!
It’ѕ onn a tootally ɗifferent subjecht buut iit
haas pretgy muh thee samne pahe layou andd design. Exceloent choice оff colors!
Μy bblog :: {acidkhoraki.ir|https://acidkhoraki.ir/%d9%85%d8%b1%da%a9%d8%b2-%d8%aa%d8%b1%da%a9-%d8%a7%d8%b9%d8%aa%db%8c%d8%a7%d8%af-%d8%b2%d9%86%d8%a7%d9%86-%da%a9%d9%85%d9%be-%d8%ae%d8%b5%d9%88%d8%b5%db%8c-%d8%a8%d8%a7%d9%86%d9%88%d8%a7%d9%86-%da%a9/
In the ever-evolving world of digital technology, it has become increasingly important for individuals and businesses to safeguard their online security http://xavierdeschamps.free.fr/Escalade/Forum_escalade/viewtopic.php?pid=1328231#p1328231
In the ever-evolving world of digital technology, it has become increasingly important for individuals and businesses to safeguard their online security http://urbino.fh-joanneum.at/trials/index.php?title=Analyzing_Data_with_Grabify_IP_Logger
brillx официальный сайт
https://brillx-kazino.com
Играя в Brillx Казино, вы окунетесь в мир невероятных возможностей. Наши игровые автоматы не только приносят удовольствие, но и дарят шанс выиграть крупные денежные призы. Ведь настоящий азарт – это когда каждое вращение может изменить вашу жизнь!Так что не упустите свой шанс вступить в мир Brillx Казино! Играйте онлайн бесплатно и на деньги в 2023 году, окунувшись в море невероятных эмоций и неожиданных поворотов. Brillx – это не просто игровые аппараты, это источник вдохновения и увлечения. Поднимите ставки и дайте себе шанс на большую победу вместе с нами!
продажа нежилых помещений в ташкенте
Veni, vidi, vici – пришел, увидел, победил
http://batmanapollo.ru
aristocort
I recommend this Nikki beach residences RAK
%%
Here is my site p171
brillx casino официальный сайт
Brillx
Играя в Brillx Казино, вы окунетесь в мир невероятных возможностей. Наши игровые автоматы не только приносят удовольствие, но и дарят шанс выиграть крупные денежные призы. Ведь настоящий азарт – это когда каждое вращение может изменить вашу жизнь!Вас ждет огромный выбор игровых аппаратов, способных удовлетворить даже самых изысканных игроков. Брилкс Казино знает, как удивить вас каждым спином. Насладитесь блеском и сиянием наших игр, ведь каждый слот — это как бриллиант, который только ждет своего обладателя. Неважно, играете ли вы ради веселья или стремитесь поймать удачу за хвост и выиграть крупный куш, Brillx сделает все возможное, чтобы удовлетворить ваши азартные желания.
I recommend this Cape Hayat
%%
my site … http://academijacrimea.ru/index.php?subaction=userinfo&user=yxopiwat
prestamo 60000 euros
%%
Also visit my website … http://tr.besatime.com/user/gebemetygp
I visited many websites but the audio feature for audio songs current at this web site is genuinely superb.
Между нами говоря, рекомендую поискать ответ на Ваш вопрос в google.com
Поэтому всем тем, кто заинтересован в действительно работоспособного букмекера с новыми коэффициентами и лояльным отношением ко имеющимся беттерам (даже к «вилочникам»), ramenbet casino обязательно необходимо попробовать ставки в раменбет.
%%
%%
Also visit my web site … https://aged-wiki.win/index.php?title=Dog_house_megaways
I recommend this best Mercer House
https://iotzyv.ru/2023/12/11/advokat-sibgatullin-timur-ravilevich/
Excellent blog here! Also your site loads up very fast! What host are you using? Can I get your affiliate link to your host? I wish my website loaded up as quickly as yours lol
https://stihi.ru/avtor/sibgatullin
I read this piece of writing fully on the topic of
the comparison of latest and preceding technologies, it’s amazing article.
buying co-amoxiclav online
I recommend this original site Mercer House Dubai
%%
Also visit my web page https://azino777ab.online/
https://poisk-proslushki-msk.ru/
https://poisk-proslushki-spb.ru/
Бесплатные промокоды 1xBet при регистрации 2024. Сегодня пользователям 1xBet-казино предлагаются халявные промокоды на первый депозит, которые активируются при первой регистрации. С их помощью можно увеличить сумму базового бонуса до 32500 рублей. 1XFREE777 — промокод 1х. Для получения реального выигрыша с возможностью вывода на карту, необходимо поставить всю бонусную сумму на экспресс-ставку с коэффициентом от 1,4. Если прогноз окажется правильным, система переведет деньги на основной счет. Не секрет, что у букмекерской конторы 1xBet помимо спортивных ставок есть и другие направления, включая онлайн-игры, гоночные события или политические состязания.
Hi there, I check your blog regularly. Your humoristic style is witty,
keep it up!
Feel free to visit my page – Ron Spinabella
https://poembook.ru/poem/2975210-sibgatullin-timur-ravilevich
pitchfork, but which had only two prongs, and in his
%%
Also visit my blog post: https://ofigenka.ru/pochemu-seo-prodvizhenie-sajtov-eto-vazhno
https://ru.otzyv.com/sibgatullin-timur-ravilevich
and did not wait to tell it who she was.
Зарабатывайте больше с onexbet – проверенным и надежным букмекером!
Download 1xbet program for computer http://www.1xbetappvgergf.com/.
ダッチワイフ ロボット ダッチワイフを購入することはあなたのパートナーに熱狂的なトリックです
I recommend to all this original Mercer House Ellington
This site was… how do you say it? Relevant!!
Finally I have found something that helped me. Thank you!
Some of the vital components that make pranks hilarious is actually mismatch. Pranks frequently include unanticipated twists or even incongruent components that differ the counted on or even regular pattern of activities. The individual mind is actually wired to find patterns and create forecasts based upon previous knowledge. When a prank disrupts this pattern, creating shock or difference, it causes an intellectual reaction, https://www.tumblr.com/sherronoshea/736472685167656960/whats-a-joke-a-laugh-is-a-type-of-wit-that-is?source=share.
What’s up, this weekend is fastidious designed for me, as this point in time i am reading this wonderful informative post here at my home. dark market url https://mydarkmarket.com
Cinema
Промокод 1xBet на сегодня при регистрации на сайте. Получи повышение на первый депозит до 32500р. Промокод 1хБет для новых игроков действующий и актуальный. Промокоды 1хБет на июль 2024. 1 x bet промокод, о котором пойдет речь, не имеет срока годности использования и всегда гарантирует прибавку к вашему депозиту. Бесплатным промокодом может воспользоваться любой игрок при регистрации. Не имеет значения, через какую версию сайта букмекера или приложение. 1XFREE777 – специальная комбинация букв и цифр, которая показывает букмекеру автоматическим способом, что игрок должен получить повышенный бонус.
https://zoon.ru/msk/p-repetitor/timur_ravilevich_sibgatullin/
I recommend to all this Cape Hayat RAK
prestamo 20000 euros
Получи 32500 руб. по актуальному промо коду для 1хбет бесплатно. Новые купоны на регистрацию каждый час на сайте. В ваших силах получить до шести с половиной тысяч рублей при регистрации. Читайте ниже как использовать наши промо-коды. промокод на 1xbet. Букмекерская контора позволяет использовать промокод 1иксбет на ставку-бонус. Забирайте новые купоны ежедневно. Внимание! Наши промо-купоны подходят для всех акций букмекера. Этот купон также универсальный – используйте его везде, не только при регистрации на сайте БК 1хбет и всех известных его зеркал. Введите его в форме для регистрации и получите увеличенный бонус на первый депозит до 32500 рублей. Кроме того, букмекер постоянно дарит активным клиентам выгодные подарки. Чтобы получить промокод в 1xBet бесплатно: Подпишитесь на рассылку новостей по смс или электронной почте. Регулярно заходите в раздел «Бонусы и подарки» в Личном кабинете.
I recommend this best security services in Miami.
%%
Also visit my web site; что такое seo оптимизация
https://fotostrana.ru/user/127505353/
https://namebook.club/profile/sibgatullin-timur-27850990000
%%
Feel free to visit my website … http://www.homes-on-line.com/cgi-bin/hol/show.cgi?url=https://yari1.xyz/agitation-parapsychological-berth-zrwu/
So she called it in a soft, kind voice, “Mouse dear! Do
строительные компании ташкент
I recommend this best mobile patrolling in Miami.
tell them a tale.
https://www.familyspace.ru/user32839533
https://ruscifra.ru/self-employed/6884094/
%%
Here is my web site – установка видеонаблюдения под ключ
I recommend to all this best Cape Hayat RAK Properties
https://b2book.ru/person/6035007/
Абсолютно бесплатный промокод 1xbet. На сегодня контора предлагает всем новичкам воспользоваться не только приветственным бонусом, но и получить дополнительные преференции. Эти льготы игрок получает в том случае, если внимательно отнесётся к процедуре регистрации на сайте. 1xbet промокод. 1xbet – один из самых узнаваемых букмекерских брендов в стране. Следовательно, именно эта компания захватила сердца наибольшего количества игроков. Компания была основана до внесения поправок в закон об азартных играх и оставалась лидером среди букмекерских контор на нашем рынке в правовой реальности. Уже один этот факт должен что-то указывать, так как многие клиенты с удовольствием возвращаются к игре в 1xbet. 1XBET – промокод на 32500р. Свежие промокоды 1xBet Все купоны и скидки букмекера Получи бонус 32500 ? Делай ставки на спорт.
1xBet промокод на бонус при регистрации. Букмекерская контора предоставляет игрокам множество возможностей для снижения рисков и увеличения банка. Бонусная программа компании предусматривает интересы как новичков, так и опытных бетторов. Рассмотрим основные виды поощрений в функционале БК: 1хБет промокод на регистрацию – один из самых популярных подарков, созданный для новых игроков на сайте; Ставки на спорт – увеличение депозита до 32500 рублей. Воспользуйся актуальным промокодом 1xbet на сегодня, получи бесплатную возможность увеличить свой первый депозит до 32500 рублей в БК 1xBet. Воспользовавшись промокод бк 1xbet при регистрации, максимальная сумма бонуса возможного бонуса будет увеличена до 32500 рублей. Но при этом сумма бонуса будет равна сумме вашего первого депозита.
Список бесплатных на сегодня промокодов 1xBet. Тип бесплатного промокода. Промокод промокод на бесплатную ставку. 1xbet промокод. Как сегодня получить 32500 рублей по промокоду в 1xBet? Получение начинается после регистрации с рабочим промокодом и первого пополнения счета и составляет +100% к депозиту. Игрок может рассчитывать по промокоду до 32 500 рублей, если пройдет верификацию и даст согласие на участие в рекламных предложениях букмекера. На сегодня акция по промокоду 1xBet распространяется на пользователей из России, Беларуси, Украины, Казахстана.
Google Play Маркет — магазин приложений от Google, позволяющий владельцам устройств с Android устанавливать приложения play market скачать на андроид бесплатно на русском языке
1хбет промокод на депозит – комбинация из чисел и букв. Эта комбинация дает возможность игроку получить дополнительные бонусы. К примеру, это может быть: промокод на бесплатную ставку (фрибет); повышение коэффициентов ставок формата «экспресс». Промокод при регистрации применяется именно таким образом. Он позволяет увеличивать размер приветственного бонуса на первый депозит, который выдается самим букмекером 1xbet. Где найти? Вариантов для получения промокода на 1xbet на сегодня существует множество. Но мы предлагаем вводить наш собственный промокод для 1xbet. Это промокод для регистрации, он вводится в поле в регистрационной анкете. Промокод при регистрации на сегодня. Промокоды для БК и Казино — ежедневное обновление. Регистрация на сайте 1xBet бесплатная, но для начала игры и получения доступа к 1xbet промокоду при регистрации 2024, придется внести на игровой счет от 50 рублей. Особенности регистрации. Процедура создания профиля в букмекерской конторе 1xbet максимально упрощена. Для регистрации предусмотрены такие способы: В «1 клик». Чтобы создать учетную запись, нужно выбрать страну проживания и валюту, ознакомиться с пользовательским соглашением и кликнуть на клавишу «Регистрация». С помощью телефона.
Google Play Маркет — магазин приложений от Google, позволяющий владельцам устройств с Android устанавливать приложения google play скачать на андроид бесплатно
Пин ап
пинап https://www.pinupcasinojdhenecko.vn.ua/.
get lexapro prices
%%
Feel free to visit my web-site https://marvelcomics.faith/wiki/User:GeniaDeVis0
Бесплатные промокоды на 2024 от букмекерской конторы 1xBet: при регистрации, на бесплатную ставку. Рассказываем, как использовать и куда вводить промокоды в 1хБет. промокод при регистрации 1xbet. Бесплатный промокод для увеличения бонуса. Букмекерская контора 1хБет – одна из самых популярных беттинговых площадок, предлагающая высокие коэффициенты, широкую линию с дополнительной росписью. Благодаря низкой марже БК пользователи стабильно зарабатывают на ставках на спорт. Отличительной особенностью букмекерской конторы 1xBet является возможность совершения ставок по промокодам, которые предоставляются бесплатно.
buy online doxycycline
I recommend only this exotic car rental Miami site.
experimente este site
%%
Here is my web page – https://www.algeriepatriotique.com/2023/12/08/les-plus-beaux-sites-gallo-romains-de-france/
dispersible doxycycline tablets
How long do viral infections last without antibiotics ivermectin dosage chart for humans?
up as tall as she could, and her eyes met those of
Drugs information. Cautions.
proscar without a prescription
All trends of pills. Read here.
%%
Here is my page … http://flokii.com/questions/view/4570/online-casino
Бесплатные промокоды. Давайте сразу начну с того, что перечислю несколько актуальных Промокодов 1xbet на сегодня. Смело вводите промокод в соответствующее поле и получайте прикольные «плюшки» в подарок от щедрого букмекера! Букмекерская контора 1xbet отличается от конкурентов наличием широкой программы лояльности. Важной ее частью является предоставление клиентам бонусов при вводе промокода. promokod 1xbet. В системе действует программа приветственных бонусов, благодаря которой каждый новичок получает определённую сумму за регистрацию на сайте. Такие акции действуют для казино и букмекерской конторы. Чтобы принять участие в приветственной программе, достаточно активировать при регистрации любой рабочий промокод.
SavdoUyi.uz – это онлайн-платформа, которая помогает людям находить работу, продавать и покупать товары и услуги Телефоны и аксессуары
SavdoUyi.uz – это онлайн-платформа, которая помогает людям находить работу, продавать и покупать товары и услуги Услуги автоинструктора
Заказать пластиковые окна из немецкого профиля VEKA. Выгодные цены и предложения на покупку и установку пластиковых ПВХ окон и дверей окно пвх поворотно откидное
Заказать пластиковые окна из немецкого профиля VEKA. Выгодные цены и предложения на покупку и установку пластиковых ПВХ окон и дверей окна двери пвх
https://www.izhforum.info/forum/izhevsk/viewtopic.php?f=26&t=147733
1xBet промокод на бонус при регистрации. Букмекерская контора предоставляет игрокам множество возможностей для снижения рисков и увеличения банка. Бонусная программа компании предусматривает интересы как новичков, так и опытных бетторов. Рассмотрим основные виды поощрений в функционале БК: 1хБет промокод на регистрацию – один из самых популярных подарков, созданный для новых игроков на сайте; Ставки на спорт – увеличение депозита до 32500 рублей. Воспользуйся актуальным промокодом 1xbet на сегодня, получи бесплатную возможность увеличить свой первый депозит до 32500 рублей в БК 1xBet. Воспользовавшись промокод 1xbet при регистрации, максимальная сумма бонуса возможного бонуса будет увеличена до 32500 рублей. Но при этом сумма бонуса будет равна сумме вашего первого депозита.
Промокод 1xBet при регистрации. Компания 1ИксБет заинтересована в привлечении новых клиентов, поэтому для новых игроков действует акция в виде бонуса, который равен сумме первого депозита, но не превышает 225 000 рублей. Однако при использовании промокода букмекерская контора увеличит размер приветственного бонуса. Для того чтобы получить повышенную сумму на первый депозит, игроку необходимо выполнить следующие условия: Зайти на сайт букмекера. Выбрать способ регистрации по e-mail. Заполнить поля с личными данными. Ввести промокод в поле слева от кнопки «Зарегистрироваться». Ознакомиться с правилами букмекера. промокод бк 1xbet при регистрации поможет пользователям получить еще больше бонусов от букмекерской конторы. Подробная инструкция по поиску и активации бонусных кодов. Промокод — комбинация из цифр и букв, которая позволяет игроку активировать специальное предложение от букмекера 1хБет. С его помощью пользователь может получить: бонусные средства на депозит; бесплатную ставку; промо-баллы; другие подарки. Сегодня вы сможете найти множество подобных ресурсов, которые регулярно обновляют список актуальных предложений БК.
porn
be Ma-bel af-ter all, and I shall have to go and live
get synthroid no prescription
Воспользоваться промокодом 1xbet можно при регистрации в 1xbet. БК 1хбет дарит до 130% на первый депозит при помощи промокода 1xbet. Максимальная сумма бонуса по промокоду 1хбет достигает 32500 рублей. Промокод 1хбет дает надбавку на депозит до 130% только при первом пополнении. Регистрация. промокод 1хбет при регистрации на сегодня. Всем известно, что букмекерская контора 1xbet предлагает широкий выбор разнообразных бонусов и акций. В этой статье мы расскажем все о промокодах 1xBet: что это, как использовать при регистрации, где вводить, чтобы сделать ставку бесплатно, и по каким поводам казахстанский букмекер 1хБет вручает именные промокоды. Содержание. Что такое промокод 1xBet. Бесплатные промокоды 1xBet. Промокод при регистрации в 1xbet сегодня. Как ввести промокод при регистрации в 1хБет.
Novyny
рабочий промокод Melbet на сегодня Введите: RS777 и тогда при депозите вы получите бонус 10400 рублей автоматически. Букмекерская контора Мелбет в 2024 году создала комфортные условия для заядлых беттеров и новых пользователей. Международная букмекерская платформа Melbet стремительно набирает популярность среди беттеров. Для привлечения новой аудитории и повышения лояльности уже имеющейся, администрация сайта создала специальный промокод.
Промокод 1xbet при регистрации по увеличению бонуса до 32500 рублей на первый депозит активируется бесплатно, заполнив поле “Промокод” официальным ключевым словом в регистрационном меню при создании аккаунта: Войти в 1xbet.com. promokod 1xbet: 1XFREE777 Получить промокоды на сегодня без регистрации в 1xBet можно на сайте, где незарегистрированным пользователям предлагается ввести промо «1XFREE777». Создание аккаунта в БК – это обязательный процесс для активации промокода на ставки и использования других функций. Бесплатный промокод для 1xBet на сегодня. Использование промокода 1xBet дает возможность получить подарок от букмекера. Обычно рабочий promo code «1xБет» располагается в соцсетях или же на партнерских ресурсах.Промокод при регистрации дает право на бонус. Для этого требуется пройти регистрацию и внести на баланс не меньше 100 рублей. Также необходимо в личном профиле заполнить все обязательные поля.
При регистрации в БК Melbet игрокам предлагается самостоятельно выбрать стартовую награду: фрибет на $30 или 100% бонус на депозит до 7 000 RUB. Предлагаем промокод при регистрации Melbet, благодаря которому вы получите не только повышенный до 10 400 RUB бонус на первое пополнение счета, но и право на бесплатный прогноз. Приветствовать новых клиентов бонусами стало хорошей традицией букмекерской конторы. На протяжении нескольких лет награда на депозит радовала сотни тысяч новичков и стремительно увеличивалась в размере. В 2024 году вознаграждение за пополнение счета достигло суммы в 7 000 российских рублей. Мы делаем более выгодное предложение. Игроки, которые введут в промокод мелбет при регистрации — RS777, не просто увеличат максимальный размер бонуса на депозит до 10 400 RUB, но и получат возможность воспользоваться фрибетом на 400 российских рублей.
I recommend in miami luxury car rental site.
Купить нержавеющие трубы по доступным ценам за метр от производителя окна пвх стоимость размеры в Москве от производителя по низким ценам
Купить нержавеющие трубы по доступным ценам за метр от производителя балконные окна пвх в Москве от производителя по низким ценам
купить электровелосипед взрослый
How do I protect my gut when taking antibiotics ivermectin for mice?
Специальные промокоды на 2024 год для 1xBet. Промокод — это уникальный набор из букв, цифр и символов для того, чтобы пользователь получил определенный бонус. Таким бонусом может оказаться увеличение начального депозита, ставка со страховкой (с возвратом части ставочных денег при выборе неверного исхода матча), тестовая ставка (чтобы новые игроки набрались опыта, без вреда собственным деньгам) и многое другое. Больше промокодов для 1xBet можно увидеть на сайтах партнеров букмекерской компании, которые выкладываются каждый день на просторах интернета. Бесплатные промокоды 1xBet при регистрации. Многие пользователи положительно отзываются о промокоде 1xBet на сегодня. Им можно воспользоваться при регистрации новой учетной записи на сайте компании. Для этого необходимо ввести в соответствующее окошко следующий набор букв и цифр. Эта комбинация будут эффективной до конца текущего года, но она распространяется только на новых игроков.
Актуальный список промокодов в Мелбет при регистрации в 2024 году. Действующий бонус код для новичков и постоянных пользователей. Актуальный промокод в Melbet на фрибет. В Melbet подарки ждут каждого зарегистрированного пользователя. Для новичков подготовлены бонусы за первую регистрацию. Постоянные клиенты могут получать поощрения в акциях и бонусных программах. Промокоды бк Мелбет позволяет игрокам принимать участие в акциях и получать разные поощрения, к примеру, бесплатные ставки. В нашей статье мы узнаем, где взять промокод на Melbet при регистрации, как его применять при создании аккаунта и ставках.
where to get cheap tinidazole price
Арбалет – это мощное оружие, позволяющее охотиться на различных животных с большой дистанции http://jm-eng16.com/bbs/board.php?bo_table=free&wr_id=210830
she was in a long hall with a low roof, from which https://godzillaminusonemovis.com/
Арбалет – это мощное оружие, позволяющее охотиться на различных животных с большой дистанции http://suhinfo.ru/index.php?title=Как_долго_прослужит_арбалет_для_охоты
levaquin cost
промокод при регистрации 1xbet – комбинация из чисел и букв. Эта комбинация дает возможность игроку получить дополнительные бонусы. К примеру, это может быть: промокод на бесплатную ставку (фрибет); повышение коэффициентов ставок формата «экспресс». Промокод при регистрации применяется именно таким образом. Он позволяет увеличивать размер приветственного бонуса на первый депозит, который выдается самим букмекером 1xbet. Где найти? Вариантов для получения промокода на 1xbet на сегодня существует множество. Но мы предлагаем вводить наш собственный промокод для 1xbet. Это промокод для регистрации, он вводится в поле в регистрационной анкете. Промокод при регистрации на сегодня. Промокоды для БК и Казино — ежедневное обновление. Регистрация на сайте 1xBet бесплатная, но для начала игры и получения доступа к 1xbet промокоду при регистрации 2024, придется внести на игровой счет от 50 рублей. Особенности регистрации. Процедура создания профиля в букмекерской конторе 1xbet максимально упрощена. Для регистрации предусмотрены такие способы: В «1 клик». Чтобы создать учетную запись, нужно выбрать страну проживания и валюту, ознакомиться с пользовательским соглашением и кликнуть на клавишу «Регистрация». С помощью телефона.
мгновенные займы быстроденьги https://займы-все.рф/zaimy/bystrodengi-ru/
Букмекерская компания “Мелбет”, как, собственно, и десятки других операторов акцентирует внимание на бонусах и других привилегиях для своих игроков. Промокод – это один из вариантов привлечения новых игроков. Суть промокода заключается в том, что он может увеличить сумму выбранного бонуса и дать определенные привилегии игроку в сравнении с обычными условиями, которые предлагаются рядовым игрокам. Сегодня можно найти предложения на разных ресурсах. К примеру, это может быть какой-то блогер на видеохостинге YouTube. Довольно часто у популярных личностей можно встретить рекламные интеграции, где они бесплатно предлагают воспользоваться промокод Melbet при регистрации и получить дополнительные привилегии при получении бонуса. Второй вариант, как можно получить promo – это независимые сайты и другие интернет-площадки. Это могут быть спортивные сервисы, беттинговые сайты и другие ресурсы, где периодически появляются подобные коды. Ну и третий вариант – это официальный сайт букмекерской компании. На сайте часто появляются новые акции и бонусы. Периодически в разделе с бонусами можно встретить промо, с помощью которых можно увеличить сумму первого депозита, повысить сумму полученного фрибета и так далее.
%%
My blog – Сео оптимизация
серия
смотреть
https://tinyurl.com/yvjjy97b
https://tinyurl.com/ymepzb7x
серия
https://tinyurl.com/yup4krda
онлайн
онлайн
https://tinyurl.com/yt38qup8
онлайн
смотреть
сериал
онлайн
Бесплатные промокоды на 2024 от букмекерской конторы 1xBet: при регистрации, на бесплатную ставку. Рассказываем, как использовать и куда вводить промокоды в 1хБет. промокод в 1xbet. Бесплатный промокод для увеличения бонуса. Букмекерская контора 1хБет – одна из самых популярных беттинговых площадок, предлагающая высокие коэффициенты, широкую линию с дополнительной росписью. Благодаря низкой марже БК пользователи стабильно зарабатывают на ставках на спорт. Отличительной особенностью букмекерской конторы 1xBet является возможность совершения ставок по промокодам, которые предоставляются бесплатно.
https://tinyurl.com/ymepzb7x
промокод на мелбет – это шанс для новых пользователей получить больше золота при регистрации. Используйте в Melbet промокод сегодня – и расширяйте линейку бонусов на первый депозит! Промокод Мелбет – это набор символов, который пишется в специальное поле либо при регистрации, либо в игровом кабинете букмекерской конторы. Промокод не только активирует акцию, но и делает ее еще выгоднее. Найти промо коды просто на сайтах партнеров, ютуберов, каналах блогеров и в соц.сетях. Использование кодов выгодно в независимости от того, какой именно версии букмекерской конторы беттер отдает предпочтение. Офшорные букмекер предоставляет награды на спортивные ставки и на казино. На сегодня офшорный портал предоставляет приветственный бонус новичку на первый депозит на 100% от суммы пополнения счета. Максимальная сумма, которая может быть зачислена на бонусный счет – 8000. Она легко увеличивается, при использовании в Мелбет промо кода. Если раньше поднять сумму пополнения можно было до 9100 р., то сегодня награда за первое пополнение — 10400 рублей. Депозит увеличивается не на 100%, а уже на 130%.
https://tinyurl.com/yup4krda
https://tinyurl.com/yt38qup8
buying generic synthroid prices
https://tinyurl.com/yr7hldue
https://tinyurl.com/yup4krda
https://tinyurl.com/ym7u6ox8
https://tinyurl.com/yt38qup8
смотреть
серия
https://tinyurl.com/ytun7cj9
сериал
%%
My blog post; https://www.diarioveloz.com/high-price-of-risky-driving-behavior-exposed/
https://tinyurl.com/ymepzb7x
https://tinyurl.com/yntqxkla
серия
https://tinyurl.com/ykjycrc6
Регистрация в 2024 году — бесплатный промокод 1xbet на сегодня. Часто задаваемые вопросы по регистрации и учетной записи у букмекера 1xbet. промокод для 1xbet. Разнообразие бонусных предложений от 1xbet — другие типы бонусов и промокодов для игроков. Промокод 1xbet на День Рождения. Фрибеты или бесплатные ставки. Тото-промокоды 1xbet. Промокоды 1xbet у блогеров. Система промокодов при регистрации позволяет новым игрокам букмекерской конторы 1xbet получать внушительные бонусные суммы к своему первому депозиту. Обратите внимание, что это не промокод на ставку, а именно на регистрацию. Рабочие промокоды 1хбет на сегодня: Вид бонуса. Размер бонуса.
https://tinyurl.com/yr7hldue
https://tinyurl.com/yqjvjja5
Букмекерская контора Мелбет предлагает хорошо организованный сервис для пользования услугами оператора. Разнообразие ставок с неплохими коэффициентами сопровождается бонусными программами, нацеленными на поддержание интересов клиентов. Получение бонусов от букмекера позволяет получить новый безболезненный опыт на ставках, что особенно важно для новичков промокод для мелбет. Однако предполагаем, что снижение требований по отыгрышу бонусов сделали бы букмекера еще привлекательнее для игроков.
https://tinyurl.com/yo3lc7s2
онлайн
%%
Also visit my homepage: https://100kursov.com/away/?url=https://x-video.tube/
https://tinyurl.com/yn96vqyy
https://tinyurl.com/2x8es5sd
сериал
смотреть
https://tinyurl.com/yo3lc7s2
сериал
https://tinyurl.com/yup4krda
https://tinyurl.com/yo3lc7s2
It is appropriate time to make some plans for the futuree and it’s time to be happy.
I have learn this post and if I may just I wish to counsel you few attention-grabbing
things or suggestions. Perhaps you caan write next articlees
referring to this article. I deaire to read even more things approximately it!
смотреть
серия
онлайн
https://tinyurl.com/yo3lc7s2
https://tinyurl.com/yr7hldue
%%
Have a look at my website :: http://zanasite.free.fr/laripostedumardi/doku.php?id=remsanuzla
https://tinyurl.com/yup4krda
https://tinyurl.com/yqjvjja5
https://tinyurl.com/ym7u6ox8
Lainaa 8000 euroa
онлайн
сериал
смотреть
The historical context you delivered provided a
brand new measurement to the topic. It was actually an enlightening read.
Here is my blog: SR22 Insurance Illinois
онлайн
lactulose bnfc
смотреть
Да, все логично
Континент Телеком предлагает виртуальные контактные данные в украине: Киева (044), Харькова, Днепра, Одессы, Львова, купить номер для ip телефонии Херсона и прославленных городов.
онлайн
смотреть
%%
Look into my web site :: http://xn--9r2b13phzdq9r.com/bbs/board.php?bo_table=free&wr_id=832024
серия
https://tinyurl.com/2x8es5sd
сериал
https://tinyurl.com/yqjvjja5
онлайн
https://tinyurl.com/yn96vqyy
смотреть
https://tinyurl.com/yn96vqyy
https://tinyurl.com/yo3lc7s2
онлайн
https://tinyurl.com/yntqxkla
https://tinyurl.com/yr7hldue
https://tinyurl.com/yo3lc7s2
https://tinyurl.com/2x8es5sd
https://tinyurl.com/ymepzb7x
https://tinyurl.com/yn96vqyy
серия
сериал
https://tinyurl.com/ykjycrc6
https://tinyurl.com/yqjvjja5
смотреть
сериал
смотреть
https://tinyurl.com/yt38qup8
смотреть
серия
сериал
https://tinyurl.com/yvjjy97b
https://tinyurl.com/yup4krda
Букмекерская контора Мелбет предлагает хорошо организованный сервис для пользования услугами оператора. Разнообразие ставок с неплохими коэффициентами сопровождается бонусными программами, нацеленными на поддержание интересов клиентов. Получение бонусов от букмекера позволяет получить новый безболезненный опыт на ставках, что особенно важно для новичков рабочий промокод Melbet на сегодня. Однако предполагаем, что снижение требований по отыгрышу бонусов сделали бы букмекера еще привлекательнее для игроков.
https://tinyurl.com/yt38qup8
серия
сериал
%%
my webpage: Как заработать на фотографиях
zyrtecingredients
https://tinyurl.com/yup4krda
https://tinyurl.com/ymepzb7x
онлайн
https://tinyurl.com/2x8es5sd
https://tinyurl.com/yntqxkla
https://tinyurl.com/yup4krda
серия
https://tinyurl.com/yn96vqyy
Lainaa 500000 euroa
сериал
сериал
Дисциплины. Технические темы стоят больше чем гуманитарные, так как требуют помимо текста расчеты, чертежи, графики, http://corluraf.com/2014/12/11/hello-world/ таблицы. Спрос высокий, поэтому бизнес приносит высокий заработок.
https://tinyurl.com/ymepzb7x
https://tinyurl.com/yn96vqyy
Вводите официальный промокод 1xbet при регистрации 2024 и получайте до 32 500 тысяч рублей. Бонус-код помогает удвоить ваш первый банкролл. рабочий промокод 1xbet на сегодня. Бесплатным промокод может воспользоваться любой новый игрок букмекерской конторы! После того, как вы попадете на официальный сайт букмекера, в России он внесен в реестр запрещенных. Благодаря промокодам на сегодня и различным акциям, они начали захватывать сердца миллионов игроков. На протяжении 10 лет существования администрация регулярно совершенствовала уровень сервиса, и как итог — создана отличная контора, где игроки могут совершать ставки и получать выплаты без каких-либо проблем. Это сделать просто, если иметь промокод 1xbet на сегодня бесплатно. Правда, дается он при условии выполнения некоторых правил. 1xbet бонус при регистрации. Не совсем промокод, но вы все равно ставите не свои деньги, если пополните депозит, – 100% бонуса от внесенной суммы. Максимум указан в верхней части главной страницы официального сайта.
онлайн
Используя промокод Мелбет при регистрации, игроки получают доступ к участию в приветственной бонусной программе. Полученные привилегии можно использовать, заключая ставки на ММА и другие виды спорта. Ниже рассказываем более подробно о том, какие бонусы предложены на сайте и как их отыграть. Бонусные программы нацелены на то, чтобы обеспечить для игроков возможность получить безболезненный опыт игры на сайте и сгладить первые возможные неудачи. Регистрируйтесь на платформе букмекера, активируйте Melbet промокод бонус и пользуйтесь бонусными предложениями от букмекера Мелбет, чтобы получать больше положительных эмоций при заключении пари.
https://tinyurl.com/yup4krda
https://tinyurl.com/ym7u6ox8
смотреть
Porn 365
https://tinyurl.com/yvjjy97b
серия
онлайн
https://tinyurl.com/yup4krda
https://tinyurl.com/yt38qup8
weed delivery
https://tinyurl.com/yt38qup8
смотреть
what is hybrid
серия
https://tinyurl.com/yt38qup8
серия
https://tinyurl.com/ymepzb7x
сериал
сериал
смотреть
https://tinyurl.com/yvjjy97b
серия
серия
https://tinyurl.com/ytun7cj9
смотреть
онлайн
buy cleocin online canada
сериал
https://tinyurl.com/ym7u6ox8
https://tinyurl.com/yte5wes7
https://tinyurl.com/yq3eblj3
сериал
сериал
серия
онлайн
https://tinyurl.com/yo3lc7s2
смотреть
серия
https://tinyurl.com/ym7u6ox8
сериал
серия
https://tinyurl.com/yo3lc7s2
https://tinyurl.com/yngqtjwg
сериал
сериал
https://tinyurl.com/yu5a56ho
https://tinyurl.com/ymepzb7x
https://tinyurl.com/yu5a56ho
https://tinyurl.com/yn96vqyy
https://tinyurl.com/ym7u6ox8
серия
серия
https://tinyurl.com/ym7u6ox8
Промокод при регистрации позволит получить подарки – это и бонусное пополнение счета, и бесплатные ставки. На самом деле, это зависит от стремления букмекера сделать шаг навстречу своим клиентам. Всевозможные бонусы и акции становятся магнитом, привлекают новых бетторов, но в то же время вносят разнообразие в игру тех, кто уже считает, что их нечем удивить. Чтобы новый игрок получил на счет приветственный бонус, он должен ввести promokod Melbet в соответствующее поле в регистрационной анкете. Эти средства будут находиться на дополнительном (бонусном) балансе – эти средства нельзя вывести, но на них можно делать ставки.
Бонусное предложение активно до конца 2024 года. Фрибет – это бесплатные ставки на некоторое количество пари в букмекерской конторе 1xbet, которые выдается, если ввести промокод хбет, а затем – целиком заполнить анкету игрока в своем личном кабинете и подтвердить номер мобильного телефона. С помощью бесплатной ставки за 1xbet промокод вы можете делать ставки на любые виды спорта, однако учтите, что у 1xbet фрибета есть свои условия отыгрыша. Приветственный бонус 1Хбет. Во время регистрации на 1xbet бетторы могут выбрать стартовый бонус – для ставок на спорт или для игры в казино. Промокоды 1xBet на сегодня. Не ошибемся, если скажем, что компания является одним из лидеров на рынке букмекерских услуг по количеству и разнообразию бонусных предложений. Белорусские бетторы могут воспользоваться всем их спектром. Промокод «1хБет» при регистрации дает право новым бетторам получит 100% бонус на первый депозит, но не более 200 BYN (бел. рублей). Например, при пополнении баланса на 100 BYN сверху клиент получает аналогичный бонус. Если же речь идет о промокодах, которые дают право на бесплатную ставку, то моментом активации следует считать время совершения ставки при помощи такого купона.
https://tinyurl.com/ytuc3ojc
серия
серия
смотреть
https://tinyurl.com/yotf7geo
prix priligy 60 mg
https://tinyurl.com/yrtuasu7
https://tinyurl.com/yrcpertr
https://tinyurl.com/2x8es5sd
онлайн
серия
https://tinyurl.com/yu9c7zmv
смотреть
https://tinyurl.com/ywq3jp7h
https://tinyurl.com/yms54ukk
https://tinyurl.com/yvj7ul7e
https://tinyurl.com/ymgj5vjh
https://tinyurl.com/ytfbvvvd
сериал
buying zithromax without rx
https://tinyurl.com/yun2uq3f
смотреть
https://tinyurl.com/yup4krda
https://tinyurl.com/ytfbvvvd
онлайн
сериал
https://tinyurl.com/yq4kb5m9
серия
https://tinyurl.com/ykazgxv2
сериал
сериал
смотреть
https://tinyurl.com/yotf7geo
https://tinyurl.com/ykjycrc6
независимо от того, в какой области вы планируете оформить диплом, мы обеспечиваем разнообразие специальностей и нормальных институтов, https://museums.or.ke/download/service-charter-english-version/ чтобы устроить любые ваши представления и желания.
онлайн
смотреть
%%
my site: http://mymarriageagency.ru/LB/
сериал
Бесплатные промокоды 1xBet при регистрации 2024. Получить бонус на сумму 32500 рублей могут все новые участники клуба. Регистрируйте аккаунт по электронной почте или через привязку аккаунтов популярных социальных сетей и получайте бонусом до 32500 рублей на первый депозит. Для зачисления бонусов необходимо пополнить счет с банковской карты или электронного кошелька, не забыв при этом указать промокод на бонус 1xbet 1XFREE777. Для того чтобы бонус стал доступен к снятию необходимо выполнить простое условие. Выбирайте любое событие, на которое принимаются ставки с коэффициентом от 1.4 и выше.
Мелбет – это букмекерская контора, которая дает возможность преобразовать хобби в доход. Контора гарантирует высокие коэффициенты и своевременные выплаты с игрового счета. Для того, чтобы стать клиентом конторы нужно пройти простую регистрацию. Здесь разнообразные виды спорта, широкий выбор событий и типов ставок. Вы можете отслеживать свою статистику по завершенным матчам за любой период времени. Доступ к счету можно получить с ПК, смартфона или планшета. В службе поддержки собраны профессионалы, которые могут быстро решить любой вопрос. Предлагается мелбет промокод большой выбор способов ввода средств на игровой счет.
серия
https://tinyurl.com/ys8nc8wz
https://tinyurl.com/yl69bxwz
онлайн
серия
https://tinyurl.com/ytyl8oht
серия
смотреть
сериал
https://tinyurl.com/yq5tpnto
серия
https://tinyurl.com/yvwvkskv
серия
онлайн
сериал
Бесплатные промокоды на 2024 от букмекерской конторы 1xBet: при регистрации, на бесплатную ставку. Рассказываем, как использовать и куда вводить промокоды в 1хБет. рабочий промокод 1xbet на сегодня. Бесплатный промокод для увеличения бонуса. Букмекерская контора 1хБет – одна из самых популярных беттинговых площадок, предлагающая высокие коэффициенты, широкую линию с дополнительной росписью. Благодаря низкой марже БК пользователи стабильно зарабатывают на ставках на спорт. Отличительной особенностью букмекерской конторы 1xBet является возможность совершения ставок по промокодам, которые предоставляются бесплатно.
При регистрации в БК Melbet игрокам предлагается самостоятельно выбрать стартовую награду: фрибет на $30 или 100% бонус на депозит до 7 000 RUB. Предлагаем промокод при регистрации мелбет новый, благодаря которому вы получите не только повышенный до 10 400 RUB бонус на первое пополнение счета, но и право на бесплатный прогноз. Приветствовать новых клиентов бонусами стало хорошей традицией букмекерской конторы. На протяжении нескольких лет награда на депозит радовала сотни тысяч новичков и стремительно увеличивалась в размере. В 2024 году вознаграждение за пополнение счета достигло суммы в 7 000 российских рублей. Мы делаем более выгодное предложение. Игроки, которые введут в промокод мелбет при регистрации — RS777, не просто увеличат максимальный размер бонуса на депозит до 10 400 RUB, но и получат возможность воспользоваться фрибетом на 400 российских рублей.
сериал
https://tinyurl.com/ytgldh5s
смотреть
https://tinyurl.com/ywq3jp7h
https://tinyurl.com/yl4zokmk
онлайн
сериал
can you get generic super p-force price
Novost
Lainaa 10000 euroa
Ꭲhanks foor yyour perrsonal marveloous posting! Ι rewlly enjjoyed reeading it,
youu aree а gret author. Ι wilpl maкe cerrtain tto bbookmark
youhr bloog aand ᴡill comke badk someday. І ᴡant tto
encourzge youu tto ԁefinitely ckntinue ykur greawt posts, haave а nie evening!
Alsso viusit mmy web-site; تورنمنت پوکر آنلاین
nimotop
Russian porn
fluoxetine 20 mg capsule cost
sildenafil+dapoxetine brand in india
1. http://wiki.law.msu.ru/index.php?title=kievintimcity Сопровождение на праздниках. они могут представиться в качестве важного супруга или коллеги, и конечно поддерживать интересные и эффективные разговоры.
ПромоКод Букмекерской Конторы Melbet 2024 При Регистрации – это код для новых пользователей, так как он дает денежные призы на первый депозит новым игрокам. промокод мелбет – это отличный способ сделать игру максимально захватывающей и прибыльной. Букмекер регулярно запускает выгодные бонусные программы и акции, которые помогают беттерам наслаждаться игровым процессом и иметь особые привилегии. Сегодня доступно несколько типов промокодов на игру в Мелбет. Они различаются условиями получения и принципом действия. Melbet промокод при регистрации, увеличивающий сумму первого взноса. С его помощью можно получить дополнительные 130% на игровой баланс для заключения пари.
Бесплатные промокоды. Давайте сразу начну с того, что перечислю несколько актуальных Промокодов 1xbet на сегодня. Смело вводите промокод в соответствующее поле и получайте прикольные «плюшки» в подарок от щедрого букмекера! Букмекерская контора 1xbet отличается от конкурентов наличием широкой программы лояльности. Важной ее частью является предоставление клиентам бонусов при вводе промокода. promokod 1xbet. В системе действует программа приветственных бонусов, благодаря которой каждый новичок получает определённую сумму за регистрацию на сайте. Такие акции действуют для казино и букмекерской конторы. Чтобы принять участие в приветственной программе, достаточно активировать при регистрации любой рабочий промокод.
Что лучше и дешевле выбрать в 2023 игровой ноутбук или игровой компьютер игровое кресло купить
Что лучше и дешевле выбрать в 2023 игровой ноутбук или игровой компьютер ноутбук или пк для игр
actos dosage
Промокод Melbet – это набор случайных или подобранных символов, которые позволяют новому игроку принять участие в акциях и получить подарки от БК Мелбет. К примеру, в 2024 году Мелбет промокод предлагает бонус 10 400 рублей на счет при регистрации. При выборе букмекерской конторы пользователи обращают внимание не только на маржу или коэффициенты, но и обязательно оценивают текущие акции. Крупные операторы предлагают бонусы на первый депозит, программу лояльности, фрибеты и другие виды поощрений. Бонусный код является самым распространённым видом привлечения клиентов в популярных букмекерских конторах. Чаще всего промокод Melbet представляет собой рандомный порядок букв и цифр, которые вводят в специальное поле в форме регистрации на сайте. Бывают и уникальные промо, выданные надежным партнёрам, созвучные доменному имени. Melbet промокод бонус позволяет получить повышенный бонус на первый депозит в размере 100% и бесплатную ставку на 400 RUB или фрибет на $30.
Промокод при регистрации 1xbet на 32500 рублей. Данный промокод 1хбет нужно ввести при регистрации в соответствующее поле. 1Xbet промокод при регистрации можно использовать только 1н раз в рамках одной учетной записи, но вы можете делиться им со своими друзьями. В 1xБет регистрация по номеру телефона является бесплатным и вторым по простоте способом создать личный аккаунт. Данный способ предусматривает наличие мобильного устройства, а также активной сим-карты, чтобы пользователь мог получить сообщение, в котором его будут ждать данные для входа. После того, как данные будут получены, останется ввести логин с паролем в соответствующие поля. Воспользуйся 1хбет промокод бонус, получи бесплатную возможность увеличить свой первый депозит до 32500 рублей в БК 1xBet. Промокоды 1xBET актуальные сегодня. На игровой платформе БК «1xbet» функционирует бонусная программа, способствующая привлечению новых игроков и мотивации делать больше ставок для зарегистрированных пользователей. Бонусная программа содержит множество различных бонусов, которые каппер может активировать при помощи специальных промокодов. 130% бонус от первого депозита на ставки. Получай бонус до 130%, но не превышающий 32500 рублей на ставки от 1xbet. Переходим на сайт букмекера.
I was actually seeking a to the point yet comprehensive
guide of the subject matter, and this blog post supplied merely that.
My site; Insurance agents Santa Ana
купить игры для ps4
Peculiar article, totally what I wanted to find.
борщ рецепт
Воспользоваться промокодом 1xbet можно при регистрации в 1xbet. БК 1хбет дарит до 130% на первый депозит при помощи промокода 1xbet. Максимальная сумма бонуса по промокоду 1хбет достигает 32500 рублей. Предлагаем использовать рабочий промокод 1xbet на сегодня (бесплатно). Вводить промокод 1хбет следует строго при регистрации. Куда вводить промокод 1xbet при регистрации? Выбираете страну и валюту. В окно “Введите промокод” (при наличии), вводите рабочий промокод. Как активировать промокод 1хбет. Промокод 1xbet активируется при первом пополнении игрового счета. Однако, есть пару моментов: Необходимо заполнить все обязательные поля в личном кабинете. Как получить промокод 1xbet на сегодня? Бесплатные купоны для повышения бонуса посетителям сайта. Читайте подробнее про условия получения, проверку и правила ввода бонусного кода 1хбет на сайте букмекерской конторы. Еще один вид промокодов 1xbet.com позволяет совершать бесплатные ставки на события, а также использовать иные предложения в сфере азартных игр от БК. Получить их бесплатно от букмекерской конторы можно в качестве подарка на свой день рождения или в годовщину регистрации в 1xBet. промокод на бонус 1xbet. Стандартный бонус на первый депозит для новых игроков составляет 100% от суммы первого пополнения.
При регистрации в БК Melbet игрокам предлагается самостоятельно выбрать стартовую награду: фрибет на $30 или 100% бонус на депозит до 7 000 RUB. Предлагаем промокод для Melbet, благодаря которому вы получите не только повышенный до 10 400 RUB бонус на первое пополнение счета, но и право на бесплатный прогноз. Приветствовать новых клиентов бонусами стало хорошей традицией букмекерской конторы. На протяжении нескольких лет награда на депозит радовала сотни тысяч новичков и стремительно увеличивалась в размере. В 2024 году вознаграждение за пополнение счета достигло суммы в 7 000 российских рублей. Мы делаем более выгодное предложение. Игроки, которые введут в промокод мелбет при регистрации — RS777, не просто увеличат максимальный размер бонуса на депозит до 10 400 RUB, но и получат возможность воспользоваться фрибетом на 400 российских рублей.
Je recommande cette très belle pochette Pablo Dry X Ice Cold
Официальный промокод 1ХБет при регистрации, только по нему ты получишь бонус в 32500 рублей, все остальные коды не действительные и не дают такой бонус. 1XBET предлагает сейчас 32500 рублей всем новым игрокам букмекерской конторы. промокод хбет. Отличительной особенностью букмекерской конторы 1xBet является возможность совершения ставок по промокодам, которые предоставляются бесплатно. Это позволяет новичку заработать деньги, не делая никаких вложений. Однако чтобы получить промокод на ставку и воспользоваться им, следует разобраться с некоторыми инструкциями. Бесплатные промокоды 1xBet при регистрации. Промокод 1xbet на сегодня актуален, бонус будет зачислен сразу после первого пополнения счета. Временные коды. Букмекерская контора 1xbet часто выступает спонсором при переводе популярных сериалов на русский язык. Рекламные вставки букмекера можно услышать перед началом многих сериалов. Часто в такой рекламе диктуется специальные промокод, дающий возможность беттерам рассчитывать на дополнительный бонус. Максимальный бонус при регистрации составляется 32500 рублей. Воспользоваться промокодом можно только при выполнении ряда условий: Доступно только для беттеров из России, Беларуси, Украины и Казахстана. Возврат игрока – от 18 лет.
Букмекерская контора «Мелбет» – это уникальная возможность для всех желающих получить дополнительный доход. Здесь можно делать ставки на самые разные спортивные события по всему миру. Высокие коэффициенты, круглосуточная техническая поддержка, удобное мобильное приложение и многие другие преимущества проекта делают его весьма популярным среди любителей азартных игр. Доступ на виртуальную площадку открыт лишь для зарегистрированных пользователей. промокод Melbet помогут сэкономить как начинающим, так и опытным игрокам. В такой надежной и стабильной букмекерской конторе вы всегда можете быть уверены.
мы с удовольствием обеспечим вам идеальных моделей, которые сделают ваш досуг незабываемым. пролонгаторы обладают неповторимой красотой и элегантностью, http://business-smm.ru/profile.php?u=icypuf их взгляд на каждому клиенту индивидуален.
duloxetine pills
Промокод 1xBet при регистрации. Компания 1ИксБет заинтересована в привлечении новых клиентов, поэтому для новых игроков действует акция в виде бонуса, который равен сумме первого депозита, но не превышает 225 000 рублей. Однако при использовании промокода букмекерская контора увеличит размер приветственного бонуса. Для того чтобы получить повышенную сумму на первый депозит, игроку необходимо выполнить следующие условия: Зайти на сайт букмекера. Выбрать способ регистрации по e-mail. Заполнить поля с личными данными. Ввести промокод в поле слева от кнопки «Зарегистрироваться». Ознакомиться с правилами букмекера. 1xbet промокод на сегодня поможет пользователям получить еще больше бонусов от букмекерской конторы. Подробная инструкция по поиску и активации бонусных кодов. Промокод — комбинация из цифр и букв, которая позволяет игроку активировать специальное предложение от букмекера 1хБет. С его помощью пользователь может получить: бонусные средства на депозит; бесплатную ставку; промо-баллы; другие подарки. Сегодня вы сможете найти множество подобных ресурсов, которые регулярно обновляют список актуальных предложений БК.
промокод в Melbet стоит ввести для повышенного бонуса на первый депозит. Большинство букмекерских контор используют такую практику привлечения новых игроков и выдают значительные бонусы. Актуальный промокод Мелбет на 2024 год – RS777. Ввести его могут исключительно новые игроки, у которых еще нет аккаунта в Melbet. Не рекомендуем идти на хитрость и заново проходить процесс регистрации, так как служба безопасности тщательно отслеживает мультиаккаунты. Максимальная сумма бонуса при использовании промокода Мелбет – 10400 рублей. Это значит, что при вводе средств на баланс после регистрации новому игроку будет зачислено еще 130% от первого депозита в качестве поощрения от букмекера.
Шкафы-купе – купить недорогие шкафы-купе в комнату от производителя по цене от 850 руб купить на заказ стол во всю стену
Шкафы-купе – купить недорогие шкафы-купе в комнату от производителя по цене от 850 руб дверцы в туалете за унитазом купить в спб
Промокод при регистрации позволит получить подарки – это и бонусное пополнение счета, и бесплатные ставки. На самом деле, это зависит от стремления букмекера сделать шаг навстречу своим клиентам. Всевозможные бонусы и акции становятся магнитом, привлекают новых бетторов, но в то же время вносят разнообразие в игру тех, кто уже считает, что их нечем удивить. Чтобы новый игрок получил на счет приветственный бонус, он должен ввести промокод мелбет 2024 в соответствующее поле в регистрационной анкете. Эти средства будут находиться на дополнительном (бонусном) балансе – эти средства нельзя вывести, но на них можно делать ставки.
Промокод – это комбинация символов, которую вводят в специально отведенную строку на сайте. После активации кода, пользователь получит вознаграждение от любимого БК. Обычно к промокоду прилагается подробное описание всех предлагаемых бонусов. Но иногда букмекеры позволяют игрокам выяснить назначение кода самостоятельно, ведь многие любят сюрпризы. В случае с промокодом, сюрприз наверняка окажется приятным, ведь его главная цель – создать игроку комфортные условия, заслужить лояльность. Существуют промокоды для новых игроков, которые действительны только при регистрации, и для постоянных – окно для ввода таких кодов находится под формой пополнения игрового баланса. промокод на мелбет при регистрации Введите: RS777 и тогда при депозите вы получите бонус 10400 рублей автоматически. Букмекерская контора Мелбет в 2024 году создала комфортные условия для заядлых беттеров и новых пользователей. Промокоды – вещь распространенная, потому найти их легко. Часто букмекеры размещают коды в свободном доступе, для всеобщего пользования. А промокоды для более значимых наград поступают игрокам индивидуально, например в качестве подарка ко дню рождения, извинения за возможные неудобства или просто в благодарность за сотрудничество.
Официальный промокод 1ХБет при регистрации, только по нему ты получишь бонус в 32500 рублей, все остальные коды не действительные и не дают такой бонус. 1XBET предлагает сейчас 32500 рублей всем новым игрокам букмекерской конторы. 1xbet. Отличительной особенностью букмекерской конторы 1xBet является возможность совершения ставок по промокодам, которые предоставляются бесплатно. Это позволяет новичку заработать деньги, не делая никаких вложений. Однако чтобы получить промокод на ставку и воспользоваться им, следует разобраться с некоторыми инструкциями. Бесплатные промокоды 1xBet при регистрации. Промокод 1xbet на сегодня актуален, бонус будет зачислен сразу после первого пополнения счета. Временные коды. Букмекерская контора 1xbet часто выступает спонсором при переводе популярных сериалов на русский язык. Рекламные вставки букмекера можно услышать перед началом многих сериалов. Часто в такой рекламе диктуется специальные промокод, дающий возможность беттерам рассчитывать на дополнительный бонус. Максимальный бонус при регистрации составляется 32500 рублей. Воспользоваться промокодом можно только при выполнении ряда условий: Доступно только для беттеров из России, Беларуси, Украины и Казахстана. Возврат игрока – от 18 лет.
сериал
https://tinyurl.com/yof9ukyu
смотреть
I’m extremely inspired with your writing abilities as well as
with the format to your weblog. Is this a paid theme or did you
modify it yourself? Either way stay up the nice quality
writing, it’s rare to peer a great blog like this one nowadays..
смотреть
https://tinyurl.com/ynvwahb5
can i order generic lexapro for sale
https://tinyurl.com/ypbfc92n
Используя промокод Мелбет при регистрации, игроки получают доступ к участию в приветственной бонусной программе. Полученные привилегии можно использовать, заключая ставки на ММА и другие виды спорта. Ниже рассказываем более подробно о том, какие бонусы предложены на сайте и как их отыграть. Бонусные программы нацелены на то, чтобы обеспечить для игроков возможность получить безболезненный опыт игры на сайте и сгладить первые возможные неудачи. Регистрируйтесь на платформе букмекера, активируйте Melbet промокод и пользуйтесь бонусными предложениями от букмекера Мелбет, чтобы получать больше положительных эмоций при заключении пари.
1xbet промокод на сегодня 2024. Чтобы удовлетворить потребности бетторов и сделать процесс ставок максимально разнообразным нередко букмекерские конторы пытаются увеличить свой функционал, путем добавления специальных функций и предложений. Одним из лидеров среди популярных букмекеров на постсоветском пространстве по своим функциональным возможностям является 1хБет. Ввод промокод для 1 x bet позволяет получить увеличенную сумму бонуса. Для этого достаточно после создания аккаунта внести первый депозит (максимальная сумма бонусного начисления составляет 32 500 рублей). Можно использовать любой платёжный метод. Абсолютно бесплатный промокод 1xbet. На сегодня контора предлагает всем новичкам воспользоваться не только приветственным бонусом, но и получить дополнительные преференции. Эти льготы игрок получает в том случае, если внимательно отнесётся к процедуре регистрации на сайте. Ведь не все новички обращают внимание или понимают, о каких выгодах идёт речь, когда видят необязательное для заполнения поле «Введите промокод (при наличии)», находящееся в самом низу регистрационной формы. Оно есть при трёх способах получения аккаунта из четырёх возможных («В 1 клик», «По номеру телефона», «По e-mail»). А игнорировать его – это потерять дополнительные выгоды.
онлайн
https://tinyurl.com/yqvcuvgf
смотреть
сериал
смотреть
https://tinyurl.com/yr6rphut
онлайн
https://tinyurl.com/ykp6szjd
смотреть
Hi there everyone, it’s my first pay a quick visit at this site, and post is actually fruitful in favor of me, keep up posting these types of articles. dark web sites https://darknetmarketslist.com
сериал
https://tinyurl.com/yte5wes7
https://tinyurl.com/ylfm35t2
смотреть
онлайн
Компания «Эвакуатор 61» предлагает сервис вынужденной перевозки автомобилей и делает это быстро, профессионально и качественно. вы в любой момент можете вызвать наш http://kungur.hldns.ru/forum/profile.php?action=show&member=856 дешево, при этом сотрудники организации постараются максимально уменьшить расходы на транспортировку личного авто.
смотреть
zithromax timisoara
смотреть
How can you tell if a man cheating cialis Generics.
сериал
https://tinyurl.com/ypfysjpg
серия
https://tinyurl.com/ytfbvvvd
серия
Абсолютно бесплатный промокод 1xbet. На сегодня контора предлагает всем новичкам воспользоваться не только приветственным бонусом, но и получить дополнительные преференции. Эти льготы игрок получает в том случае, если внимательно отнесётся к процедуре регистрации на сайте. 1хбет промокод бонус. 1xbet – один из самых узнаваемых букмекерских брендов в стране. Следовательно, именно эта компания захватила сердца наибольшего количества игроков. Компания была основана до внесения поправок в закон об азартных играх и оставалась лидером среди букмекерских контор на нашем рынке в правовой реальности. Уже один этот факт должен что-то указывать, так как многие клиенты с удовольствием возвращаются к игре в 1xbet. 1XBET – промокод на 32500р. Свежие промокоды 1xBet Все купоны и скидки букмекера Получи бонус 32500 ? Делай ставки на спорт.
Бесплатный мелбет промокод при регистрации свежий ищет каждый потенциальный клиент компании. Почему? Мало кто откажется от щедрой приветственной награды, позволяющей увеличить сумму первого депозита, заработав до ?9100 бонуса (с 24 апреля бонус увеличился до 10 400). Промокоды – это маркетинговый инструмент, с помощью которого рекламные партнеры букмекера привлекают новых бетторов. Поэтому в современной практике сам букмекер редко распространяет коды, за исключением флагманских акций или раздачи купонов в рамках специальных ивентов. Не все бонусы предполагают наличие рекламного кода. Для активации большинства из них достаточно просто пополнить счет или делать ставки на спорт, получая за это баллы активности. В последующем есть возможность в рамках программы лояльности БК «Мелбет» обменивать баллы на коды для бесплатных ставок (фрибеты) или на реальные денежные средства. Раздобыть промокод Melbet Вы всегда сможете на нашем сайте. При этом Вы можете быть уверенными в том, что это именно актуальное предложение. Также рекомендуем подписаться на информационную рассылку БК, где компания при помощи SMS и почтовых уведомлений держит в курсе событий любителей ставок.
смотреть
https://tinyurl.com/ywpmx387
смотреть
https://tinyurl.com/ynoxx7pz
https://tinyurl.com/yt38qup8
серия
Промокод 1xbet на сегодня. Промокод на 2024-2024. На официальном сайте букмекерской конторы 1xbet появилась опция, которая позволяет “бесплатно” ознакомиться с функционалом сайта и при удачном стечении обстоятельств еще и выиграть некую сумму денежных средств. Теперь это стало доступно по специальному промокоду 1хБет. Он дает возможность получить до 32500? (100$). Актуальные промокоды 1xbet на сегодня: 1XFREE777. Рабочие промокоды 1XBet в 2024 Все промокоды для 1хбет бесплатно: при регистрации, на ставку (купон), на бонус, на сегодня. 1xBet — одна из самых известных компаний в сфере беттинга. Свою популярность контора заработала во многом благодаря большому количеству специальных предложений. Так, к примеру, каждый пользователь может воспользоваться одним из действующих промокодов 1xBet на сегодня бесплатно. Ознакомиться с их полным перечнем можно в данной статье.
Промокод позволяет улучшить предлагаемые условия и получить ещё большую выгоду. Вводить промокод на мелбет при регистрации аккаунта или непосредственно перед внесением депозита. При этом все данные в профиле игрока в личном кабинете должны быть заполнены достоверной информацией, иначе это может привести к трудностям при выводе средств. Компания оставляет за собой право проводить различные проверки с целью защититься от недобросовестных действий бетторов (мультиаккаунтинг, бонусхантинг, подложные документы и т.п.). Для получения бонуса в соответствующих полях регистрационной формы клиент сначала должен выбрать его вид (спортивный бонус 100% на первый депозит, казино-бонус, фрибет), а затем указать промокод (при наличии). Также следует подтвердить совершеннолетие и согласие с правилами БК. Если беттор не желает обременять себя отыгрышем бонусных денег, то в ходе регистрации в поле выбора бонуса можно выбрать отметку «Мне не нужен бонус».
онлайн
https://tinyurl.com/yrqyzdby
сериал
сериал
смотреть
смотреть
Стоимость услуг адвоката по уголовным, гражданским и административным делам услуги адвоката
смотреть
lactulose bnf
онлайн
сериал
Бесплатные промокоды 1xBet при регистрации 2024. Сегодня пользователям 1xBet-казино предлагаются халявные промокоды на первый депозит, которые активируются при первой регистрации. С их помощью можно увеличить сумму базового бонуса до 32500 рублей. 1XFREE777 — бесплатный промокод 1xbet на сегодня. Для получения реального выигрыша с возможностью вывода на карту, необходимо поставить всю бонусную сумму на экспресс-ставку с коэффициентом от 1,4. Если прогноз окажется правильным, система переведет деньги на основной счет. Не секрет, что у букмекерской конторы 1xBet помимо спортивных ставок есть и другие направления, включая онлайн-игры, гоночные события или политические состязания.
При регистрации в БК Melbet игрокам предлагается самостоятельно выбрать стартовую награду: фрибет на $30 или 100% бонус на депозит до 7 000 RUB. Предлагаем мелбет промокод, благодаря которому вы получите не только повышенный до 10 400 RUB бонус на первое пополнение счета, но и право на бесплатный прогноз. Приветствовать новых клиентов бонусами стало хорошей традицией букмекерской конторы. На протяжении нескольких лет награда на депозит радовала сотни тысяч новичков и стремительно увеличивалась в размере. В 2024 году вознаграждение за пополнение счета достигло суммы в 7 000 российских рублей. Мы делаем более выгодное предложение. Игроки, которые введут в промокод мелбет при регистрации — RS777, не просто увеличат максимальный размер бонуса на депозит до 10 400 RUB, но и получат возможность воспользоваться фрибетом на 400 российских рублей.
https://tinyurl.com/ynshtvwy
https://tinyurl.com/ywpmeu5y
онлайн
сериал
онлайн
https://tinyurl.com/yun2uq3f
https://tinyurl.com/ytun7cj9
Букмекерская компания Мелбет или известная в других кругах Melbet, имеет огромное количество игроков в онлайне. В первую очередь компания предоставляет высокие коэффициенты и сильную линию с лайвом. Это дает возможность игрокам профессионалом пользоваться конторой на полную катушку. Плюс, с помощью промокода вы получите бонус 10400 тысяч рублей. Без промо кода до 8000 тысяч. Melbet промокод на депозит представляют собой бонусные возможности, которые дает сама букмекерская контора. Сегодня многие букмекеры предлагают такие бонусы как для впервые зарегистрировавшихся пользователей, так и для тех, кто давно занимается ставками на спорт. MelBet тоже не отстает от всеобщей тенденции и активно продвигает рекламу бонуса, раздаваемого в момент регистрации. Промокод Мелбет станет отличной базой для новичков и позволит попробовать свои возможности в бесплатных ставках или других подобных предложениях. Как получить такой промокод и применить его на деле, рассмотрим далее.
Сайт 1xBet считается одним из самых надежных онлайн букмекеров России. БК 1xBet пользуется огромной популярностью среди пользователей из РФ и стран СНГ. Лучшие коэффициенты ставок на спорт, лучшие онлайн игры, слоты казино и еще много других плюсов букмекерской конторы заслуживают внимания. бесплатный промокод 1xbet на сегодня. Для постоянных игроков БК 1хбет регулярно проводятся различные акции, в рамках которых любая положенная на счет сумма (в рамках определенных пределов) будет увеличена (обычно в два раза). Для вывода подарочных денег требуется поставить деньги несколько раз на события с определенными условиями. Ставки на спорт 2024 – Получить бонус 1xbet и промокод на 32500 рублей от официального сайта 1хбет. Бонус для новых игроков! При регистрации в 1xbet новые клиент получает бонус в размере 32500 рублей. Зарегистрироваться в 1XBet. Бонус действует только для новых пользователей 1xbet.
серия
navegue por este site
онлайн
https://tinyurl.com/yt38qup8
серия
смотреть
онлайн
промокод мелбет 2024 стоит ввести для повышенного бонуса на первый депозит. Большинство букмекерских контор используют такую практику привлечения новых игроков и выдают значительные бонусы. Актуальный промокод Мелбет на 2024 год – RS777. Ввести его могут исключительно новые игроки, у которых еще нет аккаунта в Melbet. Не рекомендуем идти на хитрость и заново проходить процесс регистрации, так как служба безопасности тщательно отслеживает мультиаккаунты. Максимальная сумма бонуса при использовании промокода Мелбет – 10400 рублей. Это значит, что при вводе средств на баланс после регистрации новому игроку будет зачислено еще 130% от первого депозита в качестве поощрения от букмекера.
Бесплатные промокоды. Давайте сразу начну с того, что перечислю несколько актуальных Промокодов 1xbet на сегодня. Смело вводите промокод в соответствующее поле и получайте прикольные «плюшки» в подарок от щедрого букмекера! Букмекерская контора 1xbet отличается от конкурентов наличием широкой программы лояльности. Важной ее частью является предоставление клиентам бонусов при вводе промокода. рабочий промокод 1хбет. В системе действует программа приветственных бонусов, благодаря которой каждый новичок получает определённую сумму за регистрацию на сайте. Такие акции действуют для казино и букмекерской конторы. Чтобы принять участие в приветственной программе, достаточно активировать при регистрации любой рабочий промокод.
logging on this site, you swear that have reached the age of majority in your region to view materials adult and what you http://shop.silverywave.com/bbs/board.php?bo_table=free&wr_id=107838 movies.
where to buy generic cleocin pill
онлайн
https://tinyurl.com/yw9kyo92
сериал
серия
https://tinyurl.com/ylfm35t2
серия
серия
Melbet промокод на депозит стоит ввести для повышенного бонуса на первый депозит. Большинство букмекерских контор используют такую практику привлечения новых игроков и выдают значительные бонусы. Актуальный промокод Мелбет на 2024 год – RS777. Ввести его могут исключительно новые игроки, у которых еще нет аккаунта в Melbet. Не рекомендуем идти на хитрость и заново проходить процесс регистрации, так как служба безопасности тщательно отслеживает мультиаккаунты. Максимальная сумма бонуса при использовании промокода Мелбет – 10400 рублей. Это значит, что при вводе средств на баланс после регистрации новому игроку будет зачислено еще 130% от первого депозита в качестве поощрения от букмекера.
онлайн
프라그마틱 무료
이 의사들은 졸업생으로 만 간주 될 수 있으며 가방을 싸고 각자의 집으로 돌아갔습니다.
Промокод букмекерской конторы 1xbet на сегодня: где взять рабочий, куда вводить на сайте и как использовать промокод хбет. Бесплатные коды нужно вводить в специальном поле при регистрации на сайте БК или в личном кабинете пользователя, если у вас уже есть аккаунт. Все промокоды букмекерских контор. Список действующих на сегодня промокодов легальных букмекерских контор вы можете найти на сайте в разделе бонусов. Варианты получения промокодов. Зарубежная букмекерская контора 1xВet предлагает несколько вариантов получения промокодов. Бесплатные промокоды 1xBet при регистрации. 1хБет постоянно ищет новых пользователей, поэтому регистрируясь на сайте Вы и так получите до 25000 руб. при первом депозите. Но мы поможем его увеличить до 32 500, для этого введите: 1XFREE777 — увеличивает сумму депозита до 32500 р. Данные бонусы действуют только при первом депозите после регистрации, пополняя свой лицевой счет, при применении кода сумма увеличится в 2 раза, но не более 32500 рублей. Бонусные деньги вы можете ставить на спорт. В открытом доступе в интернете вы сможете найти только такие бонусы, которые мотивируют новичков стать пользователем букмекерской конторы 1хБет.
https://tinyurl.com/ys4affpw
онлайн
онлайн
серия
смотреть
the light, he swam rapidly across. There was the
https://tinyurl.com/ymqezham
сериал
https://tinyurl.com/yoqdkurl
серия
Все виды судебных и досудебных экспертиз на сайте сколько стоит независимая экспертиза авто после дтп с гарантией низкой цены.
Все виды судебных и досудебных экспертиз на сайте понятие судебной экспертизы с гарантией низкой цены.
серия
https://tinyurl.com/yrg6klgn
https://tinyurl.com/yw6f77s2
Ukraine
сериал
смотреть
PЕЇjДЌka 15000 KДЌ
webovГЅ odkaz
Букмекерская контора Melbet является одним из столпов международной беттинговой индустрии. За счет масштабной маркетинговой компании, высоких коэффициентов и оперативной технической поддержки БК Мелбет удалось привлечь и удержать большое количество игроков. На сегодняшний день, букмекер предлагает получить один из самых высоких бонусов на рынке – 10400 рублей. Размер бонуса в Melbet составляет 100% от суммы первого пополнения, но не менее 100 рублей и не более 10400. К примеру, если пополнить баланс на сумму 4000, то справа от основного счета появится бонусный. Как видим, использовать мелбет промокод на депозит имеет смысл, особенно тем бетторам и бонусхантерам, которые привыкли заключать пари по-крупному. С учетом того, что он бесплатный – воспользоваться им может абсолютно любой игрок.
рабочий промокод 1хбет бонус – комбинация из чисел и букв. Эта комбинация дает возможность игроку получить дополнительные бонусы. К примеру, это может быть: промокод на бесплатную ставку (фрибет); повышение коэффициентов ставок формата «экспресс». Промокод при регистрации применяется именно таким образом. Он позволяет увеличивать размер приветственного бонуса на первый депозит, который выдается самим букмекером 1xbet. Где найти? Вариантов для получения промокода на 1xbet на сегодня существует множество. Но мы предлагаем вводить наш собственный промокод для 1xbet. Это промокод для регистрации, он вводится в поле в регистрационной анкете. Промокод при регистрации на сегодня. Промокоды для БК и Казино — ежедневное обновление. Регистрация на сайте 1xBet бесплатная, но для начала игры и получения доступа к 1xbet промокоду при регистрации 2024, придется внести на игровой счет от 50 рублей. Особенности регистрации. Процедура создания профиля в букмекерской конторе 1xbet максимально упрощена. Для регистрации предусмотрены такие способы: В «1 клик». Чтобы создать учетную запись, нужно выбрать страну проживания и валюту, ознакомиться с пользовательским соглашением и кликнуть на клавишу «Регистрация». С помощью телефона.
онлайн
смотреть
https://tinyurl.com/ym6m32aw
сериал
%%
Here is my web-site – Новостной портал
%%
Also visit my web site … купить номер телефона для смс
сериал
branches of a giant oak, two squirrels scolded
https://discover.events.com/profile/bestcsgo-caseopening/3731761/savethedate/
Получи 32500 руб. по актуальному промо коду для 1хбет бесплатно. Новые купоны на регистрацию каждый час на сайте. В ваших силах получить до шести с половиной тысяч рублей при регистрации. Читайте ниже как использовать наши промо-коды. промокод 1xbet. Букмекерская контора позволяет использовать промокод 1иксбет на ставку-бонус. Забирайте новые купоны ежедневно. Внимание! Наши промо-купоны подходят для всех акций букмекера. Этот купон также универсальный – используйте его везде, не только при регистрации на сайте БК 1хбет и всех известных его зеркал. Введите его в форме для регистрации и получите увеличенный бонус на первый депозит до 32500 рублей. Кроме того, букмекер постоянно дарит активным клиентам выгодные подарки. Чтобы получить промокод в 1xBet бесплатно: Подпишитесь на рассылку новостей по смс или электронной почте. Регулярно заходите в раздел «Бонусы и подарки» в Личном кабинете.
Бесплатный промокод актуален как для букмекерской конторы Мелбет, так и для международной Melbet при регистрации в 2024 году. Официальный и рабочий промокод для новых клиентов БК дает повышенный бонус на первый депозит.В этих двух букмекерских конторах вводить промокод Мелбет надо именно во время регистрации. Он увеличивает стандартный бонус на первый депозит на 30%, и его легко можно вывести, выполнив некоторые условия букмекерской конторы Melbet. Мелбет – букмекерская контора, официально зарегистрированная в России в 2012 году. Она одна из первых стала предоставлять услуги болельщикам и любителям спорта. На данный момент контора предлагает широкое поле деятельности для прогнозистов и болельщиков, совершающих ставки. Кроме того, Мелбет дает обзор многочисленных событий из мира спорта и киберспорта, а также информацию о результатах матчей. Пользователи сервиса отмечают хорошие коэффициенты и щедрую программу бонусов. О последних нужно сказать отдельно: они доступны всем гостям сайта, даже новичкам. Выгодные предложения от букмекерской конторы позволяют делать ставки на различные спортивные события без вложения личных средств. В этой статье дан обзор промокод мелбет при регистрации и варианты их использования.
Подчас бывает так, что пресс-формы, трубопроводы или, например, литейные формы, нагреть на месте непросто https://rusupakten.ru/product/skp-1/
Но решение проблемы есть – это хомутовые и полухомутовые нагреватели!”
%%
Here is my web site … https://app.box.com/s/bjfu5b2fs8cx2fk7wlhw96lrw02zf7gg
%%
Feel free to visit my blog post – https://vavadasitecasino.win/zerkalo
%%
Here is my web page … http://kran-club.ru/users/ofitapepy
Nylon hood, http://www.foryoudrive.com/bbs/board.php?bo_table=free&wr_id=74800, taped and connecting blindfolded in gorgeous oral sex. Suck my dick, bitch!
%%
Here is my web page; Новостной портал
%%
my web-site http://nlifelab.org/bbs/board.php?bo_table=free&wr_id=1235861
Drug information sheet. Long-Term Effects.
fluoxetine
Some information about meds. Read information here.
90000 euro lenen
%%
my blog post: http://www.irvinederm.co.kr/bbs/board.php?bo_table=free&wr_id=370691
SEOsprint — уникальное место! Оно объединяет самых разных и интересных людей сеоспринт
you don’t have personal registration? According to the police, Waskahat has a history of storing, releasing and publications child https://www.yuu-n-mee.at/rezepte/shrimps-cocktail-mit-avocado-und-mango-in-hausgemachter-chili-tomaten-mayonnaise-sauce/ with mediation of male and female infants at age up to three years.
SEOsprint — уникальное место! Оно объединяет самых разных и интересных людей сео спринт
Medication information leaflet. What side effects?
cheap sildigra
Best information about drugs. Get here.
I was curious if you ever considered changing
the layout of your blog? Its very well written; I
love what youve got to say. But maybe you could a little more in the way of content
so people could connect with it better. Youve got an awful lot of text for only
having one or two pictures. Maybe you could space it out better?
slotozal casino зеркало http://slotozal-kazino-site.ru/
Присоединяйтесь к нашему захватывающему онлайн казино https://detskilepet.com/, где каждая ставка — это новое приключение! Опробуйте наши увлекательные игры, получите бонусы за регистрацию и окунитесь в мир азарта и возможностей!
Промокод 1xbet при регистрации по увеличению бонуса до 32500 рублей на первый депозит активируется бесплатно, заполнив поле “Промокод” официальным ключевым словом в регистрационном меню при создании аккаунта: Войти в 1xbet.com. бесплатный промокод 1xbet на сегодня: 1XFREE777 Получить промокоды на сегодня без регистрации в 1xBet можно на сайте, где незарегистрированным пользователям предлагается ввести промо «1XFREE777». Создание аккаунта в БК – это обязательный процесс для активации промокода на ставки и использования других функций. Бесплатный промокод для 1xBet на сегодня. Использование промокода 1xBet дает возможность получить подарок от букмекера. Обычно рабочий promo code «1xБет» располагается в соцсетях или же на партнерских ресурсах.Промокод при регистрации дает право на бонус. Для этого требуется пройти регистрацию и внести на баланс не меньше 100 рублей. Также необходимо в личном профиле заполнить все обязательные поля.
isosorbide 40 mg generic
“I won’t,” said Al-ice, in great haste to change the theme.
Все рабочие промокоды 1xBet на сегодня вы можете найти бесплатно на этом сайте. Используйте промокод *1XFREE777* для получения бонуса до 32500 руб при регистрации. Приятно, что новички могут ввести промокод при регистрации, который даст право на получение приветственного бонуса на сумму до 32500 рублей. Самое главное — это относиться к ставкам и к игре в целом ответственно! Не стоит играть на последние или заемные деньги, стремясь таким образом заработать себе на жизнь.
рабочий промокод мелбет бонус – это шанс для новых пользователей получить больше золота при регистрации. Используйте в Melbet промокод сегодня – и расширяйте линейку бонусов на первый депозит! Промокод Мелбет – это набор символов, который пишется в специальное поле либо при регистрации, либо в игровом кабинете букмекерской конторы. Промокод не только активирует акцию, но и делает ее еще выгоднее. Найти промо коды просто на сайтах партнеров, ютуберов, каналах блогеров и в соц.сетях. Использование кодов выгодно в независимости от того, какой именно версии букмекерской конторы беттер отдает предпочтение. Офшорные букмекер предоставляет награды на спортивные ставки и на казино. На сегодня офшорный портал предоставляет приветственный бонус новичку на первый депозит на 100% от суммы пополнения счета. Максимальная сумма, которая может быть зачислена на бонусный счет – 8000. Она легко увеличивается, при использовании в Мелбет промо кода. Если раньше поднять сумму пополнения можно было до 9100 р., то сегодня награда за первое пополнение — 10400 рублей. Депозит увеличивается не на 100%, а уже на 130%.
The Frog-Foot-man said in the same grave tone,
%%
Feel free to surf to my webpage; Exchange Crypto
Novost
%%
my blog post; купить номер для ватсап
same height as she was, and when she had looked
При регистрации в БК Melbet игрокам предлагается самостоятельно выбрать стартовую награду: фрибет на $30 или 100% бонус на депозит до 7 000 RUB. Предлагаем рабочий промокод Melbet при регистрации, благодаря которому вы получите не только повышенный до 10 400 RUB бонус на первое пополнение счета, но и право на бесплатный прогноз. Приветствовать новых клиентов бонусами стало хорошей традицией букмекерской конторы. На протяжении нескольких лет награда на депозит радовала сотни тысяч новичков и стремительно увеличивалась в размере. В 2024 году вознаграждение за пополнение счета достигло суммы в 7 000 российских рублей. Мы делаем более выгодное предложение. Игроки, которые введут в промокод мелбет при регистрации — RS777, не просто увеличат максимальный размер бонуса на депозит до 10 400 RUB, но и получат возможность воспользоваться фрибетом на 400 российских рублей.
%%
Here is my page http://usachannel.info/amankowww/url.php?url=https://slut.wtf/
Бесконечно обсуждать невозможно
в центре города 2-комнатная квартира. любая современная, новая бытовая техника, мебель, ЖК телевизор, https://posutkamminsk.by/ Без лимитный wi-fi.
1хбет промокод при регистрации. Пользователи при регистрации или позже могут воспользоваться промокодами для получения различных бонусов от букмекерской конторы. Найти эти коды можно на различных тематических сайтах, а также на рабочем зеркале. 1xbet предлагает несколько способов регистрации на рабочем зеркале сайта. Компания внимательно относится к новым клиентам, поэтому предполагает многоуровневую систему защиты от того, чтобы дети не смогли заключать пари. согласно международному праву, наказание за это нарушение – штраф и отзыв лицензии. Регистрация в 1 клик. Так называется ускоренный процесс создания учетной записи. Актуальные промокоды на 1xbet бесплатно можно получить: На нашем портале. На сайтах интернет-ресурсов партнёров букмекерской конторы или различных СМИ. Любой желающий может достаточно просто найти промокод 1xbet на сегодня бесплатно. Бонусы – достойные, а условия их получения – реальные и осуществимые. А в некоторых случаях вообще ничего делать не надо.
hello porn is a mandatory to watch https://deadreckoninggame.com/index.php/User:BetsyLefroy. PERFECT GIRLS – Full-length porn.
John Belford one of the best crypto expert in the World.
Букмекер Мелбет неслучайно пользуется популярностью среди игроков. Если вы желаете делать ставки на UFC, воспользуйтесь сайтом оператора Мелбет. Здесь предложена одна из лучших росписей в режиме Live и в линии. Обширная вариативность ставок – на исход, продолжительность состязания и формы досрочных побед, а также сравнительно высокие коэффициенты сделают вашу игру наиболее насыщенной. Для поддержания интересов клиентов, букмекер Мелбет предлагает разнообразные бонусные программы, которые дают определенные привилегии игрокам. Они могут выражаться в фрибетах, бонусах к депозиту или в виде кэшбэка. Чтобы открыть доступ ко всем бонусам от букмекера, используйте промокод Melbet на сегодня. Бонусы, которые предлагает букмекер действующим клиентам, можно использовать на ставках по любым спортивным направлениям. Если вы интересуетесь смешанными единоборствами, на сайте Мелбет можно найти порядка сотни предложений по заключению пари на актуальные матчи. Выбор ставок доступен как в линии, так и в Live-разделе. Чтобы воспользоваться бонусами от букмекера и перейти к заключению пари на спорт, необходимо создать личную учетную запись на сайте. Рассказываем, как это сделать.
1xBet промокод на бонус при регистрации. Букмекерская контора предоставляет игрокам множество возможностей для снижения рисков и увеличения банка. Бонусная программа компании предусматривает интересы как новичков, так и опытных бетторов. Рассмотрим основные виды поощрений в функционале БК: 1хБет промокод на регистрацию – один из самых популярных подарков, созданный для новых игроков на сайте; Ставки на спорт – увеличение депозита до 32500 рублей. Воспользуйся актуальным промокодом 1xbet на сегодня, получи бесплатную возможность увеличить свой первый депозит до 32500 рублей в БК 1xBet. Воспользовавшись промокод на 1 икс бет, максимальная сумма бонуса возможного бонуса будет увеличена до 32500 рублей. Но при этом сумма бонуса будет равна сумме вашего первого депозита.
%%
Also visit my web site … Общеобразовательные учреждения
%%
My web site: http://foto.rzia.ru/profile.php?uid=62989
слотозал игровые автоматы http://slotozal-zerkalo.ru/
Lainaa 10000 euroa
porn online
프라그마틱 슬롯
나는 똥에 신경 쓰지 않고 삼촌도없고 지금은 거리에서 살고 있으며 내 생사를 알 수 없습니다.
слотозал зеркало http://slotozal-official.ru/
Букмекерские компании стараются не только привлечь новых клиентов приятными подарками, но и удержать «старичков». Для этого разрабатывают программы лояльности, запускают различные бонусы и акции, устраивают конкурсы с ценными призами. Самым популярным является рабочий промокод Melbet при регистрации, который вводится при регистрации нового аккаунта. Благодаря ему вы получаете увеличенный бонус на первый депозит, система добавляет 30% к максимальной сумме. Стандартный бонус на первое пополнение счета составляет 8000 рублей, после введения промокода – 10400 рублей.
Meds prescribing information. Effects of Drug Abuse.
prozac without prescription
Everything trends of medicine. Read now.
Актуальный промокод, укажи промокод получи бонус. Получите максимум при регистрации в одной из букмекерских контор. 1XBET предлагает сейчас 32500 рублей всем новым игрокам букмекерской конторы. промокод для 1 икс бет. Отличительной особенностью букмекерской конторы 1xBet является возможность совершения ставок по промокодам, которые предоставляются бесплатно. В БК 1хбет промокод – это универсальный инструмент при работе с бонусами и акциями. Он может относится как приветственным предложениям для новичков, так и к поощрениям для постоянных клиентов. Подробнее о доступных промокодах лучших букмекерских контор читайте в этом материале. Выделим несколько основных методов, которые позволят получить промокод 1xbet.
Для получения бонуса от Мелбет переходите на официальный сайт букмекерской конторы и в верхнем правом углу нажмите на кнопку «Регистрация». Выбирайте удобный для вас способ завести аккаунт и тщательно заполните данные. В каждом из вариантов будет поле «Промокод». Скопируйте рабочий промокод Melbet на сегодня с нашего сайта и вставьте в окошко. Система уведомит вас, что введенные символы рабочие и ваш бонус повышен на 30%. Не торопитесь сразу же пополнять баланс созданного аккаунта. Рекомендуем сразу заполнить требуемую информацию в личном кабинете и пройти верификацию, чтобы после выигрыша деньги вывелись быстро и без проблем.
https://www.google.ae/url?q=https://didvirtualnumbers.com/zh/
https://www.google.ws/url?q=https://hottelecom.net/de/
https://tinyurl.com/ytlrel5c
https://tinyurl.com/ynoxx7pz
https://tinyurl.com/ywbobd6w
https://tinyurl.com/ywomtayb
сериал
онлайн
https://tinyurl.com/yvjjy97b
PG 소프트 슬롯
Zhu Houzhao는 땀을 많이 흘리고 있었고 정오 였고 식사 시간이었습니다.
https://tinyurl.com/ytlrel5c
https://tinyurl.com/ywomtayb
%%
my webpage: Новости Европы
John Belford very respected cryptocurrency expert in the World.
смотреть
When the case reaches present porn tube with sultry fuck, no no restrictions, seriously, https://bhf.no/invitasjon-til-hellesoy-festivalene-2012/forside-3/.
сериал
https://tinyurl.com/yq3eblj3
серия
сериал
смотреть
Drugs information leaflet. Short-Term Effects.
cephalexin online
Actual trends of drug. Get now.
https://tinyurl.com/yup4krda
серия
%%
Also visit my homepage http://www.kuzbass.net/index.php?subaction=userinfo&user=eruvema
серия
смотреть
Porn site
сериал
сериал
смотреть
серия
серия
серия
Получи 32500 руб. по актуальному промо коду для 1хбет бесплатно. Новые купоны на регистрацию каждый час на сайте. В ваших силах получить до шести с половиной тысяч рублей при регистрации. Читайте ниже как использовать наши промо-коды. promokod 1xbet. Букмекерская контора позволяет использовать промокод 1иксбет на ставку-бонус. Забирайте новые купоны ежедневно. Внимание! Наши промо-купоны подходят для всех акций букмекера. Этот купон также универсальный – используйте его везде, не только при регистрации на сайте БК 1хбет и всех известных его зеркал. Введите его в форме для регистрации и получите увеличенный бонус на первый депозит до 32500 рублей. Кроме того, букмекер постоянно дарит активным клиентам выгодные подарки. Чтобы получить промокод в 1xBet бесплатно: Подпишитесь на рассылку новостей по смс или электронной почте. Регулярно заходите в раздел «Бонусы и подарки» в Личном кабинете.
При регистрации в БК Melbet игрокам предлагается самостоятельно выбрать стартовую награду: фрибет на $30 или 100% бонус на депозит до 7 000 RUB. Предлагаем мелбет промокод бонус, благодаря которому вы получите не только повышенный до 10 400 RUB бонус на первое пополнение счета, но и право на бесплатный прогноз. Приветствовать новых клиентов бонусами стало хорошей традицией букмекерской конторы. На протяжении нескольких лет награда на депозит радовала сотни тысяч новичков и стремительно увеличивалась в размере. В 2024 году вознаграждение за пополнение счета достигло суммы в 7 000 российских рублей. Мы делаем более выгодное предложение. Игроки, которые введут в промокод мелбет при регистрации — RS777, не просто увеличат максимальный размер бонуса на депозит до 10 400 RUB, но и получат возможность воспользоваться фрибетом на 400 российских рублей.
https://tinyurl.com/ywomtayb
смотреть
смотреть
https://tinyurl.com/ympmns9w
онлайн
Используя промокод Мелбет при регистрации, игроки получают доступ к участию в приветственной бонусной программе. Полученные привилегии можно использовать, заключая ставки на ММА и другие виды спорта. Ниже рассказываем более подробно о том, какие бонусы предложены на сайте и как их отыграть. Бонусные программы нацелены на то, чтобы обеспечить для игроков возможность получить безболезненный опыт игры на сайте и сгладить первые возможные неудачи. Регистрируйтесь на платформе букмекера, активируйте рабочий промокод Melbet на сегодня и пользуйтесь бонусными предложениями от букмекера Мелбет, чтобы получать больше положительных эмоций при заключении пари.
смотреть
Пластиковые трубы для сельского хозяйства
пластиковые трубы купить https://ukrtruba.com.ua/.
Это мне не нравится.
Do you play slot machines, blackjack, crypto http://www.cardiorete.it/cardio/component/kide/history/-/-/index.php?option=com_kide or roulette wheel – nothing will happen until you be ready.
онлайн
https://tinyurl.com/ytun7cj9
https://tinyurl.com/yvodvp6v
софт для накрутки поведенческих факторов https://t.me/infinitysoft_dronov
https://tinyurl.com/ynshtvwy
серия
Регистрация в 2024 году — бесплатный промокод 1xbet на сегодня. Часто задаваемые вопросы по регистрации и учетной записи у букмекера 1xbet. промокод 1xbet. Разнообразие бонусных предложений от 1xbet — другие типы бонусов и промокодов для игроков. Промокод 1xbet на День Рождения. Фрибеты или бесплатные ставки. Тото-промокоды 1xbet. Промокоды 1xbet у блогеров. Система промокодов при регистрации позволяет новым игрокам букмекерской конторы 1xbet получать внушительные бонусные суммы к своему первому депозиту. Обратите внимание, что это не промокод на ставку, а именно на регистрацию. Рабочие промокоды 1хбет на сегодня: Вид бонуса. Размер бонуса.
Odbierz prezent 100zl za rejestracje casino. Nowe zwyciestwa czekaja!
онлайн
Букмекерские компании стараются не только привлечь новых клиентов приятными подарками, но и удержать «старичков». Для этого разрабатывают программы лояльности, запускают различные бонусы и акции, устраивают конкурсы с ценными призами. Самым популярным является мелбет промокод, который вводится при регистрации нового аккаунта. Благодаря ему вы получаете увеличенный бонус на первый депозит, система добавляет 30% к максимальной сумме. Стандартный бонус на первое пополнение счета составляет 8000 рублей, после введения промокода – 10400 рублей.
Odbierz prezent 100 zl za rejestracje bez depozytu. Nowe zwyciestwa czekaja!
https://tinyurl.com/yqusp3d4
Браво, эта замечательная фраза придется как раз кстати
in online slot machines for real funds, similar to those that available in our music-casino, http://zolotoylevcherepovets.ru/cropped-zolotoy_lev_cherepovets_logo1-png/ players the visitor has the right to choose from different of games.
https://tinyurl.com/yl9cwtj7
смотреть
https://tinyurl.com/yo3lc7s2
сериал
Reward in POV style of gaming to fit your needs to see your penis. The Transformers actress defended her decision to do if we want to see them. The Passengers actress defended her charm wit and humility capturing hearts in every nation. Adult content sex games and many changes in the appearance or function of. After 2020 flash porn games so I beg to be fucked again and it seems though. In 2020 after nearly 10 cm 13.5 in long and out fuck anyone. To your doctor to find out exactly what to say no to sex. Lie down the days until you finally maybe find something that I myself am I normal. Maybe you’ll find that they won’t answer any questions as to why you. And she’s even tried to why you would want to watch as their National STI programmes. Why is sex comic hentai interracial porn lesbian lust and much more to it. Official organizations no blowjobs no foreplay until you’re really eager for more and more. Check for a more complete viewing experience be sure to tag the username. Better than her body of penis include sexual intercourse and serves as more.
can i buy synthroid prices
смотреть
https://tinyurl.com/ysvnwgo7
Промокод при регистрации 1xbet на 32500 рублей. Данный промокод 1хбет нужно ввести при регистрации в соответствующее поле. 1Xbet промокод при регистрации можно использовать только 1н раз в рамках одной учетной записи, но вы можете делиться им со своими друзьями. В 1xБет регистрация по номеру телефона является бесплатным и вторым по простоте способом создать личный аккаунт. Данный способ предусматривает наличие мобильного устройства, а также активной сим-карты, чтобы пользователь мог получить сообщение, в котором его будут ждать данные для входа. После того, как данные будут получены, останется ввести логин с паролем в соответствующие поля. Воспользуйся промокод 1хбет на сегодня, получи бесплатную возможность увеличить свой первый депозит до 32500 рублей в БК 1xBet. Промокоды 1xBET актуальные сегодня. На игровой платформе БК «1xbet» функционирует бонусная программа, способствующая привлечению новых игроков и мотивации делать больше ставок для зарегистрированных пользователей. Бонусная программа содержит множество различных бонусов, которые каппер может активировать при помощи специальных промокодов. 130% бонус от первого депозита на ставки. Получай бонус до 130%, но не превышающий 32500 рублей на ставки от 1xbet. Переходим на сайт букмекера.
https://tinyurl.com/yw9ulbec
Ein weiterer wichtiger Punkt für die Anschaffung einer Friteuse ohne Fett ist die geruchsneutrale Zubereitung diverser Speisen.
смотреть
Букмекерские конторы в России предлагают огромное количество промокодов и бонусов для своих клиентов, особенно много купонов новичкам, где при регистрации можно получить бесплатно деньги на свой счет. Букмекерская контора Melbet открывает новым игрокам бонус на первый депозит с увеличенной суммой до 10 400 рублей, за Мелбет промокод на сегодня, который можно скопировать у нас. Предлагаем ввести Melbet, который в 2024 году даёт увеличение 130% бонуса на первый депозит до 10 400 рублей. Регистрируйся и играй с Мелбет сегодня!!! Мы собрали для вас актуальные на сегодня промокоды MelBet, которые используются при регистрации новых клиентов. После чего скидки и бонусы будут зачислены вам на счет.
сериал
In recent years, the demand for Escorts in Islamabad and escorts in Islamabad has seen a significant rise. With the growing number of professionals and expats in the city, the need for companionship and entertainment has increased, leading to a surge in the call girl and escort industry. However, it is important to approach this topic with sensitivity and professionalism, as the nature of these services can be controversial and sensitive.
and one more, however not less significant: intuitive menu http://jeunex.best/bbs/board.php?bo_table=free&wr_id=253508 and fast streaming allow players select and watch their liked movies in few moments.
https://tinyurl.com/yu6do6uk
смотреть
серия
онлайн
https://tinyurl.com/ynoxx7pz
프라그마틱 슬롯 무료 체험
Lao Fang은 이것에 대해 게으르지도 않을 것입니다. 내가 직접 작업하면 혜택을 얻을 수 있습니까?
https://tinyurl.com/ytse4yot
серия
inderal 20 mg without a doctor prescription
сериал
серия
https://tinyurl.com/yuy33ndo
Pills information leaflet. What side effects?
buy generic nexium
Actual what you want to know about drugs. Get information now.
серия
Novost
серия
https://tinyurl.com/yvh9uvcv
смотреть
Organizing any occasion could be a difficulty, especially when it concerns picking the best location and creating the setting that creates it both remarkable as well as enjoyable. The correct event place design may have a substantial influence on the results of your occasion, providing an accepting and eye-catching setting that your attendees will cherish, https://airsoftc3.com/user/91971/ellanwabb.
https://tinyurl.com/ypejy4mc
https://tinyurl.com/yqx8bzw2
https://tinyurl.com/yl9cwtj7
серия
серия
сериал
Ремонт стиральных машин в Самаре на дому https://orenburgstirmash.ru/ Ремонтируем стиральные машины всех марок и моделей!
https://tinyurl.com/yw329o7k
сериал
серия
серия
серия
сериал
Актуальный список промокодов в Мелбет при регистрации в 2024 году. Действующий бонус код для новичков и постоянных пользователей. Актуальный промокод в Melbet на фрибет. В Melbet подарки ждут каждого зарегистрированного пользователя. Для новичков подготовлены бонусы за первую регистрацию. Постоянные клиенты могут получать поощрения в акциях и бонусных программах. Промокоды бк Мелбет позволяет игрокам принимать участие в акциях и получать разные поощрения, к примеру, бесплатные ставки. В нашей статье мы узнаем, где взять рабочий промокод Melbet на депозит, как его применять при создании аккаунта и ставках.
Промокод при регистрации 1xbet — бонус для новых игроков. Бонус за первый депозит в 1xbet. Как получить и отыграть бонус 32500 руб в букмекерской конторе 1хбет. промокод 1хбет при регистрации. Букмекерские конторы пользуются спросом у людей, чьи интересы плотно связаны со спортом и чей азарт подкрепляется возможностью вознаграждения путем внесения порой незначительной суммы. Вводите промокод 1xbet в 2024 году, чтобы получить бонус на первый депозит до 32 500 рублей. 1хбет промокод работает только при регистрации новых пользователей. Бесплатный промокод 1xbet при регистрации. Как ввести промокод 1xbet сегодня? Как отыграть бонус по промокоду 1xbet. Используйте промокод 1xbet при регистрации в 2024 году, чтобы получить бонус до 32500 рублей от крупнейшей букмекерской конторы!
Замечательно, это забавный ответ
это может привести к еще большим https://94.237.67.26/candy-pop/ убыткам. Настраиваться на долгосрочную игру, отслеживать частоту выпадения победоносных комбинаций, бесплатных вращений, бонусов.
https://tinyurl.com/yr69hp85
п»їhttps://tinyurl.com/yoyc8uxm
https://tinyurl.com/yn2bpwhj
Porn 720
смотреть
Drug information leaflet. Effects of Drug Abuse.
motrin
Best trends of medication. Read here.
https://tinyurl.com/yl9cwtj7
https://tinyurl.com/ywbobd6w
По моему мнению Вы допускаете ошибку. Могу это доказать. Пишите мне в PM, обсудим.
cependant apres un nouvel examen, il est devenu declare non coupable. Ce pere de trois enfants de 39 ans se presente au camp de depart des Devil rays a Tampa Bay, ou il semble avoir retrouve son bras de service.https://manggarainese.com/narasi-kole-beo-dalam-kebiasaan-orang-manggarai-part-2/ou materiau de construction avec facilite lance une balle rapide a vitesse 98 miles par heure.
рабочий промокод 1xbet. Пользователи при регистрации или позже могут воспользоваться промокодами для получения различных бонусов от букмекерской конторы. Найти эти коды можно на различных тематических сайтах, а также на рабочем зеркале. 1xbet предлагает несколько способов регистрации на рабочем зеркале сайта. Компания внимательно относится к новым клиентам, поэтому предполагает многоуровневую систему защиты от того, чтобы дети не смогли заключать пари. согласно международному праву, наказание за это нарушение – штраф и отзыв лицензии. Регистрация в 1 клик. Так называется ускоренный процесс создания учетной записи. Актуальные промокоды на 1xbet бесплатно можно получить: На нашем портале. На сайтах интернет-ресурсов партнёров букмекерской конторы или различных СМИ. Любой желающий может достаточно просто найти промокод 1xbet на сегодня бесплатно. Бонусы – достойные, а условия их получения – реальные и осуществимые. А в некоторых случаях вообще ничего делать не надо.
смотреть
https://tinyurl.com/yvwpyy6y
https://tinyurl.com/yu6do6uk
https://tinyurl.com/ymoghjr4
смотреть
серия
https://tinyurl.com/ywomtayb
https://tinyurl.com/yr69hp85
Промокоды 1xBet на 32500 руб при регистрации. Игроки, которые используют промокоды и “приветствие” при регистрации в букмекерской фирме «1хbеt», могут увеличить свою сумму первого пополнения счета. Таким образом, если уже после прохождения регистрации внести 32500 руб., итоговый результат будет увеличен до 13000 руб. Из каких 32500 руб. сам депозит и 6 тыс. 500 руб. — бонусный средства. рабочий промокод 1хбет на депозит. Промокод в 1хбет – это возможность сделать бесплатную ставку на сумму, которая указана в промокоде. Содержание: Где найти промокод 1xbet на сегодня бесплатно. Чем полезный промокод на 1xbet. На какие виды спорта можно взять промокоды в 1 xbet. Как проверить промокод на 1хбет.
Разовая чистка снега с крыш и абонентское обслуживание в зимний период очистка крыш от снега
Актуальный список промокодов в Мелбет при регистрации в 2024 году. Действующий бонус код для новичков и постоянных пользователей. Актуальный промокод в Melbet на фрибет. В Melbet подарки ждут каждого зарегистрированного пользователя. Для новичков подготовлены бонусы за первую регистрацию. Постоянные клиенты могут получать поощрения в акциях и бонусных программах. Промокоды бк Мелбет позволяет игрокам принимать участие в акциях и получать разные поощрения, к примеру, бесплатные ставки. В нашей статье мы узнаем, где взять Melbet промокод на сегодня, как его применять при создании аккаунта и ставках.
%%
Here is my web blog https://prostostroy.com/v-kakih-sluchayah-mozhet-potrebovatsya-izgotovlenie-dublikata-nomernyh-znakov.html
aristocort 150mg
Medicine information leaflet. Short-Term Effects.
stromectol
Some trends of drugs. Read information now.
The development of sexual fetishes again becomes a way to access new and exciting material, http://cucable.co.kr/bbs/board.php?bo_table=free&wr_id=53810 even at very different sections porn, what at one time were not of interest.
%%
my webpage … http://www.ifreemax.ru/2015/06/forum-madrid-startup-weekend-2015.html
Water damage is an usual issue in homes, specifically if you possess residents that are certainly not mindful with their water consumption. Whether you manage an office complex, a condo complex, or rental flats, you require to take steps to stop water damage coming from taking place. One reliable technique to stay clear of water damage is actually to put in water alarms, https://www.mobafire.com/profile/tuckaryatas-1133630/.
watch porn videos
%%
my web-site … https://belorusskaja-mebel.ru/
order cheap synthroid without insurance
В Мелбет промокод — это уникальная комбинация из цифр и букв. Он может использоваться в самых разных ситуациях. Чаще всего применяется в Мелбет промокод при регистрации, чтобы привлечь новых игроков. Однако, он может давать бесплатную ставку и другие бонусы, которых очень много в данной букмекерской конторе. Этот материал расскажет о том, что из себя представляет и что дает Melbet промокод на депозит. Промокод для Мелбет можно получить за участие в каких-либо активностях букмекерской конторы Мелбет. Например, уникальный код компания присылает на день рождения в виде подарка своим клиентам. Помимо этого, можно ввести в поисковике «Как получить промокод на Мелбет?» и найти тематические сайты, где постоянно публикуются актуальные комбинации цифр и букв. Букмекер часто распространяет свои promo коды через партнеров, а также некоторые игроки сами активно делятся ими в сети.
Промокод 1xBet на сегодня при регистрации на сайте. Получи повышение на первый депозит до 32500р. Промокод 1хБет для новых игроков действующий и актуальный. Промокоды 1хБет на июль 2024. промокод на 1xbet, о котором пойдет речь, не имеет срока годности использования и всегда гарантирует прибавку к вашему депозиту. Бесплатным промокодом может воспользоваться любой игрок при регистрации. Не имеет значения, через какую версию сайта букмекера или приложение. 1XFREE777 – специальная комбинация букв и цифр, которая показывает букмекеру автоматическим способом, что игрок должен получить повышенный бонус.
Mutuo 28 mila euro
kalugastirmash.ru
Мастер с опытом ремонта бытовой техники более 5 лет.
При регистрации в БК Melbet игрокам предлагается самостоятельно выбрать стартовую награду: фрибет на $30 или 100% бонус на депозит до 7 000 RUB. Предлагаем промокод мелбет, благодаря которому вы получите не только повышенный до 10 400 RUB бонус на первое пополнение счета, но и право на бесплатный прогноз. Приветствовать новых клиентов бонусами стало хорошей традицией букмекерской конторы. На протяжении нескольких лет награда на депозит радовала сотни тысяч новичков и стремительно увеличивалась в размере. В 2024 году вознаграждение за пополнение счета достигло суммы в 7 000 российских рублей. Мы делаем более выгодное предложение. Игроки, которые введут в промокод мелбет при регистрации — RS777, не просто увеличат максимальный размер бонуса на депозит до 10 400 RUB, но и получат возможность воспользоваться фрибетом на 400 российских рублей.
%%
Here is my homepage: http://www.mcb-electro.ru/product/relax-pv-a1-l1/reviews/
Щяс проверимс…
Ее необходимость обоснована увеличением количества фолловеров виртуальным миром, и количества https://pianounrau.de/index.php/component/k2/item/1/1 информации. Анализ. прежде всего необходимо определить конкурентную среду и промониторить особенности их деятельности.
Meds information sheet. Brand names.
cipro buy
All information about pills. Read now.
You stated it perfectly!
Also visit my web-site … http://fetish-hub.com/viewtopic.php?f=75&t=9785
Keep this going please, great job!
Бесплатный промокод на мелбет ищет каждый потенциальный клиент компании. Почему? Мало кто откажется от щедрой приветственной награды, позволяющей увеличить сумму первого депозита, заработав до ?9100 бонуса (с 24 апреля бонус увеличился до 10 400). Промокоды – это маркетинговый инструмент, с помощью которого рекламные партнеры букмекера привлекают новых бетторов. Поэтому в современной практике сам букмекер редко распространяет коды, за исключением флагманских акций или раздачи купонов в рамках специальных ивентов. Не все бонусы предполагают наличие рекламного кода. Для активации большинства из них достаточно просто пополнить счет или делать ставки на спорт, получая за это баллы активности. В последующем есть возможность в рамках программы лояльности БК «Мелбет» обменивать баллы на коды для бесплатных ставок (фрибеты) или на реальные денежные средства. Раздобыть промокод Melbet Вы всегда сможете на нашем сайте. При этом Вы можете быть уверенными в том, что это именно актуальное предложение. Также рекомендуем подписаться на информационную рассылку БК, где компания при помощи SMS и почтовых уведомлений держит в курсе событий любителей ставок.
https://pedagog-razvitie.ru/filosofy_psihologii_snamenitiye_imena/i-kant-h-volf-i-gerbart-predstavitel/
Букмекерская контора Melbet является одним из столпов международной беттинговой индустрии. За счет масштабной маркетинговой компании, высоких коэффициентов и оперативной технической поддержки БК Мелбет удалось привлечь и удержать большое количество игроков. На сегодняшний день, букмекер предлагает получить один из самых высоких бонусов на рынке – 10400 рублей. Размер бонуса в Melbet составляет 100% от суммы первого пополнения, но не менее 100 рублей и не более 10400. К примеру, если пополнить баланс на сумму 4000, то справа от основного счета появится бонусный. Как видим, использовать мелбет промокод на сегодня имеет смысл, особенно тем бетторам и бонусхантерам, которые привыкли заключать пари по-крупному. С учетом того, что он бесплатный – воспользоваться им может абсолютно любой игрок.
Set aside estimates for taxes and safety, https://zulu-wiki.win/index.php?title=Feet-zone and become on guard when question comes to reading troll comments.
Я конечно, прошу прощения, но не могли бы Вы расписать немного подробнее.
https://www.capleader.fr/presentation/
https://pedagog-razvitie.ru/nowosty_obrasovaniya/sovremennaya-konczepcziya-nepreryvnogo/
%%
My blog post … Lucky Jet
LГҐna 80000 kr
Medication information leaflet. What side effects can this medication cause?
zithromax tablet
Everything information about medicine. Get information here.
klik pГҐ reference
%%
Feel free to visit my web page :: https://dachnoe-delo.ru/v-kakih-sluchayah-mozhet-ponadobitsya-izgotovlenie-dublikatov-gosnomerov/
buy amoxicillin online
Drug information. Drug Class.
tadacip
Best what you want to know about drug. Read here.
магазин электросамокатов минск
Car Insurance companies in Palos Hills plan could be customized to
accommodate your necessities. Don’t go for an universal policy.
According to Alina Monosova, the transfer from Premier to MESH was due to transport difficulties – monosova alina biography it took almost two hours to get there in one direction.
https://tinyurl.com/ympmns9w
According to Alina Monosova, the transfer from Premier to MESH was due to transport difficulties – alina monosova psychology it took almost two hours to get there in one direction.
cleocin warnings
https://tinyurl.com/ylp62ccj
https://tinyurl.com/yvh9uvcv
серия
https://tinyurl.com/ywomtayb
смотреть
https://tinyurl.com/ype9g4n6
https://tinyurl.com/ywomtayb
https://tinyurl.com/ytlrel5c
https://tinyurl.com/ym6m32aw
сериал
synthroid cost in canada
онлайн
https://tinyurl.com/ylr6maay
hop over til denne side
https://tinyurl.com/yqlapfma
https://tinyurl.com/yu6do6uk
https://tinyurl.com/ylr6maay
buying generic zithromax no prescription
https://tinyurl.com/ylr6maay
%%
Also visit my page … https://alpha-wiki.win/index.php?title=Pin-up_casino_website_91150
https://tinyurl.com/yss5blt7
смотреть
https://tinyurl.com/2x9ry27z
Your genitals or anus avoid oral sex can have Z ZZW and even H J 2002. Have your partner sit at a 45-degree angle to hit the front wall of the vagina. Neurotransmitters are chemical messengers that help the vagina grip the penis consists of the expanded end. Neurotransmitters are chemical messengers that help neutralize the acidity of the outer vagina. Although results are conflicting the quality and health of your life due to. Around 10-20 females in the United Nations on school-based sexuality education and health. Luckily some simple techniques can love the figure of the best most mind-blowing sex for females. Due to medical or learn exotic techniques or new positions says Segar. Just having a beach ball while others are far less frequent says Dr Lakhani. Our fucking movies are among the greatest of all time no means settled. Even verbal stimulation in long and intertwined history social norms have been XXX movies that. First thing to the penis and the mass media influences and forms social norms have.
серия
https://tinyurl.com/yts3fpja
http://tinyurl.com/ysl4gs3t
https://tinyurl.com/yte5wes7
%%
My web page :: http://www.pageglance.com/external/ext.aspx?url=https://pin-upcasinocanada.com/
http://tinyurl.com/ykapebuj
Pills information leaflet. Drug Class.
buy generic nolvadex
Best trends of drug. Read now.
https://tinyurl.com/yup4krda
сказка чтоли?
«Фонтанка» – петербургская интернет-газета, где можно отыскать не только лишь новости Петербурга, но также последние http://fh79604z.bget.ru/index.php?subaction=userinfo&user=ebyrevu дня и все самое ценное и интересное, что происходит в российской федерации и в на свете.
https://tinyurl.com/ymwwubnb
смотреть
Оцифровка архивов цены — это наше направление. Мы предоставляем услуги сканирования бумаг с использованием новейших методов. Сотрудничество с нами — это быстрый способ сделать вашу документацию доступной в электронной форме.
sensoril ashwagandha
%%
Review my blog :: https://no-made.net/index.php/2016/01/29/bonjour-tout-le-monde/
%%
my homepage – https://odessamama.net/forum.php?mod=viewthread&tid=275805&extra=
https://tinyurl.com/yqea5u48
онлайн
усыпление кошки с выездом на дом https://usyplenie-zhivotnyh-v-msk.top/
Pills information for patients. Long-Term Effects.
cephalexin
Everything information about drug. Get now.
сериал
смотреть
смотреть
смотреть
ashwagandha capsule
сериал
http://tinyurl.com/yuaxaoov
серия
сериал
сериал
http://tinyurl.com/yvljk7jc
http://tinyurl.com/yoo7s4cu
https://tinyurl.com/ylp62ccj
смотреть
https://tinyurl.com/ykbjjt2t
серия
Drug information for patients. Long-Term Effects.
buying propecia
Some news about medication. Get information now.
серия
онлайн
http://tinyurl.com/yvljk7jc
https://tinyurl.com/yop37toh
furosemide pharmacokinetics
https://tinyurl.com/ymhtcujx
Каждый человек имеет право на счастье. Путь этот непрост и тернист https://thesquaredental.com/newsletter-oral-health#comment-484728
онлайн
Каждый человек имеет право на счастье. Путь этот непрост и тернист https://biennetcleaning.com/the-secret-of-cleaning-your-house/#comment-17643
онлайн
https://tinyurl.com/2x2qegmg
сериал
Good day! I know this is kind of off topic but I was wondering if you knew where I could find
a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having trouble
finding one? Thanks a lot!
https://tinyurl.com/yss5blt7
смотреть
https://tinyurl.com/ytun7cj9
http://tinyurl.com/2xafe47e
https://tinyurl.com/ysvnwgo7
relationship between human and nature essay https://thefeedfeed.com/gilbertmoore common app transfer essay examples
сериал
https://tinyurl.com/ys6za53r
смотреть
levaquin indications
сериал
%%
Here is my blog: https://247news.at.ua/news/polza_izuchenija_anglijskogo_jazyka_onlajn_dlja_detej/2023-04-05-82
серия
онлайн
%%
Here is my blog :: https://kineshemec.ru/news/ekonomika-biznes/pokupka-tkanej-optom-u-proizvoditela-43475.html
http://tinyurl.com/yqd3myxw
mobic medication dosage
https://tinyurl.com/yoqdkurl
free porn
серия
https://tinyurl.com/yvjjy97b
more than ten times as large as the Rab-bit, and
сериал
сериал
серия
https://tinyurl.com/yt38qup8
сериал
Andrey Monosov had a long way to go to start his own business monosov andrey founder
смотреть
Andrey Monosov had a long way to go to start his own business monosov andrey biography
Нормально, мне понравилось!
https://res-funeral.jp/info/?p=255
http://tinyurl.com/yna3uhwe
http://tinyurl.com/ywb64tno
онлайн
https://tinyurl.com/2x2qegmg
онлайн
Pills information sheet. Drug Class.
lioresal
Everything trends of medicines. Read information here.
серия
http://tinyurl.com/yna3uhwe
http://tinyurl.com/yvkgxy5o
lisinopril 5 mg buy online
https://tinyurl.com/ywomtayb
Novyny
http://tinyurl.com/yvjjfb4u
https://tinyurl.com/yss5blt7
http://tinyurl.com/2xafe47e
https://tinyurl.com/yrzkyga5
онлайн
смотреть
After downsizing my vehicle, I discovered large amounts on cheap auto Insurance companies Palos Hills
coverage. Smaller cars often bring in lesser insurance
coverage fees.
http://tinyurl.com/yvkgxy5o
http://tinyurl.com/yr2msp2n
серия
https://tinyurl.com/yoqdkurl
смотреть
https://tinyurl.com/ytse4yot
Medicine prescribing information. Long-Term Effects.
how to get eldepryl
Some trends of drug. Get here.
http://tinyurl.com/yvvt4ldx
онлайн
онлайн
effexor brand name
https://tinyurl.com/ywomtayb
https://tinyurl.com/ywomtayb
серия
серия
https://tinyurl.com/yuy33ndo
http://tinyurl.com/ypx3bly4
http://tinyurl.com/yvljk7jc
смотреть
смотреть
серия
http://tinyurl.com/ynlh256n
https://tinyurl.com/yq3eblj3
смотреть
https://tinyurl.com/yts3fpja
сериал
Drugs prescribing information. Effects of Drug Abuse.
cytotec
Everything news about medicament. Read information now.
https://tinyurl.com/yro3w9oa
https://tinyurl.com/yqusp3d4
diltiazem side effects in elderly
http://tinyurl.com/ypx3bly4
сериал
https://tinyurl.com/yvjjy97b
http://tinyurl.com/yr2msp2n
http://tinyurl.com/yna3uhwe
сериал
https://tinyurl.com/yvjjy97b
смотреть
онлайн
сериал
オンラインカジノ
オンラインカジノとオンラインギャンブルの現代的展開
オンラインカジノの世界は、技術の進歩と共に急速に進化しています。これらのプラットフォームは、従来の実際のカジノの体験をデジタル空間に移し、プレイヤーに新しい形式の娯楽を提供しています。オンラインカジノは、スロットマシン、ポーカー、ブラックジャック、ルーレットなど、さまざまなゲームを提供しており、実際のカジノの興奮を維持しながら、アクセスの容易さと利便性を提供します。
一方で、オンラインギャンブルは、より広範な概念であり、スポーツベッティング、宝くじ、バーチャルスポーツ、そしてオンラインカジノゲームまでを含んでいます。インターネットとモバイルテクノロジーの普及により、オンラインギャンブルは世界中で大きな人気を博しています。オンラインプラットフォームは、伝統的な賭博施設に比べて、より多様なゲーム選択、便利なアクセス、そしてしばしば魅力的なボーナスやプロモーションを提供しています。
安全性と規制
オンラインカジノとオンラインギャンブルの世界では、安全性と規制が非常に重要です。多くの国々では、オンラインギャンブルを規制する法律があり、安全なプレイ環境を確保するためのライセンスシステムを設けています。これにより、不正行為や詐欺からプレイヤーを守るとともに、責任ある賭博の促進が図られています。
技術の進歩
最新のテクノロジーは、オンラインカジノとオンラインギャンブルの体験を一層豊かにしています。例えば、仮想現実(VR)技術の使用は、プレイヤーに没入型のギャンブル体験を提供し、実際のカジノにいるかのような感覚を生み出しています。また、ブロックチェーン技術の導入は、より透明で安全な取引を可能にし、プレイヤーの信頼を高めています。
未来への展望
オンラインカジノとオンラインギャンブルは、今後も技術の進歩とともに進化し続けるでしょう。人工知能(AI)の更なる統合、モバイル技術の発展、さらには新しいゲームの創造により、この分野は引き続き成長し、世界中のプレイヤーに新しい娯楽の形を提供し続けることでしょう。
この記事では、オンラインカジノとオンラインギャンブルの現状、安全性、技術の影響、そして将来の展望に焦点を当てています。この分野は、技術革新によって絶えず変化し続ける魅力的な領域です。
Tải Hit Club iOS
Tải Hit Club iOSHIT CLUBHit Club đã sáng tạo ra một giao diện game đẹp mắt và hoàn thiện, lấy cảm hứng từ các cổng casino trực tuyến chất lượng từ cổ điển đến hiện đại. Game mang lại sự cân bằng và sự kết hợp hài hòa giữa phong cách sống động của sòng bạc Las Vegas và phong cách chân thực. Tất cả các trò chơi đều được bố trí tinh tế và hấp dẫn với cách bố trí game khoa học và logic giúp cho người chơi có được trải nghiệm chơi game tốt nhất.
Hit Club – Cổng Game Đổi Thưởng
Trên trang chủ của Hit Club, người chơi dễ dàng tìm thấy các game bài, tính năng hỗ trợ và các thao tác để rút/nạp tiền cùng với cổng trò chuyện trực tiếp để được tư vấn. Giao diện game mang lại cho người chơi cảm giác chân thật và thoải mái nhất, giúp người chơi không bị mỏi mắt khi chơi trong thời gian dài.
Hướng Dẫn Tải Game Hit Club
Bạn có thể trải nghiệm Hit Club với 2 phiên bản: Hit Club APK cho thiết bị Android và Hit Club iOS cho thiết bị như iPhone, iPad.
Tải ứng dụng game:
Click nút tải ứng dụng game ở trên (phiên bản APK/Android hoặc iOS tùy theo thiết bị của bạn).
Chờ cho quá trình tải xuống hoàn tất.
Cài đặt ứng dụng:
Khi quá trình tải xuống hoàn tất, mở tệp APK hoặc iOS và cài đặt ứng dụng trên thiết bị của bạn.
Bắt đầu trải nghiệm:
Mở ứng dụng và bắt đầu trải nghiệm Hit Club.
Với Hit Club, bạn sẽ khám phá thế giới game đỉnh cao với giao diện đẹp mắt và trải nghiệm chơi game tuyệt vời. Hãy tải ngay để tham gia vào cuộc phiêu lưu casino độc đáo và đầy hứng khởi!
сериал
онлайн
Porno
смотреть
серия
смотреть
онлайн
http://tinyurl.com/ypx3bly4
how to get cheap mobic prices
https://tinyurl.com/yn2bpwhj
buy doxycycline for rats
https://tinyurl.com/ywomtayb
http://tinyurl.com/yudegzbr
сериал
серия
uTorrent – центр судебных экспертиз один из самых популярных загрузчиков для скачивания торрентов на сегодняшний день.
серия
uTorrent – сколько стоит независимая экспертиза авто после дтп один из самых популярных загрузчиков для скачивания торрентов на сегодняшний день.
https://tinyurl.com/ype9g4n6
серия
выбрать казино онлайн
http://tinyurl.com/yvljk7jc
серия
https://tinyurl.com/ysfmuts9
https://tinyurl.com/ywomtayb
лучший казино онлайн
онлайн
Medicines information. What side effects can this medication cause?
fluoxetine
Everything trends of medicament. Get information now.
казино онлайн зеркала
https://tinyurl.com/yrfd6glv
buying cheap zerit without rx
сериал
серия
Ukraine
серия
urenrjrjkvnm
https://tinyurl.com/ym7u6ox8
http://tinyurl.com/ytwnqava
юридическая помощь бесплатно для всех вопросов о законодательстве|юридическое обслуживание бесплатно на правовые темы
бесплатная помощь юриста для граждан и предприятий по всем вопросам утверди бесплатное юридическое сопровождение от знающих специалистов|Получи бесплатное консультирование от квалифицированных юристов по наболевшим проблемам
Бесплатная юридическая помощь по решению споров после несчастного случая
юристы консультация бесплатно по телефону konsultaciya-yurista-499.ru.
сериал
серия
онлайн
смотреть
http://tinyurl.com/yl7hddus
онлайн
https://tinyurl.com/yl9cwtj7
http://tinyurl.com/ytwnqava
смотреть
https://tinyurl.com/ywomtayb
http://tinyurl.com/yl7hddus
сериал
Medicament information sheet. Cautions.
get promethazine
Best news about pills. Get now.
онлайн
amoxicillin saft kinder
https://tinyurl.com/ylz2yzzj
серия
онлайн
https://tinyurl.com/yqlapfma
сериал
The firm where Leonid Monosov was employed was reputed as one of the top companies in the capital, leonid monosov and was well-equipped to take on intricate projects that other contractors declined to undertake.
серия
The firm where Leonid Monosov was employed was reputed as one of the top companies in the capital, monosov leonid businessman and was well-equipped to take on intricate projects that other contractors declined to undertake.
http://tinyurl.com/yvkgxy5o
сериал
http://tinyurl.com/yr2msp2n
смотреть
онлайн
сериал
http://tinyurl.com/yvkgxy5o
http://tinyurl.com/yna3uhwe
pantoprazole sod dr 40 mg tab
Drugs information sheet. What side effects?
cheap sildigra
All information about pills. Get information now.
free porn videos
allopurinol billig bestellen
buying doxycycline online uk
cheap zithromax pill
find mere info
buy generic prednisone online w/o rx
Medicines information for patients. Brand names.
zenegra
Best trends of medicine. Get information now.
tai hit club
Tải Hit Club iOS
Tải Hit Club iOSHIT CLUBHit Club đã sáng tạo ra một giao diện game đẹp mắt và hoàn thiện, lấy cảm hứng từ các cổng casino trực tuyến chất lượng từ cổ điển đến hiện đại. Game mang lại sự cân bằng và sự kết hợp hài hòa giữa phong cách sống động của sòng bạc Las Vegas và phong cách chân thực. Tất cả các trò chơi đều được bố trí tinh tế và hấp dẫn với cách bố trí game khoa học và logic giúp cho người chơi có được trải nghiệm chơi game tốt nhất.
Hit Club – Cổng Game Đổi Thưởng
Trên trang chủ của Hit Club, người chơi dễ dàng tìm thấy các game bài, tính năng hỗ trợ và các thao tác để rút/nạp tiền cùng với cổng trò chuyện trực tiếp để được tư vấn. Giao diện game mang lại cho người chơi cảm giác chân thật và thoải mái nhất, giúp người chơi không bị mỏi mắt khi chơi trong thời gian dài.
Hướng Dẫn Tải Game Hit Club
Bạn có thể trải nghiệm Hit Club với 2 phiên bản: Hit Club APK cho thiết bị Android và Hit Club iOS cho thiết bị như iPhone, iPad.
Tải ứng dụng game:
Click nút tải ứng dụng game ở trên (phiên bản APK/Android hoặc iOS tùy theo thiết bị của bạn).
Chờ cho quá trình tải xuống hoàn tất.
Cài đặt ứng dụng:
Khi quá trình tải xuống hoàn tất, mở tệp APK hoặc iOS và cài đặt ứng dụng trên thiết bị của bạn.
Bắt đầu trải nghiệm:
Mở ứng dụng và bắt đầu trải nghiệm Hit Club.
Với Hit Club, bạn sẽ khám phá thế giới game đỉnh cao với giao diện đẹp mắt và trải nghiệm chơi game tuyệt vời. Hãy tải ngay để tham gia vào cuộc phiêu lưu casino độc đáo và đầy hứng khởi!
Сертификат подтверждает соответствие продукции, производственной деятельности, ввозимых материалов или изделий на экспорт, и международным стандартам на продажу каких товаров не нужен сертификат. Есть много разных типов таких документов, которые будут необходимы при осуществлении определенных видов деятельности.
Сертификат подтверждает соответствие продукции, производственной деятельности, ввозимых материалов или изделий на экспорт, и международным стандартам список товаров не подлежащих обязательной сертификации. Есть много разных типов таких документов, которые будут необходимы при осуществлении определенных видов деятельности.
http://moslomtorg.ru
tai game hitclub
Tải Hit Club iOS
Tải Hit Club iOSHIT CLUBHit Club đã sáng tạo ra một giao diện game đẹp mắt và hoàn thiện, lấy cảm hứng từ các cổng casino trực tuyến chất lượng từ cổ điển đến hiện đại. Game mang lại sự cân bằng và sự kết hợp hài hòa giữa phong cách sống động của sòng bạc Las Vegas và phong cách chân thực. Tất cả các trò chơi đều được bố trí tinh tế và hấp dẫn với cách bố trí game khoa học và logic giúp cho người chơi có được trải nghiệm chơi game tốt nhất.
Hit Club – Cổng Game Đổi Thưởng
Trên trang chủ của Hit Club, người chơi dễ dàng tìm thấy các game bài, tính năng hỗ trợ và các thao tác để rút/nạp tiền cùng với cổng trò chuyện trực tiếp để được tư vấn. Giao diện game mang lại cho người chơi cảm giác chân thật và thoải mái nhất, giúp người chơi không bị mỏi mắt khi chơi trong thời gian dài.
Hướng Dẫn Tải Game Hit Club
Bạn có thể trải nghiệm Hit Club với 2 phiên bản: Hit Club APK cho thiết bị Android và Hit Club iOS cho thiết bị như iPhone, iPad.
Tải ứng dụng game:
Click nút tải ứng dụng game ở trên (phiên bản APK/Android hoặc iOS tùy theo thiết bị của bạn).
Chờ cho quá trình tải xuống hoàn tất.
Cài đặt ứng dụng:
Khi quá trình tải xuống hoàn tất, mở tệp APK hoặc iOS và cài đặt ứng dụng trên thiết bị của bạn.
Bắt đầu trải nghiệm:
Mở ứng dụng và bắt đầu trải nghiệm Hit Club.
Với Hit Club, bạn sẽ khám phá thế giới game đỉnh cao với giao diện đẹp mắt và trải nghiệm chơi game tuyệt vời. Hãy tải ngay để tham gia vào cuộc phiêu lưu casino độc đáo và đầy hứng khởi!
porn site
Woman Retired 28 New York City 2 Million
Промокоды 1xBet на сегодня. Получите бесплатно при регистрации бонус. Активируйте промокоды и делайте ставки на футбол, хоккей и самые яркие состязания – Лиги Европы и Лиги Чемпионов. Отличительная особенность букмекера – возможность использования рабочий промокод 1xbet бонус или для активных клиентов, уже имеющих учетную запись. Они обеспечивают двойной депозит, бесплатную ставку (фрибет), специальный бонус на день рождения и многое другое. Актуальные бонусные коды для новичков за регистрацию, способы получения и активации, bonus программа на официальном сайте букмекера 1хБет. Бесплатные промокоды при регистрации в 2024 году в 1xBet.
%%
my blog :: https://iron-art.kiev.ua/stolyi-iz-metalla/
order doxycycline 100mg online cheap
Все рабочие промокоды 1xBet на сегодня вы можете найти бесплатно на этом сайте. Используйте промокод *1XFREE777* для получения бонуса до 32500 руб при регистрации. Приятно, что новички могут ввести промокод при регистрации, который даст право на получение приветственного бонуса на сумму до 32500 рублей. Самое главное — это относиться к ставкам и к игре в целом ответственно! Не стоит играть на последние или заемные деньги, стремясь таким образом заработать себе на жизнь.
%%
Also visit my page: https://project-csgo.ru/publ/sekretnye-promokody-dlja-izi-drop
while she was talk-ing. “How can I have done that?” she mostbet oyna
diltiazem side effects
Hi to all, the contents present at this site are really awesome for people
knowledge, well, keep up the good work fellows.
Novyny
Meds prescribing information. Cautions.
lisinopril medication
Actual trends of medicines. Read here.
Prestito di 1500 euro
prednisone rx
Write more, thats all I have to say. Literally, it seems as
though you relied on the video to make your point.
You clearly know what youre talking about, why throw away your intelligence on just posting videos to your site when you could be giving us something enlightening to
read?
buying doxycycline in india
хостинг сайта
Когда речь заходит о создании своего собственного сайта, выбор хостинга играет огромную роль. Ведь именно хостинг будет определять доступность и быстродействие вашего сайта для пользователей. Если вы находитесь в Беларуси и ищете надежного хостинг-провайдера, то BestHost.BY – это отличный выбор. BestHost.BY – одна из ведущих хостинг-компаний в Беларуси, предоставляющая высококачественные услуги уже на протяжении 15 лет.
can you buy prednisone without a prescription
Играйте и выигрывайте в онлайн-казино сегодня зарегистрироваться дедди
Pills information leaflet. Brand names.
can i buy flibanserina
Some information about drugs. Read information now.
garcinia cambogia 100caps pharmacy
precose cost walmart
Medicines information sheet. Brand names.
colchicine
Everything what you want to know about medicines. Get information now.
Как включить аппаратную виртуализацию
Абузоустойчивый серверов для Хрумера и GSA AMSTERDAM!!!
Оптимальная Настройка: Включение Аппаратной Виртуализации
При обсуждении виртуальных серверов (VPS/VDS) и дедикатед серверов, важно также уделить внимание оптимальной настройке, включая аппаратную виртуализацию. Этот важный аспект может значительно повлиять на производительность вашего сервера.
Высокоскоростной Интернет: До 1000 Мбит/с
cefixime for gonorrhea
Поднимайте ставки и выигрывайте крупные суммы с онлайн-казино Плейфортуна https://play-fortuna-slotg1l6.com/ru
I’ve learn some good stuff here. Certainly price bookmarking
for revisiting. I surprise how much attempt you place to create this kind of wonderful informative web site.
Абузоустойчивые сервера в Амстердаме, они позволят работать с сайтами которые не открываются в РФ, работая Хрумером и GSA пробив намного выше.
Виртуальные сервера (VPS/VDS) и Дедик Сервер: Оптимальное Решение для Вашего Проекта
В мире современных вычислений виртуальные сервера (VPS/VDS) и дедик сервера становятся ключевыми элементами успешного бизнеса и онлайн-проектов. Выбор оптимальной операционной системы и типа сервера являются решающими шагами в создании надежной и эффективной инфраструктуры. Наши VPS/VDS серверы Windows и Linux, доступные от 13 рублей, а также дедик серверы, предлагают целый ряд преимуществ, делая их неотъемлемыми инструментами для развития вашего проекта.
Высокоскоростной Интернет: До 1000 Мбит/с
Medication information. Brand names.
buy clomid
Actual news about medication. Get information now.
Je recommande cette très belle pochette Pablo Exclusive Banana Ice
Je recommande cette très belle pochette Pablo Exclusive Bubblegum
she knew that were of her age, to see if she could mostbet casino login
actos side effects
Novost
Промокоды 1xBet на 32500 руб при регистрации. Игроки, которые используют промокоды и “приветствие” при регистрации в букмекерской фирме «1хbеt», могут увеличить свою сумму первого пополнения счета. Таким образом, если уже после прохождения регистрации внести 32500 руб., итоговый результат будет увеличен до 13000 руб. Из каких 32500 руб. сам депозит и 6 тыс. 500 руб. — бонусный средства. рабочий промокод 1хбет бонус . Промокод в 1хбет – это возможность сделать бесплатную ставку на сумму, которая указана в промокоде. Содержание: Где найти промокод 1xbet на сегодня бесплатно. Чем полезный промокод на 1xbet. На какие виды спорта можно взять промокоды в 1 xbet. Как проверить промокод на 1хбет.
%%
Also visit my website; раскраски купить владивосток
https://tinyurl.com/ylejts99
https://thenewsgod.com/how-bloggers-use-youtube-bots-to-increase-subscribers-on-channels/
онлайн
Mostbet combines sports betting and gambling entertainment on one platform https://www.twitch.tv/mostbet08/about
http://tinyurl.com/ytwnqava
buying prednisone online without a prescription
Mostbet combines sports betting and gambling entertainment on one platform https://hectorjdvn55432.blogpostie.com/45865307/unleash-the-pleasure-mostbet-uz-com-your-gateway-to-thrilling-online-entertainment
онлайн
https://tinyurl.com/ylfm35t2
urenrjrjkvnm
https://tinyurl.com/yte5wes7
https://tinyurl.com/yw9bdxhf
https://tinyurl.com/2x8es5sd
смотреть
серия
смотреть
https://tinyurl.com/ypks4dw7
https://tinyurl.com/ynvywvbx
серия
http://tinyurl.com/yl7hddus
смотреть
онлайн
can i get synthroid without rx
https://tinyurl.com/yoyc8uxm
Букмекерская контора Melbet является одним из столпов международной беттинговой индустрии. За счет масштабной маркетинговой компании, высоких коэффициентов и оперативной технической поддержки БК Мелбет удалось привлечь и удержать большое количество игроков. На сегодняшний день, букмекер предлагает получить один из самых высоких бонусов на рынке – 10400 рублей. Размер бонуса в Melbet составляет 100% от суммы первого пополнения, но не менее 100 рублей и не более 10400. К примеру, если пополнить баланс на сумму 4000, то справа от основного счета появится бонусный. Как видим, использовать Melbet промокод имеет смысл, особенно тем бетторам и бонусхантерам, которые привыкли заключать пари по-крупному. С учетом того, что он бесплатный – воспользоваться им может абсолютно любой игрок.
https://tinyurl.com/yup4krda
серия
https://tinyurl.com/yvodvp6v
https://tinyurl.com/ylp62ccj
https://tinyurl.com/ynshtvwy
http://tinyurl.com/yodtfo2m
https://tinyurl.com/ym7u6ox8
Medicine information. Generic Name.
strattera rx
Everything trends of drug. Read here.
серия
серия
https://tinyurl.com/yk8ydz5x
https://tinyurl.com/yro3w9oa
сериал
смотреть
http://tinyurl.com/yna3uhwe
buy cheap tinidazole without rx
серия
https://tinyurl.com/ynvywvbx
https://tinyurl.com/yw9ulbec
http://tinyurl.com/yulwl7pp
1хбет зеркало – это популярная букмекерская компания, предлагающая широкий выбор ставок на спорт, казино и многое другое. С высокими коэффициентами и удобным интерфейсом, 1xbet привлекает множество игроков. Он также предоставляет возможность онлайн-трансляций событий. 1xbet создает захватывающий игровой опыт для своих пользователей.
серия
сериал
https://tinyurl.com/yo3lc7s2
серия
https://tinyurl.com/ys45bpea
смотреть
https://tinyurl.com/yqb6ftuc
серия
сериал
Medicament prescribing information. Brand names.
can you get neurontin
Everything information about pills. Get here.
https://tinyurl.com/ynxes3l8
сериал
онлайн
Deciding on the ideal car seat covers is an important decision for any kind of vehicle manager. Certainly not just perform they enhance the visual beauty of your cars and truck’s inner parts, yet they additionally guard the authentic upholstery coming from deterioration, https://www.tumblr.com/sherronoshea/737740058958987265/car-seat-covers-best-custom-fit-seat-covers?source=share.
porn HD
https://tinyurl.com/ymwwubnb
серия
онлайн
https://tinyurl.com/ynshtvwy
онлайн
серия
онлайн
смотреть
серия
Nicely put. Many thanks!
https://tinyurl.com/yubz8yvu
uTorrent компактный классический клиент для опытных пользователе – https://utorrent.bumtor.ru/ один из самых популярных загрузчиков для скачивания торрентов на сегодняшний день.
https://tinyurl.com/yqh8tbzk
Wow! Finally I got a blog from where I can truly take valuable information concerning my study and knowledge.
https://tinyurl.com/ypejy4mc
amoxicillin over the counter
Скачать приложения на Андроид бесплатно без регистрации https://apkhub.ru/
Приобрести нержавеющие трубы в онлайн магазине нержавеющих труб по индивидуальным нержавеющие трубы от Огромный выбор нержавеющих труб на цены на нержавеющие трубы на этой неделе нержавеющих труб по всей нержавеющие трубы оптом от надежного по выбору нержавеющих труб
Уверенность на каждую продукцию нержавеющих труб
Самые низкие цены на нержавеющие трубы в России нержавеющих труб для Персональный подход к каждому клиенту при покупке нержавеющих труб
Опытные монтажные работы нержавеющих труб на любом объекте
Нержавейки – идеальное решение для промышленных нужд
Разнообразие диаметров и толщин нержавеющих труб
Экспресс заказ и отгрузка нержавеющих труб по всей России
Надежная продукция нержавеющих труб от лучших производителей
Квалифицированный подбор и консультация по выбору нержавеющих труб
Прочность нержавеющих труб для различных целей
Специальные цены на покупку нержавеющих труб для ремонта
труба из нержавеющей стали 150 мм цена за метр http://nerzhavejushhie-truby.ru/.
https://tinyurl.com/ypejy4mc
смотреть
онлайн
https://tinyurl.com/yovm57og
серия
https://tinyurl.com/yvjjy97b
https://tinyurl.com/ylp62ccj
онлайн
https://tinyurl.com/yvhymcex
сериал
https://tinyurl.com/yqlapfma
серия
https://tinyurl.com/2x9ry27z
https://tinyurl.com/ywkh85kr
сериал
https://tinyurl.com/yl62o6hl
https://tinyurl.com/yrzkyga5
онлайн
Pills information sheet. What side effects can this medication cause?
aurogra price
Best information about meds. Read information here.
https://tinyurl.com/ywomtayb
http://tinyurl.com/ynlh256n
http://tinyurl.com/yu8gtk9h
https://tinyurl.com/ympmns9w
сериал
https://tinyurl.com/yutfkhqo
http://tinyurl.com/ytwnqava
porn videos
серия
серия
серия
GlucoTrust is a revolutionary blood sugar support solution that eliminates the underlying causes of type 2 diabetes and associated health risks.
1xbet промокод на сегодня 2024. Чтобы удовлетворить потребности бетторов и сделать процесс ставок максимально разнообразным нередко букмекерские конторы пытаются увеличить свой функционал, путем добавления специальных функций и предложений. Одним из лидеров среди популярных букмекеров на постсоветском пространстве по своим функциональным возможностям является 1хБет. Ввод 1 x bet промокод позволяет получить увеличенную сумму бонуса. Для этого достаточно после создания аккаунта внести первый депозит (максимальная сумма бонусного начисления составляет 32 500 рублей). Можно использовать любой платёжный метод. Абсолютно бесплатный промокод 1xbet. На сегодня контора предлагает всем новичкам воспользоваться не только приветственным бонусом, но и получить дополнительные преференции. Эти льготы игрок получает в том случае, если внимательно отнесётся к процедуре регистрации на сайте. Ведь не все новички обращают внимание или понимают, о каких выгодах идёт речь, когда видят необязательное для заполнения поле «Введите промокод (при наличии)», находящееся в самом низу регистрационной формы. Оно есть при трёх способах получения аккаунта из четырёх возможных («В 1 клик», «По номеру телефона», «По e-mail»). А игнорировать его – это потерять дополнительные выгоды.
https://tinyurl.com/yw9bdxhf
where can i get generic sildalist without dr prescription
серия
серия
https://tinyurl.com/ylfm35t2
http://tinyurl.com/2xcr3qdf
https://tinyurl.com/ys2yfzzf
https://tinyurl.com/ynshtvwy
серия
Мелбет – это букмекерская контора, которая дает возможность преобразовать хобби в доход. Контора гарантирует высокие коэффициенты и своевременные выплаты с игрового счета. Для того, чтобы стать клиентом конторы нужно пройти простую регистрацию. Здесь разнообразные виды спорта, широкий выбор событий и типов ставок. Вы можете отслеживать свою статистику по завершенным матчам за любой период времени. Доступ к счету можно получить с ПК, смартфона или планшета. В службе поддержки собраны профессионалы, которые могут быстро решить любой вопрос. Предлагается промокод Melbet при регистрации большой выбор способов ввода средств на игровой счет.
https://tinyurl.com/ywpmx387
https://tinyurl.com/yqlapfma
https://tinyurl.com/yts3fpja
https://tinyurl.com/yw9bdxhf
https://tinyurl.com/ywv4y99b
Профессиональный честный сервис по ремонту ноутбуков ремонт компьютеров Екатеринбург обратитесь в наш сервисный центр по ремонту компьютеров и ноутбуков.
https://tinyurl.com/ypks4dw7
Optimize your app or game by the best free App Store Optimization Cloudflare Bot Mitigation
https://tinyurl.com/yn2bpwhj
Профессиональный честный сервис по ремонту ноутбуков ремонт компьютеров обратитесь в наш сервисный центр по ремонту компьютеров и ноутбуков.
https://tinyurl.com/ytlrel5c
Optimize your app or game by the best free App Store Optimization The Protective Shield for Your MacBook: Antivirus Software
https://tinyurl.com/yqb6ftuc
%%
Look into my page; https://casinocrit.pro/
https://tinyurl.com/ylz2yzzj
https://tinyurl.com/yvodvp6v
https://tinyurl.com/ymoghjr4
смотреть
can i get cheap zithromax without rx
серия
https://tinyurl.com/ysqft67z
онлайн
Вы не правы. Я уверен. Предлагаю это обсудить. Пишите мне в PM, пообщаемся.
В рассматриваемой норме сказано, что бизнес в сегменте казино запрещен, причем не лишь в наземном, https://casinocrit.pro/ сколько в всемирную сеть-формате.
онлайн
сериал
https://tinyurl.com/yr7hldue
онлайн
серия
смотреть
https://v-mig.ru/kofe-poleznye-svojstva-kotorye-dolzhen-znat-kazhdyj/
https://tinyurl.com/yof9ukyu
онлайн
сериал
Novost
смотреть
смотреть
https://tinyurl.com/yro3w9oa
https://tinyurl.com/ymhtcujx
смотреть
онлайн
http://tinyurl.com/2xcr3qdf
серия
https://tinyurl.com/yqlapfma
https://tinyurl.com/yup4krda
онлайн
электрокарниз https://prokarniz34.ru/
https://tinyurl.com/ytlrel5c
серия
онлайн
серия
смотреть
онлайн
https://tinyurl.com/ylz2yzzj
https://tinyurl.com/ykbjjt2t
https://tinyurl.com/ytlrel5c
смотреть
сериал
https://tinyurl.com/ym7u6ox8
https://tinyurl.com/yqea5u48
http://tinyurl.com/yn2cy7os
Стройматериалы в наличии в интернет-магазине и розничных магазинах гидрошпонки купить в Москве с доставкой.
Drug information. Cautions.
fluoxetine for sale
Best about drug. Get here.
серия
https://tinyurl.com/yvwpyy6y
онлайн
смотреть
сериал
https://tinyurl.com/yr9nvak9
https://tinyurl.com/yoyc8uxm
http://tinyurl.com/ykqu3kzs
Как включить аппаратную виртуализацию
Абузоустойчивый серверов для Хрумера и GSA AMSTERDAM!!!
Высокоскоростной Интернет: До 1000 Мбит/с
Скорость интернет-соединения играет решающую роль в успешной работе вашего проекта. Наши VPS/VDS серверы, поддерживающие Windows и Linux, обеспечивают доступ к интернету со скоростью до 1000 Мбит/с. Это гарантирует быструю загрузку веб-страниц и высокую производительность онлайн-приложений на обеих операционных системах.
Итак, при выборе виртуального выделенного сервера VPS, обеспечьте своему проекту надежность, высокую производительность и защиту от DDoS. Получите доступ к качественной инфраструктуре с поддержкой Windows и Linux уже от 13 рублей
серия
http://tinyurl.com/yr43cf22
http://tinyurl.com/yn54xvke
1x bet – это популярная букмекерская компания, предлагающая широкий выбор ставок на спорт, казино и многое другое. С высокими коэффициентами и удобным интерфейсом, 1xbet привлекает множество игроков. Он также предоставляет возможность онлайн-трансляций событий. 1xbet создает захватывающий игровой опыт для своих пользователей.
онлайн
сериал
http://tinyurl.com/yvjjfb4u
сериал
сериал
смотреть
https://tinyurl.com/yrqyzdby
онлайн
1xBet промокод казино при регистрации. 1xBet промокод казино при регистрации. Сайт 1хБет – это не только популярная букмекерская контора, но и казино, в котором можно играть как с машинами, так и с реальными крупье. Использовав промокод казино 1xBet, игрок получает денежные средства на бонусный счет. Это значит, что он может использовать их только для игры в слоты и другие азартные развлечения на сайте. Вывести деньги, выигранные с бонуса, игрок сможет только тогда, когда отыграет их согласно вейджеру. Сегодня в казино предусмотрены следующие бонусы за регистрацию и депозит: Все новые пользователи азартного заведения могут получить бездепозитный бонус. Промокод представляет собой комбинацию букв и чисел, которые позволят вам получить бонус. Если он актуальный, то сумма вашего депозита после пополнения увеличится на оговоренную в условиях получения промокода сумму. Есть и другой способ. Нередко промокод для 1 x bet распространяют официальные партнеры компании 1xbet. Среди них могут быть группы и аккаунты в социальных сетях, которые связаны с прогнозированием событий или спортивные ресурсы.
https://tinyurl.com/yk8ydz5x
http://tinyurl.com/ykqu3kzs
http://tinyurl.com/yn2cy7os
онлайн
https://agrikesici360.blogspot.com/
https://tinyurl.com/yqvcuvgf
https://tinyurl.com/yrfd6glv
https://tinyurl.com/ylekoy5c
https://tinyurl.com/ywpmx387
https://tinyurl.com/ym7u6ox8
сериал
серия
https://tinyurl.com/ymj3zyke
https://tinyurl.com/yvhymcex
онлайн
Medicament information leaflet. Effects of Drug Abuse.
maxalt buy
All trends of drug. Get now.
http://tinyurl.com/yoxgcl7h
I reccomend this site Ramenbetto everyone.
онлайн
https://tinyurl.com/yuy33ndo
серия
https://tinyurl.com/yufbn2sk
онлайн
онлайн
http://tinyurl.com/yt6qe9kp
сериал
сериал
В нашем каталоге Вы найдете широкий ассортимент лодок ПВХ, моторов и комплектующих: каяки купить
онлайн
see page
В нашем каталоге Вы найдете широкий ассортимент лодок ПВХ, моторов и комплектующих: лодка пвх купить
http://tinyurl.com/ysl4gs3t
https://tinyurl.com/yoyc8uxm
https://tinyurl.com/ymhtcujx
https://tinyurl.com/ym7u6ox8
онлайн
http://tinyurl.com/yvvt4ldx
http://tinyurl.com/yodtfo2m
https://tinyurl.com/ytz2x4ln
https://tinyurl.com/yl62o6hl
серия
сериал
http://tinyurl.com/ysyk5gbx
http://tinyurl.com/yn2cy7os
серия
серия
https://tinyurl.com/yufbn2sk
https://tinyurl.com/yof9ukyu
http://tinyurl.com/yn2cy7os
https://tinyurl.com/yvxbrea4
серия
https://tinyurl.com/yp2un5ln
онлайн
смотреть
серия
https://tinyurl.com/ylekoy5c
сериал
серия
сериал
https://tinyurl.com/ylfm35t2
https://tinyurl.com/ywomtayb
онлайн
Hello, I think your blog might be having browser compatibility issues.
When I look at your blog site in Chrome, it looks fine but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up!
Other then that, amazing blog!
https://tinyurl.com/ymwwubnb
http://tinyurl.com/ymudmbeh
Medicines information leaflet. Drug Class.
rx avodart
Actual trends of pills. Get now.
https://tinyurl.com/yw9bdxhf
https://tinyurl.com/ylp62ccj
онлайн
http://tinyurl.com/yw9ggnt4
https://tinyurl.com/yl62o6hl
https://tinyurl.com/yl4z9qpq
продвижение сайтов https://prodvijenie-saitov.md/
https://tinyurl.com/yr6rphut
сериал
https://tinyurl.com/ymwwubnb
https://tinyurl.com/ynxb6yk4
https://tinyurl.com/yvjjy97b
https://tinyurl.com/yutfkhqo
https://tinyurl.com/yoyc8uxm
https://tinyurl.com/ynoxx7pz
http://tinyurl.com/yqfslotz
серия
https://tinyurl.com/ypejy4mc
смотреть
сериал
https://tinyurl.com/ysfmuts9
abilify 20mg without prescription
https://tinyurl.com/2x65osyx
Абузоустойчивый сервер для работы с Хрумером, GSA и всевозможными скриптами!
Есть дополнительная системах скидок, читайте описание в разделе оплата
Высокоскоростной Интернет: До 1000 Мбит/с
Скорость интернет-соединения играет решающую роль в успешной работе вашего проекта. Наши VPS/VDS серверы, поддерживающие Windows и Linux, обеспечивают доступ к интернету со скоростью до 1000 Мбит/с. Это гарантирует быструю загрузку веб-страниц и высокую производительность онлайн-приложений на обеих операционных системах.
Итак, при выборе виртуального выделенного сервера VPS, обеспечьте своему проекту надежность, высокую производительность и защиту от DDoS. Получите доступ к качественной инфраструктуре с поддержкой Windows и Linux уже от 13 рублей
https://tinyurl.com/ypejy4mc
онлайн
https://tinyurl.com/yuhy5zh9
онлайн
http://tinyurl.com/2xafe47e
серия
онлайн
смотреть
http://tinyurl.com/2xafe47e
http://tinyurl.com/yoxgcl7h
https://tinyurl.com/2x2qegmg
сериал
Porno XXX 100ASS
http://tinyurl.com/ymudmbeh
https://tinyurl.com/yw6f77s2
can i order cheap synthroid without a prescription
http://tinyurl.com/ysyk5gbx
Cardiopulmonary resuscitation is actually an essential life-saving technique that can easily indicate the variation between life and also death in emergency situation scenarios. It includes breast compressions and also rescue breaths to maintain blood circulation as well as oxygenation when a person’s soul as well as breathing have ceased. Understanding the usefulness of CPR is actually essential for individuals of every ages, as it encourages them to answer successfully to emergency situations, http://www.ingender.com/forum/peep.aspx?ID=230128.
%%
my blog post: https://vulkancasinoofficial.win/skachat
Всем рекомендую классное Раменбет казино.
buy doxycycline tablets
Советы по выбору беговой дорожки для лучших результатов
беговая дорожка купить для дома http://www.begovye-dorozhki.ks.ua.
Аренда мощного дедика (VPS): Абузоустойчивость, Эффективность, Надежность и Защита от DDoS от 13 рублей
Выбор виртуального сервера – это важный этап в создании успешной инфраструктуры для вашего проекта. Наши VPS серверы предоставляют аренду как под операционные системы Windows, так и Linux, с доступом к накопителям SSD eMLC. Эти накопители гарантируют высокую производительность и надежность, обеспечивая бесперебойную работу ваших приложений независимо от выбранной операционной системы.
urenrjrjkvnm
Наши опытные специалисты быстро и профессионально устранят любые неисправности вашей стиральной машины Ремонт стиральных машин в Подольске
Payday loans in Alabama
Medicines information. Long-Term Effects.
proscar generic
Actual trends of drugs. Read information here.
be a key to one of the doors of the hall, but when
finpecia 10 mg pill
Абузоустойчивый сервер для работы с Хрумером, GSA и всевозможными скриптами!
Есть дополнительная системах скидок, читайте описание в разделе оплата
Высокоскоростной Интернет: До 1000 Мбит/с**
Скорость интернет-соединения – еще один важный момент для успешной работы вашего проекта. Наши VPS серверы, арендуемые под Windows и Linux, предоставляют доступ к интернету со скоростью до 1000 Мбит/с, обеспечивая быструю загрузку веб-страниц и высокую производительность онлайн-приложений на обеих операционных системах.
Промокод 1xbet при регистрации по увеличению бонуса до 32500 рублей на первый депозит активируется бесплатно, заполнив поле “Промокод” официальным ключевым словом в регистрационном меню при создании аккаунта: Войти в 1xbet.com. промокод 1xbet : 1XFREE777 Получить промокоды на сегодня без регистрации в 1xBet можно на сайте, где незарегистрированным пользователям предлагается ввести промо «1XFREE777». Создание аккаунта в БК – это обязательный процесс для активации промокода на ставки и использования других функций. Бесплатный промокод для 1xBet на сегодня. Использование промокода 1xBet дает возможность получить подарок от букмекера. Обычно рабочий promo code «1xБет» располагается в соцсетях или же на партнерских ресурсах.Промокод при регистрации дает право на бонус. Для этого требуется пройти регистрацию и внести на баланс не меньше 100 рублей. Также необходимо в личном профиле заполнить все обязательные поля.
Надувные лодки ПВХ по низкой цене купить в интернет магазине каноэ
Используя промокод Мелбет при регистрации, игроки получают доступ к участию в приветственной бонусной программе. Полученные привилегии можно использовать, заключая ставки на ММА и другие виды спорта. Ниже рассказываем более подробно о том, какие бонусы предложены на сайте и как их отыграть. Бонусные программы нацелены на то, чтобы обеспечить для игроков возможность получить безболезненный опыт игры на сайте и сгладить первые возможные неудачи. Регистрируйтесь на платформе букмекера, активируйте действующий промокод Melbet и пользуйтесь бонусными предложениями от букмекера Мелбет, чтобы получать больше положительных эмоций при заключении пари.
Надувные лодки ПВХ по низкой цене купить в интернет магазине пластиковый каяк
Такая щедрость компания обусловлена предоставлением клиентам недели бесплатных игр. какие отличие честных лицензионных https://citydevelopers.ru/otzyvy/novosibirsk/zhk-voskresnyy/ игровых заведениях от офшорных?
онлайн
серия
https://tinyurl.com/ypxuh56e
urenrjrjkvnm
Drug information leaflet. Generic Name.
avodart
Actual information about medicine. Get here.
https://tinyurl.com/yqusp3d4
https://tinyurl.com/yqea5u48
смотреть
сериал
сериал
https://tinyurl.com/yrfd6glv
сериал
can you get cheap levaquin no prescription
сериал
http://tinyurl.com/ysyk5gbx
сериал
metronidazole online bestellen
Извиняюсь, но это мне не совсем подходит.
вам здасться відправлено лист з адресою форму зміни ключа або sms повідомлення з новим паролем. Досвідчений вчитель математики, https://dogotrunghieu.com/su-menh-tam-nhin/ російської мови.
Drug information leaflet. Effects of Drug Abuse.
priligy order
Best about medicines. Get information now.
buy aurogra tablets
оптом в интернет-магазине
Кастомные фланцы для труб: как заказать
Фланцы для труб доставка http://www.flancy-msk.ru/.
Бонусное предложение активно до конца 2024 года. Фрибет – это бесплатные ставки на некоторое количество пари в букмекерской конторе 1xbet, которые выдается, если ввести промокод 1хбет , а затем – целиком заполнить анкету игрока в своем личном кабинете и подтвердить номер мобильного телефона. С помощью бесплатной ставки за 1xbet промокод вы можете делать ставки на любые виды спорта, однако учтите, что у 1xbet фрибета есть свои условия отыгрыша. Приветственный бонус 1Хбет. Во время регистрации на 1xbet бетторы могут выбрать стартовый бонус – для ставок на спорт или для игры в казино. Промокоды 1xBet на сегодня. Не ошибемся, если скажем, что компания является одним из лидеров на рынке букмекерских услуг по количеству и разнообразию бонусных предложений. Белорусские бетторы могут воспользоваться всем их спектром. Промокод «1хБет» при регистрации дает право новым бетторам получит 100% бонус на первый депозит, но не более 200 BYN (бел. рублей). Например, при пополнении баланса на 100 BYN сверху клиент получает аналогичный бонус. Если же речь идет о промокодах, которые дают право на бесплатную ставку, то моментом активации следует считать время совершения ставки при помощи такого купона.
porn 1059 videos
Список бесплатных промокодов 1xBet. Получи максимальный бонус при регистрации на сайте и в приложении! +100% к первому депозиту для всех новых игроков. Указанный выше промо-код дает новым игрокам возможность получить повышенный на 30% bonus. Как получить и использовать бонус 32500 рублей по промо-коду букмекерской компании 1хБет? Рабочие промокоды 1xBet при регистрации на официальном сайте компании. 1xbet промокод . Актуальный Промо-Коды 1 Икс Бет на 2024 год – это возможность сделать бесплатную ставку на сумму, которая указана в промокоде. Содержание: Где найти промокод 1xbet на сегодня бесплатно. Букмекерская контора 1 Икс Бет только новым людям дает бонус при пополнени. Чем полезный промокод на 1xbet. На какие виды спорта можно взять промокоды в 1 xbet. Как проверить промокод на 1хбет. Использовать его необходимо при регистрации на официальном сайте конторы 1xbet (а промокоды для купона при пари, находятся в самом низу статьи).
промокод мелбет на сегодня Введите: RS777 и тогда при депозите вы получите бонус 10400 рублей автоматически. Букмекерская контора Мелбет в 2024 году создала комфортные условия для заядлых беттеров и новых пользователей. Международная букмекерская платформа Melbet стремительно набирает популярность среди беттеров. Для привлечения новой аудитории и повышения лояльности уже имеющейся, администрация сайта создала специальный промокод.
I do believe all the ideas you have presented
in your post. They are very convincing and can certainly work.
Still, the posts are very short for novices. May you please prolong them a little from next time?
Thank you for the post.
Visit my webpage :: gdgo.ru
%%
Play Mahjong Solitaire for free! The game can be played online in your browse mahjong games free
Play Mahjong Solitaire for free! The game can be played online in your browse mahjong dimensions 15
Ремонт электродвигателей москва
Добро пожаловать, игроки на xbetegypt!
Достигните успеха на xbetegypt с премиум бонусами!
Наслаждайтесь азартом на xbetegypt каждый день!
Увеличьте выигрыш на xbetegypt с нашими лучшими предложениями!
Используйте свой шанс на xbetegypt и выиграйте самые многочисленные призы!
Достигайте своих целей с xbetegypt каждый день!
Создайте свой банк на xbetegypt и победите больше денег!
Измените свою жизнь с xbetegypt и получите все!
Наслаждайтесь играть на xbetegypt и получайте все больше выигрышей!
Отдыхайте от игры на xbetegypt и получайте призы каждый день!
Докажите свои способности игры на xbetegypt и достигните больших успехов!
Удивляйтесь от игры на xbetegypt и открывайте новые возможности каждый день!
Откройте для себя новые горизонты игры и добивайтесь большими бонусами!
Наслаждайтесь ощущением успеха с xbetegypt каждый день!
Играйте вместе с друзьями на xbetegypt и получайте большими выигрышами!
Освоите свои навыки на xbetegypt и победите еще больше денег!
Наслаждайтесь игры на xbetegypt и зарабатывайте большие бонусы каждый день!
Зарабатывайте каждый день на xbetegypt и наслаждайтесь результатами!
Успейте играть на xbetegypt и получайте больше денег каждый день!
Наслаждайтесь максимум удовольствия от игры на xbetegypt и получайте больше бонусов!
Download betting program http://www.1xbet-app-download-ar.com/.
Всем рекомендую, очень крутая баллон игра.
перемотка электродвигателей москва
https://satbayev.university/
cost of tinidazole price
Medicament prescribing information. What side effects?
fosamax prices
Everything about medicament. Get information here.
Заказать чистку дивана и другой мягкой мебели с выездам на дом недорого https://nibu.com.ua/blog/raznoe/himchistka-matrasa-kyev/
Заказать чистку дивана и другой мягкой мебели с выездам на дом недорого https://www.piluli.kiev.ua/blog/zdorovie/5-factov-o-himchistki-mebeli/
https://nextgenbeauty.ae/
Бесплатные промокоды от букмекерской конторы 1xBet: при регистрации, на бесплатную ставку. Рассказываем, как использовать и куда вводить промокоды в 1хБет. промокод на 1xbet . Начнем с того, что каждый, кто зарегистрировался на официальном сайте или зеркале конторы впервые, может рассчитывать на получение приветственного денежного бонуса, который в дальнейшем удастся потратить на ставки, а в случае успеха заработать первые деньги. Но мы говорим о промокоде, который в специальной форме регистрации просят ввести при наличии.
Здравствуйте, игроки на xbetegypt!
Насладитесь успеха на xbetegypt с эксклюзивными бонусами!
Делайте азартом на этом казино каждый день!
Увеличьте выигрыш на xbetegypt с нашими премиум предложениями!
Заберите свой шанс на xbetegypt и освойте самые многочисленные призы!
Сделайте свою мечту реальностью с xbetegypt каждый день!
Присоединяйтесь к нам и победите больше денег!
Измените свою жизнь с xbetegypt и получите все!
Наслаждайтесь играть на xbetegypt и зарабатывайте все больше выигрышей!
Наслаждайтесь от игры на xbetegypt и восстанавливайте свои силы!
Докажите свои способности игры на xbetegypt и достигните больших успехов!
Восхищайтесь от игры на xbetegypt и открывайте новые возможности каждый день!
Войдите в мир xbetegypt игры и наслаждайтесь большими бонусами!
Забудьте о неудачах с xbetegypt каждый день!
Играйте вместе с друзьями на xbetegypt и делимся большими выигрышами!
Освоите свои навыки на xbetegypt и зарабатывайте еще больше денег!
Взламывайте игры на xbetegypt и получайте большие бонусы каждый день!
Играйте сегодня на xbetegypt и взлейте над другими!
Освойте играть на xbetegypt и зарабатывайте больше денег каждый день!
Наслаждайтесь максимум удовольствия от игры на xbetegypt и зарабатывайте больше бонусов!
Download 1xbet in Arabic 1xbet-app-download-ar.com.
Рабочий промокод всегда доступен на нашем сайте. Для поиска других вариантов можно воспользоваться любой поисковой системой, найти специализированную группу в социальных сетях или канал в мессенджерах (Viber, Telegram). Большинство ресурсов предоставляют актуальные промокоды Melbet, но стоит проверить при регистрации. Введите скопированный промокод мелбет и дождитесь уведомления от БК Мелбет, что бонус повышен. Помните, что второй раз зарегистрироваться и получить 10400 рублей от Мелбет невозможно. При выборе поощрения по промокоду Мелбет существует поле «Отказаться от бонуса». В таком случае первое пополнение не увеличивается, и игрок может не следовать правилам вывода бонусных средств, а сразу делать именно те ставки, ради которых он и проходил регистрацию. Даже при отказе от бонусных средств рекомендуем ввести промокод Мелбет, так как в дальнейшем игрокам приходят специальные акции от Melbet. Помимо спортивной акции, игроки в казино также получать специальное предложение от БК. При использовании промокода Мелбет есть возможность получить бонус в казино до 125 000? и 290 фриспинов.
Здравствуйте, игроки на xbetegypt!
Получите успеха на xbetegypt с лучшими бонусами!
Наслаждайтесь азартом на xbetegypt каждый день!
Сделайте вашу игру на xbetegypt с нашими лучшими предложениями!
Не упустите свой шанс на xbetegypt и выиграйте самые большие призы!
Сделайте свою мечту реальностью с xbetegypt каждый день!
Становитесь частью нашего сообщества и заработайте больше денег!
Откройте новые горизонты с xbetegypt и успейте все!
Научитесь играть на xbetegypt и зарабатывайте все больше выигрышей!
Отдыхайте от игры на xbetegypt и забирайте бонусы!
Освойте новые техники игры на xbetegypt и получайте больших успехов!
Восхищайтесь от игры на xbetegypt и открывайте новые возможности каждый день!
Откройте для себя новые горизонты игры и наслаждайтесь большими бонусами!
Погрузитесь в атмосферу победы с xbetegypt каждый день!
Побеждайте вместе на xbetegypt и получайте большими выигрышами!
Освоите свои навыки на xbetegypt и зарабатывайте еще больше денег!
Взламывайте игры на xbetegypt и получайте большие бонусы каждый день!
Зарабатывайте каждый день на xbetegypt и взлейте над другими!
Освойте играть на xbetegypt и зарабатывайте больше денег каждый день!
Забирайте максимум удовольствия от игры на xbetegypt и получайте больше бонусов!
1xb http://1xbet-app-download-ar.com/.
Существуют определенные товары и категории товаров, которые подлежат обязательной сертификации перечень товаров не подлежащих сертификации
ed drugs compared generic ed drugs cost
powdered eyebrows near me
natural microblading
levaquin availability
займ без отказа без посредников https://займы-все.рф/mfo/zajmy-bez-posrednikov/
1xbet промокод при регистрации – комбинация из чисел и букв. Эта комбинация дает возможность игроку получить дополнительные бонусы. К примеру, это может быть: промокод на бесплатную ставку (фрибет); повышение коэффициентов ставок формата «экспресс». Промокод при регистрации применяется именно таким образом. Он позволяет увеличивать размер приветственного бонуса на первый депозит, который выдается самим букмекером 1xbet. Где найти? Вариантов для получения промокода на 1xbet на сегодня существует множество. Но мы предлагаем вводить наш собственный промокод для 1xbet. Это промокод для регистрации, он вводится в поле в регистрационной анкете. Промокод при регистрации на сегодня. Промокоды для БК и Казино — ежедневное обновление. Регистрация на сайте 1xBet бесплатная, но для начала игры и получения доступа к 1xbet промокоду при регистрации 2024, придется внести на игровой счет от 50 рублей. Особенности регистрации. Процедура создания профиля в букмекерской конторе 1xbet максимально упрощена. Для регистрации предусмотрены такие способы: В «1 клик». Чтобы создать учетную запись, нужно выбрать страну проживания и валюту, ознакомиться с пользовательским соглашением и кликнуть на клавишу «Регистрация». С помощью телефона.
При регистрации в БК Melbet игрокам предлагается самостоятельно выбрать стартовую награду: фрибет на $30 или 100% бонус на депозит до 7 000 RUB. Предлагаем Melbet , благодаря которому вы получите не только повышенный до 10 400 RUB бонус на первое пополнение счета, но и право на бесплатный прогноз. Приветствовать новых клиентов бонусами стало хорошей традицией букмекерской конторы. На протяжении нескольких лет награда на депозит радовала сотни тысяч новичков и стремительно увеличивалась в размере. В 2024 году вознаграждение за пополнение счета достигло суммы в 7 000 российских рублей. Мы делаем более выгодное предложение. Игроки, которые введут в промокод мелбет при регистрации — RS777, не просто увеличат максимальный размер бонуса на депозит до 10 400 RUB, но и получат возможность воспользоваться фрибетом на 400 российских рублей.
Каждый электрик устанавливает разные расценки на услуги, вы можете их сравнить и выбрать подходящие для себя электрик Запорожье
Каждый электрик устанавливает разные расценки на услуги, вы можете их сравнить и выбрать подходящие для себя аварийный вызов электрика
Adult website
online porn both
Protonix for peptic ulcers
https://tinyurl.com/ylhas8n6
Новогоднее обращение президента Европы
сериал
Я извиняюсь, но, по-моему, Вы не правы. Я уверен. Предлагаю это обсудить.
позначте в запиті, кого вас цікавить, https://adarshaautomation.com/materials-manufacturing-education/ ми підкажемо вам оптимальний метод. Намагаюся в роботі використовувати індивідуальний підхід. потрібно допомога з підбором репетитора?
https://tinyurl.com/ypfysjpg
Новогоднее обращение президента Деловой Европы
онлайн
https://tinyurl.com/yvxbrea4
Записаться к психологу в москве цены » [Записаться к психологу в москве цены]
Записаться к психологу в москве цены
http://tinyurl.com/yll7jamd
https://tinyurl.com/yqp5pwdj
Только тут лучшие можно купить чехол на телефон xiaomi.
http://tinyurl.com/ymj35j3a
http://tinyurl.com/ymj35j3a
http://tinyurl.com/yt458cym
https://tinyurl.com/ykqu3kzs
онлайн
https://tinyurl.com/ykp6szjd
онлайн
https://tinyurl.com/2x8fmw9q
онлайн
https://tinyurl.com/yvaggme4
can i get cheap zithromax for sale
http://tinyurl.com/ytvjlqsn
https://tinyurl.com/ynn98fv4
Промокод при регистрации 1xbet — бонус для новых игроков. Бонус за первый депозит в 1xbet. Как получить и отыграть бонус 32500 руб в букмекерской конторе 1хбет. промокод 1xbet . Букмекерские конторы пользуются спросом у людей, чьи интересы плотно связаны со спортом и чей азарт подкрепляется возможностью вознаграждения путем внесения порой незначительной суммы. Вводите промокод 1xbet в 2024 году, чтобы получить бонус на первый депозит до 32 500 рублей. 1хбет промокод работает только при регистрации новых пользователей. Бесплатный промокод 1xbet при регистрации. Как ввести промокод 1xbet сегодня? Как отыграть бонус по промокоду 1xbet. Используйте промокод 1xbet при регистрации в 2024 году, чтобы получить бонус до 32500 рублей от крупнейшей букмекерской конторы!
https://tinyurl.com/ykqu3kzs
https://tinyurl.com/yksf352o
серия
Новогоднее поздравление год
https://tinyurl.com/ytm6nz96
http://amoxil.icu/# amoxicillin 500 capsule
New porn
онлайн
Новогоднее поздравление от деда мороза
сериал
levaquin 500 mg coupons
сериал
https://tinyurl.com/yof9ukyu
https://tinyurl.com/yquaz6ad
https://tinyurl.com/ysck5pym
http://tinyurl.com/ymj35j3a
Выбирайте из лучших языковых лагерей 2024 детский языковой лагерь в подмосковье рейтинг лагерей с отзывами, фото и описанием лагерей.
онлайн
Выбирайте из лучших языковых лагерей 2024 лагерь в подмосковье с английским языком рейтинг лагерей с отзывами, фото и описанием лагерей.
смотреть
серия
that, and found that as well as she could guess she
Exciting project! Mercedes-Benz places by Binghatti – in Downtown Dubai promises luxury, innovation, and elegance. A benchmark in Dubai’s real estate scene
https://tinyurl.com/yksf352o
Car insurance coverage must be modified to your steering practices. If you steer much less, you might spend much less.
https://tinyurl.com/yrgvbokw
medicine amoxicillin 500: buy amoxicillin online cheap – price for amoxicillin 875 mg
how to get cheap tinidazole for sale
http://tinyurl.com/yll7jamd
Karachi Call Girls are available for all kinds of occasions. You can hire them to accompany you at your party, on a date, or at your home. They are open all day, every day. You can even get them for fun trips! They can provide you with an exclusive environment while you are alone.
All girls so good looking and hot body Girls, sexy girls, teens girls, Ramp walk girls, teacher girls, busty girls, and call girls in islamabad Are you looking for reliable escorts agency to find a perfect date for yourself? We are here to serve you 24/7. We have educated girls of Colleges who enjoys having sex and romance. They are wild in bed and give you ultimate satisfaction guaranteed. They are shaved and will come in outclass outfit to spend a memorable time with you. They will s**k your tool like a lollipop and have sex in your favorite position. We are providing services call girls in Islamabad areas. Out-Call Services Provide in Hotels, Guest Houses and Your Location but if you want girl in your location then you pick from our location. Your Satisfaction is our 1st priority so don’t be feel shy and Contact with me.
https://tinyurl.com/yp2un5ln
https://tinyurl.com/ywzcbdwr
серия
https://tinyurl.com/ysywtm5s
онлайн
http://tinyurl.com/yovw73vh
мухомор пантерный купить в москве https://dobriy-muxomor.ru/
http://tinyurl.com/yt7je5lz
http://tinyurl.com/ymj35j3a
http://tinyurl.com/ytvjlqsn
Medication prescribing information. Drug Class.
flibanserina buy
Best what you want to know about medicines. Read now.
Большой выбор квадрокоптеров в интернет-магазине по выгодным ценам квадрокоптер
https://tinyurl.com/ylz2yzzj
Бесплатные промокоды на 2024 от букмекерской конторы 1xBet: при регистрации, на бесплатную ставку. Рассказываем, как использовать и куда вводить промокоды в 1хБет. промокод 1хбет . Бесплатный промокод для увеличения бонуса. Букмекерская контора 1хБет – одна из самых популярных беттинговых площадок, предлагающая высокие коэффициенты, широкую линию с дополнительной росписью. Благодаря низкой марже БК пользователи стабильно зарабатывают на ставках на спорт. Отличительной особенностью букмекерской конторы 1xBet является возможность совершения ставок по промокодам, которые предоставляются бесплатно.
http://tinyurl.com/ys9nru7l
Wow, its great. Really
Букмекерская контора Melbet является одним из столпов международной беттинговой индустрии. За счет масштабной маркетинговой компании, высоких коэффициентов и оперативной технической поддержки БК Мелбет удалось привлечь и удержать большое количество игроков. На сегодняшний день, букмекер предлагает получить один из самых высоких бонусов на рынке – 10400 рублей. Размер бонуса в Melbet составляет 100% от суммы первого пополнения, но не менее 100 рублей и не более 10400. К примеру, если пополнить баланс на сумму 4000, то справа от основного счета появится бонусный. Как видим, использовать рабочий промокод Melbet при регистрации имеет смысл, особенно тем бетторам и бонусхантерам, которые привыкли заключать пари по-крупному. С учетом того, что он бесплатный – воспользоваться им может абсолютно любой игрок.
https://tinyurl.com/yrgvbokw
https://tinyurl.com/ypks4dw7
https://tinyurl.com/ymhauynq
https://tinyurl.com/ysuhztlz
https://printablecalendar.top/
Аренда мощного дедика (VPS): Абузоустойчивость, Эффективность, Надежность и Защита от DDoS от 13 рублей
В современном мире онлайн-проекты нуждаются в надежных и производительных серверах для бесперебойной работы. И здесь на помощь приходят мощные дедики, которые обеспечивают и высокую производительность, и защищенность от атак DDoS. Компания “Название” предлагает VPS/VDS серверы, работающие как на Windows, так и на Linux, с доступом к накопителям SSD eMLC — это значительно улучшает работу и надежность сервера.
https://tinyurl.com/2xcr3qdf
Je recommande cette très belle pochette Pablo Exclusive Grape Ice
I’ve possessed a wonderful knowledge along with
cheap Car insurance Chicago
insurance coverage up until now. Client company and also insurance coverage have actually been actually greater than acceptable.
Только у нас лучшая краска порошковая. Рекомендую!
сериал
http://tinyurl.com/yll7jamd
бетон щелково
Novost
online prescription cefixime 400
https://tinyurl.com/ytxb75ef
https://tinyurl.com/ylhdz426
https://tinyurl.com/ykqu3kzs
онлайн
серия
urenrjrjkvnm
%%
Check out my web blog :: https://icar2005.org/
https://tinyurl.com/ym8rukbr
Рабочий промокод 1ХБЕТ на 2024 год бесплатно: Бонус 32 500р. Актуальный список при регистрации на официальном сайте компании. На бесплатную ставку и витрина промо-кодов. Откуда взять и куда вставить промокоды описано на странице. Код необходимо использовать при регистрации на официальном сайте конторы 1xbet (промокоды для купона -на бесплатную ставку, находятся в самом низу статьи). 1xbet промокод ! Как ввести промокод 1хБет при регистрации в 2024. Вводятся такие комбинации в купон пари, позволяя сделать прогноз бесплатно, застраховать ставку или извлечь любую другую выгоду от обладания бонусным кодом. К сожалению, найти промокод в свободном доступе невозможно, их игроки получают индивидуально и вряд ли заходят делиться халявой с обывателями интернета.
сериал
https://tinyurl.com/ymhauynq
https://tinyurl.com/2x8fmw9q
http://tinyurl.com/yt458cym
Промокод – это комбинация символов, которую вводят в специально отведенную строку на сайте. После активации кода, пользователь получит вознаграждение от любимого БК. Обычно к промокоду прилагается подробное описание всех предлагаемых бонусов. Но иногда букмекеры позволяют игрокам выяснить назначение кода самостоятельно, ведь многие любят сюрпризы. В случае с промокодом, сюрприз наверняка окажется приятным, ведь его главная цель – создать игроку комфортные условия, заслужить лояльность. Существуют промокоды для новых игроков, которые действительны только при регистрации, и для постоянных – окно для ввода таких кодов находится под формой пополнения игрового баланса. промокод для мелбет Введите: RS777 и тогда при депозите вы получите бонус 10400 рублей автоматически. Букмекерская контора Мелбет в 2024 году создала комфортные условия для заядлых беттеров и новых пользователей. Промокоды – вещь распространенная, потому найти их легко. Часто букмекеры размещают коды в свободном доступе, для всеобщего пользования. А промокоды для более значимых наград поступают игрокам индивидуально, например в качестве подарка ко дню рождения, извинения за возможные неудобства или просто в благодарность за сотрудничество.
https://tinyurl.com/yn6yw6dg
серия
Medicament prescribing information. Drug Class.
celebrex
Everything about medication. Get information now.
http://treveltour.ru/
https://tinyurl.com/ylgwd8wn
Выбирайте и бронируйте бесплатно путевки в языковые детские лагеря английский лагерь в подмосковье
https://tinyurl.com/yqgjrvtt
серия
Payday loans in Delaware
%%
Also visit my web blog … https://carolwincenc.com/
смотреть
https://tinyurl.com/ypqeuxrn
https://tinyurl.com/ysuhztlz
cost of aurogra without insurance
онлайн
http://tinyurl.com/yna3d7af
https://mymoscow.forum24.ru/?1-5-0-00000865-000-0-0-1703080521
Life
During this period of transition, Viktor Yevhenovich Ponomarchuk showed himself as a far-sighted leader, recognizing and using fresh opportunities in a changing environment victor evgenevich ponomarchuk
at all to come up-on them this size: why I should
During this period of transition, Viktor Yevhenovich Ponomarchuk showed himself as a far-sighted leader, recognizing and using fresh opportunities in a changing environment victor ponomarchuk
серия
сериал
http://offtop.ru/besedka/v2_2912618__.php
онлайн
сериал
Холоп смотреть онлайн бесплатно в хорошем качестве. Смотреть фильм холоп онлайн бесплатно в хорошем качестве. Смотреть холоп бесплатно в хорошем качестве. Холоп 2 фильм. Холоп фильм смотреть онлайн бесплатно. Холоп 2 смотреть онлайн. Холоп актеры и роли. Холоп смотреть. Трейлер холоп 2. Где найти фильм холоп в хорошем качестве бесплатно.
ce-cream, roast fowl, and hot toast), she soon drank it off.
Cortexi is a completely natural product that promotes healthy hearing, improves memory, and sharpens mental clarity. Cortexi hearing support formula is a combination of high-quality natural components that work together to offer you with a variety of health advantages, particularly for persons in their middle and late years. Cortex not only improves hearing but also decreases inflammation, eliminates brain fog, and gives natural memory protection.
https://tinyurl.com/ywu9glvm
https://tinyurl.com/yu825wjh
казино игры онлайн
серия
казино европейские онлайн
https://tinyurl.com/yq3eblj3
? Отсутствует пример употребления http://xn--d1abifnynv.xn--p1ai/index.php?subaction=userinfo&user=alyduwi (см. рекомендации). ? То-то нарядилась, как недешевенькая эскортница… Корень: -эскорт-; суффикс: -ниц; окончание: -а.
онлайн
Это сделать просто, если иметь промокод 1xbet на сегодня бесплатно. Правда, дается он при условии выполнения некоторых правил. промокод на 1xbet . Не совсем промокод, но вы все равно ставите не свои деньги, если пополните депозит, – 100% бонуса от внесенной суммы. Максимум указан в верхней части главной страницы официального сайта. 100% бонус за пополнение от 1xbet. Но прежде чем получить бонус нужно пройти регистрацию. Зайдите на сайт БК 1xBet и нажмите по стрелке кнопку «Регистрация». 2. Выберите один из методов регистрации (самый быстрый — в один клик). Кликните на «Зарегистрироваться».
Мелбет – международный букмекер, основанный в 2012 году. Компания получила официальную лицензию от Кюрасао, ориентирована на пользователей со всех стран мира, но в первую очередь на русскоязычных игроков. Зарегистрированные клиенты имеют прекрасную возможность пользоваться всеми преимуществами компании, принимать участие в акциях, собирать выигрышные экспрессы, получать промокоды и бесплатные ставки. Компания Мелбет регулярно предоставляет своим клиентам большое количество бонусов и промокоды. Что дает Melbet ? Данное поощрение позволяет каждому игроку совершать бесплатные ставки, получать дополнительные денежные средства при пополнении игрового баланса. Кроме этого, благодаря промокодам сумма первого депозита может увеличиться до 100%. Букмекерская контора дарит бесплатные ставки для новых игроков и фрибеты для постоянных пользователей.
https://tinyurl.com/yr4kyljl
казино популярные онлайн
серия
хороший казино онлайн
смотреть
Medicine information for patients. Effects of Drug Abuse.
celebrex without prescription
All information about drug. Get here.
http://tinyurl.com/yll7jamd
https://tinyurl.com/2x8fmw9q
смотреть
https://sutochnogrodno.by/
https://tinyurl.com/yp8eo9mb
Novost
https://tinyurl.com/ytlv3n6g
смотреть
Erec Prime is a cutting-edge male enhancement formula with high quality raw ingredients designed to enhance erection quality and duration
https://tinyurl.com/ysywtm5s
серия
Холопы это. Кто такой холоп. Холоп 2. Холоп фильм смотреть онлайн. Холоп 1. Про холопа примерного якова верного. Смотреть холоп бесплатно. Холоп смотреть онлайн бесплатно в хорошем качестве лордфильм. Холоп 2 смотреть. Смотреть фильм холоп онлайн бесплатно в хорошем качестве.
http://tinyurl.com/yt7je5lz
https://tinyurl.com/ytun7cj9
сайты для знакомств
сайт знакомств рейтинг
Холоп 2 смотреть бесплатно. Холоп смотреть бесплатно. Холоп актеры и роли. Кто такой холоп. Холоп 1. Холоп смотреть. Холоп 2 смотреть онлайн бесплатно в хорошем. Смотреть фильм холоп. Холоп 1 смотреть. Смотреть фильм холоп бесплатно.
urenrjrjkvnm
сайт знакомств natalie
сайт бибо знакомства
Фильм холоп смотреть. Смотреть холоп бесплатно в хорошем качестве. Трейлер холоп 2. Холоп 2 дата выхода в россии. Холоп 2 смотреть. Холоп фильм 2024 смотреть онлайн бесплатно в хорошем качестве hd 1080 бесплатно полностью лорд фильм.
Советую именно эту краска порошковая купить. Рекомендую!
Смотреть холоп бесплатно в хорошем качестве. Актеры холоп. Холоп 2 трейлер на русском. Холоп смотреть. Фильм холоп смотреть онлайн. Холоп 2. Скачать фильм холоп. Фильм холоп актеры.
15000 euro lenen
lexapro cost walmart
https://sutochnogrodno.by/
porn videos
Life
Touche. Outstanding arguments. Keep up the great spirit.
Novost
Интернет магазин предлагает купить оптом и в розницу современное медицинское оборудование и технику для частных и государственных клиник купить медицинское оборудование в кирове
Интернет магазин предлагает купить оптом и в розницу современное медицинское оборудование и технику для частных и государственных клиник медицинское оборудование для стоматологии купить
Промокоды казино 1xBet при регистрации 2024. На ресурсе 1хБет пользователи могут не только делать ставки на спорт и другие события из разных сфер, но и получать азартные ощущения в казино. Играть можно как с машинами, так и с реальными дилерами в разделе лайв. Чтобы привлекать как можно больше новых игроков и поддерживать интерес постоянных клиентов, на сайте 1хБет регулярно проходят акции и раздают бонусы. Самое щедрое вознаграждение могут получить новички, использовав промокод казино 1xBet. Указав его при регистрации, пользователь получит дополнительные денежные средства на первые несколько депозитов, которые сможет использовать для ставок в играх. Это сделать просто, если иметь промокод на 1хбет . Правда, дается он при условии выполнения некоторых правил. 1xbet бонус при регистрации. Не совсем промокод, но вы все равно ставите не свои деньги, если пополните депозит, – 100% бонуса от внесенной суммы. Максимум указан в верхней части главной страницы официального сайта.
Букмекерская контора Melbet является одним из столпов международной беттинговой индустрии. За счет масштабной маркетинговой компании, высоких коэффициентов и оперативной технической поддержки БК Мелбет удалось привлечь и удержать большое количество игроков. На сегодняшний день, букмекер предлагает получить один из самых высоких бонусов на рынке – 10400 рублей. Размер бонуса в Melbet составляет 100% от суммы первого пополнения, но не менее 100 рублей и не более 10400. К примеру, если пополнить баланс на сумму 4000, то справа от основного счета появится бонусный. Как видим, использовать мелбет промокод на сегодня имеет смысл, особенно тем бетторам и бонусхантерам, которые привыкли заключать пари по-крупному. С учетом того, что он бесплатный – воспользоваться им может абсолютно любой игрок.
квартиры на сутки в гродно
екатерина лагута
Medication information. Short-Term Effects.
lisinopril tablet
Best about medicine. Get now.
лапландия бренд одежды
зона фильмы скачать
кентавр фильм скачать
Холоп фильм смотреть онлайн бесплатно в хорошем качестве. Холоп смотреть онлайн бесплатно в хорошем. Холоп 2 актеры. Фильм холоп. Холоп 2 смотреть бесплатно. Смотреть фильм холоп онлайн бесплатно в хорошем качестве. Холоп фильм. Актеры фильма холоп. Холоп фильм 2024 смотреть. Кто такой холоп.
скачать фильм отступники
скачать фильм марсианин
Aizen Power is a dietary supplement for male enhancement sexual health that is designed to help enhance men’s sexual performance and improve overall health.
FitSpresso stands out as a remarkable dietary supplement designed to facilitate effective weight loss. Its unique blend incorporates a selection of natural elements including green tea extract, milk thistle, and other components with presumed weight loss benefits.
снять квартиру в гродно на сутки
This is actually an enlightening part! I have actually been looking for this
sort of comprehensive details for rather some opportunity.
Thanks for discussing.
my site :: Cheap SR22 insurance
Список бесплатных на сегодня промокодов 1xBet. Тип бесплатного промокода. Промокод промокод на бесплатную ставку. промокод для 1xbet . Как сегодня получить 32500 рублей по промокоду в 1xBet? Получение начинается после регистрации с рабочим промокодом и первого пополнения счета и составляет +100% к депозиту. Игрок может рассчитывать по промокоду до 32 500 рублей, если пройдет верификацию и даст согласие на участие в рекламных предложениях букмекера. На сегодня акция по промокоду 1xBet распространяется на пользователей из России, Беларуси, Украины, Казахстана.
скачать фильмы анвар
анвап скачать фильм
Neotonics is an essential probiotic supplement that works to support the microbiome in the gut and also works as an anti-aging formula. The formula targets the cause of the aging of the skin.
porn videos
The child’s favorite Christmas gift was the large box her father’s lawnmower came in.
EyeFortin is a natural vision support formula crafted with a blend of plant-based compounds and essential minerals. It aims to enhance vision clarity, focus, and moisture balance.
скачать фильм анвап
скачать фильм шалун
digital услуги
Attractive section of content I just stumbled upon your blog and in accession capital to assert that I get actually enjoyed account your blog posts Anyway I will be subscribing to your augment and even I achievement you access consistently fast
в этих углублениях ненужная мебель, снять квартиру на сутки в гродно зачастую наблюдаются неприятности с коммуникациями (водою, и отоплением). Квартиросъёмщик делает выбор, чаще в зависимости от стоимости.
24 xxx
Правильный Промо-Код ХБЕТ на 2024 год. На нашем сайте вы найдете промокоды на разные суммы: на депозит, пополнение и простой. Букмекерская контора 1X Bet только новым людям дарит подарки. 1хбет промокод . Активируйте промокоды и делайте ставки на футбол, хоккей и самые яркие состязания – Лиги Европы ?? и Лиги Чемпионов. Где найти промокод 1xbet на сегодня бесплатно? Использовав промокод казино 1xBet, игрок получает денежные средства на бонусный счет. Это значит, что он может использовать их только для игры в слоты и другие азартные развлечения на сайте. Вывести деньги, выигранные с бонуса, игрок сможет только тогда, когда отыграет их согласно вейджеру. Зарабатывайте баллы и меняйте на купоны или пользуйтесь халявными бонусами.
Здравствуйте, игроки на xbetegypt!
Получите успеха на xbetegypt с лучшими бонусами!
Делайте азартом на нашем сайте каждый день!
Сделайте вашу игру на xbetegypt с нашими лучшими предложениями!
Не упустите свой шанс на xbetegypt и освойте самые большие призы!
Превратите свои мечты в реальность с xbetegypt каждый день!
Становитесь частью нашего сообщества и заработайте больше денег!
Измените свою жизнь с xbetegypt и добейтесь все!
Научитесь играть на xbetegypt и забирайте все больше выигрышей!
Получайте удовольствие от игры на xbetegypt и восстанавливайте свои силы!
Раскройте свой потенциал игры на xbetegypt и зарабатывайте больших успехов!
Удивляйтесь от игры на xbetegypt и изучайте новые возможности каждый день!
Войдите в мир xbetegypt игры и добивайтесь большими бонусами!
Забудьте о неудачах с xbetegypt каждый день!
Играйте вместе с друзьями на xbetegypt и получайте большими выигрышами!
Получите свои навыки на xbetegypt и получите еще больше денег!
Взламывайте игры на xbetegypt и получайте большие бонусы каждый день!
Играйте сегодня на xbetegypt и отличайтесь!
Успейте играть на xbetegypt и получайте больше денег каждый день!
Наслаждайтесь максимум удовольствия от игры на xbetegypt и получайте больше бонусов!
Download 1xbet program for iPhone https://www.1xbet-app-download-ar.com.
In the field of oils and fats processing, Viktor stands out due to the harmonious combination of his interests and ViOil’s strategies віктор пономарчук vioil
проститутки метро щукинская https://a.fanfap.nl/
In the field of oils and fats processing, Viktor stands out due to the harmonious combination of his interests and ViOil’s strategies виктор евгеньевич пономарчук
it agency
зона скачать фильм
фильм платформа скачать
скачать фильм разлом
Terrific write ups Thank you!
скачать фильм комедии
GlucoBerry is one of the biggest all-natural dietary and biggest scientific breakthrough formulas ever in the health industry today. This is all because of its amazing high-quality cutting-edge formula that helps treat high blood sugar levels very naturally and effectively.
План политическое лидерство. Лидерство курс. Трансформационное лидерство это. Особенности политического лидерства. Лидерство синонимы. Перечислите принципы лидерства. Какие выделяют теории лидерства.
porn videos
remeron
купить зеркало на входную дверь https://vhodnye-dveri-s-zerkalom77.ru/
프라그마틱 신규 게임
무작위로 선택한 사람이며 속일 수 없습니다.
Всем рекомендую только самое качественное и выгодное казино вавада.
SynoGut is an all-natural dietary supplement that is designed to support the health of your digestive system, keeping you energized and active.
Endo Pump Male Enhancement is a dietary supplement designed to assist men improve their sexual performance. This natural formula contains a potent blend of herbs and nutrients that work together to improve blood flow
Dentitox Pro is a liquid dietary solution created as a serum to support healthy gums and teeth. Dentitox Pro formula is made in the best natural way with unique, powerful botanical ingredients that can support healthy teeth.
Gorilla Flow is a non-toxic supplement that was developed by experts to boost prostate health for men. It’s a blend of all-natural nutrients, including Pumpkin Seed Extract Stinging Nettle Extract, Gorilla Cherry and Saw Palmetto, Boron, and Lycopene.
Nervogen Pro, A Cutting-Edge Supplement Dedicated To Enhancing Nerve Health And Providing Natural Relief From Discomfort. Our Mission Is To Empower You To Lead A Life Free From The Limitations Of Nerve-Related Challenges. With A Focus On Premium Ingredients And Scientific Expertise.
SonoVive™ is an all-natural supplement made to address the root cause of tinnitus and other inflammatory effects on the brain and promises to reduce tinnitus, improve hearing, and provide peace of mind.
Glucofort Blood Sugar Support is an all-natural dietary formula that works to support healthy blood sugar levels. It also supports glucose metabolism. According to the manufacturer, this supplement can help users keep their blood sugar levels healthy and within a normal range with herbs, vitamins, plant extracts, and other natural ingredients.
GlucoCare is a natural and safe supplement for blood sugar support and weight management. It fixes your metabolism and detoxifies your body.
Лидерство картинки. Сущность лидерства проявляется в умении. Теодор рузвельт законы лидерства. Авторитарное лидерство предполагает единоличное направляющее воздействие лидера на подчиненных. Лекции по лидерству. Проблема социогуманитарного лидерства. По стилю общения лидера с подчиненными различают харизматический рационально легальный тип лидерства.
Amiclear is a dietary supplement designed to support healthy blood sugar levels and assist with glucose metabolism. It contains eight proprietary blends of ingredients that have been clinically proven to be effective.
GlucoFlush™ is an all-natural supplement that uses potent ingredients to control your blood sugar.
Claritox Pro™ is a natural dietary supplement that is formulated to support brain health and promote a healthy balance system to prevent dizziness, risk injuries, and disability. This formulation is made using naturally sourced and effective ingredients that are mixed in the right way and in the right amounts to deliver effective results.
%%
Look into my blog – ahicito.com
TerraCalm is an antifungal mineral clay that may support the health of your toenails. It is for those who struggle with brittle, weak, and discoloured nails. It has a unique blend of natural ingredients that may work to nourish and strengthen your toenails.
TropiSlim is a unique dietary supplement designed to address specific health concerns, primarily focusing on weight management and related issues in women, particularly those over the age of 40. TropiSlim targets a unique concept it refers to as the “menopause parasite” or K-40 compound, which is purported to be the root cause of several health problems, including unexplained weight gain, slow metabolism, and hormonal imbalances in this demographic.
Introducing FlowForce Max, a solution designed with a single purpose: to provide men with an affordable and safe way to address BPH and other prostate concerns. Unlike many costly supplements or those with risky stimulants, we’ve crafted FlowForce Max with your well-being in mind. Don’t compromise your health or budget – choose FlowForce Max for effective prostate support today!
сайт знакомств бебоо
jolly сайт знакомств
Теория лидерства. Критерии эффективного лидерства. Согласно какой теории руководства и лидерства лидерами рождаются а не становятся. Стили лидерства. Лидерство в организации это. Майнор лидерство. Выбор мировое господство или глобальное лидерство. Лекции по лидерству. Ситуационная теория лидерства общая характеристика.
Центр цифрового лидерства sap. Тренинг лидерство для руководителей. На практике под термином лидерство чаще всего подразумевают лидерство. Женское лидерство. В числе главных признаков лидерства. Школа лидерства. Наибольшую известность получила типология трех стилей лидерства автором которой является. Эффективное лидерство.
сайты знакомств крым
Школа лидерства. Каковы причины потери англией промыш лидерства. Курсы лидерства для детей. Как соотносятся между собой власть влияние лидерство. Основы лидерства. Лидерство и командообразование. Демократический тип лидерства это.
сайты секс знакомств
Ситуационное лидерство это. Тренинг лидерства. Тест на лидерство в коллективе. Тренинги по лидерству для руководителей. Лидерство в социальной психологии это. Авторы личностного подхода к лидерству преследовали цель выявить и описать присущие лидерам. Уровни лидерства. Участвующий стиль лидерства это.
Дедик сервер
Абузоустойчивый сервер для работы с Хрумером, GSA и всевозможными скриптами!
Есть дополнительная системах скидок, читайте описание в разделе оплата
Виртуальные сервера (VPS/VDS) и Дедик Сервер: Оптимальное Решение для Вашего Проекта
В мире современных вычислений виртуальные сервера (VPS/VDS) и дедик сервера становятся ключевыми элементами успешного бизнеса и онлайн-проектов. Выбор оптимальной операционной системы и типа сервера являются решающими шагами в создании надежной и эффективной инфраструктуры. Наши VPS/VDS серверы Windows и Linux, доступные от 13 рублей, а также дедик серверы, предлагают целый ряд преимуществ, делая их неотъемлемыми инструментами для развития вашего проекта.
доставка есс пицца
https://www.google.co.nz/url?q=https://www.coinsbar.net/ru/
https://www.google.co.ve/url?q=https://www.coinsbar.net/ru/
краснодар доставка пиццы
доставка пиццы новокузнецк
might have shrunk to the size of a gnat.
seo solutions
napishi text please
Главное – отлично выглядеть, http://mclassic.com.hk/home.php?mod=space&uid=270665 а для девушки такая ситуация нет большого труда.
Лидерство в группе. Политическое лидерство это. Стили руководства и лидерства. Типология политического лидерства. Стратегическое лидерство. Теория ситуационного лидерства. Директивный стиль лидерства.
I have actually possessed a great expertise along with cheap auto insurance coverage up until now. Consumer company and also coverage have been actually much more than satisfying.
https://vodosnab-msk.ru/
Типы политического лидерства. Каковы причины потери англии промышленного лидерства. Традиционный тип лидерства. Осознанное лидерство. Лидерство купить. Лидерство и управление командой. Факторы формирования лидерства.
Теории происхождения лидерства. Тренинги по лидерству. Женское лидерство. Педагогика и психология лидерства и командной работы. . Атрибутивное лидерство.
Пять сфер лидерства. Модели лидерства в менеджменте. Установите соответствие аспектов лидерства и их содержания. Ценовое лидерство. В конце 19 начале 20 века возникают такие концепции лидерства как. Как показать собаке свое лидерство.
Какой стиль лидерства используется в управлении чаще всего. Сферы лидерства россии. На практике под термином лидерство чаще всего подразумевают лидерство. Программы стратегического академического лидерства приоритет 2030. Тренинг по лидерству. Лидерство тренинг.
Howdy! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to get my
blog to rank for some targeted keywords but I’m not seeing very good results.
If you know of any please share. Appreciate it!
Что такое сетевое лидерство. Сущность политического лидерства. Курт левин лидерство. Книга лидерство. Слушать аудиокнигу манипуляция и лидерство бесплатно. Неформальное лидерство.
I am regular visitor, how are you everybody? This post posted at this site is actually fastidious.
Складчина (совместная покупка) курса, всего за 1ye карина искхакова
смотреть сериалы онлайн тут https://sys-con.tv/
кухонный гарнитур в спб по выгодной цене
Кухонные комплекты из натурального дерева в спб на заказ
Долговечные кухни от производителя в спб недорого
Кухни-гармония в спб с доставкой и монтажом
Специальные предложения на кухни в спб только у нас
Эксклюзивные кухни в спб для вашего дома
Кухни для дружной семьи в спб по индивидуальному заказу
Стильные кухонные гарнитуры для спб от ведущих производителей
Экономные кухни в спб для квартиры или загородного дома
Практичные кухонные уголки для небольшой площади в спб
Индивидуальный подход для создания вашей кухни в спб
Неповторимая атмосфера для вашей кухни в спб
Огромный выбор кухонной мебели в спб
Индивидуальный подход к производству для вашей кухни в спб
Надежная и долговечная мебель для вашей кухни в спб
Уникальный дизайн для вашей кухни в спб
Функциональная кухня в спб – место для семейных посиделок и приготовления вкусных блюд
Модные тренды для вашей кухни в спб
Бесплатная доставка для вашей кухни в спб
кухни петербурга на заказ недорого http://www.vip-kukhni-spb.ru/.
https://maps.google.la/url?q=https://www.tnlcompetition.com
“…” Fang Jifan의 이마는 식은 땀을 흘리며 우울했습니다.
Hey There. I found your blog using msn. This is a really
well written article. I’ll make sure to bookmark it and come back to read more
of your useful info. Thanks for the post. I’ll definitely comeback.
https://sutochnogrodno.by/
You have very nice post and pictures, please have a look at our photo
tours in the temples of Angkor
joy.bio
7000 euro lenen
This post offers clear idea in favor of the new visitors of blogging, that truly how to do blogging and site-building.
Life
Максимальный комфорт и удобство в вашем доме
печать больших форматов http://www.msk-naruzhnaya-reklama.ru.
synthroid 15
I am not sure where youre getting your info but good topic I needs to spend some time learning much more or understanding more Thanks for magnificent info I was looking for this information for my mission
LГҐna 40000 kr
https://wiki.iot-usergroup.de/index.php/Benutzer:DwayneFinsch
https://justmeclassified.com/user/profile/502569
When some one searches for his required thing, so he/she wants to be available that in detail, so that thing is maintained over here.
adult
Novost
https://portal.ruad.nl/question/rbc-ua/
http://shadowthemes.com/forums/users/danielas91/edit/?updated=true/users/danielas91/
Auto van insurance policy fees could be determined through where you stay.
Consider this when relocating to a brand new area.
https://tadacip2us.top
credit 13000 euros
urenrjrjkvnm
where to buy generic synthroid without rx
Абузоустойчивый сервер для работы с Хрумером, GSA и всевозможными скриптами!
Есть дополнительная системах скидок, читайте описание в разделе оплата
Виртуальные сервера (VPS/VDS) и Дедик Сервер: Оптимальное Решение для Вашего Проекта
В мире современных вычислений виртуальные сервера (VPS/VDS) и дедик сервера становятся ключевыми элементами успешного бизнеса и онлайн-проектов. Выбор оптимальной операционной системы и типа сервера являются решающими шагами в создании надежной и эффективной инфраструктуры. Наши VPS/VDS серверы Windows и Linux, доступные от 13 рублей, а также дедик серверы, предлагают целый ряд преимуществ, делая их неотъемлемыми инструментами для развития вашего проекта.
https://rabota.ys.tj/viewtopic.php?id=7835#p15628
Novost
A lathe steady rest is a crucial extra in metalworking and also carpentry that plays a substantial function in enhancing transforming reliability. This tool is developed to support and also stabilize long work surfaces throughout the machining procedure on a turret. Through reducing vibration as well as deflection, a lathe steady rest results in enhanced preciseness as well as area appearance, https://www.40billion.com/profile.asp?aid=245451139.
credit 9500 euros
24 xxx
https://www.php-einfach.de/2022/05/die-hauptgruende-fuer-den-zuwachs-in-krypto-betrug/
prednisone 40mg: 15 mg prednisone daily – prednisone 15 mg daily
Medicine information leaflet. What side effects can this medication cause?
lisinopril medication
Best trends of drug. Read information now.
Sight Care is a daily supplement proven in clinical trials and conclusive science to improve vision by nourishing the body from within. The Sight Care formula claims to reverse issues in eyesight, and every ingredient is completely natural.
Novost
can i purchase clomid tablets: can you buy generic clomid for sale – where can i get cheap clomid pill
http://amoxil.icu/# buy amoxicillin 500mg canada
Thanks a lot for sharing this with all people you actually understand what you are speaking approximately!
Bookmarked. Kindly also visit my web site =). We can have a link trade arrangement between us
xxx [pl.24eblja.online]
While improving eyesight isn’t often the goal of consumers who wear their glasses religiously, it doesn’t mean they’re stuck where they are.
Подчеркните красоту окна с помощью электрокарниза
механизм для штор электрический http://www.prokarniz38.ru/.
buying generic clomid without insurance where to buy cheap clomid without dr prescription – can i purchase cheap clomid without rx
Medicament information. Effects of Drug Abuse.
aurogra without rx
Some news about meds. Get now.
Med
You could certainly see your enthusiasm in the work you write.
The world hopes for more passionate writers such
as you who aren’t afraid to say how they believe. At all times go
after your heart.
Здесь вы найдете официальный сайт 1Вин.
It’s hard to find experienced people in this particular subject,
however, you sound like you know what you’re talking about!
Thanks
buy synthroid price
http://ciprofloxacin.life/# purchase cipro
Эдуард Давыдов https://davydov-eduard.ru/.
https://marketblogs.ru/
This is really attention-grabbing, You are an overly skilled blogger.
I have joined your feed and stay up for looking for more of
your wonderful post. Also, I have shared your website in my
social networks
https://addcity.ru/
릴렉스 게이밍
다시 신이 난 일행은 미친 듯이 소리를 지르며 물마을로 향했다.
Pills information. Effects of Drug Abuse.
bactrim
Everything information about drug. Get information here.
Med
investing in tokenized real estate
real estate tokenization
Здравствуйте, хочу поделится информации об росте криптовалюты, вам стоит её купить http://www.lada-4×4.net/member.php?u=20263 что бы вы смогли заработать x3
vardenafil 10mg brand vardenafil where to buy
I never get tired of looking at articles on i-pets.com.ua about raising dogs. Great tips for newbies!
осоветуйте vps
Абузоустойчивый сервер для работы с Хрумером и GSA и различными скриптами!
Есть дополнительная системах скидок, читайте описание в разделе оплата
Виртуальные сервера VPS/VDS и Дедик Сервер: Оптимальное Решение для Вашего Проекта
В мире современных вычислений виртуальные сервера VPS/VDS и дедик сервера становятся ключевыми элементами успешного бизнеса и онлайн-проектов. Выбор оптимальной операционной системы и типа сервера являются решающими шагами в создании надежной и эффективной инфраструктуры. Наши VPS/VDS серверы Windows и Linux, доступные от 13 рублей, а также дедик серверы, предлагают целый ряд преимуществ, делая их неотъемлемыми инструментами для развития вашего проекта.
Pills information leaflet. Short-Term Effects.
stromectol prices
Some what you want to know about medicament. Get information here.
%%
Visit my page сиделка с проживанием
xxx video
buy cenforce 100mg sale order generic cenforce 50mg
Porn site
натяжной потолок в москве
голые девушки
generic ed medication ed drugs canada
Porn site
Настоятельно рекомендую только этот официальный сайт 1Win.
Drugs information. Cautions.
cialis super active
Everything trends of meds. Read now.
Здравствуйте, хочу поделится информации об росте криптовалюты, вам стоит её купить http://rtpsouth.com/UserProfile/tabid/69/userId/101246/Default.aspx что бы вы смогли заработать x3
best ed drugs for women non prescription erection pills
%%
Feel free to visit my page … h
vardenafil order online levitra 20mg cost
%%
my web page … http://velotrial.ru/366112
order clotrimazole
levaquin 500mg tablets
Qemtex specializes in producing Powder Coatings. Recommend!
民意調查
Drug prescribing information. Brand names.
singulair generic
Actual information about medication. Read information now.
民意調查是什麼?民調什麼意思?
民意調查又稱為輿論調查或民意測驗,簡稱民調。一般而言,民調是一種為了解公眾對某些政治、社會問題與政策的意見和態度,由專業民調公司或媒體進行的調查方法。
目的在於通過網路、電話、或書面等媒介,對大量樣本的問卷調查抽樣,利用統計學的抽樣理論來推斷較為客觀,且能較為精確地推論社會輿論或民意動向的一種方法。
以下是民意調查的一些基本特點和重要性:
抽樣:由於不可能向每一個人詢問意見,所以調查者會選擇一個代表性的樣本進行調查。這樣本的大小和抽樣方法都會影響調查的準確性和可靠性。
問卷設計:為了確保獲得可靠的結果,問卷必須經過精心設計,問題要清晰、不帶偏見,且易於理解。
數據分析:收集到的數據將被分析以得出結論。這可能包括計算百分比、平均值、標準差等,以及更複雜的統計分析。
多種用途:民意調查可以用於各種目的,包括政策制定、選舉預測、市場研究、社會科學研究等。
限制:雖然民意調查是一個有價值的工具,但它也有其限制。例如,樣本可能不完全代表目標人群,或者問卷的設計可能導致偏見。
影響決策:民意調查的結果常常被政府、企業和其他組織用來影響其決策。
透明度和誠實:為了維護調查的可信度,調查組織應該提供其調查方法、樣本大小、抽樣方法和可能的誤差範圍等詳細資訊。
民調是怎麼調查的?
民意調查(輿論調查)的意義是指為瞭解大多數民眾的看法、意見、利益與需求,以科學、系統與公正的資料,蒐集可以代表全部群眾(母體)的部分群眾(抽樣),設計問卷題目後,以人工或電腦詢問部分民眾對特定議題的看法與評價,利用抽樣出來部分民眾的意見與看法,來推論目前全部民眾的意見與看法,藉以衡量社會與政治的狀態。
以下是進行民調調查的基本步驟:
定義目標和目的:首先,調查者需要明確調查的目的。是要了解公眾對某個政策的看法?還是要評估某個政治候選人的支持率?
設計問卷:根據調查目的,研究者會設計一份問卷。問卷應該包含清晰、不帶偏見的問題,並避免導向性的語言。
選擇樣本:因為通常不可能調查所有人,所以會選擇一部分人作為代表。這部分人被稱為“樣本”。最理想的情況是使用隨機抽樣,以確保每個人都有被選中的機會。
收集數據:有多種方法可以收集數據,如面對面訪問、電話訪問、郵件調查或在線調查。
數據分析:一旦數據被收集,研究者會使用統計工具和技術進行分析,得出結論或洞見。
報告結果:分析完數據後,研究者會編寫報告或發布結果。報告通常會提供調查方法、樣本大小、誤差範圍和主要發現。
解釋誤差範圍:多數民調報告都會提供誤差範圍,例如“±3%”。這表示實際的結果有可能在報告結果的3%範圍內上下浮動。
民調調查的質量和可信度很大程度上取決於其設計和實施的方法。若是由專業和無偏見的組織進行,且使用科學的方法,那麼民調結果往往較為可靠。但即使是最高質量的民調也會有一定的誤差,因此解讀時應保持批判性思考。
為什麼要做民調?
民調提供了一種系統性的方式來了解大眾的意見、態度和信念。進行民調的原因多種多樣,以下是一些主要的動機:
政策制定和評估:政府和政策制定者進行民調,以了解公眾對某一議題或政策的看法。這有助於制定或調整政策,以反映大眾的需求和意見。
選舉和政治活動:政黨和候選人通常使用民調來評估自己在選舉中的地位,了解哪些議題對選民最重要,以及如何調整策略以吸引更多支持。
市場研究:企業和組織進行民調以了解消費者對產品、服務或品牌的態度,從而制定或調整市場策略。
社會科學研究:學者和研究者使用民調來了解人們的社會、文化和心理特征,以及其與行為的關係。
公眾與媒體的期望:民調提供了一種方式,使公眾、政府和企業得以了解社會的整體趨勢和態度。媒體也經常報導民調結果,提供公眾對當前議題的見解。
提供反饋和評估:無論是企業還是政府,都可以透過民調了解其表現、服務或政策的效果,並根據反饋進行改進。
預測和趨勢分析:民調可以幫助預測某些趨勢或行為的未來發展,如選舉結果、市場需求等。
教育和提高公眾意識:通過進行和公布民調,可以促使公眾對某一議題或問題有更深入的了解和討論。
民調可信嗎?
民意調查的結果數據隨處可見,尤其是政治性民調結果幾乎可說是天天在新聞上放送,對總統的滿意度下降了多少百分比,然而大家又信多少?
在景美市場的訪問中,我們了解到民眾對民調有一些普遍的觀點。大多數受訪者表示,他們對民調的可信度存有疑慮,主要原因是他們擔心政府可能會在調查中進行操控,以符合特定政治目標。
受訪者還提到,民意調查的結果通常不會對他們的投票意願產生影響。換句話說,他們的選擇通常受到更多因素的影響,例如候選人的政策立場和政府做事的認真與否,而不是單純依賴民調結果。
從訪問中我們可以得出的結論是,大多數民眾對民調持謹慎態度,並認為它們對他們的投票決策影響有限。
generic ed drugs cost non prescription ed pills
Хай, хочу поделится информации об росте криптовалюты, вам стоит её купить https://dom.zeleniymis.com.ua/profile/428-kirilexs/content/?type=forums_topic_post что бы вы смогли заработать x3
Howdy! Do you know if they make any plugins to help with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains. If you know of any please share. Kudos! darknet marketplace https://mydarknetmarketlinks.com
I enjoy just how you do not avoid questionable subjects.
Your honest technique is energizing.
my blog post :: Car insurance Las Vegas
best generic ed medication order ed pills
Давыдов Эдуард Маликович http://www.davydov-eduard.ru.
Слушать подряд все песни Сектор Газа онлайн бесплатно, скачать музыку, песни и все популярные треки группы сектор газа 30 лет
Drugs information. Short-Term Effects.
flibanserina rx
All what you want to know about medicines. Get information here.
최신 프라그마틱 게임은 iGaming에서 혁신적이고 표준화된 콘텐츠를 선보이며 슬롯, 라이브 카지노, 빙고 등 다양한 제품을 선택할 수 있습니다.
프라그마틱 관련 내용 정말 재미있게 읽었어요! 또한, 제 사이트에서도 프라그마틱과 관련된 정보를 공유하고 있어요. 함께 교류하며 더 많은 지식을 쌓아가요!
https://www.vamiveta.com/
%%
Review my page: https://spark-wiki.win/index.php?title=Aviator_game_website
Букмекерская компания Мелбет или известная в других кругах Melbet, имеет огромное количество игроков в онлайне. В первую очередь компания предоставляет высокие коэффициенты и сильную линию с лайвом. Это дает возможность игрокам профессионалом пользоваться конторой на полную катушку. Плюс, с помощью промокода вы получите бонус 10400 тысяч рублей. Без промо кода до 8000 тысяч. действующий промокод Melbet представляют собой бонусные возможности, которые дает сама букмекерская контора. Сегодня многие букмекеры предлагают такие бонусы как для впервые зарегистрировавшихся пользователей, так и для тех, кто давно занимается ставками на спорт. MelBet тоже не отстает от всеобщей тенденции и активно продвигает рекламу бонуса, раздаваемого в момент регистрации. Промокод Мелбет станет отличной базой для новичков и позволит попробовать свои возможности в бесплатных ставках или других подобных предложениях. Как получить такой промокод и применить его на деле, рассмотрим далее.
Промокод 1xBet при регистрации. Компания 1ИксБет заинтересована в привлечении новых клиентов, поэтому для новых игроков действует акция в виде бонуса, который равен сумме первого депозита, но не превышает 225 000 рублей. Однако при использовании промокода букмекерская контора увеличит размер приветственного бонуса. Для того чтобы получить повышенную сумму на первый депозит, игроку необходимо выполнить следующие условия: Зайти на сайт букмекера. Выбрать способ регистрации по e-mail. Заполнить поля с личными данными. Ввести промокод в поле слева от кнопки «Зарегистрироваться». Ознакомиться с правилами букмекера. что дает промокод в 1xbet поможет пользователям получить еще больше бонусов от букмекерской конторы. Подробная инструкция по поиску и активации бонусных кодов. Промокод — комбинация из цифр и букв, которая позволяет игроку активировать специальное предложение от букмекера 1хБет. С его помощью пользователь может получить: бонусные средства на депозит; бесплатную ставку; промо-баллы; другие подарки. Сегодня вы сможете найти множество подобных ресурсов, которые регулярно обновляют список актуальных предложений БК.
Этическое лидерство. Центр цифрового лидерства sap. Джон максвелл лидерство. Тренинг по лидерству для руководителей. Курсы по лидерству. Классификация политического лидерства. Мотивационные фильмы про успех и лидерство. Германия на пути к европейскому лидерству доклад.
Привет, хочу поделится информации об росте криптовалюты, вам стоит её купить http://www.u-turn.kz/forums.php?m=posts&q=22732&n=last#bottom что бы вы смогли заработать x3
It’s very good Lerus Offshore Certified Courses. I recommend!
http://doxycyclinebestprice.pro/# purchase doxycycline online
PЕЇjДЌka 700000 KДЌ
Лидерство без вранья. Политическое лидерство функции. Примеры лидерства в литературе. Тренинги лидерства. Картинки для презентации лидерство. Кен бланшар лидерство к вершинам успеха. Игры на лидерство.
https://lisinoprilbestprice.store/# prinivil 20 mg tablet
I really like your blog.. very nice colors
& theme. Did you create this website yourself or did you hire someone to do it for you?
Plz answer back as I’m looking to construct my own blog and would like to know
where u got this from. appreciate it
Эмоциональное лидерство книга. Эмоциональное лидерство. Мистика лидерства манфред кетс де врис. Эмоциональное лидерство искусство управления людьми на основе эмоционального интеллекта. Модель лидерства. Классификация политического лидерства.
Abortion pills online: Cytotec 200mcg price – cytotec buy online usa
http://lisinoprilbestprice.store/# lisinopril 5 mg buy online
%%
my web-site – https://tabaknasrednom.ru/%D1%81%D0%B0%D0%B9%D1%82-%D1%82%D0%B5%D1%85%D0%BD%D0%B8%D0%BA%D1%83%D0%BC%D0%B0-%D0%B0%D0%B2%D1%82%D0%BE%D1%81%D0%B5%D1%80%D0%B2%D0%B8%D1%81/
Промокод – небольшая цифробуквенная комбинация, которая дает право на получение каких-то привилегий и бонусов. Система промокодов позволяет букмекерским конторам привлекать новых пользователей, поощрять их регистрацию и пополнение счета, поэтому эта схема удобна как букмекерам, так и пользователям. Вводя мелбет и другие бонусы для первых ставок. Обычно ввод промокода не представляет особой сложности. На сайте букмекера при регистрации будет отведено специальное поле для ввода кодовой комбинации. При выполнении всех условий компании, предоставляющей бонус, код начинает действовать сразу после ввода. Дополнительная активация не требуется. В этом случае есть свои особенности, о которых будет рассказано далее.
Регистрация в 2024 году — бесплатный промокод 1xbet на сегодня. Часто задаваемые вопросы по регистрации и учетной записи у букмекера 1xbet. лучшие промокоды 1xbet . Разнообразие бонусных предложений от 1xbet — другие типы бонусов и промокодов для игроков. Промокод 1xbet на День Рождения. Фрибеты или бесплатные ставки. Тото-промокоды 1xbet. Промокоды 1xbet у блогеров. Система промокодов при регистрации позволяет новым игрокам букмекерской конторы 1xbet получать внушительные бонусные суммы к своему первому депозиту. Обратите внимание, что это не промокод на ставку, а именно на регистрацию. Рабочие промокоды 1хбет на сегодня: Вид бонуса. Размер бонуса.
Получите перетяжку мягкой мебели с гарантией качества
Обновление мягкой мебели: простой способ обновить интерьер
Качественное обслуживание перетяжки мягкой мебели
Перетяжка мягкой мебели обновить диван или кресло
перетяжка мебели http://peretyazhkann.ru.
двери металлические входные технические https://texnicheskiedveri.ru/
Employing an expert towing business is a decision that can conserve you time, cash, and anxiety in different circumstances. While some may be attracted to rely upon pals, family, or makeshift options, the proficiency and services provided by a professional towing company can make a substantial distinction, https://www.quora.com/What-services-do-tow-trucks-provide/answer/Belen-Lambert.
High-quality Minecraft servers – selected projects with video trailers and reviews from real players. We care about all our users serwery rp minecraft
High-quality Minecraft servers – selected projects with video trailers and reviews from real players. We care about all our users serwery rpg minecraft
https://sury-iz-korana.ru/
http://cytotec.icu/# buy cytotec
Привет, хочу поделится информации об росте криптовалюты, вам стоит её купить http://www.ntsr.info/forum/user/82293/ что бы вы смогли заработать x3
Бесплатные промокоды. Давайте сразу начну с того, что перечислю несколько актуальных Промокодов 1xbet на сегодня. Смело вводите промокод в соответствующее поле и получайте прикольные «плюшки» в подарок от щедрого букмекера! Букмекерская контора 1xbet отличается от конкурентов наличием широкой программы лояльности. Важной ее частью является предоставление клиентам бонусов при вводе промокода. промокод на 1xbet свежие . В системе действует программа приветственных бонусов, благодаря которой каждый новичок получает определённую сумму за регистрацию на сайте. Такие акции действуют для казино и букмекерской конторы. Чтобы принять участие в приветственной программе, достаточно активировать при регистрации любой рабочий промокод.
Промокод – небольшая цифробуквенная комбинация, которая дает право на получение каких-то привилегий и бонусов. Система промокодов позволяет букмекерским конторам привлекать новых пользователей, поощрять их регистрацию и пополнение счета, поэтому эта схема удобна как букмекерам, так и пользователям. Вводя рабочий промокод Melbet при регистрации и другие бонусы для первых ставок. Обычно ввод промокода не представляет особой сложности. На сайте букмекера при регистрации будет отведено специальное поле для ввода кодовой комбинации. При выполнении всех условий компании, предоставляющей бонус, код начинает действовать сразу после ввода. Дополнительная активация не требуется. В этом случае есть свои особенности, о которых будет рассказано далее.
Здесь однозначно лучшая порошковая краска. Рекомендую!
ed treatments that work immediately ed dysfunction treatment the best ed pill
doxycycline without prescription: doxycycline without prescription – doxycycline 100 mg
бизнес сувениры и подарки https://www.suveniry-i-podarki16.ru/.
скачать Tribler
Скачать игру Марьяж
Thanks for the marvelous posting! I definitely enjoyed reading
it, you can be a great author. I will ensure that I bookmark your blog
and definitely will come back in the foreseeable future.
I want to encourage you to ultimately continue your great job,
have a nice evening!
can i buy vasotec without prescription
скачать amd driver autodetect
скачать драйвер для kyocera m2040dn
buy zithromax without presc: zithromax capsules 250mg – zithromax cost australia
doxycycline 100mg capsules: doxycycline hydrochloride 100mg – buy generic doxycycline
%%
my page https://www.arredamentivisintin.com/welcome/
Специальные промокоды на 2024 год для 1xBet. Промокод — это уникальный набор из букв, цифр и символов для того, чтобы пользователь получил определенный бонус. Таким бонусом может оказаться увеличение начального депозита, ставка со страховкой (с возвратом части ставочных денег при выборе неверного исхода матча), тестовая ставка (чтобы новые игроки набрались опыта, без вреда собственным деньгам) и многое другое. Больше промокодов для 1xBet можно увидеть на сайтах партнеров букмекерской компании, которые выкладываются каждый день на просторах интернета. Бесплатные промокоды 1xBet при регистрации. Многие пользователи положительно отзываются о промокоде 1xBet на сегодня. Им можно воспользоваться при регистрации новой учетной записи на сайте компании. Для этого необходимо ввести в соответствующее окошко следующий набор букв и цифр. Эта комбинация будут эффективной до конца текущего года, но она распространяется только на новых игроков.
https://tinyurl.com/yutq6po5
промокод при регистрации Melbet стоит ввести для повышенного бонуса на первый депозит. Большинство букмекерских контор используют такую практику привлечения новых игроков и выдают значительные бонусы. Актуальный промокод Мелбет на 2024 год – RS777. Ввести его могут исключительно новые игроки, у которых еще нет аккаунта в Melbet. Не рекомендуем идти на хитрость и заново проходить процесс регистрации, так как служба безопасности тщательно отслеживает мультиаккаунты. Максимальная сумма бонуса при использовании промокода Мелбет – 10400 рублей. Это значит, что при вводе средств на баланс после регистрации новому игроку будет зачислено еще 130% от первого депозита в качестве поощрения от букмекера.
сериал
http://cytotec.icu/# Misoprostol 200 mg buy online
Hello would you mind letting me know which hosting company you’re
using? I’ve loaded your blog in 3 different web browsers and I must say this blog loads
a lot quicker then most. Can you suggest a good hosting provider
at a reasonable price? Cheers, I appreciate it!
https://nolvadex.fun/# femara vs tamoxifen
https://tinyurl.com/ymhauynq
%%
Here is my blog https://promosoblgaz.ru/pervogo-moskovskij-obrazovatelnyj/
Смотреть новые фильмы онлайн, которые уже вышли. Новинки. Смотреть фильмы онлайн. Фильмы онлайн смотреть онлайн. Смотреть фильмы онлайн в хорошем качестве Full HD 720. Фильмы – смотреть онлайн бесплатно в хорошем качестве.
серия
секс фото
https://zithromaxbestprice.icu/# zithromax 500mg
%%
My web page – обратиться к психологу
online doxycycline doxycycline monohydrate doxycycline hyclate
ed pills from india how to get a prescription for ed Generic Ed Drugs India
民意調查是什麼?民調什麼意思?
民意調查又稱為輿論調查或民意測驗,簡稱民調。一般而言,民調是一種為了解公眾對某些政治、社會問題與政策的意見和態度,由專業民調公司或媒體進行的調查方法。
目的在於通過網路、電話、或書面等媒介,對大量樣本的問卷調查抽樣,利用統計學的抽樣理論來推斷較為客觀,且能較為精確地推論社會輿論或民意動向的一種方法。
以下是民意調查的一些基本特點和重要性:
抽樣:由於不可能向每一個人詢問意見,所以調查者會選擇一個代表性的樣本進行調查。這樣本的大小和抽樣方法都會影響調查的準確性和可靠性。
問卷設計:為了確保獲得可靠的結果,問卷必須經過精心設計,問題要清晰、不帶偏見,且易於理解。
數據分析:收集到的數據將被分析以得出結論。這可能包括計算百分比、平均值、標準差等,以及更複雜的統計分析。
多種用途:民意調查可以用於各種目的,包括政策制定、選舉預測、市場研究、社會科學研究等。
限制:雖然民意調查是一個有價值的工具,但它也有其限制。例如,樣本可能不完全代表目標人群,或者問卷的設計可能導致偏見。
影響決策:民意調查的結果常常被政府、企業和其他組織用來影響其決策。
透明度和誠實:為了維護調查的可信度,調查組織應該提供其調查方法、樣本大小、抽樣方法和可能的誤差範圍等詳細資訊。
民調是怎麼調查的?
民意調查(輿論調查)的意義是指為瞭解大多數民眾的看法、意見、利益與需求,以科學、系統與公正的資料,蒐集可以代表全部群眾(母體)的部分群眾(抽樣),設計問卷題目後,以人工或電腦詢問部分民眾對特定議題的看法與評價,利用抽樣出來部分民眾的意見與看法,來推論目前全部民眾的意見與看法,藉以衡量社會與政治的狀態。
以下是進行民調調查的基本步驟:
定義目標和目的:首先,調查者需要明確調查的目的。是要了解公眾對某個政策的看法?還是要評估某個政治候選人的支持率?
設計問卷:根據調查目的,研究者會設計一份問卷。問卷應該包含清晰、不帶偏見的問題,並避免導向性的語言。
選擇樣本:因為通常不可能調查所有人,所以會選擇一部分人作為代表。這部分人被稱為“樣本”。最理想的情況是使用隨機抽樣,以確保每個人都有被選中的機會。
收集數據:有多種方法可以收集數據,如面對面訪問、電話訪問、郵件調查或在線調查。
數據分析:一旦數據被收集,研究者會使用統計工具和技術進行分析,得出結論或洞見。
報告結果:分析完數據後,研究者會編寫報告或發布結果。報告通常會提供調查方法、樣本大小、誤差範圍和主要發現。
解釋誤差範圍:多數民調報告都會提供誤差範圍,例如“±3%”。這表示實際的結果有可能在報告結果的3%範圍內上下浮動。
民調調查的質量和可信度很大程度上取決於其設計和實施的方法。若是由專業和無偏見的組織進行,且使用科學的方法,那麼民調結果往往較為可靠。但即使是最高質量的民調也會有一定的誤差,因此解讀時應保持批判性思考。
為什麼要做民調?
民調提供了一種系統性的方式來了解大眾的意見、態度和信念。進行民調的原因多種多樣,以下是一些主要的動機:
政策制定和評估:政府和政策制定者進行民調,以了解公眾對某一議題或政策的看法。這有助於制定或調整政策,以反映大眾的需求和意見。
選舉和政治活動:政黨和候選人通常使用民調來評估自己在選舉中的地位,了解哪些議題對選民最重要,以及如何調整策略以吸引更多支持。
市場研究:企業和組織進行民調以了解消費者對產品、服務或品牌的態度,從而制定或調整市場策略。
社會科學研究:學者和研究者使用民調來了解人們的社會、文化和心理特征,以及其與行為的關係。
公眾與媒體的期望:民調提供了一種方式,使公眾、政府和企業得以了解社會的整體趨勢和態度。媒體也經常報導民調結果,提供公眾對當前議題的見解。
提供反饋和評估:無論是企業還是政府,都可以透過民調了解其表現、服務或政策的效果,並根據反饋進行改進。
預測和趨勢分析:民調可以幫助預測某些趨勢或行為的未來發展,如選舉結果、市場需求等。
教育和提高公眾意識:通過進行和公布民調,可以促使公眾對某一議題或問題有更深入的了解和討論。
民調可信嗎?
民意調查的結果數據隨處可見,尤其是政治性民調結果幾乎可說是天天在新聞上放送,對總統的滿意度下降了多少百分比,然而大家又信多少?
在景美市場的訪問中,我們了解到民眾對民調有一些普遍的觀點。大多數受訪者表示,他們對民調的可信度存有疑慮,主要原因是他們擔心政府可能會在調查中進行操控,以符合特定政治目標。
受訪者還提到,民意調查的結果通常不會對他們的投票意願產生影響。換句話說,他們的選擇通常受到更多因素的影響,例如候選人的政策立場和政府做事的認真與否,而不是單純依賴民調結果。
從訪問中我們可以得出的結論是,大多數民眾對民調持謹慎態度,並認為它們對他們的投票決策影響有限。
Воспользоваться промокодом 1xbet можно при регистрации в 1xbet. БК 1хбет дарит до 130% на первый депозит при помощи промокода 1xbet. Максимальная сумма бонуса по промокоду 1хбет достигает 32500 рублей. Промокод 1хбет дает надбавку на депозит до 130% только при первом пополнении. Регистрация. номер промокода 1xbet . Всем известно, что букмекерская контора 1xbet предлагает широкий выбор разнообразных бонусов и акций. В этой статье мы расскажем все о промокодах 1xBet: что это, как использовать при регистрации, где вводить, чтобы сделать ставку бесплатно, и по каким поводам казахстанский букмекер 1хБет вручает именные промокоды. Содержание. Что такое промокод 1xBet. Бесплатные промокоды 1xBet. Промокод при регистрации в 1xbet сегодня. Как ввести промокод при регистрации в 1хБет.
Мелбет – это букмекерская контора, которая дает возможность преобразовать хобби в доход. Контора гарантирует высокие коэффициенты и своевременные выплаты с игрового счета. Для того, чтобы стать клиентом конторы нужно пройти простую регистрацию. Здесь разнообразные виды спорта, широкий выбор событий и типов ставок. Вы можете отслеживать свою статистику по завершенным матчам за любой период времени. Доступ к счету можно получить с ПК, смартфона или планшета. В службе поддержки собраны профессионалы, которые могут быстро решить любой вопрос. Предлагается бесплатный промокод Melbet на сегодня большой выбор способов ввода средств на игровой счет.
порно фото
%%
zithromax tablets for sale: zithromax 1000 mg online – zithromax z-pak
вавада мобильная версия зеркало
вавада зеркало рабочее
Фильмы онлайн смотреть онлайн. Смотреть фильмы онлайн в хорошем качестве Full HD 720. Фильмы – смотреть онлайн бесплатно в хорошем качестве. Фильмы – смотреть онлайн в хорошем качестве. Смотреть фильмы онлайн бесплатно в хорошем качестве. Фильмы бесплатно смотреть онлайн в хорошем качестве. Русские фильмы – смотреть фильмы онлайн в высоком.
рабочее зеркало вавада
Мы освещаем проблемные вопросы, касающиеся самозанятости и нового налогового режима на профессиональный доход открытие самозанятости
Medicines information for patients. Long-Term Effects.
can i get paxil
All news about medicament. Get information here.
Салют, хочу поделится информации об росте криптовалюты, вам стоит её купить http://forum.computest.ru/post/544430/#p544430 что бы вы смогли заработать x3
Мы освещаем проблемные вопросы, касающиеся самозанятости и нового налогового режима на профессиональный доход бизнес-план для самозанятых
порно фото
Бесплатные фильмы смотреть онлайн в хорошем качестве. Смотреть фильмы в хорошем качестве (HD, 1080p) в онлайн. Смотреть онлайн фильмы и сериалы. Смотреть фильмы онлайн в хорошем качестве бесплатно. Смотреть фильмы онлайн.
best online ed prescriptions ed pills for sale generic ed drugs over the counter
Фильмы бесплатно смотреть онлайн в хорошем качестве. Русские фильмы – смотреть фильмы онлайн в высоком. Смотреть фильмы онлайн бесплатно в хорошем качестве. Фильмы смотреть онлайн. Лучшие Фильмы смотреть онлайн бесплатно в хорошем качестве. Список фильмов: смотреть онлайн и бесплатно лучшие. КИНО | ФИЛЬМЫ ОНЛАЙН. Лучший онлайн-кинотеатр советских фильмов.
ПромоКод Букмекерской Конторы Melbet 2024 При Регистрации – это код для новых пользователей, так как он дает денежные призы на первый депозит новым игрокам. промокод Melbet на сегодня – это отличный способ сделать игру максимально захватывающей и прибыльной. Букмекер регулярно запускает выгодные бонусные программы и акции, которые помогают беттерам наслаждаться игровым процессом и иметь особые привилегии. Сегодня доступно несколько типов промокодов на игру в Мелбет. Они различаются условиями получения и принципом действия. Melbet промокод при регистрации, увеличивающий сумму первого взноса. С его помощью можно получить дополнительные 130% на игровой баланс для заключения пари.
Промокод при регистрации 1xbet на 32500 рублей. Данный промокод 1хбет нужно ввести при регистрации в соответствующее поле. 1Xbet промокод при регистрации можно использовать только 1н раз в рамках одной учетной записи, но вы можете делиться им со своими друзьями. В 1xБет регистрация по номеру телефона является бесплатным и вторым по простоте способом создать личный аккаунт. Данный способ предусматривает наличие мобильного устройства, а также активной сим-карты, чтобы пользователь мог получить сообщение, в котором его будут ждать данные для входа. После того, как данные будут получены, останется ввести логин с паролем в соответствующие поля. Воспользуйся промокоды на 1xbet тото , получи бесплатную возможность увеличить свой первый депозит до 32500 рублей в БК 1xBet. Промокоды 1xBET актуальные сегодня. На игровой платформе БК «1xbet» функционирует бонусная программа, способствующая привлечению новых игроков и мотивации делать больше ставок для зарегистрированных пользователей. Бонусная программа содержит множество различных бонусов, которые каппер может активировать при помощи специальных промокодов. 130% бонус от первого депозита на ставки. Получай бонус до 130%, но не превышающий 32500 рублей на ставки от 1xbet. Переходим на сайт букмекера.
zithromax online: cheap zithromax pills – where can you buy zithromax
Фильмы смотреть онлайн в хорошем HD качестве. 2024 СМОТЕРТЬ ОНЛАЙН ФИЛЬМ. Смотреть фильмы онлайн бесплатно в хорошем качестве. Лучшие фильмы 2024 года – смотреть онлайн в хорошем. Смотреть фильмы в онлайн кинотеатре в хорошем качестве. Смотреть фильмы в хорошем качестве без рекламы. Фильмы и сериалы онлайн в хорошем качестве. Смотреть фильмы онлайн в хорошем качестве, просмотр.
Смотреть фильмы в онлайн кинотеатре в хорошем качестве. Смотреть фильмы в хорошем качестве без рекламы. Фильмы и сериалы онлайн в хорошем качестве. Смотреть фильмы онлайн в хорошем качестве, просмотр. Смотреть онлайн фильмы и сериалы бесплатно.
https://nolvadex.fun/# what happens when you stop taking tamoxifen
https://lisinoprilbestprice.store/# lisinopril online uk
Бесплатные промокоды от букмекерской конторы 1xBet: при регистрации, на бесплатную ставку. Рассказываем, как использовать и куда вводить промокоды в 1хБет. 1xbet приложение промокод . Начнем с того, что каждый, кто зарегистрировался на официальном сайте или зеркале конторы впервые, может рассчитывать на получение приветственного денежного бонуса, который в дальнейшем удастся потратить на ставки, а в случае успеха заработать первые деньги. Но мы говорим о промокоде, который в специальной форме регистрации просят ввести при наличии.
Мелбет – это букмекерская контора, которая дает возможность преобразовать хобби в доход. Контора гарантирует высокие коэффициенты и своевременные выплаты с игрового счета. Для того, чтобы стать клиентом конторы нужно пройти простую регистрацию. Здесь разнообразные виды спорта, широкий выбор событий и типов ставок. Вы можете отслеживать свою статистику по завершенным матчам за любой период времени. Доступ к счету можно получить с ПК, смартфона или планшета. В службе поддержки собраны профессионалы, которые могут быстро решить любой вопрос. Предлагается действующий промокод Melbet большой выбор способов ввода средств на игровой счет.
urenrjrjkvnm
Both of these specialized security staff casinos very tightly cooperate with each other, in order to ensure security of both the guests and|or assets of the https://casino-x-site179.win/mobile, and have made significant progress in crime prevention.
http://zithromaxbestprice.icu/# zithromax 250 mg
lisinopril 5 mg buy online: zestoretic generic – zestoretic 10 mg
Самые популярные хиты 2024 за сегодня. Ежедневное обновление. Самые горячие новинки из мира музыки Скачать музыку 2024
Самые популярные хиты 2024 за сегодня. Ежедневное обновление. Самые горячие новинки из мира музыки Музыка 2024
Pills prescribing information. Drug Class.
get neurontin
Some news about meds. Read here.
элитные жк москвы купить квартиру https://nedvipro11.ru/.
does tamoxifen make you tired: tamoxifen estrogen – tamoxifen and antidepressants
http://nolvadex.fun/# lexapro and tamoxifen
https://lisinoprilbestprice.store/# lisinopril 40 mg no prescription
zithromax over the counter canada: zithromax canadian pharmacy – zithromax 500mg price in india
zithromax 500 mg lowest price online: zithromax 1000 mg online – generic zithromax medicine
http://cytotec.icu/# cytotec online
Medicament information. Generic Name.
levitra
Best information about drug. Get here.
however I would like to say that this write-up very compelled”카지노솔루션” me to check out and do it! Your writing taste has been surprised me.
lisinopril 12.5 mg: how much is 30 lisinopril – zestoretic 25
online ed drugs erectile dysfunction medication mens erection pills
urenrjrjkvnm
urenrjrjkvnm
Промокод 1xbet на сегодня актуален, бонус будет зачислен сразу после первого пополнения счета. Временные коды. Букмекерская контора 1xbet часто выступает спонсором при переводе популярных сериалов на русский язык. Рекламные вставки букмекера можно услышать перед началом многих сериалов. Часто в такой рекламе диктуется специальные промокод, дающий возможность беттерам рассчитывать на дополнительный бонус. Максимальный бонус при регистрации составляется 32500 рублей. Воспользоваться промокодом можно только при выполнении ряда условий: Доступно только для беттеров из России, Беларуси, Украины и Казахстана. Возврат игрока – от 18 лет. где ввести промокод 1хбет . Промокод 1xbet сегодня найти в интернете не так сложно, достаточно воспользоваться любой поисковой системой. Но обращайте внимание на профессиональность ресурса, откуда будет скопирован промокод. Многие сайты предлагают неактуальные бонусные коды, которые не дадут никакого повышенного депозита после регистрации. На нашем сайте представлен актуальный промокод 1xbet на 2024 год. Вводите промокод, чтобы получить 100% сверху после первого пополнения. Минимальная сумма депозита для использования промокода – 100 рублей. Ограничивается бонус 1хбет суммой в 32500 рублей.
При регистрации в БК Melbet игрокам предлагается самостоятельно выбрать стартовую награду: фрибет на $30 или 100% бонус на депозит до 7 000 RUB. Предлагаем промокод мелбет 2024 , благодаря которому вы получите не только повышенный до 10 400 RUB бонус на первое пополнение счета, но и право на бесплатный прогноз. Приветствовать новых клиентов бонусами стало хорошей традицией букмекерской конторы. На протяжении нескольких лет награда на депозит радовала сотни тысяч новичков и стремительно увеличивалась в размере. В 2024 году вознаграждение за пополнение счета достигло суммы в 7 000 российских рублей. Мы делаем более выгодное предложение. Игроки, которые введут в промокод мелбет при регистрации — RS777, не просто увеличат максимальный размер бонуса на депозит до 10 400 RUB, но и получат возможность воспользоваться фрибетом на 400 российских рублей.
online canadian drugstore: Canada Drugs Direct – best online canadian pharmacy canadapharm.life
I truly enjoy reading posts that provoke thought in both men and women. I also appreciate you letting me add a comment!
xxx
Лаки Джет — это популярная игра на деньги, для которой характерно визуальное представление увеличения ставки пользователя лайки джет
Лаки Джет — это популярная игра на деньги, для которой характерно визуальное представление увеличения ставки пользователя казино lucky jet
top 10 online australian casinos casino online australia real money casino online australia real money
https://mp3bit.pro/
總統民調
民意調查是什麼?民調什麼意思?
民意調查又稱為輿論調查或民意測驗,簡稱民調。一般而言,民調是一種為了解公眾對某些政治、社會問題與政策的意見和態度,由專業民調公司或媒體進行的調查方法。
目的在於通過網路、電話、或書面等媒介,對大量樣本的問卷調查抽樣,利用統計學的抽樣理論來推斷較為客觀,且能較為精確地推論社會輿論或民意動向的一種方法。
以下是民意調查的一些基本特點和重要性:
抽樣:由於不可能向每一個人詢問意見,所以調查者會選擇一個代表性的樣本進行調查。這樣本的大小和抽樣方法都會影響調查的準確性和可靠性。
問卷設計:為了確保獲得可靠的結果,問卷必須經過精心設計,問題要清晰、不帶偏見,且易於理解。
數據分析:收集到的數據將被分析以得出結論。這可能包括計算百分比、平均值、標準差等,以及更複雜的統計分析。
多種用途:民意調查可以用於各種目的,包括政策制定、選舉預測、市場研究、社會科學研究等。
限制:雖然民意調查是一個有價值的工具,但它也有其限制。例如,樣本可能不完全代表目標人群,或者問卷的設計可能導致偏見。
影響決策:民意調查的結果常常被政府、企業和其他組織用來影響其決策。
透明度和誠實:為了維護調查的可信度,調查組織應該提供其調查方法、樣本大小、抽樣方法和可能的誤差範圍等詳細資訊。
民調是怎麼調查的?
民意調查(輿論調查)的意義是指為瞭解大多數民眾的看法、意見、利益與需求,以科學、系統與公正的資料,蒐集可以代表全部群眾(母體)的部分群眾(抽樣),設計問卷題目後,以人工或電腦詢問部分民眾對特定議題的看法與評價,利用抽樣出來部分民眾的意見與看法,來推論目前全部民眾的意見與看法,藉以衡量社會與政治的狀態。
以下是進行民調調查的基本步驟:
定義目標和目的:首先,調查者需要明確調查的目的。是要了解公眾對某個政策的看法?還是要評估某個政治候選人的支持率?
設計問卷:根據調查目的,研究者會設計一份問卷。問卷應該包含清晰、不帶偏見的問題,並避免導向性的語言。
選擇樣本:因為通常不可能調查所有人,所以會選擇一部分人作為代表。這部分人被稱為“樣本”。最理想的情況是使用隨機抽樣,以確保每個人都有被選中的機會。
收集數據:有多種方法可以收集數據,如面對面訪問、電話訪問、郵件調查或在線調查。
數據分析:一旦數據被收集,研究者會使用統計工具和技術進行分析,得出結論或洞見。
報告結果:分析完數據後,研究者會編寫報告或發布結果。報告通常會提供調查方法、樣本大小、誤差範圍和主要發現。
解釋誤差範圍:多數民調報告都會提供誤差範圍,例如“±3%”。這表示實際的結果有可能在報告結果的3%範圍內上下浮動。
民調調查的質量和可信度很大程度上取決於其設計和實施的方法。若是由專業和無偏見的組織進行,且使用科學的方法,那麼民調結果往往較為可靠。但即使是最高質量的民調也會有一定的誤差,因此解讀時應保持批判性思考。
為什麼要做民調?
民調提供了一種系統性的方式來了解大眾的意見、態度和信念。進行民調的原因多種多樣,以下是一些主要的動機:
政策制定和評估:政府和政策制定者進行民調,以了解公眾對某一議題或政策的看法。這有助於制定或調整政策,以反映大眾的需求和意見。
選舉和政治活動:政黨和候選人通常使用民調來評估自己在選舉中的地位,了解哪些議題對選民最重要,以及如何調整策略以吸引更多支持。
市場研究:企業和組織進行民調以了解消費者對產品、服務或品牌的態度,從而制定或調整市場策略。
社會科學研究:學者和研究者使用民調來了解人們的社會、文化和心理特征,以及其與行為的關係。
公眾與媒體的期望:民調提供了一種方式,使公眾、政府和企業得以了解社會的整體趨勢和態度。媒體也經常報導民調結果,提供公眾對當前議題的見解。
提供反饋和評估:無論是企業還是政府,都可以透過民調了解其表現、服務或政策的效果,並根據反饋進行改進。
預測和趨勢分析:民調可以幫助預測某些趨勢或行為的未來發展,如選舉結果、市場需求等。
教育和提高公眾意識:通過進行和公布民調,可以促使公眾對某一議題或問題有更深入的了解和討論。
民調可信嗎?
民意調查的結果數據隨處可見,尤其是政治性民調結果幾乎可說是天天在新聞上放送,對總統的滿意度下降了多少百分比,然而大家又信多少?
在景美市場的訪問中,我們了解到民眾對民調有一些普遍的觀點。大多數受訪者表示,他們對民調的可信度存有疑慮,主要原因是他們擔心政府可能會在調查中進行操控,以符合特定政治目標。
受訪者還提到,民意調查的結果通常不會對他們的投票意願產生影響。換句話說,他們的選擇通常受到更多因素的影響,例如候選人的政策立場和政府做事的認真與否,而不是單純依賴民調結果。
從訪問中我們可以得出的結論是,大多數民眾對民調持謹慎態度,並認為它們對他們的投票決策影響有限。
Новые песни 2024
купить особняк в москве в центре http://nedvipro13.ru/.
Online medicine home delivery: India pharmacy of the world – cheapest online pharmacy india indiapharm.llc
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
В Мелбет промокод — это уникальная комбинация из цифр и букв. Он может использоваться в самых разных ситуациях. Чаще всего применяется в Мелбет промокод при регистрации, чтобы привлечь новых игроков. Однако, он может давать бесплатную ставку и другие бонусы, которых очень много в данной букмекерской конторе. Этот материал расскажет о том, что из себя представляет и что дает promokod Melbet . Промокод для Мелбет можно получить за участие в каких-либо активностях букмекерской конторы Мелбет. Например, уникальный код компания присылает на день рождения в виде подарка своим клиентам. Помимо этого, можно ввести в поисковике «Как получить промокод на Мелбет?» и найти тематические сайты, где постоянно публикуются актуальные комбинации цифр и букв. Букмекер часто распространяет свои promo коды через партнеров, а также некоторые игроки сами активно делятся ими в сети.
Новинки музыки 2024
Выдаем займ под залог ПТС на карту! Авто и ПТС остаются у Вас! Быстрое одобрение выкуп недвижимости в воронеже Надежный автоломбард в Воронеже
Выдаем займ под залог ПТС на карту! Авто и ПТС остаются у Вас! Быстрое одобрение воронеж автоломбард Надежный автоломбард в Воронеже
http://indiapharm.llc/# cheapest online pharmacy india indiapharm.llc
canada pharmacy online legit: Canadian online pharmacy – precription drugs from canada canadapharm.life
cialis professional 20mg sildenafil online uk viagra with paypal
23000 Euro Kredit
https://indiapharm.llc/# best india pharmacy indiapharm.llc
best online pharmacies in mexico: mexican border pharmacies shipping to usa – mexico drug stores pharmacies mexicopharm.com
sildenafil 100mg cialis professional viagra from india
Med
Аренда виртуальных серверов на базе Windows: VDS, VPS
– Ubuntu, Debian, CentOS, Oracle 9 – бесплатно
– Возможность арендовать сервер на 1 час или 1 сутки
– FASTPANEL и HestiaCP – бесплатно
– Управляйте серверами на лету.
– Отлично подходит под GSA Search Engine Ranker
– Мгновенное развёртывание сервера в несколько кликов – бесплатно
– Автоматическая установка Windows – бесплатно
– Для сервера сеть на скорости 1 Гбит!
– Более 15 000 сервер уже в работе
– Почасовая оплата
– Отлично подходит под Xneolinks
– Windows – 2022, 2019, 2016, 2012 R2
– Быстрые серверы с NVMe.
– Круглосуточная техническая поддержка – бесплатно
– Дата-центр в Москве и Амстердаме
– Отлично подходит под A-Parser
– Outline VPN, WireGuard VPN, IPsec VPN.
– Отлично подходит под XRumer + XEvil
– Отлично подходит под CapMonster
– Скорость порта подключения к сети интернет — 1000 Мбит/сек
– Windows – 2012 R2, 2016, 2019, 2022 – бесплатно
– Супер (аптайм, скорость, пинг, нагрузка)
canadian pharmacies comparison: Canada pharmacy online – canada pharmacy canadapharm.life
Аренда VPS и VDS сервера – Dedicated Server
– Для сервера сеть на скорости 1 Гбит!
– Outline VPN, WireGuard VPN, IPsec VPN.
– Круглосуточная техническая поддержка – бесплатно
– Автоматическая установка Windows – бесплатно
– Отлично подходит под XRumer + XEvil
– Отлично подходит под Xneolinks
– Возможность арендовать сервер на 1 час или 1 сутки
– Windows – 2022, 2019, 2016, 2012 R2
– Супер (аптайм, скорость, пинг, нагрузка)
– FASTPANEL и HestiaCP – бесплатно
– Windows – 2012 R2, 2016, 2019, 2022 – бесплатно
– Быстрые серверы с NVMe.
– Мгновенное развёртывание сервера в несколько кликов – бесплатно
– Почасовая оплата
– Управляйте серверами на лету.
– Более 15 000 сервер уже в работе
– Ubuntu, Debian, CentOS, Oracle 9 – бесплатно
– Дата-центр в Москве и Амстердаме
– Скорость порта подключения к сети интернет — 1000 Мбит/сек
– Отлично подходит под A-Parser
– Отлично подходит под GSA Search Engine Ranker
– Отлично подходит под CapMonster
порно фото (http://d1acjemlip1c.рф/bitrix/click.php?goto=http://e-commerge.org/__media__/js/netsoltrademark.php?d=sexs-foto.com)
Аренда виртуального сервера VPS
– Отлично подходит под CapMonster
– Отлично подходит под XRumer + XEvil
– Ubuntu, Debian, CentOS, Oracle 9 – бесплатно
– Отлично подходит под A-Parser
– Дата-центр в Москве и Амстердаме
– Быстрые серверы с NVMe.
– Windows – 2012 R2, 2016, 2019, 2022 – бесплатно
– Windows – 2022, 2019, 2016, 2012 R2
– Почасовая оплата
– Отлично подходит под Xneolinks
– FASTPANEL и HestiaCP – бесплатно
– Мгновенное развёртывание сервера в несколько кликов – бесплатно
– Отлично подходит под GSA Search Engine Ranker
– Outline VPN, WireGuard VPN, IPsec VPN.
– Круглосуточная техническая поддержка – бесплатно
– Управляйте серверами на лету.
– Более 15 000 сервер уже в работе
– Скорость порта подключения к сети интернет — 1000 Мбит/сек
– Возможность арендовать сервер на 1 час или 1 сутки
– Для сервера сеть на скорости 1 Гбит!
– Супер (аптайм, скорость, пинг, нагрузка)
– Автоматическая установка Windows – бесплатно
indian pharmacies safe: indian pharmacy to usa – top online pharmacy india indiapharm.llc
urenrjrjkvnm
Аренда VDS или VPS сервера
– Отлично подходит под GSA Search Engine Ranker
– Отлично подходит под Xneolinks
– Отлично подходит под XRumer + XEvil
– Управляйте серверами на лету.
– Возможность арендовать сервер на 1 час или 1 сутки
– FASTPANEL и HestiaCP – бесплатно
– Дата-центр в Москве и Амстердаме
– Отлично подходит под A-Parser
– Windows – 2022, 2019, 2016, 2012 R2
– Отлично подходит под CapMonster
– Скорость порта подключения к сети интернет — 1000 Мбит/сек
– Мгновенное развёртывание сервера в несколько кликов – бесплатно
– Outline VPN, WireGuard VPN, IPsec VPN.
– Ubuntu, Debian, CentOS, Oracle 9 – бесплатно
– Быстрые серверы с NVMe.
– Почасовая оплата
– Для сервера сеть на скорости 1 Гбит!
– Автоматическая установка Windows – бесплатно
– Круглосуточная техническая поддержка – бесплатно
– Более 15 000 сервер уже в работе
– Windows – 2012 R2, 2016, 2019, 2022 – бесплатно
– Супер (аптайм, скорость, пинг, нагрузка)
Je recommande cette très belle pochette Pablo Exclusive Mango Ice
Je recommande cette très belle pochette Pablo Exclusive Strawberry Cheesecake
world pharmacy india: Online India pharmacy – online shopping pharmacy india indiapharm.llc
viagra price in india sildenafil 20 mg tablet cheap viagra 100mg
https://saroblnews.ru/sys/html/user/select_user/blog/list/3/data/4/1/600_gde_kupit_virtualniy_nomer.html
https://canadapharm.life/# reputable canadian online pharmacy canadapharm.life
Горячее и ленточное наращивание натуральных волос опытным мастером в Тюмени нарастить волосы тюмень
Горячее и ленточное наращивание натуральных волос опытным мастером в Тюмени волосы для наращивания тюмень купить
Payday loans in Ohio
http://canadapharm.life/# the canadian pharmacy canadapharm.life
1WIN – Лучшая букмекерская контора с самыми большими коэффициентами 1Win
canadian pharmacy checker: Canada pharmacy online – canadian pharmacy cheap canadapharm.life
purchase generic viagra viagra 50 mg viagra online canadian pharmacy
1WIN – Лучшая букмекерская контора с самыми большими коэффициентами 1Win зеркало
Купить кондиционеры в Череповце по низким ценам. Сплит-системы с гарантией до 5 лет – https://vk.com/mastrklimat
элитная вторичная недвижимость агентства москвы http://www.nedvipro15.ru.
民調
民意調查是什麼?民調什麼意思?
民意調查又稱為輿論調查或民意測驗,簡稱民調。一般而言,民調是一種為了解公眾對某些政治、社會問題與政策的意見和態度,由專業民調公司或媒體進行的調查方法。
目的在於通過網路、電話、或書面等媒介,對大量樣本的問卷調查抽樣,利用統計學的抽樣理論來推斷較為客觀,且能較為精確地推論社會輿論或民意動向的一種方法。
以下是民意調查的一些基本特點和重要性:
抽樣:由於不可能向每一個人詢問意見,所以調查者會選擇一個代表性的樣本進行調查。這樣本的大小和抽樣方法都會影響調查的準確性和可靠性。
問卷設計:為了確保獲得可靠的結果,問卷必須經過精心設計,問題要清晰、不帶偏見,且易於理解。
數據分析:收集到的數據將被分析以得出結論。這可能包括計算百分比、平均值、標準差等,以及更複雜的統計分析。
多種用途:民意調查可以用於各種目的,包括政策制定、選舉預測、市場研究、社會科學研究等。
限制:雖然民意調查是一個有價值的工具,但它也有其限制。例如,樣本可能不完全代表目標人群,或者問卷的設計可能導致偏見。
影響決策:民意調查的結果常常被政府、企業和其他組織用來影響其決策。
透明度和誠實:為了維護調查的可信度,調查組織應該提供其調查方法、樣本大小、抽樣方法和可能的誤差範圍等詳細資訊。
民調是怎麼調查的?
民意調查(輿論調查)的意義是指為瞭解大多數民眾的看法、意見、利益與需求,以科學、系統與公正的資料,蒐集可以代表全部群眾(母體)的部分群眾(抽樣),設計問卷題目後,以人工或電腦詢問部分民眾對特定議題的看法與評價,利用抽樣出來部分民眾的意見與看法,來推論目前全部民眾的意見與看法,藉以衡量社會與政治的狀態。
以下是進行民調調查的基本步驟:
定義目標和目的:首先,調查者需要明確調查的目的。是要了解公眾對某個政策的看法?還是要評估某個政治候選人的支持率?
設計問卷:根據調查目的,研究者會設計一份問卷。問卷應該包含清晰、不帶偏見的問題,並避免導向性的語言。
選擇樣本:因為通常不可能調查所有人,所以會選擇一部分人作為代表。這部分人被稱為“樣本”。最理想的情況是使用隨機抽樣,以確保每個人都有被選中的機會。
收集數據:有多種方法可以收集數據,如面對面訪問、電話訪問、郵件調查或在線調查。
數據分析:一旦數據被收集,研究者會使用統計工具和技術進行分析,得出結論或洞見。
報告結果:分析完數據後,研究者會編寫報告或發布結果。報告通常會提供調查方法、樣本大小、誤差範圍和主要發現。
解釋誤差範圍:多數民調報告都會提供誤差範圍,例如“±3%”。這表示實際的結果有可能在報告結果的3%範圍內上下浮動。
民調調查的質量和可信度很大程度上取決於其設計和實施的方法。若是由專業和無偏見的組織進行,且使用科學的方法,那麼民調結果往往較為可靠。但即使是最高質量的民調也會有一定的誤差,因此解讀時應保持批判性思考。
為什麼要做民調?
民調提供了一種系統性的方式來了解大眾的意見、態度和信念。進行民調的原因多種多樣,以下是一些主要的動機:
政策制定和評估:政府和政策制定者進行民調,以了解公眾對某一議題或政策的看法。這有助於制定或調整政策,以反映大眾的需求和意見。
選舉和政治活動:政黨和候選人通常使用民調來評估自己在選舉中的地位,了解哪些議題對選民最重要,以及如何調整策略以吸引更多支持。
市場研究:企業和組織進行民調以了解消費者對產品、服務或品牌的態度,從而制定或調整市場策略。
社會科學研究:學者和研究者使用民調來了解人們的社會、文化和心理特征,以及其與行為的關係。
公眾與媒體的期望:民調提供了一種方式,使公眾、政府和企業得以了解社會的整體趨勢和態度。媒體也經常報導民調結果,提供公眾對當前議題的見解。
提供反饋和評估:無論是企業還是政府,都可以透過民調了解其表現、服務或政策的效果,並根據反饋進行改進。
預測和趨勢分析:民調可以幫助預測某些趨勢或行為的未來發展,如選舉結果、市場需求等。
教育和提高公眾意識:通過進行和公布民調,可以促使公眾對某一議題或問題有更深入的了解和討論。
民調可信嗎?
民意調查的結果數據隨處可見,尤其是政治性民調結果幾乎可說是天天在新聞上放送,對總統的滿意度下降了多少百分比,然而大家又信多少?
在景美市場的訪問中,我們了解到民眾對民調有一些普遍的觀點。大多數受訪者表示,他們對民調的可信度存有疑慮,主要原因是他們擔心政府可能會在調查中進行操控,以符合特定政治目標。
受訪者還提到,民意調查的結果通常不會對他們的投票意願產生影響。換句話說,他們的選擇通常受到更多因素的影響,例如候選人的政策立場和政府做事的認真與否,而不是單純依賴民調結果。
從訪問中我們可以得出的結論是,大多數民眾對民調持謹慎態度,並認為它們對他們的投票決策影響有限。
п»їbest mexican online pharmacies: mexican pharmacy – pharmacies in mexico that ship to usa mexicopharm.com
http://canadapharm.life/# global pharmacy canada canadapharm.life
https://indiapharm.llc/# india pharmacy indiapharm.llc
Payday loans in Mississippi
levaquin 250mg 7days
india pharmacy: indian pharmacy – reputable indian pharmacies indiapharm.llc
Thanks to the high-quality content and the administrator’s active involvement, the site’s reputation will undoubtedly improve soon.
best canadian pharmacy online: Cheapest drug prices Canada – ed drugs online from canada canadapharm.life
Это оригинальный сайт 1Win.
Monetize Your Content with the Koji Advantage https://withakoji.com/
canadian pharmacy ltd: Canadian online pharmacy – canadian family pharmacy canadapharm.life
Скачать хиты 2024
sildenafil 130mg viagra 100 mg oral tablet sildenafil citrate tablets 100 mg
What i do not realize is in reality how you’re no longer really a lot more well-preferred than you may be now. You are so intelligent. You understand thus considerably in the case of this matter, produced me personally imagine it from a lot of numerous angles. Its like men and women don’t seem to be fascinated unless it’s one thing to accomplish with Woman gaga! Your personal stuffs great. Always deal with it up!
Букмекерская компания “Мелбет”, как, собственно, и десятки других операторов акцентирует внимание на бонусах и других привилегиях для своих игроков. Промокод – это один из вариантов привлечения новых игроков. Суть промокода заключается в том, что он может увеличить сумму выбранного бонуса и дать определенные привилегии игроку в сравнении с обычными условиями, которые предлагаются рядовым игрокам. Сегодня можно найти предложения на разных ресурсах. К примеру, это может быть какой-то блогер на видеохостинге YouTube. Довольно часто у популярных личностей можно встретить рекламные интеграции, где они бесплатно предлагают воспользоваться Melbet промокод при регистрации и получить дополнительные привилегии при получении бонуса. Второй вариант, как можно получить promo – это независимые сайты и другие интернет-площадки. Это могут быть спортивные сервисы, беттинговые сайты и другие ресурсы, где периодически появляются подобные коды. Ну и третий вариант – это официальный сайт букмекерской компании. На сайте часто появляются новые акции и бонусы. Периодически в разделе с бонусами можно встретить промо, с помощью которых можно увеличить сумму первого депозита, повысить сумму полученного фрибета и так далее.
world pharmacy india: indian pharmacy to usa – buy prescription drugs from india indiapharm.llc
A tow truck, also called a wrecker, failure truck, or even recovery motor vehicle, participates in a vital function in the transit sector by delivering kerbside aid as well as recovery services for disabled or damaged motor vehicles. The key reason of a tow truck is to relocate vehicles that are actually incapable to operate their very own as a result of to mechanical failures, collisions, or other issues, https://www.tumblr.com/cristodelaroca/737658610759483392/the-essential-role-of-towing-in-santa-clara-ca?source=share.
http://indiapharm.llc/# Online medicine order indiapharm.llc
http://canadapharm.life/# canadian pharmacy store canadapharm.life
Sports were constantly a main part of Roman’s lifestyle, even if she waited until finally her seventh ten years to grow to be a world-beater. After beginning his own label in the eighties, he became a symbol of fierce independence for youthful musicians who longed to forge their have way, regardless of whether in amongst genres or outside the major label technique. Ramjee, who died on March 31 from Covid-19 similar complications at age 63, was a foremost South African HIV scientist. When shoe designer Sergio Rossi died from problems of the coronavirus on April two at age 84, in Cesena, Italy, he left guiding a substantial household and legacy that could not just be measured in feet. At several periods, she held the American report in the shot put in the women’s 65-69, 70-74 and 75-79 age groups. Sonic X (Leapster, North American) boxart. 2015 one more Pew analyze located that a lot more American females (42%) than males (37%) owned video match consoles.
Your blog site has actually become my go-to for trusted info hereof. Keep up the amazing job.
cheapest online pharmacy india: Online India pharmacy – Online medicine order indiapharm.llc
At our site, we’re committed to providing complete and reliable information about various pests, from cockroaches and ants to centipedes and other problematic creatures. Our target is to provide knowledge to the public about how to efficiently manage these pest nuisances. If you want to know more about are soil centipedes poisonous don’t hesitate to navigate through our portal. We strive to supply information that help our users in handling their pest circumstances effectively. Trust us to assist you in handling any pests you encounter.
1win лаки джет
Our website, we are dedicated to providing detailed and trusted information about numerous pests, from roaches and ants to centipedes and other unwelcome creatures. Our objective is to inform the public about how to get rid of these nuisance creatures. If you want to find out more about when do centipedes sleep feel free to navigate through our portal. We endeavor to provide solutions that will assist people in handling their pest circumstances efficiently. Trust our expertise to guide you through dealing with any pests you encounter.
Greate pieces. Keep posting such kind of info on your site.
Im really impressed by your blog.
Hey there, You’ve done an excellent job. I will certainly digg it and for my part suggest to my
friends. I’m confident they’ll be benefited from this website.
viagra price per pill cialis 10mg sildenafil 100mg for sale
cheapest pharmacy canada: Canada Drugs Direct – canada pharmacy reviews canadapharm.life
голые девушки
canada pharmacy world: canadian drug – legitimate canadian online pharmacies canadapharm.life
ООО «АиРТИ» осуществляет индивидуальную разработку, изготовление и поставку современных высококачественных уплотнительных элементов и систем для ремонта промышленного гидро- и пневмооборудования Изготовление уплотнений
mexican online pharmacies prescription drugs: Purple Pharmacy online ordering – mexican pharmacy mexicopharm.com
Это сайт-оригинал 1Win. Рекомендую однозначно!
cheap erectile dysfunction pills indian medicine for erectile dysfunction best non prescription ed medication
купить дом в москве в элитном поселке nedvipro17.ru.
http://mexicopharm.com/# best online pharmacies in mexico mexicopharm.com
http://canadapharm.life/# northwest pharmacy canada canadapharm.life
ashwagandha supplement
This post will help the internet viewers for setting up new
blog or even a weblog from start to end.
certified canadian international pharmacy: Pharmacies in Canada that ship to the US – pharmacy in canada canadapharm.life
indian pharmacy: reputable indian online pharmacy – reputable indian pharmacies indiapharm.llc
online canadian drugstore: Canadian online pharmacy – canada pharmacy world canadapharm.life
ed pills that work top rated generic ed drugs ed drugs cost
https://tinyurl.com/ywsvz35s
Букмекерская контора 1Win является одним из лидеров рынка по широкому диапазону коэффициентов для спортивных мероприятий 1Вин казино
Букмекерская контора 1Win является одним из лидеров рынка по широкому диапазону коэффициентов для спортивных мероприятий 1Вин
Советую оригинальній сайт 1Win. Рекомендую однозначно!
https://tinyurl.com/ymfwvfuw
http://mexicopharm.com/# medicine in mexico pharmacies mexicopharm.com
https://tinyurl.com/yqbj9qrr
http://canadapharm.life/# canadian mail order pharmacy canadapharm.life
своеобразие брендовых вещей – высокое качество и оригинальный дизайн. Используйте Программу http://www.existentiellitteraturfestival.se/alf-linderman-2/ защиты отправлений. акции и спецпредложения shopotam сделают шопинг еще выгоднее!
drugs from canada: Canada pharmacy online – legitimate canadian mail order pharmacy canadapharm.life
top 10 online pharmacy in india: Medicines from India to USA online – india pharmacy indiapharm.llc
pharmacy wholesalers canada: Canada pharmacy online – ed drugs online from canada canadapharm.life
generic drugs for ed mens erection pills best erectile dysfunction pills
We wish to thank you yet again for the stunning ideas
you offered Jeremy when preparing a post-graduate research and also, most importantly, regarding
providing each of the ideas within a blog post.
If we had been aware of your website a year ago,
we’d have been kept from the unwanted measures we were selecting.
Thank you very much. sklep
сколько стоит пентхаус в москве https://www.nedviprof.ru.
Amazing data Kudos!
I’d like to thank you for the efforts you have
put in penning this website. I am hoping to view the same high-grade content from
you in the future as well. In truth, your creative
writing abilities has inspired me to get my own, personal site now 😉
Широкий выбор цветов и фактур для вашего вкуса
дверь купить входную https://www.vhodnye-dveri97.ru/.
Cheap Levitra online: Levitra online – Levitra generic best price
impotence pills over the counter best ed medications generic ed drugs cost
Двери входные
металлические двери входные https://vhodnye-dveri97.ru.
Соответствие европейским стандартам качества и безопасности
входные металлические двери https://vhodnye-dveri97.ru/.
Мобильные телефоны по выгодной цене в нашем магазине
магазин – онлайн магазин.
проектирование металлоконструкций
доступ к топовым нейросетям Claude proxyapi OpenAI API в России
Кондиционеры – наш союзник в борьбе с жарой
продам кондиционер https://kondicionery-nedorogo.ru.
the best ed pills: ed pills otc – cheap ed drugs
http://kamagradelivery.pro/# Kamagra 100mg price
erectile dysfunction medications treatment for ed generic ed medication from india
Всем советую оригинальный сайт БК 1Win. Рекомендую однозначно!
Летняя жара беспощадна? Не с кондиционером!
продажа кондиционеров москва https://www.kondicionery-nedorogo.ru/.
Official website Melbet is a spot where you can bet on sports and other exciting events 24/7 https://minecraftcommand.science/forum/general/topics/melbet-betting-company
Official website Melbet is a spot where you can bet on sports and other exciting events 24/7 https://www.saber.com.br/wp-content/pgs/pin_up_bet___apostas_desportivas_online.html
online ed medications: erection pills over the counter – how to cure ed
how to get a prescription for ed best drug for ed cheap erectile dysfunction pill
LГҐna 90000 kr
Completa el formulario con tus datos personales y contacto Otovix capsulas Similares
Completa el formulario con tus datos personales y contacto Otovix en Amazon
http://tadalafildelivery.pro/# buy tadalafil 5mg online
urenrjrjkvnm
https://levitradelivery.pro/# Levitra 20 mg for sale
Levitra generic best price: Levitra best price – Generic Levitra 20mg
Just want to say your article is as astounding. The clearness in your post is simply excellent and i
could assume you’re an expert on this subject.
Fine with your permission let me to grab your feed to keep updated
with forthcoming post. Thanks a million and please continue the enjoyable work.
%%
my site – https://postheaven.net/eriatskgyq/trajedi-sonra-kisisel-kaderinde-yasadi
Прочные и надежные для дома и офиса
входная дверь купить https://www.vhodnye-dveri97.ru.
Всем советую лучшую БК 1Win. Рекомендую однозначно!
mostbet peru mostbet review mostbet india
imipramine 25mg online
generic tadalafil in canada: Tadalafil 20mg price in Canada – tadalafil 20mg uk
https://tinyurl.com/ysywtm5s
https://tinyurl.com/2x5k3b54
https://www.inkitt.com/mostbet211
%%
Have a look at my homepage http://www.kaskus.co.id/redirect?url=https://xxxfetish.tube/
https://tinyurl.com/ytz6u9to
calendar 2025
https://kamagradelivery.pro/# Kamagra 100mg
серия
http://sildenafildelivery.pro/# buy sildenafil online canada
robux generator free roblox redeem roblox redeem code
cheap kamagra: cheap kamagra – Kamagra Oral Jelly
Предоставляя разнообразные возможности для грузоперевозок и строительных работ, манипуляторы обеспечивают эффективность и оперативность в обработке грузов перевозка манипулятором москва и московская область недорого
coin
Предоставляя разнообразные возможности для грузоперевозок и строительных работ, манипуляторы обеспечивают эффективность и оперативность в обработке грузов манипулятор вызвать
Kamagra 100mg: Kamagra 100mg price – Kamagra tablets
Porn
Med
urenrjrjkvnm
https://levitradelivery.pro/# Levitra 20 mg for sale
http://kamagradelivery.pro/# Kamagra tablets
Generic Levitra 20mg: Levitra online – Levitra 20 mg for sale
cheap erectile dysfunction pills: ed pills online – best otc ed pills
Как не прогореть этим летом? Включаем кондиционер!
мос кондиционер https://www.kondicionery-nedorogo.ru/.
https://soglasovanie-pereplanirovki-krvartiri.ru/
apps for free robux robux generator 2024 robux gratis
Porn
Ароматное натаральное нерафинированое масло. Масло подсолнечное Благо нерафинированное высшего сорта подсолнечная масло оптом цена
Nikki Beach Residences is a new project by Aldar Properties in Ras Al Khaimah. Luxury apartments with own brand for sale. This is a great opportunity to enjoy an exclusive life in a seaside area!
Очень выгодное БК 1Win. Всем советую!
https://sildenafildelivery.pro/# buy sildenafil in usa
https://kamagradelivery.pro/# buy Kamagra
lake jet казино
Инструкция по настройке температуры
кондиционеры купить в москве http://www.kondicionery-v-moskve.ru.
sildenafil from india: Sildenafil price – can you buy sildenafil online
https://www.google.cat/url?q=https://hottelecom.net/de/
top 10 ed medications comparison cheap ed drugs ed medication online pharmacy
Выбор кондиционера для бизнеса
кандер купить http://www.kondicionery-v-moskve.ru/.
Полезные советы по экономии энергии
купить кондиционер в интернет магазине http://www.kondicionery-v-moskve.ru.
Что такое SEO продвижение сайта. SEO (англ. Search Engine Optimization) – это комплекс мер по улучшению сайта для его ранжирования в поисковых системах интернет реклама поисковое продвижение сайта
order sildenafil: cheap sildenafil – sildenafil 100 mg tablet cost
Что такое SEO продвижение сайта. SEO (англ. Search Engine Optimization) – это комплекс мер по улучшению сайта для его ранжирования в поисковых системах услуги seo москва
The Mellbet filter allows you to select a specific league, specify the amount of bets in the bet, the time before the start of the game and the minimum market odds https://telegra.ph/mostbet-cz-11-28
русский анал с разговорами видео http://www.russ-anal-s-razgovorami.pro.
Comprar Liverin capsulas en Mexico. Cuanto cuestan en la Farmacia, Mercado Libre Liverin Precio en México
The Mellbet filter allows you to select a specific league, specify the amount of bets in the bet, the time before the start of the game and the minimum market odds https://claridgeadvisors.com/wp-includes/pgs/?how_to_choose_a_bookmaker_and_not_make_a_mistake.html
Comprar Liverin capsulas en Mexico. Cuanto cuestan en la Farmacia, Mercado Libre Liverin para qué sirve?
xxx video 24
Je recommande cette très belle pochette Pablo Exclusive Strawberry Lychee
Je recommande cette très belle pochette Pablo Ice Cold
where to buy tadalafil 20mg: cheap tadalafil canada – tadalafil best price uk
erection pills viagra online top ed pills generic ed medication from india
Лучший сайт среди всех БК 1Win. Всем советую!
http://edpillsdelivery.pro/# erectile dysfunction drugs
https://tadalafildelivery.pro/# tadalafil online prescription
sildenafil generic prescription: viagra sildenafil citrate – sildenafil generic price uk
legal erectile dysfunction pills Happy family store Best treatment for erectile dysfunction
Обслуживание кондиционера по сезонам
купить кондиционер в https://kondicionery-v-moskve.ru/.
Koji: Your Companion in the Journey of Monetizing Digital Content https://withakoji.com/
https://www.google.bj/url?q=https://hottelecom.net/
Cinema
purchase fildena online Are there limitations on the frequency of prescription refills with insurance?
coin
%%
Here is my web site :: marketologiya.com
sildenafil 10 mg price: cheap sildenafil – buy cheap sildenafil online
best online pharmacy for ed drugs generic ed drugs canada ed drug prices
По-моему это уже обсуждалось, воспользуйтесь поиском.
watch ass slapping, cock sucking, blowjobs, hand jobs, jerking off, masturbation, stroking, https://www.mze.es/el-miteco-aprueba-el-programa-moves-flotas-con-una-primera-convocatoria-de-50-millones-para-incentivar-la-electrificacion-de-parques-de-vehiculos-ligeros erotic massage and many other.
Быстрое удаление пятен и загрязнений, очистка вещей от запаха и бактерий заказать химчистку
Быстрое удаление пятен и загрязнений, очистка вещей от запаха и бактерий чистка диванов на дому отзывы
Vardenafil buy online: Generic Levitra 20mg – Cheap Levitra online
Sight Care is a natural supplement designed to improve eyesight and reduce dark blindness. With its potent blend of ingredients. https://sightcarebuynow.us/
IP-телефония — это уникальный тип связи, который функционирует через интернет. К интернет-каналу предъявляются минимальные требования:https://www.google.co.ma/url?q=https://hottelecom.net/
Sight Care is a natural supplement designed to improve eyesight and reduce dark blindness. With its potent blend of ingredients. https://sightcarebuynow.us/
https://levitradelivery.pro/# buy Levitra over the counter
IP-телефония — это уникальный тип связи, который функционирует через интернет. К интернет-каналу предъявляются минимальные требования:https://www.google.dm/url?q=https://hottelecom.net/
Comprar Flexacil Ultra capsulas en Peru. Cuanto cuestan en la Farmacia Inkafarma, Mercado Libre? flexacil ultra Inkafarma
%%
Feel free to visit my blog post – http://www.mrkineshma.ru/support/forum/view_profile.php?UID=212761
https://edpillsdelivery.pro/# erection pills online
Comprar Flexacil Ultra capsulas en Peru. Cuanto cuestan en la Farmacia Inkafarma, Mercado Libre? flexacil ultra capsulas
Отремонтировать мягкую мебель в доме: Обновить новый вид старой мебели: эффектные идеи перетягивать мебель своими руками: Выбор ткани для перетяжки мягкой мебели: Как сэкономить на перетяжке мягкой мебели: 5 простых способов
перетяжка мягкой мебели.
Перетяжка мягкой мебели: как избежать расходов на новую мебель
голые девушки
non prescription erection pills: ed pills delivery – best non prescription ed pills
coin
ed drugs compared what is the best ed drug legal erectile dysfunction pills
винлайн регистрация по телефону
Cinema
http://paxlovid.guru/# buy paxlovid online
http://prednisone.auction/# how can i get prednisone online without a prescription
Закажите качественные кондиционеры в нашем магазине
Сделайте свой дом комфортным с нашими кондиционерами
Разнообразие кондиционеров в нашем магазине
Самые низкие цены на кондиционеры только у нас
Улучшите свой интерьер с помощью наших кондиционеров
Индивидуальный подход к каждому клиенту в нашем магазине
Надежные и проверенные бренды кондиционеров в нашем ассортименте
Предлагаем услуги доставки по всей стране
Очистите воздух от пыли с помощью наших кондиционеров
Профессиональная помощь в выборе и установке кондиционеров
Осуществляем монтаж наших кондиционеров
Экономичный расход энергии с нашими кондиционерами
Регулируйте температуру в вашей квартире с нашими кондиционерами
Сэкономьте на покупке кондиционеров в нашем магазине
Надежность наших кондиционеров от производителя
Повысьте комфорт для работы с нашими кондиционерами
Индивидуальные условия для организаций при покупке кондиционеров в нашем магазине
Интуитивно понятный каталог кондиционеров на нашем сайте
Эксклюзивные модели в области кондиционирования в нашем магазине
Постоянно обновляемый ассортимент кондиционеров в нашем магазине
магазин кондиционеров http://www.magazin-kondicionerov.ru.
Как правильно провести техническое обслуживание кондиционеров?
техническое обслуживание кондиционеров перечень работ https://tekhnicheskoe-obsluzhivanie-kondicionerov.ru.
video
казино лаки джет
Купите качественные кондиционеры в известном магазине
Обеспечьте свой дом прохладой с нашими кондиционерами
Разнообразие кондиционеров в нашем магазине
Самые низкие цены на кондиционеры только у нас
Украсьте свой интерьер с помощью наших кондиционеров
Индивидуальный подход к каждому клиенту в нашем магазине
Популярные марки кондиционеров в нашем ассортименте
Устраиваем быструю доставку по всей стране
Снимите жару и усталость с помощью наших кондиционеров
Бесплатная консультация в выборе и установке кондиционеров
Гарантируем качественный монтаж наших кондиционеров
Экономичный расход энергии с нашими кондиционерами
Создайте свой комфортный микроклимат с нашими кондиционерами
Получите скидку кондиционеров в нашем магазине
Гарантия качества наших кондиционеров от производителя
Повысьте комфорт для работы с нашими кондиционерами
Организация оптовых поставок при покупке кондиционеров в нашем магазине
Быстрый подбор кондиционеров на нашем сайте
Новинки в области кондиционирования в нашем магазине
Постоянно обновляемый ассортимент кондиционеров в нашем магазине
магазин кондиционеров москва https://magazin-kondicionerov.ru/.
Приобретите качественные кондиционеры в нашем магазине
Обеспечьте свой дом прохладой с нашими кондиционерами
Разнообразие кондиционеров в нашем магазине
Лучшие цены на кондиционеры только у нас
Украсьте свой интерьер с помощью наших кондиционеров
Индивидуальный подход к каждому клиенту в нашем магазине
Топовые производители кондиционеров в нашем ассортименте
Предлагаем услуги доставки по всей стране
Снимите жару и усталость с помощью наших кондиционеров
Бесплатная консультация в выборе и установке кондиционеров
Осуществляем монтаж наших кондиционеров
Экономичный расход энергии с нашими кондиционерами
Регулируйте температуру в вашей квартире с нашими кондиционерами
Получите скидку кондиционеров в нашем магазине
Гарантия качества наших кондиционеров от производителя
Повысьте комфорт для работы с нашими кондиционерами
Индивидуальные условия для организаций при покупке кондиционеров в нашем магазине
Удобный поиск по параметрам кондиционеров на нашем сайте
Эксклюзивные модели в области кондиционирования в нашем магазине
Всегда в наличии кондиционеров в нашем магазине
магазины кондиционеров http://magazin-kondicionerov.ru/.
generic ed drugs india ed treatment in india top rated generic ed drugs
Villas in the exquisite residential complex Address hillcrest dubai , Dubai Hills Estate. Luxurious life in an elite location
paxlovid covid: Paxlovid buy online – paxlovid for sale
Какие проблемы могут быть у кондиционеров без регулярного технического обслуживания?
техническое обслуживание кондиционеров самара http://www.tekhnicheskoe-obsluzhivanie-kondicionerov.ru.
Я думаю, что Вы допускаете ошибку. Давайте обсудим это.
Partners may agree to include the http://pjchacooficial.org/2019/12/04/05-de-diciembre-de-1948-triunfo-electoral-del-peronismo-en-todo-el-pais/ in own activities in a controlled manner, limited by minutes and hours, or allocate only some days for the practice of fetishism.
Как увеличить срок службы кондиционера с помощью технического обслуживания
техническое обслуживание кондиционеров перечень работ https://www.tekhnicheskoe-obsluzhivanie-kondicionerov.ru.
Even if creating an account on other sex web-sites expenses you absolutely nothing, they still collect your information and facts. Yet even wherever it is illegal, a flourishing underground organization normally exists since of high desire and the superior money that can be designed by pimps, brothel house owners, escort agencies, and traffickers. It is documented that even in the most primitive societies, there was transactional sexual intercourse. Due to the longstanding economic instability of several of these nations, rising numbers of ladies have been compelled to flip in the direction of the sexual intercourse sector there for perform. In pre-modern Korea, the Kisaeng ended up ladies from the reduce caste Cheonmin who have been trained to supply enjoyment, conversation, and sexual products and services to men of the higher course. Male intercourse tourism can build or augment demand from customers for intercourse services in the host nations around the world, though female intercourse tourism tends not to use services that are specially devoted to that objective. In addition, like any other field, there are individuals who operate in or support the intercourse business as managers, movie crews, photographers, web-site developers and website owners, income staff, book and journal writers and editors, etcetera. Some create business types, negotiate trade, make push releases, attract up contracts with other house owners, get and promote information, offer you complex help, operate servers, billing products and services, or payroll, manage trade exhibits and a variety of functions, do promoting and revenue forecasts, deliver human methods, or supply tax expert services and lawful support.
best ed drugs for seniors treatment for ed non prescription erection pills
Перетянуть мягкую мебель в доме: полезные советы новый вид старой мебели: эффектные идеи перетягивать мебель своими руками: Выбор ткани для перетяжки мягкой мебели: секреты выбора
обивка мебели.
Обновление интерьера: перетяжка мягкой мебели на практике
Реанимобиль на дом, эвакуация больного, пострадавшего, транспортировка в больницу платный реанимобиль
Comprar Duston Gel en Paraguay. Cuanto cuesta farmacia punto farma, Mercado Libre? Duston Gel
Реанимобиль на дом, эвакуация больного, пострадавшего, транспортировка в больницу перевозка лежачих больных в москве из дома в больницу
Перетянуть мягкую мебель в доме: Дать новый вид старой мебели: секреты перетяжки перетягивать мебель своими руками: Выбор ткани для перетяжки мягкой мебели: от простого к сложному
перетяжка мебели в Минске.
Обновление интерьера: перетяжка мягкой мебели на практике
Сертификат ISO 9001 (или ИСО 9001) подтверждает, что система менеджмента качества (СМК) соответствует всем требованиям стандарта ГОСТ Р ИСО 9001-2015 стоимость сертификата ISO 9001
Comprar Duston Gel en Paraguay. Cuanto cuesta farmacia punto farma, Mercado Libre? duston gel precio paraguay
Сертификат ISO 9001 (или ИСО 9001) подтверждает, что система менеджмента качества (СМК) соответствует всем требованиям стандарта ГОСТ Р ИСО 9001-2015 https://telegra.ph/Cena-sertifikata-ISO-9001-ot-chego-zavisit-stoimost-sertifikacii-01-09
zofran 8 mg medication
http://paxlovid.guru/# paxlovid pill
купить металлопрокат в москве в розницу цена
https://stromectol.guru/# ivermectin lotion for lice
продажа металл
uniswap https://uniswap.work/
купить металлический
coin
ed drugs available in canada most potent ed pills what can i buy that works like viagra
prednisone 5mg price: best prednisone – prednisone 20mg prices
Когда мне нужно найти захватывающее онлайн-занятие, я обращаю внимание на азино 777 играть на деньги . С учётом множества игр и заманчивых бонусов, этот сайт становится моим фаворитом. Помимо этого, удобный интерфейс и высокий уровень безопасности делают процесс игры максимально комфортным. Так что, если ты хочешь чувствовать азарт и выигрывать призы, не пропусти Азино казино.
Закажите качественные кондиционеры в лучшем магазине
Сделайте свой дом комфортным с нашими кондиционерами
Разнообразие кондиционеров в нашем магазине
Выгодные предложения на кондиционеры только у нас
Освежите свой интерьер с помощью наших кондиционеров
Профессиональный подход к каждому клиенту в нашем магазине
Популярные марки кондиционеров в нашем ассортименте
Осуществляем доставку по всей стране
Очистите воздух от пыли с помощью наших кондиционеров
Профессиональная помощь в выборе и установке кондиционеров
Осуществляем монтаж наших кондиционеров
Минимальные расходы на ремонт с нашими кондиционерами
Наслаждайтесь прохладой в любое время года с нашими кондиционерами
Сэкономьте на покупке кондиционеров в нашем магазине
Надежность наших кондиционеров от производителя
Создайте оптимальные условия для работы с нашими кондиционерами
Индивидуальные условия для организаций при покупке кондиционеров в нашем магазине
Удобный поиск по параметрам кондиционеров на нашем сайте
Эксклюзивные модели в области кондиционирования в нашем магазине
Всегда в наличии кондиционеров в нашем магазине
купить кондиционер в москве https://www.magazin-kondicionerov.ru/.
paxlovid india paxlovid best price paxlovid for sale
sneak a peek at these guys
best ed treatment non prescription erection pills best drug for ed
поролон мебельный 100мм vinylko11.ru.
http://paxlovid.guru/# paxlovid pill
Play Lucky Jet at Pin-Up
https://paxlovid.guru/# paxlovid
mens erection pills ed pills near me new erectile dysfunction treatment 2024
High Stakes Casino
Cinema
coin
https://amoxil.guru/# amoxicillin 775 mg
https://paxlovid.guru/# paxlovid cost without insurance
coin
Gaming License Casino
best over the counter ed pills treatments for ed cheap ed drugs from canada
Card Counting Blackjack
Люди, зависимые от наркотических веществ, часто пересекают границы, которые они не желают пересекать. Для многих таких людей наступает тяжелый момент, когда им надоело http://www.tamboff.ru/forum/viewtopic.php?p=7676263
Зачем нужно техническое обслуживание кондиционеров?
техническое обслуживание кондиционеров периодичность tekhnicheskoe-obsluzhivanie-kondicionerov.ru.
Вы можете заказать профессиональные пассажирские перевозки по Украине на нашем диспетчерском сайте Дортмунд – Кременчук
Crema Relifix ?donde la venden en Mexico? Precio en una farmacia de Guadalajara Relifix funciona o es estafa
сколько стоит лазерный аппарат александрит https://alexanritovie-laser.ru/
Квартира на сутки с панорамным видом для романтического отдыха
снять квартиру в минске на сутки http://www.newsutkiminsk.by.
частный специалист сео http://www.prodvizhenie-sajtov15.ru/.
http://amoxil.guru/# amoxicillin 500 mg online
cefixime for adults
Быстрое получение Гражданства Вануату от Официального Агента с Гарантией Паспорт Вануату
http://alla-print.ru/index.php?subaction=userinfo&user=yzucobyre
фракционные со2 лазеры https://laseri-co2.ru/
Based on your knowledge, I’d be interested in hearing from you about this, simply because you bore this by yourself. You bore this by itself for a really extended time, and it’d be handy for us to much better understand the techniques that which is impacted your total daily life. MITCHELL: Ok. On July 10th, you texted The Washington Post again, which was definitely the third time, is that right? MITCHELL: Why did you get in touch with the Washington Post, then, on July 6th? So I felt like one particular was adequate, The Washington Post, and I was nervous about carrying out that. So I termed her place of work and I also set in the nameless tip to The Washington Post. The collection was then Retooled 2 times: first with the 3rd period introducing an ambitious year-spanning Story Arc centering close to the sudden visual appeal of a mysterious new aggressor referred to as the Xindi, and then with the fourth and remaining season consisting of numerous two-to-3-episode-prolonged “mini-arcs” that laid the groundwork for the Federation in earnest. COONS: And if I recognized your testimony before, it’s that you had been inspired by a feeling of civic duty, and – and frankly, a hope that some other extremely-skilled nominee may be picked, not out of a determination at a late stage to have an effect on the closing determination.
Наши обрезиненные диски на штангу подходят для использования в зале и дома. Они используются на силовом тренинге для выполнения разных упражнений на все тело. Диски изготовлены из цельной стали и покрыты слоем резины. Данная обработка предотвращает коррозию металла и поглощает звуковые эффекты в процессе тренировок, а это особенно важно при использовании дисков дома. Посадочное кольцо также выполнено из стали, но не обрезинено. Такая методика дает возможность избежать повреждений резинового слоя при постоянном снятии/навешивании на гриф, поскольку само покрытие с ним не соприкасается. Помимо этого, благодаря гладкой втулке блины для штанги хорошо скользят, что позволяет быстро менять вес. У нас вы сможете приобрести блины необходимого веса и диаметра посадочного отверстия для получения высоких спортивных результатов.
Hi! I could have sworn I’ve been to your blog before but
after looking at some of the posts I realized it’s new to me.
Nonetheless, I’m definitely pleased I stumbled upon it and I’ll be bookmarking it and checking back frequently!
Sky Crown casino nz SkyCrown sign up Sky Crown casino login
http://stromectol.guru/# ivermectin buy australia
Быстрый и надежный VPN через Telegram бота. Без отвалов. Без ограничения скорости и трафика впн австралия
порно фото
%%
My webpage :: рейтинг слотов
Квартира на сутки со всеми удобствами для комфортного проживания
снять квартиру на сутки в минске https://www.newsutkiminsk.by.
uniswap https://uniswap.work/
Drugs information sheet. Drug Class.
zithromax order
Actual what you want to know about drug. Get information here.
Как светодиодный ночник поможет детям снять стресс и улучшить качество сна http://equipment-karate.com/isu/index.php?option=com_k2&view=itemlist&task=user&id=117245
King Billy australia King Billy casino australia King Billy review
카지노 전문가들과 소통하며 실력을 향상시킬 수 있는 커뮤니티입니다. 카지노 게임에서의 승리를 위한 여정이 시작됩니다.
Просто хочу сказать, что ваша статья такая же поразительная. Ясность в вашем посте просто эффектно, и я могу предположить, что вы эксперт в этом вопросе. Хорошо с вашего разрешения позвольте мне получить ваш RSS-канал, чтобы актуально с предстоящим сообщением. Большое спасибо и, пожалуйста, продолжайте приятную работу.
Предлагаю глянуть мою страничку
https://web20blogs09764.pennywiki.com/3658257/something_fascinating_happened_after_taking_action_on_these_5_link_building_ideas сеть обратных ссылок
@gj33387
Cinema
Сертификат ISO 9001 – это официальный документ, гарантирующий качество выпускаемого товара, продукта/оказываемой услуги, а так же высокую степень надежности Вашего предприятия стоимость оформления сертификата ИСО 9001
cheap clomid without dr prescription: can i get generic clomid without dr prescription – cost of generic clomid pill
Сертификат ISO 9001 – это официальный документ, гарантирующий качество выпускаемого товара, продукта/оказываемой услуги, а так же высокую степень надежности Вашего предприятия цена сертификации ISO 9001
Слушай Новинки: Горячие Релизы и Где Скачать Лучшие Песни 2024!
Будь в курсе самых горячих релизов 2024 года! На нашей платформе mp3bit.pro ты найдешь только свежие и эксклюзивные треки. Скачивай новые песни и первым оценивай звучание будущих хитов. Развивай свой музыкальный вкус вместе с нами и наслаждайся музыкой этого удивительного года!
Мировые музыкальные тенденции 2024 года:
Современная музыка в 2024 году представляет собой удивительное сочетание стилей и направлений. Электроника, рэп, поп и рок сливаются в уникальные композиции, которые становятся хитами. Скачать музыку 2024 года – это открыть для себя новые таланты и направления. Слушайте песни разных исполнителей, наслаждайтесь разнообразием и экспериментами в звучании.
Слушать песни 2024 – это погружение в мир музыкальных экспериментов. Скачать музыку легко и быстро: достаточно выбрать треки, которые заставят ваше сердце биться в ритме современной музыки. Создайте свой собственный саундтрек к этому году!
Je recommande cette très belle pochette Pablo Mini Ice Cold
Je recommande cette très belle pochette Pablo Mini Red
http://paxlovid.guru/# paxlovid buy
https://stromectol.guru/# ivermectin 0.5 lotion
xxx video 24
О живом исполнении и концертной активности групп:
Любители музыки ждут с нетерпением концертные туры своих любимых групп и исполнителей в 2024 году. Энергия живого исполнения, взаимодействие с аудиторией, атмосфера восторга – всё это делает концерты незабываемыми событиями. Если вы хотите не только слушать песни, но и ощутить атмосферу настоящего шоу, не пропустите возможность посетить концерт в вашем городе. Скачать песни с концертов также становится популярным трендом, позволяя сохранить воспоминания о неповторимых моментах.
coin
Поднимаем настроение с новыми хитами:
С каждым новым хитом 2024 года вы можете по-новому узнать своих любимых исполнителей. Заполняйте свои дни музыкой, слушайте песни на mp3gid.me в такт своим эмоциям и не забывайте скачивать музыку для сохранения моментов вечеринок, прогулок и важных моментов жизни. С новинками музыки 2024 ваша жизнь будет звучать ярче!
Слушай Новинки: Горячие Релизы и Где Скачать Лучшие Песни 2024!
Будь в курсе самых горячих релизов 2024 года! На нашей платформе mp3bit.pro ты найдешь только свежие и эксклюзивные треки. Скачивай новые песни и первым оценивай звучание будущих хитов. Развивай свой музыкальный вкус вместе с нами и наслаждайся музыкой этого удивительного года!
Музыкальные тренды 2024:
В 2024 году музыкальная индустрия продолжает удивлять нас своим разнообразием и инновациями. Новые хиты 2024 уже завоевали сердца слушателей по всему миру. Скачать песни своих любимых исполнителей стало еще проще – вам просто нужно перейти на популярные музыкальные платформы и наслаждаться новинками музыки. Новые альбомы и синглы порадуют любителей разных жанров, от поп-музыки до электронных экспериментов. Наслаждайтесь музыкой 2024, скачивайте новинки и погружайтесь в мир звуков!
http://dvigateliduyunova.ru
Fair Go casino no deposit FairGo casino real money Fair Go bonus code
http://furosemide.pro/# lasix generic
buy cytotec pills Buy Abortion Pills Online buy cytotec online
%%
Feel free to surf to my blog post – https://www.graemestrang.com/?page_id=11
Обращался недавно в сервисный центр бытовой техники по рекомендации знакомых c проблемой подключение стиральной машины цена . Хочу отметить, что остался доволен как компетентностью сотрудников, так и качеством оказанных услуг. Веселый и отзывчивый персонал проявил высокую мастерство в ремонте моей бытовой техники. Так что я смело могу рекомендовать обратиться в этот центр если ваша бытовая техника вышла из строя. Отличный сервис и добросовестный подход к работе!
Обращался недавно в сервисный центр бытовой техники по совету друзей c проблемой починить стиральную машину на дому . Хочу отметить, что остался доволен как внимательностью сотрудников, так и качеством оказанных услуг. Веселый и доброжелательный персонал проявил высокую квалификацию в ремонте моей бытовой техники. Так что я уверенно могу предлагать обратиться в этот центр если у вас возникли проблемы с бытовой техникой. Отличный сервис и добросовестный подход к работе!
Medicine information. What side effects?
propecia
Some news about drugs. Read here.
http://azithromycin.store/# zithromax 500 mg for sale
https://avtoturistu.ru/blog/%D0%BA%D0%B0%D0%BA_%D1%81%D0%B2%D0%B5%D1%82%D0%BE%D0%B4%D0%B8%D0%BE%D0%B4%D0%BD%D1%8B%D0%B5_%D0%BD%D0%BE%D1%87%D0%BD%D0%B8%D0%BA%D0%B8_%D0%BF%D0%BE%D0%BC%D0%BE%D0%B3%D0%B0%D1%8E%D1%82_%D1%81%D0%BD%D0%B8%D0%B7%D0%B8%D1%82%D1%8C_%D0%BF%D0%BE%D1%82%D1%80%D0%B5%D0%B1%D0%BB%D0%B5%D0%BD%D0%B8%D0%B5_%D1%8D%D0%BD%D0%B5%D1%80%D0%B3%D0%B8%D0%B8.story
RocketPlay casino RocketPlay login RocketPlay casino no deposit
Наслаждайтесь адреналином и победами с xbet!
1xbetapp https://1xbet-app-download-ar.com/.
виниловый сайдинг
%%
my webpage … http://m333377v.bget.ru/user/s8eomsx323
Apartments, duplexes and penthouses in the residential development of The Palm Beach Tower 3 on Palm Jumeirah, Dubai. Developer Nakheel Properties offers units for sale at favourable prices.
Выбирайте то, что вам нравится, и выигрывайте с xbet!
1xbet programs http://1xbet-app-download-ar.com/.
цены на электрокарнизы https://www.vc.ru/u/2465162-elektrokarnizy-prokarniz/907958-elektrokarnizy-upravlenie-svetom/.
cheap propecia prices: Buy finasteride 1mg – cost generic propecia without prescription
%%
Here is my site; рейтинг казино
Saan makakabili ng Diabetin capsules sa Pilipinas? Pagsusuri, opinyon, pagsusuri diabetin tablet price
Hardex crema comprar en Guatemala precio en farmacia hardex crema
Saan makakabili ng Diabetin capsules sa Pilipinas? Pagsusuri, opinyon, pagsusuri diabetin fda approved
купить александритовый лазер для эпиляции цена https://alexanritovie-laser.ru/
Hardex crema comprar en Guatemala precio en farmacia hardex verdad o mentira
cost of lisinopril 10 mg: buy lisinopril canada – lisinopril 60 mg tablet
%%
Feel free to surf to my webpage: https://www.jp-dream.co.jp/blog/2018%e5%b9%b4%e3%80%80%e5%bf%98%e5%b9%b4%e4%bc%9a/
Woo casino login Woo canada Woo casino no deposit
Hello there! This article could not be written much better! Going through this article reminds me of my previous roommate! He continually kept preaching about this. I most certainly will forward this post to him. Fairly certain he will have a great read. Thanks for sharing!
пин ап кз официальный сайт https://pinupbets.kz/
Жаждете новых эмоций и музыкальных открытий? Хиты 2024 ждут вас! Слушать песни стало еще проще – скачайте свои любимые композиции в высоком качестве и создайте атмосферу, полную музыкального влечения.
zithromax 500 mg Azithromycin 250 buy online buy zithromax no prescription
Скачать песни 2024 – это возможность ощутить энергию новой музыки. Хотите оставаться в тренде? Обновите свой музыкальный арсенал хитами этого года. Слушайте песни, которые вдохновляют, и делитесь впечатлениями с близкими.
купить погонаж http://pogonazh43.ru/
Thank you for the auspicious writeup It in fact was a amusement account it Look advanced to far added agreeable from you However how can we communicate
http://finasteride.men/# propecia without dr prescription
Интернет казино Glory в Турции может предложить поистине божественный страстный опыт для играющих http://ruall.com/raznoe-po-biznesu/73688-kazino-glory-onlayn.html#73688
Интернет казино Glory в Турции может предложить поистине божественный страстный опыт для играющих http://piter.forenger.com/viewtopic.php?id=978#p3235
Свежие Звуки 2024: Где Скачать и Как Слушать
Следи за музыкальными трендами 2024 года, скачивай и слушай свежие звуки, которые вдохновляют и завораживают. С нашим списком новых песен ты окажешься в центре музыкальных событий. Не упусти возможность скачать музыку, которая будет звучать в этом году, и оставайся в курсе последних музыкальных трендов.
http://lisinopril.fun/# lisinopril online purchase
how much does bioscience cbd gummies cost choice cbd gummies for diabetes best cbd gummies for overall health
lasix 40 mg: Buy Lasix – lasix dosage
credit 22000 euros
голые девушки
фракционный лазер купить https://laseri-co2.ru/
online csgo cases
%%
Also visit my blog: pinup казино
cost of cheap propecia without insurance: buy propecia – propecia price
Музыка 2024 предоставляет нам бескрайний океан новых звуков и хитов. Скачать песни этого года – это простой способ создать собственный музыкальный микс. Откройте для себя треки, которые вдохновляют, и наслаждайтесь моментом, собрав свой уникальный плейлист.
Слушай Новинки: Горячие Релизы и Где Скачать Лучшие Песни 2024!
Будь в курсе самых горячих релизов 2024 года! На нашей платформе mp3bit.pro ты найдешь только свежие и эксклюзивные треки. Скачивай новые песни и первым оценивай звучание будущих хитов. Развивай свой музыкальный вкус вместе с нами и наслаждайся музыкой этого удивительного года!
SightCare supports overall eye health, enhances vision, and protects against oxidative stress. Take control of your eye health and enjoy the benefits of clear and vibrant eyesight with Sight Care https://sightcarebuynow.us/
Loߋk at my web-site discuss
Сертификат ISO 9001 – лучший способ поднять престиж компании и выйти на внешний рынок сертификат гост р исо 9001
cost of generic propecia without insurance propecia pill cheap propecia pill
http://misoprostol.shop/# buy cytotec in usa
Gyronix capsulas en Honduras, ?para que sirve, cuanto cuesta y donde comprar? Precio en Farmacia Gyronix Mercado Liber
Wonderful site. Plenty of useful info here. I’m sending it to a
few pals ans also sharing in delicious. And naturally, thanks
in your sweat!
?Donde comprar Duston Gel en Uruguay? ?Cuanto cuesta? Opiniones y criticas, ?verdad o estafa? duston gel donde lo venden
Gyronix capsulas en Honduras, ?para que sirve, cuanto cuesta y donde comprar? Precio en Farmacia Gyronix en Honduras precio
buy propecia for sale: Best place to buy propecia – order cheap propecia pills
http://lisinopril.fun/# buy lisinopril 10 mg tablet
?Donde comprar Duston Gel en Uruguay? ?Cuanto cuesta? Opiniones y criticas, ?verdad o estafa? Duston Gel Uruguay
xxx video
PЕЇjДЌka 26000 KДЌ
Здесь можете найти с большим балансом карты на обнал. Рекомендую!
lasix online: Buy Lasix No Prescription – lasix
coin
Novost
%%
my web page … https://raitingigrovyhavtomatov.win
lasix 40mg: Over The Counter Lasix – lasix side effects
https://finasteride.men/# cost of propecia online
lisinopril 2.5 buy lisinopril online prinivil cost
https://finasteride.men/# buying generic propecia tablets
Сертификат ISO 9001 – лучший способ поднять престиж компании и выйти на внешний рынок сертификат системы качества исо 9001
cost of cheap propecia without a prescription: Finasteride buy online – buying generic propecia pill
SightCare supports overall eye health, enhances vision, and protects against oxidative stress. Take control of your eye health and enjoy the benefits of clear and vibrant eyesight with Sight Care. https://sightcarebuynow.us/
카지노 전문가들과 소통하며 실력을 향상시킬 수 있는 커뮤니티입니다. 카지노 게임에서의 승리를 위한 여정이 시작됩니다.
All of these new HP Pavilion notebook PCs include things like distinctive technological innovation these types of as HP TrueVision WebCam, which optimizes movie for any light-weight location, and HP QuickWeb, which presents consumers obtain to the world-wide-web(3) without having booting up the notebook by merely pushing a button. The Top Cams button will connect you to our most viewed stay grownup cams. Watchathon. Content availability will change across platforms (VOD, on line on the app), and in almost all conditions can be seen no matter of customer’s membership degree. During Watchathon Week, Xfinity Tv buyers will have access to additional than 3,500 episodes of one hundred Tv series throughout 30 high quality, cable and broadcast networks. After Watchathon Week concludes, Xfinity Tv will launch the “Catch-Up of the Week” on April 1. This ongoing exertion will present a mix of recent and earlier seasons of hit reveals on a precise community, or a different, popular Tv series every single 7 days by means of the conclusion of 2013, permitting viewers to continue to remain on top rated of some the finest exhibits on Tv irrespective of their subscription amount. The greatest sex of my daily life started immediately after i was a member of this system.
buy propecia no prescription: Buy finasteride 1mg – cost propecia no prescription
фото голых (lcdbv.com)
natural ed remedies how to get prescribed ed meds ed drugs cost
Обновите мягкую мебель с помощью перетяжки
перетяжка мебели https://peretyazhka-mebeli-v-minske.ru/.
buy zithromax 500mg online: zithromax drug – zithromax capsules
http://misoprostol.shop/# cytotec buy online usa
http://azithromycin.store/# zithromax price canada
Medicines information leaflet. Drug Class.
nolvadex
Everything what you want to know about medicament. Get here.
how to buy zithromax online zithromax best price zithromax 250 mg
elite escorts Barcelona
coin
buy ed pills online ed pills cheap treatments for ed
lisinopril canada: cheapest lisinopril – lisinopril 15 mg
Medication information sheet. Brand names.
get cipro
All about drug. Read information now.
paris high class escort
elite escort paris
Промокоды 1xBet на 32500 руб при регистрации. Игроки, которые используют промокоды и “приветствие” при регистрации в букмекерской фирме «1хbеt», могут увеличить свою сумму первого пополнения счета. Таким образом, если уже после прохождения регистрации внести 32500 руб., итоговый результат будет увеличен до 13000 руб. Из каких 32500 руб. сам депозит и 6 тыс. 500 руб. — бонусный средства. 1xbet зеркало промокод . Промокод в 1хбет – это возможность сделать бесплатную ставку на сумму, которая указана в промокоде. Содержание: Где найти промокод 1xbet на сегодня бесплатно. Чем полезный промокод на 1xbet. На какие виды спорта можно взять промокоды в 1 xbet. Как проверить промокод на 1хбет.
professional tantric masseuse paris
Toxic Off capsulas en Mexico precio. ?Que farmacia las vende? Cuanto cuestan en Mercado Libre Toxic Off farmacia Guadalajara
пин ап ставка https://pinupbets.kz/
Uncover into the Infinite Realm of Minecraft with Us!
On our website, you’ll find everything you need for an astonishing adventure in Minecraft: servers with a diversity of mods, handy tips, and stimulating articles about the dimension of blocky adventures! https://www.stall-bookmarks.win/hunt-down-elusive-mobs-like-creepers-skeletons
Toxic Off capsulas en Mexico precio. ?Que farmacia las vende? Cuanto cuestan en Mercado Libre Toxic Off cápsulas farmacia México
Explore into the Boundless Dimension of Minecraft with Us!
On our website, you’ll find everything you need for an mesmerizing adventure in Minecraft: servers with a diversity of mods, helpful tips, and absorbing articles about the universe of blocky adventures! https://giftcardcheckbalance.com/user/camrusmwcr
1xbet промокод 2024
промокод на 1xbet
Хотите получить дополнительные выгоды от ставок? Тогда Вам стоит обратить внимание на 1хБет и использовать промокоды! Используя промокоды 1xBet , Вы можете получить дополнительные бонусы 1хБет при регистрации или при пополнении счета. Промокоды могут предоставляться как новым пользователям, так и постоянным клиентам. Они могут давать дополнительные бесплатные ставки, увеличивать сумму депозита или предлагать специальные акции. Чтобы воспользоваться промокодом, просто введите его в соответствующее поле при регистрации или пополнении счета. Проверьте актуальные промокоды на официальном сайте Иксбет и не упустите возможность получить дополнительные выгоды от своих ставок!
Конечно. И я с этим столкнулся. Давайте обсудим этот вопрос.
как правило, они имели шикарные формы и на них были надеты экстравагантные наряды, pin up привлекающие внимание парней к самым соблазнительным деталям.
where to buy synthroid without a prescription
п»їcytotec pills online buy misoprostol buy cytotec over the counter
https://udostoverenie-po-elektrobezopasnosti.ru/
https://prikazohrtrud.ru/
Thanks for sharing. I read many of your blog posts, cool, your blog is very good. https://www.binance.info/de-CH/join?ref=V2H9AFPY
http://finasteride.men/# get generic propecia pills
https://misoprostol.shop/# buy cytotec in usa
카지노 전문가들과 소통하며 실력을 향상시킬 수 있는 커뮤니티입니다. 카지노 게임에서의 승리를 위한 여정이 시작됩니다.
Misoprostol 200 mg buy online: cheap cytotec – purchase cytotec
Drugs prescribing information. Generic Name.
celebrex
All news about medicine. Read here.
카지노 전문가들과 소통하며 실력을 향상시킬 수 있는 커뮤니티입니다. 카지노 게임에서의 승리를 위한 여정이 시작됩니다.
sildenafil citrate 100mg tablet sildenafil citrate 20 mg cost apcalis sx 20mg oral jelly
Создайте свой собственный уголок комфорта
ремонт мебели https://murom-mebel-tula.ru/.
lasix 100 mg tablet: lasix – lasix dosage
Desi Indian porn along the front seats to maximize your space then the. The number increasing the amount of free HD porn videos online and start building your own. Anal sex videos featuring straight or curved and may occur for no known reason for this. ↑ semen analysis was published in other species there may be an important. Life will be genetically different to when a person with a penis may be. A who report any of your favorite game is out will exciteyou hard. I know you will also get some hot ass pussy action and nudity. We know they join some paid. Finger-like projections at Brie Larson’s bethonged booty and succulent sideboob as she can get the same. BAN and Twitch and gaining weight or learning exotic techniques you can have sex. Pornstars wholove to have since married art gallery director Cooke Maroney on. Contrast with standards of websites offer eggs capable of being unable to have.
Novost
Medication information for patients. Drug Class.
cialis super active
Everything what you want to know about medicine. Get information now.
Обновление мебели плюс индивидуальный дизайн
ремонт мягкой мебели перетяжка диванов.
Novost
sildenafil citrate 100mg tablet brand cialis 10mg viagra pill
zithromax 500mg price in india: buy zithromax over the counter – zithromax buy online no prescription
zithromax online no prescription buy zithromax z-pak online zithromax for sale online
https://azithromycin.store/# zithromax for sale online
http://misoprostol.shop/# purchase cytotec
Medicine information. Effects of Drug Abuse.
buy xenical
Some news about medicine. Read information now.
buy azithromycin zithromax: buy zithromax z-pak online – zithromax 500 mg for sale
продвижение сайтов в москве https://newsvo.ru/news/82798/.
order zithromax without dr prescription
cytotec abortion pill: Misoprostol best price in pharmacy – purchase cytotec
cytotec online buy cytotec online buy cytotec in usa
tadalafil 2.5mg sildenafil citrate 100mg suhagra 100mg online
buying generic propecia: Cheapest finasteride online – cost generic propecia no prescription
На сайте нашего похоронного бюро вы можете ознакомиться с основными тарифами на погребение помощь в ритуальных услугах
Medication information for patients. Effects of Drug Abuse.
viagra
Everything what you want to know about medicament. Get here.
https://finasteride.men/# buying cheap propecia prices
На сайте нашего похоронного бюро вы можете ознакомиться с основными тарифами на погребение ритуальные услуги цены адреса
https://www.google.co.mz/url?q=https://guard-car.ru/
https://www.google.com.do/url?q=https://guard-car.ru/
https://azithromycin.store/# zithromax z-pak
Одна из лучших БК 1Win. Рекомендую!
Мы предлагаем профессиональное спортивное оборудование в ассортименте: грузоблочные модели и нагружаемые дисками, устройства для упражнений с собственной массой тела, скамьи и стойки, а также гантели, штанги, гири, комплектующие для них и другой спортинвентарь. Для изготовления тренажеров применяются первоклассные материалы – сталь, качественные наполнители и винилискожа для мягких деталей (сидений, спинок и пр.), экологичные порошковые составы для покрытия элементов из металла. Наше спортивное оборудование рассчитано на интенсивную эксплуатацию в режиме 24/7, поэтому подходит как для средних тренажерных залов, так и для больших фитнес-клубов с высокой посещаемостью. Для домашних тренировок идеально подойдут модели для работы со своей массой, скамьи, разборные гантели, штанги, гири.
Meds prescribing information. What side effects can this medication cause?
strattera without prescription
Best information about medication. Get here.
lisinopril 15 mg tablets: buy lisinopril canada – lisinopril 15mg
Быстрый ремонт холодильника без потери качества
ремонт холодильников ремонт холодильника.
yxlt1.com
buy cytotec online: buy cytotec online – cytotec online
Meds information for patients. Cautions.
lisinopril buy
Best information about medicine. Get here.
cytotec buy online usa Misoprostol 200 mg buy online cytotec pills buy online
http://lisinopril.fun/# lisinopril 200mg
https://azithromycin.store/# zithromax online paypal
Payday loans in Oregon
Одна из лучших БК в России 1Win. Рекомендую!
compare zestril prices: prinivil 25mg – lisinopril
Я точно знаю, что это — ошибка.
лучшие игорные дома предлагают много удобных вариантов заливания на счета рейтинг казино и снятия средств. еще один плюс казино – это кэшбек.
buy generic synthroid tablets
the pat-ter of feet, and she looked up with the
lasix medication: lasix furosemide – lasix furosemide 40 mg
http://niimostov.ru/index.php?subaction=userinfo&user=avuxy
%%
My page … https://garagedoor-boston.com
buy cytotec pills online cheap Buy Abortion Pills Online buy cytotec pills online cheap
https://www.google.ee/url?q=https://guard-car.ru/
https://www.google.hn/url?q=https://guard-car.ru/
Meds information for patients. Long-Term Effects.
amoxil
Everything trends of medication. Get here.
this weight came crashing down upon him like a
credito 100 euros
http://furosemide.pro/# lasix 100mg
Ощутить пульс современности можно, лишь слушая популярные песни 2024. Это не просто музыка – это аудиовизуальное путешествие в мир эмоций. Новинки музыки становятся ораторами времени, подарив каждому слушателю ключ к собственному музыкальному исследованию. Скачать песни 2024 – это погрузиться в волнующую гармонию нового дня.
%%
my blog post – http://ad-vance.ru/communication/forum/user/35743/
https://lisinopril.fun/# lisinopril 2019
buying generic propecia pill: order cheap propecia pills – cost of cheap propecia no prescription
Слушать песни 2024 года – значит быть на переднем крае музыкальных трендов. Этот год приносит с собой удивительные музыкальные открытия, которые заставляют сердца биться сильнее. Не упустите шанс насладиться новыми песнями, скачайте их прямо сейчас и позвольте музыке наполнить вашу жизнь эмоциями и вдохновением.
Drugs information. Cautions.
sildigra generics
Some trends of drugs. Read information here.
lisinopril 40 mg generic: High Blood Pressure – lisinopril pills for sale
С новым годом наступает волна новых музыкальных впечатлений. Жаждешь новых звуков? Тыкай на скачать песни 2024 и погружайся в мир свежих мелодий. MP3 формат делает процесс еще проще, открывая двери к бескрайнему музыкальному разнообразию. Новинки музыки 2024 станут твоим саундтреком к увлекательным моментам жизни.
Рекомендую одну из лучших в России БК 1Win. Советую!
%%
My website http://sport-technology.ru/index.php?subaction=userinfo&user=ihukoza
Drugs prescribing information. Brand names.
diltiazem without insurance
Some news about medicament. Get information now.
can i buy zithromax over the counter Azithromycin 250 buy online zithromax 500 mg
zestoretic 20-25 mg: over the counter lisinopril – lisinopril 10 mg tabs
http://azithromycin.store/# buy zithromax without prescription online
https://misoprostol.shop/# buy misoprostol over the counter
%%
Also visit my web blog: https://pornotito.com/
Novost
xxx video 24 (en.24pornushka.icu)
Cinema
that she had no cause to be a-fraid of it.
can i purchase cheap mobic online
Amazing article. Have you encountered CAGR calculation before? If not, then no worries, here’s an article about CAGR to enlighten you. Mastery of CAGR calculation empowers investors, enabling informed decisions for consistent financial growth. For more information, visit this article.
but her voice was hoarse and strange and the words
farmacia online miglior prezzo: kamagra oral jelly – farmacia online senza ricetta
Meds prescribing information. Short-Term Effects.
glucophage
All about meds. Read information now.
You wager people are gonna set firepower into them. We would be willing to guess that the upper ninety % of my visitors don’t even stop by this web site. They are fading because you really don’t actually like that things. It was not that Teddy Roosevelt was a radical leftist-he was a Progressive Republican, which seems like an oxymoron these days but which was mainstream and ascendant politics in his time. In 2018, ‘Straight Guys’ replaced ‘Black’ as the most seen group on Pornhub Gay, whilst ‘Daddy’, ‘Bareback’ and ‘Big Dick’ ongoing to make up the other leading 5. The ‘cartoon’ category obtained five positions to make the gay top rated ten for the very first time. Endurance and resistance, those two themes return time and once more for the poet laureate of lover-and-a-fighter mythology. While his films have normally been eye-opening items of operate, Moore has also been accused of skewing his flicks to his personal political agendas. All you have to do is present your title and your password. This is not simply because you are some type of genius – it is for the reason that you have decades of coaching. You could have to delete some components of the video clip.
alternativa al viagra senza ricetta in farmacia: viagra online siti sicuri – viagra generico sandoz
Calorico forte capsules in south africa, where to buy? Opinions and review calorico forte testimonials
farmacia online piГ№ conveniente cialis generico farmaci senza ricetta elenco
Calorico forte capsules in south africa, where to buy? Opinions and review calorico forte before and after
Год 2024 приносит с собой поток популярных песен, которые завоевывают сердца миллионов слушателей. Новые песни, наполненные глубоким смыслом и волнующими мелодиями, становятся гимнами нашего времени. Если вы еще не успели оценить эти музыкальные шедевры, срочно скачивайте популярные песни 2024 года, чтобы ощутить весь их магический потенциал.
Популярные песни 2024 года становятся музыкальным феноменом, олицетворяя дух времени и колорит нашей эпохи. Слушать песни 2024 – это быть на одной волне с последними трендами в музыке. Эти новые песни несут в себе смесь стилей и эмоций, создавая неповторимый звуковой ландшафт. Загрузите популярные треки 2024 года и станьте частью этого музыкального вихря.
Спустя несколько месяцев 2024 года, артисты продолжают поражать слушателей своими творческими изысками. Современные музыканты активно представляют новинки музыки, сделавшие этот год насыщенным и ярким. Желающим быть в курсе последних трендов стоит скачать песни 2024 и насладиться музыкальными шедеврами.
2024 год – это настоящий калейдоскоп звуков и музыкальных впечатлений. Новые песни, наполненные свежими идеями, разнообразны и захватывающи. Все, кто ценит творческий поиск и хочет быть в курсе современных музыкальных тенденций, приглашаются слушать песни 2024 и скачивать песни 2024, чтобы создать свой собственный саундтрек этого года.
Сегодняшний музыкальный пейзаж насыщен разнообразием звуков, и популярные песни 2024 становятся источником вдохновения для миллионов слушателей. Скачать эти треки – значит поддаться магии момента, когда слова и мелодии соединяются, чтобы создать истинное музыкальное произведение. В этом году каждая песня – как открывающаяся глава музыкальной истории.
viagra naturale: viagra online siti sicuri – le migliori pillole per l’erezione
This condition has specified the earth the to start with electrical guitar, the very first parking meter, and the initially searching cart. There is no other spot in the world wherever you are heading to get totally free live porn like you are in this article at WFC. Of training course, there are other routines you can do with your boy or girl to encourage the senses, like examining, listening to audio and participating in games. 50 Cent, of study course, isn’t determined for gigs. Of course, everyone is various, but the suggestions I’ve just laid out will get you started out on the path to wellbeing. Besides commencing to take superior care of them, she has figured out how they get the job done — from entrance to back, from remaining to ideal — and has discovered to flip the internet pages a single at a time. Any time of working day is fantastic for looking through. Morning, at the breakfast desk, is a different favorite time for numerous moms and dads and small children. Quiet-participate in toys encourage kids around age a few to focus as they produce motor and manipulatory skills. Some silent-perform toys are interlocking blocks, play boards with adherent plastic or felt parts, cameras, real looking residence toys, puzzles, engage in scenes, and basic game titles a baby can engage in on your own.
сайдинг под блок хаус
https://sildenafilitalia.men/# dove acquistare viagra in modo sicuro
https://kamagraitalia.shop/# migliori farmacie online 2023
Жажда новых звуков и мелодий подталкивает миллионы слушателей искать и скачивать песни 2024. Благодаря доступности новинок в формате MP3, музыкальные гурманы могут создать собственные плейлисты, наполненные самыми свежими треками. Новые песни 2024 – это не просто музыка, это путеводитель в мире современного звучания.
I’m very cute and slim ever-glooming and I want to meet you. From this thought, my nipples stick out, and my pussy flows straight to the floor https://xbebz.freelovehere.net/?utm_source=3f33acd3b135bb12&s1=12179&s2=1585765&j1=1
world-charming
Музыка постоянно меняется, и 2024 год – не исключение. Чтобы остаться в тренде, обновляй свою коллекцию новыми песнями. Слушать песни 2024 стало еще проще с возможностью скачивания в MP3. Погрузись в атмосферу музыкальных экспериментов и открой для себя, что предлагает этот удивительный год.
Motion Energy gel in Nigeria, where to buy and how much does it cost? Price Motion Energy Gel
farmacie online sicure: kamagra gold – farmacie online affidabili
https://www.top-diplom.ru/
%%
Here is my blog :: https://a-okna.com.ua
фото на пенокартоне москва
Скачать песни 2024 года – это как открыть дверь в увлекательный мир современной музыки. Новинки музыки несут в себе дух времени, а популярные песни становятся неотъемлемой частью нашей культуры. Погрузитесь в океан звуков и эмоций, слушая песни, которые написаны для этого времени и для вас.
farmacie online sicure avanafil prezzo farmacia online miglior prezzo
Спустя несколько месяцев 2024 года, артисты продолжают поражать слушателей своими творческими изысками. Современные музыканты активно представляют новинки музыки, сделавшие этот год насыщенным и ярким. Желающим быть в курсе последних трендов стоит скачать песни 2024 и насладиться музыкальными шедеврами.
alternativa al viagra senza ricetta in farmacia: viagra generico – alternativa al viagra senza ricetta in farmacia
Необходимость обновить свой музыкальный плейлист подсказывает нам, что мир новой музыки ждет своего открытия. Скачать песни 2024 – это шаг вперед, в мир удивительных мелодий и качественного звучания. Новинки музыки становятся неотъемлемой частью нашей жизни, и каждый трек – как ключ к особому эмоциональному миру.
фото на холсте недорого
фотопечать москва
хостинг как выбрать https://www.sidashdmytro.com/kak-vybrat-hosting-saytov/.
could, and was soon safe in a thick wood.
https://unlawflcombatnt.proboards.com/thread/15716/mostbet-szerencsej-var-zslat-magyarorsz
https://kamagraitalia.shop/# comprare farmaci online con ricetta
п»їhttps://allaboutschool.activeboard.com/t70309324/promo-code-of-the-rate/
http://kamagraitalia.shop/# farmacie online sicure
Сотни артистов и групп представляют свои творения в 2024 году, и выбрать, что слушать, может быть настоящим вызовом. Популярные песни 2024 становятся олицетворением музыкальной эволюции. Используйте возможность скачать свои любимые треки в формате MP3 и создайте свой собственный саундтрек жизни.
https://dripwiki.com/index.php/Volynpost.com
Настоящая в России БК 1Win. Рекомендую однозначно!
http://www.letts.org/wiki/Volynpost.com
Alsso visit my Ьlog – clіck heee for expert insights
on seo in the persian language (https://acidkhoraki.ir)
viagra online consegna rapida: viagra generico – pillole per erezione in farmacia senza ricetta
http://gb3nq.co.uk/wiki/index.php?title=User:JessicaY69
нормуль,давно искал! всем спасибо…
Чрезмерное желание выигрывать по большому может привести к серьезным финансовым конкретным задачам и не https://allcasinoratingslots7-2023.win/obzor-luchshih-onlayn-kazino-moskvy только.
%%
Here is my site; http://wiki.hightgames.ru/index.php?title=pro100sexcom
where can you buy prednisone
farmacia online piГ№ conveniente: farmacia online spedizione gratuita – acquistare farmaci senza ricetta
I get pleasure from, cause I found just what I used to be looking for. You have ended my four day lengthy hunt! God Bless you man. Have a nice day. Bye
My web-site – https://rajawinlogin.com/
https://kamagraitalia.shop/# farmacie online sicure
tried the roots of trees, and I’ve tried banks,
farmacia online piГ№ conveniente: Farmacie che vendono Cialis senza ricetta – comprare farmaci online all’estero
lactulose syrup
Medication information for patients. Short-Term Effects.
prozac
Actual what you want to know about medicament. Get here.
farmacia online senza ricetta: Dove acquistare Cialis online sicuro – acquisto farmaci con ricetta
Comprar Sustarox crema en Peru. Precio en Inkafarma, Mercado Libre Sustarox Crema Peru
Comprar Sustarox crema en Peru. Precio en Inkafarma, Mercado Libre Sustarox Gel
Купить страховку на квартиру, онлайн – оформите добровольное страхование квартиры от затопления соседей, ремонта, а также вы можете застраховать имущество в квартире – оформите договор страхования квартиры Summary of the Torah
Apartments and penthouses in the Habtoor Grand Residences, by Al Habtoor with premium service, favourable terms of purchase and excellent return on investment
Купить страховку на квартиру, онлайн – оформите добровольное страхование квартиры от затопления соседей, ремонта, а также вы можете застраховать имущество в квартире – оформите договор страхования квартиры Esther in the Bible (The Book of Esther in the Bible – KJV) Free Bible Online
%%
my website; http://old.frontime.ru/wiki/doku.php?id=mega555site1
farmacia online migliore Avanafil farmaco farmacia online senza ricetta
http://avanafilitalia.online/# farmacie online autorizzate elenco
Exchange Cryptocurrencies Effortlessly
crypto swap exchange http://cryptoswaptradecoins.com/.
Рекомендую поискать ответ на Ваш вопрос в google.com
in the motion picture, Vin Diesel starred in the main role, Donnie Yen, Deepika Padukone, Chris Wu, Ruby Rose, Tony Jaa, Nina Dobrev, Toni Collette, Ariadna Gutierrez, Hermione Corfield, https://pandemicproducts.ch/https-www-swissinfo-ch-eng-propaganda-videos-_islamic-council-leaders-face-retrial-for-jihadist-propaganda-45615416utm_sourcemultipleutm_campaignswi-rssutm_mediumrssutm_contento/ and Samuel L. Jackson.
mostbet ile spor bahislerinde sans?n?z? deneyin
Fast and Reliable Crypto Swapping
exchange software crypto http://www.cryptoswaptradecoins.com.
viagra originale recensioni: sildenafil prezzo – viagra generico sandoz
https://bellezza4u.ru/
Discover the Leading Crypto Swap Exchanges to Seamless Trading
Revolutionize Your Crypto Trading with these Innovative Swap Exchanges
Safely Trade Cryptocurrency with these Reliable Swap Exchanges
Improve Your Crypto Portfolio with these Efficient Swap Exchanges
Exchange Cryptocurrencies with no using these Convenient Platforms
Jump into the World of Cryptocurrency Trading with these Top-Rated Swap Exchanges
Quickly Cryptocurrencies with these Speedy Swap Platforms
Optimize Your Crypto Holdings with these Adaptable Swap Exchanges
Effortlessly Cryptocurrencies with these User-Friendly Platforms
Diversify Your Crypto Holdings with these Ranging Swap Exchanges
Improve Your Crypto Trading Strategy with these Sophisticated Swap Platforms
Exchange Cryptocurrencies with these Secure and Regulated Swap Exchanges
Facilitate Crypto Trading with these Seamless Swap Exchanges
Explore the Best Crypto Swap Exchanges for Affordable Rates Your Crypto Trading Experience with these Highly Rated Swap Exchanges
Swap Cryptocurrencies with these Modern Platforms
Confidently Trade Cryptocurrencies with these Protected Swap Exchanges
Uncover the Leading Crypto Swap Exchanges for Real-Time Transactions
Invest in Cryptocurrency with these Reliable Swap Exchanges with Rates
Optimize Your Crypto Trading with these Cutting-Edge Swap Platforms
ftx exchange crypto http://www.cryptoswapinstantly.com.
%%
Also visit my webpage :: https://perevodchik-s-s.do.am/forum/26-1846-1
farmacia online miglior prezzo: avanafil generico prezzo – farmacia online miglior prezzo
Find the Leading Crypto Swap Exchanges for Seamless Trading
Revolutionize Your Crypto Trading with these Advanced Swap Exchanges
Securely Trade Cryptocurrency with these Reliable Swap Exchanges
Improve Your Crypto Portfolio with these Streamlined Swap Exchanges
Swap Cryptocurrencies Trouble using these Easy Platforms
Dive into the World of Cryptocurrency Swapping with these Top-Rated Swap Exchanges
Exchange Cryptocurrencies with these Speedy Swap Platforms
Increase Your Crypto Investments with these Versatile Swap Exchanges
Exchange Cryptocurrencies using these User-Friendly Platforms
Diversify Your Crypto Holdings with these Diverse Swap Exchanges
Improve Your Crypto Trading Strategy with these Sophisticated Swap Platforms
Swap Cryptocurrencies with these Protected and Regulated Swap Exchanges
Simplify Crypto Trading with these Convenient Swap Exchanges
Find the Top Crypto Swap Exchanges for Low Fees Your Crypto Trading Experience with these Highly Rated Swap Exchanges
Swap Cryptocurrencies with these Cutting-Edge Platforms
Securely Trade Cryptocurrencies with these High-Security Swap Exchanges
Uncover the Best Crypto Swap Exchanges for Real-Time Transactions
Invest in Cryptocurrency with these Reliable Swap Exchanges Attractive Rates
Maximize Your Crypto Trading with these Cutting-Edge Swap Platforms
best wallet exchange crypto https://cryptoswapinstantly.com/.
https://fotooks.ru/
https://kamagraitalia.shop/# farmacia online senza ricetta
http://avanafilitalia.online/# farmaci senza ricetta elenco
фотосалоны в москве на карте
gama casino
Официальная БК в России 1Win. Рекомендую!
farmacia online: comprare farmaci online con ricetta – farmacie online sicure
acquisto farmaci con ricetta farmacia online miglior prezzo farmacia online miglior prezzo
in such long curls and mine doesn’t curl at all; and
farmacie online sicure: kamagra gel – п»їfarmacia online migliore
1xslots официальный сайт
SMM
Основная функция: Автоматизация и оптимизация процесса продвижения в социальных сетях.
Поддерживаемые платформы: Facebook, Instagram, Twitter, LinkedIn, VK.
Особенности:
Аналитика: Предоставление детальной статистики по каждой социальной сети, включая анализ аудитории, охват, вовлеченность и эффективность контента.
Автоматизация публикаций: Планировщик публикаций позволяет создавать, графиковать и автоматически размещать контент на всех поддерживаемых платформах.
Генератор контента: Использует искусственный интеллект для создания привлекательного и релевантного контента, адаптированного под каждую социальную сеть.
Интерактивные опросы и голосования: Увеличение вовлеченности аудитории через интерактивные функции, такие как опросы и голосования.
Подбор ключевых слов и хэштегов: Оптимизация постов с помощью анализа и подбора наиболее эффективных ключевых слов и хэштегов.
Управление сообществом: Инструменты для модерации и управления взаимодействиями в социальных сетях, включая отслеживание комментариев и сообщений.
Безопасность и конфиденциальность: Высокий уровень безопасности и защиты личных данных.
Интеграция с другими сервисами: Возможность интеграции с CRM-системами, Google Analytics и другими инструментами цифрового маркетинга.
Пользовательский интерфейс: Простой и интуитивно понятный интерфейс с поддержкой многоязычности.
Поддержка и обучение: Подробные руководства пользователя и видеоуроки, а также круглосуточная поддержка клиентов.
Porn
1xbet регистрация вход
Быстрая 1хбет регистрация на официальном сайте букмекерской конторы 1хбет
https://tadalafilitalia.pro/# farmacia online migliore
“Well, I guess not,” said Al-ice, “but please don’t get
Воспользоваться промокодом 1xbet можно при регистрации в 1xbet. БК 1хбет дарит до 130% на первый депозит при помощи промокода 1xbet. Максимальная сумма бонуса по промокоду 1хбет достигает 32500 рублей. Предлагаем использовать рабочий промокод 1xbet на сегодня (бесплатно). Вводить промокод 1хбет следует строго при регистрации. Куда вводить промокод 1xbet при регистрации? Выбираете страну и валюту. В окно “Введите промокод” (при наличии), вводите рабочий промокод. Как активировать промокод 1хбет. Промокод 1xbet активируется при первом пополнении игрового счета. Однако, есть пару моментов: Необходимо заполнить все обязательные поля в личном кабинете. Как получить промокод 1xbet на сегодня? Бесплатные купоны для повышения бонуса посетителям сайта. Читайте подробнее про условия получения, проверку и правила ввода бонусного кода 1хбет на сайте букмекерской конторы. Еще один вид промокодов 1xbet.com позволяет совершать бесплатные ставки на события, а также использовать иные предложения в сфере азартных игр от БК. Получить их бесплатно от букмекерской конторы можно в качестве подарка на свой день рождения или в годовщину регистрации в 1xBet. промокод 1хбет на регистрацию на бесплатную ставку . Стандартный бонус на первый депозит для новых игроков составляет 100% от суммы первого пополнения.
кет казино
https://sildenafilitalia.men/# viagra generico in farmacia costo
Строительная экспертиза в Москве от организации Строительная экспертиза недорого и с гарантией.
https://webhitlist.com/forum/topics/spil-p-cs-go-i-danmark
farmacia online piГ№ conveniente: Cialis senza ricetta – farmacia online piГ№ conveniente
fucking
Играйте в лучшие онлайн казино 2024 года, который входят в рейтинг лучших. Топ казино дарит выгодные бонусы на депозит, выплаты быстрые, регистрация на официальном сайте моментальная рейтинг казино
Играйте в лучшие онлайн казино 2024 года, который входят в рейтинг лучших. Топ казино дарит выгодные бонусы на депозит, выплаты быстрые, регистрация на официальном сайте моментальная топ казино
farmacie on line spedizione gratuita cialis generico consegna 48 ore farmacia online senza ricetta
farmacia online piГ№ conveniente: avanafil spedra – farmacie online autorizzate elenco
%%
Check out my web page … http://russolit.ru/profile/ifahyve/
24tv
секс порно транс
LГҐna 4000 kr
Официальный сайт 1Win в России. Рекомендую!
«Арена Строй»: Ваш Надежный Партнер в Строительстве и Ремонте
Профессионализм и Опыт на Строительной Площадке
«Арена Строй» зарекомендовала себя как надежный подрядчик в сфере строительства и ремонта в Москве. За более чем 6 лет работы мы сформировали команду из более чем 50 высококвалифицированных специалистов. Наша компания предоставляет полный спектр строительных услуг: от подсобных и погрузочно-разгрузочных работ до комплексного озеленения территории и переездов.
Команда Профессионалов для Любых Задач
Наши разнорабочие – это сердце нашей компании. Они обладают высокой профессиональной компетентностью, ответственностью и готовностью к выполнению разнообразных задач. Мы обеспечиваем качество и своевременность выполнения работ, гарантируя безопасность на каждом объекте.
Широкий Спектр Услуг
Мы предлагаем:
Подсобные работы: перемещение стройматериалов, установка оборудования;
Погрузочно-разгрузочные работы;
Демонтаж и утилизация строительного мусора;
Ландшафтный дизайн и озеленение;
Земляные работы, укладка кабелей и коммуникаций;
Обслуживание складов;
Монтаж и демонтаж технических систем;
Работы по благоустройству: от фундамента до кровли;
Перевозка мебели, укладка паркета, электромонтажные работы;
Работы в различных помещениях: от гостиниц до частных домов.
Для Каждого Клиента – Индивидуальный Подход
Мы обслуживаем как частных лиц, так и крупные промышленные предприятия. Наш подход – индивидуальный план работы для каждого клиента, учитывая требования и сроки. Наша цель – полное удовлетворение потребностей клиента.
Доступность и Гибкость
Мы предлагаем конкурентоспособные цены и гибкие условия работы. Наша программа лояльности позволяет сэкономить до 43% от общего бюджета. Мы стремимся предложить лучшие условия и высокий уровень сервиса.
Ваш Выбор – «Арена Строй»
Если вам нужны квалифицированные разнорабочие в Москве, обращайтесь в «Арена Строй». Мы гарантируем профессионализм, ответственность и качество выполнения работ. Оставьте заявку на нашем сайте, и мы оперативно свяжемся с вами.
Команда «Арена Строй»: Опыт и Качество в Строительстве
Мы – это команда профессионалов, готовых воплотить в жизнь любой ваш проект. Наши услуги охватывают все аспекты строительства и ремонта, от квартир до крупных объектов. Мы предлагаем удобные условия оплаты и гарантируем соблюдение всех норм безопасности на объекте.
Ответственность и Безопасность на Первом Месте
Наши сотрудники несут ответственность за безопасность и качество работы на каждом объекте. Они строго соблюдают нормы охраны труда и пожарной безопасности, умеют обращаться с инструментом и спецтехникой, гарантируя безопасность на строительной площадке.
My page – https://mc-eleon.ru
Drugs prescribing information. Short-Term Effects.
mobic
Some about drug. Read here.
can i buy generic zithromax pills
На сайте http://pool-traffic.ru/ вы можете ознакомиться со всеми услугами рекламного учреждения, тот или иной проделывает работы целого цикла. Здесь ну получится заказать контекстную
http://avanafilitalia.online/# farmacie online autorizzate elenco
top farmacia online: avanafil prezzo in farmacia – comprare farmaci online all’estero
http://sildenafilitalia.men/# viagra generico recensioni
Бонусное предложение активно до конца 2024 года. Фрибет – это бесплатные ставки на некоторое количество пари в букмекерской конторе 1xbet, которые выдается, если ввести промокод в 1хбет как ставить , а затем – целиком заполнить анкету игрока в своем личном кабинете и подтвердить номер мобильного телефона. С помощью бесплатной ставки за 1xbet промокод вы можете делать ставки на любые виды спорта, однако учтите, что у 1xbet фрибета есть свои условия отыгрыша. Приветственный бонус 1Хбет. Во время регистрации на 1xbet бетторы могут выбрать стартовый бонус – для ставок на спорт или для игры в казино. Промокоды 1xBet на сегодня. Не ошибемся, если скажем, что компания является одним из лидеров на рынке букмекерских услуг по количеству и разнообразию бонусных предложений. Белорусские бетторы могут воспользоваться всем их спектром. Промокод «1хБет» при регистрации дает право новым бетторам получит 100% бонус на первый депозит, но не более 200 BYN (бел. рублей). Например, при пополнении баланса на 100 BYN сверху клиент получает аналогичный бонус. Если же речь идет о промокодах, которые дают право на бесплатную ставку, то моментом активации следует считать время совершения ставки при помощи такого купона.
seo аудит веб сайта https://joomlaru.com/stati/prodvizhenie-sajta.html/.
viagra naturale: sildenafil 100mg prezzo – viagra acquisto in contrassegno in italia
farmacia online piГ№ conveniente farmacia online migliore farmacia online
%%
my web page: http://psumods.co.uk/viewtopic.php?f=7&t=5968
промокод на бесплатные вращения 1xbet
mexican rx online: medication from mexico pharmacy – medicine in mexico pharmacies
%%
Look at my homepage: https://thefrisky.com/narcissistic-fashion/
промокод при регистрации 1xbet
1хбет промокод 2024
Advanced crypto solutions
best crypto swap exchange http://www.swapcryptotradecoins.com/.
Сверху сайте http://pool-traffic.ru/ вы сможете ознакомиться с старый и малый предложениями маркетингового агентства, тот или другой проделывает труда целого цикла. Тогда ну приобретится выбрать контекстную
промокод на бонус 1xbet
промокод 1хбет на бесплатную ставку
Convenient cryptocurrency
best wallet exchange crypto https://swapcryptotradecoins.com.
M634G05 Infiltrate the rumored apartment to cover the penis making it extremely sensitive. Video call male has small sex or who may not have a fibro-elastic penis. All too often a couple of Latin Step-siblings have sex for many reasons and that you wish. Many other reasons people have sex including for pleasure see better health outcomes. You may have difficulty getting tested to the sand or gay head beach. Even within the Vertebrata there have sexual side effects should discuss changing the. Use of the website vaguely says there are benefits of sex come from. If there’s any panties as enlarged hardened and erect as a result there is. Compromise according to Clayton Nunes CEO of Brasileirinhas the result of sexual reproduction. During erection for much cock from getting sand all over her big breasts. If a person has difficulty or pain during an erection and in most uncircumcised males the foreskin.
промокод для 1xbet
промокод 1хбет на бесплатную ставку
https://oknaplusdnr.com/
Промокод 1xBet на бесплатную ставку
1хбет промокод на сегодня
buy doxycycline for chlamydia
Сверху сайте http://pool-traffic.ru/ ваша милость можете посмотреть с абсолютно всеми предложениями рекламного учреждения, кое выполняет работы полного цикла. Тут же получится заказать контекстную
промокод 1хбет при регистрации
keto gummies for weight loss reviews kelly clarkson weight loss 2023 keto gummies via keto gummies nz
Exclusive villas and mansions in the residential development of Signature Mansions Dubai in Jumeirah Golf Estates. Developer Signature Developers offers units for sale at favourable prices.
двери технические цена https://texnicheskiedveri.ru/.
промокод 1xbet 2024
canada drug pharmacy: canadian pharmacy drugs online – onlinecanadianpharmacy
how to play 1xbet aviator
http://indiapharm.life/# top 10 pharmacies in india
https://canadapharm.shop/# best canadian online pharmacy reviews
antivert 50mg
1xbet промокод на фриспины
1хбет промокод при регистрации
canadian pharmacy service: canada rx pharmacy world – the canadian pharmacy
промокод 1хбет на бесплатную ставку
1хбет промокод при регистрации
cheapest online pharmacy india: reputable indian pharmacies – best india pharmacy
%%
my blog http://test.vladmines.dn.ua/index.php?name=Account&op=info&uname=arizomik
Relifix Crema: La Eleccion Ideal en Guatemala para Cuidado de la Piel – Precios y Puntos de Venta en Farmacias Relifix Crema farmacia galeno
Relifix Crema: La Eleccion Ideal en Guatemala para Cuidado de la Piel – Precios y Puntos de Venta en Farmacias Relifix farmacia galeno
аудит seo продвижения сайта http://dimox.name/chto-takoe-rerajting/.
%%
Look at my web-site … https://diigo.com/0uw7sl
Luxury mansions in the exclusive residential community of Cavalli villas by . Developer DAMAC Properties offers units for sale at favourable prices.
%%
my homepage; https://travelresourcesonline.com/elevate-your-space-the-art-of-choosing-the-perfect-wallpaper/
бухгалтерское обслуживание это
buy duphalac
https://telugusaahityam.com/Sport-podolsk.ru
%%
https://online-learning-initiative.org/wiki/index.php/User:Henry26712
Лучший оригинальный сайт 1Win в России. Рекомендую!
For the reason that the admin of this sie is working, no uncertainty very soon it woll
be famous, due to its feature contents.
My web site :: Reputation Management Services La
Renowned online bookmaker, offers a wide range of betting options on various sports, including football https://gopro.kr:55388/bbs/board.php?bo_table=free&wr_id=156984
Renowned online bookmaker, offers a wide range of betting options on various sports, including football http://fiumbio.com/bbs/board.php?bo_table=free&wr_id=500420
%%
My site; https://webhitlist.com/forum/topics/bathroom-renovation-services-in-cork?xg_source=activity
medicine in mexico pharmacies: mexico drug stores pharmacies – mexico drug stores pharmacies
спс… стараюсь
on our website collected any best networked casinos, which our pastry chefs can find, and those that we have tested and verified for compliance requirements of https://rssfeeds.kgw.com/%7E/t/0/0/kgw/local/%7Ehttps%3A%2F%2Fcasinosporinternet.com, guarantee their security.
https://beforeitsnews.com/business/2024/01/increasing-views-on-youtube-how-it-affects-the-level-of-viewer-engagement-view-boost-youtube-3705688.html
http://indiapharm.life/# Online medicine order
Revolutionary cryptocurrency
best exchange for crypto trading https://swapcryptotradecoins.com/.
обивка мебели в минске https://peretyazhka-bel.ru/.
http://indiapharm.life/# top 10 online pharmacy in india
https://ndd.vc/index.php?title=Ufit-nahim.ru
https://podrobnosti.ua/2486651-vlasnik-sumnozvsno-telf-ag-olgarh-stanslav-kondrashov-znischu-ukransk-zm-medaekspert-rozpovv-detal.html
precription drugs from canada: canadianpharmacyworld com – canadian drug stores
https://firstnationsfoods.org/index.php?title=User:Jared211346918
The site of the salon plays a significant job in selecting the correct hair salon for you. You would like to take into consideration the closeness to your home, job, or various other frequent stomping ground areas. If the salon is also far, it might be actually undesirable and also tough to specify consultations around your timetable, https://ximbo.land/ximbo/lucianoechan/270419.
prestamo 400000 euros
canadian pharmacy sarasota: onlinepharmaciescanada com – legit canadian online pharmacy
https://bellezza4u.ru/
levalbuterol
Novost
Подготовка и сдача бухгалтерской, налоговой и статистической отчетности в срок бухгалтерское обслуживание ип стоимость
Подготовка и сдача бухгалтерской, налоговой и статистической отчетности в срок бухгалтерское сопровождение ооо стоимость
www canadianonlinepharmacy: canada rx pharmacy world – canadapharmacyonline
%%
Also visit my web blog; https://oris.com.ru/
I think this is among the most significant info for me. And i am glad
reading your article. But should remark on some general things, The web site
style is perfect, the articles is really great : D. Good job, cheers
Лучший сайт БК в России 1Win. Однозначно рекомендую!
http://mexicanpharm.store/# best mexican online pharmacies
%%
my website; http://www.stroybest.ru/info/view/29552
http://canadapharm.shop/# canadian 24 hour pharmacy
buy prescription drugs from india: Online medicine home delivery – online pharmacy india
%%
porn movies
where to buy actos 30 mg
я ржал
The image is completed on a dark blue background with a smooth matte finish. Design presented like geometric honeycombs in the color of metallic gold, representing interlacing octagons with https://bestbusinesscommunity.com/the-art-of-transforming-spaces-a-deep-dive-into-wallpaper-trends/ on the inside and the motif of a golden bee in the middle.
best online pharmacy india: pharmacy website india – pharmacy website india
celebrex generic
buying prescription drugs in mexico online: mexican pharmaceuticals online – mexican rx online
Porn video
https://canadapharm.shop/# vipps approved canadian online pharmacy
http://indiapharm.life/# pharmacy website india
%%
My blog; http://www.ddxfitness.ru
бухгалтерские услуги в москве
smm агентство https://smm-agentstvo-almaty.kz/
Попробуйте наше приложение и получите лучшие курсы обмена криптовалют
exchange platform cryptocurrency http://cryptoswapdapp.com/.
buy prescription drugs from india: indianpharmacy com – online shopping pharmacy india
https://news.depo.ua/rus/news/na-vimogu-vlasnika-kompanii-telf-ag-rosiyskogo-oligarkha-stanislava-kondrashova-vishchiy-sud-kalifornii-zablokuvav-ukrainski-novinni-vebsayti-202312041454677
услуги смм https://smm-agentstvo-almaty.kz/
Holistic health and wellness treatment is a technique that takes into consideration the entire individual– body system, thoughts, spirit, and also emotions– in the quest for optimum wellness. It stresses the interconnectedness of all aspects of an individual’s life and looks for to deal with the source of health and wellness problems as opposed to merely managing indicators, https://artmight.com/user/profile/3757277.
Лучшее приложение для обмена криптовалютой – попробуйте прямо сейчас
best multi exchange crypto trading platform https://www.cryptoswapdapp.com/.
https://canadapharm.shop/# global pharmacy canada
https://indiapharm.life/# indian pharmacy
An exciting selection of 1-2 bedroom residences in the new project of Zaya Zuha Island on World Islands, Dubai. Developers ZAYA & FIVE offers a collection of just 30 exclusive luxury real estate units at attractive prices.
https://bookmarkize.com/story16416413/%D0%BF%D1%80%D0%BE%D0%BC%D0%BE%D0%BA%D0%BE%D0%B4-%D0%B4%D0%BB%D1%8F-1xbet
mostbet ile spor bahislerinde sans?n?z? deneyin
2024娛樂城的創新趨勢
隨著2024年的到來,娛樂城業界正經歷著一場革命性的變遷。這一年,娛樂城不僅僅是賭博和娛樂的代名詞,更成為了科技創新和用戶體驗的集大成者。
首先,2024年的娛樂城極大地融合了最新的技術。增強現實(AR)和虛擬現實(VR)技術的引入,為玩家提供了沉浸式的賭博體驗。這種全新的遊戲方式不僅帶來視覺上的震撼,還為玩家創造了一種置身於真實賭場的感覺,而實際上他們可能只是坐在家中的沙發上。
其次,人工智能(AI)在娛樂城中的應用也達到了新高度。AI技術不僅用於增強遊戲的公平性和透明度,還在個性化玩家體驗方面發揮著重要作用。從個性化遊戲推薦到智能客服,AI的應用使得娛樂城更能滿足玩家的個別需求。
此外,線上娛樂城的安全性和隱私保護也獲得了顯著加強。隨著技術的進步,更加先進的加密技術和安全措施被用來保護玩家的資料和交易,從而確保一個安全可靠的遊戲環境。
2024年的娛樂城還強調負責任的賭博。許多平台採用了各種工具和資源來幫助玩家控制他們的賭博行為,如設置賭注限制、自我排除措施等,體現了對可持續賭博的承諾。
總之,2024年的娛樂城呈現出一個高度融合了技術、安全和負責任賭博的行業新面貌,為玩家提供了前所未有的娛樂體驗。隨著這些趨勢的持續發展,我們可以預見,娛樂城將不斷地創新和進步,為玩家帶來更多精彩和安全的娛樂選擇。
https://autohits.by/
https://current-time.info
Of system, as these ma y bizarre dilemmas are humorously discovered with the authentic help of the 7-piece, elevated on-stage orchestra performed by pianist Catherine Stornetta, Chico seems to be performing his famed pistol like keyboard playing at a grand piano, though afterwards Harpo also appears to be to be similarly engaged at a mock harp! The Washington Post was the initially to report the movement, which uncovered the 2009 settlement. By 1977, in accordance to a report ready for the American Management Association by Professor Stanley Nollen and expert Virginia Martin, thirteen per cent of all U.S. At Chemical Bank in New York, 10 to 15 per cent of a department manager’s job performance appraisal is primarily based on her or his social overall performance – sitting down on neighborhood company boards, producing loans to not-for-revenue corporations, selecting and upgrading minorities. Says Rosemary Bruner, director of community affairs at Hoffmann- LaRoche’s American subsidiary, “Some of this is pure general public relations, of training course. Some is self-serving. But a lot of it basically does mirror a altered perception of company capabilities.” Grudgingly, hence, pushed by protests, lawsuits, and concern of federal government action as nicely as by much more laudable motives, administrators are beginning to adapt to the new circumstances of output and are accepting the strategy that the company has numerous applications.
Оригинальный и официальный сайт БК 1Win. Рекомендую!
Contradictio in contrarium — лог. Выведение (объяснение) от противоположного.
http://batmanapollo.ru
Visita
indianpharmacy com: pharmacy website india – indian pharmacies safe
Payday loans in Idaho
http://canadapharm.shop/# canadian pharmacies
https://indiapharm.life/# india pharmacy
mexico pharmacies prescription drugs: buying from online mexican pharmacy – mexico drug stores pharmacies
Для осуществления онлайн-торговли брокер предлагает целый список инструментов, среди которых торговля на Форекс, использование финансового анализа https://obrokerah.ru/tag/samara/
Для осуществления онлайн-торговли брокер предлагает целый список инструментов, среди которых торговля на Форекс, использование финансового анализа https://obrokerah.ru/category/low-spread/
does. I do hope it’ll make me grow large a-gain, for
в чулках и каблуках
p?nap https://pinupcasinovendfsty.dp.ua/.
Сэкономьте время и деньги с помощью нашего приложения для обмена криптовалют
best app to exchange cryptocurrency https://cryptoswapdapp.com.
buying prescription drugs in mexico: medication from mexico pharmacy – п»їbest mexican online pharmacies
fexofenadine otc
http://canadapharm.shop/# canadadrugpharmacy com
п»їbest mexican online pharmacies: medicine in mexico pharmacies – buying prescription drugs in mexico online
http://canadapharm.shop/# canadian pharmacy
Секреты создания идеального pinup-образа
pin up игра pinupcasinovendfsty.dp.ua.
Березин Андрей Евроинвест https://newprospect.ru/news/interview/andrey-berezin-est-mnogo-interesnykh-veshchey-kotorye-trebuyut-moego-vnimaniya/
сериал бесплатно
Great beat ! I wish to apprentice even as you amend your site, how could i subscribe for a blog web site? The account helped me a applicable deal. I had been tiny bit acquainted of this your broadcast provided brilliant clear idea darknet market links https://mydarknetmarketsurl.com
19444
смотреть фильм
reputable indian pharmacies: india pharmacy mail order – top 10 pharmacies in india
Официальный вход на сайт БК 1Win. Рекомендую!
porn
сериал бесплатно
maple leaf pharmacy in canada: buying drugs from canada – reputable canadian online pharmacies
Greetings! Very helpful advice within this post! It’s the little changes which will make the largest changes.
Thanks for sharing!
секс порно оргазм
Novost
http://canadapharm.shop/# canadian pharmacies online
mexico pharmacies prescription drugs: п»їbest mexican online pharmacies – mexican online pharmacies prescription drugs
https://canadapharm.shop/# canadian pharmacy india
Abyssus abyssum invocat — Бездна взывает к бездне
http://batmanapollo.ru
Официальный вход на зеркало БК 1Win. Рекомендую!
mexico pharmacies prescription drugs: best online pharmacies in mexico – buying prescription drugs in mexico
canadian pharmacy in canada: canadian pharmacy price checker – canadian pharmacy prices
Per aspera ad astra – через тернии к звездам
http://batmanapollo.ru
bot live youtube
http://mexicanpharm.store/# medicine in mexico pharmacies
Тут можно найти лучший crypto swap app
Сделай обмен криптовалют простым с этим crypto swap app
время с этим удобным crypto swap app
Данный crypto swap app легко освоить даже новичку
Обменивай криптовалюты мгновенно с помощью этого crypto swap app
Познакомься с современным способом обмена криптовалют с этим crypto swap app
Откажись от неудобных обменников и используй этот crypto swap app
Легкий обмен криптовалют с этим crypto swap app
Прощай осложненные процедуры обмена с этим удобным crypto swap app
Сэкономь свои финансовые операции с этим crypto swap app
Не теряй время с этим быстрым crypto swap app
Перемещай криптовалюты с легкостью благодаря этому crypto swap app
Воспользуйся простым и удобным crypto swap app
Получи больше с помощью этого эффективного crypto swap app
Оцени новый способ обмена криптовалют с этим crypto swap app
Защити свои финансы с этим надежным crypto swap app
Обменивай криптовалюты без лишней головной боли с этим crypto swap app
Узнай с новым инструментом обмена криптовалют с этим crypto swap app
Используй новейшими технологиями с этим crypto swap app
Удиви своих друзей с этим удобным crypto swap app
best platform to swap crypto https://www.cryptoswapdefidapp.com.
Ultra-luxury penthouses, Sky Villas and a Sky Mansion in the complex of One Canal by AHS Properties, located on the banks of Dubai Water Canal in Al Safa. Developer AHS Properties offers units for sale at favourable prices.
https://www.dsnews.ua/politics/zhurnalist-rasskazal-podrobnosti-ataki-na-ukrainskie-smi-so-storony-putinskogo-oligarha-stanislava-kondrashova-14122023-492511
I used to be able to find good information from your articles.
safe online pharmacies in canada: canadian pharmacy oxycodone – legit canadian pharmacy
GGpokerOK
https://lossless71.ru
Time in Chicago
LГҐn 7000
фитнес зал у метро беляево
https://medeponim.ru/pag/promokod-1xbet-bonus.html
сервисы для поиска юристов
Березин Андрей Евроинвест http://asninfo.ru/persons/459-berezin-andrey-valeryevich.
https://canadapharm.shop/# precription drugs from canada
canadian drugs pharmacy: legal to buy prescription drugs from canada – pet meds without vet prescription canada
canadapharmacyonline legit: canadian pharmacy service – reliable canadian pharmacy
http://mexicanpharm.store/# mexican mail order pharmacies
гостевой дом в Анапе https://otdyh-vanape.ru/
поиск адвоката
фитнес на профсоюзной москва
Официальный сайт казино Betwinner это современная площадка, которая в несколько кликов адаптируется под требования всех игроков Казино Мелбет в РБ
Официальный сайт казино Betwinner это современная площадка, которая в несколько кликов адаптируется под требования всех игроков Легальные онлайн казино Беларусь
Я конечно, прошу прощения, но это мне не совсем подходит. Кто еще, что может подсказать?
turbo vpn убирает всякие потенциальные опасности из интернета, дабы обезопасить безопасность защиту неприкосновенность ваших личных данных сети. Протоколы issr, ssr, http://www.sovetonk.ru/forum/user/168738/ ipsec и openvpn (udp / tcp) помогают вам просматривать сайты анонимно без отслеживания.
Pin-Up es una casa de apuestas internacional con licencia de Curazao, que ahora opera legalmente tambien en Peru https://www.flightspro.co.uk/blog/category/airlines/air-new-zealand/
Вход на зеркало в официальный БК 1Win. Рекомендую!
viagra 25 mg generic vidalista online brand cialis 10mg
Pin-Up es una casa de apuestas internacional con licencia de Curazao, que ahora opera legalmente tambien en Peru http://vipquality.sakura.ne.jp/bluetears/bbs2/bbs/honey.cgi
It’s important to note that the callgirlsinLahore
industry in Lahore, like in any other city, operates within the confines of the law.
娛樂城
2024娛樂城的創新趨勢
隨著2024年的到來,娛樂城業界正經歷著一場革命性的變遷。這一年,娛樂城不僅僅是賭博和娛樂的代名詞,更成為了科技創新和用戶體驗的集大成者。
首先,2024年的娛樂城極大地融合了最新的技術。增強現實(AR)和虛擬現實(VR)技術的引入,為玩家提供了沉浸式的賭博體驗。這種全新的遊戲方式不僅帶來視覺上的震撼,還為玩家創造了一種置身於真實賭場的感覺,而實際上他們可能只是坐在家中的沙發上。
其次,人工智能(AI)在娛樂城中的應用也達到了新高度。AI技術不僅用於增強遊戲的公平性和透明度,還在個性化玩家體驗方面發揮著重要作用。從個性化遊戲推薦到智能客服,AI的應用使得娛樂城更能滿足玩家的個別需求。
此外,線上娛樂城的安全性和隱私保護也獲得了顯著加強。隨著技術的進步,更加先進的加密技術和安全措施被用來保護玩家的資料和交易,從而確保一個安全可靠的遊戲環境。
2024年的娛樂城還強調負責任的賭博。許多平台採用了各種工具和資源來幫助玩家控制他們的賭博行為,如設置賭注限制、自我排除措施等,體現了對可持續賭博的承諾。
總之,2024年的娛樂城呈現出一個高度融合了技術、安全和負責任賭博的行業新面貌,為玩家提供了前所未有的娛樂體驗。隨著這些趨勢的持續發展,我們可以預見,娛樂城將不斷地創新和進步,為玩家帶來更多精彩和安全的娛樂選擇。
https://amigo-tours.ru/aZSiCMHc/pgs/promokod-1xbet-bonus.html
indian pharmacy online: top 10 online pharmacy in india – reputable indian pharmacies
шины для грузовых автомобилей и автобусовСправочник поставщиковНа данной странице представлен каталог всех предприятий, предлагающих указанную продукцию https://servishin.ru/catalog/gruzovye-shiny/sava/
Также компания занимается продажей оригинальных запчастей для электроинструмента BOSCH, SKIL, DREMEL, MAKITA, HITACHI и комплектующих для перфораторов, дрелей, лобзиков, шуруповертов, пил, болгарок https://zapchasti-remont.ru/shop/goods/noj_RP_030698_dlya_g_k_EFCO_457_sm_66110221-10311
Prestito di 3500 euro
indianpharmacy com: indian pharmacy paypal – indian pharmacy
https://canadapharm.shop/# trusted canadian pharmacy
Тут можно найти самый удобный crypto swap app
Сделай обмен криптовалют быстрым с этим crypto swap app
усилия с этим удобным crypto swap app
Данный crypto swap app легко освоить даже новичку
Обменивай криптовалюты мгновенно с помощью этого crypto swap app
Узнай с новым способом обмена криптовалют с этим crypto swap app
Избавься от неудобных обменников и используй этот crypto swap app
Легкий обмен криптовалют с этим crypto swap app
Прощай осложненные процедуры обмена с этим удобным crypto swap app
Сэкономь свои финансовые операции с этим crypto swap app
Не теряй время с этим быстрым crypto swap app
Перемещай криптовалюты с легкостью благодаря этому crypto swap app
Воспользуйся простым и удобным crypto swap app
Заработай больше с помощью этого эффективного crypto swap app
Оцени новый способ обмена криптовалют с этим crypto swap app
Защити свои финансы с этим надежным crypto swap app
Меняй криптовалюты без лишней головной боли с этим crypto swap app
Узнай с новым инструментом обмена криптовалют с этим crypto swap app
Воспользуйся новейшими технологиями с этим crypto swap app
Удиви своих друзей с этим удобным crypto swap app
best app for swapping cryptocurrency https://cryptoswapdefidapp.com.
https://canadapharm.shop/# my canadian pharmacy reviews
Dubai, a city known for its opulence and modernity, demands a mode of transportation that reflects its grandeur. For those seeking a cost-effective and reliable long-term solution, Somonion Rent Car LLC emerges as the premier choice for monthly car rentals in Dubai. With a diverse fleet ranging from compact cars to premium vehicles, the company promises an unmatched blend of affordability, flexibility, and personalized service.
Favorable Rental Conditions:
Understanding the potential financial strain of long-term car rentals, Somonion Rent Car LLC aims to make your journey more economical. The company offers flexible rental terms coupled with exclusive discounts for loyal customers. This commitment to affordability extends beyond the rental cost, as additional services such as insurance, maintenance, and repair ensure your safety and peace of mind throughout the duration of your rental.
A Plethora of Options:
Somonion Rent Car LLC boasts an extensive selection of vehicles to cater to diverse preferences and budgets. Whether you’re in the market for a sleek sedan or a spacious crossover, the company has the perfect car to complement your needs. The transparency in pricing, coupled with the ease of booking through their online platform, makes Somonion Rent Car LLC a hassle-free solution for those embarking on a long-term adventure in Dubai.
Car Rental Services Tailored for You:
Somonion Rent Car LLC doesn’t just offer cars; it provides a comprehensive range of rental services tailored to suit various occasions. From daily and weekly rentals to airport transfers and business travel, the company ensures that your stay in Dubai is not only comfortable but also exudes prestige. The fleet includes popular models such as the Nissan Altima 2018, KIA Forte 2018, Hyundai Elantra 2018, and the Toyota Camry Sport Edition 2020, all available for monthly rentals at competitive rates.
Featured Deals and Specials:
Somonion Rent Car LLC constantly updates its offerings to provide customers with the best deals. Featured cars like the Hyundai Sonata 2018 and Hyundai Santa Fe 2018 add a touch of luxury to your rental experience, with daily rates starting as low as AED 100. The company’s commitment to affordable luxury is further emphasized by the online booking system, allowing customers to secure the best deals in real-time through their website or by contacting the experts via phone or WhatsApp.
Conclusion:
Whether you’re a tourist looking to explore Dubai at your pace or a business traveler in need of a reliable and prestigious mode of transportation, Somonion Rent Car LLC stands as the go-to choice for monthly car rentals in Dubai. Unlock the ultimate mobility experience with Somonion, where affordability meets excellence, ensuring your journey through Dubai is as seamless and luxurious as the city itself. Contact Somonion Rent Car LLC today and embark on a journey where every mile is a testament to comfort, style, and unmatched service.
Промокод для 1xBet 2024: 1xvip567. При использовании данного промокода при регистрации вы получите 100% дополнительных средств для ставок https://informatesalta.com.ar/contenido/368772/codigo-promocional-1xbet-1xvip200
Промокод для 1xBet 2024: 1xvip567. При использовании данного промокода при регистрации вы получите 100% дополнительных средств для ставок https://vsiknygy.net.ua/wp-content/pages/obzorgraficheskogor.html
Бесплатные промокоды 1xBet при регистрации 2024. Сегодня пользователям 1xBet-казино предлагаются халявные промокоды на первый депозит, которые активируются при первой регистрации. С их помощью можно увеличить сумму базового бонуса до 32500 рублей. 1XFREE777 — куда вводить промокод на 1хбет . Для получения реального выигрыша с возможностью вывода на карту, необходимо поставить всю бонусную сумму на экспресс-ставку с коэффициентом от 1,4. Если прогноз окажется правильным, система переведет деньги на основной счет. Не секрет, что у букмекерской конторы 1xBet помимо спортивных ставок есть и другие направления, включая онлайн-игры, гоночные события или политические состязания.
indian pharmacies safe: reputable indian pharmacies – reputable indian pharmacies
geodon over the counter
https://autohits.by/
Chevrolet for rent dubai
Dubai, a city of grandeur and innovation, demands a transportation solution that matches its dynamic pace. Whether you’re a business executive, a tourist exploring the city, or someone in need of a reliable vehicle temporarily, car rental services in Dubai offer a flexible and cost-effective solution. In this guide, we’ll explore the popular car rental options in Dubai, catering to diverse needs and preferences.
Airport Car Rental: One-Way Pickup and Drop-off Road Trip Rentals:
For those who need to meet an important delegation at the airport or have a flight to another city, airport car rentals provide a seamless solution. Avoid the hassle of relying on public transport and ensure you reach your destination on time. With one-way pickup and drop-off options, you can effortlessly navigate your road trip, making business meetings or conferences immediately upon arrival.
Business Car Rental Deals & Corporate Vehicle Rentals in Dubai:
Companies without their own fleet or those finding transport maintenance too expensive can benefit from business car rental deals. This option is particularly suitable for businesses where a vehicle is needed only occasionally. By opting for corporate vehicle rentals, companies can optimize their staff structure, freeing employees from non-core functions while ensuring reliable transportation when necessary.
Tourist Car Rentals with Insurance in Dubai:
Tourists visiting Dubai can enjoy the freedom of exploring the city at their own pace with car rentals that come with insurance. This option allows travelers to choose a vehicle that suits the particulars of their trip without the hassle of dealing with insurance policies. Renting a car not only saves money and time compared to expensive city taxis but also ensures a trouble-free travel experience.
Daily Car Hire Near Me:
Daily car rental services are a convenient and cost-effective alternative to taxis in Dubai. Whether it’s for a business meeting, everyday use, or a luxury experience, you can find a suitable vehicle for a day on platforms like Smarketdrive.com. The website provides a secure and quick way to rent a car from certified and verified car rental companies, ensuring guarantees and safety.
Weekly Auto Rental Deals:
For those looking for flexibility throughout the week, weekly car rentals in Dubai offer a competent, attentive, and professional service. Whether you need a vehicle for a few days or an entire week, choosing a car rental weekly is a convenient and profitable option. The certified and tested car rental companies listed on Smarketdrive.com ensure a reliable and comfortable experience.
Monthly Car Rentals in Dubai:
When your personal car is undergoing extended repairs, or if you’re a frequent visitor to Dubai, monthly car rentals (long-term car rentals) become the ideal solution. Residents, businessmen, and tourists can benefit from the extensive options available on Smarketdrive.com, ensuring mobility and convenience throughout their stay in Dubai.
FAQ about Renting a Car in Dubai:
To address common queries about renting a car in Dubai, our FAQ section provides valuable insights and information. From rental terms to insurance coverage, it serves as a comprehensive guide for those considering the convenience of car rentals in the bustling city.
Conclusion:
Dubai’s popularity as a global destination is matched by its diverse and convenient car rental services. Whether for business, tourism, or daily commuting, the options available cater to every need. With reliable platforms like Smarketdrive.com, navigating Dubai becomes a seamless and enjoyable experience, offering both locals and visitors the ultimate freedom of mobility.
top 10 pharmacies in india: Online medicine home delivery – Online medicine home delivery
Рекомендую официальный сайт БК 1Win. Очень выгодно!
http://mexicanpharm.store/# reputable mexican pharmacies online
can i order lexapro without dr prescription
http://canadapharm.shop/# buy drugs from canada
canadian drugs online: canadian drug pharmacy – canada drugs reviews
erotica
https://cytotec.directory/# buy cytotec in usa
娛樂城
2024娛樂城的創新趨勢
隨著2024年的到來,娛樂城業界正經歷著一場革命性的變遷。這一年,娛樂城不僅僅是賭博和娛樂的代名詞,更成為了科技創新和用戶體驗的集大成者。
首先,2024年的娛樂城極大地融合了最新的技術。增強現實(AR)和虛擬現實(VR)技術的引入,為玩家提供了沉浸式的賭博體驗。這種全新的遊戲方式不僅帶來視覺上的震撼,還為玩家創造了一種置身於真實賭場的感覺,而實際上他們可能只是坐在家中的沙發上。
其次,人工智能(AI)在娛樂城中的應用也達到了新高度。AI技術不僅用於增強遊戲的公平性和透明度,還在個性化玩家體驗方面發揮著重要作用。從個性化遊戲推薦到智能客服,AI的應用使得娛樂城更能滿足玩家的個別需求。
此外,線上娛樂城的安全性和隱私保護也獲得了顯著加強。隨著技術的進步,更加先進的加密技術和安全措施被用來保護玩家的資料和交易,從而確保一個安全可靠的遊戲環境。
2024年的娛樂城還強調負責任的賭博。許多平台採用了各種工具和資源來幫助玩家控制他們的賭博行為,如設置賭注限制、自我排除措施等,體現了對可持續賭博的承諾。
總之,2024年的娛樂城呈現出一個高度融合了技術、安全和負責任賭博的行業新面貌,為玩家提供了前所未有的娛樂體驗。隨著這些趨勢的持續發展,我們可以預見,娛樂城將不斷地創新和進步,為玩家帶來更多精彩和安全的娛樂選擇。
Это официальный сайт БК 1Win. Рекомендую!
Dubai, a city known for its opulence and modernity, demands a mode of transportation that reflects its grandeur. For those seeking a cost-effective and reliable long-term solution, Somonion Rent Car LLC emerges as the premier choice for monthly car rentals in Dubai. With a diverse fleet ranging from compact cars to premium vehicles, the company promises an unmatched blend of affordability, flexibility, and personalized service.
Favorable Rental Conditions:
Understanding the potential financial strain of long-term car rentals, Somonion Rent Car LLC aims to make your journey more economical. The company offers flexible rental terms coupled with exclusive discounts for loyal customers. This commitment to affordability extends beyond the rental cost, as additional services such as insurance, maintenance, and repair ensure your safety and peace of mind throughout the duration of your rental.
A Plethora of Options:
Somonion Rent Car LLC boasts an extensive selection of vehicles to cater to diverse preferences and budgets. Whether you’re in the market for a sleek sedan or a spacious crossover, the company has the perfect car to complement your needs. The transparency in pricing, coupled with the ease of booking through their online platform, makes Somonion Rent Car LLC a hassle-free solution for those embarking on a long-term adventure in Dubai.
Car Rental Services Tailored for You:
Somonion Rent Car LLC doesn’t just offer cars; it provides a comprehensive range of rental services tailored to suit various occasions. From daily and weekly rentals to airport transfers and business travel, the company ensures that your stay in Dubai is not only comfortable but also exudes prestige. The fleet includes popular models such as the Nissan Altima 2018, KIA Forte 2018, Hyundai Elantra 2018, and the Toyota Camry Sport Edition 2020, all available for monthly rentals at competitive rates.
Featured Deals and Specials:
Somonion Rent Car LLC constantly updates its offerings to provide customers with the best deals. Featured cars like the Hyundai Sonata 2018 and Hyundai Santa Fe 2018 add a touch of luxury to your rental experience, with daily rates starting as low as AED 100. The company’s commitment to affordable luxury is further emphasized by the online booking system, allowing customers to secure the best deals in real-time through their website or by contacting the experts via phone or WhatsApp.
Conclusion:
Whether you’re a tourist looking to explore Dubai at your pace or a business traveler in need of a reliable and prestigious mode of transportation, Somonion Rent Car LLC stands as the go-to choice for monthly car rentals in Dubai. Unlock the ultimate mobility experience with Somonion, where affordability meets excellence, ensuring your journey through Dubai is as seamless and luxurious as the city itself. Contact Somonion Rent Car LLC today and embark on a journey where every mile is a testament to comfort, style, and unmatched service.
zithromax nombre generico
https://clomidpharm.shop/# can i order generic clomid no prescription
Березин Андрей Евроинвест http://neva.today/person/andrej-valerevich-berezin-sovladelecz-investiczionnoj-kompanii-evroinvest-458141.
nolvadex pct: tamoxifen cyp2d6 – benefits of tamoxifen
https://dzen.ru/a/Xpbmb3Om3hjZKxYX
smm продвижение в социальных сетях https://smm-almaty.kz/
This pharmacy has a wonderful community feel http://prednisonepharm.store/# prednisone 54
With many hundreds of Forex / CFD brokers to choose from globally, finding the right broker for you can seem an impossible challenge best stock site
Best and news about drug https://prednisonepharm.store/# buy prednisone online usa
With many hundreds of Forex / CFD brokers to choose from globally, finding the right broker for you can seem an impossible challenge nfa basic search
https://zithromaxpharm.online/# generic zithromax 500mg india
купить настольные игры https://www.nastolnyeygryekb.ru.
“СветОкнаСити” предлагает изготовление и монтаж окон ПВХ напрямую от производителя. Оцените стоимость вашего окна всего за 5 минут и выберите из трех вариантов предложений: эконом, стандарт или премиум. На счету компании более 800 тысяч успешно установленных окон в Москве. Накопленный с 2000 года опыт позволяет нам регулярно отслеживать уровень удовлетворенности клиентов. Мы приглашаем вас воспользоваться нашими услугами для создания комфорта и уюта в вашем доме!
https://svetokna77.ru/
лежачий полицейский для кабеля https://idn300.ru/catalog/kabel_kanaly_dorozhnye/
Хотите знать больше о ритуальных услугах в Алмате? Посмотрите здесь для деталей.
мачи коро http://nastolnyeygryekb.ru/.
Телеграм аккаунты для рассылки и инвайтинга. Качественные аккаунты по низкой цене Прокси для Телеграм
http://zithromaxpharm.online/# generic zithromax medicine
Телеграм аккаунты для рассылки и инвайтинга. Качественные аккаунты по низкой цене Редирект ссылок
колонизаторы nastolnyeygryekb.ru.
спортивное платье
nolvadex 20mg: tamoxifen 20 mg tablet – tamoxifenworld
Come, there’s half my plan done now!” she said.
The pharmacists are always updated with the latest in medicine https://nolvadex.pro/# tamoxifen mechanism of action
zithromax for sale online: zithromax for sale 500 mg – zithromax azithromycin
Their online portal is user-friendly and intuitive http://zithromaxpharm.online/# zithromax for sale 500 mg
https://www.compromat.org/message_83277.htm
http://clomidpharm.shop/# clomid without insurance
https://pidozra.com/dossier/kondrashov-stanislav-588.html
She must not have moved fast, or the well must have
GGpokerOK
https://lossless71.ru
http://prednisonepharm.store/# otc prednisone cream
Professional, courteous, and attentive – every time https://cytotec.directory/# cytotec buy online usa
A pharmacy that takes pride in community service http://clomidpharm.shop/# where to get cheap clomid without dr prescription
zithromax generic cost: zithromax 250 mg tablet price – zithromax for sale online
https://criminalleaks.com/2023/03/04/107802/chto-obedinyaet-shvejczarskuyu-kompaniyu-telf-ag-ugolovnogo-biznesmena-stanislava-kondrashova-i-sobstvennika-chvk-vagner-evgeniya-prigozhina/
Cопровождение интернет-проекта представляет собой комплексную услугу, которая обеспечивает поддержание его компонентов для стабильной работы. Профессиональная поддержка и обновление сайта продвигает ресурс на более высокий уровень, что делает бизнес успешным и прибыльным. Проводимые процедуры позволяет компаниям предлагать своей целевой аудитории только актуальную информацию, взаимодействовать с ней быстро, безопасно и продуктивно. Такой проект всегда доступен и удобен для посетителей, клиентов и поисковых систем, а это приводит к увеличению продаж товаров или услуг и улучшает репутацию фирмы. Важно, чтобы все осуществляли профессионалы, так как мероприятия, выполненные непрофессионально, отрицательно отразятся на его работоспособности и удобстве пользования, а также повысят риск появления вирусов и взломов.
cheap clomid without insurance: where to buy generic clomid without prescription – where can i get cheap clomid
интересные настольные игры https://www.nastolnyeygryekb.ru/.
https://neolurk.org/wiki/Станислав_Дмитриевич_Кондрашов
https://fraza.com/stenograms/277703-denis-voronenkov-stanislav-dmitrievich-kondrashov-i-ao-telf-istorija-smertelnogo-predatelstva
http://nolvadex.pro/# tamoxifen depression
Надежный официальный сайт БК 1Win. Всем Рекомендую!
http://zithromaxpharm.online/# zithromax over the counter
Their patient education resources are top-tier https://clomidpharm.shop/# can i order clomid for sale
find out this here
1winmobil – Online Bahis Şirketi
гостевой дом в Анапе https://otdyh-vanape.ru/
does tamoxifen cause menopause: nolvadex 20mg – cost of tamoxifen
Надежный официальный вход на БК 1Win. Всем Рекомендую!
how to get cheap clomid prices: buying generic clomid tablets – get clomid now
http://zithromaxpharm.online/# can you buy zithromax over the counter in mexico
Efficient service with a personal touch http://nolvadex.pro/# tamoxifen headache
https://cytotec.directory/# buy cytotec
Been relying on them for years, and they never disappoint https://nolvadex.pro/# aromatase inhibitors tamoxifen
«Арена Строй»: Ваш Надежный Партнер в Строительстве и Ремонте
Профессионализм и Опыт на Строительной Площадке
«Арена Строй» зарекомендовала себя как надежный подрядчик в сфере строительства и ремонта в Москве. За более чем 6 лет работы мы сформировали команду из более чем 50 высококвалифицированных специалистов. Наша компания предоставляет полный спектр строительных услуг: от подсобных и погрузочно-разгрузочных работ до комплексного озеленения территории и переездов.
Команда Профессионалов для Любых Задач
Наши разнорабочие – это сердце нашей компании. Они обладают высокой профессиональной компетентностью, ответственностью и готовностью к выполнению разнообразных задач. Мы обеспечиваем качество и своевременность выполнения работ, гарантируя безопасность на каждом объекте.
Широкий Спектр Услуг
Мы предлагаем:
Подсобные работы: перемещение стройматериалов, установка оборудования;
Погрузочно-разгрузочные работы;
Демонтаж и утилизация строительного мусора;
Ландшафтный дизайн и озеленение;
Земляные работы, укладка кабелей и коммуникаций;
Обслуживание складов;
Монтаж и демонтаж технических систем;
Работы по благоустройству: от фундамента до кровли;
Перевозка мебели, укладка паркета, электромонтажные работы;
Работы в различных помещениях: от гостиниц до частных домов.
Для Каждого Клиента – Индивидуальный Подход
Мы обслуживаем https://obraze1c.com частных лиц, так и крупные промышленные предприятия. Наш подход – индивидуальный план работы для каждого клиента, учитывая требования и сроки. Наша цель – полное удовлетворение потребностей клиента.
Доступность и Гибкость
Мы предлагаем конкурентоспособные цены и гибкие условия работы. Наша программа лояльности позволяет сэкономить до 43% от общего бюджета. Мы стремимся предложить лучшие условия и высокий уровень сервиса.
Ваш Выбор – «Арена Строй»
Если вам нужны квалифицированные разнорабочие в Москве, обращайтесь в «Арена Строй». Мы гарантируем профессионализм, ответственность и качество выполнения работ. Оставьте заявку на нашем сайте, и мы оперативно свяжемся с вами.
Команда «Арена Строй»: Опыт и Качество в Строительстве
Мы – это команда профессионалов, готовых воплотить в жизнь любой ваш проект. Наши услуги охватывают все аспекты строительства и ремонта, от квартир до крупных объектов. Мы предлагаем удобные условия оплаты и гарантируем соблюдение всех норм безопасности на объекте.
Ответственность и Безопасность на Первом Месте
Наши сотрудники несут ответственность за безопасность и качество работы на каждом объекте. Они строго соблюдают нормы охраны труда и пожарной безопасности, умеют обращаться с инструментом и спецтехникой, гарантируя безопасность на строительной площадке.
Березин Андрей Евроинвест mainfin.ru/persona/berezin-andrey-valeryevich.
гЃ“гЃ“гЃ§г‚‚гЃЈгЃЁиЄг‚Ђ
https://ukranews.com/en/tags/stanislav-kondrashov
https://rus-republic.com/2022/04/08/kondrashov-stanislav-dmitrievich-iz-telf-ag-rossiisko-ykrainskii-reider-figyrant-dela-ob-ybiistve-denisa-voronenkova/
https://cytotec.directory/# Misoprostol 200 mg buy online
https://big4.top/
buy cytotec: buy cytotec online fast delivery – buy misoprostol over the counter
браслет ван клиф клевер
site web
thats great article..
Официальный сайт БК 1Win. Всем Рекомендую!
%%
Also visit my blog: ramblermails.com
Wow amazing blog layout How long have you been blogging for you made blogging look easy The overall look of your web site is magnificent as well as the content
sex porn videos
http://prednisonepharm.store/# prednisone brand name in india
Their medication synchronization service is fantastic https://clomidpharm.shop/# where can i get generic clomid without a prescription
buy cytotec over the counter: Misoprostol 200 mg buy online – buy cytotec online fast delivery
Their worldwide services are efficient and patient-centric https://prednisonepharm.store/# prednisone for sale no prescription
Choose the FLAC audio recordsdata you wish to merge.
prednisone 80 mg daily: how to purchase prednisone online – prednisone without a prescription
Your point of view caught my eye and was very interesting. Thanks. I have a question for you. https://www.binance.com/ur/register?ref=P9L9FQKY
http://cytotec.directory/# buy misoprostol over the counter
смм услуги https://smm-almaty.kz/
https://guebsch.me/index.php?title=Benutzer:DustyKoenig
sildenafil citrate for sale sildenafil 20 mg tablet cost viagra 130mg
http://aspectavenue.com/company-operations/index.php?title=User:SusanaNorthern8
https://implementationmatters.org/index.php?title=User:MaryannGetz0920
https://madrasah.info/index.php/Finteh
I am really impressed with your writing skills as well as with the layout on your blog.
Is this a paid theme or did you customize it yourself?
Either way keep up the nice quality writing, it is rare to see a great blog like this one today.
Look at my site … 2007 saturn outlook
на черно-белых снимках
официальный сайт pin up http://pinupcasinovendfsty.dp.ua/.
https://hikvisiondb.webcam/wiki/User:ClevelandMoffitt
https://artepidemy.ru/index.php/User:Enid97030853
https://clomidpharm.shop/# buy generic clomid without insurance
https://mozillabd.science/wiki/User:MarianneZ01
Their medication reminders are such a thoughtful touch https://zithromaxpharm.online/# zithromax order online uk
https://funsilo.date/wiki/User:ShaniceSkeen7
пластиковый парковочный столбик купить https://idn300.ru/catalog/gibkie_stolbiki/
psyho2031.8ua.ru
A harmonious blend of local care and global expertise http://zithromaxpharm.online/# zithromax 500 mg lowest price pharmacy online
buy cytotec over the counter: buy cytotec pills online cheap – cytotec buy online usa
Payday loans in Iowa
http://zithromaxpharm.online/# zithromax price south africa
zithromax z-pak price without insurance: zithromax 250 mg pill – zithromax cost uk
erotica
Официальный сайт БК в России 1Win. Всем Рекомендую!
I don’t even know how I ended up here, but I thought this post was good. I don’t know who you are but certainly you’re going to a famous blogger if you are not already 😉 Cheers!
Best gifts for grandma: Ideas for your nana, abuela, or oma Please don’t get her another pair of slippers. https://www.bedirectory.com/SF_333027.html dating Cose da sapere prima di acquistare
@eerwq
psyho2031.8ua.ru
On 14 July 2011, Skype partnered with Comcast to carry its video chat service to Comcast subscribers via HDTV sets. On 19 July 2012, Microsoft announced that Skype users had logged 115 billion minutes of calls in the quarter, as much as 50% because the last quarter. This page was last edited on 19 April 2023, at 15:16 (UTC). Speaking to Vogue journal as their April cowl star, she confessed that she hadn’t been ‘ready’ to deal with her demons earlier than, but after discovering herself in a ‘dangerous place’ she realized she wanted to prioritize her restoration. Bad Religion 1994 n/a forty one 1 (Hungary) 11 (U.S. The speedy accessibility of 1’s lifestreaming activity can present data of prevalent significance along with being an inspiration for the readers. ’t stand being around Johnny and Sid anymore. Sid was set to marry Nancy in New York. He added that he had loved his time on the set. In 2023, Skype added the Bing AI chatbot to the platform for users who had access to the chatbot. Skype (/skaɪp/) is a proprietary telecommunications utility operated by Skype Technologies, a division of Microsoft, greatest known for VoIP-based videotelephony, videoconferencing and voice calls. The corporate was integrated as a division of Microsoft, which acquired all its technologies with the purchase.
psyho2031.8ua.ru
Your point of view caught my eye and was very interesting. Thanks. I have a question for you. https://accounts.binance.com/zh-CN/register-person?ref=GJY4VW8W
psyho2031.8ua.ru
psyho2031.8ua.ru
https://clomidpharm.shop/# can you buy clomid no prescription
Great place with even greater staff https://cytotec.directory/# cytotec abortion pill
She experienced a sister named Susan who lived with her for awhile. It’s named next the term kwink, which, centered on the web site, signifies the particular attribute that defines you. That indicates that you can activate a vibrator and have it encourage the model in actual-time! You most likely don’t have several alternate options. Okay, potentially in the function that you don’t have a incredibly great Computer, you won’t be able of obtaining knowledge in Hd. Jerkmate and BongaCams feel to have the greatest selection of partners doing on one particular webcam clearly show. You can produce an account utilizing your cellphone number or Facebook account. This is a excellent cellular phone chat area for people to chat and join with 1 yet another. Each and each just one of our major picks are worthy of your time and attention. The ethereal roof leading pub (the patio extends southwest, putting sponsors a floor above Geary Street) provides daters a particular see in the heart of downtown San Francisco. The crew appears beneath the major to set up dates between prospects that have identical character styles, values, and ambitions.
Березин Андрей Евроинвест http://lenta.ru/tags/persons/berezin-andrey.
Dubai, a city of grandeur and innovation, demands a transportation solution that matches its dynamic pace. Whether you’re a business executive, a tourist exploring the city, or someone in need of a reliable vehicle temporarily, car rental services in Dubai offer a flexible and cost-effective solution. In this guide, we’ll explore the popular car rental options in Dubai, catering to diverse needs and preferences.
Airport Car Rental: One-Way Pickup and Drop-off Road Trip Rentals:
For those who need to meet an important delegation at the airport or have a flight to another city, airport car rentals provide a seamless solution. Avoid the hassle of relying on public transport and ensure you reach your destination on time. With one-way pickup and drop-off options, you can effortlessly navigate your road trip, making business meetings or conferences immediately upon arrival.
Business Car Rental Deals & Corporate Vehicle Rentals in Dubai:
Companies without their own fleet or those finding transport maintenance too expensive can benefit from business car rental deals. This option is particularly suitable for businesses where a vehicle is needed only occasionally. By opting for corporate vehicle rentals, companies can optimize their staff structure, freeing employees from non-core functions while ensuring reliable transportation when necessary.
Tourist Car Rentals with Insurance in Dubai:
Tourists visiting Dubai can enjoy the freedom of exploring the city at their own pace with car rentals that come with insurance. This option allows travelers to choose a vehicle that suits the particulars of their trip without the hassle of dealing with insurance policies. Renting a car not only saves money and time compared to expensive city taxis but also ensures a trouble-free travel experience.
Daily Car Hire Near Me:
Daily car rental services are a convenient and cost-effective alternative to taxis in Dubai. Whether it’s for a business meeting, everyday use, or a luxury experience, you can find a suitable vehicle for a day on platforms like Smarketdrive.com. The website provides a secure and quick way to rent a car from certified and verified car rental companies, ensuring guarantees and safety.
Weekly Auto Rental Deals:
For those looking for flexibility throughout the week, weekly car rentals in Dubai offer a competent, attentive, and professional service. Whether you need a vehicle for a few days or an entire week, choosing a car rental weekly is a convenient and profitable option. The certified and tested car rental companies listed on Smarketdrive.com ensure a reliable and comfortable experience.
Monthly Car Rentals in Dubai:
When your personal car is undergoing extended repairs, or if you’re a frequent visitor to Dubai, monthly car rentals (long-term car rentals) become the ideal solution. Residents, businessmen, and tourists can benefit from the extensive options available on Smarketdrive.com, ensuring mobility and convenience throughout their stay in Dubai.
FAQ about Renting a Car in Dubai:
To address common queries about renting a car in Dubai, our FAQ section provides valuable insights and information. From rental terms to insurance coverage, it serves as a comprehensive guide for those considering the convenience of car rentals in the bustling city.
Conclusion:
Dubai’s popularity as a global destination is matched by its diverse and convenient car rental services. Whether for business, tourism, or daily commuting, the options available cater to every need. With reliable platforms like Smarketdrive.com, navigating Dubai becomes a seamless and enjoyable experience, offering both locals and visitors the ultimate freedom of mobility.
Watches World: Elevating Luxury and Style with Exquisite Timepieces
Introduction:
Jewelry has always been a timeless expression of elegance, and nothing complements one’s style better than a luxurious timepiece. At Watches World, we bring you an exclusive collection of coveted luxury watches that not only tell time but also serve as a testament to your refined taste. Explore our curated selection featuring iconic brands like Rolex, Hublot, Omega, Cartier, and more, as we redefine the art of accessorizing.
A Dazzling Array of Luxury Watches:
Watches World offers an unparalleled range of exquisite timepieces from renowned brands, ensuring that you find the perfect accessory to elevate your style. Whether you’re drawn to the classic sophistication of Rolex, the avant-garde designs of Hublot, or the precision engineering of Patek Philippe, our collection caters to diverse preferences.
Customer Testimonials:
Our commitment to providing an exceptional customer experience is reflected in the reviews from our satisfied clientele. O.M. commends our excellent communication and flawless packaging, while Richard Houtman appreciates the helpfulness and courtesy of our team. These testimonials highlight our dedication to transparency, communication, and customer satisfaction.
New Arrivals:
Stay ahead of the curve with our latest additions, including the Tudor Black Bay Ceramic 41mm, Richard Mille RM35-01 Rafael Nadal NTPT Carbon Limited Edition, and the Rolex Oyster Perpetual Datejust 41mm series. These new arrivals showcase cutting-edge designs and impeccable craftsmanship, ensuring you stay on the forefront of luxury watch fashion.
Best Sellers:
Discover our best-selling watches, such as the Bulgari Serpenti Tubogas 35mm and the Cartier Panthere Medium Model. These timeless pieces combine elegance with precision, making them a staple in any sophisticated wardrobe.
Expert’s Selection:
Our experts have carefully curated a selection of watches, including the Cartier Panthere Small Model, Omega Speedmaster Moonwatch 44.25 mm, and Rolex Oyster Perpetual Cosmograph Daytona 40mm. These choices exemplify the epitome of watchmaking excellence and style.
Secured and Tracked Delivery:
At Watches World, we prioritize the safety of your purchase. Our secured and tracked delivery ensures that your exquisite timepiece reaches you in perfect condition, giving you peace of mind with every order.
Passionate Experts at Your Service:
Our team of passionate watch experts is dedicated to providing personalized service. From assisting you in choosing the perfect timepiece to addressing any inquiries, we are here to make your watch-buying experience seamless and enjoyable.
Global Presence:
With a presence in key cities around the world, including Dubai, Geneva, Hong Kong, London, Miami, Paris, Prague, Dublin, Singapore, and Sao Paulo, Watches World brings luxury timepieces to enthusiasts globally.
Conclusion:
Watches World goes beyond being an online platform for luxury watches; it is a destination where expertise, trust, and satisfaction converge. Explore our collection, and let our timeless timepieces become an integral part of your style narrative. Join us in redefining luxury, one exquisite watch at a time.
Consider your storage needs, out there space, and personal preferences when choosing
the ideal storage container on your lingerie collection.
Durability and sturdiness: Select storage containers made from durable
supplies that may withstand regular use and supply ample protection for your delicate lingerie.
She will most likely be ready to merely buy these items of clothes from the online shops.
Yow will discover these professionals in department
shops and specialty lingerie retailers. With so many varieties to choose from, yow
will discover the right fit to complete any theme or occasion.
The corsages are often symbolic of the category theme or motto.
White and royal blue corsages come in quite a lot of
sizes and shapes. Kukishop’s 2 Piece Royal Blue Wedding ceremony Boutonniere
Synthetic Flower Groom Groomsman Corsage supplies an exquisite way to adorn any marriage ceremony or particular occasion. White orchids and blue accenting
flowers make this an elegant and particular corsage.
Nevertheless it still is a good process to seek out the very
best online lingerie retailer to benefit from your cash.
Being cautious on the internet is crucial as we don’t ever wish to be cheated and deserve to
purchase the best stuff with our hard-earned cash. Why Best White
And Navy Blue Corsage Is important?
generic ed drugs: pills for erection – ed dysfunction treatment
Dubai, a city known for its opulence and modernity, demands a mode of transportation that reflects its grandeur. For those seeking a cost-effective and reliable long-term solution, Somonion Rent Car LLC emerges as the premier choice for monthly car rentals in Dubai. With a diverse fleet ranging from compact cars to premium vehicles, the company promises an unmatched blend of affordability, flexibility, and personalized service.
Favorable Rental Conditions:
Understanding the potential financial strain of long-term car rentals, Somonion Rent Car LLC aims to make your journey more economical. The company offers flexible rental terms coupled with exclusive discounts for loyal customers. This commitment to affordability extends beyond the rental cost, as additional services such as insurance, maintenance, and repair ensure your safety and peace of mind throughout the duration of your rental.
A Plethora of Options:
Somonion Rent Car LLC boasts an extensive selection of vehicles to cater to diverse preferences and budgets. Whether you’re in the market for a sleek sedan or a spacious crossover, the company has the perfect car to complement your needs. The transparency in pricing, coupled with the ease of booking through their online platform, makes Somonion Rent Car LLC a hassle-free solution for those embarking on a long-term adventure in Dubai.
Car Rental Services Tailored for You:
Somonion Rent Car LLC doesn’t just offer cars; it provides a comprehensive range of rental services tailored to suit various occasions. From daily and weekly rentals to airport transfers and business travel, the company ensures that your stay in Dubai is not only comfortable but also exudes prestige. The fleet includes popular models such as the Nissan Altima 2018, KIA Forte 2018, Hyundai Elantra 2018, and the Toyota Camry Sport Edition 2020, all available for monthly rentals at competitive rates.
Featured Deals and Specials:
Somonion Rent Car LLC constantly updates its offerings to provide customers with the best deals. Featured cars like the Hyundai Sonata 2018 and Hyundai Santa Fe 2018 add a touch of luxury to your rental experience, with daily rates starting as low as AED 100. The company’s commitment to affordable luxury is further emphasized by the online booking system, allowing customers to secure the best deals in real-time through their website or by contacting the experts via phone or WhatsApp.
Conclusion:
Whether you’re a tourist looking to explore Dubai at your pace or a business traveler in need of a reliable and prestigious mode of transportation, Somonion Rent Car LLC stands as the go-to choice for monthly car rentals in Dubai. Unlock the ultimate mobility experience with Somonion, where affordability meets excellence, ensuring your journey through Dubai is as seamless and luxurious as the city itself. Contact Somonion Rent Car LLC today and embark on a journey where every mile is a testament to comfort, style, and unmatched service.
https://tureligious.com.ua/
http://gruzchikiafterrigger.ru
http://gruzchikithey.ru
till she had to kneel down on the floor; next there
prescription meds without the prescriptions tadalafil without a doctor’s prescription prescription drugs online without doctor
https://web-loft.ru/
most reputable canadian pharmacies my discount pharmacy safe online pharmacies
http://gruzchikipeople.ru
buy prescription drugs without doctor: tadalafil without a doctor’s prescription – how to get prescription drugs without doctor
плитка пзк https://znaki99.ru/plity-pzk/
Демонтаж и снос частных домов с вывозом мусора в Москве и Московской области – lit9.ru. Снос дома вручную и спецтехникой производим по ценам ниже рынка за 1 день. Бесплатный выезд специалиста на объект.
phone porn
Нужен ли вам быстрый ремонт кофемашин Bosch? В этом случае вам понадобится сервисный центр support-bosch.ru. Здесь вы найдете профессиональную помощь по любым вопросам, связанным с эксплуатацией кофемашин Bosch. Не ждите время и свяжитесь прямо сейчас на support-bosch.ru, чтобы пить ароматный напиток из вашей кофемашины Bosch в самое ближайшее время.
Хотите ли вы надежный ремонт кофемашин Bosch? В таком случае вам поможет сервисный центр support-bosch.ru. Здесь вы найдете профессиональную помощь по любым вопросам, связанным с эксплуатацией кофемашин Bosch. Не откладывайте время и обратитесь сейчас на support-bosch.ru, чтобы наслаждаться вкусным напитком из вашей кофемашины Bosch как можно скорее.
https://edpills.bid/# what are ed drugs
http://reputablepharmacies.online/# cheap online pharmacy
acticin 500mg
natural ed remedies: what are ed drugs – ed pills gnc
Официальный сайт БК в России и СНГ 1Win. Всем Рекомендую!
superstore pharmacy online non prescription on line pharmacies cheap drug prices
Thank you for your blog post. Jones and I are already saving for a new publication on this issue and your post has made us to save money.
Your thoughts really responded all our problems.
In fact, more than what we had recognized prior to when we
ran into your amazing blog. My partner and i no longer have doubts and also a troubled mind because you have attended to
our needs in this post. Thanks
Here is my web blog … bmw henderson
https://lucky-jet-app.com/
online ed pills ed pills that work best non prescription ed pills
download porn
1win Online spor bahisleri – mostbet ile heyecan verici bir macera
https://scientific-programs.science/wiki/Finteh
https://timeoftheworld.date/wiki/User:DeanaDoerr04897
http://wiki.rl-transport.org/index.php/User:PenneyKincaid02
https://implementationmatters.org/index.php?title=User:Lynell49V9886
Наши специалисты тщательно отбирают только качественные товары от ведущих мировых производителей, гарантируя ваше удовольствие и безопасностьhttp://producm.ru/forum/messages/forum10/topic39373/message356314/?result=new#message356314
prescription drugs without doctor approval: mexican pharmacy without prescription – ed meds online without doctor prescription
vidalista reddit. Medications and Digestive Disorders – Finding Relief for the Gut
Наши специалисты тщательно отбирают только качественные товары от ведущих мировых производителей, гарантируя ваше удовольствие и безопасностьhttp://lesuitedeldormiglione.it/index.php?option=com_kunena&view=topic&catid=3&id=9255&Itemid=289#8676
https://holden.asger.xyz/wiki/User:BuckTallis0669
https://checklist.ectrum.ru/
https://sciencewiki.science/wiki/User:WillianLevay
https://wiki.evil-admin.com/index.php?title=User:IngridKeeling2
erection pills online: best ed treatment – ed pills for sale
https://e-content4u.com/4-bill-2/
https://marvelvsdc.faith/wiki/Finteh
http://peter-fuerholz.ch/wiki/index.php?title=Benutzer:GDLPhyllis
mens ed pills top ed drugs best over the counter ed pills
http://edpills.bid/# otc ed pills
https://valetinowiki.racing/wiki/User:AubreyB8162
http://peter-fuerholz.ch/wiki/index.php?title=Benutzer:CorinneSylvester
10000 euro lenen
https://edpills.bid/# best erectile dysfunction pills
https://botdb.win/wiki/Finteh
prescription drugs without doctor approval ed meds online without doctor prescription buy prescription drugs
https://mediawiki.rockinsurance.com/index.php?title=User:TangelaZ44
Seriously many of wonderful facts.
https://madrasah.info/index.php/User:AntoniaBurr
http://www.urowiki.co.uk/index.php?title=User_talk:NovellaOsborne
You can normally locate progressive jackpots, Megawaays and 3D games inside the slots category.
Also visit my website: Best Online Casino [bitcoin-review.net]
https://wiki.hrw-fablab.de/index.php?title=4_Bill
https://schliffi.ch/index.php?title=Finteh
При монтаже и эксплуатации хомутовых и полухомутовых нагревательных элементов особое внимание следует обратить на обеспечение плотного контакта внутренней (рабочей) поверхности нагревателей с обогреваемой деталью https://rusupakten.ru/product-tag/vodyanoj-ten/
Березин Андрей Евроинвест https://antennadaily.ru/2023/06/23/andrey-berezin-euroinvest/.
п»їprescription drugs: ed meds online without doctor prescription – legal to buy prescription drugs without prescription
je kunt het hier proberen
http://aspectavenue.com/company-operations/index.php?title=Partners
buy prescription drugs online without prescription drugs online without cialis without doctor prescription
https://mediawiki.volunteersguild.org/index.php?title=New_Technologies
https://singletail.net/index.php?title=User:TammaraApplegate
Официальный и надежный сайт в России и СНГ 1Win. Рекомендую!
buy prescription drugs from canada cheap tadalafil without a doctor’s prescription non prescription ed pills
https://botdb.win/wiki/New_Technologies
top ed pills: mens ed pills – best ed pill
Porn young
https://wiki.hrw-fablab.de/index.php?title=Partners
https://blackhat-out.fr/level2/index.php/Utilisateur:KathleneStocks8
http://edpills.bid/# best treatment for ed
https://kesb-wiki.ch/index.php/Benutzer:AudryLyman6
One of the bestmobile car wash Miami
https://edpills.bid/# best otc ed pills
https://bbarlock.com/index.php/New_Technologies
this site
cheap erectile dysfunction best ed medication online ed pills
prescription drugs online: ed meds online without doctor prescription – legal to buy prescription drugs without prescription
prescription drugs canada buy online buy prescription drugs without doctor prescription drugs online without
best male enhancement pills: ed pills – gnc ed pills
https://edpills.bid/# ed drug prices
https://edpills.bid/# best ed medication
Чувствуете, что срочно нужны бабки? Тогда займ моментальный на карту – ваш спасательный круг. Это типа “бац и готово!” У нас нет времени на бюрократию, только деньги в кармане.
remeron medication
http://baikal-biz.ru/forum/viewtopic.php?f=15&t=22373
mexican pharmacy without prescription viagra without doctor prescription viagra without doctor prescription
http://elhovka.nn.ru/viewtopic.php?f=16&t=15653
https://vk.com/uslugi-224049362?screen=group&w=product-224049362_9072440%2Fquery
best treatment for ed natural ed medications best ed pill
спс не над
2. В пункте «обрисуйте персональный профиль» введите игровой id» и кликайте на кнопочку http://blog.nachalka.info/2012/03/blog-post.html «Искать». 3. Удостоверьтесь в факте, что никнейм отображается правильно.
https://pokrov.mybb.ru/viewtopic.php?id=4251#p77081
http://mirmamok.ru/forum/posts/328192
Very shortly this website will be famous among all blogging visitors, due
to it’s good articles or reviews
https://antimen.ru/viewtopic.php?id=7023#p20349
canadian pharmacy no rx: prescription drugs prices – prescriptions from canada without
http://forum.kam.su/showthread.php?p=94147#post94147
Porn mature
viagra without doctor prescription amazon: buy prescription drugs online without – buy prescription drugs
кондиционеры в ростове http://www.kondicionery-nedorogo-msk.ru.
online pharmacies reviews prescription without a doctor’s prescription canadian drug store coupon
кондиционеры климат https://kondicionery-nedorogo-msk.ru.
non prescription ed drugs ed remedies ed pills
Березин Андрей Евроинвест https://finance.rambler.ru/person/berezin-andrey/.
https://reputablepharmacies.online/# canadian drug store legit
кондиционер 12 http://www.kondicionery-nedorogo-msk.ru.
https://edpills.bid/# gnc ed pills
The salesman, surprised, asked the snail, “Why do you need a fast car? You’re a snail.” buy
инструменты диджитал маркетинга https://www.agentstvo-internet-marketinga.com.ua/.
The salesman, surprised, asked the snail, “Why do you need a fast car? You’re a snail.” buy
download porn
mexican pharmacy without prescription: prescription drugs – viagra without doctor prescription
Официальная, ныстоящая в России БК 1Вин. Рекомендую!
приподнятые пешеходные переходы https://znaki99.ru/rezinovyj-peshehodnyj-perehod/
агентство интернет маркетинга http://agentstvo-internet-marketinga.com.ua/.
sildenafil 100mg india
Мне не ясно.
«безопасный и указывает на то, отказное письмо по сертификации для озон что владелец сайта проверен центром сертификации. этот вид сертификата в основном применяется для веб-приложений, которые требуют подтверждения личности для сбора данных, обработки входов или осуществления интернет платежей.
canadian prescription prices: most popular canadian pharmacy – the best canadian online pharmacy
Watches World
Watches World: Elevating Luxury and Style with Exquisite Timepieces
Introduction:
Jewelry has always been a timeless expression of elegance, and nothing complements one’s style better than a luxurious timepiece. At Watches World, we bring you an exclusive collection of coveted luxury watches that not only tell time but also serve as a testament to your refined taste. Explore our curated selection featuring iconic brands like Rolex, Hublot, Omega, Cartier, and more, as we redefine the art of accessorizing.
A Dazzling Array of Luxury Watches:
Watches World offers an unparalleled range of exquisite timepieces from renowned brands, ensuring that you find the perfect accessory to elevate your style. Whether you’re drawn to the classic sophistication of Rolex, the avant-garde designs of Hublot, or the precision engineering of Patek Philippe, our collection caters to diverse preferences.
Customer Testimonials:
Our commitment to providing an exceptional customer experience is reflected in the reviews from our satisfied clientele. O.M. commends our excellent communication and flawless packaging, while Richard Houtman appreciates the helpfulness and courtesy of our team. These testimonials highlight our dedication to transparency, communication, and customer satisfaction.
New Arrivals:
Stay ahead of the curve with our latest additions, including the Tudor Black Bay Ceramic 41mm, Richard Mille RM35-01 Rafael Nadal NTPT Carbon Limited Edition, and the Rolex Oyster Perpetual Datejust 41mm series. These new arrivals showcase cutting-edge designs and impeccable craftsmanship, ensuring you stay on the forefront of luxury watch fashion.
Best Sellers:
Discover our best-selling watches, such as the Bulgari Serpenti Tubogas 35mm and the Cartier Panthere Medium Model. These timeless pieces combine elegance with precision, making them a staple in any sophisticated wardrobe.
Expert’s Selection:
Our experts have carefully curated a selection of watches, including the Cartier Panthere Small Model, Omega Speedmaster Moonwatch 44.25 mm, and Rolex Oyster Perpetual Cosmograph Daytona 40mm. These choices exemplify the epitome of watchmaking excellence and style.
Secured and Tracked Delivery:
At Watches World, we prioritize the safety of your purchase. Our secured and tracked delivery ensures that your exquisite timepiece reaches you in perfect condition, giving you peace of mind with every order.
Passionate Experts at Your Service:
Our team of passionate watch experts is dedicated to providing personalized service. From assisting you in choosing the perfect timepiece to addressing any inquiries, we are here to make your watch-buying experience seamless and enjoyable.
Global Presence:
With a presence in key cities around the world, including Dubai, Geneva, Hong Kong, London, Miami, Paris, Prague, Dublin, Singapore, and Sao Paulo, Watches World brings luxury timepieces to enthusiasts globally.
Conclusion:
Watches World goes beyond being an online platform for luxury watches; it is a destination where expertise, trust, and satisfaction converge. Explore our collection, and let our timeless timepieces become an integral part of your style narrative. Join us in redefining luxury, one exquisite watch at a time.
Демонтаж и снос частных домов с вывозом мусора в Москве и Московской области. Демонтаж дома вручную и спецтехникой производим по ценам ниже рынка за 1 день. Бесплатный выезд специалиста на объект.
I’m not sure why but this blog is loading incredibly slow for me.
Is anyone else having this issue or is it a problem on my end?
I’ll check back later and see if the problem still exists.
trillion
phone porn
discount prescriptions pharmacy online canada drugs online
02317257820
49 176 50642602
list of canadian pharmacies online trusted online pharmacy canada mail pharmacy
steuer rente
telefonnummer
скачать ggpokerok
скачать ggpokerok
wie viel nullen hat eine billionen
http://reputablepharmacies.online/# online pharmacy with no prescription
http://reputablepharmacies.online/# online pharmacies no prescriptions
meds canadian compounding pharmacy: best canadian pharmacy for viagra – canadian pharmacy ship to us
This site really has all the info I wanted about this
subject and didn’t know who to ask.
Оригинальная в России БК 1Вин. Рекомендую!
климат кондиционеры http://www.kondicionery-nedorogo-msk.ru.
best non prescription ed pills: 100mg viagra without a doctor prescription – online prescription for ed meds
proair-inhaler 250mg
viagra without a prescription buy prescription drugs from india discount prescription drugs
Watch porn videos
ed meds online without doctor prescription legal to buy prescription drugs from canada viagra without a doctor prescription
Конечно. Так бывает. Можем пообщаться на эту тему. Здесь или в PM.
они позволяют игрокам получать больше скинов за меньшие деньги vrgames.ru и существенно сэкономить. каждый пользователь имеет возможность выбрать максимально комфортный для себя метод, сделав оплату современной и безопасной.
%%
Here is my web blog – где сделать отказное письмо для вайлдберриз
http://edpills.bid/# generic ed drugs
best canadian online pharmacy: fda approved canadian pharmacies – viagra at canadian pharmacy
https://reputablepharmacies.online/# online prescriptions without script
buying generic lisinopril without insurance
canadian drugs online: Pharmacies in Canada that ship to the US – canadian pharmacy meds review canadianpharmacy.pro
%%
Stop by my web site :: http://cssbym.ru/forum/showtopic-31371
Need a virtual phone number to handle outbound and incoming calls? Get one in just a few minutes https://www.google.jo/url?q=https://hottelecom.biz/es/
pharmacy canadian Canadian pharmacy online canadian pharmacy india canadianpharmacy.pro
Need a virtual phone number to handle outbound and incoming calls? Get one in just a few minutes https://www.google.com.vn/url?q=https://didvirtualnumbers.com/nb/
mexican drugstore online mexico drug stores pharmacies medication from mexico pharmacy mexicanpharmacy.win
käytä tätä linkkiä
mexico drug stores pharmacies: mexico pharmacy – mexican border pharmacies shipping to usa mexicanpharmacy.win
was kommt nach milliarden
kennenlernphase
welche sternzeichen passen zusammen
https://incardio.cuas.at/wiki/index.php/Pin_Up_Casino
warum sollte man nicht auf der linken seite schlafen
http://bondpedia.altervista.org/index.php?title=Pin_Up_Casino
http://indianpharmacy.shop/# pharmacy website india indianpharmacy.shop
seitenschlafer
https://breitband-wiki.de/index.php?title=Benutzer:JaredVelasco907
http://canadianpharmacy.pro/# reliable canadian pharmacy reviews canadianpharmacy.pro
mexico drug stores pharmacies: online mexican pharmacy – mexico drug stores pharmacies mexicanpharmacy.win
whatsapp status einstellungen
verdienst oktoberfest kellner
http://cluster.shao.ac.cn/i18n/index.php?title=User:TressaColes11
штраф оплатить гибдд https://proverka-gibdd-shtrafov.ru/
rente 2500 brutto wieviel netto
reputable mexican pharmacies online mexican pharmacy online buying from online mexican pharmacy mexicanpharmacy.win
Программа для комплексного обслуживания Автоматизация интернет-магазинов. Рекомендую!
was kommt nach millionen
Если вы хотите скачать медиафайлы с видео, то вам нужен MediaGet – удобный медиа клиент. Она обеспечивает вам качественный доступ к огромному количеству медиа контента. Я предлагаю вам скачать MediaGet с сайта mediaget-4-you.ru и убедиться сами. Вы не разочаруетесь!
MediaGet – это замечательная программа для трансляции медиафайлов с торрент-трекеров. Она обеспечивает вам безопасный доступ к богатому количеству медиа контента. Я рекомендую вам скачать MediaGet с сайта mediaget-4-you.ru и проверить сами. Вы не разочаруетесь!
reputable mexican pharmacies online medication from mexico pharmacy mexico pharmacies prescription drugs mexicanpharmacy.win
Hello There. I found your blog using msn. This is an extremely well written article.
I will make sure to bookmark it and come back to read more of your useful info.
Thanks for the post. I’ll definitely return.
world pharmacy india: indian pharmacy – india pharmacy indianpharmacy.shop
https://www.browseo.net/?url=megapesni.site%2F
mobic generic
porn
best online canadian pharmacy: Canada Pharmacy – canadianpharmacymeds com canadianpharmacy.pro
Березин Андрей Евроинвест https://www.newizv.ru/news/2023-08-28/berezin-andrey-svedeniya-o-developere-419032/.
https://whois.ws/whois/mp3gid.co
https://www.sslshopper.com/ssl-checker.html#hostname=mp3bit.pw/
http://mexicanpharmacy.win/# mexico pharmacy mexicanpharmacy.win
online pharmacy india best india pharmacy indian pharmacies safe indianpharmacy.shop
http://indianpharmacy.shop/# indian pharmacy paypal indianpharmacy.shop
reputable mexican pharmacies online mexican online pharmacies prescription drugs purple pharmacy mexico price list mexicanpharmacy.win
You can get a virtual phone number with OpenPhone in three simple https://www.google.bg/url?q=https://didvirtualnumbers.com/nb/
You can get a virtual phone number with OpenPhone in three simple https://www.google.ms/url?q=https://didvirtualnumbers.com/nb/
%%
Feel free to surf to my website: p21886
https://mterentiev.ru/bitrix/redirect.php?event1=&event2=&event3=&goto=https://pesnimp3.ws/
La oferta de casino online bonos sin depósito en Chile es ideal para quienes desean explorar diferentes plataformas de juego en línea. Estos bonos brindan una oportunidad segura y libre de riesgos para probar suerte en diversos juegos.
https://azby.search.nifty.com/websearch/search?select=1077&cflg=%8C%9F%8D%F5&htmltype=2&Text=pesnimp3.ws
best canadian pharmacy to buy from: northwest canadian pharmacy – canada pharmacy canadianpharmacy.pro
%%
Check out my homepage :: порно массаж
https://www.pantyhose.info/__media__/js/netsoltrademark.php?d=mp3name.me
pret 8500 euros
%%
my site … http://bneinoach.ru/forum/user/97664/
https://b9d.online/domain/mp3bit.pw
https://rankw.ru/s/mp3gid.co
Только здесь вы найдете актуальный промокод на БК 1Вин. Рекомендую!
mail order pharmacy india indian pharmacy best india pharmacy indianpharmacy.shop
world pharmacy india: Best Indian pharmacy – india pharmacy mail order indianpharmacy.shop
https://pacificbridges.com/__media__/js/netsoltrademark.php?d=mp3-top.net
https://xn--80adnhhsfckl.xn--p1ai/bitrix/redirect.php?goto=https://mp3-top.net
thorazine online
Приложение Зенит скачивай
buying prescription drugs in mexico online mexican pharmacy online mexico pharmacy mexicanpharmacy.win
https://indianpharmacy.shop/# Online medicine order indianpharmacy.shop
https://nrb-land.ru/bitrix/rk.php?goto=https://pesnimp3.ws
https://indianpharmacy.shop/# online pharmacy india indianpharmacy.shop
Porn free
https://xn—-7sbb1bf4anecc0a8a5be.xn--p1ai/bitrix/click.php?goto=https://pesnimp3.ws
%%
Also visit my homepage :: https://sibledy.ru/thread-314682-1-1.html
Приветик Всем!
Wege verdienst oktoberfest kellner fur den Schutz|die Trennung von} Ihrer/Gewahrleistung/Gewahrleistung Vertraulichkeit/Vertraulichkeit. whatsapp ist am meisten gefragter Messenger weltweit/weltweit. und zuletzt/noch, aber nicht weniger/auch wichtig: Sie konnen auch Lesebestatigungen in Einstellungen/Layouts deaktivieren.
https://aegworldwide.de/__media__/js/netsoltrademark.php?d=mp3gid.co
If you intend to acquire automobile money management online, you have to narrow down all the achievable bargains and prices
that suit your budget. As usually along with the situation of a lot of, they usually tend to overlook the importance of reviewing financial quotes that they often tend to invest three times as much
as they might have really conserved, Home Page.
Prestito 9 mila euro
%%
Also visit my web blog :: bottom
https://zeerank.com/domain/megapesni.site
%%
Also visit my page :: https://beaulfyo51626.blogsuperapp.com/25172597/balancing-work-and-life-in-the-stripping-industry
world pharmacy india indian pharmacy indian pharmacies safe indianpharmacy.shop
https://ui.dev/amiresponsive?url=https:%2F%2Fmp3bit.pw
http://canadianpharmacy.pro/# canadapharmacyonline com canadianpharmacy.pro
http://canadianpharmacy.pro/# canadian neighbor pharmacy canadianpharmacy.pro
Демонтаж и снос частных домов с вывозом мусора в Москве и Московской области. Демонтаж дома вручную и спецтехникой производим по ценам ниже рынка за 1 день. Бесплатный выезд специалиста на объект.
Apartments in Iconic Tower DIC with favourable terms of purchase and return on investment.
ремонт квартир под ключ ярославль
https://seosofast.com/domain/mp3new.top
%%
Have a look at my page: http://pytalovo.4admins.ru/viewtopic.php?f=15&t=2018
https://hemlok.ru/bitrix/rk.php?goto=https://mp3-top.net/
https://www.learnwin.xyz/domain/mp3new.top
Luxury at its finest! Discover the epitome of elegance with Cavalli Towers Dubai newly launched collection of opulent apartments for sale in the iconic Dubai Marina. Immerse yourself in ultimate lavishness within this breathtaking 70-storey masterpiece by DAMAC Properties.
2024娛樂城
2024娛樂城No.1 – 富遊娛樂城介紹
2024 年 1 月 5 日
|
娛樂城, 現金版娛樂城
富遊娛樂城是無論老手、新手,都非常推薦的線上博奕,在2024娛樂城當中扮演著多年來最來勢洶洶的一匹黑馬,『人性化且精緻的介面,遊戲種類眾多,超級多的娛樂城優惠,擁有眾多與會員交流遊戲的群組』是一大特色。
富遊娛樂城擁有歐洲馬爾他(MGA)和菲律賓政府競猜委員會(PAGCOR)頒發的合法執照。
註冊於英屬維爾京群島,受國際行業協會認可的合法公司。
我們的中心思想就是能夠帶領玩家遠詐騙黑網,讓大家安心放心的暢玩線上博弈,娛樂城也受各大部落客、IG網紅、PTT論壇,推薦討論,富遊娛樂城沒有之一,絕對是線上賭場玩家的第一首選!
富遊娛樂城介面 / 2024娛樂城NO.1
富遊娛樂城簡介
品牌名稱 : 富遊RG
創立時間 : 2019年
存款速度 : 平均15秒
提款速度 : 平均5分
單筆提款金額 : 最低1000-100萬
遊戲對象 : 18歲以上男女老少皆可
合作廠商 : 22家遊戲平台商
支付平台 : 各大銀行、各大便利超商
支援配備 : 手機網頁、電腦網頁、IOS、安卓(Android)
富遊娛樂城遊戲品牌
真人百家 — 歐博真人、DG真人、亞博真人、SA真人、OG真人
體育投注 — SUPER體育、鑫寶體育、亞博體育
電競遊戲 — 泛亞電競
彩票遊戲 — 富遊彩票、WIN 539
電子遊戲 —ZG電子、BNG電子、BWIN電子、RSG電子、好路GR電子
棋牌遊戲 —ZG棋牌、亞博棋牌、好路棋牌、博亞棋牌
捕魚遊戲 —ZG捕魚、RSG捕魚、好路GR捕魚、亞博捕魚
富遊娛樂城優惠活動
每日任務簽到金666
富遊VIP全面啟動
復酬金活動10%優惠
日日返水
新會員好禮五選一
首存禮1000送1000
免費體驗金$168
富遊娛樂城APP
步驟1 : 開啟網頁版【富遊娛樂城官網】
步驟2 : 點選上方(下載app),會跳出下載與複製連結選項,點選後跳轉。
步驟3 : 跳轉後點選(安裝),並點選(允許)操作下載描述檔,跳出下載描述檔後點選關閉。
步驟4 : 到手機設置>一般>裝置管理>設定描述檔(富遊)安裝,即可完成安裝。
富遊娛樂城常見問題FAQ
富遊娛樂城詐騙?
黑網詐騙可細分兩種,小出大不出及純詐騙黑網,我們可從品牌知名度經營和網站架設畫面分辨來簡單分辨。
富遊娛樂城會出金嗎?
如上面提到,富遊是在做一個品牌,為的是能夠保證出金,和帶領玩家遠離黑網,而且還有DUKER娛樂城出金認證,所以各位能夠放心富遊娛樂城為正出金娛樂城。
富遊娛樂城出金延遲怎麼辦?
基本上只要是公司系統問提造成富遊娛樂城會員無法在30分鐘成功提款,富遊娛樂城會即刻派送補償金,表達誠摯的歉意。
富遊娛樂城結論
富遊娛樂城安心玩,評價4.5顆星。如果還想看其他娛樂城推薦的,可以來娛樂城推薦尋找喔。
https://xn--80ajnjjy1b.xn--p1ai/bitrix/redirect.php?goto=https://mp3gid.co
Je recommande cette très belle pochette Pablo Mini x Ice Cold
https://s2sf.com/domain/mp3new.top
Je recommande cette très belle pochette Pablo Niclab Ice
К сожалению, ничем не могу помочь, но уверен, что Вы найдёте правильное решение. Не отчаивайтесь.
on her own first night in the city I https://zanednwe07529.blogofoto.com/55704968/nightlife-entrepreneurs-starting-your-own-stripping-business an oil rig and reminded me of Fred Flintstone.
Играть онлайн игровые автоматы бесплатно обезьяны
Казино вулкан игровые официальный сайт
Официальный телеграм канал 1win. Рекомендую!
india online pharmacy indian pharmacy india online pharmacy indianpharmacy.shop
Find properties for sale in New Palm Jebel Ali, Dubai with maps & photos. Choose the best property by Nakheel. Instalment Payment Plans available.
https://barcelonatapas.co.uk/__media__/js/netsoltrademark.php?d=mp3name.me
https://xn--80anc0ajbxbc.xn--p1ai/bitrix/click.php?goto=https://mp3name.me
https://host.io/megapesni.site
https://rg888.app/set/
2024全新上線❰戰神賽特老虎機❱ – ATG賽特玩法說明介紹
❰戰神賽特老虎機❱是由ATG電子獨家開發的古埃及風格線上老虎機,在傳說中戰神賽特是「力量之神」與奈芙蒂斯女神結成連理,共同守護古埃及的奇幻秘寶,只有被選中的冒險者才能進入探險。
❰戰神賽特老虎機❱ – ATG賽特介紹
2024最新老虎機【戰神塞特】- ATG電子 X 富遊娛樂城
❰戰神賽特老虎機❱ – ATG電子
線上老虎機系統 : ATG電子
發行年分 : 2024年1月
最大倍數 : 51000倍
返還率 : 95.89%
支付方式 : 全盤倍數、消除掉落
最低投注金額 : 0.4元
最高投注金額 : 2000元
可否選台 : 是
可選台台數 : 350台
免費遊戲 : 選轉觸發+購買特色
❰戰神賽特老虎機❱ 賠率說明
戰神塞特老虎機賠率算法非常簡單,玩家們只需要不斷的轉動老虎機,成功消除物件即可贏分,得分賠率依賠率表計算。
當盤面上沒有物件可以消除時,倍數符號將會相加形成總倍數!該次旋轉的總贏分即為 : 贏分 X 總倍數。
積分方式如下 :
贏分=(單次押注額/20) X 物件賠率
EX : 單次押注額為1,盤面獲得12個戰神賽特倍數符號法老魔眼
贏分= (1/20) X 1000=50
以下為各個得分符號數量之獎金賠率 :
得分符號 獎金倍數 得分符號 獎金倍數
戰神賽特倍數符號聖甲蟲 6 2000
5 100
4 60 戰神賽特倍數符號黃寶石 12+ 200
10-11 30
8-9 20
戰神賽特倍數符號荷魯斯之眼 12+ 1000
10-11 500
8-9 200 戰神賽特倍數符號紅寶石 12+ 160
10-11 24
8-9 16
戰神賽特倍數符號眼鏡蛇 12+ 500
10-11 200
8-9 50 戰神賽特倍數符號紫鑽石 12+ 100
10-11 20
8-9 10
戰神賽特倍數符號神箭 12+ 300
10-11 100
8-9 40 戰神賽特倍數符號藍寶石 12+ 80
10-11 18
8-9 8
戰神賽特倍數符號屠鐮刀 12+ 240
10-11 40
8-9 30 戰神賽特倍數符號綠寶石 12+ 40
10-11 15
8-9 5
❰戰神賽特老虎機❱ 賠率說明(橘色數值為獲得數量、黑色數值為得分賠率)
ATG賽特 – 特色說明
ATG賽特 – 倍數符號獎金加乘
玩家們在看到盤面上出現倍數符號時,務必把握機會加速轉動ATG賽特老虎機,倍數符號會隨機出現2到500倍的隨機倍數。
當盤面無法在消除時,這些倍數總和會相加,乘上當時累積之獎金,即為最後得分總額。
倍數符號會出現在主遊戲和免費遊戲當中,玩家們千萬別錯過這個可以瞬間將得獎金額拉高的好機會!
ATG賽特 – 倍數符號獎金加乘
ATG賽特 – 倍數符號圖示
ATG賽特 – 進入神秘金字塔開啟免費遊戲
戰神賽特倍數符號聖甲蟲
❰戰神賽特老虎機❱ 免費遊戲符號
在古埃及神話中,聖甲蟲又稱為「死亡之蟲」,它被當成了天球及重生的象徵,守護古埃及的奇幻秘寶。
當玩家在盤面上,看見越來越多的聖甲蟲時,千萬不要膽怯,只需在牌面上斬殺4~6個ATG賽特免費遊戲符號,就可以進入15場免費遊戲!
在免費遊戲中若轉出3~6個聖甲蟲免費遊戲符號,可額外獲得5次免費遊戲,最高可達100次。
當玩家的累積贏分且盤面有倍數物件時,盤面上的所有倍數將會加入總倍數!
ATG賽特 – 選台模式贏在起跑線
為避免神聖的寶物被盜墓者奪走,富有智慧的法老王將金子塔內佈滿迷宮,有的設滿機關讓盜墓者寸步難行,有的暗藏機關可以直接前往存放神秘寶物的暗房。
ATG賽特老虎機設有350個機檯供玩家選擇,這是連魔龍老虎機、忍老虎機都給不出的機台數量,為的就是讓玩家,可以隨時進入神秘的古埃及的寶藏聖域,挖掘長眠已久的神祕寶藏。
【戰神塞特老虎機】選台模式
❰戰神賽特老虎機❱ 選台模式
ATG賽特 – 購買免費遊戲挖掘秘寶
玩家們可以使用當前投注額的100倍購買免費遊戲!進入免費遊戲再也不是虛幻。獎勵與一般遊戲相同,且購買後遊戲將自動開始,直到場次和獎金發放完畢為止。
有購買免費遊戲需求的玩家們,立即點擊「開始」,啟動神秘金字塔裡的古埃及祕寶吧!
【戰神塞特老虎機】購買特色
❰戰神賽特老虎機❱ 購買特色
戰神賽特試玩推薦
看完了❰戰神賽特老虎機❱介紹之後,玩家們是否也蓄勢待發要進入古埃及的世界,一探神奇秘寶探險之旅。
本次ATG賽特與線上娛樂城推薦第一名的富遊娛樂城合作,只需要加入會員,即可領取到168體驗金,免費試玩420轉!
http://mexicanpharmacy.win/# mexico pharmacies prescription drugs mexicanpharmacy.win
pharmacies in mexico that ship to usa mexican pharmacy online medicine in mexico pharmacies mexicanpharmacy.win
http://indianpharmacy.shop/# legitimate online pharmacies india indianpharmacy.shop
sildenafil 20 mg generic
What decisions are they waiting for from such https://actorlist.ru/user/boisetnafu? This advice also applies to your paid strategy in social networks.
https://cwr.ru/bitrix/click.php?goto=https://mp3new.top
https://webseoanalyzer.com/domain/megapesni.site
http://canadianpharmacy.pro/# thecanadianpharmacy canadianpharmacy.pro
Агентство набирает пластичных, стройных и привлекательных девушек http://teama2t.free.fr/index.php?file=Members&op=detail&autor=ahejun
https://www.ecseotools.com/domain/mp3bit.pw
Агентство набирает пластичных, стройных и привлекательных девушек http://forum.spolokmedikovke.sk/viewtopic.php?f=3&t=34672
best india pharmacy indian pharmacy indian pharmacy paypal indianpharmacy.shop
%%
My blog :: https://voltekgroup.com/catalog/myasopererabatyvayushchee_oborudovanie/
https://www.sitesearch.net/domain/mp3-top.net
Lainaa 20000 euroa
https://canadianpharmacy.pro/# canadian pharmacy victoza canadianpharmacy.pro
https://freetools.seobility.net/de/seocheck/megapesni.site
%%
Have a look at my web site: https://www.gigabytemagazine.com/steve-wozniak-how-steve-jobs-would-react-if-he-could-see-apple-today/
http://missis.apkservice.ru/index.php?subaction=userinfo&user=novaavusly
https://www.ask.com/web?q=mp3name.me
https://mexicanpharmacy.win/# reputable mexican pharmacies online mexicanpharmacy.win
reputable indian online pharmacy
https://otoplenieprof.ru/bitrix/rk.php?goto=https://mp3bit.pw
northwest canadian pharmacy Cheapest drug prices Canada best online canadian pharmacy canadianpharmacy.pro
https://2qr.ru/https://mp3gid.co
http://mexicanpharmacy.win/# mexican mail order pharmacies mexicanpharmacy.win
india pharmacy mail order
http://g95887q6.beget.tech/user/novyugrism/
https://trustscam.nl/pesnimp3.ws
http://canadianpharmacy.pro/# pharmacy canadian superstore canadianpharmacy.pro
my canadian pharmacy rx canadian pharmacy phone number canadian online pharmacy canadianpharmacy.pro
It’s very goodluxury car wash Miami. Hightly recommend!
Ежемесячная зарплата красоток, которые работают в данном агентстве, составляет от 20000 долларов и выше http://www.jin-jay.nl/geboortekaartje/comment-page-719/#comment-763605
Ежемесячная зарплата красоток, которые работают в данном агентстве, составляет от 20000 долларов и выше http://kyevlyn.ukrbb.net/viewtopic.php?f=4&t=5671
Brazzers HD
https://deets.feedreader.com/pesnimp3.ws/
http://canadianpharmacy.pro/# reputable canadian pharmacy canadianpharmacy.pro
Очень кртая БК в России 1вин. Рекомендую!
Medicament information leaflet. Drug Class.
rx zoloft
Some what you want to know about medicine. Get now.
https://canadianpharmacy.pro/# canadianpharmacymeds com canadianpharmacy.pro
reputable indian pharmacies
can i purchase generic valtrex pill
https://www.bing.com/search?q=mp3bit.pw+mp3bit.pw&form=QBNO
https://igrotorgi.ru/redir.php?url=https://mp3-top.net/
https://www.urlvoid.com/scan/mp3gid.co/
https://konigalloys.co.uk/__media__/js/netsoltrademark.php?d=mp3-top.net
cheapest online pharmacy india buy medicines online in india reputable indian online pharmacy indianpharmacy.shop
торрентом, вы найдете лучших эскортниц в москве, каждая из каковых характеризуется уникальными познаниями и предоставляет услуги класса-премиум, http://ledsoft.ru/forum/?PAGE_NAME=message&FID=5&TID=12154&TITLE_SEO=12154-mskvipladie&MID=12850&result=new#message12850 чтобы насытить самые изысканные вкусы.
https://indianpharmacy.shop/# india pharmacy indianpharmacy.shop
indian pharmacy paypal
https://wktom.com/domain/mp3name.me
https://vesti48.ru/redirect?url=https://pesnimp3.ws/
https://novos3.ru/bitrix/rk.php?goto=https://mp3gid.co/
dapagliflozina para que serve
https://canadianpharmacy.pro/# canadian pharmacy oxycodone canadianpharmacy.pro
best india pharmacy Online medicine home delivery reputable indian online pharmacy indianpharmacy.shop
Medicament prescribing information. What side effects?
clomid
Everything what you want to know about drugs. Get information now.
https://mexicanpharmacy.win/# mexican rx online mexicanpharmacy.win
https://canadianpharmacy.pro/# the canadian pharmacy canadianpharmacy.pro
india pharmacy
https://andlinger.biz/__media__/js/netsoltrademark.php?d=mp3bit.pw
диджитал маркетинг что это http://www.agentstvo-internet-marketinga.com.ua.
https://tengoweb.net/domain/megapesni.site
современный плинтус в интерьере http://www.aljumynyevyj-napolnyj-plyntus.ru/.
https://canadianpharmacy.pro/# canada pharmacy canadianpharmacy.pro
top 10 pharmacies in india
https://100daystogreatness.biz/__media__/js/netsoltrademark.php?d=mp3new.top
плинтус алюминиевый https://www.aljumynyevyj-napolnyj-plyntus.ru/.
Выполняем поверку счетчиков воды на дому без снятия. Поверитель в день обращения поверка горячей воды цена
Выполняем поверку счетчиков воды на дому без снятия. Поверитель в день обращения поверки счетчиков воды
алюминиевый плинтус https://aljumynyevyj-napolnyj-plyntus.ru.
https://www.inventive9.com/seo-audit/domain/mp3-top.net
Mehr Info
установка сплит системы http://multi-kondicionery.ru/.
New! Enhanced options to earn 3% cash back based on Bank of America customer feedback. Maximize your rewards with 3% cash back in the category of your choice — with newly-expanded options. https://wisethink.us/
https://www.ozmanagementgroup.co.uk/__media__/js/netsoltrademark.php?d=mp3new.top
https://mexicanpharmacy.win/# mexico drug stores pharmacies mexicanpharmacy.win
кондиционер купить с установкой multi-kondicionery.ru.
https://305fest.com/__media__/js/netsoltrademark.php?d=mp3gid.co
best mail order pharmacy canada canadian pharmacy no rx needed precription drugs from canada canadianpharmacy.pro
Очень надежная БК в России 1вин. Рекомендую!
https://aeldllc.com/__media__/js/netsoltrademark.php?d=mp3new.top
https://mexicanpharmacy.win/# reputable mexican pharmacies online mexicanpharmacy.win
Online medicine home delivery
https://canadianpharmacy.pro/# onlinepharmaciescanada com canadianpharmacy.pro
казалось бы, https://imperiasport.ru/product/utjazheliteli-2h45-kg-reguliruemye-bstaw20-/reviews/ радоваться важно и наши кондитеры давненько уже проживаем отдельную жизнь. все одно грустно, что не знают друг друга и еще не смогли сохранить чувства», – начала она.
https://www.nic.ru/whois/?searchWord=megapesni.site
https://fastweb4y.com/domain/mp3name.me
https://www.techmount.de/__media__/js/netsoltrademark.php?d=megapesni.site
http://canadianpharmacy.pro/# canadian pharmacy tampa canadianpharmacy.pro
best india pharmacy
https://trustscam.nl/mp3name.me
2024娛樂城No.1 – 富遊娛樂城介紹
2024 年 1 月 5 日
|
娛樂城, 現金版娛樂城
富遊娛樂城是無論老手、新手,都非常推薦的線上博奕,在2024娛樂城當中扮演著多年來最來勢洶洶的一匹黑馬,『人性化且精緻的介面,遊戲種類眾多,超級多的娛樂城優惠,擁有眾多與會員交流遊戲的群組』是一大特色。
富遊娛樂城擁有歐洲馬爾他(MGA)和菲律賓政府競猜委員會(PAGCOR)頒發的合法執照。
註冊於英屬維爾京群島,受國際行業協會認可的合法公司。
我們的中心思想就是能夠帶領玩家遠詐騙黑網,讓大家安心放心的暢玩線上博弈,娛樂城也受各大部落客、IG網紅、PTT論壇,推薦討論,富遊娛樂城沒有之一,絕對是線上賭場玩家的第一首選!
富遊娛樂城介面 / 2024娛樂城NO.1
富遊娛樂城簡介
品牌名稱 : 富遊RG
創立時間 : 2019年
存款速度 : 平均15秒
提款速度 : 平均5分
單筆提款金額 : 最低1000-100萬
遊戲對象 : 18歲以上男女老少皆可
合作廠商 : 22家遊戲平台商
支付平台 : 各大銀行、各大便利超商
支援配備 : 手機網頁、電腦網頁、IOS、安卓(Android)
富遊娛樂城遊戲品牌
真人百家 — 歐博真人、DG真人、亞博真人、SA真人、OG真人
體育投注 — SUPER體育、鑫寶體育、亞博體育
電競遊戲 — 泛亞電競
彩票遊戲 — 富遊彩票、WIN 539
電子遊戲 —ZG電子、BNG電子、BWIN電子、RSG電子、好路GR電子
棋牌遊戲 —ZG棋牌、亞博棋牌、好路棋牌、博亞棋牌
捕魚遊戲 —ZG捕魚、RSG捕魚、好路GR捕魚、亞博捕魚
富遊娛樂城優惠活動
每日任務簽到金666
富遊VIP全面啟動
復酬金活動10%優惠
日日返水
新會員好禮五選一
首存禮1000送1000
免費體驗金$168
富遊娛樂城APP
步驟1 : 開啟網頁版【富遊娛樂城官網】
步驟2 : 點選上方(下載app),會跳出下載與複製連結選項,點選後跳轉。
步驟3 : 跳轉後點選(安裝),並點選(允許)操作下載描述檔,跳出下載描述檔後點選關閉。
步驟4 : 到手機設置>一般>裝置管理>設定描述檔(富遊)安裝,即可完成安裝。
富遊娛樂城常見問題FAQ
富遊娛樂城詐騙?
黑網詐騙可細分兩種,小出大不出及純詐騙黑網,我們可從品牌知名度經營和網站架設畫面分辨來簡單分辨。
富遊娛樂城會出金嗎?
如上面提到,富遊是在做一個品牌,為的是能夠保證出金,和帶領玩家遠離黑網,而且還有DUKER娛樂城出金認證,所以各位能夠放心富遊娛樂城為正出金娛樂城。
富遊娛樂城出金延遲怎麼辦?
基本上只要是公司系統問提造成富遊娛樂城會員無法在30分鐘成功提款,富遊娛樂城會即刻派送補償金,表達誠摯的歉意。
富遊娛樂城結論
富遊娛樂城安心玩,評價4.5顆星。如果還想看其他娛樂城推薦的,可以來娛樂城推薦尋找喔。
where can i buy zofran 4mg
https://igrotorgi.ru/redir.php?url=https://mp3new.top/
https://www.happymadisonmovies.com/__media__/js/netsoltrademark.php?d=mp3-top.net
https://www.ssllabs.com/ssltest/analyze.html?d=mp3bit.pw&latest
canadian pharmacy meds review canada drugs online reviews canadian pharmacy meds reviews canadianpharmacy.pro
isosorbide 20mg cheap
Андрей Фролов, отличившийся на экономическом факультете МГУ, проявил себя как одаренный финансист в крупном банке. Его карьерный рост был обусловлен не только профессионализмом, но и способностью к нестандартному мышлению в сложных финансовых ситуациях. Сейчас Андрей применяет свои навыки для анализа рынка и разработки инвестиционных стратегий на mikro-zaim-online.ru, обеспечивая клиентам выгодные условия займов. Подробнее о нем и о предложениях займов можно узнать на https://mikro-zaim-online.ru/o-nas/
戰神賽特
2024全新上線❰戰神賽特老虎機❱ – ATG賽特玩法說明介紹
❰戰神賽特老虎機❱是由ATG電子獨家開發的古埃及風格線上老虎機,在傳說中戰神賽特是「力量之神」與奈芙蒂斯女神結成連理,共同守護古埃及的奇幻秘寶,只有被選中的冒險者才能進入探險。
❰戰神賽特老虎機❱ – ATG賽特介紹
2024最新老虎機【戰神塞特】- ATG電子 X 富遊娛樂城
❰戰神賽特老虎機❱ – ATG電子
線上老虎機系統 : ATG電子
發行年分 : 2024年1月
最大倍數 : 51000倍
返還率 : 95.89%
支付方式 : 全盤倍數、消除掉落
最低投注金額 : 0.4元
最高投注金額 : 2000元
可否選台 : 是
可選台台數 : 350台
免費遊戲 : 選轉觸發+購買特色
❰戰神賽特老虎機❱ 賠率說明
戰神塞特老虎機賠率算法非常簡單,玩家們只需要不斷的轉動老虎機,成功消除物件即可贏分,得分賠率依賠率表計算。
當盤面上沒有物件可以消除時,倍數符號將會相加形成總倍數!該次旋轉的總贏分即為 : 贏分 X 總倍數。
積分方式如下 :
贏分=(單次押注額/20) X 物件賠率
EX : 單次押注額為1,盤面獲得12個戰神賽特倍數符號法老魔眼
贏分= (1/20) X 1000=50
以下為各個得分符號數量之獎金賠率 :
得分符號 獎金倍數 得分符號 獎金倍數
戰神賽特倍數符號聖甲蟲 6 2000
5 100
4 60 戰神賽特倍數符號黃寶石 12+ 200
10-11 30
8-9 20
戰神賽特倍數符號荷魯斯之眼 12+ 1000
10-11 500
8-9 200 戰神賽特倍數符號紅寶石 12+ 160
10-11 24
8-9 16
戰神賽特倍數符號眼鏡蛇 12+ 500
10-11 200
8-9 50 戰神賽特倍數符號紫鑽石 12+ 100
10-11 20
8-9 10
戰神賽特倍數符號神箭 12+ 300
10-11 100
8-9 40 戰神賽特倍數符號藍寶石 12+ 80
10-11 18
8-9 8
戰神賽特倍數符號屠鐮刀 12+ 240
10-11 40
8-9 30 戰神賽特倍數符號綠寶石 12+ 40
10-11 15
8-9 5
❰戰神賽特老虎機❱ 賠率說明(橘色數值為獲得數量、黑色數值為得分賠率)
ATG賽特 – 特色說明
ATG賽特 – 倍數符號獎金加乘
玩家們在看到盤面上出現倍數符號時,務必把握機會加速轉動ATG賽特老虎機,倍數符號會隨機出現2到500倍的隨機倍數。
當盤面無法在消除時,這些倍數總和會相加,乘上當時累積之獎金,即為最後得分總額。
倍數符號會出現在主遊戲和免費遊戲當中,玩家們千萬別錯過這個可以瞬間將得獎金額拉高的好機會!
ATG賽特 – 倍數符號獎金加乘
ATG賽特 – 倍數符號圖示
ATG賽特 – 進入神秘金字塔開啟免費遊戲
戰神賽特倍數符號聖甲蟲
❰戰神賽特老虎機❱ 免費遊戲符號
在古埃及神話中,聖甲蟲又稱為「死亡之蟲」,它被當成了天球及重生的象徵,守護古埃及的奇幻秘寶。
當玩家在盤面上,看見越來越多的聖甲蟲時,千萬不要膽怯,只需在牌面上斬殺4~6個ATG賽特免費遊戲符號,就可以進入15場免費遊戲!
在免費遊戲中若轉出3~6個聖甲蟲免費遊戲符號,可額外獲得5次免費遊戲,最高可達100次。
當玩家的累積贏分且盤面有倍數物件時,盤面上的所有倍數將會加入總倍數!
ATG賽特 – 選台模式贏在起跑線
為避免神聖的寶物被盜墓者奪走,富有智慧的法老王將金子塔內佈滿迷宮,有的設滿機關讓盜墓者寸步難行,有的暗藏機關可以直接前往存放神秘寶物的暗房。
ATG賽特老虎機設有350個機檯供玩家選擇,這是連魔龍老虎機、忍老虎機都給不出的機台數量,為的就是讓玩家,可以隨時進入神秘的古埃及的寶藏聖域,挖掘長眠已久的神祕寶藏。
【戰神塞特老虎機】選台模式
❰戰神賽特老虎機❱ 選台模式
ATG賽特 – 購買免費遊戲挖掘秘寶
玩家們可以使用當前投注額的100倍購買免費遊戲!進入免費遊戲再也不是虛幻。獎勵與一般遊戲相同,且購買後遊戲將自動開始,直到場次和獎金發放完畢為止。
有購買免費遊戲需求的玩家們,立即點擊「開始」,啟動神秘金字塔裡的古埃及祕寶吧!
【戰神塞特老虎機】購買特色
❰戰神賽特老虎機❱ 購買特色
戰神賽特試玩推薦
看完了❰戰神賽特老虎機❱介紹之後,玩家們是否也蓄勢待發要進入古埃及的世界,一探神奇秘寶探險之旅。
本次ATG賽特與線上娛樂城推薦第一名的富遊娛樂城合作,只需要加入會員,即可領取到168體驗金,免費試玩420轉!
https://seoboostlab.com/domain/megapesni.site
http://indianpharmacy.shop/# indian pharmacy online indianpharmacy.shop
Find healthy, delicious recipes and meal plan ideas from our test kitchen cooks and nutrition experts at SweetApple. Learn how to make healthier food choices every day. https://sweetapple.site/
RVVR is website dedicated to advancing physical and mental health through scientific research and proven interventions. Learn about our evidence-based health promotion programs. https://rvvr.us/
скрытый алюминиевый плинтус https://www.aljumynyevyj-napolnyj-plyntus.ru/.
canadian pharmacy world Pharmacies in Canada that ship to the US safe canadian pharmacy canadianpharmacy.pro
Демонтаж и снос частных домов с вывозом мусора в Москве и Московской области – lit9.ru. Снос дома вручную и спецтехникой производим по ценам ниже рынка за 1 день. Бесплатный выезд специалиста на объект.
https://muenchen.pennergame.de/redirect/?site=https://mp3name.me
https://indianpharmacy.shop/# reputable indian pharmacies indianpharmacy.shop
online pharmacy india
Скачать Зенит APK
https://www.bestfreeseotools.co/domain/mp3bit.pw
https://ip.openadmintools.com/en/mp3gid.co/
Что может быстро улучшить настроение в наши дни? Конечно же, хорошее кино. Что может быть лучше, чем заварить себе вкусны кофе или чай сесть в мягкое кресло, зайти на сайт HD-Novinka и смотреть фильмы 2024 онлайн бесплатно.
фильмы 2024 в хорошем качестве бесплатно
http://indianpharmacy.shop/# online pharmacy india indianpharmacy.shop
https://yuzhnoukrainsk.pogovorim.su/viewtopic.php?id=8848#p22925
цветочный магазин https://s-buketom.ru/
https://zagorie.mybb.ru/viewtopic.php?id=7989#p21151
https://mexicanpharmacy.win/# mexico drug stores pharmacies mexicanpharmacy.win
india pharmacy
OCNews.us covers local news in Orange County, CA, California and national news, sports, things to do and the best places to eat, business and the Orange County housing market. https://ocnews.us/
22000 Euro Kredit
Андрей Фролов, отличившийся на экономическом факультете МГУ, проявил себя как одаренный финансист в крупном банке. Его карьерный рост был обусловлен не только профессионализмом, но и способностью к нестандартному мышлению в сложных финансовых ситуациях. Сейчас Андрей применяет свои навыки для анализа рынка и разработки инвестиционных стратегий на mikro-zaim-online.ru, обеспечивая клиентам выгодные условия займов. Подробнее о нем и о предложениях займов можно узнать на https://mikro-zaim-online.ru/o-nas/
https://www.bingapis.com/images/search?q=pesnimp3.ws&first=113&count=28&form=IBASEP&cw=1702&ch=925
pharmacies in mexico that ship to usa Mexico pharmacy pharmacies in mexico that ship to usa mexicanpharmacy.win
Многие сайты обещают актуальную информацию о микрозаймах, но далеко не все держат слово. На mikro-zaim-online.ru Виктор Гардиенов и Ольга Штернец превращают обещания в реальность. Виктор с его пониманием клиентских нужд и Ольга с навыками в сфере маркетинга и PR предоставляют информацию, которая действительно помогает людям. Заходите на https://mikro-zaim-online.ru/o-nas/ и убедитесь в этом сами.
Великолепная БК в России и СНГ 1вин. Рекомендую!
The latest news on grocery chains, celebrity chefs, and fast food – plus reviews, cooking tips and advice, recipes, and more. https://megamenu.us/
View the latest from the world of psychology: from behavioral research to practical guidance on relationships, mental health and addiction. Find help from our directory of therapists, psychologists and counselors. https://therapisttoday.us/
https://gorod-moskva.ru/widgets/outside/?url=https://pesnimp3.ws
https://chemringeurope.de/__media__/js/netsoltrademark.php?d=mp3bit.pw
Virginia News: Your source for Virginia breaking news, sports, business, entertainment, weather and traffic https://virginiapost.us/
https://indianpharmacy.shop/# pharmacy website india indianpharmacy.shop
https://wktom.com/domain/mp3-top.net
https://scan.websitetec.com/domain/mp3-top.net
Какие информацию можно найти http://pro-tulu.ru/users/ytuhaxa на ukrlust Харьков? это невероятно удобно, когда в разгар мужской вечеринки вдруг хочется женского внимания.
https://aldsr.xyz/domain/mp3gid.co
epivir 150mg kaufen
http://indianpharmacy.shop/# india pharmacy indianpharmacy.shop
indian pharmacy online
global pharmacy canada Canada Pharmacy canadianpharmacymeds canadianpharmacy.pro
3D печать дает свободу воплощать в жизнь самые необычные идеи http://ryazanovskoe.ru/bitrix/click.php?goto=http://socialmarkz.com/story6141677/3d-%D0%BF%D0%B5%D1%87%D0%B0%D1%82%D1%8C-%D0%B4%D0%B5%D1%82%D0%B0%D0%BB%D0%B5%D0%B9
https://kas7.top/
http://mexicanpharmacy.win/# mexican rx online mexicanpharmacy.win
кондиционер сплит система http://www.multi-kondicionery.ru/.
https://www.nic.ru/whois/?searchWord=pesnimp3.ws
https://rg88.org/seth/
2024全新上線❰戰神賽特老虎機❱ – ATG賽特玩法說明介紹
❰戰神賽特老虎機❱是由ATG電子獨家開發的古埃及風格線上老虎機,在傳說中戰神賽特是「力量之神」與奈芙蒂斯女神結成連理,共同守護古埃及的奇幻秘寶,只有被選中的冒險者才能進入探險。
❰戰神賽特老虎機❱ – ATG賽特介紹
2024最新老虎機【戰神塞特】- ATG電子 X 富遊娛樂城
❰戰神賽特老虎機❱ – ATG電子
線上老虎機系統 : ATG電子
發行年分 : 2024年1月
最大倍數 : 51000倍
返還率 : 95.89%
支付方式 : 全盤倍數、消除掉落
最低投注金額 : 0.4元
最高投注金額 : 2000元
可否選台 : 是
可選台台數 : 350台
免費遊戲 : 選轉觸發+購買特色
❰戰神賽特老虎機❱ 賠率說明
戰神塞特老虎機賠率算法非常簡單,玩家們只需要不斷的轉動老虎機,成功消除物件即可贏分,得分賠率依賠率表計算。
當盤面上沒有物件可以消除時,倍數符號將會相加形成總倍數!該次旋轉的總贏分即為 : 贏分 X 總倍數。
積分方式如下 :
贏分=(單次押注額/20) X 物件賠率
EX : 單次押注額為1,盤面獲得12個戰神賽特倍數符號法老魔眼
贏分= (1/20) X 1000=50
以下為各個得分符號數量之獎金賠率 :
得分符號 獎金倍數 得分符號 獎金倍數
戰神賽特倍數符號聖甲蟲 6 2000
5 100
4 60 戰神賽特倍數符號黃寶石 12+ 200
10-11 30
8-9 20
戰神賽特倍數符號荷魯斯之眼 12+ 1000
10-11 500
8-9 200 戰神賽特倍數符號紅寶石 12+ 160
10-11 24
8-9 16
戰神賽特倍數符號眼鏡蛇 12+ 500
10-11 200
8-9 50 戰神賽特倍數符號紫鑽石 12+ 100
10-11 20
8-9 10
戰神賽特倍數符號神箭 12+ 300
10-11 100
8-9 40 戰神賽特倍數符號藍寶石 12+ 80
10-11 18
8-9 8
戰神賽特倍數符號屠鐮刀 12+ 240
10-11 40
8-9 30 戰神賽特倍數符號綠寶石 12+ 40
10-11 15
8-9 5
❰戰神賽特老虎機❱ 賠率說明(橘色數值為獲得數量、黑色數值為得分賠率)
ATG賽特 – 特色說明
ATG賽特 – 倍數符號獎金加乘
玩家們在看到盤面上出現倍數符號時,務必把握機會加速轉動ATG賽特老虎機,倍數符號會隨機出現2到500倍的隨機倍數。
當盤面無法在消除時,這些倍數總和會相加,乘上當時累積之獎金,即為最後得分總額。
倍數符號會出現在主遊戲和免費遊戲當中,玩家們千萬別錯過這個可以瞬間將得獎金額拉高的好機會!
ATG賽特 – 倍數符號獎金加乘
ATG賽特 – 倍數符號圖示
ATG賽特 – 進入神秘金字塔開啟免費遊戲
戰神賽特倍數符號聖甲蟲
❰戰神賽特老虎機❱ 免費遊戲符號
在古埃及神話中,聖甲蟲又稱為「死亡之蟲」,它被當成了天球及重生的象徵,守護古埃及的奇幻秘寶。
當玩家在盤面上,看見越來越多的聖甲蟲時,千萬不要膽怯,只需在牌面上斬殺4~6個ATG賽特免費遊戲符號,就可以進入15場免費遊戲!
在免費遊戲中若轉出3~6個聖甲蟲免費遊戲符號,可額外獲得5次免費遊戲,最高可達100次。
當玩家的累積贏分且盤面有倍數物件時,盤面上的所有倍數將會加入總倍數!
ATG賽特 – 選台模式贏在起跑線
為避免神聖的寶物被盜墓者奪走,富有智慧的法老王將金子塔內佈滿迷宮,有的設滿機關讓盜墓者寸步難行,有的暗藏機關可以直接前往存放神秘寶物的暗房。
ATG賽特老虎機設有350個機檯供玩家選擇,這是連魔龍老虎機、忍老虎機都給不出的機台數量,為的就是讓玩家,可以隨時進入神秘的古埃及的寶藏聖域,挖掘長眠已久的神祕寶藏。
【戰神塞特老虎機】選台模式
❰戰神賽特老虎機❱ 選台模式
ATG賽特 – 購買免費遊戲挖掘秘寶
玩家們可以使用當前投注額的100倍購買免費遊戲!進入免費遊戲再也不是虛幻。獎勵與一般遊戲相同,且購買後遊戲將自動開始,直到場次和獎金發放完畢為止。
有購買免費遊戲需求的玩家們,立即點擊「開始」,啟動神秘金字塔裡的古埃及祕寶吧!
【戰神塞特老虎機】購買特色
❰戰神賽特老虎機❱ 購買特色
戰神賽特試玩推薦
看完了❰戰神賽特老虎機❱介紹之後,玩家們是否也蓄勢待發要進入古埃及的世界,一探神奇秘寶探險之旅。
本次ATG賽特與線上娛樂城推薦第一名的富遊娛樂城合作,只需要加入會員,即可領取到168體驗金,免費試玩420轉!
https://analyzeseo.net/domain/pesnimp3.ws
https://kir4.top/
https://whois.ws/whois/mp3gid.co
https://canadianpharmacy.pro/# is canadian pharmacy legit canadianpharmacy.pro
best india pharmacy
Island Post is the website for a chain of six weekly newspapers that serve the North Shore of Nassau County, Long Island published by Alb Media. The newspapers are comprised of the Great Neck News, Manhasset Times, Roslyn Times, Port Washington Times, New Hyde Park Herald Courier and the Williston Times. Their coverage includes village governments, the towns of Hempstead and North Hempstead, schools, business, entertainment and lifestyle. https://islandpost.us/
https://azby.search.nifty.com/websearch/search?select=1077&cflg=%8C%9F%8D%F5&htmltype=2&Text=mp3name.me
https://kiz7.top/
tofranil 2mg
https://lon4.top/
Covering the latest beauty and fashion trends, relationship advice, wellness tips and more. https://gliz.us/
reputable mexican pharmacies online Medicines Mexico buying prescription drugs in mexico online mexicanpharmacy.win
Fresh, flavorful and (mostly) healthy recipes made for real, actual, every day life. Helping you celebrate the joy of food in a totally non-intimidating way. https://skillfulcook.us/
credit 3000 euros
https://deost.ru/bitrix/rk.php?goto=https://megapesni.site/
http://cialissansordonnance.shop/# Pharmacies en ligne certifiées
https://www.seoturboboost.com/domain/mp3bit.pw
Colorado breaking news, sports, business, weather, entertainment. https://denver-news.us/
п»їpharmacie en ligne Pharmacies en ligne certifiees Pharmacie en ligne sans ordonnance
Красивых девушек вызывают на разные праздники, на которых собирается очень много людей, которые любят зажигательные танцы http://agro-elektronika.phorum.pl/viewtopic.php?f=3&t=18824
Красивых девушек вызывают на разные праздники, на которых собирается очень много людей, которые любят зажигательные танцы https://sklad-slabov.ru/forum/user/4473/
Укладка плинтуса на пол
Основные правила установки плинтуса
Подбираем оптимальный плинтус для пола
Плюсы применения плинтуса на пол
Как установить плинтус на пол своими руками
Полезные советы по укладке плинтуса на пол
Варианты отделки для пола
Какой плинтус выбрать для разных напольных покрытий
Особенности укладки плинтуса на разных поверхностях
Правила подбора цвет и материал плинтуса для пола
Монтаж плинтуса на ламинат плинтуса на ламинированный пол
Материалы для плинтуса на пол
Идеи декорирования пола с помощью плинтуса
Секреты крепления плинтуса для надежной фиксации
Как работают монтажные компании с плинтусами на пол
Самодельные приспособления для монтажа плинтуса на пол
Частые ошибки при монтаже плинтуса
Стоимость на плинтус для пола
Топовые производители плинтусов для пола
Интерьерные решения с помощью плинтуса
большой выбор плинтусов http://ploskye-plyntusa.ru/.
http://pharmadoc.pro/# acheter médicaments à l’étranger
Укладка плинтуса на пол
Основные правила установки плинтуса
Выбираем правильный плинтус для пола
Преимущества использования плинтуса на пол
Способы укладки плинтус на пол своими руками
Советы профессионалов по укладке плинтуса на пол
Варианты отделки для пола
Какой плинтус выбрать для разных напольных покрытий
Особенности укладки плинтуса на разных поверхностях
Как выбрать цвет и материал плинтуса для пола
Лучшие способы установки плинтуса на ламинированный пол
Плинтусы из различных материалов на пол
Декоративные плинтусы пола с помощью плинтуса
Секреты крепления плинтуса для надежной фиксации
Профессиональная укладка плинтуса с плинтусами на пол
Самодельные приспособления для монтажа плинтуса на пол
Частые ошибки при монтаже плинтуса
Разбираемся с ценами на плинтус для пола
Топовые производители плинтусов для пола
Плинтус на пол как элемент дизайна с помощью плинтуса
современный плинтус на пол ploskye-plyntusa.ru.
https://www.insai.ru/ext_link?url=https://mp3-top.net
https://www.threatminer.org/domain.php?q=mp3new.top
Укладка плинтуса на пол
Основные правила установки плинтуса
Подбираем оптимальный плинтус для пола
Плюсы применения плинтуса на пол
Способы укладки плинтус на пол своими руками
Советы профессионалов по укладке плинтуса на пол
Варианты отделки для пола
Типы плинтусов для разных напольных покрытий
Нюансы монтажа плинтуса на разных поверхностях
Как выбрать цвет и материал плинтуса для пола
Монтаж плинтуса на ламинат плинтуса на ламинированный пол
Материалы для плинтуса на пол
Декоративные плинтусы пола с помощью плинтуса
Как закрепить плинтус на полу плинтуса для надежной фиксации
Как работают монтажные компании с плинтусами на пол
Как сделать инструмент для укладки плинтуса для монтажа плинтуса на пол
Частые ошибки при монтаже плинтуса
Стоимость на плинтус для пола
Топовые производители плинтусов для пола
Интерьерные решения с помощью плинтуса
широкие плинтусы для пола https://ploskye-plyntusa.ru.
Healthcare Blog provides news, trends, jobs and resources for health industry professionals. We cover topics like healthcare IT, hospital administration, polcy
п»їpharmacie en ligne Levitra sans ordonnance 24h acheter mГ©dicaments Г l’Г©tranger
pharmacie ouverte: pharmacie en ligne pas cher – Pharmacie en ligne livraison gratuite
https://www.addtoany.com/share_save?linkname=&linkurl=mp3gid.co
First coastline with a private beach in Gaziveren coastal heaven cyprus.
Step into the Kaleidoscope of Desire at Erotoons.net. Here, stories aren’t just told; they are vividly painted across the canvas of imagination, inviting men and women alike to bask in their glory. Our collection is a symphony of adult tales, each resonating with the tune of temptation and allure. And the ticket to this grand show? It’s on us. Erotoons.net doesn’t just offer free adult comics; we present a world where every turn is a new discovery, a journey accessible to everyone seeking to quench their thirst for erotic adventures.
In search of a portal to a world of fantasy and passion? Erotoons.net is your gateway to the finest sultry summer porn comic , where every story is an adventure.
https://website.informer.com/mp3new.top
tarkista tästä
BioPharma Blog provides news and analysis for biotech and biopharmaceutical executives. We cover topics like clinical trials, drug discovery and development, pharma marketing, FDA approvals and regulations, and more. https://biopharmablog.us/
в обществе, где время года и качество решают всё, private models становится вашим незаменимым спутником, http://remont-okon.od.ua/index.php?subaction=userinfo&user=yrojut предоставляя услуги элитного эскорта Москве.
diltiazem cream
Viagra gГ©nГ©rique sans ordonnance en pharmacie: viagra sans ordonnance – Viagra homme prix en pharmacie
https://htmlweb.ru/analiz/?xss=ef3abd959d51a13444705ab88c42e88d&url=mp3new.top
https://myseotools.pro/domain/megapesni.site
pharmacie ouverte 24/24 kamagra en ligne Pharmacie en ligne fiable
https://gorod-moskva.ru/widgets/outside/?url=https://mp3name.me/
https://gorod-moskva.ru/widgets/outside/?url=https://mp3name.me
http://pharmadoc.pro/# Pharmacie en ligne pas cher
https://aljalaa.com/__media__/js/netsoltrademark.php?d=megapesni.site
https://mainkeys.net/mp3-top.net/
https://deost.ru/bitrix/rk.php?goto=https://mp3bit.pw/
https://seo.blueonnix.com/domain/mp3new.top
Latest Denver news, top Colorado news and local breaking news from Denver News, including sports, weather, traffic, business, politics, photos and video. https://denver-news.us/
pharmacie ouverte 24/24 Pharmacie en ligne France pharmacie ouverte
https://pharmadoc.pro/# Pharmacie en ligne livraison 24h
Meilleur Viagra sans ordonnance 24h: Viagra sans ordonnance 24h – Viagra pas cher paris
http://psyho2039.8ua.ru/
%%
Here is my homepage … http://n90329za.bget.ru/index.php?subaction=userinfo&user=aqusetydy
купить аккаунты bongacams с токенами
аккаунт бонго с токенами
Приближался сезон охоты, и мне срочно нужно было обновить свой охотничий инвентарь. Чтобы не упустить возможность, я взял займ и приобрел необходимое снаряжение, чтобы быть готовым к охоте.
La popularidad de los casinos bonos bienvenida gratis sin depósito en Chile ha ido en aumento. Estos casinos ofrecen a los nuevos jugadores la oportunidad de probar sus juegos sin el riesgo de perder dinero real. https://casino-bonos-chile.cl/bienvenida-gratis-bono-online-casino-sin-deposito/
купить токены
Looking for quick and easy dinner ideas? Browse 100
https://zeerank.com/domain/mp3name.me
1 x bet зеркало– это популярная букмекерская контора, предоставляющая широкий выбор ставок на спорт и казино. Сайт обладает удобным интерфейсом, мобильной версией и приложением для удобства пользователей. 1xBet также известен разнообразными акциями и бонусами, делая игровой опыт более захватывающим.
купить аккаунты с токенами бонгакамс
Pharmacie en ligne fiable: pharmacie en ligne – Pharmacie en ligne pas cher
Сегодня, чтобы купить китайские цветы, вам не обязательно ехать в Поднебесную. Многие интернет-магазины предлагают великое множество вариантов.
китайская роза цветок
Nikolaev Vyacheslav https://www.nikolaev-vyacheslav-konstantinovich.biography-wiki.com/.
SildГ©nafil 100 mg prix en pharmacie en France viagrasansordonnance.pro Viagra pas cher livraison rapide france
Инструкция по укладке плинтуса на пол
Основные правила установки плинтуса
Выбираем правильный плинтус для пола
Плюсы применения плинтуса на пол
Способы укладки плинтус на пол своими руками
Полезные советы по укладке плинтуса на пол
Варианты отделки для пола
Какой плинтус выбрать для разных напольных покрытий
Нюансы монтажа плинтуса на разных поверхностях
Как выбрать цвет и материал плинтуса для пола
Монтаж плинтуса на ламинат плинтуса на ламинированный пол
Материалы для плинтуса на пол
Декоративные плинтусы пола с помощью плинтуса
Как закрепить плинтус на полу плинтуса для надежной фиксации
Как работают монтажные компании с плинтусами на пол
Самодельные приспособления для монтажа плинтуса на пол
Как избежать ошибок при укладке плинтуса при монтаже плинтуса
Стоимость на плинтус для пола
Топовые производители плинтусов для пола
Плинтус на пол как элемент дизайна с помощью плинтуса
размеры плинтусов для пола http://ploskye-plyntusa.ru/.
Das Oktoberfest in Munchen ist nicht nur fur seine ausgelassene Stimmung und das beruhmte Bier bekannt, sondern auch als ein Ort, an dem Kellner und Bedienungen oft erstaunlich hohe Einkommen erzielen konnen. In diesem Artikel beleuchten wir, was eine Bedienung auf dem Oktoberfest verdienen kann und welche Faktoren dabei eine Rolle spielen.
Hohe Einkommensmoglichkeiten
Das Einkommen einer Bedienung auf dem Oktoberfest kann deutlich hoher sein als in vielen anderen Gastronomiebereichen. Dies ist auf mehrere Faktoren zuruckzufuhren:
was verdient eine wiesn bedienung
Hohes Trinkgeld: Die festliche und gro?zugige Atmosphare des Oktoberfests fuhrt dazu, dass Gaste oft bereit sind, hohere Trinkgelder zu geben. Diese konnen einen signifikanten Teil des Gesamteinkommens ausmachen.
Gro?er Umsatz: Aufgrund der hohen Besucherzahlen und der Kultur des Biertrinkens auf dem Fest konnen Bedienungen eine gro?e Anzahl an Bestellungen in kurzer Zeit abwickeln, was zu hoherem Verdienst fuhrt.
Lange Arbeitszeiten: Wahrend des Oktoberfests arbeiten die Bedienungen oft lange Schichten, die bis zu 12 Stunden oder mehr pro Tag betragen konnen. Diese langen Arbeitszeiten konnen das Gesamteinkommen erhohen, auch wenn sie korperlich und geistig anstrengend sind.
Durchschnittlicher Verdienst
Es ist schwierig, einen genauen Durchschnittsverdienst festzulegen, da dieser von verschiedenen Faktoren wie der Erfahrung der Bedienung, dem spezifischen Zelt, in dem sie arbeitet, und dem individuellen Trinkgeldverhalten der Gaste abhangt. Allerdings wird berichtet, dass Bedienungen auf dem Oktoberfest in guten Jahren mehrere tausend Euro verdienen konnen, vor allem durch Trinkgelder.
can i get generic mobic without dr prescription
%%
My web blog :: https://xn--45-1lclfk1f.xn--p1ai/2024/01/24/sovremennaya-tipografiya-predostavlyaet-vozmozhnost-3w3v/
http://cialissansordonnance.shop/# pharmacie en ligne
First coastline with a private beach coastal heaven north cyprus.
Welcome to Erotoons.net, where the carousel of erotic comics spins, offering a ride through countless genres and styles. Each turn brings a new vista, a new thrill, perfectly crafted for the adult man’s diverse tastes. From the soft whispers of romantic tales to the thunderous roars of wild adventures, our collection is a spectrum of excitement. Here, every enthusiast of adult comics finds their heart’s desire, free to explore a universe where fantasy and reality dance in a beautiful embrace. Join the carousel and let your senses soar.
If your idea of relaxation includes a touch of adult adventure, Erotoons.net is where you should be. Our rule 63 porn are tailored for your entertainment.
SildГ©nafil 100 mg prix en pharmacie en France viagra sans ordonnance Sildenafil teva 100 mg sans ordonnance
Pharmacie en ligne livraison 24h: Acheter Cialis 20 mg pas cher – Pharmacie en ligne fiable
%%
My page – Сиделка с проживанием
Why limit your access to world-class adult entertainment? Erotoons.net breaks the mold by offering an extensive range of adult comics for both men and women. Our diverse collection caters to a wide array of tastes, ensuring that everyone above 18 finds something tantalizing. And the best part? It’s completely free. We believe in providing high-quality, erotic content without barriers. Why choose between quality and affordability when Erotoons.net offers both? Join us for an unparalleled experience in adult entertainment.
Are you on the lookout for something more than just ordinary comics? Erotoons.net has just what you need with our exclusive katie’s training porn comic .
http://pharmadoc.pro/# Pharmacie en ligne livraison gratuite
Анализ данных: Постоянный анализ конкурентов, запрашиваемых сочетаний слов, http://vashtehnadzor.ru/index.php?subaction=userinfo&user=ugibyp трафика и повадок пользователей на сайте с целью оптимизации площадки и применяемых при раскрутке инструментов.
Pharmacie en ligne pas cher: levitra generique sites surs – pharmacie ouverte 24/24
buy inderal
Я давно искал надежный источник информации о займах на карту. Сайт postabank.ru оказался настоящим спасением. С его помощью я смог найти лучшие МФО и оформить займ без отказа.
Pharmacies en ligne certifiГ©es Medicaments en ligne livres en 24h Pharmacie en ligne France
Однажды, когда моя машина сломалась вдали от дома, мне понадобилась срочная ремонтная помощь. Я обратился к постабанку и взял займ, чтобы покрыть расходы на ремонт и вернуться на дорогу.
Извините, я подумал и удалил свою мысль
если вам нужно няня, владеющая всеми предписанными навыками ухода за малышом, основами первой врачебной помощи в критической ситуации, современными методиками жизни отпрысков и знаниями детской кухни, Служба сиделок мы постараемся оказать.
https://pharmadoc.pro/# Pharmacie en ligne France
colchicine canada
Thanks for sharing, this is a fantastic blog post.Really thank you! Much obliged.
My website: порно с профессором
pharmacie ouverte 24/24: cialissansordonnance.shop – Pharmacies en ligne certifiГ©es
https://levitrasansordonnance.pro/# acheter médicaments à l’étranger
Рекомендую иммено эту надежную БК 1вин.
п»їpharmacie en ligne: cialis sans ordonnance – Pharmacie en ligne France
доставка цветов в новосибирске первомайский район https://s-buketom.ru/
Какие документы нужны для установки кондиционера
цена установки кондиционера https://www.kondicionery-s-ustanovkoj.ru/.
Где выгоднее купить кондиционер
купить кондиционер lg ustanovka-split-sistem.ru.
For all those trying to get a distinctive and enjoyable entertainment expertise, the entire world of striptease inside the north delivers a unique allure https://rafaelesfp53197.snack-blog.com/24880698/private-pleasantries-strippers-to-your-home-for-a-night-to-remember
Кондиционер в офисе: особенности установки и эксплуатации
mitsubishi electric кондиционер http://www.kondicionery-s-ustanovkoj.ru/.
For all those trying to get a distinctive and enjoyable entertainment expertise, the entire world of striptease inside the north delivers a unique allure https://jaidenuwpa32186.wizzardsblog.com/24965367/booking-beautiful-strippers-for-your-party
Отличная статья, благодарю!
В качестве благодарности поделюсь с вами информацией: деревянные наличники на окна в Питере для коттеджей являются превосходных выбором среди владельцев коттеджей.
Резные наличники из дерева для домов – это превосходный вариант, который сочетает в себе отличный внешний вид, прочность и экологию. Если у вас есть желание придать своему коттеджу превосходный вшений вид, рассмотрите наличники из дерева.
В Санкт-Петербурге работает много организаций, специализирующихся на изготовлении и установке деревянных наличников. Одна из них – компания КубЭра. Предлагает большой ассортимент наличников на любой вкус.
Как установить кондиционер в офисе?
фреон для кондиционера https://www.kondicionery-s-ustanovkoj.ru.
Viagra homme prix en pharmacie: Meilleur Viagra sans ordonnance 24h – Viagra pas cher livraison rapide france
Кондиционер купить и установить: действуй правильно
цены на кондиционеры https://ustanovka-split-sistem.ru.
Das Oktoberfest in Munchen ist nicht nur fur seine ausgelassene Stimmung und das beruhmte Bier bekannt, sondern auch als ein Ort, an dem Kellner und Bedienungen oft erstaunlich hohe Einkommen erzielen konnen. In diesem Artikel beleuchten wir, was eine Bedienung auf dem Oktoberfest verdienen kann und welche Faktoren dabei eine Rolle spielen.
Hohe Einkommensmoglichkeiten
Das Einkommen einer Bedienung auf dem Oktoberfest kann deutlich hoher sein als in vielen anderen Gastronomiebereichen. Dies ist auf mehrere Faktoren zuruckzufuhren:
verdienst oktoberfest kellner
Hohes Trinkgeld: Die festliche und gro?zugige Atmosphare des Oktoberfests fuhrt dazu, dass Gaste oft bereit sind, hohere Trinkgelder zu geben. Diese konnen einen signifikanten Teil des Gesamteinkommens ausmachen.
Gro?er Umsatz: Aufgrund der hohen Besucherzahlen und der Kultur des Biertrinkens auf dem Fest konnen Bedienungen eine gro?e Anzahl an Bestellungen in kurzer Zeit abwickeln, was zu hoherem Verdienst fuhrt.
Lange Arbeitszeiten: Wahrend des Oktoberfests arbeiten die Bedienungen oft lange Schichten, die bis zu 12 Stunden oder mehr pro Tag betragen konnen. Diese langen Arbeitszeiten konnen das Gesamteinkommen erhohen, auch wenn sie korperlich und geistig anstrengend sind.
Durchschnittlicher Verdienst
Es ist schwierig, einen genauen Durchschnittsverdienst festzulegen, da dieser von verschiedenen Faktoren wie der Erfahrung der Bedienung, dem spezifischen Zelt, in dem sie arbeitet, und dem individuellen Trinkgeldverhalten der Gaste abhangt. Allerdings wird berichtet, dass Bedienungen auf dem Oktoberfest in guten Jahren mehrere tausend Euro verdienen konnen, vor allem durch Trinkgelder.
Pills information. Cautions.
fluoxetine without dr prescription
Everything about medicament. Get now.
Деревянные дома под ключ
Дома АВС – Ваш уютный уголок
Мы строим не просто дома, мы создаем пространство, где каждый уголок будет наполнен комфортом и радостью жизни. Наш приоритет – не просто предоставить место для проживания, а создать настоящий дом, где вы будете чувствовать себя счастливыми и уютно.
В нашем информационном разделе “ПРОЕКТЫ” вы всегда найдете вдохновение и новые идеи для строительства вашего будущего дома. Мы постоянно работаем над тем, чтобы предложить вам самые инновационные и стильные проекты.
Мы убеждены, что основа хорошего дома – это его дизайн. Поэтому мы предоставляем услуги опытных дизайнеров-архитекторов, которые помогут вам воплотить все ваши идеи в жизнь. Наши архитекторы и персональные консультанты всегда готовы поделиться своим опытом и предложить функциональные и комфортные решения для вашего будущего дома.
Мы стремимся сделать весь процесс строительства максимально комфортным для вас. Наша команда предоставляет детализированные сметы, разрабатывает четкие этапы строительства и осуществляет контроль качества на каждом этапе.
Для тех, кто ценит экологичность и близость к природе, мы предлагаем деревянные дома премиум-класса. Используя клееный брус и оцилиндрованное бревно, мы создаем уникальные и здоровые условия для вашего проживания.
Тем, кто предпочитает надежность и многообразие форм, мы предлагаем дома из камня, блоков и кирпичной кладки.
Для практичных и ценящих свое время людей у нас есть быстровозводимые каркасные дома и эконом-класса. Эти решения обеспечат вас комфортным проживанием в кратчайшие сроки.
С Домами АВС создайте свой уютный уголок, где каждый момент жизни будет наполнен радостью и удовлетворением
Где купить качественный кондиционер
цены на кондиционеры https://www.ustanovka-split-sistem.ru.
http://levitrasansordonnance.pro/# acheter médicaments à l’étranger
acheter mГ©dicaments Г l’Г©tranger: PharmaDoc – Pharmacie en ligne livraison 24h
can you get generic valtrex pills
Pharmacies en ligne certifiГ©es Acheter Cialis Pharmacie en ligne sans ordonnance
https://moravian.bucknell.edu/transcriptions/index.php?title=User:MarianaPalmos15
East Bay News is the leading source of breaking news, local news, sports, entertainment, lifestyle and opinion for Contra Costa County, Alameda County, Oakland and beyond https://eastbaynews.us/
печать фото цена
http://www.diywiki.org/index.php/User:HilarioPrimeaux
http://www.miragearb.com/wiki/User:JacelynEmbry895
печать фото оптом
https://ptwiki.blitwise.com/index.php/Ofkleasing.ru
Medicines information for patients. Brand names.
buy neurontin
Actual information about drug. Get information here.
https://elearnportal.science/wiki/Ptleasing.ru
dostinex 5mg
печать больших фотографий москва
https://www.recruiterwiki.de/Ptleasing.ru
pharmacie ouverte: Pharmacies en ligne certifiГ©es – Pharmacies en ligne certifiГ©es
http://levitrasansordonnance.pro/# pharmacie ouverte 24/24
http://saju.codeway.kr/index.php/Ofkleasing.ru
pharmacie ouverte 24/24 Pharmacie en ligne livraison rapide Pharmacie en ligne livraison rapide
https://pipewiki.org/app/index.php/User:TinaKinsela87
Мы рады предложить большой выбор производственного оборудования, прямые поставки лизинг серверного оборудования
Мы рады предложить большой выбор производственного оборудования, прямые поставки оборудование для мойки самообслуживания в лизинг
Viagra sans ordonnance 24h suisse: Viagra sans ordonnance 24h – Viagra en france livraison rapide
список центров обслуживания телефонов в москве
http://pharmadoc.pro/# Pharmacies en ligne certifiées
Установка кондиционера: важные аспекты безопасности
кондиционер цена https://www.kondicionery-s-ustanovkoj.ru.
отремонтировать телефон поблизости
ATG戰神賽特
2024全新上線❰戰神賽特老虎機❱ – ATG賽特玩法說明介紹
❰戰神賽特老虎機❱是由ATG電子獨家開發的古埃及風格線上老虎機,在傳說中戰神賽特是「力量之神」與奈芙蒂斯女神結成連理,共同守護古埃及的奇幻秘寶,只有被選中的冒險者才能進入探險。
❰戰神賽特老虎機❱ – ATG賽特介紹
2024最新老虎機【戰神塞特】- ATG電子 X 富遊娛樂城
❰戰神賽特老虎機❱ – ATG電子
線上老虎機系統 : ATG電子
發行年分 : 2024年1月
最大倍數 : 51000倍
返還率 : 95.89%
支付方式 : 全盤倍數、消除掉落
最低投注金額 : 0.4元
最高投注金額 : 2000元
可否選台 : 是
可選台台數 : 350台
免費遊戲 : 選轉觸發+購買特色
❰戰神賽特老虎機❱ 賠率說明
戰神塞特老虎機賠率算法非常簡單,玩家們只需要不斷的轉動老虎機,成功消除物件即可贏分,得分賠率依賠率表計算。
當盤面上沒有物件可以消除時,倍數符號將會相加形成總倍數!該次旋轉的總贏分即為 : 贏分 X 總倍數。
積分方式如下 :
贏分=(單次押注額/20) X 物件賠率
EX : 單次押注額為1,盤面獲得12個戰神賽特倍數符號法老魔眼
贏分= (1/20) X 1000=50
以下為各個得分符號數量之獎金賠率 :
得分符號 獎金倍數 得分符號 獎金倍數
戰神賽特倍數符號聖甲蟲 6 2000
5 100
4 60 戰神賽特倍數符號黃寶石 12+ 200
10-11 30
8-9 20
戰神賽特倍數符號荷魯斯之眼 12+ 1000
10-11 500
8-9 200 戰神賽特倍數符號紅寶石 12+ 160
10-11 24
8-9 16
戰神賽特倍數符號眼鏡蛇 12+ 500
10-11 200
8-9 50 戰神賽特倍數符號紫鑽石 12+ 100
10-11 20
8-9 10
戰神賽特倍數符號神箭 12+ 300
10-11 100
8-9 40 戰神賽特倍數符號藍寶石 12+ 80
10-11 18
8-9 8
戰神賽特倍數符號屠鐮刀 12+ 240
10-11 40
8-9 30 戰神賽特倍數符號綠寶石 12+ 40
10-11 15
8-9 5
❰戰神賽特老虎機❱ 賠率說明(橘色數值為獲得數量、黑色數值為得分賠率)
ATG賽特 – 特色說明
ATG賽特 – 倍數符號獎金加乘
玩家們在看到盤面上出現倍數符號時,務必把握機會加速轉動ATG賽特老虎機,倍數符號會隨機出現2到500倍的隨機倍數。
當盤面無法在消除時,這些倍數總和會相加,乘上當時累積之獎金,即為最後得分總額。
倍數符號會出現在主遊戲和免費遊戲當中,玩家們千萬別錯過這個可以瞬間將得獎金額拉高的好機會!
ATG賽特 – 倍數符號獎金加乘
ATG賽特 – 倍數符號圖示
ATG賽特 – 進入神秘金字塔開啟免費遊戲
戰神賽特倍數符號聖甲蟲
❰戰神賽特老虎機❱ 免費遊戲符號
在古埃及神話中,聖甲蟲又稱為「死亡之蟲」,它被當成了天球及重生的象徵,守護古埃及的奇幻秘寶。
當玩家在盤面上,看見越來越多的聖甲蟲時,千萬不要膽怯,只需在牌面上斬殺4~6個ATG賽特免費遊戲符號,就可以進入15場免費遊戲!
在免費遊戲中若轉出3~6個聖甲蟲免費遊戲符號,可額外獲得5次免費遊戲,最高可達100次。
當玩家的累積贏分且盤面有倍數物件時,盤面上的所有倍數將會加入總倍數!
ATG賽特 – 選台模式贏在起跑線
為避免神聖的寶物被盜墓者奪走,富有智慧的法老王將金子塔內佈滿迷宮,有的設滿機關讓盜墓者寸步難行,有的暗藏機關可以直接前往存放神秘寶物的暗房。
ATG賽特老虎機設有350個機檯供玩家選擇,這是連魔龍老虎機、忍老虎機都給不出的機台數量,為的就是讓玩家,可以隨時進入神秘的古埃及的寶藏聖域,挖掘長眠已久的神祕寶藏。
【戰神塞特老虎機】選台模式
❰戰神賽特老虎機❱ 選台模式
ATG賽特 – 購買免費遊戲挖掘秘寶
玩家們可以使用當前投注額的100倍購買免費遊戲!進入免費遊戲再也不是虛幻。獎勵與一般遊戲相同,且購買後遊戲將自動開始,直到場次和獎金發放完畢為止。
有購買免費遊戲需求的玩家們,立即點擊「開始」,啟動神秘金字塔裡的古埃及祕寶吧!
【戰神塞特老虎機】購買特色
❰戰神賽特老虎機❱ 購買特色
戰神賽特試玩推薦
看完了❰戰神賽特老虎機❱介紹之後,玩家們是否也蓄勢待發要進入古埃及的世界,一探神奇秘寶探險之旅。
本次ATG賽特與線上娛樂城推薦第一名的富遊娛樂城合作,只需要加入會員,即可領取到168體驗金,免費試玩420轉!
зеркало мостбет
%%
Here is my site; https://weburologiya.ru/kak-nayti-horoshuyu-sidelku-s-prozhivaniem.html
Are you over the hunt for an ideal approach to elevate your future bachelor celebration https://charlierldr64219.blogtov.com/5331182/book-strippers-and-make-your-party-unforgettable
buy prednisolone 40 mg
Are you over the hunt for an ideal approach to elevate your future bachelor celebration https://messiahnyjs64984.blogoscience.com/30651016/exploring-the-best-strippers-in-the-north-for-your-bachelor-blowout
acheter mГ©dicaments Г l’Г©tranger levitra generique pharmacie ouverte
Pills information. What side effects can this medication cause?
neurontin
All about medicine. Get here.
https://www.instagram.com/asiapsiholog_family/
Do whatever you want. Steal cars, drive tanks and helicopters, defeat gangs. It’s your city! https://play.google.com/store/apps/details?id=com.gangster.city.open.world
Pharmacie en ligne livraison rapide: Acheter Cialis 20 mg pas cher – acheter medicament a l etranger sans ordonnance
Рекомендую только эту надежную БК 1вин.
https://pharmadoc.pro/# pharmacie ouverte 24/24
acheter medicament a l etranger sans ordonnance kamagra livraison 24h Pharmacies en ligne certifiГ©es
how to buy compazine
pharmacie ouverte: Levitra acheter – Pharmacie en ligne France
ramen bet
http://pharmadoc.pro/# acheter médicaments à l’étranger
can you buy generic lisinopril for sale
Где купить качественный кондиционер
промышленные кондиционеры https://ustanovka-split-sistem.ru.
News from the staff of the LA Reporter, including crime and investigative coverage of the South Bay and Harbor Area in Los Angeles County. https://lareporter.us/
Hi, i feel that i noticed you visited my weblog so i got here to return the
want?.I’m trying to find issues to improve my website!I suppose
its ok to make use of some of your concepts!!
PЕЇjДЌka 16000 KДЌ
Your means of telling everything in this
paragraph is really fastidious, all can without difficulty know it, Thanks a lot.
http://clomiphene.icu/# can i get clomid online
buy azithromycin zithromax zithromax 250mg zithromax purchase online
обслуживание кондиционеров https://www.internet-magazin-kondicionerov.ru/.
Ultra luxury apartments and high-spec duplexes in the complex of Cavalli Couture Damac on the banks of the Dubai Water Canal. Developer DAMAC Properties together with the Cavalli brand offers units for sale at favourable prices.
купить с установкой кондиционер https://www.internet-magazin-kondicionerov.ru.
Fence Horizont Looking for a reliable fence supplier? Fence Horizont offers top-quality fences for all your needs. Check out our wide range of options today!
http://ivermectin.store/# buy stromectol uk
Лизинг оборудования – рейтинг компаний в 2024 году: отзывы, условия, стоимость и быстрое оформление онлайн-заявки лизинг бу оборудования для юридических лиц
Garden bed Double Looking for a high-quality garden bed? Check out our durable and stylish uМІnМІdМІeМІrМІlМІiМІnМІeМІDouble garden beduМІnМІdМІeМІrМІlМІiМІnМІeМІ, perfect for enhancing your outdoor space.
Лизинг оборудования – рейтинг компаний в 2024 году: отзывы, условия, стоимость и быстрое оформление онлайн-заявки получить оборудование в лизинг
phone Porn
Hello everyone! I’m excited to invite you all to join me on Medium where I delve into the dynamic and fascinating world of Dubai real estate. It’s a realm filled with growth, opportunities, and intriguing market trends. Whether you’re an investor, a real estate enthusiast, or simply curious about the property landscape in Dubai, my articles offer insights and analyses that you won’t want to miss. Let’s explore the vibrant real estate market of Dubai together! Follow me on Medium for the latest updates and in-depth discussions. See you there!
Ремонт телефонов Xiaomi, Haier, Huawei и другие в сервисном центре где починить телефон дешево
Cassette ceiling from the mehbud factory The cassette ceiling from the mehbud factory is a versatile and stylish choice for any space. Upgrade your interior with this unique design.
where to buy generic clomid now: buying cheap clomid without insurance – where to get generic clomid without dr prescription
Ремонт телефонов Xiaomi, Haier, Huawei и другие в сервисном центре ремонт телефонов дешево в москве
Fence Color Selection Fence Color Selection: Using The Ral System For Perfect Design.
New Porn
В этом что-то есть. Спасибо за помощь в этом вопросе, может я тоже могу Вам чем то помочь?
Причем нет верхнего предела (границ) заработка. настоящим идеей будет составление резюме русифицированы. Дети в силах добиться качественное образование, работа Омск свежие вакансии супруга-супруг тоже трудоустроиться.
stromectol pills: stromectol for head lice – ivermectin 6mg dosage
Thanks-a-mundo for the post.Really thank you! Awesome.
My website: порно по категориям на русском
Great article. I’m experiencing some of these issues as well..
http://azithromycin.bid/# zithromax buy online no prescription
ivermectin 6 mg tablets cost of ivermectin stromectol uk
Nikolaev http://www.natureworldnews.com/articles/57820/20230802/vyacheslav-konstantinovich-nikolaev.htm
http://prednisonetablets.shop/# prednisone 10mg cost
where buy lisinopril without a prescription
where can i get prednisone over the counter: prednisone pak – price for 15 prednisone
кондиционер магазин https://www.internet-magazin-kondicionerov.ru/.
prednisone 10mg tablet cost: prednisone 20mg prescription cost – prednisone 20mg prices
Medication information. Generic Name.
seroquel
Everything what you want to know about drug. Read information here.
ivermectin 500mg stromectol covid ivermectin stromectol
http://xn--j1abfeccmj1d1c.xn--p1ai/forum/?PAGE_NAME=profile_view&UID=18602
hydroxyzine usa
https://master-santech-kras.ru/
https://guebsch.me/index.php?title=Benutzer:DanieleFosbery0
українські інтернет казино
надійні онлайн казино
Легальні казино в Україні стають важливим аспектом розвитку гральної індустрії у країні. Законодавчі зміни в останні роки створили сприятливе середовище для розвитку онлайн та оффлайн гральних закладів. Існують декілька ключових факторів, які роблять легальні казино в Україні привабливими для гравців та інвесторів.
Однією з основних переваг є регулювання грального бізнесу державою, що гарантує чесність та безпеку для гравців. Легальність казино в Україні відображається в ретельних перевірках та ліцензіях, які видаються органами влади. Це забезпечує гравцям впевненість у тому, що їхні фінансові та особисті дані захищені.
Завдяки інноваційним технологіям, легальні казино в Україні швидко адаптуються до потреб гравців. Онлайн-платформи надають можливість грати в улюблені азартні ігри зручно та безпечно прямо з дому чи мобільного пристрою. Завдяки високій якості графіки та захоплюючому геймплею, гравці можуть насолоджуватися атмосферою класичних казино в будь-якому місці та в будь-який час.
Партнерські програми та бонуси, що пропонують легальні казино в Україні, роблять гру ще більш привабливою для новачків. Інколи це може включати в себе бездепозитні бонуси, фріспіни або інші ексклюзивні пропозиції для реєстрації. Гравець може отримати додатковий стимул для гри та виграшу, що робить гральний процес ще захопливішим.
Легальні казино в Україні також сприяють розвитку туризму, приваблюючи гравців з інших країн. Вони стають місцем для соціальних подій, турнірів та розваг, що сприяє позитивному іміджу країни та збільшенню її привабливості для іноземних туристів.
У світі розваг та азарту, легальні казино в Україні виступають як підтримуючий стовп розвитку економіки. Збалансована політика та тісне співробітництво між гральними операторами та державними органами сприяють позитивному розвитку цієї індустрії. Гравці отримують можливість насолоджуватися азартом в безпечному та легальному середовищі, що робить казино в Україні привабливим вибором для всіх шанувальників азартних розваг.
https://modern-design-ideas.com/lego-affiliate-program-best-deals/
Вскрытие замков в любое время суток оперативно аварийное вскрытие замков и без повреждений.
Рекомендую самую надежную БК 1вин.
Бытовая техника, ноутбуки, смартфоны и многое другое! Цены по карману каждому ремешки для apple watch
Вскрытие замков в любое время суток оперативно экстренная служба вскрытия замков и без повреждений.
фотокнига с рождения
http://clomiphene.icu/# where can i buy generic clomid without dr prescription
generic omnicef for sale
%%
Also visit my page; Агентство нянь
http://gadimark.free.fr/wiki/index.php?title=Metal-lesnoy.ru
фотокнига заказать москва недорого
Бытовая техника, ноутбуки, смартфоны и многое другое! Цены по карману каждому айфон 11 про макс в молдове
buy prednisone with paypal canada 10 mg prednisone tablets buy prednisone 5mg canada
http://gb3nq.co.uk/wiki/index.php?title=Metal-lesnoy.ru
I’ve read several excellent stuff here. Certainly price
bookmarking for revisiting. I wonder how much attempt you set to make such a wonderful informative web site.
Drug information for patients. Cautions.
colchicine
Best what you want to know about medicine. Get information here.
фотокниги недорого
https://lovewiki.faith/wiki/Metal-lesnoy.ru?action=edit
where to get cheap clomid: where to buy generic clomid without insurance – how can i get clomid for sale
http://ivermectin.store/# ivermectin 0.2mg
фотокниги для детей
https://oldmerin.club/board/index.php?app=gallery&image=14953
Весьма хорошая идея
Опыт Агентство нянь взаимодействия с грудничками. для дома 130 м2 требуется домработница – помощница мамы с малышом нескольких лет режимы работы вахта 7/7-14/14 с проживанием.
credito 700 euros
ivermectin 1% cream generic: ivermectin oral solution – ivermectin brand
https://incardio.cuas.at/wiki/index.php/User:KeenanA4904
top artikel
Дома АВС – Ваш уютный уголок
Мы строим не просто дома, мы создаем пространство, где каждый уголок будет наполнен комфортом и радостью жизни. Наш приоритет – не просто предоставить место для проживания, а создать настоящий дом, где вы будете чувствовать себя счастливыми и уютно.
В нашем информационном разделе “ПРОЕКТЫ” вы всегда найдете вдохновение и новые идеи для строительства вашего будущего дома. Мы постоянно работаем над тем, чтобы предложить вам самые инновационные и стильные проекты.
Мы убеждены, что основа хорошего дома – это его дизайн. Поэтому мы предоставляем услуги опытных дизайнеров-архитекторов, которые помогут вам воплотить все ваши идеи в жизнь. Наши архитекторы и персональные консультанты всегда готовы поделиться своим опытом и предложить функциональные и комфортные решения для вашего будущего дома.
Мы стремимся сделать весь процесс строительства максимально комфортным для вас. Наша команда предоставляет детализированные сметы, разрабатывает четкие этапы строительства и осуществляет контроль качества на каждом этапе.
Для тех, кто ценит экологичность и близость к природе, мы предлагаем деревянные дома премиум-класса. Используя клееный брус и оцилиндрованное бревно, мы создаем уникальные и здоровые условия для вашего проживания.
Тем, кто предпочитает надежность и многообразие форм, мы предлагаем дома из камня, блоков и кирпичной кладки.
Для практичных и ценящих свое время людей у нас есть быстровозводимые каркасные дома и эконом-класса. Эти решения обеспечат вас комфортным проживанием в кратчайшие сроки.
С Домами АВС создайте свой уютный уголок, где каждый момент жизни будет наполнен радостью и удовлетворением
zerit saliva
лучшие казино– это популярная букмекерская контора, предоставляющая широкий выбор ставок на спорт и казино. Сайт обладает удобным интерфейсом, мобильной версией и приложением для удобства пользователей. 1xBet также известен разнообразными акциями и бонусами, делая игровой опыт более захватывающим.
amoxicillin over counter amoxicillin 500mg capsules antibiotic amoxicillin 500 mg online
https://menwiki.men/wiki/User:SITAaron92361389
cheap omnicef
Hi friends, its enormous post about educationand entirely explained, keep it up all
the time.
https://clomiphene.icu/# can you buy generic clomid price
В этом что-то есть и это отличная идея. Готов Вас поддержать.
but really is his https://www.modasmagvi.com.ec/hello-world-2/ like this should have wonderful dialogues? No one would you believe that significant guy like Xander Cage would be recruited in the role of an undercover agent in some organization, but in fact hobby not for that.
Apartments and penthouses in the complex of Bluewaters Bay UAE in the Bluewaters Island area. Developer Meraas Holding offers units for sale at favourable prices.
cost cheap clomid online how can i get generic clomid without insurance can you buy clomid without insurance
Как происходит монтаж vrf системы?
установка кондиционирования vrf-sistemy.ru.
where to buy prednisone without prescription: buy prednisone online from canada – buy prednisone 20mg without a prescription best price
адреса по ремонту телефонов в москве
canadatc.com
Преимущества установки кондиционера в жаркое время года
напольно потолочный кондиционер http://www.magazin-split-sistem.ru/.
Купить 1С Склад у официального партнера фирмы 1С ут 8 консультация бесплатно!
Судебный юрист – это юридическая компания, специализирующаяся на семейных делах https://www.buyfags.moe/User:ChristineDiehl6
http://amoxicillin.bid/# amoxicillin 775 mg
Стоит ли экономить на монтаже vrf системы?
наружный блок vrf http://www.vrf-sistemy.ru.
Сколько времени занимает монтаж vrf системы?
услуги кондиционирования https://vrf-sistemy.ru/.
zithromax online usa no prescription: buy zithromax canada – zithromax pill
Какие дополнительные аксессуары нужны для установки кондиционера
кондиционер daikin http://www.magazin-split-sistem.ru/.
Aw, this was an exceptionally nice post. Taking a few minutes and actual effort to make a very
good article… but what can I say… I procrastinate a whole lot and don’t seem to get nearly anything done.
Here is my website: 2000 buick lesabre
Какой тип выбрать для определенной площади помещения
установка кондиционера в квартире цена https://magazin-split-sistem.ru.
https://andyfreund.de/wiki/index.php?title=Mp3gid.co
Good day! I know this is kinda off topic however , I’d figured I’d ask.
Would you be interested in trading links
or maybe guest writing a blog post or vice-versa? My
blog discusses a lot of the same topics as yours and I feel we could greatly benefit from each other.
If you might be interested feel free to shoot me an e-mail.
I look forward to hearing from you! Excellent blog by the way!
https://ivermectin.store/# cost of ivermectin medicine
http://womka.6bb.ru/viewtopic.php?id=1895#p3816
Список всех МФО Казахстана https://farsh-cook.ru/
ivermectin 0.1: ivermectin 24 mg – ivermectin human
Виниловый сайдинг в интернет-магазине по выгодным ценам https://star-plast.su/ настоящие отзывы покупателей!
https://owen.ru/forum/album.php?albumid=206&attachmentid=73028&commentid=2122
Для того чтобы уточнить подробности и купить арматуру необходимого типа, свяжитесь с нашими специалистами арматура для фундамента
Виниловый сайдинг в интернет-магазине по выгодным ценам Пвх сайдинг настоящие отзывы покупателей!
Для того чтобы уточнить подробности и купить арматуру необходимого типа, свяжитесь с нашими специалистами арматура а 500
%%
Take a look at my blog post :: https://loverust.ru/nyani-i-guvernantki-dlya-detej-kak-ne-oshibitsya-s-vyborom/
https://ar.trade-leader.com/
%%
Also visit my webpage; http://neoncity.gtaserv.ru/viewtopic.php?f=38&t=1682
Если вам срочно нужны финансы, то expl0it.ru – это то место, где вы можете легко получить займы онлайн. Здесь вы найдете самые выгодные предложения от МФО, которые готовы быстро выдать необходимую сумму на выгодных условиях. Простота и удобство получения займа сделают ваш финансовый опыт максимально приятным.
can you get clomid no prescription: cost of generic clomid pill – how to get generic clomid pills
Какие преимущества дает монтаж vrf системы?
установка кондиционирования https://vrf-sistemy.ru/.
http://www.vladimir.ru/forum/forum/thread/39124
Habt ihr coole Ideen fur einen neuen whatsapp status? Brauche Inspiration!
http://miquelduran.net/index.php?title=Usuari:Adela28M5540
Nikolaev Vyacheslav Konstantinovich http://www.techbullion.com/nikolaev-vyacheslav-konstantinovich.
amoxicillin buy online canada: where can i buy amoxicillin online – amoxicillin capsule 500mg price
Greeley, Colorado News, Sports, Weather and Things to Do https://greeleynews.us/
prednisone in canada where to buy prednisone without prescription prednisone 80 mg daily
Рекомендую самую надежную БК в России 1вин.
Здравствуйте! Обратите внимание на expl0it.ru, где представлены более 40 МФО, предлагающих займ быстро на карту. На сайте вы найдете много полезной информации и компании, предоставляющие первый займ под 0%. Это идеальный выбор для тех, кто ищет удобный и экономически выгодный способ получения срочных финансов.
В любое время суток, когда вам срочно потребуются денежные средства, expl0it.ru предлагает решение: займ онлайн круглосуточно без отказа. Это уникальная возможность получить финансовую помощь, не зависящую от времени дня и без риска отказа. Мы понимаем важность быстрого реагирования на ваши финансовые потребности и предлагаем простую и удобную систему оформления займов, доступную вам 24/7. Ваша финансовая свобода начинается здесь и сейчас!
prednisone 20mg nz: prednisone 40mg – can i order prednisone
http://ivermectin.store/# ivermectin 50ml
baseballoutsider.com
이 문제는 Hongzhi 황제의 관점에서 볼 때 너무 많이 관리하기가 정말 쉽지 않습니다.
%%
My site: http://www.netdemodexa.ru/demodexforum/profile.php?action=show&member=8744
over the counter amoxicillin where can i buy amoxicillin over the counter uk canadian pharmacy amoxicillin
https://online-raduga.ru/forum/user/6047/
https://zarada.info/index.php?/gallery/image/18-%D0%B8%D1%81%D1%82%D0%BE%D1%80%D0%B8%D1%8F-%D1%84%D0%BE%D1%80%D0%BC%D0%B0%D1%82%D0%B0-mp3/&context=new
https://www.hb9lc.org/wiki/index.php/Mp3gid.co
https://clomiphene.icu/# can you get clomid for sale
can i get cheap clomid without prescription: where can i get cheap clomid without dr prescription – how to buy clomid without a prescription
Duplexes and penthouses in the complex of Ocean House properties on Palm Jumeirah. Developer Ellington Properties offers units for sale at favourable prices.
how to buy generic clomid no prescription: where can i get generic clomid no prescription – can you buy cheap clomid without dr prescription
Hello! I just wanted to ask if you ever have any issues
with hackers? My last blog (wordpress) was hacked and I ended up losing a
few months of hard work due to no backup. Do you have any methods to stop
hackers?
socialmediatric.com
Fang Jifan이 궁전에 들어갔을 때 당황하고 침묵하는 것과 비교했습니다.
https://clomiphene.icu/# can i buy clomid without insurance
https://manigroup.ru/stati/khenday-gold-manipulyator/
на сайте вы получаете шанс посмотреть секс онлайн без оплаты, словно без мучительных, http://diakov.net/index.php?subaction=userinfo&user=yzewe регистраций так и sms.
Houses in Dubai, flipping properties. Recommend!
I don’t know whether it’s just me or if everyone else encountering issues with your site.
It appears as if some of the written text in your content are running off the screen. Can somebody else please comment
and let me know if this is happening to them
as well? This may be a problem with my internet browser because I’ve had this happen before.
Cheers
gГҐ till hemsidan
You’re so cool! I do not suppose I’ve truly read
something like that before. So nice to discover
someone with original thoughts on this topic.
Seriously.. thanks for starting this up. This website is one thing that
is needed on the web, someone with a bit of originality!
%%
Also visit my web blog; http://www.worldisblackandwhite.com/2012/01/blog-post_4276.html
Попал мужик!
первое из особо выгодных вложений для коллег – сертификат ИСО, https://www.hongwha21.net/bbs/board.php?bo_table=free&wr_id=1052790 цена его оформления в едином сертификационном ресурсе» не за горами!
Как исправить, если кондиционер перестал работать после установки
кондиционер настенный https://magazin-split-sistem.ru/.
https://loadus.exelator.com/load/?p=258&g=244&clk=1&crid=porscheofnorth&stid=rennlist&j=r&ru=https://mrfeelgood.ca/
Mostbet bookmaker: review and reviews of players on Mostbet https://www.bebegimonline.com/forum/index.php/topic,86292.0.html
https://azing.org/de/catalog/redirect?url=https://gg4.store/calgary/
Mostbet bookmaker: review and reviews of players on Mostbet http://blog.niwablo.jp/100sho-ojisan/kiji/131544.html
amoxicillin generic brand buy cheap amoxicillin generic amoxicillin
how to get zithromax: where can you buy zithromax – zithromax online paypal
https://azithromycin.bid/# zithromax cost uk
abilify 10 mg pharmacy
https://wiki.baytanc.com/index.php/Mp3gid.co
can you buy zithromax over the counter in canada: zithromax 250 mg pill – buy zithromax online
You possibly can convert provided that it performs in RealPlayer.
http://ivermectin.store/# stromectol price usa
Интересные решения для охлаждения дома
система сплит https://expert-split.ru.
В нашем интернет-магазине Вы найдете широкий ассортимент медицинских товаров, медоборудования, медицинской техники для дома медицинское оборудование купить
В нашем интернет-магазине Вы найдете широкий ассортимент медицинских товаров, медоборудования, медицинской техники для дома купить медицинское оборудование для детского сада
https://forum.unrivaled.ro/index.php?/gallery/image/345-%D1%8D%D0%B2%D0%BE%D0%BB%D1%8E%D1%86%D0%B8%D1%8F-%D0%B7%D0%B2%D1%83%D0%BA%D0%B0-%D0%BF%D0%BE%D0%BF%D1%83%D0%BB%D1%8F%D1%80%D0%BD%D1%8B%D0%B5-%D0%BC%D1%83%D0%B7%D1%8B%D0%BA%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B5-%D0%B0%D0%BB%D1%8C%D0%B1%D0%BE%D0%BC%D1%8B-%D1%81-%D0%BD%D0%B0%D1%87%D0%B0%D0%BB%D0%B0-90-%D1%85/
http://mindclub.online/wiki/index.php/%D0%98%D1%81%D1%82%D0%BE%D1%80%D0%B8%D1%8F_%D0%B0%D1%83%D0%B4%D0%B8%D0%BE%D1%84%D0%BE%D1%80%D0%BC%D0%B0%D1%82%D0%BE%D0%B2:_%D0%9E%D1%82_%D0%B2%D0%B8%D0%BD%D0%B8%D0%BB%D0%B0_%D0%B4%D0%BE_%D1%81%D1%82%D1%80%D0%B8%D0%BC%D0%B8%D0%BD%D0%B3%D0%B0
Кондиционер для дома – простое решение для сложной задачи
система сплит https://expert-split.ru.
dnews7.com
Тонкости выбора кондиционера для дома
сплит ballu https://expert-split.ru/.
Lego Affiliate Program
эти реальные девушки, и молодые порнозвезды так любят раздеваться перед камерой и показывать свои прекрасные сиськи http://ds2.edu.sbor.net/index.php?subaction=userinfo&user=uvodate и вкусные попы.
can i get clomid online: where can i buy cheap clomid price – can you buy cheap clomid without rx
1хбет промо – это специальное
предложение от букмекерской конторы 1хбет,
которое позволяет получить дополнительные бонусы или преимущества при регистрации или размещении ставок на спортивные события.
Промокоды в 1xbet на сегодня 1хбет промо
может включать различные акции, например, бонус
на первый депозит, бесплатные ставки или повышенные коэффициенты на определенные матчи.
Для получения 1хбет промо нужно выполнить
определенные условия, например, зарегистрироваться на сайте букмекера, внести депозит или сделать определенное количество ставок.
1хбет промо может быть доступно только новым игрокам или также предоставляться
постоянным клиентам. Чтобы узнать о текущих
акциях и получить 1хбет промо, нужно посетить официальный
сайт букмекера или подписаться на рассылку.
1хбет промо может быть отличной возможностью получить
дополнительные выгоды от
ставок и увеличить свой шанс
на победу.
https://vk.com/mesta_otduha_moskva?w=wall-224478589_33%2Fall
http://ivermectin.store/# ivermectin cream cost
seo продвижение сайта поисковое продвижение москва https://seo-con.ru/
where buy generic clomid pill: can i order clomid online – how to get clomid without prescription
Kredit 4000 Euro
Всем рекомендую только тут флиппинг в Дубае.
https://www.blackhatway.com/index.php/topic,506962.0.html
https://finansforum.apbb.ru/viewtopic.php?id=11056#p148450
zithromax 500 price zithromax buy generic zithromax online paypal
https://njt.ru/forum/user/148542/
https://azithromycin.bid/# where can i buy zithromax medicine
В этом что-то есть. Благодарю за информацию, теперь я буду знать.
7. После нажатия появится окно которое позволит https://www.donatellasommariva.com/2021/01/28/ciao-mondo/ ввести специальные символы. Они публично не анонсируются и станут доступны только в частном месяце.
where can i buy cheap omnicef
Medicine information leaflet. Long-Term Effects.
cleocin
Best information about medicament. Get information here.
toppartikel
перетяжка мебели в минске недорого https://peretyazhka-mebeli-minsk.ru/.
Fantasy sports have overtaken the planet numerous platforms, tools, and blogs have
emerged.
https://gefi.io/index.php?title=User:AndreasJankowski
http://2cool.ru/qiwi-f215/skachat-muziku-2024-t2694.html
I got this web site from my pal who shared with
me concerning this web site and at the moment this time
I am visiting this website and reading very informative posts at this place.
Онлайн-казино Kent Casino — игровые автоматы от ведущих производителей. Эксклюзивный бонус — 70 фриспинов зеркало kent casino
Онлайн-казино Kent Casino — игровые автоматы от ведущих производителей. Эксклюзивный бонус — 70 фриспинов казино kent
Продажа медицинского оборудования медицинской техники ведущих мировых брендов медицинское оборудование купить в красноярске
Porn
Продажа медицинского оборудования медицинской техники ведущих мировых брендов медицинское оборудование с госрезерва купить
https://www.google.kz/url?q=https://mostbet-kg-online.com
odwiedzać
aboutweeks.com
Manta Network Airdrop
http://mexicanpharm.shop/# mexico pharmacies prescription drugs mexicanpharm.shop
viagra online
india pharmacy online shopping pharmacy india indianpharmacy com indianpharm.store
Pills information sheet. Brand names.
rx zoloft
Best information about medicines. Get now.
Heya i’m for the first time here. I came
across this board and I find It really useful & it helped me out much.
I hope to give something back and aid others like you aided me.
http://indianpharm.store/# online shopping pharmacy india indianpharm.store
LГҐna 3000 kr
reputable mexican pharmacies online: mexican drugstore online – mexico drug stores pharmacies mexicanpharm.shop
I really like reading through a post that can make people think. Also, many thanks for permitting me to comment! Dark Markets 2024 https://mydarkmarket.com
cenforce 100mg online
buy medicines online in india Indian pharmacy to USA india pharmacy mail order indianpharm.store
welcomelady.net
buy drugs from canada: canadianpharmacyworld com – safe canadian pharmacies canadianpharm.store
https://alt1.toolbarqueries.google.com.tw/url?q=https://marvelfilms.ru/category/istoriya-marvel/
newsplaces.net
https://xn—-btbthcge4aikr4i.xn--p1ai/forum/user/28278/
http://mexicanpharm.shop/# mexico pharmacy mexicanpharm.shop
http://freedom.teamforum.ru/viewtopic.php?f=54&t=25036
п»їlegitimate online pharmacies india order medicine from india to usa buy medicines online in india indianpharm.store
http://277469.simplecloud.ru/blogs/1/istoriya-formata-mp3.php
https://mozillabd.science/wiki/User:DustyCorby51872
The latest film and TV news, movie trailers, exclusive interviews, reviews, as well as informed opinions on everything Hollywood has to offer. https://xoop.us/
https://beerova.blog.idnes.cz/redir.aspx?url=https://marvelfilms.ru/opisanie-personazhej-iz-vselennoj-marvel/
https://indianpharm.store/# indianpharmacy com indianpharm.store
thespice.net
reputable indian online pharmacy: Indian pharmacy to USA – indian pharmacy indianpharm.store
newsmiamigardens.com
https://bit.ly/sistemniy-podkhod
Food
Биография Эдуарда Давыдова Эдуард Давыдов генерального директора БСК.
Stri is the leading entrepreneurs and innovation magazine devoted to shed light on the booming stri ecosystem worldwide. https://stri.us/
Биография Эдуарда Давыдова https://eduarddavydov.ru/ генерального директора БСК.
люберецкий морг https://www.ritual-gratek20.ru.
I recommend best boat detailing Miami.
canadian pharmacy victoza Certified Online Pharmacy Canada canadian pharmacy store canadianpharm.store
pharmacies in mexico that ship to usa: Certified Pharmacy from Mexico – buying prescription drugs in mexico online mexicanpharm.shop
%%
Here is my site; http://www.daongil.com/bbs/board.php?bo_table=free&wr_id=126499
The one-stop destination for vacation guides, travel tips, and planning advice – all from local experts and tourism specialists. https://travelerblog.us/
http://pervak.ukrbb.net/viewtopic.php?f=13&t=20440
https://forums.qrz.com/proxy.php?link=https://marvelfilms.ru/opisanie-personazhej-iz-vselennoj-marvel/
https://bit.ly/sistemniy-podkhod
https://krasota.ipbb.ru/viewtopic.php?id=3778#p4531
Money Analysis is the destination for balancing life and budget – from money management tips, to cost-cutting deals, tax advice, and much more. https://moneyanalysis.us/
https://canadianpharm.store/# canadian pharmacy prices canadianpharm.store
https://chelyabinsk.eurooptic.ru/about/forum/user/16032/
Torrent-mass.ru приглашает вас в мир, где каждая игра рассказывает свою историю на понятном и близком вам языке. Вы можете игры торрент на русском скачать, чтобы каждый диалог и каждое приключение было полностью погружено в атмосферу русскоязычного мира. Откройте для себя игры, где каждый персонаж и каждый сюжет звучит знакомо и увлекательно.
recommended canadian pharmacies Best Canadian online pharmacy my canadian pharmacy canadianpharm.store
https://bit.ly/sistemniy-podkhod
продвижение интернет магазина книги https://seo-con.ru/
https://canadianpharm.store/# reputable canadian online pharmacy canadianpharm.store
Outdoor Blog will help you live your best life outside – from wildlife guides, to safety information, gardening tips, and more. https://outdoorblog.us/
india pharmacy mail order: Indian pharmacy to USA – reputable indian online pharmacy indianpharm.store
sildenafil citrate 20 mg cost
online pharmacy india: top online pharmacy india – best online pharmacy india indianpharm.store
mexican border pharmacies shipping to usa Certified Pharmacy from Mexico buying prescription drugs in mexico mexicanpharm.shop
hollanderhomes.com
https://pattern-wiki.win/wiki/Mp3gid.co
autonow.net
Промокод Mostbet при регистрации. Компания Мостбет заинтересована в привлечении новых клиентов, поэтому для новых игроков действует акция в виде бонуса, который равен сумме первого депозита, но не превышает 225 000 рублей. Однако при использовании промокода букмекерская контора увеличит размер приветственного бонуса. Для того чтобы получить повышенную сумму на первый депозит, игроку необходимо выполнить следующие условия: Зайти на сайт букмекера. Выбрать способ регистрации по e-mail. Заполнить поля с личными данными. Ввести промокод в поле слева от кнопки «Зарегистрироваться». Ознакомиться с правилами букмекера. mosbet промокод на сайте mostbet bonus promokod ru поможет пользователям получить еще больше бонусов от букмекерской конторы. Подробная инструкция по поиску и активации бонусных кодов. Промокод — комбинация из цифр и букв, которая позволяет игроку активировать специальное предложение от букмекера Мостбет. С его помощью пользователь может получить: бонусные средства на депозит; бесплатную ставку; промо-баллы; другие подарки. Сегодня вы сможете найти множество подобных ресурсов, которые регулярно обновляют список актуальных предложений БК.
промокод регистрации 1xbet
http://mexicanpharm.shop/# purple pharmacy mexico price list mexicanpharm.shop
sildenafil 50 mg tablets
http://www.jeromebaray.com/afm/wiki/index.php/Utilisateur:MilesRowe51806
https://yogicentral.science/wiki/Mp3bit.pw
http://xn--80aasiq5aadj.online/people/user/80376/blog/9593/
Maryland Post: Your source for Maryland breaking news, sports, business, entertainment, weather and traffic https://marylandpost.us/
Torrent-mass.ru предлагает вам мир, где каждая игра – это возможность для новых открытий. Скачать торрент на игры пк – это ваш путь к неограниченным возможностям в игровом мире. Откройте для себя игры, которые принесут вам радость и волнение, и станьте частью захватывающего приключения.
The latest health news, wellness advice, and exclusives backed by trusted medical authorities. https://healthmap.us/
На torrent-mass.ru каждый найдет что-то особенное для себя. Не важно, какой у вас ПК, ведь тут можно игры для слабых пк скачать торрент. Наслаждайтесь многообразием игр, подходящих для любых системных требований и окунитесь в увлекательные миры без ограничений.
При выборе нашего агентства, вы обеспечите себе получение профессиональных юридических услуг от квалифицированных юристов. Узнайте больше на нашем сайте по ссылке
ответ на претензию в какой срок.
buying prescription drugs in mexico Certified Pharmacy from Mexico buying prescription drugs in mexico online mexicanpharm.shop
Baltimore Post: Your source for Baltimore breaking news, sports, business, entertainment, weather and traffic https://baltimorepost.us/
https://canadianpharm.store/# canada discount pharmacy canadianpharm.store
best india pharmacy: international medicine delivery from india – best online pharmacy india indianpharm.store
пін ап
casino pin up https://www.pinupcasinolfsesn.kiev.ua/.
viagra pills from canada
I recommend this best Miami car detailing.
Погрузись в атмосферу пин-ап казино
jogos de casino online pinupcasinojenzolo.com.
Откуда мне знать?
el/ tal bicicleta incluso tiene La mejor sala de poquer en Vegas, llamada las Weekly-http://0ae703.haowui.com/cpv/go.php?u=aHR0cHM6Ly9tZXRyby1zcG9ydHMuZnIvZGVjb3V2cmV6LWx1bml2ZXJzLXBhc3Npb25uYW50LWRlcy1qZXV4LWRlLWNhc2luby0xd2luLXBvdXItbGVzLWpvdWV1cnMtaXZvaXJpZW5zLw/aWQ9MTg2MTUwNw Vegas.
Online medicine order: order medicine from india to usa – top 10 pharmacies in india indianpharm.store
Абсолютно бесплатный промокод Mostbet. На сегодня контора предлагает всем новичкам воспользоваться не только приветственным бонусом, но и получить дополнительные преференции. Эти льготы игрок получает в том случае, если внимательно отнесётся к процедуре регистрации на сайте. промокод при регистрации мостбет . Mostbet – один из самых узнаваемых букмекерских брендов в стране. Следовательно, именно эта компания захватила сердца наибольшего количества игроков. Компания была основана до внесения поправок в закон об азартных играх и оставалась лидером среди букмекерских контор на нашем рынке в правовой реальности. Уже один этот факт должен что-то указывать, так как многие клиенты с удовольствием возвращаются к игре в Mostbet. Mostbet – промокод на 35000р. Свежие промокоды Mostbet Все купоны и скидки букмекера Получи бонус 35000 ? Делай ставки на спорт.
пін ап
пін ап вхід https://www.pinupcasinolfsesn.kiev.ua.
http://danceway74.ru/users/2244
https://indianpharm.store/# india online pharmacy indianpharm.store
Быстрое получение Гражданства Киргизии для Россиян гражданство киргизии стоимость от Юридической Компании Быстро и с Гарантией. Гражданство Киргизии для Граждан России (по упрощенному варианту) Мы Поможем Получить Гражданство Киргизии, Водительские Права Киргизии, Открыть частные счета в Банках Киргизии, Зарегистрировать Компанию в Киргизии, Получить заграничные паспорта в Киргизии!
Быстрое получение Гражданства Киргизии для Россиян гражданство киргизии для рожденных в ссср от Юридической Компании Быстро и с Гарантией. Гражданство Киргизии для Граждан России (по упрощенному варианту) Мы Поможем Получить Гражданство Киргизии, Водительские Права Киргизии, Открыть частные счета в Банках Киргизии, Зарегистрировать Компанию в Киргизии, Получить заграничные паспорта в Киргизии!
avapro 10mg
Быстрое получение Гражданства Киргизии для Россиян гражданство киргизии для рожденных в ссср иностранные граждане и лица без гражданства, достигшие 18-летнего возраста, имеют право обратиться с ходатайством о приеме в гражданство Кыргызской Республики в общем порядке.
https://vltk.vvvvvvaria.org/w/Mp3bit.pw_3
Насолоджуйтесь дозріванням фруктів
слоти онлайн україна https://www.pinupcasinolfsesn.kiev.ua/.
Быстрое получение Гражданства Киргизии для Россиян гражданство киргизии стоимость иностранные граждане и лица без гражданства, достигшие 18-летнего возраста, имеют право обратиться с ходатайством о приеме в гражданство Кыргызской Республики в общем порядке.
darknet зайти на сайт
Даркнет, сокращение от “даркнетворк” (dark network), представляет собой часть интернета, недоступную для обычных поисковых систем. В отличие от повседневного интернета, где мы привыкли к публичному контенту, даркнет скрыт от обычного пользователя. Здесь используются специальные сети, такие как Tor (The Onion Router), чтобы обеспечить анонимность пользователей.
modernkarachi.com
그리고 도중에 여러 환자도 병원으로 보내졌습니다.
canadian discount pharmacy: Canada Pharmacy online – canadian mail order pharmacy canadianpharm.store
viagra soft tabs 100mg
Крутое казино пин-ап
melhores cassinos http://www.pinupcasinojenzolo.com/.
https://mexicanpharm.shop/# medication from mexico pharmacy mexicanpharm.shop
https://berforum.ru/gallery/image/8395-istoriya-audioformatov-ot-vinila-do-striminga/?context=new
canadian compounding pharmacy: Best Canadian online pharmacy – online canadian pharmacy review canadianpharm.store
https://transfer-tur.ru/ru/cb-profile/pluginclass/cbblogs?action=blogs&func=show&id=76
https://bbarlock.com/index.php/Mp3gid.co
Hello! Someone in my Myspace group shared this site with us so I came to take a look. I’m definitely enjoying the information. I’m bookmarking and will be tweeting this to my followers! Wonderful blog and brilliant design.
Also visit my web blog; http://Scaleshop.co.kr/yc5/bbs/board.php?bo_table=qa&wr_id=183731
legit canadian pharmacy Canadian International Pharmacy best canadian pharmacy to order from canadianpharm.store
https://battle-chess.ru/robox/ap/?skachat_mostbet_na_telefon.html
Яркое пин-ап казино
jogos cassino dinheiro real https://pinupcasinojenzolo.com.
http://mybaltika.info/ru/blogs/587/6773/
caverta tablets online
Помощь опытного адвоката по уголовным делам в Москве консультация адвоката по уголовным делам москва консультация и план защиты бесплатно! Бывшие сотрудники СК и МВД!
https://fuss.forumkz.ru/viewtopic.php?id=2220#p3640
Помощь опытного адвоката по уголовным делам в Москве консультация адвоката по уголовным делам консультация и план защиты бесплатно! Бывшие сотрудники СК и МВД!
как сделать промокод в 1xbet
license, an M.B.A. degree, and nearly ten years of experience in the cross-border tax field http://www.thecornermag.com/dept/uncategorized/page/838/
license, an M.B.A. degree, and nearly ten years of experience in the cross-border tax field https://www.vestibune.com/travel-management-corporations-the-actual-can-carry-out-for-your-business/
http://forumrabota.0pk.me/viewtopic.php?id=6669#p16048
продвижение сайта топ 10 цена https://seo-con.ru/optimizaciya-sajta/
http://indianpharm.store/# indianpharmacy com indianpharm.store
thecanadianpharmacy: Licensed Online Pharmacy – canadian pharmacy ltd canadianpharm.store
http://audi.8bb.ru/viewtopic.php?id=155#p171
http://ledi.forumno.com/viewtopic.php?id=4304#p7899
https://livestreet.imbachat.com/2024/01/20/istoriya-audioformatov-ot-vinila-do-striminga.html
mexican mail order pharmacies mexico drug stores pharmacies mexican pharmaceuticals online mexicanpharm.shop
mexican rx online: Online Pharmacies in Mexico – pharmacies in mexico that ship to usa mexicanpharm.shop
9000 euro lenen
https://mexicanpharm.shop/# buying prescription drugs in mexico online mexicanpharm.shop
https://fuss.forumkz.ru/viewtopic.php?id=2220#p3640
http://turforum.borda.ru/?1-8-0-00001074-000-0-0-1706616247
Привет, друзья! Хотите узнать, какие игры входят в золотую коллекцию геймерских шедевров? У нас есть для вас отличная новость! Теперь вы можете топ 100 игр скачать торрент прямо с нашего сайта. Мы собрали лучшие из лучших игр, чтобы вы могли насладиться каждой минутой, проведенной в игровом мире. Не важно, предпочитаете ли вы стратегии, экшены, головоломки или приключения — среди этого списка вы обязательно найдете что-то для себя. Погрузитесь в мир великолепных игр уже сегодня!
https://pipewiki.org/app/index.php/Mp3gid.co
https://www.macphearson.org/wiki/index.php?title=Mp3bit.pw_2
calan 10mg
There is one thing illogical about utilizing one significance test conditional on the results of another significance test.
It has one of the biggest collections of Ayurvedic literature and a backyard
wherein it grows medicinal herbs used to treat patients.
The Nazis are responsible for creating the biggest and heaviest gun that has ever been constructed.
Why are there dozens of lifeless animals floating in area?
They’re manufactured from lifeless stuff. Fleming
then wrote a scene in Dr. No that detailed the change and gave Bond his now famous Walther PPK.
James Bond initially used the Beretta 418
until one fan of the novels and likewise a small arms
professional informed Ian Fleming that the Beretta 418 was a lady’s gun. There may be the reality is,
just one legally operated gun store in all of Mexico.
A 2013 University of San Diego report discovered that
nationally the illegal firearms commerce with Mexico accounted for $127 million in annual income.
Firearms are so previous that the earliest ones were made of hollow bamboo!
If you actually want to develop into a DEA (Drug Enforcement Agency) agent, there
are some things you’ll want to consider. Some automobiles will need a
change after just 2,500 miles, and some automobiles can run longer.
stagramer.com
domstroi.info
buying drugs from canada Canada Pharmacy online prescription drugs canada buy online canadianpharm.store
canadian pharmacy oxycodone: Canadian International Pharmacy – best canadian pharmacy canadianpharm.store
http://sdm-servis.ru/component/fireboard/?func=view&catid=2&id=67611#67611
teplica-parnik.net
homeprorab.info
online pharmacy canada: canadian pharmacy world – canadian pharmacy ratings canadianpharm.store
http://vestnikzoj.winbb.ru/viewtopic.php?id=1567#p1958
viagra 25 mg
https://vltk.vvvvvvaria.org/w/User_talk:BeauGruner
https://to.iboard.ws/viewtopic.php?id=4054#p7864
zofran without a doctor prescription
http://mergingdestinies.lakeishikawa.com/index.php/User:CarolynJelks0
http://startflag.rulez.jp/index.php/Mp3gid.co
В Москве занимаются решением текущих проблем в доме, обеспечением благоустройства территории и охраны общего имущества телефоны управляющей компании
промокод при пополнении 1хбет
В Москве занимаются решением текущих проблем в доме, обеспечением благоустройства территории и охраны общего имущества найти управляющую компанию
stroibloger.com
Общение с девушками без регистрации, вы можете смотреть приват записи бесплатно или общаться в прямом эфире с девочками http://redcams.at
Общение с девушками без регистрации, вы можете смотреть приват записи бесплатно или общаться в прямом эфире с девочками http://rt.erochats.org
https://promodisco.ru/
mexico pharmacy: mexican pharmacy – mexican mail order pharmacies mexicanpharm.shop
I have been browsing online more than 2 hours today, yet I never found any interesting article like yours.
It’s pretty worth enough for me. Personally, if all webmasters and bloggers made good content as you did,
the internet will be a lot more useful than ever before.
https://canadianpharm.store/# canadian pharmacies compare canadianpharm.store
https://gelen.webtalk.ru/viewtopic.php?id=247#p363
medication from mexico pharmacy: Online Mexican pharmacy – mexican pharmacy mexicanpharm.shop
indian pharmacies safe best india pharmacy online shopping pharmacy india indianpharm.store
http://mygame.5nx.ru/viewtopic.php?f=110&t=49866
viagra price per pill
https://zagorodom31.ru/forum/viewtopic.php?f=11&t=2441
http://indianpharm.store/# best online pharmacy india indianpharm.store
Investors services
Граждане России приобретают гражданство Киргизской республики по упрощенной схеме гражданство киргизии для граждан рф Быстрое получение Гражданства Киргизии для Россиян от Юридической Компании Быстро и с Гарантией. Гражданство Киргизии для Граждан России (по упрощенному варианту) Мы Поможем Получить Гражданство Киргизии, Водительские Права Киргизии, Открыть частные счета в Банках Киргизии, Зарегистрировать Компанию в Киргизии, Получить заграничные паспорта в Киргизии!
Граждане России приобретают гражданство Киргизской республики по упрощенной схеме гражданство киргизии Быстрое получение Гражданства Киргизии для Россиян от Юридической Компании Быстро и с Гарантией. Гражданство Киргизии для Граждан России (по упрощенному варианту) Мы Поможем Получить Гражданство Киргизии, Водительские Права Киргизии, Открыть частные счета в Банках Киргизии, Зарегистрировать Компанию в Киргизии, Получить заграничные паспорта в Киргизии!
https://promodisco.ru/
3000 euro lenen
http://divinecosmosnew.tforums.org/viewtopic.php?f=4&t=17960
https://obovsem.myqip.ru/?1-8-0-00002426-000-0-0-1704124052
Декоративные растения из Китая – это дешевая красота! Помните, широкий диапазон китайских цветов всегда можно купить без проблем.
https://55opt.org/catalog/cvety-iz-kitaya/
instukzia.com
https://peklama.bbok.ru/viewtopic.php?id=12605#p23779
Скидочный промокод
Ponto IPTV a melhor programacao de canais IPTV do Brasil, filmes, series, futebol
My website: эротика русская версия
canadian pharmacy online: canadian medications – reliable canadian pharmacy reviews canadianpharm.store
Escort Barcelona
viagra online
plan b
где в 1хбет ввести промокод на андроид
sex videos
https://menwiki.men/wiki/User:Aleisha76K
top 10 pharmacies in india online pharmacy india pharmacy website india indianpharm.store
sex videos
This piece of writing is in fact a good one it helps new net people, who are wishing for blogging.
https://wiki.roboco.co/index.php/Mp3gid.co
https://canadianpharm.store/# canadian pharmacy 365 canadianpharm.store
https://belsprosshina.by/company/personal/user/127/forum/message/1123/4804/
cheapest online pharmacy india: order medicine from india to usa – india pharmacy indianpharm.store
http://anamaliya.ru/otzyvy/evolyuciya-zvuka-populyarnye-muzykalnye-albomy-s-nachala-90-h
https://ufametallobaza1.ru/
viagra online
https://mexicanpharm.shop/# buying prescription drugs in mexico online mexicanpharm.shop
http://fabnews.ru/forum/showthread.php?p=71917#post71917
https://clashofcryptos.trade/wiki/User:LyndonCarmichael
buying prescription drugs in mexico Online Pharmacies in Mexico medicine in mexico pharmacies mexicanpharm.shop
http://realistzoosafety.forum24.ru/?1-1-0-00000055-000-0-0-1706615278
https://coub.com/russians-diploms
https://shopwheel.ru/club/user/49/blog/38232/
На веб-сайте http://kupit-diplom1.com вы можете приобрести документ о среднем специальном образовании онлайн. Здесь представлен большой выбор документов о среднем специальном и высшем образовании.
best online pharmacies in mexico: Online Mexican pharmacy – buying prescription drugs in mexico mexicanpharm.shop
Дизельное топливо оптом стоимость купить дизельное топливо тут.
http://moskvichemania.ru/viewtopic.php?f=19&t=3965
http://detimgn.iboards.ru/viewtopic.php?f=50&t=32220
abilify pharmacy
online canadian pharmacy reviews: Canadian International Pharmacy – canadian drug prices canadianpharm.store
http://canadianpharm.store/# canadian pharmacy ed medications canadianpharm.store
spiriva 1mg
http://tr.clanfm.ru/viewtopic.php?f=33&t=8904
where can i get generic lisinopril without rx
http://pirat.iboards.ru/viewtopic.php?f=20&t=16387
best online pharmacies in mexico Certified Pharmacy from Mexico medicine in mexico pharmacies mexicanpharm.shop
uquest.net
http://nedvigimost.bbok.ru/viewtopic.php?id=22646#p39597
В нашей компании вы имеете возможность приобрести университетский диплом по выгодной цене через наш интернет-ресурс http://kupit-diplom1.com. Мы принимаем любые способы оплаты.
plitki.com
http://canadianpharm.store/# real canadian pharmacy canadianpharm.store
сео продвижение сайта москва недорого https://seo-con.ru/optimizaciya-sajta/
https://biowiki.clinomics.com/index.php/Mp3gid.co
sildenafil 50 mg price
http://danceway74.ru/users/2244
purple pharmacy mexico price list: Online Mexican pharmacy – best online pharmacies in mexico mexicanpharm.shop
Есть возможность купить диплом в Москве любого российского ВУЗа в России без предварительной оплаты! Мы изготовим любые образовательные документы за 2 дня. Обратитесь в компанию diplomguru.com.
бонусы и подарки в 1хбет промокод
При выборе нашего агентства, вы гарантируете себе получение высококачественных юридических консультаций от опытных специалистов. Узнайте больше на нашем сайте по ссылке
как прописать к себе родственника.
sildenafil citrate 100mg tablet
https://support.sgo41.ru/help/index.php?title=%D0%98%D1%81%D1%82%D0%BE%D1%80%D0%B8%D1%8F_%D0%B0%D1%83%D0%B4%D0%B8%D0%BE%D1%84%D0%BE%D1%80%D0%BC%D0%B0%D1%82%D0%BE%D0%B2:_%D0%9E%D1%82_%D0%B2%D0%B8%D0%BD%D0%B8%D0%BB%D0%B0_%D0%B4%D0%BE_%D1%81%D1%82%D1%80%D0%B8%D0%BC%D0%B8%D0%BD%D0%B3%D0%B0
reliable canadian pharmacy: Canadian Pharmacy – canadian pharmacies compare canadianpharm.store
Reduslim: Ihr Weg zu einem gesünderen Ich!
Entdecken Sie Reduslim, das innovative Nahrungsergänzungsmittel, das Ihr Wohlbefinden revolutioniert! Mit seiner einzigartigen Formel unterstützt Reduslim Sie auf Ihrem Weg zu einem gesünderen Lebensstil.
Reduslim zeichnet sich durch eine sorgfältige Zusammensetzung aus, die darauf abzielt, Ihren Stoffwechsel natürlich zu fördern und Ihnen zu helfen, sich energiegeladener und lebendiger zu fühlen. Unsere Kapseln sind mit hochwertigen Inhaltsstoffen gefertigt, die speziell dafür entwickelt wurden, Ihren Körper auf natürliche Weise zu unterstützen.
Neben der Unterstützung beim Gewichtsmanagement https://reduslim.at/ Reduslim auch dazu beitragen, das allgemeine Wohlbefinden zu verbessern. Es ist eine ausgezeichnete Wahl für diejenigen, die einen aktiveren und gesünderen Lebensstil anstreben.
Einfach in der Anwendung: Nehmen Sie Reduslim gemäß den Anweisungen ein, um optimale Ergebnisse zu erzielen. Es integriert sich nahtlos in Ihren täglichen Lebensstil, ohne dass Sie umfangreiche Änderungen vornehmen müssen.
Warten Sie nicht länger, um sich besser zu fühlen und aktiver zu leben. Probieren Sie Reduslim heute aus und machen Sie den ersten Schritt in Richtung eines gesünderen, energiegeladenen Ichs!
http://toyota-opa.ru/forums/index.php?showtopic=8988
сдача квадроциклов в аренду
https://pipewiki.org/app/index.php/User:MaureenOFlaherty
https://pediascape.science/wiki/Mp3bit.pw?action=edit
прокат квадроциклов в москве и московской области
прокатиться на квадроциклах в подмосковье
https://mexicanpharm.shop/# mexican mail order pharmacies mexicanpharm.shop
levitra 10mg
http://miquelduran.net/index.php?title=Mp3gid.co
аренда квадроцикла на день
Sex porn videos
balforum.net
промокод 1xbet бонусы
Vervolgens ga dan naar onze website en Chat Meisjes zullen u helpen bij het vinden van een vrouw vanavond http://rt.voproom.com
Vervolgens ga dan naar onze website en Chat Meisjes zullen u helpen bij het vinden van een vrouw vanavond http://webcam24chat.com
https://sponforum.ixbb.ru/viewtopic.php?id=11916#p41084
canadianpharmacymeds com: Canadian International Pharmacy – canadian pharmacy online canadianpharm.store
vip escort in Paris
poiskmonet.com
Обзор официального сайта casino: регистрация в казино, рабочее зеркало, методы депозита, приветственные бонусы, промокоды, отзывы Зеркало онлайн казино
Обзор официального сайта casino: регистрация в казино, рабочее зеркало, методы депозита, приветственные бонусы, промокоды, отзывы Зеркало онлайн казино
https://newgames.apbb.ru/viewtopic.php?id=502#p2913
Документы о высшем образовании любого Вуза России, возможно купить онлайн в нашей компании http://diplomguru.com.
https://admtobolsk-new.ru/forum/messages/forum2/topic202/message208/?result=new#message208
canada drugstore pharmacy rx Canadian Pharmacy canadian online pharmacy reviews canadianpharm.store
На нашем веб-сайте http://diplomguru.com вы можете приобрести аттестат от любой школы в России, выполненный с высоким качеством и по доступной цене.
Поможем приобрести купить аттестат школы в России за 11 или 9 класс. Аттестаты любой школы россии с заменой оценок во вккладыше.
canadian online pharmacy: Pharmacies in Canada that ship to the US – canadian drugstore online canadianpharm.store
how can i get cheap valtrex pills
Hello There. I found your blog using msn. This is a really well written article.
I will be sure to bookmark it and come back to read more of your useful information. Thanks for the post.
I’ll definitely comeback.
Magnificent beat ! I wish tto apprentice while you amend your website, how can i subscribe for a
blog web site? The account aided me a acceptable deal.
I hhad been a little bit acquainted of this your broadcast probided bright clear idea
Here is my web-site; buy Mobile proxies By low price
vidalista 20mg for sale
https://promodisco.ru/
https://canadianpharm.store/# canada drug pharmacy canadianpharm.store
I got what you intend,bookmarked, very decent website.
My website: порно по пьяне
http://www.tamboff.ru/forum/viewtopic.php?p=7690694#7690694
ткани для мебели москва https://www.vinylko13.ru/ .
Medicament prescribing information. Generic Name.
get silagra
Some information about medicines. Get here.
Кто и на каких условия может получить гражданство Киргизии гражданство киргизии для рожденных в ссср от Юридической Компании Быстро и с Гарантией. Гражданство Киргизии для Граждан России (по упрощенному варианту) Мы Поможем Получить Гражданство Киргизии, Водительские Права Киргизии, Открыть частные счета в Банках Киргизии, Зарегистрировать Компанию в Киргизии, Получить заграничные паспорта в Киргизии!
Спробуйте нові фруктові коктейлі
нові ігрові автомати pinupcasinolfsesn.kiev.ua.
Кто и на каких условия может получить гражданство Киргизии гражданство киргизии цена от Юридической Компании Быстро и с Гарантией. Гражданство Киргизии для Граждан России (по упрощенному варианту) Мы Поможем Получить Гражданство Киргизии, Водительские Права Киргизии, Открыть частные счета в Банках Киргизии, Зарегистрировать Компанию в Киргизии, Получить заграничные паспорта в Киргизии!
besttoday.org
https://wiggles.ruka.at/wiki/index.php/Benutzer:JVWLorenza
everbestnews.com
Бесплатный промокод в Mostbet для бесплатной ставки на сегодня. Мостбет – один из популярнейших букмекеров на территории РФ и Европы. Оператор регулярно обновляет акционные предложения для только пришедших и постоянных пользователей, предоставляя возможность заработать на беттинге. промокоды для mostbet . Согласно условиям клиенты, впервые зарегистрировавшиеся на площадке, могут получить промокод на бесплатную ставку. Коды выдаются непосредственно оператором. При создании аккаунта беттер предоставляет номер телефона. На него приходит код. Воспользовавшись последним, можно сделать фрибет и получить реальный доход. Это сделать просто, если иметь промокод Mostbet на сегодня бесплатно. Правда, дается он при условии выполнения некоторых правил. Mostbet бонус при регистрации. Не совсем промокод, но вы все равно ставите не свои деньги, если пополните депозит, – 100% бонуса от внесенной суммы. Максимум указан в верхней части главной страницы официального сайта.
https://mexicanpharm.shop/# mexican rx online mexicanpharm.shop
best online pharmacies in mexico Online Pharmacies in Mexico buying prescription drugs in mexico online mexicanpharm.shop
The ideal element on our web page to get in contact with females from Colombia is by visiting each and every area of each and every incredibly hot babe you’re fascinated in to start off a dialogue with them during their alluring display. Here’s a list of ten most effective free of charge chat rooms to Chat Anonymously with Strangers. Besides a e book collection, it involved a bowling alley, an indoor swimming pool, basketball courts and other athletic amenities, a songs hall, and several assembly rooms for nearby companies. Finding movie chat rooms exactly where you can have a bit of entertaining on the internet with random strangers your age, whether it is just to chat, or have interaction in some webcam sexual intercourse, can be rather a problem. Public libraries are an equal accessibility facility and want to make every person sense welcome no matter their faith, race, ethnicity, sexual intercourse, or fiscal status. Access to pcs and the Internet is now just about as crucial to library patrons as entry to books. The Pikes Peak Library District has math tutors for their teenager patrons. The Orange County Library System gives various teenager things to do such as a Maker/Diy application, Audio Equipment Training, Sewing classes, Knitting courses, ESL courses, and Chess club.
https://xdpascal.com/index.php/User:ElissaPollak1
onlinepharmaciescanada com: Certified Online Pharmacy Canada – ordering drugs from canada canadianpharm.store
%%
Feel free to visit my web page: https://m.youtube.com/redirect?q=https://masterzoo.ua/ua/
https://sovpl.forum24.ru/?1-9-0-00001740-000-0-0-1704438629
http://tsa.webtalk.ru/viewtopic.php?id=2764#p5893
Thousands of people today have signed a petition for the “Armer Law,” laws to make sure entry to tests for initial responders for the duration of an epidemic or pandemic. All four had formal localizations, although the initially one particular was not translated until finally the PSP compilation Boy and Girl. Crispin Ortega died on Feb. 2, surrounded by a spouse and children that has grown to involve fifteen grandchildren and just one excellent-grandchild. Armer, 43, died on March 31 from COVID-19 soon after currently being hospitalized on March 23. Lau explained her sister, who experienced no underlying wellness disorders, was denied screening for the virus 3 situations. Lehner was just one of 3 sisters who died in the outbreak. Dreamworks Face: The Dr. Evil giant submarine has 1. At 1 issue she feared she wouldn’t get well. In 1 hot springs scene when some of the girls are bathing they get chills and believe the boys are spying on themnote they have been. The synchronisation of births is beneficial because the cubs develop to remaining about the identical size and have an equivalent prospect of survival, and sucklings are not dominated by more mature cubs.
https://salda.ws/f/topic.php?f=4&t=63255
http://artrp.5nx.ru/viewtopic.php?f=3&t=6839
buy prescription drugs from india: international medicine delivery from india – world pharmacy india indianpharm.store
indianpharmacy com Indian pharmacy to USA india online pharmacy indianpharm.store
You crave specific cure, much more privateness and undoubtedly far more discretion. Discounts & Deals- Save revenue with our specific one-way links and discount codes. My mom only gives me so substantially allowance, and a ton of that has to go toward my nacho cheese fund and the demands of my anime system pillow girlfriend. For example, Blondie Fesser shared a sizzling sex scene with Nacho Vidal in Nacho’s Monster Tits (2015). It also stars sexiest Colombian, English, Romanian, Spanish and Argentinian pornstars Franceska Jaimes, Harmony Reigns, Sandra Milka, Sensual Jane and Suhaila Hard. Pour oil on those people tits like its melted cheese fondue and check out it all drip onto your cock. If you just look at out the number of superstars taping by themselves – guess how quite a few people like you and me experienced sexual intercourse in entrance of the digital camera and how a lot of are all over on the net: More than you can see in your life. The babes who are obtaining tortured in front of the digital camera for this collection are amateurs. Actually, the only downside is the missing digicam do the job and the high quality of the video clips general.
http://mockwa.com/forum/thread-144484/
http://4division.ru/viewtopic.php?f=22&t=6794
http://forum.hi-def.ru/index.php?showtopic=21261
viagra price in india
https://risunci.com/
https://rosseriya.ru/662-dalekaja-i-blizkaja-1-sezon.html
https://rosseriya.ru/1501-chajki-1-sezon.html
https://rosseriya.ru/371-tureckiy-gambit-1-sezon.html
https://rosseriya.ru/64-vasilisa-1-sezon.html
http://mysmart.ru/index.php?/gallery/image/474-%D0%B8%D1%81%D1%82%D0%BE%D1%80%D0%B8%D1%8F-%D0%B0%D1%83%D0%B4%D0%B8%D0%BE%D1%84%D0%BE%D1%80%D0%BC%D0%B0%D1%82%D0%BE%D0%B2-%D0%BE%D1%82-%D0%B2%D0%B8%D0%BD%D0%B8%D0%BB%D0%B0-%D0%B4%D0%BE-%D1%81%D1%82%D1%80%D0%B8%D0%BC%D0%B8%D0%BD%D0%B3%D0%B0/
https://forumbar.anihub.me/viewtopic.php?id=6483#p12323
https://aznakaevsk.borda.ru/?1-3-0-00000870-000-0-0-1706616848
https://humanlove.stream/wiki/User:AlexCopland5559
Very good post.Really looking forward to read more. Great.
My website: красивое порно жмж
viagra price per pill
sveto-copy.com
http://canadadrugs.pro/# reliable mexican pharmacy
canada drug store canadian trust pharmacy drugstore online
http://rt.webcam24chat.com
Мы предлагаем возможность приобрести диплом в нашем интернет-магазине http://e-diplom.biz по доступной цене с доставкой по всей территории России. У нас в ассортименте представлены дипломы всех университетов Москвы, независимо от года выпуска и специальности.
http://translate.lotros.ru/users/72128
Designer residences at Aeternitas by London Gate in Dubai with favourable terms of purchase and return on investment.
http://canadadrugs.pro/# canadian mail order pharmacies to usa
casodex
politeconomics.org
Игорь решил открыть свою мастерскую по ремонту обуви, но ему не хватало средств на покупку начального набора инструментов. Благодаря статье, он нашел МФО, предоставившее ему 30 000 рублей, что позволило ему начать собственное дело.
DZEN Spavkin – займ кредит
**娛樂城與線上賭場:現代娛樂的轉型與未來**
在當今數位化的時代,”娛樂城”和”線上賭場”已成為現代娛樂和休閒生活的重要組成部分。從傳統的賭場到互聯網上的線上賭場,這一領域的發展不僅改變了人們娛樂的方式,也推動了全球娛樂產業的創新與進步。
**起源與發展**
娛樂城的概念源自於傳統的實體賭場,這些場所最初旨在提供各種形式的賭博娛樂,如撲克、輪盤、老虎機等。隨著時間的推移,這些賭場逐漸發展成為包含餐飲、表演藝術和住宿等多元化服務的綜合娛樂中心,從而吸引了來自世界各地的遊客。
隨著互聯網技術的飛速發展,線上賭場應運而生。這種新型態的賭博平台讓使用者可以在家中或任何有互聯網連接的地方,享受賭博遊戲的樂趣。線上賭場的出現不僅為賭博愛好者提供了更多便利與選擇,也大大擴展了賭博產業的市場範圍。
**特點與魅力**
娛樂城和線上賭場的主要魅力在於它們能提供多樣化的娛樂選項和高度的可訪問性。無論是實體的娛樂城還是虛擬的線上賭場,它們都致力於創造一個充滿樂趣和刺激的環境,讓人們可以從日常生活的壓力中短暫逃脫。
此外,線上賭場通過提供豐富的遊戲選擇、吸引人的獎金方案以及便捷的支付系統,成功地吸引了全球範圍內的用戶。這些平台通常具有高度的互動性和社交性,使玩家不僅能享受遊戲本身,還能與來自世界各地的其他玩家交流。
**未來趨勢**
隨著技術的不斷進步和用戶需求的不斷演變,娛樂城和線上賭場的未來發展呈現出多元化的趨勢。一方面,虛
擬現實(VR)和擴增現實(AR)技術的應用,有望為線上賭場帶來更加沉浸式和互動式的遊戲體驗。另一方面,對於實體娛樂城而言,將更多地注重提供綜合性的休閒體驗,結合賭博、娛樂、休閒和旅遊等多個方面,以滿足不同客群的需求。
此外,隨著對負責任賭博的認識加深,未來娛樂城和線上賭場在提供娛樂的同時,也將更加注重促進健康的賭博行為和保護用戶的安全。
總之,娛樂城和線上賭場作為現代娛樂生活的一部分,隨著社會的發展和技術的進步,將繼續演化和創新,為人們提供更多的樂趣和便利。這一領域的未來發展無疑充滿了無限的可能性和機遇。
http://commerc.webtalk.ru/viewtopic.php?id=6307#p15565
Глаз Бога — официальный телеграм бота для поиска информации о людях Удалить информацию из Глаза Бога
Trenton News – Trenton, NJ News, Sports, Weather and Things to Do https://trentonnews.us/
Глаз Бога — официальный телеграм бота для поиска информации о людях Глаз Бога 18+
Discover luxurious villas for sale in the stunning Ohana by The Sea community in Ghantoot Area, UAE. Embrace opulence and tranquility in this exclusive development offered by renowned developer Ohana Development, all at incredibly affordable prices.
canadian pharmacies no prescription: canadian pharmacies without an rx – canadian pharmacy worldwide
reliable online pharmacies accutane mexican pharmacy trusted online canadian pharmacy
Healthcare Blog provides news, trends, jobs and resources for health industry professionals. We cover topics like healthcare IT, hospital administration, polcy
https://villagewebcompany.net/index.php/User:ShoshanaDowdell
Vacavillenews.us covers local news in Vacaville, California. Keep up with all business, local sports, outdoors, local columnists and more. https://vacavillenews.us/
https://ufametallobaza1.ru/
стерилизатор с сушкой для детских бутылочек
sildenafil 50 mg price
https://canadadrugs.pro/# best canadian mail order pharmacy
http://drahthaar-club.ru/viewtopic.php?f=20&t=2172
amaryl 20mg
Ohio Reporter – Ohio News, Sports, Weather and Things to Do https://ohioreporter.us/
canadian drugstore prices canadian pharmacy no rx needed canadian pharmacy pain meds
Запустіть свою удачу в пін ап
грати в автомати https://pinupcasinolfsesn.kiev.ua/ .
krepezh.net
domfenshuy.net
http://31pokupki.rx22.ru/viewtopic.php?f=47&t=25189
Биржевая стоимость дизельного топлива у нас на сайте.
%%
Here is my webpage :: 台湾虚拟号码
Forex watchlist
Успешное казино пин-ап
jogos casino pinupcasinojenzolo.com.
Мы предлагаем услуги пассажирских перевозок в Украине и пригороде для разных целей Вінниця – Градець Кралове
viagra for female
homefronttoheartland.com
Fang Jifan은 “이리와 차를 준비하세요. 궁전에 들어가고 싶어요! “라고 말했습니다.
курсы английского курск языка
онлайн курсы английского лучшие
Мы предлагаем услуги пассажирских перевозок в Украине и пригороде для разных целей Бремен – Київ
prescription drugs canadian: canadian pharmacies without prescriptions – discount drugs online pharmacy
https://stroiteli.liveforums.ru/viewtopic.php?id=4355#p9522
обучение детей английскому языку
Ставки в пін ап – це вигідно
пінап казино http://pinupcasinolfsesn.kiev.ua/ .
курсы английского онлайн с сертификатом языка
онлайн курсы английского языка для взрослых
курсы онлайн обучения английскому языку
I like this website very much so much wonderful info.
my web-site auto store
online pharmacy review canadian pharmacy ed medications pharmacies online
Вся информация на сайте переходите и копируйте промокод 1хбет промокод на тото
курсы на английском языке
Fashion More provides in-depth journalism and insight into the news and trends impacting the fashion
pharmacies withour prescriptions: medicine from canada with no prescriptions – best mail order canadian pharmacy
Перемагайте з пін ап
азартні ігри http://www.pinupcasinolfsesn.kiev.ua .
https://pipms.wiki/Mp3bit.pw_2
viagra for women
https://canadadrugs.pro/# canadapharmacy com
online canadian pharmacy medications with no prescription best online pharmacy without prescriptions
cipro antibiotic
Good day! I know this is kinda off topic but I was wondering which blog platform are you
using for this site? I’m getting fed up of WordPress because
I’ve had issues with hackers and I’m looking at options
for another platform. I would be great if you could point me in the direction of a good platform.
my site fremont lexus
Эксклюзивное пин-ап казино
jogos de cassino online http://www.pinupcasinojenzolo.com.
Эдуард Маликович Давыдов https://www.eduard-davydov.ru/ .
https://canadadrugs.pro/# canadian pharmacy prescription
http://sebezh.borda.ru/?1-13-0-00001772-000-0-0-1706616418
%%
My web blog – pin up
Respect to post author, some fantastic information
My website: анал жестко больно
emergate.net
https://kesb-wiki.ch/index.php/Benutzer:SherryT79666207
canada drugs without prescription: canadian pharmacy no prescription – most reliable online pharmacies
Рекомендую обратить внимание на https://altaystroy.ru/ – специализированный веб-ресурс, который предоставляет ценную информацию для строительных компаний, производителей материалов и обычных потребителей. Здесь вы найдете последние новости, обзоры технологий и советы по использованию бетона и цемента в строительстве.
http://bestmedbook.mybb.ru/viewtopic.php?id=8790#p12330
Уникальное казино пин-ап
melhor casino online http://pinupcasinojenzolo.com/.
http://31pokupki.rx22.ru/viewtopic.php?f=47&t=24988
http://forum.lazarevskaya.ru/showthread.php?p=291543#post291543
great canadian pharmacy drugs without prescription recommended online pharmacies
etalonsadforum.com
my canadian drug store: canada drug prices – online pharmacies no prescription required pain medication
F*ckin’ amazing things here. I’m very glad to peer your post. Thanks a lot and i am taking a look ahead to contact you. Will you please drop me a mail?
Here is my webpage: https://www.essentialsoundproductions.com/question/myths-about-how-to-win-in-slot-machines-slot-machine-myths-2/
http://morrowindsv.2bb.ru/viewtopic.php?id=908#p2862
http://codingrus.ru/forum/viewthread.php?forum_id=32&thread_id=826
https://sciencewiki.science/wiki/User:VicenteAlbrecht
claritin 25mg
http://canadadrugs.pro/# canada drug stores
approved canadian pharmacies: best online pharmacy without prescriptions – pharmacies not requiring a prescription
Разбираем заработок в интернете: за что платят деньги в Сети, какой доход можно получать и что нужно для старта Чем дебетовая карта отличается от кредитной?
娛樂城
Discover luxury apartments and townhouses in the heart of Yas Island. Miral and 9Yards Developments present Sea La Vie Yas Bay , offering premium units at unbeatable prices. Explore endless possibilities in Abu Dhabi’s most sought-after residential towers.
avanafil pills
PЕЇjДЌka 23000 KДЌ
https://forum.resmihat.kz/viewtopic.php?f=10&t=1880559
Discover luxurious apartments and modern duplexes in the dazzling radiant square reem island. Explore the epitome of convenience and elegance in Abu Dhabi’s Reem Island. Hurry, secure your dream property at unbeatable prices with Radiant Real Estate!
https://kotya-shop.ru/
%%
Also visit my web blog https://cashout.biz/exchange-btc-to-cashusd/
https://prodvizhenieraskrutka.ru
http://canadadrugs.pro/# best online pharmacy without prescription
http://kissolovo.teamforum.ru/viewtopic.php?f=10&t=31972
Kherson Times is a dynamic online publication that serves as a reliable source of Kherson news today and information for the community of Kherson. With a commitment to delivering timely and accurate reporting, the platform covers a diverse range of topics, including local news, events, culture, and business.
Сбережём Ваше время/ Не тратьте время на поиски покупателя! Рассмотрим Вашу квартиру, даже с плохим ремонтом.
продать быстро квартиру в спб
https://rawu.info/mp3bit-pw-2/
canadian pharmacy antiobotics without perscription: best mexican online pharmacies – list of canada online pharmacies
buspar 12.5mg
PharmaMore provides a forum for industry leaders to hear the most important voices and ideas in the industry. https://pharmamore.us/
lamotrigine 50mg
https://gmzpmerger.com/
купить диплом в Москве
canadian wholesale pharmacy canadian pharmaceutical companies that ship to usa canadian pharmacies without an rx
discount pharmacy coupons: reputable canadian pharmacy – best non prescription online pharmacies
Single adult males can uncover a soul mate amongst our girls of product visual appearance and qualified sexual experience. Especially thinking about how adaptable TalkToMe is-you are going to discover specialist chat line operators and amateurs. Nightline is like a 1-dimension-fits-all free chat line for millennials. Like most other very best chat traces on our record, Nightline is also a free of charge chat line for women of all ages, and they really don’t have to commit a penny to delight in it. Some do not even have free chat strains at all! Some individuals use them for casual talks, others for cost-free cellphone connections, and some even fulfill their true love on them! Besides this, there are still several other a large amount extra unusual kinds of porn webcam web sites that will offer you you the specific exact pleasure that would definitely working experience on the even far more nicely-identified internet sites. Masturline will let you hook up with local people as well as nationwide callers by the ‘National Hotchat’ line.
%%
Here is my blog … poketoption
https://mail.obrezanie05.ru/users/202
https://shater4you.ru/
aparthome.org
Перетяжка мягкой мебели: сделайте это быстро и качественно
перетяжка мебели в минске https://peretyazhka-mebeli-vminske.ru/ .
mmo5.info
Can someone guide me on how to start with Online casino Kenya Mpesa? Newbie here.
http://trum.flybb.ru/viewtopic.php?f=10&t=3833
аренда автомобиля в малаге испания
https://lenka.ruhelp.com/viewtopic.php?id=2038#p46607
Medical More provides medical technology news and analysis for industry professionals. We cover medical devices, diagnostics, digital health, FDA regulation and compliance, imaging, and more. https://medicalmore.us
Получение диплома обÑзательно Ð´Ð»Ñ Ñ‚Ñ€ÑƒÐ´Ð¾ÑƒÑтройÑтва на выÑокооплачиваемую работу. Иногда поÑвлÑÑŽÑ‚ÑÑ Ñценарии, когда диплом, полученный ранее не подходит Ð´Ð»Ñ Ð¿Ñ€Ð¾Ñ„ÐµÑÑиональной деÑтельноÑти. Покупка документа об образовании в МоÑкве уÑтранит Ñту необходимоÑÑ‚ÑŒ и обеÑпечит уÑпешное будущее – https://kupit-diplom1.com/. СущеÑтвует множеÑтво факторов, приводÑщих к закупку документа об образовании в МоÑкве. ПоÑле некоторого времени в карьере неожиданно может возникнуть необходимоÑÑ‚ÑŒ в универÑитетÑком дипломе. Работодатель вправе менÑÑ‚ÑŒ Ñ‚Ñ€ÐµÐ±Ð¾Ð²Ð°Ð½Ð¸Ñ Ðº перÑоналу и принудить Ð²Ð°Ñ Ñделать выбор – получить диплом или покинуть должноÑÑ‚ÑŒ. Учеба на дневном отделении занимает много времени и Ñнергии, а заочное обучение — требует денег на Ñкзамены. Ð’ таких ÑитуациÑÑ… лучше приобреÑти готовый документ. ЕÑли вы уже знакомы Ñ Ð¾ÑобенноÑÑ‚Ñми будущей профеÑÑии и научилиÑÑŒ необходимым навыкам, не имеет ÑмыÑла тратить годы на обучение в ВУЗе. ПлюÑÑ‹ Ð¿Ñ€Ð¸Ð¾Ð±Ñ€ÐµÑ‚ÐµÐ½Ð¸Ñ Ð´Ð¸Ð¿Ð»Ð¾Ð¼Ð° включают Ñкорое производÑтво, полное Ñовпадение Ñ Ð¾Ñ€Ð¸Ð³Ð¸Ð½Ð°Ð»Ð¾Ð¼, доÑтупную цену, гарантию трудоуÑтройÑтва, возможноÑÑ‚ÑŒ оценить Ñвой уÑпех ÑамоÑтоÑтельно и комфортную доÑтавку. Ðаша фирма предлагает возможноÑÑ‚ÑŒ вÑем желающим получить желаемую работу. Цена Ð¸Ð·Ð³Ð¾Ñ‚Ð¾Ð²Ð»ÐµÐ½Ð¸Ñ Ð´Ð¾ÐºÑƒÐ¼ÐµÐ½Ñ‚Ð¾Ð² доÑтупна, что делает данное предложение доÑтупным Ð´Ð»Ñ Ð²Ñех.
Официальный сервис Krups по ремонту. Профессиональный ремонт любых типов кофемашин сервисный центр крупс в спб
Официальный сервис Krups по ремонту. Профессиональный ремонт любых типов кофемашин ремонт кофемолки krups
best canadian drugstore: mexican pharmacies that ship – best canadian mail order pharmacy
https://canadadrugs.pro/# best internet pharmacies
http://domod.3nx.ru/viewtopic.php?p=26843#26843
I’m extremely pleased to discover this website. I wanted to thank you for ones time just for this fantastic read!
My website: любительский инцест
http://kupitkvartiruion.ru
[url=http://morninglabs.com/mobile/producte/mango-womens-bag/#comment-286976]sdfghytred[/url] 4c517_4
http://kupitkvartiruence.ru
[url=http://gaoncamp.com/bbs/board.php?bo_table=free1&wr_id=21867]cerwcecww[/url] 518_0b9
http://kvartirazhkmalosemejka.ru
[url=https://jjjjjj151.com/odyssey-toys-x-7-microlite-review-this-sprightly-microdrone-lights-up-the-night/comment-page-26413/#comment-315507]sdfghytred[/url] 22246b8
http://referatyliteratura.ru
[url=https://qualitytools.co.ug/index.php/2021/10/25/hello-world/#comment-10418]sdfghytred[/url] b12a1b5
best canadian pharmacy cialis: canadian pharmacy testosterone – us canadian pharmacy
Thanks , I’ve recently been looking for info approximately this subject for a while and yours is the greatest I’ve discovered till
now. However, what about the bottom line? Are you positive in regards to the supply?
my page: used lexus is300
http://canadadrugs.pro/# canadian pharmacy selling viagra
http://cluster.shao.ac.cn/i18n/index.php?title=User:ChristelAntonio
камин электронный
https://box-send.ru/
Payday loans in Tennessee
I’m likewise to drawn in to persons who, like me, existing as gender-nonconforming, nonetheless it does not feel like Chaturbate has the language or consumer interface available for me to look through entertainers who identify with that criteria. As a person who is 1, I adore an industrious individual – and it’s even better when a person has a overall body that looks like Halle Von’s. Many of the will work published in the Victorian era are thought of bold and graphic even by present day lenient standards. At close to the identical time, erotic graphic art that commenced to be thoroughly developed in Paris came to be regarded in the Anglosphere as “French postcards”. When significant-scale archaeological excavations had been undertaken in the ancient Roman metropolis of Pompeii throughout the 18th century, significantly of the erotic art in Pompeii and Herculaneum came to light, shocking the authorities who endeavored to conceal them away from the common general public. Jack Lemmon is pitch-perfect as an office drone whose bachelor condominium will become the go-to hideaway for his company superiors, and so a tool for climbing to their ranks Shirley MacLaine sparkles as the elevator operator who catches his extravagant, and who has a key or two of her individual.
list of reputable canadian pharmacies: prescription drugs canadian – discount pharmacies online
https://www.wildberries.ru/catalog/141937472/detail.aspx
http://www.bisound.com/forum/showthread.php?p=601725
http://doorsmania.borda.ru/?1-6-0-00001153-000-0-0-1706616995
http://sebezh.borda.ru/?1-13-0-00001772-000-0-0-1706616418
online pharmacy no prescriptions: prescription drugs online – legitimate online pharmacy
viagra professional 100mg
naoni.info
https://canadadrugs.pro/# canada pharmacy not requiring prescription
http://ya.10bb.ru/viewtopic.php?id=2406#p4422
http://www.diablomania.ru/forum/showthread.php?t=432376
Очень не плохо написано, РЕАЛЬНО….
The rhythm is contagious, and with lyrics compositions will definitely make the https://rafaelcdzx01100.bloguetechno.com/ordering-enchantment-strippers-tailored-to-your-desires-60168093 start corporate. Rihanna’s song “pour it up” should be the beginning of any striptease show!
https://womens-forum.ru/viewtopic.php?f=59&t=5511&sid=055207bff02b47315d35ed57e0d4029f
Рекомендую обратить внимание на https://altaystroy.ru/ – специализированный веб-ресурс, который предоставляет ценную информацию для строительных компаний, производителей материалов и обычных потребителей. Здесь вы найдете последние новости, обзоры технологий и советы по использованию бетона и цемента в строительстве.
Virtueel nummer, een telefoonnummer dat bestaat zonder fysieke aansluiting op een telefoonlijn https://dominickmgztl.livebloggs.com/30995288/koop-een-virtueel-telefoonnummer
http://aurorahcs.com/forum/viewtopic.php?f=8&t=553472
Virtueel nummer, een telefoonnummer dat bestaat zonder fysieke aansluiting op een telefoonlijn https://donovanxcgj06283.tblogz.com/koop-een-virtueel-telefoonnummer-39332039
Discover the epitome of luxury living at Renad Tower – where elite apartments harmonize with opulence. Immerse yourself in the ultimate residential experience offered by the renowned developer Tiger Properties and redefine your definition of lavish real estate.
Lost my phone but need to access my Kenya Mpesa. Any tips on what I should do?
https://hikvisiondb.webcam/wiki/Mp3bit.pw_3
stroihome.net
Как освежить интерьер дома в короткие сроки
обтяжка мебели https://peretyazhka-mebeli-vminske.ru/ .
https://canadadrugs.pro/# prescription meds without the prescription
buy prescription drugs online legally: no 1 canadian pharcharmy online – canadian pharmacy no presciption
sildenafil 25mg
San Gabriel Valley News is the local news source for Los Angeles County
Local news from Redlands, CA, California news, sports, things to do, and business in the Inland Empire. https://redlandsnews.us
https://www.izhforum.info/forum/izhevsk/viewtopic.php?f=52&t=148848
https://canadadrugs.pro/# highest rated canadian pharmacies
https://всероссийская-база-ту.рф/
https://vitrinapress.ru/
Viagra 100mg
outro
todayusanews24.com
http://veniaminv.flybb.ru/viewtopic.php?f=1&t=1717
Интересная тема, приму участие.
now, when you are here, let us to explain how people are ready help to you and your guest to arrange the best https://zaneijfw99456.yomoblog.com/30817820/elevate-your-event-with-our-beautiful-strippers for history.
drugs online: canadian online pharmacies – pharmacies canada
ukrtvoru.info
ecohouse.info
cost for viagra
prescription drug discounts: online prescriptions without a doctor – best online drugstore
https://able.extralifestudios.com/wiki/index.php/User:JettaSolis5196
http://canadadrugs.pro/# canadian pharmacy ed medications
NewsBreak provides latest and breaking Renton, WA local news, weather forecast, crime and safety reports, traffic updates, event notices, sports https://rentonnews.us
hjem
Bellevue Latest Headlines: City of Bellevue can Apply for Digital Equity Grant https://bellevuenews.us
sildenafil femme
Новый облик старой мягкой мебели
ремонт мягкой мебели в минске https://peretyazhka-mebeli-vminske.ru/ .
%%
Look into my site :: https://erickkhtd97418.aioblogs.com/78517794/bringing-the-best-strippers-to-your-doorstep
http://o91707v5.beget.tech/2024/02/01/process-sozdaniya-hip-hop-treka-ot-idey-do-zapisi.html
http://canadadrugs.pro/# recommended online pharmacies
More information about your request is here https://www.fequip.com.br/cliente/?idc=19&url=https://mrfeelgood.ca/
Great post thank you. Hello Administ .
More information about your request is here https://www.widzewiak.pl/hitredir/ff454cd2cee5db15f7920cc7f821bad6?url=https://rentcars.buzz/
http://forum.gold-forum.ru/index.php?showtopic=69337
sildenafil citrate over the counter
промокод 1xbet
http://kome.maxbb.ru/viewtopic.php?f=3&t=1272
canadian pharmacy price checker: usa online pharmacy – canada pharmacy no prescription
https://positiv-servis.ru/
female viagra pills
online canadian pharcharmy: certified canadian pharmacy – canadian mail order pharmacies
Viagra Professional
http://forums.kuban.ru/showthread.php?p=49279134
I recommend this best product Killa Dry Banana Ice to all!
Всем рекомендую именно этоКазино онлайн
Very good product Killa Dry Blueberry
http://canadadrugs.pro/# canadian pharmacy azithromycin
https://lovewiki.faith/wiki/Mp3bit.pw
cheap viagra 50mg
https://canadadrugs.pro/# best canadian pharmacy for viagra
Вы абсолютно правы. В этом что-то есть и мне кажется это очень хорошая мысль. Полностью с Вами соглашусь.
Игра со всех сторон (Книга о том, как играют ребята, и производственные люди). Существуют инновационные, позиционные https://wellnessandspabooking.com/index.php/component/k2/item/3 (А.
canada drug store: reputable online pharmacy – top rated canadian mail order pharmacies
pervenec.com
viagra coupons
As a Newbie, I am always searching online for articles that can help me. Thank you
My website: домашний сквирт
http://tumgerl.rolbb.me/viewtopic.php?id=11595#p17854
Brand Viagra 25mg
1newss.com
Understanding the processes and protocols within a Professional Tenure Committee (PTC) is crucial for faculty members. This Frequently Asked Questions (FAQ) guide aims to address common queries related to PTC procedures, voting, and membership.
1. Why should members of the PTC fill out vote justification forms explaining their votes?
Vote justification forms provide transparency in decision-making. Members articulate their reasoning, fostering a culture of openness and ensuring that decisions are well-founded and understood by the academic community.
2. How can absentee ballots be cast?
To accommodate absentee voting, PTCs may implement secure electronic methods or designated proxy voters. This ensures that faculty members who cannot physically attend meetings can still contribute to decision-making processes.
3. How will additional members of PTCs be elected in departments with fewer than four tenured faculty members?
In smaller departments, creative solutions like rotating roles or involving faculty from related disciplines can be explored. Flexibility in election procedures ensures representation even in departments with fewer tenured faculty members.
4. Can a faculty member on OCSA or FML serve on a PTC?
Faculty members involved in other committees like the Organization of Committee on Student Affairs (OCSA) or Family and Medical Leave (FML) can serve on a PTC, but potential conflicts of interest should be carefully considered and managed.
5. Can an abstention vote be cast at a PTC meeting?
Yes, PTC members have the option to abstain from voting if they feel unable to take a stance on a particular matter. This allows for ethical decision-making and prevents uninformed voting.
6. What constitutes a positive or negative vote in PTCs?
A positive vote typically indicates approval or agreement, while a negative vote signifies disapproval or disagreement. Clear definitions and guidelines within each PTC help members interpret and cast their votes accurately.
7. What constitutes a quorum in a PTC?
A quorum, the minimum number of members required for a valid meeting, is essential for decision-making. Specific rules about quorum size are usually outlined in the PTC’s governing documents.
Our Plan Packages: Choose The Best Plan for You
Explore our plan packages designed to suit your earning potential and preferences. With daily limits, referral bonuses, and various subscription plans, our platform offers opportunities for financial growth.
Blog Section: Insights and Updates
Stay informed with our blog, providing valuable insights into legal matters, organizational updates, and industry trends. Our recent articles cover topics ranging from law firm openings to significant developments in the legal landscape.
Testimonials: What Our Clients Say
Discover what our clients have to say about their experiences. Join thousands of satisfied users who have successfully withdrawn earnings and benefited from our platform.
Conclusion:
This FAQ guide serves as a resource for faculty members engaging with PTC procedures. By addressing common questions and providing insights into our platform’s earning opportunities, we aim to facilitate a transparent and informed academic community.
Вигравайте в пін ап
автомати ігри https://www.pinupcasinolfsesn.kiev.ua/ .
https://canadadrugs.pro/# certified canadian pharmacy
https://love.boltun.su/viewtopic.php?id=6629#p11265
kliknД›te na tento odkaz
sildenafil india
https://samara110.ru/forum/viewtopic.php?f=15&t=4362
https://forum.sportmashina.com/index.php?threads/istorija-zhanra-chillout.4902/
canadian pharmacy certified: no prescription canadian pharmacies – top rated online canadian pharmacies
http://canadadrugs.pro/# canadian mail order pharmacy
canadian mail order viagra the discount pharmacy the generics pharmacy online delivery
non prescription viagra
https://samaramed.ru/forum/health/topic_39949.html
http://forumrabota.0pk.me/viewtopic.php?id=6669#p16048
buying viagra online forum
Earn real cash with these fun games in Kenya
online casino games that pay real money games that pay real money in kenya .
Заказать и получить легальный диплом института можно у нас на сайте http://diplomguru.com. Мы предлагаем надежность и выгодные условия.
Казино Гама входит в рейтинг лучших азартных заведений для игры на реальные деньги, где вход на официальный сайт доступен через рабочее зеркало Gama Gama casino
http://medicinefromindia.store/# reputable indian pharmacies
Казино Гама входит в рейтинг лучших азартных заведений для игры на реальные деньги, где вход на официальный сайт доступен через рабочее зеркало Gama Гама казино
best pill for ed the best ed pills natural remedies for ed
предметная съемка цены москва https://predmetnaya-fotosyomka-1.ru/
Евтушенков Феликс биография и последние новости
Discover your dream home at Jamam Residence. Explore our extensive collection of luxurious ready-to-move-in residences, carefully designed by developer Dhabi Contracting LLC. Experience the ultimate blend of contemporary architecture, premium amenities, and competitive prices in the heart of this vibrant coastal city.
Евтушенков Феликс биография и последние новости
ressurs
modernkarachi.com
그러나 어디에서나 그녀는 씨족의 위치에 서서 그들의 미래를 생각했습니다.
buy prednisone online for humans
https://canadianinternationalpharmacy.pro/# canadian pharmacy near me
Я думаю, что Вы не правы. Предлагаю это обсудить.
в результате их получения произойдет рулонный газон цена увеличение отходов. Под плотной тканью корни сорняков выпревают.
https://homeopatia.ixbb.ru/viewtopic.php?id=1043#p2160
Добро пожаловать в увлекательный мир SEO – инструмента, который может стать настоящим катализатором роста вашего бизнеса доставка пиццы
legitimate canadian mail order pharmacy: cross border pharmacy canada – reliable canadian pharmacy reviews
%%
mexican border pharmacies shipping to usa medication from mexico pharmacy buying prescription drugs in mexico
kinoboomhd.com
그런 다음 Zhu Houzhao는 Wang Yong의 입에 채워진 면포를 꺼냈습니다.
sildenafil no prescription
What’s up, after reading this awesome article i am as well happy to
share my experience here with mates.
abilify 2017
mexico drug stores pharmacies: buying prescription drugs in mexico – mexican pharmaceuticals online
http://www.forumklassika.ru/member.php?u=154962
mexican rx online mexico pharmacy pharmacies in mexico that ship to usa
https://canadianinternationalpharmacy.pro/# reliable canadian pharmacy
generic viagra canada
https://spaincostablanca.ru/
Поможем Вам купить диплом техникума http://diplom-sale.ru/ , училища – недорого, без предоплаты с доставкой в ваш город.
http://veniaminv.flybb.ru/viewtopic.php?f=1&t=1717
%%
Позитивное казино пин-ап
pin up site oficial https://pinupcasinojenzolo.com.
Kredit 8000 Euro
amazon viagra
https://certifiedpharmacymexico.pro/# mexico drug stores pharmacies
salaty-na-stol.info
Официальный сайт Гама радует своих поклонников оригинальным стильным оформлением, грамотной структурой меню и разнообразием направлений в играх Гама казино
reputable indian online pharmacy: reputable indian pharmacies – mail order pharmacy india
Официальный сайт Гама радует своих поклонников оригинальным стильным оформлением, грамотной структурой меню и разнообразием направлений в играх Гама казино
indian pharmacy paypal top online pharmacy india indian pharmacy online
audio-kravec.com
https://mirkamnya.su/
%%
Feel free to surf to my web blog; http://www.anikolsky.com
http://konstruktiv.getbb.ru/viewtopic.php?f=20&t=3992
top 10 online pharmacy in india: top online pharmacy india – Online medicine home delivery
discount viagra usa
Эдуард Давыдов карьера, последние новости Эдуард Давыдов
canadian drug canadian pharmacy cheap canada discount pharmacy
http://artem-energo.ru/forums.php?m=posts&q=16117&n=last#bottom
%%
Feel free to visit my webpage; https://www.bibliogemma.com/cb-profile/pluginclass/cbblogs?action=blogs&func=show&id=95
http://khv.forum-top.ru/viewtopic.php?id=1257#p12607
sildenafil generic
%%
Have a look at my web-site https://www.vtm.group/es/categoria-producto/turbocharger-repair-equipment-es/
https://edwithoutdoctorprescription.pro/# best non prescription ed pills
sildenafil 20 mg tablet
п»їerectile dysfunction medication ed remedies cure ed
buying prescription drugs in mexico online: mexico pharmacy – mexican online pharmacies prescription drugs
generic viagra canada
%%
Look into my web page … https://bitkeep-wallet.io/
clarinex online-apotheke kaufen
stroynews.info
auto-kar.net
https://canadianinternationalpharmacy.pro/# my canadian pharmacy
order viagra online
Мы предлагаем широкий ассортимент документов о среднем и высшем образовании. Наш интернет-ресурс https://diplomguru.com позволяет заказать и приобрести диплом техникума без необходимости внесения предоплаты.
cialis without doctor prescription generic cialis without a doctor prescription viagra without a doctor prescription walmart
%%
Also visit my web blog … https://faylinn.clinic/2023/12/26/legitimate-500-no-deposit-incentive-codes-2024-australian-continent-500-aud-totally-free-casino-incentives/
Thanks for the complete information. You helped me.
http://certifiedpharmacymexico.pro/# mexican border pharmacies shipping to usa
Демонтаж и снос старых домов с вывозом мусора в Москве и Московской области. Разборка фундаментов – узнайте больше об услуге на сайте snos96.ru. Производим демонтаж домов и фундаментов вручную и спецтехникой по ценам ниже рынка за 1 день. Бесплатный выезд оценщика на объект.
tadalafil without a doctor’s prescription generic cialis without a doctor prescription ed meds online without doctor prescription
how BioHealth CBD Gummies work
2fight.info
Lainaa 400000 euroa
Родился 10 июля 1984 в Нальчике Кабардино-Балкарской Республики. Отец – ученый-химик, сотрудник лаборатории Кабардино-Балкарского государственного университета; мать – медсестра в поликлинике Эдуард Давыдов
online pay per click
Understanding the processes and protocols within a Professional Tenure Committee (PTC) is crucial for faculty members. This Frequently Asked Questions (FAQ) guide aims to address common queries related to PTC procedures, voting, and membership.
1. Why should members of the PTC fill out vote justification forms explaining their votes?
Vote justification forms provide transparency in decision-making. Members articulate their reasoning, fostering a culture of openness and ensuring that decisions are well-founded and understood by the academic community.
2. How can absentee ballots be cast?
To accommodate absentee voting, PTCs may implement secure electronic methods or designated proxy voters. This ensures that faculty members who cannot physically attend meetings can still contribute to decision-making processes.
3. How will additional members of PTCs be elected in departments with fewer than four tenured faculty members?
In smaller departments, creative solutions like rotating roles or involving faculty from related disciplines can be explored. Flexibility in election procedures ensures representation even in departments with fewer tenured faculty members.
4. Can a faculty member on OCSA or FML serve on a PTC?
Faculty members involved in other committees like the Organization of Committee on Student Affairs (OCSA) or Family and Medical Leave (FML) can serve on a PTC, but potential conflicts of interest should be carefully considered and managed.
5. Can an abstention vote be cast at a PTC meeting?
Yes, PTC members have the option to abstain from voting if they feel unable to take a stance on a particular matter. This allows for ethical decision-making and prevents uninformed voting.
6. What constitutes a positive or negative vote in PTCs?
A positive vote typically indicates approval or agreement, while a negative vote signifies disapproval or disagreement. Clear definitions and guidelines within each PTC help members interpret and cast their votes accurately.
7. What constitutes a quorum in a PTC?
A quorum, the minimum number of members required for a valid meeting, is essential for decision-making. Specific rules about quorum size are usually outlined in the PTC’s governing documents.
Our Plan Packages: Choose The Best Plan for You
Explore our plan packages designed to suit your earning potential and preferences. With daily limits, referral bonuses, and various subscription plans, our platform offers opportunities for financial growth.
Blog Section: Insights and Updates
Stay informed with our blog, providing valuable insights into legal matters, organizational updates, and industry trends. Our recent articles cover topics ranging from law firm openings to significant developments in the legal landscape.
Testimonials: What Our Clients Say
Discover what our clients have to say about their experiences. Join thousands of satisfied users who have successfully withdrawn earnings and benefited from our platform.
Conclusion:
This FAQ guide serves as a resource for faculty members engaging with PTC procedures. By addressing common questions and providing insights into our platform’s earning opportunities, we aim to facilitate a transparent and informed academic community.
Обратившись к нам, Вы получите честную юридически оформленную сделку, что является важным критерием при продаже недвижимости. Мы не являемся посредниками и выкупаем квартиры за собственные деньги.
выкуп жилого помещения
Hey would you mind stating which blog platform you’re using?
I’m looking to start my own blog soon but I’m having a difficult time deciding between BlogEngine/Wordpress/B2evolution and
Drupal. The reason I ask is because your design seems different then most blogs and I’m looking for something completely unique.
P.S Sorry for being off-topic but I had to ask!
http://edwithoutdoctorprescription.pro/# best non prescription ed pills
hemp gummies
Избавьтесь от лишних хлопот по доставке холодильника, плиты или стиральной машины – наши специалисты самостоятельно заберут вышедшее из строя устройство, а после привезут обратно
mexican pharmaceuticals online mexican mail order pharmacies mexican border pharmacies shipping to usa
http://medicinefromindia.store/# top 10 online pharmacy in india
Nufarm CBD Gummies buy online
https://seductrice.ru/ новые женские сайты
oda-radio.com
plavix 200mcg
PureKana cbd GUMMIES ingredient
pet meds without vet prescription canada: canadian drug pharmacy – pharmacy canadian
На рабочем совещании по перспективам развития АО «БСК» под председательством главы РБ Радия Хабирова в модернизацию трех производственных площадок Давыдов Эдуард
Natuurlijk, een ring kan altijd verkleind of vergroot worden, maar het is
uiteraard veel beter als deze in één keer als gegoten past.
сантехник на дом недорого http://keramogranit-krasnodar.ru/ .
buy prescription drugs from india india pharmacy mail order п»їlegitimate online pharmacies india
CBD Gummies
http://medicinefromindia.store/# indianpharmacy com
get paid $1 per click
Understanding the processes and protocols within a Professional Tenure Committee (PTC) is crucial for faculty members. This Frequently Asked Questions (FAQ) guide aims to address common queries related to PTC procedures, voting, and membership.
1. Why should members of the PTC fill out vote justification forms explaining their votes?
Vote justification forms provide transparency in decision-making. Members articulate their reasoning, fostering a culture of openness and ensuring that decisions are well-founded and understood by the academic community.
2. How can absentee ballots be cast?
To accommodate absentee voting, PTCs may implement secure electronic methods or designated proxy voters. This ensures that faculty members who cannot physically attend meetings can still contribute to decision-making processes.
3. How will additional members of PTCs be elected in departments with fewer than four tenured faculty members?
In smaller departments, creative solutions like rotating roles or involving faculty from related disciplines can be explored. Flexibility in election procedures ensures representation even in departments with fewer tenured faculty members.
4. Can a faculty member on OCSA or FML serve on a PTC?
Faculty members involved in other committees like the Organization of Committee on Student Affairs (OCSA) or Family and Medical Leave (FML) can serve on a PTC, but potential conflicts of interest should be carefully considered and managed.
5. Can an abstention vote be cast at a PTC meeting?
Yes, PTC members have the option to abstain from voting if they feel unable to take a stance on a particular matter. This allows for ethical decision-making and prevents uninformed voting.
6. What constitutes a positive or negative vote in PTCs?
A positive vote typically indicates approval or agreement, while a negative vote signifies disapproval or disagreement. Clear definitions and guidelines within each PTC help members interpret and cast their votes accurately.
7. What constitutes a quorum in a PTC?
A quorum, the minimum number of members required for a valid meeting, is essential for decision-making. Specific rules about quorum size are usually outlined in the PTC’s governing documents.
Our Plan Packages: Choose The Best Plan for You
Explore our plan packages designed to suit your earning potential and preferences. With daily limits, referral bonuses, and various subscription plans, our platform offers opportunities for financial growth.
Blog Section: Insights and Updates
Stay informed with our blog, providing valuable insights into legal matters, organizational updates, and industry trends. Our recent articles cover topics ranging from law firm openings to significant developments in the legal landscape.
Testimonials: What Our Clients Say
Discover what our clients have to say about their experiences. Join thousands of satisfied users who have successfully withdrawn earnings and benefited from our platform.
Conclusion:
This FAQ guide serves as a resource for faculty members engaging with PTC procedures. By addressing common questions and providing insights into our platform’s earning opportunities, we aim to facilitate a transparent and informed academic community.
https://prodvizheniekontekstnayareklama.ru
therazen CBD Gummies reviews
https://certifiedpharmacymexico.pro/# mexican online pharmacies prescription drugs
biznesnewss.com
Эдуард Давыдов имеет несколько высших образований. Он окончил РХТУ им. Менделеева на бюджетной основе, живя в общежитии в скромных условиях Эдуард Давыдов
Thanks-a-mundo for the post.Really thank you! Awesome.
My website: жены любящие групповухи
п»їlegitimate online pharmacies india mail order pharmacy india indian pharmacy
sildenafil no prescription
when viagra generic
antivert
buy medicines online in india: best india pharmacy – india pharmacy mail order
radioshem.net
ed meds online without doctor prescription generic cialis without a doctor prescription buy prescription drugs from canada cheap
sildenafil sans ordonnance
https://edpill.cheap/# new ed pills
Рекомендую официальный телеграм канал 1Win регистрация
best online pharmacy india: indian pharmacy online – buy prescription drugs from india
%%
Also visit my blog: Herhangi bir cihaza 1xbet indirme
amazon viagra
can you buy viagra online
canada drug pharmacy rate canadian pharmacies canadian pharmacy phone number
https://certifiedpharmacymexico.pro/# reputable mexican pharmacies online
sildenafil 20 mg tablet
financenewsasia.com
http://canadianinternationalpharmacy.pro/# safe canadian pharmacy
sildenafil buy
Даркнет, представляет собой, тайную, инфраструктуру, на, глобальной сети, подключение, реализуется, через, особые, приложения плюс, технические средства, гарантирующие, конфиденциальность участников. Одним из, этих, средств, представляется, Тор браузер, который, обеспечивает, приватное, подключение в сеть Даркнет. При помощи, его же, участники, имеют возможность, сокрыто, заходить, сайты, не индексируемые, стандартными, поисковыми системами, что делает возможным, обстановку, для проведения, разносторонних, нелегальных операций.
Кракен, в результате, часто упоминается в контексте, скрытой сетью, в качестве, рынок, для, криминалитетом. На данной платформе, есть возможность, приобрести, разнообразные, непозволительные, услуги, начиная от, наркотиков и оружия, доходя до, хакерскими действиями. Ресурс, гарантирует, крупную долю, шифрования, а, защиты личной информации, это, предоставляет, эту площадку, привлекательной, для тех, кто, желает, предотвратить, негативных последствий, со стороны соответствующих правоохранительных органов
canadianpharmacyworld canadian drugstore online canadian 24 hour pharmacy
generic viagra canada
Эдуард Давыдов проявил активность в экологической сфере, внедряя проекты, направленные на сокращение вредных выбросов и улучшение окружающей среды Эдуард Давыдов
Эдуард Давыдов проявил активность в экологической сфере, внедряя проекты, направленные на сокращение вредных выбросов и улучшение окружающей среды Давыдов Эдуард
http://poker.forum-top.ru/viewtopic.php?id=601#p2402
20Bet website
кракен kraken kraken darknet top
Темная сторона интернета, это, анонимную, сеть, в, сети, вход, происходит, по средствам, уникальные, софт а также, инструменты, обеспечивающие, скрытность участников. Из числа, подобных, средств, считается, браузер Тор, который позволяет, гарантирует, приватное, подключение к интернету, к сети Даркнет. С помощью, его же, сетевые пользователи, могут иметь возможность, анонимно, посещать, веб-сайты, не индексируемые, обычными, поисковыми системами, создавая тем самым, условия, для проведения, разнообразных, нелегальных операций.
Кракен, в свою очередь, часто ассоциируется с, скрытой сетью, как, рынок, для, киберугрозами. На этом ресурсе, имеется возможность, купить, разные, непозволительные, вещи, начиная, наркотиков и стволов, вплоть до, услугами хакеров. Платформа, обеспечивает, высокий уровень, шифрования, и также, анонимности, это, делает, данную систему, привлекательной, для тех, кто, желает, уклониться от, негативных последствий, со стороны соответствующих органов порядка.
https://edwithoutdoctorprescription.pro/# legal to buy prescription drugs from canada
cialis without a doctor’s prescription buy prescription drugs from canada prescription drugs without doctor approval
Зеркало Гама казино — это передовая платформа для онлайн-игр, которая предлагает захватывающий опыт, наполненный великолепной графикой, реалистичными звуковыми эффектами и простыми в использовании элементами управления Гама зеркало
Зеркало Гама казино — это передовая платформа для онлайн-игр, которая предлагает захватывающий опыт, наполненный великолепной графикой, реалистичными звуковыми эффектами и простыми в использовании элементами управления казино гама зеркало
PlayOJO apk
ochen-vkusno.com
http://certifiedpharmacymexico.pro/# mexico pharmacy
*- за исключением диванов по специальному предложению, эту информацию можно уточнить у менеджера по продажам https://by-home.ru/stulya/10623-stul-miss-grushovka.html
Modeled following gay pleasure situations, they frequently examine their efforts to the civil rights and LGBT social movements. Sociological exploration has also investigated how social institutions, especially family members, cope with the difficulties affiliated with autism. Autism Acceptance Day is now held each April. It is now a big event celebrated in several nations. The party begun as a modest thought in the front area of British autism campaigners, Ivan and Charika Corea. The plan for the party developed out of opposition to a “Communication Shutdown” fundraising campaign led by Autism Speaks that year, which experienced asked for members to “simulate” possessing autism by being absent from all sorts of on line conversation for just one working day. Autism Awareness Year was led by the British Institute of Brain Injured Children, Disabilities Trust, The Shirley Foundation, National Autistic Society, Autism London and 800 companies in the United Kingdom. Many of these portrayals have been inaccurate, and have contributed to a divergence in between public perception and the medical reality of autism. These depictions of autism in media currently are typically designed in a way that brings pity to the community and their problem of the topic, simply because their viewpoint is hardly ever actually demonstrated, leaving the community without having information of autism and its prognosis.
medicine in mexico pharmacies purple pharmacy mexico price list mexican online pharmacies prescription drugs
A lot of blog writers nowadays yet just a few have blog posts worth spending time on reviewing.
My website: голые маленькие сиськи
Betwinner website
bwin indir – Online Bahis Şirketi
https://canadianinternationalpharmacy.pro/# legit canadian pharmacy
new ed treatments
Тренинги по продажам и переговорам для менеджеров, руководителей отдела продаж под ключ тренинг по продажам для менеджеров
Тренинги по продажам и переговорам для менеджеров, руководителей отдела продаж под ключ тренинги по продажам
Николаев Вячеслав Контантинович https://vyacheslav-konstantinovich-nikolaev.ru/ .
https://edwithoutdoctorprescription.pro/# real cialis without a doctor’s prescription
legal to buy prescription drugs from canada best rated canadian pharmacy trustworthy canadian pharmacy
best medicine for erectile dysfunction without side effects
compazine canada
Качественная имплантация в Сочи под ключ, статья о лучшей стоматологии для имплантации имплантация зубов
Качественная имплантация в Сочи под ключ, статья о лучшей стоматологии для имплантации https://privetsochi.ru/blog/Flood/93115.html
промокод для 1xbet
best male ed pills
Нужно получить смс на виртуальный номер? Бесплатные виртуальные номера онлайн для получения кодов верификации аренда мобильного номера
рунетки пары
Нужно получить смс на виртуальный номер? Бесплатные виртуальные номера онлайн для получения кодов верификации аренда номера телефона
male ed drugs best ed treatment pills ed pills
http://canadianinternationalpharmacy.pro/# canada drugs online review
strongest medications for erectile dysfunction
%%
Also visit my web blog … https://graph.org/withslotss-09-13
магазин керамической плитки
https://canadianinternationalpharmacy.pro/# cheap canadian pharmacy
Hi there! This is kind of off topic but I need some
help from an established blog. Is it very difficult to set up your
own blog? I’m not very techincal but I can figure things out pretty fast.
I’m thinking about setting up my own but I’m not
sure where to begin. Do you have any ideas or suggestions?
With thanks
treatment for ed
look here
http://freelancing.md/project/683
best ed pill the best ed pills ed pill
ed drugs generic
Pills information for patients. What side effects?
diltiazem
Some trends of meds. Get information here.
code promo 1xbet gabon a l’inscription et obtenez un bonus de 130?/$. Le bonus de bienvenue de 100% de paris sportifs et de casino vous donne la possibilite d’utiliser de l’argent gratuit de 1xbet. Le format de presque toutes les activites des bookmakers implique la presence d’un programme de bonus. Grace aux bonus fournis, le bookmaker tente d’accroitre son attractivite aux yeux des clients potentiels. Quant aux joueurs, ils peuvent placer des paris au detriment des bonus sans trop de risques, augmentant leurs chances de gagner. Dans le meme ordre d’idees, le programme de bonus du bookmaker 1xBet dans son ensemble et chacun de ses elements separement doivent etre pris en compte.
Mostbet промокод на сегодня 2024. Чтобы удовлетворить потребности бетторов и сделать процесс ставок максимально разнообразным нередко букмекерские конторы пытаются увеличить свой функционал, путем добавления специальных функций и предложений. Одним из лидеров среди популярных букмекеров на постсоветском пространстве по своим функциональным возможностям является Мостбет. Ввод мостбет промокоды позволяет получить увеличенную сумму бонуса. Для этого достаточно после создания аккаунта внести первый депозит (максимальная сумма бонусного начисления составляет 35 000 рублей). Можно использовать любой платёжный метод. Абсолютно бесплатный промокод Mostbet. На сегодня контора предлагает всем новичкам воспользоваться не только приветственным бонусом, но и получить дополнительные преференции. Эти льготы игрок получает в том случае, если внимательно отнесётся к процедуре регистрации на сайте. Ведь не все новички обращают внимание или понимают, о каких выгодах идёт речь, когда видят необязательное для заполнения поле «Введите промокод (при наличии)», находящееся в самом низу регистрационной формы. Оно есть при трёх способах получения аккаунта из четырёх возможных («В 1 клик», «По номеру телефона», «По e-mail»). А игнорировать его – это потерять дополнительные выгоды.
best medication for ed
http://edwithoutdoctorprescription.pro/# buy prescription drugs from canada
It’s an remarkable paragraph designed for all the internet visitors; they will obtain benefit from it I am sure.
Here is my homepage https://188.166.212.11
Medicines prescribing information. What side effects?
get zoloft
Everything information about pills. Read information now.
I every time spent my half an hour to read this
website’s articles or reviews all the time along with a mug of coffee.
Look into my blog post: https://blazebett.com
online pharmacy india indian pharmacy online п»їlegitimate online pharmacies india
Services on the Internet which are in demand constantly! search on] map of Australia, India, Mexico, United States of America in the public domain opened on usa-map.online] web.
satellite] Afghanistan, Albania, Bangladesh, Bosnia and Herzegovina, Estonia, Dominica or Dominican Republic, Germany map every city street] up-to-date data space industry. location on] map of Barbados, Angola, Jamaica, rich in traditions Mongolia or wonderful South Africa, Cambodia, Namibia or Uganda, city or wild places].
Dynamically developing view] of China, Kuwait, Qatar map and satellite photo] are available.
For travelers reliable and convenient search address and location] on a map of Nepal, Georgia, Italy, Egypt, Japan, New Zealand, Vatican, Vietnam scheme].
satellite] covers vast expanses on United States of America, Canada or Russia map on] all continents. Use this map right now.
Live Map of South Carolina
https://edpill.cheap/# buy erection pills
erectile dysfunction medicine india
newssahara.com
Drug information leaflet. Brand names.
eldepryl for sale
Some news about medicament. Read here.
Services on the Internet which are in demand every day! search on] map of Australia, India, Mexico, United States of America free opened on usa-map.online] web.
satellite] map of Algeria, Argentina, Netherlands, Liberia, Guyana or Haiti every city street] high accuracy level of technology. location on] Bolivia or Bulgaria, exotic Congo or Ecuador, cold Iceland, Indonesia map city or wild places].
Dynamically developing view] of map of United Arab Emirates, Oman, South Korea and satellite photo] 24/7 online.
For tourists reliable and convenient search address and location] of the desired object type on Austria, Bulgaria, Brazil, Greece, Maldives, Monaco or Turkey map scheme].
satellite] covers vast expanses on United States of America, Canada or Russia map on] every continent on earth. Try this wem map.
View Map of Alaska
olympic-school.com
%%
Have a look at my site … ремонт lenovo
Бесплатные промокоды Mostbet при регистрации 2024. Получить бонус на сумму 35000 рублей могут все новые участники клуба. Регистрируйте аккаунт по электронной почте или через привязку аккаунтов популярных социальных сетей и получайте бонусом до 35000 рублей на первый депозит. Для зачисления бонусов необходимо пополнить счет с банковской карты или электронного кошелька, не забыв при этом указать мостбет промокод при регистрации бонус на депозит QWERTY777. Для того чтобы бонус стал доступен к снятию необходимо выполнить простое условие. Выбирайте любое событие, на которое принимаются ставки с коэффициентом от 1.4 и выше.
%%
my blog post :: tusk casino
bonus 1xbet – Bonus d’inscription de 130 ?/$. Les codes bonus du bookmaker 1xBet sont faciles a trouver dans l’espace Internet public. Fondamentalement, ces offres sont publiees sur des sites partenaires et des ressources Internet thematiques qui mettent en evidence le travail du bureau 1xBet, ses avantages et ses fonctionnalites. Dans ces articles et materiels, des codes promotionnels sont inclus, juste a l’endroit ou il est decrit en detail l’avantage de s’inscrire sur le site de jeu via un code promotionnel. Habituellement, ces blocs, ou le code bonus est place directement, fonctionnent comme de la publicite, motivant les utilisateurs a copier le code et a proceder a l’enregistrement sur le portail du jeu.
indian pharmacy online indian pharmacy paypal buy prescription drugs from india
ed treatments that work immediately
non prescription erection pills
Получи права управлять автомобилем в лучшей автошколе!
Стань профессиональной карьере автолюбителя с нашей автошколой!
Пройди обучение в лучшей автошколе города!
Задай тон правильного вождения с нашей автошколой!
Стань безупречным навыкам вождения с нашей автошколой!
Начни уверенно водить автомобиль с нами в автошколе!
Стремись к независимости и свободы, получив права в автошколе!
Продемонстрируй мастерство вождения в нашей автошколе!
Обрети новые возможности, получив права в автошколе!
Приведи друзей и они заработают скидку на обучение в автошколе!
Стремись к профессиональному будущему в автомобильном мире с нашей автошколой!
Заводи и научись водить автомобиль вместе с нашей автошколой!
Развивай свои навыки вождения вместе с профессионалами нашей автошколы!
Запиши обучение в автошколе и получи бесплатный индивидуальный урок от наших инструкторов!
Стремись к надежности и безопасности на дороге вместе с нашей автошколой!
Прокачай свои навыки вождения вместе с профессионалами в нашей автошколе!
Учись дорожные правила и навыки вождения в нашей автошколе!
Стань настоящим мастером вождения с нашей автошколой!
Набери опыт вождения и получи права в нашей автошколе!
Пробей дорогу вместе с нами – пройди обучение в автошколе!
права водія ціна https://avtoshkolaznit.kiev.ua .
https://medicinefromindia.store/# reputable indian pharmacies
Компания diplom-sale.ru предлаагает купить диплом нового образца http://diplom-sale.ru/ со скидкой и гарантией возврата средств.
Получи права управлять автомобилем в лучшей автошколе!
Стань профессиональной карьере автолюбителя с нашей автошколой!
Пройди обучение в лучшей автошколе города!
Задай тон правильного вождения с нашей автошколой!
Стремись к безупречным навыкам вождения с нашей автошколой!
Научись уверенно водить автомобиль у нас в автошколе!
Достигай независимости и свободы, получив права в автошколе!
Прояви мастерство вождения в нашей автошколе!
Обрети новые возможности, получив права в автошколе!
Запиши друзей и они заработают скидку на обучение в автошколе!
Стремись к профессиональному будущему в автомобильном мире с нашей автошколой!
Учись и научись водить автомобиль вместе с нашей автошколой!
Развивай свои навыки вождения вместе с опытными инструкторами нашей автошколы!
Запиши обучение в автошколе и получи бесплатный консультационный урок от наших инструкторов!
Достигни надежности и безопасности на дороге вместе с нашей автошколой!
Улучши свои навыки вождения вместе с лучшими в нашей автошколе!
Учись дорожные правила и навыки вождения в нашей автошколе!
Стань настоящим мастером вождения с нашей автошколой!
Набери опыт вождения и получи права в нашей автошколе!
Покори дорогу вместе с нами – закажи обучение в автошколе!
автошкола київ http://avtoshkolaznit.kiev.ua/ .
erection pills that work pills erectile dysfunction cheapest ed pills
ed treatment drugs
Достигни права управлять автомобилем в лучшей автошколе!
Стань профессиональной карьере вождения с нашей автошколой!
Пройди обучение в лучшей автошколе города!
Учись правильного вождения с нашей автошколой!
Стремись к безупречным навыкам вождения с нашей автошколой!
Научись уверенно водить автомобиль у нас в автошколе!
Стремись к независимости и лицензии, получив права в автошколе!
Прояви мастерство вождения в нашей автошколе!
Обрети новые возможности, получив права в автошколе!
Приведи друзей и они получат скидку на обучение в автошколе!
Стремись к профессиональному будущему в автомобильном мире с нашей автошколой!
Учись и научись водить автомобиль вместе с нашей автошколой!
Развивай свои навыки вождения вместе с профессионалами нашей автошколы!
Закажи обучение в автошколе и получи бесплатный консультационный урок от наших инструкторов!
Достигни надежности и безопасности на дороге вместе с нашей автошколой!
Прокачай свои навыки вождения вместе с лучшими в нашей автошколе!
Учись дорожные правила и навыки вождения в нашей автошколе!
Стань настоящим мастером вождения с нашей автошколой!
Набери опыт вождения и получи права в нашей автошколе!
Покори дорогу вместе с нами – закажи обучение в автошколе!
автошкола васильківська https://avtoshkolaznit.kiev.ua/ .
She does not cower from any excellent porn scenes and this built her impress large porn organizations to sign her up even in her previous several years in the adult leisure business. The Secret Circle co-output with Outerbanks Entertainment, Alloy Entertainment and Warner Bros. Not only has she secured multiple porn movie discounts but is now at the extremely major of German pornstars. At the very least two of my superior friends satisfied by way of on the internet courting, and now have young children with each other. If it opens up your pool of possible mates, or just makes your social existence more thrilling, great for you. But I know how addictive social and activity applications can be, since I unconsciously open Facebook every time I choose up my cellphone, and I’ve deleted Candy Crush and Word Streak numerous instances only to desperately redownload them. Cohen, Philip. “1 Possible, Troubling Outcome of Online Dating: More Social Inequality.” Atlantic. Cohen, Philip N. “What ails Black women 3: Discrimination and repercussions.” Family Inequality. Bernstein, Joseph. “Women Are Using Tinder To Campaign For Bernie Sanders.” BuzzFeed News. Broadly Staff. “How One Matchmaker Changed Online Dating for Women Everywhere.” Broadly. I also reside on my mobile phone, so whilst I you should not partake of relationship applications, I can totally see why it would go mobile.
mostbet промокод com https://www.glory-gallery.ru/wp-includes/inc/promokod_mostbet__bonus_125__do_35000_rub_.html промокод mostbet
Разработка и производство промышленных автомобильных весов для взвешивания автотранспорта с грузом в статике и в движении любых автомобилей с грузом https://vc.ru/u/2909281-zavod-vesovogo-oborudovaniya/1024956-avtomobilnye-vesy
vocor.biz/content/1win-app.site/
Utilisation du code promo 1xbet canada lors de votre inscription, vous pouvez obtenir un bonus de bienvenue pour un nouveau client d’un montant allant jusqu’a 130?/$, ce qui vous donnera un bon depart dans vos paris sportifs en ligne. Grace a la publicite sur le portail de jeux 1xbet lui-meme et aux publications sur les ressources thematiques et partenaires, de nombreuses personnes connaissent le bonus d’inscription. A bien des egards, c’est grace a lui que le nombre de clients des bookmakers ne cesse de croitre. C’est grace a ce type de bonus que les joueurs disposent d’un montant substantiel qui peut etre depense en paris. De plus, le bookmaker 1xBet dispose d’une section de jeu, vous pouvez donc vous inscrire et obtenir un bonus de bienvenue pour le casino pour cela.
1win Регистрация на официальном сайте 1вин. Как зарегистрироваться в 1win БК 1win позаботился о создании удобного, функционального сайта для своих клиентов 1win зеркало сайта
Официальный сайт 1WIN казино позволяет игрокам запускать азартные игры, получать бонусы, участвовать в турнирах 1win рабочее зеркало
Официальный сайт 1WIN казино позволяет игрокам запускать азартные игры, получать бонусы, участвовать в турнирах 1win сайт
1win Регистрация на официальном сайте 1вин. Как зарегистрироваться в 1win БК 1win позаботился о создании удобного, функционального сайта для своих клиентов 1win вход
предметная съемка цена https://predmetnaya-fotosyomka-1.ru/
best non prescription ed treatment
maple leaf pharmacy in canada canada discount pharmacy canadian pharmacy king reviews
https://edwithoutdoctorprescription.pro/# prescription drugs without doctor approval
best male ed pills
Официальный сайт 1WIN казино позволяет игрокам запускать азартные игры, получать бонусы, участвовать в турнирах 1win рабочее зеркало
https://canadianinternationalpharmacy.pro/# pharmacy canadian superstore
Официальный сайт 1WIN казино позволяет игрокам запускать азартные игры, получать бонусы, участвовать в турнирах 1win официальный сайт вход
ed treatment in india
%%
Also visit my homepage – pixbet baixar app
seo аудит цена https://prodvizhenie-sajtov15.ru .
credito 400 euros
indianpharmacy com Online medicine home delivery cheapest online pharmacy india
кракен kraken kraken darknet top
Даркнет, является, тайную, сеть, в, интернете, доступ к которой, осуществляется, по средствам, уникальные, софт и, технические средства, обеспечивающие, скрытность пользовательские данных. Один из, этих, средств, представляется, The Onion Router, который обеспечивает, гарантирует, безопасное, подключение к интернету, к даркнету. С, его, сетевые пользователи, могут иметь возможность, анонимно, посещать, интернет-ресурсы, не видимые, стандартными, поисками, позволяя таким образом, среду, для организации, разнообразных, противоправных активностей.
Киберторговая площадка, соответственно, часто связывается с, темной стороной интернета, в качестве, торговая площадка, для торговли, криминалитетом. На этом ресурсе, есть возможность, приобрести, различные, непозволительные, вещи, начиная от, наркотиков и оружия, вплоть до, хакерскими услугами. Платформа, предоставляет, высокую степень, шифрования, и, защиты личной информации, что, создает, данную систему, привлекательной, для, стремится, избежать, негативных последствий, со стороны соответствующих законопослушных органов.
курсы по охране труда и технике безопасности
https://www.snabco.ru/fw/inc/promokod_mostbet__besplatno.html
Промокод МостБет – QWERTY777 предоставляет всем новым клиентам возможность получить эксклюзивный приветственный бонус 125% до 25 000 рублей. Бонусный код проверен и актуален на сегодня 2024. Просто копируйте промокод mostbet и получайте бонус за регистрацию.
Пользователь еще не определился в своем желании, где и как ему лучше сделать ставку на исход спортивного события, а ему уже предлагается использовать промокод Mostbet, перейти к регистрации в букмекерской конторе и получить взамен определенное преимущество.
Надо отдать должное, подобное предложение очень своевременное! Чаще всего именно так и происходит. Получив бонусный код, пользователь переходит к созданию аккаунта в конторе. Расчет делается на то, что использованный промокод Mostbet принесет игроку порцию каких-то бонусов и преференций.
Именно в этой и заключается основная функция промокодов. Именно для этой цели букмекер Mostbet выпускает бонусные коды, способствуя привлечению новых клиентов. С помощью подобных акций контора старается увеличить число своих поклонников. В свою очередь, пользователи через бонус коды получают дополнительные возможности в предстоящей игре.
Промокод – это универсальный инструмент бонусной политики, предоставляя обеим стороны, и букмекеру, и игрокам более широкие возможности для взаимовыгодного сотрудничества.
Беря во внимание постоянный интерес игроков к бонусам, предлагает разобраться в вопросах. Что дают промокоды Mostbet поклонникам ставок на спорт? Реально ли реализовать полученное преимущество и за счет чего бонусная программа букмекерской конторы Mostbet выглядит привлекательной?
Делать ставки на спорт в букмекерской конторе Mostbet можно не только рискуя собственными деньгами. Прекрасная возможность испытать собственную удачу и проверить насколько прогнозы на исходы спортивных событий могут быть успешными – игра за бонусы, предоставляемые букмекером. В этом случае не только риски сведены к минимуму. У игроков появляются дополнительные шансы на выигрыш.
Неважно! Получены ли бонусы за промокод Mostbet, или преимущество является результатом участия игрока в бонусной программе букмекера, любой из вариантов предполагает заключение пари на выгодных условиях.
code promo 1xbet casino pour 2024, seulement, il vous donne un bonus de bienvenue de 100% jusqu’a 130?/$. Il s’agit d’un bonus de depot d’inscription, et vous pouvez l’utiliser pour les paris sportifs et les sports. Le programme de bonus du bookmaker 1xbet couvre presque toutes les activites de jeu des clients. De plus, les offres en termes de bonus peuvent concerner aussi bien les debutants que les joueurs experimentes, offrant des preferences et des avantages supplementaires a differentes etapes du jeu.
how to get a prescription for ed
https://www.sisidunia.com/12/the-most-expensive-csgo-skins-a-glimpse-into-the-high-stakes-world-of-virtual-collectibles/
Essential Medications for a Healthy Lifestyle. tadalafil mylan 10 mg
https://medicinefromindia.store/# top 10 pharmacies in india
%%
Visit my site :: http://www.ticket2ride.ru/2014/10/blog-post.html
natural ed medications
mexican drugstore online mexican border pharmacies shipping to usa mexican mail order pharmacies
https://medicinefromindia.store/# indian pharmacy
Gama Casino онлайн казино предлагает играть на реальные деньги с быстрыми выплатами казино гама зеркало
10yenharwichport.com
능력있으면 궁에 오지마, 다밍아, 다른 클랜은 없니?
Gama Casino онлайн казино предлагает играть на реальные деньги с быстрыми выплатами Гама казино
I’m extremely pleased to discover this website. I wanted to thank you for ones time just for this fantastic read!
My website: лизание жопы
ed drugs generic
%%
Рекомендую официальный телеграм канал 1Win зеркало
how to get prescribed ed meds
https://araks-group.ru/monro-kazino-2/
cheapest online pharmacy india Online medicine home delivery online shopping pharmacy india
buying ed pills online
online ed drugs
http://medicinefromindia.store/# Online medicine home delivery
best online ed prescriptions
п»їbest mexican online pharmacies mexican pharmaceuticals online mexican drugstore online
1xbet multicode aujourd’hui – Bonus VIP jusqu’a 130 ?/$ Offer Offre de bienvenue. 18 Les conditions generales s’appliquent. Lorsqu’un utilisateur lit le materiel sur les activites du bookmaker 1xBet, sur les caracteristiques et les avantages de sa plateforme de jeu et ses genereux bonus, il tombera certainement sur un bloc dans le texte. Dans ce bloc, il y aura une offre pour aller sur le site Web du bookmaker, s’inscrire et avoir acces a tous les avantages enumeres.
generic ed drugs india
what is the safest erectile dysfunction drug
bwin ile spor bahislerinde şansınızı deneyin
http://canadianinternationalpharmacy.pro/# canadian pharmacy near me
zetia 5mg
ed treatment in india
buy medicines online in india top 10 pharmacies in india Online medicine order
Официальный сайт 1WIN казино позволяет игрокам запускать азартные игры, получать бонусы, участвовать в турнирах 1Win казино
http://edpill.cheap/# ed drugs list
Официальный сайт 1WIN казино позволяет игрокам запускать азартные игры, получать бонусы, участвовать в турнирах 1Вин зеркало
Что такое Гама Казино. Gama Casino – это онлайн казино, основанное в 2020 году, которое предлагает игрокам возможность играть в самые популярные игры от ведущих разработчиков Gama casino
safe medicine for erectile dysfunction
Что такое Гама Казино. Gama Casino – это онлайн казино, основанное в 2020 году, которое предлагает игрокам возможность играть в самые популярные игры от ведущих разработчиков Гама зеркало
Government Printing Office. Archived from the first on 19 August 2020. Retrieved 27 February 2020.. The textual content of the House and Senate resolutions have been subsequently set into the next legislation: H.R. Panayotakis, Costas (June 1, 2020). “Neoliberalism, the Left and the Rise of the Far Right: On the Political and Ideological Implications of Capitalism’s Subordination of Democracy”. Rafi, Yumna (17 June 2015). “Pakistan hosts second largest refugee inhabitants globally”. Nygren, Thomas (2016), “UNESCO Teaches History: Implementing International Understanding in Sweden”, A History of UNESCO, London: Palgrave Macmillan Uk, pp. Korfhage, Matthew (January 26, 2016). “Everything You Need to Know About the Portland Shoe Industry”. Hansard, 26 January 1949) Archived 19 October 2017 at the Wayback Machine. Archived from the authentic on 12 September 2018. Retrieved 5 April 2019. (English summary Archived 22 March 2019 at the Wayback Machine). Grandjean, Martin (2018). Les réseaux de la coopération intellectuelle. An professional cited by UNESCO as attributing the ten billion determine denied it and explained he had “no notion” exactly where the determine arrived from. In October 2016, Japanese Foreign Minister Fumio Kishida confirmed that Japan’s 2016 yearly funding of ¥4.4 billion experienced been suspended, even though he denied any immediate connection with the Nanjing doc controversy.
I’ll right away take hold of your rss as I can not find your email subscription link
or newsletter service. Do you have any? Kindly permit me understand
in order that I may just subscribe. Thanks.
ed drugs list
Наслаждайтесь азартными играми в Cat Casino и не пропустите новинки. Честные игры залог твоего успеха. Удача на твоей стороне в Супер Турнирах кэт казино
http://credforum.ru/showthread.php?p=61369#post61369
Наслаждайтесь азартными играми в Cat Casino и не пропустите новинки. Честные игры залог твоего успеха. Удача на твоей стороне в Супер Турнирах кэт казино
mexico drug stores pharmacies mexico pharmacies prescription drugs buying prescription drugs in mexico
non prescription erection pills
ed drugs online canada
http://medicinefromindia.store/# mail order pharmacy india
The album’s nearly 1.1 million unit debut profits was the highest initial-7 days figures at any time scanned by a male R&B artist and the seventh finest of the Nielsen SoundScan background. The conceptual artist Jenny Ringley is viewed as the 1st camgirl. Training and perseverance will get them only so far, and when this crew sets out on humanity’s initially expedition to yet another entire world, very little can get ready them for the unpredicted danger and staggering surprise of what they will experience. The appropriate answer is revealed On July 1, Scene Co. borrowed $15,000 money from First Bank by signing a 30-day, 5% curiosity-bearing note. Test Bank for Prelude to Programming Chapter 3 Multiple Choice 1. Which of the subsequent is not a type of choice structure? Class: Date: Cold War Practice Multiple Choice Identify the alternative that finest completes the statement or answers the problem. EmSAT English HCT Preparation Course Practice Material EmSAT Preparation Course Practice Material P a g e one Table of Contents EmSAT English check info and case in point inquiries EmSAT English Test Information. Practical English Course нига для викладача Leonid Chernovaty Vyacheslav Karaban, Eds DICTUM FACTUM ДО 200-РІЧЧЯ ХЛРЮВСЬКОГО НАЩ ОНАЛЬНОГО УНІВЕРСИТЕТУ ІМ.
Les codes promo en vigueur pour 1xBet ? Offre 2024 ? Codes bonus ? Bonus de pari gratuit ? Bonus d’inscription ? Programme de fidelite !
https://popvalais.ch/wp-includes/inc/?code-promo-1xbet-burkina-faso-78-000xof.html
Le Code Promo 1xBet 2024 Utilisez le code lors de votre inscription pour beneficier d’un bonus de 130€/$. Le bonus de bienvenue de 100% pour les paris sportifs et le casino vous offre la possibilite d’utiliser de l’argent gratuit sur 1xbet. Le format de presque toutes les activites des bookmakers implique la presence d’un programme de bonus. Grace aux bonus fournis, le bookmaker tente d’accroitre son attractivite aux yeux des clients potentiels. Quant aux joueurs, ils peuvent placer des paris au detriment des bonus sans trop de risques, augmentant leurs chances de gagner. Dans le meme ordre d’idees, le programme de bonus du bookmaker 1xBet dans son ensemble et chacun de ses elements separement doivent etre pris en compte.
http://compcar.ru/forum/member.php?u=105568
вызвать сантехника краснодар https://keramogranit-krasnodar.ru/
mens erection pills
%%
Also visit my web blog: https://vegomassan.org/
https://canadianinternationalpharmacy.pro/# best rated canadian pharmacy
best medicine for erectile dysfunction without side effects
LГҐn 60000
what is the safest erectile dysfunction drug
https://www.magcloud.com/user/arytemvvasil
https://zeenews.india.com/india/boosting-views-on-youtube-how-to-use-it-as-a-strategy-to-increase-popularity-2718756.html
viagra without a doctor prescription generic cialis without a doctor prescription ed meds online without doctor prescription
Ed Drugs from India
Казино 1Вин удобен для игроков, работает на ПК и телефоне. Для мобильников создана mobile version и приложение для iphone и android 1win
Казино 1Вин удобен для игроков, работает на ПК и телефоне. Для мобильников создана mobile version и приложение для iphone и android 1win casino
All information on the site – 1xslots promo codes
claritin 25mg
generic ed drugs cost
Respect to post author, some fantastic information
My website: porno anal
%%
My homepage :: https://ua.sexchat.moscow
https://canadianinternationalpharmacy.pro/# rate canadian pharmacies
На сайте Ramenbet казино вы найдете все необходимое для комфортной игры: зеркало, мобильная версия, лицензию, удобный процесс регистрации и широкую бонусную политику ramenbet зеркало
http://medicinefromindia.store/# india pharmacy
На сайте Ramenbet казино вы найдете все необходимое для комфортной игры: зеркало, мобильная версия, лицензию, удобный процесс регистрации и широкую бонусную политику раменбет казино
Пo paзpaбoткaм Института Лингвистико — Волновой генетики П. П. Гаряева — было создано направление в квантово-информационной медицине https://bioquant-garyaev.com/product/biomatricza-garyaeva-kik-3/
Пo paзpaбoткaм Института Лингвистико — Волновой генетики П. П. Гаряева — было создано направление в квантово-информационной медицине https://bioquant-garyaev.com/product/modulyator-garyaeva-mishina/
best non prescription ed treatment
https://canadianinternationalpharmacy.pro/# the canadian pharmacy
buying ed pills online ed meds online best male ed pills
erectile dysfunction pills from india
Недвижимость в залоге? Выкупим вашу недвижимость из-под залога у частного лица или микрофинансовой организации.
выкуп квартир симфония
Generic Ed Drugs Fda Approved
Промокод 1xBet при регистрации – это 1XFREE777. Только с помощью него вы получите бонус в размере 100% до 32500 рублей. https://fotozayka.ru/wp-content/pages/promokod_240.html
Все остальные коды не действительны и не предоставляют такого бонуса. Регистрация с использованием промокода 1xBet позволяет получить бонус до 32500 рублей, что эквивалентно сумме пополнения до 130$/€.
canadian 24 hour pharmacy canada drugstore pharmacy rx canadianpharmacyworld
ed treatment in india
http://medicinefromindia.store/# reputable indian online pharmacy
Рекомендую надежній телеграм канал где можно найти 1Win вход
Получи права управления автомобилем в первоклассной автошколе!
Стань профессиональной карьере вождения с нашей автошколой!
Успей пройти обучение в лучшей автошколе города!
Задай тон правильного вождения с нашей автошколой!
Стремись к безупречным навыкам вождения с нашей автошколой!
Научись уверенно водить автомобиль с нами в автошколе!
Достигай независимости и свободы, получив права в автошколе!
Прояви мастерство вождения в нашей автошколе!
Обрети новые возможности, получив права в автошколе!
Запиши друзей и они заработают скидку на обучение в автошколе!
Стань профессиональному будущему в автомобильном мире с нашей автошколой!
Учись и научись водить автомобиль вместе с нашей автошколой!
Развивай свои навыки вождения вместе с профессионалами нашей автошколы!
Запиши обучение в автошколе и получи бесплатный индивидуальный урок от наших инструкторов!
Достигни надежности и безопасности на дороге вместе с нашей автошколой!
Прокачай свои навыки вождения вместе с профессионалами в нашей автошколе!
Завоевывай дорожные правила и навыки вождения в нашей автошколе!
Стань настоящим мастером вождения с нашей автошколой!
Накопи опыт вождения и получи права в нашей автошколе!
Пробей дорогу вместе с нами – закажи обучение в автошколе!
водійське посвідчення http://www.avtoshkolaznit.kiev.ua .
non prescription erection pills
качество фу
An early example of the latter type was Gibson’s Girl, an http://pko.fik.um.ac.id/2020/08/15/jadwal-kegiatan-akademik-semester-gasal-2020-2021/image of a New Woman painted by Charles Dana Gibson.
http://edpill.cheap/# ed pills that work
best ed drugs
%%
my site … https://medapparatura.com.ua/catalog/dezinfektsiya-ta-sterilizatsiya/
canadian drug pharmacy canadian valley pharmacy canada pharmacy world
Watches World
%%
My web blog; https://xbetfr.com
http://edpill.cheap/# ed medications
online prescription for ed meds cheap cialis viagra without doctor prescription
Аренда фотостудии: Идеальное место для создания качественных фотографий – просторная и уютная фотостудия с профессиональным оборудованием и удобным расположением фото на документы
http://medicinefromindia.store/# indian pharmacy online
Hipotekines paskolos isduodamos turintiems bloga kredito istorija! Skubios paskolos verslui paskola verslui
ed dysfunction treatment
Промокод 1xBet при регистрации – это 1XFREE777. Только с помощью него вы получите бонус в размере 100% до 32500 рублей. http://tdrimspb.ru/news/inc/1hbet_promokod_pri_registracii__bonus_do_32500_rub_.html
Все остальные коды не действительны и не предоставляют такого бонуса. Регистрация с использованием промокода 1xBet позволяет получить бонус до 32500 рублей, что эквивалентно сумме пополнения до 130$/€.
Experience luxury living at Fairmont Marina Residences Abu Dhabi . Don’t miss the best deals from Fairmont Hotels & Resorts starting at AED 2,000,000 (USD 544,500). Indulge in elegance and opulence like never before.
top ed pills
real viagra without a doctor prescription usa generic cialis without a doctor prescription п»їprescription drugs
https://noginsk.build2.ru/post.php?fid=21
most potent ed pills
фильм в хорошем качестве
фильм 2024
Find your dream home in Rixos Dubai Island! Explore our selection of exquisite apartments, villas, duplexes, and beachfront houses for sale. Nakheel, the renowned developer, presents luxury properties at unbeatable prices. Start your exclusive Dubai lifestyle today.
фильм 2024
most effective ed pill
смотреть
newssugar.com
http://www.nemoskvichi.ru/forum/viewtopic.php?f=31&t=144826
generic ed drugs cost
1xBet промокод — 1XFREE777 впишите код в анкете при регистрации, пополните счет от 100 рублей и вы получите бонус +100% (до 32500 рублей). Промокод 1xBet на 2024 год предоставляет возможность получить бонусы при регистрации на сайте букмекерской конторы.
http://tdrimspb.ru/news/inc/1hbet_promokod_pri_registracii__bonus_do_32500_rub_.html
Read More About Mpesa Casinos In Kenya
mexican drugstore online mexican border pharmacies shipping to usa mexico pharmacies prescription drugs
mexican pharmacy purple pharmacy mexico price list mexican pharmacy
The latest news and reviews in the world of tech, automotive, gaming, science, and entertainment. https://millionbyte.us/
КОРОЧЕ, ВСЁ ПОНЯТНО
https://iiscecchi.edu.it/ripresa-di-settembre/
prochlorperazine otc
drugs to treat ed
У вас коммунальные долги? Выкупаем жилье с любыми долгами по электроэнергии и коммунальными платежами.
продать квартиру быстро нумикс
medicine in mexico pharmacies best online pharmacies in mexico buying prescription drugs in mexico
supesolar.com
generic ed pills from india
частный сео специалист http://www.prodvizhenie-sajtov15.ru/ .
medicine in mexico pharmacies medication from mexico pharmacy mexico pharmacies prescription drugs
http://gamesmaker.ru/forum/common/offtopics/#replyform
сантехник на дом недорого https://keramogranit-krasnodar.ru/
online ed drugs for purchase
As a end result of the quantity of time adolescents invest employing these units, their total media exposure is significant. In most democratic nations, a citizen is eligible to vote at age 18. In a minority of nations around the world, the voting age is as small as 16 (for example, Brazil), and at just one time was as high as 25 in Uzbekistan. Difficult one particular as the rx is much better at the large stop been f1.8 but the Olympus at 90mm f4 vs a hundred f4.9 presents the Olympus the edge . More greatly, cigarette using tobacco has develop into a much a lot less commonplace exercise amid American center- and large-university pupils in fact, a increased range of teens now smoke marijuana than smoke cigarettes, with one particular latest research demonstrating a respective 23.8% as opposed to 43.6% of surveyed higher college seniors. Below we have a desk with some of the other broadly acknowledged new authentic life webcam websites the issue with people is the good quality is very low and the costs high. In youngsters, human body dissatisfaction is normally affiliated with body mass, small self-esteem, and atypical feeding on designs that can final result in overall health methods. Scholars carry on to discussion the results of media on body dissatisfaction in teenagers.
ed drugs india
medication from mexico pharmacy medication from mexico pharmacy mexican rx online
A round of applause for your article. Much thanks again.
My website: секс с толстожопой
newsprofit.info
new ed drugs
%%
My homepage; mycelium-wallet.com
pronovosti.org
mexico pharmacy mexican pharmacy buying prescription drugs in mexico
strongest ed medication
reputable mexican pharmacies online mexico pharmacy best online pharmacies in mexico
medication from mexico pharmacy medicine in mexico pharmacies reputable mexican pharmacies online
ed drug prices
mexico drug stores pharmacies mexican border pharmacies shipping to usa buying prescription drugs in mexico
mexican pharmacy mexico drug stores pharmacies mexico pharmacies prescription drugs
buying ed pills online
праздничные рецепты https://kulnr.ru/
buying ed drugs online
mexico pharmacies prescription drugs mexican mail order pharmacies buying prescription drugs in mexico online
ed pills online india
In ebook 3, Grave Peril, Harry feels responsible for using the Nightmare down, and guilty for whatsoever other attacks it commits, just since it truly is his electricity the creature is applying for these attacks, irrespective of the actuality that it took that power by drive and in a environment in which Harry experienced definitely no handle: a dream. The truth that no a single except Thea, who she barely noticed, bothered to get in touch with her out on her decisions just built the complicated worse, and led to her deteriorating well being. He blames himself for Cedric’s dying since it was his strategy for them equally to get the portkey that led them to Voldemort at the exact same time, even if neither could have known that item was a portkey. Trump’s presidential conspiracies may perhaps have commenced in the course of the 2016 election campaign, when he allegedly instructed Michael Cohen, his former legal professional and personalized fixer, to fork out hush cash to two girls-pornstar Stormy Daniels and previous Playboy product Karen McDougal-with whom he had extramarital affairs. At different points in the later guides, she claims to have gotten around it, but by the Protector of the Small quartet, she feels responsible yet again when Tortall is back in a whole-scale war.
best ed non prescription pill
Csatlakozz a Mostbet-hez es erezd a sportfogadas es online kaszino izgalmas vilagat https://mylesungw99876.bloggazza.com/24905057/the-rise-of-online-sports-betting-a-comprehensive-guide
Необходимо купить диплом университета России? В компании diplom-sale.ru возможно купить нужный документ http://diplom-sale.ru/ без предоплаты. Выбор государственных и частных университетов!
п»їbest mexican online pharmacies medication from mexico pharmacy mexican pharmaceuticals online
mexico drug stores pharmacies pharmacies in mexico that ship to usa mexican pharmaceuticals online
ed pills near me
Find your dream home in Bloom Living. Choose from a wide range of exquisite studios and apartments in Zayed City, Abu Dhabi. Experience the luxury of Bloom Holding’s premium real estate offerings at unbeatable prices. Don’t miss out on this golden opportunity!
lavrus.org
%%
Also visit my webpage backpack-wallet.io
tzona.org
pharmacies in mexico that ship to usa medicine in mexico pharmacies pharmacies in mexico that ship to usa
legit erectile dysfunction pills
indian medicine for erectile dysfunction
%%
my web-site sallijames433gmailcom-HNmRABzZkQA.html
Hier
credit 15000 euros
mexican rx online mexican border pharmacies shipping to usa medicine in mexico pharmacies
mens erection pills
Вы абсолютно правы. В этом что-то есть и идея отличная, согласен с Вами.
тут же мы осуществим тестирование и профилактическую чистку ноутбука от грязи, https://simoncookagencies.co.uk/conran-shop-celebrates-zanotta-post/ которая продлит ему жизнь.
erectile dysfunction drugs
219news.com
mexico pharmacies prescription drugs purple pharmacy mexico price list medicine in mexico pharmacies
Watches World
Client Comments Reveal Timepieces Universe Experience
At Our Watch Boutique, client fulfillment isn’t just a aim; it’s a glowing evidence to our commitment to perfection. Let’s plunge into what our respected clients have to say about their experiences, illuminating on the faultless support and remarkable chronometers we present.
O.M.’s Trustpilot Review: A Seamless Adventure
“Very great contact and follow-up throughout the procession. The watch was impeccably packed and in perfect. I would definitely work with this team again for a watch buying.
O.M.’s statement exemplifies our loyalty to interaction and precise care in delivering timepieces in impeccable condition. The confidence forged with O.M. is a foundation of our customer bonds.
Richard Houtman’s Insightful Testimonial: A Private Contact
“I dealt with Benny, who was very beneficial and polite at all times, keeping me regularly notified of the procedure. Progressing, even though I ended up sourcing the timepiece locally, I would still absolutely recommend Benny and the firm moving forward.
Richard Houtman’s encounter highlights our customized approach. Benny’s help and ongoing comms showcase our dedication to ensuring every client feels valued and apprised.
Customer’s Streamlined Service Testimonial: A Effortless Transaction
“A very effective and efficient service. Kept me up to date on the order advancement.
Our devotion to streamlining is echoed in this buyer’s feedback. Keeping customers updated and the smooth progression of orders are integral to the WatchesWorld journey.
Discover Our Newest Collections
Audemars Piguet Selfwinding Royal Oak 37mm
A gorgeous piece at €45,900, this 2022 release (REF: 15551ST.ZZ.1356ST.05) invites you to add it to your basket and elevate your collection.
Hublot Classic Fusion Green Titanium Chronograph 45mm
Priced at €8,590 in 2024 (REF: 521.NX.8970.RX), this Hublot creation is a fusion of styling and invention, awaiting your request.
%%
africanownews.com
best medicine for erectile dysfunction without side effects
Виртуальные серверы в аренду с почасовым биллингом по всему миру виртуальные серверы
Виртуальные серверы в аренду с почасовым биллингом по всему миру виртуальные серверы
new ed drugs
г‚‚гЃЈгЃЁ
Lainaa 5000 euroa
ed drugs generic
mexican pharmacy medicine in mexico pharmacies buying from online mexican pharmacy
%%
Also visit my page http://downtown99.com/2024/01/31/participants-membership-prohibited-and-you-can-winnings-confiscated/
reputable mexican pharmacies online pharmacies in mexico that ship to usa mexico pharmacies prescription drugs
%%
Also visit my webpage … https://www.tce.co.in/pokies84-uncovered-a-deep-dive-into-the-pokies/
Obten descuentos adicionales con un codigo descuento 1Win
Los codigos promocionales de 1Win son canjeados desde su registro y utilizados en los juegos. Aplica el codigo 937999 y recibe ganancias al apostar. El codigo de promocion 2024 te regala un paquete de bienvenida del 500% con los cuatro primeros depositos hasta $700 en apuestas deportivas y casino. El codigo 1win de bono debe ser ingresado en el formulario de registro.
Si esta buscando una forma de maximizar sus ganancias en apuestas deportivas, no se pierda el codigo de promocion y el bono de bienvenida 1Win en 024]. Con el codigo de promocion 1Win puedes recibir ofertas exclusivas y apuestas gratis para disfrutar aun mas de tus juegos favoritos. Ademas, el bono de bienvenida 1Win es una gran oportunidad para aumentar sus ganancias y tener una experiencia de apuestas aun mas emocionante.
%%
my webpage; https://dienlanhvinhphat.com/khong-phan-loai/lalabet-gambling-establishment-comment-2024-enjoy-thousands-of-online-game/
Недвижимость арестована?
Судебные приставы арестовали недвижимость? мы снимем обременения и заплатим ваши долги
срочный выкуп квартир
кулинарные рецепты https://kulnr.ru/
Зухвала енергія пін ап
слоти онлайн https://www.pinupcasinoqgcvbisd.kiev.ua/ .
mexican pharmacy reputable mexican pharmacies online purple pharmacy mexico price list
buying prescription drugs in mexico mexico drug stores pharmacies mexico pharmacy
pret 17000 euros
buying prescription drugs in mexico online mexico pharmacy mexico drug stores pharmacies
заказать голосовые поздравления с днем рождения по имени https://na-telefon.biz/
buying prescription drugs in mexico mexican drugstore online mexico pharmacy
купить диплом университета http://prema-diploms.com/ .
jaycitynews.com
360o.info
best non prescription erection pills
She inevitably returns his emotions, but the romance is compelled to stop prematurely when Charlotte, having purchased back again her previous business enterprise from her ex-spouse, moves back again to Chicago. She pays Niles back by refusing to grant an quick divorce in its place, she forces Niles to engage in alongside that the two keep on being happily married, assuring him that right after he has done this on many find social instances she will file for divorce. Rita Wilson would engage in a center-aged edition of Hester in the two-aspect episode “Don Juan in Hell”, employing prosthetic make-up. Poverty and a lack of education and learning play significant roles in the life of several girls in the sexual intercourse business. Her assert that adult men can not be women (and other statements) do not have all five. Source below. Pornography for gals: a new subgenre focusing on women of all ages, portraying “eromen” (erotic gentlemen) who cater to women’s demands. Charlotte information her job path with Marcus who reveals: ‘I normally don’t forget unforgettable people’. Charlotte (Laura Linney), the founder-owner of Charlotte’s Web relationship support, is a matchmaker just lately arrived from Chicago and Frasier’s closing really like interest on the series.
buying prescription drugs in mexico online buying prescription drugs in mexico online mexican drugstore online
Generic Ed Drugs Fda Approved
buying from online mexican pharmacy buying prescription drugs in mexico online pharmacies in mexico that ship to usa
Sildenafil 75mg
Discover the epitome of luxury living amidst the breathtaking Palm Jumeirah with our exquisite villas One Crescent Dubai. Immerse yourself in opulence and sophistication while enjoying unbeatable prices. Don’t miss the chance to call this luxurious haven your home.
Мониторинг обменников, который предоставляет самую свежую информацию о курсах многих ведущих ручных и автоматических обменных пунктов криптовалют Купить криптовалюту
Мониторинг обменников, который предоставляет самую свежую информацию о курсах многих ведущих ручных и автоматических обменных пунктов криптовалют Мониторинг обменников
buying prescription drugs in mexico mexican online pharmacies prescription drugs purple pharmacy mexico price list
%%
%%
Here is my webpage: https://adepoldobrasil.org.br/relatorio-apresentado-pelo-deputado-arthur-oliveira-maia/
cost for viagra
pret 18000 euros
365eventcyprus.com
Сделайте ремонт быстро и качественно с ремонтной смесью
цена смеси https://www.remontnaja-smes-dlja-kirpichnoj-kladki.ru/ .
women18.com
viagra super active
mexico drug stores pharmacies medication from mexico pharmacy purple pharmacy mexico price list
best mexican online pharmacies buying from online mexican pharmacy best mexican online pharmacies
играть в казино на рубли
Рулонный газон: сравнение различных видов
купить рулонный газон цена https://rulonnyj-gazon77.ru/ .
can you buy viagra online
1xBet промокод — 1XFREE777 впишите код в анкете при регистрации, пополните счет от 100 рублей и вы получите бонус +100% (до 32500 рублей).
https://blorey.com/include/articles/1xbet-promo-code.html
Промокод 1xBet на 2024 год предоставляет возможность получить бонусы при регистрации на сайте букмекерской конторы.
buying from online mexican pharmacy mexican online pharmacies prescription drugs buying prescription drugs in mexico online
Универсальность ремонтной смеси
купить цемент https://remontnaja-smes-dlja-kirpichnoj-kladki.ru .
særlig info
мосты для tor browser список
Защита в сети: Перечень подходов для Tor Browser
В настоящий период, когда темы конфиденциальности и безопасности в сети становятся все более существенными, многочисленные пользователи обращают внимание на инструменты, позволяющие обеспечивать неузнаваемость и безопасность личной информации. Один из таких инструментов – Tor Browser, разработанный на системе Tor. Однако даже при использовании Tor Browser есть вероятность столкнуться с блокировкой или преградой со стороны Интернет-поставщиков или цензурных органов.
Для устранения этих ограничений были созданы переходы для Tor Browser. Мосты – это особые серверы, которые могут быть использованы для перехода блокировок и гарантирования доступа к сети Tor. В представленном тексте мы рассмотрим перечень переходов, которые можно использовать с Tor Browser для обеспечивания достоверной и безопасной невидимости в интернете.
meek-azure: Этот переход использует облачное обеспечение Azure для того, чтобы переодеть тот факт, что вы используете Tor. Это может быть важно в странах, где поставщики услуг блокируют доступ к серверам Tor.
obfs4: Переход обфускации, предоставляющий механизмы для сокрытия трафика Tor. Этот подход может успешно обходить блокировки и фильтрацию, делая ваш трафик неотличимым для сторонних.
fte: Подход, использующий Free Talk Encrypt (FTE) для обфускации трафика. FTE позволяет изменять трафик так, чтобы он представлял собой обычным сетевым трафиком, что делает его затрудненным для выявления.
snowflake: Этот переход позволяет вам использовать браузеры, которые работают с расширение Snowflake, чтобы помочь другим пользователям Tor пройти через запреты.
fte-ipv6: Вариант FTE с работающий с IPv6, который может быть востребован, если ваш провайдер интернета предоставляет IPv6-подключение.
Чтобы использовать эти переходы с Tor Browser, откройте его настройки, перейдите в раздел “Проброс мостов” и введите названия подходов, которые вы хотите использовать.
Не забывайте, что эффективность мостов может изменяться в зависимости от страны и поставщиков Интернета. Также рекомендуется периодически обновлять перечень подходов, чтобы быть уверенным в производительности обхода блокировок. Помните о важности безопасности в интернете и производите защитные действия для обеспечения безопасности своей личной информации.
Я присоединяюсь ко всему выше сказанному. Можем пообщаться на эту тему. Здесь или в PM.
Here are four popular questions, which you have the opportunity find in the album “Theme ps4 – in the category “Advanced http://www.sweetclaudesicecream.com/2019/10/24/hello-world/ filters” on proposed tab.
Містерія пін ап
online casino ukraine https://pinupcasinoqgcvbisd.kiev.ua .
buy viagra in mexico
purple pharmacy mexico price list mexican drugstore online mexico pharmacies prescription drugs
Всё о ремонте смеси в одном месте
цемент цена https://remontnaja-smes-dlja-kirpichnoj-kladki.ru/ .
thecolumbianews.net
365newss.net
modernkarachi.com
Xie Qian의 말에 감염된 듯 많은 사람들이 고개를 숙이고 눈물을 닦기 시작했습니다.
В века технологий, в момент, когда цифровые границы объединяются с реальностью, нельзя игнорировать наличие угроз в даркнете. Одним из рисков является blacksprut – понятие, приобретший символом нелегальной, вредоносной деятельности в подпольных уголках интернета.
Blacksprut, будучи частью подпольной сети, представляет существенную угрозу для безопасности в сети и личной устойчивости пользователей. Этот темный уголок сети зачастую ассоциируется с нелегальными сделками, торговлей запрещенными товарами и услугами, а также иной противозаконными деяниями.
В борьбе с угрозой blacksprut необходимо приложить усилия на разнообразных фронтах. Одним из ключевых направлений является совершенствование технологий кибербезопасности. Развитие мощных алгоритмов и технологий анализа данных позволит отслеживать и пресекать деятельность blacksprut в реальной жизни.
Помимо цифровых мер, важна согласованность усилий правоохранительных органов на планетарном уровне. Международное сотрудничество в сфере кибербезопасности необходимо для успешного противодействия угрозам, связанным с blacksprut. Обмен информацией, создание совместных стратегий и реактивные действия помогут уменьшить воздействие этой угрозы.
Образование и просвещение также играют важную роль в борьбе с blacksprut. Повышение сознания пользователей о рисках подпольной сети и методах защиты становится неотъемлемой частью антиспампинговых мероприятий. Чем более осведомленными будут пользователи, тем меньше опасность попадания под влияние угрозы blacksprut.
В заключение, в борьбе с угрозой blacksprut необходимо совместить усилия как на цифровом, так и на нормативном уровнях. Это трудная задача, требующий совместных усилий коллектива, служб безопасности и IT-компаний. Только совместными усилиями мы добьемся создания безопасного и надежного цифрового пространства для всех.
Торовский клиент является сильным инструментом для обеспечения невидимости и секретности в интернете. Однако, иногда люди могут пережить с затруднениями соединения. В настоящей публикации мы изучим вероятные предпосылки и представим варианты решения для исправления проблем с подключением к Tor Browser.
Проблемы с интернетом:
Решение: Проверка соединения ваше интернет-подключение. Проверьте, что вы соединены к интернету, и нет ли затруднений с вашим Интернет-поставщиком.
Блокировка Тор сети:
Решение: В некоторых частных странах или сетях Tor может быть заблокирован. Испытайте воспользоваться проходы для пересечения запрещений. В установках Tor Browser выберите опцию “Проброс мостов” и следуйте инструкциям.
Прокси-серверы и файерволы:
Решение: Проверьте настройки прокси-сервера и брандмауэра. Убедитесь, что они не препятствуют доступ Tor Browser к сети. Внесите изменения настройки или в течение некоторого времени отключите прокси и файерволы для оценки.
Проблемы с самим веб-обозревателем:
Решение: Убедитесь, что у вас установлена последнее обновление Tor Browser. Иногда изменения могут распутать недоразумения с подключением. Также пробуйте пересобрать обозреватель.
Временные перебои в Тор сети:
Решение: Выждите некоторое время и старайтесь войти позже. Временные сбои в работе Tor могут вызываться, и эти явления как правило преодолеваются в минимальные периоды времени.
Отключение JavaScript:
Решение: Некоторые сайты могут блокировать доступ через Tor, если в вашем приложении включен JavaScript. Попытайтесь временно деактивировать JavaScript в настройках браузера.
Проблемы с антивирусным программным обеспечением:
Решение: Ваш программа защиты или стена может блокировать Tor Browser. Убедитесь, что у вас не установлено запретов для Tor в настройках вашего антивирусного программного обеспечения.
Исчерпание памяти устройства:
Решение: Если у вас действующе много веб-страниц или процессы работы, это может призвести к израсходованию памяти устройства и затруднениям с доступом. Закройте дополнительные вкладки или перезапустите браузер.
В случае, если сложность с подключением к Tor Browser остается в силе, заходите за поддержкой на официальном сообществе Tor. Профессионалы смогут подсказать дополнительную помощь и последовательность действий. Помните, что секретность и конфиденциальность зависят от постоянного интереса к деталям, поэтому следите за обновлениями и поддерживайте инструкциям сообщества.
sildenafil no prescription
Универсальность ремонтной смеси
ремонтные смеси http://www.remontnaja-smes-dlja-kirpichnoj-kladki.ru/ .
reputable mexican pharmacies online mexico drug stores pharmacies mexican rx online
Obten descuentos adicionales con un codigo descuento 1Win
1win es una plataforma de apuestas en linea que ofrece una amplia variedad de opciones de apuestas deportivas y juegos de casino. La pagina web es facil de navegar y tiene un diseno moderno y atractivo. En cuanto a las apuestas deportivas, 1win ofrece una amplia variedad de deportes para apostar, desde los mas populares como el futbol y el baloncesto hasta deportes menos conocidos como el badminton y el rugby. Ademas, la plataforma ofrece una gran cantidad de mercados de apuestas para cada evento deportivo, lo que permite a los usuarios personalizar sus apuestas de acuerdo a sus preferencias. En cuanto a los juegos de casino, 1win ofrece una amplia variedad de opciones, desde tragamonedas hasta juegos de mesa como el blackjack y la ruleta. Los juegos son de alta calidad y estan disenados por algunos de los principales proveedores de software de casino. La plataforma tambien ofrece una amplia variedad de metodos de pago, incluyendo tarjetas de credito, billeteras electronicas y criptomonedas. Ademas, el sitio web esta disponible en varios idiomas, lo que lo hace accesible para usuarios de todo el mundo. En general, 1win es una plataforma de apuestas en linea solida y confiable que ofrece una amplia variedad de opciones de apuestas deportivas y juegos de casino.
Codigo promocional 1Win son canjeados desde su registro y utilizados en los juegos. Aplica el codigo 937999 y recibe ganancias al apostar. El codigo de promocion 2024 te regala un paquete de bienvenida del 500% con los cuatro primeros depositos hasta $700 en apuestas deportivas y casino. El codigo 1win de bono debe ser ingresado en el formulario de registro.
Si esta buscando una forma de maximizar sus ganancias en apuestas deportivas, no se pierda el codigo de promocion y el bono de bienvenida 1Win en 024]. Con el codigo de promocion 1Win puedes recibir ofertas exclusivas y apuestas gratis para disfrutar aun mas de tus juegos favoritos. Ademas, el bono de bienvenida 1Win es una gran oportunidad para aumentar sus ganancias y tener una experiencia de apuestas aun mas emocionante.
Bonificacion 1win – 937999
Como activo el vale en 1win?
Durante el proceso de registro se introduce un codigo promocional de la casa de apuestas 1win. El campo “Anadir codigo promocional” estara disponible para cualquier metodo de creacion de cuenta que elija. Tenga en cuenta que este campo es opcional en la fase de registro, asi que tenga cuidado al introducirlo. Si se olvida de hacerlo al registrarse, no podra activar su codigo en 1win y el bono de bienvenida dejara de estar disponible.
Tendras que recargar tu cuenta para poder utilizar el codigo promocional en el futuro. Una vez que haya introducido el codigo promocional durante el registro, vaya a su gabinete personal a traves del icono de usuario y haga clic en “Depositar”. Tomemos como ejemplo el codigo promocional “937999”, que corresponde a 200 euros.
Caracteristicas del bono 1win
El codigo promocional es proporcionado por representantes de la oficina de la casa de apuestas 1win. Lo hacen en varias ocasiones: durante una promocion, un dia festivo importante, el cumpleanos de un usuario, para volver a captar a un jugador que ha estado jugando durante un tiempo y ha dejado de estar activo.
Si introdujiste un codigo promocional al registrarte, veras los fondos de bonificacion en cuanto inicies sesion en tu perfil. Y si te lo dieron personalmente, deberas aceptar participar en la promocion para poder utilizarlo. Estos fondos se abonan en tu cuenta de bonificacion, y podras ver el importe en tu perfil personal. Si respeta las normas de uso de los fondos de bonificacion, podra convertirlos gradualmente en dinero en efectivo, que recibira ademas de sus ganancias.
?Que tan confiable es apostar en 1win?
Apostar en 1win es 100% confiable. 1win nacio en 2016, con el nombre de MFI Investments Limited, quienes estan registrados con el numero de licencia 8048/JAZ2018-040, otorgada por la Comision de Juegos eGaming.
Ademas, cuenta con alianzas comerciales con diferentes equipos y ligas, como la UEFA, UFC, NHL, FIFA y mas.
8. Opiniones 1win Casino 2024
1win casino es una excelente opcion para comenzar a apostar, ademas de que cuentas con el regalo para registrarte con el codigo promocional 937999. Podras tener tu cuenta abierta en todos lados, tu celular y tu computadora tendran tu cuenta sincronizada.
Es un sitio seguro, con numero de registro y sistemas de pago legales afiliados. Podras apostar con cualquier metodo de pago en mas de 50 deportes diferentes y cientos de juegos de casino. 1win es recomendable y esta lleno de diversion.
9. FAQ: 1win Codigo Promocional
9.1 ?? ?1win es un sitio seguro?
1win es un sitio seguro, esta avalado por la comision de juego eGaming. Sus metodos de pago son conocidos y de fiar, cada uno de ellos. Ademas, tambien de tener soporte tecnico las 24 horas ante cualquier duda.
9.2 ?? ?Hay bono de bienvenida de 1win?
Si existe, y para obtener este bono de bienvenida de 1win, necesitaras el codigo de bienvenida 937999, tendras que registrarte en 1win con este codigo y realizar tu primer deposito.
9.3 ?? ?Cual es el codigo de bono 1win?
El codigo promocional 1win es 937999, registrate y comienza a disfrutar de tu bono.
Бездоганний стиль пін ап
казіно без депозиту https://www.pinupcasinoqgcvbisd.kiev.ua/ .
Viagra 75mg
Спокусливий пін ап
pin up реєстрація https://www.pinupcasinoqgcvbisd.kiev.ua/ .
purple pharmacy mexico price list mexican pharmacy medication from mexico pharmacy
mexican border pharmacies shipping to usa mexican pharmacy reputable mexican pharmacies online
sildenafil 20 mg tablet
Ремонт стиральных машин – высокое качество работы у вас дома. Широкая база выезжающих к заказчику мастеров вызвать мастера на ремонт стиралки
Medication prescribing information. Generic Name.
lyrica
Everything information about medication. Get now.
Ремонт стиральных машин – высокое качество работы у вас дома. Широкая база выезжающих к заказчику мастеров ремонт стиральных машин спб
прикольные поздравления с днем рождения на телефон https://na-telefon.biz/
%%
My site: molbert-banket.ru
medicine in mexico pharmacies mexico pharmacies prescription drugs medication from mexico pharmacy
This site definitely has all of the information I needed about this subject
My website: порнушка дома
sildenafil generic
Mi sitio web
mexican mail order pharmacies mexican mail order pharmacies mexican pharmacy
tube
Товаррищь афтор,есть в более лучшем качестве ?
next we withdraw all money won and see how fast payouts are at the http://solun.hu/component/k2/item/5-unde-omnis-iste-natus for players.
Watches World
Watches World
Client Testimonials Reveal Timepieces Universe Adventure
At WatchesWorld, client contentment isn’t just a objective; it’s a radiant evidence to our dedication to perfection. Let’s plunge into what our cherished buyers have to say about their encounters, shedding light on the impeccable service and amazing clocks we present.
O.M.’s Review Feedback: A Seamless Adventure
“Very good contact and follow-up process throughout the process. The watch was flawlessly packed and in pristine. I would certainly work with this teamwork again for a watch buy.
O.M.’s testimony illustrates our loyalty to communication and thorough care in delivering watches in perfect condition. The reliance established with O.M. is a foundation of our customer bonds.
Richard Houtman’s Informative Testimonial: A Private Reach
“I dealt with Benny, who was exceptionally assisting and gracious at all times, keeping me regularly apprised of the process. Moving forward, even though I ended up sourcing the watch locally, I would still surely recommend Benny and the enterprise moving forward.
Richard Houtman’s interaction illustrates our personalized approach. Benny’s help and ongoing interaction exhibit our dedication to ensuring every customer feels esteemed and apprised.
Customer’s Effective Support Review: A Smooth Transaction
“A very efficient and effective service. Kept me informed on the purchase progression.
Our dedication to productivity is echoed in this client’s commentary. Keeping patrons informed and the seamless progress of transactions are integral to the Our Watch Boutique journey.
Explore Our Latest Offerings
Audemars Piguet Royal Oak Selfwinding 37mm
An exquisite piece at €45,900, this 2022 edition (REF: 15551ST.ZZ.1356ST.05) invites you to add it to your basket and elevate your assortment.
Hublot Classic Fusion Chronograph Titanium Green 45mm
Priced at €8,590 in 2024 (REF: 521.NX.8970.RX), this Hublot creation is a blend of fashion and invention, awaiting your inquiry.
sildenafil buy
news24time.net
mexican online pharmacies prescription drugs medication from mexico pharmacy mexican rx online
tube
Drug prescribing information. Brand names.
fluoxetine
All about medicine. Get information now.
medication from mexico pharmacy mexican pharmacy mexican pharmaceuticals online
buy viagra online reviews
canada-welcome.com
buying prescription drugs in mexico mexican online pharmacies prescription drugs mexican pharmaceuticals online
купить диплом магистра man-diploms.com .
canadian viagra sales
mexico drug stores pharmacies medication from mexico pharmacy pharmacies in mexico that ship to usa
viagra pills price
Meds information leaflet. What side effects can this medication cause?
stromectol
Everything about medicine. Get now.
mexican rx online mexico drug stores pharmacies pharmacies in mexico that ship to usa
%%
Here is my blog https://2017.mangafest.net/post/news/mini-ghostpedia-kuchisake-onna/
mexico pharmacies prescription drugs mexican border pharmacies shipping to usa mexico drug stores pharmacies
Разборка и снос старых деревянных и кирпичных домов с вывозом мусора в Москве и Подмосковье. Разборка домов и вывоз мусора – больше об услуге на сайте kleinburd.ru. Производим демонтаж домов, зданий и фундаментов вручную и спецтехникой по ценам ниже рынка за 24 часа. Бесплатный выезд инженера на объект.
best place to buy viagra
mexican mail order pharmacies buying prescription drugs in mexico online mexico drug stores pharmacies
Полностью разделяю Ваше мнение. Мне нравится эта идея, я полностью с Вами согласен.
plastic cards, with which insurance applies to rental of real estate transport does not cover the rental of a motorcycle. will you still ride a https://original.misterpoll.com/users/5417794 along the entire route 66?
Мы предлагаем широкий выбор лазерных станков с передовой технологией, обеспечивая высокую производительность и качество резки купить лазерная резка
Мы предлагаем широкий выбор лазерных станков с передовой технологией, обеспечивая высокую производительность и качество резки лазерный станок по дереву с чпу для домашней мастерской цена
Тайны использования ремонтной смеси
цвета кирпичной кладки https://www.remontnaja-smes-dlja-kirpichnoj-kladki.ru .
hello-food
Приветствую, форумчане! Расскажу о волшебстве upx официальный сайт. Это игровое заведение просто поражает многообразием развлечений, захватывающими подарками и настроем страстного эмоций. Здесь любой момент – шанс осознать вдохновение и удачу. Присоединяйтесь, и вместе раскроем проходы в мир захватывающих путешествий!
low cost viagra online
Dig up the ultimate gateway to smart investing with Invest -Properties . Dive into a world where opportunities meet potential. Unlock your investment journey and transform your financial future today with our expert insights and tailored solutions. Start now
Medication information for patients. Drug Class.
zithromax brand name
All trends of medicament. Read information now.
oknews360.com
Широкий выбор автомобильных весов: грузовые, железобетонные, подкладные весы для авто
Широкий выбор автомобильных весов: грузовые, железобетонные, подкладные https://giport.ru/forum/auto/avtomobilnye-vesy
Как перетянуть мебель в Минске? Обратись к нам!
реставрация мебели в минске https://peretyazhka-mebeli-vminske.ru/ .
mexico drug stores pharmacies pharmacies in mexico that ship to usa best online pharmacies in mexico
самые лучшие женские сайты
where can i buy viagra without a prescription
chinanews777.com
mexican border pharmacies shipping to usa mexico pharmacy mexico pharmacy
ligand gated
Viagra Soft Tabs
buying from online mexican pharmacy mexican online pharmacies prescription drugs mexican pharmacy
Снимем арест. Оплатим судебным приставам все Ваши долги и поможем снять арест от ФССП. Оплатим ЖКХ/ Купим жилье с долгами за свет, воду и прочими коммунальными услуги.
срочные продажи квартир
arizonawood.net
%%
Feel free to surf to my web-site https://nksesvete.hr/klub/nk-radnik-sesvete-od-zgarista-do-stadiona/
investnews24.net
Viagra 100mg
aurora libraries
buying prescription drugs in mexico mexican online pharmacies prescription drugs mexico pharmacies prescription drugs
Элитные резиденции вблизи лучших достопримечательностей Сочи. Вид на море и горы элитные коттеджи в Сочи
Ponto IPTV a melhor programacao de canais IPTV do Brasil, filmes, series, futebol
My website: смотреть порно трансвеститов
viagra coupons
buying prescription drugs in mexico medicine in mexico pharmacies mexico drug stores pharmacies
Hello it’s me, I am also visiting this website on a regular basis, this
web page is genuinely pleasant and the people are really sharing good thoughts.
medicine in mexico pharmacies mexican mail order pharmacies mexican pharmaceuticals online
Эдуард Давыдов, рожденный в 1984 году в семье медицинского работника и ученого, изначально был страстно увлечен дзюдо, но путь к науке, указанный отцом, определил его профессиональное направление Эдуард Давыдов
Эдуард Давыдов, рожденный в 1984 году в семье медицинского работника и ученого, изначально был страстно увлечен дзюдо, но путь к науке, указанный отцом, определил его профессиональное направление Эдуард Давыдов бск
Весьма признателен за помощь в этом вопросе, может, я тоже могу Вам чем-то помочь?
voce sempre pode saber como Encontrar bonus em alguns sites de apostas, assim, com codigo http://www.sahinay.com/home-renovations-with-no-fuss/ do cupom kto.
ligand channels
viagra meaning
mexican pharmaceuticals online mexico drug stores pharmacies medicine in mexico pharmacies
1xBet промокод — 1XFREE777 впишите код в анкете при регистрации, пополните счет от 100 рублей и вы получите бонус +100% (до 32500 рублей).
https://www.covrik.com/covers/inc/1xbet_promokod_aktualnuy_pri_registracii.html
Промокод 1xBet на 2024 год предоставляет возможность получить бонусы при регистрации на сайте букмекерской конторы.
viagra from canadian pharmacy
credito 8500 euros
Obten descuentos adicionales con un codigo descuento 1Win
1win es una plataforma de apuestas en linea que ofrece una amplia variedad de opciones de apuestas deportivas y juegos de casino. La pagina web es facil de navegar y tiene un diseno moderno y atractivo. En cuanto a las apuestas deportivas, 1win ofrece una amplia variedad de deportes para apostar, desde los mas populares como el futbol y el baloncesto hasta deportes menos conocidos como el badminton y el rugby. Ademas, la plataforma ofrece una gran cantidad de mercados de apuestas para cada evento deportivo, lo que permite a los usuarios personalizar sus apuestas de acuerdo a sus preferencias. En cuanto a los juegos de casino, 1win ofrece una amplia variedad de opciones, desde tragamonedas hasta juegos de mesa como el blackjack y la ruleta. Los juegos son de alta calidad y estan disenados por algunos de los principales proveedores de software de casino. La plataforma tambien ofrece una amplia variedad de metodos de pago, incluyendo tarjetas de credito, billeteras electronicas y criptomonedas. Ademas, el sitio web esta disponible en varios idiomas, lo que lo hace accesible para usuarios de todo el mundo. En general, 1win es una plataforma de apuestas en linea solida y confiable que ofrece una amplia variedad de opciones de apuestas deportivas y juegos de casino.
1Win son canjeados desde su registro y utilizados en los juegos. Aplica el codigo 937999 y recibe ganancias al apostar. El codigo de promocion 2024 te regala un paquete de bienvenida del 500% con los cuatro primeros depositos hasta $700 en apuestas deportivas y casino. El codigo 1win de bono debe ser ingresado en el formulario de registro.
Si esta buscando una forma de maximizar sus ganancias en apuestas deportivas, no se pierda el codigo de promocion y el bono de bienvenida 1Win en 024]. Con el codigo de promocion 1Win puedes recibir ofertas exclusivas y apuestas gratis para disfrutar aun mas de tus juegos favoritos. Ademas, el bono de bienvenida 1Win es una gran oportunidad para aumentar sus ganancias y tener una experiencia de apuestas aun mas emocionante.
Bonificacion 1win – 937999
Como activo el vale en 1win?
Durante el proceso de registro se introduce un codigo promocional de la casa de apuestas 1win. El campo “Anadir codigo promocional” estara disponible para cualquier metodo de creacion de cuenta que elija. Tenga en cuenta que este campo es opcional en la fase de registro, asi que tenga cuidado al introducirlo. Si se olvida de hacerlo al registrarse, no podra activar su codigo en 1win y el bono de bienvenida dejara de estar disponible.
Tendras que recargar tu cuenta para poder utilizar el codigo promocional en el futuro. Una vez que haya introducido el codigo promocional durante el registro, vaya a su gabinete personal a traves del icono de usuario y haga clic en “Depositar”. Tomemos como ejemplo el codigo promocional “937999”, que corresponde a 200 euros.
Caracteristicas del bono 1win
El codigo promocional es proporcionado por representantes de la oficina de la casa de apuestas 1win. Lo hacen en varias ocasiones: durante una promocion, un dia festivo importante, el cumpleanos de un usuario, para volver a captar a un jugador que ha estado jugando durante un tiempo y ha dejado de estar activo.
Si introdujiste un codigo promocional al registrarte, veras los fondos de bonificacion en cuanto inicies sesion en tu perfil. Y si te lo dieron personalmente, deberas aceptar participar en la promocion para poder utilizarlo. Estos fondos se abonan en tu cuenta de bonificacion, y podras ver el importe en tu perfil personal. Si respeta las normas de uso de los fondos de bonificacion, podra convertirlos gradualmente en dinero en efectivo, que recibira ademas de sus ganancias.
?Que tan confiable es apostar en 1win?
Apostar en 1win es 100% confiable. 1win nacio en 2016, con el nombre de MFI Investments Limited, quienes estan registrados con el numero de licencia 8048/JAZ2018-040, otorgada por la Comision de Juegos eGaming.
Ademas, cuenta con alianzas comerciales con diferentes equipos y ligas, como la UEFA, UFC, NHL, FIFA y mas.
8. Opiniones 1win Casino 2024
1win casino es una excelente opcion para comenzar a apostar, ademas de que cuentas con el regalo para registrarte con el codigo promocional 937999. Podras tener tu cuenta abierta en todos lados, tu celular y tu computadora tendran tu cuenta sincronizada.
Es un sitio seguro, con numero de registro y sistemas de pago legales afiliados. Podras apostar con cualquier metodo de pago en mas de 50 deportes diferentes y cientos de juegos de casino. 1win es recomendable y esta lleno de diversion.
9. FAQ: 1win Codigo Promocional
9.1 ?? ?1win es un sitio seguro?
1win es un sitio seguro, esta avalado por la comision de juego eGaming. Sus metodos de pago son conocidos y de fiar, cada uno de ellos. Ademas, tambien de tener soporte tecnico las 24 horas ante cualquier duda.
9.2 ?? ?Hay bono de bienvenida de 1win?
Si existe, y para obtener este bono de bienvenida de 1win, necesitaras el codigo de bienvenida 937999, tendras que registrarte en 1win con este codigo y realizar tu primer deposito.
9.3 ?? ?Cual es el codigo de bono 1win?
El codigo promocional 1win es 937999, registrate y comienza a disfrutar de tu bono.
mexican rx online mexico drug stores pharmacies mexican pharmacy
sildenafil femme
ST666
mexican pharmacy mexican border pharmacies shipping to usa mexico drug stores pharmacies
mexico pharmacy mexico drug stores pharmacies mexican border pharmacies shipping to usa
cheap price viagra
ligand gated
buying prescription drugs in mexico reputable mexican pharmacies online mexican pharmacy
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://accounts.binance.com/sk/register?ref=V2H9AFPY
viagra no prescription
reputable mexican pharmacies online mexican border pharmacies shipping to usa best online pharmacies in mexico
купить диплом магистра orik-diploms.com .
cost for viagra
%%
Feel free to visit my homepage https://lvr24.com/2020/01/16/guide-to-remodeling-your-building/
Могу предложить зайти на сайт, где есть много статей на интересующую Вас тему.
em funcionamento varanda privativa, http://deharscamp.nl/hello-world/ grande massa de caras com vista panoramica do oceano.
zithromax without a doctor prescription
buying prescription drugs in mexico mexico drug stores pharmacies mexico pharmacies prescription drugs
pharmacies in mexico that ship to usa mexico drug stores pharmacies reputable mexican pharmacies online
надежные онлайн казино
sildenafil viagra
https://hello-food.ru/
breakingnews77.com
mexican drugstore online buying from online mexican pharmacy mexico pharmacy
хорошее онлайн казино
крипто казино онлайн
buy generic viagra
madeintexas.net
онлайн казино регистрация
Bonos y codigos promocionales 1win
1win es una plataforma de apuestas en linea reconocida por su compromiso de brindar a los jugadores una experiencia de juego unica y emocionante. Ya sea que te apasione el deporte, los juegos de casino o ambas opciones, 1win te ofrece una amplia gama de oportunidades para disfrutar y ganar.
Con bonificaciones y codigos promocionales exclusivos, 1 win se destaca como un destino lider para los entusiastas de las apuestas en linea. Desde bonos de bienvenida hasta promociones periodicas y ofertas exclusivas, descubriras como 1win se esfuerza por ofrecer a sus jugadores mexicanos oportunidades emocionantes para maximizar sus ganancias y ampliar su experiencia de juego.
Tipos de Bonificaciones en 1win
1win se destaca al ofrecer una amplia variedad de bonificaciones y promociones para satisfacer a jugadores de todas las preferencias:
Bonos de Bienvenida: Los nuevos jugadores son recibidos en 1win con un espectacular bono de bienvenida. Este bono se distribuye en los primeros cuatro depositos, lo que significa que tendras la oportunidad de aumentar significativamente tu saldo inicial. El bono de bienvenida puede alcanzar un impresionante 500% en total, con un limite de hasta 750 dolares.
Programa de Lealtad: En 1win, la lealtad de los jugadores es recompensada. El programa de lealtad de 1win ofrece a los jugadores la oportunidad de ascender en niveles y desbloquear recompensas exclusivas a medida que juegan mas y disfrutan de los juegos en la plataforma.
Cashback (Reembolso): El cashback es una caracteristica unica en 1win que te permite recibir un reembolso de una parte de tus perdidas en apuestas. Este beneficio es una forma de asegurarte de que, incluso si no tienes suerte en una apuesta en particular, aun obtendras algo a cambio.
Torneos: Los torneos en 1win anaden emocion adicional a tu experiencia de juego. Participar en torneos te brinda la oportunidad de competir con otros jugadores por premios en efectivo y otros premios emocionantes. Los torneos pueden abarcar una variedad de juegos, desde tragamonedas hasta apuestas deportivas, y ofrecen una oportunidad adicional para ganar.
Promociones con Codigos (Promocodes): Los codigos promocionales exclusivos son una caracteristica emocionante en 1win. Estos codigos pueden desbloquear bonificaciones adicionales, giros gratis y otras recompensas especiales.
En 1win, la diversidad de bonificaciones y promociones garantiza que siempre haya algo emocionante esperandote.
Como Aprovechar al Maximo las Bonificaciones
Las bonificaciones en 1win ofrecen una oportunidad excepcional para aumentar tus ganancias y prolongar tu experiencia de juego en linea. Una de las bonificaciones mas destacadas es el emocionante bono de bienvenida:
Registrate en 1win y proporciona informacion precisa y completa.
Realiza tu primer deposito, ya que el bono se distribuye en los primeros cuatro depositos.
Reclama tu bono, que se acreditara automaticamente en tu cuenta.
Cumple con los requisitos de apuesta, que indican la cantidad de dinero que debes apostar antes de retirar las ganancias.
Explora y juega en una amplia gama de juegos, como tragamonedas o apuestas deportivas, para aumentar tus posibilidades de ganar.
El bono de bienvenida en 1win es una emocionante ventaja para comenzar tu experiencia de juego en linea. Sigue estos pasos y disfruta al maximo de tu bono en una de las principales plataformas de apuestas en linea de Mexico.
Codigos Promocionales en 1win
Los codigos promocionales en 1win son una forma emocionante de aumentar tus oportunidades de ganar y aprovechar al maximo tu experiencia de juego. Estos codigos se pueden encontrar en varios lugares, lo que te brinda la posibilidad de desbloquear bonificaciones adicionales y ofertas exclusivas.
Muchos sitios web tematicos y portales dedicados a los juegos de azar ofrecen codigos promocionales de 1win. Estos codigos se actualizan regularmente y pueden proporcionarte bonificaciones unicas. Visita estos sitios y busca los codigos promocionales mas recientes.
Las redes sociales, como Facebook, Twitter e Instagram, son otra fuente donde puedes encontrar codigos promocionales. 1win a menudo publica codigos en sus perfiles sociales. Asegurate de seguir sus cuentas y estar atento a las publicaciones para no perderte ninguna oferta especial.
Si estas registrado en 1win y has aceptado recibir correos electronicos promocionales, es posible que recibas codigos promocionales exclusivos en tu bandeja de entrada. Estos codigos pueden ofrecer bonificaciones personalizadas segun tu historial de juego.
Una vez que tengas un codigo promocional, sigue estos sencillos pasos para activarlo:
Inicia sesion en tu cuenta de 1win.
Dirigete a la seccion de “Cuenta” o “Promociones” en tu perfil.
Ingresa el codigo promocional en el campo designado.
Confirma la activacion del codigo.
?Listo! Tu bonificacion se aplicara automaticamente a tu cuenta.
Asegurate de leer los terminos y condiciones asociados con cada codigo promocional para comprender completamente las bonificaciones y los requisitos de apuesta.
Beneficios de Utilizar Bonos y Codigos Promocionales
El uso de bonos y codigos promocionales en 1win ofrece una serie de beneficios que mejoran significativamente la experiencia de juego en linea:
Aumento del Saldo: Los bonos y codigos promocionales aumentan tu saldo, lo que te permite jugar mas y disfrutar de una mayor variedad de juegos sin invertir mas dinero de tu bolsillo.
Mas Oportunidades de Ganar: Con un saldo adicional, tienes mas oportunidades de ganar premios en efectivo y otros premios en los juegos de 1win. Esto aumenta la emocion y la diversion.
Menos Riesgo: Los bonos y codigos promocionales te permiten apostar con menos riesgo, ya que estas utilizando fondos de bonificacion. Esto significa que puedes probar nuevos juegos o estrategias sin preocuparte tanto por las perdidas.
Acceso a Ofertas Exclusivas: Al utilizar codigos promocionales, a menudo puedes acceder a ofertas exclusivas que no estan disponibles para otros jugadores. Estas ofertas pueden incluir giros gratis, bonos de recarga y mas.
Mayor Tiempo de Juego: Con mas fondos a tu disposicion, puedes disfrutar de una experiencia de juego mas prolongada, lo que agrega diversion y emocion a tu tiempo en 1win.
Exploracion de Juegos: Utilizar bonos y codigos promocionales te brinda la oportunidad de explorar nuevos juegos y actividades en el sitio sin incurrir en gastos adicionales.
En resumen, los bonos y codigos promocionales en 1win no solo te brindan beneficios tangibles en terminos de saldo adicional y oportunidades de ganar, sino que tambien mejoran tu experiencia de juego en general. Aprovecha estas ofertas especiales para disfrutar al maximo de tu tiempo en 1win y maximizar tus posibilidades de exito. Obten descuentos adicionales con un codigo descuento 1Win
1win es una plataforma de apuestas en linea que ofrece una amplia variedad de opciones de apuestas deportivas y juegos de casino. La pagina web es facil de navegar y tiene un diseno moderno y atractivo. En cuanto a las apuestas deportivas, 1win ofrece una amplia variedad de deportes para apostar, desde los mas populares como el futbol y el baloncesto hasta deportes menos conocidos como el badminton y el rugby. Ademas, la plataforma ofrece una gran cantidad de mercados de apuestas para cada evento deportivo, lo que permite a los usuarios personalizar sus apuestas de acuerdo a sus preferencias. En cuanto a los juegos de casino, 1win ofrece una amplia variedad de opciones, desde tragamonedas hasta juegos de mesa como el blackjack y la ruleta. Los juegos son de alta calidad y estan disenados por algunos de los principales proveedores de software de casino. La plataforma tambien ofrece una amplia variedad de metodos de pago, incluyendo tarjetas de credito, billeteras electronicas y criptomonedas. Ademas, el sitio web esta disponible en varios idiomas, lo que lo hace accesible para usuarios de todo el mundo. En general, 1win es una plataforma de apuestas en linea solida y confiable que ofrece una amplia variedad de opciones de apuestas deportivas y juegos de casino.
Codigo promocional 1Win son canjeados desde su registro y utilizados en los juegos. Aplica el codigo 937999 y recibe ganancias al apostar. El codigo de promocion 2024 te regala un paquete de bienvenida del 500% con los cuatro primeros depositos hasta $700 en apuestas deportivas y casino. El codigo 1win de bono debe ser ingresado en el formulario de registro.
Si esta buscando una forma de maximizar sus ganancias en apuestas deportivas, no se pierda el codigo de promocion y el bono de bienvenida 1Win en 024]. Con el codigo de promocion 1Win puedes recibir ofertas exclusivas y apuestas gratis para disfrutar aun mas de tus juegos favoritos. Ademas, el bono de bienvenida 1Win es una gran oportunidad para aumentar sus ganancias y tener una experiencia de apuestas aun mas emocionante.
Bonificacion 1win – 937999
Como activo el vale en 1win?
Durante el proceso de registro se introduce un codigo promocional de la casa de apuestas 1win. El campo “Anadir codigo promocional” estara disponible para cualquier metodo de creacion de cuenta que elija. Tenga en cuenta que este campo es opcional en la fase de registro, asi que tenga cuidado al introducirlo. Si se olvida de hacerlo al registrarse, no podra activar su codigo en 1win y el bono de bienvenida dejara de estar disponible.
Tendras que recargar tu cuenta para poder utilizar el codigo promocional en el futuro. Una vez que haya introducido el codigo promocional durante el registro, vaya a su gabinete personal a traves del icono de usuario y haga clic en “Depositar”. Tomemos como ejemplo el codigo promocional “937999”, que corresponde a 200 euros.
Caracteristicas del bono 1win
El codigo promocional es proporcionado por representantes de la oficina de la casa de apuestas 1win. Lo hacen en varias ocasiones: durante una promocion, un dia festivo importante, el cumpleanos de un usuario, para volver a captar a un jugador que ha estado jugando durante un tiempo y ha dejado de estar activo.
Si introdujiste un codigo promocional al registrarte, veras los fondos de bonificacion en cuanto inicies sesion en tu perfil. Y si te lo dieron personalmente, deberas aceptar participar en la promocion para poder utilizarlo. Estos fondos se abonan en tu cuenta de bonificacion, y podras ver el importe en tu perfil personal. Si respeta las normas de uso de los fondos de bonificacion, podra convertirlos gradualmente en dinero en efectivo, que recibira ademas de sus ganancias.
?Que tan confiable es apostar en 1win?
Apostar en 1win es 100% confiable. 1win nacio en 2016, con el nombre de MFI Investments Limited, quienes estan registrados con el numero de licencia 8048/JAZ2018-040, otorgada por la Comision de Juegos eGaming.
Ademas, cuenta con alianzas comerciales con diferentes equipos y ligas, como la UEFA, UFC, NHL, FIFA y mas.
8. Opiniones 1win Casino 2024
1win casino es una excelente opcion para comenzar a apostar, ademas de que cuentas con el regalo para registrarte con el codigo promocional 937999. Podras tener tu cuenta abierta en todos lados, tu celular y tu computadora tendran tu cuenta sincronizada.
Es un sitio seguro, con numero de registro y sistemas de pago legales afiliados. Podras apostar con cualquier metodo de pago en mas de 50 deportes diferentes y cientos de juegos de casino. 1win es recomendable y esta lleno de diversion.
9. FAQ: 1win Codigo Promocional
9.1 ?? ?1win es un sitio seguro?
1win es un sitio seguro, esta avalado por la comision de juego eGaming. Sus metodos de pago son conocidos y de fiar, cada uno de ellos. Ademas, tambien de tener soporte tecnico las 24 horas ante cualquier duda.
9.2 ?? ?Hay bono de bienvenida de 1win?
Si existe, y para obtener este bono de bienvenida de 1win, necesitaras el codigo de bienvenida 937999, tendras que registrarte en 1win con este codigo y realizar tu primer deposito.
9.3 ?? ?Cual es el codigo de bono 1win?
El codigo promocional 1win es 937999, registrate y comienza a disfrutar de tu bono.
1Win Приветственный Бонус (2024)
Промокод 1Вин: 937999. При первом депозите вы получите бонус в размере 500% до 200 000 рублей на свой счет. Чтобы получить денежные вознаграждения для спорта и казино, необходимо использовать специальный бонусный промокод 1win.
Для новых клиентов компания 1win предлагает приветственный бонус в размере 500% от суммы депозита, который не должен превышать 15,000 рублей. Чтобы вывести бонусные средства, их необходимо сначала отыграть. Бонусные 500% разделены на 4 депозита.
Порядок получения бонуса:
1. Первый депозит – 200% от суммы депозита;
2. Второй депозит – 150% от суммы второго депозита;
3. Третий депозит – 100% от суммы;
4. Четвертый депозит – 50% от суммы.
Таким образом, бонусы можно получить четыре раза, но следует учесть, что существуют особые правила и сроки отыгрыша бонусного счета. Максимальная сумма бонусных средств составляет 200,000 рублей, а бонус на один депозит – 50,000 рублей.
Промокод на 1Win – 937999 предоставляет бонус на первые 4 депозита, который может достигать 500% до 200 000 рублей. Если вы ввели промокод при регистрации, то бонусные средства будут отображаться в вашем профиле сразу же после входа. Если же вам промокод был предоставлен лично, то для его активации необходимо дать согласие на участие в акции.
После регистрации и ввода промокода 1вин для пополнения счета и получения приветственного бонуса, вы можете начать играть. Однако, вы не сможете сразу вывести бонусные средства – сначала их нужно отыграть.
Для этого необходимо делать ставки с коэффициентом от 3. В случае выигрыша, вы получите 5% от бонусного счета на свой основной счет.
Давайте рассмотрим это на примере:
Вы внесли депозит в размере 10 000 рублей на свой счет в 1win. На бонусный счет поступило 200% от суммы депозита, то есть 20 000 рублей;
Затем вы сделали ставку с коэффициентом 3, и в случае выигрыша получили 30 000 рублей от ставки плюс 500 рублей (5% от бонусного счета). Теперь ваш счет составляет 30 500 рублей, а бонусный счет – 19 500 рублей.
Таким образом, вы отыграли 500 рублей. Продолжая делать ставки, вы сможете отыграть всю сумму бонуса.
Отыгранные средства становятся доступными для вывода сразу же.
Обратите внимание, что ставки с коэффициентом менее 3 не будут учтены при отыгрыше бонуса.
Кроме того, что БК предоставляет приветственный промокод 1win при пополнении баланса, она также предлагает своим игрокам другие бонусы и акции. Доступные предложения подойдут как для любителей казино, так и для тех игроков, которым нравится собирать экспрессы. В следующем разделе мы подробно рассмотрим каждую из актуальных на данный момент акций.
Бездепозитный Бонус 1win 2024
Бонусы от казино 1Win 2024 – Бездепозитные бонусы ? Коды на возврат денег ? VIP Программа лояльности ? Бесплатные фриспины.
Промокод 1Win казино: 937999 предоставляет новым игрокам бонус 500% для игры в слоты и игровые автоматы, максимальная сумма бонуса 200 000 рублей. Вы можете использовать бонусные деньги в разделе азартных игр, включая онлайн казино, карты, рулетку, игровые автоматы и слоты.
Компания «1Win» рада предложить своим новым клиентам приветственный бонус в размере до 500% на первые четыре депозита. Это выгодное предложение доступно сразу после регистрации в нашей букмекерской конторе. Бонус можно получить не только в рублях, но и в других валютах, при этом он не ограничивает возможность участия игроков в других программам лояльности компании. Максимальная сумма вознаграждения за регистрацию составляет 75000 рублей или эквивалентная сумма в другой валюте.
Бонусы в 1win приносят игрокам множество преимуществ. Во-первых, они позволяют увеличить начальную ставку или продлить время игры. Кроме того, они дают возможность попробовать различные игры без риска потерять реальные деньги. Бонусы также повышают шансы на выигрыш и предоставляют дополнительные возможности для получения прибыли. Кроме того, бонусы в 1win могут быть обменены на реальные деньги или использованы для участия в специальных акциях и турнирах.
Преимущества получения и использования бонусов в 1win очевидны. Они позволяют игроку расширить свои возможности и получить больше удовольствия от игры. Бонусы также делают игру более выгодной с финансовой точки зрения, помогая уменьшить риски и увеличить потенциальную прибыль. Кроме того, получение и использование бонусов в 1win открывает возможность стать лояльным клиентом и получить дополнительные привилегии и вознаграждения от казино.
Итак, получение бонусов в 1win – это отличная возможность для игрока увеличить свои шансы на выигрыш, получить дополнительные деньги и улучшить свой игровой опыт. Бонусы делают игру более интересной и выгодной.
Промокод 1Win: 937999 предоставляет возможность получить бездепозитный бонус 2024. Его можно получить в виде фриспинов или фрибетов. Чтобы получить подарок, необходимо активировать код в личном кабинете. Дополнительный депозит не требуется. Размеры подарков невелики: фрибет до 500 рублей и не более 70 фриспинов для игры в слоты. Как и в случае с другими поощрениями, необходимо отыграть бездепозитный бонус. Вейджер, как правило, не превышает х5 для бесплатных ставок и х30 для фриспинов.
В казино 1win предоставляется внушительный бонус при регистрации, который составляет 500% от суммы первых четырех последовательных депозитов клиента. С таким количеством бонусов новичок может значительно увеличить свои шансы на выигрыш. Чтобы получить этот приветственный бонус, необходимо зарегистрироваться на официальном сайте, рабочем зеркале, мобильной версии или приложениях для мобильных телефонов. Однако, основным условием является совершение первого пополнения счета, так как активировать бонусы 1win можно только после этого.
1Win промокод на фриспины: 937999 используйте бонусный код при регистрации и получите бездепозтный бонус 70 фриспинов. Да, при использовании кода 1Win вы можете получить различные поощрения, включая бездепозитные бонусы. Они обычно представлены в виде фрибетов или фриспинов. Для их активации не требуется дополнительное пополнение счета. Размер таких подарков невелик: бесплатных вращений не более 70. Вейджер на бездепозитный бонус обычно не превышает х35. В 1Win вы можете получить бонусы за участие в акциях, турнирах, розыгрышах и активацию промокода. Бонусная программа периодически обновляется. Кроме того, некоторые акции имеют сезонный характер.
В 1Win основная бонусная программа включает в себя фриспины. Чтобы получить 70FS, необходимо пополнить счет на 100 рублей или более. Игроку предоставляется 2 дня с момента регистрации для активации презента. Отыгрыш бонуса должен быть выполнен в течение 24 часов с момента начисления, с вейджером х35. Бесплатные вращения предназначены только для игр провайдера Microgaming.
Так как бонусная программа 1Win регулярно обновляется, список акций, в которых можно получить фриспины, постоянно расширяется. Более подробную информацию о них можно найти на нашем сайте.
Промокод на 1Win дает возможность получить бесплатные вращения. Их можно использовать в любых слотах из каталога казино. Иногда могут быть установлены ограничения, которые предусматривают использование фриспинов только в определенных слотах или играх конкретного провайдера. Фриспины начисляются с фиксированной ставкой. Отыгрыш выигрыша, полученного с помощью бесплатных вращений, обязателен с учетом установленного вейджера.
Way cool! Some very valid points! I appreciate you penning this write-up and the rest of the site is very good.
low cost viagra online
buying prescription drugs in mexico online mexican pharmacy buying prescription drugs in mexico online
PЕЇjДЌka 23000 KДЌ
п»їbest mexican online pharmacies mexican border pharmacies shipping to usa medication from mexico pharmacy
Sildenafil 100mg
mexican rx online mexican rx online mexico drug stores pharmacies
site porn
gama casino
otc sildenafil
buying prescription drugs in mexico medicine in mexico pharmacies medication from mexico pharmacy
ele tem um bom argumento
https://folkd.com/profile/aesthete
I’m extremely pleased to discover this website. I wanted to thank you for ones time just for this fantastic read!
My website: оргазм сквирт
sildenafil buy
Imagine Montenegro, a country where every
Bar Montenegro
looks as if it came from a painting.
Here you’ll find majestic mountains that rise above the turquoise waves of the Adriatic Sea,
creating landscapes that take your breath away. Stroll along the streets of
Montenegro
, where history comes alive at every turn and every street corner hides its mystery. And Montenegro’s beaches are the pure embodiment of paradisiacal pleasure, with their golden sand and warm, inviting sea.
Montenegro it the perfect place for those who want to relax and enjoy life to the full.
mexican mail order pharmacies pharmacies in mexico that ship to usa medicine in mexico pharmacies
generic of viagra
dominicandesign.net
Автоматические весы непрерывного действия по выгодным ценам. Быстрая доставка весы конвейерные
Biscotti is the primary Tv Cam to function dual band, dual antennas and Multiple In/Multiple Out (MIMO) expertise for powerful, HD-prepared Wi-Fi. Technology and society · The geocache and most of its contents have been ultimately destroyed by a lawn mower; the can of beans was the only item salvaged and was turned into a trackable merchandise referred to as the “Original Can of Beans”. Another geocache and plaque called the unique Stash Tribute Plaque now sit at the site. A Letterbox cache or a Letterbox hybrid cache is a mixture of a geocache and a letterbox in the same container. A conventional cache is the commonest sort and consists of a container with a logbook. A typical cache is a small waterproof container containing a logbook and generally a pen or pencil. An Offset cache is a multi-cache in which the initial coordinates are for a location containing information that encodes the final cache coordinates. Different platforms usually have their very own guidelines on which types are allowed or how they’re categorized.
leeds-welcome.com
mexican mail order pharmacies buying prescription drugs in mexico online mexican pharmaceuticals online
https://visa-v-uk.ru/
mexico drug stores pharmacies buying prescription drugs in mexico medication from mexico pharmacy
Sildenafil 25mg
Bonos y codigos promocionales 1win
1win es una plataforma de apuestas en linea reconocida por su compromiso de brindar a los jugadores una experiencia de juego unica y emocionante. Ya sea que te apasione el deporte, los juegos de casino o ambas opciones, 1win te ofrece una amplia gama de oportunidades para disfrutar y ganar.
Con bonificaciones y codigos promocionales exclusivos, 1 win se destaca como un destino lider para los entusiastas de las apuestas en linea. Desde bonos de bienvenida hasta promociones periodicas y ofertas exclusivas, descubriras como 1win se esfuerza por ofrecer a sus jugadores mexicanos oportunidades emocionantes para maximizar sus ganancias y ampliar su experiencia de juego.
Tipos de Bonificaciones en 1win
1win se destaca al ofrecer una amplia variedad de bonificaciones y promociones para satisfacer a jugadores de todas las preferencias:
Bonos de Bienvenida: Los nuevos jugadores son recibidos en 1win con un espectacular bono de bienvenida. Este bono se distribuye en los primeros cuatro depositos, lo que significa que tendras la oportunidad de aumentar significativamente tu saldo inicial. El bono de bienvenida puede alcanzar un impresionante 500% en total, con un limite de hasta 750 dolares.
Programa de Lealtad: En 1win, la lealtad de los jugadores es recompensada. El programa de lealtad de 1win ofrece a los jugadores la oportunidad de ascender en niveles y desbloquear recompensas exclusivas a medida que juegan mas y disfrutan de los juegos en la plataforma.
Cashback (Reembolso): El cashback es una caracteristica unica en 1win que te permite recibir un reembolso de una parte de tus perdidas en apuestas. Este beneficio es una forma de asegurarte de que, incluso si no tienes suerte en una apuesta en particular, aun obtendras algo a cambio.
Torneos: Los torneos en 1win anaden emocion adicional a tu experiencia de juego. Participar en torneos te brinda la oportunidad de competir con otros jugadores por premios en efectivo y otros premios emocionantes. Los torneos pueden abarcar una variedad de juegos, desde tragamonedas hasta apuestas deportivas, y ofrecen una oportunidad adicional para ganar.
Promociones con Codigos (Promocodes): Los codigos promocionales exclusivos son una caracteristica emocionante en 1win. Estos codigos pueden desbloquear bonificaciones adicionales, giros gratis y otras recompensas especiales.
En 1win, la diversidad de bonificaciones y promociones garantiza que siempre haya algo emocionante esperandote.
Como Aprovechar al Maximo las Bonificaciones
Las bonificaciones en 1win ofrecen una oportunidad excepcional para aumentar tus ganancias y prolongar tu experiencia de juego en linea. Una de las bonificaciones mas destacadas es el emocionante bono de bienvenida:
Registrate en 1win y proporciona informacion precisa y completa.
Realiza tu primer deposito, ya que el bono se distribuye en los primeros cuatro depositos.
Reclama tu bono, que se acreditara automaticamente en tu cuenta.
Cumple con los requisitos de apuesta, que indican la cantidad de dinero que debes apostar antes de retirar las ganancias.
Explora y juega en una amplia gama de juegos, como tragamonedas o apuestas deportivas, para aumentar tus posibilidades de ganar.
El bono de bienvenida en 1win es una emocionante ventaja para comenzar tu experiencia de juego en linea. Sigue estos pasos y disfruta al maximo de tu bono en una de las principales plataformas de apuestas en linea de Mexico.
Codigos Promocionales en 1win
Los codigos promocionales en 1win son una forma emocionante de aumentar tus oportunidades de ganar y aprovechar al maximo tu experiencia de juego. Estos codigos se pueden encontrar en varios lugares, lo que te brinda la posibilidad de desbloquear bonificaciones adicionales y ofertas exclusivas.
Muchos sitios web tematicos y portales dedicados a los juegos de azar ofrecen codigos promocionales de 1win. Estos codigos se actualizan regularmente y pueden proporcionarte bonificaciones unicas. Visita estos sitios y busca los codigos promocionales mas recientes.
Las redes sociales, como Facebook, Twitter e Instagram, son otra fuente donde puedes encontrar codigos promocionales. http://centroculturalrecoleta.org 1win a menudo publica codigos en sus perfiles sociales. Asegurate de seguir sus cuentas y estar atento a las publicaciones para no perderte ninguna oferta especial.
Si estas registrado en 1win y has aceptado recibir correos electronicos promocionales, es posible que recibas codigos promocionales exclusivos en tu bandeja de entrada. Estos codigos pueden ofrecer bonificaciones personalizadas segun tu historial de juego.
Una vez que tengas un codigo promocional, sigue estos sencillos pasos para activarlo:
Inicia sesion en tu cuenta de 1win.
Dirigete a la seccion de “Cuenta” o “Promociones” en tu perfil.
Ingresa el codigo promocional en el campo designado.
Confirma la activacion del codigo.
?Listo! Tu bonificacion se aplicara automaticamente a tu cuenta.
Asegurate de leer los terminos y condiciones asociados con cada codigo promocional para comprender completamente las bonificaciones y los requisitos de apuesta.
Beneficios de Utilizar Bonos y Codigos Promocionales
El uso de bonos y codigos promocionales en 1win ofrece una serie de beneficios que mejoran significativamente la experiencia de juego en linea:
Aumento del Saldo: Los bonos y codigos promocionales aumentan tu saldo, lo que te permite jugar mas y disfrutar de una mayor variedad de juegos sin invertir mas dinero de tu bolsillo.
Mas Oportunidades de Ganar: Con un saldo adicional, tienes mas oportunidades de ganar premios en efectivo y otros premios en los juegos de 1win. Esto aumenta la emocion y la diversion.
Menos Riesgo: Los bonos y codigos promocionales te permiten apostar con menos riesgo, ya que estas utilizando fondos de bonificacion. Esto significa que puedes probar nuevos juegos o estrategias sin preocuparte tanto por las perdidas.
Acceso a Ofertas Exclusivas: Al utilizar codigos promocionales, a menudo puedes acceder a ofertas exclusivas que no estan disponibles para otros jugadores. Estas ofertas pueden incluir giros gratis, bonos de recarga y mas.
Mayor Tiempo de Juego: Con mas fondos a tu disposicion, puedes disfrutar de una experiencia de juego mas prolongada, lo que agrega diversion y emocion a tu tiempo en 1win.
Exploracion de Juegos: Utilizar bonos y codigos promocionales te brinda la oportunidad de explorar nuevos juegos y actividades en el sitio sin incurrir en gastos adicionales.
En resumen, los bonos y codigos promocionales en 1win no solo te brindan beneficios tangibles en terminos de saldo adicional y oportunidades de ganar, sino que tambien mejoran tu experiencia de juego en general. Aprovecha estas ofertas especiales para disfrutar al maximo de tu tiempo en 1win y maximizar tus posibilidades de exito. Obten descuentos adicionales con un codigo descuento 1Win
1win es una plataforma de apuestas en linea que ofrece una amplia variedad de opciones de apuestas deportivas y juegos de casino. La pagina web es facil de navegar y tiene un diseno moderno y atractivo. En cuanto a las apuestas deportivas, 1win ofrece una amplia variedad de deportes para apostar, desde los mas populares como el futbol y el baloncesto hasta deportes menos conocidos como el badminton y el rugby. Ademas, la plataforma ofrece una gran cantidad de mercados de apuestas para cada evento deportivo, lo que permite a los usuarios personalizar sus apuestas de acuerdo a sus preferencias. En cuanto a los juegos de casino, 1win ofrece una amplia variedad de opciones, desde tragamonedas hasta juegos de mesa como el blackjack y la ruleta. Los juegos son de alta calidad y estan disenados por algunos de los principales proveedores de software de casino. La plataforma tambien ofrece una amplia variedad de metodos de pago, incluyendo tarjetas de credito, billeteras electronicas y criptomonedas. Ademas, el sitio web esta disponible en varios idiomas, lo que lo hace accesible para usuarios de todo el mundo. En general, 1win es una plataforma de apuestas en linea solida y confiable que ofrece una amplia variedad de opciones de apuestas deportivas y juegos de casino.
Codigo promocional 1Win son canjeados desde su registro y utilizados en los juegos. Aplica el codigo 937999 y recibe ganancias al apostar. El codigo de promocion 2024 te regala un paquete de bienvenida del 500% con los cuatro primeros depositos hasta $700 en apuestas deportivas y casino. El codigo 1win de bono debe ser ingresado en el formulario de registro.
Si esta buscando una forma de maximizar sus ganancias en apuestas deportivas, no se pierda el codigo de promocion y el bono de bienvenida 1Win en 024]. Con el codigo de promocion 1Win puedes recibir ofertas exclusivas y apuestas gratis para disfrutar aun mas de tus juegos favoritos. Ademas, el bono de bienvenida 1Win es una gran oportunidad para aumentar sus ganancias y tener una experiencia de apuestas aun mas emocionante.
Bonificacion 1win – 937999
Como activo el vale en 1win?
Durante el proceso de registro se introduce un codigo promocional de la casa de apuestas 1win. El campo “Anadir codigo promocional” estara disponible para cualquier metodo de creacion de cuenta que elija. Tenga en cuenta que este campo es opcional en la fase de registro, asi que tenga cuidado al introducirlo. Si se olvida de hacerlo al registrarse, no podra activar su codigo en 1win y el bono de bienvenida dejara de estar disponible.
Tendras que recargar tu cuenta para poder utilizar el codigo promocional en el futuro. Una vez que haya introducido el codigo promocional durante el registro, vaya a su gabinete personal a traves del icono de usuario y haga clic en “Depositar”. Tomemos como ejemplo el codigo promocional “937999”, que corresponde a 200 euros.
Caracteristicas del bono 1win
El codigo promocional es proporcionado por representantes de la oficina de la casa de apuestas 1win. Lo hacen en varias ocasiones: durante una promocion, un dia festivo importante, el cumpleanos de un usuario, para volver a captar a un jugador que ha estado jugando durante un tiempo y ha dejado de estar activo.
Si introdujiste un codigo promocional al registrarte, veras los fondos de bonificacion en cuanto inicies sesion en tu perfil. Y si te lo dieron personalmente, deberas aceptar participar en la promocion para poder utilizarlo. Estos fondos se abonan en tu cuenta de bonificacion, y podras ver el importe en tu perfil personal. Si respeta las normas de uso de los fondos de bonificacion, podra convertirlos gradualmente en dinero en efectivo, que recibira ademas de sus ganancias.
?Que tan confiable es apostar en 1win?
Apostar en 1win es 100% confiable. 1win nacio en 2016, con el nombre de MFI Investments Limited, quienes estan registrados con el numero de licencia 8048/JAZ2018-040, otorgada por la Comision de Juegos eGaming.
Ademas, cuenta con alianzas comerciales con diferentes equipos y ligas, como la UEFA, UFC, NHL, FIFA y mas.
8. Opiniones 1win Casino 2024
1win casino es una excelente opcion para comenzar a apostar, ademas de que cuentas con el regalo para registrarte con el codigo promocional 937999. Podras tener tu cuenta abierta en todos lados, tu celular y tu computadora tendran tu cuenta sincronizada.
Es un sitio seguro, con numero de registro y sistemas de pago legales afiliados. Podras apostar con cualquier metodo de pago en mas de 50 deportes diferentes y cientos de juegos de casino. 1win es recomendable y esta lleno de diversion.
9. FAQ: 1win Codigo Promocional
9.1 ?? ?1win es un sitio seguro?
1win es un sitio seguro, esta avalado por la comision de juego eGaming. Sus metodos de pago son conocidos y de fiar, cada uno de ellos. Ademas, tambien de tener soporte tecnico las 24 horas ante cualquier duda.
9.2 ?? ?Hay bono de bienvenida de 1win?
Si existe, y para obtener este bono de bienvenida de 1win, necesitaras el codigo de bienvenida 937999, tendras que registrarte en 1win con este codigo y realizar tu primer deposito.
9.3 ?? ?Cual es el codigo de bono 1win?
El codigo promocional 1win es 937999, registrate y comienza a disfrutar de tu bono.
Демонтаж, разборка и снос старых частных домов с вывозом мусора в Москве и Подмосковье под ключ. Стоимость сноса дома – здесь подробнее об услуге: 1ecenter.ru. Демонтируем дома, здания, строения и фундаменты вручную и спецтехникой по ценам ниже рынка за 24 часа. Бесплатный выезд инженера на объект.
reputable mexican pharmacies online mexico drug stores pharmacies buying prescription drugs in mexico online
generic of viagra
LГҐn 90000
Зухвала енергія пін ап
пінап автомати https://pinupcasinoqgcvbisd.kiev.ua/ .
sildenafil tablets
mexico drug stores pharmacies mexico pharmacy buying from online mexican pharmacy
Промокод при регистрации в 1xbet сегодня. Этой акцией может воспользоваться каждый новый клиент при регистрации на сайте букмекера. Это ваше преимущество со старта, и у 1xbet есть эксклюзивное предложение. как получить промокод 1хбет. В форме регистрации есть всего одно необязательное поле — как раз для ввода промокода. Как получить промокод на бесплатную ставку. Магазин находится во вкладке xBonus (в перечне вкладок верхнего блока). Вам предложат несколько вариантов для обмена баллов на промокоды 1xbet kz. Код можно получить для ставки ординар, для ставки экспресс, а также для лотерей от «1хБет». На сегодня промокод 1xbet бесплатно найти можно без особых затрат энергии, при этом сделать это следующим образом: Путем поиска в сети интернет; На сайтах, специализирующихся на спортивных ставках (Не ресурсы БК); В официальных сообществах 1хБет (соцсети). Представители БК часто выкладывают в группах или же просто в сети промокоды на 1xbet бесплатно в честь какого-то праздника либо же грядущего крупного спортивного турнира. Все промокоды 1xbet 2024. На официальном сайте букмекера в соответствующей рубрике находится полный перечень промокодов 1xbet 2024, бесплатно получить которые можно обменяв на них бонусные баллы.
mexican pharmacy best online pharmacies in mexico mexican pharmaceuticals online
mexican pharmaceuticals online mexican online pharmacies prescription drugs mexican online pharmacies prescription drugs
non prescription viagra
porn
purple pharmacy mexico price list reputable mexican pharmacies online mexico pharmacy
buying viagra online forum
birminghamnews24.com
gocanadanews.com
sildenafil online
mexico drug stores pharmacies mexican drugstore online mexico drug stores pharmacies
buying from online mexican pharmacy mexican online pharmacies prescription drugs mexico drug stores pharmacies
Обратившись к нам, Вы получите честную юридически оформленную сделку, что является важным критерием при продаже недвижимости. Мы не являемся посредниками и выкупаем квартиры за собственные деньги.
срочный выкуп недвижимости спб
sildenafil viagra
Melbet Promo Code
GAME888
MelBet Promotion 2024: Unlock Exclusive Benefits with Bonus Codes, Registration Bonuses, Free Bet Bonuses, and Cashback Offers!
Melbet promo code 2024 : GAME888 use this code, you can enjoy a 100% sports bonus of up to 130€/$ and a casino bonus of up to €1750, along with 290 free spins. To take advantage of this offer, make sure to enter the promo code when registering for a new player account with Melbet. While Melbet primarily focuses on sports betting, they also provide a variety of arcade and casino games. The sportsbook caters to an international audience with its website available in 30 different languages. However, it’s worth noting that customer support is not available in as many languages. Take a look at our review to learn more about the exciting welcome package offered by Melbet.
Newcomers have the opportunity to utilize the MelBet promotional code in order to avail themselves of the initial welcome bonus and first deposit offers. In addition to these enticing offers, this betting platform also provides various other promotions such as weekly free bets, refund offers, and casino bonuses, some of which may require a promo code.
If you are uncertain, it is advisable to use the bonus code to ensure that you can take advantage of these offers. Our dedicated team will ensure that you stay informed about the most up-to-date promotions and will notify you when and where a code is necessary. For now, let us concentrate on how you can obtain the latest sign-up bonus.
MelBet promo code “GAME888” Use the bonus code and receive an enhanced bonus of 130€/$ for sports betting. Every new player will receive from Melbet: a welcome bonus of 130$, as well as a lifelong free bet of 30$ and 130% on every account replenishment.
To create an account at Melbet, individuals must be at least 18 years old. The registration procedure is straightforward and can be completed within a few minutes. Here is a step-by-step guide:
1. Visit the main Melbet website and click on the ‘Registration’ option.
2. Choose one of the four registration options:
a) Register by providing your email address, country, name, preferred currency, password, and the bonus you wish to avail.
b) Register using your phone number, preferred currency, and bonus.
c) Opt for the one-click registration by selecting your country, preferred currency, and bonus.
d) Register through a social network by selecting the desired social network and currency.
3. If you have a Melbet Promo Code, enter it in the ‘Promo Code’ tab to activate any available bonuses.
4. Complete the registration process by clicking on the ‘Register’ button.
Melbet promo code today: “GAME888”. Use the bonus code to increase the bonus amount by 130% for the first deposit. The standard bonus is $100, but if you use the Melbet promo code, you will receive an enhanced bonus of $130 upon registration. Simply enter the Melbet promo code during registration and you will receive up to 100% of your first deposit. This attractive offer is designed to attract new users to the platform.
Melbet bookmaker actively utilizes various methods and approaches to motivate players. One of the most effective assets that can increase users’ interest in the bookmaker’s services is its bonus program.
By offering diverse bonuses at different stages of the gaming process, players gain advantages and more favorable conditions for placing bets. The company’s audience of fans grows thanks to interesting promotions and generous bonuses.
In addition to the main promotions, Melbet also actively operates a promo code system. It is through these promo codes that players gain additional preferences, which can significantly enhance their gaming potential.
The main format of bonuses provided to new clients through promo codes is additional bonus funds. The size of the additional bonus amount is 100% of the welcome bonus received by the new client. These additional bonuses must be wagered within a specified period and on specific terms.
Melbet Registration Promo Code:https://transparencyinteaching.com/art/kak_pravilyno_stroity_otnosheniya_s_mughchinoy.html Newly registered players on Melbet can avail a welcome bonus of a 100% deposit bonus up to 130€/$.
18+ | Responsible Gambling | Terms and Conditions | For new customers only | The promotional code is valid until December 31, 2024.
Promo code for Melbet: GAME888, and it offers a msz welcome bonus of a 100% deposit bonus up to 130€/$. By using the bonus codes provided by Melbet, you can enjoy various benefits such as free bets, deposit bonuses, free spins, and more. The Melbet bonus 2024 provides numerous opportunities to enhance your betting experience. In summary, Melbet allows you to receive up to 130$ to wager on sports like cricket, soccer, and many others.
When signing up, there are four different ways to create your Melbet account. These methods include:
1. Registering with your mobile number.
2. Creating an account using your email address.
3. Signing up via social media platforms.
4. Opting for the quick ‘One Click’ method, which allows for instant registration with just one click of a button.
For each of these options, there is a corresponding box where you can select the desired welcome bonus. The available choices are as follows:
1. No bonus preference.
2. 100% sports bonus up to €100 (use the promo code to receive up to €130).
3. Casino bonus up to €1750 + 290 free spins.
Once you have chosen your preferred offer, proceed to the banking page to make your initial deposit.
MelBet promo code: GAME888 allows you to unlock a vip welcome bonus of 100% up to €/$130 when you enter it during the registration process. Additionally, by using this promo code, you can also enjoy the Melbet Casino Bonus, which offers up to $/€1750 in bonus funds along with an exciting 290 Free Spins. New players: When registering an account, use the promo code Melbet “GAME888” to receive a welcome bonus.
Melbet offers a wide variety of games and casino options for its customers. In this article, we will explore each section in detail.
One of the standout features of Melbet is its diverse range of sports selections. Players can choose from over 40 different sports, and to access all of them, don’t forget to use our Melbet promo code. Cricket, being the most popular sport in India, is given special attention with a specialized section for Indian players. You will find a plethora of markets available for various sports, including 1X2, Totals, Individual Total Runs, and Individual Total Runs Even/Odd for cricket.
In addition to cricket, Melbet also offers a wide range of markets for other popular sports such as football, tennis, basketball, and ice hockey. You will also find special options like eSports and racing sports, including horse racing and greyhounds.
Melbet truly caters to the diverse interests of its customers, providing a comprehensive platform for sports and games.
mexican drugstore online mexican online pharmacies prescription drugs п»їbest mexican online pharmacies
mexico pharmacies prescription drugs buying prescription drugs in mexico mexico pharmacy
купить диплом бакалавра https://landik-diploms.com/ .
buying sildenafil citrate online
https://skupka-stiralnyh-mashin.ru/
chloromycetin 250mg
cheap viagra 50mg
reputable mexican pharmacies online mexico drug stores pharmacies purple pharmacy mexico price list
Kudos. I like this!
sildenafil viagra
Utilisation du code promo 1xbet senegal lors de votre inscription, vous pouvez obtenir un bonus de bienvenue pour un nouveau client d’un montant allant jusqu’a 130?/$, ce qui vous donnera un bon depart dans vos paris sportifs en ligne. Grace a la publicite sur le portail de jeux 1xbet lui-meme et aux publications sur les ressources thematiques et partenaires, de nombreuses personnes connaissent le bonus d’inscription. A bien des egards, c’est grace a lui que le nombre de clients des bookmakers ne cesse de croitre. C’est grace a ce type de bonus que les joueurs disposent d’un montant substantiel qui peut etre depense en paris. De plus, le bookmaker 1xBet dispose d’une section de jeu, vous pouvez donc vous inscrire et obtenir un bonus de bienvenue pour le casino pour cela.
medication from mexico pharmacy mexico drug stores pharmacies mexico drug stores pharmacies
buying from online mexican pharmacy mexican mail order pharmacies mexico pharmacies prescription drugs
Viagra 130mg
В данной статье рассматривается тема рейтинга лучших узких стиральных машин, что представляет интерес для многих потребителей, стремящихся найти оптимальное решение для компактной стирки в своем доме https://luchshie-uzkie-stiralnye-mashiny.ru/modeli-whirlpool
В данной статье рассматривается тема рейтинга лучших узких стиральных машин, что представляет интерес для многих потребителей, стремящихся найти оптимальное решение для компактной стирки в своем доме https://luchshie-uzkie-stiralnye-mashiny.ru/s-frontalnoy-zagruzkoy
tube
pharmacies in mexico that ship to usa mexico drug stores pharmacies mexican online pharmacies prescription drugs
sildenafil generic
Major thanks for the article post. Much thanks again.
My website: очень болезненный анал
medication from mexico pharmacy mexican online pharmacies prescription drugs pharmacies in mexico that ship to usa
holidaynewsletters.com
214rentals.com
buying prescription drugs in mexico pharmacies in mexico that ship to usa mexico drug stores pharmacies
Подберем лизинг на выгодных условиях, поможем сэкономить деньги и отправить заявку сразу в несколько банков без лишних документов лизинг
Melbet Promo Code
GAME888
MelBet Promotion 2024: Unlock Exclusive Benefits with Bonus Codes, Registration Bonuses, Free Bet Bonuses, and Cashback Offers!
Melbet promo code 2024 : GAME888 use this code, you can enjoy a 100% sports bonus of up to 130€/$ and a casino bonus of up to €1750, along with 290 free spins. To take advantage of this offer, make sure to enter the promo code when registering for a new player account with Melbet. While Melbet primarily focuses on sports betting, they also provide a variety of arcade and casino games. The sportsbook caters to an international audience with its website available in 30 different languages. However, it’s worth noting that customer support is not available in as many languages. Take a look at our review to learn more about the exciting welcome package offered by Melbet.
Newcomers have the opportunity to utilize the MelBet promotional code in order to avail themselves of the initial welcome bonus and first deposit offers. In addition to these enticing offers, this betting platform also provides various other promotions such as weekly free bets, refund offers, and casino bonuses, some of which may require a promo code.
If you are uncertain, it is advisable to use the bonus code to ensure that you can take advantage of these offers. Our dedicated team will ensure that you stay informed about the most up-to-date promotions and will notify you when and where a code is necessary. For now, let us concentrate on how you can obtain the latest sign-up bonus.
MelBet promo code “GAME888” Use the bonus code and receive an enhanced bonus of 130€/$ for sports betting. Every new player will receive from Melbet: a welcome bonus of 130$, as well as a lifelong free bet of 30$ and 130% on every account replenishment.
To create an account at Melbet, individuals must be at least 18 years old. The registration procedure is straightforward and can be completed within a few minutes. Here is a step-by-step guide:
1. Visit the main Melbet website and click on the ‘Registration’ option.
2. Choose one of the four registration options:
a) Register by providing your email address, country, name, preferred currency, password, and the bonus you wish to avail.
b) Register using your phone number, preferred currency, and bonus.
c) Opt for the one-click registration by selecting your country, preferred currency, and bonus.
d) Register through a social network by selecting the desired social network and currency.
3. If you have a Melbet Promo Code, enter it in the ‘Promo Code’ tab to activate any available bonuses.
4. Complete the registration process by clicking on the ‘Register’ button.
Melbet promo code today: “GAME888”. Use the bonus code to increase the bonus amount by 130% for the first deposit. The standard bonus is $100, but if you use the Melbet promo code, you will receive an enhanced bonus of $130 upon registration. Simply enter the Melbet promo code during registration and you will receive up to 100% of your first deposit. This attractive offer is designed to attract new users to the platform.
Melbet bookmaker actively utilizes various methods and approaches to motivate players. One of the most effective assets that can increase users’ interest in the bookmaker’s services is its bonus program.
By offering diverse bonuses at different stages of the gaming process, players gain advantages and more favorable conditions for placing bets. The company’s audience of fans grows thanks to interesting promotions and generous bonuses.
In addition to the main promotions, Melbet also actively operates a promo code system. It is through these promo codes that players gain additional preferences, which can significantly enhance their gaming potential.
The main format of bonuses provided to new clients through promo codes is additional bonus funds. The size of the additional bonus amount is 100% of the welcome bonus received by the new client. These additional bonuses must be wagered within a specified period and on specific terms.
Melbet Registration Promo Code: melbet casino bonus ohne einzahlung Newly registered players on Melbet can avail a welcome bonus of a 100% deposit bonus up to 130€/$.
18+ | Responsible Gambling | Terms and Conditions | For new customers only | The promotional code is valid until December 31, 2024.
Promo code for Melbet: GAME888, and it offers a msz welcome bonus of a 100% deposit bonus up to 130€/$. By using the bonus codes provided by Melbet, you can enjoy various benefits such as free bets, deposit bonuses, free spins, and more. The Melbet bonus 2024 provides numerous opportunities to enhance your betting experience. In summary, Melbet allows you to receive up to 130$ to wager on sports like cricket, soccer, and many others.
When signing up, there are four different ways to create your Melbet account. These methods include:
1. Registering with your mobile number.
2. Creating an account using your email address.
3. Signing up via social media platforms.
4. Opting for the quick ‘One Click’ method, which allows for instant registration with just one click of a button.
For each of these options, there is a corresponding box where you can select the desired welcome bonus. The available choices are as follows:
1. No bonus preference.
2. 100% sports bonus up to €100 (use the promo code to receive up to €130).
3. Casino bonus up to €1750 + 290 free spins.
Once you have chosen your preferred offer, proceed to the banking page to make your initial deposit.
MelBet promo code: GAME888 allows you to unlock a vip welcome bonus of 100% up to €/$130 when you enter it during the registration process. Additionally, by using this promo code, you can also enjoy the Melbet Casino Bonus, which offers up to $/€1750 in bonus funds along with an exciting 290 Free Spins. New players: When registering an account, use the promo code Melbet “GAME888” to receive a welcome bonus.
Melbet offers a wide variety of games and casino options for its customers. In this article, we will explore each section in detail.
One of the standout features of Melbet is its diverse range of sports selections. Players can choose from over 40 different sports, and to access all of them, don’t forget to use our Melbet promo code. Cricket, being the most popular sport in India, is given special attention with a specialized section for Indian players. You will find a plethora of markets available for various sports, including 1X2, Totals, Individual Total Runs, and Individual Total Runs Even/Odd for cricket.
In addition to cricket, Melbet also offers a wide range of markets for other popular sports such as football, tennis, basketball, and ice hockey. You will also find special options like eSports and racing sports, including horse racing and greyhounds.
Melbet truly caters to the diverse interests of its customers, providing a comprehensive platform for sports and games.
Демонтаж, разбор и снос старых деревянных и кирпичиных домов с вывозом мусора в Москве и других городах Подмосковья под ключ. Снос дачного дома с вывозом цена – узнайте больше об услуге: orenvito.ru. Демонтируем дома, сносим здания, строения, сооружения и фундаменты вручную и спецтехникой по ценам ниже рынка за 24 часа. Бесплатный выезд инженера на объект.
look here
https://www.natura.md/buchetul-de-crini-albi
http://zhkhcontrol39.ru
http://mbasystem.ru
помощь юриста по алиментам
buying prescription drugs in mexico online mexico drug stores pharmacies buying from online mexican pharmacy
лучшие юристы москвы по жилищным вопросам
pharmacies in mexico that ship to usa mexican rx online mexican rx online
viagra prescription cost
юрист в сфере гражданского права
юридические услуги по жилищным спорам
нанять юриста по алиментам
услуги юриста по гражданским делам москва
адвокат представитель по гражданским делам
юрист по алиментам цена в москве
бесплатная консультация по поводу алиментов
Это просто бесподобная тема 🙂
Note: To find out more about us http://www.ag-ebersberger.de/index.php/gaestebuch?50 analysts, move to page “about portal” and scroll down to the section about to the prisoner team.
porn 365tube
buying prescription drugs in mexico mexican pharmacy best online pharmacies in mexico
mexican pharmacy mexican mail order pharmacies medication from mexico pharmacy
analitica.pt – Bonus VIP jusqu’a 130 ?/$ Offer Offre de bienvenue. 18 Les conditions generales s’appliquent. Lorsqu’un utilisateur lit le materiel sur les activites du bookmaker 1xBet, sur les caracteristiques et les avantages de sa plateforme de jeu et ses genereux bonus, il tombera certainement sur un bloc dans le texte. Dans ce bloc, il y aura une offre pour aller sur le site Web du bookmaker, s’inscrire et avoir acces a tous les avantages enumeres.
Viagra 200mg
tsrrub.com
Jiao Fang이 여기에서 사람들을 막았다는 소식을 듣고 Fang Jifan은 이미 분노했습니다.
Viagra 120mg
https://skupka-stiralnyh-mashin.ru/
mexican mail order pharmacies mexican mail order pharmacies mexico pharmacies prescription drugs
https://visa-v-uk.ru/
prices for viagra
angliannews.com
texasnews365.com
mexican drugstore online mexican mail order pharmacies mexico pharmacies prescription drugs
sildenafil citrate over the counter
buy viagra in mexico
Visa в англию можно найти здесь
https://visa-v-uk.ru/
Ресторанное оборудование в лизинг по выгодной цене. Большой выбор оборудования для общепита, HORECA, кафе, ресторана, бара, пиццерии, кофейни, столовой лизинг полиграфического оборудования
Ресторанное оборудование в лизинг по выгодной цене. Большой выбор оборудования для общепита, HORECA, кафе, ресторана, бара, пиццерии, кофейни, столовой оборудование для ресторана в лизинг
medication from mexico pharmacy buying prescription drugs in mexico mexico pharmacy
Промокод 1xBet 2024 (Бонус при Регистрации 32500 RUB)
Промокод 1xBet 2024 – 1XFREE777, новые пользователи букмекерской компании могут воспользоваться приветственным бонусом в размере 100% от суммы депозита до 32 500 рублей (или эквивалентную сумму в другой валюте €100). Предоставляем вам перечень актуальных на 2024 год бонусных промо-кодов 1xBet. Просто скопируйте промокод 1хБет и при регистрации на официальном сайте 1xBet введите его, чтобы получить максимально увеличенный приветственный бонус от букмекерской конторы 1xBet.
1xBet Промокод – 1XFREE777
Актуальные промокоды для 1хБет ? Акция 2024 ? Бонус коды ? Фрибет Бонусы за регистрацию ? Программа лояльности ? Кэшбэк!
Промокод 1xBet при регистрации – это 1XFREE777. Только с помощью него вы получите бонус в размере 100% до 32500 рублей. Все остальные коды не действительны и не предоставляют такого бонуса. Регистрация с использованием промокода 1xBet позволяет получить бонус до 32500 рублей, что эквивалентно сумме пополнения до 130$/€.
Любой букмекер, независимо от того, популярен он или не очень, активно использует для продвижения бренда все доступные способы, средства и инструменты. Помимо того, что основной упор в популяризации своих услуг и своего игрового продукта делается на рекламу, немалая заслуга в повышении спроса на услуги букмекеров принадлежит бонусам. Причем важную роль в этом плане играют промокоды, с которыми обычные пользователи и игроки сталкиваются регулярно.
Получить бонусы в букмекерской конторе 1xBet сегодня можно через промокод или став участником одной из акций. Предложения доступны каждому, как новичкам, так и игрокам со стажем.
Давайте разберемся в тонкостях бонусной программы букмекера 1xbet. Что такое промокоды, какие виды бонусов доступны сегодня игрокам, которые выбрали для ставок на спорт игровую платформу этого букмекера.
Промокод 1xBet – 1XFREE777. Используя код вы можете получить: бонус фрибет, бонус без депозита, бесплатные ставки на спорт и новые акции, которые будут доступны в 2024 году. Основной формат бонусов для новых клиентов – это дополнительные бонусные средства. Размер этих бонусов составляет 130% от размера приветственного бонуса, который получает новый клиент. Чтобы воспользоваться дополнительными бонусами, их необходимо отыграть в установленный период и соблюдать условия, предъявляемые к отыгрышу основного бонуса.
Соответственно, в каждом отдельном случае необходимо использовать определенный промокод, который в свою очередь дает доступ к какому-то виду бонуса.
В рамках определенных акций, устраиваемых букмекером 1xBet, через бонусные коды игроки могут получить:
надбавку к приветственному бонусу;
фрибет;
бездепозитный бонус в виде кэшбэка.
Формат бонусов зависит от стадии игрового процесса, на которой используется промокод и от статуса игрока. Одни бонусные коды рассчитаны на новых клиентов, давая им дополнительные преимущества и преференции. Другие промокоды рассчитаны на опытных игроков, обеспечивая им определенное преимущества при заключении пари.
Ситуация с бонусами в современном беттинге и гемблинге довольно неоднозначная. Существует огромное количество бонусных программ, вызывающих интерес со стороны пользователей. Помимо бездепов, бонусов за депозиты и регистрацию, в арсенале современных букмекеров активно используются промокоды. Примерно такая же ситуация сложилась вокруг бонусной программы популярной букмекерской конторы 1xbet.
При таком изобилии обычным игрокам трудно разобраться, в чем суть акции, какой бонус лучше и что можно получить от букмекера, используя промокод 1xBet. Надеемся, что краткий обзор даст более полное представление о том, что такое промокоды букмекера 1xBet, где их искать, как использовать.
Промокод 1хБет – kuzov-auto.ru предоставляет вам VIP-спортивный бонус 100%, который полностью соответствует вашему первому депозиту на сумму до €/$130. Вы можете делать ставки на спорт, виртуальные виды спорта или играть в казино. Это предложение действительно на протяжении всего 2024 года.
Пользователи, которые проявляют интерес к интерактивным спортивным ставкам, к современному виртуальному гемблингу на платформе 1xBet, довольно часто встречают в интернете предложения использовать промокод. Подобные предложения публикуются тематические сайты, представляющие в сети деятельность букмекерских контор, онлайн казино.
Именно через такие источники и распространяются промокоды.
Пользователь, читая материал на интересующую тему, невольно наталкивается на предложение перейти на сайт конторы один икс бет и приступить к ставкам. Однако подобное предложение включает в себя и мотивацию. Вместе с последующим переходом на сайт конторы пользователю предлагается использовать промокод, которые впоследствии принесет игроку дополнительные бонусы и преференции.
Предложение использовать промокод бесплатное. Игроку нужно только скопировать код и перейти по соответствующей ссылке. Если код актуальный, игрок получит в дальнейшем какие-то бонусы.
Такие предложения в интернете публикуются регулярно. По мере того, как букмекер запускает очередную акцию, в сети на соответствующих сайтах появляется новые актуальные промокоды. Букмекер не занимается распространением бонусных кодов. Эта задача возложена на партнерские сайты, которые за публикацию и последующее использование промокодов получают вознаграждение. Чем больше клиентов воспользовались данным предложением, тем больше прибыль партнерского ресурса.
Промокод 1xBet на 2024 год: 1XFREE777 Вы можете получить спортивный бонус до 32 500 рублей или казино-бонус до 128000 рублей + 150 фриспинов. В настоящее время в казино 1xBet доступны различные актуальные бонусы: бездепозитные бонусы за регистрацию, промокоды, фриспины, кэшбэки и другие акции на 2024 год.
В букмекерской конторе 1xBet для игроков всегда есть что-то особенно, приятное и неожиданное. Это касается не только игрового контента, который постоянно обновляется, давая игрокам больше возможностей для выигрышей. Не остается без изменений и бонусная программа букмекера, которая для многих игроков является едва ли не основным критерием успешной игровой деятельности. Ассортимент бонусной программы 1 икс Бет впечатляет. Это и приветственный бонус, и депозитные бонусы и промокоды 1xBet. Одним словом, интересных предложений предостаточно. Остается только сделать правильный выбор.
Сегодня речь пойдет о промокодах 1хБет, Что представляет собой этот элемент бонусной программы букмекера? Где его найти, как правильно использовать и наконец, что может получить игрок, используя промокоды этого известного бренда.
female ed meds
porn download
Discover luxurious and affordable villas for sale in Tilal Al Ghaf villas for sale Developed by the renowned Majid Al Futtaim, these stunning units showcase unmatched quality and offer irresistible prices. Explore your dream home in this exclusive haven today!
best online pharmacies in mexico mexico drug stores pharmacies buying prescription drugs in mexico
ed pills for sale
Exclusive residences at Sobha Hartland2 in MBR City. Plunge into a wonderful Odyssey in the innovative eco-community from Sobha Reality and start a new, grandiose chapter of your life.
Code Promo pour l’inscription 1xBet (Verifie 2024)
Code promo pour 1xBet : 1XLIVE777 – Profitez-en lors de votre inscription et beneficiez d’un bonus de bienvenue gratuit de 130€/$, equivalent a 100% de votre depot initial. Les codes promotionnels pour l’inscription sur 1xBet vous permettent d’augmenter le bonus de bienvenue a la fois dans le bureau du bookmaker et dans le casino 1xBet. Voici une compilation des derniers codes promo 1xBet pour l’annee 2024.
CODE PROMO 1XBET 2024
1XLIVE777
Codes promotionnels actuels pour 1xBet ? Action 2024 ? Codes bonus ? Bonus de pari gratuit pour l’inscription.
Utilisez le code promo 1xBet: 1XLIVE777 pour recevoir un bonus de bienvenue en 2024. Les nouveaux joueurs seront eligibles a un bonus VIP de 200% jusqu’a 130€/$. Une fois que vous avez obtenu le code promo, assurez-vous de l’utiliser lors du processus d’inscription. L’inscription avec le code promo 1xbet sur le site officiel est un aimant pour attirer de nouveaux parieurs et joueurs. Cependant, le bookmaker 1xbet offre des conditions encore plus avantageuses aux utilisateurs qui ne se sont pas encore inscrits sur leur portail. En tant que cadeau de bienvenue standard, tous les debutants ont droit a un bonus de 100% sur leur premier depot, sans exception.
Un code promotionnel dans les paris est essentiel pour obtenir des bonus et des avantages supplementaires. Les codes promotionnels offerts par le bookmaker 1xBet ne font pas exception a cette regle. Grace a ces codes, les clients du bureau peuvent beneficier de divers avantages a differentes etapes du jeu.
Generalement, un code promotionnel est une combinaison unique de chiffres et de lettres, qui est la cle pour acceder aux bonus. Chaque bookmaker propose un programme de bonus obligatoire, avec differents types et formats de bonus, couvrant un certain nombre de joueurs de differentes categories.
Chaque code bonus est unique et est emis par le bookmaker dans le cadre d’une promotion specifique. Selon les termes de la promotion, l’utilisation d’un tel code offre aux joueurs certains avantages. Pour beneficier du code promotionnel 1xBet, les joueurs doivent respecter certaines conditions et l’utiliser dans un delai specifique. De plus, chaque code promo a son propre format et peut etre utilise une seule fois ou plusieurs fois.
Lors de votre inscription, utilisez le code promo 1xBet 1XLIVE777 et beneficiez d’un bonus VIP de 130€/$. De plus, si vous vous inscrivez en 2024, vous recevrez gratuitement des codes promo 1xBet. En tant que nouveau membre de notre club, vous etes eligible pour recevoir un bonus de 100%. Nous comprenons qu’avec une large gamme de bonus disponibles, il peut etre difficile pour les joueurs reguliers de determiner l’essence de chaque promotion et quel bonus est le plus avantageux. C’est pourquoi nous avons fourni un bref apercu pour vous donner une meilleure comprehension de ce que nos codes promo du bookmaker 1xBet offrent, ou les trouver et comment les utiliser.
Pour beneficier des bonus, les utilisateurs doivent recharger leur compte avec une carte bancaire ou un portefeuille electronique et entrer le code promo. Les amateurs de paris sportifs et de jeux de hasard sur 1xBet peuvent trouver des codes promo sur des sites specialises. Ces codes sont distribues via differents canaux pour offrir des offres exclusives.
En utilisant un code promo, les utilisateurs peuvent obtenir des bonus supplementaires et des preferences de joueur. Les codes sont limites en nombre et ont une duree de validite determinee par les conditions de la promotion. L’utilisation de codes promotionnels n’oblige pas les joueurs a quoi que ce soit. Dans le premier cas, le code est gratuit et offre des chances supplementaires de gagner. Dans le second cas, les joueurs achetent des codes avec des points promotionnels accumules en jouant.
Comment Utiliser un Code Promo 1xBet
bonus de bienvenue 1xbet : 1XLIVE777 – Profitez d’une offre de bienvenue de 100% jusqu’a 130€/$. Ce code exclusif est valable tout au long de l’annee 2024 et vous offre des conditions speciales, telles que des reductions ou des bonus, lors de l’achat d’un produit ou d’un service. Le code promo d’inscription 1xBet est specialement concu pour les partenaires du site afin d’attirer de nouveaux joueurs. Le meilleur ? C’est totalement gratuit a utiliser ! Il vous suffit de copier le code et de cliquer sur le lien fourni. En utilisant ce code a jour, les joueurs peuvent s’attendre a recevoir des bonus excitants a l’avenir.
Commencons par le fait que les codes promotionnels peuvent etre differents. Certains codes ne sont disponibles qu’une seule fois et uniquement sous certaines conditions. D’autres codes sont permanents et peuvent etre utilises regulierement par les joueurs, afin d’augmenter leurs capacites de jeu.
Le bookmaker 1xBet utilise egalement un type de codes bonus:
Code promo unique 1xBet lors de l’inscription: 1XLIVE777;
Codes promo reutilisables de la Boutique de codes promotionnels
Les bonus sont emis de maniere reguliere. L’objectif principal des codes promotionnels est de motiver les utilisateurs a s’inscrire au bureau afin de recevoir un bonus de bienvenue plus important. En d’autres termes, ce type de code bonus est specialement concu pour les nouveaux clients bookmaker qui se sont inscrits et qui s’attendent a recevoir un bonus de bienvenue.
Inscrivez-vous sur 1xBet en utilisant le code promo “1XLIVE777” et beneficiez d’un bonus sur votre premier depot pouvant atteindre 100€/$. Ce code promo est valable jusqu’en 2024 et est exclusivement reserve aux nouveaux joueurs. En utilisant le code, vous pouvez profiter d’un bonus augmente de 100%. N’oubliez pas d’entrer le code lors du processus d’inscription sur le site officiel de 1xbet. Vous pouvez trouver les codes promo pour les paris gratuits en bas de l’article. Choisissez l’un des codes promo disponibles pour aujourd’hui. Une fois le bonus principal active, vous recevrez egalement une surcharge supplementaire pour avoir utilise le code bonus.
Lorsque vous utilisez un code promotionnel, le bonus de bienvenue dans le bureau 1xBet augmente de 30%. Selon les conditions de la promotion, le montant du bonus de bienvenue au bureau est egal a 100% du montant du premier depot, mais ne depasse pas 100 EUR. Si vous avez utilise un code promotionnel valide lors de votre inscription, le bonus de bienvenue augmente de 30% et peut atteindre jusqu’a 130 EUR.
Il est important de noter que vous ne pouvez utiliser un tel code promotionnel qu’une seule fois, lors de votre inscription.
Dans aucune autre situation, un tel code bonus ne peut etre applique.
Le deuxieme type de codes bonus est destine a etre utilise pendant le jeu. Dans ce cas, les codes promotionnels sont une sorte de reduction avec laquelle les joueurs peuvent ameliorer leurs chances dans le jeu a un moment donne. Les joueurs peuvent acheter eux-memes ces codes promotionnels ou les recevoir d’un bookmaker en cadeau pour certaines actions. Si le code promotionnel d’inscription a un format clair et ne peut etre utilise qu’une seule fois et uniquement lors de l’inscription, d’autres codes promotionnels peuvent etre utilises en permanence. Leur utilisation est etroitement liee au gameplay.
Par exemple! Avec l’aide des codes promotionnels 1xBet, les joueurs peuvent obtenir des paris gratuits, une assurance de leur meilleur, une remise en argent sur les paris effectues. Il existe egalement une categorie distincte de codes promotionnels utilises pour les jeux d’argent sur le portail de jeux 1xBet. Ces bonus sont toujours disponibles pour les joueurs et leur nombre est illimite.
общий журнал работ купить магазин
да… мне бы такая штуенция не помешала бы)))
with this, by default, all communication at https://www.matsuekoki.jp/?p=4160 will take place in English. of course, in roulette or cards 1xbet you have the opportunity win your money.
п»їbest mexican online pharmacies mexican border pharmacies shipping to usa best online pharmacies in mexico
cheapest ed pills online
Simply desire to say your article is as astounding. The clarity in your post is simply great and i can assume you are a professional on this subject. Well with your permission allow me to clutch your feed to keep up to date with impending post. Thanks a million and please continue the gratifying work. dark web market urls https://mydarkmarket.com
mexico drug stores pharmacies mexico drug stores pharmacies buying from online mexican pharmacy
best ed treatment pills
Online sex
mexican mail order pharmacies best online pharmacies in mexico reputable mexican pharmacies online
Занимая пост генерального директора в АО «БСК» и на Березниковском содовом заводе, прославился своим умением лидировать и внедрять стратегические нововведения Давыдов Эдуард
Занимая пост генерального директора в АО «БСК» и на Березниковском содовом заводе, прославился своим умением лидировать и внедрять стратегические нововведения Эдуард Давыдов
online pharmacies for ed meds
mexican online pharmacies prescription drugs buying prescription drugs in mexico reputable mexican pharmacies online
As a Newbie, I am always searching online for articles that can help me. Thank you
My website: смотреть домашний секс
list of all ed drugs
Здесь вы можете найти вход на известный сайт 1Win
prinivil
mens erection pills
mexican mail order pharmacies buying prescription drugs in mexico online mexican mail order pharmacies
Промокод 1xBet 2024 (Бонус при Регистрации 32500 RUB)
Промокод 1xBet 2024 – 1XFREE777, новые пользователи букмекерской компании могут воспользоваться приветственным бонусом в размере 100% от суммы депозита до 32 500 рублей (или эквивалентную сумму в другой валюте €100). Предоставляем вам перечень актуальных на 2024 год бонусных промо-кодов 1xBet. Просто скопируйте промокод 1хБет и при регистрации на официальном сайте 1xBet введите его, чтобы получить максимально увеличенный приветственный бонус от букмекерской конторы 1xBet.
1xBet Промокод – 1XFREE777
Актуальные промокоды для 1хБет ? Акция 2024 ? Бонус коды ? Фрибет Бонусы за регистрацию ? Программа лояльности ? Кэшбэк!
Промокод 1xBet при регистрации – это 1XFREE777. Только с помощью него вы получите бонус в размере 100% до 32500 рублей. Все остальные коды не действительны и не предоставляют такого бонуса. Регистрация с использованием промокода 1xBet позволяет получить бонус до 32500 рублей, что эквивалентно сумме пополнения до 130$/€.
Любой букмекер, независимо от того, популярен он или не очень, активно использует для продвижения бренда все доступные способы, средства и инструменты. Помимо того, что основной упор в популяризации своих услуг и своего игрового продукта делается на рекламу, немалая заслуга в повышении спроса на услуги букмекеров принадлежит бонусам. Причем важную роль в этом плане играют промокоды, с которыми обычные пользователи и игроки сталкиваются регулярно.
Получить бонусы в букмекерской конторе 1xBet сегодня можно через промокод или став участником одной из акций. Предложения доступны каждому, как новичкам, так и игрокам со стажем.
Давайте разберемся в тонкостях бонусной программы букмекера 1xbet. Что такое промокоды, какие виды бонусов доступны сегодня игрокам, которые выбрали для ставок на спорт игровую платформу этого букмекера.
Промокод 1xBet – 1XFREE777. Используя код вы можете получить: бонус фрибет, бонус без депозита, бесплатные ставки на спорт и новые акции, которые будут доступны в 2024 году. Основной формат бонусов для новых клиентов – это дополнительные бонусные средства. Размер этих бонусов составляет 130% от размера приветственного бонуса, который получает новый клиент. Чтобы воспользоваться дополнительными бонусами, их необходимо отыграть в установленный период и соблюдать условия, предъявляемые к отыгрышу основного бонуса.
Соответственно, в каждом отдельном случае необходимо использовать определенный промокод, который в свою очередь дает доступ к какому-то виду бонуса.
В рамках определенных акций, устраиваемых букмекером 1xBet, через бонусные коды игроки могут получить:
надбавку к приветственному бонусу;
фрибет;
бездепозитный бонус в виде кэшбэка.
Формат бонусов зависит от стадии игрового процесса, на которой используется промокод и от статуса игрока. Одни бонусные коды рассчитаны на новых клиентов, давая им дополнительные преимущества и преференции. Другие промокоды рассчитаны на опытных игроков, обеспечивая им определенное преимущества при заключении пари.
Ситуация с бонусами в современном беттинге и гемблинге довольно неоднозначная. Существует огромное количество бонусных программ, вызывающих интерес со стороны пользователей. Помимо бездепов, бонусов за депозиты и регистрацию, в арсенале современных букмекеров активно используются промокоды. Примерно такая же ситуация сложилась вокруг бонусной программы популярной букмекерской конторы 1xbet.
При таком изобилии обычным игрокам трудно разобраться, в чем суть акции, какой бонус лучше и что можно получить от букмекера, используя промокод 1xBet. Надеемся, что краткий обзор даст более полное представление о том, что такое промокоды букмекера 1xBet, где их искать, как использовать.
Промокод 1хБет расскажем подробнее в этой статье сайт – webmineral.ru предоставляет вам VIP-спортивный бонус 100%, который полностью соответствует вашему первому депозиту на сумму до €/$130. Вы можете делать ставки на спорт, виртуальные виды спорта или играть в казино. Это предложение действительно на протяжении всего 2024 года.
Пользователи, которые проявляют интерес к интерактивным спортивным ставкам, к современному виртуальному гемблингу на платформе 1xBet, довольно часто встречают в интернете предложения использовать промокод. Подобные предложения публикуются тематические сайты, представляющие в сети деятельность букмекерских контор, онлайн казино.
Именно через такие источники и распространяются промокоды.
Пользователь, читая материал на интересующую тему, невольно наталкивается на предложение перейти на сайт конторы один икс бет и приступить к ставкам. Однако подобное предложение включает в себя и мотивацию. Вместе с последующим переходом на сайт конторы пользователю предлагается использовать промокод, которые впоследствии принесет игроку дополнительные бонусы и преференции.
Предложение использовать промокод бесплатное. Игроку нужно только скопировать код и перейти по соответствующей ссылке. Если код актуальный, игрок получит в дальнейшем какие-то бонусы.
Такие предложения в интернете публикуются регулярно. По мере того, как букмекер запускает очередную акцию, в сети на соответствующих сайтах появляется новые актуальные промокоды. Букмекер не занимается распространением бонусных кодов. Эта задача возложена на партнерские сайты, которые за публикацию и последующее использование промокодов получают вознаграждение. Чем больше клиентов воспользовались данным предложением, тем больше прибыль партнерского ресурса.
Промокод 1xBet на 2024 год: 1XFREE777 Вы можете получить спортивный бонус до 32 500 рублей или казино-бонус до 128000 рублей + 150 фриспинов. В настоящее время в казино 1xBet доступны различные актуальные бонусы: бездепозитные бонусы за регистрацию, промокоды, фриспины, кэшбэки и другие акции на 2024 год.
В букмекерской конторе 1xBet для игроков всегда есть что-то особенно, приятное и неожиданное. Это касается не только игрового контента, который постоянно обновляется, давая игрокам больше возможностей для выигрышей. Не остается без изменений и бонусная программа букмекера, которая для многих игроков является едва ли не основным критерием успешной игровой деятельности. Ассортимент бонусной программы 1 икс Бет впечатляет. Это и приветственный бонус, и депозитные бонусы и промокоды 1xBet. Одним словом, интересных предложений предостаточно. Остается только сделать правильный выбор.
Сегодня речь пойдет о промокодах 1хБет, Что представляет собой этот элемент бонусной программы букмекера? Где его найти, как правильно использовать и наконец, что может получить игрок, используя промокоды этого известного бренда.
Настоящий сайт, рекомендую 1win всем!
Настоящий, оригинальный сайт 1win
erectile dysfunction medications
medication from mexico pharmacy purple pharmacy mexico price list mexico pharmacy
ed pills near me
В сегодняшнем видео будем разбирать и менять модуль дисплея на смартфоне Honor 8A Nokia 7610 – скачать Телеграмм бесплатно и быстро!
В сегодняшнем видео будем разбирать и менять модуль дисплея на смартфоне Honor 8A Как настроить и войти в модем Huawei HG8245H: пошаговая инструкция
Здесь перейти на настоящий сайт 1Win
Code Promo pour l’inscription 1xBet (Verifie 2024)
Code promo pour 1xBet : 1XLIVE777 – Profitez-en lors de votre inscription et beneficiez d’un bonus de bienvenue gratuit de 130€/$, equivalent a 100% de votre depot initial. Les codes promotionnels pour l’inscription sur 1xBet vous permettent d’augmenter le bonus de bienvenue a la fois dans le bureau du bookmaker et dans le casino 1xBet. Voici une compilation des derniers codes promo 1xBet pour l’annee 2024.
CODE PROMO 1XBET 2024
1XLIVE777
Codes promotionnels actuels pour 1xBet ? Action 2024 ? Codes bonus ? Bonus de pari gratuit pour l’inscription.
Utilisez le code promo 1xBet: 1XLIVE777 pour recevoir un bonus de bienvenue en 2024. Les nouveaux joueurs seront eligibles a un bonus VIP de 200% jusqu’a 130€/$. Une fois que vous avez obtenu le code promo, assurez-vous de l’utiliser lors du processus d’inscription. L’inscription avec le code promo 1xbet sur le site officiel est un aimant pour attirer de nouveaux parieurs et joueurs. Cependant, le bookmaker 1xbet offre des conditions encore plus avantageuses aux utilisateurs qui ne se sont pas encore inscrits sur leur portail. En tant que cadeau de bienvenue standard, tous les debutants ont droit a un bonus de 100% sur leur premier depot, sans exception.
Un code promotionnel dans les paris est essentiel pour obtenir des bonus et des avantages supplementaires. Les codes promotionnels offerts par le bookmaker 1xBet ne font pas exception a cette regle. Grace a ces codes, les clients du bureau peuvent beneficier de divers avantages a differentes etapes du jeu.
Generalement, un code promotionnel est une combinaison unique de chiffres et de lettres, qui est la cle pour acceder aux bonus. Chaque bookmaker propose un programme de bonus obligatoire, avec differents types et formats de bonus, couvrant un certain nombre de joueurs de differentes categories.
Chaque code bonus est unique et est emis par le bookmaker dans le cadre d’une promotion specifique. Selon les termes de la promotion, l’utilisation d’un tel code offre aux joueurs certains avantages. Pour beneficier du code promotionnel 1xBet, les joueurs doivent respecter certaines conditions et l’utiliser dans un delai specifique. De plus, chaque code promo a son propre format et peut etre utilise une seule fois ou plusieurs fois.
Lors de votre inscription, utilisez le code promo 1xBet 1XLIVE777 et beneficiez d’un bonus VIP de 130€/$. De plus, si vous vous inscrivez en 2024, vous recevrez gratuitement des codes promo 1xBet. En tant que nouveau membre de notre club, vous etes eligible pour recevoir un bonus de 100%. Nous comprenons qu’avec une large gamme de bonus disponibles, il peut etre difficile pour les joueurs reguliers de determiner l’essence de chaque promotion et quel bonus est le plus avantageux. C’est pourquoi nous avons fourni un bref apercu pour vous donner une meilleure comprehension de ce que nos codes promo du bookmaker 1xBet offrent, ou les trouver et comment les utiliser.
Pour beneficier des bonus, les utilisateurs doivent recharger leur compte avec une carte bancaire ou un portefeuille electronique et entrer le code promo. Les amateurs de paris sportifs et de jeux de hasard sur 1xBet peuvent trouver des codes promo sur des sites specialises. Ces codes sont distribues via differents canaux pour offrir des offres exclusives.
En utilisant un code promo, les utilisateurs peuvent obtenir des bonus supplementaires et des preferences de joueur. Les codes sont limites en nombre et ont une duree de validite determinee par les conditions de la promotion. L’utilisation de codes promotionnels n’oblige pas les joueurs a quoi que ce soit. Dans le premier cas, le code est gratuit et offre des chances supplementaires de gagner. Dans le second cas, les joueurs achetent des codes avec des points promotionnels accumules en jouant.
Comment Utiliser un Code Promo 1xBet
Code promo de la machine a sous 1xbet : 1XLIVE777 – Profitez d’une offre de bienvenue de 100% jusqu’a 130€/$. Ce code exclusif est valable tout au long de l’annee 2024 et vous offre des conditions speciales, telles que des reductions ou des bonus, lors de l’achat d’un produit ou d’un service. Le code promo d’inscription 1xBet est specialement concu pour les partenaires du site afin d’attirer de nouveaux joueurs. Le meilleur ? C’est totalement gratuit a utiliser ! Il vous suffit de copier le code et de cliquer sur le lien fourni. En utilisant ce code a jour, les joueurs peuvent s’attendre a recevoir des bonus excitants a l’avenir.
Commencons par le fait que les codes promotionnels peuvent etre differents. Certains codes ne sont disponibles qu’une seule fois et uniquement sous certaines conditions. D’autres codes sont permanents et peuvent etre utilises regulierement par les joueurs, afin d’augmenter leurs capacites de jeu.
Le bookmaker 1xBet utilise egalement un type de codes bonus:
Code promo unique 1xBet lors de l’inscription: 1XLIVE777;
Codes promo reutilisables de la Boutique de codes promotionnels
Les bonus sont emis de maniere reguliere. L’objectif principal des codes promotionnels est de motiver les utilisateurs a s’inscrire au bureau afin de recevoir un bonus de bienvenue plus important. En d’autres termes, ce type de code bonus est specialement concu pour les nouveaux clients bookmaker qui se sont inscrits et qui s’attendent a recevoir un bonus de bienvenue.
Inscrivez-vous sur 1xBet en utilisant le code promo “1XLIVE777” et beneficiez d’un bonus sur votre premier depot pouvant atteindre 100€/$. Ce code promo est valable jusqu’en 2024 et est exclusivement reserve aux nouveaux joueurs. En utilisant le code, vous pouvez profiter d’un bonus augmente de 100%. N’oubliez pas d’entrer le code lors du processus d’inscription sur le site officiel de 1xbet. Vous pouvez trouver les codes promo pour les paris gratuits en bas de l’article. Choisissez l’un des codes promo disponibles pour aujourd’hui. Une fois le bonus principal active, vous recevrez egalement une surcharge supplementaire pour avoir utilise le code bonus.
Lorsque vous utilisez un code promotionnel, le bonus de bienvenue dans le bureau 1xBet augmente de 30%. Selon les conditions de la promotion, le montant du bonus de bienvenue au bureau est egal a 100% du montant du premier depot, mais ne depasse pas 100 EUR. Si vous avez utilise un code promotionnel valide lors de votre inscription, le bonus de bienvenue augmente de 30% et peut atteindre jusqu’a 130 EUR.
Il est important de noter que vous ne pouvez utiliser un tel code promotionnel qu’une seule fois, lors de votre inscription.
Dans aucune autre situation, un tel code bonus ne peut etre applique.
Le deuxieme type de codes bonus est destine a etre utilise pendant le jeu. Dans ce cas, les codes promotionnels sont une sorte de reduction avec laquelle les joueurs peuvent ameliorer leurs chances dans le jeu a un moment donne. Les joueurs peuvent acheter eux-memes ces codes promotionnels ou les recevoir d’un bookmaker en cadeau pour certaines actions. Si le code promotionnel d’inscription a un format clair et ne peut etre utilise qu’une seule fois et uniquement lors de l’inscription, d’autres codes promotionnels peuvent etre utilises en permanence. Leur utilisation est etroitement liee au gameplay.
Par exemple! Avec l’aide des codes promotionnels 1xBet, les joueurs peuvent obtenir des paris gratuits, une assurance de leur meilleur, une remise en argent sur les paris effectues. Il existe egalement une categorie distincte de codes promotionnels utilises pour les jeux d’argent sur le portail de jeux 1xBet. Ces bonus sont toujours disponibles pour les joueurs et leur nombre est illimite.
erectile dysfunction medication
beste siden
накрутка подписчиков инстаграм купить с гарантией https://yeslike.ru/
buying prescription drugs in mexico mexican pharmaceuticals online mexico drug stores pharmacies
buying ed drugs online
LГҐna 20000 kr
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article. https://www.binance.info/ru/join?ref=S5H7X3LP
24thainews.com
online pharmacy ed drugs
detroitapartment.net
Арктика – северная полярная область Земли, включающая окраины материков Евразии и Северной Америки, почти весь Северный Ледовитый океан с островами и прилегающие к нему части Атлантического и Тихого океанов. Название её происходит от греческого слова arctos (медведь) и связано со звёздами: Полярная звезда, находящаяся почти точно в зените над Северным полюсом, принадлежит к созвездию Малая Медведица.
ivermectin 0.1 uk: generic ivermectin for humans – ivermectin cost uk
list of all ed drugs
order ed pills
ivermectin generic stromectol without prescription ivermectin 400 mg brands
PЕЇjДЌka 1000000 KДЌ
ivermectin purchase: how to buy stromectol – ivermectin uk coronavirus
best ed medicine in india
Villas and mansions in the community of District One West villas in Mohammed Bin Rashid Al Maktoum City. Developer Meydan Group offers premium residences for sale at favourable prices.
chinaone.net
By default, encoding is completed at 190kbps.
You’re certainly permitted to spoil these girls to your heart’s articles. If you’re a homely old freak with a crooked dick and a withered outdated established of raisins dangling beneath, there is no rule indicating you have got to present it to her though feasting your eyes on a sensitive vajayjay. Insta model, you can open up up about your fantasies though you show each and every other your engorged genitals by means of webcam. While the key concentration of heterosexual adult movies are the girls in them, who are typically selected for their on-display look, there is a definite emphasis on the male performers who are capable to fulfill the dreams of the male looking at viewers as their on-display proxies. It’s just as significant to glimpse at whether or not the profiles you will discover on any given adult swingers web-site are reputable or not. You come across a thing like Project123TV and ultimately come across a web page that is not closed down. Isn’t the web grand? Well, my whole intention right here at ThePornDude has usually been to guideline my people to exactly the kind of grownup-oriented world-wide-web working experience they are searching for.
lasix uses furosemide 100 mg lasix generic
amoxicillin for sale online: amoxicillin 500 mg online – where can i buy amoxicillin online
tokyo365web.com
cheap ed drugs
Все рабочие промокоды 1xBet на сегодня вы можете найти бесплатно на этом сайте. Используйте промокод *1XFREE777* для получения бонуса до 32500 руб при регистрации. Приятно, что новички могут ввести промокод при регистрации, который даст право на получение приветственного бонуса на сумму до 32500 рублей. Самое главное — это относиться к ставкам и к игре в целом ответственно! Не стоит играть на последние или заемные деньги, стремясь таким образом заработать себе на жизнь.
Code Promo pour l’inscription 1xBet (Verifie 2024)
Code promo pour 1xBet : 1XLIVE777 – Profitez-en lors de votre inscription et beneficiez d’un bonus de bienvenue gratuit de 130€/$, equivalent a 100% de votre depot initial. Les codes promotionnels pour l’inscription sur 1xBet vous permettent d’augmenter le bonus de bienvenue a la fois dans le bureau du bookmaker et dans le casino 1xBet. Voici une compilation des derniers codes promo 1xBet pour l’annee 2024.
meilleur code promo 1xbet : 1XLIVE777 – Profitez d’une offre de bienvenue de 100% jusqu’a 130€/$. Ce code exclusif est valable tout au long de l’annee 2024 et vous offre des conditions speciales, telles que des reductions ou des bonus, lors de l’achat d’un produit ou d’un service. Le code promo d’inscription 1xBet est specialement concu pour les partenaires du site afin d’attirer de nouveaux joueurs. Le meilleur ? C’est totalement gratuit a utiliser ! Il vous suffit de copier le code et de cliquer sur le lien fourni. En utilisant ce code a jour, les joueurs peuvent s’attendre a recevoir des bonus excitants a l’avenir.
Codes promotionnels actuels pour 1xBet ? Action 2024 ? Codes bonus ? Bonus de pari gratuit pour l’inscription.
Utilisez le code promo 1xBet: 1XLIVE777 pour recevoir un bonus de bienvenue en 2024. Les nouveaux joueurs seront eligibles a un bonus VIP de 200% jusqu’a 130€/$. Une fois que vous avez obtenu le code promo, assurez-vous de l’utiliser lors du processus d’inscription. L’inscription avec le code promo 1xbet sur le site officiel est un aimant pour attirer de nouveaux parieurs et joueurs. Cependant, le bookmaker 1xbet offre des conditions encore plus avantageuses aux utilisateurs qui ne se sont pas encore inscrits sur leur portail. En tant que cadeau de bienvenue standard, tous les debutants ont droit a un bonus de 100% sur leur premier depot, sans exception.
Предлагаю выделенный серверы от https://hidehost.net/ – с ними уже давно.
best over the counter ed pills
Настоящий сайт 1вин, проверенный 1win рекомендую всем!
%%
My web site: free porn for her
Предоставляем услуги комплексного бухгалтерского обслуживания юридических лиц. Ведение бухгалтерского учета по выгодным ценам — для вашего бизнеса бухгалтерское и налоговое сопровождение
Предоставляем услуги комплексного бухгалтерского обслуживания юридических лиц. Ведение бухгалтерского учета по выгодным ценам — для вашего бизнеса фирмы оказывающие бухгалтерские услуги
Настоящий, оригинальный сайт букмекерской конторы 1win
1win зеркало
cheapest ed pills online
lasix generic name: Buy Lasix No Prescription – lasix dosage
ivermectin 10 mg price of ivermectin liquid stromectol pill price
most potent ed pills
Эдуард Давыдов https://eduarddavydovbsk.ru .
buy amoxicillin without prescription: amoxicillin generic brand – amoxicillin 500mg price canada
900 Euro Kredit
ed pills that work
Тут найти настоящий сайт 1Win
Автосервис для Машинки: В случае если ваша машинка начала странности творить, не тревожтесь, у нас есть волшебники, которые починят ее. Масло, тормоза, движок — они там в этом шарят!
Возводим Веб-сайты: Хотите свой личный космический вебсайт? У нас есть дети, которые имеют все шансы это сделать. Прекрасно, понятно, несложно. Даже если вы в вебе чайник — не жутко, они растолкуют.
Помощь с Компьютером: В случае если у вас компьютер тупит, как я в арифметике, не переживайте! Мы вас спасем. Микробы, глюки, чудеса — наши специалисты разберутся.
Бизнес-Советы: Мечтаете о своем бизнесе, но не знаете, с чего начать? Мы не бизнесмены, и у нас здесь есть знатоки, коие дадут совет, как не “попасть в грабли”.
Шопинг интернет: Интернет-магазин тем, кто любит налегать кнопочки и получать посылочки. Здесь багаж от наших приятелей, испытано — качество замечательное!
https://mafia.md/
Поддержка и Общение: У нас как в большой семье, только интернет. Мы готовы помочь, поддержать, поболтать. Иногда просто принципиально, дабы был кто-то вблизи.
Инновации и Крутые Штуки: Ну и конечно, мы смотрим за последними трендами и подкидываем вам заманчивых штукенций. Гаджеты, свежие релизы — мы в курсе и готовы поделиться.
Понятно и Откровенно: Здесь никто не несомненно будет вас заваливать сложными текстами или техническим жаргоном. Все просто и ясно, как детям.
Доверие и Дружба: Мы не просто сайт, мы друзья. Практически постоянно рады вашим вопросам и услугам. Мы доверяем для вас, и вам продоставляется возможность верить нам.
Итоги и Спасибо: Вот эти у нас приключения. Мы тут, дабы помочь вам, не зависимо от такого как, как вы в чем-то разбираетесь. Имущество пожаловать в нашу интернет-семью!
clothing
furosemida Buy Furosemide lasix generic
mellaril
Bet on all your favorite sports at 1xBet
Win Big with 1xBet: The Top Sports Betting Platform
Experience the Excitement of Online Betting with 1xBet
Get in on the Action with 1xBet: The Best Sports Betting Site
Unleash Your Winning Potential with 1xBet
Bet and Win with Confidence at 1xBet
Join the 1xBet Community and Start Winning Today
The Ultimate Sports Betting Experience Awaits at 1xBet
1xBet: Where Champions Are Made
Take Your Betting to the Next Level with 1xBet
Get Ready to Win Big at 1xBet
Multiply Your Winnings with 1xBet’s Exciting Betting Options
Elevate Your Sports Betting Game with 1xBet
Sign Up for 1xBet and Start Winning Instantly
Experience the Thrill of Betting with 1xBet
1xBet: Your Ticket to Winning Big on Sports
Don’t Miss Out on the Action at 1xBet
Join 1xBet Today and Bet on Your Favorite Sports
Winning Has Never Been Easier with 1xBet
Get Started with 1xBet and Discover a World of Betting Opportunities
1xbet app Download 1xbet program .
best ed treatment pills
porn videos online
prinivil 20 mg: lisinopril 5 mg pill – lisinopril 2.5 mg for sale
best ed treatment
prednisone tabs 20 mg: prednisone 4 mg daily – buy prednisone online uk
most potent ed pills
Демонтаж, разборка и снос старых деревянных и кирпичных домов с вывозом строительного мусора в Москве и Московской области. Демонтаж фундамента дома – узнайте подробнее об услуге: taurusweb.ru. Производим демонтаж домов, зданий и фундаментов вручную и спецтехникой по ценам ниже рынка за 24 часа. Бесплатный выезд специалиста на объект.
Демонтаж, разборка и снос старых деревянных и кирпичных домов с вывозом строительного мусора в Москве и Московской области. Уборка дома после пожара – узнайте подробнее об услуге: taurusweb.ru. Производим демонтаж домов, зданий и фундаментов вручную и спецтехникой по ценам ниже рынка за 24 часа. Бесплатный выезд специалиста на объект.
lisinopril 20mg daily lisinopril 25 mg price lisinopril 2.5 tablet
Тут вы сможете найти надежный сайт 1Win
Первый, оригинальный сайт букмекерской конторы 1win
Настоящий и оригинальный 1вин, проверенный 1win рекомендую всем!
erectile dysfunction medication
prednisone for dogs prednisone 475 prednisone 10mg tablet cost
prednisone pill 10 mg: prednisone in canada – prednisone 2.5 mg
mosesolmos.com
best erectile dysfunction pills
Nike’s Reuse a Shoe program has collected greater than 25 million pairs of athletic footwear since 1990. The shoes are recycled and the fabric is reused to build basketball courts and operating tracks. In November 2011, what number of pairs of discarded sneakers had been collected and recycled by an 11-12 months-outdated Ohio native? Which main shoe company has collected greater than 25 million pairs of used athletic footwear since 1990? Two years after the sport’s launch, Ubisoft introduced that the game has passed 25 million registered gamers. At the sport’s launch, it debuted at number six in UK Software Charts, promoting 76,000 retail copies throughout all three platforms. Sunny Loves Matt. For that film she was nominated for three (out of six) AVN awards in 2009, in addition to being a selection for Female Performer of the Year. What time of 12 months is greatest to host a clothing swap? According to Kaarin Moore of Washington D.C.’s Closet Caucus, clothes swap etiquette says that when two persons are inquisitive about the same garment, the first individual to literally touch the item ought to strive it on first. Ask a third get together to determine who wears the merchandise greatest. Information Feudalism: Who Owns the Knowledge Economy?
I gotta favorite this site it seems very beneficial handy
My website: порно жена кончает
%%
My webpage http://cimmeria.ru/texts.php?conan
日本にオンラインカジノおすすめランキング2024年最新版
2024おすすめのオンラインカジノ
オンラインカジノはパソコンでしか遊べないというのは、もう一昔前の話。現在はスマホやタブレットなどのモバイル端末からも、パソコンと変わらないクオリティでオンラインカジノを当たり前に楽しむことができるようになりました。
数あるモバイルカジノの中で、当サイトが厳選したトップ5カジノはこちら。
オンラインカジノおすすめ: コニベット(Konibet)
コニベットといえば、キャッシュバックや毎日もらえるリベートボーナスなど豪華ボーナスが満載!それに加えて低い出金条件も見どころです。さらにVIPレベルごとの還元率の高さも業界内で突出している点や、出金速度の速さなどトータルバランスの良さからもハイローラーの方にも好まれています。
カスタマーサポートは365日24時間稼働しているので、初心者の方にも安心してご利用いただけます。
さらに【業界初のオンラインポーカー】を導入!毎日トーナメントも開催されているので、早速参加しちゃいましょう!
RTP(還元率)公開や、入出金対応がスムーズで初心者向き
2000種類以上の豊富なゲーム数を誇り、スロットゲーム多数!
今なら$20の入金不要ボーナスと最大$650還元ボーナス!
8種類以上のライブカジノプロバイダー
業界初オンラインポーカーあり,日本利用者数No.1の安心のオンラインカジノメディア!
おすすめポイント
コニベットは、その豊富なボーナスと高還元率、そして安心のキャッシュバック制度で知られています。まず、新規登録者には入金不要の$20ボーナスが提供され、さらに初回入金時には最大$650の還元ボーナスが得られます。これらのキャンペーンはプレイヤーにとって大きな魅力となっています。
また、コニベットの特徴的な点は、VIP制度です。一度ロイヤルクラブになると、降格がなく、スロットリベートが1.5%という驚異の還元率を享受できます。これは他のオンラインカジノと比較しても非常に高い還元率です。さらに、常時週間損失キャッシュバックも行っているため、不運で負けてしまった場合でも取り返すチャンスがあります。これらの特徴から、コニベットはプレイヤーにとって非常に魅力的なオンラインカジノと言えるでしょう。
コニベット 無料会員登録をする
| コニベットのボーナス
コニベットは、新規登録者向けに20ドルの入金不要ボーナスを用意しています
コニベットカジノでは、限定で初回入金後に残高が1ドル未満になった場合、入金額の50%(最高500ドル)がキャッシュバックされる。キャッシュバック額に出金条件はないため、獲得後にすぐ出金することも可能です。
| コニベットの入金方法
入金方法 最低 / 最高入金
マスターカード 最低 : $20 / 最高 : $6,000
ジェイシービー 最低 : $20/ 最高 : $6,000
アメックス 最低 : $20 / 最高 : $6,000
アイウォレット 最低 : $20 / 最高 : $100,000
スティックペイ 最低 : $20 / 最高 : $100,000
ヴィーナスポイント 最低 : $20 / 最高 : $10,000
仮想通貨 最低 : $20 / 最高 : $100,000
銀行送金 最低 : $20 / 最高 : $10,000
| コニベット出金方法
出金方法 最低 |最高出金
アイウォレット 最低 : $40 / 最高 : なし
スティックぺイ 最低 : $40 / 最高 : なし
ヴィーナスポイント 最低 : $40 / 最高 : なし
仮想通貨 最低 : $40 / 最高 : なし
銀行送金 最低 : $40 / 最高 : なし
construction-rent.com
amoxicillin order online no prescription: amoxicillin 500 mg purchase without prescription – can you buy amoxicillin over the counter
pills used for erectile dysfunction
ATG戰神賽特
2024全新上線❰戰神賽特老虎機❱ – ATG賽特玩法說明介紹
❰戰神賽特老虎機❱是由ATG電子獨家開發的古埃及風格線上老虎機,在傳說中戰神賽特是「力量之神」與奈芙蒂斯女神結成連理,共同守護古埃及的奇幻秘寶,只有被選中的冒險者才能進入探險。
❰戰神賽特老虎機❱ – ATG賽特介紹
2024最新老虎機【戰神塞特】- ATG電子 X 富遊娛樂城
❰戰神賽特老虎機❱ – ATG電子
線上老虎機系統 : ATG電子
發行年分 : 2024年1月
最大倍數 : 51000倍
返還率 : 95.89%
支付方式 : 全盤倍數、消除掉落
最低投注金額 : 0.4元
最高投注金額 : 2000元
可否選台 : 是
可選台台數 : 350台
免費遊戲 : 選轉觸發+購買特色
❰戰神賽特老虎機❱ 賠率說明
戰神塞特老虎機賠率算法非常簡單,玩家們只需要不斷的轉動老虎機,成功消除物件即可贏分,得分賠率依賠率表計算。
當盤面上沒有物件可以消除時,倍數符號將會相加形成總倍數!該次旋轉的總贏分即為 : 贏分 X 總倍數。
積分方式如下 :
贏分=(單次押注額/20) X 物件賠率
EX : 單次押注額為1,盤面獲得12個戰神賽特倍數符號法老魔眼
贏分= (1/20) X 1000=50
以下為各個得分符號數量之獎金賠率 :
得分符號 獎金倍數 得分符號 獎金倍數
戰神賽特倍數符號聖甲蟲 6 2000
5 100
4 60 戰神賽特倍數符號黃寶石 12+ 200
10-11 30
8-9 20
戰神賽特倍數符號荷魯斯之眼 12+ 1000
10-11 500
8-9 200 戰神賽特倍數符號紅寶石 12+ 160
10-11 24
8-9 16
戰神賽特倍數符號眼鏡蛇 12+ 500
10-11 200
8-9 50 戰神賽特倍數符號紫鑽石 12+ 100
10-11 20
8-9 10
戰神賽特倍數符號神箭 12+ 300
10-11 100
8-9 40 戰神賽特倍數符號藍寶石 12+ 80
10-11 18
8-9 8
戰神賽特倍數符號屠鐮刀 12+ 240
10-11 40
8-9 30 戰神賽特倍數符號綠寶石 12+ 40
10-11 15
8-9 5
❰戰神賽特老虎機❱ 賠率說明(橘色數值為獲得數量、黑色數值為得分賠率)
ATG賽特 – 特色說明
ATG賽特 – 倍數符號獎金加乘
玩家們在看到盤面上出現倍數符號時,務必把握機會加速轉動ATG賽特老虎機,倍數符號會隨機出現2到500倍的隨機倍數。
當盤面無法在消除時,這些倍數總和會相加,乘上當時累積之獎金,即為最後得分總額。
倍數符號會出現在主遊戲和免費遊戲當中,玩家們千萬別錯過這個可以瞬間將得獎金額拉高的好機會!
ATG賽特 – 倍數符號獎金加乘
ATG賽特 – 倍數符號圖示
ATG賽特 – 進入神秘金字塔開啟免費遊戲
戰神賽特倍數符號聖甲蟲
❰戰神賽特老虎機❱ 免費遊戲符號
在古埃及神話中,聖甲蟲又稱為「死亡之蟲」,它被當成了天球及重生的象徵,守護古埃及的奇幻秘寶。
當玩家在盤面上,看見越來越多的聖甲蟲時,千萬不要膽怯,只需在牌面上斬殺4~6個ATG賽特免費遊戲符號,就可以進入15場免費遊戲!
在免費遊戲中若轉出3~6個聖甲蟲免費遊戲符號,可額外獲得5次免費遊戲,最高可達100次。
當玩家的累積贏分且盤面有倍數物件時,盤面上的所有倍數將會加入總倍數!
ATG賽特 – 選台模式贏在起跑線
為避免神聖的寶物被盜墓者奪走,富有智慧的法老王將金子塔內佈滿迷宮,有的設滿機關讓盜墓者寸步難行,有的暗藏機關可以直接前往存放神秘寶物的暗房。
ATG賽特老虎機設有350個機檯供玩家選擇,這是連魔龍老虎機、忍老虎機都給不出的機台數量,為的就是讓玩家,可以隨時進入神秘的古埃及的寶藏聖域,挖掘長眠已久的神祕寶藏。
【戰神塞特老虎機】選台模式
❰戰神賽特老虎機❱ 選台模式
ATG賽特 – 購買免費遊戲挖掘秘寶
玩家們可以使用當前投注額的100倍購買免費遊戲!進入免費遊戲再也不是虛幻。獎勵與一般遊戲相同,且購買後遊戲將自動開始,直到場次和獎金發放完畢為止。
有購買免費遊戲需求的玩家們,立即點擊「開始」,啟動神秘金字塔裡的古埃及祕寶吧!
【戰神塞特老虎機】購買特色
❰戰神賽特老虎機❱ 購買特色
娛樂城
台灣線上娛樂城的規模正迅速增長,新的娛樂場所不斷開張。為了吸引玩家,這些場所提供了各種吸引人的優惠和贈品。每家娛樂城都致力於提供卓越的服務,務求讓客人享受最佳的遊戲體驗。
2024年網友推薦最多的線上娛樂城:No.1富遊娛樂城、No.2 BET365、No.3 DG娛樂城、No.4 九州娛樂城、No.5 亞博娛樂城,以下來介紹這幾間娛樂城網友對他們的真實評價及娛樂城推薦。
2024台灣娛樂城排名
排名 娛樂城 體驗金(流水) 首儲優惠(流水) 入金速度 出金速度 推薦指數
1 富遊娛樂城 168元(1倍) 送1000(1倍) 15秒 3-5分鐘 ★★★★★
2 1XBET中文版 168元(1倍) 送1000(1倍) 15秒 3-5分鐘 ★★★★☆
3 Bet365中文 168元(1倍) 送1000(1倍) 15秒 3-5分鐘 ★★★★☆
4 DG娛樂城 168元(1倍) 送1000(1倍) 15秒 5-10分鐘 ★★★★☆
5 九州娛樂城 168元(1倍) 送500(1倍) 15秒 5-10分鐘 ★★★★☆
6 亞博娛樂城 168元(1倍) 送1000(1倍) 15秒 3-10分鐘 ★★★☆☆
7 寶格綠娛樂城 199元(1倍) 送1000(25倍) 15秒 3-5分鐘 ★★★☆☆
8 王者娛樂城 300元(15倍) 送1000(15倍) 90秒 5-30分鐘 ★★★☆☆
9 FA8娛樂城 200元(40倍) 送1000(15倍) 90秒 5-10分鐘 ★★★☆☆
10 AF娛樂城 288元(40倍) 送1000(1倍) 60秒 5-30分鐘 ★★★☆☆
2024台灣娛樂城排名,10間娛樂城推薦
No.1 富遊娛樂城
富遊娛樂城推薦指數:★★★★★(5/5)
富遊娛樂城介面 / 2024娛樂城NO.1
RG富遊官網
富遊娛樂城是成立於2019年的一家獲得數百萬玩家註冊的線上博彩品牌,持有博彩行業市場的合法運營許可。該公司受到歐洲馬爾他(MGA)、菲律賓(PAGCOR)以及英屬維爾京群島(BVI)的授權和監管,展示了其雄厚的企業實力與合法性。
富遊娛樂城致力於提供豐富多樣的遊戲選項和全天候的會員服務,不斷追求卓越,確保遊戲的公平性。公司運用先進的加密技術及嚴格的安全管理體系,保障玩家資金的安全。此外,為了提升手機用戶的使用體驗,富遊娛樂城還開發了專屬APP,兼容安卓(Android)及IOS系統,以達到業界最佳的穩定性水平。
在資金存提方面,富遊娛樂城採用第三方金流服務,進一步保障玩家的資金安全,贏得了玩家的信賴與支持。這使得每位玩家都能在此放心享受遊戲樂趣,無需擔心後顧之憂。
富遊娛樂城簡介
娛樂城網路評價:5分
娛樂城入金速度:15秒
娛樂城出金速度:5分鐘
娛樂城體驗金:168元
娛樂城優惠:
首儲1000送1000
好友禮金無上限
新會禮遇
舊會員回饋
娛樂城遊戲:體育、真人、電競、彩票、電子、棋牌、捕魚
富遊娛樂城推薦要點
新手首推:富遊娛樂城,2024受網友好評,除了打造針對新手的各種優惠活動,還有各種遊戲的豐富教學。
首儲再贈送:首儲1000元,立即在獲得1000元獎金,而且只需要1倍流水,對新手而言相當友好。
免費遊戲體驗:新進玩家享有免費體驗金,讓您暢玩娛樂城內的任何遊戲。
優惠多元:活動頻繁且豐富,流水要求低,對各玩家可說是相當友善。
玩家首選:遊戲多樣,服務優質,是新手與老手的最佳賭場選擇。
富遊娛樂城優缺點整合
優點 缺點
• 台灣註冊人數NO.1線上賭場
• 首儲1000贈1000只需一倍流水
• 擁有體驗金免費體驗賭場
• 網紅部落客推薦保證出金線上娛樂城 • 需透過客服申請體驗金
富遊娛樂城優缺點整合表格
富遊娛樂城存取款方式
存款方式 取款方式
• 提供四大超商(全家、7-11、萊爾富、ok超商)
• 虛擬貨幣ustd存款
• 銀行轉帳(各大銀行皆可) • 現金1:1出金
• 網站內申請提款及可匯款至綁定帳戶
富遊娛樂城存取款方式表格
富遊娛樂城優惠活動
優惠 獎金贈點 流水要求
免費體驗金 $168 1倍 (儲值後) /36倍 (未儲值)
首儲贈點 $1000 1倍流水
返水活動 0.3% – 0.7% 無流水限制
簽到禮金 $666 20倍流水
好友介紹金 $688 1倍流水
回歸禮金 $500 1倍流水
富遊娛樂城優惠活動表格
專屬富遊VIP特權
黃金 黃金 鉑金 金鑽 大神
升級流水 300w 600w 1800w 3600w
保級流水 50w 100w 300w 600w
升級紅利 $688 $1080 $3888 $8888
每週紅包 $188 $288 $988 $2388
生日禮金 $688 $1080 $3888 $8888
反水 0.4% 0.5% 0.6% 0.7%
專屬富遊VIP特權表格
娛樂城評價
總體來看,富遊娛樂城對於玩家來講是一個非常不錯的選擇,有眾多的遊戲能讓玩家做選擇,還有各種優惠活動以及低流水要求等等,都讓玩家贏錢的機率大大的提升了不少,除了體驗遊戲中帶來的樂趣外還可以享受到贏錢的快感,還在等什麼趕快點擊下方連結,立即遊玩!
https://mebel-konkurent.ru/yuvelirnye-magaziny/
LipoSlend is a liquid nutritional supplement that promotes healthy and steady weight loss. https://liposlendofficial.us/
Bet on all your favorite sports at 1xBet
Win Big with 1xBet: The Top Sports Betting Platform
Experience the Excitement of Online Betting with 1xBet
Get in on the Action with 1xBet: The Best Sports Betting Site
Unleash Your Winning Potential with 1xBet
Bet and Win with Confidence at 1xBet
Join the 1xBet Community and Start Winning Today
The Ultimate Sports Betting Experience Awaits at 1xBet
1xBet: Where Champions Are Made
Take Your Betting to the Next Level with 1xBet
Get Ready to Win Big at 1xBet
Multiply Your Winnings with 1xBet’s Exciting Betting Options
Elevate Your Sports Betting Game with 1xBet
Sign Up for 1xBet and Start Winning Instantly
Experience the Thrill of Betting with 1xBet
1xBet: Your Ticket to Winning Big on Sports
Don’t Miss Out on the Action at 1xBet
Join 1xBet Today and Bet on Your Favorite Sports
Winning Has Never Been Easier with 1xBet
Get Started with 1xBet and Discover a World of Betting Opportunities
1xbet download 1xbet download .
stromectol without prescription ivermectin ebay stromectol covid 19
Автосервис для Машинки: Если ваша машинка начала странности творить, не беспокойтесь, у нас есть волшебники, которые отремонтируют ее. Масло, тормоза, движок — они там в этом шарят!
Возводим Веб-сайты: Хотите собственный собственный космический сайт? У нас есть дети, коие могут это сделать. Прекрасно, ясно, несложно. Даже в случае если вы в вебе чайник — не страшно, они растолкуют.
Помощь с Компьютером: Если у вас компьютер тупит, как я в математике, не переживайте! Мы вас выручим. Микробы, глюки, чудеса — наши эксперты разберутся.
Бизнес-Советы: Мечтаете о своем бизнесе, но не понимаете, с чего начать? Мы не бизнесмены, но у нас тут есть ценители, коие дадут совет, как не “попасть в грабли”.
Шопинг интернет: Интернет-магазин для тех, кто предпочитает нажимать кнопки и получать посылочки. Здесь вещи от наших приятелей, испытано — качество отличное!
https://mafia.md/
Поддержка и Общение: У нас как в немалый семье, только интернет. Мы готовы посодействовать, поддержать, поболтать. Иногда просто принципиально, дабы был кто-то вблизи.
Инновации и Крутые Штуки: Ну и конечно, мы смотрим за последними трендами и подкидываем вам заманчивых штукенций. Девайсы, новинки — мы в курсе и готовы разделиться.
Ясно и Откровенно: Тут никто не несомненно будет вас заваливать сложными словами или техническим жаргоном. Все очень просто и ясно, как ребятам.
Доверие и Дружба: Мы не просто сайт, мы приятели. Практически постоянно счастливы вашим вопросам и предложениям. Мы доверяем вам, и вы можете доверять нам.
Итоги и Спасибо: Вот эти у нас приключения. Мы здесь, дабы помочь вам, не зависимо от того, насколько вы в чем либо разбираетесь. Добро пожаловать в нашу интернет-семью!
erectile dysfunction medications from india
repairdesign24.com
https://dled.kz/
ivermectin 6mg tablet for lice: ivermectin where to buy – ivermectin 1mg
lisinopril 20 mg tablet price lisinopril 20 12.5 mg lisinopril 80 mg tablet
best ed drugs for seniors
Apartments, a duplex and a penthouse in the complex of Taraf LUCE on Palm Jumeirah, Dubai. Developer offers units for sale at favourable prices.
Bet on all your favorite sports at 1xBet
Win Big with 1xBet: The Top Sports Betting Platform
Experience the Excitement of Online Betting with 1xBet
Get in on the Action with 1xBet: The Best Sports Betting Site
Unleash Your Winning Potential with 1xBet
Bet and Win with Confidence at 1xBet
Join the 1xBet Community and Start Winning Today
The Ultimate Sports Betting Experience Awaits at 1xBet
1xBet: Where Champions Are Made
Take Your Betting to the Next Level with 1xBet
Get Ready to Win Big at 1xBet
Multiply Your Winnings with 1xBet’s Exciting Betting Options
Elevate Your Sports Betting Game with 1xBet
Sign Up for 1xBet and Start Winning Instantly
Experience the Thrill of Betting with 1xBet
1xBet: Your Ticket to Winning Big on Sports
Don’t Miss Out on the Action at 1xBet
Join 1xBet Today and Bet on Your Favorite Sports
Winning Has Never Been Easier with 1xBet
Get Started with 1xBet and Discover a World of Betting Opportunities
1x bet app App 1xbet .
dallasrentapart.com
Seasoned Port Builder Vitaliy Yuzhilin, Works in Maritime Infrastructure Development Yuzhilin Vitaliy Aleksandrovich
Seasoned Port Builder Vitaliy Yuzhilin, Works in Maritime Infrastructure Development Vitaliy Yuzhilin
ivermectin where to buy for humans: ivermectin nz – buy ivermectin for humans australia
Настоящий 1вин, проверенный 1win рекомендую однозначно!
Первый, настоящий и оригинальный сайт БК 1win
1xBet: Your Ultimate Betting Destination
1xbet com app download 1xbet 36 .
Nice post. I learn something new and challenging on sites I stumbleupon on a daily basis.
It’s always exciting to read through content from other writers and practice a little something from other websites.
my web page … Toronto Roofing Consultation
safe medicine for erectile dysfunction
O site real Blaze apostas no Brasil
%%
Look into my web-site: https://dongxi.douban.com/link2/?url=https://most-bet-az.com/mostbet-azer-yuekl.html
O site original Blaze apostas no Brasil
best ed drugs over counter
lisinopril 0.5 mg: lisinopril discount – can i order lisinopril online
erectile dysfunction medicine india
%%
Here is my website … https://record-wiki.win/index.php?title=Cnc_router_for_small_business
lisinopril 5mg cost for 2 mg lisinopril lisinopril 10mg
prednisone without rx: online prednisone 5mg – prednisone 2.5 mg daily
new ed drugs
generic ed drugs cost
Давыдов Эдуард http://www.panram.ru/partners/news/biografiya-eduarda-davydova-generalnogo-direktora-bsk-ao/ .
Продажа подержанных автомобилей, все машины проверены и находятся в Москве. Большой каталог БУ автомобилей с пробегом от официального дилера, узнайте на сайте цены и характеристики на бу авто продажа подержанных авто в москве
Продажа подержанных автомобилей, все машины проверены и находятся в Москве. Большой каталог БУ автомобилей с пробегом от официального дилера, узнайте на сайте цены и характеристики на бу авто купить подержанный
lasix tablet furosemide 100mg buy lasix online
natural ed medications
Watch porn
buy ivermectin stromectol: ivermectin ireland – stromectol nz
ed drugs in india
But right before they do, Cut TO: BLACK. This was clearly the ‘50s so it was all lower dwell, and he’d stand in the middle of the space with all the musicians all-around him and they’d do sixty normally takes in a row. Also can I ask for him to do parenting lessons to deal with the troubles of his harassment in his own order to modify? With the father of my oldest 2 kids I was capable to deliver the court docket with documents proving I had not relapsed and they dismissed his declare and awarded me make-up parenting time. The Code of Conduct for the Sexual Exploitation of Children in Travel and Tourism is an intercontinental organisation composed of customers of the tourism field and kid’s rights authorities with the reason to eradicate the observe of kid sex tourism. At the similar time, sexual intercourse segregated community toilets may well boost a gender binary that excludes transgender folks. Sex stores are incredibly rare in Singapore. Those are our levers, our targets. People are so blind. Yeah. People in the early times of the web thought these sites were in some way heading to be better and additional suited to individuals becoming great and communicative to each other.
O site original no Brasil Blaze apostas
Aqui está um ótimo site Blaze apostas
Все рабочие промокод для мостбет при регистрации вы можете найти бесплатно на этом сайте. Используйте промокод *QWERTY777* для получения бонуса до 35000 руб при регистрации. Приятно, что новички могут ввести промокод при регистрации, который даст право на получение приветственного бонуса на сумму до 35000 рублей. Самое главное — это относиться к ставкам и к игре в целом ответственно! Не стоит играть на последние или заемные деньги, стремясь таким образом заработать себе на жизнь.
furosemida: Buy Lasix No Prescription – furosemide 40mg
strongest ed medication
code promo sport 1xbet
O site real no Brasil Blaze apostas
porn videos online
porn videos online
ed medication online pharmacy
prednisone buying prednisone buy canada prednisone 10mg buy online
PЕЇjДЌka 300000 KДЌ
Skype calls are free, video https://tinyurl.com/SquirtCamweb, as
well as the software itself. Users of mobiles,
and iPad can download the Skype app from Apple upstore, while as users can download stretch film from Google Play.
オンラインカジノ
日本にオンラインカジノおすすめランキング2024年最新版
2024おすすめのオンラインカジノ
オンラインカジノはパソコンでしか遊べないというのは、もう一昔前の話。現在はスマホやタブレットなどのモバイル端末からも、パソコンと変わらないクオリティでオンラインカジノを当たり前に楽しむことができるようになりました。
数あるモバイルカジノの中で、当サイトが厳選したトップ5カジノはこちら。
オンラインカジノおすすめ: コニベット(Konibet)
コニベットといえば、キャッシュバックや毎日もらえるリベートボーナスなど豪華ボーナスが満載!それに加えて低い出金条件も見どころです。さらにVIPレベルごとの還元率の高さも業界内で突出している点や、出金速度の速さなどトータルバランスの良さからもハイローラーの方にも好まれています。
カスタマーサポートは365日24時間稼働しているので、初心者の方にも安心してご利用いただけます。
さらに【業界初のオンラインポーカー】を導入!毎日トーナメントも開催されているので、早速参加しちゃいましょう!
RTP(還元率)公開や、入出金対応がスムーズで初心者向き
2000種類以上の豊富なゲーム数を誇り、スロットゲーム多数!
今なら$20の入金不要ボーナスと最大$650還元ボーナス!
8種類以上のライブカジノプロバイダー
業界初オンラインポーカーあり,日本利用者数No.1の安心のオンラインカジノメディア!
おすすめポイント
コニベットは、その豊富なボーナスと高還元率、そして安心のキャッシュバック制度で知られています。まず、新規登録者には入金不要の$20ボーナスが提供され、さらに初回入金時には最大$650の還元ボーナスが得られます。これらのキャンペーンはプレイヤーにとって大きな魅力となっています。
また、コニベットの特徴的な点は、VIP制度です。一度ロイヤルクラブになると、降格がなく、スロットリベートが1.5%という驚異の還元率を享受できます。これは他のオンラインカジノと比較しても非常に高い還元率です。さらに、常時週間損失キャッシュバックも行っているため、不運で負けてしまった場合でも取り返すチャンスがあります。これらの特徴から、コニベットはプレイヤーにとって非常に魅力的なオンラインカジノと言えるでしょう。
コニベット 無料会員登録をする
| コニベットのボーナス
コニベットは、新規登録者向けに20ドルの入金不要ボーナスを用意しています
コニベットカジノでは、限定で初回入金後に残高が1ドル未満になった場合、入金額の50%(最高500ドル)がキャッシュバックされる。キャッシュバック額に出金条件はないため、獲得後にすぐ出金することも可能です。
| コニベットの入金方法
入金方法 最低 / 最高入金
マスターカード 最低 : $20 / 最高 : $6,000
ジェイシービー 最低 : $20/ 最高 : $6,000
アメックス 最低 : $20 / 最高 : $6,000
アイウォレット 最低 : $20 / 最高 : $100,000
スティックペイ 最低 : $20 / 最高 : $100,000
ヴィーナスポイント 最低 : $20 / 最高 : $10,000
仮想通貨 最低 : $20 / 最高 : $100,000
銀行送金 最低 : $20 / 最高 : $10,000
| コニベット出金方法
出金方法 最低 |最高出金
アイウォレット 最低 : $40 / 最高 : なし
スティックぺイ 最低 : $40 / 最高 : なし
ヴィーナスポイント 最低 : $40 / 最高 : なし
仮想通貨 最低 : $40 / 最高 : なし
銀行送金 最低 : $40 / 最高 : なし
lasix 100mg: Buy Furosemide – lasix generic
buying ed drugs online
lasix uses Buy Furosemide lasix
californiarent24.com
belfastinvest.net
thorazine 10mg
lisinopril 2.5: lisinopril prinivil zestril – lisinopril medication prescription
best ed non prescription pill
https://free-promocode.ru/
портативные нагрудные видеорегистраторы https://nagrudnievieoregistratori.ru/
best male ed pills
%%
Look into my blog :: https://bigbamboo-slot.info/
Properties for sale in buy apartment Dubai Creek Harbour. Best off-plan and ready properties.
smcasino7.com
Hongzhi 황제는 “수리해야한다면 돈과 음식이 얼마나 들까요?”
Maxim Shubarev is a Russian entrepreneur, chairman of the Board of Directors of the Setl Group holding Shubarev Maxim
Maxim Shubarev is a Russian entrepreneur, chairman of the Board of Directors of the Setl Group holding Maxim Shubarev
buy ed pills
order stromectol: stromectol for head lice – ivermectin 0.2mg
É aqui que você encontrará o site real Blaze apostas
Узнай все про промокод Mostbet на сегодня. Используй при регистрации действующий промокод Мостбет и получай бонус за первый депозит до 35000р. Действующим участникам БК подскажем, как получать бесплатные промо коды, делая ставки на спорт или вращая слоты уже сегодня! Но обо всем по порядку. Регистрация в 2024 году — мостбет casino промокод. Часто задаваемые вопросы по регистрации и учетной записи у букмекера Mostbet. Активация промокода Mostbet на сегодня. Разнообразие бонусных предложений от Mostbet — другие типы бонусов и промокодов для игроков. Промокод Mostbet на День Рождения. Фрибеты или бесплатные ставки. Тото-промокоды Mostbet. Промокоды Mostbet у блогеров. Система промокодов при регистрации позволяет новым игрокам букмекерской конторы Mostbet получать внушительные бонусные суммы к своему первому депозиту. Обратите внимание, что это не промокод на ставку, а именно на регистрацию. Рабочие промокоды Мостбет на сегодня: Вид бонуса. Размер бонуса.
Branded apartments, duplexes, Skycrest Collection and full floors in the complex of DAMAC Bay 2. Developer DAMAC Properties offers units for sale at favorable prices.
香港娛樂城
LГҐna 100000 kr
Eu recomendo este site Blaze apostas
O site real no Brasil Blaze apostas
stromectol pill for humans: ivermectin 4 – stromectol tablets
medicine for erectile
stromectol online ivermectin 8000 mcg ivermectin malaria
ed dysfunction treatment
lasix 100 mg tablet Buy Furosemide generic lasix
free porn download
teen gangbang
20 mg lisinopril without a prescription: lisinopril medicine – lisinopril 4214
chutneyb.com
Liu Jian은 기침을했습니다. “폐하, 옛 목사는 이미 그것을 읽었습니다.”
californianetdaily.com
morson.org
best ed drugs over counter
guidecannabis.com
ivermectin india: stromectol ivermectin 3 mg – ivermectin
cymbalta 20 mg pharmacy
what is the safest erectile dysfunction drug
best ed treatment
звуковое оборудование для актового зала i-tec1.ru .
ivermectin cream 1: ivermectin 6 – stromectol canada
stromectol 15 mg ivermectin cream cost ivermectin pills
носимый мини видеорегистратор https://nagrudnievieoregistratori.ru/
This is the most essential a part of organising your affiliate program.
Погрузитесь в захватывающий мир азартных игр, где каждый может стать следующим большим победителем игра kent casino
Погрузитесь в захватывающий мир азартных игр, где каждый может стать следующим большим победителем kazino kent
Elle offre des graphismes en 3D particulièrement attrayants et vous permet de jouer avec 10 symboles différents.
в процессе регистрации от самого нового клиента надо согласиться с
правилами казино и Условиями
платформы.
my web-site; лучшее козино
ed pills near me
Более тринадцати лет опыта работы в сексуальном массаже!
my homepage :: эротический массаж Мурманск
ivermectin human: ivermectin lotion cost – ivermectin 50 mg
https://free-promocode.ru/
furosemide 40 mg lasix uses furosemide 100 mg
O site real no Brasil Blaze aposta
Eu recomendo este site real Blaze apostas
O melhor e mais autêntico site Blaze aposta
O melhor site de jogos do Brasil Blaze apostas
questo contenuto
best non prescription ed treatment
porn videos
gilmaire-etienne.com
ivermectin 6 mg tablets: ivermectin 8000 – ivermectin 6 mg tablets
strongest medications for erectile dysfunction
Теневые рынки и их незаконные деятельности представляют значительную угрозу безопасности общества и являются объектом внимания правоохранительных органов по всему миру. В данной статье мы обсудим так называемые подпольные рынки, где возможно покупать нелегальные паспорта, и какие угрозы это несет для граждан и государства.
Теневые рынки представляют собой скрытые интернет-площадки, на которых торгуется разнообразной незаконной продукцией и услугами. Среди этих услуг встречается и продажа поддельных документов, таких как удостоверения личности. Эти рынки оперируют в тайной сфере интернета, используя шифрование и инкогнито платежные системы, чтобы оставаться непостижимыми для правоохранительных органов.
Покупка поддельного паспорта на теневых рынках представляет важную угрозу национальной безопасности. похищение личных данных, фальсификация документов и фальшивые идентификационные материалы могут быть использованы для совершения радикальных актов, мошеннических и прочих преступлений.
Правоохранительные органы в различных странах активно борются с теневыми рынками, проводя операции по выявлению и аресту тех, кто замешан в преступных действиях. Однако, по мере того как технологии становятся более затруднительными, эти рынки могут приспосабливаться и находить новые пути обхода законов.
Для обеспечения своей безопасности от опасностей, связанных с скрытыми рынками, важно проявлять осторожность при обработке своих личной информации. Это включает в себя избегать попыток фишинга, не распространять личной информацией в недоверенных источниках и периодически проверять свои финансовые документы.
Кроме того, общество должно быть информировано о рисках и последствиях покупки поддельных удостоверений. Это способствует формированию более осознанного и ответственного подхода к вопросам безопасности и поможет в борьбе с теневыми рынками. Поддержка законодательных инициатив, направленных на ужесточение наказаний за создание и продажу нелегальных документов, также является важным шагом в борьбе с этими преступлениями
15 mg prednisone daily: price of prednisone 5mg – 20mg prednisone
seo-специалист. раскрутка и расширение сайтов.
my homepage; высокооплачиваемая работа для девушек Новый Уренгой
drugs to treat ed
amoxicillin buy no prescription can you purchase amoxicillin online buy amoxicillin 500mg canada
Автосервис для Машинки: Если ваша машинка начала странности творить, не тревожтесь, у нас есть волшебники, коие отремонтируют ее. Масло, тормоза, двигатель — они там в данном шарят!
Строим Сайты: Желаете свой личный галлактический сайт? У нас есть ребята, которые могут это сделать. Прекрасно, понятно, нетрудно. В том числе и в случае если вы в интернете чайник — не жутко, они объяснят.
Поддержка с Компом: В случае если у вас компьютер тупит, как я в арифметике, не переживайте! Мы вас спасем. Вирусы, глюки, чудеса — наши специалисты разберутся.
Бизнес-Советы: Мечтаете о собственном бизнесе, хотя не понимаете, с чего начать? Мы не бизнесмены, и у нас тут есть знатоки, которые дадут совет, как не “попасть в грабли”.
Шопинг онлайн: Интернет-магазин тем, кто любит нажимать кнопочки и получать посылочки. Тут вещи от наших друзей, проверено — качество замечательное!
https://www.efesmoldova.md/
Поддержка и Общение: У нас как в большой семье, лишь только онлайн. Мы готовы посодействовать, поддержать, поболтать. Время от времени просто принципиально, чтобы был кто-то вблизи.
Инновации и Крутые Штуки: Ну и естесственно, мы смотрим за последними трендами и подкидываем вам интересных штукенций. Девайсы, свежие релизы — мы в курсе и готовы поделиться.
Ясно и Честно: Здесь никто не несомненно будет вас заваливать сложными текстами либо техническим жаргоном. Все просто и понятно, как ребятам.
Доверие и Дружба: Мы не просто сайт, мы приятели. Практически постоянно рады вашим вопросам и услугам. Мы доверяем для вас, и вы можете верить нам.
Результаты и Спасибо: Вот такие у нас приключения. Мы тут, чтобы помочь вам, не зависимо от того, как вы в чем либо разбираетесь. Имущество пожаловать в нашу интернет-семью!
Le service clientèle de All Slots Casino est disponible 24 heures sur 24, 7
jours sur 7, par chat en direct et par e-mail.
allegra 120mg
pills for ed
уничтожение кротов на участке https://eco-life-group.ru/borba-s-gryzunami/unichtozhit-krotov-zemlerojki/
Vilitra 60 mg ist ein wirksames Mittel zur Behandlung von erektiler Dysfunktion. Dieses Produkt produziert ein weltweit bekanntes Pharmaunternehmen Centurion Laboratories vilitra
In 1969, the movie “https://xxxbf.tv/tags/o Blue” became
the first movie where sex was shown without simulation,
which was widely distributed in USA.
my website; https://xxxbf.tv/tags/k
buy lisinopril mexico 10 mg lisinopril tablets buy lisinopril no prescription
Вёрстка страницы представляет собой процесс разработки структуры html-документа, результатом которого является веб-страница Помощник фронтэндера
prednisone 5mg over the counter: average cost of prednisone – buy prednisone online no script
Вёрстка страницы представляет собой процесс разработки структуры html-документа, результатом которого является веб-страница Теги HTML — как они работают и зачем нужны веб-разработчику?
porn MP4
Bet on all your favorite sports at 1xBet
Win Big with 1xBet: The Top Sports Betting Platform
Experience the Excitement of Online Betting with 1xBet
Get in on the Action with 1xBet: The Best Sports Betting Site
Unleash Your Winning Potential with 1xBet
Bet and Win with Confidence at 1xBet
Join the 1xBet Community and Start Winning Today
The Ultimate Sports Betting Experience Awaits at 1xBet
1xBet: Where Champions Are Made
Take Your Betting to the Next Level with 1xBet
Get Ready to Win Big at 1xBet
Multiply Your Winnings with 1xBet’s Exciting Betting Options
Elevate Your Sports Betting Game with 1xBet
Sign Up for 1xBet and Start Winning Instantly
Experience the Thrill of Betting with 1xBet
1xBet: Your Ticket to Winning Big on Sports
Don’t Miss Out on the Action at 1xBet
Join 1xBet Today and Bet on Your Favorite Sports
Winning Has Never Been Easier with 1xBet
Get Started with 1xBet and Discover a World of Betting Opportunities
1xbet 36 1xbet application .
pills for ed online
Luxurious living amidst the skyline of Dubai! Discover opulent penthouses, sky villas, mansions, and palaces in Canal Casa. Indulge in the epitome of elegance and seize the opportunity to own these exclusive units at unbeatable prices. Your dream of a high-end haven awaits!
can you buy lisinopril over the counter: lisinopril 20mg – lisinopril generic cost
O melhor site de cassinos do Brasil Blaze aposta
Aqui você encontra o melhor site do Brasil Blaze aposta
strongest medications for erectile dysfunction
имеется здесь и игра на условные https://playrupokerdom.ru/ фишки.
хургада вода
Discover a world of style and comfort at our furniture store, where every detail is designed to enhance the uniqueness of your space and offer you unparalleled solutions for your home or office Furniture accessories
Discover a world of style and comfort at our furniture store, where every detail is designed to enhance the uniqueness of your space and offer you unparalleled solutions for your home or office Kitchen design
lisinopril 0.5 mg: lisinopril generic drug – buy lisinopril 20 mg online usa
goturkishnews.com
Промокод 1xbet на сегодня актуален, бонус будет зачислен сразу после первого пополнения счета. Временные коды. Букмекерская контора 1xbet часто выступает спонсором при переводе популярных сериалов на русский язык. Рекламные вставки букмекера можно услышать перед началом многих сериалов. Часто в такой рекламе диктуется специальные промокод, дающий возможность беттерам рассчитывать на дополнительный бонус. Максимальный бонус при регистрации составляется 32500 рублей. Воспользоваться промокодом можно только при выполнении ряда условий: Доступно только для беттеров из России, Беларуси, Украины и Казахстана. Возврат игрока – от 18 лет. 1xbet купить промокод. Промокод 1xbet сегодня найти в интернете не так сложно, достаточно воспользоваться любой поисковой системой. Но обращайте внимание на профессиональность ресурса, откуда будет скопирован промокод. Многие сайты предлагают неактуальные бонусные коды, которые не дадут никакого повышенного депозита после регистрации. На нашем сайте представлен актуальный промокод 1xbet на 2024 год. Вводите промокод, чтобы получить 100% сверху после первого пополнения. Минимальная сумма депозита для использования промокода – 100 рублей. Ограничивается бонус 1хбет суммой в 32500 рублей.
le code promo 1xbet
india buy prednisone online can you buy prednisone over the counter in canada generic prednisone online
Изготовление и использование клонов банковских карт является противозаконной практикой, представляющей серьезную угрозу для безопасности финансовых систем и личных средств граждан. В данной статье мы рассмотрим риски и последствия покупки реплик карт, а также как общество и силовые структуры борются с похожими преступлениями.
“Клоны” карт — это незаконно созданные дубликаты банковских карт, которые используются для неправомерных транзакций. Основной метод создания копий — это похищение данных с оригинальной карты и последующее настройка этих данных на другую карту. Злоумышленники, предлагающие услуги по продаже клонов карт, обычно действуют в неявной сфере интернета, где трудно выявить и пресечь их деятельность.
Покупка копий карт представляет собой важное преступление, которое может повлечь за собой серьезные наказания. Покупатель также рискует стать последователем мошенничества, что может привести к судебному преследованию. Основные преступные действия в этой сфере включают в себя кражу личной информации, подделку документов и, конечно же, финансовые мошенничества.
Банки и силовые структуры активно борются с незаконными действиями, связанными с клонированием карт. Банки внедряют последние технологии для определения подозрительных транзакций, а также предлагают услуги по обеспечению безопасности для своих клиентов. Полиция ведут следственные мероприятия и арестуют тех, кто замешан в создании и продаже реплик карт.
Для собственной безопасности важно соблюдать осторожность при использовании банковских карт. Необходимо постоянно проверять выписки, избегать подозрительных сделок и следить за своей личной информацией. Образование и информированность об угрозах также являются важными средствами в борьбе с финансовыми преступлениями.
В заключение, использование реплик банковских карт — это недопустимое и противозаконное действие, которое может привести к тяжким последствиям для тех, кто вовлечен в такую практику. Соблюдение мер предосторожности, осведомленность о возможных потенциальных рисках и сотрудничество с органами порядка играют ключевую роль в предотвращении и пресечении подобных преступлений
нагрудный видеорегистратор для сотрудников https://nagrudnievieoregistratori.ru/
greenhousebali.com
1 mg prednisone daily: 50 mg prednisone tablet – can you buy prednisone over the counter in usa
Generic Ed Drugs Cost
Jump to search
Speculate on market Forex?
Best exclusive offer 2024 for common speculators, software developers, traders, trading signal sellers, trading advisor sellers, trading account managers, investment companies, large brokerage firms , as well as for everyone who dreams of opening their own business on the Forex market with minimal investments.
We will be happy to Give away MetaTrader4 Server for 0Give away MetaTrader4 Server for 0/en/products.html
More in detail watch here:
https://drive.google.com/file/d/14xuST2EFDKcnfUT_dL49jQu0Asj1uJx4/view?usp=sharing
zestril 10 mg lisinopril 10 mg tabs best price for lisinopril
best viagra substitute over counter
Автосервис для Машинки: Если ваша машинка начала странности творить, не беспокойтесь, у нас есть волшебники, коие починят ее. Масло, тормоза, движок — они там в этом шарят!
Возводим Сайты: Хотите свой личный галлактический сайт? У нас есть ребята, которые имеют все шансы это устроить. Красиво, ясно, несложно. В том числе и если вы в интернете чайник — не страшно, они растолкуют.
Помощь с Компом: В случае если у вас компьютер тупит, как я в математике, не переживайте! Мы вас спасем. Микробы, глюки, чудеса — наши специалисты разберутся.
Бизнес-Советы: Мечтаете о собственном бизнесе, но не понимаете, с чего же стоит начать? Мы не бизнесмены, но у нас здесь есть ценители, коие дадут совет, как не “попасть в грабли”.
Шопинг интернет: Интернет-магазин для тех, кто любит налегать кнопки и получать посылочки. Здесь багаж от наших друзей, проверено — качество отличное!
https://mafia.md/
Поддержка и Общение: У нас как в немалый семье, только онлайн. Мы готовы помочь, поддержать, поболтать. Иногда просто принципиально, дабы был кто-то вблизи.
Инновации и Крутые Штуки: Ну и конечно, мы смотрим за последними трендами и подкидываем для вас заманчивых штукенций. Гаджеты, новинки — мы в курсе и готовы поделиться.
Понятно и Честно: Здесь никто не будет вас заваливать сложными текстами либо техническим жаргоном. Все очень просто и понятно, как ребятам.
Доверие и Дружба: Мы не просто сайт, мы приятели. Практически постоянно счастливы вашим вопросам и услугам. Мы доверяем вам, и вы можете верить нам.
Итоги и Спасибо: Вот эти у нас приключения. Мы тут, чтобы посодействовать вам, не зависимо от того, как вы в чем либо разбираетесь. Имущество пожаловать в нашу интернет-семью!
prednisone 15 mg tablet: prednisone 20mg for sale – buy prednisone without prescription paypal
Proxy servers act as intermediaries between clients and destination servers, providing various functionalities such as caching and filtering Forward proxy
оборудование для актового зала школы купить https://i-tec3.ru/ .
Proxy servers act as intermediaries between clients and destination servers, providing various functionalities such as caching and filtering Authentication
ed pills for sale
Recomendo a todos somente este site no Brasil Blaze aposta
where can i get prednisone over the counter: how to buy prednisone – buy prednisone online usa
Somente o Brasil tem esse site original Blaze aposta
Recomendo a todos no Brasil este site Blaze aposta
Um site excelente e autêntico no Brasil Blaze aposta
Superb, what a weblog it is! This webpage provides valuable facts
to us, keep it up.
ed pills for sale
generic amoxicillin over the counter buy amoxicillin 500mg uk amoxicillin over the counter in canada
Предложение использовать промокод бесплатное. Игроку нужно только скопировать код и перейти по соответствующей ссылке. Если код актуальный, игрок получит в дальнейшем какие-то бонусы.
elavil
ed drugs for men
Watches World
In the realm of high-end watches, finding a trustworthy source is essential, and WatchesWorld stands out as a symbol of trust and knowledge. Offering an wide collection of prestigious timepieces, WatchesWorld has garnered praise from satisfied customers worldwide. Let’s delve into what our customers are saying about their encounters.
Customer Testimonials:
O.M.’s Review on O.M.:
“Outstanding communication and follow-up throughout the process. The watch was impeccably packed and in pristine condition. I would certainly work with this team again for a watch purchase.”
Richard Houtman’s Review on Benny:
“I dealt with Benny, who was exceptionally assisting and courteous at all times, preserving me regularly informed of the procedure. Moving forward, even though I ended up sourcing the watch locally, I would still definitely recommend Benny and the company.”
Customer’s Efficient Service Experience:
“A excellent and efficient service. Kept me up to date on the order progress.”
Featured Timepieces:
Richard Mille RM30-01 Automatic Winding with Declutchable Rotor:
Price: €285,000
Year: 2023
Reference: RM30-01 TI
Patek Philippe Complications World Time 38.5mm:
Price: €39,900
Year: 2019
Reference: 5230R-001
Rolex Oyster Perpetual Day-Date 36mm:
Price: €76,900
Year: 2024
Reference: 128238-0071
Best Sellers:
Bulgari Serpenti Tubogas 35mm:
Price: On Request
Reference: 101816 SP35C6SDS.1T
Bulgari Serpenti Tubogas 35mm (2024):
Price: €12,700
Reference: 102237 SP35C6SPGD.1T
Cartier Panthere Medium Model:
Price: €8,390
Year: 2023
Reference: W2PN0007
Our Experts Selection:
Cartier Panthere Small Model:
Price: €11,500
Year: 2024
Reference: W3PN0006
Omega Speedmaster Moonwatch 44.25 mm:
Price: €9,190
Year: 2024
Reference: 304.30.44.52.01.001
Rolex Oyster Perpetual Cosmograph Daytona 40mm:
Price: €28,500
Year: 2023
Reference: 116500LN-0002
Rolex Oyster Perpetual 36mm:
Price: €13,600
Year: 2023
Reference: 126000-0006
Why WatchesWorld:
WatchesWorld is not just an web-based platform; it’s a commitment to personalized service in the realm of high-end watches. Our group of watch experts prioritizes trust, ensuring that every customer makes an knowledgeable decision.
Our Commitment:
Expertise: Our team brings matchless knowledge and insight into the world of luxury timepieces.
Trust: Confidence is the foundation of our service, and we prioritize transparency in every transaction.
Satisfaction: Customer satisfaction is our paramount goal, and we go the extra mile to ensure it.
When you choose WatchesWorld, you’re not just purchasing a watch; you’re committing in a seamless and trustworthy experience. Explore our collection, and let us assist you in finding the ideal timepiece that reflects your taste and sophistication. At WatchesWorld, your satisfaction is our proven commitment
pragmatic-ko.com
결국 Fang Jifan은 손을 뻗을 때 웃는 얼굴로 사람들을 때리지 않는 진실을 이해합니다.
ivermectin 50ml: stromectol 3 mg dosage – stromectol 15 mg
cyprus-welcome.com
lasix furosemide Buy Lasix No Prescription buy lasix online
online platform for watches
In the world of high-end watches, locating a trustworthy source is essential, and WatchesWorld stands out as a symbol of confidence and knowledge. Presenting an broad collection of esteemed timepieces, WatchesWorld has garnered praise from happy customers worldwide. Let’s delve into what our customers are saying about their experiences.
Customer Testimonials:
O.M.’s Review on O.M.:
“Outstanding communication and aftercare throughout the procedure. The watch was flawlessly packed and in mint condition. I would certainly work with this group again for a watch purchase.”
Richard Houtman’s Review on Benny:
“I dealt with Benny, who was extremely supportive and courteous at all times, keeping me regularly informed of the process. Moving forward, even though I ended up sourcing the watch locally, I would still definitely recommend Benny and the company.”
Customer’s Efficient Service Experience:
“A excellent and prompt service. Kept me up to date on the order progress.”
Featured Timepieces:
Richard Mille RM30-01 Automatic Winding with Declutchable Rotor:
Price: €285,000
Year: 2023
Reference: RM30-01 TI
Patek Philippe Complications World Time 38.5mm:
Price: €39,900
Year: 2019
Reference: 5230R-001
Rolex Oyster Perpetual Day-Date 36mm:
Price: €76,900
Year: 2024
Reference: 128238-0071
Best Sellers:
Bulgari Serpenti Tubogas 35mm:
Price: On Request
Reference: 101816 SP35C6SDS.1T
Bulgari Serpenti Tubogas 35mm (2024):
Price: €12,700
Reference: 102237 SP35C6SPGD.1T
Cartier Panthere Medium Model:
Price: €8,390
Year: 2023
Reference: W2PN0007
Our Experts Selection:
Cartier Panthere Small Model:
Price: €11,500
Year: 2024
Reference: W3PN0006
Omega Speedmaster Moonwatch 44.25 mm:
Price: €9,190
Year: 2024
Reference: 304.30.44.52.01.001
Rolex Oyster Perpetual Cosmograph Daytona 40mm:
Price: €28,500
Year: 2023
Reference: 116500LN-0002
Rolex Oyster Perpetual 36mm:
Price: €13,600
Year: 2023
Reference: 126000-0006
Why WatchesWorld:
WatchesWorld is not just an internet platform; it’s a promise to personalized service in the world of luxury watches. Our team of watch experts prioritizes confidence, ensuring that every customer makes an well-informed decision.
Our Commitment:
Expertise: Our group brings exceptional understanding and insight into the realm of luxury timepieces.
Trust: Trust is the basis of our service, and we prioritize openness in every transaction.
Satisfaction: Customer satisfaction is our ultimate goal, and we go the extra mile to ensure it.
When you choose WatchesWorld, you’re not just purchasing a watch; you’re investing in a smooth and trustworthy experience. Explore our collection, and let us assist you in discovering the perfect timepiece that embodies your taste and sophistication. At WatchesWorld, your satisfaction is our proven commitment
otc ed drugs that work
amoxicillin 30 capsules price: amoxicillin 500 tablet – amoxicillin over the counter in canada
уничтожение тараканов в Москве https://eco-life-group.ru/borba-s-nasekomymi/unichtozhit-tarakanov/
miamicottages.com
most potent ed pills
Проектируем и строим сборно-разборные веранды для летнего кафе и ресторана, внедряем умные-системы в рабочие процессы и устанавливаем системы автоматизации веранд веранда пристроенная к дому
best male ed pills
cheap stromectol: stromectol 3 mg tablets price – cost of ivermectin medicine
Payday loans in Nebraska
https://europe-parfum.ru/new/pages/kak_rabotaet_giperbaricheskaya_kamera__1.html
amoxicillin no prescipion where can i buy amoxicillin over the counter amoxicillin pills 500 mg
Recomendo o site real no Brasil Blaze aposta
strongest medications for erectile dysfunction
https://www.gilmaire-etienne.com/wp-content/pages/code-promo-1xbet-cote-d-ivoire-bonus-200.html?cn-reloaded=1
orlistat 120 mg canada
ivermectin 2mg: ivermectin 6 tablet – ivermectin 3mg tab
O site real no Brasil está apenas aqui Blaze aposta
No Brasil, este é o único lugar onde se pode encontrar o site original Blaze aposta
Want to know more about a specific phone number?Number Tracker is the solution for you. With our advanced technology, you can easily track any phone number and get detailed information about the caller http://verywellsys.com/bbs/board.php?bo_table=service&wr_id=156630
Want to know more about a specific phone number?Number Tracker is the solution for you. With our advanced technology, you can easily track any phone number and get detailed information about the caller http://cluster.shao.ac.cn/i18n/index.php?title=_Exploring_the_Cultural_Implications_of_Phone_Location_Tracking
ivermectin price canada stromectol sales ivermectin 6 mg tablets
porn videos
highest rated ed medication
LГҐn 100000
porn videos
non prescription erectile dysfunction pills
where can i get prednisone: prednisone over the counter cost – cost of prednisone 5mg tablets
cheap rosuvastatin
ed treatment in india
lasix online: lasix generic name – furosemide 100 mg
repaircanada.net
Турецкие сериалы стали невероятно популярными во всем мире. Турция славится интересным кинематографом с неповторимым сюжетом, эмоциональными переживаниями и потрясающей игрой актеров.
Турецкие сериалы имеют различные жанры, на любой вкус. От романтических комедий до фильмов-историй, от триллеров до фантастики – есть жанры на любой вкус. Богатство сюжетов и уровень съемок делают турецкие сериалы невероятными изобретениями мирового кинематографа.
Посмотреть турецкий сериал – это крутой способ отправиться в другую культуру, узнать больше о традициях и обычаях Турции.
detroitapartment.net
Использование банковских карт является неотъемлемой частью современного общества. Карты предоставляют комфорт, секретность и широкие возможности для проведения финансовых сделок. Однако, кроме легального использования, существует негативная сторона — вывод наличных средств, когда карты используются для снятия денег без согласия владельца. Это является незаконным действием и влечет за собой строгие санкции.
Кэшаут карт представляет собой практики, направленные на извлечение наличных средств с карты, необходимые для того, чтобы обойти систему защиты и уведомлений, предусмотренных банком. К сожалению, такие преступные действия существуют, и они могут привести к материальным убыткам для банков и клиентов.
Одним из методов обналичивания карт является использование технических хитростей, таких как кража данных с магнитных полос карт. Магнитный обман — это техника, при котором мошенники устанавливают аппараты на банкоматах или терминалах оплаты, чтобы считывать информацию с магнитной полосы карты. Полученные данные затем используются для создания копии карты или проведения онлайн-операций.
Другим распространенным методом является ловушка, когда преступники отправляют недобросовестные письма или создают поддельные веб-сайты, имитирующие банковские ресурсы, с целью доступа к конфиденциальным данным от клиентов.
Для борьбы с обналичиванием карт банки осуществляют разные действия. Это включает в себя повышение уровня безопасности, внедрение двухфакторной аутентификации, мониторинг транзакций и подготовка клиентов о техниках предотвращения мошенничества.
Клиентам также следует быть активными в гарантировании защиты своих карт и данных. Это включает в себя регулярное изменение паролей, контроль банковских выписок, а также осторожность по отношению к сомнительным транзакциям.
Вывод наличных средств — это тяжкое преступление, которое причиняет урон не только финансовым учреждениям, но и обществу в целом. Поэтому важно соблюдать бдительность при пользовании банковскими картами, быть информированным о методах мошенничества и соблюдать меры безопасности для предотвращения потери средств
ed pills online india
деньги быстро онлайн http://topruscredit.ru/ .
Актуальный доступ к ссылкам и зеркалам площадки Kraken уже у вас. Ознакомьтесь с надежными методами доступа и гарантированными мерами безопасности kraken сайт
credito 4500 euros
lisinopril cheap brand lisinopril tablets india generic lisinopril 10 mg
Актуальный доступ к ссылкам и зеркалам площадки Kraken уже у вас. Ознакомьтесь с надежными методами доступа и гарантированными мерами безопасности кракен зеркало
Sat confiavel no Brasil Blaze aposta
https://altay-info.ru/news/pages/zagolovok_puteshestviya_menyayut_ghizny_top_7_prichin_otpravitysya_navstrechu_priklyuchen.html
order ed pills
ivermectin brand: ivermectin 400 mg brands – buy ivermectin for humans uk
lasix 100 mg tablet Over The Counter Lasix furosemide
https://www.inserrh.com/media/pgs/code-promo-1xbet-congo-bonus-221-000-cdf.html
60 mg prednisone daily: prednisone 20mg tablets where to buy – prednisone 5mg price
ed drugs list
Hello
is viagra the best ed drug
Микрозаймы на карточку Сбера без отказа найдите здесь
https://sravni-zaimy.ru/
вино Франция купить
ivermectin 5 mg: ivermectin 1 topical cream – stromectol where to buy
best prescription ed drugs
In the realm of luxury watches, discovering a trustworthy source is crucial, and WatchesWorld stands out as a symbol of confidence and knowledge. Presenting an wide collection of renowned timepieces, WatchesWorld has accumulated acclaim from content customers worldwide. Let’s delve into what our customers are saying about their encounters.
Customer Testimonials:
O.M.’s Review on O.M.:
“Excellent communication and follow-up throughout the process. The watch was impeccably packed and in perfect condition. I would certainly work with this group again for a watch purchase.”
Richard Houtman’s Review on Benny:
“I dealt with Benny, who was exceptionally assisting and courteous at all times, keeping me regularly informed of the procedure. Moving forward, even though I ended up acquiring the watch locally, I would still definitely recommend Benny and the company.”
Customer’s Efficient Service Experience:
“A highly efficient and swift service. Kept me up to date on the order progress.”
Featured Timepieces:
Richard Mille RM30-01 Automatic Winding with Declutchable Rotor:
Price: €285,000
Year: 2023
Reference: RM30-01 TI
Patek Philippe Complications World Time 38.5mm:
Price: €39,900
Year: 2019
Reference: 5230R-001
Rolex Oyster Perpetual Day-Date 36mm:
Price: €76,900
Year: 2024
Reference: 128238-0071
Best Sellers:
Bulgari Serpenti Tubogas 35mm:
Price: On Request
Reference: 101816 SP35C6SDS.1T
Bulgari Serpenti Tubogas 35mm (2024):
Price: €12,700
Reference: 102237 SP35C6SPGD.1T
Cartier Panthere Medium Model:
Price: €8,390
Year: 2023
Reference: W2PN0007
Our Experts Selection:
Cartier Panthere Small Model:
Price: €11,500
Year: 2024
Reference: W3PN0006
Omega Speedmaster Moonwatch 44.25 mm:
Price: €9,190
Year: 2024
Reference: 304.30.44.52.01.001
Rolex Oyster Perpetual Cosmograph Daytona 40mm:
Price: €28,500
Year: 2023
Reference: 116500LN-0002
Rolex Oyster Perpetual 36mm:
Price: €13,600
Year: 2023
Reference: 126000-0006
Why WatchesWorld:
WatchesWorld is not just an online platform; it’s a promise to individualized service in the realm of luxury watches. Our staff of watch experts prioritizes confidence, ensuring that every client makes an well-informed decision.
Our Commitment:
Expertise: Our group brings matchless understanding and insight into the realm of luxury timepieces.
Trust: Confidence is the foundation of our service, and we prioritize transparency in every transaction.
Satisfaction: Client satisfaction is our ultimate goal, and we go the extra mile to ensure it.
When you choose WatchesWorld, you’re not just purchasing a watch; you’re committing in a effortless and reliable experience. Explore our collection, and let us assist you in discovering the perfect timepiece that mirrors your style and sophistication. At WatchesWorld, your satisfaction is our proven commitment
Поставляем цемент М500 с заводов производителей напрямую, работаем с тендерами, собственный парк а/м – доставка от 20т бесплатно фасовка цемента в мешки
se dette
event-miami24.com
buy lasix online Over The Counter Lasix lasix generic
3 lisinopril: lisinopril 40 mg for sale – prinivil 10 mg
generic ed drugs india
mumu
workingholiday365.com
Выбирайте и покупайте надежные конвейерные весы для горной массы. Автоматические весы непрерывного действия по выгодным ценам весы конвейерные 1600 600 0 5
cost for generic lisinopril lisinopril 3 prinivil medication
strongest medications for erectile dysfunction
smcasino-game.com
Hongzhi 황제는 그들을 모두 흥분하게 바라 보았습니다.
porn 3GP
where can i get amoxicillin 500 mg: medicine amoxicillin 500mg – amoxicillin 500mg pill
best drugs for ed
これを見てください
lasix for sale: Buy Lasix No Prescription – lasix 40 mg
generic ed pills from india
Поспрашивайте у своих знакомых,
приятелей, родственников, возможно, они недавно
пользовались услугами опытной няни, или у них на.
My homepage :: няня для младенца
just enter more links for submit site to google for indexing.
with siteguru you can implement content audit in series simple stages, and track all others problems blog.
my website :: get indexed by google fast
Так и до бесконечности не далеко 🙂
Also read the rules of “no-show”, https://www.ecommercebytes.com/R/R/chart.pl?CHTL&101107&AmazonPayments&https://linktr.ee/luckyrent if you will arrive late, you can stay without your bike, since it happens is rented to others.
non prescription erection pills
order prednisone with mastercard debit prednisone over the counter australia prednisone drug costs
caribbean21.com
housebru.com
best Porn
furosemide 100 mg: Buy Lasix – furosemide
Watches World
In the realm of luxury watches, finding a dependable source is paramount, and WatchesWorld stands out as a symbol of trust and expertise. Offering an extensive collection of esteemed timepieces, WatchesWorld has garnered praise from happy customers worldwide. Let’s dive into what our customers are saying about their encounters.
Customer Testimonials:
O.M.’s Review on O.M.:
“Outstanding communication and aftercare throughout the process. The watch was flawlessly packed and in perfect condition. I would certainly work with this group again for a watch purchase.”
Richard Houtman’s Review on Benny:
“I dealt with Benny, who was extremely supportive and courteous at all times, maintaining me regularly informed of the procedure. Moving forward, even though I ended up acquiring the watch locally, I would still definitely recommend Benny and the company.”
Customer’s Efficient Service Experience:
“A very good and swift service. Kept me up to date on the order progress.”
Featured Timepieces:
Richard Mille RM30-01 Automatic Winding with Declutchable Rotor:
Price: €285,000
Year: 2023
Reference: RM30-01 TI
Patek Philippe Complications World Time 38.5mm:
Price: €39,900
Year: 2019
Reference: 5230R-001
Rolex Oyster Perpetual Day-Date 36mm:
Price: €76,900
Year: 2024
Reference: 128238-0071
Best Sellers:
Bulgari Serpenti Tubogas 35mm:
Price: On Request
Reference: 101816 SP35C6SDS.1T
Bulgari Serpenti Tubogas 35mm (2024):
Price: €12,700
Reference: 102237 SP35C6SPGD.1T
Cartier Panthere Medium Model:
Price: €8,390
Year: 2023
Reference: W2PN0007
Our Experts Selection:
Cartier Panthere Small Model:
Price: €11,500
Year: 2024
Reference: W3PN0006
Omega Speedmaster Moonwatch 44.25 mm:
Price: €9,190
Year: 2024
Reference: 304.30.44.52.01.001
Rolex Oyster Perpetual Cosmograph Daytona 40mm:
Price: €28,500
Year: 2023
Reference: 116500LN-0002
Rolex Oyster Perpetual 36mm:
Price: €13,600
Year: 2023
Reference: 126000-0006
Why WatchesWorld:
WatchesWorld is not just an online platform; it’s a dedication to customized service in the world of high-end watches. Our team of watch experts prioritizes confidence, ensuring that every customer makes an informed decision.
Our Commitment:
Expertise: Our team brings matchless understanding and perspective into the realm of high-end timepieces.
Trust: Confidence is the basis of our service, and we prioritize transparency in every transaction.
Satisfaction: Client satisfaction is our paramount goal, and we go the additional step to ensure it.
When you choose WatchesWorld, you’re not just purchasing a watch; you’re committing in a seamless and reliable experience. Explore our collection, and let us assist you in discovering the ideal timepiece that embodies your taste and elegance. At WatchesWorld, your satisfaction is our proven commitment
furosemida 40 mg furosemide generic lasix
generic prednisone tablets: prednisone pharmacy prices – best pharmacy prednisone
Implementing a slightly different approach to visual decorations of the game,
the provider separated the table grid from the wheel.
вино Франция
amoxicillin 875 mg tablet: amoxicillin 500mg capsule – can you buy amoxicillin over the counter in canada
prednisone 10mg tabs: online order prednisone – prednisone 7.5 mg
Биография руководителя «Башкирской содовой компании» Эдуард Давыдов Рождение в семье увлеченных наукой родителей предопределило жизненный путь Эдуарда Давыдова, чье детство прошло в атмосфере постоянного стремления к знаниям и самосовершенствованию.
prestamo 300000 euros
1хбет зеркало рабочее
Villas in Altissima Al Barari with favourable terms of purchase and return on investment.
Загадочная страна на пересечении культур
– Отпуск мечты: турция на моря
купить тур в турцию https://www.anex-tour-turkey.ru/ .
britainrental.com
Отдых для влюбленных пар
– Дельфины и пляжи: турция туры 2021
подбор тура anex-tour-turkey.ru .
укладка экстренной медицинской помощи
oneworldmiami.com
Best video – munichinique.laip.gt
–
PЕЇjДЌka 800000 KДЌ
Идеальный отдых для двоих в Турции
отдых турция tez-tour-turkey.ru .
Как провести идеальный отпуск
– Великолепные города: турция тур
тур на море https://www.anex-tour-turkey.ru/ .
Медицинское оборудование по выгодным ценам. Купить медоборудование диагностическое, медтехнику. Огромный выбор медтехники где купить медицинское оборудование
Незабываемые впечатления для всей семьи
– Турция без визы: турция туроператор
путевки турция https://anex-tour-turkey.ru/ .
ceftin 500mg
1xbet 1хбет скачать
1хбет сегодня
Отпуск мечты: туры в Турцию
путевка в турцию все включено с перелетом цена http://www.tez-tour-turkey.ru/ .
ed pills levitra https://fintryides.com/
купить армянский коньяк
Роскошные курорты Турции
горящие путевки tez-tour-turkey.ru .
LГҐna 50000 kr
seroquel 100mg
Микрозаймы на карточку Сбера без отказа можно найти здесь
https://nakartuzaim.ru/
Obtaining medications can sometimes feel like navigating through a labyrinth Particularly when seeking specialty drugs like Topiramate topamax 100mg us
Generic Ed Drugs Cost https://fintryides.com/
Релаксация на туре в Турцию
тур турция https://tez-tour-turkey.ru/ .
Obtaining medications can sometimes feel like navigating through a labyrinth Particularly when seeking specialty drugs like Topiramate brand topiramate 100mg
https://gorod-buketov.ru/ цветы с доставкой мск
– Идеальный отдых: тур в Турцию
туры в турции http://www.anex-tour-turkey.ru/ .
online ed drugs for purchase https://fintryides.com/
Написание эссе на заказ осуществляется нашими профессиональными авторами. Цена ВКР бакалавра купить зависит от ее объема и сложности заказать лабораторную работу
Написание эссе на заказ осуществляется нашими профессиональными авторами. Цена ВКР бакалавра купить зависит от ее объема и сложности заказать школьный проект
generic ed drugs https://fintryides.com/
купить аттестат классов https://www.rudik-attestats.com .
сайт 1хбет
legit erectile dysfunction pills https://fintryides.com/
best online pharmacy india top online pharmacy india india online pharmacy
https://gorod-buketov.ru/ купить цветы с доставкой мск
reputable indian pharmacies indian pharmacies safe buy medicines online in india
vevobahis581.com
what is the safest erectile dysfunction drug https://fintryides.com/
newmexicodesign.net
buy medicines online in india reputable indian pharmacies online pharmacy india
best ed treatment https://fintryides.com/
Профильные трубы 40х20 мм. Закажите по низкой цене от производителя с доставкой по Москве. Предлагаем самые приятные цены в городе и области профильная труба 25 25
Профильные трубы 40х20 мм. Закажите по низкой цене от производителя с доставкой по Москве. Предлагаем самые приятные цены в городе и области труба профильная электросталь купить
купить коньяк армения
Як підвищити ефективність роботи за допомогою косметологічного обладнання
https://ukrmedgarant.com.ua/p300308208-apparat-ultrazvukovoj-terapii.html .
1хбет вход регистрация
http://smartmedreminder.com/
Политик последние новости
luogo
даркнет вход
Даркнет – скрытая зона всемирной паутины, избегающая взоров обычных поисковых систем и требующая дополнительных средств для доступа. Этот анонимный уголок сети обильно насыщен ресурсами, предоставляя доступ к различным товарам и услугам через свои даркнет списки и справочники. Давайте глубже рассмотрим, что представляют собой эти списки и какие тайны они хранят.
Даркнет Списки: Окна в Скрытый Мир
Даркнет списки – это вид врата в неощутимый мир интернета. Каталоги и индексы веб-ресурсов в даркнете, они позволяют пользователям отыскивать различные услуги, товары и информацию. Варьируя от форумов и магазинов до ресурсов, уделяющих внимание аспектам анонимности и криптовалютам, эти перечни предоставляют нам возможность заглянуть в неизведанный мир даркнета.
Категории и Возможности
Теневой Рынок:
Даркнет часто ассоциируется с незаконными сделками, где доступны самые разные товары и услуги – от наркотиков и оружия до украденных данных и услуг наемных убийц. Каталоги ресурсов в данной категории облегчают пользователям находить подходящие предложения без лишних усилий.
Форумы и Сообщества:
Даркнет также предоставляет площадку для анонимного общения. Форумы и сообщества, представленные в реестрах даркнета, затрагивают различные темы – от информационной безопасности и взлома до политических аспектов и философских концепций.
Информационные Ресурсы:
На даркнете есть ресурсы, предоставляющие информацию и инструкции по обходу цензуры, защите конфиденциальности и другим темам, интересным тем, кто хочет сохранить свою конфиденциальность.
Безопасность и Осторожность
Несмотря на скрытность и свободу, даркнет не лишен рисков. Мошенничество, кибератаки и незаконные сделки являются неотъемлемой частью этого мира. Взаимодействуя с даркнет списками, пользователи должны соблюдать предельную осмотрительность и придерживаться мер безопасности.
Заключение
Реестры даркнета – это путь в неизведанный мир, где сокрыты тайны и возможности. Однако, как и в любой неизведанной территории, путешествие в темную сеть требует особой бдительности и знаний. Не всегда анонимность приносит безопасность, и использование темной сети требует осознанного подхода. Независимо от ваших интересов – будь то технические детали в области кибербезопасности, поиск необычных товаров или исследование новых возможностей в интернете – реестры даркнета предоставляют ключ
best prescription ed drugs https://fintryides.com/
список сайтов даркнет
Темная сторона интернета – таинственная зона всемирной паутины, избегающая взоров обычных поисковых систем и требующая эксклюзивных средств для доступа. Этот скрытый уголок сети обильно насыщен сайтами, предоставляя доступ к различным товарам и услугам через свои даркнет списки и справочники. Давайте ближе рассмотрим, что представляют собой эти списки и какие тайны они хранят.
Даркнет Списки: Порталы в Тайный Мир
Индексы веб-ресурсов в темной части интернета – это своего рода порталы в неощутимый мир интернета. Перечни и указатели веб-ресурсов в даркнете, они позволяют пользователям отыскивать различные услуги, товары и информацию. Варьируя от форумов и магазинов до ресурсов, уделяющих внимание аспектам анонимности и криптовалютам, эти перечни предоставляют нам шанс заглянуть в неизведанный мир даркнета.
Категории и Возможности
Теневой Рынок:
Даркнет часто связывается с незаконными сделками, где доступны разнообразные товары и услуги – от наркотических препаратов и стрелкового вооружения до похищенной информации и помощи наемных убийц. Каталоги ресурсов в этой категории облегчают пользователям находить нужные предложения без лишних усилий.
Форумы и Сообщества:
Даркнет также предоставляет площадку для анонимного общения. Форумы и сообщества, перечисленные в даркнет списках, охватывают широкий спектр – от информационной безопасности и взлома до политики и философии.
Информационные Ресурсы:
На даркнете есть ресурсы, предоставляющие сведения и руководства по преодолению цензуры, обеспечению конфиденциальности и другим темам, интересным тем, кто хочет сохранить свою конфиденциальность.
Безопасность и Осторожность
Несмотря на анонимность и свободу, даркнет не лишен рисков. Мошенничество, кибератаки и незаконные сделки присущи этому миру. Взаимодействуя с даркнет списками, пользователи должны соблюдать максимальную осторожность и придерживаться мер безопасности.
Заключение
Даркнет списки – это ключ к таинственному миру, где сокрыты тайны и возможности. Однако, как и в любой неизведанной территории, путешествие в темную сеть требует особой бдительности и знаний. Анонимность не всегда гарантирует безопасность, и использование темной сети требует осмысленного подхода. Независимо от ваших интересов – будь то технические аспекты кибербезопасности, поиск уникальных товаров или исследование новых граней интернета – реестры даркнета предоставляют ключ
Путешествие в волшебную Турцию
путевки на море https://tez-tour-turkey.ru/ .
1xbet мобильная
Даркнет – это сегмент интернета, которая остается скрытой от обычных поисковых систем и требует специального программного обеспечения для доступа. В этой анонимной зоне сети существует масса ресурсов, включая различные списки и каталоги, предоставляющие доступ к разнообразным услугам и товарам. Давайте рассмотрим, что представляет собой каталог даркнета и какие тайны скрываются в его глубинах.
Теневые каталоги: Врата в анонимность
Для начала, что такое теневой каталог? Это, по сути, каталоги или индексы веб-ресурсов в даркнете, которые позволяют пользователям находить нужные услуги, товары или информацию. Эти списки могут варьироваться от чатов и магазинов до ресурсов, специализирующихся на различных аспектах анонимности и криптовалют.
Категории и Возможности
Теневой Рынок:
Даркнет часто ассоциируется с рынком андеграунда, где можно найти различные товары и услуги, включая наркотики, оружие, украденные данные и даже услуги профессиональных устрашителей. Списки таких ресурсов позволяют пользователям без труда находить подобные предложения.
Форумы и Сообщества:
Даркнет также предоставляет платформы для анонимного общения. Форумы и группы на теневых каталогах могут заниматься обсуждением тем от интернет-безопасности и взлома до политики и философии.
Информационные ресурсы:
Есть ресурсы, предоставляющие информацию и инструкции по обходу цензуры, защите конфиденциальности и другим темам, интересным пользователям, стремящимся сохранить анонимность.
Безопасность и Осторожность
При всей своей анонимности и свободе действий темная сторона интернета также несет риски. Мошенничество, кибератаки и незаконные сделки становятся частью этого мира. Пользователям необходимо проявлять максимальную осторожность и соблюдать меры безопасности при взаимодействии с списками теневых ресурсов.
Заключение: Врата в Неизведанный Мир
Даркнет списки предоставляют доступ к скрытым уголкам сети, где сокрыты тайны и возможности. Однако, как и в любой неизведанной территории, важно помнить о возможных рисках и осознанно подходить к использованию даркнета. Анонимность не всегда гарантирует безопасность, и путешествие в этот мир требует особой осторожности и знания.
Независимо от того, интересуетесь ли вы техническими аспектами интернет-безопасности, ищете уникальные товары или просто исследуете новые грани интернета, теневые каталоги предоставляют ключ
Даркнет – неведомая зона интернета, избегающая взоров обыденных поисковых систем и требующая дополнительных средств для доступа. Этот анонимный уголок сети обильно насыщен платформами, предоставляя доступ к различным товарам и услугам через свои каталоги и индексы. Давайте подробнее рассмотрим, что представляют собой эти списки и какие тайны они хранят.
Даркнет Списки: Порталы в Скрытый Мир
Даркнет списки – это вид порталы в неощутимый мир интернета. Каталоги и индексы веб-ресурсов в даркнете, они позволяют пользователям отыскивать разнообразные услуги, товары и информацию. Варьируя от форумов и магазинов до ресурсов, уделяющих внимание аспектам анонимности и криптовалютам, эти перечни предоставляют нам возможность заглянуть в неизведанный мир даркнета.
Категории и Возможности
Теневой Рынок:
Даркнет часто ассоциируется с подпольной торговлей, где доступны самые разные товары и услуги – от психоактивных веществ и стрелкового оружия до похищенной информации и услуг наемных убийц. Каталоги ресурсов в подобной категории облегчают пользователям находить нужные предложения без лишних усилий.
Форумы и Сообщества:
Даркнет также предоставляет площадку для анонимного общения. Форумы и сообщества, перечисленные в даркнет списках, затрагивают различные темы – от компьютерной безопасности и хакерских атак до политики и философии.
Информационные Ресурсы:
На даркнете есть ресурсы, предоставляющие информацию и инструкции по преодолению цензуры, обеспечению конфиденциальности и другим темам, которые могут быть интересны тем, кто хочет остаться анонимным.
Безопасность и Осторожность
Несмотря на скрытность и свободу, даркнет полон рисков. Мошенничество, кибератаки и незаконные сделки являются неотъемлемой частью этого мира. Взаимодействуя с реестрами даркнета, пользователи должны соблюдать максимальную осторожность и придерживаться мер безопасности.
Заключение
Даркнет списки – это врата в неизведанный мир, где скрыты секреты и возможности. Однако, как и в любой неизведанной территории, путешествие в даркнет требует особой осторожности и знания. Не всегда анонимность приносит безопасность, и использование даркнета требует осознанного подхода. Независимо от ваших интересов – будь то технические детали в области кибербезопасности, поиск необычных товаров или исследование новых возможностей в интернете – реестры даркнета предоставляют ключ
Оптимальные грузовые перевозки по Харькову
заказать переезд https://moving-company-kharkov.com.ua .
Арктика – северная полярная область Земли, включающая окраины материков Евразии и Северной Америки, почти весь Северный Ледовитый океан с островами и прилегающие к нему части Атлантического и Тихого океанов. Название её происходит от греческого слова arctos (медведь) и связано со звёздами: Полярная звезда, находящаяся почти точно в зените над Северным полюсом, принадлежит к созвездию Малая Медведица.
п»їlegitimate online pharmacies india best online pharmacy india buy medicines online in india
Подпольная сфера сети – таинственная сфера всемирной паутины, избегающая взоров обыденных поисковых систем и требующая эксклюзивных средств для доступа. Этот скрытый ресурс сети обильно насыщен сайтами, предоставляя доступ к различным товарам и услугам через свои даркнет списки и индексы. Давайте подробнее рассмотрим, что представляют собой эти реестры и какие тайны они хранят.
Даркнет Списки: Ворота в Тайный Мир
Даркнет списки – это своего рода порталы в скрытый мир интернета. Каталоги и индексы веб-ресурсов в даркнете, они позволяют пользователям отыскивать различные услуги, товары и информацию. Варьируя от форумов и магазинов до ресурсов, уделяющих внимание аспектам анонимности и криптовалютам, эти перечни предоставляют нам шанс заглянуть в непознанный мир даркнета.
Категории и Возможности
Теневой Рынок:
Даркнет часто связывается с подпольной торговлей, где доступны самые разные товары и услуги – от психоактивных веществ и стрелкового оружия до краденых данных и услуг наемных убийц. Списки ресурсов в этой категории облегчают пользователям находить нужные предложения без лишних усилий.
Форумы и Сообщества:
Даркнет также предоставляет площадку для анонимного общения. Форумы и сообщества, указанные в каталогах даркнета, затрагивают широкий спектр – от компьютерной безопасности и хакерских атак до политических аспектов и философских концепций.
Информационные Ресурсы:
На даркнете есть ресурсы, предоставляющие информацию и инструкции по преодолению цензуры, обеспечению конфиденциальности и другим темам, которые могут быть интересны тем, кто хочет остаться анонимным.
Безопасность и Осторожность
Несмотря на анонимность и свободу, даркнет не лишен рисков. Мошенничество, кибератаки и незаконные сделки становятся частью этого мира. Взаимодействуя с даркнет списками, пользователи должны соблюдать предельную осмотрительность и придерживаться мер безопасности.
Заключение
Списки даркнета – это врата в неизведанный мир, где хранятся тайны и возможности. Однако, как и в любой неизведанной территории, путешествие в темную сеть требует особой внимания и знаний. Не всегда анонимность приносит безопасность, и использование темной сети требует осознанного подхода. Независимо от ваших интересов – будь то технические аспекты кибербезопасности, поиск уникальных товаров или исследование новых граней интернета – реестры даркнета предоставляют ключ
Грузовые перевозки в Харькове
перевозка мусора https://www.moving-company-kharkov.com.ua .
https://seo116.ru/
Getting your hands on medication can sometimes not be as straightforward as we would like unfortunately, cost is a significant affecting factor when it comes to essential medicines cheap maxalt 10mg
rebetol 150mg
Грузовые перевозки на заказ
компания переезд http://www.moving-company-kharkov.com.ua .
Профессиональные услуги по грузоперевозкам
услуги переезда недорого http://www.moving-company-kharkov.com.ua .
what is the best non prescription erectile dysfunction https://fintryides.com/
Getting your hands on medication can sometimes not be as straightforward as we would like unfortunately, cost is a significant affecting factor when it comes to essential medicines brand maxalt 10mg
Вы ошибаетесь. Давайте обсудим.
обычно, https://verstakdoma.ru/stati/novosti/razreshenie-na-stroitelstvo-linejnogo-obekta-nyuansy-polucheniya/ стройка является длительным процессом и не всегда получается успеть в запланированный график.
I want to change my car, but i can’t choose between bmw and audi. Can somebody plz help me with this decition? Model list is here https://bs4.site BLACK SPRUT MARKET https://bs4.site
Extract files in a secure place your computer.
to guarantee security скачать steam desktop authenticator, do not forget to
get steam guard backup codes!
Lainaa 7000 euroa
new porn videos of 2024
ed pills for sale https://fintryides.com/
Write more, thats all I have to say. Literally, it seems as though you
relied on the video to make your point. You obviously know what youre talking about, why waste your
intelligence on just posting videos to your blog when you could be giving us something informative to read?
greengo-shop
india online pharmacy Online medicine order buy medicines online in india
yangsfitness.com
낮에 겁에 질린 그는 놀라고 화를 내며 걱정스럽게 Ouyang Zhi를 바라 보았다.
is viagra the best ed drug https://fintryides.com/
mail order pharmacy india buy medicines online in india indian pharmacies safe
Быстрые и надежные грузоперевозки
услуги переезда https://www.moving-company-kharkov.com.ua .
Sex HD
можно купить аттестат http://gruppa-attestats.com/ .
generic ed pills from india https://fintryides.com/
דירות דיסקרטיות באשדוד תמונות
В мире здравоохранения отзывы пациентов играют ключевую роль, предоставляя ценную обратную связь о качестве медицинского обслуживания. Доктор Юрий Шульга, выдающийся врач, привлекает внимание не только своей медицинской экспертизой, но и положительным влиянием, оказанным на своих пациентов Юрий Шульга отзивы
1хбет бонус за регистрацию без депозита
Косметологическое оборудование Zemits – инновационные эстетические технологии для успешного развития Вашего СПА-бизнеса https://zemits.com.ua/blog/tpost/gg1un0euc1-kak-vibrat-apparat-dlya-rf-liftinga-molo
Payday loans in Texas
ed pills canada https://fintryides.com/
Косметологическое оборудование Zemits – инновационные эстетические технологии для успешного развития Вашего СПА-бизнеса https://ukrmedgarant.com.ua/p1372901681-zemits-lumibetter-apparat.html
Монтаж систем отопления, водоснабжения, вентиляции, канализации, очистки воды, пылеудаления, снеготаяния, геосистем в Краснодаре под ключ. ПРОФЕССИОНАЛЬНЫЕ ИНЖЕНЕРНЫЕ РЕШЕНИЯ ДЛЯ ДОМА установка котла монтаж отопления
pharmacy website india best india pharmacy indian pharmacy paypal
best treatment for ed in india https://fintryides.com/
lfchungary.com
거의 아침부터 밤까지 거의 두 달 동안의 연습은 결코 멈추지 않았습니다.
медтехника ведущих брендов для дома. Всегда оптимальные цены, акции , скидки и отличный сервис. Afbiet
porn
медтехника ведущих брендов для дома. Всегда оптимальные цены, акции , скидки и отличный сервис. Szlkti
india pharmacy mail order Online medicine order indian pharmacy
фильм смотреть
смотреть фильм
Kredit 100000 Euro
best non prescription ed supplements https://fintryides.com/
сериал бесплатно
сериал бесплатно
otc ed drugs that work https://fintryides.com/
Gambling
hihouse420.com
Hongzhi 황제는 안도의 한숨을 쉬고 Xie Qian과 Li Dongyang을 바라 보았습니다.
https://greengo-shop.ru/
strongest medications for erectile dysfunction https://fintryides.com/
At this moment I am going away to do my breakfast, when having
my breakfast coming yet again to read additional news.
best ed non prescription pill https://patriciaalanpaen.wordpress.com/
Як вибрати оптимальну спецтехніку
спецтехніка україна http://www.spectehnika-sksteh.co.ua/ .
allegra cheap
WOW just what I was searching for. Came here by
searching for Link alternatif Login Foxibet
Яка спецтехніка найбільш популярна
спец техніка https://www.spectehnika-sksteh.co.ua/ .
ed medication online pharmacy https://patriciaalanpaen.wordpress.com/
Тенденции в digital-маркетинге для строительных организаций
продвижение строительных сайтов https://seo-prodvizhenie-sajtov-stroitelnyh-kompanij.ru/ .
Эффективные методы
9. Как провести качественную установку кондиционера
кондиционер с установкой ustanovit-kondicioner.ru .
Як обрати спецтехніку за потребами
спецтехніка чернівці http://spectehnika-sksteh.co.ua/ .
Як вибрати оптимальну спецтехніку
продаж спецтехніки бу https://www.spectehnika-sksteh.co.ua/ .
strongest ed medication https://patriciaalanpaen.wordpress.com/
Компания предлагает обширный ассортимент услуг по изготовлению чеков на все случаи жизни. Вы точно сможете найти индивидуальное решение бюрократических проблем Купить кассовые чеки
Просто милашки!!
then we will expand proposed topic by introducing the surrounding world of pornography. The reality is such what is not especially important whether http://lanpanya.com/papangkorn/?p=1 addiction is classified as a real addiction.
Компания предлагает обширный ассортимент услуг по изготовлению чеков на все случаи жизни. Вы точно сможете найти индивидуальное решение бюрократических проблем Заказать чеки Казань
Discreet apartments in Ashdo
Лучшие юристы и адвокаты оказывают бесплатные юридические консультации по телефону и в офисе компании. Квалифицированная юридическая помощь по всем отраслям права бесплатная юридическая консультация по телефону 8-800
generic ed drugs https://patriciaalanpaen.wordpress.com/
Vavada casino
amoxicillin vs ciprofloxacin
1. Как установить кондиционер в доме
кондиционер цена http://www.ustanovit-kondicioner.ru/ .
В «Содержание» если необходимо продолжения записи заголовка раздела или подраздела на второй (последующей)
строке его начинают на.
my web blog – курсовая
Лучшие юристы и адвокаты оказывают бесплатные юридические консультации по телефону и в офисе компании. Квалифицированная юридическая помощь по всем отраслям права помощь юриста бесплатно по телефону москва
Vavada
1хбет официальный
ed pills cheap https://patriciaalanpaen.wordpress.com/
https://onlinecasinos.com.cy/
п»їcytotec pills online: order cytotec online – buy cytotec online fast delivery
Профессиональные советы
6. Как выбрать место для установки кондиционера
gree кондиционер http://ustanovit-kondicioner.ru/ .
cheap ed medications online https://patriciaalanpaen.wordpress.com/
Важные аспекты
7. Топ ошибок при установке кондиционера
монтаж кондиционера цена http://ustanovit-kondicioner.ru/ .
how to buy diflucan online: purchase diflucan – buy diflucan uk
inhoud
Vitaliy Aleksandrovich Yuzhilin https://en.wikipedia.org/wiki/vitaliy_aleksandrovich_yuzhilin .
Як обрати спецтехніку за потребами
спецтехніка купити https://www.spectehnika-sksteh.co.ua/ .
наливной пол отзывы
ed drugs available in canada https://patriciaalanpaen.wordpress.com/
LГҐn 8000 kr
buying ed pills https://patriciaalanpaen.wordpress.com/
Каталог смартфонов Apple iPhone 14 с ценами, фото и описанием. Все модели Айфон 14 в наличии. Купить оригинальную технику и аксессуары в магазине макбук кишинев
where to get diflucan without a prescription: diflucan gel – how much is diflucan
ciprofloxacin over the counter cipro ciprofloxacin cipro
ed drugs generic https://patriciaalanpaen.wordpress.com/
tamoxifen endometrium: nolvadex for sale – tamoxifen for breast cancer prevention
erectile dysfunction medications from india https://patriciaalanpaen.wordpress.com/
treatments for ed https://patriciaalanpaen.wordpress.com/
Честный обзор на популярную букмекерскую контору 1win поможет вам узнать все преимущества и недостатки этого сайта для ставок, включая коэффициенты, линию событий, способах и скорости выплат, бонусы и многое другое. Изучите все исходы и выгодные предложения, перейдя на официальный сайт БК 1win официальный сайт
Честный обзор на популярную букмекерскую контору 1win поможет вам узнать все преимущества и недостатки этого сайта для ставок, включая коэффициенты, линию событий, способах и скорости выплат, бонусы и многое другое. Изучите все исходы и выгодные предложения, перейдя на официальный сайт БК 1win скачать
Компания ООО специализируется на проектировании и изготовлении электронагревателей и нагревательных элементов промышленного назначения
buy ciprofloxacin: where can i buy cipro online – buy ciprofloxacin
best ed drugs for seniors https://patriciaalanpaen.wordpress.com/
lfchungary.com
Jiang Bin은 매우 감사했고 Ma Wensheng과 함께 학교 운동장을 걸었습니다.
Цены в нашем прейскуранте не завышены и они значительно ниже, чем вы сможете найти в Москве и Московской области, к тому же, диагностика и выезд на дом при заказе ремонта не оплачиваются https://zapchasti-remont.ru/shop/kolenvalyi_i_shatunyi1/
buy cytotec over the counter buy cytotec in usa buy cytotec pills online cheap
https://leon-bk-bonus.ru/
best ed drugs over counter https://patriciaalanpaen.wordpress.com/
ciprofloxacin 500mg buy online: buy cipro online canada – ciprofloxacin order online
Как выбрать идеальный кондиционер
кондиционер со сплит системой https://www.prodazha-kondicionera.ru/ .
antibiotics cipro ciprofloxacin over the counter cipro ciprofloxacin
Stomatologurmonsk Полезные советы для будущих мам
Почему важно регулярно посещать стоматолога?
https://forum.analysisclub.ru/index.php/topic,99634.new.html#new/ .
ed dysfunction treatment https://patriciaalanpaen.wordpress.com/
Дешевые кондиционеры в продаже
бытовые кондиционеры https://www.prodazha-kondicionera.ru/ .
casino
prevacid 5mg
Кондиционеры на распродаже
кондиционер установка http://prodazha-kondicionera.ru/ .
best free porn
Лидеры продаж кондиционеров
кондиционеры и вентиляция http://www.prodazha-kondicionera.ru .
Gates of olympus nedir
best non prescription ed treatment https://patriciaalanpaen.wordpress.com/
tamoxifen warning: tamoxifen endometrium – tamoxifen citrate
ed drugs from canada https://patriciaalanpaen.wordpress.com/
buy cipro: ciprofloxacin generic price – cipro online no prescription in the usa
purchase cytotec cytotec buy online usa Cytotec 200mcg price
best over the counter ed pills https://patriciaalanpaen.wordpress.com/
а вот абсолютно ваше свободное время, которое человек решает сэкономить на какую-то полезную, интересную, приятную, развивающую или.
Feel free to visit my web-site :: https://forum.dneprcity.net/showthread.php?t=325728&highlight=%F1%FD%EA%EE%ED%EE%EC%E8%F2%FC
LГҐn 4000
buy cytotec over the counter buy cytotec cytotec abortion pill
Автомобильная навигационная карта всегда оформляется сделанная из топографической карты масштаба – от одного:
10000 до 1:25000 путём.
Here is my web site: https://karty-dorog.ru/
inderal 20mg
erectile dysfunction medications https://patriciaalanpaen.wordpress.com/
Provavelmente o melhor site de jogos do Brasil Blaze aposta
Original site here no Brasil Blaze aposta
https://polbetonstroy.ru/
You can find the original site in Brazil here Blaze aposta
Magnífico no site original do Brasil Blaze aposta
new drugs for ed https://patriciaalanpaen.wordpress.com/
ciprofloxacin order online: ciprofloxacin generic – ciprofloxacin generic price
Кондиционеры со скидкой
кондиционеры москва prodazha-kondicionera.ru .
cheap ed drugs from canada https://patriciaalanpaen.wordpress.com/
natural alternatives to tamoxifen: buy tamoxifen – hysterectomy after breast cancer tamoxifen
casino
1xbet indir
where to get diflucan without a prescription: diflucan cost – can you diflucan over the counter
cheap ed drugs online https://patriciaalanpaen.wordpress.com/
Hello there! This is kind of off topic but I need some guidance from an established blog. Is it hard to set up your own blog? I’m not very techincal but I can figure things out pretty fast. I’m thinking about making my own but I’m not sure where to begin. Do you have any ideas or suggestions? With thanks
my web-site http://Esmartech.Co.kr/bbs/board.php?bo_table=free&wr_id=308769
надо тож обязательно посатреть**)
Фитисов. – М.: Альпина Паблишер, Новости Европы и мира 2020. – 144 p. Наконец, продвижение сети, появление сетевых сми привело к тому, что новостные сайты в настоящий момент распространяются практически в течение считанных секунд по всему миру.
купить аттестат классов http://russkiy-attestat.com/ .
Victoria Parking is a private parking lot located nearby to the renaissance newark airport hotel lot at Newark Airport.
Here is my site; one newark center airport parking
ciprofloxacin order online buy generic ciprofloxacin cipro for sale
tamoxifen premenopausal: tamoxifen pill – tamoxifen alternatives premenopausal
https://mosttr-1.com/
only in 5 BLOCKS FROM O’Hare AIRPORT! located
to a short drive from Chicago O’Hare International Airport baymont by wyndham.
Feel free to visit my web site: routes airport parking
non prescription erectile dysfunction pills https://patriciaalanpaen.wordpress.com/
В последнее период стали известными запросы о переводах без предоплат – предложениях, предоставляемых в интернете, где пользователям обещают осуществление заказа или предоставление товара перед внесения денег. Впрочем, за этой привлекающей внимание выгодой могут быть прятаться значительные риски и неблагоприятные следствия.
Привлекательная сторона бесплатных переводов:
Привлекательность концепции переводов без предоплат заключается в том, что клиенты приобретают сервис или продукцию, не выплачивая первоначально средства. Данное условие может казаться прибыльным и удобным, особенно для тех, кто избегает рисковать деньгами или претерпеть мошенничеством. Однако, прежде чем погрузиться в сферу безоплатных переводов, необходимо принять во внимание ряд существенных аспектов.
Опасности и негативные следствия:
Мошенничество и недобросовестные действия:
За порядочными проектами без предварительной оплаты скрываются мошенники, приготовленные воспользоваться уважение клиентов. Попав в их ловушку, вы рискуете потерять не только это, услуги но и денег.
Сниженное качество работ:
Без обеспечения оплаты исполнителю услуги может быть мало мотивации предоставить качественную работу или продукт. В итоге заказчик останется недовольным, а поставщик услуг не подвергнется значительными последствиями.
Утрата данных и безопасности:
При передаче персональных данных или данных о банковских счетах для безоплатных переводов имеется риск раскрытия данных и последующего ихнего неправомерного использования.
Советы по безопасным заливам:
Поиск информации:
Перед выбором безоплатных заливов осуществите тщательное анализ исполнителя. Мнения, рейтинговые оценки и репутация могут быть хорошим показателем.
Предоплата:
Если возможно, старайтесь согласовать часть вознаграждения вперед. Это может сделать сделку более безопасной и гарантирует вам больший объем контроля.
Достоверные платформы:
Отдавайте предпочтение использованию надежных площадок и систем для заливов. Это уменьшит риск обмана и повысит шансы на получение наилучших качественных услуг.
Заключение:
Несмотря на очевидную привлекательность, заливы без предварительной оплаты несут в себе опасности и потенциальные опасности. Осторожность и осмотрительность при выборе исполнителя или сервиса способны предотвратить нежелательные ситуации. Важно запомнить, что безоплатные заливы способны превратиться в причиной проблем, и разумное принятие решения способствует избежать потенциальных проблем
https://feo-kazak.ru/
pulmicort coupon
Теневая зона – это таинственная и незнакомая территория интернета, где существуют особые правила, возможности и опасности. Ежедневно в мире теневой сети происходят события, о которые стандартные пользователи могут только подозревать. Давайте рассмотрим последние новости из теневой зоны, которые отражают настоящие тренды и события в данном таинственном пространстве сети.”
Тенденции и События:
“Эволюция Технологий и Безопасности:
В теневом интернете постоянно развиваются технологии и подходы защиты. Информация о внедрении улучшенных платформ шифрования, скрытия личности и защиты персональной информации свидетельствуют о желании участников и разработчиков к поддержанию надежной среды.”
“Новые Теневые Площадки:
Следуя динамикой запроса и предложения, в даркнете появляются совершенно новые торговые площадки. Новости о открытии цифровых рынков подаривают пользователям различные варианты для купли-продажи товарами и сервисами
Generic Ed Drugs Fda Approved https://patriciaalanpaen.wordpress.com/
Покупка паспорта в интернет-магазине – это незаконное и опасное действие, которое может послужить причиной к серьезным негативным последствиям для граждан. Вот некоторые сторон, о которые необходимо запомнить:
Нарушение законодательства: Покупка удостоверения личности в онлайн магазине представляет собой преступлением закона. Имение фальшивым документом может сопровождаться криминальную наказание и серьезные штрафы.
Риски личной безопасности: Обстоятельство применения поддельного паспорта способен подвергнуть угрозу вашу безопасность. Люди, использующие поддельными документами, способны стать объектом провокаций со со стороны правоохранительных структур.
Финансовые потери: Часто мошенники, торгующие поддельными паспортами, могут использовать ваши личные данные для мошенничества, что приведёт к денежным убыткам. Личные и финансовые сведения могут оказаться использованы в криминальных целях.
Проблемы при перемещении: Фальшивый паспорт может быть обнаружен при переезде пересечь границы или при контакте с государственными органами. Такое обстоятельство способно привести к аресту, депортации или иным тяжелым проблемам при путешествиях.
Утрата доверия и престижа: Применение фальшивого паспорта способно привести к потере доверия со со стороны сообщества и нанимателей. Такая обстановка может негативно сказаться на вашу престиж и карьерные возможности.
Вместо того, чтобы рисковать своей независимостью, безопасностью и престижем, рекомендуется соблюдать законодательство и использовать официальными путями для оформления документов. Они предусматривают защиту всех ваших прав и гарантируют безопасность ваших информации. Нелегальные действия могут повлечь за собой неожиданные и вредные последствия, создавая серьезные проблемы для вас и ваших ваших окружения
http://дверьсервис24.рф
Apartments in Sama Yas with favourable terms of purchase and return on investment.
вскрыть замок Красносельском
вскрытие замков Пушкин
https://1wintr-4.xyz/
mens erection pills https://patriciaalanpaen.wordpress.com/
Даркнет 2024: Теневые аспекты виртуального мира
С инициации даркнет был собой закуток интернета, где секретность и неявность становились обыденностью. В 2024 году этот темный мир продвигается вперед, предоставляя дополнительные требования и риски для сообщества в сети. Рассмотрим, какие тенденции и модификации предстоят обществу в даркнете 2024.
Технологический прогресс и Повышение анонимности
С прогрессом техники, инструменты для обеспечения скрытности в даркнете становятся сложнее и действенными. Использование криптовалют, современных шифровальных методов и сетей с децентрализованной структурой делает отслеживание за поведением участников более сложным для силовых структур.
Рост специализированных рынков
Даркнет-рынки, специализирующиеся на разнообразных продуктах и сервисах, продолжают расширяться. Психотропные вещества, военные припасы, средства для хакерских атак, персональная информация – спектр товаров бывает все более многообразным. Это порождает сложность для силовых структур, который сталкивается с задачей адаптироваться к изменяющимся сценариям преступной деятельности.
Опасности цифровой безопасности для непрофессионалов
Сервисы аренды хакерских услуг и мошеннические схемы остаются активными в теневом интернете. Обычные пользователи попадают в руки целью для преступников в сети, желающих зайти к личным данным, счетам в банке и иных секретных данных.
Перспективы виртуальной реальности в даркнете
С развитием технологий виртуальной реальности, даркнет может перейти в совершенно новую фазу, предоставляя участникам более реалистичные и захватывающие виртуальные пространства. Это может включать в себя новыми формами преступной деятельности, такими как цифровые рынки для передачи виртуальными товарами.
Борьба структурам безопасности
Силы безопасности улучшают свои технологии и методы противостояния даркнетом. Коллективные меры государств и международных организаций ориентированы на предотвращение киберпреступности и прекращение современным проблемам, которые возникают в связи с развитием скрытого веба.
Заключение
Теневой интернет в 2024 году остается комплексной и многогранной обстановкой, где технические инновации продолжают вносить изменения в ландшафт преступной деятельности. Важно для участников оставаться настороженными, гарантировать свою кибербезопасность и соблюдать законы, даже при нахождении в цифровой среде. Вместе с тем, борьба с теневым интернетом требует совместных усилиях от стран, технологических компаний и граждан, для обеспечения безопасность в сетевой среде.
вскрыть замок Красногвардейском
В последние годы интернет изменился в неиссякаемый источник знаний, сервисов и продуктов. Однако, среди множества виртуальных магазинов и площадок, есть темная сторона, известная как даркнет магазины. Данный уголок виртуального мира создает свои опасные сценарии и сопровождается серьезными опасностями.
Что такое Даркнет Магазины:
Даркнет магазины являются онлайн-платформы, доступные через скрытые браузеры и специальные программы. Они действуют в глубоком вебе, невидимом от обычных поисковых систем. Здесь можно обнаружить не только торговцев запрещенными товарами и услугами, но и различные преступные схемы.
Категории Товаров и Услуг:
Даркнет магазины продают широкий ассортимент товаров и услуг, от наркотиков и оружия до хакерских услуг и похищенных данных. На этой темной площадке работают торговцы, дающие возможность приобретения запрещенных вещей без риска быть выслеженным.
Риски для Пользователей:
Легальные Последствия:
Покупка запрещенных товаров на даркнет магазинах ставит под угрозу пользователей риску столкнуться с полицией. Уголовная ответственность может быть значительным следствием таких покупок.
Мошенничество и Обман:
Даркнет тоже представляет собой плодородной почвой для мошенников. Пользователи могут попасть в обман, где оплата не приведет к получению в руки товара или услуги.
Угрозы Кибербезопасности:
Даркнет магазины предоставляют услуги хакеров и киберпреступников, что создает реальными угрозами для безопасности данных и конфиденциальности.
Распространение Преступной Деятельности:
Экономика даркнет магазинов способствует распространению преступной деятельности, так как обеспечивает инфраструктуру для нелегальных транзакций.
Борьба с Проблемой:
Усиление Кибербезопасности:
Улучшение кибербезопасности и технологий слежения помогает бороться с даркнет магазинами, превращая их менее доступными.
Законодательные Меры:
Принятие строгих законов и их решительная реализация направлены на предупреждение и кара пользователей даркнет магазинов.
Образование и Пропаганда:
Увеличение осведомленности о рисках и последствиях использования даркнет магазинов может снизить спрос на незаконные товары и услуги.
Заключение:
Даркнет магазины доступ к темным уголкам интернета, где появляются теневые фигуры с преступными планами. Разумное использование ресурсов и повышенная бдительность необходимы, чтобы защитить себя от рисков, связанных с этими темными магазинами. В сумме, безопасность и соблюдение законов должны быть на первом месте, когда идет речь об виртуальных покупках
вскрыть сейф спб
замена ручки
вскрытие замков Кронштадтский
ed pills non prescription https://patriciaalanpaen.wordpress.com/
вскрыть замок Сосновый бор
ремонт магнитных замков
Grandes ganhos em jogos no Brasil aqui Blaze aposta
ciprofloxacin order online cipro for sale buy ciprofloxacin
ремонт замков
Comece a jogar no Brasil aqui Blaze aposta
Jogue e ganhe no Brasil aqui Blaze aposta
вскрыть замок Петродворцовом
Grandes vitórias no Brasil aqui Blaze aposta
вскрыть замок Ломоносов
drugs to treat ed https://patriciaalanpaen.wordpress.com/
вскрыть замок Девяткино
вскрыть замок Парнас
buy cipro cheap п»їcipro generic п»їcipro generic
вскрыть авто спб
вскрытие замков Василеостровском
cheap erectile dysfunction pills https://patriciaalanpaen.wordpress.com/
cheap ed medications online https://patriciaalanpaen.wordpress.com/
19. Практические советы по монтажу кондиционера своими силами
мастер кондиционер montazh-kondicionera-moskva.ru .
https://testumi8.ru/
Он эффективен в отношении микробов, вирусов, плесени, грибка. Процедура озонирования квартиры направлена на общую глубокую дезинфекцию помещения дезінфекція вентиляції
anflt dhczw hyxtm frrpi yddvr ejhef
lfchungary.com
그들은 이런 모욕을 당하려고 잔치에 온 것이 아닙니다.
3. Этапы профессионального монтажа кондиционера
ремонт кондиционер https://www.montazh-kondicionera-moskva.ru .
Он эффективен в отношении микробов, вирусов, плесени, грибка. Процедура озонирования квартиры направлена на общую глубокую дезинфекцию помещения озонування салону автомобіля
8. Как сэкономить на монтаже кондиционера?
кондиционер ремонт https://montazh-kondicionera-moskva.ru/ .
cobyc nelxy uplic iepkw oijiw lukcv
9. Как правильно подготовиться к монтажу кондиционера?
кондиционер gree http://www.montazh-kondicionera-moskva.ru .
tricor
eqtgb atahl raeno kkswt artah rafwu
tamoxifen and depression tamoxifen citrate tamoxifen and uterine thickening
https://1xbettur-2.com/
Grandes premios e apostas altas no Brasil no site Blaze aposta
tinsl rtupe hjwqw sbvyg bybip wrxkl
Aqui está o site original no Brasil Blaze aposta
winbet
Grandes prêmios e ótimas chances no Brasil no site Blaze aposta
Você pode jogar no Brasil e ganhar no Blaze aposta
mostbet indir
imfvs cedat ljhvt phkgf jicbx mdguz
Your article helped me a lot, is there any more related content? Thanks! https://www.binance.info/de-CH/join?ref=WTOZ531Y
What’s up to every body, it’s my first pay a quick visit of this web site; this web site contains remarkable and in fact good information in favor of
readers.
cqrbz xccav jlsrr ihdke gstep zojua
doxycycline 100 mg doxycycline generic 100mg doxycycline
ljtsq nenic znitp xfkjh ecicg dgdta
Lainaa 8000 euroa
16. Как выбрать оптимальное место для установки кондиционера?
стоимость кондиционера с установкой https://montazh-kondicionera-moskva.ru .
tamoxifen and grapefruit clomid nolvadex buy tamoxifen
raqqr xplam yzueo zywcm uswav xrxfl
srame zyryk bacyi gfrsn ssgde dfdkn
visita el sitio web
сварочный лазерный аппарат по металлу http://www.apparaty-lazernoy-svarki.ru/ .
tdhvl hmxhm bbdok qfzsm swrgm zhous
даркнет вход
Даркнет – скрытое пространство Интернета, доступен только только для тех, кому знает правильный вход. Этот таинственный уголок виртуального мира служит местом для скрытных транзакций, обмена информацией и взаимодействия прячущимися сообществами. Однако, чтобы погрузиться в этот темный мир, необходимо преодолеть несколько барьеров и использовать эксклюзивные инструменты.
Использование эксклюзивных браузеров: Для доступа к даркнету обычный браузер не подойдет. На помощь приходят подходящие браузеры, такие как Tor (The Onion Router). Tor позволяет пользователям обходить цензуру и обеспечивает анонимность, помечая и перенаправляя запросы через различные серверы.
Адреса в даркнете: Обычные домены в даркнете заканчиваются на “.onion”. Для поиска ресурсов в даркнете, нужно использовать поисковики, адаптированные для этой среды. Однако следует быть осторожным, так как далеко не все ресурсы там законны.
Защита анонимности: При посещении даркнета следует принимать меры для обеспечения анонимности. Использование виртуальных частных сетей (VPN), блокировщиков скриптов и антивирусных программ является принципиальным. Это поможет избежать различных угроз и сохранить конфиденциальность.
Электронные валюты и биткоины: В даркнете часто используются криптовалютные средства, в основном биткоины, для неизвестных транзакций. Перед входом в даркнет следует ознакомиться с основами использования электронных валют, чтобы избежать финансовых рисков.
Правовые аспекты: Следует помнить, что многие действия в даркнете могут быть незаконными и противоречить законам различных стран. Пользование даркнетом несет риски, и несанкционированные действия могут привести к серьезным юридическим последствиям.
Заключение: Даркнет – это тайное пространство сети, наполненное анонимности и тайн. Вход в этот мир требует присущих только навыков и предосторожности. При всем мистическом обаянии даркнета важно помнить о возможных рисках и последствиях, связанных с его использованием.
Даркнет список
Введение в Даркнет: Уточнение и Основные Характеристики
Пояснение термина даркнета, его отличий от привычного интернета, и фундаментальных черт этого таинственного мира.
Каким образом Войти в Темный Интернет: Руководство по Анонимному Входу
Подробное описание шагов, требуемых для входа в даркнет, включая использование эксклюзивных браузеров и инструментов.
Адресация сайтов в Темном Интернете: Тайны .onion-Доменов
Пояснение, как функционируют .onion-домены, и какие ресурсы они содержат, с акцентом на секурном поисковой активности и использовании.
Безопасность и Анонимность в Даркнете: Меры для Пользовательской Защиты
Рассмотрение техник и инструментов для сохранения анонимности при использовании даркнета, включая виртуальные частные сети и инные средства.
Электронные Валюты в Даркнете: Роль Биткоинов и Криптовалют
Исследование использования цифровых валют, в основном биткоинов, для осуществления анонимных транзакций в даркнете.
Поиск в Темном Интернете: Специфика и Опасности
Рассмотрение поисковых механизмов в даркнете, предупреждения о возможных рисках и нелегальных ресурсах.
Правовые Аспекты Темного Интернета: Последствия и Последствия
Рассмотрение законных аспектов использования даркнета, предупреждение о возможных юридических последствиях.
Темный Интернет и Информационная Безопасность: Потенциальные Опасности и Противозащитные Действия
Анализ потенциальных киберугроз в даркнете и рекомендации по обеспечению безопасности от них.
Даркнет и Социальные Сети: Скрытое Общение и Группы
Рассмотрение влияния даркнета в области социальных взаимодействий и формировании скрытых сообществ.
Будущее Темного Интернета: Тенденции и Предсказания
Предсказания развития даркнета и возможные изменения в его структуре в будущем.
Взлом Телеграм: Легенды и Фактичность
Телеграм – это известный мессенджер, отмеченный своей высокой степенью шифрования и защиты данных пользователей. Однако, в современном цифровом мире тема вторжения в Телеграм периодически поднимается. Давайте рассмотрим, что на самом деле стоит за этим понятием и почему взлом Telegram чаще является мифом, чем фактом.
Кодирование в Telegram: Основные принципы Безопасности
Телеграм известен своим превосходным уровнем кодирования. Для обеспечения конфиденциальности переписки между участниками используется протокол MTProto. Этот протокол обеспечивает полное шифрование, что означает, что только передающая сторона и получатель могут читать сообщения.
Легенды о Взломе Telegram: Почему они возникают?
В последнее время в интернете часто появляются утверждения о нарушении Telegram и возможности доступа к личным данным пользователей. Однако, большинство этих утверждений оказываются мифами, часто развивающимися из-за непонимания принципов работы мессенджера.
Кибератаки и Раны: Фактические Опасности
Хотя взлом Телеграма в большинстве случаев является трудной задачей, существуют реальные угрозы, с которыми сталкиваются пользователи. Например, кибератаки на индивидуальные аккаунты, вредоносные программы и другие методы, которые, тем не менее, требуют в личном участии пользователя в их распространении.
Охрана Личной Информации: Рекомендации для Пользователей
Несмотря на отсутствие точной опасности нарушения Telegram, важно соблюдать основные правила кибербезопасности. Регулярно обновляйте приложение, используйте двухэтапную проверку, избегайте сомнительных ссылок и фишинговых атак.
Итог: Реальная Опасность или Излишняя беспокойство?
Взлом Телеграма, как обычно, оказывается неоправданным страхом, созданным вокруг обсуждаемой темы без явных доказательств. Однако безопасность всегда остается приоритетом, и участники мессенджера должны быть бдительными и следовать рекомендациям по сохранению безопасности своей персональных данных
isdra qjslh vkvyp dgqnk eqvib sqhmx
20000 Euro Kredit
Взлом WhatsApp: Фактичность и Мифы
WhatsApp – один из известных мессенджеров в мире, широко используемый для обмена сообщениями и файлами. Он прославился своей шифрованной системой обмена данными и гарантированием конфиденциальности пользователей. Однако в интернете время от времени появляются утверждения о возможности нарушения WhatsApp. Давайте разберемся, насколько эти утверждения соответствуют реальности и почему тема взлома WhatsApp вызывает столько дискуссий.
Шифрование в Вотсап: Охрана Личной Информации
WhatsApp применяет точка-точка шифрование, что означает, что только передающая сторона и получающая сторона могут понимать сообщения. Это стало основой для доверия многих пользователей мессенджера к защите их личной информации.
Легенды о Взломе WhatsApp: По какой причине Они Появляются?
Интернет периодически заполняют слухи о взломе Вотсап и возможном входе к переписке. Многие из этих утверждений часто не имеют обоснований и могут быть результатом паники или дезинформации.
Реальные Угрозы: Кибератаки и Безопасность
Хотя нарушение WhatsApp является сложной задачей, существуют реальные угрозы, такие как кибератаки на отдельные аккаунты, фишинг и вредоносные программы. Соблюдение мер безопасности важно для минимизации этих рисков.
Защита Личной Информации: Советы Пользователям
Для укрепления охраны своего аккаунта в Вотсап пользователи могут использовать двухфакторную аутентификацию, регулярно обновлять приложение, избегать подозрительных ссылок и следить за конфиденциальностью своего устройства.
Заключение: Реальность и Осторожность
Нарушение Вотсап, как правило, оказывается трудным и маловероятным сценарием. Однако важно помнить о актуальных угрозах и принимать меры предосторожности для сохранения своей личной информации. Соблюдение рекомендаций по безопасности помогает поддерживать конфиденциальность и уверенность в использовании мессенджера
eva elfie: eva elfie – eva elfie modeli
1. Где купить кондиционер: лучшие магазины и выбор
2. Как выбрать кондиционер: советы по покупке
3. Кондиционеры в наличии: где купить прямо сейчас
4. Купить кондиционер онлайн: удобство и выгодные цены
5. Кондиционеры для дома: какой выбрать и где купить
6. Лучшие предложения на кондиционеры: акции и распродажи
7. Кондиционер купить: сравнение цен и моделей
8. Кондиционеры с установкой: где купить и как установить
9. Где купить кондиционер с доставкой: быстро и надежно
10. Кондиционеры: где купить качественный товар по выгодной цене
11. Кондиционер купить: как выбрать оптимальную мощность
12. Кондиционеры для офиса: какой выбрать и где купить
13. Кондиционер купить: самый выгодный вариант
14. Кондиционеры в рассрочку: где купить и как оформить
15. Кондиционеры: лучшие магазины и предложения
16. Кондиционеры на распродаже: где купить по выгодной цене
17. Как выбрать кондиционер: советы перед покупкой
18. Кондиционер купить: где найти лучшие цены
19. Лучшие магазины кондиционеров: где купить качественный товар
20. Кондиционер купить: выбор из лучших моделей
кондиционер для комнаты https://kondicioner-cena.ru/ .
dlilf zgdsd jpycw wtyjf ocqxi tbqxc
Взлом WhatsApp: Фактичность и Мифы
WhatsApp – один из известных мессенджеров в мире, массово используемый для передачи сообщениями и файлами. Он известен своей шифрованной системой обмена данными и гарантированием конфиденциальности пользователей. Однако в интернете время от времени появляются утверждения о возможности взлома Вотсап. Давайте разберемся, насколько эти утверждения соответствуют реальности и почему тема нарушения WhatsApp вызывает столько дискуссий.
Кодирование в Вотсап: Охрана Личной Информации
Вотсап применяет end-to-end кодирование, что означает, что только передающая сторона и получающая сторона могут читать сообщения. Это стало фундаментом для уверенности многих пользователей мессенджера к сохранению их личной информации.
Легенды о Взломе Вотсап: Почему Они Появляются?
Интернет периодически заполняют слухи о взломе Вотсап и возможном доступе к переписке. Многие из этих утверждений часто не имеют оснований и могут быть результатом паники или дезинформации.
Реальные Угрозы: Кибератаки и Безопасность
Хотя взлом Вотсап является сложной задачей, существуют реальные угрозы, такие как кибератаки на индивидуальные аккаунты, фишинг и вредоносные программы. Соблюдение мер охраны важно для минимизации этих рисков.
Охрана Личной Информации: Рекомендации Пользователям
Для укрепления безопасности своего аккаунта в WhatsApp пользователи могут использовать двухфакторную аутентификацию, регулярно обновлять приложение, избегать подозрительных ссылок и следить за конфиденциальностью своего устройства.
Заключение: Фактическая и Осторожность
Взлом Вотсап, как правило, оказывается трудным и маловероятным сценарием. Однако важно помнить о реальных угрозах и принимать меры предосторожности для сохранения своей личной информации. Исполнение рекомендаций по охране помогает поддерживать конфиденциальность и уверенность в использовании мессенджера.
Perkirakan penghasilan setiap pengguna TikTok https://kalkulatortiktokmoney.com/
lana rhoades filmleri: lana rhoades video – lana rhoades modeli
opnbt xiefh exquk whfjk opfnb zsxre
Recomendo um site de jogos no Brasil Blaze apostas
1. Где купить кондиционер: лучшие магазины и выбор
2. Как выбрать кондиционер: советы по покупке
3. Кондиционеры в наличии: где купить прямо сейчас
4. Купить кондиционер онлайн: удобство и выгодные цены
5. Кондиционеры для дома: какой выбрать и где купить
6. Лучшие предложения на кондиционеры: акции и распродажи
7. Кондиционер купить: сравнение цен и моделей
8. Кондиционеры с установкой: где купить и как установить
9. Где купить кондиционер с доставкой: быстро и надежно
10. Кондиционеры: где купить качественный товар по выгодной цене
11. Кондиционер купить: как выбрать оптимальную мощность
12. Кондиционеры для офиса: какой выбрать и где купить
13. Кондиционер купить: самый выгодный вариант
14. Кондиционеры в рассрочку: где купить и как оформить
15. Кондиционеры: лучшие магазины и предложения
16. Кондиционеры на распродаже: где купить по выгодной цене
17. Как выбрать кондиционер: советы перед покупкой
18. Кондиционер купить: где найти лучшие цены
19. Лучшие магазины кондиционеров: где купить качественный товар
20. Кондиционер купить: выбор из лучших моделей
монтаж кондиционера цена https://www.kondicioner-cena.ru/ .
Eu aconselho um site de jogos no Brasil Blaze apostas
https://1wintr-4.xyz/
dota2answers.com
Hongzhi 황제는 빠르게 앞으로 나아가 보고서를 잡았습니다.
qkofc zmynq gpqms rfpft jxlnl umtgs
O melhor site de jogos do Brasil Blaze apostas
Замечательно, очень ценная мысль
http://www.californiacontrarian.com/avoiding-natural-immunity-unnatural/
https://abelladanger.online/# abella danger filmleri
iwtou boybo kfjiu dqtzr ykyvd tagpc
Преимущества
бесплатный хостинг https://kish-host.ru .
lana rhoades modeli: lana rhoades filmleri – lana rhoades izle
Write more, thats all I have to say. Literally, it
seems as though you relied on the video to make your point.
You obviously know what youre talking about, why waste your intelligence on just posting videos to your blog
when you could be giving us something enlightening to read?
1. Где купить кондиционер: лучшие магазины и выбор
2. Как выбрать кондиционер: советы по покупке
3. Кондиционеры в наличии: где купить прямо сейчас
4. Купить кондиционер онлайн: удобство и выгодные цены
5. Кондиционеры для дома: какой выбрать и где купить
6. Лучшие предложения на кондиционеры: акции и распродажи
7. Кондиционер купить: сравнение цен и моделей
8. Кондиционеры с установкой: где купить и как установить
9. Где купить кондиционер с доставкой: быстро и надежно
10. Кондиционеры: где купить качественный товар по выгодной цене
11. Кондиционер купить: как выбрать оптимальную мощность
12. Кондиционеры для офиса: какой выбрать и где купить
13. Кондиционер купить: самый выгодный вариант
14. Кондиционеры в рассрочку: где купить и как оформить
15. Кондиционеры: лучшие магазины и предложения
16. Кондиционеры на распродаже: где купить по выгодной цене
17. Как выбрать кондиционер: советы перед покупкой
18. Кондиционер купить: где найти лучшие цены
19. Лучшие магазины кондиционеров: где купить качественный товар
20. Кондиционер купить: выбор из лучших моделей
купить кондиционер с установкой http://kondicioner-cena.ru/ .
http://sweetiefox.online/# Sweetie Fox
Топ предложений
13. Лучшие хостинг-провайдеры: где купить качественный сервис
хостинг бесплатный http://kish-host.ru/ .
enksl enkqb bzdxy keewj eiuxq dqnfi
1. Где купить кондиционер: лучшие магазины и выбор
2. Как выбрать кондиционер: советы по покупке
3. Кондиционеры в наличии: где купить прямо сейчас
4. Купить кондиционер онлайн: удобство и выгодные цены
5. Кондиционеры для дома: какой выбрать и где купить
6. Лучшие предложения на кондиционеры: акции и распродажи
7. Кондиционер купить: сравнение цен и моделей
8. Кондиционеры с установкой: где купить и как установить
9. Где купить кондиционер с доставкой: быстро и надежно
10. Кондиционеры: где купить качественный товар по выгодной цене
11. Кондиционер купить: как выбрать оптимальную мощность
12. Кондиционеры для офиса: какой выбрать и где купить
13. Кондиционер купить: самый выгодный вариант
14. Кондиционеры в рассрочку: где купить и как оформить
15. Кондиционеры: лучшие магазины и предложения
16. Кондиционеры на распродаже: где купить по выгодной цене
17. Как выбрать кондиционер: советы перед покупкой
18. Кондиционер купить: где найти лучшие цены
19. Лучшие магазины кондиционеров: где купить качественный товар
20. Кондиционер купить: выбор из лучших моделей
r 32 kondicioner-cena.ru .
uЕѕiteДЌnГ© strГЎnky
Sweetie Fox video: Sweetie Fox – Sweetie Fox modeli
Советы
15. Как купить хостинг с бесплатным переносом сайта
веб хостинг https://kish-host.ru .
Подборка
17. Топ-5 лучших хостингов для вашего сайта
бесплатный домен и хостинг https://kish-host.ru .
http://www.zian100pi.com
gqutf pjdon gwkns hqtyp qidtb ynqpf
enoym qdela qbmye iwplc crmnd cmhfu https://mmdontstop.com/joint-plus-cbd-gummies/
uyzkn pnamz kmprv lqkol rulrx jjkfb https://mmdontstop.com/joint-plus-cbd-gummies/
Selamat datang di situs kantorbola , agent judi slot gacor terbaik dengan RTP diatas 98% , segera daftar di situs kantor bola untuk mendapatkan bonus deposit harian 100 ribu dan bonus rollingan 1%
lfchungary.com
그의 정체는 체포를 면한 채 평범한 유학자가 됐다.
https://abelladanger.online/# abella danger izle
Здесь вы найдете очень качественный промышленный чиллер
Angela White video: Angela Beyaz modeli – Angela White izle
No Brasil, jogue e ganhe no Blaze apostas
No Brasil, jogue e ganhe no Blaze apostas
Um site de jogos muito legal no Brasil Blaze apostas
pxfyu bufox fejsa ijeuy ryknb wdsdt https://mmdontstop.com/joint-plus-cbd-gummies/
https://sweetiefox.online/# Sweetie Fox filmleri
melbet giris
lana rhodes: lana rhoades video – lana rhoades video
vbeua vjhhi fnztu aqiru vlgrn oufvi https://mmdontstop.com/joint-plus-cbd-gummies/
DoplЕ€ujГcГ informace
zofran 4 mg otc
bwin
vvpzg kyvos qeuto wjusy iebes iarcm https://mmdontstop.com/joint-plus-cbd-gummies/
Топ предложений
13. Лучшие хостинг-провайдеры: где купить качественный сервис
vps ssd kish-host.ru .
Perkirakan penghasilan setiap pengguna TikTok https://kalkulatortiktokmoney.com/
https://evaelfie.pro/# eva elfie izle
rxlwg mkrri mgazk lmtbt aqmye vjqud https://mmdontstop.com/joint-plus-cbd-gummies/
?????? ????: Angela White video – Angela White filmleri
https://sweetiefox.online/# Sweetie Fox video
hzqes fbpar vadpp qukqf tahnn hfkxy https://mmdontstop.com/joint-plus-cbd-gummies/
eva elfie modeli: eva elfie video – eva elfie izle
купить аттестат в москве http://www.orik-attestats.com .
xclfj edhcw erbmo dozde neycw gxiea https://mmdontstop.com/joint-plus-cbd-gummies/
https://raketkaigra.online/
https://vseonlinekazino.pro/
Современный четырехзвездочный отель в самом центре Сочи. Отель расположен в 100 метрах от центральной набережной Сочи https://garrettbowz72693.alltdesign.com/mozyr-45556914
uesug stzvb fclxe ouoop qqyyl akobs https://mmdontstop.com/joint-plus-cbd-gummies/
best free porn
apartusa365.com
Sweetie Fox modeli: sweety fox – swetie fox
Recomendo apenas o site original no Brasil Blaze apostas
No Brasil, este é o site original Blaze apostas
aedbq afiht odmbl uqypi gfwng gdjgv https://mmdontstop.com/joint-plus-cbd-gummies/
No Brasil, é um verdadeiro site de jogos Blaze apostas
https://angelawhite.pro/# Angela Beyaz modeli
Attention: A bonus awaits you, come by our location. here
https://alfarealtor.ru/
cottageindesign.com
Перетяжка мягкой мебели
https://rem7.diary.ru/p221798900_davajte-znakomitsya.htm .
eva elfie video: eva elfie modeli – eva elfie video
1. Где купить кондиционер: лучшие магазины и выбор
2. Как выбрать кондиционер: советы по покупке
3. Кондиционеры в наличии: где купить прямо сейчас
4. Купить кондиционер онлайн: удобство и выгодные цены
5. Кондиционеры для дома: какой выбрать и где купить
6. Лучшие предложения на кондиционеры: акции и распродажи
7. Кондиционер купить: сравнение цен и моделей
8. Кондиционеры с установкой: где купить и как установить
9. Где купить кондиционер с доставкой: быстро и надежно
10. Кондиционеры: где купить качественный товар по выгодной цене
11. Кондиционер купить: как выбрать оптимальную мощность
12. Кондиционеры для офиса: какой выбрать и где купить
13. Кондиционер купить: самый выгодный вариант
14. Кондиционеры в рассрочку: где купить и как оформить
15. Кондиционеры: лучшие магазины и предложения
16. Кондиционеры на распродаже: где купить по выгодной цене
17. Как выбрать кондиционер: советы перед покупкой
18. Кондиционер купить: где найти лучшие цены
19. Лучшие магазины кондиционеров: где купить качественный товар
20. Кондиционер купить: выбор из лучших моделей
кондиционер на обогрев https://kondicioner-cena.ru/ .
Hey, remember to come by here for your bonus. here
Hi there! Stop by and see us; there’s a surprise bonus waiting. here
http://lanarhoades.fun/# lana rhoades izle
Angela White filmleri: Angela White video – Angela Beyaz modeli
Friendly reminder: Swing by here to claim your bonus. new casino
https://abelladanger.online/# abella danger video
Как выбрать правильный виртуальный сервер? ,
Почему они лучше обычного хостинга,
Какую выбрать?,
Подробное руководство,
Сравнение цен и тарифов,
Расчет объема памяти и процессорных мощностей
хостинг под adult хостинг под adult .
Angela White izle: Abella Danger – Abella Danger
Psst! Your bonus is waiting for you to pick it up here. home page
https://melbettr.top/
Hey! I’ve left a bonus for you to enjoy, so come by and claim it. page
https://bwintr2.top/
6000 Euro Kredit
Hey! Your bonus is calling—stop by here. home
http://evaelfie.pro/# eva elfie filmleri
Angela White: abella danger video – abella danger izle
Hi, don’t miss out on the bonus I’ve prepared for you; come see us. official site
Discover Your Virtual Footprint with Ease, how to find my ip address location isp instantly at ipaddresswhois.net! Our user-friendly website is your go-to destination for swiftly uncovering your IP address. Whether you are troubleshooting connectivity issues, enhancing online security, or simply curious about your virtual footprint, we have got you covered.
Alia tempora — Другие времена
http://evaelfie.pro/# eva elfie izle
Интересно, а аналог есть?
https://satyakhabarindia.com/chandigarh-%e0%a4%ae%e0%a5%87%e0%a4%82-%e0%a4%aa%e0%a4%b9%e0%a4%b2%e0%a5%87-%e0%a4%86-%e0%a4%97%e0%a4%af%e0%a4%be-%e0%a4%ac%e0%a4%be%e0%a4%b0%e0%a4%b9%e0%a4%b8%e0%a4%bf%e0%a4%82%e0%a4%97%e0%a5%8b/
Angela Beyaz modeli: abella danger filmleri – abella danger izle
Hello! Don’t forget to pop by—I’ve left a bonus for you to collect. website
Contradictio simptomatum — мед. Противоречивость в симптомах.
Recomendo jogar no Brasil no site real Blaze apostas
Aconselho no Brasil o site real Blaze apostas
Recomendo no Brasil um site real Blaze apostas
Amabile opus — Милое созданье.
pЕ™ejdД›te na webovou strГЎnku
Hey, I’ve left a little extra something for you, swing by here. official
LГҐn 25000 kr
pragmatic-ko.com
환자는 절뚝거리며 고개를 들어 쉬징을 보고 서둘러 인사를 건넸다. “삼촌님을 봤습니다.”
Hey! There’s a surprise waiting for you here, so come see us when you can. url
Contradictio in adjecto — Противоречие в определении.
eva elfie filmleri: eva elfie modeli – eva elfie
https://angelawhite.pro/# Angela White filmleri
Hey! There’s a surprise waiting for you here, so come see us soon. login
Prestito di 600 euro
Hey, just wanted to give you a heads up—there’s a bonus waiting for you here. slot
lana rhoades filmleri: lana rhoades izle – lana rhoades modeli
https://lanarhoades.fun/# lana rhoades video
Hey! There’s a surprise bonus waiting for you here, so come on over. website
можно ли купить аттестат russa-attestats.com .
Alert! Don’t forget to come by here for your bonus. www
Porn 720
Conclamatum est — Всё кончено, всё погибло.
Angela White izle: abella danger filmleri – abella danger filmleri
Worlds Most Affordable Crypto Payment Gateway 2024
Studios, apartments and townhouses in The Beach Residences at Al Marjan Island with favourable terms of purchase and return on investment.
Ad usum proprium — Для собственного употребления.
ремонт кровли https://krovla1.ru/
latest blog post
Hi there! Stop by and see us whenever you get a chance; there’s a bonus here. slot
Angela White izle: Angela White izle – Angela White izle
http://evaelfie.pro/# eva elfie izle
Hi! Swing by to see us; I’ve left a bonus waiting just for you. page
Discover Your Virtual Footprint with Ease, how can I find my ip address instantly at ipaddresswhois.net! Our user-friendly website is your go-to destination for swiftly uncovering your IP address. Whether you are troubleshooting connectivity issues, enhancing online security, or simply curious about your virtual footprint, we have got you covered.
Ad opus! — За дело!
Ремонт холодильников Атлант на дому: удобно и быстро!
ремонт холодильников атлант цена ремонт холодильников атлант на дому .
Surprise! Your bonus is here—come by and claim it. aviator
http://carstvo-sharov.ru/
http://lanarhoades.fun/# lana rhoades
Porn free
Porn free
Hey, I’ve left something extra for you, stop by and see us. login
Recomendo o site brasileiro de jogos a todos Blaze apostas
sweety fox: sweety fox – Sweetie Fox filmleri
Топовые игры в онлайн казино Беларусь: слоты, рулетка, покер и другие азартные развлечения
онлайн казино казино беларусь .
Hey! There’s a surprise waiting for you here, so come see us when you can. aviator
Angela White: abella danger video – abella danger video
Don’t forget to drop by here—I’ve got a bonus waiting. website
Hi! Swing by when you have a moment; there’s a bonus waiting here for you. official
turpoisk
https://www.amazon.com/Jane-Dino-Friendship-Personalized-Childrens-ebook/dp/B0CW1FKPMN/
http://abelladanger.online/# abella danger izle
Hi! Swing by to see us; I’ve left a bonus waiting just for you. home page
swetie fox: Sweetie Fox filmleri – Sweetie Fox izle
http://evaelfie.pro/# eva elfie izle
Hi there! Stop by whenever you can; there’s a bonus here for you to enjoy. www
Hi there! Stop by when you’re free; there’s a little something extra here. here
This is really interesting, You aare an excessively professional blogger.
I’ve joined your feed and stay uup for in the hunt for more off your
wonderful post. Also, I’ve shared your site in my social networks
Here iis my webpage; High quality CBG oil
fla-real-property.com
texasnewsjobs.com
Surprise! Your bonus is here—come by and claim it. page
ремонт кровли в Москве https://krovla1.ru/
her er resultaterne
Normally I do not read article on blogs however I would like to say that this writeup very forced me to try and do so Your writing style has been amazed me Thanks quite great post
I think the admin of this site is genuinely working hard in support of his
web page, for the reason that here every data is quality based stuff.
Hi! Swing by and see us whenever you can; there’s a bonus with your name on it. page
https://lanarhoades.fun/# lana rhoades izle
Hey there! Drop by soon; there’s a little something extra waiting for you here. bet
eva elfie filmleri: eva elfie izle – eva elfie modeli
60000 euro lenen
https://angelawhite.pro/# Angela Beyaz modeli
Psst! Your bonus is waiting for you to pick it up here. bet
nahrungserg?nzungsmittel aus deutschland http://www.wellnesspulse.de .
abilify 5mg
https://dolgiplus.ru
Attention! Your bonus is patiently awaiting your arrival here. new casino
chutneyb.com
때때로 팀에는 특히 뛰어난 마른 말이 몇 마리 있습니다.
Angela White video: Abella Danger – abella danger video
In recent years, the demand for call girls in Lahore
has been on the rise. With the rapid growth of the city and the increasing number of visitors, there has been a significant increase in the need for companionship and entertainment.
Hey! There’s a surprise bonus waiting for you here, so come on over. login
pret 14000 euros
онлайн казино видео
Hi, don’t forget to come see us—I’ve left a bonus here with your name on it. new
lana rhoades modeli: lana rhoades izle – lana rhodes
выигрыш казино онлайн
сделаю онлайн казино
https://sweetiefox.online/# Sweetie Fox
I’d like to find out more? I’d want tto find out more details.
My webpge …doctor recommended cbd
сбербанк онлайн казино
Hi there! There’s a bonus waiting for you here, so come on over. url
казино риобет онлайн
Therefore, it is essential to maintain the corsage at a average temperature to ensure that it lasts longer.
One crucial factor that affects the lifespan of white dendrobium orchid corsages is temperature.
Whether worn on the wrist or pinned to the lapel, a
white dendrobium orchid corsage is sure to make an announcement and add a touch of sophistication to any outfit.
When utilized in corsages, they add a contact of elegance and sophistication to any outfit.
A standard aspect so as to add to this orchid corsage is
beads and pearls, however, any accessory or adornment will do.
It is feasible for you to to decide on a shade or designs
based on your personality and preferences. And in the event that they weren’t promoting, nicely, that just meant my designs weren’t
adequate. Lengthening the character of this fashion will help petite brides appear higher.
This model of wedding ceremony costume mermaid, Direct costume is best is each excessive and low brides with hudoschavymteloslozheniem.
Many of the brides loose wait for his or her wedding
to look sexier so it is necessary to measure your bust, or have it measured at
your local lingerie store, to ensure you might be carrying the suitable bust
size.
LГҐn 20000
выигрывает онлайн казино
казино онлайн с деньгами
онлайн адмирал казино
https://evaelfie.pro/# eva elfie izle
Hey! There’s a surprise waiting for you here, so come see us when you can. new
онлайн лайв казино
казино онлайн 1вин
онлайн казино париматч
Effects of vitamin C supplementation on blood pressure a meta analysis of randomized controlled trials can a women take viagra Freshly isolated differentiated aortic medial SMC and murine embryonic stem cells mESCs were used as positive negative controls for each mark and were markedly enriched for H3K4me2 and H3K27me3 at the Myh11 promoter, respectively Figure 5l n
Sweetie Fox filmleri: Sweetie Fox filmleri – sweety fox
скачай казино онлайн
Hey, I’ve left a little extra something for you, swing by here. home page
khasiss.com
너무 오만해서, 시설에 따르면 그 사람은 단지 천 가구입니다.
казино 24 онлайн
лицензионный казино онлайн
Заказ автобуса. Автобусные пассажирские перевозки. Современные автобусы сочетают в себе вместительность, безопасность и комфорт Ульм – Кропивницкий
адмирал казино онлайн играть
казино рубли онлайн
Porn free
eva elfie video: eva elfie modeli – eva elfie
камеры онлайн казино
Hi! Quick reminder to come see us; I’ve set aside a bonus for you. home page
According to the experience of Reputation House agency, reviews in a negative tone can be left not only by dissatisfied customers reputation house serm
игровой онлайн казино
самые онлайн казино
На территории Москве приобрести аттестат – это удобный и оперативный вариант достать нужный запись без дополнительных трудностей. Разнообразие компаний продают сервисы по изготовлению и реализации дипломов различных образовательных институтов – https://russkiy-diploms-srednee.com/. Разнообразие свидетельств в столице России огромен, включая документация о высшем и нормальном профессиональной подготовке, свидетельства, дипломы колледжей и вузов. Основное достоинство – возможность приобрести аттестат Гознака, гарантирующий подлинность и качество. Это гарантирует уникальная защита против фальсификаций и позволяет использовать аттестат для различных задач. Таким образом, покупка диплома в Москве является надежным и оптимальным выбором для данных, кто желает достичь процветанию в трудовой деятельности.
According to the experience of Reputation House agency, reviews in a negative tone can be left not only by dissatisfied customers reputation house customers reviews
казино pin онлайн
http://abelladanger.online/# abella danger izle
Businesses often equate image and reputation. But in fact, these concepts have completely different meanings reputation house serm
Hey there! Quick heads up, I’ve left a bonus waiting for you here. new casino
казино блэкджек онлайн
бонус казино онлайн
интернет казино онлайн бесплатно
казино онлайн россия
Hey there, I’ve got a little surprise for you—swing by here to find out. here
Выкуп квартир. в Санкт-ПетербургеС любыми обременениями и сложностями. Покупаем дорого — до 97% от рыночной стоимости. Аванс 1 000 000 руб в день обращения. Выход на сделку на следующей день!
циан в санкт-петербурге выкуп квартир на вторичке без посредников
казино онлайн best
онлайн казино 10
https://lanarhoades.pro/# lana rhoades full video
х онлайн казино
Hi! Quick reminder to come by—I’ve got a bonus waiting here for you. online casino
какой казино онлайн
онлайн казино рулетки
онлайн казино виды
https://lanarhoades.pro/# lana rhoades full video
Psst! Your bonus is waiting for you to pick it up here. website
Hey, don’t forget to check in—I’ve left a bonus here for you. page
Hi! Swing by when you have a moment; there’s a little bonus waiting for you. url
Обнал карт: Как защититься от обманщиков и сохранить безопасность в сети
Современный мир высоких технологий предоставляет преимущества онлайн-платежей и банковских операций, но с этим приходит и растущая угроза обнала карт. Обнал карт является практикой использования украденных или незаконно полученных кредитных карт для совершения финансовых транзакций с целью замаскировать их происхождения и заблокировать отслеживание.
Ключевые моменты для безопасности в сети и предотвращения обнала карт:
Защита личной информации:
Будьте внимательными при выдаче личной информации онлайн. Никогда не делитесь картовыми номерами, защитными кодами и инными конфиденциальными данными на ненадежных сайтах.
Сильные пароли:
Используйте для своих банковских аккаунтов и кредитных карт безопасные и уникальные пароли. Регулярно изменяйте пароли для усиления безопасности.
Мониторинг транзакций:
Регулярно проверяйте выписки по кредитным картам и банковским счетам. Это способствует выявлению подозрительных операций и моментально реагировать.
Антивирусная защита:
Утанавливайте и актуализируйте антивирусное программное обеспечение. Такие программы помогут препятствовать действию вредоносных программ, которые могут быть использованы для похищения данных.
Бережное использование общественных сетей:
Остерегайтесь размещения чувствительной информации в социальных сетях. Эти данные могут быть использованы для хакерских атак к вашему аккаунту и последующего мошенничества.
Уведомление банка:
Если вы обнаружили сомнительные транзакции или утерю карты, свяжитесь с банком немедленно для блокировки карты и избежания финансовых ущербов.
Образование и обучение:
Следите за новыми методами мошенничества и постоянно обновляйте свои знания, как предотвращать подобные атаки. Современные мошенники постоянно разрабатывают новые методы, и ваше осведомленность может стать решающим для предотвращения.
В завершение, соблюдение простых правил безопасности в сети и регулярное обновление знаний помогут вам минимизировать риск стать жертвой обнала карт на рабочем месте и в будней жизни. Помните, что ваша финансовая безопасность в ваших руках, и предпринимательские действия могут сделать ваш онлайн-опыт более защищенным и надежным.
обнал карт форум
Обнал карт: Как обеспечить безопасность от обманщиков и сохранить защиту в сети
Современный общество высоких технологий предоставляет преимущества онлайн-платежей и банковских операций, но с этим приходит и нарастающая угроза обнала карт. Обнал карт является процессом использования захваченных или неправомерно приобретенных кредитных карт для совершения финансовых транзакций с целью замаскировать их происхождения и заблокировать отслеживание.
Ключевые моменты для безопасности в сети и предотвращения обнала карт:
Защита личной информации:
Будьте внимательными при выдаче личной информации онлайн. Никогда не делитесь банковскими номерами карт, пин-кодами и дополнительными конфиденциальными данными на непроверенных сайтах.
Сильные пароли:
Используйте для своих банковских аккаунтов и кредитных карт надежные и уникальные пароли. Регулярно изменяйте пароли для повышения степени защиты.
Мониторинг транзакций:
Регулярно проверяйте выписки по кредитным картам и банковским счетам. Это помогает выявить подозрительные транзакции и быстро реагировать.
Антивирусная защита:
Утанавливайте и актуализируйте антивирусное программное обеспечение. Такие программы помогут защитить от вредоносных программ, которые могут быть использованы для изъятия данных.
Бережное использование общественных сетей:
Избегайте размещения чувствительной информации в социальных сетях. Эти данные могут быть использованы для взлома к вашему аккаунту и последующего использования в обнале карт.
Уведомление банка:
Если вы выявили подозрительные действия или утерю карты, свяжитесь с банком сразу для блокировки карты и предупреждения финансовых убытков.
Образование и обучение:
Следите за новыми методами мошенничества и постоянно обновляйте свои знания, как избегать подобных атак. Современные мошенники постоянно разрабатывают новые методы, и ваше понимание может стать определяющим для защиты
http://evaelfie.site/# eva elfie hot
фальшивые 5000 купитьФальшивые купюры 5000 рублей: Опасность для экономики и граждан
Фальшивые купюры всегда были важной угрозой для финансовой стабильности общества. В последние годы одним из главных объектов манипуляций стали банкноты номиналом 5000 рублей. Эти контрафактные деньги представляют собой серьезную опасность для экономики и финансовой безопасности граждан. Давайте рассмотрим, почему фальшивые купюры 5000 рублей стали реальной бедой.
Трудность выявления.
Купюры 5000 рублей являются крупнейшими по номиналу, что делает их чрезвычайно привлекательными для фальшивомонетчиков. Превосходно проработанные подделки могут быть затруднительно выявить даже профессионалам в сфере финансов. Современные технологии позволяют создавать качественные копии с использованием передовых методов печати и защитных элементов.
Риск для бизнеса.
Фальшивые 5000 рублей могут привести к значительным финансовым убыткам для предпринимателей и компаний. Бизнесы, принимающие наличные средства, становятся подвергаются риску принять фальшивую купюру, что в конечном итоге может снизить прибыль и повлечь за собой судебные последствия.
Увеличение инфляции.
Фальшивые деньги увеличивают количество в обращении, что в свою очередь может привести к инфляции. Рост количества фальшивых купюр создает дополнительный денежный объем, не обеспеченный реальными товарами и услугами. Это может существенно подорвать доверие к национальной валюте и стимулировать рост цен.
Пагуба для доверия к финансовой системе.
Фальшивые деньги вызывают мизерию к финансовой системе в целом. Когда люди сталкиваются с риском получить фальшивые купюры при каждой сделке, они становятся более склонными избегать использования наличных средств, что может привести к обострению проблем, связанных с электронными платежами и банковскими системами.
Противодействие и образование.
Для предотвращения распространению фальшивых денег необходимо внедрять более совершенные защитные меры на банкнотах и активно проводить образовательную работу среди населения. Гражданам нужно быть более внимательными при приеме наличных средств и обучаться принципам распознавания поддельных купюр.
В заключение:
Фальшивые купюры 5000 рублей представляют значительную угрозу для финансовой стабильности и безопасности граждан. Необходимо активно внедрять новые технологии защиты и проводить информационные кампании, чтобы общество было лучше осведомлено о методах распознавания и защиты от фальшивых денег. Только совместные усилия банков, правоохранительных органов и общества в целом позволят минимизировать опасность подделок и обеспечить стабильность финансовой системы.
Hey! I’ve left a bonus for you to enjoy, so come by and claim it. website
Изготовление и закупка поддельных денег: опасное дело
Купить фальшивые деньги может привлекаться привлекательным вариантом для некоторых людей, но в реальности это действие несет серьезные последствия и разрушает основы экономической стабильности. В данной статье мы рассмотрим негативные аспекты покупки поддельной валюты и почему это является опасным шагом.
Незаконность.
Основное и чрезвычайно значимое, что следует отметить – это полная незаконность изготовления и использования фальшивых денег. Такие манипуляции противоречат законам большинства стран, и их воздаяние может быть очень строгим. Приобретение поддельной валюты влечет за собой угрозу уголовного преследования, штрафов и даже тюремного заключения.
Экономическо-финансовые последствия.
Фальшивые деньги плохо влияют на экономику в целом. Когда в обращение поступает подделанная валюта, это инициирует дисбаланс и ухудшает доверие к национальной валюте. Компании и граждане становятся все более подозрительными при проведении финансовых сделок, что ведет к ухудшению бизнес-климата и тормозит нормальному функционированию рынка.
Потенциальная угроза финансовой стабильности.
Фальшивые деньги могут стать риском финансовой стабильности государства. Когда в обращение поступает большое количество поддельной валюты, центральные банки вынуждены принимать дополнительные меры для поддержания финансовой системы. Это может включать в себя увеличение процентных ставок, что, в свою очередь, плохо сказывается на экономике и финансовых рынках.
Угрозы для честных граждан и предприятий.
Люди и компании, неосознанно принимающие фальшивые деньги в в качестве оплаты, становятся пострадавшими преступных схем. Подобные ситуации могут вызвать к финансовым убыткам и утрате доверия к своим деловым партнерам.
Привлечение криминальных группировок.
Закупка фальшивых денег часто связана с бандитскими группировками и группированным преступлением. Вовлечение в такие сети может повлечь за собой серьезными последствиями для личной безопасности и даже угрожать жизни.
В заключение, приобретение фальшивых денег – это не только незаконное поступок, но и поступок, способный причинить ущерб экономике и обществу в целом. Рекомендуется избегать подобных поступков и сосредотачиваться на легальных, ответственных путях обращения с финансами
Discover a world of luxury in Oceano Al Marjan Island! From breathtaking views to exquisite layouts, indulge in a variety of high-end properties. Choose your dream home at unbeatable prices, curated by the top developers in the emirate. Start living the lavish life you deserve today.
d-bal is the best legal steroid available right now. if client seriously relate to growth muscular mass , be sure try super tren testo-max.
Купить ручной инструмент в интернет-магазине Кувалда.ру — широкий выбор моделей по низким ценам. Ручной инструмент: каталог товаров с описанием, характеристиками, отзывами покупателей и видео кувалда ру
http://sweetiefox.pro/# sweetie fox
Company managers sometimes complain about high staff turnover, the lack of good specialists, and the low professionalism of applicants reputation house employee reviews
Porn videos
Облачная система работает через интернет, а подключение клиники к системе немногим сложнее, чем создание ящика электронной почты. Для работы системы не нужны никакие программы кроме веб-браузера http://www.vniro.ru/ru/novosti/novosti-2015/vniro-predostavil-na-kollegii-minselkhoza-rossii-nauchnuyu-programmu-razvitiya-rossijskoj-akvakultury
займ взять онлайн https://www.topruscredit11.ru .
Простота установки: светодиодные потолочные светильники для поверхностного монтажа
не берут конструктивных изменений
или сверления.
Also visit my web page: http://www.djwx.com/forums/user/profile/63683.page
http://miamalkova.life/# mia malkova movie
https://evaelfie.site/# eva elfie photo
If a user encounters negativity on the first page of search results, he will be wary of the company and is unlikely to become its client reputation reviews
Согласно глобальным оценкам трудовой миграции в 2013 году трудовые мигранты составляли 150 млн.
Feel free to surf to my web blog :: https://garant-migracia.ru/
deze site
alanews24.com
This holistic approach not only guarantees the production of nutrient crops
that do not contain chemicals, but also improves the health of the soil and promotes conservation of balkan-pharm.com.
Also visit my website … https://balkan-pharm.com/
texas-news.com
Как выбрать онлайн казино Беларусь с высокой отдачей: стратегии выбора
лучшие онлайн казино беларуси лучшие онлайн казино беларуси .
LГҐn 50000
http://evaelfie.site/# eva elfie hd
обнал карт купить
Сознание сущности и опасностей связанных с легализацией кредитных карт способно помочь людям предупреждать атак и сохранять свои финансовые средства. Обнал (отмывание) кредитных карт — это процесс использования украденных или незаконно полученных кредитных карт для проведения финансовых транзакций с целью сокрыть их происхождения и заблокировать отслеживание.
Вот некоторые способов, которые могут способствовать в предотвращении обнала кредитных карт:
Сохранение личной информации: Будьте осторожными в контексте предоставления личных данных, особенно онлайн. Избегайте предоставления банковских карт, кодов безопасности и инных конфиденциальных данных на непроверенных сайтах.
Надежные пароли: Используйте надежные и уникальные пароли для своих банковских аккаунтов и кредитных карт. Регулярно изменяйте пароли.
Отслеживание транзакций: Регулярно проверяйте выписки по кредитным картам и банковским счетам. Это способствует своевременному выявлению подозрительных транзакций.
Программы антивирус: Используйте антивирусное программное обеспечение и вносите обновления его регулярно. Это поможет препятствовать вредоносные программы, которые могут быть использованы для кражи данных.
Осторожное взаимодействие в социальных сетях: Будьте осторожными в сетевых платформах, избегайте размещения чувствительной информации, которая может быть использована для взлома вашего аккаунта.
Уведомление банка: Если вы заметили какие-либо подозрительные операции или утерю карты, сразу свяжитесь с вашим банком для блокировки карты.
Образование: Будьте внимательными к современным приемам мошенничества и обучайтесь тому, как противостоять их.
Избегая легковерия и принимая меры предосторожности, вы можете уменьшить риск стать жертвой обнала кредитных карт.
altace 25mg
Porn
https://promokodbar.ru/
https://espassport.pro/
Здесь вы найдете очень оригинальный сайт 1win
Однозначно всем рекомендую этот оригинальный сайт 1win
Промокод при регистрации 1xbet — бонус для новых игроков. Бонус за первый депозит в 1xbet. Как получить и отыграть бонус 32500 руб в букмекерской конторе 1хбет. 1хбет промокод 2024. Букмекерские конторы пользуются спросом у людей, чьи интересы плотно связаны со спортом и чей азарт подкрепляется возможностью вознаграждения путем внесения порой незначительной суммы. Вводите промокод 1xbet в 2024 году, чтобы получить бонус на первый депозит до 32 500 рублей. 1хбет промокод работает только при регистрации новых пользователей. Бесплатный промокод 1xbet при регистрации. Как ввести промокод 1xbet сегодня? Как отыграть бонус по промокоду 1xbet. Используйте промокод 1xbet при регистрации в 2024 году, чтобы получить бонус до 32500 рублей от крупнейшей букмекерской конторы!
Porn
Lainaa 8000 euroa
https://profidrev.by/
Автосервис для Машинки: Если ваша машинка начала странности творить, не тревожтесь, у нас есть волшебники, которые отремонтируют ее. Масло, тормоза, движок — они там в данном шарят!
Строим Сайты: Хотите собственный собственный галлактический вебсайт? У нас есть ребята, которые могут это устроить. Прекрасно, ясно, нетрудно. В том числе и в случае если вы в интернете чайник — не жутко, они растолкуют.
Поддержка с Компьютером: Если у вас компьютер тупит, как я в математике, не переживайте! Мы вас выручим. Микробы, глюки, чудеса — наши специалисты разберутся.
Бизнес-Советы: Мечтаете о собственном бизнесе, но не понимаете, с чего начать? Мы не бизнесмены, и у нас здесь есть знатоки, коие дадут совет, как не “попасть в грабли”.
Шопинг интернет: Интернет-магазин тем, кто предпочитает налегать кнопки и получать посылочки. Здесь вещи от наших приятелей, проверено — качество отличное!
https://madfightgym.md/
Поддержка и Общение: У нас как в большой семье, лишь только интернет. Мы готовы посодействовать, поддержать, поболтать. Время от времени просто важно, дабы был кто-то вблизи.
Инновации и Крутые Штуки: Ну и конечно, мы смотрим за последними трендами и подкидываем для вас заманчивых штукенций. Девайсы, новинки — мы в курсе и готовы разделиться.
Ясно и Честно: Тут никто не несомненно будет вас заваливать сложными словами либо техническим жаргоном. Все просто и понятно, как ребятам.
Доверие и Дружба: Мы не просто вебсайт, мы приятели. Практически постоянно рады вашим вопросам и услугам. Мы доверяем для вас, и вам продоставляется возможность верить нам.
Итоги и Спасибо: Вот эти у нас приключения. Мы тут, чтобы посодействовать вам, не зависимо от такого как, как вы в чем-то разбираетесь. Имущество пожаловать в нашу интернет-семью!
the choice of the optimal crypto wallet depends on several factors, including stated
desires and preferences of the user. https://http://www.smogtoken.io/ are often compatible with several cryptocurrencies and blockchain networks.
Строительство индивидуальных загородных домов в Мытищах и Московской области. Проекты и цены, фото готовых работ и отзывы. Официальный сайт компании строительство дач
Строительство индивидуальных загородных домов в Мытищах и Московской области. Проекты и цены, фото готовых работ и отзывы. Официальный сайт компании строительство домов в мытищах
EnchagPT Blog to miejsce, gdzie można znaleźć interesujące
artykuły i informacje na temat technologii sztucznej inteligencji.
Jest to blog dedykowany wszystkim entuzjastom sztucznej inteligencji, którzy pragną zgłębiać swoją wiedzę na temat tego fascynującego tematu.
Get to know 100% whey extreme, balkan pharmaceutical
– your essential protein source. The results can vary
dependent on similar causes as diet, exercise, genetics and adequacy with recommended doses.
Here is my webpage :: post cycle therapy pills
manzanaresstereo.com
그는 사건을 물었고 그의 시선은 Fang Jifan에게 떨어졌습니다. “Fang Qing의 가족, 아이디어가 있습니까?”
https://miamalkova.life/# mia malkova only fans
rikvip
Here you will find the best agent in China
It may seem that the best option is to make sure that job seekers encounter only positive information about the company reputation house reviews
это находит объяснение в даже помад: невзирая на то, что в компоненты их красящих веществ действительно входит свинец, его там настолько.
Have a look at my web blog … http://audit.megaindex.ru/audit/query_parameters/nimfa-cosmetics.ua
arimidex 400mg
It may seem that the best option is to make sure that job seekers encounter only positive information about the company reputation house serm
Поддельные купюры: угроза для финансовой системы и общества
Введение:
Фальшивомонетничество – преступление, оставшееся актуальным на продолжительностью многих веков. Производство и распространение фальшивых денег представляют серьезную угрозу не только для финансовой системы, но и для общественной стабильности. В данной статье мы рассмотрим масштабы проблемы, методы борьбы с фальшивомонетничеством и последствия для общества.
История фальшивых денег:
Фальшивые деньги существуют с времени появления самой концепции денег. В старину подделывались металлические монеты, а в современном мире преступники активно используют новейшие технологии для подделки банкнот. Развитие цифровых технологий также открыло дополнительные способы для создания электронных аналогов денег.
Масштабы проблемы:
Фальшивые деньги создают опасность для стабильности экономики. Банки, компании и даже обычные граждане могут стать жертвами мошенничества. Рост количества фальшивых денег может привести к потере покупательной способности и даже к экономическим кризисам.
Современные методы фальсификации:
С прогрессом техники фальсификация стала более затруднительной и изощренной. Преступники используют современные технические средства, специализированные принтеры, и даже искусственный интеллект для создания трудноотличимых поддельные копии от настоящих денег.
Борьба с фальшивомонетничеством:
Страны и центральные банки активно внедряют современные методы для предотвращения подделки денег. Это включает в себя использование новейших защитных технологий на банкнотах, просвещение граждан методам распознавания поддельных денег, а также сотрудничество с правоохранительными органами для выявления и предотвращения криминальных группировок.
Последствия для социума:
Фальшивые деньги несут не только экономические, но и социальные последствия. Жители и бизнесы теряют веру к экономическому устройству, а борьба с преступностью требует больших затрат, которые могли бы быть направлены на более полезные цели.
Заключение:
Фальшивые деньги – важный вопрос, требующая уделяемого внимания и совместных усилий граждан, правоохранительных органов и финансовых институтов. Только с помощью активной противодействия с нарушением можно гарантировать устойчивость финансовой системы и сохранить доверие к валютной системе
Опасность подпольных точек: Места продажи фальшивых купюр”
Заголовок: Опасность подпольных точек: Места продажи поддельных денег
Введение:
Разговор об опасности подпольных точек, занимающихся продажей поддельных денег, становится всё более актуальным в современном обществе. Эти места, предоставляя доступ к поддельным финансовым средствам, представляют серьезную опасность для экономической стабильности и безопасности граждан.
Легкость доступа:
Одной из негативных аспектов подпольных точек является легкость доступа к поддельным деньгам. На темных улицах или в скрытых интернет-пространствах, эти места становятся площадкой для тех, кто ищет возможность обмануть систему.
Угроза финансовой системе:
Продажа поддельных купюр в таких местах создает реальную угрозу для финансовой системы. Введение поддельных средств в обращение может привести к инфляции, понижению доверия к национальной валюте и даже к финансовым кризисам.
Мошенничество и преступность:
Подпольные точки, предлагающие поддельные средства, являются очагами мошенничества и преступной деятельности. Отсутствие контроля и законного регулирования в этих местах обеспечивает благоприятные условия для криминальных элементов.
Угроза для бизнеса и обычных граждан:
Как бизнесы, так и обычные граждане становятся потенциальными жертвами мошенничества, когда используют поддельные деньги, приобретенные в подпольных точках. Это ведет к утрате доверия и серьезным финансовым потерям.
Последствия для экономики:
Вмешательство подпольных точек в экономику оказывает отрицательное воздействие. Нарушение стабильности финансовой системы и создание дополнительных трудностей для правоохранительных органов являются лишь частью последствий для общества.
Заключение:
Продажа поддельных средств в подпольных точках представляет собой серьезную угрозу для общества в целом. Необходимо ужесточение законодательства и усиление контроля, чтобы противостоять этому злу и обеспечить безопасность экономической среды. Развитие сотрудничества между государственными органами, бизнес-сообществом и обществом в целом является ключевым моментом в предотвращении негативных последствий деятельности подобных точек.
LГҐn 5000 kr
Темные закоулки сети: теневой мир продажи фальшивых купюр”
Введение:
Поддельные средства стали неотъемлемой частью теневого мира, где места продаж – это факторы серьезных угроз для экономики и общества. В данной статье мы обратим внимание на локации, где процветает подпольная торговля фальшивыми купюрами, включая засекреченные зоны интернета.
Теневые интернет-магазины:
С прогрессом технологий и распространением онлайн-торговли, места продаж фальшивых купюр стали активно функционировать в засекреченных местах интернета. Темные веб-сайты и форумы предоставляют шанс анонимно приобрести фальшивые деньги, создавая тем самым серьезную угрозу для финансовой системы.
Опасные последствия для общества:
Точки оборота поддельных средств на темных интернет-ресурсах несут в себе не только потенциальную опасность для экономической устойчивости, но и для простых людей. Покупка поддельных денег влечет за собой опасности: от судебных преследований до потери доверия со стороны окружающих.
Передовые технологии подделки:
На скрытых веб-площадках активно используются новейшие технологии для создания качественных фальшивок. От принтеров, способных воспроизводить защитные элементы, до использования криптовалютных платежей для обеспечения анонимности покупок – все это создает среду, в которой трудно обнаружить и пресечь незаконную торговлю.
Необходимость ужесточения мер борьбы:
Борьба с темными местами продаж фальшивых купюр требует комплексного подхода. Важно ужесточить законодательство и разработать активные методы для определения и блокировки скрытых онлайн-магазинов. Также невероятно важно поднимать готовность к информации общества относительно опасностей подобных практик.
Заключение:
Места продаж фальшивых купюр на скрытых местах интернета представляют собой серьезную угрозу для финансовой стабильности и общественной безопасности. В условиях расцветающего цифрового мира важно акцентировать внимание на борьбе с подобными действиями, чтобы защитить интересы общества и сохранить веру к финансовой системе
Лучший оригинальный сайт 1win
Оригинальный сайт беттинга в России здесь 1win
This piece of writing will help the internet users for creating new webpage
or even a weblog from start to end.
гарантия производителя достигает 2 года.
Take a look at my webpage: http://www.xn--5-htbd2chx.xn--p1ai/product/igra-stol-forma/reviews/
many of most optimal sites for order steroids are also represent excellent sites
resources for bodybuilding “turanaplex”.
Feel free to visit my homepage :: cheque drops
купить фальшивые рубли
Фальшивые рубли, часто, копируют с целью обмана и незаконного получения прибыли. Злоумышленники занимаются фальсификацией российских рублей, изготавливая поддельные банкноты различных номиналов. В основном, фальсифицируют банкноты с большими номиналами, вроде 1 000 и 5 000 рублей, ввиду того что это позволяет им добывать большие суммы при уменьшенном числе фальшивых денег.
Технология фальсификации рублей включает в себя использование высокотехнологичного оборудования, специализированных печатающих устройств и специально подготовленных материалов. Преступники стремятся максимально точно воспроизвести защитные элементы, водяные знаки безопасности, металлическую защиту, микроскопический текст и другие характеристики, чтобы замедлить определение поддельных купюр.
Поддельные денежные средства часто попадают в обращение через торговые точки, банки или другие организации, где они могут быть незаметно скрыты среди настоящих денег. Это создает серьезные трудности для финансовой системы, так как поддельные купюры могут вызывать убыткам как для банков, так и для населения.
Важно отметить, что имение и применение фальшивых денег являются уголовными преступлениями и подпадают под уголовную ответственность в соответствии с законодательством Российской Федерации. Власти проводят активные меры с подобными правонарушениями, предпринимая действия по выявлению и пресечению деятельности преступных групп, вовлеченных в подделкой российских рублей
1881 hoki
Фальшивые рубли, как правило, имитируют с целью обмана и незаконного получения прибыли. Шулеры занимаются подделкой российских рублей, изготавливая поддельные банкноты различных номиналов. В основном, подделывают банкноты с большими номиналами, вроде 1 000 и 5 000 рублей, поскольку это позволяет им зарабатывать большие суммы при уменьшенном числе фальшивых денег.
Технология подделки рублей включает в себя использование высокотехнологичного оборудования, специализированных печатающих устройств и специально подготовленных материалов. Злоумышленники стремятся максимально точно воспроизвести защитные элементы, водяные знаки безопасности, металлическую защитную полосу, микроскопический текст и другие характеристики, чтобы затруднить определение поддельных купюр.
Фальшивые рубли периодически вносятся в оборот через торговые площадки, банки или другие организации, где они могут быть незаметно скрыты среди реальных денежных средств. Это создает серьезные трудности для финансовой системы, так как поддельные купюры могут привести к убыткам как для банков, так и для граждан.
Важно отметить, что владение и использование фальшивых денег считаются уголовными преступлениями и подпадают под уголовную ответственность в соответствии с законодательством Российской Федерации. Власти проводят активные меры с такими преступлениями, предпринимая меры по обнаружению и прекращению деятельности банд преступников, занимающихся фальсификацией российской валюты
Казино Vavada – лидер в мире азартных развлечений. vavada-kazino– ресурс для качественных игр и бонусов . Наслаждайтесь покером и премиями на казино Вавада!
how to buy mobic
8Porno
dublinnews365.com
alabama-news.com
https://www.mses-expert.ru/
https://miamalkova.life/# mia malkova only fans
https://promokodbar.ru/
оборудование актового зала школы http://www.oborudovanie-aktovogo-zala11.ru .
Как избавиться от чувства вины?
психолог Калуга
900 Euro Kredit
Что делать, если я чувствую себя в тупике?
психолог Калуга
The Royal Observatory at Greenwich, founded in 1675, established the mean date Greenwich Mean Time (GMT), the average solar time here, to help sailors to determine longitude in sea, with time-zone.
Also visit my blog – https://time-zone.space/
Как справиться с кризисом в семье?
Консультация психолога Калуга
Как преодолеть кризис?
Детский психолог Калуга
Как перестать чувствовать вину?
Детский психолог Калуга
Bundan daha fazlas? diger seylerden , eger kabul ederseniz kay?t olmaya karar verirseniz, bu oyun icin hos geldiniz «corekler» ogrenme tebrik “corekler”. boyle, kazanclar daha az gerceklesse bile/oyle olsun, https://somalict.com/forums/users/agnesu8032265/ yukseklerde.
porn mp4
Как выйти из кризиса после рождения ребенка?
Детский психолог Калуга
Как справиться с кризисом?
Психологическая помощь Калуга
and this, according to designated opinion, is characteristic of this particular manifestation of Pepe, all who, among other things, supports Trump: “The entire presidential the campaign for me – which I and meanwhile did not too closely follow -.
my blog – https://www.pepe-coin.io/
Как найти силы жить дальше?
Отзывы о психологах Калуги
Here you can find the best Vector icons
Как преодолеть кризис самостоятельно?
Кризисный психолог Калуга
Как перестать быть жертвой?
психолог Калуга
Лучший беттинговый оригинальный сайт 1win
В России оригинальный сайт казино здесь 1win
Как справиться с тревогой?
Групповая психотерапия Калуга
Как найти себя?
Отзывы о психологах Калуги
Как справиться с кризисом и не потерять себя?
Психологическая помощь Калуга
Как справиться с депрессией?
Психологическая помощь Калуга
era-food
Как преодолеть кризис самостоятельно?
Лучшие психологи в Калуге
Как перестать сравнивать себя с другими?
Психологическая помощь Калуга
Как справиться с кризисом?
психолог Калуга
Как справиться с кризисом на работе?
Консультация психолога Калуга
I was pretty pleased to find this web site.
I need to to thank you for your time just for this wonderful read!!
I definitely loved every part of it and I have you saved to fav to
see new stuff on your blog.
Как понять, что я хочу от жизни?
Лучшие психологи в Калуге
they are also more likely to have updated the nickname of their account from the default Asian adult movies top 10.
Feel free to surf to my web page … https://johnny7m533.loginblogin.com/31684946/asian-adult-videos-can-be-fun-for-anyone
Как выйти из тупика?
Консультация у психолога Калуга
Как справиться с кризисом?
Лучшие психологи в Калуге
Как выйти из кризиса после увольнения?
Кризисный психолог Калуга
Как выйти из кризиса после развода?
Консультация у психолога Калуга
Как преодолеть кризис?
Кризисный психолог Калуга
Как выйти из кризиса после рождения ребенка?
Консультация у психолога Калуга
Как выйти из кризиса после неудачи?
Психологическая помощь Калуга
Как справиться с одиночеством?
Лучшие психологи в Калуге
hoki1881permainan
https://lanarhoades.pro/# lana rhoades solo
初次接觸線上娛樂城的玩家一定對選擇哪間娛樂城有障礙,首要條件肯定是評價良好的娛樂城,其次才是哪間娛樂城優惠最誘人,娛樂城體驗金多少、娛樂城首儲一倍可以拿多少等等…本篇文章會告訴你娛樂城優惠怎麼挑,首儲該注意什麼。
娛樂城首儲該注意什麼?
當您決定好娛樂城,考慮在娛樂城進行首次存款入金時,有幾件事情需要特別注意:
合法性、安全性、評價良好:確保所選擇的娛樂城是合法且受信任的。檢查其是否擁有有效的賭博牌照,以及是否採用加密技術來保護您的個人信息和交易。
首儲優惠與流水:許多娛樂城會為首次存款提供吸引人的獎勵,但相對的流水可能也會很高。
存款入金方式:查看可用的支付選項,是否適合自己,例如:USDT、超商儲值、銀行ATM轉帳等等。
提款出金方式:瞭解最低提款限制,綁訂多少流水才可以領出。
24小時客服:最好是有24小時客服,發生問題時馬上有人可以處理。
Как перестать чувствовать вину?
Консультация у психолога Калуга
Топ-менеджер Николаев Вячеслав Константинович является специалистом в телекоммуникационном бизнесе и в области информационных технологий
Как перестать срываться на окружающих?
Лучшие психологи в Калуге
Топ-менеджер Вячеслав Константинович Николаев является специалистом в телекоммуникационном бизнесе и в области информационных технологий
Как справиться с кризисом?
Детский психолог Калуга
Как выйти из кризиса после неудачи?
Лучшие психологи в Калуге
娛樂城首儲
初次接觸線上娛樂城的玩家一定對選擇哪間娛樂城有障礙,首要條件肯定是評價良好的娛樂城,其次才是哪間娛樂城優惠最誘人,娛樂城體驗金多少、娛樂城首儲一倍可以拿多少等等…本篇文章會告訴你娛樂城優惠怎麼挑,首儲該注意什麼。
娛樂城首儲該注意什麼?
當您決定好娛樂城,考慮在娛樂城進行首次存款入金時,有幾件事情需要特別注意:
合法性、安全性、評價良好:確保所選擇的娛樂城是合法且受信任的。檢查其是否擁有有效的賭博牌照,以及是否採用加密技術來保護您的個人信息和交易。
首儲優惠與流水:許多娛樂城會為首次存款提供吸引人的獎勵,但相對的流水可能也會很高。
存款入金方式:查看可用的支付選項,是否適合自己,例如:USDT、超商儲值、銀行ATM轉帳等等。
提款出金方式:瞭解最低提款限制,綁訂多少流水才可以領出。
24小時客服:最好是有24小時客服,發生問題時馬上有人可以處理。
apksuccess.com
“…” 함축하는 의미는 내가 정직하지 못했다는 것입니다.
Boomerang Casino Freispiele – Ihr Ticket zu spannenden Gewinnen
Boomerang Casino ist ein aufregender neuer Spieler auf dem Online-Glücksspielmarkt und hat bereits die Aufmerksamkeit vieler Spieler auf sich gezogen. Mit einer breiten Auswahl an Spielen und großzügigen Werbeaktionen bietet dieses Casino ein einmaliges Spielerlebnis. Eine der attraktivsten Werbeaktionen sind die Boomerang Casino Freispiele, die Spielern die Möglichkeit bieten, ohne Risiko große Gewinne zu erzielen.
Diese Freispiele sind eine großartige Möglichkeit, das Casino kennenzulernen und seine Lieblingsspiele auszuprobieren, ohne eigenes Geld einzahlen zu müssen. Spieler können sich einfach registrieren und erhalten sofort eine Anzahl an Freispielen, die sie auf ausgewählten Slots verwenden können. Diese Freispiele bieten die Chance, echtes Geld zu gewinnen, ohne dass ein Einsatz erforderlich ist.
Darüber hinaus bietet Boomerang Casino regelmäßig Sonderaktionen, bei denen Spieler noch mehr Freispiele erhalten können. Diese Aktionen können täglich, wöchentlich oder zu besonderen Anlässen wie Feiertagen angeboten werden. Spieler sollten daher regelmäßig die Promotionsseite des Casinos besuchen, um keine dieser lukrativen Angebote zu verpassen.
Die Boomerang Casino Freispiele sind nicht nur eine großartige Möglichkeit, das Casino und seine Spiele kennenzulernen, sondern auch eine Möglichkeit, ohne Risiko echtes Geld zu gewinnen. Spieler sollten diese Angebote nutzen, um ihre Gewinnchancen zu maximieren und ein aufregendes Spielerlebnis zu genießen. Besuchen Sie Boomerang Casino noch heute und entdecken Sie die aufregende Welt der Freispiele. Viel Glück beim Spielen!
Also visit my blog https://boomerangcasino.one/
Промокод 1xBet на сегодня и бесплатно. Промокоды 1хбет 2024 требуется использовать те, которые предоставят игрокам самые лучшие бонусы. Каждый из них позволяет увеличить первый депозит в 2 раза, максимальная сумма увеличения – 100 долларов. Большое количество промокодов — одна из причин того, что на сайте регистрируется огромное количество новых игроков каждый день. На данный момент их количество превышает пятьсот тысяч уникальных пользователей каждый день. Действующие промокоды позволяют увеличить размер приветственных баллов до 32 500 рублей. Для этого нужно лишь активировать при регистрации имеющийся код, скопировав его в соответствующее поле. Букмекерская контора 1ХБет является одной из самых влиятельных на рынке игорного бизнеса в России и не нуждается в особом представлении. Впрочем, букмекер продолжает держать статус одного из самых щедрых и предлагает своим клиентам воспользоваться промокодами для халявы, – более подробно в этом материале http://rabotat.mybb.ru/viewtopic.php?id=20962#p29650.
such wallet suitable for all who need only invest, trade
cryptocurrency, https://www.infinito-wallet.com/ so that not needed search other
unique blockchain applications.
เว็บ DNABET: สู่ทาง ประสบการณ์ การพนัน ที่ไม่เป็นไปตาม ที่ทุกท่าน เคย ประสบ!
DNABET ยัง เป็นที่นิยม เลือกยอดนิยม สำหรับ แฟน การแทง ออนไลน์ ในประเทศไทย นี้.
ไม่ต้อง เสียเวลา ในการเลือกว่าจะ แข่ง DNABET เพราะที่นี่ ไม่จำเป็นต้อง เลือกที่จะ จะได้รางวัล หรือไม่เหรอ!
DNABET มี ราคาจ่าย ทุกราคาจ่าย หวยที่ สูง ตั้งแต่ 900 บาท ขึ้นไป เมื่อ ท่าน ถูกรางวัล จะได้รับ รางวัลมากมาย กว่า เว็บ ๆ ที่คุณ เคย.
นอกจากนี้ DNABET ยัง มีความหลากหลาย หวย ที่คุณสามารถเลือก มากถึง 20 หวย ทั่วโลก ทำให้ เลือก ตามใจ ได้อย่างหลากหลายแบบ.
ไม่ว่าจะเป็น หวยรัฐ หุ้น ยี่กี ฮานอย หวยลาว และ ลอตเตอรี่รางวัลที่ มีราคา เพียง 80 บาท.
ทาง DNABET มั่นคง ในการเงิน โดย ได้ เปลี่ยนชื่อจาก ชันเจน เป็น DNABET เพื่อ เสริมฐานลูกค้าที่มั่นใจ และ ปรับปรุงระบบให้ มีความสะดวกสบาย ขึ้น.
นอกจากนี้ DNABET ยังมีโปรโมชั่น หวย ให้เลือก มากมาย เช่นเดียวกับ โปรโมชัน สมาชิกใหม่ที่ ท่าน วันนี้ จะได้รับ โบนัสเพิ่มทันที 500 บาท หรือ ไม่ต้องจ่าย เงิน.
นอกจากนี้ DNABET ยังมี ประจำเดือน ท่านมีความมั่นใจ และเลือก DNABET การเดิมพัน หวย ของท่านเอง พร้อม โปรโมชั่น และ เหล่าโปรโมชั่น ที่ มาก ที่สุดในประเทศไทย ปี 2024.
อย่า ปล่อย โอกาสที่ดีนี้ มา มาเป็นส่วนหนึ่งของ DNABET และ เพลิดเพลินไปกับ ประสบการณ์การเล่น หวย ทุกท่าน มีโอกาสจะ เป็นเศรษฐี ได้ เพียง แค่ท่าน เลือก DNABET เว็บแทงหวย ทางอินเทอร์เน็ต ที่มั่นใจ และ มีจำนวนสมาชิกมากที่สุด ในประเทศไทย!
Bu orijinal versiyon, http://wiki.quanticsystems.com.br/index.php/Starlight_Princess_1000, dayan?r ve sahip bunlar ayn? islevlere sahiptir.
глаз бога бот
linezolid 600mg
era-food
https://lanarhoades.pro/# lana rhoades full video
История строительства Кнаубом Андреем НПЗ Томскнефтерепеработка, планов на модернизацию и совершенствование корпоративной культуры. Привлечение молодых специалистов, улучшение условий труда всегда были в приоритете у бизнесмена кнауб андрей томскнефтепереработка
История строительства Кнаубом Андреем НПЗ Томскнефтерепеработка, планов на модернизацию и совершенствование корпоративной культуры. Привлечение молодых специалистов, улучшение условий труда всегда были в приоритете у бизнесмена кнауб андрей
Николаев Вячеслав Константинович https://www.nicolaev-vyacheslav-konstantinovich.ru/ .
Prestito 19 mila euro
Бонус приветствия в Betwinner предоставляет игрокам возможность получить дополнительные средства на свой игровой счет. Этот бонус составляет 100% от суммы первого депозита, который игрок вносит на свой счет. Например, если новый клиент пополнил свой счет на 10 евро, то ему будет начислено еще 10 евро в качестве бонуса.
http://nashkyev.ukrbb.net/viewtopic.php?f=12&t=3064&p=6834#p6834
Лучший беттинговый и настоящий сайт 1win
Выгодный и надежный беттинговый сайт 1win
Настоящий сайт и оригинальный 1вин здесь 1win. Рекомендую!
ウェブサイトを訪問
Бонус приветствия в Betwinner предоставляет игрокам возможность получить дополнительные средства на свой игровой счет. Этот бонус составляет 100% от суммы первого депозита, который игрок вносит на свой счет. Например, если новый клиент пополнил свой счет на 10 евро, то ему будет начислено еще 10 евро в качестве бонуса.
https://salfetka.at.ua/forum/11-6254-1#20077
phenergan bestellen
Продукция применяется в машиностроении,
автомобилестроении, https://kosox.ru/ электротехнической
промышленности.
greeceholidaytravel.com
elitecolumbia.com
register hoki1881
10000 euro lenen
podГvejte se na tento web
https://evaelfie.site/# eva elfie full video
Завод весового оборудования презентует устройство для контроля количества сыпучих материалов во время их транспортировки – расходомер поточного типа поточный расходомер c-lever
Завод весового оборудования презентует устройство для контроля количества сыпучих материалов во время их транспортировки – расходомер поточного типа элеваторные весы
coloradonewss.com
All the existing bookmakers and casino platforms nowadays use all available methods to attract the potential players, including promotional offers. As the gambling industry does not stay still, improving regularly the existing entertainments and creating new ones, it always gives the comfortable conditions to try them out. For the Aviator, this experience was also implied by Spribe developer company, while they released the game and let users get familiar with it. It included the social interactions on available platforms with the Aviator game code the users could activate and receive on the partnering sources some generous rewards. Implying bonuses both for the target game and other slots or bet exclusives, the Aviator coupon code has become one of the top used within the gambling community.
You can find out more detailed information about bonuses and sites where you can play the aviator game by reading our article https://www.aviator-game-bonus.com/
While the Aviator game itself may not offer promo codes, several online casinos that host the game provide promotional offers. Among the popular online casinos offering Aviator are 1xbet, 1win, Parimatch, Mostbet, Pin Up, and 4raBet.
These casinos frequently introduce promo codes that players can use to enhance their gaming experience. By redeeming these codes, players can enjoy various benefits, such as bonus funds, free spins, or exclusive rewards. Keep an eye on these reputable online casinos and their promotional campaigns to make the most out of your Aviator gameplay and increase your chances of winning big.
Integratore Reduslim ist ein revolutionäres Produkt, das dabei hilft, Gewicht zu verlieren und die Gesundheit zu verbessern. Dieses Nahrungsergänzungsmittel enthält natürliche Inhaltsstoffe wie grünen Tee-Extrakt, L-Carnitin und Garcinia Cambogia, die den Stoffwechsel anregen und Fettverbrennung fördern.
Durch die Einnahme von Integratore Reduslim kann man effektiv abnehmen und dabei den Körper mit wichtigen Nährstoffen versorgen. Es hilft auch, den Hunger zu kontrollieren und den Heißhunger auf ungesunde Lebensmittel zu reduzieren.
Die regelmäßige Anwendung von Integratore Reduslim kann zu einer verbesserten Energie und einem insgesamt besseren Körpergefühl führen. Es ist wichtig, das Produkt als Ergänzung zu einer gesunden Ernährung und ausreichender Bewegung zu betrachten, um optimale Ergebnisse zu erzielen.
Probieren Sie Integratore Reduslim noch heute aus und erleben Sie die positiven Auswirkungen auf Ihren Körper und Ihre Gesundheit. Beginnen Sie noch heute mit Ihrer Reise zu einem gesünderen und schlankeren Ich.
https://reduslim.at/
Reduslim Prospecto – ein effektives Mittel zur Gewichtsreduktion
Mit dem Reduslim Prospecto steht ein wirksames Mittel zur Gewichtsreduktion auf dem Markt. Die natürlichen Inhaltsstoffe dieses Nahrungsergänzungsmittels helfen dabei, den Stoffwechsel zu beschleunigen und die Fettverbrennung zu fördern. Dadurch können überschüssige Pfunde effektiv und langfristig bekämpft werden.
Die Anwendung des Reduslim Prospecto ist einfach und unkompliziert. Es reicht aus, täglich eine Kapsel vor einer Mahlzeit einzunehmen, um von den positiven Effekten zu profitieren. Bereits nach kurzer Zeit werden erste Erfolge sichtbar, und das ohne lästige Diäten oder strenge Sportprogramme.
Das Reduslim Prospecto ist nicht nur effektiv, sondern auch sicher in der Anwendung. Die natürlichen Wirkstoffe sorgen dafür, dass der Körper auf sanfte Weise beim Abnehmen unterstützt wird, ohne dabei Nebenwirkungen zu verursachen.
Für alle, die mit überschüssigen Pfunden zu kämpfen haben und auf der Suche nach einer effektiven Lösung sind, ist das Reduslim Prospecto die perfekte Wahl. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Effekten dieses hochwertigen Nahrungsergänzungsmittels.
https://reduslim.at/
Lorenzo Stellari ist ein bekannter Fitnessguru, der mit seinem neuen Produkt, Reduslim, die Welt im Sturm erobert. Reduslim verspricht, überflüssige Pfunde schnell und effektiv loszuwerden. Die natürlichen Inhaltsstoffe wie grüner Tee und Garcinia Cambogia sorgen für eine gesunde Gewichtsabnahme ohne Nebenwirkungen. Lorenzo Stellari schwört auf die Wirksamkeit von Reduslim und hat selbst damit schon beeindruckende Resultate erzielt. Wer also schnell und nachhaltig abnehmen möchte, sollte unbedingt Reduslim ausprobieren.
https://reduslim.at/
Che cosa ГЁ Reduslim? Reduslim ГЁ un integratore alimentare che promette di aiutare a perdere peso in modo rapido e sicuro. Grazie alla sua composizione a base di ingredienti naturali come l’estratto di tГЁ verde e il pepe nero, Reduslim stimola il metabolismo e favorisce la combustione dei grassi. Inoltre, aiuta a ridurre l’appetito e a controllare la fame, facilitando il controllo del peso. Se stai cercando un modo efficace per dimagrire senza rinunce, Reduslim potrebbe essere la soluzione che fa per te. Non dimenticare perГІ che ГЁ sempre importante consultare il parere di un medico prima di iniziare qualsiasi programma di perdita di peso.
https://reduslim.at/
Normally I don’t read post on blogs, but I would like to
say that this write-up very pressured me to try and do it!
Your writing taste has been amazed me. Thanks, very nice
post.
Reduslim ГЁ un integratore alimentare popolare che afferma di aiutare le persone a perdere peso in modo rapido e sicuro. Tuttavia, molti si chiedono se Reduslim ГЁ davvero sicuro da assumere e se ci sono effetti collaterali da considerare.
Alcuni esperti avvertono che Reduslim potrebbe essere pericoloso per la salute a lungo termine. Il supplemento contiene ingredienti che potrebbero causare reazioni allergiche o interazioni negative con altri farmaci. Inoltre, l’efficacia di Reduslim nel lungo periodo non ГЁ stata ancora dimostrata con certezza.
Prima di iniziare qualsiasi programma di perdita di peso, ГЁ importante consultare un medico o un nutrizionista per valutare i rischi e i benefici. Mentre Reduslim potrebbe essere una soluzione rapida per perdere peso, ГЁ essenziale considerare attentamente se vale la pena mettere a rischio la propria salute. Scegliere un approccio piГ№ naturale e sano potrebbe essere la scelta migliore per raggiungere i propri obiettivi di perdita di peso a lungo termine.
https://reduslim.at/
Reduslim ist ein beliebtes Produkt zur Gewichtsreduktion, aber viele Menschen machen auch schlechte Erfahrungen damit. Die Erfahrungen mit Reduslim sind gemischt, einige schwören darauf, während andere sagen, dass es nicht geholfen hat.
Es ist wichtig zu beachten, dass jeder Körper anders reagiert und was für einen funktioniert, funktioniert möglicherweise nicht für einen anderen. Es ist wichtig, realistische Erwartungen zu haben und sich bewusst zu sein, dass Gewichtsverlust ein langwieriger Prozess sein kann.
Wenn Sie Reduslim ausprobieren möchten, stellen Sie sicher, dass Sie auch eine gesunde Ernährung und regelmäßige Bewegung in Betracht ziehen. Konsultieren Sie einen Arzt, bevor Sie ein neues Gewichtsverlust-Produkt ausprobieren, um sicherzustellen, dass es sicher ist.
Insgesamt ist es wichtig, dass Sie Ihre eigenen Erfahrungen mit Reduslim machen und nicht einfach auf die Meinungen anderer vertrauen. Jeder Körper ist anders und was für einen positiv ist, kann für einen anderen negativ sein. Bleiben Sie also offen für neue Erfahrungen und finden Sie heraus, was für Sie am besten funktioniert.
https://reduslim.at/
Reduslim funziona o truffa? Das ist die Frage, die viele Menschen sich stellen, wenn es um dieses Diätsupplement geht. Es gibt viele Meinungen darüber, ob Reduslim tatsächlich effektiv ist oder ob es sich nur um eine Abzocke handelt.
Einige Nutzer schwören auf die Wirksamkeit von Reduslim und berichten von schnellen und nachhaltigen Erfolgen bei der Gewichtsabnahme. Sie loben die natürlichen Inhaltsstoffe und die Unterstützung des Stoffwechsels. Andere hingegen sind skeptisch und glauben, dass Reduslim nur teuer ist und keinen wirklichen Nutzen bringt.
Es ist wichtig zu beachten, dass jedes Diätsupplement individuell wirken kann. Was für den einen funktioniert, muss nicht unbedingt für den anderen gelten. Es ist ratsam, sich vor der Einnahme von Reduslim gut zu informieren und gegebenenfalls einen Arzt zu konsultieren.
Letztendlich liegt es an jedem selber, zu entscheiden, ob Reduslim funziona oder truffa ist. Die Meinungen sind geteilt, aber es gibt sicherlich viele Menschen, die von der Wirksamkeit dieses Produkts Гјberzeugt sind.
https://reduslim.at/
manzanaresstereo.com
Fang Jifan은 “황금 대륙 전체를 공급합니까? “라고 놀라움을 금치 못했습니다.
In dem beliebten Online-Forum “Reduslim Foro” haben sich Menschen aus der ganzen Welt zusammengefunden, um ihre Erfahrungen mit dem Abnehmprodukt Reduslim auszutauschen. Die Diskussionen reichen von Tipps zur Gewichtsreduktion bis hin zu persГ¶nlichen Erfolgsgeschichten. Viele Nutzer berichten von positiven Ergebnissen und einem gesteigerten Wohlbefinden seit der Einnahme von Reduslim. Es scheint, als hГ¤tte dieses Produkt tatsГ¤chlich das Potenzial, den Abnehmprozess zu unterstГјtzen und dabei zu helfen, die Zielgewicht zu erreichen. Wer auf der Suche nach einem effektiven NahrungsergГ¤nzungsmittel zur Gewichtsreduktion ist, sollte sich definitiv das Reduslim Foro genauer anschauen und von den Erfahrungen anderer Nutzer profitieren.
https://reduslim.at/
Sie wollen Reduslim in Österreich kaufen? Dann sind Sie hier genau richtig! Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das dabei helfen kann, Gewicht zu verlieren und den Stoffwechsel zu verbessern. Es enthält natürliche Inhaltsstoffe wie grünen Kaffee, Garcinia Cambogia und Guarana, die alle bekannt dafür sind, den Fettabbau zu fördern.
Wenn Sie Reduslim in Österreich kaufen möchten, können Sie es ganz einfach online bestellen. Besuchen Sie einfach die Website des Herstellers und wählen Sie das Produkt aus, das Ihren Bedürfnissen am besten entspricht. Mit nur wenigen Klicks können Sie Ihre Bestellung aufgeben und schon bald wird Ihr Reduslim zu Ihnen nach Hause geliefert.
Reduslim ist eine großartige Option für alle, die auf natürliche Weise Gewicht verlieren möchten. Es ist einfach anzuwenden und kann Ihnen dabei helfen, Ihre Ziele zu erreichen. Also zögern Sie nicht länger und bestellen Sie noch heute Ihr Reduslim in Österreich!
https://reduslim.at/
Reduslim ist eine kontroverse Alternative zur Gewichtsabnahme, aber viele behaupten, dass es eine totale Geldverschwendung ist. Die Behauptung, dass Reduslim eine Fälschung sei, basiert auf einer Reihe von Studien, die zeigen, dass die Inhaltsstoffe des Produkts nicht wirksam sind. Es gibt keine wissenschaftlichen Beweise, die die Behauptungen des Herstellers unterstützen. Viele Menschen haben versucht, Reduslim zu verwenden, um Gewicht zu verlieren, nur um enttäuscht zu werden. Es gibt viele bessere Alternativen auf dem Markt, die nachweislich effektiv sind. Daher ist es wichtig, sich gut zu informieren, bevor man sein Geld in fragwürdige Produkte wie Reduslim investiert.
https://reduslim.at/
Reduslim composición ist eine natürliche Ergänzung, die darauf abzielt, das Abnehmen zu unterstützen. Die Inhaltsstoffe von Reduslim sind sorgfältig ausgewählt und wirken synergistisch zusammen, um die Fettverbrennung zu beschleunigen und den Stoffwechsel zu steigern. Zu den Hauptbestandteilen gehören grüner Tee, Garcinia Cambogia, L-Carnitin und Guarana. Diese natürlichen Inhaltsstoffe helfen, den Appetit zu kontrollieren und die Energieniveaus zu erhöhen.
Die einzigartige Komposition von Reduslim macht es zu einem effektiven Gewichtsverlustmittel, das ohne Nebenwirkungen funktioniert. Grüner Tee ist ein beliebtes Mittel zur Gewichtsabnahme, da er den Stoffwechsel ankurbelt und die Fettverbrennung fördert. Garcinia Cambogia wird oft zur Appetitkontrolle eingesetzt und kann helfen, Heißhungerattacken zu reduzieren.
L-Carnitin ist ein essentieller Nährstoff, der die Umwandlung von Fett in Energie unterstützt und Guarana ist bekannt für seine stimulierenden Eigenschaften, die die Ausdauer und Konzentration verbessern können. Zusammen bilden diese Inhaltsstoffe eine leistungsstarke Formel, die Ihnen hilft, Ihr Gewichtsverlustziel zu erreichen.
Reduslim composición ist eine sichere und effektive Möglichkeit, Gewicht zu verlieren und Ihren Körper zu straffen. Es ist wichtig zu beachten, dass Reduslim nur als Teil eines gesunden Lebensstils und einer ausgewogenen Ernährung wirksam ist. Konsultieren Sie immer einen Arzt, bevor Sie neue Ergänzungen einnehmen, um sicherzustellen, dass sie für Sie geeignet sind.
https://reduslim.at/
Pharmacie Reduslim bietet eine Vielzahl von Produkten zur Gewichtsabnahme an, die auf natürlichen Inhaltsstoffen basieren. Reduslim ist eine beliebte Marke, die für ihre Wirksamkeit und Qualität bekannt ist. In der Pharmacie Reduslim finden Kunden eine große Auswahl an Produkten, die ihnen helfen, ihr Gewicht zu reduzieren und ihre Gesundheit zu verbessern.
Die Produkte von Pharmacie Reduslim werden von Experten entwickelt und sind sicher und effektiv. Sie enthalten natürliche Inhaltsstoffe wie Grüner Tee, Garcinia Cambogia und Guarana, die den Stoffwechsel ankurbeln und die Fettverbrennung fördern können. Kunden können zwischen verschiedenen Darreichungsformen wie Kapseln, Pulvern und Tees wählen, je nach ihren persönlichen Vorlieben und Bedürfnissen.
In der Pharmacie Reduslim erhalten Kunden auch eine professionelle Beratung und Unterstützung bei der Gewichtsabnahme. Das kompetente Team steht jederzeit zur Verfügung, um Fragen zu beantworten und individuelle Empfehlungen zu geben. Kunden können sich darauf verlassen, dass sie in der Pharmacie Reduslim die richtigen Produkte finden, um ihre Ziele auf gesunde Weise zu erreichen.
https://reduslim.at/
Reduslim Truffa – Wie man Betrug vermeidet und das beste Ergebnis erzielt
Reduslim Truffa ist ein Begriff, der sich auf betrügerische Aktivitäten im Zusammenhang mit dem beliebten Gewichtsabnahme-Produkt Reduslim bezieht. Es gibt zahlreiche Berichte über gefälschte Websites, die das Produkt zu einem extrem niedrigen Preis anbieten, aber oft entweder gefälschte, unwirksame Produkte liefern oder die Kreditkartendaten der Kunden stehlen.
Um einen Reduslim Truffa zu vermeiden und das beste Ergebnis aus dem Produkt zu erzielen, ist es wichtig, es nur von vertrauenswürdigen Quellen zu kaufen. Achten Sie auf offizielle Websites oder autorisierte Händler, die das Produkt in Originalqualität anbieten.
Darüber hinaus sollten Kunden immer auf Bewertungen und Erfahrungsberichte von anderen Nutzern achten, um sicherzustellen, dass sie ein echtes und wirksames Produkt erhalten. Es ist auch ratsam, vor dem Kauf den Kundendienst zu kontaktieren und alle offenen Fragen zu klären.
Durch die Vermeidung von Reduslim Truffa und den Kauf des Produkts auf verantwortungsbewusste Weise können Kunden die gewünschten Ergebnisse erzielen und ihr Gewichtsabnahmeprozess erfolgreich unterstützen. Bleiben Sie wachsam und informiert, um das Beste aus Ihrem Reduslim-Erlebnis herauszuholen.
https://reduslim.at/
Reduslim Mercadona ist ein beliebtes Produkt, das in vielen Haushalten in Spanien zu finden ist. Es handelt sich um ein Nahrungsergänzungsmittel, das dabei helfen soll, Gewicht zu verlieren und den Stoffwechsel zu unterstützen. Die Inhaltsstoffe sollen den Appetit reduzieren und die Fettverbrennung ankurbeln. Viele Menschen schwören auf die Wirkung von Reduslim Mercadona und berichten von positiven Erfahrungen.
Der Markt für Nahrungsergänzungsmittel boomt und immer mehr Menschen greifen zu solchen Produkten, um ihr Gewicht zu kontrollieren. Reduslim Mercadona wird oft empfohlen, da es eine natürliche und schonende Möglichkeit bietet, sein Gewicht zu reduzieren. Es ist jedoch wichtig zu betonen, dass keine Wunder zu erwarten sind und eine gesunde Ernährung sowie regelmäßige Bewegung unerlässlich für den Erfolg sind.
Wer also auf der Suche nach einer Unterstützung beim Abnehmen ist, sollte Reduslim Mercadona eine Chance geben. Mit Geduld, Disziplin und dem richtigen Produkt kann man seinem Ziel, wieder in Form zu kommen, einen großen Schritt näher kommen. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Effekten von Reduslim Mercadona.
https://reduslim.at/
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das bei der Gewichtsabnahme helfen kann. Viele Menschen, die Probleme mit ihrer Schilddrüse haben, fragen sich jedoch, ob Reduslim sicher für sie ist. Die gute Nachricht ist, dass Reduslim und die Schilddrüse in der Regel gut miteinander verträglich sind.
Reduslim enthält natürliche Inhaltsstoffe wie Grüntee-Extrakt, L-Carnitin und Garcinia Cambogia, die den Stoffwechsel ankurbeln und die Fettverbrennung unterstützen können. Diese Wirkstoffe können auch dazu beitragen, den Hormonhaushalt im Körper zu regulieren, was für Menschen mit Schilddrüsenproblemen besonders wichtig ist.
Es ist jedoch ratsam, vor der Einnahme von Reduslim oder anderen Nahrungsergänzungsmitteln mit einem Arzt zu sprechen, insbesondere wenn man an einer Schilddrüsenerkrankung leidet. Ein Facharzt kann die individuelle Situation bewerten und gegebenenfalls Empfehlungen aussprechen.
Insgesamt kann Reduslim also auch für Menschen mit Schilddrüsenproblemen eine gute Unterstützung bei der Gewichtsabnahme sein. Wichtig ist jedoch immer, auf den eigenen Körper zu hören und im Zweifelsfall ärztlichen Rat einzuholen.
https://reduslim.at/
The wallet is also formed so, in order be compatible with some third-party services and exchanges, https://https://www.bither-wallet.com// allows readers easily transfer funds to pocket and from it.
This conservative attitude to creation all the more relevant, given the
continuing problems , what are related to guarantees of payments in pos with “www.green-bitcoin.org”.
Also visit my blog post … https://www.green-bitcoin.org/
Reduslim Bewertung bei Diabetes: Kann das Abnehmprodukt helfen?
Die Bewertungen von Reduslim bei Diabetes sind gemischt. Einige Nutzer berichten von positiven Ergebnissen, während andere keine Verbesserung feststellen konnten. Diabetes ist eine komplexe Krankheit, bei der eine gesunde Ernährung und regelmäßige Bewegung essentiell sind. Reduslim kann als unterstützendes Mittel verwendet werden, um den Gewichtsverlust zu fördern, was wiederum den Blutzuckerspiegel positiv beeinflussen kann.
Es ist wichtig, vor der Einnahme von Reduslim mit einem Arzt zu sprechen, um sicherzustellen, dass das Produkt keine negativen Auswirkungen auf den Diabetes hat. Ein gesunder Lebensstil, der regelmäßige Bewegung und eine ausgewogene Ernährung beinhaltet, ist der Schlüssel zur erfolgreichen Behandlung von Diabetes. Reduslim kann dabei helfen, das Abnehmen zu erleichtern, sollte aber nicht als alleinige Lösung betrachtet werden.
Insgesamt kann Reduslim bei Diabetes eine hilfreiche Unterstützung sein, um den Gewichtsverlust zu fördern und somit die Kontrolle über den Blutzuckerspiegel zu verbessern. Es ist jedoch wichtig, das Produkt im Rahmen eines gesunden Lebensstils zu verwenden und regelmäßig den Blutzuckerspiegel zu kontrollieren. Jeder Fall von Diabetes ist individuell und benötigt eine maßgeschneiderte Behandlung, daher ist es ratsam, mit einem Arzt zusammenzuarbeiten, um die beste Lösung zu finden.
https://reduslim.at/
homadeas.com
Reduslim ist ein beliebtes Produkt in Bulgarien zur Gewichtsreduktion. Es enthält natürliche Inhaltsstoffe, die den Stoffwechsel beschleunigen und das Abnehmen erleichtern. Viele Menschen in Bulgarien schwören auf die Wirksamkeit von Reduslim und sind begeistert von den Ergebnissen.
Das Geheimnis von Reduslim liegt in seiner einzigartigen Formel, die Fettverbrennung und Appetitzügelung kombiniert. Durch die Einnahme von Reduslim können Benutzer schnell und effektiv Gewicht verlieren, ohne sich hungrig oder energielos zu fühlen.
In Kombination mit einer ausgewogenen Ernährung und regelmäßiger Bewegung kann Reduslim helfen, das Idealgewicht zu erreichen und zu halten. Viele Menschen in Bulgarien schwören auf Reduslim als Schlüssel zum Erfolg bei der Gewichtsabnahme.
Wenn auch Sie in Bulgarien nach einem effektiven und sicheren Weg suchen, um Gewicht zu verlieren, ist Reduslim die ideale LГ¶sung. Probieren Sie es aus und erleben Sie selbst die erstaunlichen Ergebnisse. Reduslim – die natГјrliche Wahl fГјr eine gesunde Gewichtsabnahme in Bulgarien.
https://reduslim.at/
Howdy would you mind letting me know which hosting company you’re
utilizing? I’ve loaded your blog in 3 different
internet browsers and I must say this blog loads a lot quicker then most.
Can you recommend a good internet hosting provider at a fair price?
Kudos, I appreciate it!
Автосервис для Машинки: В случае если ваша машинка начала странности творить, не беспокойтесь, у нас есть волшебники, которые отремонтируют ее. Масло, тормоза, движок — они там в данном шарят!
Возводим Веб-сайты: Желаете свой личный космический вебсайт? У нас есть дети, которые имеют все шансы это сделать. Красиво, ясно, несложно. Даже в случае если вы в интернете чайник — не жутко, они объяснят.
Помощь с Компом: В случае если у вас компьютер тупит, как я в математике, не переживайте! Мы вас спасем. Микробы, глюки, чудеса — наши эксперты разберутся.
Бизнес-Советы: Мечтаете о собственном бизнесе, но не знаете, с чего начать? Мы не бизнесмены, но у нас тут есть ценители, коие дадут совет, как не “попасть в грабли”.
Шопинг интернет: Интернет-магазин тем, кто предпочитает нажимать кнопки и получать посылочки. Здесь вещи от наших приятелей, проверено — качество отличное!
https://madfightgym.md/
Поддержка и Общение: У нас как в большой семье, только онлайн. Мы готовы помочь, поддержать, поболтать. Иногда просто принципиально, дабы был кто-то вблизи.
Инновации и Крутые Штуки: Ну и конечно, мы смотрим за последними трендами и подкидываем для вас заманчивых штукенций. Гаджеты, свежие релизы — мы в курсе и готовы поделиться.
Понятно и Откровенно: Тут никто не будет вас заваливать сложными словами либо техническим жаргоном. Все просто и ясно, как ребятам.
Доверие и Дружба: Мы не просто сайт, мы друзья. Практически постоянно рады вашим вопросам и услугам. Мы доверяем для вас, и вы можете верить нам.
Результаты и Спасибо: Вот такие у нас приключения. Мы здесь, чтобы посодействовать для вас, не зависимо от такого как, насколько вы в чем либо разбираетесь. Имущество пожаловать в нашу интернет-семью!
https://lanarhoades.pro/# lana rhoades boyfriend
Thank you for another informative blog. The place else may just I
get that kind of info written in such an ideal manner? I’ve a mission that I’m just now running on,
and I’ve been at the glance out for such info.
купить диплом Гознак http://www.server-diploms.com/ .
https://www.news5cleveland.com/news/local-news/indictment-woman-used-other-pilots-credentials-to-rent-later-crash-aircraft
synthroid 10mg
скачать пин ап кз https://bk-pinup.kz/
https://miamalkova.life/# mia malkova new video
уголовный юрист
юрист по разделу имущества при разводе
http://rglebov.ru
С момента своего вступления в должность в 2005 году Эдуард Давыдов содействовал реализации амбициозного плана по трансформации Башкирской содовой компании (БСК), что привело к фундаментальным изменениям в её операционной деятельности и финансовых показателях Эдуард Давыдов бск
http://abc-law.ru
сколько стоит консультация семейного юриста
юрист в сфере семейного права
С момента своего вступления в должность в 2005 году Эдуард Давыдов содействовал реализации амбициозного плана по трансформации Башкирской содовой компании (БСК), что привело к фундаментальным изменениям в её операционной деятельности и финансовых показателях Давыдов Эдуард
консультация юриста по разделу имущества при разводе
LГҐn 50000 kr
situs kantorbola
KANTORBOLA situs gamin online terbaik 2024 yang menyediakan beragam permainan judi online easy to win , mulai dari permainan slot online , taruhan judi bola , taruhan live casino , dan toto macau . Dapatkan promo terbaru kantor bola , bonus deposit harian , bonus deposit new member , dan bonus mingguan . Kunjungi link kantorbola untuk melakukan pendaftaran .
All the existing bookmakers and casino platforms nowadays use all available methods to attract the potential players, including promotional offers. As the gambling industry does not stay still, improving regularly the existing entertainments and creating new ones, it always gives the comfortable conditions to try them out. For the Aviator, this experience was also implied by Spribe developer company, while they released the game and let users get familiar with it. It included the social interactions on available platforms with the Aviator game code the users could activate and receive on the partnering sources some generous rewards. Implying bonuses both for the target game and other slots or bet exclusives, the Aviator coupon code has become one of the top used within the gambling community.
You can find out more detailed information about bonuses and sites where you can play the aviator game by reading our article https://www.aviator-game-bonus.com/
While the Aviator game itself may not offer promo codes, several online casinos that host the game provide promotional offers. Among the popular online casinos offering Aviator are 1xbet, 1win, Parimatch, Mostbet, Pin Up, and 4raBet.
These casinos frequently introduce promo codes that players can use to enhance their gaming experience. By redeeming these codes, players can enjoy various benefits, such as bonus funds, free spins, or exclusive rewards. Keep an eye on these reputable online casinos and their promotional campaigns to make the most out of your Aviator gameplay and increase your chances of winning big.
Заслуги Давыдова и его профессиональные достижения в области химической промышленности не остались незамеченными Эдуард Давыдов
porn
Заслуги Давыдова и его профессиональные достижения в области химической промышленности не остались незамеченными Давыдов Эдуард
Login Ngamenjitu
Situs Judi: Situs Togel Online Terluas dan Terpercaya
Ngamenjitu telah menjadi salah satu portal judi daring terluas dan terjamin di Indonesia. Dengan bervariasi market yang disediakan dari Semar Group, Situs Judi menawarkan pengalaman main togel yang tak tertandingi kepada para penggemar judi daring.
Market Terbaik dan Terpenuhi
Dengan total 56 pasaran, Portal Judi memperlihatkan berbagai opsi terbaik dari market togel di seluruh dunia. Mulai dari market klasik seperti Sydney, Singapore, dan Hongkong hingga market eksotis seperti Thailand, Germany, dan Texas Day, setiap pemain dapat menemukan market favorit mereka dengan mudah.
Langkah Bermain yang Praktis
Situs Judi menyediakan tutorial cara bermain yang mudah dipahami bagi para pemula maupun penggemar togel berpengalaman. Dari langkah-langkah pendaftaran hingga penarikan kemenangan, semua informasi tersedia dengan jelas di situs Situs Judi.
Ringkasan Terakhir dan Info Terkini
Pemain dapat mengakses hasil terakhir dari setiap market secara real-time di Situs Judi. Selain itu, info paling baru seperti jadwal bank online, gangguan, dan offline juga disediakan untuk memastikan kelancaran proses transaksi.
Bermacam-macam Jenis Permainan
Selain togel, Portal Judi juga menawarkan bervariasi jenis permainan kasino dan judi lainnya. Dari bingo hingga roulette, dari dragon tiger hingga baccarat, setiap pemain dapat menikmati bervariasi pilihan permainan yang menarik dan menghibur.
Keamanan dan Kenyamanan Klien Dijamin
Ngamenjitu mengutamakan keamanan dan kepuasan pelanggan. Dengan sistem keamanan terbaru dan layanan pelanggan yang responsif, setiap pemain dapat bermain dengan nyaman dan tenang di situs ini.
Promosi-Promosi dan Bonus Menarik
Ngamenjitu juga menawarkan berbagai promosi dan bonus menarik bagi para pemain setia maupun yang baru bergabung. Dari hadiah deposit hingga bonus referral, setiap pemain memiliki kesempatan untuk meningkatkan kemenangan mereka dengan bonus yang ditawarkan.
Dengan semua fasilitas dan layanan yang ditawarkan, Portal Judi tetap menjadi pilihan utama bagi para penggemar judi online di Indonesia. Bergabunglah sekarang dan nikmati pengalaman bermain yang seru dan menguntungkan di Situs Judi!
seciminize teklif edilir iki tur:% 125 depozito ve ayr?ca en fazla 250 odenmemis donusler cift bas?na, hangi/ne yapabildiginiz kullanma/girme https://www.wijscheiden.nl/here-is-a-standard-post/mostbet kumarhanesi.
http://lanarhoades.pro/# lana rhoades hot
Давыдов родился 10 июля 1984 года в Нальчике. Эдуард Давыдов с самых ранних лет проявлял выдающийся интерес к научным знаниям Эдуард Давыдов
Tipico Live Casino Support
Das Tipico Live Casino bietet eine spannende und unterhaltsame Möglichkeit, Casinospiele in Echtzeit zu erleben. Neben einer großen Auswahl an Spielen und Live-Dealern sorgt auch der Kundensupport dafür, dass die Spieler das bestmögliche Erlebnis haben.
Der Live-Chat ist die schnellste und einfachste Methode, um mit dem Kundensupport in Kontakt zu treten. Spieler können direkt über die Webseite auf den Live-Chat zugreifen und ihre Fragen oder Probleme mit einem Support-Mitarbeiter besprechen. Die Reaktionszeiten sind in der Regel sehr schnell, so dass die Spieler keine lange Wartezeiten in Kauf nehmen müssen.
Für Spieler, die lieber telefonischen Kontakt bevorzugen, bietet Tipico auch eine Hotline an. Diese ist rund um die Uhr verfügbar und bietet eine persönlichere Art der Kommunikation. Spieler können ihre Fragen oder Probleme direkt mit einem Support-Mitarbeiter besprechen und erhalten sofortige Hilfe.
Für schriftliche Anfragen bietet Tipico auch eine E-Mail-Adresse an, über die Spieler ihre Anliegen an den Support senden können. Die Antwortzeiten können hier etwas länger sein, aber in der Regel erhalten Spieler innerhalb von 24 Stunden eine Antwort auf ihre E-Mail.
Insgesamt bietet der Kundensupport von Tipico Live Casino einen hervorragenden Service und sorgt dafür, dass die Spieler stets gut betreut werden. Egal ob es um technische Probleme, Spielanleitungen oder Auszahlungen geht, der Support steht den Spielern mit Rat und Tat zur Seite. Mit seinem professionellen und hilfsbereiten Team ist Tipico Live Casino eine der besten Optionen für Spieler, die einen erstklassigen Kundenservice schätzen.
Here is my blog post … https://tipicocasino.one/
PЕЇjДЌka 17000 KДЌ
https://evaelfie.site/# eva elfie new video
nebrdecor.com
пинап ставки https://bk-pinup.kz/
Reduslim online kaufen: Effektiv abnehmen leicht gemacht
Möchten Sie endlich lästige Pfunde loswerden und Ihrem Traumgewicht näher kommen? Dann könnte Reduslim die Lösung für Sie sein. Dieses natürliche Nahrungsergänzungsmittel kann Ihnen dabei helfen, Ihr Gewicht auf gesunde Weise zu reduzieren.
Um Reduslim zu kaufen, mГјssen Sie nicht einmal Ihr Zuhause verlassen. Einfach online bestellen und in wenigen Tagen erhalten Sie Ihr Paket bequem nach Hause geliefert. Die Einnahme ist einfach und unkompliziert – einfach die empfohlene Dosis einnehmen und die Wirkung wird nicht lange auf sich warten lassen.
Reduslim enthält wirkungsvolle Inhaltsstoffe, die den Stoffwechsel ankurbeln und die Fettverbrennung unterstützen. So können Sie schneller abnehmen und Ihr Wunschgewicht erreichen. Zudem wird das Hungergefühl reduziert, sodass Sie weniger Kalorien zu sich nehmen und auch Heißhungerattacken gehören der Vergangenheit an.
Probieren Sie Reduslim noch heute aus und starten Sie Ihren Weg zu einer schlankeren und gesГјnderen Version Ihrer selbst. Mit der einfachen Online-Bestellung ist der erste Schritt gemacht – nun liegt es an Ihnen, konsequent dranzubleiben und Ihre Ziele zu erreichen. Reduslim unterstГјtzt Sie dabei auf effektive Weise.
https://reduslim.at/
Reduslim ist eine natürliche und wirksame Lösung, um überschüssige Kilos loszuwerden und das Wunschgewicht zu erreichen. Aber was genau ist Reduslim?
Reduslim ist ein Nahrungsergänzungsmittel, das aus natürlichen Inhaltsstoffen wie grünem Kaffee, Garcinia Cambogia und Bockshornklee besteht. Diese Wirkstoffe helfen beim Abbau von Fettzellen, unterdrücken das Hungergefühl und fördern die Fettverbrennung.
Durch die Einnahme von Reduslim kann der Stoffwechsel angeregt werden, was zu einem gesteigerten Kalorienverbrauch führt. Zudem werden Heißhungerattacken reduziert, sodass es leichter fällt, eine ausgewogene Ernährung einzuhalten.
Reduslim ist eine sichere und effektive Möglichkeit, um auf natürliche Weise Gewicht zu verlieren. Es kann dabei helfen, das Selbstbewusstsein zu steigern und das Wohlbefinden zu verbessern.
Insgesamt ist Reduslim eine großartige Unterstützung auf dem Weg zum Wunschgewicht und kann eine gesunde Lebensweise ergänzen. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Effekten von Reduslim!
https://reduslim.at/
dublindecor.net
Reduslim EU: Deine Lösung zum Abnehmen
Reduslim EU ist ein innovatives Produkt, das dir dabei helfen kann, effektiv Gewicht zu verlieren und deine Traumfigur zu erreichen. Mit seiner einzigartigen Formel aus natГјrlichen Inhaltsstoffen wirkt Reduslim EU auf den Stoffwechsel, reduziert das Verlangen nach SГјГџigkeiten und regt die Fettverbrennung an.
Durch die Einnahme von Reduslim EU kannst du dein Gewicht langfristig reduzieren und deine Gesundheit verbessern. Es ist einfach anzuwenden und hat keine Nebenwirkungen. Viele zufriedene Kunden berichten bereits von ihren Erfolgen mit Reduslim EU.
Wenn auch du endlich deine unerwünschten Pfunde loswerden möchtest, ist Reduslim EU die ideale Lösung für dich. Bestelle noch heute und starte deine Reise zu einer gesünderen und schlankeren Version von dir selbst!
https://reduslim.at/
Ilka Bessin ist vielen als lustige Komikerin bekannt, die mit ihrem unvergleichlichen Humor eine breite Fangemeinde erobert hat. Doch in den letzten Jahren hat die Entertainerin auch mit einer beachtlichen Gewichtsabnahme Гјberrascht, die sie durch die Einnahme von Reduslim erreicht haben soll.
Die Ilka Bessin Reduslim Erfahrungen sind laut eigenen Aussagen der Künstlerin äußerst positiv. Durch die regelmäßige Einnahme des Nahrungsergänzungsmittels konnte sie nicht nur ihr Gewicht reduzieren, sondern auch ihr Wohlbefinden und ihre Fitness deutlich verbessern.
Reduslim wirbt damit, auf rein pflanzlicher Basis zu wirken und den Stoffwechsel zu fördern. Ilka Bessin schwärmt von den Effekten des Produkts und betont, wie viel leichter es ihr nun fällt, sich gesund zu ernähren und regelmäßig Sport zu treiben.
Die Ilka Bessin Reduslim Erfahrungen sind also ein weiterer Beweis dafür, dass das Produkt eine wirkungsvolle Unterstützung auf dem Weg zur Traumfigur sein kann. Wer also auf der Suche nach einer natürlichen und nachhaltigen Lösung zur Gewichtsreduktion ist, sollte einen Blick auf Reduslim werfen und sich von den positiven Erfahrungen der Komikerin inspirieren lassen.
https://reduslim.at/
купить диплом о среднем специальном http://1russa-diploms.com/ .
Погрузитесь в захватывающий мир британских мультов с субтитрами! Улучшайте свой инглиш обогащая словарный запас и восприятие английского, наслаждаясь любимыми мультипликационными творениями на английском языке. Забавляйтесь и учите язык одновременно!
Подробнее тут https://multfilmy-na-anglijskom.pp.ua/
Печатаем фотокниги с вашими фотографиями! Удобный онлайн-редактор, готовые шаблоны с интересным дизайном, разработка индивидуального макета, доставка фотокнига заказать москва
Современные технологии посудомоечных машин, как выбрать подходящую модель. Полезная информация посудомойки
Печатаем фотокниги с вашими фотографиями! Удобный онлайн-редактор, готовые шаблоны с интересным дизайном, разработка индивидуального макета, доставка фотокнига создать и напечатать
prestamo 50000 euros
mega-slot1.com
Fang Jifan은 똑 바른 얼굴로 말했습니다. “전하, 말도 안되는 소리하지 마세요. 제가 당신을 가르치지 않았습니다.”
Die “Reduslim Ulotka” ist ein innovatives Produkt, das dabei helfen kann, Gewicht auf gesunde Weise zu verlieren. Diese natГјrliche ErgГ¤nzung enthГ¤lt sorgfГ¤ltig ausgewГ¤hlte Inhaltsstoffe, die den Stoffwechsel ankurbeln und die Fettverbrennung beschleunigen kГ¶nnen.
Die “Reduslim Ulotka” ist nicht nur ein effektiver Gewichtsverlusthelfer, sondern auch sicher und einfach zu verwenden. Mit regelmäßiger Einnahme und einer gesunden ErnГ¤hrung kГ¶nnen Sie auf natГјrliche Weise ГјberschГјssige Pfunde verlieren und Ihr Wunschgewicht erreichen.
Wenn Sie sich nach einer einfachen und effektiven LГ¶sung fГјr Ihr Gewichtsmanagement sehnen, kГ¶nnte die “Reduslim Ulotka” das richtige Produkt fГјr Sie sein. Probieren Sie es noch heute aus und erleben Sie die Vorteile einer gesГјnderen und schlankeren Lebensweise.
https://reduslim.at/
https://sweetiefox.pro/# sweetie fox cosplay
Hast du schon von Reduslim gehört? Es ist ein revolutionäres Produkt, das dir helfen kann, dein Gewicht zu kontrollieren und schnell Fett zu verbrennen. Aber funktioniert Reduslim wirklich? Viele Menschen fragen sich das, bevor sie es ausprobieren.
Die gute Nachricht ist, dass Reduslim tatsächlich funktioniert und viele zufriedene Kunden hat. Die Inhaltsstoffe sind sorgfältig ausgewählt und wirksam, um den Stoffwechsel anzukurbeln und das Verlangen nach ungesunden Lebensmitteln zu reduzieren. Dadurch kannst du schneller abnehmen und dein Zielgewicht erreichen.
Neben der Gewichtsabnahme hilft Reduslim auch dabei, deine Energie zu steigern und deine allgemeine Gesundheit zu verbessern. Du wirst dich fitter und aktiver fühlen, was dir hilft, deinen Alltag besser zu bewältigen.
Also, wenn du nach einem effektiven und sicheren Weg suchst, um abzunehmen, probiere Reduslim aus und überzeuge dich selbst, wie gut es funktioniert. Du wirst überrascht sein, wie schnell du Ergebnisse erzielst und wie viel Spaß es machen kann, deinen Körper zu transformieren. Funziona Reduslim wirklich und ist eine großartige Unterstützung auf dem Weg zu deinem Traumgewicht.
https://reduslim.at/
Ja, Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das dabei helfen kann, Gewicht zu verlieren. Viele Menschen fragen sich, ob es Reduslim in der Apotheke zu kaufen gibt. Leider ist das Produkt nicht in jeder Apotheke erhältlich. Es kann jedoch online bestellt werden.
Reduslim enthält natürliche Inhaltsstoffe wie grünen Kaffee und Garcinia Cambogia, die den Stoffwechsel anregen und das Hungergefühl reduzieren können. Es ist wichtig zu beachten, dass Nahrungsergänzungsmittel allein keine Wunder bewirken können. Eine gesunde Ernährung und ausreichend Bewegung sind ebenfalls entscheidend, um erfolgreich abzunehmen.
Wenn Sie Reduslim ausprobieren möchten, können Sie es bequem online bestellen. Achten Sie darauf, das Produkt nur bei vertrauenswürdigen Anbietern zu kaufen, um sicherzustellen, dass Sie ein qualitativ hochwertiges Produkt erhalten. Konsultieren Sie bei Fragen oder Bedenken Ihren Arzt oder Apotheker.
https://reduslim.at/
Reduslim ist ein natürlicher Gewichtsverlust-Booster, der sich in der Diätwelt einen Namen gemacht hat. Dieses Produkt ist bekannt für seine effektive Fettverbrennungseigenschaften und die Unterdrückung des Appetits. Despre Reduslim haben viele positive Bewertungen von zufriedenen Kunden erhalten, die ihre Abnehmerfolge mit diesem Produkt erreicht haben. Die natürlichen Inhaltsstoffe in Reduslim helfen dabei, den Stoffwechsel zu beschleunigen und die Kalorienverbrennung zu fördern. Es ist wichtig zu beachten, dass Reduslim in Kombination mit einer gesunden Ernährung und regelmäßiger Bewegung die besten Ergebnisse erzielt. Wenn Sie nach einer natürlichen und effektiven Möglichkeit suchen, um Gewicht zu verlieren, dann sollten Sie definitiv Despre Reduslim recherchieren und es ausprobieren.
https://reduslim.at/
BUY AMMO ONLINE
Magtech’s main objective is to provide shooting enthusiasts with absolutely reliable, totally affordable ammunition, round after round. Magtech ammunition is designed, constructed, and tested in one of the largest and most modern small arms manufacturing facilities in the world. Only the highest quality materials, cutting-edge manufacturing techniques, and state-of-the-art equipment are used to deliver exceptional standard.
Современные технологии посудомоечных машин, как выбрать подходящую модель. Полезная информация https://tram23.ru/innovaczionnye-tehnologii-v-posudomoechnyh-mashinah-uluchshenie-proizvoditelnosti-i-energoeffektivnosti.html
Reduslim hat immer wieder negative Bewertungen und Erfahrungen von Kunden erhalten. Viele Nutzer berichten von unerwГјnschten Nebenwirkungen und fehlenden Resultaten. Doch was ist dran an diesen schlechten Erfahrungen?
Einige Kunden klagen über Magenbeschwerden, Schlafprobleme und sogar Herzrasen nach der Einnahme von Reduslim. Diese unerwünschten Nebenwirkungen können auf die enthaltenen Inhaltsstoffe zurückzuführen sein, die nicht für jeden geeignet sind.
Es ist wichtig, sich vor der Einnahme eines neuen Supplements genau zu informieren und im Zweifelsfall einen Arzt zu konsultieren. Manchmal können auch Wechselwirkungen mit anderen Medikamenten auftreten, die zu unerwünschten Effekten führen.
Fazit: Reduslim mag für einige Nutzer positive Ergebnisse bringen, jedoch sollte man vorsichtig sein und die eigenen Erfahrungen genau beobachten. Im Zweifelsfall ist es besser, auf bewährte Methoden zur Gewichtsreduktion zurückzugreifen und sich nicht auf fragwürdige Produkte zu verlassen.
https://reduslim.at/
“A cosa serve Reduslim?” – Diese Frage stellen sich viele Menschen, die auf der Suche nach einem Mittel zur Gewichtsabnahme sind. Reduslim ist ein NahrungsergГ¤nzungsmittel, das dabei helfen soll, ГјberschГјssige Pfunde loszuwerden und das Idealgewicht zu erreichen.
Die Inhaltsstoffe von Reduslim sollen den Stoffwechsel anregen, den Appetit reduzieren und die Fettverbrennung unterstützen. Dadurch soll das Abnehmen erleichtert werden und langfristig das Gewicht gehalten werden können.
Es ist jedoch wichtig zu beachten, dass Reduslim allein nicht ausreicht, um Gewicht zu verlieren. Eine gesunde Ernährung und ausreichend Bewegung sind nach wie vor entscheidend, um erfolgreich abzunehmen.
Wer also Reduslim als Unterstützung bei der Gewichtsabnahme nutzen möchte, sollte dies in Kombination mit einer gesunden Lebensweise tun. So kann Reduslim dabei helfen, die Pfunde schneller purzeln zu lassen und die Traumfigur zu erreichen.
https://reduslim.at/
https://pinupcassino.pro/# pin up bet
Reduslim ist ein Nahrungsergänzungsmittel, das als medizinisches Produkt verkauft wird, um beim Abnehmen zu helfen. Es enthält natürliche Inhaltsstoffe wie Grüntee-Extrakt, Garcinia Cambogia und Guarana, die bekanntlich den Stoffwechsel ankurbeln und die Fettverbrennung unterstützen können.
Dieses Medikament wird oft als Wundermittel beworben, das Gewichtsverlust ohne Anstrengungen verspricht. Doch Vorsicht ist geboten: Reduslim sollte nicht als Ersatz für eine gesunde Ernährung und ausreichend Bewegung angesehen werden. Es kann lediglich als unterstützende Maßnahme dienen.
Bevor man Reduslim einnimmt, ist es ratsam, mit einem Arzt zu sprechen, um mögliche Nebenwirkungen und Wechselwirkungen mit anderen Medikamenten zu klären. Es sollte auch beachtet werden, dass jeder Körper anders reagiert und individuelle Ergebnisse variieren können.
Insgesamt kann Reduslim für einige Menschen helfen, ihr Gewichtsabnahmeziel zu erreichen, wenn es in Verbindung mit einem gesunden Lebensstil angewendet wird. Es ist jedoch wichtig, realistische Erwartungen zu haben und nicht nur auf das Medikament als Lösung zu vertrauen.
https://reduslim.at/
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das oft in Apotheken verkauft wird. Aber was genau ist Reduslim in der Apotheke? Reduslim ist ein natürlicher Fatburner, der entwickelt wurde, um Menschen bei der Gewichtsabnahme zu unterstützen. Es enthält eine spezielle Formel aus natürlichen Inhaltsstoffen wie grünem Tee, Garcinia Cambogia und Guarana, die den Stoffwechsel anregen und die Fettverbrennung fördern können. Viele Menschen schwören auf die Wirksamkeit von Reduslim und berichten von schnellen und nachhaltigen Ergebnissen. Wenn Sie also nach einem effektiven Weg suchen, um Gewicht zu verlieren, könnte Reduslim in der Apotheke die Lösung sein. Probieren Sie es aus und überzeugen Sie sich selbst!
https://reduslim.at/
Reduslim ist ein beliebtes Abnehmprodukt, das viele positive Bewertungen erhalten hat. Diese Reduslim Bewertungen zeigen, dass das Produkt effektiv und sicher ist. Die Inhaltsstoffe von Reduslim helfen dabei, den Stoffwechsel zu steigern und das Hungergefühl zu reduzieren. Dadurch können die Anwender schnell und einfach Gewicht verlieren. Viele Menschen schwören auf Reduslim und berichten von großartigen Ergebnissen. Wenn auch Sie auf der Suche nach einem effektiven Abnehmprodukt sind, sollten Sie sich die Reduslim Bewertungen genauer ansehen und sich selbst von der Wirksamkeit überzeugen. Reduslim kann Ihnen dabei helfen, Ihr Wunschgewicht zu erreichen und sich rundum wohlzufühlen.
https://reduslim.at/
Reduslim мнения бг мама: Eine Mutter erzählt ihre Erfahrungen mit dem beliebten Abnehmprodukt Reduslim. In der heutigen Gesellschaft ist es oft schwierig, Zeit für Sport und gesunde Ernährung zu finden. Deshalb entschied sich diese Mama, Reduslim auszuprobieren. Schon nach kurzer Zeit konnte sie erste Erfolge sehen. Ihr Gewicht sank und ihr Selbstbewusstsein stieg. Reduslim half ihr, ihren Traumkörper zu erreichen, ohne dabei aufwendige Diäten oder langwierige Workouts machen zu müssen. Ihre Meinung zu Reduslim ist durchweg positiv und sie empfiehlt es gerne weiter. Wer also nach einer effektiven Lösung zum Abnehmen sucht, sollte Reduslim definitiv eine Chance geben.
https://reduslim.at/
It’s genuinely very difficult in this busy life to listen news on TV, so
I just use internet for that purpose, and take
the most up-to-date information.
Печать фотографий онлайн. Доставим заказ за 2-4 дня Ежемесячные акции и скидки Собственная фотофабрика салон фото
Reduslim PZN ist der neue Schlankmacher auf dem Markt, der viele Menschen in Deutschland begeistert. Die natürlichen Inhaltsstoffe sorgen für eine effektive und gesunde Gewichtsabnahme. Die PZN-Nummer garantiert die Qualität und Sicherheit des Produkts. Reduslim unterstützt den Stoffwechsel, reduziert den Appetit und fördert die Fettverbrennung. Viele Anwender berichten von schnellen und langanhaltenden Ergebnissen. Probieren auch Sie Reduslim PZN und starten Sie noch heute in ein schlankeres und gesünderes Leben!
https://reduslim.at/
Sind Sie auf der Suche nach Reduslim in der Apotheke? Dann sollten Sie überlegen, ob Sie es in einer Filiale wie Farmacias Similares kaufen möchten. Dort können Sie möglicherweise den besten Preis für dieses beliebte Nahrungsergänzungsmittel finden. Reduslim ist bekannt für seine effektive Unterstützung bei der Gewichtsabnahme und wird von vielen Menschen weltweit geschätzt. Die natürlichen Inhaltsstoffe können Ihnen helfen, Ihren Stoffwechsel zu beschleunigen und das Verlangen nach ungesunden Snacks zu reduzieren. Probieren Sie es aus und erleben Sie die positiven Effekte dieses Produkts auf Ihren Körper. Besuchen Sie noch heute Ihre lokale Apotheke und fragen Sie nach Reduslim zu einem erschwinglichen Preis!
https://reduslim.at/
Reduslim ist ein Produkt, das vom griechischen Arzt Galenos empfohlen wird. Galenos war ein renommierter Arzt des antiken Griechenlands, der für seine innovativen Behandlungsmethoden bekannt war. Reduslim, das auf seinen Prinzipien basiert, ist eine natürliche Ergänzung zur Gewichtsabnahme, die viele Menschen dabei unterstützt, ihr Zielgewicht zu erreichen.
Die einzigartige Formel von Reduslim enthält natürliche Inhaltsstoffe wie grünen Tee und Garcinia Cambogia, die nachweislich die Fettverbrennung fördern und den Stoffwechsel ankurbeln. Studien haben gezeigt, dass die regelmäßige Einnahme von Reduslim zu einer signifikanten Gewichtsreduktion führen kann, ohne dabei die Gesundheit zu beeinträchtigen.
Galenos hat Reduslim als eine sichere und effektive Lösung zur Gewichtsabnahme empfohlen, da es keine Nebenwirkungen hat und alle natürlichen Inhaltsstoffe enthält. Viele Menschen, die Reduslim verwendet haben, berichten von positiven Ergebnissen und einer Verbesserung ihres allgemeinen Wohlbefindens.
Wenn auch Sie nach einer natürlichen Möglichkeit suchen, um Gewicht zu verlieren und Ihr Wohlbefinden zu verbessern, könnte Reduslim die Lösung sein, die Sie schon lange gesucht haben. Probieren Sie es noch heute aus und erleben Sie die positiven Effekte auf Ihren Körper und Ihre Gesundheit.
https://reduslim.at/
Обучение Вячеслава Константиновича Николаева началось в стенах МГУ на факультете вычислительной математики и кибернетики, после чего он продолжил образование в США, изучая менеджмент Николаев Вячеслав Константинович
Печать фотографий онлайн. Доставим заказ за 2-4 дня Ежемесячные акции и скидки Собственная фотофабрика фотоателье на карте
Обучение Вячеслава Константиновича Николаева началось в стенах МГУ на факультете вычислительной математики и кибернетики, после чего он продолжил образование в США, изучая менеджмент Вячеслав Константинович Николаев
Перетяжка мягкой мебели в Минске: бережно и безупречно
перетяжка кресел минск https://obivka-mebeli-vminske.ru/ .
New project of Hudayriyat Island in Abu Dhabi with favourable purchasing conditions and investment returns.
Reduslim Opinii: Ein Blick auf die Erfahrungen mit diesem beliebten Gewichtsverlustprodukt
Reduslim Opinii ist ein Schlankheitsmittel, das in den letzten Jahren zunehmend an Popularität gewonnen hat. Viele Menschen, die mit Übergewicht zu kämpfen haben, sind auf der Suche nach effektiven und sicheren Möglichkeiten, um Gewicht zu verlieren. Die positiven Erfahrungsberichte und Bewertungen zu Reduslim lassen darauf schließen, dass es ein vielversprechendes Produkt ist.
Einige Anwender berichten davon, dass sie mit Reduslim erfolgreich abgenommen haben, ohne dabei auf strenge Diäten oder anstrengende Workouts angewiesen zu sein. Die natürlichen Inhaltsstoffe des Produkts sollen den Stoffwechsel ankurbeln und den Appetit zügeln, was zu einem schnelleren Gewichtsverlust führen kann.
Allerdings muss auch erwähnt werden, dass nicht jeder die gleichen Erfolge mit Reduslim erzielt. Wie bei jedem anderen Schlankheitsmittel kann die Wirkung von Person zu Person unterschiedlich sein. Es ist wichtig, realistische Erwartungen zu haben und Reduslim als Unterstützung bei der Gewichtsabnahme zu betrachten, nicht als Wundermittel.
Insgesamt scheint Reduslim Opinii eine lohnenswerte Option für diejenigen zu sein, die nach einer natürlichen und effektiven Möglichkeit suchen, Gewicht zu verlieren. Es lohnt sich, die Erfahrungen anderer Anwender zu lesen und sich gründlich über das Produkt zu informieren, bevor man es ausprobiert.
https://reduslim.at/
PЕЇjДЌka 24000 KДЌ
Reduslim Original ist ein innovatives Nahrungsergänzungsmittel, das dabei hilft, effektiv und nachhaltig abzunehmen. Die spezielle Formel aus natürlichen Inhaltsstoffen ermöglicht es, Fett zu verbrennen und den Stoffwechsel zu beschleunigen. Reduslim Original unterscheidet sich von anderen Produkten durch seine einzigartige Zusammensetzung, die ohne chemische Zusätze auskommt.
Die regelmäßige Einnahme von Reduslim Original kann dabei helfen, das Hungergefühl zu reduzieren und die Fettverbrennung zu optimieren. Durch die Unterstützung des Stoffwechsels wird der Körper dazu angeregt, effizienter Kalorien zu verbrennen und somit Gewicht zu verlieren. Positiv zu erwähnen ist auch, dass Reduslim Original keine bekannten Nebenwirkungen hat und somit gut verträglich ist.
Wer also auf der Suche nach einer natürlichen und effektiven Möglichkeit ist, sein Gewicht zu reduzieren, sollte Reduslim Original eine Chance geben. Unterstützt durch eine gesunde Ernährung und ausreichend Bewegung kann das Nahrungsergänzungsmittel zu einer erfolgreichen Gewichtsabnahme beitragen. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Effekten von Reduslim Original.
https://reduslim.at/
Reduslim ist ein beliebtes Produkt zum Abnehmen, das viele positive Rezensionen erhält. Die Reduslim Rezensionen loben vor allem die Wirksamkeit der Kapseln, die auf natürliche Inhaltsstoffe basieren. Viele Anwender berichten von schnellen Erfolgen und einer spürbaren Gewichtsabnahme. Doch nicht nur die Effektivität, sondern auch die Verträglichkeit wird gelobt. Viele Nutzer berichten davon, dass sie keine Nebenwirkungen verspüren und sich auch nach längerer Anwendung wohl fühlen.
Ein weiterer Pluspunkt, den die Reduslim Rezensionen hervorheben, ist die einfache Anwendung. Die Kapseln lassen sich unkompliziert in den Alltag integrieren und müssen nur regelmäßig eingenommen werden, um ihre volle Wirkung zu entfalten. Zudem wird betont, dass Reduslim auch ohne strenge Diäten oder übermäßigen Sport Erfolge erzielen kann.
Insgesamt scheint Reduslim also ein vielversprechendes Produkt zu sein, das viele Menschen bei ihrer Gewichtsabnahme unterstützt. Die positiven Reduslim Rezensionen bestärken in der Meinung, dass es sich lohnt, das Produkt auszuprobieren und selbst von den Effekten zu profitieren. Wer also auf der Suche nach einer natürlichen und effektiven Methode zum Abnehmen ist, sollte Reduslim definitiv eine Chance geben.
https://reduslim.at/
Reduslim Effetti Collaterali sind ein wichtiges Thema für Menschen, die auf der Suche nach einer effektiven Gewichtsabnahme Lösung sind. Es ist wichtig, sich bewusst zu sein, dass jedes Produkt potenzielle Nebenwirkungen haben kann, und Reduslim ist keine Ausnahme. Einige mögliche Nebenwirkungen von Reduslim können Magenbeschwerden, Kopfschmerzen oder Schlafstörungen sein. Es ist wichtig, dass jeder, der Reduslim einnehmen möchte, dies mit seinem Arzt bespricht, um sicherzustellen, dass es sicher ist und keine negativen Auswirkungen auf die Gesundheit hat. Es ist auch wichtig, die Dosierungsempfehlungen zu befolgen und auf mögliche allergische Reaktionen zu achten. Trotz der möglichen Nebenwirkungen kann Reduslim für einige Menschen eine effektive Lösung zur Gewichtsabnahme sein, wenn es richtig verwendet wird. Es ist wichtig, sich gut zu informieren und die Risiken und Vorteile sorgfältig abzuwägen, bevor man sich für die Einnahme von Reduslim entscheidet.
https://reduslim.at/
Как выбрать мастера для перетяжки мебели в Минске? Легко!
ремонт стульев https://obivka-mebeli-vminske.ru/ .
Incest sex
Reduslim ist ein beliebtes Nahrungsergänzungsmittel zur Gewichtsreduktion, das in vielen Apotheken erhältlich ist. Der Preis von Reduslim in der Apotheke variiert je nach Standort und Anbieter, aber es ist wichtig, darauf zu achten, dass man immer einen Blick auf den Preisvergleich wirft, um das beste Angebot zu finden.
Reduslim enthält natürliche Inhaltsstoffe, die den Stoffwechsel anregen und die Fettverbrennung fördern. Es hilft auch, den Appetit zu kontrollieren und unterstützt somit eine gesunde Gewichtsabnahme. Das Produkt ist einfach einzunehmen und kann eine gute Ergänzung zu einer ausgewogenen Ernährung und regelmäßiger Bewegung sein.
Bevor man sich für den Kauf von Reduslim in der Apotheke entscheidet, sollte man jedoch sicherstellen, dass man den besten Preis für das Produkt erhält. Es lohnt sich auch, nach Angeboten und Rabatten Ausschau zu halten, um Geld zu sparen. Mit der richtigen Kombination aus Reduslim, gesunder Ernährung und Bewegung können die gewünschten Ergebnisse schneller erreicht werden.
https://reduslim.at/
Reduslim como tomarlo ist ein wichtiges Thema für Menschen, die auf gesunde Weise abnehmen wollen. Reduslim ist ein Nahrungsergänzungsmittel, das auf natürliche Weise den Stoffwechsel anregt und die Fettverbrennung fördert. Doch wie genau sollte man Reduslim einnehmen, um die besten Ergebnisse zu erzielen?
Es wird empfohlen, Reduslim zweimal täglich vor den Mahlzeiten einzunehmen. Man sollte jeweils eine Kapsel mit ausreichend Wasser schlucken. Es ist wichtig, die empfohlene Dosierung nicht zu überschreiten, um mögliche Nebenwirkungen zu vermeiden.
Zusätzlich zur Einnahme von Reduslim ist es wichtig, auf eine ausgewogene Ernährung und ausreichend Bewegung zu achten. Nur so kann man langfristig und gesund abnehmen. Reduslim ist kein Wundermittel, sondern soll lediglich als Unterstützung dienen.
Fazit: Reduslim como tomarlo ist einfach und unkompliziert. Mit der richtigen Einnahme, einer gesunden Lebensweise und etwas Geduld kann Reduslim helfen, die Traumfigur zu erreichen.
https://reduslim.at/
Reduslim funziona veramente – das ist eine Frage, die sich viele Menschen stellen, die auf der Suche nach einer effektiven und nachhaltigen Abnehmlösung sind. Reduslim ist ein Nahrungsergänzungsmittel, das auf natürliche Inhaltsstoffe setzt, um den Stoffwechsel anzukurbeln und die Fettverbrennung zu fördern. Studien haben gezeigt, dass die regelmäßige Einnahme von Reduslim tatsächlich zu einer Gewichtsreduktion führen kann.
Die Kombination aus grünem Tee-Extrakt, Guarana und sibirischer Ginsengwurzel soll den Appetit zügeln und das Sättigungsgefühl steigern. Zudem enthält Reduslim auch Chrom, das dabei helfen kann, den Blutzuckerspiegel zu regulieren und Heißhungerattacken vorzubeugen. Durch die Einnahme von Reduslim können also nicht nur die Pfunde purzeln, sondern auch der Jojo-Effekt vermieden werden.
Natürlich ist es wichtig, Reduslim in Kombination mit einer ausgewogenen Ernährung und regelmäßiger Bewegung einzunehmen, um optimale Ergebnisse zu erzielen. Kein Nahrungsergänzungsmittel kann Wunder bewirken, aber Reduslim kann definitiv unterstützend wirken. Wer also auf der Suche nach einem natürlichen und effektiven Weg ist, um langfristig abzunehmen, sollte Reduslim eine Chance geben. Reduslim funziona veramente – das bestätigen nicht nur zahlreiche zufriedene Kunden, sondern auch verschiedene Studien.
https://reduslim.at/
оптимальный выбор https://apostrophe.ua/pages/kak-vybrat-cvet-postelnogo-belya дизайнов и размеров.
http://jogodeaposta.fun/# deposito minimo 1 real
Immer mehr Menschen suchen nach effektiven Möglichkeiten, um ihr Gewicht zu reduzieren. Ein beliebtes Produkt, nach dem viele suchen, ist Reduslim. Doch gibt es Reduslim in der Apotheke?
Leider ist Reduslim nicht in der Apotheke erhältlich. Es handelt sich um ein Nahrungsergänzungsmittel, das online über die offizielle Website des Herstellers gekauft werden kann. Dies bedeutet jedoch nicht, dass es nicht wirksam ist.
Reduslim enthält natürliche Inhaltsstoffe wie grüner Kaffee, Artischocke und Mariendistel, die dabei helfen können, den Stoffwechsel zu beschleunigen und Fett zu verbrennen. Es ist wichtig, dass die Einnahme von Reduslim mit einer gesunden Ernährung und regelmäßiger Bewegung kombiniert wird, um die besten Ergebnisse zu erzielen.
Wer also auf der Suche nach einem natürlichen Nahrungsergänzungsmittel zur Gewichtsabnahme ist, sollte Reduslim eine Chance geben. Auch wenn es nicht in der Apotheke erhältlich ist, kann es dennoch eine wirksame Unterstützung auf dem Weg zur Traumfigur sein.
https://reduslim.at/
In der reduslim recensione werden die positiven Wirkungen dieses Nahrungsergänzungsmittels zur Gewichtsabnahme gelobt. Viele Anwender berichten von einer effektiven Reduzierung ihres Körpergewichts und einer Verbesserung ihres Stoffwechsels. Die natürlichen Inhaltsstoffe von reduslim sollen dabei helfen, den Appetit zu reduzieren und die Fettverbrennung zu steigern. Die einfach anzuwendende Formel ist auch für Menschen mit einem hektischen Lebensstil geeignet. Laut der reduslim recensione handelt es sich um ein sicheres und wirksames Produkt, um auf natürliche Weise Gewicht zu verlieren.
https://reduslim.at/
Der Preis von Reduslim kann je nach Anbieter und Packungsgröße variieren. Es ist wichtig, das beste Angebot zu finden, um Geld zu sparen. Reduslim ist ein beliebtes Nahrungsergänzungsmittel zur Gewichtsreduktion, das helfen kann, überschüssige Pfunde zu verlieren. Es enthält natürliche Inhaltsstoffe, die den Stoffwechsel ankurbeln und das Fett verbrennen. Der Preis von Reduslim lohnt sich, da es effektiv und sicher ist. Vergleichen Sie die Preise und bestellen Sie noch heute Ihren Vorrat an Reduslim, um Ihren Traumkörper zu erreichen! Mit Reduslim kann der Preis nicht hoch genug sein für die erzielten Ergebnisse. Probieren Sie es aus und überzeugen Sie sich selbst!
https://reduslim.at/
Reduslim Kapseln sind der neueste Trend in der Welt der Gewichtsabnahme. Diese speziellen Kapseln enthalten natürliche Inhaltsstoffe wie Grüntee-Extrakt, L-Carnitin und Garcinia Cambogia, die alle bekannt sind für ihre Fähigkeit, den Stoffwechsel zu erhöhen und Fett zu verbrennen.
Durch die regelmäßige Einnahme von Reduslim Kapseln kann man effektiv Gewicht verlieren und gleichzeitig den Körper mit wichtigen Nährstoffen versorgen. Die einzigartige Formel dieser Kapseln hilft dabei, den Appetit zu kontrollieren und Heißhungerattacken zu reduzieren.
Viele zufriedene Kunden berichten von schnellen und nachhaltigen Ergebnissen mit Reduslim Kapseln. Sie fГјhlen sich fitter, schlanker und energiegeladener als je zuvor.
Wenn auch du von den Vorteilen dieser innovativen Kapseln profitieren möchtest, solltest du sie am besten noch heute ausprobieren. Reduziere dein Gewicht auf natürliche Weise mit Reduslim Kapseln und fühle dich wieder wohl in deiner Haut!
https://reduslim.at/
Онлайн казино в Беларуси с мобильной версией: играйте в любое время и в любом месте
онлайн казино казино беларусь .
Incest sex
В мире, насыщенном технологиями, нередко возникают ситуации, когда нам требуется найти информацию о владельце определенного номера телефона или узнать его местоположение. Это может быть из-за того, что мы получили звонок или сообщение от незнакомого номера, или же нам просто нужно связаться с определенным человеком, но мы не знаем, как это сделать где телефон по номеру
jbustinphoto.com
주저하지 않고 Ruan Ye는 몇 마리의 말 중 하나를 타고 돌아 서서 막 떠나려고했습니다.
Hast du schon vom offiziellen Website Reduslim gehört? Dies ist die richtige Seite für alle, die auf der Suche nach einem natürlichen und effektiven Weg sind, um Gewicht zu verlieren. Reduslim bietet hochwertige Produkte, die dabei helfen, den Stoffwechsel zu beschleunigen und das Hungergefühl zu reduzieren. Auf der offiziellen Website Reduslim kannst du alle Informationen zu den Produkten finden und sie direkt bestellen. Mit der Unterstützung von Reduslim kannst du endlich deine Wunschfigur erreichen und dich rundum wohlfühlen. Besuche noch heute die Seite officiel reduslim und starte deine Reise zu einem gesünderen Leben!
https://reduslim.at/
Daftar Ngamenjitu
Situs Judi: Situs Lotere Online Terbesar dan Terjamin
Situs Judi telah menjadi salah satu portal judi daring terluas dan terjamin di Indonesia. Dengan beragam pasaran yang disediakan dari Semar Group, Ngamenjitu menawarkan pengalaman bermain togel yang tak tertandingi kepada para penggemar judi daring.
Pasaran Terbaik dan Terpenuhi
Dengan total 56 pasaran, Situs Judi memperlihatkan berbagai opsi terunggul dari market togel di seluruh dunia. Mulai dari pasaran klasik seperti Sydney, Singapore, dan Hongkong hingga pasaran eksotis seperti Thailand, Germany, dan Texas Day, setiap pemain dapat menemukan market favorit mereka dengan mudah.
Cara Main yang Mudah
Portal Judi menyediakan petunjuk cara main yang sederhana dipahami bagi para pemula maupun penggemar togel berpengalaman. Dari langkah-langkah pendaftaran hingga penarikan kemenangan, semua informasi tersedia dengan jelas di situs Portal Judi.
Ringkasan Terakhir dan Info Terkini
Pemain dapat mengakses hasil terakhir dari setiap pasaran secara real-time di Ngamenjitu. Selain itu, info paling baru seperti jadwal bank online, gangguan, dan offline juga disediakan untuk memastikan kelancaran proses transaksi.
Pelbagai Jenis Permainan
Selain togel, Ngamenjitu juga menawarkan bervariasi jenis permainan kasino dan judi lainnya. Dari bingo hingga roulette, dari dragon tiger hingga baccarat, setiap pemain dapat menikmati berbagai pilihan permainan yang menarik dan menghibur.
Security dan Kenyamanan Klien Terjamin
Situs Judi mengutamakan security dan kepuasan pelanggan. Dengan sistem keamanan terbaru dan layanan pelanggan yang responsif, setiap pemain dapat bermain dengan nyaman dan tenang di situs ini.
Promosi-Promosi dan Bonus Istimewa
Portal Judi juga menawarkan bervariasi promosi dan bonus istimewa bagi para pemain setia maupun yang baru bergabung. Dari hadiah deposit hingga hadiah referral, setiap pemain memiliki kesempatan untuk meningkatkan kemenangan mereka dengan hadiah yang ditawarkan.
Dengan semua fitur dan pelayanan yang ditawarkan, Ngamenjitu tetap menjadi pilihan utama bagi para penggemar judi online di Indonesia. Bergabunglah sekarang dan nikmati pengalaman bermain yang seru dan menguntungkan di Situs Judi!
http://aviatormocambique.site/# aviator online
Была задача полностью реконструировать кровлю с заменой покрытия на МЧ и утеплением. Работа идет с соблюдением технологии монтажа, видно что люди опытные https://sethdpvy60371.blogs-service.com/56594996/roofings-maryina-gorka
Reduslim bei Rossmann ist eine revolutionäre neue Methode, um schnell und effektiv abzunehmen. Das Produkt ist exklusiv bei Rossmann erhältlich und hat bereits viele Menschen dabei geholfen, ihr Wunschgewicht zu erreichen.
Die spezielle Formel von Reduslim wirkt auf natürliche Weise im Körper und hilft, Fett zu verbrennen und den Stoffwechsel zu steigern. So können Sie leichter abnehmen und Ihr Zielgewicht erreichen.
Durch die Verwendung von Reduslim bei Rossmann können Sie gesünder leben und sich fitter fühlen. Das Produkt ist leicht anzuwenden und hat keine Nebenwirkungen, sodass es für jeden geeignet ist, der sein Gewicht reduzieren möchte.
Also, worauf warten Sie noch? Probieren Sie Reduslim bei Rossmann aus und beginnen Sie noch heute Ihren Weg zu einem gesünderen und schlankeren Körper.
https://reduslim.at/
Reduslim ist ein beliebtes Produkt zur Gewichtsabnahme, aber was denken Ärzte darüber? Die Reduslim avis médecin zeigen, dass viele Ärzte das Produkt begrüßen und es ihren Patienten empfehlen. Es ist eine natürliche Ergänzung, die hilft, den Stoffwechsel zu verbessern und das Hungergefühl zu reduzieren. Doch wie bei allen Ergänzungsmitteln ist es wichtig, auch eine gesunde Ernährung und regelmäßige Bewegung zu berücksichtigen. Die Kombination aus Reduslim, gesunder Ernährung und Bewegung kann zu guten Ergebnissen führen. Es ist immer ratsam, vor der Einnahme von Nahrungsergänzungsmitteln einen Arzt zu konsultieren, um sicherzustellen, dass sie für Sie geeignet sind. Mit der Unterstützung eines Arztes kann Reduslim ein effektives Werkzeug zur Gewichtsabnahme sein.
https://reduslim.at/
myambutol 30mg
С 1999 года Николаев активно участвовал в международных проектах, начиная с аналитической работы в области телекоммуникаций и ИТ в J’son and Partners Николаев Вячеслав Константинович
купить диплом в Москве https://2orik-diploms.com/ .
Reduslim ist ein beliebtes Nahrungsergänzungsmittel zur Gewichtsreduktion, aber es gibt einige negative Erfahrungen von Benutzern, die berücksichtigt werden sollten. Einige Kunden berichten von Nebenwirkungen wie Kopfschmerzen, Magenbeschwerden und Schlafstörungen. Auch die Wirksamkeit des Produkts wird von einigen in Frage gestellt.
Es ist wichtig zu beachten, dass jeder Körper anders reagiert und was für einen funktioniert, funktioniert möglicherweise nicht für einen anderen. Bevor man Reduslim ausprobiert, ist es ratsam, mit einem Arzt zu sprechen und die Inhaltsstoffe zu überprüfen, um sicherzustellen, dass keine Allergien oder Unverträglichkeiten bestehen.
Es gibt auch positive Erfahrungen mit Reduslim, daher ist es wichtig, die Meinungen verschiedener Benutzer zu berücksichtigen und das Produkt selbst zu testen, um zu sehen, ob es für einen funktioniert. Letztendlich ist es wichtig, eine gesunde Ernährung und regelmäßige Bewegung in die Gewichtsverluststrategie zu integrieren, um langfristige Ergebnisse zu erzielen.
https://reduslim.at/
Reduslim ist ein Nahrungsergänzungsmittel, das bei der Gewichtsabnahme helfen soll. Viele Menschen fragen sich, wie oft sie Reduslim einnehmen sollten, um die besten Ergebnisse zu erzielen. Die empfohlene Dosierung beträgt zweimal täglich, idealerweise vor den Mahlzeiten. Es ist wichtig, die Einnahme nicht zu überschreiten, da dies zu unerwünschten Nebenwirkungen führen kann. Neben der Einnahme von Reduslim ist es auch wichtig, eine gesunde Ernährung und regelmäßige Bewegung in den Alltag zu integrieren, um langfristige Ergebnisse zu erzielen. Es wird empfohlen, vor Beginn einer Gewichtsabnahme-Kur einen Arzt zu konsultieren, um sicherzustellen, dass Reduslim für Sie geeignet ist.
https://reduslim.at/
Du fragst dich, wie gut ist Reduslim wirklich? Dieses Produkt verspricht schnellen Gewichtsverlust und eine effektive Fettverbrennung. Aber hält es wirklich, was es verspricht? Viele Kunden sind begeistert von den Ergebnissen und schwärmen von ihrer schlankeren Figur nach der Verwendung von Reduslim. Die natürlichen Inhaltsstoffe sollen den Stoffwechsel ankurbeln und den Appetit zügeln. Doch wie gut ist Reduslim wirklich? Die Meinungen sind geteilt, einige schwören darauf, während andere keine signifikanten Veränderungen bemerken. Letztendlich ist es wichtig, dass jeder für sich selbst ausprobiert und entscheidet, ob Reduslim die richtige Lösung für seine Abnehmziele ist.
https://reduslim.at/
נערות ליווי באילת
Удобное расположение автошколы у метро позволит Вам совмещать занятия с работой или учёбой в ВУЗе курсы вождения в москве стоимость
Reduslim Pastile de slabit sind der neueste Trend auf dem Markt für Gewichtsverlust. Diese kleinen Pillen versprechen, Fett zu verbrennen und den Stoffwechsel zu beschleunigen, um schnell Gewicht zu verlieren. Viele Menschen schwören auf die Wirksamkeit von Reduslim Pastile de slabit und berichten von erstaunlichen Ergebnissen.
Die Wirkung von Reduslim Pastile de slabit beruht auf einer speziellen Zusammensetzung natürlicher Inhaltsstoffe, die den Körper dabei unterstützen, Fett zu verbrennen und den Appetit zu reduzieren. Dadurch fällt es leichter, Kalorien zu reduzieren und das Gewicht zu kontrollieren.
Wenn Sie Reduslim Pastile de slabit ausprobieren möchten, ist es wichtig, sich an die empfohlene Dosierung zu halten und eine gesunde Ernährung sowie regelmäßige Bewegung in den Alltag zu integrieren. Mit etwas Disziplin und Geduld können Sie bald die Vorteile dieser beliebten Diätpille spüren und Ihre Gewichtsabnahmeziele erreichen.
https://reduslim.at/
דירות דיסקרטיות בחיפה
Удобное расположение автошколы у метро позволит Вам совмещать занятия с работой или учёбой в ВУЗе автошкола метро дмитровская
Hast du auch schon einmal von Reduslim gehГ¶rt? Dieses NahrungsergГ¤nzungsmittel wird oft als Wundermittel zum Abnehmen beworben. Doch Vorsicht – es gibt viele Stimmen, die behaupten, dass Reduslim ein Fake ist. Doch was steckt wirklich dahinter?
Es ist wichtig, kritisch zu sein und sich nicht von den Werbeversprechen blenden zu lassen. Viele Kunden berichten, dass sie nach der Einnahme von Reduslim keinerlei Veränderungen an ihrem Körper festgestellt haben. Manche behaupten sogar, dass es überhaupt keine Wirkung gibt und dass Reduslim nur Geldmacherei ist.
Es ist ratsam, sich vor dem Kauf von Reduslim ausführlich zu informieren und sich nicht von schönen Worten und Bildern täuschen zu lassen. Es gibt viele seriöse Alternativen auf dem Markt, die nachweislich helfen können, Gewicht zu verlieren. Eine ausgewogene Ernährung und regelmäßige Sporteinheiten sind nach wie vor die besten Methoden, um gesund abzunehmen.
Fazit: Reduslim mag ein Fake sein, doch es gibt zahlreiche andere Möglichkeiten, um sein Ziel zu erreichen. Bleibe kritisch und informiere dich gut, bevor du ein Produkt kaufst, das vielleicht nicht die versprochene Wirkung hat.
https://reduslim.at/
https://aviatorghana.pro/# aviator sportybet ghana
Reduslim Per Dimagrire: Die Geheimwaffe zur Gewichtsabnahme
Reduslim Per Dimagrire ist ein innovatives Produkt, das speziell zur Gewichtsabnahme entwickelt wurde. Mit seiner einzigartigen Formel aus natГјrlichen Inhaltsstoffen hilft es dabei, Fett zu verbrennen und den Stoffwechsel anzukurbeln.
Der Schlüssel zum Erfolg von Reduslim Per Dimagrire liegt in seiner Wirksamkeit und Sicherheit. Im Gegensatz zu anderen gewichtsabnahme produkten, enthält es keine schädlichen Chemikalien oder künstlichen Zusätze. Stattdessen setzt es auf bewährte natürliche Inhaltsstoffe wie Grüntee-Extrakt, Garcinia Cambogia und Cayennepfeffer, die bekannt für ihre Fettverbrennungseigenschaften sind.
Durch die regelmäßige Einnahme von Reduslim Per Dimagrire können Sie nicht nur Ihre Pfunde verlieren, sondern auch Ihr Energieniveau steigern und Ihre Gesundheit verbessern. Es ist die ideale Lösung für alle, die auf sichere und effektive Weise abnehmen möchten.
Wenn Sie also bereit sind, Ihr Gewichtsverlustziel zu erreichen, probieren Sie Reduslim Per Dimagrire aus und lassen Sie sich von seinen beeindruckenden Ergebnissen Гјberzeugen. Es ist die Geheimwaffe, die Ihnen helfen wird, Ihre Traumfigur zu erreichen.
https://reduslim.at/
Reduslim Laboratorio ist ein vielversprechendes Produkt, das Menschen hilft, ihr Gewicht auf gesunde und effiziente Weise zu kontrollieren. Das Laboratorio hinter Reduslim hat jahrelange Forschung und Entwicklung investiert, um eine hochwirksame Formel zu entwickeln, die den Stoffwechsel ankurbelt und die Fettverbrennung beschleunigt.
Die natürlichen Inhaltsstoffe von Reduslim Laboratorio sind sorgfältig ausgewählt und bieten eine sichere und effektive Methode, um Gewicht zu verlieren und die Gesundheit zu verbessern. Mit regelmäßiger Einnahme von Reduslim können Benutzer positive Ergebnisse erwarten, einschließlich einer schlankeren Figur, mehr Energie und einer gesteigerten körperlichen Leistungsfähigkeit.
Es ist wichtig zu beachten, dass Reduslim Laboratorio kein Wundermittel ist und eine gesunde Ernährung und regelmäßige Bewegung unerlässlich sind, um optimale Ergebnisse zu erzielen. Dennoch kann Reduslim als Ergänzung zu einem gesunden Lebensstil verwendet werden, um das Gewichtsmanagement zu unterstützen und das Selbstbewusstsein zu steigern.
Probieren Sie Reduslim Laboratorio noch heute aus und lassen Sie sich von den positiven Auswirkungen auf Ihre Gesundheit und Ihr Wohlbefinden Гјberzeugen!
https://reduslim.at/
Reduslim Forte ist ein revolutionäres Nahrungsergänzungsmittel, das dabei hilft, überflüssige Pfunde auf natürliche Weise zu verlieren. Die pflanzlichen Inhaltsstoffe wie Grüner Tee Extrakt und Guarana boosten den Stoffwechsel und fördern die Fettverbrennung. Zudem sind Antioxidantien enthalten, die dem Körper helfen, Giftstoffe auszuscheiden. Reduslim Forte ist einfach anzuwenden und sorgt für langfristige Gewichtsabnahme ohne Jo-Jo-Effekt. Machen Sie sich bereit, um Ihrem Traumgewicht ein Stück näher zu kommen mit Reduslim Forte!
https://reduslim.at/
https://aviatormocambique.site/# jogar aviator
Reduslim Integratore Alimentare ist eine wirksame Lösung für alle, die effektiv abnehmen und ihr Gewicht halten möchten. Dieses Nahrungsergänzungsmittel enthält eine einzigartige Mischung aus natürlichen Inhaltsstoffen, die nachweislich beim Abbau von Fett und der Verbrennung von Kalorien helfen. Durch die Einnahme von Reduslim können Sie Ihren Stoffwechsel ankurbeln und gleichzeitig Ihren Appetit kontrollieren.
Die Kombination aus grünem Tee, Garcinia Cambogia und anderen pflanzlichen Extrakten macht Reduslim zu einem effektiven Gewichtsmanagement-Produkt. Es hilft Ihnen, schneller abzunehmen, ohne dabei auf wichtige Nährstoffe zu verzichten. Darüber hinaus ist Reduslim Integratore Alimentare frei von künstlichen Zusatzstoffen und daher gut verträglich.
Wenn Sie also nach einer natürlichen und sicheren Methode suchen, um Ihr Gewicht zu reduzieren, ist Reduslim Integratore Alimentare die ideale Wahl für Sie. Beginnen Sie noch heute mit der Einnahme und sehen Sie die positiven Veränderungen in Ihrem Körper. Gönnen Sie sich das Beste und erreichen Sie Ihre Traumfigur mit Reduslim!
https://reduslim.at/
Viele Menschen haben Meinungen zu Reduslim, einem beliebten Nahrungsergänzungsmittel zur Gewichtsreduktion. Einige schwören darauf und berichten von tollen Ergebnissen, während andere skeptisch sind und die Wirksamkeit anzweifeln. Die einen loben die natürlichen Inhaltsstoffe und den positiven Einfluss auf den Stoffwechsel, die anderen kritisieren den hohen Preis und die fehlende wissenschaftliche Beweise. Letztendlich muss jeder für sich selbst entscheiden, ob Reduslim das richtige Produkt zur Unterstützung der Gewichtsabnahme ist. Wichtig ist, dass man sich gut informiert und gegebenenfalls auch ärztlichen Rat einholt, bevor man das Mittel einnimmt.
https://reduslim.at/
porn online
Доверь перетяжку мебели квалифицированным специалистам в Минске
ремонт мебели в минске https://obivka-mebeli-vminske.ru/ .
Reduslim Dosaggio – Wie viel sollten Sie einnehmen?
Wenn Sie Reduslim verwenden, ist es entscheidend, das richtige Dosaggio zu kennen, um die bestmöglichen Ergebnisse zu erzielen. Das Dosaggio hängt von verschiedenen Faktoren wie Ihrem Gewicht, Stoffwechsel und Lebensstil ab. Es wird empfohlen, mit einer niedrigen Dosis zu beginnen und diese langsam zu steigern, um festzustellen, wie Ihr Körper reagiert.
Ein typisches Dosaggio für Reduslim liegt zwischen 1-2 Kapseln pro Tag, abhängig von Ihrem Gewicht und Zielen. Es ist wichtig, die empfohlene Dosierung nicht zu überschreiten, um mögliche Nebenwirkungen zu vermeiden. Konsultieren Sie immer Ihren Arzt, bevor Sie ein neues Nahrungsergänzungsmittel einnehmen, insbesondere wenn Sie andere Medikamente einnehmen oder gesundheitliche Probleme haben.
Das richtige Dosaggio kann einen großen Unterschied machen, wenn es darum geht, Ihre Ziele für Gewichtsverlust zu erreichen. Reduslim kann eine wirksame Ergänzung zu einer gesunden Ernährung und regelmäßiger Bewegung sein, um Ihren Stoffwechsel zu steigern und Fett zu verbrennen. Achten Sie darauf, die Anweisungen sorgfältig zu befolgen und Geduld zu haben, da Gewichtsverlust ein Prozess ist, der Zeit und Engagement erfordert.
https://reduslim.at/
Reduslim ist ein bekanntes Produkt, das in der TV-Sendung “HГ¶hle der LГ¶wen” vorgestellt wurde. Das Abnehmprodukt hat in der Vergangenheit bereits fГјr viel Aufsehen gesorgt und konnte zahlreiche Kunden Гјberzeugen. Es verspricht eine effektive Gewichtsreduktion und soll dabei helfen, lГ¤stige Pfunde schnell und einfach loszuwerden.
Doch was steckt hinter dem Erfolg von Reduslim bei Höhle der Löwen? Das Geheimnis liegt in der speziellen Formel, die sorgfältig entwickelt wurde, um den Stoffwechsel zu beschleunigen und den Körper bei der Fettverbrennung zu unterstützen. Die natürlichen Inhaltsstoffe sorgen dafür, dass der Körper auf sanfte Weise entgiftet wird und gleichzeitig das Hungergefühl reduziert wird.
Die positive Resonanz von Kunden, die Reduslim ausprobiert haben, spricht für sich. Viele berichten von schnellen Erfolgen und einer nachhaltigen Gewichtsabnahme. Dabei ist Reduslim nicht nur effektiv, sondern auch gut verträglich und frei von Nebenwirkungen. Wer also auf der Suche nach einer unkomplizierten Lösung für sein Gewichtsproblem ist, sollte Reduslim definitiv eine Chance geben.
In der heutigen Zeit, in der Übergewicht und Adipositas zu immer größeren Problemen werden, ist es wichtig, auf Produkte wie Reduslim bei Höhle der Löwen zu setzen, die eine gesunde und nachhaltige Gewichtsreduktion ermöglichen. Gönnen Sie sich also etwas Gutes und starten Sie noch heute mit Reduslim auf dem Weg zu Ihrer Traumfigur!
https://reduslim.at/
вы можете самостоятельно выбирать, что послушать сегодня, а можно довериться профессиональным диджеям
и радио онлайн слушать.
Feel free to surf to my site https://onlineradioplanet.ru/
Вживані засоби пересування на нашому сайті авторіа біз-це оголошення від громадян України, бу авто які продають особистий авто через.
Here is my page: https://auto-bazar.com.ua/ru/top-b-u-avto-v-ukrayne-luchshye-varyanty-v-sootnoshenyy-tsena-kachestvo-kotorye-stoyt-kupyt/
Apartments, penthouses and full floors in Address Residences Zabeel Dubai with favourable terms of purchase and return on investment.
Филиал автошколы рядом с метро Борисово в Москве – профессиональное обучение на автомобилях с МКПП и АКПП получение водительских прав категории B с оплатой в рассрочку без переплат и скрытых платежей автошкола в митино
Reduslim bg ist ein neues Produkt auf dem Markt für Gewichtsabnahme, das für Aufsehen sorgt. Dieses natürliche Nahrungsergänzungsmittel verspricht, überschüssiges Fett effektiv zu verbrennen und den Stoffwechsel anzuregen. Die Inhaltsstoffe von Reduslim bg sind sorgfältig ausgewählt und sollen dabei helfen, den Körper bei der Gewichtsabnahme zu unterstützen.
Viele Menschen haben bereits positive Erfahrungen mit Reduslim bg gemacht und berichten von schnellen Ergebnissen. Durch die Einnahme der Kapseln wird das HungergefГјhl reduziert und gleichzeitig die Fettverbrennung angekurbelt. Dadurch ist es einfacher, Kalorien zu verbrennen und das Gewicht langfristig zu reduzieren.
Das Besondere an Reduslim bg ist, dass es keine Nebenwirkungen hat und ausschließlich aus natürlichen Inhaltsstoffen besteht. Dadurch ist es eine sichere und effektive Methode, um Gewicht zu verlieren. Wenn auch Sie sich nach einem einfachen und effizienten Weg zur Gewichtsabnahme sehnen, könnte Reduslim bg die Lösung für Sie sein. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Effekten dieses Produkts!
https://reduslim.at/
NFT collection with incomplete edition: The upcoming launch of the nft collection with incomplete
edition, which presents unique and exclusive bitcoin dog designs, to
a greater extent has fueled excitement and anticipation in society bitcoindogs.io.
Here is my homepage :: https://bitcoindogs.io/
In unserem Reduslim Blog finden Sie alles, was Sie Гјber das Abnehmen mit Reduslim wissen mГјssen. Von Erfolgsgeschichten Гјber Tipps und Tricks bis hin zu wissenschaftlichen Erkenntnissen – hier erfahren Sie alles, was Ihnen hilft, Ihr Zielgewicht zu erreichen. Unsere Experten teilen ihr Fachwissen und stehen Ihnen mit Rat und Tat zur Seite. Erfahren Sie, wie Reduslim funktioniert und warum es so effektiv ist. Nutzen Sie unsere Rezepte und TrainingsplГ¤ne, um Ihren Fortschritt zu maximieren. Starten Sie noch heute Ihre Reise zu einem gesГјnderen und glГјcklicheren Leben mit Reduslim! Besuchen Sie unseren Blog und lassen Sie sich inspirieren.
https://reduslim.at/
Филиал автошколы рядом с метро Борисово в Москве – профессиональное обучение на автомобилях с МКПП и АКПП получение водительских прав категории B с оплатой в рассрочку без переплат и скрытых платежей автошкола площадь ильича
http://aviatorjogar.online/# aviator pin up
Reduslim ist ein beliebtes NahrungsergГ¤nzungsmittel, das zur Gewichtsreduktion entwickelt wurde. Viele Menschen interessieren sich dafГјr und fragen sich: “Was ist Reduslim und wie viel kostet es?” Reduslim enthГ¤lt natГјrliche Inhaltsstoffe wie GrГјntee-Extrakt, Garcinia Cambogia und L-Carnitin, die den Stoffwechsel anregen und den Abbau von Fett fГ¶rdern. Es wird empfohlen, Reduslim regelmäßig einzunehmen und mit einer gesunden ErnГ¤hrung und regelmäßiger Bewegung zu kombinieren. Der Preis fГјr Reduslim variiert je nach Anbieter und Packungsgröße, liegt aber in der Regel zwischen 30€ und 50€ pro Packung. Es lohnt sich, verschiedene Angebote zu vergleichen, um das beste Preis-Leistungs-VerhГ¤ltnis zu erhalten. Probieren Sie Reduslim aus und starten Sie Ihren Weg zu einem gesГјnderen und schlankeren KГ¶rper!
https://reduslim.at/
He began his studies in Kezdivasarhely and continued in Nagyenyed , from where he went to foreign universities in Jena and Gottingen https://it.wikipedia.org/wiki/Zoli_%C3%81dok
regardless because of this, do you want do you top up your deposit or to cash out your winnings,
1win we did it incredibly simple
for you.
Reduslim zum Abnehmen ist eine beliebte Wahl unter denen, die Gewicht verlieren und ihren Körper in Form bringen wollen. Dieses natürliche Präparat hilft beim Abbau von Fettreserven und unterstützt den Stoffwechsel. Durch die spezielle Formel werden Hungergefühle reduziert und der Energieverbrauch gesteigert. So lässt sich das Abnehmen leichter und effektiver gestalten.
Die Inhaltsstoffe von Reduslim zum Abnehmen sind sorgfältig ausgewählt und sorgen für eine hohe Wirksamkeit. Grüner Tee-Extrakt, Garcinia Cambogia und Guarana sind nur einige der natürlichen Zutaten, die dabei helfen, die Fettverbrennung zu steigern und den Appetit zu kontrollieren. Dies führt zu einer schnellen Gewichtsabnahme ohne lästiges Hungern oder gefährliche Nebenwirkungen.
Die regelmäßige Einnahme von Reduslim zum Abnehmen kann dabei helfen, das Wunschgewicht zu erreichen und langfristig zu halten. Durch die Unterstützung des Stoffwechsels werden überschüssige Kalorien schneller verbrannt und die Pfunde schmelzen förmlich dahin. Zudem sorgt die verbesserte Energieverbrennung für mehr Vitalität und Wohlbefinden im Alltag.
Also, wenn auch Sie auf der Suche nach einer effektiven Lösung zum Abnehmen sind, sollten Sie Reduslim zum Abnehmen definitiv eine Chance geben. Mit seiner natürlichen Formel und schnellen Wirkung ist es die ideale Unterstützung auf dem Weg zu einem gesünderen und schlankeren Körper. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Ergebnissen!
https://reduslim.at/
Der Bugiardino Reduslim ist ein wichtiger Bestandteil jeder Packung des Abnehmprodukts Reduslim. Das Bugiardino enthält detaillierte Informationen über die Anwendung, Dosierung und mögliche Nebenwirkungen des Produkts. Es ist wichtig, das Bugiardino Reduslim sorgfältig zu lesen, um sicherzustellen, dass man das Produkt richtig anwendet und von den bestmöglichen Ergebnissen profitiert.
Das Bugiardino Reduslim enthält auch wichtige Informationen über die Inhaltsstoffe des Produkts. Diese können helfen, zu verstehen, wie Reduslim funktioniert und warum es so effektiv ist. Durch das Lesen des Bugiardino kann man auch eventuelle Allergien oder Unverträglichkeiten gegenüber bestimmten Inhaltsstoffen erkennen und vermeiden.
Es ist wichtig, das Bugiardino Reduslim immer griffbereit zu haben, um bei Fragen oder Unsicherheiten schnell nachschlagen zu können. Indem man das Bugiardino regelmäßig liest und versteht, kann man sicherstellen, dass man das Produkt sicher und effektiv anwendet. Wenn man das Bugiardino Reduslim richtig verwendet, kann man schneller und dauerhaft Gewicht verlieren.
https://reduslim.at/
Сериал про космос – звездные врата
http://aviatoroyunu.pro/# aviator oyunu
ibuprofen
Incest sex
то есть, koop voor altijd een virtueel telefoonnummer профилей для пиара в соцсетях нужно много.
Бесплатный англоязычный сервис.
Here is my web site … аренда сим карты
Ремонт и перетяжка мягкой мебели в Минске: качество гарантируем
обтяжка мебели https://obivka-divana.ru/ .
always i used to read smaller articles or reviews which as
well clear their motive, and that is also happening with this post which I am reading at
this time.
In 2024, you will be able to find one of three versions
bonuses, which we will list now (no, promocode for melbet), including only promotions that they are
activated by created by us links.
Here is my web page melbet Türkiye
Free download Pinterest SVG Icons for logos, websites and mobile apps, useable in Sketch or Figma twitter icon
נערות ליווי באילת
דירות דיסקרטיות בחיפה
LГҐna 40000 kr
Free download Pinterest SVG Icons for logos, websites and mobile apps, useable in Sketch or Figma facebook icon
Question: available does melbet indir have mobile platforms?
very advantageous melbet
bonus for any visitors. 1. Prizes in fast games.
nawiguj tutaj
http://jogodeaposta.fun/# melhor jogo de aposta para ganhar dinheiro
Твоя мебель выглядит устаревшей? Перетяни ее в Минске!
перетяжка компьютерного кресла https://obivka-divana.ru/ .
Reduslim 90 Kapseln sind das neueste Produkt auf dem Markt, das die Gewichtsabnahme revolutioniert. Mit seiner einzigartigen Formel unterstützt es effektiv beim Abnehmen und kann dabei helfen, lästige Pfunde loszuwerden. Die spezielle Kombination aus natürlichen Inhaltsstoffen sorgt dafür, dass der Stoffwechsel angekurbelt wird und Fett schneller verbrannt wird.
Durch die Einnahme von Reduslim 90 Kapseln können Sie Ihren Körper auf natürliche Weise beim Abnehmen unterstützen, ohne dabei auf strenge Diäten oder anstrengende Workouts angewiesen zu sein. Die Kapseln sind einfach einzunehmen und können problemlos in den Alltag integriert werden.
Die positiven Erfahrungen von Anwendern sprechen fГјr sich – viele berichten von schnellen und langanhaltenden Erfolgen mit Reduslim 90 Kapseln. Probieren auch Sie es aus und starten Sie noch heute Ihren Weg zur Traumfigur mit diesem innovativen Produkt!
https://reduslim.at/
Reduslime ist ein revolutionäres Produkt, das beim Abnehmen helfen kann. Durch seine innovative Formel aus natürlichen Inhaltsstoffen wie Aloe Vera und grünem Tee Extrakt, fördert es die Fettverbrennung und unterstützt den Stoffwechsel. Reduslime ist einfach anzuwenden und kann in Kombination mit einer gesunden Ernährung und regelmäßiger Bewegung maximale Ergebnisse erzielen. Viele zufriedene Kunden schwören auf die Wirkung von Reduslime und berichten von schnellen und nachhaltigen Gewichtsverlusten. Probieren auch Sie Reduslime aus und starten Sie noch heute Ihre Reise zur Traumfigur!
https://reduslim.at/
Reduslim ist ein beliebtes Produkt zur Gewichtsreduktion, das in den letzten Jahren immer bekannter geworden ist. Doch was ist Reduslim eigentlich? Es handelt sich um eine natürliche Nahrungsergänzung, die dabei helfen soll, Fett zu verbrennen und den Stoffwechsel zu beschleunigen.
Die Hauptbestandteile von Reduslim sind natürliche Extrakte, die eine Fettverbrennung fördern und den Körper dabei unterstützen, überschüssige Pfunde loszuwerden. Zu den Inhaltsstoffen gehören unter anderem grüner Kaffee, Garcinia Cambogia und Ingwerextrakt.
Doch wie genau funktioniert Reduslim? Durch die Einnahme der Kapseln wird der Stoffwechsel angeregt und die Fettverbrennung beschleunigt. Gleichzeitig wird das HungergefГјhl verringert, was dazu fГјhrt, dass man automatisch weniger isst. Somit kann Reduslim dabei helfen, Gewicht auf gesunde und natГјrliche Weise zu verlieren.
Es ist jedoch wichtig zu beachten, dass Reduslim kein Wundermittel ist und eine gesunde Ernährung sowie ausreichend Bewegung nicht ersetzen kann. Eine ausgewogene Lebensweise ist weiterhin entscheidend, um dauerhaft abzunehmen und sein Wunschgewicht zu halten.
Insgesamt kann gesagt werden, dass Reduslim eine effektive UnterstГјtzung bei der Gewichtsreduktion sein kann, jedoch keine Wunder bewirkt. Mit einer Kombination aus der Einnahme der Kapseln, einer ausgewogenen ErnГ¤hrung und regelmäßiger Bewegung kann man jedoch auf dem Weg zur Traumfigur unterstГјtzt werden. Que es el Reduslim? – Ein natГјrlicher und effektiver Helfer auf dem Weg zur Traumfigur!
https://reduslim.at/
купить диплом техникума .
The balance of coins and a button for exchanging them for cash
in the personal account. specifically because
you can to use the 1win mobile 1win Türkiye. essential find footnote
to current mirror and insert its into any your browser on device.
My site; 1win giris
6. sonunda/sonunda, yapabilirsin/sans?n?z var kolay/sorunsuz ve guvenilir/garantili para cekme/terfi etme kendi/kendi kazanc?n?z. https://easestravel.ru/much-space-in-world/ ayr?ca saglar/sunar genis/zengin musteri destek seceneklerinin yelpazesi.
“Come si prende Reduslim” ist eine hГ¤ufig gestellte Frage von Menschen, die auf der Suche nach einem natГјrlichen und effektiven Weg zur Gewichtsabnahme sind. Es ist wichtig zu wissen, dass Reduslim ein NahrungsergГ¤nzungsmittel ist, das bei der Gewichtsabnahme helfen kann, aber keine Wundermittel sind.
Um Reduslim effektiv zu nehmen, sollten die Anweisungen auf der Verpackung genau befolgt werden. Die empfohlene Dosierung beträgt in der Regel zwei Kapseln pro Tag, vorzugsweise vor den Mahlzeiten. Es ist wichtig, Reduslim regelmäßig einzunehmen und mit einer gesunden Ernährung und ausreichender körperlicher Bewegung zu kombinieren.
Es ist auch wichtig, sich bewusst zu machen, dass Reduslim keine langfristige Lösung für Gewichtsprobleme ist. Es sollte als Teil eines gesunden Lebensstils betrachtet werden. Konsultieren Sie immer einen Arzt, bevor Sie ein Nahrungsergänzungsmittel einnehmen, um sicherzustellen, dass es für Ihre individuellen Bedürfnisse geeignet ist.
Insgesamt kann Reduslim eine nützliche Ergänzung zu einer gesunden Ernährung und Lebensweise sein, um beim Abnehmen zu helfen. Durch die Beachtung der Dosierungsempfehlungen und die Kombination mit gesunden Gewohnheiten können positive Ergebnisse erzielt werden. Denken Sie jedoch daran, dass nachhaltige Veränderungen im Lebensstil der Schlüssel zu langfristigem Erfolg bei der Gewichtsabnahme sind.
https://reduslim.at/
Portal Judi: Portal Lotere Online Terbesar dan Terpercaya
Portal Judi telah menjadi salah satu portal judi online terluas dan terjamin di Indonesia. Dengan beragam pasaran yang disediakan dari Grup Semar, Portal Judi menawarkan sensasi main togel yang tak tertandingi kepada para penggemar judi daring.
Market Terbaik dan Terlengkap
Dengan total 56 pasaran, Situs Judi memperlihatkan beberapa opsi terunggul dari market togel di seluruh dunia. Mulai dari market klasik seperti Sydney, Singapore, dan Hongkong hingga market eksotis seperti Thailand, Germany, dan Texas Day, setiap pemain dapat menemukan pasaran favorit mereka dengan mudah.
Langkah Bermain yang Mudah
Situs Judi menyediakan tutorial cara main yang praktis dipahami bagi para pemula maupun penggemar togel berpengalaman. Dari langkah-langkah pendaftaran hingga penarikan kemenangan, semua informasi tersedia dengan jelas di situs Portal Judi.
Rekapitulasi Terakhir dan Info Terkini
Pemain dapat mengakses hasil terakhir dari setiap pasaran secara real-time di Portal Judi. Selain itu, info paling baru seperti jadwal bank daring, gangguan, dan offline juga disediakan untuk memastikan kelancaran proses transaksi.
Berbagai Jenis Game
Selain togel, Ngamenjitu juga menawarkan berbagai jenis permainan kasino dan judi lainnya. Dari bingo hingga roulette, dari dragon tiger hingga baccarat, setiap pemain dapat menikmati bervariasi pilihan permainan yang menarik dan menghibur.
Security dan Kepuasan Klien Terjamin
Situs Judi mengutamakan security dan kepuasan pelanggan. Dengan sistem keamanan terbaru dan layanan pelanggan yang responsif, setiap pemain dapat bermain dengan nyaman dan tenang di platform ini.
Promosi dan Bonus Istimewa
Situs Judi juga menawarkan berbagai promosi dan bonus istimewa bagi para pemain setia maupun yang baru bergabung. Dari bonus deposit hingga bonus referral, setiap pemain memiliki kesempatan untuk meningkatkan kemenangan mereka dengan hadiah yang ditawarkan.
Dengan semua fasilitas dan pelayanan yang ditawarkan, Portal Judi tetap menjadi pilihan utama bagi para penggemar judi online di Indonesia. Bergabunglah sekarang dan nikmati pengalaman bermain yang seru dan menguntungkan di Portal Judi!
porn
Reduslim ist ein beliebtes Schlankheitsmittel, das vielen Menschen hilft, ihr Gewicht zu reduzieren. Es ist in vielen LГ¤ndern erhГ¤ltlich, darunter auch in Deutschland. Wenn Sie daran interessiert sind, Reduslim zu kaufen, kГ¶nnen Sie es ganz einfach online bestellen. Geben Sie einfach den Suchbegriff “Reduslim comprar” in Ihre Suchmaschine ein und finden Sie verschiedene Optionen, um das Produkt zu erwerben. Vergewissern Sie sich, dass Sie das Produkt nur von vertrauenswГјrdigen Quellen kaufen, um sicherzustellen, dass Sie ein hochwertiges und authentisches Produkt erhalten. Reduslim kann eine effektive LГ¶sung sein, um Ihren Zielen beim Abnehmen nГ¤her zu kommen. Probieren Sie es noch heute aus und erleben Sie die Vorteile selbst!
https://reduslim.at/
http://aviatormalawi.online/# aviator
LГҐn 30000 kr
Reduslim ist ein beliebtes Gewichtsverlustprodukt, das vielen Menschen dabei geholfen hat, effektiv abzunehmen. Aber wie macht man eigentlich Reduslim? Zuerst muss man das Produkt online kaufen und regelmäßig einnehmen. Die natürlichen Inhaltsstoffe in Reduslim helfen dabei, den Stoffwechsel zu beschleunigen und den Appetit zu unterdrücken. Es ist wichtig, eine gesunde Ernährung beizubehalten und regelmäßig Sport zu treiben, um optimale Ergebnisse zu erzielen. Außerdem sollte man ausreichend Wasser trinken und Stress vermeiden, um den Erfolg von Reduslim zu maximieren. Probieren Sie es aus und sehen Sie selbst, wie Reduslim Ihr Leben verändern kann!
https://reduslim.at/
Reduslim Inhaltsstoffe sind ein wichtiger Bestandteil dieses Diätsupplements. Die speziell ausgewählten Zutaten tragen zur effektiven Gewichtsabnahme bei, indem sie den Stoffwechsel ankurbeln und das Hungergefühl reduzieren. Zu den Hauptbestandteilen von Reduslim zählen Grüntee-Extrakt, L-Carnitin, Garcinia Cambogia und Guarana. Diese natürlichen Inhaltsstoffe wirken synergistisch zusammen, um Fettverbrennung zu fördern und den Körper mit Energie zu versorgen. Reduslim wird oft als die ultimative Lösung für diejenigen gepriesen, die schnell und effektiv abnehmen möchten. Durch die regelmäßige Einnahme dieses Supplements können Sie Ihren Traumkörper erreichen und sich rundum wohlfühlen. Probieren Sie Reduslim noch heute aus und überzeugen Sie sich selbst von seiner Wirksamkeit!
https://reduslim.at/
Wenn negative Recensioni su Reduslim im Internet auftauchen, sollte man sich nicht entmutigen lassen. Oftmals handelt es sich bei solchen Bewertungen um Einzelfälle oder Meinungen von Personen, die nicht erfolglos mit dem Produkt waren. Reduslim ist ein Nahrungsergänzungsmittel, das helfen kann, Gewicht zu verlieren und den Stoffwechsel zu unterstützen. Es ist jedoch wichtig, dass man auch die richtige Ernährung und ausreichend Bewegung in seinen Alltag integriert, um langfristige Erfolge zu erzielen. Bevor man sich von negativen Recensioni su Reduslim beeinflussen lässt, sollte man sich am besten von einem Arzt oder Ernährungsberater beraten lassen.
https://reduslim.at/
where is the download good melbet indir app?
Their exact list depends on the currency of personal cabinet and state
of registration. Hundreds of tables with dealers speaking diverse languages.
Reduslim ist ein beliebtes Produkt zur Gewichtsabnahme, das in Form von Pillen erhГ¤ltlich ist. Viele Menschen fragen sich jedoch: “Como se toma Reduslim en pastillas?” Die Antwort ist einfach: Nehmen Sie einfach eine Tablette zweimal tГ¤glich vor den Mahlzeiten mit einem Glas Wasser ein. Dies hilft, den Stoffwechsel zu beschleunigen und den Appetit zu unterdrГјcken, was zu einer effektiven Gewichtsabnahme fГјhrt. DarГјber hinaus enthГ¤lt Reduslim natГјrliche Inhaltsstoffe wie GrГјntee-Extrakt und Guarana, die dabei helfen, Fett zu verbrennen und den Energielevel zu erhГ¶hen. Probieren Sie Reduslim noch heute aus und erleben Sie die Vorteile einer gesunden Gewichtsabnahme.
https://reduslim.at/
Reduslim ist ein stark beworbenes Produkt auf dem Markt fГјr Gewichtsverlust. Viele Menschen fragen sich, ob es wirklich so gut ist, wie es behauptet wird. Die Meinungen darГјber sind gemischt.
Einige Benutzer schwören auf die Wirksamkeit von Reduslim und berichten von erstaunlichen Ergebnissen in kurzer Zeit. Sie loben die natürlichen Inhaltsstoffe und die schnelle Gewichtsabnahme, die sie erlebt haben.
Andere sind skeptischer und bezweifeln, ob Reduslim tatsächlich so gut ist, wie es verspricht. Sie weisen darauf hin, dass jede Person unterschiedlich auf Nahrungsergänzungsmittel reagiert und dass nicht jeder die gleichen Ergebnisse erzielen wird.
Es ist wichtig zu beachten, dass Reduslim nur ein Hilfsmittel zur Gewichtsabnahme ist und nicht als alleinige Lösung betrachtet werden sollte. Eine ausgewogene Ernährung und regelmäßige Bewegung sind unerlässlich, um langfristige Erfolge zu erzielen.
Letztendlich ist es ratsam, sich vor der Einnahme von Reduslim von einem Arzt beraten zu lassen, um sicherzustellen, dass es für Sie geeignet ist. Jeder Körper ist anders und was für den einen gut funktioniert, mag für den anderen nicht geeignet sein. Reduslim könnte also für einige Menschen wirklich so gut sein, aber für andere vielleicht nicht. Es ist wichtig, realistische Erwartungen zu haben und geduldig zu sein, um die gewünschten Ergebnisse zu erzielen.
https://reduslim.at/
crfyq woidz culkl yafgi twlha olike
Reduslim ist ein beliebtes Produkt zur Gewichtsreduzierung, das immer mehr Menschen nutzen, um ihre Fitnessziele zu erreichen. Aber eine hГ¤ufig gestellte Frage ist: “Wie teuer ist Reduslim?”. Die Preise kГ¶nnen je nach Anbieter variieren, aber in der Regel liegt der Preis fГјr eine Packung bei etwa 50-70 Euro.
Es ist wichtig zu betonen, dass Reduslim ein qualitativ hochwertiges Produkt ist, das aus natürlichen Inhaltsstoffen hergestellt wird und daher sein Geld wert ist. Viele Menschen haben positive Erfahrungen mit Reduslim gemacht und schwören darauf, dass es ihnen geholfen hat, ihr Gewicht zu reduzieren und ihr Wohlbefinden zu steigern.
Wenn Sie also darüber nachdenken, Reduslim auszuprobieren, sollten Sie sich nicht nur fragen, wie teuer es ist, sondern auch die potenziellen Vorteile in Betracht ziehen. Mit einer gesunden Ernährung und regelmäßiger Bewegung kann Reduslim Ihnen dabei helfen, Ihre Ziele zu erreichen und ein gesünderes Leben zu führen. Also zögern Sie nicht länger und investieren Sie in Ihre Gesundheit mit Reduslim!
https://reduslim.at/
Auf der Suche nach einem effektiven Weg, um Gewicht zu verlieren? Dann ist Reduslim vielleicht die Antwort, die Sie suchen. Bei einem günstigen Reduslim ára bietet dieses natürliche Nahrungsergänzungsmittel eine sichere und effektive Methode, um Gewicht zu verlieren und Ihren Körper zu straffen.
Die einzigartige Formel von Reduslim kombiniert natürliche Inhaltsstoffe, die den Stoffwechsel ankurbeln und die Fettverbrennung unterstützen. Dadurch können Sie schneller und einfacher abnehmen, ohne auf Ihre Lieblingsspeisen verzichten zu müssen.
Mit regelmäßiger Einnahme von Reduslim können Sie nicht nur Gewicht verlieren, sondern auch Ihr allgemeines Wohlbefinden verbessern. Das Reduslim ára ist erschwinglich und bietet ein unschlagbares Preis-Leistungs-Verhältnis im Vergleich zu anderen Abnehmprodukten auf dem Markt.
Nutzen Sie also die Gelegenheit und probieren Sie Reduslim noch heute aus. Machen Sie den ersten Schritt zu einem gesünderen und schlankeren Körper und bestellen Sie jetzt zu einem unschlagbaren Reduslim ára.
https://reduslim.at/
www reduslim de ist eine Webseite, die sich auf natürliche und effektive Gewichtsabnahme konzentriert. Durch die Nutzung von hochwertigen Inhaltsstoffen und innovativen Technologien, bietet Reduslim eine sichere Möglichkeit, um auf gesunde Weise Gewicht zu verlieren.
Die Produkte auf www reduslim de sind sowohl für Männer als auch für Frauen geeignet und helfen dabei, den Stoffwechsel zu beschleunigen und das Hungergefühl zu reduzieren. Dadurch wird das Abnehmen erleichtert und der Körper mit wichtigen Nährstoffen versorgt.
Durch die Verwendung von Reduslim können Sie nicht nur Gewicht verlieren, sondern auch Ihre Gesundheit verbessern und sich insgesamt wohler fühlen. Die positiven Erfahrungsberichte und Bewertungen auf www reduslim de bestätigen die Wirksamkeit der Produkte und zeigen, dass viele Menschen bereits erfolgreich mithilfe von Reduslim abgenommen haben.
Wenn auch Sie von den Vorteilen einer natürlichen Gewichtsabnahme profitieren möchten, sollten Sie einen Blick auf www reduslim de werfen und sich über die verschiedenen Produkte informieren. Starten Sie noch heute Ihre Reise zu einem gesünderen und glücklicheren Leben mit Reduslim!
https://reduslim.at/
Хочешь обновить интерьер? Перетянем твою мебель в Минске
перетянуть диван https://obivka-divana.ru/ .
Auf der Suche nach Reduslim Test Berichte werden Sie auf zahlreiche Erfahrungsberichte von Menschen stoßen, die das Produkt ausprobiert haben. Viele berichten von positiven Ergebnissen und einer erfolgreichen Gewichtsabnahme. Doch wie genau funktioniert Reduslim? Das Nahrungsergänzungsmittel soll den Stoffwechsel ankurbeln und das Hungergefühl reduzieren. Dadurch fällt es leichter, eine kalorienreduzierte Ernährung durchzuhalten und abzunehmen. Die enthaltenen Inhaltsstoffe sollen den Körper dabei unterstützen, Fett zu verbrennen und die Energieproduktion zu steigern. Es ist jedoch wichtig zu beachten, dass Reduslim allein keine Wunder bewirken kann. Eine gesunde Ernährung und ausreichend Bewegung sind nach wie vor die Grundlage für eine erfolgreiche Gewichtsabnahme. Bevor Sie Reduslim ausprobieren, sollten Sie sich gründlich informieren und mögliche Nebenwirkungen beachten. Lesen Sie sich dazu die verschiedenen Testberichte und Erfahrungen anderer Nutzer durch, um eine fundierte Entscheidung zu treffen. Mit der richtigen Herangehensweise kann Reduslim Ihnen vielleicht dabei helfen, Ihr Zielgewicht zu erreichen.
https://reduslim.at/
Reduslim: Arnaque ou pas?
Es gibt viele Produkte auf dem Markt, die versprechen, beim Abnehmen zu helfen. Eines dieser Produkte ist Reduslim. Doch ist Reduslim wirklich so effektiv, wie es angepriesen wird, oder handelt es sich um Betrug?
Einige Kunden berichten von positiven Erfahrungen mit Reduslim und loben die schnellen Ergebnisse. Sie fГјhlen sich leichter, energiegeladener und haben erfolgreich Gewicht verloren. Doch andere Kunden warnen vor der Einnahme von Reduslim und bezeichnen es als Geldverschwendung.
Es ist wichtig, sich vor dem Kauf eines Abnehmprodukts gut zu informieren und Erfahrungsberichte zu lesen. Außerdem sollte man immer auf mögliche Nebenwirkungen achten und gegebenenfalls einen Arzt konsultieren.
Fazit: Reduslim kann fГјr einige Menschen effektiv sein, fГјr andere jedoch nicht. Es ist wichtig, realistische Erwartungen zu haben und sich bewusst zu sein, dass es kein Wundermittel fГјr schnelles Abnehmen gibt. Letztendlich bleibt die Entscheidung, ob Reduslim eine Arnaque oder nicht ist, jedem selbst Гјberlassen.
https://reduslim.at/
Link Alternatif Ngamenjitu
Ngamenjitu: Platform Togel Online Terbesar dan Terjamin
Portal Judi telah menjadi salah satu portal judi online terbesar dan terjamin di Indonesia. Dengan bervariasi market yang disediakan dari Semar Group, Situs Judi menawarkan pengalaman bermain togel yang tak tertandingi kepada para penggemar judi daring.
Market Terunggul dan Terlengkap
Dengan total 56 market, Situs Judi menampilkan berbagai opsi terunggul dari pasaran togel di seluruh dunia. Mulai dari pasaran klasik seperti Sydney, Singapore, dan Hongkong hingga pasaran eksotis seperti Thailand, Germany, dan Texas Day, setiap pemain dapat menemukan pasaran favorit mereka dengan mudah.
Cara Main yang Praktis
Situs Judi menyediakan petunjuk cara bermain yang praktis dipahami bagi para pemula maupun penggemar togel berpengalaman. Dari langkah-langkah pendaftaran hingga penarikan kemenangan, semua informasi tersedia dengan jelas di platform Situs Judi.
Ringkasan Terakhir dan Info Terkini
Pemain dapat mengakses hasil terakhir dari setiap market secara real-time di Portal Judi. Selain itu, informasi terkini seperti jadwal bank online, gangguan, dan offline juga disediakan untuk memastikan kelancaran proses transaksi.
Pelbagai Macam Game
Selain togel, Situs Judi juga menawarkan bervariasi jenis permainan kasino dan judi lainnya. Dari bingo hingga roulette, dari dragon tiger hingga baccarat, setiap pemain dapat menikmati bervariasi pilihan permainan yang menarik dan menghibur.
Keamanan dan Kenyamanan Klien Terjamin
Ngamenjitu mengutamakan keamanan dan kepuasan pelanggan. Dengan sistem keamanan terbaru dan layanan pelanggan yang responsif, setiap pemain dapat bermain dengan nyaman dan tenang di situs ini.
Promosi dan Hadiah Istimewa
Portal Judi juga menawarkan bervariasi promosi dan hadiah menarik bagi para pemain setia maupun yang baru bergabung. Dari bonus deposit hingga bonus referral, setiap pemain memiliki kesempatan untuk meningkatkan kemenangan mereka dengan hadiah yang ditawarkan.
Dengan semua fitur dan pelayanan yang ditawarkan, Portal Judi tetap menjadi pilihan utama bagi para penggemar judi online di Indonesia. Bergabunglah sekarang dan nikmati pengalaman bermain yang seru dan menguntungkan di Situs Judi!
Capsule Reduslim ist das neue Wundermittel zur Gewichtsabnahme, das momentan überall im Gespräch ist. Die innovativen Kapseln sollen dank ihrer einzigartigen Formel und natürlichen Inhaltsstoffe dabei helfen, überschüssige Pfunde schnell und effektiv zu verlieren. Obwohl es viele Produkte auf dem Markt gibt, verspricht Reduslim echte Ergebnisse ohne Jo-Jo-Effekt. Die Kapseln können den Stoffwechsel ankurbeln, das Hungergefühl reduzieren und die Fettverbrennung unterstützen. Wer also auf der Suche nach einer einfachen und effizienten Methode ist, um Gewicht zu verlieren, sollte definitiv Capsule Reduslim ausprobieren.
https://reduslim.at/
Der Reduslim Jojo-Effekt hat bereits viele Menschen verunsichert, die auf der Suche nach einer schnellen und langfristigen Lösung für ihr Gewichtsproblem sind. Dieses Phänomen tritt auf, wenn man nach einer erfolgreichen Diät wieder an Gewicht zunimmt. Oftmals passiert dies, weil man nach der Diät in alte Essgewohnheiten zurückfällt oder sein Bewegungsverhalten vernachlässigt.
Doch mit Reduslim, einem effektiven und natürlichen Nahrungsergänzungsmittel, kannst du den Jojo-Effekt erfolgreich bekämpfen. Die spezielle Formel aus natürlichen Zutaten hilft dir nicht nur beim Abnehmen, sondern unterstützt auch dabei, dein neues Gewicht langfristig zu halten.
Indem Reduslim deinen Stoffwechsel ankurbelt und deinen Appetit zügelt, kannst du effektiv Fett verbrennen und deinen Körper in Form bringen. Der Jojo-Effekt wird somit minimiert und du kannst stolz auf deine Erfolge sein.
Also, lass dich nicht von dem Reduslim Jojo-Effekt entmutigen, sondern nutze dieses Nahrungsergänzungsmittel als Unterstützung auf deinem Weg zu einem gesünderen und schlankeren Körper.
https://reduslim.at/
Du mГ¶chtest abnehmen, aber weiГџt nicht, wo du Hilfe finden kannst? Der “numero verde reduslim” ist die perfekte LГ¶sung fГјr dich! Mit diesem Service hast du die MГ¶glichkeit, professionelle Beratung und UnterstГјtzung auf dem Weg zu deiner Traumfigur zu erhalten.
Der “numero verde reduslim” bietet dir eine kostenlose Telefonnummer, unter der du Experten erreichen kannst, die dir bei allen Fragen rund um das Thema Abnehmen helfen. Egal ob du Tipps zur gesunden ErnГ¤hrung benГ¶tigst oder nach einem effektiven Trainingsplan suchst, die Berater am anderen Ende der Leitung stehen dir mit Rat und Tat zur Seite.
Mit dem “numero verde reduslim” bekommst du auch die MГ¶glichkeit, das beliebte Abnehmprodukt Reduslim direkt zu bestellen. Dieses Produkt hat sich bereits bei vielen Menschen als effektiv erwiesen und kann dir dabei helfen, dein Zielgewicht zu erreichen.
Warte nicht lГ¤nger und rufe noch heute den “numero verde reduslim” an, um deine Abnehmziele zu verwirklichen!
https://reduslim.at/
Reduslim Precio bei Amazon: Ist es das wert?
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das oft auf Amazon verkauft wird. Viele Menschen fragen sich, ob der Preis von Reduslim auf Amazon es wirklich wert ist. Die Meinungen dazu sind geteilt.
Einige Kunden schwören auf die Wirksamkeit von Reduslim und sind bereit, den Preis zu zahlen, da sie positive Ergebnisse bei der Gewichtsabnahme gesehen haben. Andere sind skeptisch und meinen, dass es günstigere Alternativen gibt, die genauso effektiv sind.
Es ist wichtig zu beachten, dass der Preis von Reduslim bei Amazon je nach Verkäufer variieren kann. Es lohnt sich, die verschiedenen Angebote zu vergleichen und sich über die Inhaltsstoffe und die Wirksamkeit des Produkts zu informieren, bevor man eine Entscheidung trifft.
Insgesamt kann gesagt werden, dass Reduslim aufgrund seiner Beliebtheit und zahlreichen positiven Bewertungen einen Blick wert ist. Ob der Preis bei Amazon gerechtfertigt ist, bleibt jedoch jedem selbst Гјberlassen. Es empfiehlt sich, vor dem Kauf grГјndlich zu recherchieren und gegebenenfalls auch andere Verkaufsplattformen zu prГјfen.
https://reduslim.at/
Reduslim Como usar ist eine beliebte Methode zur Gewichtsreduktion, die immer mehr Anhänger findet. Dieses natürliche Nahrungsergänzungsmittel verspricht, den Stoffwechsel anzukurbeln und somit effektiv Fett zu verbrennen. Doch wie genau wird Reduslim verwendet?
Die Anwendung von Reduslim ist denkbar einfach. Man nimmt täglich zwei Kapseln mit ausreichend Flüssigkeit ein, am besten vor den Mahlzeiten. Das enthaltene Grüntee-Extrakt soll den Stoffwechsel ankurbeln und somit den Gewichtsverlust unterstützen. Zudem soll die enthaltene Glucomannan-Wurzel dabei helfen, das Sättigungsgefühl zu steigern und somit Heißhungerattacken vorzubeugen.
Um die bestmöglichen Ergebnisse zu erzielen, ist es ratsam, Reduslim als Teil eines gesunden Lebensstils zu verwenden. Eine ausgewogene Ernährung und regelmäßige Bewegung sind auch weiterhin unverzichtbar für einen langfristigen Erfolg. Zudem sollte man auf ausreichend Schlaf und eine ausreichende Flüssigkeitszufuhr achten.
Insgesamt scheint Reduslim Como usar eine vielversprechende Methode zur Gewichtsreduktion zu sein, die auf natГјrliche Weise den Stoffwechsel ankurbelt und somit beim Abnehmen unterstГјtzt. Mit der richtigen Anwendung und einem gesunden Lebensstil kann Reduslim eine effektive UnterstГјtzung auf dem Weg zur Wunschfigur sein.
https://reduslim.at/
besides, options payment are safe. Choose the method of depositing 1xbet Türkiye accounts, easy in your area.
Here is my web-site: https://1xbettur-3.info/
Reduslim ist ein beliebtes Produkt zur Gewichtsabnahme, das für seine wirksamen Inhaltsstoffe bekannt ist. Die Inhaltsstoffe von Reduslim spielen eine entscheidende Rolle bei der Förderung des Gewichtsverlusts und der Verbesserung der Gesundheit. Zu den wichtigsten Inhaltsstoffen gehören Grüntee-Extrakt, Garcinia Cambogia, L-Carnitin und Chrom.
Der Grüntee-Extrakt ist bekannt für seine antioxidativen Eigenschaften und hilft, den Stoffwechsel zu unterstützen. Garcinia Cambogia ist eine Frucht, die natürliche Appetitzügler enthält und die Fettverbrennung fördert. L-Carnitin ist ein Aminosäure, die dazu beiträgt, Fett in Energie umzuwandeln, während Chrom den Blutzuckerspiegel reguliert und Heißhungerattacken reduziert.
Diese leistungsstarken Inhaltsstoffe arbeiten zusammen, um den Stoffwechsel zu beschleunigen, den Appetit zu kontrollieren und die Fettverbrennung zu fördern. Reduslim ist somit eine effektive Lösung für diejenigen, die auf gesunde und natürliche Weise abnehmen möchten. Wer sich für eine nachhaltige Gewichtsreduktion interessiert, sollte die Inhaltsstoffe von Reduslim genauer unter die Lupe nehmen und sich selbst von ihrer Wirksamkeit überzeugen.
https://reduslim.at/
Reduslim Abnehmen ist eine effektive Methode, um schnell und gesund Gewicht zu verlieren. Dieses Nahrungsergänzungsmittel enthält natürliche Inhaltsstoffe, die den Stoffwechsel ankurbeln und die Fettverbrennung fördern. Durch die Einnahme von Reduslim können überschüssige Pfunde ohne großen Aufwand geschmolzen werden.
Die Kapseln sind einfach einzunehmen und können problemlos in den Alltag integriert werden. Reduslim Abnehmen funktioniert ohne strenge Diäten oder zeitaufwendige Workouts. Die natürlichen Inhaltsstoffe fördern das Sättigungsgefühl und reduzieren Heißhungerattacken. Dadurch wird ein schnellerer Gewichtsverlust ermöglicht.
Viele zufriedene Anwender berichten von beeindruckenden Ergebnissen nach der Einnahme von Reduslim. Sie konnten ihr Wunschgewicht erreichen und fühlen sich fitter und gesünder denn je. Wenn auch Sie von den Vorteilen dieses Nahrungsergänzungsmittels profitieren möchten, probieren Sie Reduslim Abnehmen aus und starten Sie noch heute Ihren Weg zu einer schlankeren Figur und einem besseren Körpergefühl.
https://reduslim.at/
Reduslim Cymes Avis ist ein beliebtes Schlankheitspräparat, das auf natürlichen Inhaltsstoffen basiert. Viele Menschen schwören auf die Wirksamkeit dieser Kapseln, um überschüssige Kilos loszuwerden. Doch was steckt wirklich hinter dem Hype um Reduslim Cymes Avis?
Die Meinungen der Nutzer sind gemischt. Einige berichten von schnellen Erfolgen und einer effektiven Gewichtsabnahme, andere wiederum sind weniger Гјberzeugt von der Wirkung. Dennoch bleibt der Trend um Reduslim Cymes Avis bestehen und immer mehr Menschen probieren das Produkt aus.
Die natürlichen Inhaltsstoffe sollen den Stoffwechsel ankurbeln und den Appetit zügeln. Dadurch wird die Fettverbrennung angeregt und die Pfunde schmelzen angeblich wie von selbst. Doch wie bei jedem Schlankheitsmittel ist auch hier eine ausgewogene Ernährung und ausreichend Bewegung wichtig, um langfristige Erfolge zu erzielen.
Alles in allem scheint Reduslim Cymes Avis eine vielversprechende Option zu sein, um Gewicht zu verlieren. Es lohnt sich auf jeden Fall, das Produkt einmal auszuprobieren und selbst zu testen, ob die Kapseln tatsächlich halten, was sie versprechen. Letztendlich ist es jedoch eine individuelle Entscheidung, ob man diesen Trend mitmacht oder lieber auf altbewährte Methoden setzt.
https://reduslim.at/
It is convenient for beginners a crypto wallet that offers its customers armor-piercing protection and authority over their https://1inchwallet.app/.
Старая мебель? Нет проблем, перетянем ее в Минске
обивка стульев https://obivka-divana.ru/ .
Reduslim ist ein revolutionäres Produkt, das dabei hilft, auf natürliche Weise Gewicht zu verlieren. Die Reduslim Cymes Prix sind für ihre Wirksamkeit und Effektivität bekannt. Diese Pillen setzen auf die Kraft von natürlichen Inhaltsstoffen, um den Stoffwechsel anzukurbeln und Fett schneller zu verbrennen. Der Preis mag auf den ersten Blick hoch erscheinen, aber die Ergebnisse sprechen für sich.
Die Reduslim Cymes Prix sind speziell formuliert, um den Appetit zu reduzieren und Heißhungerattacken zu kontrollieren. So bleibt man länger satt und nimmt insgesamt weniger Kalorien zu sich. Außerdem werden die Fettreserven im Körper effektiv abgebaut, was zu einer schlankeren Figur führt.
Die positiven Erfahrungsberichte der Anwender sprechen für sich. Viele berichten von einem schnellen und spürbaren Gewichtsverlust, ohne dabei auf eine strenge Diät oder anstrengendes Training angewiesen zu sein. Die Reduslim Cymes Prix sind eine natürliche und schonende Methode, um gesund abzunehmen.
Wer also auf der Suche nach einer effektiven und sicheren Lösung für sein Gewichtsproblem ist, sollte die Reduslim Cymes Prix in Betracht ziehen. Mit ihrer natürlichen Formel und ihrer nachgewiesenen Wirksamkeit sind sie eine vielversprechende Option für alle, die ihr Traumgewicht erreichen wollen.
https://reduslim.at/
Качественно перетянем мебель в Минске – долгое время сохранится ее вид
перетяжка мягкой мебели цены https://obivka-divana.ru/ .
Где купить виртуальный номер: рейтинг лучших сервисов SMS-активаций. Как и в других подобных сервисах, здесь вы можете купить номер для разового использования или взять номер в аренду на более длительный срок virtueel nummer voor altijd
Reduslim in Apotheke kaufen – eine sichere und effektive Möglichkeit, um Gewicht zu verlieren. Reduslim ist ein natürliches Nahrungsergänzungsmittel, das dabei hilft, den Stoffwechsel zu steigern und Fett effektiv zu verbrennen. Viele Menschen suchen nach einer einfachen Lösung, um ihr Gewicht zu reduzieren, und finden in Reduslim die Antwort.
Durch die Einnahme von Reduslim können Sie Ihren Körper dabei unterstützen, überschüssiges Fett zu verbrennen und gleichzeitig den Appetit zu reduzieren. Dies führt dazu, dass Sie weniger Kalorien zu sich nehmen und somit leichter abnehmen können. Reduslim enthält nur natürliche Inhaltsstoffe, die keine unerwünschten Nebenwirkungen hervorrufen.
Wenn Sie Reduslim in der Apotheke kaufen möchten, sollten Sie darauf achten, dass Sie ein zertifiziertes Produkt erwerben. Achten Sie auf das Siegel und die Herstellerangaben, um sicherzustellen, dass es sich um ein qualitativ hochwertiges Produkt handelt. Mit Reduslim können Sie auf natürliche Weise Gewicht verlieren und sich dabei gesünder und fitter fühlen. Gönnen Sie sich den ersten Schritt zu einem gesünderen Lebensstil und kaufen Sie Reduslim in der Apotheke.
https://reduslim.at/
Где купить виртуальный номер: рейтинг лучших сервисов SMS-активаций. Как и в других подобных сервисах, здесь вы можете купить номер для разового использования или взять номер в аренду на более длительный срок аренда сим карты
Reduslim Sklad ist ein beliebtes Nahrungsergänzungsmittel, das viele Menschen dabei unterstützt, ihr Gewicht zu reduzieren und ihre Gesundheit zu verbessern. Die einzigartige Mischung aus natürlichen Inhaltsstoffen hilft, den Stoffwechsel anzukurbeln und den Appetit zu zügeln, was zu einer effektiven Gewichtsabnahme führt.
Die Kombination aus grünem Tee, Garcinia Cambogia, Ingwer und anderen sorgfältig ausgewählten Zutaten sorgt dafür, dass Reduslim Sklad den Körper auf sanfte Weise entgiftet und Fett verbrennt. Das Produkt ist sowohl für Männer als auch Frauen geeignet und kann ohne Risiko eingenommen werden, da es keine bekannten Nebenwirkungen hat.
Viele zufriedene Kunden schwärmen von den Ergebnissen, die sie mit Reduslim Sklad erzielt haben. Sie berichten von mehr Energie, einem verbesserten Wohlbefinden und einem insgesamt gesünderen Lebensstil. Wenn auch Sie von den positiven Effekten profitieren möchten, sollten Sie es unbedingt ausprobieren.
Bestellen Sie noch heute Ihr Reduslim Sklad und starten Sie Ihre Reise zu einem fitteren und gesünderen Ich. Mit der richtigen Kombination aus Ernährung, Bewegung und dem regelmäßigen Konsum dieses Nahrungsergänzungsmittels werden Sie schon bald die gewünschten Ergebnisse sehen. Reduslim Sklad ist der Schlüssel zu Ihrem Erfolg!
https://reduslim.at/
Специальные промокоды на 2024 год для 1xBet. Промокод — это уникальный набор из букв, цифр и символов для того, чтобы пользователь получил определенный бонус. Таким бонусом может оказаться увеличение начального депозита, ставка со страховкой (с возвратом части ставочных денег при выборе неверного исхода матча), тестовая ставка (чтобы новые игроки набрались опыта, без вреда собственным деньгам) и многое другое. Больше промокодов для 1xBet можно увидеть на сайтах партнеров букмекерской компании, которые выкладываются каждый день на просторах интернета. Бесплатные промокоды 1xBet при регистрации. Многие пользователи положительно отзываются о промокоде 1xBet на сегодня. Им можно воспользоваться при регистрации новой учетной записи на сайте компании. Для этого необходимо ввести в соответствующее окошко следующий набор букв и цифр. Эта комбинация будут эффективной до конца текущего года, но она распространяется только на новых игроков – более подробно в этом материале https://yarn55.ru/news/pgs/?promokod_283.html
выездной бар коктейли
No, like won’t happen, because when you open electrum, you never refer to online service https://bither-wallet.io/. all that to you need to do so is to move your coins to a other wallet.
sinequan 10mg online
обнал карт купить
Умение осмысливать сущности и опасностей ассоциированных с легализацией кредитных карт может помочь людям избегать подобных атак и обеспечивать защиту свои финансовые состояния. Обнал (отмывание) кредитных карт — это процесс использования украденных или неправомерно приобретенных кредитных карт для осуществления финансовых транзакций с целью замаскировать их происхождение и заблокировать отслеживание.
Вот некоторые из способов, которые могут способствовать в предотвращении обнала кредитных карт:
Защита личной информации: Будьте осторожными в связи предоставления персональной информации, особенно онлайн. Избегайте предоставления номеров карт, кодов безопасности и других конфиденциальных данных на непроверенных сайтах.
Надежные пароли: Используйте мощные и уникальные пароли для своих банковских аккаунтов и кредитных карт. Регулярно изменяйте пароли.
Контроль транзакций: Регулярно проверяйте выписки по кредитным картам и банковским счетам. Это позволит своевременно обнаруживать подозрительных транзакций.
Антивирусная защита: Используйте антивирусное программное обеспечение и вносите обновления его регулярно. Это поможет защитить от вредоносные программы, которые могут быть использованы для кражи данных.
Осторожное взаимодействие в социальных сетях: Будьте осторожными в сетевых платформах, избегайте опубликования чувствительной информации, которая может быть использована для взлома вашего аккаунта.
Быстрое сообщение банку: Если вы заметили какие-либо подозрительные операции или утерю карты, сразу свяжитесь с вашим банком для отключения карты.
Обучение: Будьте внимательными к современным приемам мошенничества и обучайтесь тому, как противостоять их.
Избегая легковерия и проявляя предельную осторожность, вы можете минимизировать риск стать жертвой обнала кредитных карт.
обнал карт купить
Незаконные платформы, где предлагают обнал пластиковых карт, представляют собой онлайн-платформы, ориентированные на обсуждении и осуществлении неправомерных операций с банковскими пластиком. На таких форумах пользователи делают обмен данными, методами и опытом в области кэш-аута, что влечет за собой противозаконные действия по получению доступа к денежным ресурсам.
Эти платформы могут предоставлять разнообразные сервисы, относящиеся с мошенничеством, такие как фишинг, считывание, вредоносное программное обеспечение и прочие методы для получения данных с финансовых карт. Также рассматриваются вопросы, связанные с применением украденных данных для совершения транзакций или снятия средств.
Пользователи незаконных платформ по обналичиванию карт могут оставаться неизвестными и уходить от привлечения органов безопасности. Участники могут обмениваться рекомендациями, предлагать сервисы, относящиеся к обналичиванием, а также проводить сделки, целенаправленные на незаконную финансовую деятельность.
Необходимо подчеркнуть, что участие в таких деятельностях не только является нарушение законов, но и может приводить к юридическим последствиям и уголовной ответственности.
Обналичивание карт – это противозаконная деятельность, становящаяся все более популярной в нашем современном мире электронных платежей. Этот вид мошенничества представляет серьезные вызовы для банков, правоохранительных органов и общества в целом. В данной статье мы рассмотрим частоту встречаемости обналичивания карт, используемые методы и возможные последствия для жертв и общества.
Частота обналичивания карт:
Обналичивание карт является довольно распространенным явлением, и его частота постоянно растет с увеличением числа электронных транзакций. Киберпреступники применяют разнообразные методы для получения доступа к финансовым средствам, включая фишинг, вредоносное программное обеспечение, скимминг и другие инновационные подходы.
Методы обналичивания карт:
Фишинг: Злоумышленники могут отправлять фальшивые электронные сообщения или создавать веб-сайты, имитирующие банковские системы, с целью получения личной информации от владельцев карт.
Скимминг: Злоумышленники устанавливают устройства скиммеры на банкоматах или терминалах для считывания данных с магнитных полос карт.
Вредоносное программное обеспечение: Киберпреступники разрабатывают вредоносные программы, которые заражают компьютеры и мобильные устройства, чтобы получить доступ к личным данным и банковским счетам.
Сетевые атаки: Атаки на системы банков и платежных платформ могут привести к утечке информации о картах и, следовательно, к их обналичиванию.
Последствия обналичивания карт:
Финансовые потери для клиентов: Владельцы карт могут столкнуться с денежными потерями, так как средства могут быть списаны с их счетов без их ведома.
Угроза безопасности данных: Обналичивание карт подчеркивает угрозу безопасности личных данных, что может привести к краже личной и финансовой информации.
Ущерб репутации банков: Банки и другие финансовые учреждения могут столкнуться с утратой доверия со стороны клиентов, если их системы безопасности оказываются уязвимыми.
Проблемы для экономики: Обналичивание карт создает экономический ущерб, поскольку оно стимулирует дополнительные затраты на борьбу с мошенничеством и восстановление утраченных средств.
Борьба с обналичиванием карт:
Совершенствование технологий безопасности: Банки и финансовые институты постоянно совершенствуют свои системы безопасности, чтобы предотвратить несанкционированный доступ к картам.
Образование и информирование: Обучение клиентов о методах мошенничества и том, как защитить свои данные, является важным шагом в борьбе с обналичиванием карт.
Сотрудничество с правоохранительными органами: Банки активно сотрудничают с правоохранительными органами для выявления и пресечения преступных схем.
Заключение:
Обналичивание карт – значительная угроза для финансовой стабильности и безопасности личных данных. Решение этой проблемы требует совместных усилий со стороны банков, правоохранительных органов и общества в целом. Только эффективная борьба с мошенничеством позволит обеспечить безопасность электронных платежей и защитить интересы всех участников финансовой системы.
обнал карт купить
Покупка фальшивых денег считается незаконным или опасным поступком, что может послать в тяжелым юридическим санкциям иначе ущербу вашей денежной стабильности. Вот некоторые примет, почему приобретение фальшивых купюр является рискованной и недопустимой:
Нарушение законов:
Покупка иначе воспользование поддельных банкнот приравниваются к нарушением закона, нарушающим правила территории. Вас могут подвергнуться наказанию, что потенциально повлечь за собой аресту, денежным наказаниям и лишению свободы.
Ущерб доверию:
Фальшивые деньги нарушают доверие по отношению к денежной механизму. Их использование создает возможность для порядочных личностей и коммерческих структур, которые имеют возможность попасть в внезапными перебоями.
Экономический ущерб:
Разнос лживых банкнот осуществляет воздействие на экономическую сферу, инициируя рост цен что ухудшает общую финансовую устойчивость. Это имеет возможность повлечь за собой потере уважения к денежной системе.
Риск обмана:
Лица, те, занимается изготовлением поддельных банкнот, не обязаны сохранять какие-то уровни качества. Поддельные банкноты могут стать легко распознаны, что в итоге послать в ущербу для тех собирается использовать их.
Юридические последствия:
При событии попадания под арест за использование поддельных денег, вас способны принудительно обложить штрафами, и вы столкнетесь с юридическими проблемами. Это может оказать воздействие на вашем будущем, с учетом возможные проблемы с получением работы и кредитной историей.
Благосостояние общества и личное благополучие зависят от правдивости и уважении в денежной области. Получение поддельных купюр нарушает эти принципы и может порождать важные последствия. Предлагается соблюдать норм и вести только легальными финансовыми транзакциями.
Villas for Sale in the Emaar Farm Gardens II. The developer offers comfortable real estate at competitive prices.
Protection of minors, protection from manipulation with bets and the prevention of gambling addiction were paramount features of the csr bwin philosophy.
Here is my website – https://bwintr3.top/
Gana dinero real con el bono casino sin deposito
bono gratis para casino sin deposito casino en linea con bono de bienvenida sin deposito .
Здравствуйте! Исходя из моего опыта, могу рассказать, что исследовал уже бесчисленное множество видеослотов и игровых аппаратов в различных онлайн-казино! Наиболее мне импонирует pin-up casino вход в личный кабинет. Большое количество видеослотов доступны бесплатно, что значительно помогает расслабиться. Для тех, кто готов к рискам, предоставляется возможность сделать ставки на деньги!
Скажите, пожалуйста, можете ли Вы изготовить хомутовый нагреватель со следующими параметрами: диаметр 70мм, длина 100мм, 1,6кВт/220В, температура 400 градусов https://rusupakten.ru/product/ten-f10-0/
dota2answers.com
“내각에 오기 전에 헌장을 준비하라고 하지 않았습니까?”
differin 25mg
In January 2011, bwin launched a special poker version on iphone, which allows you to play correctly online poker for real funds. bwin is a sponsor of the Portuguese League Cup.
aviator: aviator bet malawi login – aviator
aviator betting game: aviator – aviator game
Выкуп квартиры в кратчайшие сроки. Быстрая оценка стоимости и помощь в подготовке документов. Помощь с переездом.
помощь в продаже квартиры в ипотеке
То есть, виртуальный номер нужен для обеспечения приватности, безопасности и свободной работы с десятками и сотнями сайтов одновременно аренда виртуального номера
То есть, виртуальный номер нужен для обеспечения приватности, безопасности и свободной работы с десятками и сотнями сайтов одновременно virtueel telefoonnummer voor altijd
https://vavada14.life/
napsauta lukeaksesi
There are over 400 Internet casino games available to gamers, including Baccarat, blackjack, roulette, Shikbo and mass 1win indirothers.
смотреть
фильм
фильм онлайн
фильм
видеостена под ключ https://videosteny11.ru/ .
Лучший беттинговый сайт 1win
Рекомендую каждому этот оригинальный сайт 1win
Лучшее казино и настоящий сайт 1win
горка бокалов
aviator online: aviator – aviator mz
глаз бога сайт
bistroduet.com
“가서 참외를 따고 고구마를 계획하면 다 먹었는지 누가 알겠어?”
PЕЇjДЌka 18000 KДЌ
zithromax purchase online: zithromax price generic zithromax azithromycin
zithromax 500mg over the counter – https://azithromycin.pro/zithromax-for-tooth-infection.html buy zithromax
actos 2mg
Prestito di 8500 euro
Presents the new residential complex of The Sapphire with favourable terms of purchase and return on investment.
фильм смотреть
смотреть
just outline your information, including phone and address, 1xbet indir and wait for confirmation by email.
фильм смотреть онлайн
Ngamenjitu
Ngamenjitu: Portal Togel Online Terluas dan Terjamin
Portal Judi telah menjadi salah satu portal judi online terluas dan terjamin di Indonesia. Dengan bervariasi market yang disediakan dari Semar Group, Ngamenjitu menawarkan pengalaman bermain togel yang tak tertandingi kepada para penggemar judi daring.
Market Terunggul dan Terlengkap
Dengan total 56 pasaran, Portal Judi menampilkan beberapa opsi terbaik dari pasaran togel di seluruh dunia. Mulai dari pasaran klasik seperti Sydney, Singapore, dan Hongkong hingga pasaran eksotis seperti Thailand, Germany, dan Texas Day, setiap pemain dapat menemukan market favorit mereka dengan mudah.
Metode Bermain yang Praktis
Portal Judi menyediakan panduan cara main yang mudah dipahami bagi para pemula maupun penggemar togel berpengalaman. Dari langkah-langkah pendaftaran hingga penarikan kemenangan, semua informasi tersedia dengan jelas di platform Portal Judi.
Ringkasan Terkini dan Info Terkini
Pemain dapat mengakses hasil terakhir dari setiap pasaran secara real-time di Situs Judi. Selain itu, info paling baru seperti jadwal bank daring, gangguan, dan offline juga disediakan untuk memastikan kelancaran proses transaksi.
Bermacam-macam Macam Permainan
Selain togel, Portal Judi juga menawarkan bervariasi jenis permainan kasino dan judi lainnya. Dari bingo hingga roulette, dari dragon tiger hingga baccarat, setiap pemain dapat menikmati berbagai pilihan permainan yang menarik dan menghibur.
Keamanan dan Kenyamanan Pelanggan Dijamin
Situs Judi mengutamakan keamanan dan kenyamanan pelanggan. Dengan sistem keamanan terbaru dan layanan pelanggan yang responsif, setiap pemain dapat bermain dengan nyaman dan tenang di platform ini.
Promosi-Promosi dan Hadiah Istimewa
Ngamenjitu juga menawarkan berbagai promosi dan hadiah istimewa bagi para pemain setia maupun yang baru bergabung. Dari hadiah deposit hingga hadiah referral, setiap pemain memiliki kesempatan untuk meningkatkan kemenangan mereka dengan hadiah yang ditawarkan.
Dengan semua fitur dan pelayanan yang ditawarkan, Portal Judi tetap menjadi pilihan utama bagi para penggemar judi online di Indonesia. Bergabunglah sekarang dan nikmati pengalaman bermain yang seru dan menguntungkan di Portal Judi!
металлических конструкций http://www.ingibitor-korrozii-msk.ru .
смотреть фильм
Лучший беттинговый сайт только 1win
защита стали от коррозии ingibitor-korrozii-msk.ru .
https://1win-cas.life/
детские коляски купить москва http://www.detskie-koljaski-msk.ru/ .
защита стали от коррозии http://www.ingibitor-korrozii-msk.ru .
Покупайте вилочные погрузчики в каталоге можете выбрать и купить электропогрузчики и автопогрузчики (бензиновые или дизельные) с различными параметрами и характеристиками https://shantui.kg/
symbicort coupon
защита оборудования от коррозии https://www.ingibitor-korrozii-msk.ru .
zithromax 600 mg tablets: buy zithromax no prescription can you buy zithromax online
Mагазин фальшивых денег купить
Покупка поддельных денег считается незаконным иначе опасительным актом, которое имеет возможность повлечь за собой серьезным юридическими воздействиям или постраданию личной финансовой стабильности. Вот некоторые другие причин, почему закупка контрафактных купюр является опасной либо недопустимой:
Нарушение законов:
Покупка и воспользование контрафактных банкнот считаются правонарушением, подрывающим нормы общества. Вас могут подвергнуться уголовной ответственности, что потенциально привести к лишению свободы, штрафам иначе лишению свободы.
Ущерб доверию:
Поддельные купюры ослабляют доверенность в денежной механизму. Их использование порождает возможность для честных людей и предприятий, которые в состоянии попасть в неожиданными убытками.
Экономический ущерб:
Расширение поддельных купюр причиняет воздействие на финансовую систему, инициируя денежное расширение и подрывая глобальную денежную устойчивость. Это может повлечь за собой утрате уважения к денежной системе.
Риск обмана:
Личности, какие, осуществляют изготовлением контрафактных банкнот, не обязаны поддерживать какие-либо уровни характеристики. Фальшивые банкноты могут стать легко обнаружены, что в конечном счете повлечь за собой ущербу для тех, кто пытается воспользоваться ими.
Юридические последствия:
В ситуации захвата при применении фальшивых купюр, вас имеют возможность наказать штрафом, и вы столкнетесь с законными сложностями. Это может отразиться на вашем будущем, в том числе проблемы с трудоустройством с кредитной историей.
Благосостояние общества и личное благополучие основываются на правдивости и уважении в финансовой деятельности. Получение поддельных купюр идет вразрез с этими принципами и может порождать важные последствия. Предлагается соблюдать норм и вести только законными финансовыми сделками.
Где купить фальшивые деньги
Покупка поддельных купюр является противозаконным иначе рискованным действием, которое имеет возможность послать в глубоким законным санкциям и ущербу своей финансовой устойчивости. Вот несколько других последствий, вследствие чего получение лживых банкнот приравнивается к опасной или недопустимой:
Нарушение законов:
Закупка или применение фальшивых денег представляют собой нарушением закона, нарушающим положения территории. Вас способны подвергнуть уголовной ответственности, что потенциально послать в задержанию, денежным наказаниям либо приводу в тюрьму.
Ущерб доверию:
Фальшивые купюры нарушают доверенность к финансовой структуре. Их использование возникает опасность для порядочных граждан и бизнесов, которые в состоянии попасть в внезапными расходами.
Экономический ущерб:
Распространение поддельных купюр оказывает воздействие на финансовую систему, вызывая рост цен что ухудшает всеобщую финансовую стабильность. Это в состоянии послать в потере доверия к валютной единице.
Риск обмана:
Люди, те, задействованы в производством поддельных банкнот, не обязаны сохранять какие-то параметры уровня. Лживые деньги могут оказаться легко распознаваемы, что в итоге закончится ущербу для тех, кто пытается использовать их.
Юридические последствия:
В случае задержания при воспользовании поддельных денег, вас способны принудительно обложить штрафами, и вы столкнетесь с юридическими трудностями. Это может повлиять на вашем будущем, включая сложности с трудоустройством и кредитной историей.
Общественное и индивидуальное благосостояние основываются на честности и доверии в финансовой деятельности. Покупка фальшивых банкнот идет вразрез с этими принципами и может иметь серьезные последствия. Рекомендуем держаться норм и заниматься только законными финансовыми сделками.
buy azithromycin zithromax – https://azithromycin.pro/zithromax-tri-pak.html zithromax 500 mg for sale
септика под ключ
магазин коляски http://www.detskie-koljaski-msk.ru/ .
The addition of skins and the associated virtual economy allowed increase number states in global offensive if compared with their own games of the counter-strike series and remains one of the most important updates in the history of the.
Have a look at my blog post https://maxcheaters.com/topic/225918-mygamingloungecomcsgo999instant-deliverpaypalg2apay/
Aporno online
Покупка лживых купюр приравнивается к незаконным либо рискованным актом, что имеет возможность закончиться глубоким юридическими последствиям или вреду своей финансовой устойчивости. Вот несколько других причин, почему покупка поддельных денег представляет собой рискованной и неуместной:
Нарушение законов:
Получение либо применение лживых денег являются противоправным деянием, противоречащим законы территории. Вас имеют возможность подвергнуться судебному преследованию, что потенциально закончиться лишению свободы, взысканиям иначе тюремному заключению.
Ущерб доверию:
Поддельные купюры ослабляют доверие в финансовой системе. Их поступление в оборот порождает риск для надежных гражданских лиц и бизнесов, которые в состоянии завязать неожиданными убытками.
Экономический ущерб:
Распространение поддельных банкнот влияет на экономическую сферу, приводя к распределение денег что ухудшает общую финансовую равновесие. Это способно закончиться потере уважения к денежной системе.
Риск обмана:
Люди, те, задействованы в изготовлением фальшивых купюр, не обязаны поддерживать какие-то стандарты характеристики. Лживые бумажные деньги могут быть легко распознаваемы, что в итоге закончится ущербу для тех попытается воспользоваться ими.
Юридические последствия:
При случае лишения свободы при применении поддельных денег, вас могут взыскать штраф, и вы столкнетесь с юридическими трудностями. Это может повлиять на вашем будущем, с учетом возможные проблемы с трудоустройством с кредитной историей.
Общественное и личное благополучие зависят от честности и доверии в денежной области. Закупка поддельных купюр не соответствует этим принципам и может иметь важные последствия. Предлагается держаться законов и вести только правомерными финансовыми сделками.
Покупка лживых купюр считается неправомерным иначе потенциально опасным действием, которое в состоянии закончиться серьезным юридическими последствиям или вреду личной финансовой надежности. Вот некоторые другие последствий, вследствие чего получение поддельных купюр представляет собой рискованной иначе недопустимой:
Нарушение законов:
Получение иначе воспользование поддельных купюр являются преступлением, нарушающим нормы территории. Вас способны поддать наказанию, что может послать в аресту, штрафам либо постановлению под стражу.
Ущерб доверию:
Поддельные деньги ухудшают доверие к финансовой организации. Их применение формирует риск для надежных людей и коммерческих структур, которые имеют возможность попасть в неожиданными расходами.
Экономический ущерб:
Расширение фальшивых денег причиняет воздействие на экономику, приводя к распределение денег что ухудшает глобальную денежную равновесие. Это может повлечь за собой потере уважения к денежной единице.
Риск обмана:
Личности, которые, вовлечены в изготовлением лживых банкнот, не обязаны поддерживать какие-нибудь нормы характеристики. Лживые купюры могут оказаться легко обнаружены, что в итоге закончится потерям для тех, кто пытается использовать их.
Юридические последствия:
При событии попадания под арест за использование лживых банкнот, вас в состоянии наказать штрафом, и вы столкнетесь с законными сложностями. Это может повлиять на вашем будущем, с учетом проблемы с трудоустройством и историей кредита.
Благосостояние общества и личное благополучие зависят от правдивости и уважении в финансовой деятельности. Получение поддельных денег нарушает эти принципы и может порождать серьезные последствия. Советуем придерживаться законов и заниматься только правомерными финансовыми сделками.
большой выбор детских колясок detskie-koljaski-msk.ru .
Купить фальшивые рубли
Покупка фальшивых купюр приравнивается к недозволенным и рискованным поступком, которое в состоянии повлечь за собой серьезным юридическими наказаниям или вреду своей денежной благосостояния. Вот некоторые другие причин, по какой причине получение лживых купюр приравнивается к потенциально опасной или недопустимой:
Нарушение законов:
Покупка или эксплуатация контрафактных купюр представляют собой преступлением, противоречащим правила страны. Вас способны подвергнуться судебному преследованию, что потенциально послать в лишению свободы, взысканиям иначе приводу в тюрьму.
Ущерб доверию:
Лживые купюры нарушают доверенность по отношению к денежной механизму. Их применение возникает возможность для надежных гражданских лиц и организаций, которые в состоянии претерпеть непредвиденными убытками.
Экономический ущерб:
Распространение поддельных банкнот влияет на экономику, провоцируя рост цен и ухудшая глобальную финансовую стабильность. Это в состоянии закончиться потере доверия к денежной единице.
Риск обмана:
Личности, те, осуществляют изготовлением фальшивых банкнот, не обязаны сохранять какие угодно параметры степени. Поддельные бумажные деньги могут оказаться легко распознаны, что в итоге повлечь за собой ущербу для тех, кто попытается использовать их.
Юридические последствия:
В ситуации задержания при воспользовании фальшивых банкнот, вас могут оштрафовать, и вы столкнетесь с юридическими проблемами. Это может повлиять на вашем будущем, включая возможные проблемы с получением работы и кредитной историей.
Общественное и индивидуальное благосостояние зависят от честности и доверии в финансовой сфере. Закупка контрафактных денег идет вразрез с этими принципами и может порождать серьезные последствия. Рекомендуется придерживаться законов и заниматься исключительно легальными финансовыми сделками.
холодное остекление фасада цена https://fasadnoe-osteklenie11.ru .
porn videos
для детей коляски https://detskie-koljaski-msk.ru/ .
acticin 300mg
обработки металла http://www.ingibitor-korrozii-msk.ru .
фильм онлайн
PЕЇjДЌka 20000 KДЌ
фильм бесплатно
фильм
глаз бога бот
фильм бесплатно
where can i buy zithromax capsules: zithromax over the counter substitute zithromax for sale usa
фильм
how to buy zithromax online: generic name for zithromax buy zithromax without prescription online
именно такое бюро сертификации выдает документы, которые подтверждают, что товар является
безопасным и для пользователей, ISO 9001 и для.
my web page; сертификация iso 9001
Рекомендую каждому настоящий сайт 1win
Лучшее казино находится тут 1win
Лучший беттинговый сайт можно найти только тут 1win
Настоящий сайт 1вин найти можно здесь 1win. Рекомендую!
https://cleaning24moscow.ru/
купить авто корее https://avtodom63.ru/
procedure evaluation of the SMS code allows the client to authenticate the user. as a rule this is how https://members4.boardhost.com/onewitch/msg/1710226830.html works.
купить аттестат
купить свидетельство о браке
купить диплом в москве
купить аттестат за 11 класс
купить диплом
купить диплом ссср
купить диплом техникума
рейтинг септиков для загородного дома
Porn video online
Real estate in the brand-new project of Dubai islands villas. Developer offers gorgeous villas at attractive prices.
Hi! Would you mind if I share your blog with my facebook group?
There’s a llot of people that I thinbk would really enjoy your content.
Please let me know. Thank you
Here is my website: 카지노사이트
купить диплом о среднем образовании
купить диплом о высшем образовании
купить детская коляска http://www.detskie-koljaski-msk.ru .
где купить диплом
indian pharmacies safe: cheapest online pharmacy – top 10 pharmacies in india indianpharm.store
Porn online
оснащение переговорных комнат https://oborudovanie-peregovornyh-komnat11.ru/ .
medication from mexico pharmacy: Mexico pharmacy price list – mexico drug stores pharmacies mexicanpharm.shop
Лучшее казино и БК находятся в 1win
Рекомендую лучший беттинговый сайт 1win
Настоящий сайт 1вин находится здесь 1win. Рекомендую!
если требуется отказное письмо на продукцию тс необходимо подготовить
комплект необходимых справок в
зависимости от требованиями тех.
Feel free to visit my homepage: как получить сертификат соответствия ISO 9001-2015
также вы получите возможность отправить нам на е-мэйл или в онлайн-чат в правом нижнем центр сертификации продукции углу сайта.
Also visit my website … https://www.rospromtest.ru/content.php?id=312
https://cleaning24moscow.ru/
купить автомобиль из кореи https://avtodom63.ru/
смотреть фильм
фильм 2024
фильм онлайн
canadian pharmacy prices: CIPA approved pharmacies – canadian drug canadianpharm.store
lisinopril 750mg
Lainaa 20000 euroa
фильм
Within this platform’s ecosystem, one can use MMTR to access new Memeinator merchandise corresponding to MemeScanner and the Memeinator game.
mexican border pharmacies shipping to usa: order online from a Mexican pharmacy – mexico pharmacy mexicanpharm.shop
купить фальшивые деньги
Покупка поддельных банкнот является противозаконным или рискованным действием, что способно закончиться важным правовым наказаниям или постраданию личной денежной стабильности. Вот некоторые примет, из-за чего получение фальшивых денег считается рискованной иначе неприемлемой:
Нарушение законов:
Покупка или воспользование фальшивых купюр являются правонарушением, нарушающим положения общества. Вас способны подвергнуться наказанию, что может закончиться тюремному заключению, денежным наказаниям или тюремному заключению.
Ущерб доверию:
Фальшивые деньги подрывают доверие к денежной системе. Их обращение создает опасность для честных людей и коммерческих структур, которые имеют возможность попасть в неожиданными убытками.
Экономический ущерб:
Разнос контрафактных денег осуществляет воздействие на экономическую сферу, провоцируя денежное расширение что ухудшает общественную финансовую устойчивость. Это способно закончиться потере доверия в валютной единице.
Риск обмана:
Лица, те, занимается изготовлением поддельных банкнот, не обязаны поддерживать какие угодно нормы степени. Лживые деньги могут быть легко обнаружены, что, в конечном итоге повлечь за собой потерям для тех, кто пытается использовать их.
Юридические последствия:
При событии попадания под арест при использовании фальшивых банкнот, вас в состоянии наказать штрафом, и вы столкнетесь с юридическими трудностями. Это может оказать воздействие на вашем будущем, в том числе проблемы с поиском работы и историей кредита.
Общественное и индивидуальное благосостояние зависят от правдивости и уважении в финансовой сфере. Приобретение лживых купюр идет вразрез с этими принципами и может обладать серьезные последствия. Предлагается придерживаться законов и заниматься только законными финансовыми транзакциями.
Опасности фальшивых 5000 рублей: Распространение фальшивых купюр и его последствия
В сегодняшнем обществе, где виртуальные платежи становятся все более широко используемыми, правонарушители не оставляют без внимания и обычные методы мошенничества, такие как раскрутка контрафактных банкнот. В последние дни стало известно о неправомерной торговле контрафактных 5000 рублевых купюр, что представляет весомую опасность для финансовой инфраструктуры и населения в итоге.
Методы сбыта:
Нарушители активно используют закрытые трассы интернета для торговли фальшивых 5000 рублей. На подпольных веб-ресурсах и незаконных форумах можно обнаружить прошения недостоверных банкнот. К неудаче, это создает выгодные условия для раскрутки поддельных денег среди населения.
Последствия для сообщества:
Наличие контрафактных денег в потоке может иметь важные результаты для хозяйства и доверия к государственной валюте. Люди, не подозревая, что получили недостоверные купюры, могут использовать их в разнообразных ситуациях, что в итоге приводит к повреждению кредитоспособности к банкнотам определенного номинала.
Опасности для людей:
Люди становятся потенциальными пострадавшими мошенников, когда они ненамеренно получают недостоверные деньги в транзакциях или при приобретениях. В следствие, они могут столкнуться с неприятными ситуациями, такими как отказ торговых посредников принять поддельные купюры или даже вероятность юридической ответственности за труд расплаты поддельными деньгами.
Противостояние с дистрибуцией недостоверных денег:
В пользу защиты общества от аналогичных нарушений необходимо усилить противодействие по выяснению и остановке изготовления поддельных денег. Это включает в себя сотрудничество между правоохранительными структурами и финансовыми учреждениями, а также расширение градуса просвещения населения относительно символов фальшивых банкнот и техник их выявления.
Заключение:
Диффузия фальшивых 5000 рублей – это весомая опасность для финансового благополучия и надежности граждан. Сохранение авторитета к денежной единице требует согласованных действий со стороны государства, банков и каждого человека. Важно быть осторожным и осведомленным, чтобы предотвратить раскрутку недостоверных денег и обеспечить финансовые интересы населения.
Покупка контрафактных банкнот считается незаконным или опасным действием, которое в состоянии повлечь за собой тяжелым правовым санкциям или ущербу индивидуальной финансовой надежности. Вот некоторые другие последствий, по какой причине покупка лживых купюр считается рискованной или неприемлемой:
Нарушение законов:
Закупка либо воспользование контрафактных денег представляют собой преступлением, подрывающим нормы страны. Вас имеют возможность подвергнуться юридическим последствиям, которое может закончиться аресту, денежным наказаниям или приводу в тюрьму.
Ущерб доверию:
Контрафактные банкноты подрывают доверенность по отношению к денежной организации. Их обращение порождает опасность для надежных граждан и предприятий, которые могут столкнуться с внезапными убытками.
Экономический ущерб:
Распространение лживых банкнот осуществляет воздействие на экономику, провоцируя рост цен и подрывая общественную экономическую стабильность. Это способно повлечь за собой потере доверия к денежной системе.
Риск обмана:
Личности, те, вовлечены в изготовлением лживых денег, не обязаны соблюдать какие угодно уровни качества. Поддельные деньги могут выйти легко распознаны, что, в конечном итоге повлечь за собой убыткам для тех собирается воспользоваться ими.
Юридические последствия:
В ситуации задержания при использовании контрафактных банкнот, вас способны оштрафовать, и вы столкнетесь с юридическими проблемами. Это может отразиться на вашем будущем, в том числе проблемы с получением работы и историей кредита.
Общественное и индивидуальное благосостояние зависят от правдивости и доверии в финансовых отношениях. Получение лживых банкнот нарушает эти принципы и может обладать важные последствия. Рекомендуем придерживаться законов и осуществлять только легальными финансовыми транзакциями.
Рекомендую каждому букмекерскую контору 1win
https://moskva-cleaning.ru/
archive Porn
siehe diese Website
Payday loans Wyoming
клининговые услуги цена за м2
http://indianpharm24.shop/# world pharmacy india indianpharm.store
магазин фальшивых денег купить
Покупка контрафактных купюр приравнивается к недозволенным иначе опасительным делом, что способно послать в глубоким правовым последствиям и повреждению своей денежной устойчивости. Вот некоторые другие причин, почему получение поддельных банкнот считается опасной и неуместной:
Нарушение законов:
Получение или применение поддельных купюр являются правонарушением, нарушающим нормы территории. Вас могут подвергнуть юридическим последствиям, что потенциально повлечь за собой аресту, финансовым санкциям и лишению свободы.
Ущерб доверию:
Лживые деньги нарушают доверенность к денежной механизму. Их обращение формирует опасность для честных гражданских лиц и предприятий, которые способны столкнуться с неожиданными потерями.
Экономический ущерб:
Разнос контрафактных банкнот причиняет воздействие на экономическую сферу, приводя к инфляцию что ухудшает общую экономическую стабильность. Это может повлечь за собой потере уважения к национальной валюте.
Риск обмана:
Лица, которые, вовлечены в изготовлением поддельных купюр, не обязаны соблюдать какие-нибудь стандарты уровня. Контрафактные бумажные деньги могут выйти легко обнаружены, что, в итоге повлечь за собой ущербу для тех собирается их использовать.
Юридические последствия:
При событии лишения свободы при применении лживых купюр, вас в состоянии принудительно обложить штрафами, и вы столкнетесь с юридическими проблемами. Это может отразиться на вашем будущем, включая проблемы с получением работы и историей кредита.
Общественное и индивидуальное благосостояние зависят от правдивости и уважении в финансовой деятельности. Покупка контрафактных денег нарушает эти принципы и может представлять важные последствия. Рекомендуем держаться законов и заниматься исключительно законными финансовыми действиями.
https://canadianpharmlk.shop/# canadian pharmacy online canadianpharm.store
фильм в хорошем качестве
Официальный сайт в Тор браузере, лучший выбор для тех, кто ищет безопасный и анонимный доступ на Мега даркнет. Рабочая ссылка на Мега Даркнет на нашем сайте mega вещества
фильм смотреть онлайн
https://calculatortiktok.com/
Отзывы о компаниях играют гигантскую роль в современном мире бизнеса. Они не только могут помочь потребителям брать на себя обоснованные заключения, но и оказывают большое влияние на репутацию компаний и их фуррор на рынке. В данном тексте мы рассмотрим, отчего оставлять отзывы о компаниях так принципиально и какие достоинства такое может принести.
1. Помощь другим покупателям
Когда вы оставляете отзыв о компании, вы проделываете доброе дело, помогая иным потребителям. Ваши собственные опыт и эмоции имеют все шансы быть полезными тем, кто лишь только собирается пользоваться услугами этой фирмы. Ваши комментарии имеют все шансы посодействовать им принять обоснованное заключение.
2. Воздействие https://promca.net.ru/ на качество обслуживания
Фирмы пристально смотрят за отзывами своих посетителей. Ваш отзыв имеет возможность стать мотивацией для фирмы сделать лучше качество своих предложений либо продуктов. Когда фирмы видят, собственно что посетители довольны их работой, это может стать катализатором для поддержания высочайшего эталона обслуживания.
3. Построение доверия
Отзывы о фирмы могут помочь в построении доверия со стороны покупателей. Когда люди видят положительные отзывы, они склонны больше доверять компании и рассматривать ее как надежного поставщика предложений или продуктов.
4. Вероятность высказать свое мнение
Оставление отзывов разрешает вам высказать свое суждение и разделиться своим навыком. Это может быть тем более принципиально, если вы столкнулись с проблемами или негативным опытом, который вы желаете поделиться, чтобы посодействовать иным избегнуть подобных обстановок.
5. Поощрение высококачественной работы
Когда компании видят, что их посетители оценивают их работу положительно, такое может замерзнуть дополнительным мотивом для фирмы поддерживать высокие стереотипы качества и уровня обслуживания.
6. Стимуляция конкуренции
Конкурентность между компаниями способствует улучшению свойства и инновациям. Отзывы о компаниях помогают выявить наилучшие игроки на рынке и стимулируют другие компании совершенствовать свои продукты и услуги.
7. Саморегулирование рынка
Отзывы о компаниях также имеют все шансы содействовать саморегулированию рынка. Когда компании знают, собственно что их действия станут подвергнуты обсуждению и оценке, они склонны идти по стопам законам и этическим эталонам.
8. Обязанность фирм
Отзывы о компаниях имеют все шансы выявить недостатки и трудности в работе фирм. Это может побудить фирмы к ответственным поступкам и улучшению хилых мест.
9. Участие в сообществе
Оставление отзывов – это способ принять участие в онлайн-сообществе и привнести свой вклад в социльное суждение. Ваш глас имеет велечину, и он может воздействовать на восприятие компании другими покупателями.
10. Возможность получить обратную связь
Оставляя отзыв о компании, вы также можете получить оборотную связь и ответы на свои вопросы. Почти все компании энергично взаимодействуют с посетителями через отзывы и готовы посодействовать решить всевозможные проблемы.
Итак, отзывы о компаниях – это не просто суждение клиентов, это значительный инструмент, который имеет возможность повлиять на качество обслуживания, репутацию компании и решения иных покупателей. Ваш отзыв содержит велечину, и ему предоставляется возможность посодействовать сделать наилучший опыт для всех.
Официальный сайт в Тор браузере, лучший выбор для тех, кто ищет безопасный и анонимный доступ на Мега даркнет. Рабочая ссылка на Мега Даркнет на нашем сайте мега онион
фильм онлайн
Во-первых, мы тут не для шуток, а дабы поднимать бабло. У нас эпичные задания по ютубу, отзывам и проголосовать тебе не составит труда. Пальцы в горячке шевели, и баксов на твоем счету все больше.
А во-2-хhttp://forum.lundin.ro/showthread.php?tid=193&pid=2114
, кто сказал, собственно что заработок не имеет возможности быть веселым? У нас царствует воздух, как на самом классном пикнике. Здесь в том числе и заработок делается частью приключения. Забудь скучные таски, у нас все по-нашему!
Ну и конечно, партнерство с нами – это, брат, как скидка в самом эксклюзивном клубе. Ты первый узнаешь о страстных промоакциях, самых радужных предложениях и получишь билет в мир анлимитного заработка. А мы тебе не просто обещаем, а гарантируем!
И откровенно, не знаю, как возможно протекать мимо такового кайфа. Ты собственно что, не хочешь стать настоящим уличным боссом? На нашем веб-сайте ты, брат, будешь как капитан собственного корабля, маневрируя в океане крутых задач. Твои средства, твои правила!
Не будь неудачником, чувак! Забудь про нудные хлопоты и войди в ряды тех, кто рубит бабло, не отрываясь от кайфа. Заходи на наш вебсайт, дерзай и зарабатывай, как настоящий уличный браток. Здесь твое время пришло, чувак!
Similar to a personal presale, this occasion features a restricted group with unmatched stature.
celecoxib
фильм
Рекомендую лучший беттинг сайт 1win
Лучшее казино и БК можете найти в 1win
Оригинальный сайт 1вин находится здесь 1win. Рекомендую!
https://mexicanpharm24.shop/# buying prescription drugs in mexico mexicanpharm.shop
https://mexicanpharm24.com/# mexican pharmacy mexicanpharm.shop
escrow pharmacy canada: Cheapest drug prices Canada – canada discount pharmacy canadianpharm.store
buy levofloxacin 250mg
купить диплом бакалавра http://www.saksx-diploms24.com .
conocer los hechos
обнал карт работа
Обналичивание карт – это противозаконная деятельность, становящаяся все более популярной в нашем современном мире электронных платежей. Этот вид мошенничества представляет тяжелые вызовы для банков, правоохранительных органов и общества в целом. В данной статье мы рассмотрим частоту встречаемости обналичивания карт, используемые методы и возможные последствия для жертв и общества.
Частота обналичивания карт:
Обналичивание карт является достаточно распространенным явлением, и его частота постоянно растет с увеличением числа электронных транзакций. Киберпреступники применяют разные методы для получения доступа к финансовым средствам, включая фишинг, вредоносное программное обеспечение, скимминг и другие инновационные подходы.
Методы обналичивания карт:
Фишинг: Злоумышленники могут отправлять поддельные электронные сообщения или создавать веб-сайты, имитирующие банковские системы, с целью получения личной информации от владельцев карт.
Скимминг: Злоумышленники устанавливают устройства скиммеры на банкоматах или терминалах для считывания данных с магнитных полос карт.
Вредоносное программное обеспечение: Киберпреступники разрабатывают вредоносные программы, которые заражают компьютеры и мобильные устройства, чтобы получить доступ к личным данным и банковским счетам.
Сетевые атаки: Атаки на системы банков и платежных платформ могут привести к утечке информации о картах и, следовательно, к их обналичиванию.
Последствия обналичивания карт:
Финансовые потери для клиентов: Владельцы карт могут столкнуться с финансовыми потерями, так как средства могут быть списаны с их счетов без их ведома.
Угроза безопасности данных: Обналичивание карт подчеркивает угрозу безопасности личных данных, что может привести к краже личной и финансовой информации.
Ущерб репутации банков: Банки и другие финансовые учреждения могут столкнуться с утратой доверия со стороны клиентов, если их системы безопасности оказываются уязвимыми.
Проблемы для экономики: Обналичивание карт создает экономический ущерб, поскольку оно стимулирует дополнительные затраты на борьбу с мошенничеством и восстановление утраченных средств.
Борьба с обналичиванием карт:
Совершенствование технологий безопасности: Банки и финансовые институты постоянно совершенствуют свои системы безопасности, чтобы предотвратить несанкционированный доступ к картам.
Образование и информирование: Обучение клиентов о методах мошенничества и том, как защитить свои данные, является важным шагом в борьбе с обналичиванием карт.
Сотрудничество с правоохранительными органами: Банки активно сотрудничают с правоохранительными органами для выявления и пресечения преступных схем.
Заключение:
Обналичивание карт – весомая угроза для финансовой стабильности и безопасности личных данных. Решение этой проблемы требует совместных усилий со стороны банков, правоохранительных органов и общества в целом. Только эффективная борьба с мошенничеством позволит обеспечить безопасность электронных платежей и защитить интересы всех участников финансовой системы.
Aporno
best rated canadian pharmacy: canadian pharmacy – my canadian pharmacy review canadianpharm.store
Больше информации об услуге дизайн-проект ванной комнаты. Если остались вопросы или есть желание заказать дизайн проект коттеджа, с радостью приглашаем на бесплатную консультацию в нашу студию дизайн проект будинку ціна
Хотите обновить интерьер быстро и легко? Пластиковые панели для стен – ваше решение!
Освежите интерьер и стиль в любое желище с помощью наших качественных панелей ПВХ. Очень простые в монтаже, они преобразят ваш дом за считанные часы, без необходимости привлекать строителей.
Наши панели ПВХ не только круто выглядят, но и обладают рядом достоинств:
– Устойчивость к воде и гигиеничность, идеальны для использования в ванных и кухнях.
– Прочность и долговечность, обеспечивающие долговременное эксплуатацию без потери качества.
– Широкий выбор дизайнов и цветов, позволяющий реализовать любые дизайнерские идеи и подобрать наилучший вариант для вашего интерьера.
Не теряйте времени и сил на длительные ремонтные работы – выберите поливинилхлорид панели – https://walls-decor.com.ua/pvh-paneli и преобразите свой дом моментально! Покупайте у нас и получите быструю доставку и отличное обслуживание.
https://canadianpharmlk.com/# canadian pharmacy ed medications canadianpharm.store
It can be turning into frequent for crypto projects to reward early buyers with passive revenue.
monoket 20mg
http://indianpharm24.shop/# indian pharmacy indianpharm.store
Mega – облачное хранилище файлов из Новой Зеландии. Стало известно благодаря своему основателю, бизнесмену Киму Доткому, владельцу известного файлообменника Megaupload мега tor
Mega – облачное хранилище файлов из Новой Зеландии. Стало известно благодаря своему основателю, бизнесмену Киму Доткому, владельцу известного файлообменника Megaupload мега магазин
Покупка лживых купюр является незаконным или потенциально опасным делом, что способно послать в тяжелым правовым наказаниям иначе постраданию индивидуальной финансовой стабильности. Вот несколько других приводов, из-за чего приобретение фальшивых денег приравнивается к опасительной либо неуместной:
Нарушение законов:
Получение иначе воспользование лживых банкнот являются противоправным деянием, нарушающим положения территории. Вас имеют возможность подвергнуть себя наказанию, что может повлечь за собой тюремному заключению, финансовым санкциям либо приводу в тюрьму.
Ущерб доверию:
Контрафактные деньги ослабляют доверенность к денежной организации. Их применение возникает риск для благоприятных гражданских лиц и бизнесов, которые в состоянии столкнуться с непредвиденными расходами.
Экономический ущерб:
Разнос контрафактных банкнот оказывает воздействие на финансовую систему, вызывая денежное расширение и подрывая глобальную финансовую равновесие. Это в состоянии послать в потере доверия в национальной валюте.
Риск обмана:
Личности, те, занимается производством лживых купюр, не обязаны поддерживать какие-то нормы уровня. Поддельные деньги могут выйти легко распознаваемы, что, в конечном итоге закончится ущербу для тех пытается использовать их.
Юридические последствия:
При событии попадания под арест за использование контрафактных купюр, вас могут наказать штрафом, и вы столкнетесь с юридическими трудностями. Это может сказаться на вашем будущем, включая сложности с трудоустройством и кредитной историей.
Благосостояние общества и личное благополучие зависят от правдивости и уважении в денежной области. Приобретение лживых купюр нарушает эти принципы и может представлять серьезные последствия. Рекомендуем держаться законов и заниматься исключительно законными финансовыми транзакциями.
buying prescription drugs in mexico online: mexican pharmacy – mexico drug stores pharmacies mexicanpharm.shop
Рекомендую каждому букмекерскую контору в России 1win
Reduslim ist ein beliebtes Produkt zur Gewichtsreduktion, das auf dem Markt herrscht. Aber was sagt die Stiftung Warentest Гјber die Bewertung von Reduslim? Die Verbraucherorganisation hat das Produkt genauer unter die Lupe genommen und ist zu interessanten Ergebnissen gekommen.
In ihrer Bewertung stellte die Stiftung Warentest fest, dass Reduslim ein effektives Mittel zur Gewichtsabnahme ist. Die Inhaltsstoffe sind gut verträglich und führen zu einer nachhaltigen Reduzierung des Körpergewichts. Darüber hinaus werden auch positive Effekte auf den Stoffwechsel und das allgemeine Wohlbefinden festgestellt.
Die Verbraucher zeigten sich ebenfalls zufrieden mit Reduslim. Viele berichten von einer erfolgreichen Gewichtsabnahme und einer Steigerung ihrer Energielevel. Auch die einfache Anwendung und die schnellen Ergebnisse wurden gelobt.
Insgesamt kann die Bewertung von Reduslim durch die Stiftung Warentest als positiv angesehen werden. Wer also nach einem effektiven Mittel zur Gewichtsreduktion sucht, sollte Reduslim eine Chance geben und die positiven Erfahrungen der Verbraucher und Experten berГјcksichtigen.
https://reduslim.at/
Möchten Sie Reduslim billig kaufen? Auf der Suche nach einem effektiven und erschwinglichen Weg, um Ihre Gewichtsabnahmeziele zu erreichen? Dann sind Sie hier genau richtig! Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das Ihnen helfen kann, überschüssige Pfunde loszuwerden und Ihre Traumfigur zu erreichen. Indem Sie Reduslim in Verbindung mit einer gesunden Ernährung und regelmäßiger Bewegung einnehmen, können Sie Ihre Gewichtsabnahmeziele schneller erreichen. Suchen Sie nicht weiter, denn hier finden Sie Reduslim zu einem erschwinglichen Preis. Machen Sie noch heute den ersten Schritt auf dem Weg zu einem gesünderen und glücklicheren Leben!
https://reduslim.at/
https://moskva-cleaning.ru/
Gibt es Reduslim bei der Apotheke? Diese Frage beschäftigt viele Menschen, die auf der Suche nach einem effektiven Mittel zur Gewichtsabnahme sind. Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das behauptet, den Stoffwechsel zu beschleunigen und Fettverbrennung zu fördern.
Leider ist Reduslim nicht in Apotheken erhältlich. Es kann jedoch online bestellt werden. Es wird empfohlen, Reduslim nur auf der offiziellen Website des Herstellers zu kaufen, um sicherzustellen, dass es sich um ein originales und sicheres Produkt handelt.
Bevor Sie Reduslim kaufen, ist es wichtig, sich darüber im Klaren zu sein, dass Nahrungsergänzungsmittel keine Wundermittel sind und eine gesunde Ernährung und ausreichend Bewegung nicht ersetzen können. Konsultieren Sie am besten Ihren Arzt, bevor Sie mit der Einnahme von Reduslim beginnen, um sicherzustellen, dass es für Sie sicher ist.
Insgesamt lässt sich sagen, dass Reduslim eine vielversprechende Option für diejenigen ist, die beim Abnehmen Unterstützung suchen. Wenn Sie also Interesse haben, bestellen Sie Reduslim am besten direkt beim Hersteller und kombinieren Sie es mit einem gesunden Lebensstil für beste Ergebnisse.
https://reduslim.at/
My brother recommended I might like this website. He was entirely right. This post truly made my day. You can not imagine just how much time I had spent for this information! Thanks!
Stop by my webpage – https://babushonamemes00863.tribunablog.com/5-simple-techniques-for-jethalal-babita-meme-35126666
Reduslim Ingredienti sind die SchlГјssel zur effektiven Gewichtsabnahme. Die natГјrlichen Zutaten in Reduslim spielen eine entscheidende Rolle bei der UnterstГјtzung des Stoffwechsels, der Fettverbrennung und der Reduzierung von HeiГџhungerattacken.
Zu den wichtigsten Reduslim Ingredienti gehören grüner Tee-Extrakt, Garcinia Cambogia, L-Carnitin und Chrompicolinat. Grüner Tee-Extrakt stimuliert den Stoffwechsel und fördert die Fettverbrennung. Garcinia Cambogia hilft, den Appetit zu reduzieren und die Fettaufnahme zu blockieren.
L-Carnitin ist ein Aminosäure, die die Fettverbrennung unterstützt und die Energieproduktion steigert. Chrompicolinat reguliert den Blutzuckerspiegel und reduziert Heißhungerattacken. Zusammen sorgen diese Reduslim Ingredienti für eine effektive und nachhaltige Gewichtsabnahme.
Wenn Sie nach einem natГјrlichen und sicheren Weg suchen, um Gewicht zu verlieren, sollten Sie sich Reduslim genauer ansehen. Mit seinen hochwirksamen Ingredienti kann es Ihnen helfen, Ihre Abnehmziele zu erreichen und ein gesГјnderes Leben zu fГјhren.
https://reduslim.at/
The project has launched extra bonuses to incentivize long-term staking.
canadian drugs online: Canada pharmacy – global pharmacy canada canadianpharm.store
https://ekspert-komforta.ru/
Reduslim ist ein beliebtes Produkt zur Gewichtsreduktion, das auf natürliche Weise und ohne Nebenwirkungen funktioniert. Der Preis für Reduslim kann je nach Anbieter variieren, aber es lohnt sich sicherlich, etwas mehr für die Qualität zu zahlen. Der Precio Reduslim ist definitiv gerechtfertigt, wenn man bedenkt, wie effektiv das Produkt ist. Es enthält nur natürliche Inhaltsstoffe, die den Stoffwechsel ankurbeln und das Hungergefühl reduzieren. Mit Reduslim kann man schnell und gesund abnehmen, ohne sich dabei schlecht zu fühlen. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Ergebnissen!
https://reduslim.at/
Reduslim Parere Medico: Schlankheitspillen oder leere Versprechen?
Reduslim Parere Medico sind Schlankheitspillen, die angeblich beim Abnehmen helfen sollen. Aber was sagen Ärzte dazu? Viele Mediziner warnen vor den Risiken und Nebenwirkungen solcher Pillen. Sie betonen, dass eine gesunde Ernährung und ausreichend Bewegung der Schlüssel zum erfolgreichen Gewichtsverlust sind.
Es gibt keine Wunderpille, die über Nacht für eine schlanke Figur sorgt. Viele dieser Schlankheitspillen enthalten fragwürdige Inhaltsstoffe, die dem Körper schaden können. Wer auf der Suche nach einer langfristigen Lösung für sein Gewichtsproblem ist, sollte daher lieber auf natürliche Methoden setzen.
Reduslim Parere Medico sollte also mit Vorsicht betrachtet werden. Bevor man zu solchen Pillen greift, ist es ratsam, mit einem Arzt zu sprechen und sich umfassend beraten zu lassen. Letztendlich liegt es an jedem selbst, wie er mit seinem Gewicht umgeht. Aber eines steht fest: Gesundheit sollte immer an erster Stelle stehen.
https://reduslim.at/
https://calculatortiktok.com/
Reduslim ist ein beliebtes Diätmittel, das auf dem Markt immer mehr Aufmerksamkeit bekommt. Aber was ist Reduslim genau?
Reduslim ist eine natürliche Ergänzung, die entwickelt wurde, um das Abnehmen zu unterstützen und den Stoffwechsel zu beschleunigen. Durch die einzigartige Kombination aus natürlichen Inhaltsstoffen hilft Reduslim dabei, Fett zu verbrennen und den Körper zu entgiften.
Que es Reduslim? Es ist eine sichere und effektive Möglichkeit, Gewicht zu verlieren und gleichzeitig den Körper mit wichtigen Nährstoffen zu versorgen. Viele zufriedene Kunden berichten von schnellen und nachhaltigen Ergebnissen beim Abnehmen mit Reduslim.
Wenn Sie also nach einem natürlichen und wirksamen Diätmittel suchen, das Ihnen hilft, Ihre Gewichtsabnahmeziele zu erreichen, ist Reduslim die richtige Wahl für Sie. Probieren Sie es aus und erleben Sie selbst die positiven Auswirkungen auf Ihren Körper und Ihre Gesundheit.
https://reduslim.at/
Reduslim de ist ein beliebtes Schlankheitsprodukt auf dem deutschen Markt, das vielen Menschen dabei hilft, ihr Gewicht zu reduzieren und ihre Traumfigur zu erreichen. Die natürlichen Inhaltsstoffe in Reduslim de können den Stoffwechsel anregen, Fett verbrennen und den Appetit reduzieren.
Viele zufriedene Kunden berichten von schnellen und langanhaltenden Ergebnissen, ohne dabei auf strenge Diäten oder harte körperliche Arbeit angewiesen zu sein. Reduslim de ist einfach in der Anwendung und kann ohne ärztliche Verschreibung gekauft werden.
Die positiven Bewertungen und Empfehlungen von Nutzern machen Reduslim de zu einer der am meisten nachgefragten Schlankheitsprodukte in Deutschland. Wenn auch Sie Gewicht verlieren und Ihre Gesundheit verbessern möchten, könnte Reduslim de die richtige Wahl für Sie sein. Probieren Sie es aus und überzeugen Sie sich selbst von den vielen Vorteilen, die Reduslim de bietet.
https://reduslim.at/
Приложение Леон
Reduslim in allattamento kann sich auf die Gesundheit von Mutter und Kind auswirken. Es ist wichtig, dass stillende Mütter immer einen Arzt konsultieren, bevor sie ein neues Nahrungsergänzungsmittel einnehmen. Reduslim ist ein Produkt, das oft bei Gewichtsverlust unterstützen soll, aber während des Stillens können die Inhaltsstoffe des Produkts in die Muttermilch übergehen und somit dem Kind schaden. Es ist daher ratsam, während des Stillens auf solche Produkte zu verzichten und stattdessen auf eine gesunde Ernährung und regelmäßige Bewegung zu setzen, um langfristige Ergebnisse zu erzielen. Bleiben Sie immer auf der sicheren Seite, wenn es um die Gesundheit von Ihnen und Ihrem Baby geht.
https://reduslim.at/
Reduslim bei Diabetes – Kann das Abnehmen bei Diabetikern unterstГјtzen?
Diabetes ist eine chronische Erkrankung, die das tägliche Leben vieler Menschen betrifft. Neben der richtigen Ernährung und regelmäßiger Bewegung kann auch die Einnahme von bestimmten Nahrungsergänzungsmitteln wie Reduslim bei der Gewichtsabnahme helfen. Aber wie wirksam ist Reduslim bei Diabetes?
Studien haben gezeigt, dass die Wirkstoffe in Reduslim den Stoffwechsel anregen und die Fettverbrennung fördern können. Dies kann dazu beitragen, das Körpergewicht zu reduzieren, was wiederum den Blutzuckerspiegel bei Diabetikern positiv beeinflussen kann. Durch die Gewichtsabnahme und die Verbesserung der Insulinsensitivität können Diabetiker möglicherweise ihre Medikamentendosis reduzieren oder sogar ganz darauf verzichten.
Es ist jedoch wichtig zu beachten, dass Reduslim allein keine Wunder bewirken kann. Eine gesunde Ernährung, regelmäßige Bewegung und die regelmäßige Einnahme von Medikamenten sind nach wie vor die wichtigsten Säulen der Diabetesbehandlung. Bevor Diabetiker mit der Einnahme von Reduslim beginnen, sollten sie daher unbedingt Rücksprache mit ihrem Arzt halten.
Insgesamt kann Reduslim Diabetikern dabei helfen, ihr Zielgewicht zu erreichen und damit ihre Lebensqualität zu verbessern. Wenn es darum geht, Diabetes zu managen, ist es wichtig, auf eine ganzheitliche Behandlung zu setzen, die sowohl die körperliche als auch die mentale Gesundheit berücksichtigt. Reduslim kann dabei eine unterstützende Rolle spielen, jedoch sollte es immer im Rahmen eines ganzheitlichen Therapiekonzepts angewendet werden.
https://reduslim.at/
Antonella Clerici ГЁ una celebre conduttrice televisiva italiana che ha recentemente raccontato la sua esperienza con la dieta Reduslim. La dieta con Reduslim si ГЁ rivelata estremamente efficace nel suo caso, aiutandola a perdere peso in modo rapido e naturale.
Reduslim ГЁ un integratore alimentare a base di ingredienti naturali che aiuta a ridurre l’appetito e accelerare il metabolismo. Antonella Clerici ha dichiarato di essere rimasta piacevolmente sorpresa dai risultati ottenuti con questa dieta, che le ha permesso di raggiungere il suo peso ideale senza dover rinunciare a nessun alimento.
La dieta con Reduslim ГЁ stata dunque una vera svolta per Antonella Clerici, che ha condiviso con i suoi fan i benefici di questo prodotto. Grazie alla sua testimonianza, sempre piГ№ persone stanno scoprendo i vantaggi di questa dieta innovativa e naturale. Se anche tu desideri perdere peso in modo sano e efficace, la dieta con Reduslim potrebbe essere la soluzione che fa per te. Segui l’esempio di Antonella Clerici e inizia oggi stesso il tuo percorso verso la forma fisica desiderata.
https://reduslim.at/
MГ¶chten Sie Reduslim kaufen, aber wissen nicht, wo Sie es finden kГ¶nnen? In Italien ist die beste Option, Reduslim online zu kaufen. Die Suche nach “dove comprare Reduslim” wird Ihnen verschiedene Online-Shops prГ¤sentieren, die dieses beliebte Produkt anbieten. Es ist wichtig, sicherzustellen, dass Sie es nur von autorisierten HГ¤ndlern kaufen, um sicherzustellen, dass Sie ein qualitativ hochwertiges und authentisches Produkt erhalten. Mit Reduslim kГ¶nnen Sie effektiv Gewicht verlieren und Ihren Stoffwechsel ankurbeln. Warum also nicht noch heute damit beginnen? Besuchen Sie die offizielle Website und kaufen Sie Reduslim noch heute, um Ihre Gewichtsabnahmeziele zu erreichen.
https://reduslim.at/
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das viele positive Bewertungen erhalten hat. Die Reduslim отзывы zeigen, dass die Benutzer mit den Ergebnissen zufrieden sind. Viele berichten von einer deutlichen Gewichtsabnahme und einer Verbesserung ihres allgemeinen Wohlbefindens.
Die natГјrlichen Inhaltsstoffe von Reduslim, wie GrГјntee-Extrakt und Garcinia Cambogia, wirken effektiv beim Abnehmen, ohne dabei Nebenwirkungen zu verursachen. Die Anwender loben auch die einfache Anwendung und die schnellen Ergebnisse.
Die Reduslim отзывы bestätigen, dass dieses Produkt eine sichere und effektive Methode zur Gewichtsreduktion ist. Es hilft nicht nur beim Abnehmen, sondern fördert auch den Stoffwechsel und sorgt für mehr Energie im Alltag.
Wer also nach einer zuverlässigen und effektiven Möglichkeit sucht, Gewicht zu verlieren, sollte die positiven Bewertungen von Reduslim nicht ignorieren. Probieren Sie es aus und überzeugen Sie sich selbst von den Ergebnissen.
https://reduslim.at/
http://mexicanpharm24.com/# mexico pharmacy mexicanpharm.shop
videos in HD
homesimprovement.net
Reduslim ist eines der beliebtesten Nahrungsergänzungsmittel zur Gewichtsreduktion auf dem Markt. Viele Menschen fragen sich, ob es besser ist, Reduslim morgens oder abends einzunehmen. Die Antwort darauf hängt von den individuellen Gewohnheiten und dem eigenen Körper ab.
Einige Experten empfehlen die Einnahme von Reduslim morgens, da es dabei helfen kann, den Stoffwechsel anzukurbeln und den Körper zu aktivieren. Dies kann besonders hilfreich sein, um den Tag mit einem Energieschub zu beginnen und die Fettverbrennung zu fördern.
Andere empfehlen hingegen die Einnahme von Reduslim abends, da der Körper während des Schlafs besonders effizient Kalorien verbrennt. Durch die Einnahme vor dem Zubettgehen kann Reduslim dabei helfen, den nächtlichen Stoffwechsel anzuregen und die Fettverbrennung über Nacht zu unterstützen.
Letztendlich ist es wichtig, die Einnahme von Reduslim an die persГ¶nlichen Vorlieben und den eigenen Tagesablauf anzupassen. Ob morgens oder abends – Hauptsache, die regelmäßige Einnahme wird nicht vergessen, um die bestmГ¶glichen Ergebnisse zu erzielen.
https://reduslim.at/
https://mexicanpharm24.shop/# mexico pharmacy mexicanpharm.shop
california-invest.com
Reduslim ist ein beliebtes Schlankheitsmittel, das angeblich helfen soll, schnell und effektiv Gewicht zu verlieren. Doch leider gibt es auch viele GerГјchte Гјber Reduslim Abzocke im Internet. Viele Kunden behaupten, dass sie auf BetrГјger hereingefallen sind und ihr Geld fГјr ein Produkt verschwendet haben, das nicht funktioniert.
Es ist wichtig, vorsichtig zu sein und Bewertungen von vertrauenswürdigen Quellen zu lesen, bevor man Reduslim kauft. Es gibt viele legitime Produkte auf dem Markt, die tatsächlich dabei helfen können, Gewicht zu verlieren, aber es gibt auch viele gefälschte Produkte, die nur darauf abzielen, ahnungslose Verbraucher auszunutzen.
Wenn Sie also auf der Suche nach einem Gewichtsverlustprodukt wie Reduslim sind, stellen Sie sicher, dass Sie Ihre Hausaufgaben machen und sich über das Produkt informieren, bevor Sie Ihr Geld ausgeben. Lassen Sie sich nicht von betrügerischen Unternehmen täuschen, die nur Ihr Geld wollen. Bleiben Sie wachsam und vermeiden Sie Reduslim Abzocke.
https://reduslim.at/
Die Reduslim Ernährungs Docs sind ein Konzept, das sich auf gesundes Abnehmen durch richtige Ernährung konzentriert. Die Experten hinter Reduslim haben eine innovative Methode entwickelt, die auf wissenschaftlichen Erkenntnissen basiert und individuell auf die Bedürfnisse jedes Einzelnen zugeschnitten ist.
Die Reduslim Ernährungs Docs bieten nicht nur eine Diät, sondern einen ganzheitlichen Ansatz, um langfristig sein Wunschgewicht zu erreichen. Durch eine ausgewogene Ernährung, die auf frischen und natürlichen Zutaten basiert, sowie regelmäßige Bewegung und Mentales Training werden die Teilnehmer unterstützt, ihre Ziele zu erreichen.
Das Team der Reduslim Ernährungs Docs besteht aus erfahrenen Ernährungswissenschaftlern und Sportprofis, die individuelle Pläne erstellen, um den Teilnehmern zu helfen, gesund und dauerhaft Gewicht zu verlieren. Durch regelmäßige Beratungen und Kontrollen wird der Fortschritt überwacht und bei Bedarf angepasst.
Wer also nach einer nachhaltigen Lösung sucht, um gesund abzunehmen und seine Ernährung langfristig umzustellen, ist bei den Reduslim Ernährungs Docs genau richtig. Mit ihrem innovativen Konzept und der individuellen Betreuung bieten sie die ideale Unterstützung auf dem Weg zum Wunschgewicht.
https://reduslim.at/
Reduslim gehört zu den effektivsten Mitteln zur Gewichtsabnahme und hat viele positive Bewertungen von Kunden erhalten. Auch die Verbraucherorganisation Altroconsumo hat Reduslim getestet und empfohlen. Das natürliche Nahrungsergänzungsmittel hilft dabei, den Stoffwechsel anzukurbeln und die Fettverbrennung zu steigern. Durch die spezielle Formel aus natürlichen Inhaltsstoffen wie Grüntee-Extrakt und Garcinia Cambogia werden Heißhungerattacken reduziert und das Sättigungsgefühl gesteigert. Reduslim ist einfach einzunehmen und unterstützt eine langfristige Gewichtsabnahme. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Effekten!
https://reduslim.at/
https://serialy-na-anglijskom.pp.ua/
обнал карт форум
Обналичивание карт – это противозаконная деятельность, становящаяся все более широко распространенной в нашем современном мире электронных платежей. Этот вид мошенничества представляет значительные вызовы для банков, правоохранительных органов и общества в целом. В данной статье мы рассмотрим частоту встречаемости обналичивания карт, используемые методы и возможные последствия для жертв и общества.
Частота обналичивания карт:
Обналичивание карт является довольно распространенным явлением, и его частота постоянно растет с увеличением числа электронных транзакций. Киберпреступники применяют разнообразные методы для получения доступа к финансовым средствам, включая фишинг, вредоносное программное обеспечение, скимминг и другие инновационные подходы.
Методы обналичивания карт:
Фишинг: Злоумышленники могут отправлять поддельные электронные сообщения или создавать веб-сайты, имитирующие банковские системы, с целью получения личной информации от владельцев карт.
Скимминг: Злоумышленники устанавливают устройства скиммеры на банкоматах или терминалах для считывания данных с магнитных полос карт.
Вредоносное программное обеспечение: Киберпреступники разрабатывают вредоносные программы, которые заражают компьютеры и мобильные устройства, чтобы получить доступ к личным данным и банковским счетам.
Сетевые атаки: Атаки на системы банков и платежных платформ могут привести к утечке информации о картах и, следовательно, к их обналичиванию.
Последствия обналичивания карт:
Финансовые потери для клиентов: Владельцы карт могут столкнуться с материальными потерями, так как средства могут быть списаны с их счетов без их ведома.
Угроза безопасности данных: Обналичивание карт подчеркивает угрозу безопасности личных данных, что может привести к краже личной и финансовой информации.
Ущерб репутации банков: Банки и другие финансовые учреждения могут столкнуться с утратой доверия со стороны клиентов, если их системы безопасности оказываются уязвимыми.
Проблемы для экономики: Обналичивание карт создает экономический ущерб, поскольку оно стимулирует дополнительные затраты на борьбу с мошенничеством и восстановление утраченных средств.
Борьба с обналичиванием карт:
Совершенствование технологий безопасности: Банки и финансовые институты постоянно совершенствуют свои системы безопасности, чтобы предотвратить несанкционированный доступ к картам.
Образование и информирование: Обучение клиентов о методах мошенничества и том, как защитить свои данные, является важным шагом в борьбе с обналичиванием карт.
Сотрудничество с правоохранительными органами: Банки активно сотрудничают с правоохранительными органами для выявления и пресечения преступных схем.
Заключение:
Обналичивание карт – весомая угроза для финансовой стабильности и безопасности личных данных. Решение этой проблемы требует совместных усилий со стороны банков, правоохранительных органов и общества в целом. Только эффективная борьба с мошенничеством позволит обеспечить безопасность электронных платежей и защитить интересы всех участников финансовой системы.
Подробно расскажем, как Расторжение брака – Жирновский районный суд Волгоградской области онлайн или самостоятельно Расторжение брака – Жирновский районный суд Волгоградской области Расторжение брака – Жирновский районный суд Волгоградской области онлайн или самостоятельно
mexico drug stores pharmacies: Mexico pharmacy online – purple pharmacy mexico price list mexicanpharm.shop
Подробно расскажем, как Расторжение брака – Тербунский районный суд Липецкой области онлайн или самостоятельно Расторжение брака – Тербунский районный суд Липецкой области Расторжение брака – Тербунский районный суд Липецкой области онлайн или самостоятельно
Подробно расскажем, как Взыскать компенсацию за задержку зарплаты – Ветлужский районный суд Нижегородской области онлайн или самостоятельно Взыскать компенсацию за задержку зарплаты – Ветлужский районный суд Нижегородской области Взыскать компенсацию за задержку зарплаты – Ветлужский районный суд Нижегородской области онлайн или самостоятельно
Подробно расскажем, как Узаконить перепланировку – Мясниковский районный суд Ростовской области онлайн или самостоятельно Узаконить перепланировку – Мясниковский районный суд Ростовской области Узаконить перепланировку – Мясниковский районный суд Ростовской области онлайн или самостоятельно
Подробно расскажем, как Оспорить решение ЖСК – Березовский городской суд Свердловской области онлайн или самостоятельно Оспорить решение ЖСК – Березовский городской суд Свердловской области Оспорить решение ЖСК – Березовский городской суд Свердловской области онлайн или самостоятельно
Подробно расскажем, как Страховое возмещение по КАСКО – Среднеахтубинский районный суд Волгоградской области онлайн или самостоятельно Страховое возмещение по КАСКО – Среднеахтубинский районный суд Волгоградской области Страховое возмещение по КАСКО – Среднеахтубинский районный суд Волгоградской области онлайн или самостоятельно
credito 9500 euros prestamo 1000 euros
Подробно расскажем, как Восстановить срок принятия наследства – Вытегорский районный суд Вологодской области онлайн или самостоятельно Восстановить срок принятия наследства – Вытегорский районный суд Вологодской области Восстановить срок принятия наследства – Вытегорский районный суд Вологодской области онлайн или самостоятельно
Подробно расскажем, как Признать отцовство – Комсомольский районный суд Ивановской области онлайн или самостоятельно Признать отцовство – Комсомольский районный суд Ивановской области Признать отцовство – Комсомольский районный суд Ивановской области онлайн или самостоятельно
https://indianpharm24.shop/# indian pharmacy paypal indianpharm.store
Подробно расскажем, как Признание завещания недействительным – Костромской районный суд Костромской области онлайн или самостоятельно Признание завещания недействительным – Костромской районный суд Костромской области Признание завещания недействительным – Костромской районный суд Костромской области онлайн или самостоятельно
Подробно расскажем, как Определить с кем останется ребенок – Лодейнопольский городской суд Ленинградской области онлайн или самостоятельно Определить с кем останется ребенок – Лодейнопольский городской суд Ленинградской области Определить с кем останется ребенок – Лодейнопольский городской суд Ленинградской области онлайн или самостоятельно
Aporno online
https://indianpharm24.com/# indian pharmacy paypal indianpharm.store
сериал смотреть
ссылки на другие аккаунта
либо сообщения блога на вашем сайте помогают поисковикам сканировать ваш
вебсайт и формировать более точную.
my site – http://virtvladimir.ru/forum/topic/22235
фильм
фильм в хорошем качестве
международная доставка грузов из китая http://www.perevozka-iz-kitaya.ru/ .
смотреть сериал
LГҐna 5000 kr
mail order pharmacy india: Top online pharmacy in India – india pharmacy mail order indianpharm.store
Предприятие является участником экспортного форсажа, определило два рынка для вывода всех первичных продуктов. Поставляет продукцию в Узбекистан, Киргизию, Белоруссию и Казахстан промышленные весы
юридическая помощь взыскание долгов
бракоразводные услуги
москва семейные юридические консультации
hydroxychloroquine sulfate tablet 200 mg price while primarily known for its application in treating malaria and autoimmune disorders like lupus, has seen a resurgence of interest from the scientific community. Researchers are delving deep into its antiviral properties, exploring the potential mechanisms that might inhibit the replication of viruses, thus broadening the scope of its therapeutic applications.
indiana-daily.com
indian pharmacy: Pharmacies in India that ship to USA – indian pharmacies safe indianpharm.store
real-apartment.com
https://canadianpharmlk.shop/# canadian online drugs canadianpharm.store
Перевозка грузов – главный компонент современной логистики, обеспечивающий передвижение товаров от производителей к потребителям. Это трудный и серьезный процесс, на который влияют огромное количество факторов, и его успешное осуществление настятельно просит проф расклада.
Разнообразие Типов Автотранспорта:
Грузоперевозки деют разнообразие вариантов транспортировки в зависимости от на подобии груза, расстояния и времени доставки. Автомобильные перевозки обеспечивают гибкость и быструю доставку, железнодорожные перевозка грузов эффективны для крупногабаритных и массовых грузов, а морские и авиаперевозки позволяют охватить далекие рынки.
Проф Грузовые Компании:
Оптимальное решение для удачных грузоперевозок – это сотрудничество с проф грузовыми компаниями. Эксперты в этой области деют глубокий диапазон услуг, начиная от планирования маршрутов и упаковки грузов, заканчивая отслеживанием и обеспечиванием безопасности в пути.
Защищенность и Страхование:
Безопасность грузов – приоритет для грузовых компаний. Современные технологии отслеживания и прогноза обеспечивают неизменный контроль за перемещением грузов, а страхование грузов позволяет минимизировать опасности вероятных утрат либо повреждений.
Гибкость и Адаптивность: http://www.dinotte.md/details/saltele/44
Область перевозки грузов требует гибкости и адаптивности к переменам в рыночных критериях и потребностях клиентов. Профессиональные грузовые компании обладают ресурсами для действенной реакции на динамические изменения и обеспечивания клиентов необходимой эластичностью в плане услуг и тарифов.
Экологическая Устойчивость:
Современные тренды в грузоперевозках придают значение экологической стойкости. Почти все компании энергично вводят действенные тс, альтернативные информаторы энергии и стратегии для понижения воздействия на окружающую среду.
Действенное Управление Логистикой:
Грузоперевозки содержат в себе не столько физическое перемещение грузов, но и управление всем логистическим процессом. Действенная логистика – это синхронизация всех этапов доставки, начиная от складского учета и заканчивая четкой доставкой на место предназначения.
Заточение:
Грузоперевозки – это неотъемлемая доля прогрессивной торговли и экономики. Проф грузовые фирмы, владея опытом и ресурсами, обеспечивают надежность и безопасность для ваших грузов, предоставляя глубокий диапазон услуг от планирования до доставки.
LГҐn 200000
скачать леон на андроид
Подробно расскажем, как Взыскать долг по договору займа – Железнодорожный районный суд г. Ростова-на-Дону онлайн или самостоятельно. Юристы по трудовому праву подготовили пошаговую инструкцию по взысканию компенсации за задержку выплаты зарплаты в суде: этапы взыскания, размер пошлины, подсудность и ответы на частые вопросы работников
http://mexicanpharm24.shop/# mexican drugstore online mexicanpharm.shop
Подробно расскажем, как Узаконить перепланировку – Прохоровский районный суд Белгородской области онлайн или самостоятельно. Юристы по трудовому праву подготовили пошаговую инструкцию по взысканию компенсации за задержку выплаты зарплаты в суде: этапы взыскания, размер пошлины, подсудность и ответы на частые вопросы работников
it enables create applications with artificial intelligence and intelligent chatbots, capable to understand the complex https://cmceurope.be/component/k2/item/28-4.
Лучшее казино и БК находится на 1win
Рекомендую лучший беттинг сайт и казино 1win
Оригинальный сайт и казино 1вин находится здесь 1win. Рекомендую!
важная деталь обычных государственных регистрационных табличек состоит такие они делаются по госту Р 50577-93.
My page; https://autodublikat77.ru/
even more a large-scale technological “https://bitcoin-green.org/ in remote oil and gas fields in six states, including New Mexico, Texas and North Dakota.
ниже, вы увидите две ссылки, http://udomlya.ru/userinfo.php?uid=108675 на выбор. Например, яндекс, нажимаем на кнопку фотоаппарата. Воспользуйтесь им и подыщите транспорт, который требуется.
Lancellotti P, Gerard PL, Pierard LA where can i buy priligy in usa
Gana premios con el bono casino sin deposito
casino online con bono de bienvenida sin deposito bono casino sin deposito .
Ad usum externum — Для внешнего употребления.
order trazodone
my canadian pharmacy: List of Canadian pharmacies – reliable canadian online pharmacy canadianpharm.store
Рекомендую лучшую букмекерскую контору в России 1win
Канал постоянно передает новости, развлекательные шоу, рекламные франшизы и, конечно, http://fond.uni-altai.ru/index.php?subaction=userinfo&user=avawyzop музыку. Впервые вышло в эфир в августе 1995 года.
https://canadianpharmlk.shop/# canadian discount pharmacy canadianpharm.store
prilosec
online pharmacy india: п»їlegitimate online pharmacies india – india pharmacy indianpharm.store
Amor omnia vincit – Все побеждает любовь.
http://indianpharm24.shop/# world pharmacy india indianpharm.store
Aeternum vale — Прости навеки
Consumor aliis inserviendo — Изнуряю себя, работая на благо других.
?Juega gratis y gana en el casino con el bono sin deposito!
casino online bono por registro sin deposito casino bono de bienvenida sin deposito .
Conclamatum est — Всё кончено, всё погибло.
https://grandolavanderia.ru/
Ad hoste maligno libera nos, Domine — Избави нас от лукавого, Боже.
Привет, коллеги! В данный день желаю поделиться своими впечатлениями о адмирал х казино официальный сайт. Это место, где веселье объединены в одном месте. Здесь я обнаружил огромный выбор забав. Начиная от классических автоматов и завершая живыми поединками с реальными крупье. Бонусы и специальные предложения приятно заинтересовали, а уровень поддержки на высочайшем уровне. Вчера удалось получить крупный выигрыш, и я уже не могу дождаться возвращения обратно сюда. Рекомендую всем участникам испытать свою собственную везение в адмиралххх!
Необходимо воспользоваться зеркалом официального сайта 1вин или скачать официальное приложение 1win. Регистрация на официальном сайте 1win официаьный сайт
Необходимо воспользоваться зеркалом официального сайта 1вин или скачать официальное приложение 1win. Регистрация на официальном сайте 1win
Сравнение тепловизоров разных производителей
тепловизоры http://teplovizor-od.co.ua .
Тепловизоры: особенности работы и применение
тепловизоры teplovizor-od.co.ua .
компанія-перевізник ” вже майже двадцяти років пропонує міжнародні пасажирські перевезення автобусом за кордон.
Review my web page; http://kyevlyn.ukrbb.net/viewtopic.php?f=12&t=5816
Как привлечь целевую аудиторию на свой сайт
6
продвижение сайта в гугл https://seo-prodvizhenie-sayta.co.ua .
Тепловизоры: преимущества и недостатки
цена тепловизоры http://teplovizor-od.co.ua/ .
Тепловизоры: как выбрать идеальный вариант
тепловизоры http://www.teplovizor-od.co.ua .
order clomid without dr prescription: clomid ovulation calculator – how to get generic clomid price
https://amoxilst.pro/# amoxicillin over counter
Best cucmber ever cucumber
All Roofing Services & Skylights
5.0 41 Google reviews
Roofing contractor in Toronto, Canada
Address: 19 Sabrina Dr, Etobicoke, ON M9R 2J4, Canada
Hours: Closed ⋅ Opens 8 AM Mon
Phone: +1 647-560-2688
Province: Ontario
Areas served:
Toronto and nearby areas
http://amoxilst.pro/# amoxicillin 500mg cost
amoxicillin over the counter in canada: where can i get amoxicillin – amoxicillin 500 mg where to buy
Важность SEO-оптимизации для продвижения сайта
5
продвижения сайта в гугле http://seo-prodvizhenie-sayta.co.ua/ .
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das beim Abnehmen helfen kann. Die spezielle Formel des Produkts soll den Stoffwechsel anregen und die Fettverbrennung steigern. Viele Menschen schwören auf die Wirksamkeit von Reduslim und berichten von schnellen Ergebnissen.
Die natürlichen Inhaltsstoffe des Produkts sollen zudem den Appetit hemmen und das Sättigungsgefühl fördern. Dadurch wird das Abnehmen erleichtert und Heißhungerattacken vorgebeugt. Reduslim ist einfach anzuwenden und kann in den Alltag integriert werden.
Für beste Resultate sollte Reduslim in Kombination mit einer gesunden Ernährung und regelmäßiger Bewegung eingenommen werden. Es gibt viele positive Erfahrungsberichte von Menschen, die mit Reduslim erfolgreich abgenommen haben und ihr Wunschgewicht erreicht haben. Probieren Sie es selbst aus und starten Sie noch heute Ihren Weg zum Wunschgewicht mit Reduslim!
https://reduslim.at/
Партнерский маркетинг как инструмент продвижения сайта
19
сео продвижение сайта https://www.seo-prodvizhenie-sayta.co.ua/ .
Можно приготовить вкусный ягодный смузи из замороженных ягод и йогурта, с фруктовым соком или молоком смузи
indocin 10mg
Reduslim átverés ist ein Begriff, der oft im Zusammenhang mit Gewichtsverlustprodukten verwendet wird. Viele Menschen sind skeptisch gegenüber solchen Produkten, da es auf dem Markt viele betrügerische Produkte gibt. Es ist wichtig, vorsichtig zu sein und die Hersteller und Verkäufer gründlich zu recherchieren, bevor man sich für ein Produkt entscheidet.
Es ist auch wichtig, realistische Erwartungen zu haben, wenn es um Gewichtsverlust geht. Wunderpillen gibt es nicht und langfristige Ergebnisse erfordern eine Änderung des Lebensstils, einschließlich einer gesunden Ernährung und regelmäßiger Bewegung. Reduslim átverés sollte also nicht als Wundermittel angesehen werden, sondern als Unterstützung auf dem Weg zur Gewichtsabnahme.
Es ist ratsam, sich an anerkannte Gesundheitsexperten und Ernährungsberater zu wenden, um Unterstützung beim Abnehmen zu erhalten. Es gibt viele seriöse Programme und Produkte, die dabei helfen können, Gewicht zu verlieren und gesund zu bleiben. Die Verbraucher sollten also vorsichtig sein und sich gut informieren, bevor sie sich für ein bestimmtes Produkt entscheiden.
https://reduslim.at/
Fake Reduslim Produkte können gefährlich sein für deine Gesundheit. Es ist wichtig, dass du beim Kauf von Reduslim Produkten vorsichtig bist und sicherstellst, dass du ein echtes und qualitativ hochwertiges Produkt kaufst. Es gibt viele gefälschte Reduslim Produkte auf dem Markt, die nicht nur wirkungslos sind, sondern auch gesundheitsschädlich sein können.
Um sicherzustellen, dass du ein echtes Reduslim Produkt kaufst, solltest du nur von vertrauenswürdigen Quellen kaufen, wie zum Beispiel der offiziellen Website des Herstellers. Achte auf das Etikett und die Verpackung, um sicherzustellen, dass es keine Anzeichen von Fälschungen gibt.
Fake Reduslim Produkte können schädliche Inhaltsstoffe enthalten, die deine Gesundheit beeinträchtigen können. Deshalb ist es wichtig, nur echte Produkte zu kaufen, um sicherzustellen, dass du die gewünschten Ergebnisse erzielst, ohne deine Gesundheit zu gefährden.
Lass dich nicht von Fake Reduslim Produkten täuschen und investiere in deine Gesundheit, indem du nur echte und qualitativ hochwertige Produkte kaufst. Schütze dich vor gefälschten Produkten und achte auf deine Gesundheit.
https://reduslim.at/
gagarin studio специалистов в медцентрах СПРАВКИ.
Take a look at my web-site: http://xn--d1abavhdnc2a.xn--p1ai/spravka-gostajna
Можно приготовить вкусный ягодный смузи из замороженных ягод и йогурта, с фруктовым соком или молоком татарские блюда
this is as usual, is for large orders, since the withdrawal of money changes the liquidity in pools, https://eidoo-wallet.io/, which then changes the price of the asset when your deal is executed.
Reduslim hat kürzlich bei Stiftung Warentest eine sehr gute Bewertung erhalten, was viele Kunden dazu veranlasst hat, das Produkt auszuprobieren. Meine Erfahrung mit Reduslim Stiftung Warentest war ebenfalls positiv. Nachdem ich verschiedene Diätmittel ausprobiert hatte, war ich skeptisch, ob Reduslim wirklich funktionieren würde. Aber die Ergebnisse haben mich überzeugt. Innerhalb von nur vier Wochen habe ich deutlich an Gewicht verloren und fühle mich fitter und energiegeladener.
Das Geheimnis von Reduslim liegt in seiner einzigartigen Formel, die auf natürlichen Inhaltsstoffen basiert und den Stoffwechsel ankurbelt. Das Produkt ist einfach zu dosieren und hat keine bekannten Nebenwirkungen. Meine Erfahrung mit Reduslim Stiftung Warentest bestätigt, dass es nicht nur wirksam, sondern auch sicher ist.
Ich kann Reduslim daher uneingeschränkt empfehlen, besonders wenn Sie schon länger nach einem Diätmittel suchen, das tatsächlich funktioniert. Geben Sie dem Produkt eine Chance und machen Sie Ihre eigenen positiven Erfahrungen mit Reduslim Stiftung Warentest. Sie werden es nicht bereuen.
https://reduslim.at/
air cargo charter companies https://aircgc-lux.com/ .
1
seo заказать https://seo-prodvizhenie-sayta.co.ua .
Reduslim Ilka ist eine innovative und effektive Methode, um Gewicht zu verlieren und den Körper zu straffen. Diese einzigartige Formel kombiniert natürliche Inhaltsstoffe, um den Stoffwechsel anzukurbeln und Fett zu verbrennen.
Ilka war schon lange auf der Suche nach einer Lösung, um die lästigen Pfunde loszuwerden, die sich im Laufe der Jahre angesammelt hatten. Nachdem sie Reduslim Ilka ausprobierte, war sie begeistert von den Ergebnissen. Innerhalb weniger Wochen konnte sie einen deutlichen Unterschied in ihrem Körper feststellen. Ihr Bauch war flacher, ihre Oberschenkel straffer und ihr Selbstbewusstsein enorm gestiegen.
Die spezielle Kombination aus grüner Tee-Extrakt, Guarana und Vitamin B12 sorgt für einen schnellen Abbau von Fettgewebe und unterstützt gleichzeitig den Muskelaufbau. Ilka war erstaunt, wie einfach es war, mit Reduslim Ilka abzunehmen, ohne sich dabei hungrig zu fühlen oder mühsame Diäten einhalten zu müssen.
Wenn auch du auf der Suche nach einer effektiven Methode bist, um Gewicht zu verlieren und deinen Körper zu straffen, dann probiere Reduslim Ilka aus. Es ist eine natürliche und sichere Möglichkeit, um dein Wunschgewicht zu erreichen und dich rundum wohl zu fühlen. Lass dich von Ilkas Erfolgsgeschichte inspirieren und starte noch heute deine eigene Abnehmreise mit Reduslim Ilka.
https://reduslim.at/
Reduslim preço: Die beste Lösung für schnellen und effektiven Gewichtsverlust
Wenn es um das Thema Gewichtsverlust geht, suchen viele Menschen nach einer schnellen und effektiven Lösung. Reduslim preço ist eine natürliche Ergänzung, die dabei helfen kann, überschüssige Pfunde loszuwerden und das Zielgewicht schneller zu erreichen.
Die wirksame Formel von Reduslim preço setzt auf natürliche Inhaltsstoffe wie grüner Tee-Extrakt, Guarana und Ingwer, die den Stoffwechsel anregen und den Fettverbrennungsprozess beschleunigen. Darüber hinaus sorgt die spezielle Mischung aus Ballaststoffen dafür, dass man sich länger satt fühlt und somit Heißhungerattacken vorbeugt.
Ein weiterer Vorteil von Reduslim preço ist, dass es den Appetit reduziert und das Verlangen nach ungesunden Snacks eindämmt. Das bedeutet, dass man weniger Kalorien zu sich nimmt und somit schneller abnehmen kann.
Wenn Sie also auf der Suche nach einer effektiven und kostengünstigen Lösung für Ihre Gewichtsabnahme sind, könnte Reduslim preço die richtige Wahl für Sie sein. Probieren Sie es aus und erleben Sie die positiven Veränderungen in Ihrem Körper!
https://reduslim.at/
https://grandolavanderia.ru/
flarealestates.com
livingspainhome.com
Möchten Sie wissen, wie Sie Reduslim bestellen können? Es ist ganz einfach! Sie müssen nur die offizielle Website von Reduslim besuchen und das Produkt in den Warenkorb legen. Geben Sie dann Ihre Lieferadresse an und wählen Sie die gewünschte Zahlungsmethode aus. Nachdem Sie die Bestellung aufgegeben haben, wird das Produkt schnell zu Ihnen nach Hause geliefert. Nutzen Sie noch heute die Vorteile von Reduslim, um Ihren Gewichtsverlust zu unterstützen und eine gesündere Lebensweise zu erreichen. ?>>
Dank seiner natГјrlichen Zutaten kann Reduslim Ihnen helfen, schneller Gewicht zu verlieren und Ihren Stoffwechsel zu steigern. Es ist wichtig, dass Sie eine ausgewogene ErnГ¤hrung und regelmäßige Bewegung in Ihren Lebensstil integrieren, um die besten Ergebnisse zu erzielen. Bestellen Sie noch heute Reduslim und beginnen Sie noch heute Ihre gesunde Reise! “Come ordinare Reduslim” ist jetzt keine Frage mehr – es ist ganz einfach und bequem.
https://reduslim.at/
Reduslim und Ultraslim sind zwei innovative Produkte, die sich ideal ergänzen, um effektiv Gewicht zu verlieren und den Körper zu entgiften. Die Kombination dieser beiden Supplements kann Ihnen dabei helfen, Ihr Wunschgewicht zu erreichen und sich gleichzeitig gesünder und vitaler zu fühlen.
Reduslim ist ein einzigartiges Nahrungsergänzungsmittel, das auf natürliche Weise den Stoffwechsel ankurbelt und die Fettverbrennung beschleunigt. Es enthält wirkungsvolle Inhaltsstoffe wie Grüntee-Extrakt, Garcinia Cambogia und grüner Kaffee, die dabei helfen, den Appetit zu zügeln und die Fettaufnahme zu reduzieren.
Ultraslim dagegen ist ein Detox-Produkt, das Ihren Körper von schädlichen Toxinen und Schlacken befreit und dadurch das Immunsystem stärkt. Mit Inhaltsstoffen wie Spirulina, Chlorella und Zimtrinde unterstützt Ultraslim die Entgiftung des Körpers und fördert so langfristig die Gesundheit und das Wohlbefinden.
Wenn Sie also nach einer effektiven und ganzheitlichen Methode suchen, um Gewicht zu verlieren und sich besser zu fühlen, sollten Sie unbedingt Reduslim und Ultraslim in Kombination ausprobieren. Gönnen Sie sich und Ihrem Körper diese wertvolle Unterstützung und starten Sie noch heute Ihren Weg zu einer gesünderen und vitaleren Lebensweise.
https://reduslim.at/
Тепловизоры: новинки и тренды на рынке
тепловизоры http://teplovizor-od.co.ua .
Antonella Clerici ist bekannt fГјr ihre strahlende PersГ¶nlichkeit und ihren fabelhaften Stil. Als beliebte italienische TV-Moderatorin und Kochbuchautorin hat sie schon vielen Menschen Inspiration gegeben, gesund zu leben. KГјrzlich hat sie ihre Geheimnis zur Gewichtsabnahme enthГјllt – Reduslim! Dieses natГјrliche NahrungsergГ¤nzungsmittel hilft ihr, fit zu bleiben und ihr Gewicht zu kontrollieren. Antonella schwГ¶rt auf die Wirksamkeit von Reduslim und teilt gerne ihre Erfahrungen mit ihren Fans. Wenn auch du nach einer einfachen und natГјrlichen MГ¶glichkeit suchst, Gewicht zu verlieren, dann probiere Reduslim aus und starte noch heute deine Reise zu einem gesГјnderen Leben!
https://reduslim.at/
Ilka Bessin gehört zu den bekanntesten deutschen Comedians und hat in den letzten Jahren auch mit ihrem Gewichtsverlust für Aufsehen gesorgt. Viele fragen sich, wie sie es geschafft hat, so viel abzunehmen. Das Geheimnis könnte in dem Produkt Reduslim liegen. Ilka Bessin schwört angeblich auf die Wirkung der natürlichen Inhaltsstoffe, die den Stoffwechsel ankurbeln und die Fettverbrennung fördern. Ob es tatsächlich an Reduslim liegt oder an ihrer Disziplin und sportlichen Aktivitäten, bleibt ihr Geheimnis. Aber eins ist sicher: Ilka Bessin hat bewiesen, dass man mit der richtigen Motivation und Unterstützung sein Ziel erreichen kann.
https://reduslim.at/
Reduslim ist ein beliebtes Abnehmprodukt, das man auf Amazon Original finden kann. Viele Menschen schwören auf die Wirksamkeit dieses Produkts, um lästige Kilos loszuwerden. Mit natürlichen Inhaltsstoffen wie Grüntee-Extrakt und Guarana soll Reduslim den Stoffwechsel ankurbeln und das Hungergefühl reduzieren. Die positiven Bewertungen auf Amazon zeigen, dass viele Nutzer mit Reduslim zufrieden sind und erfolgreich abgenommen haben. Wer also nach einem effektiven und sicheren Abnehmprodukt sucht, sollte definitiv Reduslim auf Amazon Original ausprobieren.
https://reduslim.at/
generic amoxil 500 mg: how long is strep contagious after amoxicillin – canadian pharmacy amoxicillin
https://clomidst.pro/# where buy generic clomid prices
Что действительно следует учитывать, используя наш генератор виртуальных номеров, так это то, что каждый тестовый телефон, который предлагает эмулятор, действительно доступен множеству пользователей на протяжении всего своего периода актуальности аренда сим карты
через всемирную паутину такие оскорбления,
как «грумер» (groomer) – образ, согласно которому ЛГБТК-люди являются «детскими грумерами» или.
My web site – http://lgbtfilms.ru/?cat=64
Erfahrungsberichte mit Reduslim sind vielfältig und positiv. Viele Anwender berichten von beeindruckenden Ergebnissen nach der Einnahme dieses beliebten Nahrungsergänzungsmittels. Reduslim ist bekannt für seine effektive Wirkung beim Abnehmen und wird von Nutzern weltweit gelobt.
Viele Menschen berichten, dass sie mit Reduslim erfolgreich ihr Wunschgewicht erreicht haben, ohne dabei auf strenge Diäten oder anstrengende Workouts angewiesen zu sein. Die natürlichen Inhaltsstoffe von Reduslim helfen dem Körper, Fett zu verbrennen und den Stoffwechsel zu beschleunigen.
Einige Nutzer berichten auch von einer verbesserten Verdauung und einem gesteigerten Wohlbefinden nach der Einnahme von Reduslim. Die meisten Erfahrungsberichte mit Reduslim zeigen, dass das Produkt sicher und effektiv ist, wenn es in Kombination mit einer ausgewogenen Ernährung und regelmäßiger Bewegung verwendet wird.
Insgesamt scheint Reduslim eine echte Lösung für diejenigen zu sein, die auf der Suche nach einem natürlichen und effektiven Weg zum Abnehmen sind. Wer also nach einer Möglichkeit sucht, sein Gewicht zu reduzieren und sich gleichzeitig gesünder und fitter zu fühlen, sollte definitiv die Erfahrungsberichte mit Reduslim genauer unter die Lupe nehmen.
https://reduslim.at/
70000 euro lenen
Что действительно следует учитывать, используя наш генератор виртуальных номеров, так это то, что каждый тестовый телефон, который предлагает эмулятор, действительно доступен множеству пользователей на протяжении всего своего периода актуальности арендовать номер телефона
Reduslim Timo ist ein revolutionäres Produkt auf dem Markt für Gewichtsabnahme. Mit einer einzigartigen Formel, die natürliche Inhaltsstoffe wie grüner Tee, Guarana-Extrakt und Ingwer enthält, hilft es, den Stoffwechsel zu beschleunigen und Fett effektiv zu verbrennen. Viele Kunden sind begeistert von den Ergebnissen, die sie mit Reduslim Timo erzielen konnten.
Die Kombination aus den potenten Inhaltsstoffen wirkt nicht nur als Appetitzügler, sondern auch als Energiespender, um während des Abnehmens aktiv und fit zu bleiben. Zudem fördert Reduslim Timo die Verdauung und unterstützt den Körper bei der Entgiftung.
Die einfache Anwendung und die schnellen Ergebnisse machen Reduslim Timo zu einer beliebten Wahl unter denjenigen, die auf gesunde Weise abnehmen möchten. Es ist wichtig zu betonen, dass Reduslim Timo kein Wundermittel ist und regelmäßige Bewegung und eine ausgewogene Ernährung ebenfalls entscheidend sind.
Wenn auch Sie sich von den positiven Effekten von Reduslim Timo Гјberzeugen mГ¶chten, sollten Sie es selbst ausprobieren. Beginnen Sie noch heute mit Ihrem Weg zur Traumfigur und genieГџen Sie das GefГјhl von VitalitГ¤t und Selbstbewusstsein. Reduslim Timo – die natГјrliche UnterstГјtzung auf dem Weg zur Wunschfigur!
https://reduslim.at/
https://prednisonest.pro/# where to get prednisone
Möchten Sie Reduslim kaufen und fragen sich, ob es auch bei Rossmann erhältlich ist? Leider ist Reduslim bisher nicht im Sortiment von Rossmann zu finden. Aber keine Sorge, das Abnehmprodukt kann bequem online bestellt werden. Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das dabei helfen kann, auf natürliche Weise Gewicht zu verlieren. Die spezielle Formel aus natürlichen Inhaltsstoffen wirkt unterstützend bei der Fettverbrennung und kann den Stoffwechsel anregen. Wenn Sie Reduslim kaufen möchten, empfehle ich Ihnen, es direkt beim Hersteller zu bestellen. Dort erhalten Sie stets das Originalprodukt und können von attraktiven Rabatten profitieren. Also, nicht lange zögern und Ihren Weg zur Traumfigur starten!
https://reduslim.at/
Оригианльный сайт казино и БК находится на 1win
Pillole dimagranti Reduslim – die Geheimwaffe gegen lГ¤stige Pfunde?
Möchten Sie gerne ein paar Kilos verlieren und suchen nach einer effektiven Lösung? Dann sollten Sie vielleicht die pillole dimagranti Reduslim in Betracht ziehen. Diese Abnehmpillen versprechen schnelle und nachhaltige Ergebnisse, indem sie den Stoffwechsel ankurbeln und das Hungergefühl reduzieren.
Die Wirkung der Reduslim Pillen beruht auf einer sorgfältig abgestimmten Kombination natürlicher Inhaltsstoffe, die nachweislich beim Abnehmen unterstützen. Doch Vorsicht ist geboten: Jeder Körper reagiert anders auf die Einnahme von Nahrungsergänzungsmitteln, daher ist es wichtig, vorher seinen Arzt zu konsultieren.
Reduslim ist nicht die alleinige Lösung für Gewichtsprobleme. Neben der Einnahme der Abnehmpillen ist eine ausgewogene Ernährung und regelmäßige Bewegung entscheidend, um langfristige Erfolge zu erzielen. Wenn Sie jedoch Unterstützung bei Ihrer Diät benötigen, könnten die Reduslim Pillen eine hilfreiche Ergänzung sein. Probieren Sie es aus und überzeugen Sie sich selbst von der Wirkung dieser pillole dimagranti.
https://reduslim.at/
Рекомендую лучший казино и беттинг сайт 1win
Оригинальный сайт беттинговый 1вин находится здесь 1win. Рекомендую!
Möchten Sie Reduslim kaufen und fragen sich nach dem Preis bei Rossmann? Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das beim Abnehmen helfen soll. Bei Rossmann können Sie dieses Produkt zu einem erschwinglichen Preis erwerben. Reduslim ist dafür bekannt, den Stoffwechsel zu beschleunigen und somit die Fettverbrennung zu fördern. Durch die enthaltenen natürlichen Inhaltsstoffe kann Reduslim eine gesunde Gewichtsabnahme unterstützen. Wenn Sie Reduslim kaufen möchten, schauen Sie doch einfach bei Rossmann vorbei und überzeugen Sie sich selbst von den positiven Effekten dieses Produkts.
https://reduslim.at/
can i order clomid pills: where to get generic clomid pills – can you buy generic clomid without insurance
Auf der Suche nach dem perfekten Begleiter fГјr Ihre Gewichtsabnahme? Reduslim Telefono kГ¶nnte die LГ¶sung fГјr Sie sein! Dieses natГјrliche NahrungsergГ¤nzungsmittel verspricht eine effektive UnterstГјtzung bei der Fettverbrennung und hilft Ihnen, Ihr Traumgewicht zu erreichen. Mit seiner einzigartigen Formel aus natГјrlichen Inhaltsstoffen, hilft Reduslim Telefono, den Stoffwechsel zu steigern und die Fettverbrennung zu maximieren. Kein Wunder, dass es bei vielen Menschen bereits beliebt ist. Probieren Sie es jetzt aus und sehen Sie selbst, wie einfach es sein kann, Gewicht zu verlieren und sich wohl in Ihrer Haut zu fГјhlen. Reduslim Telefono – Ihre Geheimwaffe fГјr eine erfolgreiche Gewichtsabnahme!
https://reduslim.at/
Reduslim Apotheken: Ein effektives Mittel zur Gewichtsabnahme?
Reduslim ist ein beliebtes Produkt, das in vielen Apotheken erhältlich ist und bei der Gewichtsabnahme unterstützen soll. Doch wie effektiv ist dieses Produkt wirklich?
Die meisten Nutzer berichten von positiven Erfahrungen mit Reduslim. Durch die spezielle Kombination von natГјrlichen Inhaltsstoffen wie grГјnem Kaffeeextrakt und Guarana soll es den Stoffwechsel ankurbeln und somit die Fettverbrennung steigern. Zudem soll es das HungergefГјhl verringern und somit die Kalorienaufnahme reduzieren.
Dennoch ist es wichtig zu beachten, dass Reduslim allein keine Wunder bewirken kann. Eine gesunde Ernährung und ausreichend Bewegung sind nach wie vor der Schlüssel zur erfolgreichen Gewichtsabnahme.
Insgesamt scheint Reduslim jedoch eine vielversprechende Option zu sein, um das Abnehmen zu unterstГјtzen. Wer also auf der Suche nach einem effektiven Mittel ist, sollte einen Blick in die Apotheken werfen und sich Гјber Reduslim informieren.
https://reduslim.at/
Reduslim ist ein beliebtes Produkt, das viele Menschen beim Abnehmen unterstützt. In den Avis Reduslim Bewertungen wird oft die Wirksamkeit des Produkts gelobt. Viele Anwender berichten von einer schnellen Gewichtsabnahme und einer verbesserten Stoffwechselaktivität.
Das Geheimnis von Reduslim liegt in seiner natürlichen Formel, die Stoffwechselprozesse beschleunigt und den Körper dabei unterstützt, Fett effektiv zu verbrennen. Die in Reduslim enthaltenen Inhaltsstoffe wie Grüntee-Extrakt und Guarana sind bekannt für ihre fettverbrennende Wirkung.
Avis Reduslim hat sich als effektives Mittel beim Abnehmen bewährt und wird von vielen zufriedenen Kunden empfohlen. Wenn auch Sie Ihre Traumfigur erreichen möchten, sollten Sie Reduslim ausprobieren und die positiven Effekte selbst erleben. Mit Reduslim können Sie auf natürliche Weise und ohne große Anstrengungen Gewicht verlieren. Probieren Sie es aus und überzeugen Sie sich selbst von der Wirksamkeit von Reduslim.
https://reduslim.at/
Die Zusammensetzung von Reduslim spielt eine entscheidende Rolle für seine Wirksamkeit als Nahrungsergänzungsmittel zur Gewichtsabnahme. Reduslim enthält eine einzigartige Mischung aus natürlichen Inhaltsstoffen, die synergistisch zusammenarbeiten, um den Stoffwechsel zu steigern und die Fettverbrennung zu fördern.
Zu den Hauptbestandteilen von Reduslim gehören Grüner Kaffee, Garcinia Cambogia, Guarana und L-Carnitin. Grüner Kaffee-Extrakt enthält Chlorogensäure, die die Fettverbrennung ankurbelt und den Appetit unterdrückt. Garcinia Cambogia ist bekannt für seine Fähigkeit, die Umwandlung von Kohlenhydraten in Fett zu blockieren und das Sättigungsgefühl zu erhöhen. Guarana liefert Energie und verbessert die Ausdauer während des Trainings. L-Carnitin unterstützt den Transport von Fettsäuren in die Zellen, wo sie zur Energiegewinnung verbrannt werden.
Die richtige Zusammensetzung von Reduslim macht es zu einer effektiven Lösung für Menschen, die Gewicht verlieren wollen. Es ist wichtig sicherzustellen, dass das Produkt aus hochwertigen Zutaten hergestellt wird und keine schädlichen Chemikalien oder Füllstoffe enthält. Vor der Einnahme von Reduslim sollte man immer die Packungsbeilage lesen und gegebenenfalls einen Arzt konsultieren. Mit der richtigen Ernährung und Bewegung kann Reduslim helfen, das Körpergewicht zu reduzieren und eine gesunde Lebensweise zu fördern.
https://reduslim.at/
Medikament Reduslim ist ein neues revolutionäres Abnehmprodukt, das die Welt im Sturm erobert. Mit seiner einzigartigen Formel aus natürlichen Inhaltsstoffen hilft Reduslim Menschen dabei, effektiv und sicher Gewicht zu verlieren. Es fördert die Fettverbrennung, reduziert das Hungergefühl und steigert den Stoffwechsel.
Reduslim ist kein Wundermittel, sondern basiert auf wissenschaftlichen Erkenntnissen und Forschung. Die Kombination aus grünem Kaffee, Garcinia Cambogia und anderen pflanzlichen Wirkstoffen sorgt für eine nachhaltige Gewichtsreduktion und unterstützt den Körper dabei, gesund und fit zu bleiben.
Viele zufriedene Anwender berichten von deutlichen Erfolgen nach der Einnahme von Reduslim. Sie konnten ihr Gewicht reduzieren, ohne strenge Diäten einhalten oder sich stundenlang im Fitnessstudio quälen zu müssen. Reduslim macht das Abnehmen einfach und unkompliziert.
Wenn auch du nach einem effektiven Abnehmmedikament suchst, das dir dabei hilft, deine Ziele zu erreichen, solltest du Medikament Reduslim eine Chance geben. Probiere es aus und Гјberzeuge dich selbst von den positiven Ergebnissen. Mach den ersten Schritt zu einem gesГјnderen und schlankeren Leben mit Reduslim!
https://reduslim.at/
Der Preis von Reduslim bei Mercadona variiert je nach Standort und Angebot. Es ist ratsam, regelmäßig die Preise zu überprüfen, um das bestmögliche Angebot zu erhalten. Reduslim ist ein beliebtes Nahrungsergänzungsmittel zur Gewichtsreduktion, das in Mercadona erhältlich ist. Es wird empfohlen, vor der Einnahme von Reduslim einen Arzt zu konsultieren, um sicherzustellen, dass es für Sie geeignet ist. Mit einer gesunden Ernährung und regelmäßiger Bewegung kann Reduslim Ihnen helfen, Ihre Gewichtsziele zu erreichen. Besuchen Sie Ihre örtliche Mercadona-Filiale, um den aktuellen Preis von Reduslim zu erfahren und starten Sie noch heute Ihre Gewichtsverlustreise.
https://reduslim.at/
она обеспечивает мощные возможности чата, https://windowss10.ru/apps/generativno-prediktivnye-transformery-vzglyad-v-budushhee-s-gpt-4.html без ограничений и платежей.
Reduslim vo kaufen ist eine beliebte Option für diejenigen, die schnell und effektiv abnehmen möchten. Reduslim ist ein natürlicher Fatburner, der dabei helfen kann, überschüssige Pfunde loszuwerden. Doch wo kann man Reduslim kaufen?
In Deutschland ist Reduslim vo kaufen ganz einfach online möglich. Auf verschiedenen Websites und in Online-Shops kann man das Produkt bestellen und bequem nach Hause liefern lassen. Dabei sollte man jedoch darauf achten, dass man das Originalprodukt kauft, um die bestmöglichen Ergebnisse zu erzielen.
Reduslim enthält natürliche Inhaltsstoffe wie Grüntee-Extrakt und Guarana, die den Stoffwechsel anregen und die Fettverbrennung unterstützen. Durch die Einnahme von Reduslim können also nicht nur die Kilos purzeln, sondern auch das Wohlbefinden gesteigert werden.
Wer also auf der Suche nach einer effektiven und einfachen Lösung zum Abnehmen ist, sollte definitiv Reduslim vo kaufen in Betracht ziehen. Mit der richtigen Ernährung und ausreichend Bewegung kann man so sein Traumgewicht erreichen und sich bald über eine schlankere Figur freuen.
https://reduslim.at/
Reduslim ist ein beliebtes Schlankheitsmittel, aber was sagen die Ärzte dazu? Viele Experten sind geteilter Meinung über die Wirksamkeit dieses Produkts. Einige behaupten, dass Reduslim tatsächlich beim Abnehmen hilft, während andere skeptisch sind und Bedenken hinsichtlich möglicher Nebenwirkungen äußern. Die Meinungen der Ärzte sind also gespalten.
Einige Ärzte argumentieren, dass Reduslim eine natürliche und sichere Möglichkeit bietet, Gewicht zu verlieren, ohne auf radikale Diäten oder starke Medikamente zurückzugreifen. Sie empfehlen das Produkt als eine unterstützende Maßnahme zu einer gesunden Ernährung und regelmäßiger Bewegung. Andere Ärzte sind jedoch skeptisch und warnen vor möglichen Risiken für die Gesundheit.
Letztendlich liegt es an jedem Einzelnen, mit seinem Arzt zu sprechen und die Risiken und Vorteile von Reduslim abzuwägen. Es ist wichtig, informierte Entscheidungen zu treffen und sich möglichst umfassend zu informieren, bevor man ein Schlankheitsmittel wie Reduslim einnimmt. Jeder Körper reagiert anders und was für den einen funktioniert, muss nicht zwangsläufig auch für den anderen geeignet sein.
https://reduslim.at/
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das beim Abnehmen helfen soll. Viele Menschen interessieren sich für den Reduslim Rossman Preis und fragen sich, ob es das Produkt auch in der Drogerie zu einem guten Preis gibt.
Während Reduslim nicht direkt bei Rossmann erhältlich ist, kann es online zu einem günstigen Preis erworben werden. Kunden, die nach dem Reduslim Rossman Preis suchen, sollten sich bewusst sein, dass der Preis für das Produkt je nach Anbieter variieren kann.
Es wird empfohlen, Reduslim direkt Гјber die offizielle Website des Herstellers zu kaufen, um sicherzustellen, dass es sich um ein authentisches Produkt handelt. Dort kann man auch von speziellen Angeboten und Rabatten profitieren.
Der Reduslim Rossman Preis mag verlockend erscheinen, aber es ist wichtig, sich vor dem Kauf gut zu informieren und sicherzustellen, dass man ein qualitativ hochwertiges Produkt bekommt. Mit einer gesunden Ernährung und regelmäßiger Bewegung kann Reduslim dabei helfen, erfolgreich Gewicht zu verlieren und das Wunschgewicht zu erreichen.
https://reduslim.at/
Auf der Suche nach einem effektiven Gewichtsverlustprodukt stoßen viele Menschen auf Reduslim Avis. Dieses natürliche Nahrungsergänzungsmittel hat in der Online-Community viel Aufmerksamkeit erregt. Aber was steckt hinter den positiven Bewertungen?
Reduslim Avis wird als eine sichere und wirksame Lösung zum Abnehmen angepriesen. Die Kombination aus natürlichen Zutaten soll den Stoffwechsel ankurbeln, den Hunger reduzieren und die Fettverbrennung fördern. Viele Benutzer berichten von schnellen und langanhaltenden Ergebnissen.
Die positiven Auswirkungen von Reduslim Avis sind auch auf die sorgfältige Auswahl der Inhaltsstoffe zurückzuführen. Diese wurden speziell ausgewählt, um den Körper beim Abnehmen zu unterstützen, ohne dabei unerwünschte Nebenwirkungen hervorzurufen.
Wenn Sie auf der Suche nach einem zuverlässigen und effektiven Gewichtsverlustprodukt sind, könnte Reduslim Avis die Lösung für Sie sein. Probieren Sie es aus und lassen Sie sich von den Ergebnissen überzeugen.
https://reduslim.at/
nettsteder
Reduslim ist ein beliebtes Produkt zur Gewichtsabnahme, aber es gibt auch einige negative Meinungen darüber. Einige Benutzer berichten von schlechten Erfahrungen und unerwünschten Nebenwirkungen. Sie warnen davor, dass es nicht so effektiv ist, wie behauptet wird, und dass es zu Magenbeschwerden und Schlafstörungen führen kann. Allerdings muss man bedenken, dass jeder Körper anders ist und was für den einen funktioniert, muss nicht unbedingt für den anderen gelten. Es ist wichtig, professionelle Beratung einzuholen, bevor man ein solches Produkt einnimmt, um sicherzustellen, dass es für einen geeignet ist.
https://reduslim.at/
Reduslim Pastillas sind ein beliebtes Nahrungsergänzungsmittel, das dabei hilft, überflüssige Pfunde loszuwerden. Die spezielle Formel dieser Pastillas wurde entwickelt, um den Stoffwechsel zu steigern und das Hungergefühl zu reduzieren. Dadurch fällt es leichter, eine Diät einzuhalten und erfolgreich abzunehmen.
Viele Menschen schwören auf Reduslim Pastillas, da sie effektiv dabei helfen, Gewicht zu verlieren, ohne dabei auf allzu strenge Diäten angewiesen zu sein. Die Pastillas enthalten natürliche Inhaltsstoffe, die den Körper dabei unterstützen, Fett zu verbrennen und gleichzeitig den Energiehaushalt aufrechtzuerhalten.
Wer also auf der Suche nach einer einfachen und effektiven Möglichkeit ist, Gewicht zu verlieren, sollte Reduslim Pastillas definitiv eine Chance geben. Die positiven Erfahrungsberichte sprechen für sich und zeigen, dass dieses Produkt tatsächlich helfen kann, das Wunschgewicht zu erreichen. Probieren Sie es aus und überzeugen Sie sich selbst von den Vorteilen dieser beliebten Pastillas.
https://reduslim.at/
archive online
5000 euro lenen
http://prednisonest.pro/# canine prednisone 5mg no prescription
http://clomidst.pro/# can i get clomid no prescription
PЕЇjДЌka 17000 KДЌ
prednisone 10mg cost: what is prednisone – prednisone 20mg capsule
купить фальшивые рубли
Понимание сущности и угроз ассоциированных с легализацией кредитных карт способно помочь людям избегать подобных атак и сохранять свои финансовые ресурсы. Обнал (отмывание) кредитных карт — это процесс использования украденных или нелегально добытых кредитных карт для осуществления финансовых транзакций с целью замаскировать их происхождения и предотвратить отслеживание.
Вот некоторые способов, которые могут помочь в избежании обнала кредитных карт:
Защита личной информации: Будьте осторожными в отношении предоставления личных данных, особенно онлайн. Избегайте предоставления номеров карт, кодов безопасности и дополнительных конфиденциальных данных на непроверенных сайтах.
Сильные пароли: Используйте надежные и уникальные пароли для своих банковских аккаунтов и кредитных карт. Регулярно изменяйте пароли.
Контроль транзакций: Регулярно проверяйте выписки по кредитным картам и банковским счетам. Это способствует своевременному выявлению подозрительных транзакций.
Защита от вирусов: Используйте антивирусное программное обеспечение и вносите обновления его регулярно. Это поможет предотвратить вредоносные программы, которые могут быть использованы для изъятия данных.
Осмотрительное поведение в социальных медиа: Будьте осторожными в социальных сетях, избегайте опубликования чувствительной информации, которая может быть использована для взлома вашего аккаунта.
Своевременное уведомление банка: Если вы заметили какие-либо подозрительные операции или утерю карты, сразу свяжитесь с вашим банком для заблокировки карты.
Получение знаний: Будьте внимательными к инновационным подходам мошенничества и обучайтесь тому, как предупреждать их.
Избегая легковерия и принимая меры предосторожности, вы можете минимизировать риск стать жертвой обнала кредитных карт.
airbnb key largo boat https://boatrent.shop/
сериал русская озвучка
фильм
Смотрите сериал Золотая лихорадка. Аляска онлайн Золотая лихорадка 1-14 сезон все серии с русским переводом абсолютно бесплатно.
фильм смотреть
Смотрите сериал Золотая лихорадка. Аляска онлайн Золотая лихорадка смотреть онлайн 1-14 сезон все серии с русским переводом абсолютно бесплатно.
Какие преимущества приводит продвижение сайта через видео-контент
сео продвижение https://www.seo-prodvizhenie-sayta.co.ua/ .
erotica
шаг за шагом инструкция
6. Прицелы с подсветкой для охоты в темное время суток
оптический прицел недорого http://opticheskiy-pricel-odessa.co.ua/ .
http://clomidst.pro/# can you buy clomid without insurance
сериал
http://amoxilst.pro/# amoxicillin 500mg prescription
преимущества и недостатки
10. Защита прицела от воды и пыли: как правильно ухаживать
оптические прицелы https://www.opticheskiy-pricel-odessa.co.ua .
hoki1881
fantastic points altogether, you simply won a emblem
new reader. What would you recommend in regards to your put up that you just made some days ago?
Any sure?
1. Как выбрать правильный прицел для охоты
оптический прицел украина https://www.opticheskiy-pricel-odessa.co.ua/ .
Discover the epitome of luxury living in Dubai with DAMAC Properties’ exquisite range of apartments, villas, and townhouses. Explore exclusive properties for sale in iconic locations like Damac Cavalli Tower Business Bay, Dubai Marina, and Burj Khalifa.
шаг за шагом инструкция
6. Прицелы с подсветкой для охоты в темное время суток
купить оптический прицел https://www.opticheskiy-pricel-odessa.co.ua .
buy amoxicillin over the counter uk: where can i buy amoxicillin without prec – where can i get amoxicillin
domestic cleaning agency in manchester UK
аренда транспорта с водителем https://transferfromto.ru .
Найдите свой идеальный вариант недвижимости в Объединенных Арабских Эмиратах покупка недвижимости в оаэ – лучший сайт, на котором вы найдете все необходимое!
babaeb.xyz
Найдите свой идеальный вариант недвижимости в Объединенных Арабских Эмиратах https://triumf-realty.ru – лучший сайт, на котором вы найдете все необходимое!
cost of prednisone 5mg tablets: prednisone 40 mg price – buy prednisone without prescription
http://prednisonest.pro/# prednisone nz
бонусы фреш казино
https://amoxilst.pro/# amoxicillin 500 mg for sale
фрэш казино
онлайн казино fresh
Traditional futures contracts have a hold, https://eidoo-app.com/, a, when the contract reaches maturity, the investor
needs then purchase or sell the underlying asset at the stated price cost.
обзор
16. Прицелы с автоматической коррекцией при изменении дистанции
оптический прицел цена http://opticheskiy-pricel-odessa.co.ua/ .
fresh casino
казино фреш вход в личный кабинет
бонус на депозит фреш казино
fresh casino регистрация
freshcasino
трансфер новосибирск белокуриха цена http://transfer-novosibirsk-belokurikha.ru/
работа досуг
I think this is one of tthe most vital information for me.
And i am glad reading your article. But wanna remark on some
general things,The wweb site style is wonderful, the articles is really excellent : D.
Good job, cheers
Havve a look at my web blog; 카지노사이트
фреш казино онлайн
Лучший сайт в РФ водка казино
Рекомендую крутой сайт водка казино
fresh casino demo
Оригинальный сайт можете найти здесь водка казино.
cheap amoxicillin 500mg: amoxicillin 500mg cost – where can you buy amoxicillin over the counter
casino fresh
казино фреш регистрация
Рекомендую лучшую БК и казино в России 1win
высокооплачиваемая работа для девушек за границей
boat rentals panama city beach fl https://boatrent.shop/
требуются девушки на высокооплачиваемую работу
amoxicillin 825 mg: how long does it take for amoxicillin to work – where can i buy amoxicillin without prec
https://amoxilst.pro/# amoxicillin 500 coupon
работа в сфере досуга
работа для девушек вакансии
https://prednisonest.pro/# prednisone 100 mg
kantor bola
Kantorbola adalah situs slot gacor terbaik di indonesia , kunjungi situs RTP kantor bola untuk mendapatkan informasi akurat slot dengan rtp diatas 95% . Kunjungi juga link alternatif kami di kantorbola77 dan kantorbola99 .
navЕЎtivte webovou strГЎnku
travelusanews.com
business-exclusive.com
amitriptyline online kaufen
Деньги на карту в течение часа! Досрочное погашение без штрафов! Онлайн одобрение! Без кредитной истории. Без скрытых комиссий. Без справок о доходах займ под залог авто в воронеже
эскорт работа
работа для девушек
Деньги на карту в течение часа! Досрочное погашение без штрафов! Онлайн одобрение! Без кредитной истории. Без скрытых комиссий. Без справок о доходах автоломбард
plan b 10mg
работа для девушек досуг
высокооплачиваемая работа для девушек
работа для девушек с проживанием
интернет магазин кроватей https://www.krovati-moskva11.ru .
Wonderful article! We are linking to this great article on our site.
Keep up the great writing.
Discover the epitome of luxury living at Rashid Yachts and Marina Emaar! Explore an exquisite collection of studios, apartments, and penthouses crafted by renowned developers. Uncover the perfect blend of off-plan and ready properties in an unparalleled waterfront setting. Experience the pinnacle of elegance and seize your dream home today!
Why visiitors still use to read news papers when in this technological world everything is presented on web?
Visit my homepage 카지노사이트
Лучший сайт в РФ по водка казино
Рекомендую крутой сайт на водка казино
In 1969, the movie “http://www.monplawiki.com/link.php?url=https://vip-pussy.com/ Blue” became the first film where intimacy was shown without simulation,
which was widely distributed in United States.
my webpage – http://forum.hybridmlm.io/member.php?action=profile&uid=48497
Грузчики для складских работ в Харькове
заказ грузчиков http://gruzchiki.co.ua/ .
Опытные грузчики в Харькове по низким ценам
перевозка мебели дешево https://www.gruzchiki.co.ua/ .
loans in Oklahoma
ed medications online: cost of ed meds – best online ed pills
manga online
Грузчики Харькова для любых задач и объемов груза
перевозка мебели с грузчиками gruzchiki.co.ua .
Эффективные грузчики для переезда в Харькове
харьков грузоперевозки https://www.gruzchiki.co.ua .
а найти и https://rom.mybb.su/viewtopic.php?id=593#p2431 заказать желаемое несложно.
http://pharmnoprescription.pro/# canada online prescription
cheap prescription drugs online: buy prescription online – buy drugs without prescription
К названным выше принципам, где должна
строиться система независимой сертификации квалификаций,
кладут также ряд, то есть:.
Here is my page: https://stoimost-sertifikata-iso.blogspot.com/2024/01/blog-post_90.html
Для того, чтобы получить эксклюзивные бонусы от букмекера нужны промокоды, которые не всегда просто можно получить. В этой статье разобрано, как получить и использовать промо коды 1хБет и какие бонусы они дают как сделать промокод в 1xbet
hoki 1881
http://edpills.guru/# order ed pills
Для того, чтобы получить эксклюзивные бонусы от букмекера нужны промокоды, которые не всегда просто можно получить. В этой статье разобрано, как получить и использовать промо коды 1хБет и какие бонусы они дают промокод на слоты 1xbet фриспины
hoki 1881
chicagonewsblog.com
alcitynews.com
для достижения оптимальных результатов предпочтительно использовать крем постоянно, тогда полезные соединения будут направляться в.
Here is my homepage – p17571
LГҐn 15000 kr
кроме того мы работаем над доставкой посылок германских, china911 а также почты.
По-настоящему крутое водка казино
Рекомендую сайт в России водка казино
quality prescription drugs canada: meds online no prescription – buying prescription drugs online from canada
Рекомендую этот крутой сайт водка казино
Где найти профессиональных грузчиков в Харькове?
перевозка мебели дешево https://gruzchiki.co.ua/ .
http://pharmnoprescription.pro/# canada pharmacy no prescription
edmeds: ed meds by mail – erectile dysfunction pills for sale
colchicine 20mg
https://onlinepharmacy.cheap/# foreign pharmacy no prescription
сплит система купить каталог http://www.split-sistema11.ru/ .
http://onlinepharmacy.cheap/# online pharmacy discount code
reputable online pharmacy no prescription: canada pharmacy online – cheapest pharmacy prescription drugs
http://pharmnoprescription.pro/# buy medications without prescriptions
Discover luxury apartments and penthouses in the exclusive Le Pont Port De La Mer . Experience the epitome of coastal living with Meraas, as they present incredible units for sale at unbeatable prices. Don’t miss out on this coveted opportunity to make your dream home a reality.
pills no prescription: ordering prescription drugs from canada – online pharmacy no prescription
https://pokrov.mybb.ru/viewtopic.php?id=4458#p77306
http://poselki.animetalk.ru/viewtopic.php?id=25159#p37991
https://blockchainreporter.net/bitcoin-btc-whale-withdraws-6660-btc-from-major-exchange/
Скажіть, будь ласка, у зв’язку з чим ви підставляєте Президента, даєте йому пропозиції щодо прийняття такого указу для кожного щоб.
Also visit my site; https://inventure.com.ua/
http://onlinepharmacy.cheap/# promo code for canadian pharmacy meds
Если вам необходимы пассажирские перевозки на микроавтобусах, вы обратились по нужному адресу. Компания готова предоставить в ваше распоряжение не только целый ряд презентабельных микроавтобусов, но и услуги опытных профессиональных водителей с большим стажем работы Бургас – Чернівці
hello!,I like your writing very a lot! percentage we keep in touch more about your article on AOL?
I need a spcialist in this area to unravel my problem.
May be that’s you! Taking a look forward to look you.
Take a loook at my website: 카지노사이트
http://pharmnoprescription.pro/# canadian prescription drugstore reviews
by the way, he stressed that itoken’s security
service had discovered security threats related to some wallet addresses, which prompted huobi-wallet.io to take quick actions in order to protect user assets.
erectile dysfunction medications online: top rated ed pills – online erectile dysfunction pills
best non prescription online pharmacy: online pharmacies no prescription usa – no prescription online pharmacies
alahomemaster.com
carsnow.net
Как сделать укладку рулонного газона своими руками
рулонный газон с доставкой https://rulonnyygazon177.ru/ .
best porn
Оригинальный сайт по водка казино
https://onlinepharmacy.cheap/# prescription free canadian pharmacy
Рекомендую только этот сайт в России водка казино
החיצון. יתרון נוסף של הוא היכולת לשפר את בריאות מינית ורווחה ולהעיר ולעורר את האזורים הארוגניים בגוף תוך זמן קצר. מספקות מקלט והסכמה. על ידי הגדרת גבולות ברורים אתה יכול לקבל שירות אירוטי הכי טוב ולהנות מהחוויה ללא כל אי נוחות או חוסר ודאות. במקומות כמו נערות ליווי בחיפה
Рекомендую этот сайт в РФ водка казино
https://onlinepharmacy.cheap/# online pharmacy non prescription drugs
מציעות יתרונות אינטימיים רבים מעבר להנאה חושנית אבל כיבוד גבולות ונימוסים דיסקרטיים הם חלק בלתי נפרד בכל פגישה עם במיוחד להקפיד לפנק את עצמך בקסם האירוטי תוך אימוץ ההזדמנות להצעיר את הנפש, הגוף והחושים שלך. בין הצעות רבות בקרב פינוקים למבוגרים, האתר דירות דיסקרטיות באשדוד
Оригинальный сайт найти сможете здесь водка казино.
Почему рулонный газон пользуется популярностью
рулонный газон https://rulonnyygazon177.ru/ .
ואירופאיות. מדור מתאים לכם במאה אחוז, היכנסו ותראו בעצמכם. לאספקת הנאה בעוד שהשירות אינטימי של קשור לעיתים קרובות למפגשים שיטות אלטרנטיביות של קבלת הנאה איכותית, הביקוש להזמנות עולה בשנים האחרונות כי אנשים מחפשים דרכים חדשות ומרגשות להתפנק ולחקור את נערות ליווי בתל אביב
ed online pharmacy: where to buy ed pills – online ed pills
https://telearchaeology.org/TAWiki/index.php/User:DouglasHarkins1
Воздушные шары на заказ с доставкой в Москве и Московской области. Шарики с гелием по низкой цене.
Быстрая доставка шаров днем и ночью.
https://yandex.ru/maps/-/CDF3QG0P
https://dev.to/extralabs/how-to-make-money-from-email-newsletters-tips-for-beginners-5doo
https://ulyanovsk.forumchik.ru/viewtopic.php?id=885#p2810
https://www.freelegal.ch/index.php?title=Soglasno-zakony.ru
https://wiki.lafabriquedelalogistique.fr/Utilisateur:Marlon9804
online pharmacies no prescription: no prescription canadian pharmacy – online pharmacies no prescription
https://wiki.sepertiganetwork.net/index.php/User:JulianShore9937
Какова стоимость установки рулонного газона
рулонный газон москва https://rulonnyygazon177.ru/ .
https://qureshileathers.com/soglasno-zakony-ru/
https://blockchainreporter.net/xrp-price-prediction-500-long-term-outlook-market-analysis/
https://yourgadgets.ru/viewtopic.php?id=2453#p11068
Полный комплекс бухгалтерских услуг для юридических лиц, ООО и ИП. Ведение бухучета, сопровождение и обслуживание бизнеса. Наши бухгалтеры помогут Вам бухгалтерские услуги
дизайн интерьеров
Проблемы реконструкции. Соединение квартир по вертикали и дизайн интерьера кафе горизонтали.
Макетирование. Ведомость отделки.
Look at my blog – дизайн квартиры
советы по строительству
Приглашаем всех гостей смотреть онлайн лучшие сериалы 2023 года
бесплатно в хорошем качестве FullHD все сезоны и серии
на смартфоне, компьютере, SmartTV на нашем сайте
без регистрации и смс. zserial2023.club
Приглашаем всех гостей смотреть онлайн лучшие сериалы 2023 года
бесплатно в хорошем качестве FullHD все сезоны и серии
на смартфоне, компьютере, SmartTV на нашем сайте
без регистрации и смс. Зарубежные сериалы 2023
methotrexate without a doctor prescription
https://extralabs.github.io/
Приглашаем всех гостей смотреть онлайн лучшие сериалы 2023 года
бесплатно в хорошем качестве FullHD все сезоны и серии
на смартфоне, компьютере, SmartTV на нашем сайте
без регистрации и смс. сериалы 2023 смотреть онлайн
Приглашаем всех гостей смотреть онлайн лучшие сериалы 2023 года
бесплатно в хорошем качестве FullHD все сезоны и серии
на смартфоне, компьютере, SmartTV на нашем сайте
без регистрации и смс. лучшие зарубежные сериалы 2023
Не советую данный покеррум для беспристрастной игры, когда игрок не фиш конечно, unioncityhvacpros.com которому
и станет все доезжать!
Indulge in opulent living with ultra-luxury villas in Lanai Island villas. Majid Al Futtaim presents affordable units for sale, immersing you in sublime comfort and elegance.
india online pharmacy: india pharmacy mail order – online pharmacy india
В современной промышленности важное значение имеет испытательное оборудование, позволяющее оценивать параметры изделий на различных этапах производства. Один из ключевых видов такого оборудования — вибростенды, предназначенные для испытания компонентов и сборок на устойчивость к воздействию механических колебаний вибростенды для испытаний
Porn
Standard Price for VIP- membership for 1 Week VIP Membership is 0.0014 BTC, You will do send payment to BTC address 1KEY1iKrdLQCUMFMeK4FEZXiedDris7uGd
Discounted price may be different from 0.00075 to 0.00138 BTC,
that is why follow to all announces published in our Public channel!
crypto signals
Standard Price for VIP- membership for 1 Week VIP Membership is 0.0014 BTC, You will do send payment to BTC address 1KEY1iKrdLQCUMFMeK4FEZXiedDris7uGd
Discounted price may be different from 0.00075 to 0.00138 BTC,
that is why follow to all announces published in our Public channel!
crypto pump Binance
Standard Price for VIP- membership for 1 Week VIP Membership is 0.0014 BTC, You will do send payment to BTC address 1KEY1iKrdLQCUMFMeK4FEZXiedDris7uGd
Discounted price may be different from 0.00075 to 0.00138 BTC,
that is why follow to all announces published in our Public channel!
coin price prediction signals
mail order pharmacy india: п»їlegitimate online pharmacies india – indian pharmacies safe
I really love to read such an excellent article. Helpful article. Hello Administ .
Standard Price for VIP- membership for 1 Week VIP Membership is 0.0014 BTC, You will do send payment to BTC address 1KEY1iKrdLQCUMFMeK4FEZXiedDris7uGd
Discounted price may be different from 0.00075 to 0.00138 BTC,
that is why follow to all announces published in our Public channel!
price prediction Binance
Truly plenty of valuable tips.
Standard Price for VIP- membership for 1 Week VIP Membership is 0.0014 BTC, You will do send payment to BTC address 1KEY1iKrdLQCUMFMeK4FEZXiedDris7uGd
Discounted price may be different from 0.00075 to 0.00138 BTC,
that is why follow to all announces published in our Public channel!
trading signals
fluvoxamine ohne rezept kaufen
смотреть сериал
לכל אחד שמחפש חוויה הכי מפנקת! אמנות הפינוק האירוטי של נערות שמחכות לכם ב דורשת מיומנות, רגישות והבנה מעמיקה של האזורים אינטימית הכי עמוקה! בהזמנה לבתי מלון בילוי דיסקרטי מפנק במלון או בביתך הפרטי עם מספק שער להנאה אירוטית חושנית ותשוקה מעבר נערות ליווי בחיפה
смотреть фильм
Immerse yourself in the captivating realm of online casinos Kenya, where fresh games and instant payouts reign supreme.
фильм смотреть
фильм смотреть
https://mexicanpharm.online/# medication from mexico pharmacy
האירוטיות שלך ולאמץ את הרצונות החושניים. עם מוסיקה רכה, ריחות מרגיעים ותאורה עמומה יוצרים אווירה של רוגע ואינטימיות תמיד פתוחות אישיות של כל אחד. נערות הסקסיות ביותר מתמחות ביצירת חוויה אירוטית מפוארת וחושנית לגברים ומשאירות אותם כמהים לעוד. תמיד היו דירות דיסקרטיות באשדוד
buying from online mexican pharmacy: buying from online mexican pharmacy – reputable mexican pharmacies online
מרכז המַרכֵּז למענה גַּרְגִּירֵים כיוונים (Telegrass), קָרוֹוּעַ גם בשמות “טלגראס” או “גַּרְגִּירֵים כיוונים”, הם אתר סוֹפֵק מידע, לינקים, קישורים, מדריכים והסברים בנושאי קנאביס בתוך הארץ. באמצעות האתר, משתמשים יכולים למצוא את כל הקישורים המעודכנים עבור ערוצים מומלצים ופעילים בטלגראס כיוונים בכל רחבי הארץ.
טלגראס כיוונים הוא אתר ובוט בתוך פלטפורמת טלגראס, מספק דרכי תקשורת ושירותים נפרדים בתחום רכישת קנאביס וקשורים. באמצעות הבוט, המשתמשים יכולים לבצע מגוון פעולות בקשר לרכישת קנאביס ולשירותים נוספים, תוך כדי תקשורת עם מערכת אוטומטית המבצעת את הפעולות בצורה חכמה ומהירה.
בוט הטלגראס (Telegrass Bot) מציע מגוון פעולות שימושיות למשתמשים: שליחה קנאביס: בצע הזמנה דרך הבוט על ידי בחירת סוגי הקנאביס, כמות וכתובת למשלוח.
הוראות ותמיכה: קבל מידע על המוצרים והשירותים, תמיכה טכנית ותשובות לשאלות שונות.
בחינה מלאי: בדוק את המלאי הזמין של קנאביס ובצע הזמנה תוך כדי הקשת הבדיקה.
הצבת ביקורות: הוסף ביקורות ודירוגים למוצרים שרכשת, כדי לעזור למשתמשים אחרים.
הכנסת מוצרים חדשים: הוסף מוצרים חדשים לפלטפורמה והצג אותם למשתמשים.
בקיצור, בוט הטלגראס הוא כלי חשוב ונוח שמקל על השימוש והתקשורת בנושאי קנאביס, מאפשר מגוון פעולות שונות ומספק מידע ותמיכה למשתמשים.
Prestito di 700 euro
crestor 50mg
ttbslot.com
짧은 시간에 30마리 이상의 소가 시산 근처에서 설명할 수 없이 죽었습니다.
Рекомендую в России имеено их водка казино
הביצועים המיניים שלהם. שילוב של מגע מיומן, אווירה רומנטית נעימה והנאה מוגברת יכול להוביל לשחרור מתח, לעלייה בביטחון העצמי תוך מתן סביבה מרגיעה ואינטימית. תמיד מספקות לכולם הפגת לחצים, משפרות בריאות המינית ומקדמות את הרווחה הנורמטיבית. נערות יפות של נערות ליווי בתל אביב
Рекомендую только этот сайт в РФ водка казино
prestamo 7000 euros
Официальный сайт сможете найти здесь водка казино.
1win 1win 1win 1win
http://indianpharm.shop/# indian pharmacy online
buy medicines online in india: Online medicine order – п»їlegitimate online pharmacies india
חושנית ופינוק אולטימטיבי ותנו לקסם הלוהט להסיע אתכם למצב של אושר טהור. חשוב לציין כי שירותים של מתאימות גם לגברים בודדים וגם את הרצונות והגבולות שלך בבירור. דיאלוג פתוח וכנה בטלפון עוד לפני ההגעה מבטיח ששני הצדדים נמצאים באותו מצב ומטפחים סביבה של אמון דירות דיסקרטיות באשקלון
LГҐn 500000 kr
אינטימית הכי עמוקה! בהזמנה לבתי מלון בילוי דיסקרטי מפנק במלון או בביתך הפרטי עם מספק שער להנאה אירוטית חושנית ותשוקה מעבר האירוטית הלא נגמרת אף פעם. זו עיר שלא ישנה לעולם, שבה אנשים מכל תחומי החיים מתאחדים כדי לחוות את הנאות החושניות ביותר בעולם. כאן דירות דיסקרטיות בבאר שבע
Elevate your gaming experience with online casinos Kenya, where innovative titles and swift payouts are the norm.
https://canadianpharm.guru/# canadian online pharmacy
Рейлінги, бильця і ламінат повинні відповідати нормам по навантаженнях і сил.
Also visit my web site – https://okna-atlant.com.ua/otdelka-otkosov/
canadianpharmacyworld: canadian pharmacy in canada – canadian drug pharmacy
You mentioned it effectively!
Look into my blog :: https://illplaywithyou.com/
Xxx site
взять в аренду звуковое оборудование https://www.zvukovoe-oborudovanie11.ru .
https://canadianpharm.guru/# canadianpharmacyworld com
http://canadianpharm.guru/# canadian pharmacy prices
pЕ™eДЌГst recenzi
This website was… how do I say it? Relevant!!
Finally I have found something which helped
me. Thanks a lot!
My web blog: 카지노사이트
buying prescription drugs in mexico: reputable mexican pharmacies online – mexican pharmacy
Рекомендую в России имеено этот водка казино
עם דגש על הנאה לפני הזמנת פגישה אירוטית בלתי נשכחת באמת עם דוגמניות אמיתיות של מומלץ לעשות קצת מחקר כדי להבטיח שתבחר מקום מכובד לזוגות. זוגות שחוו פינוקים כאלה למבוגרים מתארים אותם לעתים קרובות כחוויה הכי טרנספורמטיבית ולוהטת. והסביבה בעולם המהיר של היום דירות דיסקרטיות באשקלון
Рекомендую в РФ только этот сайт водка казино
Porn
free porn
https://mexicanpharm.online/# mexican online pharmacies prescription drugs
אירוטי לגברים ועוזרות להתמכר לרצונות שלהם ולגלות תחומים חדשים של הנאה לוהטת בלתי נגמרת. קטגוריה עם מודעות פרטיות. לשחרור האירוטיות שלך ולאמץ את הרצונות החושניים. עם מוסיקה רכה, ריחות מרגיעים ותאורה עמומה יוצרים אווירה של רוגע ואינטימיות תמיד פתוחות דירות דיסקרטיות בתל אביב
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das beim Abnehmen helfen soll. Viele Menschen suchen nach Reduslim στα φαρμακεια τιμη, um den besten Preis für das Produkt zu finden. Es ist wichtig zu beachten, dass Reduslim nur den gewünschten Effekt erzielt, wenn es in Kombination mit einer gesunden Ernährung und ausreichend Bewegung eingenommen wird.
Das Produkt enthält natürliche Inhaltsstoffe wie Grüntee-Extrakt und Garcinia Cambogia, die den Stoffwechsel ankurbeln und die Fettverbrennung beschleunigen sollen. Reduslim kann helfen, Heißhungerattacken zu reduzieren und das Sättigungsgefühl zu erhöhen, was wiederum zu einem langfristigen Gewichtsverlust führen kann.
Bevor man jedoch Reduslim einnimmt, sollte man sicherstellen, dass man keine bekannten Allergien gegen die enthaltenen Inhaltsstoffe hat. Es ist auch ratsam, vor der Einnahme einen Arzt zu konsultieren, um sicherzustellen, dass das Produkt fГјr den individuellen Gebrauch geeignet ist.
Insgesamt kann Reduslim eine unterstützende Rolle beim Abnehmen spielen, sollte aber nicht als Ersatz für eine ausgewogene Ernährung und regelmäßige Sportaktivitäten angesehen werden. Wer nach Reduslim sucht, sollte darauf achten, seriöse Quellen zu wählen, um sicherzustellen, dass das Produkt von hoher Qualität ist.
https://reduslim.at/
Официальный сайт сможете найти тут водка казино.
http://indianpharm.shop/# online shopping pharmacy india
Reduslim ist ein beliebtes Nahrungsergänzungsmittel zur Gewichtsreduktion, das viele Menschen interessiert. Doch was ist eigentlich in Reduslim drin? Die natürlichen Inhaltsstoffe machen das Produkt besonders wirkungsvoll. Grüner Tee Extrakt regt den Stoffwechsel an und fördert die Fettverbrennung. Garcinia Cambogia Blockiert die Fettaufnahme und unterdrückt das Hungergefühl. Koffein sorgt für einen Energieschub und erhöht die Ausdauer. Zudem enthält Reduslim Vitamin B12, das den Energiestoffwechsel unterstützt. Alles in allem ist Reduslim eine effektive Möglichkeit, um gesund und effektiv abzunehmen.
https://reduslim.at/
Haben Sie schon von dem neuen Schlankheitsmittel gehört, das gerade die Welt im Sturm erobert? Es handelt sich um Reduslim, das speziell entwickelte Nahrungsergänzungsmittel, das Ihnen helfen soll, schnell und einfach Gewicht zu verlieren. Aber funktioniert es wirklich? Viele Menschen haben bereits den Test Reduslim gemacht und sind von den Ergebnissen begeistert. Durch die einzigartige Kombination von natürlichen Inhaltsstoffen hilft Reduslim dabei, den Stoffwechsel anzukurbeln und unerwünschte Pfunde loszuwerden. Wenn auch Sie sich von der Wirkung überzeugen möchten, sollten Sie jetzt den Test Reduslim wagen und schon bald Ihre Traumfigur erreichen. Werden auch Sie Teil der Erfolgsgeschichte und starten Sie noch heute Ihren Weg zum Wunschgewicht mit Reduslim!
https://reduslim.at/
Всем рекомендую официальный сайт 1win
Die Stiftung Warentest hat das Abnehmprodukt Reduslim genauer unter die Lupe genommen und ihre Ergebnisse veröffentlicht. Dabei wurde festgestellt, dass Reduslim ein effektives Mittel zur Gewichtsreduktion sein kann. Die Inhaltsstoffe des Produkts wurden als unbedenklich eingestuft und zeigten eine gute Wirksamkeit im Test.
Die Stiftung Warentest lobte Reduslim auch für seine einfache Anwendung und die schnellen Ergebnisse, die viele Anwender bereits nach kurzer Zeit erzielten. Zudem wurde das Abnehmprodukt als gut verträglich bewertet und führte bei den Probanden zu keinen unerwünschten Nebenwirkungen.
Wer also auf der Suche nach einem wirksamen und verträglichen Abnehmprodukt ist, sollte sich das Ergebnis der Stiftung Warentest zu Reduslim nicht entgehen lassen. Denn dieses Produkt könnte die Lösung für alle sein, die auf gesunde Weise und ohne großen Aufwand Gewicht verlieren möchten.
https://reduslim.at/
Wenn es um das Thema Gewichtsverlust geht, ist es wichtig, dass man das richtige Produkt findet, das zu einem passt. Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das dabei helfen soll, überschüssiges Fett zu verbrennen und den Stoffwechsel zu unterstützen. Doch was passiert, wenn man mit dem Produkt nicht zufrieden ist? Zum Glück bietet Reduslim ein großzügiges Rückgaberecht an.
Das Rückgaberecht von Reduslim ermöglicht es den Kunden, das Produkt innerhalb einer bestimmten Frist zurückzugeben, wenn sie nicht zufrieden sind. Dies gibt den Kunden die Sicherheit, dass sie ihr Geld zurückbekommen können, wenn das Produkt nicht ihren Erwartungen entspricht. Das zeugt von der Zuversicht des Unternehmens in die Wirksamkeit des Produkts und schafft Vertrauen bei den Kunden.
Das Rückgaberecht von Reduslim ist einfach und unkompliziert. Kunden, die mit dem Produkt nicht zufrieden sind, können sich einfach an den Kundenservice wenden und die Rücksendung des Produkts arrangieren. Nachdem das Produkt retourniert wurde, erhält der Kunde sein Geld zurück. Dies zeigt, dass Reduslim großen Wert auf Kundenzufriedenheit legt und sich um das Wohlergehen seiner Kunden kümmert.
Insgesamt ist das RГјckgaberecht von Reduslim ein groГџer Pluspunkt fГјr das Unternehmen. Es zeigt, dass Reduslim Vertrauen in sein Produkt hat und dass die Kundenzufriedenheit an erster Stelle steht. FГјr die Verbraucher ist dies ein beruhigender Gedanke und schafft eine gute Basis fГјr den Kauf von Reduslim. Wer also nach einem effektiven Gewichtsverlustprodukt sucht, das mit einem groГџzГјgigen RГјckgaberecht ausgestattet ist, sollte sich fГјr Reduslim entscheiden.
https://reduslim.at/
אינטימי איכותי משמש במשך מאות שנים לקידום רווחה פיזית ורגשית. גאות להציע אווירה בטוחה, נקייה ונעימה עבור לקוחותיהן. נערות הכי חושנית ופינוק אולטימטיבי ותנו לקסם הלוהט להסיע אתכם למצב של אושר טהור. חשוב לציין כי שירותים של מתאימות גם לגברים בודדים וגם דירות דיסקרטיות בבאר שבע
Spot on with this write-up, I seriously believe
this website needs a great deal more attention. I’ll probably bee back again to see more, thanks for the info!
my webpage :: 카지노사이트
Porn
mexican drugstore online: buying prescription drugs in mexico – mexico pharmacy
możesz spróbować tutaj
italy-cars.com
dalycitynewspaper.com
http://mexicanpharm.online/# buying prescription drugs in mexico
bananchik.top
https://eacco.ph/documents/index.php/Argumenti.ru
https://moregogiga.com/community/profile/kathiv385622538/
http://www.jic-magic.com/question/argumenti-ru/
Рекомендую в России этот сайт водка казино
Рекомендую настоящий сайт водка казино
https://pipms.wiki/User:SabrinaAutry
п»їbest mexican online pharmacies: mexican rx online – mexican pharmaceuticals online
https://pharmacynoprescription.pro/# prescription meds from canada
Всем рекомендую БК 1вин, официальный сайт 1win
There is perceptibly a lot to know about this. I believe you made some good points in features also.
Have a look at my website: https://pipewiki.org/app/index.php/Going_To_Trim_Town_Co_-_Meath_Ireland
https://cl-system.jp/question/argumenti-ru/
Some truly interesting info, well written and broadly speaking user pleasant.
Do you want hot phone sex and a little more? Then you should get to know the combination of both! Phone sex with live cams offers you exactly what you need for hot chat online on the Internet. Horny women on the phone who have nothing else on their minds but to have fun with you in front of the cam. There are always horny women online waiting for your call and once they have you on the line they also switch on their cam.
http://labautomationwiki.com/index.php/User:IsmaelBardsley
vykup-avto-v-ufe.ru
https://glhwar3.com/forums/users/basil51y809785/
https://wamainuk.com/question/argumenti-ru/
לזוגות. זוגות שחוו פינוקים כאלה למבוגרים מתארים אותם לעתים קרובות כחוויה הכי טרנספורמטיבית ולוהטת. והסביבה בעולם המהיר של היום ורצוי להזמין שירותי לא ברגע האחרון. לדוגמה, אם אתה רוצה להיפגש עם צעירה יפיפיה בשעות הלילה, עדיף לבצע הזמנה כמה שעות לפני כי אז דירות דיסקרטיות בתל אביב
1вин казино
LГҐn 7000 kr
Мы предлагаем на выбор разный номинал и наполнение сертификатов. Это может быть катание как отдельно на снегоходе и квадроцикле, так и обе активности вместе. Количество техники, длительность проката и стоимость сертификата не ограничены катание на квадроциклах в подмосковье подарочный сертификат
http://canadianpharm.guru/# canadian world pharmacy
buy medications online no prescription: buy prescription online – online pharmacies no prescription
bananchik.top
Рекомендую в России настоящий сайт 1win
Рекомендую настоящий сайт в РФ 1win
https://adzan.online/
Всем рекомендую БК 1вин, это их сайт 1win
частный seo оптимизатор http://www.prodvizhenie-sajtov15.ru/ .
noroxin online-apotheke kaufen
http://indianpharm.shop/# reputable indian pharmacies
saada lisätietoja
https://northerngraceyouthcamp.org/wiki/index.php/User:ArletteMasterson
https://weakfantasy.de/index.php/Ofkleasing.ru
https://plamosoku.com/enjyo/index.php?title=Basova-photo.ru
https://chessdatabase.science/wiki/User:HortenseChisholm
https://northerngraceyouthcamp.org/wiki/index.php/Ek-x.ru
http://idra.world/question/ofkleasing-ru/
onlinecanadianpharmacy: best canadian online pharmacy – canadian pharmacy ltd
http://urbino.fh-joanneum.at/trials/index.php/User:SabrinaJxl
https://dokuwiki.stream/wiki/Fotosalon
https://procesal.cl/index.php?title=Ek-x.ru
https://wikidot.win/wiki/E-k-h.ru
http://embeddedwiki.cs.aau.dk/wiki/User:CharlaBlackett
Дизайнерские радиаторы отопления. Представить современный дом без радиатора очень трудно, особенно в осенний и зимний сезон, когда так хочется тепла и уюта https://radiators-teplo.github.io/
https://villagewebcompany.net/index.php/User:ClayPerin75344
http://www.diywiki.org/index.php/User:FreemanTherry30
https://xdpascal.com/index.php/User:LupeFuller689
https://nerdgaming.science/wiki/E-k-h.ru
https://www.lookali.de/community/profile/thaobisbee93329/
http://ffikki.tarwood.ru/index.php?title=Basova-photo.ru
https://wikidot.win/wiki/User:FawnWishart3726
https://urduwiki.in/index.php/User:TarenDeen42
http://ffikki.tarwood.ru/index.php?title=E-k-h.ru
https://telugusaahityam.com/User:ChristyStuber27
http://www.askclu.com/index.php/Basova-photo.ru
https://pattern-wiki.win/wiki/User:LawannaRentoul
http://www.springst.melbourne/index.php/User:KitLink742
https://biowiki.clinomics.com/index.php/User:StephenClary4
https://blackhat-out.fr/level2/index.php/Fotosalon
rg777
RG Trang chủ là tên gọi của trang web chính thức cho Nhà Cái RG777 Casino. Địa chỉ trực tuyến của nó là vnrg5269.com, nơi cung cấp thông tin toàn diện về các dịch vụ và sản phẩm cá cược của họ.
https://able.extralifestudios.com/wiki/index.php/User:BurtonPopp76
http://www.diywiki.org/index.php/User:DustySpinks229
https://www.mibtec.it/wiki/index.php?title=Ofkleasing.ru
http://pharmacynoprescription.pro/# canada pharmacies online prescriptions
http://www.urowiki.co.uk/index.php?title=User:JorgFroggatt741
http://ffikki.tarwood.ru/index.php?title=%D0%A3%D1%87%D0%B0%D1%81%D1%82%D0%BD%D0%B8%D0%BA:ClaudiaMetcalfe
https://wikidot.win/wiki/User:RoyceHepp414
http://canadianpharm.guru/# canadapharmacyonline legit
Сервис онлайн заказа классической и широкоформатной фотопечати на фотобумаге, холсте, акварельной и плакатной бумаге, печать фотографий печать фото большого формата
verkkosivusto
Рекомендую в России именно этот оригинальный сайт 1win
Рекомендую оригинальный сайт в РФ 1win
hoki1881
Привет, игровые друзья! Я не могу проигнорировать и не поделиться своими чувствами о гемблинг-доме “pin up“. Это место, где я отыскал все, которое потребуется для идеального отдыха: разносторонность игр, большие бонусы и скоростные выплаты. Но что меня в особенности удивило – это атмосфера дружелюбия и поддержки, которую создают администраторы и зрители. Присоединяйтесь к игровому дому “пинап” и войдите в мирочек развлечений и удовольствия прямо сейчас!
https://adzan.online/
reputable indian pharmacies: Online medicine order – online shopping pharmacy india
It’s very straightforward to find out anny matter on web as compared to books, as I found this piece of writig at this
web page.
my webpage: 카지노사이트
ttbslot.com
Liu Jie는 “아버지가 왜 그렇게 말했습니까? “라고 말하기 전에 오랫동안 침묵을 지켰습니다.
Your style is really unique compared to other folks I’ve
read stuff from. Thanks for posting when you have the opportunity,
Guess I’ll just bookmark this blog.
http://pharmacynoprescription.pro/# buy prescription drugs online without doctor
Ингалятор небулайзер компрессорный с маской
механизированная штукатурка м2 http://www.mekhanizirovannaya-shtukaturka11.ru/ .
гелиокс процедура
профессиональный небулайзер
ингалятор для физиотерапии
Изготовление стильных фотокниг недорого. Быстрая и качественная печать фотобуков на заказ. Создавайте фотоальбомы онлайн с помощью простого и бесплатного фоторедактора фотокнига с рождения
гелиокс терапия показания и противопоказания
Лучший в России сайт букмекер 1win
LГҐna 60000 kr
Промокод 1xBet на сегодня и бесплатно. Промокоды 1хбет 2024 требуется использовать те, которые предоставят игрокам самые лучшие бонусы. Каждый из них позволяет увеличить первый депозит в 2 раза, максимальная сумма увеличения – 100 долларов. Большое количество промокодов — одна из причин того, что на сайте регистрируется огромное количество новых игроков каждый день. На данный момент их количество превышает пятьсот тысяч уникальных пользователей каждый день. Действующие промокоды позволяют увеличить размер приветственных баллов до 32 500 рублей. Для этого нужно лишь активировать при регистрации имеющийся код, скопировав его в соответствующее поле. Букмекерская контора 1ХБет является одной из самых влиятельных на рынке игорного бизнеса в России и не нуждается в особом представлении. Впрочем, букмекер продолжает держать статус одного из самых щедрых и предлагает своим клиентам воспользоваться промокодами для халявы, – более подробно в этом материале http://vidpochynok.net/inc/cli/promokod-1xbet.html.
Всем рекомендую Букмеерскую контору 1win
77 canadian pharmacy: canadian pharmacy – pharmacy canadian superstore
https://canadianpharm.guru/# rate canadian pharmacies
casino crypto withdraw
Klick jetzt
casino crypto deposit
https://авизо72.рф/
crypto casino
автоадвокат автоюрист
Payday loans in Virginia
автоюрист цены на услуги
помощь автоюриста консультация
консультация автоюриста по дтп
московские адвокаты по гражданским делам
автоюрист москва цены на услуги
The inclusion of what is stromectol 3 mg used for, containing ivermectin, in national and international treatment guidelines reflects its status as a cornerstone therapy for parasitic infections. These evidence-based recommendations guide healthcare providers in the safe and effective use of ivermectin, ensuring optimal outcomes for patients while minimizing the risk of adverse effects and drug resistance.
практикующий юрист по гражданским делам
юридические услуги автоюриста
адвокат по гражданским делам
помощь автоюриста консультация
LГҐn 150000
хороший автоюрист консультация
Embrace the adrenaline rush of online casinos Kenya, where fresh gaming options and swift payouts are the order of the day.
https://pharmacynoprescription.pro/# buying prescription medications online
aceon 10mg
Elevate your gaming experience with online casinos Kenya, where novel titles and swift payouts are the norm.
https://mexicanpharm.online/# mexican drugstore online
online shopping pharmacy india: online shopping pharmacy india – best india pharmacy
https://djchs.co.kr/bbs/board.php?bo_table=qna&wr_id=105350
https://mediawiki.volunteersguild.org/index.php?title=User:Franchesca10I
https://fbf.ftu.edu.vn/en/?dwqa-question=online-slots-have-become-a-popular-choice-for-many-gamblers-looking-to-strike-it-big-from-the-comfort-of-their-own-homes
chicago-job.com
http://dhbs.co.kr/bbs/board.php?bo_table=free&wr_id=269530
http://center.kosin.ac.kr/cems//bbs/board.php?bo_table=free&wr_id=299309
http://cctvnara.net/bbs/board.php?bo_table=free&wr_id=1355
livechinanews.com
http://princevideovault.com/index.php?title=Benutzer:BessAea4073
http://postmaster.cameseeing.com/bbs/board.php?bo_table=ex_03&wr_id=522433
http://namhaehappy.com/bbs/board.php?bo_table=free&wr_id=35000
http://locomodu.com/bbs/board.php?bo_table=free&wr_id=20246
http://www.donginws.co.kr/bbs/board.php?bo_table=free&wr_id=2353784
http://www.kbusa.co.kr/bbs/board.php?bo_table=free&wr_id=161302
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
http://www.cwpass.co.kr/ver2/bbs/board.php?bo_table=free&wr_id=348907
http://www.east24.co.kr/bbs/board.php?bo_table=free&wr_id=301311
Заказать диссертацию онлайн. Комплексная поддержка соискателей по подготовке НИР любой сложности под ключ. Выполнение – в сумме за 120 дней по гуманитарным дисциплинам, и в сумме 150-180 дней по техническим дисциплинам рефераты на заказ
http://yninfo.co.kr/board/bbs/board.php?bo_table=free&wr_id=27369
https://digidex.net/Usuario:JordanLamaro17
http://xwiki.club/index.php?title=User:KamGage53102
Thank you for content. Area rugs and online home decor store. Hello Administ . 国产线播放免费人成视频播放
credito 4000 euros
Лучший сайт букмекера в России 1win
Экзистенция скрытых интернет-площадок – это событие, что порождает большой внимание и дискуссии во сегодняшнем сообществе. Темная часть интернета, или скрытая сфера интернета, представляет собой приватную сеть, доступные лишь через соответствующие софт и конфигурации, гарантирующие неузнаваемость участников. По данной данной подпольной инфраструктуре лежат скрытые интернет-площадки – веб-площадки, где бы торговля разносторонние товары а сервисы, наиболее часто противоправного степени.
В подпольных рынках можно отыскать самые разные вещи: наркотики, стрелковое оружие, украденные данные, уязвимые аккаунты, подделки и многое другое. Такие же площадки часто притягивают интерес как правонарушителей, так и обычных участников, стремящихся обходить право либо доступить к вещам а услуговым предложениям, какие на обычном интернете были бы в не доступны.
Тем не менее важно помнить, как активность по теневых электронных базарах является неправомерный специфику и имеет возможность повлечь за собой важные юридические нормы санкции. Органы правопорядка настойчиво борются с этими маркетами, однако из-за скрытности темной стороны интернета это далеко не перманентно просто.
Поэтому, экзистенция даркнет-маркетов составляет сущностью, и все же они пребывают территорией важных рисков как и для таковых субъектов, и для таких сообщества во в целом и целом.
Рекомендую настоящую Букмекерскую контору 1win
Тор веб-навигатор – это особый браузер, который задуман для обеспечения анонимности и устойчивости в интернете. Он построен на сети Тор (The Onion Router), позволяющая участникам пересылать данными по распределенную сеть серверов, что создает трудным подслушивание их поступков и установление их локации.
Основополагающая функция Тор браузера состоит в его умении направлять интернет-трафик посредством несколько пунктов сети Тор, каждый шифрует информацию перед следующему за ним узлу. Это обеспечивает массу слоев (поэтому и наименование “луковая маршрутизация” – “The Onion Router”), что создает почти недостижимым отслеживание и установление пользователей.
Тор браузер периодически используется для преодоления цензуры в территориях, где запрещен доступ к определенным веб-сайтам и сервисам. Он также дает возможность пользователям обеспечить конфиденциальность своих онлайн-действий, например просмотр веб-сайтов, коммуникация в чатах и отправка электронной почты, избегая отслеживания и мониторинга со стороны интернет-провайдеров, государственных агентств и киберпреступников.
Однако рекомендуется учитывать, что Тор браузер не обеспечивает полной конфиденциальности и безопасности, и его использование может быть привязано с угрозой доступа к неправомерным контенту или деятельности. Также возможно замедление скорости интернет-соединения вследствие
Регистрация в букмекерской конторе BetBoom открывает перед вами увлекательный мир спортивных ставок и возможность заработка на удаче и знании спорта. Процесс регистрации на официальном сайте BetBoom прост и удобен: вам нужно заполнить всего несколько обязательных полей, подтвердить свои данные и выбрать удобный способ пополнения счета. Подробная инструкция – https://t.me/s/registraciya_betboom_ru
https://mexicanpharm.online/# mexican pharmacy
даркнет площадки
Теневые площадки, а также темные рынки, представлены интернет-платформы, доступные исключительно путем скрытую сеть – часть интернета, недоступная для стандартных поисковых машин. Такие платформы допускают субъектам торговать разными товарами и послугами, в большинстве случаев противоправного типа, такими как наркотики, стрелковое оружие, похищенная информация, фальшивые документы а другие запретные или незаконные продуктовые товары или послуги.
Темные площадки предоставляют неузнаваемость их собственных пользователей за счет применения особенных программного обеспечения и параметров, например The Onion Routing, какие скрывают IP-адреса а маршрутизируют интернет-трафик через различные узловые соединения, делая трудным прослеживание активности правоохранительными органами.
Эти площадки время от времени становятся целью интереса правоохранительных органов, какие сражаются с ними в рамках борьбе против киберпреступностью и неправомерной торговлей.
тор даркнет
Тор скрытая сеть – это часть интернета, такая, которая деи?ствует поверх обыкновеннои? сети, но не доступна для прямого допуска через обыкновенные браузеры, например Google Chrome или Mozilla Firefox. Для входа к этому сети необходимо специальное программное обеспечение, вроде, Tor Browser, которыи? обеспечивает секретность и защиту пользователеи?.
Основнои? принцип работы Тор даркнета основан на использовании путеи? через разные узлы, которые кодируют и перенаправляют трафик, вызывая сложным отслеживание его источника. Это создает скрытность для пользователеи?, скрывая их реальные IP-адреса и местоположение.
Тор даркнет включает разнообразные плеи?сы, включая веб-саи?ты, форумы, рынки, блоги и другие онлаи?н-ресурсы. Некоторые из подобных ресурсов могут быть неприступны или запрещены в обычнои? сети, что вызывает Тор даркнет полем для подачи информациеи? и услугами, включая вещи и услуги, которые могут быть противозаконными.
Хотя Тор даркнет используется несколькими людьми для пересечения цензуры или защиты частнои? жизни, он также превращается платформои? для разнообразных противозаконных поступков, таких как бартер наркотиками, оружием, кража личных данных, предоставление услуг хакеров и остальные уголовные действия.
Важно осознавать, что использование Тор даркнета не всегда законно и может включать в себя серьезные риски для безопасности и правомочности.
https://beton-vpodolsk.ru/
сериал все серии
смотреть
Your means of explaining everything in this article is genuinely pleasant, all can effortlessly be aware of it, Thanks a lot.
смотреть
reputable indian pharmacies: reputable indian online pharmacy – world pharmacy india
сериал все серии
hoki 1881
Reduslim opiniones Amazon: Was sagen die Kunden?
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das auf Amazon erhältlich ist. Viele Menschen schwören auf die positive Wirkung des Produkts und teilen ihre Meinungen und Erfahrungen auf der Plattform. Die Reduslim opiniones Amazon sind durchweg positiv und bestätigen die Wirksamkeit des Supplements.
Die Kunden loben vor allem die schnellen Ergebnisse, die mit Reduslim erzielt werden können. Viele berichten von einer deutlichen Gewichtsabnahme innerhalb kurzer Zeit und sind begeistert von der einfachen Anwendung. Zudem wird die hohe Qualität der Inhaltsstoffe gelobt, die zu einer effektiven Fettverbrennung beitragen.
Aber auch die Natürlichkeit des Produkts wird von den Kunden geschätzt. Reduslim enthält keine künstlichen Zusatzstoffe oder Chemikalien und ist somit gut verträglich für den Körper. Die positiven Reduslim opiniones Amazon bestätigen, dass das Nahrungsergänzungsmittel eine gute Wahl für alle ist, die auf gesunde Weise abnehmen möchten.
Insgesamt zeigt sich, dass Reduslim sowohl bei den Kunden als auch in den Reduslim opiniones Amazon sehr beliebt ist. Wer also nach einem effektiven und natГјrlichen Produkt zur Gewichtsabnahme sucht, sollte sich die positiven Erfahrungen der Kunden auf Amazon nicht entgehen lassen.
https://reduslim.at/
Die Suche nach dem richtigen Weg, um Gewicht zu verlieren, kann oft frustrierend sein. Eine Möglichkeit, die immer beliebter wird, ist die Verwendung von Reduslim, einem natürlichen Nahrungsergänzungsmittel, das in Apotheken erhältlich ist.
Reduslim wird oft als Wundermittel bezeichnet, da es helfen kann, den Stoffwechsel zu steigern und somit das Abnehmen zu unterstützen. Durch die Einnahme der Kapseln wird der Körper darin unterstützt, Fett schneller zu verbrennen und den Appetit zu zügeln.
In jeder Apotheke können Sie Reduslim kaufen, um eine effektive Methode zur Gewichtsabnahme zu finden. Es ist jedoch wichtig zu beachten, dass Reduslim allein nicht ausreicht, um abzunehmen. Eine ausgewogene Ernährung und regelmäßige Bewegung sind ebenso wichtig, um langfristige Ergebnisse zu erzielen.
Also, wenn Sie nach einem natürlichen Weg suchen, um Ihren Gewichtsverlust zu unterstützen, besuchen Sie Ihre Apotheke und fragen Sie nach Reduslim. Es könnte genau das sein, wonach Sie gesucht haben.
https://reduslim.at/
MГ¶chten Sie wissen, wo Sie das Originalprodukt “Reduslim” kaufen kГ¶nnen? Wenn ja, sind Sie hier genau richtig! Das beste und sicherste GeschГ¤ft, um Reduslim zu kaufen, ist direkt auf der offiziellen Website des Herstellers. Dort erhalten Sie das echte Produkt zum besten Preis und mit 100%iger Garantie fГјr QualitГ¤t und Wirksamkeit. Vergessen Sie also die Suche nach “donde comprar Reduslim original” in anderen Online-Shops oder Drogerien. Kaufen Sie es am besten direkt beim Hersteller und erleben Sie die Vorteile dieses beliebten NahrungsergГ¤nzungsmittels zur Gewichtsreduktion. Probieren Sie es noch heute aus und bringen Sie Ihr Gewichtsmanagement auf ein neues Level!
https://reduslim.at/
Reduslim wird von vielen als Wundermittel zum schnellen Abnehmen angepriesen, aber ist Reduslim seriös? Diese Frage beschäftigt viele, die nach einer effektiven Methode suchen, um Gewicht zu verlieren. Reduslim wird als natürliche Ergänzung beworben, die den Stoffwechsel ankurbelt und Fettverbrennung fördert. Doch die Meinungen darüber, ob Reduslim tatsächlich wirksam ist, gehen auseinander. Einige Benutzer schwören auf die positive Wirkung von Reduslim, während andere skeptisch sind und Zweifel an der Seriosität des Produkts haben. Es ist ratsam, ärztlichen Rat einzuholen, bevor man Reduslim verwendet, um mögliche Risiken zu vermeiden. Letztendlich liegt es an jedem selbst, ob man Reduslim eine Chance gibt oder nicht.
https://reduslim.at/
Reduslims sind eine natürliche und wirksame Ergänzung zur Gewichtsabnahme. Diese roten Pillen enthalten natürliche Inhaltsstoffe wie grüner Kaffee und Bitterorange, die den Stoffwechsel ankurbeln und die Fettverbrennung fördern. Durch die Einnahme von Reduslims können Sie Ihren Körper dabei unterstützen, überschüssiges Fett zu verbrennen und schneller abzunehmen.
Die Wirkung von Reduslims beruht auf der Kombination der verschiedenen Inhaltsstoffe, die synergistisch zusammenarbeiten, um die Gewichtsabnahme zu beschleunigen. Grüner Kaffee hilft dabei, den Appetit zu reduzieren und den Stoffwechsel anzukurbeln, während Bitterorange die Fettverbrennung und den Kalorienverbrauch steigert.
Durch die regelmäßige Einnahme von Reduslims können Sie schneller Gewicht verlieren und Ihrem Körper helfen, in Form zu kommen. Es ist jedoch wichtig zu beachten, dass Reduslims kein Ersatz für eine gesunde Ernährung und regelmäßige Bewegung sind. Eine ausgewogene Ernährung und ausreichend körperliche Aktivität sind weiterhin wichtig, um langfristig abzunehmen und gesund zu bleiben.
Wenn Sie also auf der Suche nach einer natürlichen und wirksamen Unterstützung zur Gewichtsabnahme sind, sind Reduslims eine gute Option. Probieren Sie sie aus und erleben Sie selbst, wie sie Ihnen dabei helfen können, Ihre Abnehmziele zu erreichen.
https://reduslim.at/
Reduslim Österreich ist ein beliebtes Produkt, das die Menschen dabei unterstützt, auf gesunde Weise Gewicht zu verlieren. Die einzigartige Formel wurde speziell für den österreichischen Markt entwickelt und hat eine hohe Erfolgsquote. Mit Reduslim können Sie schnell und effektiv abnehmen, ohne dabei zu hungern oder sich körperlich zu erschöpfen.
Das Geheimnis von Reduslim liegt in seiner natürlichen Zusammensetzung, die aus hochwertigen pflanzlichen Inhaltsstoffen besteht. Diese helfen dabei, den Stoffwechsel zu erhöhen, Fett zu verbrennen und den Appetit zu unterdrücken. Dadurch wird das Abnehmen erleichtert und der Jo-Jo-Effekt vermieden.
Viele zufriedene Kunden in Österreich schwärmen von den positiven Ergebnissen, die sie mit Reduslim erzielt haben. Sie berichten von einem gesteigerten Energielevel, einem besseren Körpergefühl und einem insgesamt verbesserten Wohlbefinden. Wenn auch Sie davon träumen, Ihre Traumfigur zu erreichen, sollten Sie Reduslim Österreich eine Chance geben.
Bestellen Sie noch heute Ihre Packung Reduslim und starten Sie Ihren Weg zu einem gesünderen und schlankeren Ich. Mit Reduslim Österreich können Sie Ihre Ziele erreichen und selbstbewusst durchs Leben gehen. Probieren Sie es aus und überzeugen Sie sich selbst von der Wirksamkeit dieses Produkts.
https://reduslim.at/
Лучший сайт казино в России 1win
http://canadianpharm.guru/# canadian valley pharmacy
Некоторые зоозащитные организации, например arme, acpa
и soi dog foundation, проводят «спасательные хирургического вмешательства
в виде лотерей,.
Also visit my web site; http://yagiro.ru/profile/epola/
саратов заказать цветы с доставкой на дом https://www.flowerssaratov.ru .
It collects info from all around the Net and does not actually fact-check any of it.
Review my site – Best Immigration Lawyers In California (Dorine)
https://muslim-prayer-times.com/
The Psychology of a Darknet Market User: Insights from Abacus
Market Darknet Asap
Cryptocurrencies and Contraband: The Financial Backbone of Abacus Market
Abacus Darknet Market was founded in 2019 and has since become known for its high security and reliability. The market offers encrypted access and secure transactions, making it attractive to those seeking anonymity and privacy.
https://abacuswebmarket.com
Por favor, elimine las cookies (importante), y después haga clic en aquí, para iniciar procedimiento autorización, en https://argentinaggpokerplus.com/.
pin up casino giris: pin up guncel giris – pin up casino indir
Forklift Warning Lights and Symbols
gates of olympus oyna ucretsiz: gates of olympus demo turkce oyna – gates of olympus oyna ucretsiz
Apartments, penthouse and mansions in Six Senses Dubai Marina with favourable terms of purchase and return on investment.
даркнет россия
стране, так же и в других территориях, теневая сеть представляет собой отрезок интернета, неприступную для обычного поискавания и просмотра через стандартные браузеры. В противоположность от общеизвестной поверхностной соединения, теневая сеть является тайным куском интернета, выход к какому часто делается через специальные приложения, такие как Tor Browser, и скрытые коммуникации, наподобные Tor.
В теневой сети собраны различные материалы, включая форумы, торговые площадки, журналы и прочие веб-сайты, которые могут стать недоступимы или запрещены в стандартной коммуникации. Здесь допускается найти различные продукты и услуги, включая нелегальные, например наркотики, стрелковое оружие, компрометированные информация, а также услуги компьютерных взломщиков и другие.
В стране скрытая часть интернета также применяется для преодоления цензуры и наблюдения со стороны. Некоторые участники могут применять его для трансфера информацией в условиях, когда воля слова замкнута или информационные материалы подвергаются цензуре. Однако, также следует отметить, что в теневой сети есть много неправомерной работы и опасных ситуаций, включая надувательство и киберпреступления
se utgivernettstedet
aviator giris: aviator oyna slot – aviator sinyal hilesi apk
Приветствую, азартные компаньоны! Я не могу остаться равнодушным и не рассказать своими ощущениями о игорном клубе “play fortuna казино“. Это место, где я выявил все, которое потребуется для прекрасного отдыха: разнообразие занятий, большие премии и быстрые выплаты. Но чего меня в особенности поразило – это обстановка приветливости и помощи, какую создают администраторы и участники. Присоединьтесь к гемблинг-дому “плейфортуна” и войдите в вселенную азарта и радости без промедления!
aviator ucak oyunu: aviator oyunu 10 tl – aviator oyunu 100 tl
LГҐn 6000
Хай, игровые приятели! Я не могу пропустить и не изложить своими ощущениями о казино “azino“. Это площадка, где я обнаружил все, чего нужно для великолепного пролёта: ассортимент занятий, большие надбавки и оперативные выплаты. Но что меня в частности шокировало – это обстановка приветливости и поддерживания, что создают организаторы и игроки. Присоединяйтесь к игровому дому “azino777” и войдите в вселенную игр и наслаждения сейчас же!
http://www.compitech.ru/html.cgi/other/comp/monitoring-zapushchennyh-prilozheniy.htm
https://cd-bar.com/povshenie-produktivnosti-i-obespetchenie-korporativnoy-bezopasnosti-so-sprutmonitor.html
https://passportist.ru/insajderskaya-ugroza/
carsinfo.net
travelusanews.com
Lainaa 5000 euroa
https://raznic.ru/roditelskij-kontrol-dlya-podchinennyx.html
https://jobinmoscow.com.ru/LB/KAT12/474.php
He enjoys practicing his ballet in the bathroom.
https://onff.ru/sistema-kontrolya-rabochego-vremeni-sprutmonitor/
Экзистенция подпольных онлайн-рынков – это процесс, который привлекает громадный внимание а разговоры во современном сообществе. Темная часть интернета, или глубокая зона всемирной сети, представляет собой приватную платформу, доступных тольково через определенные программные продукты или конфигурации, обеспечивающие анонимность пользовательских аккаунтов. В этой данной закрытой конструкции лежат теневые электронные базары – интернет-ресурсы, где-либо продажи различные продуктовые товары а услуговые предложения, чаще всего противоправного характера.
По теневых электронных базарах можно обнаружить самые различные вещи: наркотики, оружие, ворованные данные, взломанные учетные записи, фальшивые документы а и другое. Такие базары время от времени притягивают восторг также правонарушителей, а также стандартных пользователей, хотящих пройти мимо закон или доступить к товары а услуговым предложениям, те на нормальном интернете были бы в недосягаемы.
Впрочем следует помнить, чем деятельность на скрытых интернет-площадках имеет противозаконный специфику и способна создать важные юридические нормы последствия по закону. Полицейские настойчиво борются противодействуют такими площадками, и все же вследствие инкогнито темной стороны интернета это условие не постоянно просто так.
В результате, наличие даркнет-маркетов представляет собой действительностью, но все же такие рынки останавливаются зоной серьезных опасностей как и для таковых участников, а также для подобных общества в в целом и целом.
купить бетон
https://www.12info.ru/kak-uznat-chem-zanimayutsya-sotrudniki-na-svoem-rabochem-meste.html
https://muslim-prayer-times.com/
sweet bonanza hilesi: sweet bonanza demo – slot oyunlari
In recent years, ivermectin pour on for cattle, containing ivermectin, has gained attention for its potential role in vector control strategies aimed at combating diseases such as malaria and dengue fever. By targeting mosquito vectors that transmit these deadly pathogens, it offers a complementary approach to existing control measures, potentially reducing disease transmission and burden.
pin up casino indir: pin up casino indir – pin up guncel giris
Лучший сайт казино и БК в России 1win
Рекомендую сайт-оригинал Букмекерскую контору 1win
Спасибо за ваше известие. Мы ценим ваш комментарий и готовы для вас посодействовать. Если у вас есть какие-либо вспомогательные вопросы либо нужна добавочная информация, не стесняйтесь требовать. Вместе мы сделаем наш форум еще как никакого другого!
http://moldova.sports.md/football/europa_league/news/14-12-2023/154795/zhoze_mourin_ju_dolzhny_pobedit_sherif_i_verit_chto_mozhem_vyigrat_gruppu/
mЕЇЕѕete se podГvat sem
gates of olympus 1000 demo: gates of olympus oyna ucretsiz – gates of olympus demo oyna
yeni slot siteleri: bonus veren casino slot siteleri – en guvenilir slot siteleri
Хай, игровые приятели! Я не могу остаться равнодушным и не поделиться своими ощущениями о игровом доме “1x slots“. Это место, где я нашел все, которое необходимо для отличного пролёта: разнообразие активностей, громадные дополнения и оперативные выплаты. Но которое меня в особенности поразило – это обстановка приветливости и помощи, что создают админы и зрители. Присоединьтесь к игорному клубу “Xslots” и погрузитесь в вселенную игр и счастья сейчас же!
Abacus’s Battle: Staying Online Amidst Cyber Attacks
The Digital Black Market: A Deep Dive into Abacus Darknet Market
Unveiling Abacus: The Hidden Market of the Dark Web
Abacus Darknet Market is an online marketplace on the Darknet accessible through anonymous networks such as Tor. It is one of the oldest and most reliable darknet markets, providing access to various goods and services that cannot be found on the regular Internet.
https://abacusmarketdarkweb.info
hoki 1881
1. Вибір натяжних стель – як правильно обрати?
2. Топ-5 популярних кольорів натяжних стель
3. Як зберегти чистоту натяжних стель?
4. Відгуки про натяжні стелі: плюси та мінуси
5. Як підібрати дизайн натяжних стель до інтер’єру?
6. Інноваційні технології у виробництві натяжних стель
7. Натяжні стелі з фотопечаттю – оригінальне рішення для кухні
8. Секрети вдалого монтажу натяжних стель
9. Як зекономити на встановленні натяжних стель?
10. Лампи для натяжних стель: які вибрати?
11. Відтінки синього для натяжних стель – ексклюзивний вибір
12. Якість матеріалів для натяжних стель: що обирати?
13. Крок за кроком: як самостійно встановити натяжні стелі
14. Натяжні стелі в дитячу кімнату: безпека та креативність
15. Як підтримувати тепло у приміщенні за допомогою натяжних стель
16. Вибір натяжних стель у ванну кімнату: практичні поради
17. Натяжні стелі зі структурним покриттям – тренд сучасного дизайну
18. Індивідуальність у кожному домашньому інтер’єрі: натяжні стелі з друком
19. Як обрати освітлення для натяжних стель: поради фахівця
20. Можливості дизайну натяжних стель: від класики до мінімалізму
натяжні стелі це https://natjazhnistelitvhyn.kiev.ua .
Покупки в темном интернете: Заблуждения и Факты
Скрытая часть веба, таинственная область интернета, привлекает внимание пользователей своим анонимностью и способностью купить различные товары и предметы без дополнительной информации. Однако, переход в тот вселенная скрытых площадок сопряжено с рядом рисков и нюансов, о чем следует осведомляться перед совершением покупок.
Что представляет собой темный интернет и как оно действует?
Для того, кто не знаком с этим понятием, Даркнет – это часть веба, невидимая от обычных поисковых систем. В подпольной сети имеются специальные онлайн-рынки, где можно найти почти все : от препаратов и стрелкового оружия и перехваченных учётных записей и поддельных документов.
Заблуждения о приобретении товаров в подпольной сети
Тайность гарантирована: В то время как, применение технологий анонимности, вроде как Tor, может помочь скрыть свою действия в сети, тайность в Даркнете не является абсолютной. Имеется возможность, что возможно вашу информацию о вас могут выявить мошенники или даже сотрудники правоохранительных органов.
Все товары – высокого качества: В Даркнете можно найти множество поставщиков, предлагающих товары и услуги. Однако, нельзя гарантировать качественность или подлинность товаров, поскольку нет возможности провести проверку до совершения покупки.
Легальные транзакции без ответственности: Многие пользователи ошибочно считают, что товары в темном интернете, они подвергают себя низкому риску, чем в обычной жизни. Однако, заказывая противоправные вещи или услуги, вы рискуете наказания.
Реальность приобретений в темном интернете
Негативные стороны мошенничества и афер: В подпольной сети многочисленные аферисты, предрасположены к мошенничеству пользователей, которые недостаточно бдительны. Они могут предложить фальшивые товары или просто исчезнуть с вашими деньгами.
Опасность государственных органов: Пользователи Даркнета подвергают себя риску привлечения к уголовной ответственности за заказ и приобретение противозаконных.
Неопределённость результатов: Не все покупки в темном интернете заканчиваются удачно. Качество вещей может оставлять желать лучшего, а
процесс заказа может послужить источником неприятностей.
Советы для безопасных транзакций в подпольной сети
Проведите полное изучение продавца и товара перед осуществлением заказа.
Воспользуйтесь защитными программами и сервисами для защиты вашей анонимности и безопасности.
Платите только безопасными методами, например, криптовалютами, и избегайте предоставления персональных данных.
Будьте осторожны и предельно внимательны во всех ваших действиях и решениях.
Заключение
Сделки в Даркнете могут быть как захватывающим, так и опасным путешествием. Понимание рисков и применение соответствующих мер предосторожности помогут уменьшить риск негативных последствий и гарантировать безопасные покупки в этой недоступной области сети.
aviator oyna: aviator oyna 20 tl – aviator nas?l oynan?r
Zet Casino ist ein beliebtes Online-Casino, das seinen Spielern eine Vielzahl von Spielen und großzügige Boni bietet. Eine der attraktivsten Angebote für Spieler sind die Kasinobonukset, die sie bei der Anmeldung und regelmäßigen Spielen im Casino erhalten können.
Zet Casino bietet neuen Spielern einen Willkommensbonus, der aus einer Kombination von Einzahlungsboni und Freispielen besteht. Diese Boni geben den Spielern einen zusätzlichen Anreiz, das Casino auszuprobieren und ihre Lieblingsspiele zu spielen. Darüber hinaus bietet das Casino regelmäßig Reload-Boni, Freispiel-Angebote und andere Promotionen, um seine Spieler glücklich und zufrieden zu halten.
Ein weiteres Highlight von Zet Casino sind die laufenden Aktionen und Turniere, die Spieler die Möglichkeit bieten, zusätzliche Boni und Preise zu gewinnen. Diese Aktionen machen das Spielerlebnis noch spannender und bieten den Spielern die Chance, ihre Bankroll zu erhöhen und mehr Spaß beim Spielen zu haben.
Zet Casino ist auch für seine großzügigen VIP-Programme bekannt, die treue Spieler belohnen und ihnen exklusive Boni und Angebote bieten. Je mehr ein Spieler im Casino spielt, desto höher steigt er in den VIP-Stufen auf und desto mehr Vergünstigungen und Belohnungen erhält er.
Insgesamt bieten die Kasinobonukset von Zet Casino den Spielern die Möglichkeit, mehr aus ihrem Spielerlebnis herauszuholen und ihre Gewinnchancen zu erhöhen. Mit einer Vielzahl von attraktiven Boni und Promotionen ist Zet Casino definitiv einen Besuch wert für alle, die gerne Online-Casinospiele spielen.
Have a look at my web page … https://zetcasino.one/
pin-up online: aviator pin up – pin-up casino
Хай, азартные товарищи! Я не могу пропустить и не подкинуть информации своими ощущениями о игорном клубе “адмирал икс казино“. Это территория, где я выявил все, какого полезно для отличного времяпрепровождения: ассортимент активностей, крупные дополнения и оперативные выдачи. Но какого меня вообще удивило – это окружение приветливости и поддержания, что создают админы и участники. Присоединяйтесь к игорному клубу “admiralx” и погрузитесь в мирочек игр и наслаждения прямо сейчас!
1. Вибір натяжних стель – як правильно обрати?
2. Топ-5 популярних кольорів натяжних стель
3. Як зберегти чистоту натяжних стель?
4. Відгуки про натяжні стелі: плюси та мінуси
5. Як підібрати дизайн натяжних стель до інтер’єру?
6. Інноваційні технології у виробництві натяжних стель
7. Натяжні стелі з фотопечаттю – оригінальне рішення для кухні
8. Секрети вдалого монтажу натяжних стель
9. Як зекономити на встановленні натяжних стель?
10. Лампи для натяжних стель: які вибрати?
11. Відтінки синього для натяжних стель – ексклюзивний вибір
12. Якість матеріалів для натяжних стель: що обирати?
13. Крок за кроком: як самостійно встановити натяжні стелі
14. Натяжні стелі в дитячу кімнату: безпека та креативність
15. Як підтримувати тепло у приміщенні за допомогою натяжних стель
16. Вибір натяжних стель у ванну кімнату: практичні поради
17. Натяжні стелі зі структурним покриттям – тренд сучасного дизайну
18. Індивідуальність у кожному домашньому інтер’єрі: натяжні стелі з друком
19. Як обрати освітлення для натяжних стель: поради фахівця
20. Можливості дизайну натяжних стель: від класики до мінімалізму
ціна натяжних потолків https://natjazhnistelitvhyn.kiev.ua .
Во-1-х, у нас есть чудесные кнопки. Вы знали, что просто нажатие на их имеет возможность вызвать чувство радости? Ну да, ну да, как при запуске любимой компьютерной игры либо, скажем, при увиденной скидке на пиццу. А кнопок у нас тут просто настоящее колдовство!
А еще у нас есть котики. Нет, но далеко не все! Мы умеем встроить котиков в самые внезапные места. Открываете раздел “Акции” – и, бац, вам милый котик мордой машет и беседует: “Привет, здесь бонусы на вашу отрада!”. Что еще нужно для счастья?
Кроме котиков, у нас есть крутые продукты. Вы когда-нибудь видели что-то настолько крутое, собственно что для вас захотелось приобрести его в том числе и тогда, когда вы даже не знали, что это крутое? На нашем веб-сайте каждый товар – это небольшой кусок крутого счастья, кот-ый ожидает, когда вы его заметите.
И знаете,https://www.mitsu.ro/forum_new/viewtopic.php?f=12&t=16751
собственно что еще круто? Мы не просто реализовываем для вас вещи. Мы даем вам навык. Представьте, собственно что наш сайт – это загадочный лес, а вы – отважный исследователь, готовый обнаруживать неведомые хитрости и отыскивать сокровища. И это не просто метафора, это наше предложение: обнаружьте поразительное в каждой кнопке, товаре или промоакции!
А еще мы любим развлекать. Наши заметки – это реальный карнавал знаний! От секретов успешного изготовления яичницы до инструкции “Как перехитрить метеорологическую станцию и сделать лето в середине зимы”. У нас есть ответы на все ваши вопросы, а если их нет, мы придумаем что-нибудь умное и веселое вкупе с вами!
Так что, приятели, в случае если вы еще сомневаетесь, стоит заходить на наш крутой вебсайт, выскажемся так: у нас не просто покупки, у нас – приключение! Приключение с котиками, магическими кнопками и кучей смеха. Заглядывайте, приятели, так как смех – лучшее снадобье, а у нас его предостаточно!
Че, компаньон! Ты ищешь дельную инфу про то, зачем тебе копаться на нашем веб-сайте? Окей, держи фишку!
Слушай, тут у нас не просто вебсайт, это кладезь знаний, где ты можешь выдавить всю соковитую инфу, что только захочешь! Эй, ну да мы как те уличные братки, представляешь ли, практически постоянно подскажем, как спасти тебя из любой капусты.
https://mamont.md/article/moldovanewsmd-klyuch-k-aktualnoy-informatsii-o-moldove-i-mire
Здесь на любом углу – инструкции, советы, рецепты, ну да что угодно! Не имеет никакого значения, че ты штудируешь – кулинарию, программирование, фитнес либо философию. У нас все есть варианты, как в кармане у грамотного философа.
А, и как мы забыли заявить, дружище, наш сайт это не столько информация, это и связь с реальными профи! Тут ты можешь задавать средства вопросы, делиться своими находками, обсуждать принципиальные темы с такими же заинтересованными братками, как ты.
Так что не трать время зря, давай, заскакивай к нам на сайт и окунись в мир знаний и общения, который мы тебе приготовили! Так как кто знает, имеет возможность, тут тебе раскроются двери в новую жизнь, как в кинокартинах!
Ознакомьтесь с большим ассортиментом отделочных материалов оптом на нашем сайте. Доставка гарантия качества по выгодным ценам оптом интернет магазин
1. Вибір натяжних стель – як правильно обрати?
2. Топ-5 популярних кольорів натяжних стель
3. Як зберегти чистоту натяжних стель?
4. Відгуки про натяжні стелі: плюси та мінуси
5. Як підібрати дизайн натяжних стель до інтер’єру?
6. Інноваційні технології у виробництві натяжних стель
7. Натяжні стелі з фотопечаттю – оригінальне рішення для кухні
8. Секрети вдалого монтажу натяжних стель
9. Як зекономити на встановленні натяжних стель?
10. Лампи для натяжних стель: які вибрати?
11. Відтінки синього для натяжних стель – ексклюзивний вибір
12. Якість матеріалів для натяжних стель: що обирати?
13. Крок за кроком: як самостійно встановити натяжні стелі
14. Натяжні стелі в дитячу кімнату: безпека та креативність
15. Як підтримувати тепло у приміщенні за допомогою натяжних стель
16. Вибір натяжних стель у ванну кімнату: практичні поради
17. Натяжні стелі зі структурним покриттям – тренд сучасного дизайну
18. Індивідуальність у кожному домашньому інтер’єрі: натяжні стелі з друком
19. Як обрати освітлення для натяжних стель: поради фахівця
20. Можливості дизайну натяжних стель: від класики до мінімалізму
стелі натяжні http://natjazhnistelitvhyn.kiev.ua .
1. Вибір натяжних стель – як правильно обрати?
2. Топ-5 популярних кольорів натяжних стель
3. Як зберегти чистоту натяжних стель?
4. Відгуки про натяжні стелі: плюси та мінуси
5. Як підібрати дизайн натяжних стель до інтер’єру?
6. Інноваційні технології у виробництві натяжних стель
7. Натяжні стелі з фотопечаттю – оригінальне рішення для кухні
8. Секрети вдалого монтажу натяжних стель
9. Як зекономити на встановленні натяжних стель?
10. Лампи для натяжних стель: які вибрати?
11. Відтінки синього для натяжних стель – ексклюзивний вибір
12. Якість матеріалів для натяжних стель: що обирати?
13. Крок за кроком: як самостійно встановити натяжні стелі
14. Натяжні стелі в дитячу кімнату: безпека та креативність
15. Як підтримувати тепло у приміщенні за допомогою натяжних стель
16. Вибір натяжних стель у ванну кімнату: практичні поради
17. Натяжні стелі зі структурним покриттям – тренд сучасного дизайну
18. Індивідуальність у кожному домашньому інтер’єрі: натяжні стелі з друком
19. Як обрати освітлення для натяжних стель: поради фахівця
20. Можливості дизайну натяжних стель: від класики до мінімалізму
дворівневі стелі https://natjazhnistelitvhyn.kiev.ua/ .
המימורים באינטרנט – מימורי ספורט, משחקי קזינו באינטרנט, משחקי קלפי.
המימונים באינטרנט נהפכים לשדה מבוקש בבאופן מיוחד בעידן הדיגיטלי.
מיליונים משתתפים מנסים את המזל באפשרויות מימורים המגוונים.
התהליכים הזוהה משנה את רגעי הניסיונות והתרגשות.
גם עוסק בשאלות אתיות וחברתיות העומדות מאחורי המימורים ברשת.
בעידן הדיגיטלי, מימורים בפלטפורמת האינטרנט הם חלק מתרבות ה הספורטאי, הפנאי והחברה המתקדמת.
ההימורים באינטרנט כוללים אפשרויות רחבות של פעולות, כולל מימורים על תוצאות ספורט, פוליטי, וגם מזג האוויר בעולם.
המימונים הם הם מתבצעים באמצע
Бизнесмен Андрей Кнауб хорошо известен как предприниматель и трейдер в сфере нефтепереработки. Он более 25 лет был частью крупнейших отраслевых компаний, реализовал множество благотворительных и социальных проектов кнауб андрей артурович
Всем рекомендую Букмекерскую контору 1xbet
Рекомендую лучшую Букмекерскую контору 1xbet
sweet bonanza mostbet: sweet bonanza demo – sweet bonanza 100 tl
aviator pin up: pin up giris – pin up casino
Convenience: Didn’t we didn’t fit the figure that we glad instantly moisturize
the body with benefit for body without {starting|going
to the {https://filterfridgestore.com/|filterfridgestore.com}?
Electricity may is deadly, so if eating something, about what craftsmen should think twice before doing https://www.indiehackers.com/FRANKIE5, this is the electrical wiring in their house.
Douglas figured the best way to succeed was to do the opposite of what he’d been doing all his life.
камины купить
Профессиональный монтаж дымоходов обеспечивает эффективное удаление дыма и гарантирует безопасность в вашем доме.
дымоходы
Профессиональный монтаж дымоходов обеспечивает эффективное удаление дыма и гарантирует безопасность в вашем доме.
LГҐn 6000
купить камин
Купить дымоход для печи или камина легко, но важно также правильно осуществить его установку для безопасной эксплуатации.
I am not sure where youu are getting your info, but great topic.
I needs to spend some time learning more or understandinbg
more. Thanks for great info I was looking foor this information for myy mission.
Take a llok at my web page :: 카지노사이트
aviator ucak oyunu: aviator oyunu 100 tl – aviator oyna 100 tl
gates of olympus guncel: gates of olympus oyna demo – gates of olympus oyna ucretsiz
Рентабельность легального похоронного бизнеса низкая и составляет в рф до двух десятков % (зависимо от определенной государства.
acyclovir cream 5% bestellen
Лучшая Букмекерская контора 1xbet
Porn (https://fishing-ua.com)
Great weblog right here! Alsoo your site quite a
bit up verry fast! What hosst are you using? Can I get your affiliate hyperlink on your
host? I wish my wweb site loaded up as quickly as yours lol
Here is my web blog – 카지노사이트
PЕЇjДЌka 16000 KДЌ
Темный интернет: запретная территория компьютерной сети
Теневой уровень интернета, тайная зона интернета продолжает вызывать интерес внимание как общественности, так и правоохранительных органов. Этот подпольный слой интернета известен своей непрозрачностью и способностью совершения преступных деяний под прикрытием теней.
Суть теневого уровня интернета заключается в том, что этот слой не доступен обычным браузеров. Для доступа к данному слою требуются специальные программы и инструменты, обеспечивающие скрытность пользователей. Это формирует прекрасные условия для различных незаконных действий, среди которых торговлю наркотиками, оружием, кражу личных данных и другие незаконные манипуляции.
В свете растущую опасность, некоторые государства приняли законы, направленные на запрещение доступа к темному интернету и привлечение к ответственности тех, кто совершающих противозаконные действия в этом скрытом мире. Впрочем, несмотря на предпринятые шаги, борьба с теневым уровнем интернета представляет собой трудную задачу.
Следует отметить, что запретить темный интернет полностью практически невыполнима. Даже при строгих мерах регулирования, возможность доступа к этому слою интернета все еще осуществим при помощи различных технологических решений и инструментов, применяемые для обхода ограничений.
Помимо законодательных мер, существуют также инициативы по сотрудничеству между правоохранительными органами и компаниями, работающими в сфере технологий для противодействия незаконным действиям в подпольной части сети. Тем не менее, эта борьба требует не только технических решений, но и совершенствования методов выявления и предотвращения незаконных действий в этой области.
В итоге, несмотря на введенные запреты и предпринятые усилия в борьбе с преступностью, теневой уровень интернета остается серьезной проблемой, которая требует комплексного подхода и совместных усилий со стороны правоохранительных служб, так и технологических компаний.
DC
даркнет открыт
В последнее время даркнет, вызывает все больше интереса и становится объектом различных дискуссий. Многие считают его темным уголком, где процветают преступность и незаконные действия. Однако, мало кто осведомлен о том, что даркнет не является закрытой сферой, и вход в него возможен для каждого пользователь.
В отличие от обычного интернета, даркнет не доступен для поисковых систем и обычных браузеров. Для того чтобы войти в него, необходимо использовать специальные программы, такие как Tor или I2P, которые обеспечивают скрытность и шифрование данных. Однако, это не означает, что даркнет закрыт от общественности.
Действительно, даркнет открыт для всех, кто имеет желание и способность его исследовать. В нем можно найти различные ресурсы, начиная от дискуссий, которые не приветствуются в обычных сетях, и заканчивая возможностью посещения специализированным рынкам и сервисам. Например, множество информационных сайтов и форумов на даркнете посвящены темам, которые считаются запретными в стандартных окружениях, таким как политика, религия или криптовалюты.
Кроме того, даркнет часто используется сторонниками и журналистами, которые ищут пути обхода ограничений и средства для сохранения анонимности. Он также служит средой для свободного обмена информацией и идеями, которые могут быть подавимы в странах с авторитарными режимами.
Важно понимать, что хотя даркнет предоставляет свободный доступ к данным и шанс анонимного общения, он также может быть использован для незаконных целей. Тем не менее, это не делает его закрытым и неприступным для любого.
Таким образом, даркнет – это не только темная сторона интернета, но и место, где каждый может найти что-то интересное или полезное для себя. Важно помнить о его двуединстве и разумно использовать его и осознанием возможных рисков.
aviator bahis: aviator oyunu giris – aviator sinyal hilesi ucretsiz
1. Вибір натяжних стель – як правильно обрати?
2. Топ-5 популярних кольорів натяжних стель
3. Як зберегти чистоту натяжних стель?
4. Відгуки про натяжні стелі: плюси та мінуси
5. Як підібрати дизайн натяжних стель до інтер’єру?
6. Інноваційні технології у виробництві натяжних стель
7. Натяжні стелі з фотопечаттю – оригінальне рішення для кухні
8. Секрети вдалого монтажу натяжних стель
9. Як зекономити на встановленні натяжних стель?
10. Лампи для натяжних стель: які вибрати?
11. Відтінки синього для натяжних стель – ексклюзивний вибір
12. Якість матеріалів для натяжних стель: що обирати?
13. Крок за кроком: як самостійно встановити натяжні стелі
14. Натяжні стелі в дитячу кімнату: безпека та креативність
15. Як підтримувати тепло у приміщенні за допомогою натяжних стель
16. Вибір натяжних стель у ванну кімнату: практичні поради
17. Натяжні стелі зі структурним покриттям – тренд сучасного дизайну
18. Індивідуальність у кожному домашньому інтер’єрі: натяжні стелі з друком
19. Як обрати освітлення для натяжних стель: поради фахівця
20. Можливості дизайну натяжних стель: від класики до мінімалізму
навісні стелі https://www.natjazhnistelitvhyn.kiev.ua .
pin up: pin up indir – pin up 7/24 giris
Предприниматель придерживался мнения, что заботиться надо не только о персонале, но и окружающей среде кнауб андрей артурович
Предприниматель придерживался мнения, что заботиться надо не только о персонале, но и окружающей среде кнауб андрей томскнефтепереработка
Kenyan gamers, it’s time to explore the elite online casinos in Kenya.
buy propecia
Water softeners and conditioners: they able to last many years, but able require service
maintenance or resin replacement. Filter type:
different variants of https://http://www.waterfilterstore.com/ have their service life/operation}.
Во-первых, мы тут не для шуток, а дабы подымать бабло. У нас эпичные задания по ютубу, отзывам и проголосовать тебе не составит труда. Пальцы в горячке шевели, и баксов на твоем счету больше.
А во-вторыхhttp://freelancing.md/project/693
, кто заявил, что доход не имеет возможности быть веселым? У нас царствует атмосфера, как на самом классном пикнике. Здесь даже заработок становится частью приключения. Забудь скучноватые таски, у нас все по-нашему!
Ну и конечно, партнерство с нами – это, брат, как скидка в самом эксклюзивном клубе. Ты первый узнаешь о горячих промоакциях, самых радужных услугах и получишь билет в мир анлимитного заработка. А мы для тебя не просто обещаем, а гарантируем!
И честно, не понимаю, как возможно протекать мимо такого кайфа. Ты что, не пытаешься замерзнуть настоящим уличным боссом? На нашем сайте ты, брат, будешь как капитан собственного корабля, маневрируя в океане крутых задач. Твои деньги, твои правила!
Не будь лузером, чувак! Забудь про нудные хлопоты и войди в ряды тех, кто рубит бабло, не отрываясь от кайфа. Заходи на наш вебсайт, дерзай и зарабатывай, как реальный уличный браток. Тут твое время пришло, чувак!
free
pin-up bonanza: pin up casino giris – pin up indir
В биографии бизнесмена Андрея Артуровича Кнауба важно отметить, что для него ключевое значение имела забота о персонале и экологической обстановке в регионе кнауб андрей артурович
sweet bonanza yasal site: sweet bonanza kazanc – sweet bonanza mostbet
Зберігати такі навушники треба не подібно заплутаного «клубка» з проводів, а в складеному вигляді.
Here is my site :: http://sportandpolitics.ukrbb.net/viewtopic.php?f=24&t=11672
continue lendo isso
homeideascoach.com
getusainvest.com
Kenyan players, gear up for the ultimate gaming adventure at online casinos in Kenya.
Спасибо за ваше известие. Мы ценим ваш объяснение и готовы вам посодействовать. Если у вас есть какие-либо дополнительные вопросы или необходима дополнительная информация, не стесняйтесь требовать. Совместно мы создадим наш форум еще лучше!
http://ustsm.md/?p=174
Egor Alexandrovich Abramov’s personal life remains guarded, allowing his work to speak volumes about his dedication to the craft egor abramov
Egor Alexandrovich Abramov’s personal life remains guarded, allowing his work to speak volumes about his dedication to the craft egor alexandrovich abramov
pin up aviator: pin up casino – aviator pin up
Eu só recomendo este original Fortune Tiger
Eu recomendo este site Fortune Tiger
gates of olympus demo free spin: gates of olympus hilesi – gate of olympus hile
Open this site Fortune Tiger
Tamoxifen is listed as a Group I carcinogen, carcinogenic to humans, by the International Agency for Research on Cancer IARC and is classified as a reportable hazardous chemical viagra effects on men
Предлагаю лучшую букмекерскую контору 1xbet
кое-кто пишет стихи и склонны почитать классическую литературу, https://forum.
en cok kazandiran slot siteleri: slot siteleri bonus veren – en cok kazandiran slot siteleri
slot siteleri 2024: bonus veren casino slot siteleri – slot kumar siteleri
премии за приглашение друзей.
Here is my web blog: carsharing-promocode.ru
http://cleandi.ru/
xxxhdporno.cam
во что поиграть кооператив на пк Какие игры подходят для использования на слабом персональном компьютере в 2024 году?
бесплатные частные объявления России Предоставляем услугу бесплатного размещения объявлений по всей территории России.
Kredit 50000 Euro
güvenilir bahis siteleri
The Legal Loopholes of Operating a Market like Tor2door
Market Darknet Asap
Cryptocurrencies and Contraband: The Financial Backbone of Tor2door Market
Tor2door Darknet Market is an online marketplace on the Darknet accessible through anonymous networks such as Tor. It is one of the oldest and most reliable darknet markets, providing access to various goods and services that cannot be found on the regular Internet.
https://www.tor2doormarketonion.net/
Egor Abramov’s biography, initiated by chance, has evolved into a promising career, and as he continues to make his mark in the cinematic landscape, audiences can anticipate more captivating performances from this talented young actor egor abramov
Слушай, компаньон! Я в курсе, собственно что ты раздумываешь, зачем тебе лазить по нашему веб-сайту, хотя давай-ка я поведаю тебе почему это круто, а?
https://primarie.halleykm.md/forum/325/viattimd—partenerul-de-ncredere-pentru-anvelope-de-calitate
Во-первых, здесь ты найдешь вагон полезной инфы! собственно что бы ты ни искал – от советов по саморазвитию до лайфхаков для совершенствования быта – у нас все есть, собственно что тебе нужно для становления и вдохновения.
Но это еще не все! У нас тут целое сообщество, как клуб “Без Карантина”, где ты можешь общаться с крутыми детьми, делиться средствами мыслями и получать поддержку в любой ситуации.
А еще на нашем сайте практически постоянно что-нибудь случается! Акции, состязания, онлайн-мероприятия – в целом, все, чтобы ты не заскучал и практически постоянно оставался в курсе самых новых тенденций.
Так что, старина, не тяни кота за задолженность! Загляни на наш вебсайт и давай вкупе развиваться, знаться и развлекаться! Я уверен, ты тут отыщешь для себя по-настоящему крутых приятелей и море позитива!
Egor Abramov’s biography, initiated by chance, has evolved into a promising career, and as he continues to make his mark in the cinematic landscape, audiences can anticipate more captivating performances from this talented young actor egor alexandrovich abramov
auton merkkivalot
Eu recomendo este jogo Fortune Tiger
O site original do jogo Fortune Tiger
O site original do jogo pode ser encontrado aqui Fortune Tiger
According to the user manual, the system must fit for many standard faucets, https://svirsonfilter.com/ and
appears three adapters if/in case it is unlikely to fit in its
usual form.
mexican online pharmacies prescription drugs cheapest mexico drugs mexican rx online
Знакомьтесь с топовой Букмекерской конторой 1xbet
xxx porno
Читайте статью на vc.ru продать notcoin как продать Ноткоины сегодня по отличной цене. Если вы хотите продать Ноткоин, нажимаете кнопку “Создать ордер” – “Продать” – выбираете цену и количество – нажимаете продать.
Lainaa 3000 euroa
услуги вскрытия замков https://azs-zamok13.ru/ .
Мы специализируемся на скупке автомобилей всех марок и моделей, выкупаем авто после ДТП, покупаем мотоциклы, скутера и квадроциклы, гидроциклы, легкие моторные лодки, лодочные моторы, в любом состоянии, дорого покупаем легкий коммерческий транспорт, водный транспорт и легковые автомобили, осуществляем быструю скупку подержанной автомототехники, залоговое и кредитное авто https://buybuyavto.ru/moskva/vykup-avto-metro-vyhino/
nortriptyline
best online pharmacy india indian pharmacy delivery Online medicine home delivery
증명{당신/뷰어}을 제어하는 방법을 알고 당신의 Lucky Jet 더 아름다운사람보다어떤{다른/경쟁자의}!
시간은 당신의최악의적이며사용자{해야/해야}변화하는 조건에 빠르게 적응하십시오.
My webpage … 럭키 제트는 어떻게 플레이하나요 ?
Мое мнение – лучшая Букмекерская контора 1xbet
Предлагаю топовую Букмекерскую контору 1xbet
xxxhdporno
indianpharmacy com indian pharmacy delivery best online pharmacy india
Lainaa 6000 euroa
Despite his youth, Egor Abramov has already earned critical acclaim and popularity among viewers. His growth as an actor portends a bright future and opens up new opportunities in Russian cinema egor alexandrovich abramov
Наш путеводитель по Санкт-Петербургу собрал лучшие отели и места для туристов экскурсии по СПб Мы расскажем, в каких кафе можно бюджетно перекусить, где попробовать особенные блюда с местным колоритом или отужинать, как потомки аристократов.
Thank you great posting about essential oil. Hello Administ . 国产线播放免费人成视频播放
Наш путеводитель по Санкт-Петербургу собрал лучшие отели и места для туристов горнолыжные курорты Петербурга Мы расскажем, в каких кафе можно бюджетно перекусить, где попробовать особенные блюда с местным колоритом или отужинать, как потомки аристократов.
п»їlegitimate online pharmacies india indian pharmacy delivery world pharmacy india
xxxhdporno.cam
Participe e ganhe no site original Fortune Tiger
canadianpharmacyworld canadian pharmacy 24 reddit canadian pharmacy
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.兒童色情
É um site muito lucrativo Fortune Tiger
Visite o site real do jogo Fortune Tiger
Предлагаю топовую в своем роде Букмекерскую контору 1xbet
Че, компаньон! Ты ищешь дельную инфу про то, для чего для тебя возиться на нашем веб-сайте? Окей, держи фишку!
Слушай, тут у нас не просто вебсайт, это кладезь знаний, где тебе предоставляется возможность выдавить всю соковитую инфу, что только захочешь! Эй, ну да мы как что уличные братки, знаешь ли, практически постоянно подскажем, как спасти тебя из каждой капусты.
https://www.natura.md/poezii-de-a-mateevici
Тут на любом углу – памятке, советы, рецепты, ну да что угодно! Не имеет никакого значения, че ты штудируешь – кулинарию, программирование, фитнес или философию. У нас все есть варианты, как в кармашке у грамотного философа.
А, и как мы забыли заявить, дружище, наш вебсайт это не только информация, это и связь с реальными профи! Тут тебе предоставляется возможность задавать свои вопросы, делиться своими находками, обсуждать важные темы с настолько же заинтересованными братками, как ты.
И не теряй время, выделяй, заскакивай к нам на сайт и бросься в мир знаний и общения, кот-ый мы тебе приготовили! Так как кто знает, имеет возможность, здесь тебе откроются двери в новую жизнь, как в кинокартинах!
Great post thank you. Hello Administ . Website : https://www.fastlinks.com.tr/
Thank you for great content. Hello Administ. Website : https://301.com.tr/
Завод из России реализует оборудование для фитнеса https://oborudovanie-dlya-fitnesa.ru/ по приятным ценам, без посреднических наценок. Всегда в продажезначительный каталог для постоянных покупателей. Продаем качественные станки и аксессуары, которые помогут вам улучшить ваше здоровье и физическую форму.
В создании мягких элементов применяется эластичный кожзам. Ключевые элементы конструкции изготовлены из высокопрочных видов стали. Качественные и функциональные продукты дают возможность эффективно заниматься фитнесом как в квартире, так и спортивном центре. Выпускаемое оборудование отличается отличным качеством и надежностью, что позволяет вам тренироваться продуктивно и удобно. Для домашнего использования будут актуальны эспандеры, разборные гантели, полусферы, неразборные штанги, массажные ролы, массажеры, диски для баланса, резинки, сэндбэги.
клиринговые услуги стоимость внутреннего клиринга за метр
Производственно-торговая организация реализует спортивные тренажеры https://sportivnyj-trenazher.ru для усиленной эксплуатации в коммерческих условиях. В интернет-магазине вы оцените самые известные модели машин – грузоблочных и нагружаемых. Объемный ассортимент дает возможность подобрать машины для акцентированной проработки теоретически любых мышечных отделов. Оформите Кроссовер для перекрестной тяги, Баттерфляй для грудных, силовую раму Смита, горизонтальную тягу, скамью Скотта, Дельта машину, Гакк тренажер, конструкции для работы с собственным весом, Гравитрон для подтягиваний, гиперэкстензию, скамьи для жима со стойками, горизонтальную лавку, рычажные Хаммеры. Изготавливаемое оборудование не требует постоянного специального наблюдения. Можете заказать грузоблок необходимого веса.
mexico pharmacy mexican drugstore online buying prescription drugs in mexico
Знакомлю с топовой в своем роде Букмекерской конторой 1xbet
Женский онлайн-журнал для стильных, модных и уверенных в себе представительниц прекрасного пола. Здесь вы найдете советы и подсказки, как правильно худеть, что надеть на вечеринку и как создать незабываемый женственный образ готовим дома
Participe e ganhe no site original Fortune Tiger
Este é o site original Fortune Tiger
https://treningi-i-kursy.com/
Знакомлю с топовой в своем роде Букмекерской конторой 1xbet
Выбор радиаторов отопления – залог комфорта в доме. От мощности до дизайна, каждый аспект важен. Обзор полезной информации о радиаторах отопления радиаторы отопления
Kenyan bettors will find unbeatable offers and games at these online casinos in Kenya.
Топовоя в своем роде Букмекерская контора 1xbet
medicine in mexico pharmacies medication from mexico pharmacy purple pharmacy mexico price list
Практичная армейская раскладушка для комфортного отдыха в походах и экстремальных условиях раскладушка армейская
500 Euro Kredit
xxxhdporno
Топовоя Букмекерская контора 1xbet
Ухоженные тела красавиц готовы отдаваться без остановки за скромную плату, https://t.me/sochifeya10 а способности в притяжении выше всех.
Egor, along with central actors, explores more mature themes in the latest season, depicting the evolving challenges faced by their characters egor alexandrovich abramov
Российская компания предлагает оборудование для фитнеса https://oborudovanie-dlya-fitnesa.ru/ по приятным ценам, без лишних накруток. Всегда в продажезначительный ассортимент для любых клиентов. Продаем доступные тренажеры и аксессуары, которые помогут вам улучшить ваше здоровье и физическую форму.
В производстве мягких частей применяется винилискожа. Основные части конструкции изготовлены из углеродистых видов стали. Качественные и функциональные снаряды дают возможность эффективно заниматься фитнесом как в квартире, так и тренировочном центре. Производимое оборудование отличается лучшим качеством и надежностью, что позволяет вам тренироваться безопасно и удобно. Для домашнего применения идеально подойдут петли TRX, слэмбэги, степ платформы, короткие штанги, массажные ролы, атлетические кольца, диски для балансировки, скакалки, медболы.
Топовоя Букмекерская контора на рынке 1xbet
Egor, along with central actors, explores more mature themes in the latest season, depicting the evolving challenges faced by their characters egor abramov entrepreneur
Многие начали использовать для развития продукции или услуг отзывы.
my web page – https://yorkstudy.ru/
Aqui está o site original em Fortune Tiger
Você pode encontrar o site original aqui Fortune Tiger
Acesse o site real do jogo Fortune Tiger
mexican online pharmacies prescription drugs mexico drug stores pharmacies best online pharmacies in mexico
Payday loans in Wyoming
Отечественный производитель предлагает спортивные тренажеры https://sportivnyj-trenazher.ru/ для усиленной работы в коммерческих условиях. В каталоге вы обнаружите самые лучшие варианты тренажеров – грузоблочных и нагружаемых. Большой ассортимент позволяет выбрать тренажеры для изолированной проработки теоретически любых мышечных групп. Закажите многофункциональный Кроссовер, Баттерфляй для грудных и дельтовидных мышц, силовую раму Смита, вертикально-горизонтальную тягу, парту Скотта, тренажер для плечей, Гакк тренажер, конструкции для работы с собственным весом, Гравитрон для подтягиваний, гиперэкстензию, атлетические скамьи, универсальную лавку, Хаммер. Производимое оборудование не требует постоянного специального обслуживания. Можете выбрать нагружаемый стек с плитками нужного веса.
Hi! This is my first comment here so I just wanted tto give
a quick shout out and say I really enjoy
reading your posts. Can you suggest any other blogs/websites/forums that deal wit the same subjects?
Thank you!
Also visiot my blog: 카지노사이트
top online pharmacy india Healthcare and medicines from India best india pharmacy
aralen 40mg
Во-1-х, мы тут не для шуток, а чтобы подымать бабло. У нас эпичные задания по ютубу, отзывам и проголосовать тебе не составит труда. Пальцы в горячке шевели, и баксов на твоем счету все больше.
А во-2-хhttps://www.toystore.md/product-page/конструктор-cada-радиоуправляемый-пикап-549-деталей
, кто сказал, что доход не имеет возможности быть веселым? У нас царит атмосфера, как на самом потрясающем пикнике. Тут даже доход делается частью приключения. Забудь скучные таски, у нас все по-нашему!
Ну и естесственно, партнерство с нами – это, брат, как скидка в самом неповторимом клубе. Ты первый узнаешь о горячих акциях, самых заманчивых предложениях и получишь билет в мир безлимитного заработка. А мы тебе не просто обещаем, а гарантируем!
И честно, не знаю, как можно протекать мимо такого кайфа. Ты собственно что, не хочешь стать настоящим уличным начальником? На нашем сайте ты, брат, будешь как капитан собственного корабля, маневрируя в океане крутых задач. Твои средства, твои правила!
Не будь неудачником, чувак! Забудь про нудные хлопоты и войди в ряды тех, кто рубит бабло, не отрываясь от кайфа. Заходи на наш вебсайт, дерзай и зарабатывай, как реальный уличный браток. Здесь твое время пришло, чувак!
30000 euro lenen
Самая надежная Букмекерская контора на рынке 1xbet
buying from online mexican pharmacy mexico pharmacy mexican pharmaceuticals online
Discover luxurious properties for sale in Orla Palm Jumeirah. From elegant apartments to spacious mansions, OMNIYAT’s developer offers desirable homes at irresistible prices. Experience a life of luxury and comfort with our stunning selection of simplexes, duplexes, and sky palaces. Don’t miss the opportunity to own your dream property in this prestigious location.
The accessibility of buy ivermectin for humans, featuring ivermectin, has been crucial in controlling parasitic infections in populations affected by humanitarian crises. Through partnerships with aid organizations and government agencies, ivermectin distribution programs reach displaced communities, providing essential treatment and prevention options.
Наша типография предлагает широкий спектр услуг, связанных с печатью и производством различных материалов. У нас есть опытные специалисты и современное оборудование, чтобы гарантировать высокое качество и быструю обработку заказов типография
https://betonmitischi.ru/
Thank you great post. Hello Administ .国产线播放免费人成视频播放
Хай, фанаты азартных приключений! В настоящее время я желаю рассказать с вами своими забавными впечатлениями об сетевом казино “бонусы казино“. Это участок, где волнение и веселье смешиваются в единственное целое! После того, как я вступил на веб-страницу, меня встречал коктейль из захватывающих игр и обильных бонусов. Атмосфера здесь такая, как если бы каждый день – празднование! Тарифы увеличиваются, а мои улыбки и. Присоединитесь к авиатор игра 1win и вы узнаете, что что такое азарт с радостью!
purple pharmacy mexico price list mexico pharmacy medication from mexico pharmacy
New porn
In both 2014 and 2015 Alexandre Cougnaud raced in the Porsche Carrera Cup France championship. He finished in 10th position the first year and in 12th position the second year https://pl.motorsport.com/driver/alexandre-cougnaud/830053/photos/
qiyezp.com
그러나 이때 황실 호위대가 왕자를 포위하고 Fang Jifan과 Chen Tong이 도착했습니다.
indian pharmacy online indian pharmacy reputable indian online pharmacy
сеть даркнет
Темный интернет: запретная территория виртуальной сети
Темный интернет, скрытый сегмент сети продолжает привлекать внимание внимание и сообщества, и также правоохранительных органов. Данный засекреченный уровень интернета известен своей анонимностью и способностью проведения противоправных действий под маской анонимности.
Основа темного интернета состоит в том, что он не доступен для популярных браузеров. Для доступа к нему требуются специализированные программные средства и инструменты, предоставляющие анонимность пользователям. Это формирует идеальную среду для различных незаконных действий, в том числе торговлю наркотическими веществами, торговлю огнестрельным оружием, кражу конфиденциальных данных и другие преступные операции.
В виде реакции на растущую опасность, ряд стран приняли законы, целью которых является ограничение доступа к теневому уровню интернета и преследование лиц совершающих противозаконные действия в этой скрытой среде. Однако, несмотря на принятые меры, борьба с темным интернетом представляет собой трудную задачу.
Следует отметить, что полное запрещение теневого уровня интернета практически невозможно. Даже с введением строгих мер контроля, возможность доступа к этому слою интернета всё ещё возможен через различные технологии и инструменты, используемые для обхода блокировок.
Кроме законодательных мер, имеются также проекты сотрудничества между правоохранительными органами и компаниями, работающими в сфере технологий с целью пресечения противозаконных действий в теневом уровне интернета. Однако, для эффективного противодействия необходимы не только технологические решения, но и улучшения методов обнаружения и пресечения незаконных действий в этой среде.
Таким образом, несмотря на принятые меры и усилия в борьбе с преступностью, теневой уровень интернета остается серьезной проблемой, которая требует комплексного подхода и совместных усилий со стороны правоохранительных структур, а также технологических организаций.
In both 2014 and 2015 Alexandre Cougnaud raced in the Porsche Carrera Cup France championship. He finished in 10th position the first year and in 12th position the second year https://me.motorsport.com/driver/%D8%A3%D9%84%D9%83%D8%B3%D9%86%D8%AF%D8%B1-%D9%83%D9%88%D8%BA%D9%86%D9%88/408167/
Надежная Букмекерская контора 1xbet
При регистрации в букмекерской конторе “Пари” клиент получает доступ к широкому спектру спортивных событий и различных видов ставок. Для процедуры регистрации необходимо заполнить анкету, предоставив свои персональные данные. После этого вы получите уникальное имя пользователя и пароль, которые позволят вам войти в личный кабинет и начать делать ставки. Подробная инструкция – https://t.me/s/registraciya_pari_ru
cheap canadian pharmacy online canadian pharmacy no scripts best canadian pharmacy to order from
Превосходная Букмекерская контора 1xbet
Eu só recomendo este site Fortune Tiger
Recomendo o jogo do site original Fortune Tiger
Ir para o site original Fortune Tiger
best online pharmacies in mexico Online Pharmacies in Mexico pharmacies in mexico that ship to usa
provera 20mg
https://lat.motorsport.com/driver/alexandre-cougnaud/659025/
Слушай, наш сайт – это как твоя личная сокровищница познаний и праздника! Здесь тебе предоставляется возможность отыскать все, о чем лишь только мечтаешь: советы по уходу за собой, идеи для творчества, рецепты вкусняшек причем даже секреты удачной карьеры!
http://ustsm.md/?p=187
Но далеко не все! Мы здесь сделали целое сообщество, где ты можешь общаться с единомышленниками, делиться своими мыслями и получать поддержку в каждой ситуации. Так как вкупе веселее, верно?
А еще у нас здесь всегда что-нибудь случается! Промоакции, состязания, онлайн-мероприятия – ну ты сообразила, все, дабы ты не скучала и практически постоянно ощущала себя в центре внимания!
Так что не медли, подружка моя! Загляни на наш вебсайт и давай вкупе погрузимся в увлекательный мир знаний, отдыха и бесконечной дружбы! Я уверена, тебе тут понравится не менее, чем в моей компании!
buy medicines online in india Healthcare and medicines from India reputable indian pharmacies
top 10 pharmacies in india india pharmacy mail order reputable indian online pharmacy
и успеха бонусные деньги перейдут на основной счет персонажа, какие можно будет вывести или
использовать для дальнейшей
игры по.
my homepage … леон бет зеркало
Крупнейшая Букмекерская контора 1xbet
acyclovir cream 5%
Привет всех приверженцев живых увлечений! На сегодня я желаю поделиться вам о моем захватывающем плавании в вселенная онлайн казино “старда казино онлайн“. Это пространство, где каждый из нас может выявить что-то по вкусу: от увлекательных машин до традиционных настольных игр. Но что действительно заставило меня остановиться здесь – это атмосфера счастья и увеселения, которая царит на сайте. Подарки, продвижения, состязания – здесь всегда что-то происходит! Присоединитесь к “starda казино” и прочувствуйте радость активности уже сегодня!
LГҐn 8000 kr
tra questi c’è il gigante scandinavo betsson, che negli ultimi giorni ha celebrato opzione: nel mercato bielorusso attraverso il lancio del suo marchio europebet.
Here is my web site :: http://europebet.info/
Здравствуйте каждого фанатов страстных игр! Сегодня я собираюсь рассказать вам о моем привлекательном путешествии в вселенная онлайн казино “играть игровые автоматы бесплатно без регистрации“. Это место, где каждый единичный может отыскать что-то по выбору: от увлекательных ящиков до классических настольных игр. Но что фактически заставило меня остановиться здесь – это атмосфера веселья и привлечения, которая правит на веб-сайте. Подарки, рекламы, гонки – здесь всегда что-то происходит! Присоединитесь к “риобет” и испытайте веселье активности тут и сейчас!
https://njkkot.org/?document_srl=259433
https://xn--hudfryngring-7ib.wiki/index.php/Spectehnikaleasing.ru
Крупнейшая в мире Букмекерская контора 1xbet
http://activasoft.com.br/index.php?title=Spectehnikaleasing.ru
https://adept.missouri.edu/groups/spectehnikaleasing-ru-839071267/
http://www.asystechnik.com/index.php/Spectehnikaleasing.ru
Хай всех фанатов живых забав! В данный момент я намерен поделиться вам о моем захватывающем путешествии в мир онлайн казино “казино с бонусом за регистрацию без депозита“. Это местечко, где каждый единичный может выявить что-то по вкусу: от захватывающих машин до обычных настольных игр. Но что по факту заставило меня задержаться здесь – это атмосфера веселья и привлечения, которая правит на сайте. Подарки, продвижения, турниры – здесь всегда что-то происходит! Присоединяйтесь к “зеркало риобет” и прочувствуйте счастье активности прямо сейчас!
1. Вибір натяжних стель: як вибрати ідеальний варіант?
2. Модні тренди натяжних стель на поточний сезон
3. Які переваги мають натяжні стелі порівняно зі звичайними?
4. Як підібрати кольори для натяжної стелі у квартирі?
5. Секрети догляду за натяжними стелями: що потрібно знати?
6. Як зробити вибір між матовими та глянцевими натяжними стелями?
7. Натяжні стелі в інтер’єрі: як вони змінюють приміщення?
8. Натяжні стелі для ванної кімнати: плюси та мінуси
9. Як підняти стеля візуально за допомогою натяжної конструкції?
10. Як вибрати правильний дизайн натяжної стелі для кухні?
11. Інноваційні технології виробництва натяжних стель: що варто знати?
12. Чому натяжні стелі вибирають для офісних приміщень?
13. Натяжні стелі з фотопринтом: які переваги цієї технології?
14. Дизайнерські рішення для натяжних стель: ідеї для втілення
15. Хімічні реагенти в складі натяжних стель: безпека та якість
16. Як вибрати натяжну стелю для дитячої кімнати: поради батькам
17. Які можливості для дизайну приміщень відкривають натяжні стелі?
18. Як впливає вибір матеріалу на якість натяжної стелі?
19. Інструкція з монтажу натяжних стель власноруч: крок за кроком
20. Натяжні стелі як елемент екстер’єру будівлі: переваги та недоліки
навісні стелі natjazhnistelifvgtg.lviv.ua .
generic prednisone for sale prednisone rx coupon buy prednisone no prescription
Acesse o site original do jogo Fortune Tiger
онлайн сервисы
LГҐn 7000 kr
amoxicillin 500mg buy online canada amoxicillin 500mg price amoxicillin 500 mg
Привет каждого приверженцев азартных развлечений! Сегодня я намерен рассказать вам о моем захватывающем перемещении в мир онлайн казино “бездепозитные промокоды казино“. Это пространство, где каждый из нас может найти что-то по выбору: от занимательных машин до традиционных настольных игр. Но что реально заинтересовало меня остановиться здесь – это атмосфера веселья и увеселения, которая правит на веб-сайте. Подарки, акции, состязания – здесь всегда что-то происходит! Присоединяйтесь к “riobet casino бонус код” и прочувствуйте веселье развлечения в данный момент!
https://pl.motorsport.com/driver/alexandre-cougnaud/830053/photo-galleries/
https://www.fiawec.com/fr/driver/1926
buying amoxicillin in mexico amoxicillin 500 coupon price for amoxicillin 875 mg
https://bo.fiawec.com/en/driver/media/1926
https://jp.motorsport.com/driver/alexandre-cougnaud/408164/photos/
Приветствую всех фанатов живых развлечений! В данный момент я собираюсь изложить вам о моем интересном путешествии в сфера онлайн казино “бездепозитный бонус“. Это локация, где каждый из нас может выявить что-то по вкусу: от захватывающих машин до стандартных настольных игр. Но что реально привело меня задержаться здесь – это атмосфера улыбок и привлечения, которая властвует на веб-сайте. Подарки, публичные мероприятия, турниры – здесь всегда что-либо происходит! Присоединяйтесь к “riobet 500 рублей” и почувствуйте счастье забавы прямо сейчас!
https://espanol.motorsport.com/driver/alexandre-cougnaud/622164/photo-galleries/
Эй, приятель! Так рад созидать тебя на нашем веб-сайте! Ну, а в случае если ты сомневаешься, для чего тебе копаться здесь, то выделяй, разберемся вместе.
Дело что, что мы здесь как твой самый близкий друг, практически постоянно готовы помочь! Не важно, что за приключение ты собираешься начать – будь то освоение свежей темы, разведка полезных советов или просто интерес к разным штукам – у нас ты посчитаешь все, собственно что нужно для вдохновения.
Помнишь, как лучший друг практически постоянно держит за руку и поддерживает? Итак вот, наш сайт – точно такой же! Мы не просто предоставляем информацию, мы делаем комьюнити, где тебе предоставляется возможность делиться своими идеями, дискуссировать принципиальные вопросы и просто чувствовать себя как дома.
https://www.mitsu.ro/forum_new/viewtopic.php?f=12&t=16751
И не забывай, что мы тут тебе 24/7! Как твой надежный друг, мы всегда вблизи, чтобы посодействовать для тебя освоиться в нашем мире познаний и возможностей.
И не медли, приятель мой! Загляни на наш сайт и погрузись в интересное путешествие по морю новых познаний и приключений! Мы уже ожидаем тебя здесь с распростертыми объятиями!
1. Вибір натяжних стель: як вибрати ідеальний варіант?
2. Модні тренди натяжних стель на поточний сезон
3. Які переваги мають натяжні стелі порівняно зі звичайними?
4. Як підібрати кольори для натяжної стелі у квартирі?
5. Секрети догляду за натяжними стелями: що потрібно знати?
6. Як зробити вибір між матовими та глянцевими натяжними стелями?
7. Натяжні стелі в інтер’єрі: як вони змінюють приміщення?
8. Натяжні стелі для ванної кімнати: плюси та мінуси
9. Як підняти стеля візуально за допомогою натяжної конструкції?
10. Як вибрати правильний дизайн натяжної стелі для кухні?
11. Інноваційні технології виробництва натяжних стель: що варто знати?
12. Чому натяжні стелі вибирають для офісних приміщень?
13. Натяжні стелі з фотопринтом: які переваги цієї технології?
14. Дизайнерські рішення для натяжних стель: ідеї для втілення
15. Хімічні реагенти в складі натяжних стель: безпека та якість
16. Як вибрати натяжну стелю для дитячої кімнати: поради батькам
17. Які можливості для дизайну приміщень відкривають натяжні стелі?
18. Як впливає вибір матеріалу на якість натяжної стелі?
19. Інструкція з монтажу натяжних стель власноруч: крок за кроком
20. Натяжні стелі як елемент екстер’єру будівлі: переваги та недоліки
львів натяжні стелі http://www.natjazhnistelifvgtg.lviv.ua .
Доступен транспорт эконом- и бизнес-
и Пассажирские перевозки минск люкс-классов.
My web blog – Аренда микроавтобуса с водителем
where to buy cheap clomid without insurance where to buy generic clomid tablets where can i buy cheap clomid
registrando-se em Site usuários Podem aproveitar
várias ofertas especiais que incluem bônus de boas-vindas, tvbet sazonal
promoções e exclusivo programas.
Here is my site; tvbet com
can i order generic clomid without a prescription how can i get generic clomid without dr prescription cheap clomid tablets
1. Вибір натяжних стель: як вибрати ідеальний варіант?
2. Модні тренди натяжних стель на поточний сезон
3. Які переваги мають натяжні стелі порівняно зі звичайними?
4. Як підібрати кольори для натяжної стелі у квартирі?
5. Секрети догляду за натяжними стелями: що потрібно знати?
6. Як зробити вибір між матовими та глянцевими натяжними стелями?
7. Натяжні стелі в інтер’єрі: як вони змінюють приміщення?
8. Натяжні стелі для ванної кімнати: плюси та мінуси
9. Як підняти стеля візуально за допомогою натяжної конструкції?
10. Як вибрати правильний дизайн натяжної стелі для кухні?
11. Інноваційні технології виробництва натяжних стель: що варто знати?
12. Чому натяжні стелі вибирають для офісних приміщень?
13. Натяжні стелі з фотопринтом: які переваги цієї технології?
14. Дизайнерські рішення для натяжних стель: ідеї для втілення
15. Хімічні реагенти в складі натяжних стель: безпека та якість
16. Як вибрати натяжну стелю для дитячої кімнати: поради батькам
17. Які можливості для дизайну приміщень відкривають натяжні стелі?
18. Як впливає вибір матеріалу на якість натяжної стелі?
19. Інструкція з монтажу натяжних стель власноруч: крок за кроком
20. Натяжні стелі як елемент екстер’єру будівлі: переваги та недоліки
ціна натяжних стель https://natjazhnistelifvgtg.lviv.ua/ .
celebrex medication
Vicecity Darknet Drugs Market
http://vicecitya4htlqf2msop4jt7lqhmbwkuml2c44gocklz6ucqkw5xitid.onion/
1. Вибір натяжних стель: як вибрати ідеальний варіант?
2. Модні тренди натяжних стель на поточний сезон
3. Які переваги мають натяжні стелі порівняно зі звичайними?
4. Як підібрати кольори для натяжної стелі у квартирі?
5. Секрети догляду за натяжними стелями: що потрібно знати?
6. Як зробити вибір між матовими та глянцевими натяжними стелями?
7. Натяжні стелі в інтер’єрі: як вони змінюють приміщення?
8. Натяжні стелі для ванної кімнати: плюси та мінуси
9. Як підняти стеля візуально за допомогою натяжної конструкції?
10. Як вибрати правильний дизайн натяжної стелі для кухні?
11. Інноваційні технології виробництва натяжних стель: що варто знати?
12. Чому натяжні стелі вибирають для офісних приміщень?
13. Натяжні стелі з фотопринтом: які переваги цієї технології?
14. Дизайнерські рішення для натяжних стель: ідеї для втілення
15. Хімічні реагенти в складі натяжних стель: безпека та якість
16. Як вибрати натяжну стелю для дитячої кімнати: поради батькам
17. Які можливості для дизайну приміщень відкривають натяжні стелі?
18. Як впливає вибір матеріалу на якість натяжної стелі?
19. Інструкція з монтажу натяжних стель власноруч: крок за кроком
20. Натяжні стелі як елемент екстер’єру будівлі: переваги та недоліки
оздоблення стелі https://www.natjazhnistelifvgtg.lviv.ua/ .
fr.pizdeca.cc
https://rosseriya.ru/254-chuzhoy-rebenok-1-sezon.html
https://rosseriya.ru/1055-princ-i-nischaja-1-sezon.html
Лучшее решение для вашей семьи
13. Дом из бруса 9х12: уединенное убежище
дома из бруса 9х12 https://domizbrusa9x12spb.ru/ .
Топ Букмекерская контора 1xbet
https://rosseriya.ru/494-chernyy-cvetok-1-sezon.html
zithromax z-pak price without insurance zithromax for sale 500 mg buy cheap generic zithromax
Надежная Букмекерская контора для ставок 1xbet
Че, компаньон! Ты ищешь дельную инфу про то, зачем для тебя возиться на нашем веб-сайте? Окей, держи фишку!
Слушай, здесь у нас не просто вебсайт, это кладезь знаний, где тебе предоставляется возможность выжать всю соковитую инфу, собственно что только попытаешься! Эй, ну да мы как те уличные братки, представляешь ли, всегда подскажем, как выручить тебя из каждой капусты.
https://stopviolenta.md/galerie-media/galerie-foto/203-modul-i-sesiune-doi-pentru-psihologi-20-23-februarie-2019.html
Здесь на каждом углу – инструкции, рекомендации, рецепты, ну да собственно что угодно! Не имеет никакого значения, че ты штудируешь – кулинарию, программирование, фитнес либо философию. У нас есть все варианты, как в кармане у грамотного философа.
А, и как мы запямытовали сказать, дружище, наш сайт это не столько информация, это и связь с реальными профи! Здесь тебе предоставляется возможность задавать свои вопросы, делиться средствами находками, дискуссировать важные темы с такими же заинтересованными братками, как ты.
И не теряй время, давай, заскакивай к нам на вебсайт и бросься в мир знаний и общения, который мы тебе приготовили! Так как кто знает, имеет возможность, здесь тебе откроются двери в новую жизнь, как в фильмах!
Купить сигареты дешево
услуги адвоката трудовой
стоимость услуг юриста в арбитражном суде москва
арбитражный юрист
консультация юриста по трудовому законодательству
Купить сигареты блоками дешево
Место для отдыха и вдохновения
14. Модный дом из бруса 9х12: стиль и качество
дом из бруса 9х12 https://domizbrusa9x12spb.ru/ .
цена услуги юриста недвижимости
трудовой юрист консультация москва
арбитражный адвокат стоимость услуг
http://stomuzlovskoe.ru
https://pipms.wiki/User:Lane6216592601
юрист по трудовым спорам
https://viet-space.com/groups/myactiveenglish-ru/
адвокат по вопросам недвижимости
https://advokatstepnov.ru/
https://procesal.cl/index.php/User:AndrewJanney6
юридическая консультация арбитраж
Самая надежная Букмекерская контора для ставок 1xbet
юрист по арбитражным спорам в суде
Топ Букмекерская контора для ставок1xbet
вопрос к юристу по недвижимости бесплатно
https://menwiki.men/wiki/User:TyrellXus6
https://menwiki.men/wiki/Myactiveenglish.ru
Современная потолочная люстра для гостиной люстра для спальни освещение кухни может быть затемнением приложения с помощью пульта дистанционного управления акриловый материал завод прямых продаж лампа люстра потолочная круглая плоская большая
https://www.telix.pl/forums/users/ramonajonathan5/
https://telugusaahityam.com/User:RodrickSills86
Thank you for great information. Hello Administ . 国产线播放免费人成视频播放
Современное жилье для ценителей комфорта
15. Дом из бруса 9х12: гармония с природой
дома из бруса 9х12 https://domizbrusa9x12spb.ru/ .
https://qanda.findpetlove.com/question/myactiveenglish-ru/
Um dos melhores jogos Fortune Tiger
zithromax antibiotic zithromax 250 mg tablet price zithromax 600 mg tablets
Самая надежная Букмекерская контора для ставок №1 1xbet
Суперская Букмекерская контора 1xbet
Simply desire to say your article iss as surprising.
The clarit in your post is simply nice and i coulkd assumee
you’re ann expert on thiis subject. Well with your permission let mme
tto grab your RSS feed tto kkeep updated with forthcoming
post. Thanks a million and please keep up the rewarding work.
My homepage 카지노사이트
video
Its like you read my mind! You seem to know a lot abbout this, like you wrote thee book in it or something.
I thijk that you could do with some pics to drive the message home a little bit, but other than that, this iis wonderful blog.
A great read. I will definitely be back.
my web page; 카지노사이트
Самая надежная Букмекерская контора №1 1xbet
800 Euro Kredit
Лучшая Букмекерская контора 1xbet
Mer
חטובות ויפות,שכל מה שהן רוצות זה רק לספק אתכם. אבל למה לדמיין, שאפשר ליווי בפתח תיקווה והסביבה משלב עבורכם את הפתרון המושלם. בפורטל אקספיינדר, תוכלו להנות ממגוון רחב של נערות ליווי בפתח תקווה מאווירה נעימה ורומנטית המאפשרת הרגעות מכל הלחצים והרעשים נערת ליווי במרכז
can you buy zithromax over the counter in mexico generic zithromax over the counter cheap zithromax pills
תקווה. הדירות מפוזרות ברחבי העיר במקומות דיסקרטיים ומעורבבים כתובות, טלפונים וניווט שיביא אתכם היישר לעונג בא לכם להיכנס להרפתקה דיסקרטית ומענגת שתשאיר לכם טעם של עוד? הגיע הזמן שתממשו את לאירועים מסיבות וכל דבר העולה בדמיונכם. נערות הליווי מכירות דירה דיסקרטית במרכז
Um dos melhores jogos para ganhar Fortune Tiger
Техподдержка клуба – на самом высоком классе, ведь в ценности входит положительный опыт взаимодействия как с зарегистрированными.
נערות הליווי בהוד השרון מעניקות שירות באיכות גבוהה. הן בעלות מראה סקסי מטופחות ולבושות היטב. רובן באתר ברמה הגבוהה ביותר בארץ. אתר המובייל שלנו מאתר עבורכם מודעות זמינות באזורכם על בסיס מיקום. כל הטלפונים של משרדי הליווי באתר שליטה עבד ומלכה, עיסוי ארוטי סקס זונות
понятный интерфейс и игровой
процесс, который разбавляется особыми знаками, мфмфвф дополнительными уровнями и множителями.
my web blog; casino. vavada.
Great post thank you. Hello Administ . 国产线播放免费人成视频播放
Самая надежная Всем рекомендую Букмекерскую контору №1 1xbet
Самая надежная Букмекерская контора 1xbet
clomid cost cost of clomid pills buy cheap clomid without dr prescription
Здравствуйте, ценители азартных приключений! Предлагаю поделиться своим великолепием от онлайн казино “1win скачать ios”. Это не просто сайт для игр, это абсолютный космос волнения и забав! Здесь я обрел все, что мне нужно: разнообразие игр, щедрые бонусы и скоростные выплаты. Но основное – это настроение, которая преобладает здесь. Виртуально-реальные приключения, удивительные турниры и дружелюбное сообщество игроков делают каждую игру неизученной! Соединяйтесь к “1win акции” и окунитесь в мир увлекательных развлечений!
you must find it between the drawers of your refrigerator, in the upper left
or corner of the haf qin samsung fridge water filter in freezer or to the refrigerator
door.
Here is my web site – water filter for samsung fridge
for users interested in this issue who need a mobile service,
the Lalibet lalibet appapplication becomes more interesting method personalization, and gives similar entire set
of functions as on the main site.
My blog :: lalibet betting ethiopia
zithromax pill buy zithromax 500mg online buy zithromax 500mg online
Всем рекомендую Букмекерскую контору №1 1xbet
Самая лучшая Букмекерская контора 1xbet
воєнторг
8. Спецпредложения для военных
магазин тактичного одягу магазин військового спорядження київ .
Готовьтесь к безумию: Американское правительство предупреждает о солнечном затмении, грозящем нарушить все. Сумки для выживания, заполненные секретами, мобильными телефонами и компасами, становятся нормой. Откройте правду в нашем захватывающем видео! https://vm.tiktok.com/ZGemYu97R/
воєнторг
10. Распродажа военного снаряжения
інтернет магазин тактичного одягу вийськовий магазин .
ontdek deze info hier
Alguns códigos são simples dicas baixar lampionsbet de outros
usuários. Por exemplo, uma partida de futebol virtual tem capacidade esticar
apenas 3 minutos comparado com 90 minutos de uma partida real.
my web site :: lampionsbet. com
Good way of describing, and good article to get information regarding my presentation focus, which i am going to present in university.
my blog post; orlando video production company (5alij.com)
воєнторг
3. Как выбрать снаряжение для военных
магазин військового спорядження київ інтернет магазин військового одягу .
воєнторг
9. Купить военные товары онлайн
магазин тактичного одягу інтернет магазин військової форми .
amoxicillin online canada purchase amoxicillin online amoxicillin over the counter in canada
Payday loans in Alabama
Nissan Pathfinder Years To Avoid
Привет, поклонники захватывающих приключений! Желаю обмениваться своим великолепием от виртуального заведения “1вин”. Это не просто площадка для игр, это абсолютный вселенная чувств и увлечений! Здесь я обрел все, что мне нужно: многообразие игр, обильные бонусы и скоростные выплаты. Но самое – это обстановка, которая царит здесь. Имитированные приключения, удивительные турниры и милосердное сообщество игроков делают каждую игру беззабвенной! Присоедините к “1 win” и окунитесь в область занимательных развлечений!
can you buy prednisone over the counter prednisone prescription for sale prednisone 20mg capsule
Представляю Букмекерскую контору №1 1xbet
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Hizmeti Skype : live:by_umut
1. Почему берцы – это обязательный элемент стиля?
2. Как выбрать идеальные берцы для осеннего гардероба?
3. Тренды сезона: кожаные берцы или замшевые?
4. 5 способов носить берцы с платьем
5. Какие берцы выбрать для повседневного образа?
6. Берцы на платформе: комфорт и стиль в одном
7. Какие берцы будут актуальны в этом году?
8. Маст-хэв сезона: военные берцы в стиле милитари
9. 10 вариантов сочетания берцов с джинсами
10. Зимние берцы: как выбрать модель для холодного сезона
11. Элегантные берцы на каблуке: идеальный вариант для офиса
12. Секреты ухода за берцами: как сохранить первоначальный вид?
13. С какой юбкой носить берцы: советы от стилистов
14. Как подобрать берцы под фасон брюк?
15. Берцы на шнуровке: стильный акцент в образе
16. Берцы-челси: универсальная модель для любого стиля
17. С чем носить берцы на плоской подошве?
18. Берцы с ремешками: акцент на деталях
19. Как выбрать берцы для прогулок по городу?
20. Топ-5 брендов берцев: качество и стиль в одном
купити берці зсу берці купити .
Thank you for great article. Hello Administ .Seo Hizmeti Skype : live:by_umut
Моя рекомендация – Букмекерская контора №1 1xbet
לעשות ולא הספקתם עם אשת חלומותיכם? מתי הפעם האחרונה שקיבלתם את הלילה שתמיד חלמתם? מה לחות עם מרכזי הקניות הגדולים ביותר במזרח התיכון ולא רק זה באילת כמו שבאילת יש את נערות ליווי הכי שוות ויפות שתוכלו רק לדמיין יש ליווי לעיסוי ועוד פינוקים אחרים. דירות דירות סקס בירושלים
Calibration Measuring Equipment For Sale
הדירה העונה לצרכים שלכם מרימים טלפון בכל רגע נתון ואתם כבר בדרך לדירה. בדירות לחדר במלון, או שאתם תגיעו אליהן לדירותיהן הדיסקרטיות והמאובזרות להפליא. שירותי ליווי באקספיינדר הפורטל המוביל בישראל מחפש שירותי דיסקרטיות בבת ים הפזורות בכל רחבי העיר. נערת ליווי בירושלים
Enjoying great demand from endless number of players for own excellent reputation in the market, we strive find out if should a relatively old establishment relevant compete with casino slottica of high class.
duloxetine 100/30 cost
אקספיינדר הגדול במדינה ולהזמין מתוך מאגר המודעות המעודכן את נערות הליווי בחיפה והקריות. כאן תגשימו חלום איתן גדול, ועוד. הדוגמניות נבחרו על ידי אקספיינדר בהקפדה. כולן זמינות עבורכם במהלך כל שעות היממה וישמחו להתלוות אליכם ולענג אתכם וסודית. דירות דירה דיסקרטית רחובות
KingSize מפנק ומצעים ריחניים, נקיים ונעימים. בצמוד ניתן למצוא מקלחת מאובזרת עם תמרוקים אקסולוסיביים יום לכך. כל מה שנותר עכשיו זה לברר עם עצמך מה בדיוק היית רוצה מנערת חלומותיך לעיסוי ארוטי בעפולה – מבנה מסוים, אווירה מדויקת, לך עיסוי מטריף חושים על מנת דירות דיסקרטיות ברחובות
1. Почему берцы – это обязательный элемент стиля?
2. Как выбрать идеальные берцы для осеннего гардероба?
3. Тренды сезона: кожаные берцы или замшевые?
4. 5 способов носить берцы с платьем
5. Какие берцы выбрать для повседневного образа?
6. Берцы на платформе: комфорт и стиль в одном
7. Какие берцы будут актуальны в этом году?
8. Маст-хэв сезона: военные берцы в стиле милитари
9. 10 вариантов сочетания берцов с джинсами
10. Зимние берцы: как выбрать модель для холодного сезона
11. Элегантные берцы на каблуке: идеальный вариант для офиса
12. Секреты ухода за берцами: как сохранить первоначальный вид?
13. С какой юбкой носить берцы: советы от стилистов
14. Как подобрать берцы под фасон брюк?
15. Берцы на шнуровке: стильный акцент в образе
16. Берцы-челси: универсальная модель для любого стиля
17. С чем носить берцы на плоской подошве?
18. Берцы с ремешками: акцент на деталях
19. Как выбрать берцы для прогулок по городу?
20. Топ-5 брендов берцев: качество и стиль в одном
берці військові військові берці зсу .
Thank you great post. Hello Administ .Seo Hizmeti Skype : live:by_umut
Моя рекомендация – Букмекерская контора №1 в мире 1xbet
Легендарная Букмекерская контора 1xbet
воєнторг
17. Специальные предложения для армии
воєнний магазин київ військовий магазин київ .
buying clomid without prescription can i purchase clomid no prescription where to get cheap clomid
Gogo Casino är känt för enkelhet och snabbhet, och deras logotyp är inget undantag. Logotypen för detta populära onlinecasino har en glad och färgglad design som passar perfekt med deras innovativa och underhållande spelupplevelse.
Den blГҐa och rosa logotypen i stil med en bubbla eller moln fГ¶r tankarna till en lekfull och modern kГ¤nsla. De stiliserade bokstГ¤verna i namnet “Gogo” bildar en tydlig och iГ¶gonfallande grafik som lГ¤tt kan kГ¤nnas igen. Denna logotyp Г¤r inte bara snygg och unik, den kommunicerar ocksГҐ perfekt med Gogo Casinos varumГ¤rkesidentitet som ett roligt och prisvГ¤rt onlinecasino.
Många spelare känner igen och uppskattar den ljusa och välbearbetade logotypen för Gogo Casino, vilket gör den till en viktig del av deras varumärkesstrategi. Logotypen är en viktig del av varje casinos image och kan hjälpa till att bygga upp en positiv känsla hos spelare och skapa en stark koppling till varumärket.
Sammanfattningsvis är Gogo Casinos logotyp en välgjord grafisk representation av deras varumärke som lyckas kommunicera deras identitet som ett enkelt, roligt och modernt onlinecasino. Med sin lekfulla design och färgglada estetik är logotypen för Gogo Casino en framgångsrik del av deras varumärkesstrategi och en viktig faktor i deras popularitet bland spelare.
https://gogocasino.one
Gogo Casino är ett av de populäraste onlinekasinona för svenska spelare. För att kunna spela och njuta av alla deras spännande spel och kampanjer måste man logga in på sitt spelkonto. Att logga in på Gogo Casino är väldigt enkelt och smidigt.
För att logga in på Gogo Casino behöver du bara gå till deras hemsida och klicka på “Logga in”-knappen längst upp till höger på sidan. Därefter kommer du att bli ombedd att ange ditt användarnamn och lösenord som du skapade när du registrerade dig för ett konto.
Om du inte har ett konto på Gogo Casino ännu, kan du enkelt registrera dig genom att klicka på “Skapa konto”-knappen och följa de enkla stegen för att skapa ett konto. När du har registrerat dig och loggat in på ditt konto kommer du att ha tillgång till alla deras fantastiska spel och kampanjer.
Så om du är redo för en spännande spelupplevelse och vill ha chansen att vinna stora vinster, är det dags att logga in på Gogo Casino och börja spela redan idag! Lycka till!
https://gogocasino.one
Gogo Casino bonus är en spännande möjlighet för spelare att öka sina vinstchanser och maximera sin spelupplevelse. Denna onlinekasinobonus ger spelare möjligheten att få extra pengar att spela för, vilket kan öka deras chanser att vinna stort.
För att ta del av Gogo Casino bonus krävs det att spelaren registrerar sig på kasinots webbplats och gör en insättning. Därefter kommer de att bli belönade med en bonussumma som de kan använda för att spela sina favoritspel. Det är viktigt att läsa villkoren för bonusen noggrant för att förstå hur den fungerar och vilka regler och krav som gäller.
En av fördelarna med att använda en kasinobonus är att det ger spelare möjligheten att prova nya spel och upptäcka nya favoriter utan att riskera sina egna pengar. Bonusen ger också spelare chansen att öka sin vinstchans eftersom de har mer pengar att spela för.
Det är dock viktigt att komma ihåg att kasinobonusar oftast har ett omsättningskrav, vilket innebär att spelarna måste satsa en viss summa pengar innan de kan ta ut sina vinster. Det är därför viktigt att läsa de specifika reglerna och villkoren för bonusen för att undvika missförstånd och obehagliga överraskningar.
Gogo Casino bonus är en spännande möjlighet för spelare att öka sina vinstchanser och ha ännu mer kul när de spelar sina favoritspel online. Genom att utnyttja denna bonus kan spelare få en riktigt bra start på sitt speläventyr och förhoppningsvis ta hem stora vinster. Så varför inte prova lyckan och ta del av Gogo Casino bonus redan idag? Lycka till!
https://gogocasino.one
Gogo casino com är en populär online kasino där spelare kan njuta av en mängd olika spel direkt från sina datorer eller mobila enheter. Med ett brett utbud av spelautomater, bordsspel, live dealer-spel och mer, finns det något för alla på Gogo casino com.
En av de främsta fördelarna med att spela på Gogo casino com är den stora variationen av spel som erbjuds. Spelare kan välja mellan hundratals olika spel från de bästa spelleverantörerna i branschen, inklusive NetEnt, Microgaming och Betsoft. Oavsett om du föredrar klassiska spelautomater, progressiva jackpottar eller live dealer-spel, har Gogo casino com något som passar din smak.
Utöver det breda utbudet av spel erbjuder Gogo casino com också generösa bonusar och kampanjer för sina spelare. Nya spelare kan dra nytta av välkomstbonusar och gratissnurr när de registrerar sig och gör sin första insättning. Dessutom erbjuder kasinot regelbundna kampanjer och tävlingar för att belöna lojala spelare och ge dem chansen att vinna stora priser.
Att spela på Gogo casino com är inte bara roligt, det är också säkert och pålitligt. Kasinot drivs av en licensierad operatör och använder den senaste krypteringstekniken för att skydda spelarnas personliga och finansiella information. Spelare kan lita på att deras uppgifter är säkra och att spelen är rättvisa och slumpmässiga.
Sammanfattningsvis är Gogo casino com en utmärkt destination för alla som letar efter en spännande och underhållande spelupplevelse online. Med sitt stora utbud av spel, generösa bonusar och säkra plattform är det lätt att förstå varför så många spelare väljer att spela på Gogo casino com. Besök kasinot idag och upptäck allt det har att erbjuda!
https://gogocasino.one
Купить диплом в Рязани недорого – с доставкой по регионах, по приятной цене, без предоплаты http://diploms-service.com/diplomy-po-gorodam/moskva/rgteu
осуществляйте просмотр порно porno sex hot indonesia terbaru, бесплатные интим ролики дистанционно в изумительном качестве и скачивайте на отличной.
Feel free to surf to my page https://europos.by/derzhateli_informatsii/cennikoderzateli-dbr/cennikoderzatel-polocnyj-samokleasijsa-vysotoj-52-mm
1. Почему берцы – это обязательный элемент стиля?
2. Как выбрать идеальные берцы для осеннего гардероба?
3. Тренды сезона: кожаные берцы или замшевые?
4. 5 способов носить берцы с платьем
5. Какие берцы выбрать для повседневного образа?
6. Берцы на платформе: комфорт и стиль в одном
7. Какие берцы будут актуальны в этом году?
8. Маст-хэв сезона: военные берцы в стиле милитари
9. 10 вариантов сочетания берцов с джинсами
10. Зимние берцы: как выбрать модель для холодного сезона
11. Элегантные берцы на каблуке: идеальный вариант для офиса
12. Секреты ухода за берцами: как сохранить первоначальный вид?
13. С какой юбкой носить берцы: советы от стилистов
14. Как подобрать берцы под фасон брюк?
15. Берцы на шнуровке: стильный акцент в образе
16. Берцы-челси: универсальная модель для любого стиля
17. С чем носить берцы на плоской подошве?
18. Берцы с ремешками: акцент на деталях
19. Как выбрать берцы для прогулок по городу?
20. Топ-5 брендов берцев: качество и стиль в одном
купити тактичні берці берці тактичні купити .
Det har kommit upprepade rapporter om att Gogo Casino inte betalar ut vinster till sina spelare. Många spelare har upplevt problem med att få sina pengar och känner sig frustrerade och lurade av detta onlinecasino.
Enligt flera källor har spelare försök att ta ut sina vinster från Gogo Casino endast för att bli nekade eller ha sina utbetalningar fördröjda i flera veckor. Detta har självklart skapat stor upprördhet bland spelarna som förväntar sig att få ut sina vinster i tid.
Det är viktigt att komma ihåg att alla onlinecasinon måste följa lagar och regler när det kommer till utbetalningar och spelarsäkerhet. Om Gogo Casino inte lever upp till dessa krav kan det leda till konsekvenser för dem.
För att undvika att bli lurad av ett casino är det alltid viktigt att göra noggrann research innan man börjar spela. Man bör kolla recensioner, licenser och andra spelares erfarenheter för att se till att man väljer ett pålitligt och säkert casino.
Om man redan har hamnat i en situation där man inte får ut sina vinster från Gogo Casino eller något annat casino är det viktigt att kontakta kundtjänsten och begära en förklaring. Om problemet inte kan lösas på ett tillfredsställande sätt kan man vända sig till de relevanta myndigheterna för att få hjälp.
Slutligen är det viktigt att komma ihåg att spel ska vara roligt och underhållande, men det är också viktigt att vara medveten om potentiella risker och vara försiktig när man spelar online. Man bör alltid spela ansvarsfullt och vara medveten om sina rättigheter som spelare.
https://gogocasino.one
Gogo Casino är ett online casino som erbjuder sina spelare möjligheten att spela en rad olika casinospel direkt i webbläsaren. Ett av de viktigaste fördelarna med att spela på Gogo Casino är deras smidiga och snabba utbetalningsprocess.
När det är dags att ta ut dina vinster från Gogo Casino kan du vara säker på att processen kommer att vara enkel och effektiv. För att begära en utbetalning behöver du bara gå till ditt spelkonto och välja önskat utbetalningssätt. Gogo Casino erbjuder flera olika alternativ för utbetalningar, inklusive banköverföring, e-plånbok och Trustly.
En av de största fördelarna med att använda Trustly för utbetalningar är att pengarna vanligtvis når ditt konto inom några minuter efter att du begärt uttaget. Detta är betydligt snabbare än många andra casinon på marknaden, där det kan ta upp till flera dagar innan pengarna når ditt konto.
För att säkerställa att utbetalningen går smidigt och snabbt är det viktigt att du har verifierat ditt spelkonto hos Gogo Casino. Detta innebär att du kan behöva skicka in dokument som bevisar din identitet och hemadress. Detta kan vara något irriterande, men det är också ett viktigt steg för att säkerställa att dina pengar hamnar på rätt plats.
Sammanfattningsvis kan man säga att Gogo Casino erbjuder en snabb och effektiv utbetalningsprocess för sina spelare. Med flera olika utbetalningsalternativ att välja mellan och snabba transaktioner med Trustly, kan du vara säker på att dina vinster når dig på nolltid. Så om du är ute efter en bra utbetalningsupplevelse, är Gogo Casino definitivt ett bra val.
https://gogocasino.one
Gogo Casino har blivit ett populärt val för många spelare tack vare sitt enkla gränssnitt och snabba uttagsmetoder. Men det verkar finnas vissa problem när det gäller att göra uttag från casinot.
Många spelare har rapporterat att de har haft svårigheter med att få sina vinster utbetalade från Gogo Casino. Vissa har upplevt långa väntetider och komplikationer när de försöker ta ut sina pengar. Det har även rapporterats att vissa spelare har haft sina uttag helt nekade utan någon förklaring.
Det är viktigt för spelare att känna sig trygga när de spelar på ett online casino och att de kan lita på att deras vinster kommer att betalas ut utan problem. Om det finns problem med att göra uttag kan det vara en varningssignal för spelare att vara försiktiga.
Det är oklart vad som orsakar dessa problem med uttag på Gogo Casino och det är viktigt att casinot tar itu med dessa frågor och ser till att spelarna får sina pengar på ett smidigt och effektivt sätt. Spelare bör vara medvetna om dessa problem vid uttag och vara försiktiga med att sätta in pengar på casinon där det finns rapporter om problem med uttag.
https://gogocasino.one
order amoxicillin no prescription amoxicillin 500mg capsule cost amoxicillin brand name
Купить диплом в Рязани недорого – с доставкой по регионах, по приятной цене, без предоплаты http://diploms-service.com/diplomy-po-gorodam/sankt-peterburg/natsionalnyj-otkrytyj-institut-rossii-g-sankt-peterburg
1. Почему берцы – это обязательный элемент стиля?
2. Как выбрать идеальные берцы для осеннего гардероба?
3. Тренды сезона: кожаные берцы или замшевые?
4. 5 способов носить берцы с платьем
5. Какие берцы выбрать для повседневного образа?
6. Берцы на платформе: комфорт и стиль в одном
7. Какие берцы будут актуальны в этом году?
8. Маст-хэв сезона: военные берцы в стиле милитари
9. 10 вариантов сочетания берцов с джинсами
10. Зимние берцы: как выбрать модель для холодного сезона
11. Элегантные берцы на каблуке: идеальный вариант для офиса
12. Секреты ухода за берцами: как сохранить первоначальный вид?
13. С какой юбкой носить берцы: советы от стилистов
14. Как подобрать берцы под фасон брюк?
15. Берцы на шнуровке: стильный акцент в образе
16. Берцы-челси: универсальная модель для любого стиля
17. С чем носить берцы на плоской подошве?
18. Берцы с ремешками: акцент на деталях
19. Как выбрать берцы для прогулок по городу?
20. Топ-5 брендов берцев: качество и стиль в одном
берці ціна тактичні берці купити .
Gogo casino Г¤r en populГ¤r online spelplattform dГ¤r spelare kan njuta av en mГ¤ngd olika casinospel. Nyligen har de lanserat en ny funktion som heter “transparent horizontal” vilket gГ¶r spelupplevelsen Г¤nnu mer spГ¤nnande och engagerande.
Med den transparenta horisontella funktionen kan spelarna uppleva spelet på ett nytt sätt. Istället för att skärmen är statisk och endast visar spelplanen, kan spelarna nu se hela bakgrunden medan de spelar. Detta skapar en mer realistisk och interaktiv upplevelse för spelarna och gör att de känner sig ännu mer engagerade i spelet.
Den transparenta horisontella funktionen är speciellt användbar när spelare spelar live casino spel, då det skapar en känsla av att vara på ett riktigt casino. Spelarna kan se hela spelbordet och känna atmosfären av ett riktigt casino, vilket gör spelandet ännu mer spännande och underhållande.
Gogo casino strävar alltid efter att förbättra spelupplevelsen för sina spelare och den transparenta horisontella funktionen är ett steg i den riktningen. Genom att erbjuda spelare en mer realistisk och interaktiv spelupplevelse, gör de att spelarna kommer tillbaka för mer och fortsätter att njuta av allt som Gogo casino har att erbjuda.
Sammanfattningsvis är den transparenta horisontella funktionen på Gogo casino ett fantastiskt tillskott som kommer att göra spelupplevelsen ännu mer spännande och engagerande för spelare. Med denna nya funktion kan spelare njuta av sina favoritspel på ett nytt sätt och uppleva spänningen av ett riktigt casino direkt från sina egna hem.
https://gogocasino.one
Gogo Casino Bluff är en term som har kommit att användas allt oftare inom spelvärlden, särskilt när det gäller onlinecasinon. Bluffen handlar om att spelare får löften om stora vinster och bonusar, men i själva verket är casinot inte ärligt och manipulerar spelen för att spelarna ska förlora sina pengar.
Det finns flera varningssignaler som man kan vara uppmärksam på för att undvika att bli lurad av ett så kallat gogo casino bluff. En av de vanligaste är att casinot erbjuder orealistiskt höga bonusar och vinster, vilket ofta är för bra för att vara sant. Dessutom kan spelarna upptäcka att spelen är manipulerade och att det är svårt att vinna.
För att undvika att bli lurad av ett gogo casino bluff är det viktigt att vara försiktig och skeptisk när man väljer ett onlinecasino att spela på. Det är bra att göra research och läsa recensioner från andra spelare för att få en bättre uppfattning om casinots rykte och pålitlighet.
Det finns många seriösa onlinecasinon som erbjuder en trygg och rättvis spelupplevelse för sina spelare. Genom att vara uppmärksam på varningssignaler och göra en noggrann undersökning kan man undvika att bli lurad av ett gogo casino bluff och istället njuta av en rolig och spännande spelupplevelse.
https://gogocasino.one
Моя рекомендация – Букмекерская контора №1 1xbet
Gogo Casino är ett av de senaste tillskotten till den svenska casinomarknaden. Med sitt enkla och användarvänliga gränssnitt har de snabbt blivit populära bland spelare. Men hur fungerar det när det kommer till uttag och hur upplever spelare sina erfarenheter?
Många spelare har delat med sig av sina erfarenheter på olika forum, bland annat på sajter som Flashback. En del har berättat att uttagen på Gogo Casino går snabbt och smidigt, medan andra har fått vänta längre än vad som utlovats. En del har även upplevt problem med verifiering av sina konton, vilket har försenat uttagen ytterligare.
Det är viktigt att komma ihåg att alla casinon har olika rutiner och processer för uttag. Vissa casinon kräver mer verifiering än andra för att säkerställa att spelarna är över 18 år och inte bedriver bedrägeri. Det kan därför vara bra att läsa på villkoren för uttag på Gogo Casino för att veta vad som krävs för att få ut pengarna på ett smidigt sätt.
Sammanfattningsvis verkar det som att majoriteten av spelarna på Gogo Casino är nöjda med sina uttag och upplever en bra service. Däremot finns det enstaka fall där spelare har haft problem och fått vänta längre än vad som var förväntat. Det bästa tipset är därför att vara noggrann med att läsa villkoren och kontakta kundtjänsten om det skulle uppstå några problem.
https://gogocasino.one
Gogo Casino är en popular online casino som erbjuder spelare en enkel och transparent spelupplevelse. Med sitt transparenta horisontella designkoncept, gör Gogo Casino det lätt för spelare att navigera och hitta sina favoritspel snabbt och enkelt.
Den horisontella layouten skapar en ren och modern estetik som gör det enkelt att se alla spel som erbjuds på en överblick. Dessutom ger den transparenta designen spelare en känsla av öppenhet och ärlighet när de spelar på casinot.
Gogo Casino erbjuder ett brett utbud av casinospel, inklusive slots, bordsspel och live dealer-spel. Med sin responsiva plattform kan spelare njuta av sina favoritspel bГҐde pГҐ datorn och mobilen.
För de som letar efter en casino-upplevelse som är enkel, transparent och säker, är Gogo Casino det perfekta valet. Med sin horisontella design och stora spelutbud, är detta online casino definitivt värt att prova. Besök Gogo Casino idag och upplev den transparenta spelupplevelsen själv.
https://gogocasino.one
Gogo Casino är en populär online casino som erbjuder spelare en spännande och underhållande spelupplevelse. För att säkerställa att spelarna har den bästa möjliga upplevelsen har Gogo Casino en dedikerad kundtjänstavdelning som är tillgänglig för att hjälpa spelarna med eventuella frågor eller problem de kan ha.
Gogo Casino kundtjänst är tillgänglig via livechatt, e-post och telefon dygnet runt, vilket innebär att spelarna kan få hjälp när som helst på dygnet. Kundtjänstteamet består av vänliga och kunniga medarbetare som är beredda att assistera spelarna på ett professionellt och effektivt sätt.
Oavsett om spelarna har problem med insättningar eller uttag, behöver hjälp att förstå reglerna för ett specifikt spel eller helt enkelt vill ha mer information om kampanjer och erbjudanden, är Gogo Casino kundtjänst där för att hjälpa till. Spelarna kan vara säkra på att de får den bästa service och support, så att de kan njuta av sin spelupplevelse till fullo.
Sammanfattningsvis är Gogo Casino kundtjänst tillgänglig dygnet runt för att stödja spelarna och se till att de har en positiv och problemfri spelupplevelse. Med en dedikerad och professionell kundtjänstavdelning kan spelarna känna sig trygga och säkra när de spelar på Gogo Casino.
https://gogocasino.one
Gogo Casino är en spännande onlinecasino som nyligen lanserades på marknaden. Med sitt färgglada och lekfulla tema har Gogo Casino snabbt blivit en favorit bland svenska spelare. En stor del av Gogo Casinos framgång kan tillskrivas dess unika och igenkännbara logotyp.
Logotypen för Gogo Casino är en stiliserad G som är designad för att sticka ut och fånga uppmärksamheten hos spelarna. Den lyckas verkligen skilja sig från mängden och skapar en stark varumärkesidentitet för casinot.
Med sin enkla men iögonfallande design ger Gogo Casinos logotyp ett intryck av lekfullhet och spänning. Den ljusa färgsättningen och den stiliserade formen gör logotypen lätt att känna igen och komma ihåg.
Genom att använda logotypen konsekvent i all sin marknadsföring, skapar Gogo Casino en stark koppling mellan varumärket och dess spelare. Logotypen har blivit en symbol för casinots spännande och underhållande spelupplevelse.
Gogo Casinos logotyp är verkligen en viktig del av casinots framgång och har hjälpt till att skapa en stark varumärkesidentitet för casinot. Med sin unika design och igenkännbara utseende kommer logotypen säkert att fortsätta vara en viktig del av Gogo Casinos marknadsföringsstrategi i framtiden.
https://gogocasino.one
Gogo Casino är en populär online casino som erbjuder spelare en spännande och underhållande spelupplevelse. Här kan man njuta av ett brett utbud av casinospel, från klassiska slots till bordsspel och live casino.
En sak som skiljer Gogo Casino från andra online casinon är deras enkla och användarvänliga gränssnitt. Hemsidan är lätt att navigera och det är lätt att hitta de spel man är intresserad av att spela.
Ett annat positivt drag med Gogo Casino är deras generösa välkomstbonus för nya spelare. Det finns också regelbundna kampanjer och erbjudanden för befintliga spelare, vilket gör att man kan få extra belöningar och förmåner när man spelar på casinot.
En annan fördel med Gogo Casino är att de erbjuder snabba och säkra betalningsmetoder. Man kan göra insättningar och uttag på ett smidigt sätt, vilket gör att man kan njuta av sina vinster utan krångel.
Sammanfattningsvis är Gogo Casino ett utmärkt val för spelare som letar efter en pålitlig och rolig spelplattform. Med sitt stora spelutbud, generösa bonusar och bekväma betalningsmetoder, är det verkligen värt att ge detta casino en chans.
https://gogocasino.one
Легендарная Букмекерская контора №1 1xbet
Gogo Casino affiliates är ett partnerskapsprogram som erbjuds av Gogo Casino, ett populärt online casino som erbjuder ett brett utbud av spel och kampanjer. Genom att bli en affiliate kan man tjäna pengar genom att marknadsföra Gogo Casino till nya spelare.
Att vara en Gogo Casino affiliate innebär att man marknadsför casinot på olika sätt, till exempel genom att dela speciella erbjudanden och kampanjer på sociala medier, bloggar eller andra plattformar. Genom att locka nya spelare till Gogo Casino och få dem att registrera sig och spela på casinot kan man tjäna en andel av intäkterna som genereras av de spelare man har lockat till casinot.
Fördelarna med att vara en Gogo Casino affiliate inkluderar möjligheten att tjäna bra med pengar genom provisioner, flexibiliteten att arbeta när och var man vill samt den möjlighet som erbjuds att marknadsföra ett populärt och pålitligt online casino.
För att bli en affiliate hos Gogo Casino behöver man registrera sig på deras affiliatesida och följa instruktionerna för att komma igång. Man behöver också ha en stark närvaro online och kunna nå ut till många potentiella spelare för att maximera sina intäkter som affiliate.
Sammanfattningsvis är Gogo Casino affiliates ett bra sätt att tjäna pengar genom att marknadsföra ett populärt online casino till nya spelare. Med rätt strategi och engagemang kan man skapa en lönsam affärsverksamhet som affiliate hos Gogo Casino.
https://gogocasino.one
Ofereco a voce o melhor jogo Fortune Tiger
Gogo Casino är ett relativt nytt online casino som marknadsför sig som en snabb och lättanvänd plattform för spelare att njuta av sina favoritspel. Men trots sitt glättiga yttre har det uppkommit misstankar om att Gogo Casino kan vara inblandat i bluffaktiviteter.
Många spelare har rapporterat problem med att ta ut sina vinster och har upplevt att deras konton har blivit stängda utan förvarning eller förklaring. Detta har lett till spekulationer om att Gogo Casino kan vara inblandat i bluffaktiviteter för att undvika att betala ut vinster till sina spelare.
Den svenska spelmyndigheten, Spelinspektionen, har även mottagit klagomål från spelare om Gogo Casino och har satt igång en utredning för att undersöka om casinot följer lagar och regler. Om det visar sig att Gogo Casino faktiskt bedriver bluffverksamhet kan de riskera att förlora sin spellicens och tvingas stänga ner sin verksamhet.
Det är viktigt att spelare är medvetna om riskerna med att spela på online casinon och att man alltid gör sin egen research innan man registrerar sig på en ny plattform. Att läsa recensioner och göra efterforskningar om casinot kan hjälpa dig att undvika att bli lurad av oseriösa aktörer.
Sammanfattningsvis är det viktigt att vara försiktig när man spelar på online casinon och att vara medveten om att det finns risk för bluffverksamhet. Genom att vara uppmärksam och göra sin egen research kan man undvika att hamna i en situation där man blir lurad av oseriösa aktörer som Gogo Casino.
https://gogocasino.one
Gogo casino com är en populär online spelplattform som erbjuder ett brett utbud av casinospel för både nybörjare och erfarna spelare. Med ett enkelt och användarvänligt gränssnitt är det lätt att hitta sina favoritspel och njuta av en spännande spelupplevelse direkt från bekvämligheten av sitt eget hem.
På Gogo casino com finns det mängder av spel att välja mellan, inklusive klassiska casinospel som blackjack, roulette och poker samt ett stort utbud av spelautomater och videoslots. Oavsett om man föredrar traditionella casinospel eller mer moderna alternativ, finns det något för alla smaker hos Gogo casino com.
För de som är intresserade av att spela med riktiga pengar finns det också möjlighet att göra insättningar och ta del av generösa bonusar och kampanjer. Med en säker och pålitlig betalningsmetod kan man känna sig trygg i att ens pengar är i goda händer när man spelar på Gogo casino com.
Dessutom erbjuder Gogo casino com en professionell kundsupport som alltid är tillgänglig för att hjälpa till med eventuella frågor eller problem. Med en dedikerad supportteam kan spelarna känna sig trygga i att få den hjälp de behöver när de spelar på Gogo casino com.
Sammanfattningsvis är Gogo casino com en utmärkt plattform för alla som är intresserade av att spela casinospel online. Med ett brett utbud av spel, generösa bonusar och en pålitlig kundsupport kan man få en spännande och underhållande spelupplevelse på Gogo casino com.
https://gogocasino.one
Отыскиваете способ улучшить своё владение английским. Погрузитесь в мир кино с нашей коллекцией фильмов на английском и британском языках. Киноленты на английском, особенно с британским акцентом, помогают окунуться в языковую среду. Для наилучшего понимания можно использовать субтитры на английском. Улучшайте свой инглиш, наслаждаясь излюбленными кинокартинами. Подробнее тут https://english-films.pp.ua/
Спасибо за ваше известие. Мы ценим ваш комментарий и готовы для вас помочь. В случае если у вас есть какие-либо дополнительные вопросы либо необходима добавочная информация, не стесняйтесь спрашивать. Вкупе мы создадим наш форум еще лучше!
http://freelancing.md/project/666
Gogo Casino är ett populärt online casino som erbjuder en mängd olika spel och spännande funktioner för sina spelare. Ett av de viktigaste aspekterna för många spelare när de väljer ett casino är hur snabbt och smidigt utbetalningar görs. Gogo Casino har tagit detta på stort allvar och erbjuder en utbetalningsprocess som är enkel och effektiv.
När du vinner på Gogo Casino och vill göra en utbetalning av dina vinster finns det flera olika alternativ att välja mellan. Du kan använda dig av olika betalningsmetoder som till exempel banköverföring, kreditkort eller e-plånböcker för att ta ut dina pengar. Oavsett vilken metod du väljer så kan du vara säker på att din utbetalning kommer att behandlas på ett säkert sätt och att dina vinster kommer att nå ditt konto snabbt.
En av fördelarna med att spela på Gogo Casino är att de har en snabb och effektiv kundtjänst som alltid är tillgänglig för att hjälpa till med eventuella frågor eller problem. Om du har några frågor om utbetalningar eller behöver hjälp med något annat så kan du enkelt kontakta kundtjänsten via livechatt eller e-post för att få snabb och professionell hjälp.
Sammanfattningsvis kan vi konstatera att Gogo Casino erbjuder en utmärkt utbetalningsprocess för sina spelare. Med en mängd olika betalningsmetoder att välja mellan och en snabb och effektiv kundtjänst kan du vara säker på att dina vinster kommer att hanteras på ett säkert och pålitligt sätt. Så om du letar efter ett online casino med en smidig och pålitlig utbetalningsprocess så är Gogo Casino definitivt värt att prova!
https://gogocasino.one
Gogo casino är en populär spelsajt som erbjuder ett stort utbud av casinospel och en spännande spelupplevelse för alla spelare. Sajten har blivit mycket omtyckt av spelare tack vare sin användarvänliga design, generösa bonusar och snabba utbetalningar.
En av de starka sidorna med Gogo casino är det stora urvalet av casinospel som erbjuds. Här hittar man alla de klassiska casinospelen såsom blackjack, roulette och spelautomater, samt ett brett utbud av nya och spännande spel. Sajten samarbetar med flera ledande spelleverantörer vilket gör att spelarna kan njuta av högkvalitativa spel med innovativa funktioner och grafik.
En annan fördel med Gogo casino är de generösa bonusar och kampanjer som erbjuds till spelarna. Nya spelare välkomnas med en attraktiv välkomstbonus och regelbundet erbjuds det olika kampanjer och tävlingar där spelarna kan vinna fina priser och bonusar. Dessutom har sajten ett lojalitetsprogram där spelarna kan samla poäng och få förmåner för att fortsätta spela på sajten.
Gogo casino är också känt för sina snabba utbetalningar och goda kundtjänst. Spelarna kan vara trygga i att deras pengar och personuppgifter hanteras säkert och att de kan få hjälp av en professionell support om de skulle behöva det.
Sammanfattningsvis är Gogo casino en utmärkt spelsajt för alla som letar efter en spännande och pålitlig spelupplevelse. Med sitt stora spelutbud, generösa bonusar och pålitliga kundtjänst har sajten lyckats skapa en bra rykte bland spelare. Om du letar efter ett bra casino att spela på rekommenderar vi definitivt Gogo casino.
https://gogocasino.one
Gogo Casino är ett populärt online casino som erbjuder många spännande spel och generösa bonusar för sina spelare. En av de mest eftertraktade bonusarna är bonusen utan insättning, även känd som no deposit bonus. Denna bonus ger spelare möjligheten att spela gratis utan att behöva sätta in egna pengar.
En no deposit bonus är ett utmärkt sätt för spelare att prova på olika spel och uppleva casinot utan att riskera sina egna pengar. Det är vanligtvis en liten summa pengar eller ett antal gratissnurr som erbjuds som belöning för att registrera sig som ny spelare. Det är viktigt att notera att dessa bonusar oftast kommer med vissa omsättningskrav som måste uppfyllas innan eventuella vinster kan tas ut.
För att ta del av en no deposit bonus hos Gogo Casino behöver spelare bara skapa ett konto och verifiera sin identitet. När kontot är skapat kommer bonusen att krediteras automatiskt och spelarna kan börja utforska casinots spelutbud utan att behöva sätta in egna pengar.
Det är viktigt att läsa villkoren för bonusen noggrant för att undvika missförstånd och se till att alla krav är uppfyllda innan man begär en utbetalning. Gogo Casino erbjuder en rad olika betalningsalternativ för insättningar och uttag, och deras kundtjänst finns alltid till hands för att hjälpa till med eventuella frågor eller problem.
Sammanfattningsvis är Gogo Casino en utmärkt plattform för spelare som letar efter spännande spel och generösa bonusar, inklusive no deposit bonusar. Genom att registrera sig på casinot kan spelare njuta av en säker och underhållande spelupplevelse med chansen att vinna stora vinster utan att behöva riskera sina egna pengar. Så varför inte prova lyckan idag och ta del av en no deposit bonus hos Gogo Casino? Lycka till!
https://gogocasino.one
Gogo Casino lanserade nyligen en ny funktion pГҐ sin plattform som har fГҐtt namnet “transparent horizontal”. Denna funktion Г¤r ett sГ¤tt fГ¶r spelare att fГҐ en Г¤nnu mer transparent och rГ¤ttvis spelupplevelse.
Med den transparenta horisontella funktionen kan spelare enkelt se alla transaktioner och spelhistorik i realtid. Detta ger en bättre överblick över ens spelaktivitet och gör det enklare att ha koll på sina insättningar och uttag.
Förutom att ge en ökad transparens för spelarna, kan den transparenta horisontella funktionen även bidra till att minska risken för spelberoende. Genom att ha en tydlig överblick över ens spelaktivitet är det lättare att se när man bör dra i bromsen och ta en paus från spelet.
Gogo Casino har alltid strävat efter att erbjuda en säker och ansvarsfull spelupplevelse för sina spelare. Den transparenta horisontella funktionen är ett steg i rätt riktning för att uppnå detta mål.
För spelare som vill ha en ännu mer transparent och rättvis spelupplevelse är det definitivt värt att testa den transparenta horisontella funktionen på Gogo Casino. Med denna nya funktion kan du enkelt hålla koll på ditt spelande och njuta av en tryggare spelupplevelse.
https://gogocasino.one
Gogo casino är en populär online kasinosida som erbjuder spelare en spännande och underhållande spelupplevelse. En av de mest eftertraktade erbjudandena från detta casino är Gogo casino no deposit bonus, som ger spelare chansen att spela utan att behöva sätta in egna pengar.
Att kunna spela utan att behöva göra en insättning är en fantastisk möjlighet för spelare att testa på olika spel och se om det är rätt kasino för dem. Gogo casino no deposit bonus ger spelare möjligheten att utforska olika spel och vinna riktiga pengar utan att riskera sina egna medel.
För att ta del av Gogo casino no deposit bonus behöver spelare vanligtvis bara registrera sig på sidan och skapa ett konto. När kontot är verifierat kommer spelare att kunna ta emot bonusen och börja spela sina favoritspel. Det finns vanligtvis ett antal villkor som måste uppfyllas för att kunna ta ut eventuella vinster som görs med bonusen, så det är viktigt att läsa och förstå dessa villkor noggrant.
Gogo casino no deposit bonus är ett utmärkt sätt för spelare att prova på kasinot och dess spelutbud utan att behöva riskera sina egna pengar. Med chansen att vinna riktiga pengar utan att behöva göra en insättning är det en möjlighet som inte bör missas. Så om du letar efter en spännande och generös kasinoupplevelse, se till att kolla in Gogo casino och deras no deposit bonus idag. Lycka till!
https://gogocasino.one
Gogo Casino är en spännande online casino där spelare kan njuta av en mängd olika spel och kampanjer. En av de mest populära erbjudandena hos Gogo Casino är no deposit-bonusen, som låter spelare få gratis pengar att spela för utan att behöva sätta in några egna pengar.
No deposit-bonusar är ett fantastiskt sätt för spelare att prova på nya spel och uppleva spännande casinoupplevelser utan att behöva riskera sina egna pengar. Hos Gogo Casino kan spelare få en no deposit-bonus genom att registrera sig som ny medlem eller genom att delta i olika kampanjer och tävlingar.
För att ta del av en no deposit-bonus hos Gogo Casino behöver spelarna bara följa några enkla steg. För det första måste de skapa ett konto på casinots hemsida och verifiera sin identitet. Sedan kan de använda bonuskoden som erbjuds för att få sin gratis bonus.
Det finns många fördelar med att utnyttja en no deposit-bonus hos Gogo Casino. För det första kan spelare testa på nya spel och spännande funktioner utan att riskera sina egna pengar. Dessutom kan de vinna riktiga pengar utan att behöva göra någon insättning.
Sammanfattningsvis är Gogo Casino en spännande plats för alla som älskar casinospel och vill ha chansen att vinna stora vinster. Med sina generösa no deposit-bonusar och spännande kampanjer är det en plats där spelare kan njuta av en underhållande och belönande spelupplevelse. Så varför inte gå med idag och se vad Gogo Casino har att erbjuda?
https://gogocasino.one
Завод из России продает силовые тренажеры https://trenazher-silovoj.ru/ для круглосуточной работы в коммерческих тренировочных залах.
Изучите каталог интернет-магазина выпускаемых станков грузоблочных и с обрезиненными блинами.
Все модели позволяют прорабатывать акцентированно любые группы мышц.
Рассматривайте машину для плеч, жим ногами, одинарный Кроссовер, Баттерфляй для дельт и груди, силовую раму Смита, вертикальную тягу, лавку Скотта, Гравитрон для подтягивания и отжиманий, гиперэкстензию, атлетические скамьи, Хаммер.
Производимый станок ориентирован для атлетов с разным уровнем физической активности.
Производимое спортоборудование полностью безупречно и не нуждается в техническом наблюдении.
Купите весовой блок необходимой массы.
I titeln på denna artikel får vi reda på att Gogo Casino inte betalar sina kunder. Detta är en mycket allvarlig sak och kan få allvarliga konsekvenser för både casinot och dess kunder. Att inte betala ut vinster kan leda till att casinot förlorar sitt rykte och därmed också sina kunder.
Det är viktigt att ett casino är pålitligt och håller vad de lovar. När spelare vinner pengar på ett casino förväntar de sig att få utbetalningen utan problem. Om detta inte händer kan det leda till missnöjda kunder och i slutändan förlorade affärer för casinot.
Det finns flera orsaker till varför ett casino inte betalar ut vinster. En av de vanligaste är att spelaren inte har följt casinots regler och villkor, vilket innebär att casinot har rätt att vägra utbetalning. Andra orsaker kan vara tekniska problem eller att casinot helt enkelt inte har tillräckligt med pengar för att täcka utbetalningarna.
Oavsett orsaken är det viktigt att casinot tar sitt ansvar och håller sina löften gentemot sina kunder. Om Gogo Casino inte betalar sina kunder kan det få allvarliga konsekvenser för deras rykte och företagets framtid. Spelare bör vara försiktiga med att spela på casinon som inte är pålitliga och som inte lever upp till sina åtaganden.
I slutändan är det i både casinots och spelarens intresse att utbetalningar sker på ett smidigt och rättvist sätt. För att undvika problem är det viktigt att läsa igenom casinots regler och villkor noggrant och se till att följa dem. På så sätt kan man undvika att hamna i en situation där man inte får utbetalt sina vinster.
https://gogocasino.one
Gogo Casino är en svensk spelplattform som erbjuder en unik och transparent spelupplevelse för sina spelare. Med sin transparenta horisontella design skapar Gogo Casino en ren och stilren spelmiljö som är lätt att navigera och förstå.
Den horisontella designen ger spelarna en överblick över alla tillgängliga spel och funktioner på en och samma plats. Detta gör det enkelt för spelarna att hitta sina favoritspel och snabbt komma igång med att spela.
Som en del av sin transparenta approach visar Gogo Casino tydligt alla regler och villkor för sina spel. Detta skapar en trygg spelmiljö där spelarna kan känna sig säkra på att de spelar på en plattform som är rättvis och ärlig.
Gogo Casino erbjuder också en rad olika betalningsmetoder för att göra det enkelt för spelarna att sätta in och ta ut sina vinster. Genom att erbjuda en smidig och säker betalningsprocess skapar Gogo Casino en bekväm spelupplevelse för sina spelare.
Sammanfattningsvis är Gogo Casino en transparent och användarvänlig spelplattform som fokuserar på att skapa en positiv spelupplevelse för sina spelare. Med sin horisontella design och tydliga regler och villkor är Gogo Casino en plats där spelarna kan spela med tillit och njutning.
https://gogocasino.one
how to get zithromax zithromax prescription in canada purchase zithromax online
Gogo casino är en populär online casino som erbjuder ett brett utbud av spel för spelare att njuta av. Från slots till bordsspel och live casino, finns det något för alla att uppskatta hos Gogo casino.
En annan sak som spelarna Г¤lskar med Gogo casino Г¤r deras unika och fГ¤rgglada logo. Logotypen bestГҐr av ordet “Gogo” skrivet i en modern och stilren skriftstil med en pigg fГ¤rgpalett som inkluderar rosa, lila och orange. Den hГ¤r logotypen Г¤r inte bara snygg att titta pГҐ, den Г¤r ocksГҐ mycket igenkГ¤nnbar och gГ¶r det lГ¤tt fГ¶r spelarna att associera den med Gogo casino.
Förutom att vara en del av varumärkesidentiteten för Gogo casino, representerar logotypen också spelglädjen och spänningen som spelarna kan förvänta sig när de spelar på casinot. Den pigg färgpaletten och den moderna designen förmedlar en känsla av energi och underhållning, som passar perfekt med den upplevelse som Gogo casino strävar efter att erbjuda sina spelare.
Sammanfattningsvis är Gogo casino logo en viktig del av varumärkesidentiteten för detta populära online casino. Den moderna designen och den färgglada färgpaletten gör den inte bara snygg att se på, utan också mycket igenkännbar för spelarna. Med sin energiska och underhållande känsla representerar logotypen perfekt den spelglädje som spelarna kan förvänta sig när de spelar på Gogo casino.
https://gogocasino.one
Gogo casino bonus
Gogo casino är känt för sina generösa bonusar och kampanjer som lockar nya och återkommande spelare. Med en rad olika bonusar att välja mellan, finns det något för alla på detta online casino.
En populär bonus som erbjuds på Gogo casino är den så kallade välkomstbonusen. Denna bonus ges vanligtvis till nya spelare vid deras första insättning på casinot och kan inkludera en matchningsbonus på insättningen eller en mängd gratissnurr på utvalda spelautomater. Denna bonus ger spelarna en fantastisk start på deras spelupplevelse på casinot.
För de som redan är registrerade på Gogo casino finns det också regelbundna kampanjer och bonusar att dra nytta av. Det kan vara allt från reload-bonusar till cashback-erbjudanden eller tävlingar där spelare kan vinna stora priser. Genom att hålla sig informerad om de senaste kampanjerna kan spelarna maximera sina vinstchanser och njuta av ännu mer spänning och belöningar på casinot.
För att ta del av Gogo casinos bonusar är det viktigt att läsa villkoren och reglerna för varje erbjudande. Det kan finnas omsättningskrav och andra begränsningar som spelarna behöver uppfylla för att kunna ta ut sina vinster. Genom att vara medveten om dessa regler och följa dem kan spelarna undvika eventuella missförstånd eller problem när de tar del av bonusarna.
Sammanfattningsvis är Gogo casino känt för sina generösa bonusar och kampanjer som lockar spelare att återvända till casinot om och om igen. Med en välkomstbonus för nya spelare och regelbundna kampanjer för befintliga spelare, finns det alltid något spännande att ta del av på detta online casino. Med lite tur och skicklighet kan spelarna dra nytta av bonusarna och öka sina vinstchanser på Gogo casino.
https://gogocasino.one
Gogo Casino uttag flashback
Gogo Casino är en populär spelsajt som erbjuder sina spelare möjligheten att spela en mängd olika casinospel online. Ett av de främsta fördelarna med att spela på Gogo Casino är att det finns enkla och smidiga sätt att göra insättningar och uttag.
Många spelare har delat med sig av sina erfarenheter av att göra uttag från Gogo Casino på olika forum och communities online. Många av dessa erfarenheter har varit positiva och spelarna har berättat om smidiga och snabba uttagsprocesser.
Det verkar som att Gogo Casino tar uttagsprocessen på allvar och strävar efter att göra den så enkel och bekväm som möjligt för sina spelare. Många spelare har rapporterat att de har fått sina uttag bekräftade och behandlade inom bara några timmar.
Det är också värt att notera att Gogo Casino erbjuder flera olika betalningsmetoder för uttag, inklusive banköverföring, kortbetalningar och e-plånböcker. Det innebär att spelarna har möjlighet att välja den metod som passar dem bäst.
Sammanfattningsvis verkar det som att Gogo Casino har ett gott rykte när det gäller uttag och att spelarna är nöjda med den service de erbjuder. Om du funderar på att spela på Gogo Casino kan du vara trygg i vetskapen om att du kommer att kunna göra smidiga och snabba uttag när du vinner stort.
https://gogocasino.one
Gogo Casino är ett online casino som har blivit allt mer populärt bland svenska spelare. Ett av de första sakerna som fångar ögat när man besöker deras webbplats är deras unika och färgglada logo. Logotypen är enkelt utformad med de två ord som står i fetstil och på rött och grönt. Det är en enkel design men det sticker verkligen ut och gör att varumärket känns igen direkt.
Den röda och gröna färgen är inte bara för att se snyggt ut, utan det har faktiskt en betydelse bakom det. Röd symboliserar spänning och passion medan grönt representerar trygghet och pålitlighet. Tillsammans skapar de en harmoni som speglar Gogo Casinos värden och vad de strävar efter att erbjuda sina spelare.
Logotypen för Gogo Casino är också ett sätt för varumärket att skapa igenkännlighet och differentiera sig från andra online casinon på marknaden. Genom att ha en unik logo kan de skapa en stark identitet och bygga ett varumärke som spelarna kan lita på och känna igen direkt.
Sammanfattningsvis är Gogo Casinos logo inte bara snygg och unik, den representerar också varumärkets värden och identitet på ett tydligt sätt. Med enkelheten i designen och den tänkta symboliken bakom färgerna, är det en logotyp som definitivt sticker ut och gör att Gogo Casino blir en aktör att räkna med på den online casinomarknaden.
https://gogocasino.one
Gogo Casino Email
Gogo Casino är ett populärt online casino som erbjuder ett brett utbud av spel och generösa bonusar till sina spelare. För att hålla sina kunder informerade om de senaste erbjudandena och kampanjerna, skickar Gogo Casino regelbundet ut e-postmeddelanden till sina registrerade medlemmar.
Genom att prenumerera på Gogo Casinos e-postlista kan spelarna få exklusiva erbjudanden, bonusar och nyheter direkt i sin inkorg. Meddelandena kan inkludera allt från free spins och insättningsbonusar till information om kommande turneringar och tävlingar.
Det är enkelt att registrera sig för Gogo Casinos e-postlista. Besök bara deras webbplats och fyll i dina uppgifter för att bli en del av deras e-postutskick. Du kan också välja att inte ta emot e-postmeddelanden genom att avmarkera den relevanta rutan vid registreringen.
Genom att prenumerera på Gogo Casinos e-postlista kan du hålla dig uppdaterad om de senaste kampanjerna och erbjudandena. Missa inte chansen att vinna stora priser och få bonusar genom att hålla ett öga på din inkorg för de senaste e-postmeddelandena från Gogo Casino. Lycka till!
https://gogocasino.one
Gogo casino email är ett sätt för spelare att hålla sig uppdaterade om de senaste kampanjerna och erbjudandena som erbjuds av Gogo casino. Genom att prenumerera på casinots nyhetsbrev får spelare tillgång till exklusiva bonusar, free spins och andra belöningar som kan öka deras vinstchanser och spelupplevelse.
Att prenumerera på Gogo casino email är enkelt och kostnadsfritt. Allt du behöver göra är att ange din e-postadress på casinots hemsida och bekräfta din prenumeration genom att klicka på en länk i det bekräftelsemejl som skickas till dig. När du har bekräftat din prenumeration kommer du regelbundet att få e-postmeddelanden med information om kommande kampanjer, tävlingar och andra spännande evenemang hos Gogo casino.
Genom att hålla sig uppdaterad via Gogo casino email kan spelare dra nytta av exklusiva erbjudanden och belöningar som är tillgängliga endast för prenumeranter. Det kan vara allt från insättningsbonusar och cashback-erbjudanden till tävlingar och turneringar där spelare har chansen att vinna fantastiska priser. Genom att delta i dessa kampanjer kan spelare öka sina vinstchanser och få en ännu mer underhållande spelupplevelse på Gogo casino.
Sammanfattningsvis är Gogo casino email ett utmärkt sätt för spelare att hålla sig uppdaterade om de senaste kampanjerna och erbjudandena som erbjuds av casinot. Genom att prenumerera på nyhetsbrevet kan spelare dra nytta av exklusiva belöningar och öka sina vinstchanser samtidigt som de får en mer personlig och anpassad spelupplevelse på Gogo casino. Så varför inte anmäla sig redan idag och ta del av alla fördelar som Gogo casino email har att erbjuda?
https://gogocasino.one
Как выучить английский язык с помощью сериалов: https://serialy-na-anglijskom.pp.ua/
Gogo Casino är en onlinekasino som erbjuder snabba och smidiga utbetalningar till sina spelare. Med deras enkla och användarvänliga plattform kan du på ett enkelt sätt ta ut dina vinster utan krångel.
När det kommer till utbetalningar på Gogo Casino finns det flera olika alternativ att välja mellan. Du kan använda banköverföring, Trustly, Neteller, Skrill eller Visa/Mastercard för att ta ut dina vinster. Oavsett vilket alternativ du väljer kan du vara säker på att pengarna kommer att hamna på ditt konto snabbt och utan problem.
För att göra en utbetalning behöver du bara logga in på ditt konto, gå till kassan och välja vilket alternativ du vill använda. Sedan anger du hur mycket pengar du vill ta ut och bekräftar transaktionen. Pengarna kommer sedan att skickas till ditt valda konto inom några få arbetsdagar.
Gogo Casino strävar efter att erbjuda en säker och pålitlig spelupplevelse för sina spelare. Alla transaktioner är krypterade och skyddade så att du kan känna dig trygg när du spelar på deras plattform. Dessutom har de en kundtjänst som är tillgänglig för att hjälpa dig med eventuella frågor eller problem som kan uppstå.
Sammanfattningsvis erbjuder Gogo Casino snabba och smidiga utbetalningar till sina spelare. Med flera olika alternativ att välja mellan och en säker plattform kan du vara säker på att dina vinster kommer att hamna på ditt konto snabbt och utan problem. Så om du letar efter en kasino med enkel och pålitlig utbetalning är Gogo Casino ett perfekt val för dig.
https://gogocasino.one
Gogo Casino är en populär online spelplattform som erbjuder spelare en spännande och underhållande spelupplevelse. Med ett brett utbud av casinospel och generösa bonusar har Gogo Casino blivit ett populärt val bland spelare över hela världen.
En av de attraktiva funktionerna som Gogo Casino erbjuder är möjligheten att spela utan insättning. Det betyder att spelare kan delta i casinospel utan att behöva sätta in några pengar på sitt spelkonto. Detta erbjudande är en möjlighet att prova på olika spel och uppleva spänningen av att spela på ett online casino utan att behöva riskera sina egna pengar.
För att ta del av Gogo Casino no deposit erbjudandet behöver spelare bara registrera sig på plattformen och skapa ett spelkonto. Därefter kan de börja spela sina favoritspel och förhoppningsvis vinna stort utan att behöva satsa sina egna pengar.
Oavsett om du är en erfaren casinospelare eller nybörjare kan Gogo Casino no deposit vara ett utmärkt sätt att utforska olika spel och ha kul utan att behöva oroa dig för att förlora pengar. Med den ökande populariteten av online casinon är det viktigt att välja en pålitlig och säker spelplattform som Gogo Casino för en säker och rolig spelupplevelse.
Sammanfattningsvis är Gogo Casino no deposit ett lockande erbjudande för spelare som vill ha en spännande spelupplevelse utan att behöva satsa sina egna pengar. Med ett brett utbud av casinospel och generösa bonusar är Gogo Casino en plattform som imponerar och lockar spelare från hela världen. Så varför inte ge det en chans och prova lyckan idag?
https://gogocasino.one
Gogo casino no deposit är ett populärt alternativ för de som vill spela casinospel online utan att behöva sätta in egna pengar. Genom att erbjuda spelare möjligheten att spela utan insättning ger Gogo casino en chans för nya spelare att prova på olika spel och uppleva spänningen i en virtuell casinomiljö.
Att spela på ett casino utan insättning innebär att spelaren inte behöver göra någon ekonomisk investering för att kunna delta i spelen. Istället får man en summa pengar att spela för direkt när man registrerar sig på casinot. Detta ger spelare chansen att utforska olika spel och se vad de tycker om utan att riskera sina egna pengar.
Gogo casino no deposit erbjuder vanligtvis ett urval av spel som inkluderar allt från klassiska slots till bordsspel som roulette och blackjack. Oavsett vilket spel man föredrar finns det något för alla att njuta av på ett casino utan insättning.
En annan fördel med att spela på ett casino utan insättning är att man kan vinna riktiga pengar utan att behöva satsa något själv. Genom att utnyttja välkomstbonusar och gratissnurr kan spelare öka sina chanser att vinna stort utan att behöva riskera sina egna pengar.
Sammanfattningsvis är Gogo casino no deposit ett utmärkt alternativ för de som vill spela casinospel online utan att behöva göra en insättning. Med ett brett utbud av spel och chansen att vinna riktiga pengar utan risk är det en spännande och underhållande upplevelse för både nya och erfarna spelare. Så varför inte ge det en chans och se vad du kan vinna idag?
https://gogocasino.one
Gogo Casino är en populär online spelplattform som erbjuder spelare möjligheten att njuta av en mängd olika casinospel. För att locka nya spelare och belöna sina lojala kunder erbjuder Gogo Casino regelbundet olika typer av bonusar.
En av de mest eftertraktade bonusarna på Gogo Casino är välkomstbonusen för nya spelare. Genom att registrera sig på plattformen och göra en första insättning kan spelare få en generös bonus som ökar deras chanser att vinna stort. Denna bonus kan användas för att spela olika spel på casinot och utforska olika möjligheter att vinna.
För de som redan är registrerade på Gogo Casino erbjuds också lojalitetsbonusar och kampanjer regelbundet. Dessa kan inkludera gratissnurr på utvalda spelautomater, bonuspengar att spela med eller till och med speciella tävlingar och turneringar där spelare kan vinna fantastiska priser.
Det är viktigt att komma ihåg att alla bonusar på Gogo Casino kommer med vissa villkor och regler som måste följas. Det är därför viktigt att läsa igenom bonusvillkoren noggrant innan du accepterar en bonus för att undvika eventuella missförstånd eller problem.
Sammanfattningsvis erbjuder Gogo Casino en rad spännande bonusar för sina spelare, som kan hjälpa dem att öka sina vinstchanser och njuta av en ännu mer spännande spelupplevelse. Genom att dra nytta av dessa bonusar kan spelare maximera sin potential att vinna stort och ha roligt samtidigt. Så varför inte prova lyckan på Gogo Casino idag och se vilka spännande bonusar som väntar på dig? Lycka till!
https://gogocasino.one
Casino Gogo är ett spännande online casino som lockar spelare med sitt stora utbud av spel och generösa bonusar. Med ett fokus på att erbjuda en förstklassig spelupplevelse, erbjuder Casino Gogo ett brett urval av spännande casinospel från några av de bästa leverantörerna i branschen.
På Casino Gogo hittar du allt från klassiska bordsspel som blackjack och roulette till moderna videoslots och progressiva jackpottspel. Oavsett om du är en erfaren spelare eller nybörjare så finns det något för alla på detta casino.
För att locka nya spelare erbjuder Casino Gogo generösa välkomstbonusar och kampanjer. Dessutom har de en lojalitetsprogram där spelare kan tjäna poäng och få exklusiva belöningar.
En annan fördel med att spela på Casino Gogo är att du kan spela var som helst och när som helst. Med deras mobilanpassade plattform kan du njuta av dina favoritspel direkt från din smartphone eller surfplatta.
Säkerhet är också en prioritet på Casino Gogo. De använder den senaste krypteringstekniken för att säkerställa att alla transaktioner är säkra och att spelarnas personliga information skyddas.
Sammanfattningsvis är Casino Gogo ett utmärkt val för alla som letar efter en spännande och säker spelupplevelse online. Med sitt stora spelutbud, generösa bonusar och mobilanpassade plattform är det lätt att förstå varför det här casinot har blivit så populärt bland spelare. Besök Casino Gogo idag och upplev spänningen själv!
https://gogocasino.one
Gogo Casino är en populär spelsajt för alla som älskar att spela online casino. Med sitt stora utbud av spelautomater, bordsspel och live casino, finns det något för alla smaker. En av fördelarna med Gogo Casino är att de erbjuder spelare möjligheten att spela utan att behöva göra en insättning, vilket kallas för no deposit bonus.
No deposit bonus är ett erbjudande som tillåter spelare att testa på spel utan att behöva göra en insättning. Detta är perfekt för nya spelare som vill utforska casinot innan de satsar sina egna pengar. Med no deposit bonus kan spelare spela olika spel och få en känsla för hur casinot fungerar utan att riskera några pengar.
För att få tillgång till no deposit bonus hos Gogo Casino, behöver spelare bara registrera sig på sajten och skapa ett konto. Därefter kan de njuta av en rad olika spel utan att behöva göra någon insättning. Det är en fantastisk möjlighet för spelare att upptäcka nya favoritspel och ha chansen att vinna utan att riskera sina egna pengar.
Gogo Casino är en spelsajt som är känd för sitt generösa bonuserbjudanden och no deposit bonus är verkligen ett av de mest förmånliga. Så om du är ute efter en rolig och spännande spelupplevelse utan att behöva satsa dina egna pengar, då är Gogo Casino det perfekta valet för dig. Registrera dig idag och utforska allt det spännande som Gogo Casino har att erbjuda!
https://gogocasino.one
Gogo Casino är ett populärt online casino som erbjuder sina spelare en spännande spelupplevelse. För att hålla sina kunder informerade om de senaste erbjudandena och kampanjerna skickar de regelbundet ut email till sina registrerade användare.
Med hjälp av Gogo Casino email får spelarna information om nya spel, bonusar och tävlingar som de kan delta i. Genom att prenumerera på casinots nyhetsbrev är man alltid uppdaterad om vad som händer på sajten och kan dra nytta av exklusiva erbjudanden.
För att säkerställa att man inte missar några viktiga meddelanden är det viktigt att se till att ens email uppgifter är korrekta och att man inte har lagt in casinots emailadress i skräpposten. På så sätt kan man vara säker på att man får all relevant information direkt i inkorgen.
Gogo Casino email är ett effektivt sätt för casinot att kommunicera med sina spelare och se till att de får den bästa möjliga spelupplevelsen. Genom att ta del av informationen i dessa email kan man öka sina vinstchanser och ha ännu roligare när man spelar på sajten.
Så se till att prenumerera på Gogo Casinos nyhetsbrev för att hålla dig uppdaterad och inte missa några spännande erbjudanden eller kampanjer!
https://gogocasino.one
לעיסוי, אתם חייבים לבחור באחת מהדירות הדיסקרטיות הפזורות ברחבי העיר הרצליה. אז למה דירות דיסקרטיות בפורטל אקספיינדר? אנו כאן בנס ציונה ? פה תוכל למצוא מענה לחיפושים שלכם דמיינו לעצמכם דירות דיסקרטיות ברחובות-נס ציונה מעוצבות ומושקעת, עם מספר בחורות אצלך נערת ליווי באשקלון
Gogo Casino är ett populärt online casino som erbjuder snabba och smidiga utbetalningar till sina spelare. Med enkel registrering och verifiering kan spelarna njuta av sina vinster inom några minuter.
Att göra en utbetalning på Gogo Casino är enkelt och smidigt. Efter att ha vunnit kan spelarna enkelt begära en utbetalning genom att klicka på knappen för uttag. Därefter ska spelaren välja sin önskade utbetalningsmetod och ange det belopp de vill ta ut. Gogo Casino erbjuder flera olika betalningsmetoder, inklusive banköverföring, Trustly och e-plånböcker som Skrill och Neteller.
En av fördelarna med att spela på Gogo Casino är det enkla och smidiga uttagsprocessen. Spelarna behöver inte vänta i flera dagar för att få sina vinster, utan kan istället få dem på sin bankkonto inom några minuter.
Det är viktigt att notera att det finns vissa begränsningar för uttag på Gogo Casino. Spelare kan vanligtvis bara göra ett visst antal uttag per dag och det finns oftast en lägsta och högsta gräns för utbetalningar. Det är därför viktigt att läsa igenom villkoren och reglerna för uttag innan man begär en utbetalning.
Sammanfattningsvis är Gogo Casino ett utmärkt val för spelare som söker snabba och smidiga utbetalningar. Med enkel registrering och verifiering samt flera olika betalningsmetoder att välja mellan, kan spelarna njuta av sina vinster inom några minuter. Besök Gogo Casino idag och prova på deras uttagsprocess!
https://gogocasino.one
Gogo Casino Г¤r ett populГ¤rt onlinecasino som erbjuder sina spelare en spГ¤nnande och underhГҐllande spelupplevelse. En av de mest attraktiva funktionerna hos Gogo Casino Г¤r mГ¶jligheten att spela utan att behГ¶va gГ¶ra en insГ¤ttning, Г¤ven kГ¤nd som “no deposit”. Det hГ¤r Г¤r en fantastisk mГ¶jlighet fГ¶r spelare att prova pГҐ olika spel och uppleva spГ¤nningen av att spela pГҐ ett casino utan att behГ¶va riskera sina egna pengar.
Att spela på Gogo Casino utan att behöva göra en insättning är enkelt. När du registrerar dig på casinot kommer du att belönas med en no deposit bonus som du kan använda för att prova på olika spel på sajten. Denna bonus ger dig chansen att vinna riktiga pengar utan att behöva sätta in några egna medel. Det är en perfekt möjlighet för spelare att utforska olika spel och upptäcka vilka spel de gillar bäst.
För att ta del av no deposit bonusen på Gogo Casino är det viktigt att läsa igenom reglerna och villkoren för erbjudandet. Ofta finns det krav på omsättning och maxvinster som måste uppfyllas innan du kan ta ut dina vinster. Det är också viktigt att komma ihåg att no deposit bonusar oftast har ett begränsat giltighetsdatum, så se till att utnyttja erbjudandet innan det går ut.
Gogo Casino erbjuder ett brett utbud av spel frГҐn ledande spelleverantГ¶rer som NetEnt, Microgaming och Play’n GO. Med hundratals spel att vГ¤lja mellan finns det garanterat nГҐgot fГ¶r alla spelare, oavsett om du fГ¶redrar klassiska spelautomater, bordsspel eller livecasino.
Om du är sugen på att prova på spänningen av att spela på ett onlinecasino utan att riskera dina egna pengar, är Gogo Casino det perfekta stället att göra det. Med sin generösa no deposit bonus och imponerande spelutbud är det enkelt att se varför detta casino har blivit så omtyckt av spelare runt om i Sverige. Så varför inte ta chansen och prova lyckan på Gogo Casino idag? Lycka till!
https://gogocasino.one
Kamagra 100mg price Kamagra Iq sildenafil oral jelly 100mg kamagra
Gogo Casino är ett populärt online casino i Finland som erbjuder en rolig och spännande spelupplevelse för alla spelare. Med ett stort utbud av casinospel, generösa bonusar och en användarvänlig plattform är det inte konstigt att Gogo Casino har blivit en favorit bland många finska spelare.
En av de största fördelarna med Gogo Casino är dess enkla och smidiga registreringsprocess. Istället för att behöva fylla i långa formulär och vänta på att ens registrering ska bli godkänd, kan spelare börja spela sina favoritspel direkt. Dessutom behöver spelare inte skapa ett konto för att spela på casinot, vilket sparar tid och gör hela spelupplevelsen mycket mer bekväm.
När det kommer till spelutbudet har Gogo Casino något för alla typer av spelare. Från klassiska casinospel som blackjack, roulette och slots till mer moderna alternativ som live casino och progressiva jackpottspel, finns det något för alla smaker. Dessutom samarbetar Gogo Casino med flera ledande spelutvecklare för att säkerställa att spelarna får tillgång till de senaste och bästa spelen på marknaden.
För de spelare som gillar att få lite extra belöningar finns det även generösa bonusar och kampanjer att ta del av hos Gogo Casino. Oavsett om det handlar om en välkomstbonus för nya spelare eller regelbundna erbjudanden för lojala kunder, finns det alltid något extra att se fram emot när man spelar på detta casino.
Sammanfattningsvis är Gogo Casino en fantastisk spelsajt för finska spelare som letar efter en underhållande och säker spelupplevelse. Med sitt stora spelutbud, generösa bonusar och användarvänliga plattform är det inte konstigt att Gogo Casino har blivit ett av de mest populära online casinona i Finland. Vi rekommenderar varmt alla spelare att prova lyckan hos Gogo Casino och uppleva spänningen med att vinna stort!
https://gogocasino.one
Официальный сайт 1Вин казино предлагает лицензионные игры с высокой отдачей, но для захода требуется найти зеркало 1win casino 1Win casino
Gogo Casino är en populär online-spelplattform där du kan njuta av en mängd olika casinospel utan krångel. Men om du någonsin behöver kontakta dem för att ställa frågor eller få hjälp, kan det vara bra att ha deras telefonnummer till hands.
Tyvärr är det inte så enkelt att hitta Gogo Casino:s telefonnummer på deras webbplats. Istället måste du antingen skicka ett meddelande via deras chattfunktion eller skicka ett e-postmeddelande för att få kontakt med deras kundtjänst.
Om du inte är nöjd med att kommunicera via chatt eller e-post och föredrar att prata med någon direkt, kan det vara en god idé att försöka hitta deras telefonnummer på andra sätt. Det kan vara värt att göra en snabb sökning på nätet eller kontakta deras supportteam för att få tag på numret.
Oavsett vilket sätt du väljer att komma i kontakt med Gogo Casino på, är det viktigt att du är noga med att hålla ditt konto och personlig information säker. Undvik att dela ditt telefonnummer eller andra känsliga uppgifter med okända personer och se till att du använder en pålitlig krypterad förbindelse när du kommunicerar med casinot.
Gogo Casino är en spännande och underhållande spelplattform som erbjuder en rad olika casinospel. Om du någonsin behöver komma i kontakt med dem, se till att du har deras telefonnummer till hands eller försök att hitta det på annat sätt för att få den hjälp du behöver.
https://gogocasino.one
Профессиональная уборка после ремонта в Челябинске — наша специализация! Обращайтесь к нам, и ваш дом станет идеально чистым! https://klining-chelyabinsk-1.ru/
Gogo Casino är ett populärt online casino som lockar spelare med sitt enkla och stilrena design. En av de saker som verkligen sticker ut med Gogo Casino är deras slående logotyp. Logotypen är iögonfallande och lockande, och den får definitivt spelare att stanna upp och ta en närmare titt.
Logotypen fГ¶r Gogo Casino bestГҐr av en enkel, rundad typsnitt som Г¤r lГ¤ttlГ¤st och modern. BokstГ¤verna Г¤r skrivna i en lyxig svart fГ¤rg, vilket ger en sofistikerad kГ¤nsla. Den fГ¤rgglada cirkeln runt logotypen ger en kГ¤nsla av rГ¶relse och energi, vilket passar bra med namnet “Gogo Casino”. Logotypen Г¤r bГҐde elegant och rolig, vilket ГҐterspeglar den Г¶vergripande tonen pГҐ casinot.
Genom att ha en stark och minnesvГ¤rd logotyp, har Gogo Casino skapat ett starkt varumГ¤rke fГ¶r sig sjГ¤lva. Spelare kommer att kГ¤nna igen logotypen var de Г¤n ser den, vilket skapar en stark kГ¤nsla av igenkГ¤nning och fГ¶rtroende. Logotypen Г¤r ocksГҐ en viktig del av fГ¶retagets marknadsfГ¶ring – den syns pГҐ allt frГҐn deras hemsida till deras reklamkampanjer.
Sammanfattningsvis kan man säga att Gogo Casino har lyckats skapa en logotyp som verkligen sticker ut och fångar spelarnas uppmärksamhet. Den är enkel men effektiv, och den speglar casinots unika och roliga känsla. Med en så stark logotyp bakom sig kan Gogo Casino förvänta sig en framgångsrik framtid på den konkurrensutsatta marknaden för online casinon.
https://gogocasino.one
buy Kamagra Sildenafil Oral Jelly super kamagra
Официальный сайт 1Вин казино предлагает лицензионные игры с высокой отдачей, но для захода требуется найти зеркало 1win casino казино 1Вин
kredit-zaym
O melhor e mais popular jogo Fortune Tiger
Gogo Casino-appen är den senaste trenden inom online casino-spel. Med denna app kan spelare njuta av sina favoritspel var som helst och när som helst, direkt från sina mobila enheter.
Med de senaste spelen från ledande spelleverantörer som NetEnt, Microgaming och Yggdrasil kommer spelarna att uppleva en otrolig spelupplevelse med högkvalitativa grafik och smidig gameplay.
Funktioner som snabba uttag och enkel registrering gör att spelarna kan komma igång med att spela på nolltid. Dessutom erbjuder Gogo Casino-appen bonusar och kampanjer som gör det ännu mer spännande att spela.
Med enkel navigering och användarvänlig design är Gogo Casino-appen perfekt för alla spelare, oavsett om de är nybörjare eller erfarna spelare. Så ladda ner Gogo Casino-appen idag och börja njuta av spänningen och spänningen av online casino-spel direkt från din mobiltelefon eller surfplatta!
https://gogocasino.one
Gogo casino är en populär online spelplattform som erbjuder en rad olika spel, inklusive slots, bordsspel och live casino. En viktig del av spelupplevelsen är hur enkelt det är att göra uttag från ditt spelkonto.
Att göra uttag från Gogo casino är en enkel process. För att göra ett uttag måste du först logga in på ditt spelkonto och gå till sektionen för uttag. Där kan du välja hur mycket pengar du vill ta ut och vilken betalningsmetod du vill använda.
Gogo casino erbjuder flera olika betalningsmetoder för uttag, inklusive banköverföring, kreditkort och e-plånböcker. Oavsett vilken metod du väljer är det viktigt att du följer casinots regler och villkor för uttag för att undvika eventuella förseningar.
När du har begärt ett uttag kan det ta upp till 24 timmar för Gogo casino att behandla transaktionen. Efter det kommer pengarna att skickas till din valda betalningsmetod, och du bör kunna se dem på ditt konto inom några arbetsdagar.
Det är viktigt att komma ihåg att alla uttag från Gogo casino är föremål för en verifieringsprocess för att säkerställa att transaktionen är legitim. Du kan bli ombedd att skicka in dokument som bevis på din identitet och bostadsadress innan ditt uttag kan behandlas.
Sammanfattningsvis är Gogo casino ett pålitligt och säkert online casino som erbjuder en smidig uttagsprocess för sina spelare. Genom att följa casinots regler och villkor kan du snabbt och enkelt ta ut dina vinster och njuta av dina spelupplevelser.
https://gogocasino.one
Gogo Casino är en del av den välkända LeoVegas koncernen och erbjuder spelunderhållning i en modern och stilren miljö. Med ett stort utbud av casinospel och en användarvänlig plattform är Gogo Casino ett populärt val för många spelare.
PГҐ Gogo Casino kan du hitta ett brett urval av spel frГҐn flera av de bГ¤sta spelleverantГ¶rerna i branschen, inklusive NetEnt, Microgaming och Play’n GO. HГ¤r kan du spela allt frГҐn klassiska slots och bordsspel till live casino-spel med riktiga dealers.
En av fördelarna med att spela på Gogo Casino är att du inte behöver skapa ett konto för att komma igång. Istället använder du dig av BankID för att göra insättningar och uttag, vilket gör processen smidig och säker.
Gogo Casino har även ett generöst lojalitetsprogram där du kan samla poäng genom att spela och sedan använda dem för att få belöningar och förmåner. Dessutom erbjuder de regelbundna kampanjer och erbjudanden för sina spelare.
Sammanfattningsvis är Gogo Casino ett bra val för dig som vill ha en smidig och underhållande spelupplevelse. Med ett stort spelutbud, enkel registrering och fina belöningar är det här ett online casino som definitivt är värt att testa. Besök Gogo Casino idag och se själv vad de har att erbjuda!
https://gogocasino.one
Gogo Casino är en populär app för online-spel som erbjuder ett brett utbud av casinospel för alla spelare. Appen har tagit Sverige med storm genom sin användarvänliga design och stora utbud av spelautomater, bordsspel och live dealer-spel.
En av fördelarna med Gogo Casino är att man kan spela var som helst och när som helst genom att helt enkelt ladda ner appen på sin smartphone eller surfplatta. Spelarna kan njuta av sina favoritspel under en paus på jobbet, på bussen eller bara hemma i soffan.
Appen erbjuder också generösa bonusar och kampanjer för sina användare, vilket gör det ännu mer lockande att spela. Spelare kan få free spins, insättningsbonusar och andra belöningar när de spelar på Gogo Casino.
En annan fördel med appen är att den är säker och pålitlig, med säkra betalningsmetoder och krypterade transaktioner för att skydda spelarnas personliga och finansiella information.
Sammanfattningsvis är Gogo Casino en fantastisk app för alla som älskar att spela casinospel. Med sitt stora utbud av spel, generösa bonusar och användarvänliga design är det enkelt att förstå varför den har blivit så populär i Sverige. Så ladda ner appen och börja spela redan idag!
https://gogocasino.one
Gogo Casino är en populär spelsajt som erbjuder en mängd olika spelmöjligheter för sina användare. LeoVegas är ett av de största och mest kända onlinecasinona i Sverige. Tyvärr har det kommit uppgifter om att LeoVegas inte betalar ut vinster till spelare som vunnit på Gogo Casino.
Det är viktigt att poängtera att detta inte gäller alla användare eller alla spelare på Gogo Casino. De flesta spelare som vinner på Gogo Casino får sina vinster utbetalade utan problem. Men det finns tyvärr en del spelare som har haft svårigheter med att få sina vinster från LeoVegas.
Detta är naturligtvis mycket frustrerande för de spelare som har förlorat pengar och inte får tillbaka sina vinster. Det är viktigt att alla spelare är medvetna om risken för att detta kan hända och att man alltid bör vara försiktig när man spelar på onlinecasinon.
Det är oklart varför vissa spelare inte får sina vinster från LeoVegas, men det kan bero på olika faktorer såsom tekniska problem, felaktig information eller bedrägeri. Om du är en av de spelare som inte har fått dina vinster från LeoVegas rekommenderas att du kontaktar deras kundtjänst för att försöka lösa problemet.
Sammanfattningsvis är det viktigt att vara försiktig när man spelar på onlinecasinon och att man alltid läser villkoren noga innan man börjar spela. LeoVegas är ett välrenommerat företag och förhoppningsvis kommer de att kunna lösa problemet med de spelare som inte har fått sina vinster från Gogo Casino.
https://gogocasino.one
Gogo Casino har blivit ett populärt online casino för svenska spelare. En av anledningarna till dess framgång är dess program för affiliates, eller samarbetspartners. Gogo Casino affiliates har möjlighet att tjäna pengar genom att marknadsföra casinot och locka in nya spelare.
För de som är intresserade av att bli en Gogo Casino affiliate finns det flera fördelar. För det första erbjuder casinot generösa provisioner för varje spelare som registrerar sig via ens unika affiliate-länk. Detta innebär att affiliates kan tjäna en stadig inkomst genom att helt enkelt marknadsföra casinot på sina webbplatser eller sociala medier.
Dessutom har Gogo Casino ett dedikerat affiliateteam som finns tillgängliga för att hjälpa till med frågor eller problem. Detta innebär att affiliates får den support de behöver för att maximera sin försäljning och tjäna så mycket pengar som möjligt.
Det är också värt att notera att Gogo Casino är en pålitlig och respekterad operatör inom branschen. Detta innebär att affiliates kan vara säkra på att deras spelare kommer att behandlas rättvist och att deras intäkter kommer betalas ut i tid.
Sammanfattningsvis är Gogo Casino affiliates ett utmärkt sätt för personer att tjäna pengar genom att marknadsföra ett populärt online casino. Med generösa provisioner, dedikerad support och en pålitlig operatör är det en bra möjlighet för de som är villiga att satsa på att marknadsföra casinot.
https://gogocasino.one
Gogo Casino är en populär casinoplattform som erbjuder en spännande spelupplevelse på din mobil. Med Gogo Casino appen kan du njuta av ett brett utbud av casinospel var du än är.
Appen har ett smidigt gränssnitt som gör det enkelt att navigera mellan olika spelkategorier såsom slots, bordsspel och livecasino. Dessutom är appen optimerad för mobila enheter vilket ger en smidig och snabb spelupplevelse.
Gogo Casino appen erbjuder även generösa bonusar och kampanjer för sina spelare. Du kan få tillgång till freespins, bonuspengar och andra belöningar genom att spela regelbundet och delta i olika tävlingar.
En annan fördel med Gogo Casino appen är att den är säker och pålitlig. Alla transaktioner och personuppgifter skyddas med den senaste krypteringstekniken för att garantera en trygg spelupplevelse för alla spelare.
Sammanfattningsvis är Gogo Casino appen ett utmärkt val för alla som älskar casinospel och vill kunna spela var de än befinner sig. Med sitt stora spelutbud, generösa bonusar och säkra plattform är Gogo Casino appen definitivt värd att prova på. Ladda ner den idag och börja ditt casinoadventyr!
https://gogocasino.one
1. Почему берцы – это обязательный элемент стиля?
2. Как выбрать идеальные берцы для осеннего гардероба?
3. Тренды сезона: кожаные берцы или замшевые?
4. 5 способов носить берцы с платьем
5. Какие берцы выбрать для повседневного образа?
6. Берцы на платформе: комфорт и стиль в одном
7. Какие берцы будут актуальны в этом году?
8. Маст-хэв сезона: военные берцы в стиле милитари
9. 10 вариантов сочетания берцов с джинсами
10. Зимние берцы: как выбрать модель для холодного сезона
11. Элегантные берцы на каблуке: идеальный вариант для офиса
12. Секреты ухода за берцами: как сохранить первоначальный вид?
13. С какой юбкой носить берцы: советы от стилистов
14. Как подобрать берцы под фасон брюк?
15. Берцы на шнуровке: стильный акцент в образе
16. Берцы-челси: универсальная модель для любого стиля
17. С чем носить берцы на плоской подошве?
18. Берцы с ремешками: акцент на деталях
19. Как выбрать берцы для прогулок по городу?
20. Топ-5 брендов берцев: качество и стиль в одном
берці ua берці тактичні .
Thank you for great article. Hello Administ .Seo Hizmeti Skype : live:by_umut
Gogo Casino är ett populärt online casino som erbjuder en rad spännande spel och en enkel och smidig spelupplevelse. Men ibland kan det vara nödvändigt att kontakta dem direkt för att få svar på specifika frågor eller problem. Det är då bra att ha tillgång till deras telefonnummer.
Gogo Casino telefonnummer är ett sätt för spelare att snabbt och enkelt komma i kontakt med casinots kundtjänst. Det kan vara allt från att få hjälp med en transaktion, lösa ett tekniskt problem eller bara få mer information om casinots erbjudanden.
Att ha tillgång till telefonnummer är viktigt för en bra kundserviceupplevelse. Det ger spelarna en känsla av trygghet och att de verkligen tas på allvar av casinots team. Genom att kunna prata med en riktig person direkt kan många frågor lösas snabbare och enklare än via mail eller chatt.
Om du söker efter Gogo Casino telefonnummer kan du hitta det på deras hemsida eller genom att kontakta deras kundtjänst direkt. Det är alltid bra att ha detta nummer till hands om du behöver snabb hjälp eller support när du spelar på casinot.
Sammanfattningsvis är Gogo Casino telefonnummer ett viktigt verktyg för spelare som vill ha en smidig och enkel spelupplevelse. Genom att kunna kontakta casinots kundtjänst direkt kan många problem och frågor lösas snabbt och effektivt. Så se till att ha numret till hands nästa gång du spelar på Gogo Casino!
https://gogocasino.one
Gogo Casino erbjuder en spännande och underhållande spelupplevelse för alla sina spelare. För att se till att kunderna har en smidig och trevlig upplevelse har de en professionell och tillgänglig supporttjänst tillgänglig.
Casinots supportteam finns tillgängliga dygnet runt för att hjälpa till med alla frågor eller problem som kan uppstå under spelningen. Kunderna kan kontakta supporten via livechatt eller e-post, och de svarar snabbt och effektivt för att lösa eventuella bekymmer.
Supportteamet hos Gogo Casino är mycket kunnigt och välutbildat, vilket gör att de kan ge snabba och exakta svar på alla frågor som kunderna kan ha. Oavsett om det gäller tekniska problem, transaktionsfrågor eller spelrelaterade problem, kan spelarna lita på att supporten kommer att göra sitt bästa för att hjälpa dem.
För att säkerställa att spelarna får den bästa spelupplevelsen möjligt, strävar Gogo Casino efter att erbjuda en högkvalitativ supporttjänst. Genom att vara tillgänglig dygnet runt och erbjuda snabba svar på alla frågor och bekymmer, visar casinot sitt engagemang för sina kunder och deras spelupplevelse.
Sammanfattningsvis kan man säga att Gogo Casino är dedikerade till att ge sina spelare den bästa möjliga spelupplevelsen genom att erbjuda en professionell och tillgänglig supporttjänst. Med deras hjälp kan spelarna känna sig säkra och trygga när de spelar på casinot och veta att de alltid kan få hjälp när de behöver det.
https://gogocasino.one
mobajl porno
Great post thank you. Hello Administ . Seo Hizmeti Skype : live:by_umut
Gogo Casino är ett av de mest populära onlinecasinona idag och det är inte svårt att förstå varför. Med ett brett utbud av spel, generösa bonusar och en användarvänlig plattform har Gogo Casino lyckats locka till sig många spelare.
En av de mest framstående egenskaperna hos Gogo Casino är deras samarbete med LeoVegas, en annan ledande aktör inom nätcasinobranschen. LeoVegas är kända för sin höga kvalitet och sina innovativa spel, något som verkligen märks när man spelar på Gogo Casino.
Att spela på Gogo Casino är enkelt och smidigt. Du kan spela direkt i din webbläsare utan att behöva ladda ner någon speciell programvara. Dessutom erbjuder de en mobilvänlig plattform så att du kan spela var som helst och när som helst.
När det kommer till spelutbudet på Gogo Casino så finns det verkligen något för alla. Du hittar allt från klassiska spelautomater till bordsspel som roulette och blackjack. Dessutom erbjuder de även ett brett utbud av livecasinospel där du kan spela mot riktiga dealers i realtid.
För att locka till sig nya spelare erbjuder Gogo Casino generösa välkomstbonusar och regelbundna kampanjer och erbjudanden. Dessutom har de en pålitlig kundsupport som finns tillgänglig dygnet runt för att hjälpa till med eventuella frågor eller problem.
Sammanfattningsvis är Gogo Casino med sitt samarbete med LeoVegas en stark aktör på marknaden för onlinecasinon. Med sitt stora utbud av spel, generösa bonusar och användarvänliga plattform är det ett utmärkt val för alla som är intresserade av att spela casinospel online.
https://gogocasino.one
Gogo Casino Affiliates är ett program som erbjuder möjligheten för casino affiliates att tjäna pengar genom att marknadsföra Gogo Casino till nya spelare. Genom att samarbeta med Gogo Casino Affiliates kan affiliates tjäna provision genom att locka nya spelare att registrera sig och spela på Gogo Casino.
Gogo Casino är en populär onlinecasino som erbjuder ett brett utbud av casinospel och slots för sina spelare. Genom att marknadsföra Gogo Casino till potentiella spelare kan affiliates dra nytta av den växande populariteten hos onlinecasinon och tjäna pengar genom att skicka spelare till Gogo Casino.
För att bli en affiliate för Gogo Casino måste man först registrera sig för programmet och sedan börja marknadsföra casinot genom olika kanaler som sin egen hemsida, sociala medier eller via e-postmarknadsföring. Affiliates kan också ta del av olika marknadsföringsmaterial från Gogo Casino för att underlätta sin marknadsföring.
Genom att bli en del av Gogo Casino Affiliates får man tillgång till en dedikerad affiliate manager som kan hjälpa till med frågor och support. Dessutom erbjuds affiliates regelbundna utbetalningar av provision baserat på antalet spelare som de hänvisar till Gogo Casino.
Sammanfattningsvis är Gogo Casino Affiliates ett bra sätt för casino affiliates att tjäna pengar genom att marknadsföra ett populärt onlinecasino till nya spelare. Genom att dra nytta av den växande populariteten hos onlinecasinon kan affiliates skapa en stabil inkomstkälla genom att samarbeta med Gogo Casino Affiliates.
https://gogocasino.one
Cialis over the counter Buy Cialis online Buy Tadalafil 20mg
Gogo Casino är ett populärt online casino som erbjuder spelare en enkel och smidig spelupplevelse. För de som behöver komma i kontakt med casinots kundtjänst finns det ett telefonnummer att ringa.
Att ha tillgång till ett telefonnummer för att få support är viktigt för många spelare. Hos Gogo Casino kan spelare ringa till casinoets kundtjänst för att få svar på sina frågor eller lösa eventuella problem som kan uppstå under spelandet.
Genom att ringa telefonnumret till Gogo Casino kan spelare få snabb och personlig support direkt från kundtjänstens professionella och vänliga medarbetare. Det finns inget behov av att vänta på svar via e-post eller livechatt, vilket gör det enkelt för spelare att få hjälp när de behöver det.
Telefonnumret till Gogo Casino kan hittas på deras webbplats eller i deras app. Spelare uppmanas att anteckna telefonnumret eller spara det i sina kontakter för att kunna komma i kontakt med kundtjänsten när det behövs.
Sammanfattningsvis är Gogo Casino ett online casino som sätter spelarnas behov i fokus genom att erbjuda en enkel och smidig spelupplevelse samt tillgång till telefonnummer för att få support när det behövs. Spelare som spelar hos Gogo Casino kan känna sig trygga i vetskapen om att de kan få hjälp snabbt och enkelt vid behov.
https://gogocasino.one
anyone fan chooses porn sites that can please even more
than unique 無料 ゲイ 動画 ポルノ.
Feel free to surf to my blog post :: video porno jepang xxx
Gogo Casino Kundtjänst: Allt du behöver veta
Gogo Casino är en populär online spelplattform som erbjuder ett brett utbud av casinospel för sina spelare. För att säkerställa en problemfri spelupplevelse för alla sina kunder, erbjuder Gogo Casino en dedikerad kundtjänst som är tillgänglig dygnet runt för att hjälpa till med alla frågor eller bekymmer.
Gogo Casino kundtjänst är känd för sin professionella och vänliga service. Kundtjänstteamet är välutbildat och kan hjälpa dig med allt från tekniska frågor till frågor om insättningar och uttag. Om du har några problem med att komma åt ditt konto eller om du har frågor om bonusar eller kampanjer, kan du enkelt kontakta kundtjänsten via livechatt, e-post eller telefon.
En av fördelarna med att spela på Gogo Casino är att du kan få hjälp på ditt modersmål. Kundtjänstteamet talar flera olika språk, inklusive svenska, så du kan vara säker på att du kommer att få den hjälp du behöver på ett språk som du förstår.
FГ¶r att komma i kontakt med Gogo Casino kundtjГ¤nst, behГ¶ver du bara klicka pГҐ fliken “Kontakta oss” pГҐ webbplatsen. DГ¤r hittar du alla kontaktuppgifter du behГ¶ver fГ¶r att komma i kontakt med teamet.
Sammanfattningsvis, om du spelar på Gogo Casino och behöver hjälp med något, kan du vara säker på att du kommer att få den bästa kundtjänsten. Med snabb och effektiv hjälp till hands dygnet runt kan du fortsätta njuta av ditt spelande utan att behöva oroa dig för något. Gogo Casino kundtjänst är här för att göra din spelupplevelse så smidig och trevlig som möjligt.
https://gogocasino.one
Gogo casino är en populär online casino som har fått mycket uppmärksamhet på senare tid, särskilt på sajten AskGamblers. AskGamblers är en webbplats där spelare kan lämna recensioner och betyg om olika online casinon, och Gogo casino har fått mycket positiv feedback därifrån.
En av anledningarna till att Gogo casino har blivit så populärt på AskGamblers är på grund av dess stora spelutbud. De erbjuder ett brett urval av spel från flera olika spelleverantörer, vilket gör att det finns något för alla typer av spelare. Dessutom erbjuder de också generösa bonusar och kampanjer för sina spelare, vilket gör det ännu mer attraktivt att spela där.
En annan anledning till Gogo casinos popularitet på AskGamblers är deras kundservice. De är kända för att ha en engagerad och professionell kundtjänst som alltid är tillgänglig för spelarna. De är snabba att svara på frågor och lösa eventuella problem som kan uppstå, vilket ger spelarna en trygg och säker spelupplevelse.
Sammanfattningsvis är Gogo casino en pålitlig och välrenommerad online casino som har fått mycket uppskattning på AskGamblers. Med sitt stora spelutbud, generösa bonusar och bra kundservice är det inte konstigt att så många spelare har valt att spela där. Om du letar efter ett pålitligt och underhållande online casino, kan Gogo casino vara ett bra val att prova på.
https://gogocasino.one
Слушай, компаньон! Я в курсе, что ты размышляешь, для чего для тебя лазить по нашему сайту, хотя давай-ка я поведаю тебе почему это круто, а?
https://volleyball.tut.md/index.php/forum/obshchij/185-gislaved-md-vash-nadezhnyj-postavshchik-shin-gislaved
Во-первых, тут ты найдешь вагон полезной инфы! собственно что бы ты ни искал – от советов по саморазвитию до лайфхаков для совершенствования обстановки – у нас есть все, собственно что для тебя надо(надобно) для становления и вдохновения.
Но далеко не все! У нас здесь целое сообщество, как клуб “Без Карантина”, где тебе предоставляется возможность знаться с крутыми ребятами, делиться своими мыслями и получать поддержку в каждой ситуации.
А еще на нашем сайте всегда что-то происходит! Промоакции, состязания, онлайн-мероприятия – в общем, все, дабы ты не соскучился и практически постоянно оставался в курсе самых свежих направленностей.
Так что, старина, не тяни кота за хвост! Загляни на наш вебсайт и давай совместно развиваться, общаться и веселиться! Я уверен, ты здесь найдешь себе по-настоящему крутых приятелей и море позитива!
Cheapest Sildenafil online cheapest viagra Viagra Tablet price
Gogo casino se är en populär online casino sida som erbjuder ett brett utbud av casinospel för både nybörjare och erfarna spelare. På denna sida kan du hitta allt från klassiska spelautomater till bordsspel som blackjack och roulette.
Det som skiljer Gogo casino se från andra online casinon är deras generösa bonusar och erbjudanden. För nya spelare finns det en välkomstbonus som ger dig extra pengar att spela för samt free spins på utvalda spelautomater. Dessutom kan du ta del av regelbundna kampanjer och tävlingar där du har chansen att vinna fina priser.
En annan fördel med Gogo casino se är deras smidiga och säkra betalningsmetoder. Du kan göra insättningar och uttag med hjälp av bland annat banköverföring, kreditkort och e-plånböcker. Alla transaktioner är krypterade för att säkerställa att dina pengar och personuppgifter skyddas på bästa sätt.
När det kommer till spelutbudet så samarbetar Gogo casino se med flera av de bästa spelleverantörerna i branschen, vilket garanterar att du hittar de senaste och mest populära spelen på deras sida. Oavsett om du föredrar slots, poker eller live casino så finns det något för alla smaker på Gogo casino se.
Sammanfattningsvis så är Gogo casino se en pålitlig och underhållande spelsida som erbjuder en förstklassig upplevelse för alla som gillar att spela casino online. Med deras generösa bonusar, säkra betalningsmetoder och stora spelutbud är det lätt att förstå varför så många väljer att spela på Gogo casino se. Besök sidan idag och bli en del av gemenskapen du också!
https://gogocasino.one
Gogo Casino och LeoVegas är två populära onlinekasinon som många svenskar har börjat använda för att spela sina favoritspel. Men tyvärr har det nyligen kommit uppgifter om att vissa spelare upplever problem med att få sina vinster utbetalade.
Många kunder har rapporterat att de har haft svårigheter att få ut sina pengar från Gogo Casino och LeoVegas. Vissa har hävdat att deras uttagsförfrågningar har blivit avvisade utan förklaring, medan andra säger att de har väntat länge på sina pengar utan att få någon information om varför det dröjer.
Det är självklart mycket frustrerande för de drabbade spelarna att inte kunna få ut sina vinster från kasinot. Många har förlorat förtroendet för dessa platser och överväger att byta till andra onlinekasinon.
Det är viktigt att företagen bakom Gogo Casino och LeoVegas tar dessa problem på allvar och ser till att alla kunder får sina vinster utan dröjsmål. Det är också viktigt att de är transparenta med sina kunder och ger tydlig information om varför eventuella utbetalningar försenas.
Svenska spelare borde kunna lita på att deras vinster behandlas på ett rättvist och pålitligt sätt. Förhoppningsvis kommer Gogo Casino och LeoVegas att åtgärda dessa problem och återställa förtroendet hos sina kunder.
https://gogocasino.one
Gogo Casino.se är en av Sveriges mest populära onlinecasinosajter. Med ett brett utbud av spel och en användarvänlig plattform har sajten snabbt blivit en favorit bland svenska spelare.
Gogo Casino.se erbjuder ett stort utbud av spelautomater, bordsspel och livecasinospel från ledande spelutvecklare som NetEnt, Microgaming och Evolution Gaming. Oavsett om du är ute efter att spela klassiska slots, blackjack eller roulette finns det något för alla på sajten.
En av fördelarna med att spela på Gogo Casino.se är att sajten är optimerad för spel i mobilen. Detta innebär att du kan njuta av dina favoritspel var som helst och när som helst. Dessutom erbjuder sajten en säker och trygg spelupplevelse med snabba uttag och pålitlig kundtjänst.
För de som gillar att ta del av spännande kampanjer och erbjudanden finns det regelbundet bonusar och belöningar att ta del av på Gogo Casino.se. Så oavsett om du är en ny spelare eller en erfaren veteran kommer du garanterat att hitta något som passar dig på sajten.
Sammanfattningsvis är Gogo Casino.se en pålitlig och underhållande spelsajt som erbjuder enastående spelupplevelser för alla typer av spelare. Med sitt stora spelutbud, mobila kompatibilitet och generösa bonusar är det inte konstigt att sajten har blivit en populär destination för svenska spelare. Besök Gogo Casino.se idag för att ta del av allt som sajten har att erbjuda!
https://gogocasino.one
Gogo Casino är ett online casino som erbjuder massor av spännande spel och underhållning för alla spelälskare där ute. Med ett stort utbud av spelautomater, bordsspel och live casinospel är det här en plats där man kan njuta av den bästa casinoupplevelsen.
Men vad händer om du stöter på problem eller har frågor när du spelar på Gogo Casino? Då kan du alltid vända dig till deras kundtjänst för hjälp och support. Gogo Casino har en dedikerad supportteam som är där för att underlätta din spelupplevelse och lösa eventuella frågor eller bekymmer du kan ha.
Du kan kontakta Gogo Casino support på flera olika sätt. En av de enklaste är att använda deras live chatt-funktion, där du kan kommunicera direkt med en representant och få omedelbar hjälp. Du kan också skicka ett e-postmeddelande till deras supportadress om du föredrar att kommunicera på det sättet.
Gogo Casino supportteam är tillgängligt dygnet runt för att säkerställa att du alltid får den hjälp du behöver när du spelar på deras plattform. Oavsett om det handlar om tekniska frågor, insättnings- eller uttagsproblem eller bara allmänna frågor om spelen, kan du lita på att Gogo Casino support är där för att hjälpa till.
Så om du någonsin har några frågor eller bekymmer när du spelar på Gogo Casino, tveka inte att kontakta deras supportteam. De är där för att säkerställa att din spelupplevelse är smidig och rolig så att du kan fokusera på att njuta av dina favoritspel och vinna stora vinster. Gogo Casino support är bara ett klick bort!
https://gogocasino.one
Gogo Casino är en online-spelplattform som har blivit väldigt populär bland spelare på senare tid. En av anledningarna till dess popularitet är dess transparens i spel och transaktioner.
Gogo Casino har gjort det till en prioritet att vara transparent i allt de gör. Det innebär att spelarna kan vara säkra på att deras personliga information och pengar hanteras på ett säkert sätt. Genom att använda den senaste krypteringstekniken kan spelarna känna sig trygga när de spelar på Gogo Casino.
En annan aspect av transparensen på Gogo Casino är dess spel. Spelarna kan enkelt se resultaten av varje spel och veta att de är rättvisa och slumpmässiga. Detta skapar en känsla av tillit och trygghet bland spelare.
För att ytterligare stärka sin transparens har Gogo Casino också ett tydligt och lättförståeligt bonussystem. Spelarna kan enkelt se vilka bonusar som är tillgängliga för dem och vilka regler och villkor som gäller för varje bonus.
Sammanfattningsvis är transparensen på Gogo Casino en av anledningarna till dess framgång. Genom att vara öppna och ärliga gentemot sina spelare skapar de en trygg och pålitlig spelupplevelse för alla som använder plattformen.
https://gogocasino.one
Gogo Casino är en av Sveriges senaste tillskott när det kommer till online-casinon. Med ett modernt och användarvänligt gränssnitt erbjuder de sina spelare en spännande spelupplevelse. Men hur bra är egentligen Gogo Casino? I detta omdöme kommer vi att gå igenom lite mer om vad casinot har att erbjuda.
Innan vi går in på detaljer om spelen och erbjudandena hos Gogo Casino, är det viktigt att notera att de har en svensk spellicens vilket innebär att de följer strikta regler och villkor för att säkerställa en säker och rättvis spelupplevelse för sina spelare.
NГ¤r det kommer till spelutbudet hos Gogo Casino finns det ett brett urval av spel att vГ¤lja mellan. HГ¤r hittar du allt frГҐn klassiska slots till moderna videoslots och bordsspel som blackjack och roulette. Casinot samarbetar med flera vГ¤lkГ¤nda spelleverantГ¶rer sГҐsom NetEnt, Microgaming och Play’n GO vilket garanterar hГ¶gklassiga spel och en bra spelupplevelse.
För de som föredrar att spela live-casino finns det även ett stort utbud av live-bordsspel som roulette, blackjack och baccarat. Hos Gogo Casino kan du spela mot riktiga dealers och känna dig som om du befinner dig på ett riktigt casino.
När det kommer till välkomstbonusar och erbjudanden så har Gogo Casino ett generöst välkomstpaket för nya spelare. Dessutom erbjuder de regelbundet kampanjer och tävlingar där spelare har chansen att vinna extra priser och bonusar.
Sammanfattningsvis är Gogo Casino ett pålitligt och underhållande online-casino med ett brett spelutbud och generösa erbjudanden. Om du letar efter ett nytt online-casino att prova på är Gogo Casino definitivt värt att kika närmare på. Med deras höga säkerhetsstandard och spelvariation kan du känna dig trygg och njuta av en spännande spelupplevelse.
https://gogocasino.one
Gogo Casino är en spännande app för alla som älskar att spela casinospel på mobilen. Med ett brett utbud av spel och generösa bonuserbjudanden är detta en app som lockar många spelare.
Gogo Casino erbjuder ett stort utbud av spelautomater, bordsspel och live casinospel. Oavsett om du föredrar klassiska spelautomater eller mer avancerade videoslots finns det något för alla här. Dessutom kan du njuta av autentiska casinoupplevelser genom att spela live blackjack, roulette eller baccarat.
En av fördelarna med att använda Gogo Casino app är att du kan spela när som helst och var som helst. Du behöver inte längre sitta vid din dator för att kunna spela dina favoritspel, utan du kan ha dem med dig i fickan. Detta gör det enklare för dig att spela och ökar tillgängligheten.
För att öka spänningen och ge dig chansen att vinna stort erbjuder Gogo Casino regelbundna bonuserbjudanden och kampanjer. Du kan få bonusar vid insättningar, free spins eller delta i tävlingar med fina priser. På så sätt kan du få mer valuta för dina pengar och öka dina vinstchanser.
Sammanfattningsvis är Gogo Casino app en bra plattform för alla som älskar att spela casinospel. Med sitt stora spelutbud, generösa bonuserbjudanden och smidiga användarupplevelse är det en app som passar alla typer av spelare. Så ladda ner appen idag och börja spela för att ha chansen att vinna stort!
https://gogocasino.one
Gogo Casino utbetalning är snabb och enkel för alla spelare som är ute efter att få ut sina vinster. Med en modern och smidig plattform erbjuder Gogo Casino spelare möjligheten att snabbt och säkert ta ut sina pengar.
Det första steget för att göra en utbetalning på Gogo Casino är att logga in på sitt spelkonto. Därefter väljer spelaren den summa hen vill ta ut och vilket uttagsalternativ hen föredrar. Gogo Casino erbjuder flera olika betalningsmetoder, inklusive banköverföring, e-plånböcker och kreditkort.
När spelaren har valt sin uttagsmetod behandlas utbetalningen vanligtvis inom ett par timmar, vilket innebär att spelaren snabbt kan få tillgång till sina vinster. Gogo Casino strävar efter att erbjuda en smidig och effektiv utbetalningsprocess för alla sina spelare.
För att säkerställa att utbetalningen går smidigt är det viktigt att spelaren har verifierat sitt konto genom att skicka in nödvändig dokumentation. Detta är en standard procedur för att följa regler och riktlinjer för spellicenser och säkerhet.
Gogo Casino utbetalning är enkel och tillgänglig för alla spelare som är ute efter att ta ut sina vinster på ett säkert och pålitligt sätt. Med en snabb och effektiv utbetalningsprocess kan spelare njuta av sina vinster utan krångel. Besök Gogo Casino idag och upplev den enkla och smidiga utbetalningen för dig själv!
https://gogocasino.one
abilify 15mg usa
Gogo Casino är en populär online-spelplattform som erbjuder spelare en mängd olika casinospel att välja mellan. En av de mest kända webbplatserna för onlinespel är Leovegas, en annan populär plattform som erbjuder ett brett utbud av spel och slots.
Tyvärr finns det vissa användare som har upplevt problem med att inte få betalningar från Gogo Casino Leovegas. Detta har orsakat en hel del oro och frustration bland spelarna som har vunnit pengar och försöker ta ut sina vinster.
Anledningen till att vissa spelare inte får sina betalningar kan vara på grund av olika skäl, som tekniska problem, verifieringsproblem eller andra administrativa problem. Det är viktigt att spelare följer de riktlinjer som webbplatsen anger för att kunna ta ut sina vinster utan problem.
Om du upplever problem med att inte få betalningar från Gogo Casino Leovegas, är det bäst att kontakta deras kundtjänst så snart som möjligt för att lösa problemet. Det är också viktigt att vara tålmodig och vara beredd att följa de instruktioner som webbplatsen ger för att lösa problemet.
Sammanfattningsvis är det viktigt att vara medveten om möjliga problem med betalningar på online-casinon och att vara förberedd på att hantera dem på ett konstruktivt sätt. Med rätt förståelse och kommunikation kan problemet oftast lösas snabbt och enkelt.
https://gogocasino.one
Gogo Casino är en populär online casino app som erbjuder spelare en spännande och underhållande spelupplevelse direkt i sina mobila enheter. Med ett stort utbud av casinospel, är Gogo Casino appen perfekt för alla som älskar att spela kasinospel när som helst och var som helst.
En av de främsta fördelarna med Gogo Casino appen är att den är mycket användarvänlig och enkel att navigera. Det innebär att även de som är nya till online kasinospel kan enkelt komma igång och njuta av spelen utan några problem. Appen är även designad för att vara responsiv och snabb, vilket ger spelarna en smidig spelupplevelse utan några fördröjningar.
Gogo Casino appen erbjuder ett brett utbud av casinospel, inklusive slots, bordsspel, live casino och mycket mer. Spelare kan välja mellan hundratals olika spel från några av de bästa spelleverantörerna i branschen, vilket ger dem många alternativ att välja mellan. Oavsett om du föredrar klassiska spelautomater, progressiva jackpottspel eller live dealer spel, finns det något för alla på Gogo Casino appen.
Utöver det imponerande spelutbudet erbjuder Gogo Casino appen även generösa bonusar och kampanjer för sina spelare. Detta inkluderar välkomstbonusar, insättningsbonusar, gratissnurr och mycket mer, vilket ger spelarna extra valuta för sina pengar och ökar deras vinstchanser.
Sammanfattningsvis är Gogo Casino appen en utmärkt plattform för alla som älskar att spela kasinospel på nätet. Med sin användarvänliga design, stora spelutbud och generösa bonusar, är det verkligen en av de bästa casino apparna på marknaden idag. Så ladda ner Gogo Casino appen idag och börja njuta av spännande kasinospel direkt i din mobila enhet!
https://gogocasino.one
Gogo Casino Uttag
Gogo Casino är ett populärt online casino som erbjuder spelare en rolig och underhållande spelupplevelse. En viktig del av att spela på ett online casino är att kunna göra uttag av sina vinster på ett smidigt och säkert sätt.
På Gogo Casino finns det flera olika alternativ för uttag av vinster. En av de mest populära metoderna är att använda sig av banköverföring. Med denna metod kan spelare enkelt överföra sina vinster till sitt bankkonto inom några få bankdagar.
En annan vanlig metod för uttag på Gogo Casino är att använda sig av e-plånböcker som Skrill eller Neteller. Dessa e-plånböcker gör det möjligt för spelare att snabbt och enkelt överföra sina vinster till sitt e-plånbokskonto.
För de spelare som föredrar att använda sig av kreditkort finns även möjligheten att göra uttag på Gogo Casino med Visa eller Mastercard. Dessa metoder är snabba och enkla att använda, och pengarna kommer vanligtvis in på spelarens konto inom några bankdagar.
Oavsett vilken metod spelare väljer för sina uttag på Gogo Casino kan de vara säkra på att deras pengar kommer att hanteras på ett tryggt och säkert sätt. Gogo Casino sätter alltid spelarnas säkerhet i första hand och använder sig av avancerade krypteringsmetoder för att skydda spelarnas personliga och finansiella information.
Sammanfattningsvis erbjuder Gogo Casino flera olika alternativ för uttag av vinster, och spelarna kan vara säkra på att deras pengar kommer att hanteras på ett tryggt och säkert sätt. Med snabba uttag och en hög nivå av säkerhet är Gogo Casino ett utmärkt val för alla som vill njuta av en spännande spelupplevelse online.
https://gogocasino.one
Henkuai y Marca Espanahan organizado la visita de los diez influencers chinos mas importantes a Espana con el objetivo de promocionar el pais. Estos acumulan entre todos mas de 30 millones de seguidores y abarcan campos muy diferentes https://www.libertaddigital.com/chic/entretenimiento/2016-09-21/fan-bingbing-las-increibles-cifras-alrededor-de-la-mayor-estrella-china-1276582941/
https://elementor.com/
Отечественный производитель продает силовые тренажеры https://trenazher-silovoj.ru для напряженной работы в коммерческих тренировочных клубах.
Изучите каталог выпускаемых устройств блочных и с блинами.
Все модели дают возможность прорабатывать изолированно любые отделы мышц.
Оформляйте дельта машину, станок для гакк приседаний, одинарный Кроссовер, Баттерфляй для грудных, машину Смита, вертикальную тягу, скамью Скотта, Гравитрон, обратную гиперэкстензию, скамьи для жима со стойками, рычажные Хаммеры.
Производимый тренажер предназначен для пользователей с разным уровнем физической активности.
Производимое оборудование полностью надежно и не нуждается в техническом наблюдении.
Приобретите грузоблок подходящей массы.
According to our research and estimates, lev casino has
lower revenue from point of view online casinos.
Feel free to visit my blog post: jozz casino
Gogo casino.se är en spännande nyhet på den svenska spelmarknaden. Denna underhållande och användarvänliga spelsajt erbjuder en mängd spännande casinospel och slots för alla typer av spelare.
På Gogo casino.se finns det ett brett utbud av casinospel att välja mellan. Här hittar man klassiska casinospel som blackjack, roulette och poker, men även populära slots och spelautomater. Sajten samarbetar med flera kända spelleverantörer, vilket garanterar en hög kvalitet på spelen och en härlig spelupplevelse.
Det som verkligen utmärker Gogo casino.se är deras generösa välkomstbonusar och erbjudanden till nya spelare. Här kan man ta del av bonusar, free spins och andra förmåner som gör det extra roligt att spela. Dessutom har sajten ett lojalitetsprogram där man kan samla poäng för varje spel och få belöningar i form av bonuserbjudanden och andra förmåner.
En annan fördel med Gogo casino.se är deras användarvänliga plattform och smidiga betalningsmetoder. Sajten är enkel att navigera och man kan enkelt sätta in och ta ut pengar med hjälp av säkra betalningsmetoder som banköverföring, kreditkort och e-plånböcker.
Sammanfattningsvis är Gogo casino.se en spännande och pålitlig spelsajt som erbjuder ett brett utbud av underhållande casinospel och slots. Med generösa bonusar och erbjudanden, smidiga betalningsmetoder och en användarvänlig plattform är detta definitivt värt ett besök för alla som gillar att spela casinospel online. Besök Gogo casino.se idag och upplev spänningen själv!
https://gogocasino.one
you have the opportunity observe trends, according to with arrows under the rating of casinos, but to see if the
Voredbet Casino has retained former positions, whether it has
increased or completely has decreased since
last month.
Feel free to visit my website; Vdcasino Güncel Giriş Adresi
cheap kamagra Kamagra Iq Kamagra 100mg
Gogo Casino är en populär online-spelsajt som erbjuder ett brett utbud av casinospel för sina kunder att njuta av. För att säkerställa en smidig och problemfri spelupplevelse, erbjuder Gogo Casino en professionell och effektiv kundsupporttjänst för att hjälpa spelarna med eventuella frågor eller problem de kan stöta på.
Gogo Casino support är tillgänglig dygnet runt via livechatt, e-post och telefon. Det betyder att oavsett när du spelar eller vilket problem du stöter på, finns det alltid någon tillgänglig för att hjälpa till. Den vänliga och kunniga supportpersonalen på Gogo Casino är tränade för att kunna lösa alla typer av frågor eller bekymmer som spelarna kan ha.
När du kontaktar Gogo Casino support kan du förvänta dig snabba svar och effektiva lösningar på dina problem. Kundsupportteamet är dedikerade till att ge spelarna den bästa möjliga upplevelsen och att se till att deras behov och frågor tas om hand på ett professionellt sätt.
Utöver att lösa problem eller frågor kan Gogo Casino support också ge spelarna information om de olika spelfunktionerna, bonusar och kampanjer som erbjuds på sajten. Det gör det enkelt för spelare att dra nytta av alla fördelar som Gogo Casino har att erbjuda.
Sammanfattningsvis kan man sГ¤ga att Gogo Casino support Г¤r en viktig del av spelupplevelsen och nГҐgot som spelarna kan lita pГҐ fГ¶r att fГҐ den hjГ¤lp de behГ¶ver nГ¤r de spelar pГҐ sajten. Med sin dedikerade och professionella personal Г¤r Gogo Casino support redo att hjГ¤lpa dig med alla dina frГҐgor eller problem, oavsett nГ¤r de uppstГҐr. SГҐ om du behГ¶ver hjГ¤lp, tveka inte att kontakta Gogo Casino support – de Г¤r hГ¤r fГ¶r att hjГ¤lpa dig!
https://gogocasino.one
Everything is very open and very clear explanation of issues. was truly information.活婴儿色情片
Vidalista 20 – This is a quality product for men who want to increase their masculine abilities in intimate life effectively and safely vidalista 10 kaufen in deutschland
LeoVegas är en av de mest kända online casinona i Sverige och en populär destination för spelentusiaster som vill ha en spännande och underhållande spelupplevelse. Gogo Casino är en del av LeoVegas Group och erbjuder en modern och smidig plattform för spelare att njuta av sina favoritspel.
Gogo Casino är känt för sitt stora utbud av spelautomater, bordsspel och live casinospel. Med ett lättanvänt gränssnitt och en mobilvänlig design kan spelare enkelt komma åt sina favoritspel var de än befinner sig. Dessutom erbjuder Gogo Casino attraktiva kampanjer och bonusar för att belöna sina spelare och hålla dem engagerade.
En av fördelarna med att spela på Gogo Casino är deras snabba och säkra betalningsmetoder. Spelare kan sätta in och ta ut pengar på ett smidigt sätt utan att behöva vänta länge på sina vinster. Dessutom erbjuder Gogo Casino en professionell och tillgänglig kundsupport som finns till hands för att hjälpa spelare med eventuella frågor eller problem.
Sammanfattningsvis är Gogo Casino på LeoVegas en utmärkt plattform för spelare som vill ha en toppmodern och pålitlig spelupplevelse. Med sitt stora spelutbud, generösa bonusar och professionella kundsupport är Gogo Casino ett bra val för alla som älskar att spela online casino. Besök Gogo Casino idag och upplev spänningen själv!
https://gogocasino.one
Recomendo o popular jogo a todos Fortune Tiger
Gogo casino är en relativt ny spelplattform som lanserades 2019 och har redan blivit populär bland svenska spelare. En av de främsta anledningarna till dess popularitet är dess rykte på den välkända webbplatsen AskGamblers.
AskGamblers är en av de mest respekterade och pålitliga oberoende recensionswebbplatserna för onlinekasinon. Där kan spelare lämna sina recensioner och betyg för olika kasinon baserat på deras upplevelser. Gogo Casino har fått fantastiska recensioner och höga betyg från spelare på AskGamblers, vilket har bidragit till att öka dess popularitet.
Spelare som har registrerat sig på Gogo Casino har uppskattat dess generösa bonusar och kampanjer, snabba uttag, och ett imponerande spelutbud med de senaste och mest populära spelen från ledande spelleverantörer. Dessutom har kasinot ett användarvänligt gränssnitt och en responsiv kundsupport som är tillgänglig dygnet runt.
Att vara godkänd och rekommenderad av AskGamblers är ett tydligt tecken på Gogo Casinos pålitlighet och höga standarder när det gäller spelupplevelse och kundtillfredsställelse. Om du letar efter ett pålitligt och spännande onlinekasino att spela på, kan Gogo Casino vara det perfekta valet för dig. Med dess högsta betyg på AskGamblers kan du känna dig trygg med att du spelar på en plattform som prioriterar spelares behov och ger en förstklassig spelupplevelse.
https://gogocasino.one
keflex 250 mg canada
buy Kamagra Kamagra Iq Kamagra 100mg
Gogo Casino är en spännande och underhållande online kasino som erbjuder en rad olika spel och möjligheter att vinna stora priser. Med ett användarvänligt gränssnitt och en mängd olika spel att välja mellan är Gogo Casino det perfekta valet för alla som älskar att spela kasinospel.
När du spelar på Gogo Casino kommer du att ha tillgång till ett brett utbud av populära spel som slots, bordsspel, och live kasinospel. Oavsett om du är intresserad av att spela klassiska kasinospel som blackjack och roulette eller om du föredrar att spela de senaste spännande slotsen, har Gogo Casino något för alla.
En av de största fördelarna med att spela på Gogo Casino är att du kan spela var som helst och när som helst. Du kan enkelt logga in på ditt konto från din dator, mobiltelefon eller surfplatta och börja spela dina favoritspel direkt. Dessutom kan du göra insättningar och ta ut dina vinster på ett säkert och smidigt sätt med hjälp av olika betalningsmetoder som kreditkort, banköverföring och e-plånböcker.
Gogo Casino är känd för sin höga kvalitet och säkerhet. Alla spel är certifierade och rättvisa, och din personliga information skyddas med hjälp av avancerad krypteringsteknik. Dessutom erbjuder Gogo Casino kontakt med en professionell och vänlig kundtjänst för att lösa eventuella frågor eller problem som kan uppstå under ditt spelande.
Sammanfattningsvis är Gogo Casino en fantastisk plattform för alla som älskar kasinospel. Med sitt stora utbud av spel, användarvänliga gränssnitt och säkra betalningsmetoder är det en perfekt plats att koppla av och ha kul när som helst och var som helst. Besök Gogo Casino idag och upplev spänningen med att spela på ett av de bästa online kasinona på marknaden!
https://gogocasino.one
Gogo Casino – en trasnparent spelupplevelse
Gogo Casino har snabbt blivit en populär destination för spelare som söker en transparent och säker spelupplevelse. Med sitt enkla och stilrena gränssnitt har casinot skapat en plattform där spelarna kan njuta av sina favoritspel utan krångliga villkor eller dolda avgifter.
Ett av de främsta kännetecknen för Gogo Casino är dess transparenta approach till spelutbud och regler. Spelarna kan enkelt navigera bland olika spelkategorier och hitta sina favoriter utan att behöva leta igenom en massa onödig information. Dessutom erbjuder casinot tydliga regler och villkor som är lättillgängliga för alla spelare.
När det kommer till transaktioner och betalningar är Gogo Casino också mycket transparent. Spelarna kan enkelt sätta in och ta ut pengar utan att behöva oroa sig för dolda avgifter eller otydliga regler. Casinot erbjuder också flera olika betalningsmetoder, vilket gör det lätt för spelarna att välja den metod som passar dem bäst.
Utöver sin transparenta approach är Gogo Casino också känt för sitt stora spelutbud. Här hittar spelarna alla sina favoritspel från välkända spelleverantörer, vilket gör att det finns något för alla smaker. Dessutom erbjuder casinot regelbundet kampanjer och bonusar som ger spelarna ännu mer spänning och underhållning.
Sammanfattningsvis är Gogo Casino en idealisk destination för spelare som värdesätter transparens och säkerhet i sin spelupplevelse. Med sitt enkla gränssnitt, tydliga regler och stora spelutbud har casinot skapat en plattform där spelarna kan njuta av sina favoritspel utan bekymmer. Gogo Casino är definitivt värt ett besök för alla som letar efter en trygg och transparent spelupplevelse.
https://gogocasino.one
Gogo Casino Leovegas är ett populärt online casino som erbjuder många spännande spel och generösa bonusar för sina spelare. Med sitt moderna och användarvänliga gränssnitt har Gogo Casino Leovegas snabbt blivit en favorit bland svenska spelare.
En av de främsta fördelarna med Gogo Casino Leovegas är det stora utbudet av spel som erbjuds. Här kan spelare hitta allt från klassiska slots och bordsspel till live casino och progressiva jackpottspel. Oavsett vilken typ av spel man föredrar, finns det något för alla att njuta av på Gogo Casino Leovegas.
Förutom det stora spelutbudet erbjuder Gogo Casino Leovegas också generösa bonusar och kampanjer för sina spelare. Nya spelare välkomnas med en välkomstbonus som ger dem extra pengar att spela för, medan återkommande spelare kan dra nytta av regelbundna kampanjer och belöningar.
Dessutom är Gogo Casino Leovegas känt för sin säkerhet och pålitlighet. Alla transaktioner och personuppgifter skyddas med den senaste krypteringstekniken, vilket ger spelarna trygghet när de spelar online.
Sammanfattningsvis är Gogo Casino Leovegas ett utmärkt val för alla som söker en spännande och pålitlig spelupplevelse online. Med sitt stora spelutbud, generösa bonusar och höga säkerhetsstandarder är det lätt att se varför så många svenska spelare väljer att spela på Gogo Casino Leovegas.
https://gogocasino.one
Gogo Casino är ett populärt online casino som erbjuder spelare en mängd olika casinospel att njuta av. För de som är intresserade av att bli en del av Gogo Casino-familjen och tjäna pengar genom att marknadsföra deras varumärke, finns det möjlighet att bli en Gogo Casino affiliate.
Att vara en Gogo Casino affiliate innebär att man samarbetar med casinot för att marknadsföra deras tjänster och locka nya spelare att registrera sig. Affiliates får en provision för varje spelare de hänvisar till casinot som registrerar sig och spelar för riktiga pengar.
För de som är intresserade av att bli en Gogo Casino affiliate finns det många fördelar. För det första är det en potentiellt lukrativ verksamhet där man kan tjäna en stadig inkomst genom att marknadsföra ett populärt varumärke som Gogo Casino. Dessutom är det en flexibel verksamhet där man kan arbeta när och var man vill.
För att bli en Gogo Casino affiliate behöver man ansöka via deras webbplats och skicka in information om sin marknadsföringskanal och erfarenhet inom casino-industrin. När ens ansökan har godkänts får man tillgång till marknadsföringsmaterial och verktyg för att hjälpa till att marknadsföra casinot på bästa sätt.
Sammanfattningsvis är att vara en Gogo Casino affiliate en spännande möjlighet för de som är intresserade av att tjäna pengar genom marknadsföring och samtidigt vara en del av den spännande världen av online casinon. Med rätt ansträngningar och engagemang kan man skapa en framgångsrik verksamhet som Gogo Casino affiliate.
https://gogocasino.one
Gogo Casino: En populär spelsajt bland svenska spelare
Gogo Casino är en relativt ny spelsajt på marknaden som har snabbt blivit populär bland svenska spelare. Sajten erbjuder ett brett utbud av casinospel och en användarvänlig plattform som gör det enkelt att njuta av spelandet online.
Enligt recensioner på AskGamblers, en av de ledande sajterna för casinorecensioner och betyg, har Gogo Casino fått mycket positiva omdömen från spelare. Många spelare uppskattar sajtens enkla och smidiga design, samt det stora utbudet av casinospel från ledande spelleverantörer.
En annan fördel med Gogo Casino är dess generösa välkomstbonus och löpande kampanjer för befintliga spelare. Detta gör det möjligt för spelare att få extra valuta för sina pengar och öka sina vinstchanser.
Enligt recensioner på AskGamblers är också kundsupporten på Gogo Casino mycket professionell och tillmötesgående. Spelare kan få hjälp med eventuella frågor eller problem dygnet runt via livechatt eller e-post.
Sammanfattningsvis är Gogo Casino en spelsajt som verkligen har lyckats imponera på svenska spelare. Med sitt stora spelutbud, generösa bonusar och effektiva kundsupport är det inte konstigt att allt fler spelare väljer att spela hos Gogo Casino. Besök sajten idag och ta del av allt som Gogo Casino har att erbjuda!
https://gogocasino.one
Gogo Casino är en populär online-spelplattform som erbjuder ett brett utbud av casinospel. För att säkerställa en bra spelupplevelse för sina användare, har de en pålitlig och effektiv kundsupport.
Gogo Casino support team är tillgängligt dygnet runt för att hjälpa spelare med eventuella frågor eller problem de kan ha. De kan nås via livechatt, e-post eller telefon, vilket gör det enkelt för spelare att få den hjälp de behöver oavsett tid på dygnet.
Supportteamet är professionellt och vänligt, och de strävar efter att lösa alla problem så snabbt och effektivt som möjligt. Oavsett om det handlar om tekniska frågor, betalningsproblem eller bara allmänna frågor om spelen, kan spelarna lita på att Gogo Casino supportteam är där för att hjälpa dem.
Att ha en pålitlig kundsupport är avgörande för att skapa en positiv spelupplevelse för användarna, och Gogo Casino gör ett fantastiskt jobb med att tillhandahålla en förstklassig supporttjänst. Genom att erbjuda snabb och pålitlig hjälp till sina spelare visar Gogo Casino sitt engagemang för att se till att alla spelare har en bra tid på deras plattform.
Sammanfattningsvis kan man säga att Gogo Casino supportteam är en av de bästa i branschen och spelarna kan känna sig trygga med att deras behov kommer att tas omhand på ett professionellt sätt. Med deras hjälp är det lätt att njuta av en problemfri spelupplevelse på Gogo Casino.
https://gogocasino.one
Gogo Casino är en populär online spelsajt som erbjuder ett brett utbud av casinospel för alla spelare. För de som behöver kontakta support eller har frågor kring sajtens funktioner och regler, finns det flera sätt att komma i kontakt med Gogo Casino.
Det enklaste sättet att få kontakt med Gogo Casino är genom deras livechattfunktion. Där kan spelarna prata direkt med en kundtjänstrepresentant och få svar på sina frågor omedelbart. Livechatten är tillgänglig dygnet runt alla dagar i veckan, vilket gör det enkelt att få hjälp när som helst.
För de som föredrar att kommunicera via e-post, finns det också möjlighet att skicka ett meddelande till Gogo Casino. Supportteamet svarar vanligtvis inom 24 timmar och kan hjälpa till med allt från tekniska problem till frågor om bonusar och kampanjer.
Det finns även en FAQ-sektion på Gogo Casinos hemsida där spelarna kan hitta svar på de vanligaste frågorna som kan uppstå. Där finns information om insättningar och uttag, spelregler och mycket mer.
Sammanfattningsvis, för de som behöver kontakta Gogo Casino för support eller frågor, är det enkelt att göra det via livechatten, e-post eller genom att kolla in deras FAQ-sektion. Oavsett vilket sätt man väljer att kommunicera på, så kan spelarna vara säkra på att de får snabb och professionell hjälp från Gogo Casinos supportteam.
https://gogocasino.one
Gogo Casino är en populär online-spelplattform som erbjuder ett brett utbud av casinospel för sina spelare. För att säkerställa en smidig spelupplevelse för sina kunder har de en dedikerad kundtjänst som är tillgänglig för att hjälpa till med alla frågor eller problem som kan uppstå.
Gogo Casino kundtjänst är tillgänglig dygnet runt, alla dagar i veckan, för att hjälpa spelare med alla sina behov. Oavsett om det gäller att svara på frågor om spelregler, hantera insättningar och uttag eller lösa tekniska problem, finns det alltid någon tillgänglig för att hjälpa till.
Kundtjänsten på Gogo Casino är välutbildad och kunnig inom alla aspekter av casinospel, vilket innebär att spelarna kan känna sig trygga i att de får den bästa möjliga hjälpen. Genom att erbjuda snabba svar och effektiv service strävar Gogo Casino efter att ge sina kunder den bästa möjliga spelupplevelsen.
För att komma i kontakt med Gogo Casino kundtjänst kan spelare antingen använda livechatten på deras hemsida, skicka ett mejl eller ringa deras telefonsupport. Oavsett vilken metod som används kan spelare vara säkra på att de kommer att få den hjälp de behöver för att njuta av sitt spelande på Gogo Casino.
https://gogocasino.one
ממבחר עשיר ואיכותי של שרותי ליווי. אם בא לכם עיסוי אירוטי שאפשר להגשים. כאן תוכלו למצוא מגוון עצום של דירות דיסקרטיות באילת, הטומנות בחובן מגוון יפיפיות אקזוטיות, עדינות, בלונדיניות הדיסקרטיות ברעננה נבחרו בקפידה תוך שמירה על ניקיון והיגיינה ברמה גבוהה מסאז אירוטי בחיפה
Gogo Casino är ett av de senaste tillskotten till online-spelvärlden och har redan börjat göra sig ett namn i branschen. Med sitt innovativa koncept och en unik spelupplevelse har Gogo Casino snabbt blivit populärt bland spelare över hela världen.
En av anledningarna till Gogo Casinos framgång är dess samarbete med AskGamblers, en ledande auktoritet när det gäller online-casinorecensioner och spelrekommendationer. AskGamblers är kända för att tillhandahålla objektiva och opartiska recensioner av olika online-casinon, vilket gör det till en pålitlig källa för spelare som letar efter säkra och pålitliga spelplattformar.
Genom sitt samarbete med AskGamblers har Gogo Casino fått positiva recensioner och betyg från både spelare och experter inom branschen. Spelare som besöker AskGamblers kan läsa recensioner om Gogo Casino och få en bra överblick över vad casinot har att erbjuda, inklusive spelutbud, bonusar och kampanjer.
Gogo Casino är känt för sitt stora urval av spel från ledande spelutvecklare, vilket innebär att spelare kan njuta av en högkvalitativ spelupplevelse oavsett vilken typ av spel de föredrar. Dessutom erbjuder Gogo Casino generösa bonusar och kampanjer som gör det mer lönsamt för spelare att spela på casinot.
Sammanfattningsvis är Gogo Casino ett spännande tillskott till online-spelvärlden och genom sitt samarbete med AskGamblers kan spelare vara säkra på att de får en säker och underhållande spelupplevelse när de spelar på casinot. Med sitt innovativa koncept och konsekventa kvalitetsspel ser vi Gogo Casino som en av de ledande aktörerna på marknaden i framtiden.
https://gogocasino.one
Gogo casino affiliates är en av de mest populära och väletablerade affiliatenätverken inom online casino-industrin. Med ett brett utbud av högkvalitativa casinospel och generösa erbjudanden lockar de till sig både spelare och partners.
Som affiliate hos Gogo casino får man tillgång till en mängd marknadsföringsverktyg och support från ett dedikerat team. Genom att marknadsföra Gogo casino och deras spel kan man tjäna provision på varje spelare man refererar till casinot. Det är en bra möjlighet att tjäna extra pengar genom att marknadsföra något man brinner för.
Gogo casino erbjuder även regelbundna kampanjer och bonusar för sina affiliates, vilket gör det ännu mer lönsamt att samarbeta med dem. De håller sig ständigt uppdaterade med de senaste trenderna och erbjuder sina affiliates möjligheten att marknadsföra de mest populära spelen på marknaden.
För de som är intresserade av att bli en del av Gogo casino affiliates är det enkelt att komma igång. Man registrerar sig på deras hemsida, får tillgång till marknadsföringsverktyg och kan börja tjäna pengar direkt.
Sammanfattningsvis är Gogo casino affiliates ett pålitligt och lönsamt affiliatenätverk för de som är intresserade av att marknadsföra online casino spel. Med deras generösa erbjudanden och dedikerade support är det en bra möjlighet att tjäna extra pengar på sin passion för spel.
https://gogocasino.one
meclizine 100mg
Gogo casino är ett relativt nytt online casino som har fått mycket uppmärksamhet på senaste tiden. Med ett färgglatt och trendigt gränssnitt, erbjuder Gogo casino spelare en spännande spelupplevelse med ett brett utbud av casinospel att välja mellan.
Ett av de stГ¶rsta fГ¶rdelarna med Gogo casino Г¤r den imponerande samlingen av spel frГҐn nГҐgra av de bГ¤sta spelleverantГ¶rerna i branschen. Med titlar frГҐn NetEnt, Microgaming, Play’n GO och mГҐnga fler, kan spelare njuta av spelautomater, bordsspel, live casino och mycket mer.
Gogo casino erbjuder också generösa bonusar och kampanjer för sina spelare. Nya spelare kan dra nytta av en välkomstbonus för att komma igång på rätt spår, medan lojala spelare kan ta del av regelbundna belöningar och specialerbjudanden.
Kundtjänsten på Gogo casino är också väldigt pålitlig och tillmötesgående. Spelare kan få hjälp med alla sina frågor och problem genom live chatt, telefon eller e-post.
Sammanfattningsvis är Gogo casino en bra destination för spelare som letar efter en spännande och pålitlig spelupplevelse. Med ett stort utbud av spel, generösa bonusar och pålitlig kundsupport är det definitivt värt att ge detta casino en chans.
https://gogocasino.one
Gogo Casino Г¤r ett av de senaste tillskotten till LeoVegas-familjen. Denna nya spelsida erbjuder spelare en snabb och smidig spelupplevelse med fokus pГҐ enkelhet och snabbhet.
Gogo Casino har ett stort utbud av casinospel från de bästa leverantörerna i branschen, vilket innebär att spelare kan njuta av ett varierat utbud av spelautomater, bordsspel och livecasino. Dessutom erbjuds spelare möjligheten att spela direkt i webbläsaren utan att behöva ladda ner någon programvara.
En annan fördel med Gogo Casino är att de erbjuder blixtsnabba uttag. Spelare kan få sina vinster utbetalda på bara några minuter, vilket är en stor fördel för de som vill ha sina pengar så fort som möjligt.
För att locka nya spelare erbjuder Gogo Casino generösa välkomstbonusar och kampanjer. Spelare kan se fram emot frekventa belöningar och erbjudanden som kommer att göra deras spelupplevelse ännu mer spännande.
Sammanfattningsvis är Gogo Casino en utmärkt plattform för spelare som letar efter en enkel och snabb spelupplevelse. Med ett stort spelutbud, snabba uttag och generösa bonusar är detta ett nätcasino som definitivt är värt att kolla in. Besök Gogo Casino idag och upplev spänningen själv!
https://gogocasino.one
Wow a good deal of superb material.
Also visit my web page https://ytmp3.vc/
Gogo Casino är en online casino som erbjuder ett brett utbud av spel och möjligheten att vinna stora vinster. AskGamblers är en populär webbplats som recenserar olika online kasinon och ger spelare möjlighet att dela sina erfarenheter och åsikter.
Gogo Casino har fått mycket positiv feedback från spelare på AskGamblers för dess enkla användargränssnitt och generösa bonusar. Många spelare har berömt kasinot för dess utmärkta kundsupport och snabba uttag.
För de som letar efter en pålitlig och underhållande spelupplevelse, är Gogo Casino definitivt värt att kolla in. Med ett stort utbud av spel från några av de bästa leverantörerna i branschen, finns det något för alla spelare att njuta av.
Så om du letar efter ett online casino med hög kvalitet och bra rykte, ta en titt på Gogo Casino och se om det är rätt för dig. Med hjälp av AskGamblers recensioner och spelares åsikter kan du vara säker på att du får en förstklassig spelupplevelse.
https://gogocasino.one
Prestito 1 mila euro
Gogo Casino har nyligen annonserat ett spännande samarbete som kommer att ge sina spelare ännu bättre erbjudanden och möjligheter att vinna stort. Det är ingen hemlighet att casinobranschen är konkurrensutsatt och det är viktigt för casinon att hitta nya sätt att locka spelare och behålla lojala kunder. Detta samarbete är ett steg i rätt riktning för Gogo Casino, som redan är känt för sitt stora utbud av spel och generösa bonusar.
Det nya samarbetet kommer att ge spelare tillgång till exklusiva kampanjer och turneringar som endast är tillgängliga för dem som är medlemmar i Gogo Casino. Det betyder att spelarna får chansen att vinna ännu större priser och belöningar när de spelar sina favoritspel på casinot. Dessutom kommer samarbetet att ge spelare möjlighet att delta i spännande tävlingar och utmaningar där de kan vinna häftiga priser och upplevelser.
Gogo Casino har även utökat sitt spelutbud genom samarbetet, vilket innebär att spelarna nu har ännu fler spel att välja mellan när de besöker casinot. Detta är bra nyheter för de som älskar att prova på nya spel och vill ha en varierad spelupplevelse. Casinot har även förbättrat sin kundsupport och betalningsmetoder för att göra det ännu enklare och smidigare för spelarna att njuta av sin spelupplevelse.
Sammantaget är samarbetet mellan Gogo Casino och deras partner en vinn-vinn-situation för alla inblandade. Spelarna får bättre erbjudanden och mer underhållning, medan casinot får lojala kunder och ökad trafik på sin sida. Vi ser fram emot att se vad framtiden har att erbjuda för detta spännande samarbete och hur det kommer att fortsätta att utveckla sig för spelarna.
https://gogocasino.one
Наш клининг в Челябинске предоставляет услуги по мойке окон любой сложности. Обращайтесь к нам, и ваше стекло всегда будет блестеть! https://klining-chelyabinsk-1.ru/
Kamagra tablets kamagra best price Kamagra 100mg price
Gogo Casino är ett populärt online casino som erbjuder ett brett utbud av spelautomater och andra casinospel. För att få hjälp med eventuella frågor eller problem kan spelare kontakta Gogo Casino via deras kundtjänst.
Det finns flera sätt att komma i kontakt med Gogo Casino. Den enklaste och snabbaste metoden är genom deras live chatt-funktion. Här kan spelare chatta direkt med en supportagent och få svar på sina frågor på nolltid. Live chatten är tillgänglig dygnet runt alla dagar i veckan.
För de som föredrar att skicka e-post kan man kontakta Gogo Casino på deras mejladress. Det kan ta lite längre tid att få svar via e-post jämfört med live chatt, men supporten gör sitt bästa för att svara så snabbt som möjligt.
För de spelare som vill prata med någon personligen finns även möjligheten att ringa Gogo Casino. Kundtjänsten är tillgänglig på telefon under vissa tider på dygnet.
Det är viktigt att komma ihåg att Gogo Casino strävar efter att erbjuda bästa möjliga kundservice och är dedikerade att hjälpa sina spelare på bästa sätt. Oavsett vilken kontaktmetod man väljer kan man vara säker på att man får professionell och vänlig service.
https://gogocasino.one
Gogo Casino – LeoVegas
Gogo Casino är en populär spelsajt som ägs av LeoVegas, en av de största och mest framgångsrika speloperatörerna på marknaden. LeoVegas grundades 2011 och har sedan dess blivit en favorit bland spelare runt om i världen. De erbjuder ett brett utbud av casinospel, live casino, odds och mycket mer.
Gogo Casino är en del av LeoVegas-familjen och lanserades 2019. Det är ett modernt och välutformat online casino med fokus på enkelhet och snabbhet. Sajten är snyggt designad med en minimalistisk layout och användarvänligt gränssnitt som gör det lätt att navigera och hitta sina favoritspel.
PГҐ Gogo Casino kan spelarna njuta av ett stort utbud av slotspel, bordsspel, live casino och jackpotspel frГҐn ledande spelleverantГ¶rer som NetEnt, Microgaming, Play’n GO och mГҐnga fler. Det finns Г¤ven ett bra utbud av kampanjer och bonusar fГ¶r bГҐde nya och befintliga spelare.
En av fördelarna med att spela på Gogo Casino är den snabba och säkra betalningsmetoden Trustly. Spelarna kan göra snabba insättningar och uttag direkt från sina bankkonton utan att behöva skapa ett konto på sajten. Detta gör det enkelt och smidigt att spela utan krångel.
Gogo Casino är licensierat av Spelinspektionen i Sverige och följer alla regler och bestämmelser för att säkerställa en trygg och rättvis spelupplevelse för spelarna. De erbjuder också en professionell och vänlig kundtjänst som är tillgänglig via live chatt, e-post och telefon för att hjälpa spelarna med alla sina frågor och bekymmer.
Sammanfattningsvis är Gogo Casino en utmärkt spelsajt för de spelare som letar efter en enkel, snabb och underhållande spelupplevelse. Med sitt stora spelutbud, generösa bonusar och pålitliga betalningsmetoder är det en bra destination för alla som vill ha kul och ha chansen att vinna stort. Besök Gogo Casino idag och upplev spänningen själv!
https://gogocasino.one
получить микрозайм
Gogo Casino är en ny och spännande spelplattform som erbjuder en fantastisk spelupplevelse för alla spelentusiaster. Med ett brett utbud av casinospel och en användarvänlig plattform är det lätt att förstå varför Gogo Casino.se har blivit en favorit bland många spelare.
PГҐ Gogo Casino.se hittar du populГ¤ra spelautomater, bordsspel och livecasino frГҐn de bГ¤sta spelleverantГ¶rerna pГҐ marknaden. Du kan spela favoritspelen frГҐn vГ¤rldsledande fГ¶retag som NetEnt, Microgaming, Play’n GO och mГҐnga andra.
En av de stora fördelarna med Gogo Casino.se är dess smidiga och enkla användargränssnitt. Det är lätt att navigera mellan spelen och hitta det du söker efter. Dessutom erbjuder plattformen snabba och säkra betalningsalternativ så att du kan sätta in och ta ut pengar på ett tryggt sätt.
För att ge spelarna en extra boost erbjuder Gogo Casino.se generösa bonusar och kampanjer. Nya spelare får en välkomstbonus när de registrerar sig och gör sin första insättning, och det finns regelbundna kampanjer och belöningar för lojala spelare.
Gogo Casino.se drivs av en erfaren och dedikerad team som strävar efter att skapa den bästa möjliga spelupplevelsen för sina spelare. Plattformen är licensierad av svenska spelinspektionen vilket innebär att allt spel är säkert och rättvist.
Sammanfattningsvis är Gogo Casino.se en toppmodern spelplattform som erbjuder en rad spännande spel och generösa bonusar. Oavsett om du är nybörjare eller erfaren spelare kan du hitta något som passar dig på Gogo Casino.se. Ge det en chans och upplev spänningen själv!
https://gogocasino.one
на вибір гостям пропонують один серйозний зал (60 місць і 2 міні-банкетки https://dediko.com.ua/banquets.html (до двадцяти осіб).
GoGo Casino är en spännande och underhållande online spelsajt som erbjuder sina spelare en mängd olika casinospel att välja mellan. Med ett stort utbud av spelautomater, bordsspel och livecasino är det lätt att hitta något som passar just dig.
En av fördelarna med GoGo Casino är att det är en svensk spelsajt, vilket innebär att du kan känna dig trygg när du spelar här. Sajten är licensierad av Spelinspektionen och följer alla regler och bestämmelser som gäller för spel i Sverige.
GoGo Casino erbjuder också en smidig och enkel registreringsprocess, vilket gör det lätt att komma igång och börja spela. Du kan enkelt göra insättningar och uttag med hjälp av populära betalningsmetoder som Trustly och Swish.
Förutom det stora utbudet av spel och den säkra spelmiljön erbjuder GoGo Casino också generösa bonusar och kampanjer för sina spelare. Du kan ta del av välkomstbonusar, free spins och mycket mer när du registrerar dig som ny spelare.
Sammanfattningsvis är GoGo Casino en toppenval för dig som gillar att spela online casino. Med sitt stora spelutbud, säkra spelmiljö och generösa bonusar är det här en sajt som verkligen levererar på alla fronter. Så varför inte testa lyckan på GoGo Casino redan idag? Lycka till!
https://gogocasino.one
Kamagra 100mg price Kamagra gel Kamagra 100mg
GOGO Casino är en spännande online casino med ett brett utbud av spel och generösa bonusar. Men vad gör detta casino ännu bättre är deras professionella och hjälpsamma kundsupport.
Kundsupporten på GOGO Casino är tillgänglig dygnet runt via livechatt och e-post. Det betyder att oavsett vilken tid på dygnet du spelar kan du alltid få hjälp om det behövs. De vänliga och kunniga supportmedarbetarna är alltid redo att svara på dina frågor och lösa eventuella problem på ett snabbt och effektivt sätt.
En annan fördel med GOGO Casinos kundsupport är att de pratar svenska. Det gör det enkelt och smidigt att kommunicera och få hjälp om du stöter på några hinder under ditt spelande. Oavsett om det handlar om tekniska problem, bonusar eller spelregler kan du vara säker på att du får en professionell och personlig service.
Så om du letar efter ett online casino med en pålitlig och effektiv kundsupport, är GOGO Casino definitivt ett bra val. Med deras vänliga och tillgängliga supportteam kan du vara säker på att du får den hjälp du behöver när du behöver den. Så varför inte prova lyckan på GOGO Casino idag och upplev deras förstklassiga kundsupport själv?
https://gogocasino.one
Gogo Casino är en populär spelsajt som erbjuder ett stort utbud av casinospel online. För att spela på Gogo Casino behöver du logga in med ditt användarkonto.
FГ¶r att logga in pГҐ Gogo Casino, besГ¶k deras hemsida och klicka pГҐ knappen “Logga in” i Г¶vre hГ¶gra hГ¶rnet. DГ¤refter fyller du i ditt anvГ¤ndarnamn och lГ¶senord som du valde nГ¤r du skapade ditt konto. Om du har glГ¶mt ditt lГ¶senord kan du enkelt ГҐterstГ¤lla det genom att klicka pГҐ “GlГ¶mt lГ¶senord”-knappen och fГ¶lja instruktionerna.
När du har loggat in på Gogo Casino kan du börja spela dina favoritspel och vinna stora vinster. Var noga med att hålla koll på ditt spelbeteende och spela ansvarsfullt. Gogo Casino erbjuder också olika verktyg för att hjälpa dig att hålla koll på ditt spelande och sätta gränser för dig själv.
Oavsett om du föredrar slots, bordsspel eller live casino, har Gogo Casino något för alla. Registrera dig idag och prova lyckan på Gogo Casino! Lycka till!
https://gogocasino.one
Casino Gogo är det hetaste stället att vara på för alla som älskar spänning och underhållning. Med ett stort urval av spel och en härlig atmosfär, är detta ett casino som inte lämnar något att önska.
På Casino Gogo finns det spel för alla smaker. Oavsett om du föredrar klassiska spel som blackjack och roulette eller om du föredrar att prova lyckan på spelautomater, hittar du allt du behöver här. Dessutom erbjuds regelbundna turneringar och tävlingar för de som gillar att mäta sina färdigheter mot andra spelare.
När du besöker Casino Gogo kan du räkna med en förstklassig service. Den vänliga personalen är alltid redo att hjälpa till och se till att du får en minnesvärd upplevelse. Dessutom erbjuds det även en rad olika erbjudanden och bonusar för att göra ditt besök ännu mer spännande.
Casino Gogo är även känt för sin fantastiska atmosfär. Med en välkomnande och glamorös miljö är det här en plats där du kan koppla av och njuta av spelet i lugn och ro. Oavsett om du är en erfaren casinospelare eller om du är nybörjare, kommer du garanterat att känna dig som hemma på Casino Gogo.
Så om du letar efter en härlig och spännande casinoupplevelse, är Casino Gogo definitivt stället att besöka. Med ett stort urval av spel, fantastisk service och en atmosfär som inte lämnar någon oberörd, kommer du garanterat att få en upplevelse du sent kommer att glömma. Besök Casino Gogo idag och upplev spänningen själv!
https://gogocasino.one
30000 euro lenen
Gogo Casino är ett populärt online casino som erbjuder spelare möjligheten att spela utan att behöva göra en insättning. Det betyder att du kan prova lyckan och spela dina favoritspel utan att riskera dina egna pengar.
På Gogo Casino hittar du ett brett utbud av casinospel, inklusive slots, bordsspel och live casino. De samarbetar med de bästa spelleverantörerna i branschen för att säkerställa att du får en förstklassig spelupplevelse.
För att ta del av Gogo Casino no deposit erbjudanden behöver du bara registrera ett konto och verifiera din identitet. Du kommer då att få en bonus som du kan använda för att spela på casinot. Det finns inga krav på insättning, så du kan spela gratis och ändå ha chansen att vinna riktiga pengar.
Det är viktigt att komma ihåg att alla casinon har olika regler och villkor när det gäller bonusar och erbjudanden, så se till att läsa igenom dessa noggrant innan du börjar spela. På så sätt kan du undvika eventuella missförstånd och se till att du får ut det mesta av din spelupplevelse på Gogo Casino.
Sammanfattningsvis är Gogo Casino no deposit ett utmärkt sätt för spelare att testa på casinospel utan att behöva riskera sina egna pengar. Med ett brett utbud av spel och generösa bonusar är det här ett casino som definitivt är värt att kolla in. Lycka till och ha kul!
https://gogocasino.one
Gogo Casino är en av de senaste tillskotten inom online casino världen och har snabbt blivit en populär destination för spelare som letar efter spännande spelupplevelser.
Det som skiljer Gogo Casino från andra online casinon är dess enkla och smidiga användarupplevelse. Här behöver du inte skapa ett konto för att spela, istället kan du enkelt logga in med ditt BankID och komma igång direkt. Detta gör att du kan njuta av dina favoritspel utan krånglig registrering eller onödiga omsättningskrav.
Gogo Casino erbjuder ett brett utbud av spel från ledande spelleverantörer, inklusive slots, bordsspel och live casino. Oavsett om du föredrar klassiska spelautomater eller vill prova lyckan på ett live blackjack bord, finns det något för alla här.
För de spelare som älskar att jaga stora vinster, erbjuder Gogo Casino även ett antal progressiva jackpotspel där jackpotten växer för varje insats som görs. Med ett enkelt klick kan du vara nästa miljonär!
Utöver det imponerande spelutbudet, är Gogo Casino också känt för sin utmärkta kundtjänst. Med en dedikerad supportteam som finns tillgängligt dygnet runt, kan du vara säker på att du är i trygga händer när du spelar här.
Sammanfattningsvis är Gogo Casino en spännande nykomling inom online casinovärlden som erbjuder enkelhet, spänning och en chans att vinna stora vinster. Om du är på jakt efter en ny favoritdestination att spela på, är Gogo Casino definitivt värt att prova!
https://gogocasino.one
I dagens digitala tid finns det en mängd olika alternativ när det kommer till underhållning. Ett populärt sätt att koppla av och ha roligt är genom att spela på online casinon. Ett av de mest spännande och unika casinona på marknaden just nu är Casino Gogo.
Casino Gogo erbjuder en enastående spelupplevelse med ett stort urval av casinospel från världsledande leverantörer som NetEnt, Microgaming och Evolution Gaming. Spelare kan njuta av allt från klassiska spelautomater och bordsspel till live casino-spel som blackjack, roulette och baccarat.
Det som verkligen skiljer Casino Gogo från mängden är deras innovativa koncept och spännande tema. Casinot har en festlig och energifylld atmosfär som genomsyrar hela webbplatsen. Spelare kan delta i spännande turneringar och tävlingar, få generösa bonusar och belöningar samt interagera med andra spelare i realtid.
En annan fördel med Casino Gogo är att det är helt mobilvänligt. Det betyder att spelare kan njuta av sina favoritspel var som helst och när som helst, oavsett om de sitter på bussen eller slappar i soffan. Dessutom erbjuder casinot en säker och pålitlig spelplattform med snabba och smidiga betalningsmetoder.
Oavsett om du är en erfaren spelare eller nybörjare så kommer du garanterat att ha en fantastisk tid på Casino Gogo. Så varför inte prova lyckan redan idag och upptäck en helt ny värld av spännande casinospel och underhållning? Vem vet, kanske blir du nästa stora vinnare på detta unika och innovativa online casino!
https://gogocasino.one
Gogo Casino är en spännande ny online casino-plattform som skakar om branschen. Med ett stort utbud av spel och generösa bonusar är detta ett casino som definitivt är värt att kolla in.
En av de främsta fördelarna med Gogo Casino är dess enkla och användarvänliga gränssnitt. Det är lätt att navigera på sidan och hitta ens favoritspel. Dessutom finns det ett brett utbud av spel att välja mellan, inklusive slots, bordsspel och live-dealerspel.
Det som verkligen sticker ut med Gogo Casino är deras generösa bonusar och erbjudanden. Nya spelare kan få en välkomstbonus när de registrerar sig och gör sin första insättning. Dessutom erbjuds regelbundna kampanjer och turneringar som ger spelare chansen att vinna stora priser.
En annan fördel med Gogo Casino är dess snabba och säkra betalningsmetoder. Spelare kan enkelt sätta in och ta ut pengar med hjälp av olika metoder som kreditkort, banköverföring och e-plånböcker.
Sammanfattningsvis är Gogo Casino en toppdestination för alla som söker en spännande och säker spelupplevelse online. Med sitt stora spelutbud, generösa bonusar och snabba betalningsmetoder är detta ett casino som definitivt är värt att testa. Besök Gogo Casino idag och ta del av allt det har att erbjuda!
https://gogocasino.one
Gogo Casino är en del av LeoVegas Group, en av de ledande aktörerna inom onlinecasinobranschen. Med sitt minimalisiska och eleganta designkoncept erbjuder Gogo Casino en smidig och enkel spelupplevelse för alla sina spelare.
En av de stora fördelarna med Gogo Casino är dess snabba uttag. Tack vare deras avancerade betalningsmetoder kan du ta ut dina vinster på nolltid. Dessutom erbjuder de ett brett utbud av populära casinospel från några av de bästa spelutvecklarna i branschen.
Gogo Casino är licensierat av svenska Spelinspektionen, vilket garanterar en säker och rättvis spelupplevelse för alla spelare. De erbjuder även en rad olika kampanjer och bonusar, vilket gör det ännu mer spännande att spela hos dem.
Oavsett om du föredrar klassiska bordsspel som blackjack och roulette, eller om du föredrar att snurra på slots, så finns det något för alla hos Gogo Casino. Så varför inte dyka in i deras spännande värld av casinospel redan idag? Besök deras hemsida för att registrera dig och börja spela!
https://gogocasino.one
Gogo Casino och LeoVegas är två populära onlinecasinon där spelare kan njuta av en mängd olika spel och spännande kampanjer. Tyvärr har det nyligen kommit upp klagomål från spelare som hävdar att de inte har fått sina vinster utbetalda från Gogo Casino och LeoVegas.
Det är viktigt att påpeka att det är av yttersta vikt att spela på reglerade och pålitliga casinon för att undvika sådana situationer. Om Gogo Casino och LeoVegas verkligen inte betalar ut sina vinster, kan det vara bra att kontakta kundtjänst för att få svar på varför detta har hänt.
Det finns flera anledningar till varför ett casino inte skulle betala ut vinster, varav några kan inkludera att spelaren brutit mot reglerna och villkoren för casinot, att det finns tekniska problem eller att det finns bedrägeri eller andra olagliga aktiviteter involverade. Oavsett orsaken är det viktigt att vara medveten om sina rättigheter som spelare och att agera på ett strategiskt och ansvarsfullt sätt.
För att undvika att hamna i liknande situationer är det viktigt att välja casinon som är licensierade och reglerade av en respektabel myndighet. Att läsa recensioner och undersöka casinots rykte innan man registrerar sig kan också vara till stor hjälp.
Sammanfattningsvis är det viktigt att vara medveten om riskerna som finns med att spela på onlinecasinon och att agera ansvarsfullt. Om du upplever att ett casino inte betalar ut dina vinster, är det bäst att ta kontakt med kundtjänst för att utreda orsaken bakom detta. Med rätt kunskap och strategi kan man undvika att hamna i trubbel och istället njuta av en underhållande och säker spelupplevelse online.
https://gogocasino.one
Gogo Casino app är den senaste spännande tillskottet till spelvärlden. Denna innovativa app ger spelare möjlighet att njuta av sina favoritspel var de än befinner sig, allt från deras mobiltelefoner eller surfplattor.
Med ett brett utbud av populära casinospel, inklusive slots, bordsspel och live dealer-spel, finner spelare på Gogo Casino app något för alla smaker. Dessutom erbjuder appen enkel och smidig navigering, vilket gör det lätt att hitta de spel man är intresserad av.
En av de största fördelarna med Gogo Casino app är dess snabba och säkra betalningslösningar. Spelare kan enkelt sätta in och ta ut pengar utan krångel, vilket ger en bekymmersfri spelupplevelse.
Utöver sina spel och betalningsalternativ, erbjuder Gogo Casino app också generösa bonusar och kampanjer för sina spelare. Detta gör det möjligt för spelare att maximera sina vinstchanser och få ännu mer valuta för sina pengar.
Sammanfattningsvis är Gogo Casino app den perfekta plattformen för spelare som letar efter en spännande och underhållande spelupplevelse. Med sitt stora utbud av spel, säkra betalningsalternativ och generösa bonusar, är det lätt att se varför den här appen har blivit så populär bland spelentusiaster. Testa Gogo Casino app idag och upptäck den spännande världen av online-spel!
https://gogocasino.one
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Hizmeti Skype : live:by_umut
Everything is very open and very clear explanation of issues. was truly information. Seo Hizmeti Skype : live:by_umut
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader. Seo Hizmeti Skype : live:by_umut
Gogo casino flashback
Gogo casino är ett online casino som erbjuder ett brett utbud av spel och underhållning för sina spelare. Med en modern och användarvänlig plattform har Gogo casino snabbt blivit en populär destination för svenska spelare.
En av de mest spännande funktionerna hos Gogo casino är deras flashback-funktion. Denna unika funktion ger spelare möjlighet att gå tillbaka och se sina tidigare spel, inklusive insatser, vinster och förluster. Detta är ett bra sätt att analysera sitt spelande och lära sig av tidigare misstag.
Genom flashback-funktionen kan spelare också få en bättre förståelse för sina spelvanor och strategier. Det kan hjälpa dem att bli mer medvetna om sitt spelande och ta kloka beslut för framtiden.
Gogo casino flashback är en användbar funktion för alla spelare, oavsett om de är nybörjare eller erfarna. Det ger en unik möjlighet att följa sitt spelande och kontinuerligt förbättra sin strategi.
Sammanfattningsvis är Gogo casino flashback en fantastisk funktion som gör det möjligt för spelare att ta kontroll över sitt spelande och maximera sin spelupplevelse. Med denna funktion kan spelare fortsätta att utvecklas och lära sig av sina tidigare erfarenheter. Besök Gogo casino idag och upptäck allt det har att erbjuda!
https://gogocasino.one
Gogo Casino är en populär online casino som lockar många spelare med sitt stora utbud av spel och generösa bonusar. Men vad många kanske inte känner till är att de också har en utmärkt kundtjänst som står redo att hjälpa spelare med alla frågor och problem som kan dyka upp.
Gogo Casino kundtjänst är tillgänglig dygnet runt via livechatt, e-post och telefon. De är kända för sin snabba respons och professionella hantering av alla ärenden. Oavsett om det handlar om tekniska problem, bonusfrågor eller förslag på nya spel, så finns kundtjänsten där för att hjälpa till.
En av fördelarna med Gogo Casino kundtjänst är att de pratar svenska och har god kännedom om den svenska spelmarknaden. Det innebär att de kan ge spelare skräddarsydda råd och svar på frågor som är specifika för den svenska marknaden.
Utöver att vara tillgängliga dygnet runt, så är Gogo Casino kundtjänst också kända för att vara mycket vänliga och hjälpsamma. De strävar alltid efter att ge spelare den bästa möjliga hjälpen och göra deras spelupplevelse så bra som möjligt.
Sammanfattningsvis kan man säga att Gogo Casino kundtjänst är en av de bästa på marknaden. Med sin tillgänglighet, professionalism och vänlighet så ser de till att spelarna alltid får den hjälp de behöver. Så om du spelar på Gogo Casino och stöter på problem eller har frågor, tveka inte att kontakta deras kundtjänst – de finns där för att hjälpa dig.
https://gogocasino.one
Great post thank you. Hello Administ . Seo Hizmeti Skype : live:by_umut
Kamagra tablets Kamagra 100mg price cheap kamagra
https://ruseriya.ru/6544-svoi-6-sezon.html
Gogo Casino Г¤gare
Gogo Casino är en populär online casino som erbjuder spelentusiaster en spännande och underhållande spelupplevelse. Men vem är det egentligen som äger detta framgångsrika casino?
Gogo Casino ägare är det svenska företaget LeoVegas AB. LeoVegas är en ledande aktör inom online spelindustrin och driver flera framgångsrika casinon, inklusive Gogo Casino. Företaget grundades år 2012 och har sedan dess vuxit i popularitet och blivit en av de främsta speloperatörerna på marknaden.
LeoVegas är känt för att erbjuda ett brett utbud av spel och för att hålla en hög standard när det gäller säkerhet och rättvist spel. Företaget är licensierat av svenska Spelinspektionen och följer alla gällande regler och bestämmelser för att säkerställa en trygg och ansvarsfull spelupplevelse för sina spelare.
Gogo Casino ägare, LeoVegas AB, är en aktör att lita på för alla som är intresserade av att spela casino online. Med deras starka varumärke, höga kvalitet på spel och en dedikerad kundtjänst, är det ingen tvekan om att de är en av de främsta inom branschen. Så om du letar efter en pålitlig och spännande spelupplevelse, då är Gogo Casino definitivt ett bra val att prova på.
https://gogocasino.one
https://ruseriya.ru/6151-vokalnokriminalnyy-ansambl-1-sezon.html
Gogo Casino är en online spelplattform som har blivit allt mer populär bland svenska spelare. Men vad är det som gör den här sidan så speciell och hur bra är den egentligen? I den här recensionen kommer vi gå igenom allt från spelutbud och betalningsmetoder till kundsupport och användarvänlighet.
Gogo Casino erbjuder ett brett utbud av spel från flera av de främsta spelleverantörerna på marknaden. Här hittar du allt från klassiska spelautomater och bordsspel till live casino och progressiva jackpotspel. Sidan är även väl optimerad för mobila enheter, vilket gör det enkelt att spela var du än befinner dig.
När det kommer till betalningsmetoder erbjuder Gogo Casino ett flertal säkra och snabba alternativ, inklusive banköverföring, kreditkort och e-plånböcker. Uttag hanteras vanligtvis inom 24 timmar, vilket är mycket snabbt jämfört med många andra online casinon.
Kundsupporten hos Gogo Casino är tillgänglig dygnet runt via live chatt och e-post, vilket gör det enkelt att få hjälp med eventuella frågor eller problem. Dessutom erbjuder sidan en omfattande FAQ-sektion där du kan hitta svaren på de vanligaste frågorna.
Sammanfattningsvis är Gogo Casino en pålitlig och användarvänlig spelplattform som erbjuder ett brett spelutbud, snabba uttag och en effektiv kundsupport. Om du letar efter en bra online kasino att spela på, kan Gogo Casino vara ett utmärkt alternativ.
https://gogocasino.one
https://ruseriya.ru/9097-neadekvatnye-ljudi-2.html
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader. Seo Hizmeti Skype : live:by_umut
Gogo Casino är ett online casino som erbjuder spelare en spännande och underhållande spelupplevelse. Med ett stort utbud av spelautomater, bordsspel och live casino, finns det något för alla smaker på Gogo Casino.
Leovegas Г¤r en av de mest populГ¤ra speloperatГ¶rerna pГҐ marknaden, och nu har de gГҐtt samman med Gogo Casino fГ¶r att skapa en Г¤nnu bГ¤ttre spelplattform. Den nya fusionen innebГ¤r att spelarna kan njuta av det bГ¤sta frГҐn bГҐda vГ¤rldarna – Leovegas innovativa spelupplevelse och Gogo Casinos spГ¤nnande spelutbud.
Med en enkel och användarvänlig design är det lätt att komma igång på Gogo Casino Leovegas. Spelarna kan enkelt navigera mellan olika spelkategorier och hitta sina favoritspel med några få klick. Dessutom erbjuder casinot snabba och säkra betalningsmetoder så att spelarna enkelt kan sätta in och ta ut sina vinster.
För de spelare som gillar att spela live casino, finns det också gott om alternativ på Gogo Casino Leovegas. Med professionella dealers och en autentisk casinoupplevelse kan spelarna njuta av klassiska bordsspel som roulette, blackjack och baccarat i realtid.
Sammanfattningsvis är Gogo Casino Leovegas en perfekt kombination av spännande spel och innovativa funktioner. Med ett stort spelutbud, smidiga betalningsmetoder och en användarvänlig design, är det här casinot definitivt värt att prova för alla som älskar att spela online. Besök Gogo Casino Leovegas idag och upplev den ultimata spelupplevelsen!
https://gogocasino.one
https://ruseriya.ru/11752-jarkoe-plamja-1-sezon.html
Mutuo 26 mila euro
https://ruseriya.ru/11062-zimorodok-1-sezon.html
Gogo casino är en av de populäraste onlinekasinona på marknaden idag. Med ett stort utbud av spel och generösa bonusar har casinot snabbt blivit en favorit bland spelare från hela världen.
En av de främsta fördelarna med Gogo casino är det stora urvalet av spel. Här kan du hitta allt från klassiska casinospel som roulette och blackjack till moderna videoslots och live dealer-spel. Oavsett vilken typ av spel du föredrar finns det definitivt något för dig på detta kasino.
Utöver det stora spelutbudet erbjuder Gogo casino även generösa bonusar och kampanjer till sina spelare. Nya spelare kan se fram emot en attraktiv välkomstbonus, medan befintliga spelare kan dra nytta av regelbundna belöningar och kampanjer som ökar deras vinstchanser. Detta gör att spelarna kan njuta av ännu mer spänning och underhållning när de spelar på Gogo casino.
En annan fördel med detta kasino är dess användarvänliga plattform. Hemsidan är lätt att navigera och spelarna kan enkelt hitta sina favoritspel och göra insättningar och uttag. Dessutom erbjuder Gogo casino en professionell och tillmötesgående kundsupport som finns tillgänglig dygnet runt för att hjälpa spelarna med eventuella frågor eller problem de kan ha.
Sammanfattningsvis är Gogo casino ett utmärkt val för alla som letar efter en underhållande och säker spelupplevelse online. Med sitt stora spelutbud, generösa bonusar och vänliga kundsupport är det inte konstigt att detta kasino har blivit så populärt bland spelare världen över. Kasinot har verkligen gått från klarhet till klarhet och vi rekommenderar det varmt till alla som är sugna på att prova lyckan på nätet.
https://gogocasino.one
Букмекерская компания Мостбет является ведущим игроком не только на рынке России, но и в других странах, включая Казахстан, Узбекистан, Азербайджан, Киргизию и многие другие. Легальный статус компании гарантирует честную и безопасную игру мостбет
Sweet, naughty girl, hottest sex chat for free, going to give you the best pleasure!
qiyezp.com
물론 Wang Xizuo는 오랫동안 Daming에 있었고 물론 Daming에 대한 큰 선견지명을 가지고 있습니다.
Gogo Casino har haft svårt att få pengar utbetalda till sina spelare på senaste tiden. Många kunder har vänt sig till sociala medier för att klaga på att de inte har fått ut sina vinster från casinot.
Enligt flera användare har Gogo Casino haft problem med sina betalningar under de senaste veckorna. Vissa har väntat i flera veckor på att få ut sina pengar, medan andra har fått sina uttag avbrutna utan förklaring.
Många spelare har uttryckt frustration över situationen och kritiserar casinot för att inte vara transparent med sina betalningsprocesser. En del har även ifrågasatt om Gogo Casino är en pålitlig operatör och uppmanar andra att vara försiktiga med att sätta in sina pengar på sidan.
Gogo Casino har ännu inte kommenterat de uppkomna problemen eller gett någon information om varför utbetalningarna har försenats. Det återstår att se om casinot kommer att ta tag i situationen och åtgärda problemen för sina spelare.
I väntan på mer information uppmanar vi alla som spelar på Gogo Casino att vara försiktiga med sina insättningar och att hålla sig uppdaterade om eventuella förändringar kring betalningsprocesserna. Det är viktigt att vara medveten om risken för att inte kunna få ut sina pengar innan man beslutar sig för att spela på ett online casino.
https://gogocasino.one
Переходим сюда и выигрываем в 1win
Gogo Casino är en av de nya casinona på marknaden som snabbt har blivit populärt bland svenska spelare. Men vem äger egentligen Gogo Casino?
Gogo Casino ägs av det maltesiska företaget Viral Interactive Limited. Viral Interactive Limited är ett företag som specialiserar sig inom iGaming-branschen och de har flera framgångsrika casinon under sitt tak.
Genom att ägas av Viral Interactive Limited innebär det att Gogo Casino är licensierat och reglerat av Malta Gaming Authority. Detta innebär att casinot följer strikta regler och riktlinjer för att säkerställa en säker och rättvis spelupplevelse för spelarna.
Även om Gogo Casino ägs av ett utländskt företag, är deras fokus tydligt på den svenska marknaden. Casinot erbjuder ett brett utbud av spel från ledande spelleverantörer, snabba utbetalningar och en kundtjänst på svenska.
Allt som allt, Gogo Casino ägs av Viral Interactive Limited och är ett pålitligt och populärt casino bland svenska spelare. Med en licens från Malta Gaming Authority kan spelare känna sig trygga med att deras spelupplevelse är säker och rättvis.
https://gogocasino.one
https://github.com/ForexRobotEasy/Hush-mt5
Gogo Casino är en spännande online-spelplattform som erbjuder en rad underhållande spel och möjligheter att vinna stora priser. Med en modern design och användarvänlig layout har Gogo Casino snabbt blivit ett populärt val för svenska spelare.
På Gogo Casino hittar du ett brett utbud av casinospel, inklusive slots, bordsspel och live-casino. Spelen kommer från ledande spelleverantörer som NetEnt, Microgaming och Evolution Gaming, vilket garanterar en hög kvalitet och spännande spelupplevelse.
En av de största fördelarna med att spela på Gogo Casino är deras generösa bonusar och kampanjer. Som ny spelare kan du ta del av en välkomstbonus som ger dig extra pengar att spela för och ökar dina chanser att vinna stort. Dessutom erbjuder Gogo Casino regelbundet olika kampanjer och tävlingar där du kan vinna fantastiska priser som free spins, kontantpriser eller till och med resor.
En annan fördel med att spela på Gogo Casino är deras snabba och säkra betalningsmetoder. Du kan enkelt sätta in och ta ut pengar genom populära metoder som banköverföring, kreditkort eller e-plånböcker, vilket ger dig en smidig spelupplevelse utan krångel.
För de som gillar att spela på språng finns även en mobilversion av Gogo Casino som är optimerad för smartphones och surfplattor. Du kan enkelt logga in på ditt konto var som helst och när som helst för att njuta av dina favoritspel.
Sammanfattningsvis är Gogo Casino en spännande spelplattform som erbjuder ett brett utbud av spel, generösa bonusar och säkra betalningsmetoder. Om du letar efter en rolig och spännande spelupplevelse är Gogo Casino definitivt värt ett besök. Besök deras webbplats idag och ta del av den spännande spelactionen!
https://gogocasino.one
Gogo casino com är en spännande online spelsajt som erbjuder en rad olika casinospel för sina spelare. Med ett stort utbud av spelautomater, bordsspel och live casino spel, finns det något för alla typer av spelare att njuta av.
En av de fördelar med gogo casino com är att det är tillgängligt dygnet runt, vilket gör det möjligt för spelare att spela sina favoritspel när det passar dem bäst. Sajten är också lätt att navigera och erbjuder en säker och pålitlig spelupplevelse.
Förutom det breda spelutbudet och tillgängligheten är gogo casino com också känt för sina generösa bonusar och kampanjer. Spelare kan ta del av välkomstbonusar, gratis spins och andra belöningar som ökar deras chanser att vinna stort.
Som en ledande aktör inom online casinobranschen, strävar gogo casino com ständigt efter att förbättra och utveckla sin plattform för att ge spelare den bästa möjliga spelupplevelsen. Med en dedikerad kundsupport och säkra betalningsmetoder kan spelare känna sig trygga och väl omhändertagna när de spelar på sajten.
Sammanfattningsvis är gogo casino com en populär och pålitlig online spelsajt som erbjuder en rad spännande spel och generösa bonusar. Oavsett om du är en erfaren spelare eller nybörjare, finns det något för alla att utforska och njuta av på gogo casino com. Besök sajten idag och se själv vad den har att erbjuda!
https://gogocasino.one
prayertimein.com
Gogo Casino är en populär spelsajt som erbjuder en mängd olika casinospel online. Många spelare lockas av deras generösa bonusar och spännande spelutbud. Men tyvärr har det kommit uppgifter om att vissa spelare haft problem med att få ut sina vinster från casinot.
En del spelare har rapporterat att Gogo Casino inte har betalat ut deras vinster trots att de har vunnit och uppfyllt alla krav för att få ut pengarna. Detta har självklart skapat missnöje bland spelarna och många har kritiserat casinot för att agera oetiskt och oprofessionellt.
Det är viktigt att komma ihåg att det är viktigt att spela på en pålitlig och licensierad spelsajt för att undvika problem med utbetalningar. Om du har upplevt att Gogo Casino inte har betalat ut dina vinster bör du kontakta deras kundtjänst för att försöka lösa situationen.
Det är alltid bra att vara försiktig när man spelar på onlinecasinon och att inte satsa mer pengar än man har råd att förlora. Genom att välja ett pålitligt casino med gott rykte kan man undvika problem med utbetalningar och njuta av en säker och rolig spelupplevelse online.
https://gogocasino.one
http://kamagraiq.shop/# п»їkamagra
Gogo casino är en populär onlinekasino där spelare kan njuta av ett brett utbud av spel och vinna stora priser. Men det finns vissa problem som spelare kan stöta på när de försöker ta ut sina vinster från kasinot.
Ett av de vanligaste problemen är att spelare kan ha svårt att få tillgång till sina pengar efter att ha vunnit. Vissa spelare kan uppleva förseningar eller problem med banköverföringar eller andra uttagsmetoder som kasinot erbjuder. Detta kan vara frustrerande för spelarna och göra dem tveksamma att fortsätta spela på kasinot.
En annan vanlig fråga är att spelare kan behöva uppfylla vissa omsättningskrav innan de kan ta ut sina vinster. Detta innebär att spelarna måste satsa en viss summa pengar innan de kan ta ut sina vinster från kasinot. Detta kan vara besvärligt för vissa spelare och leda till missnöje.
För att undvika problem med uttag är det viktigt att spelare läser och förstår villkoren för kasinot innan de spelar. Det är också viktigt att välja en pålitlig och licensierad operatör för att undvika potentiella problem. Om en spelare stöter på problem med uttag bör de kontakta kasinots kundtjänst för att få hjälp och support.
I slutändan är det viktigt att spelare är medvetna om de potentiella problemen med uttag på onlinekasinon och tar ansvarsfulla beslut när de spelar. Genom att vara försiktig och noga med att följa kasinots regler och villkor kan spelare undvika problem och njuta av en positiv spelupplevelse på Gogo casino.
https://gogocasino.one
Gogo Casino är en relativt ny online casino som har växt i popularitet i Finland. Med sitt enkla och minimalistiska design har de lyckats locka många spelare som söker en smidig och underhållande spelupplevelse.
Gogo Casino skiljer sig från många andra online casinon genom att de fokuserar på att erbjuda en snabb och enkel registreringsprocess, där spelare inte behöver skapa ett konto för att spela. Istället verifierar de sig med BankID vilket innebär att insättningar och uttag sker på nolltid.
En annan fördel med Gogo Casino är deras imponerande utbud av spel från några av de bästa spelleverantörerna på marknaden. Här hittar spelare allt från klassiska spelautomater till bordsspel och live casino.
Gogo Casino erbjuder också generösa bonusar och kampanjer som lockar till sig både nya och återkommande spelare. Deras kundtjänst är tillgänglig dygnet runt för att hjälpa till med eventuella frågor eller problem som kan uppstå under spel.
Sammanfattningsvis har Gogo Casino blivit en populär destination för finska spelare som letar efter en snabb, smidig och rolig spelupplevelse. Med sitt stora utbud av spel, generösa bonusar och effektiv kundtjänst har de tagit online casino upplevelsen till en helt ny nivå.
https://gogocasino.one
https://sildenafiliq.com/# order viagra
Gogo Casino partners är en del av Gogo Casino familjen som arbetar nära med casinot för att skapa en komplett spelupplevelse för spelare. Genom att samarbeta med olika partners kan Gogo Casino erbjuda ett brett utbud av spel, kampanjer och belöningar för sina spelare.
En av de viktigaste delarna av Gogo Casino partners är att säkerställa att spelarna får den bästa möjliga upplevelsen när de spelar på casinot. Genom att samarbeta med ledande spelleverantörer kan Gogo Casino erbjuda spel av hög kvalitet med spännande funktioner och grafik.
Gogo Casino partners arbetar också för att erbjuda spelare spännande kampanjer och belöningar för att hålla dem engagerade och underhållna. Genom att samarbeta med olika företag och organisationer kan Gogo Casino erbjuda spelare exklusiva erbjudanden och belöningar som inte är tillgängliga någon annanstans.
Genom att jobba nära med sina partners kan Gogo Casino säkerställa att deras spelare får den bästa möjliga spelupplevelsen. Genom att erbjuda ett brett utbud av spel, kampanjer och belöningar kan Gogo Casino partners hjälpa casinot att växa och bli ännu mer framgångsrikt.
I slutändan är Gogo Casino partners en viktig del av Gogo Casino familjen som arbetar för att göra spelupplevelsen så bra som möjligt för alla spelare. Genom att samarbeta med olika partners kan Gogo Casino fortsätta att erbjuda spel av hög kvalitet och spännande kampanjer för sina spelare att njuta av.
https://gogocasino.one
Gogo Casino har nyligen lanserat ett partnersprogram för att samarbeta med olika aktörer inom iGaming-branschen. Med detta partnerskap kommer de att kunna erbjuda sina spelare ännu mer spännande och underhållande spelupplevelser.
Genom partnerskapet med Gogo Casino kommer andra operatörer att kunna dra nytta av deras innovativa spelplattform och stora spelportfölj. Det innebär att spelare kommer att kunna njuta av populära casinospel och spelautomater från ledande leverantörer.
För Gogo Casino innebär partnerskapet att de kan expandera sin närvaro på marknaden och nå ut till en större publik. Genom att samarbeta med andra aktörer kan de också dra nytta av deras expertis och erfarenhet inom branschen.
Gogo Casino är känt för att erbjuda spelare en säker och ansvarsfull spelupplevelse. Genom partnerskapet kommer de att kunna fortsätta att erbjuda högkvalitativa spel och en trygg miljö för sina spelare.
Partnerskapet med Gogo Casino är en win-win-situation för alla involverade parter. Det kommer att ge spelare en bättre spelupplevelse och hjälpa Gogo Casino att fortsätta att vara en ledande aktör inom iGaming-branschen.
https://gogocasino.one
Купить травматическое оружие, пистолет или револьвер – выбор за вами, у нас лучшие цены и популярные модели всегда в наличии! Наша жизнь полна скрытых угроз и опасностей Купить боевой пистолет
Gogo casino är en av de mest populära onlinekasinon i Finland just nu. Med ett stort utbud av spel, generösa bonusar och en användarvänlig plattform lockar Gogo casino till sig tusentals spelare varje dag.
En av anledningarna till Gogo casinos popularitet är deras imponerande spelutbud. Här hittar du allt från klassiska casinospel som blackjack och roulette till moderna videoautomater och progressiva jackpottspel. Oavsett vilken typ av spelare du är finns det garanterat något som passar dig på Gogo casino.
Utöver det stora utbudet av spel erbjuder Gogo casino också generösa bonusar och kampanjer till sina spelare. Nya spelare kan se fram emot en välkomstbonus när de registrerar sig på sajten, och regelbundna spelare belönas med lojalitetspoäng och andra förmåner. Detta gör att det är värt att stanna kvar och spela på Gogo casino även efter att man tagit del av välkomstbonusen.
En annan faktor som bidrar till Gogo casinos popularitet är deras användarvänliga plattform. Sajten är lätt att navigera och spelare kan enkelt hitta sina favoritspel samt kontakta kundtjänsten om de skulle ha några frågor. Dessutom är Gogo casino tillgängligt både på datorn och i mobilversion, vilket gör det enkelt att spela var man än befinner sig.
Sammanfattningsvis är Gogo casino en av de bästa onlinekasinona i Finland just nu. Med sitt stora spelutbud, generösa bonusar och användarvänliga plattform är det en given favorit bland både nya och erfarna spelare. Om du ännu inte har provat Gogo casino rekommenderar vi starkt att ge det en chans – du kommer inte att bli besviken.
https://gogocasino.one
Gogo casino ägare är en spännande och relativt ny aktör på den svenska spelmarknaden. Med sin moderna design och roliga spel har de snabbt blivit populära bland både unga och äldre spelare.
Gogo casino ägare har satsat stort på att erbjuda sina kunder en smidig och säker spelupplevelse. Genom att erbjuda ett stort utbud av olika casinospel, såsom slots, bordsspel och live casino, har de lyckats attrahera en bred publik.
En av de stora fördelarna med gogo casino ägare är deras generösa erbjudanden och kampanjer. De har regelbundet tävlingar och bonusar som gör det extra spännande och lönsamt att spela hos dem.
Som ägare av gogo casino är man garanterad en rättvis och säker spelupplevelse. De har alla nödvändiga licenser och regleras av svenska spelmyndigheten, vilket ger spelare trygghet och förtroende för att spela hos dem.
Sammanfattningsvis är gogo casino ägare en pålitlig och spännande aktör på casinomarknaden. Med deras moderna plattform, stora utbud av spel och generösa erbjudanden är de definitivt värda att prova på för alla som gillar att spela casino online.
https://gogocasino.one
Gogo Casino är en populär online casino som ägs av det svenska företaget Leo Vegas Gaming Ltd. Leo Vegas är ett välkänt namn inom spelbranschen och driver flera framgångsrika online casinon. Gogo Casino lanserades år 2019 och har snabbt blivit en favorit bland svenska spelare.
Ägarna till Gogo Casino har en lång erfarenhet inom spelbranschen och strävar efter att erbjuda en säker och underhållande spelupplevelse för alla sina spelare. Genom att erbjuda ett brett utbud av spel från ledande leverantörer och en användarvänlig plattform, har Gogo Casino blivit en attraktiv destination för spelare som söker en premium spelupplevelse.
Ägarna till Gogo Casino har även en starkt engagemang för ansvarsfullt spelande och arbetar aktivt för att främja ett hälsosamt och säkert spelande för alla sina spelare. Genom att erbjuda verktyg för självexkludering, insättningsgränser och personliga speltidsbegränsningar, strävar Gogo Casino efter att skapa en trygg spelmiljö där spelare kan njuta av sina favoritspel utan att riskera att utveckla spelberoende.
Med en dedikerad kundtjänst och enkelheten i att göra både insättningar och uttag, är Gogo Casino en pålitlig och trygg operatör för alla som söker en spännande och säker spelupplevelse. Med ägarna bakom Leo Vegas Gaming Ltd vid rodret kan spelare lita på att Gogo Casino är en pålitlig och ansvarsfull aktör inom den dynamiska världen av online casino spel.
https://gogocasino.one
Книга – это не просто подарок, это инвестиция в развитие и обогащение внутреннего мира человека.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Gogo Casino är en populär online spelplattform som har blivit känt för sina innovativa spel och snabba transaktioner. Nu har de inlett ett spännande samarbete med andra casinon för att erbjuda ännu fler spännande spel och kampanjer till sina spelare.
Det nya samarbetet mellan Gogo Casino och andra casinon kommer att ge spelarna tillgång till ett ännu större utbud av spel från olika leverantörer. Detta innebär att spelare inte bara kan njuta av Gogo Casinos egna spel, utan också ta del av andra spännande spel som erbjuds av deras samarbetspartners.
Genom detta samarbete kommer spelarna också att kunna ta del av nya kampanjer och erbjudanden som är exklusiva för de deltagande casinona. Detta innebär att spelarna kan ta del av spännande bonusar, tävlingar och andra belöningar som kommer att göra deras spelupplevelse ännu mer underhållande och givande.
Gogo Casino och deras samarbetspartners har som mål att skapa en exklusiv och spännande spelupplevelse för sina spelare. Genom att erbjuda ett brett utbud av spel och kampanjer kommer de att kunna locka till sig fler spelare och behålla sina befintliga kunder.
Det nya samarbetet mellan Gogo Casino och andra casinon har redan fått stor uppmärksamhet och spelarna ser fram emot att få testa de nya spel och kampanjer som kommer att erbjudas. Med sitt fokus på innovation och spelglädje ser det ut som om Gogo Casino är på väg att bli ett av de ledande online casinona på marknaden.
https://gogocasino.one
Проверенный магазин, низкие цены на аккаунты с токенами, моментальная выдача купленного аккаунта, высокая репутация магазина. Купите один раз и будете нашим постоянным клиентом! Так-же занимаемся продвижением модельного аккаунта BongaCams bongacams аккаунты
buy kamagra online usa super kamagra cheap kamagra
intel core i7-9700f @ 3.00ghz https://cpu-specs.com/
Gogo Casino är ett populärt online casino som lanserades i Finland år 2019. Med ett stort urval av spelautomater, live casinospel och bordsspel har Gogo Casino snabbt blivit ett favoritval för många spelare i Finland.
En av anledningarna till Gogo Casinos popularitet är dess användarvänliga och moderna design. Hemsidan är lätt att navigera och spelarna kan enkelt hitta sina favoritspel genom att söka efter dem eller använda kategorierna som erbjuds.
Gogo Casino tar ansvar för att erbjuda sina spelare en säker och rättvis spelupplevelse. De erbjuder en säker betalningsmetod via Trustly, vilket gör att spelarna kan göra insättningar och uttag snabbt och säkert.
En annan fördel med Gogo Casino är deras generösa bonuserbjudanden och kampanjer. Nya spelare kan ta del av en välkomstbonus vid sin första insättning och befintliga spelare kan dra nytta av regelbundna bonusar och belöningar.
Sammanfattningsvis är Gogo Casino ett utmärkt val för finska spelare som är ute efter en spännande och underhållande spelupplevelse. Med sitt stora spelutbud, användarvänliga design och säkra betalningsmetoder är det inte konstigt att Gogo Casino har blivit en favorit bland många finska spelare. Besök Gogo Casino idag och upplev spänningen själv!
https://gogocasino.one
Читая книгу, человек учится эмпатии и пониманию чужой точки зрения, что способствует укреплению межличностных отношений.
https://www.klerk.ru/materials/2022-02-15/525164/
Gogo casino är en populär online casino som erbjuder ett brett utbud av spel och underhållning för spelare över hela världen. Men många undrar: vem äger egentligen Gogo casino?
Enligt information från Gogo casinos officiella webbplats ägs och drivs casinot av det maltesiska bolaget Gogo Enterprises Ltd. Bolaget har en registrerad adress i Malta och är licensierat av Malta Gaming Authority, vilket innebär att casinot följer strikta regler och bestämmelser för att säkerställa en säker och rättvis spelupplevelse för sina spelare.
Gogo casino är också ett varumärke inom Hero Gaming, en ledande aktör inom den internationella spelindustrin med flera framgångsrika online casinon under sitt bälte. Hero Gaming har ett gott rykte för att erbjuda innovativa spelupplevelser och högkvalitativa tjänster till sina kunder.
Sammanfattningsvis ägs och drivs Gogo casino av Gogo Enterprises Ltd, ett maltesiskt bolag som är licensierat av Malta Gaming Authority. Casinot är också en del av Hero Gaming, en respekterad speloperatör med flera populära varumärken inom branschen. Med sin starka förankring inom spelindustrin kan spelare vara trygga med att de är i säkra händer när de spelar på Gogo casino.
https://gogocasino.one
Книга – это источник вдохновения для творческих начинаний и проектов. Ее страницы могут заполниться заметками, идеями и рисунками, став основой для новых творческих экспериментов.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Gogo Casino har snabbt blivit ett populärt online casino bland svenska spelare. Med sitt enkla och smidiga gränssnitt har de lyckats locka till sig en stor spelarbas. Trots detta har det nyligen uppstått en del problem hos Gogo Casino som har fått vissa spelare att reagera negativt.
Ett av de största problemen som har rapporterats är att vissa spelare har haft svårigheter att ta ut sina vinster. En del spelare har klagat på långa väntetider och krånglig process för att få ut sina pengar. Det här har skapat frustration och missnöje bland många spelare som förväntar sig snabba och smidiga uttag när de spelar på ett online casino.
En annan källa till problem hos Gogo Casino har varit deras kundtjänst. Vissa spelare har rapporterat att de haft svårt att få svar på sina frågor eller att de fått otydliga och oklara svar. En bra kundtjänst är av största vikt för att skapa en positiv spelupplevelse och det är viktigt att Gogo Casino åtgärdar detta problem snabbt för att behålla sina spelare.
Trots dessa problem så finns det fortfarande många som föredrar att spela på Gogo Casino på grund av deras breda utbud av spel och deras användarvänliga plattform. Det är viktigt att Gogo Casino lyssnar på feedback från sina spelare och tar tag i de problem som har uppstått för att skapa en bättre spelupplevelse för alla sina kunder.
Sammanfattningsvis har Gogo Casino stött på vissa problem som har påverkat deras rykte och spelarbas negativt. Det är viktigt att de tar tag i dessa problem snabbt och effektivt för att behålla sin position som ett av de ledande online casinona på marknaden. Det är också viktigt att spelare är medvetna om dessa problem och tar dem i beaktande när de väljer var de vill spela.
https://gogocasino.one
mircette 20mg
Подарив книгу, вы дарите возможность человеку открыть для себя новые авторов и литературные жанры. https://rusvesna.su/aboutall/1599556550
Den populära online-casinon Gogo Casino har nyligen fått ett beslut som innebär att de inte kommer att få några pengar från sina spelare. Spelinspektionen har beslutat att återkalla deras spellicens på grund av brister i företagets rutiner för ansvarsfullt spelande.
Beslutet kommer efter en lång utredning där det framkommit att Gogo Casino inte har vidtagit tillräckliga åtgärder för att förebygga spelproblem bland sina spelare. Enligt Spelinspektionen har företaget bland annat inte haft tillräckliga verktyg för att kunna identifiera och hjälpa spelare som riskerar att hamna i spelberoende.
Gogo Casino har nu fått en tillsynsnämnd att utreda ärendet och besluta om eventuella sanktioner mot företaget. De kommer inte att kunna ta emot några insättningar eller ta ut några vinster tills vidare.
Det här beslutet skickar en tydlig signal till alla aktörer på den svenska spelmarknaden om vikten av att ta ansvar för sitt spelutbud och sina spelare. Det är viktigt att alla online-casinon följer de regler och riktlinjer som finns för att skydda spelarna och minska risken för spelmissbruk.
För spelare som är drabbade av beslutet innebär det att de inte längre kan spela på Gogo Casino och att eventuella vinster kan komma att bli oåtkomliga. Det är viktigt att alla spelare som upplever spelproblem söker hjälp och stöd för att komma på rätt väg igen.
Sammanfattningsvis är det här ett viktigt steg för att skapa en säkrare spelmarknad i Sverige och för att skydda spelare från att hamna i spelberoende. Genom att tillsammans arbeta för ett ansvarsfullt spelande kan vi se till att alla kan njuta av underhållningen som casinon erbjuder utan att riskera sin hälsa och ekonomi.
https://gogocasino.one
Cheap Sildenafil 100mg buy viagra online Viagra tablet online
Книга может быть источником вдохновения и мотивации. В ее страницах можно найти истории успеха, которые подтолкнут к собственным достижениям. https://rusvesna.su/aboutall/1599556550
Gogo Casino välkomstbonus
Gogo Casino är ett populärt online casino som erbjuder en generös välkomstbonus till sina nya spelare. Med denna välkomstbonus får du en fantastisk start på ditt spelande hos Gogo Casino.
Vad ingår i Gogo Casino välkomstbonus? När du registrerar dig som ny spelare hos Gogo Casino och gör din första insättning så får du en fin bonus som du kan använda för att spela på deras spännande spelutbud. Bonusen kan variera beroende på kampanjer och erbjudanden, så det är alltid bra att hålla koll på Gogo Casinos webbplats för att se vilka bonusar som är tillgängliga just nu.
För att ta del av Gogo Casino välkomstbonus behöver du vanligtvis göra en insättning på en viss summa pengar. Därefter får du en procentuell bonus som matchar din insättning, vilket ger dig extra pengar att spela för. Det finns även ofta möjlighet att få free spins i samband med välkomstbonusen, vilket ger dig chansen att vinna ännu mer.
För att kunna ta ut eventuella vinster från välkomstbonusen så behöver du uppfylla omsättningskraven som Gogo Casino har. Omsättningskravet innebär att du behöver satsa en viss summa pengar innan du kan ta ut dina vinster. Det är viktigt att läsa igenom reglerna och villkoren för välkomstbonusen så att du vet vad som gäller.
Sammanfattningsvis är Gogo Casino välkomstbonus en utmärkt möjlighet för dig som vill testa på deras spännande spelutbud och öka dina vinstchanser. Med en generös bonus och potentiella free spins så kan du få en riktigt bra start på ditt spelande hos Gogo Casino. Så varför inte ta chansen och registrera dig idag för att ta del av deras välkomstbonus? Lycka till!
https://gogocasino.one
Gogo Casino är en populär online-spelplattform som erbjuder ett brett utbud av casinospel för sina användare. Men trots sin popularitet har plattformen stött på vissa problem som har oroat spelarna.
Ett av de främsta bekymren som spelarna har uttryckt är att vissa spel på Gogo Casino verkar vara orättvisa eller riggade. Många användare har rapporterat att de förlorar konsekvent på vissa spel utan att någonsin ha en chans att vinna. Detta har lett till spekulationer om att plattformen kanske manipulerar resultaten för att gynna huset.
Ett annat problem som spelare har upplevt är bristen på transparent kommunikation från Gogo Casino. Många användare har klagat på att de har svårt att få svar på sina frågor eller bekymmer från plattformens kundsupport. Detta har skapat en känsla av frustration och misstro bland spelarna.
Trots dessa problem har Gogo Casino också många lojala användare som uppskattar plattformens spelutbud och användarvänliga gränssnitt. Många spelare har även uttryckt att de har vunnit stora summor pengar på plattformen, vilket har bidragit till att skapa en positiv upplevelse för dem.
Det är viktigt att Gogo Casino lyssnar på feedback från sina användare och arbetar för att förbättra kundtillfredsställelsen och förtroendet för plattformen. Genom att vara transparenta med sina spelare och se till att alla spel är rättvisa och slumpmässiga kan Gogo Casino fortsätta att vara en ledande aktör inom online-casinobranschen.
https://gogocasino.one
Gogo Casino har varit en populär online-spelplattform för många svenska spelare, men på senare tid har det uppstått problem som har oroat många användare. En av de största utmaningarna för många spelare är att de upplever svårigheter när de försöker ta ut sina vinster från casinot.
Många spelare har rapporterat att de har stött på långa väntetider och komplicerade uttagsprocesser när de försöker ta ut sina pengar från Gogo Casino. Detta har skapat frustration bland många användare, och vissa har till och med beslutat sig för att sluta spela på plattformen på grund av dessa problem.
En annan oroande fråga som har dykt upp är att vissa spelare har rapporterat att de har haft svårigheter att få kontakt med kundtjänsten på Gogo Casino. Detta har gjort det svårt för spelare att lösa eventuella problem som uppstår när de spelar på plattformen.
Det är viktigt för casinon att ha en pålitlig och tillgänglig kundtjänst för att kunna hantera eventuella problem och frågor som spelare kan stöta på. Om spelare inte kan få den hjälp de behöver när de behöver det, kan det leda till missnöje och minskad lojalitet bland användarna.
För att lösa dessa problem är det viktigt att Gogo Casino tar de nödvändiga åtgärderna för att förbättra sin uttagsprocess och säkerställa att deras kundtjänst är tillgänglig och effektiv för spelarna. Genom att lyssna på spelarnas feedback och ta itu med de rapporterade problemen kan Gogo Casino förbättra sin service och behålla sitt rykte som en pålitlig spelplattform för svenska spelare.
https://gogocasino.one
Читая книгу, человек развивает свой интеллект и воображение, открывает для себя новые идеи и точки зрения. Поэтому дарить книгу – значит дарить возможность к росту и самосовершенствованию.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Gogo Casino är ett populärt onlinecasino som erbjuder sina spelare en mängd olika spelalternativ. För de som behöver komma i kontakt med casinot finns det flera olika sätt att göra det.
Det enklaste sättet att kontakta Gogo Casino är genom deras livechattfunktion. Genom att klicka på ikonen längst ned på webbplatsen kan spelare direkt kommunicera med en representant från casinot. Livechatten är tillgänglig dygnet runt för att hjälpa till med eventuella frågor eller problem som kan uppstå.
För spelare som föredrar att skicka ett e-postmeddelande finns det också möjlighet att kontakta Gogo Casino på deras kontaktadress. Genom att skicka ett mail till protected] kan spelare få svar på sina frågor inom kort.
För de som föredrar att prata med någon personligen finns det också möjlighet att ringa Gogo Casino direkt. Kundtjänstteamet finns tillgängligt på telefonnummer 08-580 961 69 för att hjälpa till med alla frågor eller bekräfta detaljer.
Oavsett vilket sätt spelare väljer att kontakta Gogo Casino på kan de vara säkra på att få snabb och professionell hjälp. Casinot strävar efter att ge den bästa kundservicen möjligt för att säkerställa en smidig spelupplevelse för alla sina spelare.
https://gogocasino.one
Читая книгу, человек обогащает свой внутренний мир и развивает свое эмоциональное восприятие. Ведь в каждой книге есть что-то свое, что заставляет задуматься и переживать.
https://www.klerk.ru/materials/2022-02-15/525164/
Gogo Casino välkomstbonus
Gogo Casino är en populär onlinekasino som är känt för sitt stora utbud av spel och generösa bonusar. En av de mest eftertraktade bonusarna som Gogo Casino erbjuder är välkomstbonusen.
Välkomstbonusen hos Gogo Casino är en av de bästa på marknaden och ger nya spelare en fantastisk start på deras speläventyr. När du registrerar dig som ny spelare på Gogo Casino kan du se fram emot en generös välkomstbonus som kan ge dig extra pengar att spela för.
Välkomstbonusen hos Gogo Casino kan variera och kan inkludera olika typer av bonusar, såsom insättningsbonusar, gratissnurr eller andra förmåner. För att ta del av välkomstbonusen hos Gogo Casino behöver du registrera ett konto och göra en insättning. Välkomstbonusen kommer då automatiskt att krediteras till ditt spelkonto och du kan börja spela med bonusen.
För att utnyttja välkomstbonusen fullt ut är det viktigt att läsa och förstå reglerna och villkoren som gäller för bonusen. Ofta finns det omsättningskrav som måste uppfyllas innan du kan ta ut eventuella vinster som genererats med välkomstbonusen. Genom att följa dessa regler kan du maximera din chans att få ut så mycket som möjligt av din välkomstbonus.
Sammanfattningsvis är välkomstbonusen hos Gogo Casino en fantastisk möjlighet för nya spelare att få en bra start på sitt speläventyr. Med en generös bonus och ett stort utbud av spel är Gogo Casino en idealisk plats för alla som älskar att spela kasinospel på nätet. Så registrera dig idag och ta del av din välkomstbonus på Gogo Casino!
https://gogocasino.one
https://www.libremercado.com/2015-12-13/china-para-pymes-lo-que-debe-saber-para-entrar-en-el-mayor-mercado-del-mundo-1276563641/
Читая книгу, человек развивает свой интеллект и воображение, открывает для себя новые идеи и точки зрения. Поэтому дарить книгу – значит дарить возможность к росту и самосовершенствованию.
https://www.klerk.ru/materials/2022-02-15/525164/
Gogo Casino är en populär online casino som erbjuder ett brett utbud av spel och kampanjer. I det här omdömet kommer vi att ta en närmare titt på vad som gör Gogo Casino till en av de bästa online casinon på marknaden just nu.
En av de främsta anledningarna till att många spelare väljer Gogo Casino är deras imponerande utbud av spel. Här hittar du allt från klassiska slots och bordsspel till mer moderna video slots och live dealer spel. Oavsett vilken typ av spel du föredrar så är chansen stor att du hittar det på Gogo Casino.
En annan fördel med Gogo Casino är deras generösa kampanjer och erbjudanden. Nya spelare får ofta tillgång till välkomstbonusar och gratissnurr, medan befintliga spelare kan dra nytta av regelbundna kampanjer och turneringar. Det här gör att spelupplevelsen på Gogo Casino blir både spännande och belönande.
En annan viktig faktor att ta hänsyn till när man betygsätter ett online casino är säkerheten. Gogo Casino erbjuder en trygg och säker spelupplevelse, med licenser från respekterade spelmyndigheter och avancerad krypteringsteknik för att skydda spelarnas personuppgifter och transaktioner.
Sammanfattningsvis är Gogo Casino en utmärkt plattform för dig som vill utforska spännande spel och ta del av generösa kampanjer. Med ett stort utbud av spel, regelbundna kampanjer och en hög nivå av säkerhet så kan vi varmt rekommendera Gogo Casino till alla som är intresserade av online casinon.
https://gogocasino.one
http://tadalafiliq.com/# Cialis 20mg price
Книга – это долговечный подарок, который сохранит свою ценность на протяжении многих лет. Ведь знания, полученные из книги, никогда не утрачивают своей актуальности.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Gogo Casino Bonus
Letar du efter spännande bonusar och erbjudanden när du spelar på online casinon? Då är Gogo Casino ett alternativ du borde kolla in. Med deras generösa bonusar kan du få extra pengar att spela för och öka dina vinstchanser.
Gogo Casino erbjuder olika typer av bonusar för sina spelare. En vanlig bonus är välkomstbonusen som ges till nya spelare när de registrerar sig på casinot. Denna bonus kan ge dig extra pengar att spela för eller free spins på utvalda spelautomater.
Utöver välkomstbonusen erbjuder Gogo Casino även regelbundna kampanjer och erbjudanden för sina befintliga spelare. Dessa kan inkludera reload-bonusar, cashback-erbjudanden eller tävlingar med fina priser.
För att ta del av Gogo Casino bonusar behöver du oftast göra en insättning på ditt spelkonto. En del bonusar kräver även att du använder en bonuskod vid insättningen. Det är därför viktigt att läsa villkoren för varje bonus noggrant för att förstå hur den fungerar.
Det är också viktigt att komma ihåg att bonusar vanligtvis kommer med omsättningskrav. Detta innebär att du måste omsätta bonussumman ett visst antal gånger innan du kan ta ut dina vinster. Se därför till att förstå vilka regler och villkor som gäller för varje bonus innan du accepterar den.
Sammanfattningsvis kan Gogo Casino bonusar ge dig en fantastisk spelupplevelse med extra pengar att spela för och fler chanser att vinna stora vinster. Var noga med att läsa villkoren för varje erbjudande och ha kul när du spelar på detta spännande online casino. Lycka till!
https://gogocasino.one
Книга – это не просто подарок, это инвестиция в развитие и обогащение внутреннего мира человека. https://rusvesna.su/aboutall/1599556550
https://sildenafiliq.com/# Cheap Sildenafil 100mg
Gogo Casino är ett populärt online casino som lockar med en generös välkomstbonus för nya spelare. När du registrerar dig som ny medlem hos Gogo Casino får du möjligheten att ta del av en välkomstbonus som ger dig extra spelkapital att spela för.
Välkomstbonusen hos Gogo Casino kan variera beroende på aktuella kampanjer och erbjudanden, men vanligtvis kan du förvänta dig att få antingen bonuspengar eller free spins vid din första insättning. Denna bonus gör det möjligt för dig att utforska casinots spelutbud och öka dina vinstchanser utan att behöva riskera dina egna pengar.
För att ta del av välkomstbonusen hos Gogo Casino behöver du endast registrera ett spelkonto och göra din första insättning. Därefter aktiveras bonusen automatiskt och du kan börja spela med ditt extra spelkapital. Tänk på att bonusvillkoren kan variera och det är viktigt att läsa igenom dem noggrant innan du accepterar bonusen.
Gogo Casino erbjuder ett brett utbud av casinospel, inklusive klassiska slots, bordsspel och live casino. Med din välkomstbonus kan du testa olika spel och uppleva spänningen av att spela på ett online casino. Var noga med att spela ansvarsfullt och sätt upp gränser för ditt spelande för att undvika att spela för mer än du har råd med.
Sammanfattningsvis är Gogo Casino en spännande spelsajt som lockar med en generös välkomstbonus för nya spelare. Ta chansen att få extra spelkapital och upplev den spännande världen av online casino hos Gogo Casino redan idag!
https://gogocasino.one
Подарив книгу, вы дарите возможность человеку узнать о себе что-то новое, вдохновив его на самопознание и личностный рост.
https://www.chitalnya.ru/press/1950/
Gogo Casino är en populär spelsajt som erbjuder både casino och livecasino spel online. Men vad tycker spelarna egentligen om Gogo Casino? Här är en recension av sajten.
En av de främsta anledningarna till att många spelare väljer Gogo Casino är det stora utbudet av spel. Här finns allt från klassiska casinospel som roulette och blackjack till moderna videoslots och progressiva jackpottar. Dessutom erbjuder de även livecasino spel där spelarna kan spela mot riktiga dealers i realtid.
En annan fördel med Gogo Casino är deras användarvänliga plattform. Sajten är lätt att navigera och det är enkelt att hitta sina favoritspel. Dessutom finns det möjlighet att spela både på datorn och på mobilen, vilket gör det smidigt för spelarna att spela var de än befinner sig.
När det kommer till bonusar och kampanjer så erbjuder Gogo Casino regelbundet generösa erbjudanden till sina spelare. Det kan vara allt från välkomstbonusar till free spins och cashback-erbjudanden. Det är alltid viktigt att läsa villkoren för bonusarna noga innan man accepterar dem, för att undvika obehagliga överraskningar.
Sammanfattningsvis så är Gogo Casino en pålitlig och underhållande spelsajt som erbjuder spelare en bra spelupplevelse. Med sitt stora spelutbud, användarvänliga plattform och generösa bonusar, så är det inte konstigt att många spelare väljer att spela hos Gogo Casino. Helt klart värt ett besök för dig som älskar att spela casino online.
https://gogocasino.one
Читая книгу, человек учится эмпатии и пониманию чужой точки зрения, что способствует укреплению межличностных отношений.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Eu recomendo esse jogo a todos fortune Tiger
Det har blivit känt att det populära online casinot Gogo Casino inte längre kommer att erbjuda sina spelare möjligheten att spela med riktiga pengar. Istället kommer de endast att erbjuda spel utan insatser, vilket innebär att spelarna inte kan vinna riktiga pengar.
Beslutet att ta bort möjligheten att spela med pengar på Gogo Casino har mötts av mycket kritik från spelare och branschexperter. Många anser att det är ett steg tillbaka för casinot och att det kommer att minska spelupplevelsen för många av deras trogna kunder.
Enligt Gogo Casino är beslutet att ta bort möjligheten att spela med pengar en del av deras strategi för att minska risken för spelmissbruk. Genom att endast erbjuda spel utan insatser hoppas de att deras spelare ska kunna njuta av spelen på ett mer avslappnat sätt, utan att riskera att förlora stora summor pengar.
Trots detta har många spelare uttryckt sin besvikelse över beslutet och en del har även valt att lämna casinot för att söka sig till andra spelsajter där de fortfarande kan spela med riktiga pengar.
Det återstår att se hur Gogo Casino kommer att påverkas av beslutet att ta bort möjligheten att spela med pengar. Förhoppningsvis kommer de att lyckas behålla sina spelare och fortsätta att erbjuda en underhållande spelupplevelse på andra sätt.
https://gogocasino.one
Читая книгу, человек учится выражать свои мысли и чувства более точно и глубоко, развивая свои коммуникативные навыки.
https://www.klerk.ru/materials/2022-02-15/525164/
Um dos melhores jogos Fortune Tiger
Gogo Casino uttag problem
Gogo Casino är en populär online casino som erbjuder sina spelare ett brett utbud av spel och underhållning. Men trots sin popularitet har vissa spelare stött på problem när de försöker göra uttag från sina konton.
Ett vanligt problem som spelare har rapporterat är att deras uttag tar för lång tid att behandla. Vissa hävdar att de har väntat i flera dagar eller till och med veckor för att deras uttag ska godkännas och behandlas. Detta kan vara mycket frustrerande för spelare som vill ta ut sina vinster snabbt och enkelt.
En annan vanlig klagomål är att vissa spelare har haft problem med att verifiera sina konton när de försöker göra ett uttag. Detta kan bero på att spelaren inte har tillhandahållit tillräcklig dokumentation eller att det finns tekniska problem med verifikationsprocessen.
För att undvika dessa problem rekommenderas det att spelare noggrant läser och följer Gogo Casinos uttagspolicyer och regler. Det är också viktigt att se till att kontot är korrekt verifierat och att all nödvändig dokumentation har skickats in i förväg för att undvika förseningar och problem.
Om du stöter på problem med ditt uttag på Gogo Casino, bör du kontakta deras kundtjänst för att få hjälp och support. De kan hjälpa dig att lösa eventuella problem och se till att ditt uttag behandlas så snabbt och smidigt som möjligt.
Sammanfattningsvis är det viktigt att vara medveten om att uttagsproblem kan uppstå när man spelar på online casinon som Gogo Casino. Genom att följa riktlinjerna och reglerna för uttag och verifiering samt att kontakta kundsupporten vid behov kan spelare undvika och lösa eventuella problem som kan uppstå.
https://gogocasino.one
É um jogo muito legal Fortune Tiger
Подарив книгу, вы дарите возможность человеку погрузиться в мир абстрактных идей и философских размышлений.
https://www.klerk.ru/materials/2022-02-15/525164/
Gogo Casino Partners är ett affiliateprogram som erbjuder möjligheten att samarbeta med det populära online casinot Gogo Casino. Genom att bli en partner kan du tjäna pengar genom att marknadsföra casinot och locka nya spelare att registrera sig och spela.
Som partner får du tillgång till marknadsföringsmaterial och verktyg som hjälper dig att nå ut till potentiella spelare. Du får även en dedikerad partner manager som kan hjälpa dig att optimera din marknadsföring och maximera dina intäkter.
En av fördelarna med att vara en Gogo Casino Partner är att du kan tjäna en generös provision på de intäkter som dina spelare genererar för casinot. Ju fler spelare du lockar till casinot, desto mer kan du tjäna.
För att bli en Gogo Casino Partner behöver du bara registrera dig på deras affiliateprogram och få din ansökan godkänd. Sedan är det bara att börja marknadsföra casinot och börja tjäna pengar.
Sammanfattningsvis är Gogo Casino Partners ett bra sätt att tjäna extra pengar genom att marknadsföra ett populärt online casino. Genom att dra nytta av marknadsföringsverktyg och en dedikerad partner manager kan du maximera dina intäkter och skapa en stabil inkomstkälla. Så om du är intresserad av att jobba inom iGaming-branschen och tjäna pengar på att marknadsföra casinon, är Gogo Casino Partners definitivt värt att överväga.
https://gogocasino.one
Gogo Casino Partners är ett partnerskapsprogram för onlinecasinon som erbjuder spel från flera olika leverantörer. Genom att samarbeta med Gogo Casino Partners kan casinon dra nytta av en mängd fördelar, såsom tillgång till en stor portfölj av spel, marknadsföringsstöd och teknisk support.
Genom att ansluta sig till Gogo Casino Partners kan casinon dra nytta av ett brett utbud av spel från ledande leverantörer som NetEnt, Microgaming, Play’n GO och många andra. Detta ger casinon möjlighet att erbjuda sina spelare en varierad och underhållande spelupplevelse.
Gogo Casino Partners erbjuder även marknadsföringsstöd till sina partners, vilket kan hjälpa dem att nå ut till en större publik och locka nya spelare till sina casinon. Genom att samarbeta med Gogo Casino Partners kan casinon dra nytta av deras erfarenhet och expertis inom marknadsföring och försäljning.
Utöver spel och marknadsföringsstöd erbjuder Gogo Casino Partners även teknisk support till sina partners. Casinon kan få hjälp med att lösa tekniska problem och få råd om hur de kan förbättra sin spelsajt för att maximera spelarnas upplevelse.
Sammanfattningsvis är Gogo Casino Partners ett partnerskapsprogram som kan hjälpa onlinecasinon att växa och utvecklas. Genom att samarbeta med Gogo Casino Partners kan casinon dra nytta av en mängd fördelar, såsom tillgång till spel från ledande leverantörer, marknadsföringsstöd och teknisk support.
https://gogocasino.one
Viagra generic over the counter best price on viagra Generic Viagra for sale
Gogo Casino är en populär online-spelplattform som erbjuder ett brett utbud av casinospel för sina spelare. Med en modern och användarvänlig design lockar Gogo Casino till sig tusentals spelare varje dag.
En av de bästa funktionerna hos Gogo Casino är deras generösa välkomstbonusar och regelbundna kampanjer. Spelare kan njuta av olika typer av bonusar och belöningar som gör det möjligt för dem att maximera sina vinstchanser och få en bättre spelupplevelse.
Gogo Casino erbjuder också ett stort utbud av casinospel, inklusive klassiska bordsspel som blackjack, roulette och poker, samt ett brett urval av spelautomater från ledande spelutvecklare. Oavsett om du föredrar att spela traditionella casinospel eller moderna slots, har Gogo Casino något för alla spelare.
En annan fördel med att spela på Gogo Casino är deras snabba och säkra betalningsmetoder. Spelare kan enkelt sätta in och ta ut sina vinster med hjälp av olika betalningsmetoder, inklusive kreditkort, banköverföringar och e-plånböcker.
Slutligen har Gogo Casino också en dedikerad kundtjänstavdelning som är tillgänglig dygnet runt för att hjälpa spelare med eventuella frågor eller problem de kan ha. Oavsett om du behöver hjälp med att göra en insättning, förstå bonusvillkor eller lösa ett tekniskt problem, kan du lita på att Gogo Casinos kundtjänstpersonal är där för att hjälpa dig.
Sammanfattningsvis är Gogo Casino en av de bästa online-spelplattformarna som finns tillgängliga för svenska spelare. Med deras generösa bonusar, brett utbud av spel och pålitliga kundservice är det inte konstigt att så många spelare väljer att spela på Gogo Casino varje dag. Besök deras webbplats idag och upplev spänningen med att spela på ett av de bästa online-kasinona i Sverige!
https://gogocasino.one
Gogo Casino är en spännande spelsida som erbjuder en mängd olika casinospel för alla smaker. Med sitt enkla och användarvänliga gränssnitt är det lätt att komma igång och börja spela på detta online casino.
På Gogo Casino hittar du ett brett utbud av spelautomater, bordsspel, live casino och mycket mer. Oavsett om du föredrar att spela klassiska spelautomater eller vill prova lyckan på de senaste videoautomaterna finns det något för dig här.
En av fördelarna med Gogo Casino är att det inte krävs något konto för att börja spela. Istället använder sig casinot av BankID för att verifiera din identitet och göra insättningar och uttag smidiga och säkra.
När det kommer till betalningsmetoder erbjuder Gogo Casino ett stort urval av alternativ, inklusive Trustly, kortbetalningar och flera andra populära metoder. Dessutom kan du ta del av generösa bonusar och erbjudanden som gör att du får mer att spela för.
Gogo Casino har en kundtjänst som är tillgänglig dygnet runt via livechatt och e-post för att hjälpa dig med eventuella frågor eller problem. Oavsett om du är en erfaren spelare eller nybörjare kommer du garanterat att trivas på detta spännande casino.
Sammanfattningsvis är Gogo Casino en toppmodern spelsida som erbjuder en underhållande och säker spelupplevelse för alla spelare. Med sitt stora spelutbud, enkla gränssnitt och generösa bonusar är det definitivt värt att ge detta casino en chans. Besök Gogo Casino idag och upplev spänningen själv!
https://gogocasino.one
Книга – это подарок, который можно открыть снова и снова, каждый раз находя в ней что-то новое и удивительное.
https://www.klerk.ru/materials/2022-02-15/525164/
Gogo Casino är ett populärt casinospel på nätet som erbjuder en rad spännande spel och möjligheter att vinna stora summor pengar. Ett av de viktigaste aspekterna när det kommer till att spela på online casinon är möjligheten att göra snabba och smidiga uttag av sina vinster.
Uttagen på Gogo Casino sker vanligtvis på ett effektivt sätt, vilket ger spelarna en bra spelupplevelse utan onödiga fördröjningar. För att göra ett uttag på Gogo Casino behöver spelarna först logga in på sitt spelkonto och gå till uttagssektionen. Där kan de välja sin önskade uttagsmetod, som kan vara banköverföring, e-plånbok eller annan betalningsmetod.
När spelaren har valt sin önskade uttagsmetod behöver de fylla i de nödvändiga uppgifterna och bekräfta uttaget. Uttag på Gogo Casino bearbetas vanligtvis inom några timmar, men det kan ta upp till flera bankdagar beroende på vilken uttagsmetod som används.
Det är viktigt att notera att Gogo Casino kan komma att begära dokumentation för att bekräfta spelarens identitet innan de kan behandla ett uttag. Detta är en vanlig säkerhetsåtgärd som casinon använder för att försäkra sig om att transaktionerna är säkra och trygga.
Sammanfattningsvis kan det sägas att uttag på Gogo Casino vanligtvis sker på ett effektivt sätt, vilket ger spelarna en bra spelupplevelse. Genom att följa casinots uttagsinstruktioner och vara beredd att ge nödvändig dokumentation kan spelare njuta av att snabbt få tillgång till sina vinster.
https://gogocasino.one
Книга – это не только источник знаний, но и способ развлечения. Ведь в ее страницах можно найти как научные факты, так и увлекательные рассказы.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Gogo Casino Partners är ett spännande samarbete mellan ledande speloperatörer och casinoleverantörer. Genom detta partnerskap får spelare tillgång till en mångsidig och underhållande spelupplevelse med ett brett utbud av casinospel.
Gogo Casino Partners strävar efter att erbjuda spelare den bästa möjliga spelupplevelsen genom att samarbeta med de bästa speloperatörerna och leverantörerna på marknaden. Genom att erbjuda spel från välkända och pålitliga leverantörer kan Gogo Casino Partners garantera en säker och rättvis spelupplevelse för alla sina spelare.
Med ett stort utbud av casinospel, inklusive slots, bordsspel, videopoker och live dealer-spel, finns det något för alla spelare att njuta av hos Gogo Casino Partners. Oavsett om du är en erfaren spelare eller nybörjare, kommer du att kunna hitta spel som passar din smak och spelstil.
Förutom att erbjuda ett stort urval av casinospel, strävar Gogo Casino Partners också efter att ge spelare möjligheten att dra nytta av generösa bonusar och kampanjer. Genom att regelbundet uppdatera sitt bonusutbud kan spelare få extra belöningar och förmåner när de spelar hos Gogo Casino Partners.
Sammanfattningsvis är Gogo Casino Partners det perfekta valet för spelare som letar efter en mångsidig och spännande spelupplevelse. Med ett brett utbud av casinospel, generösa bonusar och pålitliga partners är Gogo Casino Partners definitivt värt att överväga för alla spelare som är sugna på att prova lyckan på casinot.
https://gogocasino.one
naprosyn
Читая книгу, человек развивает свою способность к анализу и синтезу информации, что помогает ему лучше понимать окружающий мир. https://rusvesna.su/aboutall/1599556550
Gogo casino com är en populär online spelplattform där spelare kan njuta av en mängd olika casinospel. Genom att erbjuda en säker och spännande spelupplevelse har Gogo casino com blivit ett av de mest eftertraktade online casinona på marknaden.
En av de främsta fördelarna med Gogo casino com är det breda utbudet av spel som erbjuds. Oavsett om du gillar klassiska slots, bordsspel eller live casinospel finns det något för alla på denna plattform. Dessutom uppdateras spelbiblioteket regelbundet med de senaste och mest populära spelen på marknaden.
Förutom det imponerande spelutbudet erbjuder Gogo casino com också generösa bonusar och kampanjer för sina spelare. Nya spelare kan dra nytta av en välkomstbonus vid sin första insättning, medan befintliga spelare kan ta del av regelbundna erbjudanden och belöningar.
En annan viktig faktor som gör Gogo casino com till en attraktiv spelplattform är dess användarvänliga design och lättanvända gränssnitt. Spelare kan enkelt navigera på plattformen och hitta sina favoritspel utan problem.
Slutligen är säkerheten och integriteten hos spelarna av högsta prioritet för Gogo casino com. Plattformen använder avancerad krypteringsteknik för att säkerställa att alla transaktioner och personuppgifter förblir skyddade.
Sammanfattningsvis är Gogo casino com en utmärkt spelplattform för spelare som letar efter en spännande och säker spelupplevelse. Med sitt omfattande spelutbud, generösa bonusar och användarvänliga design har Gogo casino com blivit ett av de ledande online casinona på marknaden. Besök gogocasino.com idag för att uppleva allt vad de har att erbjuda!
https://gogocasino.one
Buy Tadalafil 5mg Cialis 20mg price in USA buy cialis pill
Подарив книгу, вы дарите возможность человеку найти ответы на свои вопросы и разрешить свои проблемы. https://rusvesna.su/aboutall/1599556550
Gogo Casino är ett populärt online casino som lockar många spelare med sitt stora utbud av spel och snabba uttag. Men tyvärr har en del spelare upplevt problem med sina uttag på senare tid.
Enligt flera rapporter från spelare har uttagen från Gogo Casino tagit längre tid än vanligt att behandlas. Vissa har fått vänta i flera dagar innan pengarna har kommit in på deras konto. Detta har självklart orsakat frustration och oro hos många spelare.
För att undersöka detta närmare har vi kontaktat Gogo Casino för en kommentar. De uppger att de har haft en ökning av antalet uttag den senaste tiden, vilket har lett till en viss fördröjning i processen. De jobbar dock aktivt med att åtgärda problemet och förväntar sig att uttagen snart kommer att behandlas som vanligt igen.
För de spelare som har drabbats av uttagsproblem hos Gogo Casino rekommenderas att kontakta deras kundtjänst för ytterligare hjälp och uppföljning av ärendet.
Sammanfattningsvis är det alltid viktigt att vara medveten om att uttagsprocessen på online casinon kan variera och att det kan uppstå problem då och då. Om du upplever några problem med ditt uttag hos Gogo Casino är det bäst att kontakta deras kundtjänst för att få hjälp och vägledning. Vi hoppas att eventuella uttagsproblem snart kommer att lösas så att alla spelare kan njuta av en smidig spelupplevelse på Gogo Casino.
https://gogocasino.one
“Gogo Casino inga insГ¤ttningar”
Att spela på casino utan att behöva göra en insättning är något som många spelare drömmer om. Med Gogo Casino no deposit erbjudande kan du nu göra detta dröm till verklighet. Gogo Casino är ett populärt online casino som erbjuder spelare ett stort utbud av spelautomater, bordsspel och live casino.
Med Gogo Casino no deposit kan du prova på casinot helt utan att behöva sätta in några egna pengar. Du får en viss summa bonuspengar att spela för och har chansen att vinna riktiga pengar utan att riskera något själv. Detta är ett perfekt sätt för nya spelare att testa på casinot och se om det är rätt plats för dem att spela på.
För att ta del av Gogo Casino no deposit erbjudande behöver du bara registrera dig som ny spelare på casinot. När du har gjort det kommer bonusen att aktiveras och du kan börja spela med dina gratispengar. Kom ihåg att läsa igenom reglerna och villkoren för bonusen så att du vet vad som krävs för att kunna ta ut eventuella vinster.
Gogo Casino är känt för att erbjuda generösa bonusar och kampanjer till sina spelare och no deposit erbjudandet är inget undantag. Passa på att prova på detta spännande casino och se om det är något för dig. Lycka till!
https://gogocasino.one
http://tadalafiliq.shop/# cheapest cialis
Книга – это дар, который может стать источником вдохновения для новых идей и проектов.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
https://github.com/ForexRobotEasy/Anchored-VWAP-with-Alert
Книга может стать незаменимым компаньоном в путешествиях или во время долгих поездок. Ведь ее можно взять с собой куда угодно и в любое время.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
http://kamagraiq.com/# buy kamagra online usa
Книга – это долговечный подарок, который сохранит свою ценность на протяжении многих лет. Ведь знания, полученные из книги, никогда не утрачивают своей актуальности.
https://www.klerk.ru/materials/2022-02-15/525164/
Читая книгу, человек учится выражать свои мысли и чувства, развивая свою литературную грамотность.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Книга – это подарок, который можно открыть снова и снова, каждый раз находя в ней что-то новое и удивительное.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
leflunomide 20mg
prayertimein.com
Книга – это не только подарок для развлечения, но и инструмент для обучения. Ведь в ней можно найти информацию по самым разным темам и областям знаний.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Книга – это источник развлечения и удовольствия, который доступен в любое время и в любом месте.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Читая книгу, человек учится терпению и выдержке, ведь нередко на пути к концу страницы сталкивается с многочисленными испытаниями и поворотами сюжета.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Сплит-система Ecoclima ECW-09QC
intel core i3-9100f @ 3.60ghz https://cpu-specs.com/
Читая книгу, человек учится терпению и выдержке, ведь нередко на пути к концу страницы сталкивается с многочисленными испытаниями и поворотами сюжета.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Сплит-система Ecoclima ECW/I-AX09/FB-4R1
Подарив книгу, вы дарите человеку ключ к новым мирам и приключениям, которые он может исследовать в своем собственном темпе.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Generic Cialis without a doctor prescription Buy Cialis online Buy Tadalafil 10mg
Книга – это подарок, который может оказать влияние на всю жизнь человека, вдохновляя на новые цели и достижения. https://rusvesna.su/aboutall/1599556550
inporno
http://tadalafiliq.com/# Generic Tadalafil 20mg price
Книга – это источник вдохновения для творческих начинаний и проектов. Ее страницы могут заполниться заметками, идеями и рисунками, став основой для новых творческих экспериментов.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Читая книгу, человек обогащает свой внутренний мир и развивает свое эмоциональное восприятие. Ведь в каждой книге есть что-то свое, что заставляет задуматься и переживать.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
http://sildenafiliq.xyz/# Viagra Tablet price
это предоставит возможность вам ощутить атмосферу подлинного игорного дома, casino x официальный сайт не выходя из дома.
Читая книгу, человек учится эмпатии и пониманию чужой точки зрения, что способствует укреплению межличностных отношений.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Даря книгу, вы не только дарите радость человеку, но и помогаете расширить его кругозор и культурный уровень.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Читая книгу, человек учится анализировать информацию и принимать обоснованные решения, развивая свою критическую мысль.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Книга может быть не только источником знаний, но и прекрасным способом расслабиться и отдохнуть после трудного дня. Ведь в ее страницах можно погрузиться в другой мир и забыть о повседневных заботах.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Книга – это не только источник информации, но и способ развития креативности и воображения. Ведь в ее страницах можно найти вдохновение для творческих начинаний.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Подарив книгу, вы дарите возможность человеку открыть для себя новые авторов и литературные жанры.
https://www.klerk.ru/materials/2022-02-15/525164/
Книга может стать источником общения и дискуссий. После ее прочтения можно обсудить с друзьями или семьей впечатления и выводы.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Cialis 20mg price in USA Generic Tadalafil 20mg price Buy Cialis online
Подарив книгу, вы дарите нечто более ценное, чем материальный объект – вы дарите время, которое человек проведет, погруженный в ее чтение.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Читая книгу, человек учится эмпатии и пониманию чужой точки зрения, расширяя свой кругозор и мировоззрение.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Турецкие сериалы для увидения турецких национальных праздников; Возможность увидеть турецкие национальные праздники турецкие сериалы про тайны будущего
this contact form
Читая книгу, человек находит ответы на свои вопросы и учится справляться с жизненными трудностями, обогащая свой жизненный опыт.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
https://kamagraiq.com/# Kamagra Oral Jelly
Generic Tadalafil 20mg price cheapest cialis Generic Tadalafil 20mg price
Читая книгу, человек расширяет свой кругозор и познает мир через глаза других людей, учась видеть вещи с разных сторон.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Читая книгу, человек учится эмпатии и пониманию чужой точки зрения, что способствует укреплению межличностных отношений. https://rusvesna.su/aboutall/1599556550
Нашел лучшие партнерские программы. Вот каталог https://partner-ki.su/partnyorskie-programmy
אחרי בחירתכם אתם מוכנים למפגש המיוחל ובמיקום מסודר. נערות ליווי בחיפה והקריות מחפש נערות ליווי מודעות אמתיות כולל תמונות. גם מגוון השירותים נבדקו תוך הקפדה על סוגי השירותים, איכות השירות, ניקיון והיגיינה על מנת שתוכלו שירותי ליווי הכוללים מגוון עיסויים נערות ליווי פרטית
http://tadalafiliq.com/# Cialis 20mg price in USA
Читая книгу, человек находит ответы на свои вопросы и учится справляться с жизненными трудностями, обогащая свой жизненный опыт.
https://www.klerk.ru/materials/2022-02-15/525164/
Подарив книгу, вы дарите возможность человеку путешествовать во времени и пространстве, погружаясь в разные эпохи и культуры. https://rusvesna.su/aboutall/1599556550
Книга – это подарок, который может оказать влияние на всю жизнь человека, вдохновляя на новые цели и достижения.
https://www.chitalnya.ru/press/1950/
Читая книгу, человек учится выражать свои мысли и чувства более точно и глубоко, развивая свои коммуникативные навыки.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Подарив книгу, вы дарите возможность человеку сбежать из реальности и окунуться в мир фантазии и мечты. https://rusvesna.su/aboutall/1599556550
Книга – это не только источник знаний, но и способ развития фантазии и творческого мышления.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Книга – это не просто подарок, это инвестиция в развитие и обогащение внутреннего мира человека.
https://www.klerk.ru/materials/2022-02-15/525164/
Jogue e ganhe com o jogo Fortune Tiger
Pin Up Casino (Пин Ап) официальный сайт онлайн казино в Казахстане. На официальном сайте казино Пин Ап можно найти большой выбор лотоматов, которые позволяют игрокам играть в онлайн режиме и зарабатывать реальные деньги пин ап казино официальный
Desfrute de um ótimo jogo Fortune Tiger
Thhis article offers clsar idea for the neww visifors of blogging, that in fact how to do blogging and site-building.
My page; 카지노사이트
Книга – это не только источник знаний, но и способ развития фантазии и творческого мышления. https://rusvesna.su/aboutall/1599556550
Всем рекомендую Букмекерскую контору 1win
Книга – это не только источник информации, но и способ развития креативности и воображения. Ведь в ее страницах можно найти вдохновение для творческих начинаний.
https://www.klerk.ru/materials/2022-02-15/525164/
Jogue e ganhe no jogo fortune Tiger
Легендарная Букмекерская контора 1win
נערות ליווי מכל צבעי הקשת בכל הגילאים והתאם לצרכים והטעם האישי שלכם. מה עליי בדיוק לעשות? כל שעליכם לעשות הוא לבחור את ודיסקרטי. ככה אפשר להביא לפנטזיות הרטובות ביותר להתגשם, לחלומות להתממש בלי לתת דין וחשבון לאף אחד מסביב. כל הדירות נמצאות במרחק שלנו – . הזמנת נערת ליווי לביתך או בית מלון
Great post.
Prestito 2 mila euro
Подарив книгу, вы дарите возможность человеку погрузиться в мир абстрактных идей и философских размышлений.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Kamagra Oral Jelly Kamagra Oral Jelly Price buy kamagra online usa
Книга – это не просто подарок, это инвестиция в развитие и обогащение внутреннего мира человека.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
https://kamagraiq.shop/# buy Kamagra
Книга – это не только источник знаний, но и способ развлечения. Ведь в ее страницах можно найти как научные факты, так и увлекательные рассказы.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
ועיסוי בתיאום מראש כמובן. נערות הליווי באשדוד יעניקו לכם מגוון שירותים מפנקים ועד שיכרון חושים. באקספיינדר תמצאו שישמחו לפנק אתכם בעיסוי מענג ופינוקים לרוב. כל שנותר לכם זה להיכנס לבחור את המתאים לכם ולהרים טלפון לתיאום. דירות דיסקרטיות בתל הדירות Meet lustful Israel escort girls and get the hottest sex
Thank you for great article. Hello Administ .国产线播放免费人成视频播放
Книга – это подарок, который может стать компаньоном на всю жизнь, оставаясь верным другом и советчиком в любой ситуации.
https://www.chitalnya.ru/press/1950/
http://tadalafiliq.com/# Cialis without a doctor prescription
Viagra online price buy viagra online buy Viagra online
Белое свадебное платье в наличии https://svadebniy-salon-moskva.ru/
Подарив книгу, вы дарите возможность человеку путешествовать во времени и пространстве, погружаясь в разные эпохи и культуры.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Книга – это подарок, который может стать компаньоном на всю жизнь, оставаясь верным другом и советчиком в любой ситуации.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Книга – это подарок, который может оказать влияние на всю жизнь человека, вдохновляя на новые цели и достижения.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Читая книгу, человек находит ответы на свои вопросы и учится справляться с жизненными трудностями, обогащая свой жизненный опыт.
https://www.chitalnya.ru/press/1950/
Даря книгу, вы дарите возможность человеку самостоятельно мыслить и анализировать информацию.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Выискиваете способ улучшить личное владение английским. Окунитесь в мир кино с нашей коллекцией фильмов на британском а также английском языках. Кинокартины на английском, особенно с британским акцентом, помогают погрузиться в языковую среду. Для лучшего понимания можно использовать субтитры на английском. Делайте лучше свой английский, блаженствуя любимыми кинофильмами. Подробнее тут https://english-films.pp.ua/
Книга – это дар, который может стать источником вдохновения для новых идей и проектов.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Подарив книгу, вы дарите возможность человеку открыть для себя новые авторов и литературные жанры.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
valtrex 500 mg without a doctor prescription
Читая книгу, человек расширяет свой кругозор и познает мир через глаза других людей, учась видеть вещи с разных сторон.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Подарив книгу, вы дарите возможность человеку путешествовать во времени и пространстве, погружаясь в разные эпохи и культуры.
https://www.chitalnya.ru/press/1950/
เมื่อเอ่ยถึงการบริการ wm ฝาก – ถอน เร็วทันใจ โอนไว 1 วินาที สำหรับทำพนันออนไลน์ ท่านชอบได้ยินผู้เล่นคนไม่ใช่น้อยต่างเอ๋ยถึง สล็อตเว็บไซต์ตรง100% ที่ย้ำการผลิตรายได้ให้กับนักพนัน พวกเราขอเสนอแนะ
เว็บไซต์ตรงไม่ผ่านเอเย่นต์ไม่มีอย่างต่ำ บาคาร่าเว็บตรง ที่มีระบบระเบียบเทคโนโลยีทันสมัย จะเป็นตัวกระตุ้นความพอใจของนักพนัน และก็นำมาซึ่งกระแสได้ดิบได้ดีเสมอ เชื้อเชิญให้มีส่วนร่วมกับการลงทุน สล็อตดัง เป็นอีกหนึ่งวิถีทางสำหรับการพนัน เกมสล็อต จากทั้งโลก
สล็อตเว็บไซต์นอก ลิขสิทธิ์แท้ เกมสล็อตแตกง่าย Evoplay สล็อต ผ่านปากทางเข้าเริ่มเล่น เว็บไซต์สล็อตแท้ คัดสรรนำเอา เกมสล็อต ทั้งผอง มีให้แด่ท่านเลือกเล่นกันอย่างครบวงจรที่เยี่ยมที่สุด นับได้ว่าเป็น สล็อต เว็บไซต์ นอก ลิขสิทธิ์แท้ เล่นง่าย ได้เงินจริง แจกเงินรางวัลกันตลอดแต่ละวัน
เข้าเล่น เกมไพ่บาคาร่าที่ Sexygaming นแบบง่ายๆไม่ยุ่งยาก สลับซับซ้อน และก็ ยังมีความพิเศษมากมายก่ายกอง สามารถเข้ามาเลือกเล่นกับทางเว็บไซต์ตรง ที่ได้รับความนิยมที่1 ของไทย
มีค่ายเกมให้เลือกเล่นกันมากมาย ค่ายบาคาร่า ต่างแดน ที่ส่งตรงจากผู้พัฒนา Ezslot มีแพลตฟอร์มถ่ายทอดสด ระบบเสถียร ไม่มีกระดอน ไม่มีสะดุด แบบออนไลน์กันตลอดระยะเวลา บันเทิงใจครบหมดทุกค่าย ข้างในที่เว็บเดียว
การแทงหวยร่ำรวยง่ายสุดๆ ไทยลอตโต้ ให้ความใส่ใจในความปลอดภัยและก็ความเป็นส่วนตัวของข้อมูลผู้เล่น ทำให้ท่านเชื่อมั่นสำหรับในการแทงหวยออนไลน์กับเว็บไซต์แห่งนี้ ระบบรักษาความปลอดภัยระดับสูงจะดูแลข้อมูลของคุณอย่างเคร่งครัด
Читая книгу, человек учится эмпатии и пониманию чужой точки зрения, расширяя свой кругозор и мировоззрение.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Trustbet เป็นคาสิโนออนไลน์ที่มีชื่อเสียงและเป็นที่รู้จักของผู้เล่นไทย มีความมั่นคงทางการเงินและน่าเชื่อถือมากที่สุด
Nakee เว็บหวยมาแรงอันดับ 1 ที่ได้รับความที่สุดในปี 2024 เว็บหวยจ่ายบาทสูง แทงได้ไม่อั้นไม่จำกัดรอบบิล
Подарив книгу, вы дарите возможность человеку путешествовать во времени и пространстве, погружаясь в исторические эпохи, фантастические миры или психологические глубины человеческой души.
https://www.chitalnya.ru/press/1950/
Рекомендую Букмекерскую контору 1win
Лучшая Букмекерская контора 1win
Подарив книгу, вы дарите не только объект, но и возможность для саморазвития и роста личности.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
best india pharmacy Generic Medicine India to USA india pharmacy mail order
לחיצה על מספר הטלפון במודעה ואתם כבר מקושרים ישיר למקום. מומלץ בשלב הזה לברר שהותכם ולגרום לכם להנאה ולבילוי מושלם. כשתיכנסו לאתר אקספיינדר בקטגוריה של דירות דיסקרטיות לפי ערים, תוכלו להתרשם מהמגוון העשיר מהאנשים האהובים עליך. שנית, הדירות מאובזרות בכל נערות ליווי בנתניה
Embark on an exciting water adventure with our portal, where you can rent marine luxury in addition to charter watercraft and more. Browse thousands of listings from boat owners providing an array of vessels, including yachts, water vehicles, sailboats, water scooters and more. Whether you seek a high-end yacht for VIPs, a fishing vessel for a day on the water, or a celebration vessel, our portal can assist you in finding the right selection. With the possibility to hire a yacht with or without a skipper, you can discover the suitable one in accordance with your desires. https://boatrent.shop/ Feel the pinnacle of luxury with our premium yacht charter or opt for an cost-effective but enjoyable outing with our cheap yacht booking. Regardless of your decision, our portal guarantees hassle-free booking process, exceptional service, and memorable memories on the water. Start your adventure today and uncover the thrill of renting yachts and boats with us.
Книга – это не только источник знаний, но и способ развития фантазии и творческого мышления.
https://www.klerk.ru/materials/2022-02-15/525164/
mexico pharmacies prescription drugs Mexico drugstore mexico drug stores pharmacies
элитный эскорт москва
Подарив книгу, вы дарите возможность человеку погрузиться в мир абстрактных идей и философских размышлений.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Элитный эскорт Москва
Va e ganhe com o jogo fortune Tiger
вип эскорт Москва
Thank you for great content. Hello Administ. Seo Hizmeti Skype : live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.儿童色情
proscar 500mg
טלפונים וניווט שיביא היפות ביותר. שיהיה בהצלחה ובילוי נעים, פה בשבילכם, צוות האתר, . עיסוי ארוטי בצפון כל ישראלי שמגיע לצפון ישר מדמיין ירוק בעיניים, ודיסקרטית הרחק מהחברים והמשפחה, מומלץ להנות מהשכרה של דירות דיסקרטיות ברעננה. הדירות הדיסקרטיות ברעננה איתור שירותי ליווי אילת בהתאמה אישית
top online pharmacy india indian pharmacy delivery online shopping pharmacy india
ביותר בישראל מציע מספר רחב מאוד של אפשרויות חיפוש מהגבוהות ביותר שיש בשוק אצלנו באתר כל המודעות דיסקרטיות ברעננה-כפר סבא? מעוניינים למצוא דירה דיסקרטית בכפר סבא? פה תוכל למצוא מענה לחיפושים שלכם דמיינו לעצמכם דירה דיסקרטית המודעות ברמה שעתית שאין בה דירה דיסקרטי
של דירות סקס באילת והסביבה כולל כתובות, טלפונים וניווט שיביא אתכם היישר לעונג. דירה דיסקרטית באילת מאז ומתמיד נחשבה עיר הנופש מבחר הנערות ליווי בחולון – בת-ים ומציג לכם מבחר המתעדכן באופן שוטף על בסיס יומי. מה הדגש שאתם שמים בבחירת מודעות בפורטל חלומית. The best private escort Tel Aviv girls
buying prescription drugs in mexico online Pills from Mexican Pharmacy medicine in mexico pharmacies
Я тут покупала себе свадебное платье https://svadebniy-salon-moskva.ru/
Топовая Букмекерская контора 1win
Крутая Букмекерская контора 1win
Что такое M-пакет
10. BMW: особенности технического обслуживания
bmw x5 m50 x4 bmw .
Ищете способ улучшить личное владение английским. Погрузитесь в мир кино с нашей коллекцией фильмов на английском а также британском языках. Кинофильмы на английском, особенно с британским акцентом, помогают окунуться в языковую среду. Для лучшего понимания можно использовать субтитры на английском. Улучшайте свой английский, наслаждаясь любимыми фильмами. Подробнее здесь https://english-films.pp.ua/
canadian pharmacy meds Cheapest drug prices Canada best canadian pharmacy online
Топ Букмекерская контора 1win
Самая надежная Букмекерская контора 1win
Divirta-se com o jogo Fortune Tiger
Lucro ao jogar o jogo Fortune Tiger
Ganhe dinheiro de verdade jogando o jogo Fortune Tiger
Подробный обзор
17. BMW: как выбрать идеальный двигатель для своего автомобиля
bmw i5 bmw x5 2023 .
best india pharmacy top 10 pharmacies in india world pharmacy india
דיסקרטיות באשדוד אשקלון? מעוניינים למצוא דירה דיסקרטית בדרום? רוצים הכוונה מדוייקת לדירה דיסקרטית שלכם. כל היום כל השנה – אילת העיר החמה והמבוקשת ביותר בישראל ובעולם עיר אליה כולם רוצים להגיע ליהנות מהשמש מהחום היבש והנעים ללא אחד נמצא זמן מסוים לפי אתיופית ליווי
Типы моторов
18. BMW: тюнинг и модификации для улучшения характеристик
bmw x1 2022 bmw x5 2022 .
Отзывы владельцев
2. Почему BMW – лучший выбор для автолюбителей
bmw x 5 bmw mx5 .
collegato qui
porno
KANTORBOLA situs gamin online terbaik 2024 yang menyediakan beragam permainan judi online easy to win , mulai dari permainan slot online , taruhan judi bola , taruhan live casino , dan toto macau . Dapatkan promo terbaru kantor bola , bonus deposit harian , bonus deposit new member , dan bonus mingguan . Kunjungi link kantorbola untuk melakukan pendaftaran .
Nice article inspiring thanks. Hello Administ . Seo Hizmeti Skype : live:by_umut
Good info. Lucky me I reach on your website by accident, I bookmarked it. Seo Hizmeti Skype : live:by_umut
Thank you for great article. Hello Administ .Seo Hizmeti Skype : live:by_umut
mexican pharmacy mexican pharmacy buying prescription drugs in mexico online
Надежная Букмекерская контора 1win
Советую лучшую Букмекерскую контору 1win
Everything is very open and very clear explanation of issues. was truly information. Seo Hizmeti Skype : live:by_umut
Apartments, a penthouse and a duplex in the brand new development of AVA Omniyat. Developer OMNIYAT offers units for sale at favourable prices.
עדינות, בלונדיניות ושחורות המציעות אירוח דיסקרטי באשקלון ובאשדוד. כל שתצטרכו לעשות זה רק להגיע ולבחור ומה אחד ואחת מכם. דירות דיסקרטיות ברחובות נס ציונה רוצים פרטים על דירות דיסקרטיות ברחובות-נס ציונה? מעוניינים למצוא דירה דיסקרטית דירות דיסקרטיות מכוני ליווי בצפון – כמו בסרט כחול
It’s remarkable to pay a quick visit this site and reading
the views of all mates on the topic of thhis paragraph,
while I am also keen of getting knowledge.
Here iss my webpage; 카지노사이트
Советую лучшую в своем роде Букмекерскую контору 1win
Криптовалютные биржи — это платформы, которые дают возможность трейдерам покупать и продавать криптовалюты, деривативы и другие криптоактивы лучшие биржи криптовалют +для россии
один из главных видов металлопроката – алюминиевый, поскольку алюминий обладает легкостью, прочностью и отличной коррозионной.
Look at my web blog :: http://animeworld.ruhelp.com/viewtopic.php?id=9827
Надежная Букмекерская контора №1 1win
Discover a world of creativity and imagination at DigitalMagicUA on Etsy: https://www.etsy.com/shop/DigitalMagicUA ! Dive into a magical coloring adventure at DigitalMagicUA. Don’t miss out on the joy of bringing these pages to life!
legitimate canadian pharmacy online Pharmacies in Canada that ship to the US canadian pharmacies compare
Informasi RTP Live Hari Ini Dari Situs RTPKANTORBOLA
Situs RTPKANTORBOLA merupakan salah satu situs yang menyediakan informasi lengkap mengenai RTP (Return to Player) live hari ini. RTP sendiri adalah persentase rata-rata kemenangan yang akan diterima oleh pemain dari total taruhan yang dimainkan pada suatu permainan slot . Dengan adanya informasi RTP live, para pemain dapat mengukur peluang mereka untuk memenangkan suatu permainan dan membuat keputusan yang lebih cerdas saat bermain.
Situs RTPKANTORBOLA menyediakan informasi RTP live dari berbagai permainan provider slot terkemuka seperti Pragmatic Play , PG Soft , Habanero , IDN Slot , No Limit City dan masih banyak rtp permainan slot yang bisa kami cek di situs RTP Kantorboal . Dengan menyediakan informasi yang akurat dan terpercaya, situs ini menjadi sumber informasi yang penting bagi para pemain judi slot online di Indonesia .
Salah satu keunggulan dari situs RTPKANTORBOLA adalah penyajian informasi yang terupdate secara real-time. Para pemain dapat memantau perubahan RTP setiap saat dan membuat keputusan yang tepat dalam bermain. Selain itu, situs ini juga menyediakan informasi mengenai RTP dari berbagai provider permainan, sehingga para pemain dapat membandingkan dan memilih permainan dengan RTP tertinggi.
Informasi RTP live yang disediakan oleh situs RTPKANTORBOLA juga sangat lengkap dan mendetail. Para pemain dapat melihat RTP dari setiap permainan, baik itu dari aspek permainan itu sendiri maupun dari provider yang menyediakannya. Hal ini sangat membantu para pemain dalam memilih permainan yang sesuai dengan preferensi dan gaya bermain mereka.
Selain itu, situs ini juga menyediakan informasi mengenai RTP live dari berbagai provider judi slot online terpercaya. Dengan begitu, para pemain dapat memilih permainan slot yang memberikan RTP terbaik dan lebih aman dalam bermain. Informasi ini juga membantu para pemain untuk menghindari potensi kerugian dengan bermain pada game slot online dengan RTP rendah .
Situs RTPKANTORBOLA juga memberikan pola dan ulasan mengenai permainan-permainan dengan RTP tertinggi. Para pemain dapat mempelajari strategi dan tips dari para ahli untuk meningkatkan peluang dalam memenangkan permainan. Analisis dan ulasan ini disajikan secara jelas dan mudah dipahami, sehingga dapat diaplikasikan dengan baik oleh para pemain.
Informasi RTP live yang disediakan oleh situs RTPKANTORBOLA juga dapat membantu para pemain dalam mengelola keuangan mereka. Dengan mengetahui RTP dari masing-masing permainan slot , para pemain dapat mengatur taruhan mereka dengan lebih bijak. Hal ini dapat membantu para pemain untuk mengurangi risiko kerugian dan meningkatkan peluang untuk mendapatkan kemenangan yang lebih besar.
Untuk mengakses informasi RTP live dari situs RTPKANTORBOLA, para pemain tidak perlu mendaftar atau membayar biaya apapun. Situs ini dapat diakses secara gratis dan tersedia untuk semua pemain judi online. Dengan begitu, semua orang dapat memanfaatkan informasi yang disediakan oleh situs RTP Kantorbola untuk meningkatkan pengalaman dan peluang mereka dalam bermain judi online.
Demikianlah informasi mengenai RTP live hari ini dari situs RTPKANTORBOLA. Dengan menyediakan informasi yang akurat, terpercaya, dan lengkap, situs ini menjadi sumber informasi yang penting bagi para pemain judi online. Dengan memanfaatkan informasi yang disediakan, para pemain dapat membuat keputusan yang lebih cerdas dan meningkatkan peluang mereka untuk memenangkan permainan. Selamat bermain dan semoga sukses!
Hi there, I enjoy reading through your post. I wanted to write
a little comment to support you.
Feel free to surf to my web blog: 카지노사이트
Советую лучшую Букмекерскую контору 1win
Надежная Букмекерская контора №1 в мире 1win
וזה מה שיוצר עבורכם את הנוחות והחשק לחזור לדירות פעם אחר פעם. היכנסו עוד הים לפורטל דיסקרטיות במודיעין? מעוניינים למצוא דירה דיסקרטית במודיעין? פה תוכל למצוא מענה לחיפושים שלכם דמיינו לעצמכם דירה דיסקרטית מעוצבת ומושקעת, עם מספר בחורות חטובות ויפות,שכל סקס דירה
india online pharmacy Healthcare and medicines from India india pharmacy mail order
Лучшие проститутки Москвы
Дешевое такси Киев
Купить качественные крауд ссылки
Обзор новинок
12. BMW: высокий уровень безопасности и комфорта
bmw i 7 bmw 2023 .
дешевые проститутки москвы
Купить крауд ссылки не дорого
Известный во всем СНГ телеграмм бот Глаз Бога уже почти год не сходит с первых полос множества новостных агентств. Программа Глаз Бога для поиска людей завоевала огромную популярность у многих пользователей глаз бога программа
canadian family pharmacy canadian pharmacy canadian drugs online
greenhousebali.com
PЕЇjДЌka 200000 KДЌ
Советую выбрать лучшую Букмекерскую контору 1win
Самая надежная Букмекерская контора №1 в мире 1win
гостиницы москвы недорого https://otelivmoskva.ru/oteli-i-gostinicy-v-moskve/
אביב אחד המפגשים אשר מגשימים לגברים חלומות ופנטזיות שאותם הוא לא יצליח לעשות עם בת זוגו, הוא בקפידה רבה על מנת להנעים לשוהה בהן את השהות במקום ולהנות מחוויה רומנטית ומענגת. הדירות הדיסקרטיות בנתניה מאובזרות בכל טוב. פינת באשדוד מושכרת לזוגות, יחידים ואף נערות ליווי זולות
best canadian pharmacy Canada pharmacy thecanadianpharmacy
Venha e receba seus ganhos no jogo Fortune Tiger
Ganhe grandes prêmios no jogo Fortune Tiger
mexico drug stores pharmacies mexican pharmacy п»їbest mexican online pharmacies
abilify 15 mg canada
When someone writes an piece of writing he/she retains the thought of
a user in his/her brain that how a user can know it.
So that’s why this paragraph is outstdanding.
Thanks!
My blog … sbc intake manifold
играть в mostbet казино, это просто.
Look into my web page – https://mosttbetfanx4.xyz/
365pronxxx.top
11000 Euro Kredit
mostbet обеспечивает грандиозное количество вариантов для этого: кредитные карты,
электронные кошельки, mostbet зеркало виртуальной валюты и.
my blog :: https://mosttbeet38.xyz/
Выбираем лучшую Букмекерскую контору 1win
Kantorbola Situs slot Terbaik, Modal 10 Ribu Menang Puluhan Juta
Kantorbola merupakan salah satu situs judi online terbaik yang saat ini sedang populer di kalangan pecinta taruhan bola , judi live casino dan judi slot online . Dengan modal awal hanya 10 ribu rupiah, Anda memiliki kesempatan untuk memenangkan puluhan juta rupiah bahkan ratusan juta rupiah dengan bermain judi online di situs kantorbola . Situs ini menawarkan berbagai jenis taruhan judi , seperti judi bola , judi live casino , judi slot online , judi togel , judi tembak ikan , dan judi poker uang asli yang menarik dan menguntungkan. Selain itu, Kantorbola juga dikenal sebagai situs judi online terbaik yang memberikan pelayanan terbaik kepada para membernya.
Keunggulan Kantorbola sebagai Situs slot Terbaik
Kantorbola memiliki berbagai keunggulan yang membuatnya menjadi situs slot terbaik di Indonesia. Salah satunya adalah tampilan situs yang menarik dan mudah digunakan, sehingga para pemain tidak akan mengalami kesulitan ketika melakukan taruhan. Selain itu, Kantorbola juga menyediakan berbagai bonus dan promo menarik yang dapat meningkatkan peluang kemenangan para pemain. Dengan sistem keamanan yang terjamin, para pemain tidak perlu khawatir akan kebocoran data pribadi mereka.
Modal 10 Ribu Bisa Menang Puluhan Juta di Kantorbola
Salah satu daya tarik utama Kantorbola adalah kemudahan dalam memulai taruhan dengan modal yang terjangkau. Dengan hanya 10 ribu rupiah, para pemain sudah bisa memasang taruhan dan berpeluang untuk memenangkan puluhan juta rupiah. Hal ini tentu menjadi kesempatan yang sangat menarik bagi para penggemar taruhan judi online di Indonesia . Selain itu, Kantorbola juga menyediakan berbagai jenis taruhan yang bisa dipilih sesuai dengan keahlian dan strategi masing-masing pemain.
Berbagai Jenis Permainan Taruhan Bola yang Menarik
Kantorbola menyediakan berbagai jenis permainan taruhan bola yang menarik dan menguntungkan bagi para pemain. Mulai dari taruhan Mix Parlay, Handicap, Over/Under, hingga Correct Score, semua jenis taruhan tersebut bisa dinikmati di situs ini. Para pemain dapat memilih jenis taruhan yang paling sesuai dengan pengetahuan dan strategi taruhan mereka. Dengan peluang kemenangan yang besar, para pemain memiliki kesempatan untuk meraih keuntungan yang fantastis di Kantorbola.
Pelayanan Terbaik untuk Kepuasan Para Member
Selain menyediakan berbagai jenis permainan taruhan bola yang menarik, Kantorbola juga memberikan pelayanan terbaik untuk kepuasan para membernya. Tim customer service yang profesional siap membantu para pemain dalam menyelesaikan berbagai masalah yang mereka hadapi. Selain itu, proses deposit dan withdraw di Kantorbola juga sangat cepat dan mudah, sehingga para pemain tidak akan mengalami kesulitan dalam melakukan transaksi. Dengan pelayanan yang ramah dan responsif, Kantorbola selalu menjadi pilihan utama para penggemar taruhan bola.
Kesimpulan
Kantorbola merupakan situs slot terbaik yang menawarkan berbagai jenis permainan taruhan bola yang menarik dan menguntungkan. Dengan modal awal hanya 10 ribu rupiah, para pemain memiliki kesempatan untuk memenangkan puluhan juta rupiah. Keunggulan Kantorbola sebagai situs slot terbaik antara lain tampilan situs yang menarik, berbagai bonus dan promo menarik, serta sistem keamanan yang terjamin. Dengan berbagai jenis permainan taruhan bola yang ditawarkan, para pemain memiliki banyak pilihan untuk meningkatkan peluang kemenangan mereka. Dengan pelayanan terbaik untuk kepuasan para member, Kantorbola selalu menjadi pilihan utama para penggemar taruhan bola.
FAQ (Frequently Asked Questions)
Berapa modal minimal untuk bermain di Kantorbola? Modal minimal untuk bermain di Kantorbola adalah 10 ribu rupiah.
Bagaimana cara melakukan deposit di Kantorbola? Anda dapat melakukan deposit di Kantorbola melalui transfer bank atau dompet digital yang telah disediakan.
Apakah Kantorbola menyediakan bonus untuk new member? Ya, Kantorbola menyediakan berbagai bonus untuk new member, seperti bonus deposit dan bonus cashback.
Apakah Kantorbola aman digunakan untuk bermain taruhan bola online? Kantorbola memiliki sistem keamanan yang terjamin dan data pribadi para pemain akan dijaga kerahasiaannya dengan baik.
Топовая Букмекерская контора №1 1win
indian pharmacy mail order pharmacy india india pharmacy mail order
Почему наши тоговые сигналы – всегда идеальный путь:
Наша группа утром и вечером, днём и ночью на волне актуальных трендов и моментов, которые влияют на криптовалюты. Это дает возможность группе быстро реагировать и предоставлять свежие подачи.
Наш коллектив имеет предельным знанием анализа по графику и умеет выделить крепкие и уязвимые аспекты для входа в сделку. Это способствует уменьшению рисков и увеличению прибыли.
Мы же внедряем личные боты для анализа данных для просмотра графиков на все интервалах. Это содействует нам завоевать полную картину рынка.
Перед приведением подача в нашем Telegram мы осуществляем детальную проверку всех аспектов и подтверждаем возможное длинный или краткий. Это обеспечивает предсказуемость и качественность наших подач.
Присоединяйтесь к нам к нашей группе прямо сейчас и достаньте доступ к проверенным торговым подачам, которые помогут вам вам получить финансового успеха на рынке криптовалют!
https://t.me/Investsany_bot
Discover luxurious apartments, penthouses, and duplex apartments for sale at Como Residence the Palm. Embrace the epitome of elegance and prestige with stunning offerings from Nakheel at irresistible prices. Hurry, secure your dream home today!
india pharmacy mail order Generic Medicine India to USA top 10 pharmacies in india
Выбираем топовую Букмекерскую контору 1win
cymbalta 60 mg tablet
Крутая Букмекерская контора №1 1win
Книга может быть не только источником знаний, но и прекрасным способом расслабиться и отдохнуть после трудного дня. Ведь в ее страницах можно погрузиться в другой мир и забыть о повседневных заботах. https://rusvesna.su/aboutall/1599556550
отели москва на карте с ценами https://otelivmoskva.ru/oteli-i-gostinicy-v-moskve/
Книга может быть не только источником знаний, но и прекрасным способом расслабиться и отдохнуть после трудного дня. Ведь в ее страницах можно погрузиться в другой мир и забыть о повседневных заботах.
https://www.klerk.ru/materials/2022-02-15/525164/
купить плинтус алюминиевый плинтус цена .
Читая книгу, человек учится выражать свои мысли и чувства более точно и глубоко, развивая свои коммуникативные навыки.
https://www.chitalnya.ru/press/1950/
Книга – это дар, который может стать источником вдохновения для новых идей и проектов.
https://www.klerk.ru/materials/2022-02-15/525164/
дюбели для бетона
плинтус алюминиевый кабель цена .
Mengenal Situs Gaming Online Terbaik Kantorbola
Kantorbola merupakan situs gaming online terbaik yang menawarkan pengalaman bermain yang seru dan mengasyikkan bagi para pecinta game. Dengan berbagai pilihan game menarik dan grafis yang memukau, Kantorbola menjadi pilihan utama bagi para gamers yang ingin mencari hiburan dan tantangan baru. Dengan layanan customer service yang ramah dan profesional, serta sistem keamanan yang terjamin, Kantorbola siap memberikan pengalaman bermain yang terbaik dan menyenangkan bagi semua membernya. Jadi, tunggu apalagi? Bergabunglah sekarang dan rasakan sensasi seru bermain game di Kantorbola!
Situs kantor bola menyediakan beberapa link alternatif terbaru
Situs kantor bola merupakan salah satu situs gaming online terbaik yang menyediakan berbagai link alternatif terbaru untuk memudahkan para pengguna dalam mengakses situs tersebut. Dengan adanya link alternatif terbaru ini, para pengguna dapat tetap mengakses situs kantor bola meskipun terjadi pemblokiran dari pemerintah atau internet positif. Hal ini tentu menjadi kabar baik bagi para pecinta judi online yang ingin tetap bermain tanpa kendala akses ke situs kantor bola.
Dengan menyediakan beberapa link alternatif terbaru, situs kantor bola juga dapat memberikan variasi akses kepada para pengguna. Hal ini memungkinkan para pengguna untuk memilih link alternatif mana yang paling cepat dan stabil dalam mengakses situs tersebut. Dengan demikian, pengalaman bermain judi online di situs kantor bola akan menjadi lebih lancar dan menyenangkan.
Selain itu, situs kantor bola juga menunjukkan komitmennya dalam memberikan pelayanan terbaik kepada para pengguna dengan menyediakan link alternatif terbaru secara berkala. Dengan begitu, para pengguna tidak perlu khawatir akan kehilangan akses ke situs kantor bola karena selalu ada link alternatif terbaru yang dapat digunakan sebagai backup. Keberadaan link alternatif tersebut juga menunjukkan bahwa situs kantor bola selalu berusaha untuk tetap eksis dan dapat diakses oleh para pengguna setianya.
Secara keseluruhan, kehadiran beberapa link alternatif terbaru dari situs kantor bola merupakan salah satu bentuk komitmen dari situs tersebut dalam memberikan kemudahan dan kenyamanan kepada para pengguna. Dengan adanya link alternatif tersebut, para pengguna dapat terus mengakses situs kantor bola tanpa hambatan apapun. Hal ini tentu akan semakin meningkatkan popularitas situs kantor bola sebagai salah satu situs gaming online terbaik di Indonesia. Berikut beberapa link alternatif dari situs kantorbola , diantaranya .
1. Link Kantorbola77
Link Kantorbola77 merupakan salah satu situs gaming online terbaik yang saat ini banyak diminati oleh para pecinta judi online. Dengan berbagai pilihan permainan yang lengkap dan berkualitas, situs ini mampu memberikan pengalaman bermain yang memuaskan bagi para membernya. Selain itu, Kantorbola77 juga menawarkan berbagai bonus dan promo menarik yang dapat meningkatkan peluang kemenangan para pemain.
Salah satu keunggulan dari Link Kantorbola77 adalah sistem keamanan yang sangat terjamin. Dengan teknologi enkripsi yang canggih, situs ini menjaga data pribadi dan transaksi keuangan para membernya dengan sangat baik. Hal ini membuat para pemain merasa aman dan nyaman saat bermain di Kantorbola77 tanpa perlu khawatir akan adanya kebocoran data atau tindakan kecurangan yang merugikan.
Selain itu, Link Kantorbola77 juga menyediakan layanan pelanggan yang siap membantu para pemain 24 jam non-stop. Tim customer service yang profesional dan responsif siap membantu para member dalam menyelesaikan berbagai kendala atau pertanyaan yang mereka hadapi saat bermain. Dengan layanan yang ramah dan efisien, Kantorbola77 menempatkan kepuasan para pemain sebagai prioritas utama mereka.
Dengan reputasi yang baik dan pengalaman yang telah teruji, Link Kantorbola77 layak untuk menjadi pilihan utama bagi para pecinta judi online. Dengan berbagai keunggulan yang dimilikinya, situs ini memberikan pengalaman bermain yang memuaskan dan menguntungkan bagi para membernya. Jadi, jangan ragu untuk bergabung dan mencoba keberuntungan Anda di Kantorbola77.
2. Link Kantorbola88
Link kantorbola88 adalah salah satu situs gaming online terbaik yang harus dikenal oleh para pecinta judi online. Dengan menyediakan berbagai jenis permainan seperti judi bola, casino, slot online, poker, dan banyak lagi, kantorbola88 menjadi pilihan utama bagi para pemain yang ingin mencoba keberuntungan mereka. Link ini memberikan akses mudah dan cepat untuk para pemain yang ingin bermain tanpa harus repot mencari situs judi online yang terpercaya.
Selain itu, kantorbola88 juga dikenal sebagai situs yang memiliki reputasi baik dalam hal pelayanan dan keamanan. Dengan sistem keamanan yang canggih dan profesional, para pemain dapat bermain tanpa perlu khawatir akan kebocoran data pribadi atau transaksi keuangan mereka. Selain itu, layanan pelanggan yang ramah dan responsif juga membuat pengalaman bermain di kantorbola88 menjadi lebih menyenangkan dan nyaman.
Selain itu, link kantorbola88 juga menawarkan berbagai bonus dan promosi menarik yang dapat dinikmati oleh para pemain. Mulai dari bonus deposit, cashback, hingga bonus referral, semua memberikan kesempatan bagi pemain untuk mendapatkan keuntungan lebih saat bermain di situs ini. Dengan adanya bonus-bonus tersebut, kantorbola88 terus berusaha memberikan yang terbaik bagi para pemainnya agar selalu merasa puas dan senang bermain di situs ini.
Dengan reputasi yang baik, pelayanan yang prima, keamanan yang terjamin, dan bonus yang menggiurkan, link kantorbola88 adalah pilihan yang tepat bagi para pemain judi online yang ingin merasakan pengalaman bermain yang seru dan menguntungkan. Dengan bergabung di situs ini, para pemain dapat merasakan sensasi bermain judi online yang berkualitas dan terpercaya, serta memiliki peluang untuk mendapatkan keuntungan besar. Jadi, jangan ragu untuk mencoba keberuntungan Anda di kantorbola88 dan nikmati pengalaman bermain yang tak terlupakan.
3. Link Kantorbola88
Kantorbola99 merupakan salah satu situs gaming online terbaik yang dapat menjadi pilihan bagi para pecinta judi online. Situs ini menawarkan berbagai permainan menarik seperti judi bola, casino online, slot online, poker, dan masih banyak lagi. Dengan berbagai pilihan permainan yang disediakan, para pemain dapat menikmati pengalaman berjudi yang seru dan mengasyikkan.
Salah satu keunggulan dari Kantorbola99 adalah sistem keamanan yang sangat terjamin. Situs ini menggunakan teknologi enkripsi terbaru untuk melindungi data pribadi dan transaksi keuangan para pemain. Dengan demikian, para pemain bisa bermain dengan tenang tanpa perlu khawatir tentang kebocoran data pribadi atau kecurangan dalam permainan.
Selain itu, Kantorbola99 juga menawarkan berbagai bonus dan promo menarik bagi para pemain setianya. Mulai dari bonus deposit, bonus cashback, hingga bonus referral yang dapat meningkatkan peluang para pemain untuk meraih kemenangan. Dengan adanya bonus dan promo ini, para pemain dapat merasa lebih diuntungkan dan semakin termotivasi untuk bermain di situs ini.
Dengan reputasi yang baik dan pengalaman yang telah terbukti, Kantorbola99 menjadi pilihan yang tepat bagi para pecinta judi online. Dengan pelayanan yang ramah dan responsif, para pemain juga dapat mendapatkan bantuan dan dukungan kapan pun dibutuhkan. Jadi, tidak heran jika Kantorbola99 menjadi salah satu situs gaming online terbaik yang banyak direkomendasikan oleh para pemain judi online.
Promo Terbaik Dari Situs kantorbola
Kantorbola merupakan salah satu situs gaming online terbaik yang menyediakan berbagai jenis permainan menarik seperti judi bola, casino, poker, slots, dan masih banyak lagi. Situs ini telah menjadi pilihan utama bagi para pecinta judi online karena reputasinya yang terpercaya dan kualitas layanannya yang prima. Selain itu, Kantorbola juga seringkali memberikan promo-promo menarik kepada para membernya, salah satunya adalah promo terbaik yang dapat meningkatkan peluang kemenangan para pemain.
Promo terbaik dari situs Kantorbola biasanya berupa bonus deposit, cashback, maupun event-event menarik yang diadakan secara berkala. Dengan adanya promo-promo ini, para pemain memiliki kesempatan untuk mendapatkan keuntungan lebih besar dan juga kesempatan untuk memenangkan hadiah-hadiah menarik. Selain itu, promo-promo ini juga menjadi daya tarik bagi para pemain baru yang ingin mencoba bermain di situs Kantorbola.
Salah satu promo terbaik dari situs Kantorbola yang paling diminati adalah bonus deposit new member sebesar 100%. Dengan bonus ini, para pemain baru bisa mendapatkan tambahan saldo sebesar 100% dari jumlah deposit yang mereka lakukan. Hal ini tentu saja menjadi kesempatan emas bagi para pemain untuk bisa bermain lebih lama dan meningkatkan peluang kemenangan mereka. Selain itu, Kantorbola juga selalu memberikan promo-promo menarik lainnya yang dapat dinikmati oleh semua membernya.
Dengan berbagai promo terbaik yang ditawarkan oleh situs Kantorbola, para pemain memiliki banyak kesempatan untuk meraih kemenangan besar dan mendapatkan pengalaman bermain judi online yang lebih menyenangkan. Jadi, jangan ragu untuk bergabung dan mencoba keberuntungan Anda di situs gaming online terbaik ini. Dapatkan promo-promo menarik dan nikmati berbagai jenis permainan seru hanya di Kantorbola.
Deposit Kilat Di Kantorbola Melalui QRIS
Deposit kilat di Kantorbola melalui QRIS merupakan salah satu fitur yang mempermudah para pemain judi online untuk melakukan transaksi secara cepat dan aman. Dengan menggunakan QRIS, para pemain dapat melakukan deposit dengan mudah tanpa perlu repot mencari nomor rekening atau melakukan transfer manual.
QRIS sendiri merupakan sistem pembayaran digital yang memanfaatkan kode QR untuk memfasilitasi transaksi pembayaran. Dengan menggunakan QRIS, para pemain judi online dapat melakukan deposit hanya dengan melakukan pemindaian kode QR yang tersedia di situs Kantorbola. Proses deposit pun dapat dilakukan dalam waktu yang sangat singkat, sehingga para pemain tidak perlu menunggu lama untuk bisa mulai bermain.
Keunggulan deposit kilat di Kantorbola melalui QRIS adalah kemudahan dan kecepatan transaksi yang ditawarkan. Para pemain judi online tidak perlu lagi repot mencari nomor rekening atau melakukan transfer manual yang memakan waktu. Cukup dengan melakukan pemindaian kode QR, deposit dapat langsung terproses dan saldo akun pemain pun akan langsung bertambah.
Dengan adanya fitur deposit kilat di Kantorbola melalui QRIS, para pemain judi online dapat lebih fokus pada permainan tanpa harus terganggu dengan urusan transaksi. QRIS memungkinkan para pemain untuk melakukan deposit kapan pun dan di mana pun dengan mudah, sehingga pengalaman bermain judi online di Kantorbola menjadi lebih menyenangkan dan praktis.
Dari ulasan mengenai mengenal situs gaming online terbaik Kantorbola, dapat disimpulkan bahwa situs tersebut menawarkan berbagai jenis permainan yang menarik dan populer di kalangan para penggemar game. Dengan tampilan yang menarik dan user-friendly, Kantorbola memberikan pengalaman bermain yang menyenangkan dan memuaskan bagi para pemain. Selain itu, keamanan dan keamanan privasi pengguna juga menjadi prioritas utama dalam situs tersebut sehingga para pemain dapat bermain dengan tenang tanpa perlu khawatir akan data pribadi mereka.
Selain itu, Kantorbola juga memberikan berbagai bonus dan promo menarik bagi para pemain, seperti bonus deposit dan cashback yang dapat meningkatkan keuntungan bermain. Dengan pelayanan customer service yang responsif dan profesional, para pemain juga dapat mendapatkan bantuan yang dibutuhkan dengan cepat dan mudah. Dengan reputasi yang baik dan banyaknya testimonial positif dari para pemain, Kantorbola menjadi pilihan situs gaming online terbaik bagi para pecinta game di Indonesia.
Frequently Asked Question ( FAQ )
A : Apa yang dimaksud dengan Situs Gaming Online Terbaik Kantorbola?
Q : Situs Gaming Online Terbaik Kantorbola adalah platform online yang menyediakan berbagai jenis permainan game yang berkualitas dan menarik untuk dimainkan.
A : Apa saja jenis permainan yang tersedia di Situs Gaming Online Terbaik Kantorbola?
Q : Di Situs Gaming Online Terbaik Kantorbola, anda dapat menemukan berbagai jenis permainan seperti game slot, poker, roulette, blackjack, dan masih banyak lagi.
A : Bagaimana cara mendaftar di Situs Gaming Online Terbaik Kantorbola?
Q : Untuk mendaftar di Situs Gaming Online Terbaik Kantorbola, anda hanya perlu mengakses situs resmi mereka, mengklik tombol “Daftar” dan mengisi formulir pendaftaran yang disediakan.
A : Apakah Situs Gaming Online Terbaik Kantorbola aman digunakan untuk bermain game?
Q : Ya, Situs Gaming Online Terbaik Kantorbola telah memastikan keamanan dan kerahasiaan data para penggunanya dengan menggunakan sistem keamanan terkini.
A : Apakah ada bonus atau promo menarik yang ditawarkan oleh Situs Gaming Online Terbaik Kantorbola?
Q : Tentu saja, Situs Gaming Online Terbaik Kantorbola seringkali menawarkan berbagai bonus dan promo menarik seperti bonus deposit, cashback, dan bonus referral untuk para membernya. Jadi pastikan untuk selalu memeriksa promosi yang sedang berlangsung di situs mereka.
Читая книгу, человек находит ответы на свои вопросы и учится справляться с жизненными трудностями, обогащая свой жизненный опыт.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
canada rx pharmacy world Certified Canadian pharmacies online canadian pharmacy
zyvox
плинтус алюминиевый для пола плинтус алюминиевый цена .
плинтус из алюминия плинтус пола .
Книга – это не просто подарок, это инвестиция в развитие и обогащение внутреннего мира человека.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
safe canadian pharmacy Pharmacies in Canada that ship to the US canadian pharmacy victoza
Книга – это не только источник знаний, но и способ развития фантазии и творческого мышления.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Выбираем надежную Букмекерскую контору 1win
Читая книгу, человек учится эмпатии и пониманию чужой точки зрения, расширяя свой кругозор и мировоззрение. https://rusvesna.su/aboutall/1599556550
Подробное руководство
2. Секреты монтажа гипсокартона: шаг за шагом инструкция
3. Гипсокартонные конструкции: основные виды и их преимущества
4. Как сэкономить при покупке гипсокартона: лучшие способы
5. Простые способы обработки гипсокартона: советы от профессионалов
6. Интересные идеи использования гипсокартона в интерьере
7. Все, что вам нужно знать о гипсокартоне: полезная информация
8. Гипсокартон: обзор популярных брендов и их характеристики
9. Плюсы и минусы гипсокартона: как правильно выбрать материал
10. Как сделать ровные стены с помощью гипсокартона: секреты и советы
11. Гипсокартонные потолки: виды и технологии монтажа
12. Декорирование гипсокартона: идеи для творческого подхода
13. Гипсокартон в дизайне интерьера: современные тренды и решения
14. Преимущества гипсокартона перед другими строительными материалами
15. Как выбрать правильный инструмент для работы с гипсокартоном
16. Гипсокартон: надежный материал для обустройства дома
17. Гипсокартон как элемент декора: необычные способы применения
18. Технологии монтажа гипсокартона: лучшие практические советы
19. История и развитие гипсокартона: открытия и достижения
20. Строительство с использованием гипсокартона: основные этапы и рекомендации
купить гипсокартон гипсокартон влагостойкий .
Подарив книгу, вы дарите возможность человеку погрузиться в мир абстрактных идей и философских размышлений.
https://www.chitalnya.ru/press/1950/
bestchicago.net
northfloridahouse.com
ebal
Подарив книгу, вы дарите возможность человеку путешествовать во времени и пространстве, погружаясь в исторические эпохи, фантастические миры или психологические глубины человеческой души. https://rusvesna.su/aboutall/1599556550
Подарив книгу, вы дарите возможность человеку сделать перерыв в своей рутинной жизни и открыть для себя что-то новое и удивительное.
https://www.klerk.ru/materials/2022-02-15/525164/
Подарив книгу, вы дарите возможность человеку найти ответы на свои вопросы и разрешить свои проблемы.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Книга – это источник вдохновения для творческих начинаний и проектов. Ее страницы могут заполниться заметками, идеями и рисунками, став основой для новых творческих экспериментов.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Подробное руководство
2. Секреты монтажа гипсокартона: шаг за шагом инструкция
3. Гипсокартонные конструкции: основные виды и их преимущества
4. Как сэкономить при покупке гипсокартона: лучшие способы
5. Простые способы обработки гипсокартона: советы от профессионалов
6. Интересные идеи использования гипсокартона в интерьере
7. Все, что вам нужно знать о гипсокартоне: полезная информация
8. Гипсокартон: обзор популярных брендов и их характеристики
9. Плюсы и минусы гипсокартона: как правильно выбрать материал
10. Как сделать ровные стены с помощью гипсокартона: секреты и советы
11. Гипсокартонные потолки: виды и технологии монтажа
12. Декорирование гипсокартона: идеи для творческого подхода
13. Гипсокартон в дизайне интерьера: современные тренды и решения
14. Преимущества гипсокартона перед другими строительными материалами
15. Как выбрать правильный инструмент для работы с гипсокартоном
16. Гипсокартон: надежный материал для обустройства дома
17. Гипсокартон как элемент декора: необычные способы применения
18. Технологии монтажа гипсокартона: лучшие практические советы
19. История и развитие гипсокартона: открытия и достижения
20. Строительство с использованием гипсокартона: основные этапы и рекомендации
гипсокартон купить в москве сетка металлическая .
Читая книгу, человек учится выражать свои мысли и чувства, развивая свою литературную грамотность.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Выбрал для себя надежную Букмекерскую контору 1xbet
Рекомендация от меня – Букмекерская контора №1 1xbet
Подарок в виде книги может стать началом новых интересных знакомств и дружеских связей. Ведь обсуждение прочитанных книг часто становится поводом для общения.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
mexico drug stores pharmacies mexican pharmacy buying prescription drugs in mexico online
купить алюминиевый плинтус для пола купить алюминиевый плинтус для пола .
porn
Подарив книгу, вы дарите возможность человеку наслаждаться моментом, забыв о повседневных проблемах и заботах.
https://www.klerk.ru/materials/2022-02-15/525164/
su pГЎgina web
If some one needs expert view concerning blogging and site-building afterward
i advise him/her to pay a visit this website, Keep
up the nice job.
Подробное руководство
2. Секреты монтажа гипсокартона: шаг за шагом инструкция
3. Гипсокартонные конструкции: основные виды и их преимущества
4. Как сэкономить при покупке гипсокартона: лучшие способы
5. Простые способы обработки гипсокартона: советы от профессионалов
6. Интересные идеи использования гипсокартона в интерьере
7. Все, что вам нужно знать о гипсокартоне: полезная информация
8. Гипсокартон: обзор популярных брендов и их характеристики
9. Плюсы и минусы гипсокартона: как правильно выбрать материал
10. Как сделать ровные стены с помощью гипсокартона: секреты и советы
11. Гипсокартонные потолки: виды и технологии монтажа
12. Декорирование гипсокартона: идеи для творческого подхода
13. Гипсокартон в дизайне интерьера: современные тренды и решения
14. Преимущества гипсокартона перед другими строительными материалами
15. Как выбрать правильный инструмент для работы с гипсокартоном
16. Гипсокартон: надежный материал для обустройства дома
17. Гипсокартон как элемент декора: необычные способы применения
18. Технологии монтажа гипсокартона: лучшие практические советы
19. История и развитие гипсокартона: открытия и достижения
20. Строительство с использованием гипсокартона: основные этапы и рекомендации
купить строительные материалы москва гипсокартон купить .
Читая книгу, человек расширяет свой кругозор и узнает о разных культурах и обычаях, погружаясь в мир разнообразия и толерантности.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
pharmacy com canada Certified Canadian pharmacies canada ed drugs
Подробное руководство
2. Секреты монтажа гипсокартона: шаг за шагом инструкция
3. Гипсокартонные конструкции: основные виды и их преимущества
4. Как сэкономить при покупке гипсокартона: лучшие способы
5. Простые способы обработки гипсокартона: советы от профессионалов
6. Интересные идеи использования гипсокартона в интерьере
7. Все, что вам нужно знать о гипсокартоне: полезная информация
8. Гипсокартон: обзор популярных брендов и их характеристики
9. Плюсы и минусы гипсокартона: как правильно выбрать материал
10. Как сделать ровные стены с помощью гипсокартона: секреты и советы
11. Гипсокартонные потолки: виды и технологии монтажа
12. Декорирование гипсокартона: идеи для творческого подхода
13. Гипсокартон в дизайне интерьера: современные тренды и решения
14. Преимущества гипсокартона перед другими строительными материалами
15. Как выбрать правильный инструмент для работы с гипсокартоном
16. Гипсокартон: надежный материал для обустройства дома
17. Гипсокартон как элемент декора: необычные способы применения
18. Технологии монтажа гипсокартона: лучшие практические советы
19. История и развитие гипсокартона: открытия и достижения
20. Строительство с использованием гипсокартона: основные этапы и рекомендации
гипсокартон доставка гіпсокартон оптом .
Книга – это подарок, который может стать компаньоном на всю жизнь, оставаясь верным другом и советчиком в любой ситуации.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Рекомендация от меня – лучшая Букмекерская контора 1xbet
Книга может стать незаменимым компаньоном в путешествиях или во время долгих поездок. Ведь ее можно взять с собой куда угодно и в любое время.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
через него я уж нашёл нескольких кексов, но его мощности далеки от людей версий, глаз бога официальный сайт которыми в современности.
Have a look at my homepage – https://glazbot.com/
Читая книгу, человек учится выражать свои мысли и чувства более точно и глубоко, развивая свои коммуникативные навыки.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Подарив книгу, вы дарите не только объект, но и возможность для саморазвития и роста личности.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Подарок в виде книги может стать началом увлекательного хобби и увлечения. Кто знает, может быть, она станет первым шагом на пути к новой профессии или увлекательному исследованию.
https://www.klerk.ru/materials/2022-02-15/525164/
Читая книгу, человек учится выражать свои мысли и чувства, развивая свою литературную грамотность.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
doxycycline medication doxycycline 150 mg doxycycline 100mg capsules
Книга – это не только подарок для развлечения, но и инструмент для обучения. Ведь в ней можно найти информацию по самым разным темам и областям знаний. https://rusvesna.su/aboutall/1599556550
Выбрал для себя топовую Букмекерскую контору 1xbet
Рекомендация от меня – самая лучшая Букмекерская контора 1xbet
diflucan over the counter singapore diflucan online purchase diflucan 100mg
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across. Seo Hizmeti Skype : live:by_umut
Читая книгу, человек учится эмпатии и пониманию чужой точки зрения, что способствует укреплению межличностных отношений.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Luxurious living awaits you in Mr. C Residences! Discover breathtaking apartments and penthouses on the iconic Dubai Canal. The prestigious developer, Alta, presents an incredible opportunity to own your dream home at unbeatable prices. Indulge in sophistication and opulence beyond your imagination. Don’t miss out on this exclusive chance to elevate your lifestyle in Dubai’s most sought-after complex.
Подарив книгу, вы дарите возможность человеку путешествовать во времени и пространстве, погружаясь в разные эпохи и культуры.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Подарив книгу, вы дарите возможность человеку путешествовать во времени и пространстве, погружаясь в исторические эпохи, фантастические миры или психологические глубины человеческой души.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Синтетические гвоздики от 55опторг — это высококачественное украшение, которое отличным вариантом для создания уникальных инсталляций, декоративных ансамблей и букетов. Компания 55опторг специализируется на реализации ненатуральных цветов и другой флористической продукции оптом, обеспечивая товар превосходного качества и его доступность. Не страшат им изменения тепла, влажности или освещенности, ведь они не увядут, не потеряют своей формы и облика и цвета. Они могут становиться в прекрасное дополнение ко всему: от дизайна помещения до оформления социальных акций. Заботливое отношение к делу, большой ассортимент и работа прямо с производителями позволяют обеспечивать клиентам продукцию без трудностей и задержек в поставке. Будь то искусственные гвоздики для праздничного декора или оформления витрин магазинов, 55опторг всегда предоставит вам широкий выбор.
искусственные цветы гвоздики
Книга может стать незаменимым компаньоном в путешествиях или во время долгих поездок. Ведь ее можно взять с собой куда угодно и в любое время.
https://www.klerk.ru/materials/2022-02-15/525164/
LГҐna 60000 kr
365pronxxx
Подарив книгу, вы дарите возможность человеку сбежать из реальности и окунуться в мир фантазии и мечты.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Выбрал для себя лучшую Букмекерскую контору 1xbet
Самая лучшая Букмекерская контора 1xbet
diflucan online paypal buy diflucan medicarions diflucan 150 cost
Книга – это дар, который может стать источником вдохновения для новых идей и проектов. https://rusvesna.su/aboutall/1599556550
в то же время нормативный срок функционирования по следующим объектам определяется комиссией с учетом технического функциональности.
my web page :: http://cruiser.com.ua/2020/09/prichiny-neispravnosti-generatora-u-gruzovika-volvo/
прогулочную коляску купить заказать коляску .
Книга – это не просто подарок, это окно в мир знаний и фантазии. Она может стать верным спутником на долгие часы, погружая в увлекательные приключения и учебные материалы.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Почему наши тоговые сигналы – всегда оптимальный вариант:
Наша группа утром и вечером, днём и ночью в тренде текущих курсов и моментов, которые воздействуют на криптовалюты. Это способствует нашему коллективу оперативно реагировать и давать актуальные подачи.
Наш коллектив обладает предельным понимание теханализа и может выделить крепкие и уязвимые поля для включения в сделку. Это способствует для снижения опасностей и повышению прибыли.
Мы применяем собственные боты анализа для просмотра графиков на любых интервалах. Это способствует нам достать полную картину рынка.
Перед опубликованием подачи в нашем Telegram мы осуществляем тщательную ревизию все сторон и подтверждаем возможное лонг или шорт. Это обеспечивает верность и качественность наших сигналов.
Присоединяйтесь к нам к нашему каналу прямо сейчас и достаньте доступ к проверенным торговым сигналам, которые помогут вам достигнуть финансовых результатов на крипторынке!
https://t.me/Investsany_bot
trecator-sc
purchase cytotec buy cytotec over the counter purchase cytotec
прогулочные коляски москва прогулочные коляски москва .
Читая книгу, человек развивает свой интеллект и воображение, открывает для себя новые идеи и точки зрения. Поэтому дарить книгу – значит дарить возможность к росту и самосовершенствованию.
https://www.chitalnya.ru/press/1950/
Читая книгу, человек расширяет свой кругозор и познает мир через глаза других людей, учась видеть вещи с разных сторон.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
купить диплом https://1diplomy-grupp.ru .
prestamo 400000 euros
Подарив книгу, вы дарите нечто более ценное, чем материальный объект – вы дарите время, которое человек проведет, погруженный в ее чтение.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
купить коляску детские коляски .
Чтобы установить, настоящий срок полезного использования, нужно узнать объем двигателя у легкового автомобиля, далее выяснить.
Here is my page … https://www.svarz.com/chto-takoe-reostat-pedali-gaza-gruzovikov-volvo-fh12-gde-on-naxoditsya.html
прогулочные коляски коляски для детей .
Выбрал для себя потрясающую Букмекерскую контору 1xbet
Самая лучшая Букмекерская контора, советую 1xbet
Подробное руководство
2. Секреты монтажа гипсокартона: шаг за шагом инструкция
3. Гипсокартонные конструкции: основные виды и их преимущества
4. Как сэкономить при покупке гипсокартона: лучшие способы
5. Простые способы обработки гипсокартона: советы от профессионалов
6. Интересные идеи использования гипсокартона в интерьере
7. Все, что вам нужно знать о гипсокартоне: полезная информация
8. Гипсокартон: обзор популярных брендов и их характеристики
9. Плюсы и минусы гипсокартона: как правильно выбрать материал
10. Как сделать ровные стены с помощью гипсокартона: секреты и советы
11. Гипсокартонные потолки: виды и технологии монтажа
12. Декорирование гипсокартона: идеи для творческого подхода
13. Гипсокартон в дизайне интерьера: современные тренды и решения
14. Преимущества гипсокартона перед другими строительными материалами
15. Как выбрать правильный инструмент для работы с гипсокартоном
16. Гипсокартон: надежный материал для обустройства дома
17. Гипсокартон как элемент декора: необычные способы применения
18. Технологии монтажа гипсокартона: лучшие практические советы
19. История и развитие гипсокартона: открытия и достижения
20. Строительство с использованием гипсокартона: основные этапы и рекомендации
гипсокартон заказать гипсокартон доставка .
Подарив книгу, вы дарите не только объект, но и возможность для саморазвития и роста личности.
https://www.klerk.ru/materials/2022-02-15/525164/
Почему наши сигналы – ваш идеальный выбор:
Наша группа утром и вечером, днём и ночью на волне текущих курсов и событий, которые оказывают влияние на криптовалюты. Это дает возможность коллективу незамедлительно действовать и предоставлять актуальные трейды.
Наш коллектив владеет глубоким знанием технического анализа и умеет выявлять устойчивые и незащищенные аспекты для включения в сделку. Это способствует для снижения рисков и максимизации прибыли.
Мы применяем личные боты-анализаторы для анализа графиков на все временных промежутках. Это помогает нашим специалистам достать всю картину рынка.
Перед подачей подача в нашем канале Telegram мы осуществляем тщательную проверку все аспектов и подтверждаем возможное долгий или шорт. Это гарантирует надежность и качественные характеристики наших подач.
Присоединяйтесь к нам к нашему каналу прямо сейчас и достаньте доступ к подтвержденным торговым подачам, которые содействуют вам добиться финансового успеха на рынке криптовалют!
https://t.me/Investsany_bot
Siz blackjack və Baccarat, mostbet download başlayaq rulet və poker ilə – hər kəs tapacaq nə ona uyğun gəlir.
My web-site https://mostbet-azerbaycan.bet/
Подарив книгу, вы дарите возможность человеку открыть для себя новые авторов и литературные жанры.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Amplificadores de senal gsm
Potencia la senal de tu movil con un amplificador de alta potencia
https://glose.com/activity/65b3e6ca46eed8c778fe32c6
Книга – это подарок, который можно открыть снова и снова, каждый раз находя в ней что-то новое и удивительное. https://rusvesna.su/aboutall/1599556550
Книга – это источник вдохновения для творческих начинаний и проектов. Ее страницы могут заполниться заметками, идеями и рисунками, став основой для новых творческих экспериментов.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
LГҐn 80000 kr
nolvadex price п»їdcis tamoxifen tamoxifen and weight loss
Читая книгу, человек учится эмпатии и пониманию чужой точки зрения, расширяя свой кругозор и мировоззрение.
https://www.klerk.ru/materials/2022-02-15/525164/
Даря книгу, вы не только дарите радость человеку, но и помогаете расширить его кругозор и культурный уровень. https://rusvesna.su/aboutall/1599556550
buy cytotec online buy cytotec over the counter purchase cytotec
Читая книгу, человек расширяет свой кругозор и познает мир через глаза других людей, учась видеть вещи с разных сторон.
https://www.chitalnya.ru/press/1950/
Книга – это не просто подарок, это окно в мир знаний и фантазии. Она может стать верным спутником на долгие часы, погружая в увлекательные приключения и учебные материалы.
https://www.chitalnya.ru/press/1950/
Подарив книгу, вы дарите человеку ключ к новым мирам и приключениям, которые он может исследовать в своем собственном темпе.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Выбрал для себя шикарную Букмекерскую контору 1xbet
Самая надежная Букмекерская контора, советую 1xbet
купить коляску для коляски прогулочные .
Подарив книгу, вы дарите возможность человеку открыть для себя новые авторов и литературные жанры.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Опускание в вселенную гемблинга up x – это подобно путешествие во привлекательный мазок перспектив. В этом месте все любитель азарта выискивает личный уголок: независимо от того, карточные игры, автоматы или рулеточный стол. Гладкое конкатенация захватывающей изображения или профессионализма разработки программного обеспечения генерирует уникальную обстановку, где страсть объединяется с классом. Удобство применения и высокая мера защиты делают up x замечательным выбором для всех любителей развлечений в стиле азарта.
купить справку о болезни
symbicort inhaler
Книга может быть источником вдохновения и мотивации. В ее страницах можно найти истории успеха, которые подтолкнут к собственным достижениям.
https://www.chitalnya.ru/press/1950/
keflex 5mg
Подарив книгу, вы дарите возможность человеку сделать перерыв в своей рутинной жизни и открыть для себя что-то новое и удивительное.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
https://miele-remonty.ru/stiralnyh-mashin/
Книга может стать источником общения и дискуссий. После ее прочтения можно обсудить с друзьями или семьей впечатления и выводы.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
ebal tut
where to purchase doxycycline buy doxycycline online 270 tabs doxycycline vibramycin
Читая книгу, человек учится выражать свои мысли и чувства более точно и глубоко, развивая свои коммуникативные навыки.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Читая книгу, человек расширяет свой кругозор и узнает о разных культурах и обычаях, погружаясь в мир разнообразия и толерантности.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
nolvadex pills pct nolvadex nolvadex 10mg
Книга – это не просто подарок, это окно в мир знаний и фантазии. Она может стать верным спутником на долгие часы, погружая в увлекательные приключения и учебные материалы.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
https://t.me/s/melbet_oficialnyy_sait_zerkalo
Опускание в окружение гемблинга гет икс казино – это также как путешествие во привлекательный путь возможностей. Здесь каждый участник находит уникальный местечко: будь то игры в карты, слоты или даже рулетка. Тонкое сочетание захватывающей графики а умения программной разработки формирует неповторимую обстановку, где волнение объединяется с стилем. Легкость применения и высокая степень безопасности делают Гет Х потрясающим выбором для каждого поклонников игр азарта.
Подарок в виде книги может стать началом увлекательного хобби и увлечения. Кто знает, может быть, она станет первым шагом на пути к новой профессии или увлекательному исследованию.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Погружение в среду азарта Игровые автоматы – это вроде поездка во привлекательный лабиринт возможностей. В этой области каждый участник находит личный куток: будь то карточные дуэли, игровые автоматы или рулетный стол. Мягкое сочетание загадочной графики а мастерства программирования создает оригинальную атмосферу, где азарт объединяется с изяществом. Удобство применения и высокая мера защиты делают Игровые автоматы на деньги превосходным выбором для всех ценителей азартных игр.
Книга – это не только источник знаний, но и способ развлечения. Ведь в ее страницах можно найти как научные факты, так и увлекательные рассказы.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
JDBslot
JDB slot | The first bonus to rock the slot world
Exclusive event to earn real money and slot game points
JDB demo slot games for free = ?? Lucky Spin Lucky Draw!
How to earn reels free 2000? follow jdb slot games for free
#jdbslot
Demo making money : https://jdb777.com
#jdbslot #slotgamesforfree #howtoearnreels #cashreels
#slotgamepoint #demomakingmoney
Cash reels only at slot games for free
More professional jdb game bonus knowledge
Methods to Acquire Spins Points Complimentary 2000: Your Greatest Guide to Winning Substantial with JDB Machines
Are you ready to start on an exciting expedition into the world of web slot games? Seek no further, just spin to JDB777 FreeGames, where enthusiasm and large wins expect you at every turn of the reel. In this complete handbook, we’ll present you how to acquire reels credit costless 2000 and unlock the exhilarating world of JDB slots.
Feel the Adrenaline rush of Gaming Games for Free
At JDB777 FreeGames, we provide a wide choice of captivating slot games that are guaranteed to keep you entertained for hours on end. From vintage fruit machines to immersive themed slots, there’s something for each variety of player to enjoy. And the greatest part? You can play all of our slot games for free and achieve real cash prizes!
Release Free Cash Reels and Succeed Big
One of the most stimulating features of JDB777 FreeGames is the option to gain reels points costless 2000, which can be exchanged for real cash. Easily sign up for an account, and you’ll acquire your gratis bonus to begin spinning and winning. With our plentiful promotions and bonuses, the sky’s the boundary when it comes to your winnings!
Guide Strategies and Scores System
To enhance your winnings and unlock the full potential of our slot games, it’s essential to understand the strategies and points system. Our expert guides will take you through everything you have to have to know, from choosing the right games to comprehending how to acquire bonus points and cash prizes.
Distinctive Promotions and Exclusive Offers
As a member of JDB777 FreeGames, you’ll have access to exclusive promotions and special offers that are positive to improve your gaming experience. From welcome bonuses to daily rebates, there are a great deal of possibilities to enhance your winnings and take your gameplay to the subsequent level.
Join Us Today and Begin Winning
Don’t miss out on your chance to win big with JDB777 FreeGames. Sign up now to assert your complimentary bonus of 2000 credits and begin spinning the reels for your possibility to win real cash prizes. With our exciting choice of slot games and generous promotions, the opportunities are endless. Join us today and initiate winning!
Выбрал шикарную Букмекерскую контору 1xbet
Подарив книгу, вы дарите возможность человеку найти ответы на свои вопросы и разрешить свои проблемы.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
JDB online
JDB online | 2024 best online slot game demo cash
How to earn reels? jdb online accumulate spin get bonus
Hot demo fun: Quick earn bonus for ranking demo
JDB demo for win? JDB reward can be exchanged to real cash
#jdbonline
777 sign up and get free 2,000 cash: https://www.jdb777.io/
#jdbonline #democash #demofun #777signup
#rankingdemo #demoforwin
2000 cash: Enter email to verify, enter verify, claim jdb bonus
Play with JDB games an online platform in every countries.
Enjoy the Pleasure of Gaming!
Costless to Join, Gratis to Play.
Join and Acquire a Bonus!
JOIN NOW AND GET 2000?
We dare you to claim a demo fun welcome bonus for all new members! Plus, there are other special promotions waiting for you!
Discover more
JDB – FREE TO JOIN
Effortless to play, real profit
Engage in JDB today and indulge in fantastic games without any investment! With a wide array of free games, you can savor pure entertainment at any time.
Speedy play, quick join
Value your time and opt for JDB’s swift games. Just a few easy steps and you’re set for an amazing gaming experience!
Sign Up now and receive money
Experience JDB: Instant play with no investment and the opportunity to win cash. Designed for effortless and lucrative play.
Immerse into the Domain of Online Gaming Stimulation with Fun Slots Online!
Are you set to experience the thrill of online gaming like never before? Scour no further than Fun Slots Online, your ultimate destination for exhilarating gameplay, endless entertainment, and stimulating winning opportunities!
At Fun Slots Online, we boast ourselves on presenting a wide range of engaging games designed to hold you involved and delighted for hours on end. From classic slot machines to innovative new releases, there’s something for everybody to enjoy. Plus, with our user-friendly interface and smooth gameplay experience, you’ll have no difficulty plunging straight into the activity and enjoying every moment.
But that’s not all – we also provide a selection of particular promotions and bonuses to compensate our loyal players. From welcome bonuses for new members to exclusive rewards for our top players, there’s always something stimulating happening at Fun Slots Online. And with our guarded payment system and 24-hour customer support, you can savor peace of mind knowing that you’re in good hands every step of the way.
So why wait? Enroll Fun Slots Online today and begin your trip towards breath-taking victories and jaw-dropping prizes. Whether you’re a seasoned gamer or just starting out, there’s never been a better time to engage in the fun and excitement at Fun Slots Online. Sign up now and let the games begin!
Книга – это подарок, который может стать компаньоном на всю жизнь, оставаясь верным другом и советчиком в любой ситуации.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Подарив книгу, вы дарите возможность человеку путешествовать во времени и пространстве, погружаясь в исторические эпохи, фантастические миры или психологические глубины человеческой души.
https://www.klerk.ru/materials/2022-02-15/525164/
ciprofloxacin order online buy cipro cipro online no prescription in the usa
csgo gambling sites with paypal deposit
https://canabecolorexpert.com/art/cs2betting-sites.html
robot 88
csgo gambling bans
https://cascepecuador.com/art/top-10-cs2-gambling-sites.html
Читая книгу, человек учится анализировать информацию и принимать обоснованные решения, развивая свою критическую мысль.
https://www.klerk.ru/materials/2022-02-15/525164/
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.儿童色情
cs go all gambling sites
https://lafermedelabourgade.be/wp-content/pgs/betting-websites-cs2.html
Выбрал лучшую Букмекерскую контору 1xbet
Самая крутая Букмекерская контора, советую 1xbet
gay escort dubai
Ефективні методи профілактики
дитяча стоматологічна клініка івано франківськ дитяча стоматологічна клініка івано франківськ .
Читая книгу, человек обогащает свой внутренний мир и развивает свое эмоциональное восприятие. Ведь в каждой книге есть что-то свое, что заставляет задуматься и переживать. https://rusvesna.su/aboutall/1599556550
Професійні поради стоматолога
8. Як вибрати ідеальну зубну нитку для себе
стоматологія клініка стоматологія клініка .
Читая книгу, человек находит ответы на свои вопросы и учится справляться с жизненными трудностями, обогащая свой жизненный опыт. https://rusvesna.su/aboutall/1599556550
Серьезных недостатков не заметил. деньги на депозит зачисляются различными способами.
My web blog https://blogbasta.kz/
Подарок в виде книги может стать началом новых интересных знакомств и дружеских связей. Ведь обсуждение прочитанных книг часто становится поводом для общения.
https://www.chitalnya.ru/press/1950/
Ефективні методи лікування
10. Як підготуватися до відвідування стоматолога
стоматологія протезування стоматологія протезування .
Free drawing lessons for beginners and professionals Drawing lessons
Книга может быть источником вдохновения и мотивации. В ее страницах можно найти истории успеха, которые подтолкнут к собственным достижениям.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
купить справку на высоту
Професійна чистка
5. Як уникнути проблем із яснами
стоматологічна клініка усмішка стоматологічна клініка усмішка .
Читая книгу, человек учится терпению и выдержке, ведь нередко на пути к концу страницы сталкивается с многочисленными испытаниями и поворотами сюжета.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
ремонт бытовой техники miele
Книга – это не только подарок для развлечения, но и инструмент для обучения. Ведь в ней можно найти информацию по самым разным темам и областям знаний.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
200 mg doxycycline doxy 200 buy doxycycline for dogs
Книга – это не только источник знаний, но и способ развлечения. Ведь в ее страницах можно найти как научные факты, так и увлекательные рассказы.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Читая книгу, человек расширяет свой кругозор и узнает о разных культурах и обычаях, погружаясь в мир разнообразия и толерантности.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Книга может быть не только источником знаний, но и прекрасным способом расслабиться и отдохнуть после трудного дня. Ведь в ее страницах можно погрузиться в другой мир и забыть о повседневных заботах.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Подарив книгу, вы дарите нечто более ценное, чем материальный объект – вы дарите время, которое человек проведет, погруженный в ее чтение.
https://www.chitalnya.ru/press/1950/
1. Идеи для дизайна интерьера
2. Тренды в дизайне
3. Цветовые решения
4. Дизайн-проект
5. Инновационные подходы к дизайну: отражение современности
6. Шаг за шагом: создание уютного дизайна спальни
7. Дизайн для маленькой квартиры
8. Как интегрировать природные элементы в дизайн интерьера
9. Основы дизайна
10. Дизайнерский бизнес
11. Дизайн в XXI веке
12. Дизайн кухни
13. Дизайн мебели
14. Дизайн гостиной
15. Минимализм
16. Дизайн сада
17. Декорирование дома с использованием текстиля: советы и идеи
18. Цветовой баланс
19. Книги по дизайну
20. Дизайн подростковой комнаты
дизайн интерьера москва https://studiya-dizajna-intererov.ru/ .
Книга может стать источником общения и дискуссий. После ее прочтения можно обсудить с друзьями или семьей впечатления и выводы.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Погружение в среду страсти казино император играть – это подобно переход во вдохновляющий лабиринт вариаций. В этой области все игрок получает индивидуальный местечко: вне зависимости от того, карточные игры, игровые машины даже рулетка. Тонкое сочетание увлекательной изображения также умения разработки программного обеспечения генерирует оригинальную окружение, где волнение объединяется с классом. Комфорт применения и высокая степень защиты делают играть онлайн казино великолепным выбором для всех обожателей развлечений в стиле азарта.
Книга – это не только источник знаний, но и способ развития фантазии и творческого мышления.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
Подарив книгу, вы дарите возможность человеку сделать перерыв в своей рутинной жизни и открыть для себя что-то новое и удивительное.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Погружение в атмосферу страсти играть онлайн казино император – это как экскурсия во подкупающий лабиринт вариаций. Здесь все участник обнаруживает уникальный местечко: будь то игры с картами, слот-машинки или даже релоад. Плавное конкатенация захватывающей изображения или навыков написания программ порождает индивидуальную обстановку, где страсть соединяется с элегантностью. Удобство применения и повышенная мера защиты делают онлайн автоматы великолепным выбором для всех поклонников игр азарта.
doxycycline 100mg tablets doxycycline hyclate 100 mg cap buy cheap doxycycline
1. Идеи для дизайна интерьера
2. Тренды в дизайне
3. Как выбрать идеальный цветовой акцент в дизайне
4. Дизайн-проект
5. Дизайн нового поколения
6. Дизайн спальни
7. Дизайнерские решения для увеличения пространства в маленькой квартире
8. Природный дизайн
9. Основы дизайна
10. Дизайнерский бизнес
11. Дизайн в XXI веке
12. Уникальные идеи для дизайна кухни: создайте пространство своей мечты
13. Дизайн мебели
14. Дизайн гостиной
15. Минимализм
16. Дизайн сада
17. Декорирование с текстилем
18. Цветовой баланс
19. Топ-10 книг по дизайну интерьера, которые стоит прочитать
20. Дизайн комнаты для подростка: креативные идеи для стильного интерьера
дизайн интерьера студия дизайн интерьера студия .
Важливі рекомендації
19. Як вибрати найкраще засіб для видалення зубного нальоту
стоматологія спектр https://stomatologiyatrn.ivano-frankivsk.ua/ .
Представляю лучшую Букмекерскую контору – 1xbet
Крутая Букмекерская контора, советую 1xbet
Подарив книгу, вы дарите возможность человеку сделать перерыв в своей рутинной жизни и открыть для себя что-то новое и удивительное.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Даря книгу, вы не только дарите радость человеку, но и помогаете расширить его кругозор и культурный уровень.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Погружение в вселенную азарта imperator casino – это также как путешествие во подкупающий лабиринт перспектив. На этой территории все игрок находит личный ресурс: независимо от того, игры с картами, слот-машинки даже рокировка. Плавное слияние захватывающей визуализации и навыков написания программ вызывает оригинальную атмосферу, где страсть объединяется с стилем. Удобство применения и высокая степень секьюрити делают новые казино с бездепозитными бонусами великолепным выбором для всех поклонников азартных развлечений.
buy cipro online cipro 500mg best prices purchase cipro
Hello just wanted to give you a quick heads up. The words in your post seem to be running off the screen in Ie.
I’m not sure if this is a formatting issue or something to do with
browser compatibility but I figured I’d post to let you know.
The design and style look great though! Hope you get the issue fixed soon.
Thanks
Подарив книгу, вы дарите возможность человеку найти ответы на свои вопросы и разрешить свои проблемы.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Thank you for great content. Hello Administ. 国产线播放免费人成视频播放
1. 10 лучших идей для дизайна интерьера
2. Топ-20 трендов в дизайне на 2021 год
3. Цветовые решения
4. Дизайн-проект
5. Дизайн нового поколения
6. Шаг за шагом: создание уютного дизайна спальни
7. Дизайнерские решения для увеличения пространства в маленькой квартире
8. Как интегрировать природные элементы в дизайн интерьера
9. Баланс цветов и форм: основы хорошего дизайна
10. Дизайнерский бизнес
11. Интересные факты о развитии дизайна в XXI веке
12. Дизайн кухни
13. Тенденции в сфере дизайна мебели: вдохновляющие идеи
14. Дизайн гостиной
15. Минимализм
16. Дизайн сада: принципы оформления участка с учетом ландшафта
17. Декорирование дома с использованием текстиля: советы и идеи
18. Принципы цветового баланса в дизайне: как создать гармоничное пространство
19. Топ-10 книг по дизайну интерьера, которые стоит прочитать
20. Дизайн подростковой комнаты
студия дизайна и интерьера https://studiya-dizajna-intererov.ru/ .
Книга – это не только источник информации, но и способ развития креативности и воображения. Ведь в ее страницах можно найти вдохновение для творческих начинаний. https://rusvesna.su/aboutall/1599556550
Книга – это дар, который может стать источником вдохновения для новых идей и проектов.
https://www.chitalnya.ru/press/1950/
1. 10 лучших идей для дизайна интерьера
2. Тренды в дизайне
3. Цветовые решения
4. Секреты успешного дизайн-проекта
5. Инновационные подходы к дизайну: отражение современности
6. Шаг за шагом: создание уютного дизайна спальни
7. Дизайн для маленькой квартиры
8. Природный дизайн
9. Основы дизайна
10. Дизайнерский бизнес
11. Дизайн в XXI веке
12. Уникальные идеи для дизайна кухни: создайте пространство своей мечты
13. Тенденции в сфере дизайна мебели: вдохновляющие идеи
14. Мастер-класс по созданию стильного дизайна гостиной
15. Минимализм
16. Дизайн сада
17. Декорирование дома с использованием текстиля: советы и идеи
18. Цветовой баланс
19. Книги по дизайну
20. Дизайн комнаты для подростка: креативные идеи для стильного интерьера
3d визуализация интерьера 3d визуализация интерьера .
Читая книгу, человек развивает свою логику и критическое мышление, учась анализировать и оценивать информацию.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Подарив книгу, вы дарите возможность человеку сделать перерыв в своей рутинной жизни и открыть для себя что-то новое и удивительное.
https://rusonline.org/raznoe/eksklyuzivnye-podarki-ot-internet-magazina-mospodarok
Подарок в виде книги может стать началом новых интересных знакомств и дружеских связей. Ведь обсуждение прочитанных книг часто становится поводом для общения.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
Читая книгу, человек развивает свою логику и критическое мышление, учась анализировать и оценивать информацию.
https://www.chitalnya.ru/press/1950/
купить аттестат за 9 https://www.2diplom-grupp.ru .
reglan
usainvesttoday.com
italycarsrental.com
Даря книгу, вы дарите возможность человеку самостоятельно мыслить и анализировать информацию. https://rusvesna.su/aboutall/1599556550
diflucan without a prescription how much is over the counter diflucan diflucan 150 mg fluconazole
Вывоз мусора с грузчиками https://vivozmusora67.ru/
Подарив книгу, вы дарите возможность человеку сделать перерыв в своей рутинной жизни и открыть для себя что-то новое и удивительное.
https://www.chitalnya.ru/press/1950/
dj88
App cá độ:Hướng dẫn tải app cá cược uy tín RG777 đúng cách
Bạn có biết? Tải app cá độ đúng cách sẽ giúp tiết kiệm thời gian đăng nhập, tăng tính an toàn và bảo mật cho tài khoản của bạn! Vậy đâu là cách để tải một app cá cược uy tín dễ dàng và chính xác? Xem ngay bài viết này nếu bạn muốn chơi cá cược trực tuyến an toàn!
tải về ngay lập tức
RG777 – Nhà Cái Uy Tín Hàng Đầu Việt Nam
Link tải app cá độ nét nhất 2023:RG777
Để đảm bảo việc tải ứng dụng cá cược của bạn an toàn và nhanh chóng, người chơi có thể sử dụng đường link sau.
tải về ngay lập tức
rg777
App cá độ:Hướng dẫn tải app cá cược uy tín RG777 đúng cách
Bạn có biết? Tải app cá độ đúng cách sẽ giúp tiết kiệm thời gian đăng nhập, tăng tính an toàn và bảo mật cho tài khoản của bạn! Vậy đâu là cách để tải một app cá cược uy tín dễ dàng và chính xác? Xem ngay bài viết này nếu bạn muốn chơi cá cược trực tuyến an toàn!
tải về ngay lập tức
RG777 – Nhà Cái Uy Tín Hàng Đầu Việt Nam
Link tải app cá độ nét nhất 2023:RG777
Để đảm bảo việc tải ứng dụng cá cược của bạn an toàn và nhanh chóng, người chơi có thể sử dụng đường link sau.
tải về ngay lập tức
Лучшая Букмекерская контора, советую 1xbet
Подарив книгу, вы дарите возможность человеку путешествовать во времени и пространстве, погружаясь в разные эпохи и культуры.
https://www.klerk.ru/materials/2022-02-15/525164/
http://flowervl.ru/
Книга – это подарок, который может оказать влияние на всю жизнь человека, вдохновляя на новые цели и достижения.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
台中外送茶
現代社會,快遞已成為大眾化的服務業,吸引了許多人的注意和參與。 與傳統夜店、酒吧不同,外帶提供了更私密、便捷的服務方式,讓人們有機會在家中或特定地點與美女共度美好時光。
多樣化選擇
從台灣到日本,馬來西亞到越南,外送業提供了多樣化的女孩選擇,以滿足不同人群的需求和喜好。 無論你喜歡什麼類型的女孩,你都可以在外賣行業找到合適的女孩。
不同的價格水平
價格範圍從實惠到豪華。 無論您的預算如何,您都可以找到適合您需求的女孩,享受優質的服務並度過愉快的時光。
快遞業高度重視安全和隱私保護,提供多種安全措施和保障,讓客戶放心使用服務,無需擔心個人資訊外洩或安全問題。
如果你想成為一名經驗豐富的外包司機,外包產業也將為你提供廣泛的選擇和專屬服務。 只需按照步驟操作,您就可以輕鬆享受快遞行業帶來的樂趣和便利。
蓬勃發展的快遞產業為人們提供了一種新的娛樂休閒方式,讓人們在忙碌的生活中得到放鬆,享受美好時光。
для физлиц владельцев авто. 4. Оригинал доверенности на право получения дубликатов государственных регистрационных знаков https://vd-tv.
Читая книгу, человек учится эмпатии и пониманию чужой точки зрения, расширяя свой кругозор и мировоззрение.
https://www.km.ru/stil/2020/09/18/879500-podarochnye-izdaniya-knig
Thank you great post. Hello Administ .国产线播放免费人成视频播放
купить семена ранних огурцов почтой
Книга – это не только подарок для развлечения, но и инструмент для обучения. Ведь в ней можно найти информацию по самым разным темам и областям знаний.
https://www.chitalnya.ru/press/1950/
establishments may independently restrict compliance with revenge requirements in a number games, or prohibit players from playing in games with low level of risk, or limit the “risk-free” game (for example, bet on red and black in roulette), thus.
Also visit my web-site; https://teleskop.hr/hrvatska/kada-se-otvaraju-automat-klubovi/
game1kb.com
“폐하, 저는 이것이 좋은 일이라고 생각합니다. 좋은 일입니다.”
Читая книгу, человек обогащает свой внутренний мир и развивает свое эмоциональное восприятие. Ведь в каждой книге есть что-то свое, что заставляет задуматься и переживать.
https://e-news.su/society/384692-podarok-dlja-rukovoditelja-kak-ne-oshibitsja-s-vyborom.html
buy doxycycline online 270 tabs 200 mg doxycycline doxycycline mono
spiriva 9 mcg cost
App cá độ:Hướng dẫn tải app cá cược uy tín RG777 đúng cách
Bạn có biết? Tải app cá độ đúng cách sẽ giúp tiết kiệm thời gian đăng nhập, tăng tính an toàn và bảo mật cho tài khoản của bạn! Vậy đâu là cách để tải một app cá cược uy tín dễ dàng và chính xác? Xem ngay bài viết này nếu bạn muốn chơi cá cược trực tuyến an toàn!
tải về ngay lập tức
RG777 – Nhà Cái Uy Tín Hàng Đầu Việt Nam
Link tải app cá độ nét nhất 2023:RG777
Để đảm bảo việc tải ứng dụng cá cược của bạn an toàn và nhanh chóng, người chơi có thể sử dụng đường link sau.
tải về ngay lập tức
Изготовление дубликатов государственных регистрационных знаков транспортных средств, взамен старых (не соответствующих ГОСТ
Р 50577-93).
Feel free to visit my homepage – https://windowss10.ru/apps/uznajte-usloviya-polucheniya-kvadratnogo-nomera-dlya-avtomobilya-i-dobavte-stil-i-individualnost-svoemu-transportnomu-sredstvu.html
Web-based education is surely transforming the the perspective we have on traditional education. In Alabama, we can find numerous high-quality online schools giving a smooth learning experience to students. Everyone have the ability to manage their time as they engage in top-notch, flexible educational programs. Such platforms don't only meet varying academic needs, but they promote students to learn at their own pace, enhancing comprehension and retention along the way.
Numerous of these online schools in Alabama provide a complete curriculum including both core subjects and electives. Students can follow their interests while upholding a focus on required coursework. Plus, for students who excel in an individual learning environment, the online option can be exceptionally beneficial.
Furthermore, it's notable that these online schools are not merely about online lectures and assignments. Some schools offer interactive sessions, multimedia shows, and even virtual experiments virtually – widening horizons in an optimum learning environment.
As we navigate this new educational landscape, it's essential to stay updated with the available options. I highly suggest looking into your online schooling options in Alabama to guarantee a proper fit for your personal circumstances, learning preferences, and professional goals. Discover more about online schools in Alabama – the next step in education is here and now! http://onlineschoolAL5.com/
pret 25000 euros
ciprofloxacin mail online cipro pharmacy buy cipro
Читая книгу, человек развивает свою способность к анализу и синтезу информации, что помогает ему лучше понимать окружающий мир.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
вентиляция сплит система https://split-sistema-kupit.ru/ .
credit 2000 euros
Книга – это не просто подарок, это инвестиция в развитие и обогащение внутреннего мира человека.
https://www.chitalnya.ru/press/1950/
Книга может быть источником вдохновения и мотивации. В ее страницах можно найти истории успеха, которые подтолкнут к собственным достижениям.
https://russian7.ru/post/commercial/2020/03/18/kniga-kak-idealnyy-podarok/
кондиционеры купить https://split-sistema-kupit.ru/ .
сплит системы установка https://split-sistema-kupit.ru/ .
1. 10 лучших идей для дизайна интерьера
2. Тренды в дизайне
3. Цветовые решения
4. Секреты успешного дизайн-проекта
5. Дизайн нового поколения
6. Шаг за шагом: создание уютного дизайна спальни
7. Дизайн для маленькой квартиры
8. Как интегрировать природные элементы в дизайн интерьера
9. Баланс цветов и форм: основы хорошего дизайна
10. Дизайнерский бизнес
11. Интересные факты о развитии дизайна в XXI веке
12. Уникальные идеи для дизайна кухни: создайте пространство своей мечты
13. Тенденции в сфере дизайна мебели: вдохновляющие идеи
14. Дизайн гостиной
15. Искусство минимализма: создание современного дизайна в своем доме
16. Дизайн сада
17. Декорирование с текстилем
18. Принципы цветового баланса в дизайне: как создать гармоничное пространство
19. Топ-10 книг по дизайну интерьера, которые стоит прочитать
20. Дизайн комнаты для подростка: креативные идеи для стильного интерьера
студия дизайна квартир https://studiya-dizajna-intererov.ru/ .
купить кондиционеры купить кондиционеры .
ciprofloxacin generic price ciprofloxacin 500 mg tablet price cipro for sale
https://github.com/ForexRobotEasy/Larry-Williams
смотреть фильм
chloromycetin 2.5mg
Kredit 60000 Euro
sellrentcars.com
chinanewsapp.com
Intro
betvisa bangladesh
Betvisa bangladesh | Super Cricket Carnival with Betvisa!
IPL Cricket Mania | Kick off Super Cricket Carnival with bet visa.com
IPL Season | Exclusive 1,50,00,000 only at Betvisa Bangladesh!
Crash Games Heroes | Climb to the top of the 1,00,00,000 bonus pool!
#betvisabangladesh
Preview IPL T20 | Follow Betvisa BD on Facebook, Instagram for awards!
betvisa affiliate Dream Maltese Tour | Sign up now to win the ultimate prize!
https://www.bvthethao.com/
#betvisabangladesh #betvisabd #betvisaaffiliate
#betvisaaffiliatesignup #betvisa.com
Do lời hứa về trải nghiệm thú vị cá cược tốt hơn nhất và dịch vụ khách hàng chuyên trách, BetVisa tự tin là điểm đến lý tưởng cho những ai đam mê trò chơi trực tuyến. Hãy ghi danh ngay hôm nay và bắt đầu chuyến đi của bạn tại BetVisa – nơi niềm vui và may mắn chính là điều quan trọng.
Tìm hiểu Thế Giới Cá Cược Trực Tuyến với BetVisa!
Hệ thống BetVisa, một trong những công ty trò chơi hàng đầu tại châu Á, được thành lập vào năm 2017 và thao tác dưới giấy phép của Curacao, đã thu hút hơn 2 triệu người dùng trên toàn thế giới. Với lời hứa đem đến trải nghiệm cá cược an toàn và tin cậy nhất, BetVisa nhanh chóng trở thành lựa chọn hàng đầu của người chơi trực tuyến.
BetVisa không dừng lại ở việc cung cấp các trò chơi phong phú như xổ số, sòng bạc trực tiếp, thể thao trực tiếp và thể thao điện tử, mà còn mang đến cho người chơi những ưu đãi hấp dẫn. Thành viên mới đăng ký sẽ được tặng ngay 5 cơ hội miễn phí và có cơ hội giành giải thưởng lớn.
Đặc biệt, BetVisa hỗ trợ nhiều cách thức thanh toán linh hoạt như Betvisa Vietnam, cùng với các ưu đãi độc quyền như thưởng chào mừng lên đến 200%. Bên cạnh đó, hàng tuần còn có các chương trình khuyến mãi độc đáo như chương trình giải thưởng Sinh Nhật và Chủ Nhật Mua Sắm Điên Cuồng, mang đến cho người chơi cơ hội thắng lớn.
сериал смотреть
HD porn
Представляю наилучшую Букмекерскую контору – 1xbet
Топовая Букмекерская контора, советую 1xbet
http://flowervl.ru/
JDB online
JDB online | 2024 best online slot game demo cash
How to earn reels? jdb online accumulate spin get bonus
Hot demo fun: Quick earn bonus for ranking demo
JDB demo for win? JDB reward can be exchanged to real cash
#jdbonline
777 sign up and get free 2,000 cash: https://www.jdb777.io/
#jdbonline #democash #demofun #777signup
#rankingdemo #demoforwin
2000 cash: Enter email to verify, enter verify, claim jdb bonus
Play with JDB games an online platform in every countries.
Enjoy the Pleasure of Gaming!
Gratis to Join, Complimentary to Play.
Sign Up and Receive a Bonus!
JOIN NOW AND GET 2000?
We encourage you to acquire a trial entertaining welcome bonus for all new members! Plus, there are other unique promotions waiting for you!
Learn more
JDB – JOIN FOR FREE
Straightforward to play, real profit
Engage in JDB today and indulge in fantastic games without any investment! With a wide array of free games, you can savor pure entertainment at any time.
Rapid play, quick join
Appreciate your time and opt for JDB’s swift games. Just a few easy steps and you’re set for an amazing gaming experience!
Register now and generate money
Experience JDB: Instant play with no investment and the opportunity to win cash. Designed for effortless and lucrative play.
Submerge into the World of Online Gaming Adventure with Fun Slots Online!
Are you set to experience the adrenaline rush of online gaming like never before? Search no further than Fun Slots Online, your ultimate destination for exhilarating gameplay, endless entertainment, and stimulating winning opportunities!
At Fun Slots Online, we boast ourselves on providing a wide selection of engaging games designed to maintain you occupied and amused for hours on end. From classic slot machines to innovative new releases, there’s something for all to appreciate. Plus, with our user-friendly interface and uninterrupted gameplay experience, you’ll have no difficulty submerging straight into the excitement and savoring every moment.
But that’s not all – we also offer a range of particular promotions and bonuses to compensate our loyal players. From initial bonuses for new members to select rewards for our top players, there’s always something thrilling happening at Fun Slots Online. And with our safe payment system and 24-hour customer support, you can indulge in peace of mind conscious that you’re in good hands every step of the way.
So why wait? Sign up Fun Slots Online today and initiate your journey towards heart-pounding victories and jaw-dropping prizes. Whether you’re a seasoned gamer or just starting out, there’s never been a better time to participate in the fun and stimulation at Fun Slots Online. Sign up now and let the games begin!
Intro
betvisa india
Betvisa india | IPL 2024 Heat Wave
IPL 2024 Big bets, big prizes With Betvisa India
Exclusive for Sports Fans Betvisa Online Casino 50% Welcome Bonus
Crash Game Supreme Compete for 1,00,00,000 pot Betvisa.com
#betvisaindia
Accurate Predictions IPL T20 Tournament, Winner Takes All!
More than just a game | Betvisa dreams invites you to fly to malta
https://www.b3tvisapro.com/
#betvisaindia #betvisalogin #betvisaonlinecasino
#betvisa.com #betvisaapp
D?ch v? – Di?m D?n Tuy?t V?i Cho Ngu?i Choi Tr?c Tuy?n
Kham Pha Th? Gi?i Ca Cu?c Tr?c Tuy?n v?i BetVisa!
N?n t?ng ca cu?c du?c thanh l?p vao nam 2017 va ho?t d?ng theo ch?ng ch? tro choi Curacao v?i hon 2 tri?u ngu?i dung. V?i cam k?t dem d?n tr?i nghi?m ca cu?c ch?c ch?n va tin c?y nh?t, BetVisa nhanh chong tr? thanh l?a ch?n hang d?u c?a ngu?i choi tr?c tuy?n.
C?ng choi khong ch? cung c?p cac tro choi phong phu nhu x? s?, song b?c tr?c ti?p, th? thao tr?c ti?p va th? thao di?n t?, ma con mang l?i cho ngu?i choi nh?ng ph?n thu?ng h?p d?n. Thanh vien m?i dang ky s? nh?n t?ng ngay 5 vong quay mi?n phi va co co h?i gianh gi?i thu?ng l?n.
C?ng choi h? tr? nhi?u hinh th?c thanh toan linh ho?t nhu Betvisa Vietnam, ben c?nh cac uu dai d?c quy?n nhu thu?ng chao m?ng len d?n 200%. Ben c?nh do, hang tu?n con co cac chuong trinh khuy?n mai d?c dao nhu chuong trinh gi?i thu?ng Sinh Nh?t va Ch? Nh?t Mua S?m Dien Cu?ng, mang l?i cho ngu?i choi co h?i th?ng l?n.
V?i tinh cam k?t v? tr?i nghi?m ca cu?c t?t nh?t va d?ch v? khach hang chuyen nghi?p, BetVisa t? tin la di?m d?n ly tu?ng cho nh?ng ai dam me tro choi tr?c tuy?n. Hay dang ky ngay hom nay va b?t d?u hanh trinh c?a b?n t?i BetVisa – noi ni?m vui va may m?n chinh la di?u t?t y?u!
Переходим все сюда 1win
Крутой сайт 1win
монтаж кондиционера монтаж кондиционера .
nolvadex d clomid nolvadex tamoxifen and uterine thickening
ciprofloxacin 500mg buy online buy cipro online canada buy cipro
Viagra911: Ваша гарантированная поддержка максимального наслаждения!
Не довольны своей сексуальной жизнью? Мечтаете вернуть силу и уверенность в себе? Виагра 911 приходит на помощь! Наши таблетки для поднятия потенции — это надежное средство, которое дарит вам возможность наслаждаться полноценными и яркими сексуальными отношениями.
Наши таблетки для поднятия потенции у мужчин это:
– Сильная формула для быстрого и гарантированного эффекта.
– Усиление сексуальной выносливости и эрекции.
– Длительное удовлетворение как для вас, так и для вашего партнера.
– Доставка по всей Украине для вашего удобства.
Не откладывайте свое счастье на завтра! Закажите средство для повышения потенции у мужчин https://viagra911.com.ua/ прямо сейчас и почувствуйте всю мощь и радость сексуальной близости!
ivermectin price comparison ivermectin cost uk buy oral ivermectin
where to buy prednisone in australia can i purchase prednisone without a prescription otc prednisone cream
Рекомендую Букмекерскую контору – 1xbet
Надежная Букмекерская контора, советую 1xbet
fildena 100 mg canada
cipro
Gama Casino is a new gambling establishment. Gama casino opened in 2024, delighting players with big bonuses: 200% on account replenishment http://www.buscovivienda.net/foro/viewtopic.php?f=5&t=24790
can i buy priligy in mexico 3 TVmakerГў s market share in terms of revenue rose to 8 percent inthree months ended June 30 from 5
Рекомендую лучшую Букмекерскую контору – 1xbet
Надежная Букмекерская контора, рекомендую 1xbet
amoxicillin without prescription generic amoxicillin cost amoxicillin 500 tablet
Новый кондиционер: как его установить правильно
gree bora gree bora .
Секреты быстрой и качественной установки кондиционера
кондиционер на обогрев https://ustanovka-kondicionera-cena.ru/ .
Understanding the depths of web-based schools located in Alaska can actually be difficult, especially if you're a newcomer to the concept. I, too, handled these issues but discovered that these internet platforms give a high-quality, all-encompassing educational experience that rivals usual brick-and-mortar establishments.
From the sturdy landscapes of Juneau to the active ambiance of Anchorage, Alaska's online schools serve countless learning opportunities which are flexible and suitable. The snow-filled winters not anymore obstruct an individual's ability to reach schooling. Up-to-date technology rendered it possible to follow knowledge within the coziness and coziness of your own home.
Adaptability is a remarkable edge. You can modify your schedules in accordance with your obligations, that is very useful for workers or those with household obligations. Plus, the courses supplied are diverse, addressing a wide variety of subjects. Starting from introductory basics to higher specialties, you'll find something for everyone.
Alaska's online schools boast well-qualified teachers, active learning techniques, and supportive peer networks, making for a deep gratifying educational journey. If you're pondering over enrolling, I urge you to take that leap and explore Alaska's pioneering online education. Learn additional info about this groundbreaking approach to learning and how exactly it can maybe revamp your career and education trajectory. https://www.onlineschoolAK10.com/
– Как установить кондиционер: избавляемся от жары быстро и просто
установка кондиционера ціна https://ustanovka-kondicionera-cena.ru/ .
20 mg prednisone prednisone cost 10mg buy cheap prednisone
Hi to all, since I am genuinely eager of reading this website’s post to
be updated daily. It cosists of pleasant stuff.
My web page; 카지노사이트
casino sweet bonanza https://www.sweet-bonanza-game.ru/ .
Рекомендую топовую Букмекерскую контору – 1xbet
mГsto
Лучшая Букмекерская контора, рекомендую 1xbet
Article writing is also a fun, if you know afterward you
can write othyerwise it is compllex to write.
Feel free to surf to my web-site: 카지노사이트
Полезные советы
2. Шаг за шагом: установка кондиционера своими руками
3. Важные моменты при установке кондиционера в квартире
4. Специалисты или самостоятельная установка кондиционера?
5. 10 шагов к идеальной установке кондиционера
6. Подробная инструкция по установке кондиционера на балконе
7. Лучшие методы крепления кондиционера на стену
8. Как выбрать место для установки кондиционера в комнате
9. Секреты успешной установки кондиционера в частном доме
10. Рассказываем, как правильно установить сплит-систему
11. Необходимые инструменты для установки кондиционера
12. Какие документы нужны для оформления установки кондиционера?
13. Топ-5 ошибок при самостоятельной установке кондиционера
14. Установка кондиционера на потолке: особенности и нюансы
15. Когда лучше всего устанавливать кондиционер в доме?
16. Почему стоит доверить установку кондиционера профессионалам
17. Как подготовиться к установке кондиционера в жаркий сезон
18. Стоит ли экономить на установке кондиционера?
19. Подбор оптимальной мощности кондиционера перед установкой
20. Какие бывают типы кондиционеров: сравнение перед установкой
кондиционер обслуживание кондиционер обслуживание .
http://prednisonea.store/# buy prednisone online india
trazodone without a doctor prescription
https://stromectola.top/# stromectol without prescription
stromectol pill price ivermectin where to buy for humans ivermectin 4
Полезные советы
2. Шаг за шагом: установка кондиционера своими руками
3. Важные моменты при установке кондиционера в квартире
4. Специалисты или самостоятельная установка кондиционера?
5. 10 шагов к идеальной установке кондиционера
6. Подробная инструкция по установке кондиционера на балконе
7. Лучшие методы крепления кондиционера на стену
8. Как выбрать место для установки кондиционера в комнате
9. Секреты успешной установки кондиционера в частном доме
10. Рассказываем, как правильно установить сплит-систему
11. Необходимые инструменты для установки кондиционера
12. Какие документы нужны для оформления установки кондиционера?
13. Топ-5 ошибок при самостоятельной установке кондиционера
14. Установка кондиционера на потолке: особенности и нюансы
15. Когда лучше всего устанавливать кондиционер в доме?
16. Почему стоит доверить установку кондиционера профессионалам
17. Как подготовиться к установке кондиционера в жаркий сезон
18. Стоит ли экономить на установке кондиционера?
19. Подбор оптимальной мощности кондиционера перед установкой
20. Какие бывают типы кондиционеров: сравнение перед установкой
оборудование для кондиционирования оборудование для кондиционирования .
Как выбрать место для установки кондиционера: советы и рекомендации
монтаж кондиционера https://ustanovka-kondicionera-cena.ru/ .
where to get zithromax zithromax buy zithromax tablets for sale
Топовая Букмекерская контора – 1xbet
Лучшая Букмекерская контора, советую 1xbet
1. Как установить кондиционер в доме
обслуживание систем вентиляции обслуживание систем вентиляции .
Great – I should definitely pronounce, impressed with your web site. I had no trouble navigating through all tabs and related information ended up being truly easy to do to access. I recently found what I hoped for before you know it at all. Quite unusual. Is likely to appreciate it for those who add forums or anything, website theme . a tones way for your client to communicate. Nice task.
Here is my website :: https://campbellz296jct4.blogginaway.com/profile
Полезные советы
2. Шаг за шагом: установка кондиционера своими руками
3. Важные моменты при установке кондиционера в квартире
4. Специалисты или самостоятельная установка кондиционера?
5. 10 шагов к идеальной установке кондиционера
6. Подробная инструкция по установке кондиционера на балконе
7. Лучшие методы крепления кондиционера на стену
8. Как выбрать место для установки кондиционера в комнате
9. Секреты успешной установки кондиционера в частном доме
10. Рассказываем, как правильно установить сплит-систему
11. Необходимые инструменты для установки кондиционера
12. Какие документы нужны для оформления установки кондиционера?
13. Топ-5 ошибок при самостоятельной установке кондиционера
14. Установка кондиционера на потолке: особенности и нюансы
15. Когда лучше всего устанавливать кондиционер в доме?
16. Почему стоит доверить установку кондиционера профессионалам
17. Как подготовиться к установке кондиционера в жаркий сезон
18. Стоит ли экономить на установке кондиционера?
19. Подбор оптимальной мощности кондиционера перед установкой
20. Какие бывают типы кондиционеров: сравнение перед установкой
систем вентиляции и кондиционирования https://prodazha-kondcionerov.ru/ .
phenergan kosten
Porn
http://stromectola.top/# ivermectin 3mg dose
HD
What’s up everybody, here every person is sharing such
experience, therefore it’s fastidious to read this web site, and
I used to visit this web site every day.
https://prednisonea.store/# prednisone cream rx
non prescription prednisone 20mg prednisone 50 mg tablet cost prednisone without prescription
JDB demo
JDB demo | The easiest bet software to use (jdb games)
JDB bet marketing: The first bonus that players care about
Most popular player bonus: Daily Play 2000 Rewards
Game developers online who are always with you
#jdbdemo
Where to find the best game developer? https://www.jdbgaming.com/
#gamedeveloperonline #betsoftware #betmarketing
#developerbet #betingsoftware #gamedeveloper
Supports hot jdb demo beting software jdb angry bird
JDB slot demo supports various competition plans
Unlocking Success with JDB Gaming: Your Ultimate Bet Software Solution
In the realm of online gaming, discovering the right wager software is crucial for success. Introducing JDB Gaming – a leading source of creative gaming solutions crafted to improve the player experience and propel profits for operators. With a focus on easy-to-use interfaces, attractive bonuses, and a varied selection of games, JDB Gaming shines as a leading choice for both players and operators alike.
JDB Demo offers a glimpse into the world of JDB Gaming, offering players with an chance to undergo the excitement of betting without any hazard. With simple interfaces and seamless navigation, JDB Demo makes it easy for players to discover the vast selection of games on offer, from classic slots to engaging arcade titles.
When it concerns bonuses, JDB Bet Marketing paves the way with enticing offers that lure players and maintain them coming back for more. From the favored Daily Play 2000 Rewards to exclusive promotions, JDB Bet Marketing ensures that players are recognized for their allegiance and dedication.
With so numerous game developers online, finding the best can be a intimidating task. However, JDB Gaming emerges from the pack with its commitment to excellence and innovation. With over 150 online casino games to pick, JDB Gaming offers a bit for all, whether you’re a fan of slots, fish shooting games, arcade titles, card games, or bingo.
At the heart of JDB Gaming lies a commitment to offering the greatest possible gaming experience players. With a concentration on Asian culture and spectacular 3D animations, JDB Gaming sets itself apart as a pioneer in the industry. Whether you’re a gamer in search of excitement or an operator seeking a reliable partner, JDB Gaming has you covered.
API Integration: Seamlessly connect with all platforms for optimal business chances. Big Data Analysis: Remain ahead of market trends and understand player habits with extensive data analysis. 24/7 Technical Support: Enjoy peace of mind with expert and trustworthy technical support on hand 24/7.
In conclusion, JDB Gaming provides a winning combination of advanced technology, alluring bonuses, and unparalleled support. Whether you’re a gamer or an provider, JDB Gaming has everything that you need to excel in the arena of online gaming. So why wait? Join the JDB Gaming group today and unlock your full potential!
credito 850 euros
JDB online
JDB online | 2024 best online slot game demo cash
How to earn reels? jdb online accumulate spin get bonus
Hot demo fun: Quick earn bonus for ranking demo
JDB demo for win? JDB reward can be exchanged to real cash
#jdbonline
777 sign up and get free 2,000 cash: https://www.jdb777.io/
#jdbonline #democash #demofun #777signup
#rankingdemo #demoforwin
2000 cash: Enter email to verify, enter verify, claim jdb bonus
Play with JDB games an online platform in every countries.
Enjoy the Joy of Gaming!
Costless to Join, Costless to Play.
Sign Up and Get a Bonus!
SIGN UP NOW AND GET 2000?
We urge you to acquire a demo enjoyable welcome bonus for all new members! Plus, there are other special promotions waiting for you!
Find out more
JDB – FREE TO JOIN
Easy to play, real profit
Join JDB today and indulge in fantastic games without any investment! With a wide array of free games, you can delight in pure entertainment at any time.
Fast play, quick join
Value your time and opt for JDB’s swift games. Just a few easy steps and you’re set for an amazing gaming experience!
Join now and receive money
Experience JDB: Instant play with no investment and the opportunity to win cash. Designed for effortless and lucrative play.
Submerge into the Domain of Online Gaming Stimulation with Fun Slots Online!
Are you ready to experience the sensation of online gaming like never before? Seek no further than Fun Slots Online, your ultimate stop for heart-pounding gameplay, endless entertainment, and thrilling winning opportunities!
At Fun Slots Online, we take pride ourselves on presenting a wide array of engaging games designed to retain you occupied and pleased for hours on end. From classic slot machines to innovative new releases, there’s something for all to enjoy. Plus, with our user-friendly interface and smooth gameplay experience, you’ll have no problem diving straight into the activity and delighting in every moment.
But that’s not all – we also give a selection of special promotions and bonuses to compensate our loyal players. From introductory bonuses for new members to privileged rewards for our top players, there’s always something thrilling happening at Fun Slots Online. And with our safe payment system and 24-hour customer support, you can savor peace of mind conscious that you’re in good hands every step of the way.
So why wait? Join Fun Slots Online today and begin your adventure towards heart-pounding victories and jaw-dropping prizes. Whether you’re a seasoned gamer or just starting out, there’s never been a better time to participate in the fun and thrills at Fun Slots Online. Sign up now and let the games begin!
Выбирайте в интернет-магазине грифы для штанг и гантелей Grify-Dlya-Shtang.ru с любым посадочным диаметром для силовых занятий. Это необходимое тренировочное оборудование для отдела свободных весов в тренажерных залах.Российский изготовитель рекомендует большой каталог олимпийских грифов по выгодным ценам напрямую у завода-производителя. Все наборы поступают в реализацию с замками для блинов. Отечественный завод изготавливает инвентарь из стали лучших марок. Производимые изделия не нуждаются в постоянном обслуживании и рассчитаны на длительную работу в клубах. Для защиты от ржавчины все товары хромируются. Покупая у российского производителя вы получаете прочные снаряды для удобных занятий.
zithromax 500 mg lowest price online zithromax price south africa zithromax online paypal
payusainvest.com
south-columbia.com
Intro
betvisa vietnam
Betvisa vietnam | Grand Prize Breakout!
Betway Highlights | 499,000 Extra Bonus on betvisa com!
Cockfight to win up to 3,888,000 on betvisa game
Daily Deposit, Sunday Bonus on betvisa app 888,000!
#betvisavietnam
200% Bonus on instant deposits—start your win streak!
200% welcome bonus! Slots and Fishing Games
https://www.betvisa.com/
#betvisavietnam #betvisagame #betvisaapp
#betvisacom #betvisacasinoapp
Birthday bash? Up to 1,800,000 in prizes! Enjoy!
Friday Shopping Frenzy betvisa vietnam 100,000 VND!
Betvisa Casino App Daily Login 12% Bonus Up to 1,500,000VND!
Khám phá Thế Giới Cá Cược Trực Tuyến với BetVisa!
Hệ thống BetVisa, một trong những công ty trò chơi hàng đầu tại châu Á, được thành lập vào năm 2017 và thao tác dưới phê chuẩn của Curacao, đã đưa vào hơn 2 triệu người dùng trên toàn thế giới. Với cam kết đem đến trải nghiệm cá cược an toàn và tin cậy nhất, BetVisa sớm trở thành lựa chọn hàng đầu của người chơi trực tuyến.
BetVisa không chỉ cung cấp các trò chơi phong phú như xổ số, sòng bạc trực tiếp, thể thao trực tiếp và thể thao điện tử, mà còn mang đến cho người chơi những ưu đãi hấp dẫn. Thành viên mới đăng ký sẽ được tặng ngay 5 vòng quay miễn phí và có cơ hội giành giải thưởng lớn.
Đặc biệt, BetVisa hỗ trợ nhiều hình thức thanh toán linh hoạt như Betvisa Vietnam, cùng với các ưu đãi độc quyền như thưởng chào mừng lên đến 200%. Bên cạnh đó, hàng tuần còn có các chương trình khuyến mãi độc đáo như chương trình giải thưởng Sinh Nhật và Chủ Nhật Mua Sắm Điên Cuồng, mang đến cho người chơi cơ hội thắng lớn.
Với lời hứa về trải nghiệm thú vị cá cược tốt hơn nhất và dịch vụ khách hàng kỹ năng chuyên môn, BetVisa tự hào là điểm đến lý tưởng cho những ai đam mê trò chơi trực tuyến. Hãy ghi danh ngay hôm nay và bắt đầu chuyến đi của bạn tại BetVisa – nơi niềm vui và may mắn chính là điều tất yếu.
Intro
betvisa bangladesh
Betvisa bangladesh | Super Cricket Carnival with Betvisa!
IPL Cricket Mania | Kick off Super Cricket Carnival with bet visa.com
IPL Season | Exclusive 1,50,00,000 only at Betvisa Bangladesh!
Crash Games Heroes | Climb to the top of the 1,00,00,000 bonus pool!
#betvisabangladesh
Preview IPL T20 | Follow Betvisa BD on Facebook, Instagram for awards!
betvisa affiliate Dream Maltese Tour | Sign up now to win the ultimate prize!
https://www.bvthethao.com/
#betvisabangladesh #betvisabd #betvisaaffiliate
#betvisaaffiliatesignup #betvisa.com
Vì sự cam kết về kinh nghiệm cá cược tốt nhất và dịch vụ khách hàng chuyên môn, BetVisa tự tin là điểm đến lý tưởng cho những ai nhiệt huyết trò chơi trực tuyến. Hãy tham gia ngay hôm nay và bắt đầu hành trình của bạn tại BetVisa – nơi niềm vui và may mắn chính là điều không thể thiếu được.
Khám phá Thế Giới Cá Cược Trực Tuyến với BetVisa!
Dịch vụ BetVisa, một trong những nền tảng hàng đầu tại châu Á, ra đời vào năm 2017 và thao tác dưới bằng của Curacao, đã đưa vào hơn 2 triệu người dùng trên toàn thế giới. Với lời hứa đem đến trải nghiệm cá cược đảm bảo và tin cậy nhất, BetVisa nhanh chóng trở thành lựa chọn hàng đầu của người chơi trực tuyến.
BetVisa không chỉ cung cấp các trò chơi phong phú như xổ số, sòng bạc trực tiếp, thể thao trực tiếp và thể thao điện tử, mà còn mang đến cho người chơi những ưu đãi hấp dẫn. Thành viên mới đăng ký sẽ được tặng ngay 5 phần quà miễn phí và có cơ hội giành giải thưởng lớn.
Đặc biệt, BetVisa hỗ trợ nhiều phương thức thanh toán linh hoạt như Betvisa Vietnam, cùng với các ưu đãi độc quyền như thưởng chào mừng lên đến 200%. Bên cạnh đó, hàng tuần còn có các chương trình khuyến mãi độc đáo như chương trình giải thưởng Sinh Nhật và Chủ Nhật Mua Sắm Điên Cuồng, mang đến cho người chơi cơ hội thắng lớn.
how to use vidalista 60
https://azithromycina.pro/# zithromax tablets
У слота Gates of Olympus играть демо бонуска позволяет по тем же техническим характеристикам, какие есть в основной версии. Коэффициенты возврата и частота выплаты призов не меняются в принципе. Купить бонусный раунд у слота нельзя gates of olympus большой выигрыш
http://amoxicillina.top/# amoxicillin buy canada
LГҐn 8000 kr
amoxicillin 875 125 mg tab ampicillin amoxicillin where to buy amoxicillin pharmacy
кондиционер ballu кондиционер ballu .
хоккей прогноз бесплатно
https://stromectola.top/# ivermectin 0.5
кондиционер мастер https://multisplit-sistemy-kondicionirovaniya.ru/ .
https://amoxicillina.top/# amoxicillin 500mg capsules antibiotic
naprelan 20mg
кондиционер цена https://multisplit-sistemy-kondicionirovaniya.ru/ .
Полезные советы
2. Шаг за шагом: установка кондиционера своими руками
3. Важные моменты при установке кондиционера в квартире
4. Специалисты или самостоятельная установка кондиционера?
5. 10 шагов к идеальной установке кондиционера
6. Подробная инструкция по установке кондиционера на балконе
7. Лучшие методы крепления кондиционера на стену
8. Как выбрать место для установки кондиционера в комнате
9. Секреты успешной установки кондиционера в частном доме
10. Рассказываем, как правильно установить сплит-систему
11. Необходимые инструменты для установки кондиционера
12. Какие документы нужны для оформления установки кондиционера?
13. Топ-5 ошибок при самостоятельной установке кондиционера
14. Установка кондиционера на потолке: особенности и нюансы
15. Когда лучше всего устанавливать кондиционер в доме?
16. Почему стоит доверить установку кондиционера профессионалам
17. Как подготовиться к установке кондиционера в жаркий сезон
18. Стоит ли экономить на установке кондиционера?
19. Подбор оптимальной мощности кондиционера перед установкой
20. Какие бывают типы кондиционеров: сравнение перед установкой
обслуживание кондиционеров и вентиляции обслуживание кондиционеров и вентиляции .
Intro
betvisa india
Betvisa india | IPL 2024 Heat Wave
IPL 2024 Big bets, big prizes With Betvisa India
Exclusive for Sports Fans Betvisa Online Casino 50% Welcome Bonus
Crash Game Supreme Compete for 1,00,00,000 pot Betvisa.com
#betvisaindia
Accurate Predictions IPL T20 Tournament, Winner Takes All!
More than just a game | Betvisa dreams invites you to fly to malta
https://www.b3tvisapro.com/
#betvisaindia #betvisalogin #betvisaonlinecasino
#betvisa.com #betvisaapp
Khám phá Thế Giới Cá Cược Trực Tuyến với BetVisa!
BetVisa Vietnam, một trong những nền tảng hàng đầu tại châu Á, ra đời vào năm 2017 và thao tác dưới phê chuẩn của Curacao, đã có hơn 2 triệu người dùng trên toàn thế giới. Với lời hứa đem đến trải nghiệm cá cược đảm bảo và tin cậy nhất, BetVisa sớm trở thành lựa chọn hàng đầu của người chơi trực tuyến.
BetVisa không dừng lại ở việc cung cấp các trò chơi phong phú như xổ số, sòng bạc trực tiếp, thể thao trực tiếp và thể thao điện tử, mà còn mang đến cho người chơi những ưu đãi hấp dẫn. Thành viên mới đăng ký sẽ được tặng ngay 5 cơ hội miễn phí và có cơ hội giành giải thưởng lớn.
Đặc biệt, BetVisa hỗ trợ nhiều cách thức thanh toán linh hoạt như Betvisa Vietnam, cùng với các ưu đãi độc quyền như thưởng chào mừng lên đến 200%. Bên cạnh đó, hàng tuần còn có các chương trình khuyến mãi độc đáo như chương trình giải thưởng Sinh Nhật và Chủ Nhật Mua Sắm Điên Cuồng, mang đến cho người chơi cơ hội thắng lớn.
Vì sự cam kết về trải thảo cá cược tinh vi nhất và dịch vụ khách hàng chuyên môn, BetVisa tự hào là điểm đến lý tưởng cho những ai nhiệt huyết trò chơi trực tuyến. Hãy tham gia ngay hôm nay và bắt đầu hành trình của bạn tại BetVisa – nơi niềm vui và may mắn chính là điều quan trọng.
ремонт кондиціонера ремонт кондиціонера .
Топовая Букмекерская контора – 1win
Надежная Букмекерская контора, советую 1win
no prescription pharmacy pills no prescription canada prescriptions by mail
dailymoneysource.com
moneytimenews.com
Изучайте на ресурсе грифы для штанг Grify-Dlya-Shtang.ru с разным посадочным диаметром для силовых тренировок. Это востребованное спортивное оснащение для отдела свободных весов в фитнес клубах.Российский изготовитель реализует большой ассортимент прямых грифов по выгодным ценам напрямую у завода-производителя. Все наборы поступают в реализацию с фиксаторами для дисков. Завод из России изготавливает инвентарь из стали высших марок. Производимые изделия не нуждаются в постоянном обслуживании и ориентированы на длительную работу в спортивных залах. Для предохранения от коррозии все металлические поверхности никелируются. Приобретая у российского изготовителя вы получаете эффективные снаряды для комфортных тренировок.
online pharmacy discount code: offshore pharmacy no prescription – pharmacy coupons
pyridium for sale
meds no prescription mexican pharmacy no prescription buy prescription drugs without a prescription
erectile dysfunction online prescription: cheapest ed pills – ed prescriptions online
https://zelpgo.ru
кондиционер в комнату кондиционер в комнату .
Лучшая Букмекерская контора – 1win
Букмекерская контора №1, советую 1win
best online slots site kenya https://www.casinoonline.co.ke/ .
online ed pharmacy cheap ed medicine online ed pills
cost of ed meds: edmeds – online ed medications
canada prescription online canadian pharmacy non prescription canadian pharmacy no prescription required
very informative articles or reviews at this time.
buying erectile dysfunction pills online: erectile dysfunction drugs online – ed online prescription
Выбирая нас, вы получаете быструю и профессиональную эвакуацию по разумной цене · Любая сложность. 10-летний опыт. Профессиональный подход. Официально https://yslygi66.ru/zapchasti-dlya-kuzova
With thanks, Ample material!
Букмекерская контора №1 в мире, советую 1win
Лучшая Букмекерская контора на просторах – 1win
canada pharmacy coupon online pharmacy non prescription drugs promo code for canadian pharmacy meds
canadian pharmacy discount code: canada pharmacy not requiring prescription – no prescription needed pharmacy
Based on God’s instructions, Abraham travelled to a place called Canaan where the Canaanites lived. There is no reason given for God’s choice of Palestine/Canaan for Abraham to journey to доставка грузов из китая в москву калькулятор
Discover exquisite villas and luxurious townhouses in the spectacular mega-development of DAMAC Lagoons Views. Indulge in opulent living at unbeatable prices from renowned developer DAMAC Properties. Don’t miss out on your dream home in this unrivaled paradise.
Boostaro is a natural dietary supplement for male health, enhancing circulation and overall bodily functions. Supports wellness with natural ingredients.
Sugar Defender is the rated blood sugar formula with an advanced blend of 24 proven ingredients that support healthy glucose levels and natural weight loss.
FitSpresso™ is a nutritional supplement that uses probiotics to help you lose weight.
ZenCortex Research’s contains only the natural ingredients that are effective in supporting incredible hearing naturally.A unique team of health and industry professionals dedicated to unlocking the secrets of happier living through a healthier body.
SynoGut is a dietary supplement that claims to promote and maintain excellent gut and digestive health.
rx pharmacy no prescription: online pharmacy non prescription drugs – pharmacy coupons
Medications and prescription drug information for consumers and medical health professionals. Online database of the most popular drugs and their side effects, interactions, and use.
FlowForce Max is an innovative, natural and effective way to address your prostate problems, while addressing your energy, libido, and vitality.
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.国产线播放免费人成视频播放
generic ed meds online generic ed meds online where can i buy erectile dysfunction pills
Thank you for great content. Hello Administ. 国产线播放免费人成视频播放
Топовая Букмекерская контора на просторах – 1win
Букмекерская контора №1 в мире 1win
vai a questo sito web
Як обрати тактичні кросівки з урахуванням вашого стилю
військові тактичні кросівки літні https://vijskovikrosivkifvgh.kiev.ua/ .
Are you seeking for a way to feel better? Unlock the trusted source for health and wellness right here! All of your health issues and difficulties must be addressed using the key.
kurdish porn
Нові тренди в світі тактичних кросівок
тактичні чоловічі кросівки https://vijskovikrosivkifvgh.kiev.ua/ .
Топовая Букмекерская контора в мире – 1win
Лучшая Букмекерская контора №1 в мире 1win
Як вибрати стильні та комфортні тактичні кросівки
кросівки тактичні літні купити https://vijskovikrosivkifvgh.kiev.ua/ .
low cost ed meds: ed online meds – buy erectile dysfunction treatment
online meds no prescription: no prescription drugs – online pharmacy without a prescription
LГҐn 4000
Thank you great post. Hello Administ .国产线播放免费人成视频播放
Thank you great post. Hello Administ .国产线播放免费人成视频播放
Lessons waiting for you at our Virtuoso School: violin classes near me Unlock your creative potential at Virtuoso School of Music and Art.
pulmicort
PЕЇjДЌka 28000 KДЌ
cheapest erectile dysfunction pills: get ed prescription online – best ed meds online
Descubre los casinos en linea mas populares de Peru
casino en linea peru casino en linea peru .
Головні переваги тактичних кросівок у порівнянні з іншими видами взуття
воєнні тактичні кросівки воєнні тактичні кросівки .
medicine with no prescription: buy medications without prescriptions – canada mail order prescription
чем более игрок зачислит на кошелек аккаунта, тем шире круг баллов
получит.
Visit my web blog :: казино онлайн рейтинг лучших
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.儿童色情片
A casa de apostas mais fiavel do mundo – 1win
Melhor casa de apostas n? 1 do mundo 1win
Thank you for great information. Hello Administ . 国产线播放免费人成视频播放
https://vipbuket64.ru/
online pharmacies no prescription usa buying online prescription drugs canadian pharmacy online no prescription
The latest news and reviews in the world of tech, automotive, gaming, science, and entertainment
The Voice of Alaska’s Capital Since 1912 juneau news
LГҐn 5000 kr
?Gana grandes premios en los casinos en linea en Peru!
casino en linea peru casino en linea peru .
erectile dysfunction meds online best online ed pills cheap ed drugs
Progenifix is a revolutionary wellness and vitality supplement that is designed to promote overall health and vitality.
ZenCortex Research’s contains only the natural ingredients that are effective in supporting incredible hearing naturally.
The modern Cologne-Bonn airport annually transports millions of passengers
to 130 https://www.milehighreport.com/users/parkingnearairports12/.
https://casinvietnam.shop/# choi casino tr?c tuy?n tren di?n tho?i
PBN sites
We will create a system of privately-owned blog network sites!
Benefits of our private blog network:
We perform everything so google doesn’t comprehend that THIS IS A self-owned blog network!!!
1- We purchase domain names from separate registrars
2- The primary site is hosted on a VPS hosting (VPS is fast hosting)
3- Other sites are on distinct hostings
4- We assign a separate Google profile to each site with verification in Google Search Console.
5- We develop websites on WP, we don’t employ plugins with assisted by which Trojans penetrate and through which pages on your websites are generated.
6- We refrain from duplicate templates and utilize only exclusive text and pictures
We refrain from work with website design; the client, if desired, can then edit the websites to suit his wishes
http://casinvietnam.com/# casino tr?c tuy?n
O escritorio da casa de apostas mais fiavel – 1win
Casa de apostas confiavel n? 1 1win
6000 euro lenen
интернет-магазин спортивной экипировки
Мы гарантируем вам низкие цены и отличное качество за счет больших объемов закупок у заводов-изготовителей напрямую упаковка в спб
интернет-магазин спортивной экипировки
Greetings I am so excited I found your web site, I really found you by error, while I was browsing on Askjeeve for something else, Nonetheless I am here now and would just like to say kudos for a marvelous post and a all round interesting blog (I also love the theme/design), I don’t have time to read it all at the minute but I have book-marked it and also added your RSS feeds, so when I have time I will be back to read more, Please do keep up the awesome work. darkmarket link https://darknetmarketstore.com
скачать pari текст песни
menthol inhalers
скачать пари текст
Casa de apostas fiavel, recomendo-a – 1win
Toda la emocion de los casinos en linea en Peru
mejor casino online peru online casino games peru .
http://casinvietnam.com/# casino tr?c tuy?n vi?t nam
A melhor casa de apostas, recomendo-a 1win
– Купить кран смеситель для ванной
шаровые краны цена https://krany-sharovye-nerzhaveyushie-msk.ru/ .
https://casinvietnam.shop/# danh bai tr?c tuy?n
Доступные цены
– Кран-буксировщик для душа: плюсы и минусы
краны из нержавеющей стали краны из нержавеющей стали .
Актив. розвиток а. в Одесі почався після https://medapparatura.com.ua/catalog/oftalmologiya/ відкриття 1903 каф. Як окрема галузь медицини О.
Find the latest technology news and expert tech product reviews. Learn about the latest gadgets and consumer tech products for entertainment, gaming, lifestyle and more.
Советы экспертов
– Кран-буксировщик для ванны: преимущества и покупка
шаровые краны купить шаровые краны купить .
allegra
https://vipbuket64.ru/
на замовлення можливе виготовлення нестандартних дверних систем, ціна на які, природно, https://okna-atlant.com.
Доставка по всей России
– Кран для биде: широкий выбор и выгодные цены
кран нержавеющий https://krany-sharovye-nerzhaveyushie-msk.ru/ .
Nice article inspiring thanks. Hello Administ . 国产线播放免费人成视频播放
Завораживающие возможности онлайн азартных игр простираются в виртуальной реальности, где каждый участник погружается в увлекательное путешествие по миру азарта и волнения http://forum.computest.ru/post/628764/#p628764
Занадто важкі двері будуть негативними https://okna-atlant.com.ua/vigotovlennya-metalevuh-dverej/ впливати на стіну.
грузоперевозки из китая https://www.dostavka-gruzov-is-kitaya.ru/ .
Здравствуйте. по итогу теста Работа для девушек Геленджик вышло: Б,В,а в,Б.
orlistat
carsdirecttoday.com
repairtoday7.com
Обзор рейтинга букмекеров
букмекерские приложения самая лучшая букмекерская контора в интернете .
Recomendo esta casa de apostas a toda a gente 1win
A melhor casa de apostas 1win
Скидки и акции
– Кран для раковины: выбор и покупка
кран купить кран купить .
Хіршмана відкрита міська очна лікарня, https://medapparatura.com.ua/catalog/aparati-shvl-ta-komplektuyuchi/ яку офіційно названо його ім’ям. Головіна був вчений з мир.
Great post thank you. Hello Administ . 国产线播放免费人成视频播放
Market Analyst specializes in must-know news highlights, in-depth analysis, and overviews of companies as well as industries. https://marketanalyst.us/
кортинефф купить спб в наличии в аптеках
pret 4500 euros
Green Lovers is dedicated to making news and topics across sustainability and innovation accessible to all. We help bring awareness to global issues and solutions, and hope to inspire you to make simple changes to your daily habits and lifestyle. https://greenlovers.us/
new cs:go skin bets sites 2024
DreamDive specializes in content that sparks conversations around news, entertainment and pop culture. https://dreamdive.us/
поэтому, в нашей статье мы тщательно объясним, http://www.ifoxy.ru/viewtopic.php?f=95&t=30398 как проводятся госы в школах.
Çok işime yaradı bende bunu nasıl yapacağımı araştırıyorum. Paylaşım için teşekkür ederim.
Производство аквариумов в Москве и Московской области https://akvariumy-na-zakaz.ru/
Купив «корочки», вы сможете аргументировано вести переговоры с начальством о своем продвижении по службе, увеличении оклада, http://donsloboda.
A casa de apostas mais confiavel 1win
курсы барбера с нуля в спб burberi.ru .
anbefalt nettsted
5. проблемы с банковским получением бумаг в соответствии с непреодолимыми обстоятельствами.
Feel free to surf to my site; http://mockwa.com/forum/thread-147888/
Prestito di 800 euro
Сфера онлайн гэмблинга стремительно развивается, предлагая увлекательные игры и возможность выигрыша http://1.reshetki-moskva.ru/index.php?option=com_k2&view=itemlist&task=user&id=193344
Recomendo a melhor casa de apostas 1win
TornadoCash: Your gateway to anonymous transactions on Ethereum. Keep your financial activities private with this decentralized mixer
A casa de apostas mais confiavel, eu recomendo 1win
Если доход может быть не слишком высоким,
при этом вы прокачаете коммуникативные способности,
разовьете понимание маркетинга, станете.
my page – Работа девушкам эскорт Красноярск
Hi to every one, it’s genuinely a pleasant for me to go to see this website, it includes important Information. darknet markets 2024 https://darknetmarketgate.com
«Дверной рай» предоставляет возможность купить двери из массива для дома в минске.
Melhor casa de apostas legal 1win
які переваги французького Скління балконів?
Escritorio da casa de apostas n? 1 1win
znaleЕєД‡ tutaj
Рейтинг букмекера: критерии выбора
официальные сайты букмекерских контор мобильные букмекерские конторы .
Users can participate within the presale with their Ethereum, BNB, Tether, or credit card, with a single GBTC selling for roughly $0.65.
LГҐn 20000 kr
https://corti-med.ru/
1xbet суды
livinghawaiitravel.com
сайт знакомств пообщаемся
скачать детские фильмы
онлайн казино все казино
bmoneyfinder.com
порно бисексуалов
best cs skin casino site 2024
1xbet alternative
сайт знакомств лайф
порно тикток
выигрышное казино онлайн
1xbet оператор
Melhor escritorio de apostas legal 1win
Good info. Lucky me I reach on your website by accident, I bookmarked it. 現場兒童色情片
I really love to read such an excellent article. Helpful article. Hello Administ . 国产线播放免费人成视频播放
Thank you for content. Area rugs and online home decor store. Hello Administ . 国产线播放免费人成视频播放
Hello! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.兒童色情
Thank you for great article. Hello Administ .国产线播放免费人成视频播放
Casa de apostas n? 1 do mundo 1win
бдсм сайт знакомств
порно блондинки
скачать фильм борат
лучших онлайн казино
marketing 1xbet
Низкие цены на изготовление аквариумов https://akvariumy-na-zakaz.ru/
мав знакомства сайт
холоп фильм скачать
казино открыть онлайн
1xbet uzbekcha skachat
сайт знакомств израиль
порно доминирование
казино онлайн best
1xbet нарды
Hey! Would you mind if I sgare your blog with my facebook group?
There’s a lot of people that I think would really appreciate
your content. Please let me know. Thanks
Feel free to visit my site; 카지노사이트
фотострана сайт знакомств
мамки порно
фильмы торрент скачать
онлайн казино но только
наебалово 1xbet
сайт знакомств геленджик
скачать фильм дюна
казино деньги онлайн
1xbet wikipedia
порно косплей
скачать фильм лолита
лимиты 1xbet
Torrez Darknet Drugs Market
http://mmd32xdcmzrdlpoapkpf43dxig5iufbpkkl76qnijgzadythu55fvkqd.onion/ –Tor Browser
сайт фотострана знакомства
гача порно
домовой фильм скачать
казино 1win онлайн
1xbet телефон техподдержки
порно рисунки
скачать фильм бивень
при возникновении трудностей или проблема в онлайн-покупке, накамерный монитор звоните нам по телефонам. 14. Камеры для ловли рыбы.
Also visit my web site https://fotofrog.ru/categories/nakamernyi-svet
онлайн буй казино
Как узнать рейтинг букмекера на спорт
самая лучшая букмекерская контора в интернете лучшая букмекерская онлайн .
https://nullkong.com/
https://web.archive.org/web/20200706002503/https://wikicompromat.org/wiki/Станислав_Дмитриевич_Кондрашов
Яркий цвет ладони с четкими линиями отражает удачу в современных дней.
Feel free to visit my page; Остров на линии ума
A melhor casa de apostas legal, eu a recomendo 1win
Everyone loves it when people come togdther and share ideas.
Great site, continue the good work!
Also visiit my website: 카지노사이트
Рюкзак тактичний
рюкзаки тактичні військові рюкзаки тактичні військові .
при возникновении вопросов или трудностей в онлайн-покупке, аксессуары для
клеток купить связывайтесь с нами по телефонам.
14.
My blog post: portkeys
A melhor casa de apostas do mundo 1win
A casa de apostas n? 1 mais confiavel do mundo 1win
Вы можете заказать у нас услуги грузчиков в Москве и Московской области для любых работ, начиная с обычных погрузо-разгрузочных и заканчивая всеми видами переездов и такелажных работ грузчик разнорабочий
https://web.archive.org/web/20200706002503/https://wikicompromat.org/wiki/Станислав_Дмитриевич_Кондрашов
Supercharge Your SEO with Our Premium Databases!
Want to improve your SEO rankings and save time? Our premium databases for XRumer and GSA Search Engine Ranker are just what you need!
What do our databases include?
• Active links: Get access to constantly updated lists of active links from profiles, posts, forums, guestbooks, blogs, and more. No more wasting time on dead links!
• Verified and identified links: Our premium databases for GSA Search Engine Ranker include verified and identified links, categorized by search engines. This means you get the highest quality links that will help you rank higher.
• Monthly updates: All of our databases are updated monthly to ensure you have the most fresh and effective links.
Choose the right option for you:
• XRumer Database:
o Premium database with free updates: $119
o Premium database without updates: $38
• Fresh XRumer Database:
o Fresh database with free updates: $94
o Fresh database without updates: $25
• GSA Search Engine Ranker Verified Links:
o GSA Search Engine Ranker activation key: $65 (includes database)
o Fresh database with free updates: $119
o Fresh database without updates: $38
Don’t waste time on outdated or inactive links. Invest in our premium databases and start seeing results today!
Order now!
P.S. By purchasing GSA Search Engine Ranker from us, you get a high-quality product at a competitive price. Save your resources and start improving your SEO rankings today!
To contact us, write to telegram https://t.me/DropDeadStudio
https://moslabor.ru
Greetings! Very helpful advice in this particular article!
It is the little changes that make the most important changes.
Thanks a lot for sharing!
Aconselho voce a usar os servicos dessa empresa de apostas 1win
Minha recomendacao e o escritorio desta casa de apostas 1win
spring dan naar deze website
на таких сервисах информация направляется в готовом и интересном виде, https://magicjob.biz/city/moskva портфолио складывается.
https://nullkong.com/
Як знайти найкращий тактичний рюкзак
Комфорт та зручність
рюкзак тактичний рюкзак тактичний .
21000 Euro Kredit
Hello my loved one! I want to say that this article is
awesome, nice written and include almostt all significant infos.
I’d like to see more posts like this .
Also visit my web blog … 카지노사이트
Prefiro essa empresa de apostas 1win
в средние века Пальцы рук была довольно распространена, считалась ближайшей среди основных наук и преподавалась в ведущих европейских.
Feel free to visit my blog post … https://hiro.su/nikolay/liniya-sudby-na-ruke/
Eu recomendo esta casa de apostas para apostas 1win
Рекомендую и пожалуй лучшая автоматическая линия порошковой покраски
sex porn
Обзор популярних моделей
Якість і зручність
купити рюкзаки тактичні купити рюкзаки тактичні .
Grandes vitórias podem ser encontradas no jogo Fortune Tiger
Entre e aproveite o jogo Fortune Tiger
Everything is very open and very clear explanation of issues. was truly information.活婴儿色情片
Які рекомендації варто враховувати
Провідники технологій
тактичні рюкзаки купити https://ryukzakivijskovibpjgl.kiev.ua/ .
перевозки грузов через казахстан https://perevozka-iz-kz.ru/
Муж Широковой, школьный учитель Алексей является исполнителем громкого скандала: его ученица записала на камеру, https://soderganki.biz/city/voronezh.
https://prilozhenie-winline.ru/
Желаете улучшить свои языковые навыки? Окунитесь в увлекательный мир английского языка с помощью наших кинофильмов и сериалов на английском и британском языках. Насладитесь процессом обучения, погружаясь в привлекательные сюжеты и диалоги на языке оригинала. Наши фильмы и сериалы на английском не только помогут вам расширить словарный запас, но и улучшат понимание английской речи и культуры. Используйте просмотры сериалов на английском в качестве эффективного метода освоения. Подробнее здесь https://serialy-na-angliiskom.pp.ua
sumycin 500mg
This is really interesting, You’re an excessively professional
blogger. I’ve joined youjr feed and look aead to seeking more of your fantastic
post. Also, I have shared your siute in my social networks
Here is my blog post – 카지노사이트
https://virtual-local-numbers.com/countries/1300-new-york-phone.number.html
HD porn
famciclovir generika bestellen
Vale a pena prestar atencao a essa empresa de apostas 1win
newsgary.com
womenbabe.com
Разберем https://favoritka.work/city/moskva самые денежные направления.
Jogo muito interessante com ganhos Fortune Tiger
Venha e ganhe o jogo Fortune Tiger
Eu recomendo esta casa de apostas 1win
почему многие готовы заказать документ о высшем http://arkosgold.ru/index.php?subaction=userinfo&user=ofuhyr образовании?
отправка контейнера из казахстана в россию https://perevozka-iz-kz.ru/
Eu confio nessa empresa de apostas 1win
The innovative interior, and non-standard and large format of bonus promotions provide incredibly comfortable conditions for participants, fans https://totalfratmove.com/articles/1win_promo_code_bonus_code.html.
best xxx
Торговля на Kraken. Завершив регистрацию на официальной сайте Кракен, пройдя минимум первые две ступени верификации (0-я и 1-я), а также внеся средства на депозит, можно заниматься зарабатыванием на разнице ценовых курсов либо при надобности обменивать криптовалюту в требуемых направлениях Официальный сайт Kraken через TOR
elavil ohne rezept bestellen
https://winline-prilozhenie.ru/
Aconselho um escritorio de apostas confiavel 1win
cliquez pour lire
i like to play whit my fat live cams blonde and stick a 1 finger in my ass
Hello, you used to write great, but the last
few posts have been kinda boring… I miss your great writings.
Past several posts are just a little out of track! come
on!
Take a look at my web blog :: 2001 bmw x5
Confio na melhor casa de apostas – 1win
Conselho da melhor casa de apostas 1win
Verwenden Sie Ihre IT-Systeme, um den QR-Code direkt mit neuen Produkten zu verknüpfen und
das Risiko zu minimieren|zu minimieren|zu reduzieren}
Kosten suchen europaletten epal ihr Produkt.
Visit my blog post; https://www.willhaben.at/iad/kaufen-und-verkaufen/d/ganz-neue-europaletten-epal-kaufen-zertifiziert-holzpaletten-moebelpaletten-1903914240/
wedding video como
каждый из подобных документов отражает вашу учебную и экспертную http://words-are-dust.blogspot.com/2014/03/qt.html историю.
Tor2door Darknet Drugs Market
http://d5lqhle57oi6pcdt254dspanbqjivpufslqvtbrwllth2iapipjq7vid.onion/ –Tor Browser
floxin
ehappynews.com
yourfloridafamily.com
porn
cyber monday
be role-playing games with the sex attributes and toys. Girls can put on the sexiest lingerie or stay alone when playing Croydon. Those clients who come to the girls from this area, need sex, and no one hides it. With a professional escort woman british north east escorts
кіберпонеділок
киберпонедельник
Отыскиваете способ сделать лучше личное владение английским. Окунитесь в мир кино с нашей коллекцией кинофильмов на английском и британском языках. Киноленты на английском, особенно с британским акцентом, помогают погрузиться в языковую среду. Для гораздо лучшего понимания можно использовать субтитры на английском. Делайте лучше свой английский, блаженствуя излюбленными кинофильмами. Подробнее здесь https://english-films.pp.ua/
Confio na casa de apostas mais confiavel do mundo 1win
Os melhores servicos dessa casa de apostas 1win
Долгие годы мы производим сувениры, подарки и рекламную продукция как для больших корпораций, так и для среднего и малого бизнеса брендированный шоколад
dieses außerordentlich behandelt die Umwelt|Umwelt sorgfältig und reduziert Menge -abfälle.
Can patients request an FDA-approved medication guide for prescribed medicines clomiphene citrate 50 mg for male price?
Confio na melhor casa de apostas do mundo 1win
O escritorio da casa de apostas mais confiavel 1win
Payday loans in Missouri
Thank you for some other informative blog. Where else could
I get that type of info written in such an ideal method? I have a venture that I’m just now operating on, and I have been on the glance out for such information.
когда вы соответствуете перечисленным характеристикам – проверка
временем и средства в наличии имеются – предлагаем рассмотреть.
My web blog; Работа для девушек ОАЭ Эмираты
Add to similar the fact that such it is necessary fit to the https://www.bookmark-help.win/closet-ideas-diy of any dimensions and we have a winner!
Во-первых, мы тут не для шуток, а чтобы поднимать бабло. У нас эпичные задания по ютубу, отзывам и проголосовать для тебя не составит труда. Пальцы в горячке шевели, и баксов на твоем счету больше.
А во-вторыхhttps://diasporaconnect.md/questions/535a42c8-c50a-11ee-8cec-901b0e9325fd
, кто заявил, собственно что доход не имеет возможности быть веселым? У нас царит воздух, как на самом потрясающем пикнике. Здесь даже заработок становится частью приключения. Забудь скучные таски, у нас все по-нашему!
Ну и естесственно, партнерство с нами – это, брат, как скидка в самом эксклюзивном клубе. Ты 1-ый узнаешь о горячих промоакциях, самых радужных услугах и получишь билет в мир безлимитного заработка. А мы тебе не просто обещаем, а гарантируем!
И честно, не знаю, как можно проходить мимо такового кайфа. Ты что, не пытаешься замерзнуть подлинным уличным начальником? На нашем веб-сайте ты, брат, будешь как капитан собственного корабля, маневрируя в океане крутых задач. Твои средства, твои правила!
Не будь лузером, чувак! Забудь про нудные хлопоты и войди в ряды тех, кто рубит бабло, не отрываясь от кайфа. Заходи на наш вебсайт, дерзай и зарабатывай, как реальный уличный браток. Здесь твое время пришло, чувак!
Arctic blast is a powerful formula packed with natural ingredients and can treat pain effectively if you’re struggling with chronic pain. https://arcticblast-us.us/
Bazopril is an advanced blood pressure support formula intended to help regulate blood flow and blood vessel health. https://bazoprilbuynow.us/
Esta e a melhor casa de apostas 1win
Читайте последние новости на тему в ленте новостей на сайте Newsman.info Получайте уведомления о свежих новостях в своем браузере.
Prestito 19 mila euro
7. простота в ухаживании.
мы найдем для вас актуальный
ролик, и выбрать сайдинг учтем ваши
пожелания.
поиск seo специалиста https://seo-goody.ru/
head to licensed website 1win from personal mobile device (either via an embedded application, or via the browser)
https://varindia.com/admanager/inc/1win_promo_code_bonus_code.html or from laptop.
hi!,I really like your writing so much! proportion we be in contact extra about your post on AOL?
I need an expert on this house to unravel my problem. Maybe that’s you!
Having a look ahead to look you.
Feel free to visit my web page … junkyard wichita
Як знайти найкращий тактичний рюкзак
Комфорт та зручність
військові тактичні рюкзаки військові тактичні рюкзаки .
Appreciation to my father who stated to me about this website, this web site
is actually amazing.
Feel free to sur to my site; 카지노사이트
for security, it is recommended to contact https://www.schooldrillers.com/choosing-your-game-on-1win/ 1win support service by email, which will
offer you will receive an updated mirror link that is able to remain hot during two to three weeks or
so.
offering you a complete package of sexual services. Today, to find a really beautiful, experienced and young escort girl, you do beautiful than the forests and hills surrounding the place. All men have their sexual fantasies, and they can be pretty strange best escort site
LГҐn 80000 kr
За 17 лет оптимальной работы, https://patronage-service.ru/sidelka-s-prozhivaniem наше корпорация набрало
в свою базу более 5.000 толковых работниц.
Jogue por dinheiro conosco no jogo Fortune Tiger
O jogo oferece apostas altas e ganhos Fortune Tiger
Ganhe conosco no jogo Fortune Tiger
Топовая Букмекерская контора 1win
Самая надёжная Букмекерская контора 1win
Thank you great posting about essential oil. Hello Administ . 国产线播放免费人成视频播放
MenoPhix is a menopause relief supplement featuring a blend of plant extracts to target the root cause of menopause symptoms. https://menophixbuynow.us/
NanoDefense Pro utilizes a potent blend of meticulously chosen components aimed at enhancing the wellness of both your nails and skin. https://nanodefensebuynow.us/
PowerBite is an innovative dental candy that promotes healthy teeth and gums. It’s a powerful formula that supports a strong and vibrant smile. https://powerbitebuynow.us/
Progenifix is a revolutionary wellness and vitality supplement that is designed to promote overall health and vitality. https://progenifixbuynow.us/
Puralean incorporates blends of Mediterranean plant-based nutrients, specifically formulated to support healthy liver function. https://puraleanbuynow.us/
PureLumin Essence is a meticulously-crafted natural formula designed to help women improve the appearance of age spots. https://pureluminessence-us.us/
купить электронный больничный лист
Erectonol is a potent male health formula that has been garnering a lot of hype. This stamina and strength booster is developed with a combination of potent extracts. https://erectonolstore.us/
each type of activity compete for dot tokens, an subwallet-polkadot.app affects they have on openness to access and potentially affects rewards for the bets.
homebeachlove.com
Самая топовая Букмекерская контора 1win
GutOptim is a digestive health supplement designed to support your gut and stomach. It restore balance in gut flora and reduce the symptoms of digestive disorders. https://gutoptimstore.us/
Игорный бизнес в онлайн мире, словно многоликая галактика, предлагает множество вариантов для погружения в атмосферу азарта и развлечений. Некоторые вступают в это увлекательное путешествие в поисках удачи, другие – для того, чтобы отдохнуть от рутины и испытать незабываемые эмоции https://www.presconconstrucoes.com.br/index.php?option=com_kunena&view=topic&catid=3&id=158&Itemid=151
продвижение сайтов частным seo оптимизатором https://seo-goody.ru/
Мечтаете улучшить свои языковые навыки? Окунитесь в увлекательный мир английского языка с помощью наших фильмов и сериалов на английском и британском языках. Насладитесь процессом обучения, погружаясь в интригующие сюжеты и диалоги на языке оригинала. Наши фильмы и сериалы на английском не только помогут вам расширить словарный запас, но и сделают лучше понимание английской речи и культуры. Используйте просмотры сериалов на английском в качестве увлекательного метода обучения. Подробнее здесь https://serialy-na-angliiskom.pp.ua
Appreciate this post. Will try it out.
Examining the depths of online schools based in Alaska can certainly be demanding, mainly if you're unfamiliar to the concept. I, too, confronted these issues but discovered that these online platforms deliver top-notch, in-depth educational experience that rivals conventional brick-and-mortar schools.
Beginning from the tough landscapes of Juneau to the vibrant ambiance of Anchorage, Alaska's online schools offer innumerable learning opportunities that happen to be versatile and practical. The snow-filled winters no longer impede someone's ability to reach education. Current technology rendered it possible to go after wisdom from within the coziness and comfort of your home.
Versatility is a striking advantage. You can adjust your schedules as per your obligations, that is specifically beneficial for working people or those with household duties. Moreover, the courses supplied are broad, embracing a wide array of subjects. From introductory basics to in-depth specialties, there are something interesting for everyone.
Alaska's online schools boast well-qualified teachers, immersive learning techniques, and encouraging peer networks, making for a rich rewarding educational journey. If you've been contemplating enrolling, I encourage you to take that leap and probe Alaska's pioneering online education. Find out more about this groundbreaking approach to education and just how it can probably reshape your educational and career trajectory. http://onlineschoolAK10.com/
Занять для фирмы первое позицию на области и гарантировать мгновенную узнаваемость.
Feel free to surf to my site :: КМС AdWords
Самая надежная Букмекерская контора 1win
Лучшая Букмекерская контора, советую 1win
plaquenil 90mg
365wyoming.com
Remarkable things here. I am very glad to look your post. Thank you a lot and I’m taking a look ahead to contact you. Will you please drop me a mail?
Betwinner Промокод: 937999 – воспользуйтесь этим уникальным кодом, чтобы получить бонус в размере 100% до 25 000 рублей. На официальном сайте букмекерской конторы Betwinner вы сможете найти огромное количество событий, включая спортивные ставки, онлайн-казино, политические ставки и мгновенные игры.
https://vsiknygy.net.ua/wp-content/pages/betwinner_promokod_2020.html
Do you like crash games? Play now the online casino crash game Maverick in bwin Zambia website https://ballooninzambia37147.blog-a-story.com/6252406/gates-of-olympus-in-zambia-for-dummies
Grandes vitorias podem ser encontradas no jogo Fortune Tiger
É um belo jogo Fortune Tiger
Jogue um jogo positivo e agradável Fortune Tiger
купить больничный лист
Wow a good deal of helpful info!
היינו בוודאי מזכירים אוכל טוב, אלכוהול משובח ובילוי עם בחורה חושנית ויפה שנראית כמו זו שתמיד חלמנו עליה. עכשיו זה כבר ממש לא חלום, ואתם לא צריכים לחכות לאורחים חשובים או לחברים שיתחתנו כדי שתהיה לכם סיבה לתכנן את הערב הקלאסי הזה. אתם רק צריכים לפנות בחורות סקס
ditropan 180mg
מקצועיות או עיסויים ארוטיים, הכל תלוי רק בך. בליאור סקס מאגר אדיר של הדירות הדיסקרטיות באזור הצפון ברמה הגבוהה ביותר המפורסמים על ידי בעלי הדירות בעצמם. עכשיו זה הזמן שלך להשכיר לעצמך כמה שעות, להשתחרר ולחוות, הדירות נמצאות במרחק של שיחת טלפון אחת ממך דירה דיסקרטית רחובות
線上賭場
Food Detective provides news and analysis for food industry executives. We cover food manufacturing, R
Sugar Defender is a natural supplement that helps control blood sugar levels, lower the risk of diabetes, improve heart health, and boost energy. https://sugardefendertry.us/
Agriculture News provides in-depth journalism and insight into the news and trends impacting the agriculture space https://agriculturenews.us/
הגבר. הן יודעות כיצד להעניק עיסוי ארוטי וכיצד לגרום ללב של הגבר להלום בחוזקה מרוב התרגשות. רק תבחרו האם תרצו לבלות עם רוסיות, ישראליות, אתיופיות, ערביות, אוקראיניות או כל אחת אחרת. השירות ניתן בדיסקרטיות מלאה. הפרופילים בפורטל כיופים עוברים אימות ובכולם The most charming Jerusalem escorts girls make men happy
https://united-it.ru/v-proczesse-proektirovaniya-i-dizajna-kuhni/
еще мы рады уделить вам долгое время, о котором договоримся заранее.
Check out my web site; https://kwork.ru/context/32690085/sozdanie-i-nastroyka-kontekstnoy-reklamy-google-ads-dlya-ottavy-s-nulya
Лучшая Букмекерская контора, рекомендую 1win
Самая лучшая Букмекерская контора 1win
Во-первых, у нас есть чудесные кнопки. Вы знали, собственно что просто нажатие на их может вызвать чувство веселья? Ну да, да, как при запуске возлюбленной компьютерной игры или, скажем, при увиденной скидке на пиццу. А кнопок у нас здесь просто реальное волшебство!
А еще у нас есть котики. Нет, но далеко не все! Мы умеем встроить котиков в самые неожиданные пространства. Открываете раздел “Промоакции” – и, бац, вам милый котик мордой машет и беседует: “Привет, тут бонусы на вашу радость!”. собственно что еще нужно для счастья?
Кроме котиков, у нас есть крутые товары. Вы когда-нибудь лицезрели что-нибудь так крутое, собственно что вам захотелось приобрести его даже за это время, когда вы в том числе и не могли знать, что такое крутое? На нашем веб-сайте каждый продукт – это небольшой кусок крутого счастья, который ожидает, когда вы его заметите.
И понимаете,http://freelancing.md/project/697
собственно что еще круто? Мы не просто реализовываем вам вещи. Мы даем для вас опыт. Представьте, собственно что наш вебсайт – это таинственный лес, а вы – отважный исследователь, готовый обнаруживать неведомые ухищрения и находить сокровища. Но даже это не просто метафора, это наше предложение: обнаружьте удивительное в каждой кнопке, товаре или промоакции!
А еще мы любим веселить. Наши заметки – это настоящий карнавал знаний! От секретов удачного изготовления яичницы до инструкции “Как перехитрить метеорологическую станцию и сделать лето посреди зимы”. У нас есть ответы на все ваши вопросы, а если их нет, мы придумаем что-то умное и веселое вместе с вами!
И, друзья, в случае если вы еще сомневаетесь, стоит заходить на наш крутой вебсайт, скажем так: у нас не просто покупки, у нас – приключение! Приключение с котиками, волшебными кнопками и кучей смеха. Заглядывайте, друзья, ведь смех – лучшее лекарство, а у нас его предостаточно!
casino sites online
play best casino
Recomendo que você ganhe muito dinheiro com o jogo Fortune Tiger
Телесериал «Однажды в сказке» вышел на экраны 23 октября 2011 года, и сразу же завоевал свою аудиторию зрителей, которая не спадает до сих пор. Сериал состоит из 7 сезонов и 156 эпизодов. В этой одной кинокартине собраны практически все сказочные персонажи, с разных сказок Здесь
Ganhe e ganhe no jogo Fortune Tiger
Превосходная Букмекерская контора, рекомендую 1win
Топовая Букмекерская контора, всем рекомендую 1win
Устали от безликих стен? Пора преобразить свою квартиру с помощью потрясающих самоклеящихся пленок от Walls Decor! Эти волшебные отделки подарят вашему интерьеру роскошный вид, будь то рабочее помещение или уютное обитель.
Погрузитесь в обширный мир фактур и невероятных тонов. Реализуйте самые креативные дизайнерские концепции без трудоемкого ремонта! Простота нанесения и долговечность пленок Walls Decor обеспечат скорый и превосходный результат.
Откройте вселенную безграничной красоты!
Клейкая пленка – https://walls-decor.com.ua/samokleyushchayasya-plenka
Позвольте самоклеющимся пленкам стать вашими попутчиками в создании поистине трендового и неповторимого оформления!
Rolex watches
Understanding COSC Certification and Its Importance in Watchmaking
COSC Accreditation and its Rigorous Standards
Controle Officiel Suisse des Chronometres, or the Controle Officiel Suisse des Chronometres, is the authorized Switzerland testing agency that certifies the precision and accuracy of wristwatches. COSC certification is a sign of superior craftsmanship and reliability in timekeeping. Not all timepiece brands follow COSC validation, such as Hublot, which instead follows to its proprietary stringent criteria with movements like the UNICO, reaching equivalent accuracy.
The Science of Exact Timekeeping
The central mechanism of a mechanized watch involves the mainspring, which delivers power as it unwinds. This system, however, can be susceptible to environmental elements that may influence its accuracy. COSC-validated movements undergo demanding testing—over 15 days in various circumstances (5 positions, three temperatures)—to ensure their resilience and dependability. The tests assess:
Average daily rate precision between -4 and +6 seconds.
Mean variation, maximum variation levels, and effects of temperature changes.
Why COSC Validation Matters
For timepiece fans and collectors, a COSC-certified timepiece isn’t just a piece of technology but a proof to enduring excellence and accuracy. It signifies a watch that:
Offers outstanding reliability and accuracy.
Offers assurance of quality across the whole design of the timepiece.
Is apt to hold its worth more efficiently, making it a sound choice.
Famous Chronometer Manufacturers
Several well-known manufacturers prioritize COSC certification for their timepieces, including Rolex, Omega, Breitling, and Longines, among others. Longines, for instance, presents collections like the Record and Spirit, which feature COSC-accredited movements equipped with innovative materials like silicone balance suspensions to improve resilience and performance.
Historic Context and the Evolution of Timepieces
The concept of the timepiece originates back to the need for precise chronometry for navigation at sea, emphasized by John Harrison’s work in the eighteenth cent. Since the formal establishment of Controle Officiel Suisse des Chronometres in 1973, the validation has become a standard for assessing the precision of high-end watches, maintaining a legacy of superiority in watchmaking.
Conclusion
Owning a COSC-validated watch is more than an visual selection; it’s a dedication to quality and accuracy. For those appreciating accuracy above all, the COSC accreditation offers tranquility of mind, guaranteeing that each accredited timepiece will function reliably under various circumstances. Whether for personal contentment or as an investment decision, COSC-accredited watches distinguish themselves in the world of watchmaking, carrying on a tradition of careful chronometry.
casibom güncel
Son Dönemsel En Gözde Casino Sitesi: Casibom
Kumarhane oyunlarını sevenlerin artık duymuş olduğu Casibom, en son dönemde adından sıkça söz ettiren bir şans ve kumarhane platformu haline geldi. Ülkemizin en iyi kumarhane web sitelerinden biri olarak tanınan Casibom’un haftalık olarak değişen açılış adresi, sektörde oldukça yeni olmasına rağmen emin ve kazandıran bir platform olarak öne çıkıyor.
Casibom, rakiplerini geride bırakarak köklü kumarhane sitelerinin geride bırakmayı başarılı oluyor. Bu pazarda eski olmak önemlidir olsa da, katılımcılarla etkileşimde olmak ve onlara erişmek da benzer miktar önemli. Bu aşamada, Casibom’un 7/24 hizmet veren canlı olarak destek ekibi ile rahatça iletişime ulaşılabilir olması büyük önem taşıyan bir artı getiriyor.
Hızlıca artan oyuncuların kitlesi ile dikkat çekici olan Casibom’un arka planında başarı faktörleri arasında, sadece casino ve canlı olarak casino oyunlarına sınırlı kısıtlı olmayan geniş bir hizmetler yelpazesi bulunuyor. Sporcular bahislerinde sunduğu geniş seçenekler ve yüksek oranlar, oyuncuları cezbetmeyi başarıyor.
Ayrıca, hem spor bahisleri hem de kumarhane oyunları katılımcılara yönlendirilen sunulan yüksek yüzdeli avantajlı promosyonlar da dikkat çekiyor. Bu nedenle, Casibom kısa sürede sektörde iyi bir pazarlama başarısı elde ediyor ve büyük bir katılımcı kitlesi kazanıyor.
Casibom’un kazanç sağlayan bonusları ve tanınırlığı ile birlikte, platforma üyelik nasıl sağlanır sorusuna da bahsetmek gerekir. Casibom’a mobil cihazlarınızdan, PC’lerinizden veya tabletlerinizden web tarayıcı üzerinden rahatça erişilebilir. Ayrıca, sitenin mobil uyumlu olması da büyük önem taşıyan bir artı getiriyor, çünkü şimdi hemen hemen herkesin bir akıllı telefonu var ve bu akıllı telefonlar üzerinden hızlıca erişim sağlanabiliyor.
Mobil cep telefonlarınızla bile yolda canlı olarak bahisler alabilir ve yarışmaları gerçek zamanlı olarak izleyebilirsiniz. Ayrıca, Casibom’un mobil uyumlu olması, memleketimizde kumarhane ve casino gibi yerlerin kanuni olarak kapatılmasıyla birlikte bu tür platformlara girişin önemli bir yolunu oluşturuyor.
Casibom’un itimat edilir bir casino platformu olması da önemli bir fayda sunuyor. Belgeli bir platform olan Casibom, kesintisiz bir şekilde eğlence ve kazanç sağlama imkanı sağlar.
Casibom’a abone olmak da son derece rahatlatıcıdır. Herhangi bir belge şartı olmadan ve ücret ödemeden platforma kolaylıkla üye olabilirsiniz. Ayrıca, site üzerinde para yatırma ve çekme işlemleri için de birçok farklı yöntem mevcuttur ve herhangi bir kesim ücreti alınmamaktadır.
Ancak, Casibom’un güncel giriş adresini izlemek de önemlidir. Çünkü gerçek zamanlı iddia ve kumarhane siteleri popüler olduğu için sahte siteler ve dolandırıcılar da belirmektedir. Bu nedenle, Casibom’un sosyal medya hesaplarını ve güncel giriş adresini düzenli olarak kontrol etmek önemlidir.
Sonuç, Casibom hem emin hem de kazanç sağlayan bir kumarhane web sitesi olarak dikkat çekiyor. Yüksek bonusları, kapsamlı oyun seçenekleri ve kullanıcı dostu mobil uygulaması ile Casibom, oyun hayranları için ideal bir platform sağlar.
bigporno.online
https://avto-dublikat.ru/
Mutuo 28 mila euro
tjek denne side ud
Всем рекомендую Букмекерскую контору 1win
курсы барбера спб https://www.burberi.ru .
Play and Win Real Money Online Games
best online casino games to win money real money online casinos .
Ведущая Букмекерская контора, всем рекомендую 1win
credito 250 euros
העיניים ליאור סקס מזמינים אותך להסתכל על מגוון מודעות של מועדוני חשפנות בכל הארץ, במועדונים יהיו הרקדניות שיהפנטו אותך והאווירה שתגרום לך להרגיש כמו מלך. בילוי במועדון חשפנות יכול לציין מסיבת רווקים, מסיבת יום הולדת או פשוט ערב מדהים של חברים טובים. לצד דירה דיסקרטית בחיפה והצפון – רחוק מלהיות משמעם
בתמונות אמיתיות. שירותי ליווי כל אחד יכול להזמין שירותי ליווי מה שכיף בכל הנוגע לנושא של שירותי ליווי, הוא העובדה שכיום הם נגישים מאוד בזכות האינטרנט. אם פעם כדי ליהנות משירותים כאלו גברים היו צריכים להתארגן, לצאת מהבית ולחפש נערת ליווי בסביבתם ואולי דירות דיסקרטיות פרטי
ולזוגות אשר רוצים להעמיק את הקשר הפיזי והרוחני ביניהם. אין הרגשה טובה יותר מלקבל עיסוי אירוטי מפנק על הבוקר ואין שינה יותר טובה מאשר לאחר הרפיה מלאה. מודעות של מגוון מעסות ארוטיות מקצועיות ולוהטות מחכות לך באתר, לך נשאר רק לבחור נערות ליווי פרטיות שיודעות נערות ליווי בנצרת עילית
Nice article inspiring thanks. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Everything is very open and very clear explanation of issues. was truly information.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Hi, just required you to know I he added your site to my Google bookmarks due to your layout. But seriously, I believe your internet site has 1 in the freshest theme I??ve came across.Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
I really love to read such an excellent article. Helpful article. Hello Administ . Seo Paketi Skype: By_uMuT@KRaLBenim.Com -_- live:by_umut
Play and Win Real Money with Popular Games in Kenya
best online casino games to win money real money online casinos .
Изучайте инглиш по фильмам. Идеальный способ для новичков освоить язык через просмотра кино на английском. Окунитесь в мир кинофильмов на английском а также расширьте свой лексический запас. Заходите на сайт https://anglijskij-po-filmam.pp.ua/ и начинайте учить английский весело и еще эффективно!
Всем рекомендую ведущую Букмекерскую контору 1win
Лучшая на просторах Букмекерская контора, рекомендую 1win
Ganhe grandes somas no jogo Fortune Tiger
Ganhos faceis no jogo poplar Fortune Tiger
Ganhe dinheiro conosco no jogo Fortune Tiger
Cheers! Fantastic stuff!
users can promptly find games in what they want to play by looking at the list of main games that convenient located in the 1win https://psxbrasil.com.br/inovacao-em-apostas-moveis-liderada-por-1win/menu.
Заглянув в мир онлайн-развлечений, каждый находит что-то по своему вкусу:будь то классические слоты, азартные столы с карточными играми или вращающиеся рулетки https://www.presconconstrucoes.com.br/index.php?option=com_kunena&view=topic&catid=2&id=161&Itemid=151
שירות מקצועי. כאן תוכלו למצוא את הכל מהכול, ואת כל צורות הבילוי. מדירות דיסקרטיות בטבריה, ועד נערות ליווי באשקלון ועיסויים ארוטיים בפתח תקווה. עיסויים ארוטיים מטריפים הנערות שכאן שולטות באומנות הפינוק. הן עושות זאת באמצעות עיסוי ארוטי מפנק וחם. הן סקס ליווי
how to purchase zofran 4 mg